Home — Essay Samples — Life — Healthy Lifestyle — My Health Beliefs and Behavior

My Health Beliefs and Behavior
- Categories: Healthy Lifestyle Self Assessment
About this sample

Words: 918 |
Published: Mar 3, 2020
Words: 918 | Pages: 2 | 5 min read
Table of contents
Introduction, works cited:.
- Craveri, M. (2002). The culture of the Europeans. University of Chicago Press.
- Di Napoli, R., & Paparcone, M. (2017). The Italian Cultural Experience: A journey through the arts, humanities, and everyday life. Routledge.
- Gennari, D. J. (2019). The joy of writing about Italian-American food. In Pizza, Pasta, and Cannoli: Italian-American Food (pp. 3-22). Bloomsbury Publishing USA.
- Giuffrè, L. (2017). School education in Italy: An overview. Italian Journal of Sociology of Education, 9(2), 41-55.
- Ilardo, J. (2013). Culture and customs of Italy. ABC-CLIO.
- Leaman, O. (Ed.). (2010). The future of philosophy. Wiley-Blackwell.
- Lillich, M. (2019). How to eat like an Italian. National Geographic.
- Nava, M. (2017). L’Italia del made in Italy. Società e politica, (2), 117-124.
- Scuderi, A. (2018). Family ties and migration decisions: Italy in comparison with Europe. European Journal of Population, 34(4), 491-511.
- UNESCO. (2019). Festivals in Italy. Retrieved from https://ich.unesco.org/en/lists.

Cite this Essay
Let us write you an essay from scratch
- 450+ experts on 30 subjects ready to help
- Custom essay delivered in as few as 3 hours
Get high-quality help

Verified writer
- Expert in: Life

+ 120 experts online
By clicking “Check Writers’ Offers”, you agree to our terms of service and privacy policy . We’ll occasionally send you promo and account related email
No need to pay just yet!
Related Essays
2 pages / 808 words
4 pages / 2182 words
1 pages / 558 words
3 pages / 1353 words
Remember! This is just a sample.
You can get your custom paper by one of our expert writers.
121 writers online
Still can’t find what you need?
Browse our vast selection of original essay samples, each expertly formatted and styled
Related Essays on Healthy Lifestyle
Games and amusements are critical for us. They keep us sound and fit. They offer us a change from the dullness of day by day life. It is a helpful methods for amusement and physical action. Games and recreations help in [...]
In this essay on the benefits of exercise, we will explore the multitude of advantages that regular physical activity can offer. Exercise is not merely a means to improve physical appearance; it is a powerful tool that can [...]
Virginian luxuries refer to the extravagant lifestyle and possessions of the wealthy elite in the colonial state of Virginia. During the 17th and 18th centuries, Virginia was a hub for the cultivation of tobacco, which brought [...]
Exercise is an essential component of a healthy lifestyle, and its benefits are well-documented. Engaging in regular physical activity has been shown to improve both physical and mental health, reduce the risk of chronic [...]
To have a generally healthy body, you should try to maintain a healthy weight. If you’re overweight, you are not maintaining a generally healthy body. Calories are a unit of measurement. You eat calories from food and that [...]
Currently, the world is facing an epidemic rise in Non-Communicable diseases like diabetes and high blood pressure. These diseases are caused in a part by the trend of rising in obesity which corresponds to the declining rate of [...]
Related Topics
By clicking “Send”, you agree to our Terms of service and Privacy statement . We will occasionally send you account related emails.
Where do you want us to send this sample?
By clicking “Continue”, you agree to our terms of service and privacy policy.
Be careful. This essay is not unique
This essay was donated by a student and is likely to have been used and submitted before
Download this Sample
Free samples may contain mistakes and not unique parts
Sorry, we could not paraphrase this essay. Our professional writers can rewrite it and get you a unique paper.
Please check your inbox.
We can write you a custom essay that will follow your exact instructions and meet the deadlines. Let's fix your grades together!
Get Your Personalized Essay in 3 Hours or Less!
We use cookies to personalyze your web-site experience. By continuing we’ll assume you board with our cookie policy .
- Instructions Followed To The Letter
- Deadlines Met At Every Stage
- Unique And Plagiarism Free
Health Behavior Theory
This essay about the psychological underpinnings of health behavior explores how various theories explain why people engage in health-promoting activities or avoid them. It discusses the Health Belief Model, which centers on personal beliefs about health risks and the perceived balance of benefits versus barriers to taking action. The Theory of Planned Behavior is also examined, emphasizing the importance of perceived control over health behaviors. Additionally, Social Cognitive Theory is highlighted for its focus on the interaction between individual behaviors, environmental factors, and personal factors like self-efficacy. Lastly, the essay considers the Transtheoretical Model, which outlines stages of change that individuals experience when modifying behaviors. Together, these theories provide a comprehensive framework for understanding and influencing health behaviors through targeted interventions that address both informational needs and psychological supports. This analysis underscores the complexity of health decision-making and the need for multifaceted approaches in health promotion and education.
How it works
The interplay of various psychological factors that drive our everyday health decisions forms a complex web that is crucial for developing targeted health interventions. This discussion explores diverse health behavior theories, which illuminate the underlying psychological mechanics that prompt individuals to embrace or avoid health-promoting behaviors.
One pivotal theory, the Health Belief Model (HBM), posits that personal beliefs about health problems, perceived benefits of action, and barriers to taking that action significantly influence health-related behavior. For example, someone might decide to start a fitness regimen if they believe that being overweight is seriously harmful to their health, that exercise would help them lose weight, and that they have access to a nearby gym that fits their budget.
On a slightly different note, the Theory of Planned Behavior (TPB) expands on this by incorporating the role of perceived control over the behavior. It suggests that health behaviors are not only a product of rational planning but also of the perceived ease or difficulty of performing the behavior. People will likely engage in a behavior such as quitting smoking if they feel they have sufficient resources and support to do so.
Social Cognitive Theory (SCT) introduces an interactive perspective, proposing that personal factors, environmental influences, and individual behaviors dynamically influence each other. Central to this theory is the concept of self-efficacy, or confidence in one’s ability to take action. For instance, a person’s confidence in their ability to exercise regularly can be influenced by past exercise achievements and the encouragement of friends or family.
Additionally, the Transtheoretical Model (TTM) offers a sequential view of behavior change, delineating five stages through which individuals typically progress when altering behavior, from being unprepared for change to maintaining new behaviors. This model is particularly useful in structuring health promotion programs to match the individual’s readiness to change, thus enhancing the likelihood of successful outcomes.
Each of these theories contributes to a broader understanding of health behaviors, emphasizing the need for a multi-faceted approach in health education and promotion. They remind us that health decisions are influenced by a mixture of beliefs, social pressures, environmental conditions, and personal confidence, all of which must be considered when designing public health initiatives.
Through these insights, it becomes clear that effective health behavior change interventions must address not only the informational needs of individuals but also the social and psychological supports necessary to empower action. This broader perspective helps public health professionals to design programs that are not only informative but also supportive of sustainable behavior change.
Cite this page
Health Behavior Theory. (2024, Apr 22). Retrieved from https://papersowl.com/examples/health-behavior-theory/
"Health Behavior Theory." PapersOwl.com , 22 Apr 2024, https://papersowl.com/examples/health-behavior-theory/
PapersOwl.com. (2024). Health Behavior Theory . [Online]. Available at: https://papersowl.com/examples/health-behavior-theory/ [Accessed: 18 Jul. 2024]
"Health Behavior Theory." PapersOwl.com, Apr 22, 2024. Accessed July 18, 2024. https://papersowl.com/examples/health-behavior-theory/
"Health Behavior Theory," PapersOwl.com , 22-Apr-2024. [Online]. Available: https://papersowl.com/examples/health-behavior-theory/. [Accessed: 18-Jul-2024]
PapersOwl.com. (2024). Health Behavior Theory . [Online]. Available at: https://papersowl.com/examples/health-behavior-theory/ [Accessed: 18-Jul-2024]
Don't let plagiarism ruin your grade
Hire a writer to get a unique paper crafted to your needs.

Our writers will help you fix any mistakes and get an A+!
Please check your inbox.
You can order an original essay written according to your instructions.
Trusted by over 1 million students worldwide
1. Tell Us Your Requirements
2. Pick your perfect writer
3. Get Your Paper and Pay
Hi! I'm Amy, your personal assistant!
Don't know where to start? Give me your paper requirements and I connect you to an academic expert.
short deadlines
100% Plagiarism-Free
Certified writers

Using these brief interventions, you can help your patients make healthy behavior changes.
STEPHANIE A. HOOKER, PHD, MPH, ANJOLI PUNJABI, PHARMD, MPH, KACEY JUSTESEN, MD, LUCAS BOYLE, MD, AND MICHELLE D. SHERMAN, PHD, ABPP
Fam Pract Manag. 2018;25(2):31-36
Author disclosures: no relevant financial affiliations disclosed.

Effectively encouraging patients to change their health behavior is a critical skill for primary care physicians. Modifiable health behaviors contribute to an estimated 40 percent of deaths in the United States. 1 Tobacco use, poor diet, physical inactivity, poor sleep, poor adherence to medication, and similar behaviors are prevalent and can diminish the quality and length of patients' lives. Research has found an inverse relationship between the risk of all-cause mortality and the number of healthy lifestyle behaviors a patient follows. 2
Family physicians regularly encounter patients who engage in unhealthy behaviors; evidence-based interventions may help patients succeed in making lasting changes. This article will describe brief, evidence-based techniques that family physicians can use to help patients make selected health behavior changes. (See “ Brief evidence-based interventions for health behavior change .”)
Modifiable health behaviors, such as poor diet or smoking, are significant contributors to poor outcomes.
Family physicians can use brief, evidence-based techniques to encourage patients to change their unhealthy behaviors.
Working with patients to develop health goals, eliminate barriers, and track their own behavior can be beneficial.
Interventions that target specific behaviors, such as prescribing physical activity for patients who don't get enough exercise or providing patient education for better medication adherence, can help patients to improve their health.
| SMART goal setting | Ensure that goals are specific, measurable, attainable, relevant, and timely. | |
| Problem-solving barriers | Identify possible barriers to change and develop solutions. | |
| Self-monitoring | Have patients keep a record of the behavior they are trying to change. | |
| Physical activity prescription | Collaboratively work with the patient to pick an activity type, amount, and frequency. | |
| Small changes | Have patients choose small, attainable goals to change their diets, such as reducing the frequency of desserts or soda intake or increasing daily fruit and vegetable consumption. | |
| Plate Method | Encourage patients to design their plates to include 50 percent fruits and vegetables, 25 percent lean protein, and 25 percent grains or starches. | |
| Brief behavioral therapy | After patients complete sleep diaries, use sleep restriction (reducing the amount of time in bed) and sleep scheduling (daily bed and wake-up times). | |
| Provide education | Instruct patients on drug therapy: indication, efficacy, safety, and convenience. | |
| Make medication routine | Add taking the medication to an existing habit to increase the likelihood patients will remember (e.g., use inhaler before brushing teeth). | |
| Engage social network | Close family members or friends can help fill pillboxes or remind patients to take their medications. | |
| Address the 5 Rs | Discuss the relevance to the patient, risks of smoking, rewards of quitting, roadblocks, and repeat the discussion. | |
| Set a quit date | Patients who set a quit date are more likely to stop smoking and remain abstinent. |
CROSS-BEHAVIOR TECHNIQUES
Although many interventions target specific behaviors, three techniques can be useful across a variety of behavioral change endeavors.
“SMART” goal setting . Goal setting is a key intervention for patients looking to make behavioral changes. 3 Helping patients visualize what they need to do to reach their goals may make it more likely that they will succeed. The acronym SMART can be used to guide patients through the goal-setting process:
Specific. Encourage patients to get as specific as possible about their goals. If patients want to be more active or lose weight, how active do they want to be and how much weight do they want to lose?
Measurable. Ensure that the goal is measurable. For how many minutes will they exercise and how many times a week?
Attainable. Make sure patients can reasonably reach their goals. If patients commit to going to the gym daily, how realistic is this goal given their schedule? What would be a more attainable goal?
Relevant. Ensure that the goal is relevant to the patient. Why does the person want to make this change? How will this change improve his or her life?
Timely. Help patients define a specific timeline for the goal. When do they want to reach their goal? When will you follow-up with them? Proximal, rather than distal, goals are preferred. Helping patients set a goal to lose five pounds in the next month may feel less overwhelming than a goal of losing 50 pounds in the next year.
Problem-solving barriers . Physicians may eagerly talk with patients about making changes — only to become disillusioned when patients do not follow through. Both physicians and patients may grow frustrated and less motivated to work on the problem. One way to prevent this common phenomenon and set patients up for success is to brainstorm possible obstacles to behavior change during visits.
After offering a suggestion or co-creating a plan, physicians can ask simple, respectful questions such as, “What might get in the way of your [insert behavior change]?” or “What might make it hard to [insert specific step]?” Physicians may anticipate some common barriers raised by patients but be surprised by others. Once the barriers are defined, the physician and patient can develop potential solutions, or if a particular barrier cannot be overcome, reevaluate or change the goal. This approach can improve clinical outcomes for numerous medical conditions and for patients of various income levels. 4
For example, a patient wanting to lose weight may commit to regular short walks around the block. Upon further discussion, the patient shares that the cold Minnesota winters and the violence in her neighborhood make walking in her area difficult. The physician and patient may consider other options such as walking around a local mall or walking with a family member instead. Anticipating every barrier may be impossible, and the problem-solving process may unfold over several sessions; however, exploring potential challenges during the initial goal setting can be helpful.
Self-monitoring . Another effective strategy for facilitating a variety of behavioral changes involves self-monitoring, defined as regularly tracking some specific element of behavior (e.g., minutes of exercise, number of cigarettes smoked) or a more distal outcome (e.g., weight). Having patients keep diaries of their behavior over a short period rather than asking them to remember it at a visit can provide more accurate and valuable data, as well as provide a baseline from which to track change.
When patients agree to self-monitor their behavior, physicians can increase the chance of success by discussing the specifics of the plan. For example, at what time of day will the patient log his or her behavior? How will the patient remember to observe and record the behavior? What will the patient write on the log? Logging the behavior soon after it occurs will provide the most accurate data. Although patients may be tempted to omit unhealthy behaviors or exaggerate healthy ones, physicians should encourage patients to be completely honest to maximize their records' usefulness. For self-monitoring to be most effective, physicians should ask patients to bring their tracking forms to follow-up visits, review them together, celebrate successes, discuss challenges, and co-create plans for next steps. (Several diary forms are available in the Patient Handouts section of the FPM Toolbox .)
A variety of digital tracking tools exist, including online programs, smart-phone apps, and smart-watch functions. Physicians can help patients select which method is most convenient for daily use. Most online programs can present data in charts or graphs, allowing patients and physicians to easily track change over time. SuperTracker , a free online program created by the U.S. Department of Agriculture, helps patients track nutrition and physical activity plans, set goals, and work with a group leader or coach. Apps like Lose It! or MyFitnessPal can also help.
The process of consistently tracking one's behavior is sometimes an intervention itself, with patients often sharing that it created self-reflection and resulted in some changes. Research shows self-monitoring is effective across several health behaviors, especially using food intake monitoring to produce weight loss. 5
BEHAVIOR-SPECIFIC TECHNIQUES
The following evidence-based approaches can be useful in encouraging patients to adopt specific health behaviors.
Physical activity prescriptions . Many Americans do not engage in the recommended amounts of physical activity, which can affect their physical and psychological health. Physicians, however, rarely discuss physical activity with their patients. 6 Clinicians ought to act as guides and work with patients to develop personalized physical activity prescriptions, which have the potential to increase patients' activity levels. 7 These prescriptions should list creative options for exercise based on the patient's experiences, strengths, values, and goals and be adapted to a patient's condition and treatment goals over time. For example, a physician working with a patient who has asthma could prescribe tai chi to help the patient with breathing control as well as balance and anxiety.
In creating these prescriptions, physicians should help the patient recognize the personal benefits of physical activity; identify barriers to physical activity and how to overcome them; set small, achievable goals; and give patients the confidence to attempt their chosen activity. Physicians should also put the prescriptions in writing, give patients logs to track their activity, and ask them to bring those logs to follow-up appointments for further discussion and coaching. 8 More information about exercise prescriptions and sample forms are available online.
Healthy eating goals . Persuading patients to change their diets is daunting enough without unrealistic expectations and the constant bombardment of fad diets, cleanses, fasts, and other food trends that often leave both patients and physicians uncertain about which food options are actually healthy. Moreover, physicians in training receive little instruction on what constitutes sound eating advice and ideal nutrition. 9 This confusion can prevent physicians from broaching the topic with patients. Even if they identify healthy options, common setbacks can leave both patients and physicians less motivated to readdress the issue. However, physicians can help patients set realistic healthy eating goals using two simple methods:
Small steps. Studies have shown that one way to combat the inertia of unhealthy eating is to help patients commit to small, actionable, and measurable steps. 10 First, ask the patient what small change he or she would like to make — for example, decrease the number of desserts per week by one, eat one more fruit or vegetable serving per day, or swap one fast food meal per week with a homemade sandwich or salad. 11 Agree on these small changes to empower patients to take control of their diets.
The Plate Method. This model of meal design encourages patients to visualize their plates split into the following components: 50 percent fruits and non-starchy vegetables, 25 percent protein, and 25 percent grains or starchy foods. 12 Discuss healthy options that would fit in each of the categories, or combine this method with the small steps described above. By providing a standard approach that patients can adapt to many forms of cuisine, the model helps physicians empower their patients to assess their food options and adopt healthy eating behaviors.
Brief behavioral therapy for insomnia . Many adults struggle with insufficient or unrestful sleep, and approximately 18.8 percent of adults in the United States meet the criteria for an insomnia disorder. 13 The first-line treatment for insomnia is Cognitive Behavioral Therapy for Insomnia (CBT-I), which involves changing patients' behaviors and thoughts related to their sleep and is delivered by a trained mental health professional. A physician in a clinic visit can easily administer shorter versions of CBT-I, such as Brief Behavioral Therapy for Insomnia (BBT-I). 14 BBT-I is a structured therapy that includes restricting the amount of time spent in bed but not asleep and maintaining a regular sleep schedule from night to night. Here's how it works:
Sleep diary. Have patients maintain a sleep diary for two weeks before starting the treatment. Patients should track when they got in bed, how long it took to fall asleep, how frequently they woke up and for how long, what time they woke up for the day, and what time they got out of bed. Many different sleep diaries exist, but the American Academy of Sleep Medicine's version is especially user-friendly.
Education. In the next clinic appointment, briefly explain how the body regulates sleep. This includes the sleep drive (how the pressure to sleep is based on how long the person has been awake) and circadian rhythms (the 24-hour biological clock that regulates the sleep-wake cycle).
Set a wake-up time. Have patients pick a wake-up time that will work for them every day. Encourage them to set an alarm for that time and get up at that time every day, no matter how the previous night went.
Limit “total time in bed.” Review the patient's sleep diary and calculate the average number of hours per night the patient slept in the past two weeks. Add 30 minutes to that average and explain that the patient should be in bed only for that amount of time per night until your next appointment.
Set a target bedtime. Subtract the total time in bed from the chosen wake-up time, and encourage patients to go to bed at that “target” time only if they are sleepy and definitely not any earlier.
For example, if a patient brings in a sleep diary with an average of six hours of sleep per night for the past two weeks, her recommended total time in bed will be 6.5 hours. If she picks a wake-up time of 7 a.m., her target bedtime would be 12:30 a.m. It usually takes up to three weeks of regular sleep scheduling and sleep restriction for patients to start seeing improvements in their sleep. As patients' sleep routines become more solid (i.e., they are falling asleep quickly and sleeping more than 90 percent of the time they are in bed), slowly increase the total time in bed to possibly increase time asleep. Physicians should encourage patients to increase time in bed in increments of 15 to 30 minutes per week until the ideal amount of sleep is reached. This amount is different for each patient, but patients generally have reached their ideal amount of sleep when they are sleeping more than 85 percent of the time in bed and feel rested during the day.
Patient education to prevent medication nonadherence . Medication adherence can be challenging for many patients. In fact, approximately 20 percent to 30 percent of prescriptions are never picked up from the pharmacy, and 50 percent of medications for chronic diseases are not taken as prescribed. 15 Nonadherence is associated with poor therapeutic outcomes, further progression of disease, and decreased quality of life. To help patients improve medication adherence, physicians must determine the reason for nonadherence. The most common reasons are forgetfulness, fear of side effects, high drug costs, and a perceived lack of efficacy. To help patients change these beliefs, physicians can take several steps:
Educate patients on four key aspects of drug therapy — the reason for taking it (indication), what they should expect (efficacy), side effects and interactions (safety), and how it structurally and financially fits into their lifestyle (convenience). 16
Help patients make taking their medication a routine of their daily life. For example, if a patient needs to use a controller inhaler twice daily, recommend using the inhaler before brushing his or her teeth each morning and night. Ask patients to describe their day, including morning routines, work hours, and other responsibilities to find optimal opportunities to integrate this new behavior.
Ask patients, “Who can help you manage your medications?” Social networks, including family members or close friends, can help patients set up pillboxes or provide medication reminders.
The five Rs to quitting smoking . Despite the well-known consequences of smoking and nationwide efforts to reduce smoking rates, approximately 15 percent of U.S. adults still smoke cigarettes. 17 As with all kinds of behavioral change, patients present in different stages of readiness to quit smoking. Motivational interviewing techniques can be useful to explore a patient's ambivalence in a way that respects his or her autonomy and bolsters self-efficacy. Discussing the five Rs is a helpful approach for exploring ambivalence with patients: 18
Relevance. Explore why quitting smoking is personally relevant to the patient.
Risks. Advise the patient on negative consequences of continuing to smoke.
Rewards. Ask the patient to identify the benefits of quitting smoking.
Roadblocks. Help the patient determine obstacles he or she may face when quitting. Common barriers include weight gain, stress, fear of withdrawal, fear of failure, and having other smokers such as coworkers or family in close proximity.
Repeat. Incorporate these aspects into each clinical contact with the patient.
Many patients opt to cut back on the amount of tobacco they use before their quit date. However, research shows that cutting back on the number of cigarettes is no more effective than quitting abruptly, and setting a quit date is associated with greater long-term success. 19
Once the patient sets a quit date, repeated physician contact to reinforce smoking cessation messages is key. Physicians, care coordinators, or clinical staff should consider calling or seeing the patient within one to three days of the quit date to encourage continued efforts to quit, as this time period has the highest risk for relapse. Evidence shows that contacting the patient four or more times increases the success rate in staying abstinent. 18 Quitting for good may take multiple a empts, but continued encouragement and efforts such as setting new quit dates or offering other pharmacologic and behavioral therapies can be helpful.
GETTING STARTED
Family physicians are uniquely positioned to provide encouragement and evidence-based advice to patients to change unhealthy behaviors. The proven techniques described in this article are brief enough to attempt during clinic visits. They can be used to encourage physical activity, healthy eating, better sleep, medication adherence, and smoking cessation, and they can help patients adjust their lifestyle, improve their quality of life, and, ultimately, lower their risk of early mortality.
Loef M, Walach H. The combined effects of healthy lifestyle behaviors on all-cause mortality: a systematic review and meta-analysis. Prev Med . 2012;55(3):163-170.
Bodenheimer T, Handley MA. Goal-setting for behavior change in primary care: an exploration and status report. Patient Educ Couns . 2009;76(2):174-180.
Lilly CL, Bryant LL, Leary JM, et al.; Evaluation of the effectiveness of a problem-solving intervention addressing barriers to cardiovascular disease prevention behaviors in three underserved populations: Colorado, North Carolina, West Virginia, 2009. Prev Chronic Dis . 2014;11:E32.
U.S. Department of Agriculture and U.S. Department of Health and Human Services. Dietary Guidelines for Americans (7th Ed). Washington, D.C: U.S. Government Printing Office; 2010.
Sreedhara M, Silfee VJ, Rosal MC, Waring ME, Lemon SC. Does provider advice to increase physical activity differ by activity level among U.S. adults with cardiovascular disease risk factors? Fam Pract . 2018;35(4):420-425.
Pinto BM, Lynn H, Marcus BH, DePue J, Goldstein MG. Physician-based activity counseling: intervention effects on mediators of motivational readiness for physical activity. Ann Behav Med . 2001;23(1):2-10.
Hechanova RL, Wegler JL, Forest CP. Exercise: a vitally important prescription. JAAPA . 2017;30(4):17-22.
Guo H, Pavek M, Loth K. Management of childhood obesity and overweight in primary care visits: gaps between recommended care and typical practice. Curr Nutr Rep . 2017;6(4):307-314.
Perkins-Porras L, Cappuccio FP, Rink E, Hilton S, McKay C, Steptoe A. Does the effect of behavioral counseling on fruit and vegetable intake vary with stage of readiness to change?. Prev Med . 2005;40(3):314-320.
Kahan S, Manson JE. Nutrition counseling in clinical practice: how clinicians can do better. JAMA . 2017;318(12):1101-1102.
Choose My Plate. U.S. Department of Agriculture website. https://www.choosemyplate.gov/ . Updated January 31, 2018. Accessed February 1, 2018.
Ford ES, Cunningham TJ, Giles WH, Croff JB. Trends in insomnia and excessive daytime sleepiness among U.S. adults from 2002 to 2012. Sleep Med . 2015;16(3):372-378.
Edinger JD, Sampson WS. A primary care “friendly” cognitive behavioral insomnia therapy. Sleep . 2003;26(2):177-182.
Viswanathan M, Golin CE, Jones CD, et al.; Interventions to improve adherence to self-administered medications for chronic diseases in the United States: a systematic review. Ann Intern Med . 2012;157(11):785-795.
Cipolle RJ, Strand LM, Morley PC. Pharmaceutical care practice: the patient-centered approach to medication management services . 3rd ed. New York: McGraw-Hill; 2012.
Jamal A, King BA, Neff LJ, Whitmill J, Babb SD, Graffunder CM. Current cigarette smoking among adults — United States, 2005–2015. MMWR Morb Mortal Wkly Rep . 2016;65(44):1205-1211.
Patients not ready to make a quit attempt now (the “5 Rs”). Agency for Healthcare Research and Quality website. http://bit.ly/2jVvpoY . Updated December 2012. Accessed February 2, 2018.
Larzelere MM, Williams DE. Promoting smoking cessation. Am Fam Physician . 2012;85(6):591-598.
Continue Reading
More in FPM
More in pubmed.
Copyright © 2018 by the American Academy of Family Physicians.
This content is owned by the AAFP. A person viewing it online may make one printout of the material and may use that printout only for his or her personal, non-commercial reference. This material may not otherwise be downloaded, copied, printed, stored, transmitted or reproduced in any medium, whether now known or later invented, except as authorized in writing by the AAFP. See permissions for copyright questions and/or permission requests.
Copyright © 2024 American Academy of Family Physicians. All Rights Reserved.

An official website of the United States government
Here's how you know
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
Adopting healthy habits: What do we know about the science of behavior change?
Behavioral & Social Research Longevity
For many people, living a long, healthy life can be attributed to adopting and maintaining healthy behaviors. NIA-funded researchers are looking at mechanisms that can help make behavioral interventions more successful for everyone.
On this page:
Understanding behavioral interventions
Studying mechanisms of behavior change, self-regulation: modifying or controlling your own behavior, stress reactivity and the role of coping in behavior change, social support: improving health behavior through social connections, tips to help sustain behavior change, what’s next in research.
Adopting and maintaining healthy behaviors increases the chances of living a long, healthy life, and engaging in unhealthy behaviors can have the opposite effect. Seven out of 10 deaths in the United States are the result of chronic diseases, which for many people can be prevented by eating well, staying physically active, avoiding tobacco use and excessive drinking, and getting regular health screenings. But simply knowing these facts isn’t enough to motivate most people to adopt long-lasting behavior change. Why is that?
If you’ve ever tried to start a new exercise routine or eat healthier, you may have found it was more challenging to keep up with than you anticipated. According to Donald Edmondson, Ph.D. , principal investigator of the Resource and Coordinating Center for the NIH Science of Behavior Change (SOBC) program, “Keeping behavior changes long enough to experience the benefits is incredibly hard.”
Behavior change requires letting go of old habits and adopting new ones, which is not always easy. However, what makes behavior change challenging for one person likely won’t be the same for someone else. Whether or not a person can maintain behavior change over time relies on different factors, too. For example, a person’s environment, workplace, and home life can make behavior change more or less likely to be successful.
Over the years, scientists have identified tactics for adopting healthier behaviors, such as wearing a watch to track your steps or keeping healthier foods in the home. However, these interventions don’t seem to work for everyone. Even when an approach is effective, the underlying mechanisms — why and how it works — often aren’t clear. Understanding these mechanisms could be the key to achieving effective and long-term behavior change for many people.
A behavioral intervention is an intentional change in the way you do something, such as eating healthier foods or exercising regularly, that is designed to make you healthier. In general, behavioral interventions use different ways of thinking, feeling, acting, or relating with others to stimulate a change in a person’s behavior to promote their health and well-being. For example, a behavioral intervention could be aimed at modifying something about a person’s living environment or diet, with the goal of improving their health.
It seems straightforward to assume that if someone wears a pedometer and adds 30 minutes of exercise to their day, they’re likely to notice changes in their body and overall health. The problem, however, is that even if this intervention is effective, we don’t fully understand how or why it worked for this individual. Did they set goals for daily step counts and enjoy the challenge of improving over time? Did the pedometer show them how sedentary they are normally, causing them to feel embarrassed?
If we don’t understand how an intervention worked, then we will not know if it will work for another person. And if several possible interventions are options, we will not know which one will work best for a specific individual. Learning more about the many underlying influences on behavior change can help researchers and health care professionals develop and provide more effective interventions.
Researchers involved in the SOBC Research Network — including scientists from NIA — are dedicated to discovering what underlies successful behavior change. The ultimate goal is to develop effective interventions that work consistently. Janine Simmons, Ph.D., chief of the Individual Behavioral Processes Branch in the NIA Division of Behavioral and Social Research, works closely with the SOBC program.
“Through the SOBC initiative, we are moving behavioral intervention research forward via an experimental medicine approach designed to identify the key mechanisms underlying changes in behavior,” Simmons said. “Investigators can use this approach to design experiments that answer questions about how and why a given intervention might, or might not, elicit positive health behavior change.”
How does the experimental medicine method work? Researchers first identify an underlying mechanism that may drive a certain behavior. They then develop tools to measure that mechanism and test potential interventions to change it. In the example of the pedometer, the mechanism driving behavior change might be “awareness of steps.” The researchers would first measure awareness, and then test an intervention like wearing a pedometer daily.

If the person’s behavior changes (in this case, they increase their physical activity), the researchers would need to determine whether the change resulted from the mechanism (increased awareness of steps). Then, they can be confident that the mechanism is an effective target for behavior change interventions.
Additionally, knowing which interventions worked in one area could allow for them to be adapted and applied to many other areas.
“The SOBC program is about connecting basic scientists and scientists from different subfields of behavioral psychological work. It’s important to be able to leverage years of work in a basic behavioral lab to help intervention scientists to rapidly build successful behavioral change interventions — or report failures back to the basic lab for further research,” said Edmondson.
To date, SOBC researchers have identified three broad domains that show promise as potentially powerful mechanisms of behavior change: self-regulation, stress reactivity and coping, and social support.
Self-regulation has been studied widely for years. It refers to the extent to which people are able to monitor and control their own behaviors, thoughts, and feelings to achieve their goals.
One example of a self-regulation mechanism is called “delay discounting.” Every day, individuals must make trade-offs between short-term and long-term benefits. For example, do I want to relax and watch TV or go for a run to help improve my future cardiovascular health? Delay discounting, also known as “temporal discounting,” is a way to quantify how much an individual weighs smaller, short-term rewards (relaxing watching TV) versus larger, long-term rewards (cardiovascular fitness is a major factor in how long we live and the quality of our lives). A person with a high “discounting rate” places lower value on rewards that occur in the future, and a correspondingly higher value on rewards they will experience right away, because they “discount” the future rewards more steeply. Discounting the future can make a lot of sense when quick action is needed; however, there may be a downside when it comes to choosing and maintaining healthy behaviors over time.
Researchers are exploring the concept of delay discounting as a mechanism for improving health behavior. Research shows that the extent to which individuals discount the value of delayed rewards may be associated with important health- and disease-related outcomes — essentially, the more highly people value immediate, less healthy rewards, the more unhealthy or problematic decisions they make. If scientists could design interventions to help people recognize and better appreciate the value of long-term rewards, they could help us make better, healthier decisions in the moment.
A recent review considered 98 studies that tested different behavioral interventions to help reduce delay discounting. The review found that several interventions led to improved decision-making. Among the most promising avenues to reduce delay discounting are acceptance- and mindfulness-based trainings. These approaches focus on experiencing and accepting the present moment, even when it’s uncomfortable. However, the authors of the review noted that the success of many behavioral interventions appears to be short-lived. And their effectiveness is often dependent on the context in which they’re delivered — in other words, they won’t work for everyone or in every situation.
A related intervention that may improve delay discounting is simply asking people to vividly imagine or simulate experiences that might happen in their future, like playing with their grandchildren or the day of their retirement. This approach is known as episodic future thinking.
“What we’ve found is that this type of thinking shifts how much [a person] values future things relative to the present state, so it’s sort of like opening the cognitive window to the future, where long-term benefits will be extremely valuable,” said Edmondson.
How might episodic future thinking affect a person’s ability to maintain behavior change? If an intervention strengthens specific cognitive and neural mechanisms in the brain that support a more balanced valuing of the future and the present, then it may improve decision-making and self-regulation skills. An example of an intervention using episodic future thinking would be sending a person a text twice a day asking them to think about their ideal future for a few minutes. This intervention might lead them to make better short-term decisions in support of making that ideal future a reality.
There’s no question that everyone experiences stress, but how people cope with stressors can have a major impact on their health. An individual’s mental, emotional, and physical health can be affected both by external stressors, such as job loss or the death of a loved one, and by the subjective experience of stress — the internal feeling that one does not have the capacity to cope with life’s stressors. Uncontrolled stress can also lead to negative health outcomes, including high blood pressure and cardiovascular disease.
Individuals vary in their levels of stress reactivity; that is, their mental, emotional, and physical reactions to stress. These differences may help to explain why stress affects some people’s health behaviors more than others, even when they encounter the same stressor, such as the death of a loved one. What if we could minimize stress reactivity and increase the ability to cope and adapt under stressful situations? Would that make a difference in health outcomes?
One mechanism being studied in this area is anxiety sensitivity. Anxiety sensitivity refers to fears of anxiety-related sensations (such as stomach pain or racing thoughts) based on catastrophic beliefs about what those sensations mean. For example, anxiety sensitivity might lead someone with a feeling of chest tightening to worry that they’re having a heart attack. As a result, the person may avoid certain activities, such as physical exercise, that might produce that feeling. Or they may overeat or use alcohol to cope with the anxiety. In these ways, anxiety sensitivity can negatively affect a person’s health and well-being.
In fact, anxiety sensitivity is linked to some of the top preventable causes of disease and death in the U.S., including tobacco use, poor diet, physical inactivity, and alcohol overuse. It has also been linked to poor medication adherence, which happens when people don’t take their medicines in the right way or at the right time. Understanding the scope of these effects has clear public health significance.
A recent meta-analysis found that anxiety sensitivity and associated health outcomes, such as depression, insomnia, alcohol use, and pain, can be improved with brief behavioral interventions, for example, cognitive behavioral therapy, that target anxiety sensitivity. Another study looked at anxiety sensitivity as a possible mechanism linking exercise and smoking cessation. Specifically, the researchers wanted to find out whether physical exercise could help people with high anxiety sensitivity quit smoking successfully. The study found that participants who did high-intensity exercise were more likely to quit smoking than those who did not exercise, and that their success was related to having lower anxiety sensitivity
“We’re seeing some of these interventions improve people’s fear of their bodily reactions to anxiety,” said Edmondson. He added that scientists at the Columbia Roybal Center for Fearless Behavior Change are testing interventions “to determine whether reducing anxiety sensitivity leads to healthy behavior change — better medication adherence and better physical activity, which is really exciting.”
It has been recognized for decades that social networks influence behavior, and researchers are still learning how relationships shape an individual’s health behaviors. We know that many of our norms, expectations, and preferences come to us from our community and the people we spend time with. However, knowing where and how to intervene in a social network to optimize behavior change is still a challenge for scientists. At the most basic level, one way to extend the reach of a given behavioral intervention may be to adapt the intervention to take advantage of interpersonal relationships and the influence of others in a social network.

One study looked at the effects of social support and examined whether a weight loss program delivered to one spouse had beneficial effects on the spouse who didn’t participate. The study found that the untreated spouses — despite not participating in the weight loss program directly — lost a significant amount of weight. Although future research using the experimental medicine approach is required to identify the precise mechanism, the researchers suggested that spouses who directly received the intervention may have modeled health-promoting behaviors, such as weighing themselves regularly, for their spouses, and that they were less likely to have high-fat foods in the home during the program versus before. The findings of this research suggest that behavioral interventions for weight loss can create a “ripple effect” that benefits others, and that behavioral modeling and reduced access to high-fat foods are two potential mechanisms of behavior change to test in studies of these effects.
Another study analyzed data from more than 4,000 Americans aged 60 and older to help understand the connection between social relationships and health-related behaviors. Researchers found that social factors were associated with the likelihood of several different health-related behaviors, including alcohol use, smoking, physical activity, and visiting the dentist. The study showed that older adults with strong social ties, such as being married, living with a partner, or having a group of close friends, were more likely to engage in health-promoting behaviors than people with fewer social ties. These social relationships may benefit health in older adults by helping them cope with stress, providing emotional support, and encouraging them to adopt healthier behaviors.
What does this mean? If you’re looking to eat healthier or become more physically active, it may be worth asking your spouse or friend to do it with you.
“Researchers are beginning to examine how interactions within a social network have direct beneficial effects on health behaviors, and when we can leverage social networks to promote positive health behavior change,” said Simmons. “For example, after one partner stops smoking or starts exercising, the other is more likely to follow suit. The same pattern holds true for friends, siblings, and even co-workers."
Whether you want to become more physically active, lose weight, or start another new healthy activity, these tips — based on behavior change research — may be able to help you create and maintain successful new habits:
Practice envisioning the future. As you make decisions in everyday life, be aware of how your behavior may be driven by wanting what feels good now versus what your future self will wish you had valued.
Manage stress. Stress can affect your ability to adopt healthy behaviors, such as physical activity or healthy eating. If you feel stressed or overwhelmed, you may be less likely to exercise, which in turn can increase your stress levels the next day — creating an unhelpful cycle. Healthy activity and diet can reduce stress, both in the short and long term, so paying attention to how good you feel right after exercise may also help reduce your delay discounting.
Beware of avoidance. If you have a chronic condition, you may become hyper-aware of your body and start worrying that every sensation in your chest or change in your breathing rate signals catastrophe. Those anxieties about bodily sensations can become problematic not because they signal a cardiovascular event, but because they may become an excuse to avoid exercise or to eat comfort food. If you are medically cleared to exercise, it’s important to recognize that the bodily sensations associated with being active may be amplified by fear, but most do not indicate any real health problem.
There is still a lot to learn about behavior change interventions and how they work. Scientists continue to explore these areas to help people better adopt and maintain healthy behaviors. Currently, NIH-funded researchers are investigating how an experimental medicine approach to behavior change could have an impact in two specific areas: reproductive health and willingness to receive a COVID-19 vaccine . Their innovative approach offers new opportunities to improve the health of individuals and communities.
It's important for everyone to understand the importance and benefits of adopting and maintaining healthy behaviors — including the researchers studying them, your health care providers, your family, and yourself.
Behavior change is fundamental to human health at any age. It is critically important for NIA to support research in this area because NIA’s mission encompasses the full adult lifespan, and many of the health choices we make earlier in life directly affect the likelihood of avoiding illnesses and maintaining wellness as we age.
nia.nih.gov
An official website of the National Institutes of Health
- Bipolar Disorder
- Therapy Center
- When To See a Therapist
- Types of Therapy
- Best Online Therapy
- Best Couples Therapy
- Best Family Therapy
- Managing Stress
- Sleep and Dreaming
- Understanding Emotions
- Self-Improvement
- Healthy Relationships
- Student Resources
- Personality Types
- Guided Meditations
- Verywell Mind Insights
- 2024 Verywell Mind 25
- Mental Health in the Classroom
- Editorial Process
- Meet Our Review Board
- Crisis Support
Studying Health Psychology and Illness
Kendra Cherry, MS, is a psychosocial rehabilitation specialist, psychology educator, and author of the "Everything Psychology Book."
:max_bytes(150000):strip_icc():format(webp)/IMG_9791-89504ab694d54b66bbd72cb84ffb860e.jpg)
Steven Gans, MD is board-certified in psychiatry and is an active supervisor, teacher, and mentor at Massachusetts General Hospital.
:max_bytes(150000):strip_icc():format(webp)/steven-gans-1000-51582b7f23b6462f8713961deb74959f.jpg)
- Current Issues
- Biosocial Model
- In Practice
Health psychology is a specialty area that focuses on how biology, psychology, behavior, and social factors influence health and illness. Other terms such as medical psychology and behavioral medicine are sometimes used interchangeably with the term health psychology.
Health and illness are influenced by a wide variety of factors. While contagious and hereditary illnesses are common, many behavioral and psychological factors can impact overall physical well-being and various medical conditions.
An Overview of Health Psychology
Health psychology is a field of psychology focused on promoting health as well as the prevention and treatment of disease and illness. Health psychologists also focus on understanding how people react to, cope with, and recover from illness. Some health psychologists work to improve the health care system and the government's approach to health care policy.
Division 38 of the American Psychological Association is devoted to health psychology. According to the division, their focus is on a better understanding of health and illness, studying the psychological factors that impact health, and contributing to the health care system and health policy.
The field of health psychology emerged in the 1970s to address the rapidly changing field of healthcare. Today, life expectancy in the U.S. is around 80 years, and the leading causes of mortality are chronic diseases often linked to lifestyle. Health psychology helps address these changes in health.
By looking at the patterns of behavior that underlie disease and death, health psychologists hope to help people live better, and healthier, lives.
How Is Health Psychology Unique?
Because health psychology emphasizes how behavior influences health, it is well-positioned to help people change the behaviors that contribute to health and well-being. Examples of health psychology in action would be researchers conducting applied research on how to prevent unhealthy behaviors such as smoking or to find new ways to encourage healthy actions such as exercising.
For example, while most people realize that eating a diet high in sugar is not good for their health, many people continue to engage in such behaviors regardless of the possible short-term and long-term consequences. Health psychologists look at the psychological factors that influence these health choices and explore ways to motivate people to make better health choices.
Importance of Health Psychology
The U.S. Centers for Disease Control's National Center for Health Statistics compiles data regarding death in the nation and its causes. Congruent with data trends throughout this century, nearly half of all deaths in the United States can be linked to behaviors or other risk factors that are mostly preventable.
In the CDC's 2012 report, the rate of death had declined for all leading causes except suicide. Life expectancy was also at an all-time high (78.8 years), yet about 83 Americans die from heart disease and stroke every hour. And more than a quarter of those deaths are preventable.
Cancer deaths were second, followed by chronic lower respiratory diseases—primarily chronic obstructive pulmonary diseases (COPD) such as emphysema and chronic bronchitis. COPD was followed by drug poisonings, including overdoses , then fatal falls among an increasingly elder population.
Current Issues in Health Psychology
Health psychologists work with individuals, groups, and communities to decrease risk factors, improve overall health, and reduce illness. They conduct research and provide services in areas including:
- Stress reduction
- Weight management
- Smoking cessation
- Improving daily nutrition
- Reducing risky sexual behaviors
- Hospice care and grief counseling
- Preventing illness
- Understanding the effects of illness
- Improving recovery
- Teaching coping skills
The Biosocial Model in Health Psychology
Today, the main approach used in health psychology is known as the biosocial model. According to this view, illness and health are the results of a combination of biological, psychological, and social factors.
- Biological factors include inherited personality traits and genetic conditions.
- Psychological factors involve lifestyle, personality characteristics, and stress levels.
- Social factors include such things as social support systems , family relationships, and cultural beliefs.
Health Psychology in Practice
Health psychology is a rapidly growing field. As increasing numbers of people seek to take control of their own health, more and more people are seeking health-related information and resources. Health psychologists are focused on educating people about their own health and well-being, so they are perfectly suited to fill this rising demand.
Many health psychologists work specifically in the area of prevention, focusing on helping people stop health problems before they start.
This may include helping people maintain a healthy weight, avoid unhealthy or risky behaviors , and maintain a positive outlook that can combat stress, depression, and anxiety.
Another way that health psychologists can help is by educating and training other health professionals. By incorporating knowledge from health psychology, physicians, nurses, nutritionists, and other health practitioners can better incorporate psychological approaches into how they treat patients.
Branches of Health Psychology
Individuals who are interested in a health psychology career can choose to work in a specific branch of this field. Four main branches of health psychology are:
- Clinical health psychology : This health psychology branch involves working with individuals, helping them make lifestyle changes for better health.
- Community health psychology : Health psychology workers can also work with entire communities, such as studying diseases that are common in certain communities and the causes behind them.
- Occupational health psychology : This branch of health psychology focuses on how a person's job can affect their health, in addition to finding ways to promote employee health within work environments.
- Public health psychology : Another option for health psychology professionals is to work in a position that studies and/or is able to influence policies and programs designed to promote the health of the public as a whole.
A Word From Verywell
If you are struggling to make healthy changes in your life , dealing with the onset of illness, or facing some other type of health problem, seeing a health psychologist is one way to help start you off on the right foot. By consulting with one of these professionals, you can gain access to support and resources designed to help you cope with your illness and achieve your health goals.
American Psychological Association. Society for Health Psychology .
Centers for Disease Control and Prevention. Mortality in the United States, 2017 .
DeStasio KL, Clithero JA, Berkman ET. Neuroeconomics, health psychology, and the interdisciplinary study of preventative health behavior . Soc Personal Psychol Compass . 2019;13(10):e12500. doi:10.1111/spc3.12500
Centers for Disease Control and Prevention. CDC National Health Report Highlights .
Mason PH, Roy A, Spillane J, Singh P. Social, historical and cultural dimensions of tuberculosis . J Biosoc Sci . 2016;48(2):206–232. doi:10.1017/S0021932015000115
Baum A, Revenson TA, Singer JE. Handbook of Health Psychology. Second Edition . Psychology Press; 2012.
Brannon L, Updegraff JA, Feist J. Health Psychology: An Introduction to Behavior and Health . Cengage Learning; 2014.
By Kendra Cherry, MSEd Kendra Cherry, MS, is a psychosocial rehabilitation specialist, psychology educator, and author of the "Everything Psychology Book."
AI-Driven Behavior Change Could Transform Health Care

Huffington is the founder and CEO of Thrive Global
A staggering 129 million Americans have at least one major chronic disease—and 90% of our $4.1 trillion in annual health care spending goes toward treating these physical and mental-health conditions. That financial and personal toll is only projected to grow .
We know this is unsustainable. But there are solutions, because health outcomes are shaped by more than just medical care or genes. Behavior change can be a miracle drug, both for preventing disease and for optimizing the treatment of disease.
Yes, behavior change is hard. But through hyper-personalization, it’s also something that AI is uniquely positioned to solve.
AI is already greatly accelerating the rate of scientific progress in medicine—offering breakthroughs in drug development, diagnoses, and increasing the rate of scientific progress around diseases like cancer. In fact, OpenAI is partnering with Color Health on an AI copilot to assist doctors in cancer screening and in creating treatment plans after a doctor has made a diagnosis.
But humans are more than medical profiles. Every aspect of our health is deeply influenced by the five foundational daily behaviors of sleep, food, movement, stress management, and social connection. And AI, by using the power of hyper-personalization, can significantly improve these behaviors.
These are the ideas behind Thrive AI Health, the company the OpenAI Startup Fund and Thrive Global are jointly funding to build a customized, hyper-personalized AI health coach that will be available as a mobile app and also within Thrive Global’s enterprise products. It will be trained on the best peer-reviewed science as well as Thrive’s behavior change methodology —including Microsteps , which are tiny daily acts that cumulatively lead to healthier habits. And it will also be trained on the personal biometric, lab, and other medical data you’ve chosen to share with it. It will learn your preferences and patterns across the five behaviors: what conditions allow you to get quality sleep; which foods you love and don’t love; how and when you’re most likely to walk, move , and stretch; and the most effective ways you can reduce stress. Combine that with a superhuman long-term memory, and you have a fully integrated personal AI coach that offers real-time nudges and recommendations unique to you that allows you to take action on your daily behaviors to improve your health.
Read More : Long Waits, Short Appointments, Huge Bills: U.S. Health Care Is Causing Patient Burnout
Consider what it’s like to be a busy professional with diabetes. You might be struggling to manage your blood-sugar levels, often missing meals and exercise due to a hectic schedule. A personalized AI health coach, trained on your medical data and daily routines, could provide timely reminders to take your medication, suggest quick and healthy meal options, and encourage you to take short breaks for exercise.
Most health recommendations at the moment, though important, are generic: your patient portal might send you an automated reminder to get a flu shot or mammogram, or your smartwatch may ping you to breathe or stand. The AI health coach will make possible very precise recommendations tailored to each person: swap your third afternoon soda with water and lemon; go on a 10-minute walk with your child after you pick them up from school at 3:15 p.m.; start your wind-down routine at 10 p.m. since you have to get up at 6 a.m. the next morning to make your flight.
Using AI in this way would also scale and democratize the life-saving benefits of improving daily habits and address growing health inequities. Those with more resources are already in on the power of behavior change, with access to trainers, chefs, and life coaches. But since chronic diseases—like diabetes and cardiovascular disease—are distributed unequally across demographics, a hyper-personalized AI health coach would help make healthy behavior changes easier and more accessible. For instance, it might recommend a healthy, inexpensive recipe that can be quickly made with few ingredients to replace a fast-food dinner.
Health is also what happens between doctor visits. In the same way the New Deal built out physical infrastructure to transform the country, AI will serve as part of the critical infrastructure of a much more effective health care system that supports everyday people’s health in an ongoing way.
This would have an impact not just on our physical health, but on our mental and emotional health as well. When we’re depleted and stressed, we’re more likely to choose options like endless scrolling or emotional eating that might give us a quick dopamine hit, but won’t make us healthy or happy in the long run. With personalized nudges and real-time recommendations across all five behaviors—helping us improve our sleep, reduce sugar and ultra-processed foods, get more movement in our day, lower stress, and increase connection—AI could help us be in a stronger position to make better choices that nourish our mental health. It could also use our health information to make recommendations based on what motivates and inspires us.
Read More : Your Brain Doesn't Want You to Exercise
So much of the conversation around AI has been about how much time it will save us and how productive it will make us. But AI could go well beyond efficiency and optimization to something much more fundamental: improving both our health spans and our lifespans .
How our behaviors can be used to nurture our health and our full humanity is a topic that’s long been of interest to both of us. Arianna has written several books on the subject. Throughout his career, and while building OpenAI, Sam learned the value of prioritizing these five foundational behaviors, including getting enough sleep, eating well, exercising, spending time in nature, and meditating. This has helped him deal with his stress and anxiety and be more able to stay in the eye of the hurricane.
AI-driven diagnostics have already reduced error rates and improved patient outcomes . Now, by focusing AI on healthy behavior promotion and taking advantage of its ability to process potentially several billion data points, we put in our hands a powerful tool for positive change, ensuring technology works for our well-being rather than against it. Incentives are superpowers. And so far, they’ve mostly been used to tap into outrage and increase stress. But by creating new incentives, Thrive AI Health can make it possible for the users’ personal data to be used for their own benefit, helping us all make better decisions and lead healthier lives.
With AI-driven personalized behavior change, we have the chance to finally reverse the trend lines on chronic diseases. Achieving this vision requires collaboration. Policymakers need to create a regulatory environment that fosters AI innovation while safeguarding privacy. Health care providers need to integrate AI into their practices while ensuring that these tools meet rigorous standards for safety and efficacy. And individuals need to be fully empowered through AI coaching to better manage their daily health, with assurances that these technologies are reliable and that their personal health data will be handled responsibly. This collective effort, with robust privacy and security safeguards, can transform health care, benefiting millions of people around the world.
OpenAI and TIME have a licensing and technology agreement that allows OpenAI to access TIME's archives.
More Must-Reads from TIME
- Eyewitness Accounts From the Trump Rally Shooting
- From 2022: How the Threat of Political Violence Is Transforming America
- ‘We’re Living in a Nightmare:’ Inside the Health Crisis of a Texas Bitcoin Town
- Remembering Shannen Doherty , the Quintessential Gen X Girl
- How Often Do You Really Need to Wash Your Sheets?
- Why Mail Theft Is on the Rise
- Welcome to the Noah Lyles Olympics
- Get Our Paris Olympics Newsletter in Your Inbox
Contact us at [email protected]

Health and behavior

Health psychology focuses on examining the relationships between behavioral, cognitive, psychophysiological, and social and environmental factors and the establishment, maintenance, and detriment of health.
Many behaviors, such as smoking, alcohol and drug use, diet and exercise, and more, can have positive or negative impacts on physical health.
Adapted from the APA Dictionary of Psychology
Resources from APA

Combating health misinformation
Experts are studying how false information spreads, who is most vulnerable, and how to end the “infodemic”

Spotlight: It’s all fun and games until someone gets hurt
In a recent article published in the Canadian Journal of Behavioral Science, Barbara Morrongiello and her graduate students examined whether exposing children to framed messages about safety could reduce risk behaviors.

Health Behavior Series
Webinars in this series examine numerous health behaviors through a psychological lens.
Guiding Questions: Mental and Physical Health Pillar
Questions to stimulate class discussion, encourage students to deepen their understanding of core concepts, and cultivate a culturally informed perspective to the study of psychology.
More resources about health and behavior
Psychological Assessment of Surgical Candidates
Psychological Treatments for Patients With Chronic Pain
Death as an Altered State of Consciousness
Psychological Treatment of Cardiac Patients
Psychological Treatment of Patients With Chronic Respiratory Disease
Magination Press children’s books

My Big Fat Secret

Princess Penelopea Hates Peas

Max Archer: The Case of the Wet Bed

Type 1 Teens

Woolfred Cannot Eat Dandelions

Journal special issues
Human-Animal Relations
Social Justice Training in Health Service Psychology
Multimorbidity in Health Psychology and Behavioral Medicine Research
From Ideas to Efficacy in Health Psychology
Promoting Health and Well-Being in Forcibly Displaced Asian Populations
APA journals
Families, Systems, & Health
Clinical Practice in Pediatric Psychology
Journal of Occupational Health Psychology
Stigma and Health
Health Psychology
Caregiving and Health Behaviors Essay
- To find inspiration for your paper and overcome writer’s block
- As a source of information (ensure proper referencing)
- As a template for you assignment
Contrast the positive and negative aspects of caregiving from the caregiver’s perspective and discuss the issues that tip the balance for any given individual
The positive aspects of caregiving are often linked to the nature of the relationship that the caregiver has with the care recipient. The numerous and burdensome negative aspects of caregiving can cripple a caregiver’s career long term, especially without monetary or other remuneration. On the other hand, the alternative to the sacrifice of caring for a loved one, that of abandoning the dependent person to the care of strangers, can cause worry in the short term and guilt and grief in the long term. Both paths have long term impacts.
It consumes time and imposes an opportunity cost 1 It is affecting the caregiver’s future economic security, emotional health, and social status. It can be physically strenuous and even cause back injuries, socially isolate the caregiver, and cause squeamishness or embarrassment. It is like being a nurse or nurse’s aide without the title, the camaraderie of co-workers, insurance, pension, parking space, or paycheck.
The obvious ones are avoidance of guilt and worry, although some evidence suggests that caregiving confers significant feelings of importance (Boerner, Schulz, & Horowitz, 2004). Providing no care at all can contribute to the premature death of the dependent person, causing guilt. Although helpful, there are guilt-inducing drawbacks associated with the alternative of care in the home with paid home health aides 2 The more costly option of institutional care bears risks as well 3 .
Guilt and self-reproach over not having done everything possible for a loved one in the hands can persist for decades. When the dependent person dies, the grieving process is much complicated if the bereaved has not done everything possible to care for the deceased.
The choice between career and caregiving may depend on the nature of the relationship with the dependent person. Although self-importance, inheritance, or pay may help to tip the balance, the major factor seems to the prospect of feeling rotten about having not done everything possible for a loved one.
Health behaviors are primarily under the control of the individual. What can the formal health care delivery system do to encourage healthy lifestyle behaviors?
The formal health care system can probably affect personal health choices but must do so in ways that are not discriminatory or leave patients un-cared for. Here are some ideas:
Make it preventive: Focus funding on primary and preventive services in medical, dental, and mental health services.
Make it easy: Co-locate services so that follow-up on any recommendations becomes a simple and easy matter. Make it simple to navigate the phone systems of major hospitals.
Make it cheap: It should be cheap or free to get guidance and encouragement in quitting smoking, getting gentle exercise, learning to eat healthily, dealing with mental health issues, and getting clean and sober, among other items.
Make it consistent: All health care practitioners, especially primary care professionals, should be inquiring about and following up with education about: 4 Health behaviors: substance use, exercise, driving with seat belt, firearm presence in the home, how they deal with feelings of depression, workplace hazards, use of non-prescription drugs, and sexual behavior, among other items.
Conduct your own self-risk appraisal. A number of programs are available on-line that lead you through a risk profile and give a risk score at the end. Please find one and tell us about it. Also, identify your own list of risk factors and state why you are at risk or not. Create a personal plan for minimizing risk factors. For this portion, only share information that you are comfortable sharing with everyone.
My score on the HealthStatus.com self-assessment tool (HealthStatus, 2013) was 95, or fairly low risk. However, some behaviors still needed amendment, including:
Exercise and weight loss: Time spent in front of a computer has inevitable results. My solution should be to allocate time to exercise even when I am working hard on school assignments. I could set a timer to remind me to move around every half hour.
Lower driving speed: I need to plan my time to allow for a safe speed.
Check for cancer symptoms: A family history of cancer demands vigilance in monitoring and testing, even if inconvenient or intrusive. I need to grit my teeth and make appointments for the checkups and tests that are needed.
Reduce fat in the diet: My student diet is less than ideal. I should be watchful of what I eat when I am working hard.
Bibliography
Anderson, R. (2013). Disadvantages of Insititutional Care . Web.
Boerner, K., Schulz, R., & Horowitz, A. (2004). Positive Aspects of Caregiving and Adaptation to Bereavement. Psychology and Aging, 19 (4), 668-675. Web.
Cifuentes, M., Fernald, D. H., Green, L. A., Niebauer, L. J., Crabtree, B. F., Stange, K. C., & Hassmiller, S. B. (2005). Prescription for Health: Changing Primary Care Practice to Foster Healthy Behaviors. Annals of Family Medicine, 3 (Supplement 2), 54-511. Web.
HealthStatus. (2013). Health Status . Web.
- Taking care of a dependent elder, invalid, or disabled person consumes time and imposes an opportunity cost on the caregiver. The time spent in care could otherwise be spent on a job, education, training, or just on oneself. In many cases, caregiving means a complete abdication of a career or of advancement.
- Anecdotally, paid home health care can precipitate a nightmare of long waits for home health aides and nurses’ arrival, the risk of negligence, abusive speech or behavior, victimization, or fast turnover. All this can cause worry, guilt, fear, a distraction from work, or one’s own life on the part of the family and friends of the dependent person.
- Institutional care, apart from restricting all sorts of personal liberties (Anderson, 2013), can also expose the dependent person to depression, agitation, secondary medical problems, or worsening of existing conditions. Secondary medical problems could include such inconveniences as constipation (due to change to an institutional diet) or the discomfort of a UTI (due to not staying hydrated). The change of setting, especially if the patient is not happy to be there, can lead to less assiduous management of more serious conditions such as elevated blood pressure, depression, or diabetes. The change to an institutional setting may cause disorientation and lead to wandering or resistance to treatment. In some instances, there is outright abuse (sexual, verbal, or physical) or neglect. These problems also impose guilt, worry, anger, distraction, and depression.
- Cifuentes et al., 2005.
- Pressure Ulcers as a Quality Issue in Healthcare
- International Healthcare: Medical Tourism Market
- Quality Improvement in the US Health Care
- Challenges of Living With Alzheimer Disease
- Mutual Responsibility for Child Care and Nurturing
- Multivariate Analysis in Pulmonary Hypertension Study
- Recovery Time After Concussion: Study Methods
- Focus Group Research in Healthcare Organizations
- Physical Activities and Well-Being Study: Dissemination
- Depression in Adolescents and Cognitive Therapy
- Chicago (A-D)
- Chicago (N-B)
IvyPanda. (2021, January 12). Caregiving and Health Behaviors. https://ivypanda.com/essays/caregiving-and-health-behaviors/
"Caregiving and Health Behaviors." IvyPanda , 12 Jan. 2021, ivypanda.com/essays/caregiving-and-health-behaviors/.
IvyPanda . (2021) 'Caregiving and Health Behaviors'. 12 January.
IvyPanda . 2021. "Caregiving and Health Behaviors." January 12, 2021. https://ivypanda.com/essays/caregiving-and-health-behaviors/.
1. IvyPanda . "Caregiving and Health Behaviors." January 12, 2021. https://ivypanda.com/essays/caregiving-and-health-behaviors/.
IvyPanda . "Caregiving and Health Behaviors." January 12, 2021. https://ivypanda.com/essays/caregiving-and-health-behaviors/.
Health Behaviors Essays
Childhood obesity intervention plan, exploring health behaviors and awareness., annotated bibliography: inadequate public knowledge about the significance of mental health concerns, popular essay topics.
- American Dream
- Artificial Intelligence
- Black Lives Matter
- Bullying Essay
- Career Goals Essay
- Causes of the Civil War
- Child Abusing
- Civil Rights Movement
- Community Service
- Cultural Identity
- Cyber Bullying
- Death Penalty
- Depression Essay
- Domestic Violence
- Freedom of Speech
- Global Warming
- Gun Control
- Human Trafficking
- I Believe Essay
- Immigration
- Importance of Education
- Israel and Palestine Conflict
- Leadership Essay
- Legalizing Marijuanas
- Mental Health
- National Honor Society
- Police Brutality
- Pollution Essay
- Racism Essay
- Romeo and Juliet
- Same Sex Marriages
- Social Media
- The Great Gatsby
- The Yellow Wallpaper
- Time Management
- To Kill a Mockingbird
- Violent Video Games
- What Makes You Unique
- Why I Want to Be a Nurse
- Send us an e-mail
- Skip to content
- Skip to search
- Accessibility Policy
- Report an Accessibility Issue

- Study reveals behavioral and health care utilization changes after receiving workplace genetic testing results

New research from Scott Roberts
Professor of health behavior and health education.
July 16, 2024
Workplace genetic testing (wGT) as part of employee wellness benefits may be a powerful tool for early disease intervention that helps participants make more informed decisions about their health, says a new Genetics in Medicine paper . The research team, including University of Michigan School of Public Health researcher Scott Roberts , is investigating the ethical and social implications of workplace genetic testing and whether receiving increased risk results promotes health behavior changes and healthcare utilization in employees. The goal is to help guide the future of wGT across the country.
To conduct the study, the research team surveyed approximately 30,000 participants from a large healthcare employer who had been offered wGT as part of their wellness benefits. Of the individuals who opted into testing, those who received results indicating an increased risk of cancer and/or heart disease were 8.6 times more likely to follow up with a healthcare professional and 3.23 times more likely to make a health behavior change than their peers who received “no increased risk” results.
RELATED: Scott Roberts appointed interim department chair of Health Behavior and Health Education
“It was encouraging to see that many employees who learned from wGT results of their elevated risk for cancer and heart disease were taking steps that might aid prevention of future disease,” said Roberts, interim chair and professor of Health Behavior and Health Education and co-director of the Dual Degree Program in Public Health and Genetic Counseling. “However, it will be important for future studies to examine whether these potential health benefits are truly realized among employees undergoing wGT.”
Learn more about the work in the news release from Jackson Laboratory.
“Health care utilization and behavior changes after workplace genetic testing at a large US health care system,” Genetics in Medicine . DOI: https://doi.org/10.1016/j.gim.2024.101160
Contact Destiny Cook Senior Public Relations Specialist University of Michigan School of Public Health [email protected] 734-647-8650
- Health Behavior and Health Education
- Chronic Disease
- Health Care
- Health Care Access
Recent Posts
- Research shows far-reaching costs of eviction filings to tenants--regardless of the outcome in court
- Behind Michigan's abundant agricultural economy are farmworkers facing poor living conditions
- From 'trial and error' to targeted precision: $17.9M grant accelerates U-M mental health research
What We’re Talking About
- Adolescent Health
- Air Quality
- Alternative Therapies
- Alumni News and Networking
- Biostatistics
- Child Health
- Community Partnership
- Computational Epidemiology and Systems Modeling
- Disaster Relief
- Diversity Equity and Inclusion
- Engaged Learning
- Environmental Health
- Epidemiologic Science
- Epidemiology
- Epigenetics
- First Generation Students
- Food Policy
- Food Safety
- General Epidemiology
- Global Health Epidemiology
- Global Public Health
- Health Care Management
- Health Care Policy
- Health Communication
- Health Disparities
- Health Informatics
- Health for Men
- Health for Women
- Heart Disease
- Hospital Administration
- Hospital and Molecular Epidemiology
- Immigration
- Industrial Hygiene
- Infectious Disease
- Internships
- LGBT Health
- Maternal Health
- Mental Health
- Mobile Health
- Occupational and Environmental Epidemiology
- Pain Management
- Pharmaceuticals
- Precision Health
- Professional Development
- Reproductive Health
- Scholarships
- Sexual Health
- Social Epidemiology
- Social Media
- Student Organizations
- Urban Health
- Urban Planning
- Value-Based Care
- Water Quality
- What Is Public Health?
Information For
- Prospective Students
- Current Students
- Alumni and Donors
- Community Partners and Employers
- About Public Health
- How Do I Apply?
- Departments
- Findings magazine
Student Resources
- Career Development
- Certificates
- The Heights Intranet
- Update Contact Info
- Report Website Feedback

Transforming the understanding and treatment of mental illnesses.
Información en español
Celebrating 75 Years! Learn More >>
- Science News
- Meetings and Events
- Social Media
- Press Resources
- Email Updates
- Innovation Speaker Series
Youth With Conduct Disorder Show Widespread Differences in Brain Structure
NIH-funded study of conduct disorder identifies new brain areas associated with the disorder, offering future directions for research efforts and clinical practice
July 17, 2024 • Press Release
A neuroimaging study of young people who exhibit a persistent pattern of disruptive, aggressive, and antisocial behavior, known as conduct disorder, has revealed extensive changes in brain structure. The most pronounced difference was a smaller area of the brain’s outer layer, known as the cerebral cortex, which is critical for many aspects of behavior, cognition, and emotion. The study, co-authored by researchers at the National Institutes of Health (NIH), is published in The Lancet Psychiatry .
“Conduct disorder has among the highest burden of any mental disorder in youth. However, it remains understudied and undertreated. Understanding brain differences associated with the disorder takes us one step closer to developing more effective approaches to diagnosis and treatment, with the ultimate aim of improving long-term outcomes for children and their families,” said co-author Daniel Pine, M.D., Chief of the Section on Development and Affective Neuroscience in NIH’s National Institute of Mental Health. “Critical next steps are to follow children over time to determine if differences in brain structure seen in this study are a cause of conduct disorder or a long-term consequence of living with the disorder.”
A collaborative group of researchers examined standardized MRI data from youth ages 7 to 21 who had participated in 15 studies from around the world. Analyses compared the surface area and thickness of the cerebral cortex and the volume of deeper subcortical brain regions between 1,185 youth diagnosed with conduct disorder and 1,253 youth without the disorder. Additional analyses compared the cortical and subcortical brain measures between boys and girls, age of symptom onset (childhood vs. adolescence), and level of empathy and other prosocial traits (high vs. low).
Youth with conduct disorder had lower total surface area across the cortex and in 26 of 34 individual regions, two of which showed significant changes in cortical thickness. Youth with conduct disorder also had lower volume in several subcortical brain regions, including the amygdala, hippocampus, and thalamus, which play a central role in regulating behaviors that are often challenging for people with the disorder. Although some of these brain regions, like the prefrontal cortex and amygdala, had been linked to conduct disorder in previous studies, other regions were implicated in the disorder for the first time.
The associations with brain structure did not differ between boys and girls and were seen across conduct disorder subgroups based on age of onset and level of prosocial traits. Youth who exhibited signs of a more severe form of the disorder, indicated by a low level of empathy, guilt, and remorse, showed the greatest number of brain changes.
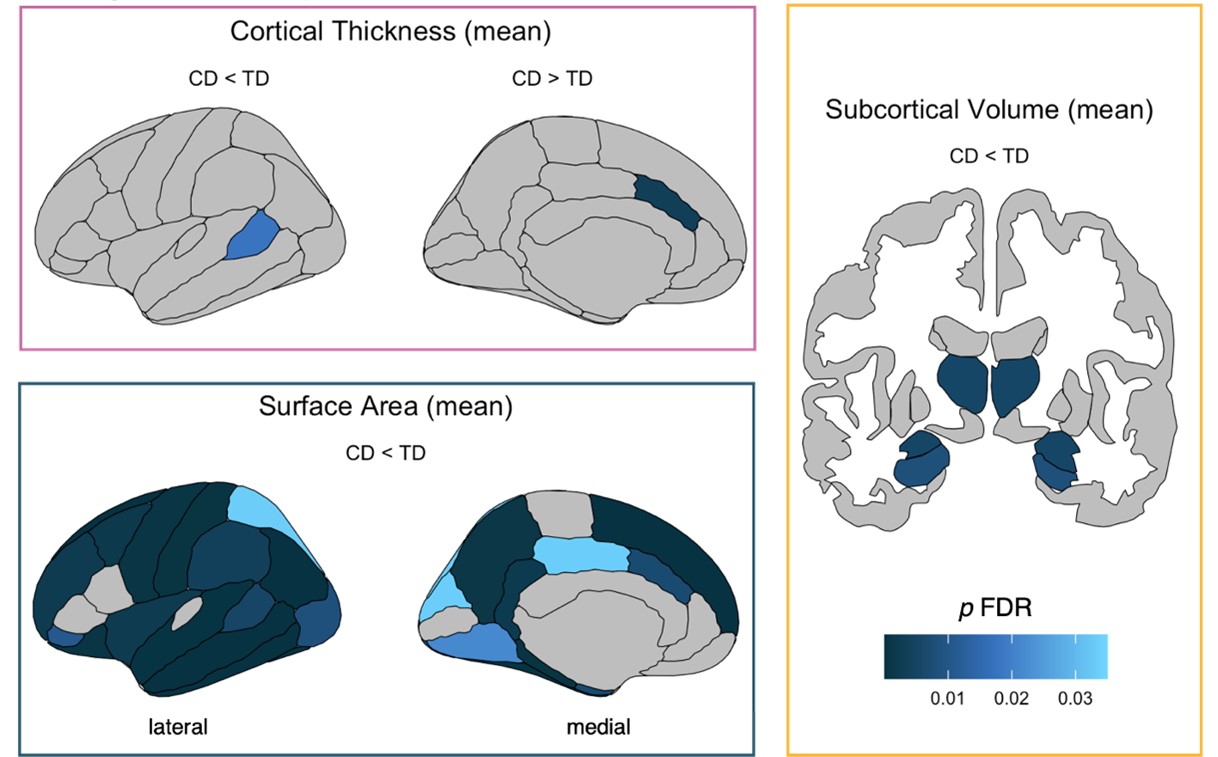
These findings from the largest, most diverse, and most robust study of conduct disorder to date are consistent with a growing body of evidence that the disorder is related to the structure of the brain. The study also provides novel evidence that brain changes are more widespread than previously shown, spanning all four lobes and both cortical and subcortical regions. These findings offer new avenues for investigating potential causal links between differences in brain structure and symptoms of conduct disorder and for targeting brain regions as part of clinical efforts to improve diagnosis and treatment.
Yidian Gao, Ph.D., at the University of Birmingham and Marlene Staginnus, Ph.D., at the University of Bath co-led the study, which was conducted by the international Enhancing Neuroimaging Genetics through Meta-Analysis (ENIGMA)–Antisocial Behavior working group. The ENIGMA consortium received funding from multiple NIH institutes through a cross-NIH alliance that funds the Big Data to Knowledge Centers of Excellence .
Gao, Y., Staginnus, M., & the ENIGMA-Antisocial Behavior Working Group. (2024). Cortical structure and subcortical volumes in conduct disorder: A coordinated analysis of 15 international cohorts from the ENIGMA Antisocial Behavior working group. The Lancet Psychiatry, 11, 620-632. https://www.thelancet.com/journals/lanpsy/article/PIIS2215-0366(24)00187-1/fulltext
EB020403
About the National Institute of Mental Health (NIMH): The mission of the NIMH is to transform the understanding and treatment of mental illnesses through basic and clinical research, paving the way for prevention, recovery and cure. For more information, visit the NIMH website .
About the National Institutes of Health (NIH) : NIH, the nation's medical research agency, includes 27 Institutes and Centers and is a component of the U.S. Department of Health and Human Services. NIH is the primary federal agency conducting and supporting basic, clinical, and translational medical research, and is investigating the causes, treatments, and cures for both common and rare diseases. For more information about NIH and its programs, visit the NIH website .
NIH…Turning Discovery Into Health ®
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- HHS Author Manuscripts

Understanding and Predicting Health Behaviour Change: A Contemporary View Through the Lenses of Meta-Reviews
Karina w. davidson.
Feinstein Institutes for Medical Research, Northwell Health
Urte Scholz
University of Zurich
Research on health behaviour change examines how to help people engage in healthy behaviours to prevent the development or worsening of chronic disease and early mortality and to improve mental health and well-being. While some of that research has been successful, it is often unclear why or how certain behaviour change interventions have worked ( Michie & Abraham, 2004 ; Nielsen et al., 2018 ; Sumner et al., 2018 ). Understanding why successful behaviour change occurs is the key to creating healthy behaviour, reducing the burden of chronic disease worldwide, and promoting health. Without understanding why a behaviour change intervention succeeds, researchers will remain with an evidence base that is fragmented and uninformed. As a result, a great deal of research wastes opportunities to build forward momentum and thereby limits opportunities to harness and synthesise findings to systematically improve behaviour change interventions. Conversely, with an understanding of the causal mechanisms, researchers can build more efficient behaviour change interventions and so create an evidence base that reveals what works for which populations in what contexts and for which behaviours. Researchers have completed thousands of health behaviour change interventions on topics ranging from improving medication adherence behaviour, to decreasing risky sexual activity, to promoting physical activity. In turn, numerous meta-analyses have attempted to examine the effectiveness and to understand the results of such interventions. These meta-analyses have tended to focus on specific behaviours, types of behaviour change interventions, ways of delivering the behaviour change intervention, health outcomes, or populations. At this point, there are often so many meta-analyses focused on a given phenomenon that it is challenging for any individual to summarise the conclusions of these analyses accurately. We present here a special issue devoted to advancing the science of behaviour change in two main ways. First, this special issue presents information across several articles to aid researchers in locating information on both effectiveness and possible explanations for the (in-)effectiveness of behaviour change interventions combined across existing meta-analyses. Second, this special issue provides information on the most important implications for future research on advancing the science of health behaviour change interventions. The first goal will be achieved by a series of meta-reviews of meta-analyses on behaviour change interventions, and the second by three narrative reviews and a series of commentaries.
So, what is a meta-review ? It is essentially a systematic review of systematic reviews ( Blackwood, 2016 ). The intent is to synthesise meta-analyses and thus examine at the highest level only the summary of current evidence. These types of reviews provide evidence to make better decisions about what exists in the research landscape, and what is missing after a comprehensive and thorough search. Similar to published guidelines on quality and reporting standard put forward for meta-analyses, best practice guidelines for meta-reviews have also been proposed, which include pre-registration and standardised quality ratings for their constituent meta-analyses ( Shea et al., 2017 ). By presenting a series of meta-reviews on differing aspects of health behaviour change, this special issue provides a clear overall picture of the current state of the research on health behaviour change research and its quality. It also delivers a clear message about what should be done now to advance the science of behaviour change to improve health.
The meta-reviews presented here were undertaken by personnel supported by The Science of Behavior Change (SOBC) Research Network. To move the health behaviour change field forward, the SOBC Research Network (funded by the U.S. National Institutes of Health) seeks to improve the understanding of underlying mechanisms of human behaviour change by promoting and a basic mechanism of action research by use of an experimental medicine method ( Nielsen et al., 2018 ; Suls et al., 2020 ; Aklin et al., 2020 ). SOBC aims to bring together basic and applied scientists to support this mechanistic research across health-related behaviours to ultimately develop more effective behavioural interventions. Work during SOBC Stage 1 (2009–2014) identified three broad classes of intervention targets that are highly relevant to the mechanisms relating to behaviour change: self-regulation, stress reactivity/stress resilience, and interpersonal and social processes. Stage 1 work also determined the need for reliable and valid ways to measure whether these hypothesised mechanisms of actions were engaged or influenced through experimental manipulation or interventions, which became the focus of SOBC Stage 2 (2015-present). In this work, when a change in the mechanism results in an observed change in behaviour, the inference is that the identified mechanism is indeed a valid mechanism of action. SOBC’s goal is to use the results of this method to optimise behaviour change interventions across disciplines.
Thus, the central goal of SOBC is to identify key mechanisms underlying successful behaviour change interventions aimed to change health behaviour, such as by improving positive health behaviours (e.g., diet and exercise) or by reducing unhealthy behaviours (e.g., smoking). SOBC also seeks to answer the critical question: What works, for whom, and under what circumstances? The SOBC network reviewed, provided feedback, and endorsed a plan for SOBC-supported personnel to undertake a systematic review of the current literature using extant meta-analyses, with the goal of a meta-review being created to understand what meta-analyses have been published thus far examining self-regulation as a means to influence health behaviour. By compiling meta-analyses across a wide range of interventions, behaviour change targets, and distal health outcomes, the results of the parent comprehensive meta-review ( Hennessy, Johnson, Acabchuk, McCloskey, & Stewart-James, 2020 ), and the accompanying targeted meta-reviews ( Protogerou, McHugh, & Johnson, 2020 ; Suls et al., 2020 ; Wilson et al., 2020 ) presented in this special issue promise to inform future studies by identifying gaps in current knowledge and advancing our knowledge where science has already established findings on the mechanisms of self-regulation.
Three salient facts make the current evidence base ripe for meta-reviewing the effectiveness and the explanatory mechanisms of behaviour change interventions: First, new strategies for characterising the content of interventions have led to a more standardised approach to descriptions in a taxonomic form, which has done much to resolve the fragmented and inconsistent way in which interventions have been previously described (e.g., Abraham & Michie, 2008 ; Knittle et al., 2020 ; Kok et al., 2016 ; Michie et al., 2013 ), with ongoing advances in nomenclature, definition, and structure promising even more precision. Thus, synthesising the evidence in meta-reviews by using existing taxonomies for identifying mechanisms most prominently and most effectively applied in behaviour change interventions is now possible. This approach also allows a more comprehensive and precise means for identifying shortcomings, gaps, and open questions in this field. The latter then allows for stimulating further improvements in planning, implementing, and describing intervention content. A long-term benefit of such an approach may be increasingly precise replication efforts together with substantial improvements in the effectiveness of the interventions tested across health behaviour change intervention research ( Byrne, 2020 ).
Second, theories to understand health behaviour itself have also grown more complex, relative to the health behaviour theories proposed in the 1970s and 1980s. Contemporary models for example consider not only reflective, but also automatic processes involved in behaviour change ( Deutsch & Strack, in press ), or place behaviour change within several contexts, such as the romantic relationship ( Lewis et al., 2006 ; Pietromonaco & Collins, 2017 ; Scholz, Berli, Lüscher, & Knoll, in press ) or broader social networks ( Berkman, Glass, Brissette, & Seeman, 2000 ) with individuals connected to others through reciprocal exchanges that vary depending both on the needs (or goals) of the individual and the needs (and goals) of the network partners. Furthermore, recent models also take into account that all this occurs within an overarching environment that facilitates or hinders behaviour change (e.g., via the presence of health-promoting policies and settings, such as bans on smoking in restaurants or streets with designated walking or bike paths; (e.g., Ruiter, Crutzen, de Leeuw, & Kok, in press ; Schuz, 2017 ). As a consequence, contemporary theories do not only more precisely specify potential mechanisms for explaining health behaviour change, but also address the crucial question about what factors are likely to moderate the intervention’s effectiveness. Using these models as theoretical frameworks for synthesising evidence in a meta-review allows a more purposive approach to this task.
Third, standards for conducting meta-analyses and meta-reviews have become increasingly rigorous, transparent, and, with this, more useful (e.g., Shea et al., 2017 ). The level of sophistication now available while exploring multiple meta-analyses creates the ability to address study-level nuances and a growing understanding of the assumptions involved in pooling the results of independent studies on a subject across summaries. Thus, the synthesis of available research results of behaviour change interventions pooled in meta-analyses can be evaluated while considering the quality of the meta-analyses. This allows a more sophisticated view on the existing research. It is also important for considering how to improve future meta-analyses and how to understand the validity of the results.
To concentrate on the most comprehensive and methodologically sophisticated meta-analyses, the parent meta-review focuses on relatively recent published meta-analyses of interventions seeking to change participants’ health behaviours, with the intent of engaging self-regulation. Results of this meta-review indicate that self-regulation is usually addressed in the form of intervention components that administer specific behaviour change techniques. Effectiveness is inconclusive and seems to be dependent on the target population and the behaviour. The following articles of this special issue address critical questions that could best be answered by targeted meta-reviews. Wilson and others examine self-regulation-related changes focused on improving medication adherence ( Wilson et al., 2020 ), while Suls et al. (2020) address the role of self-regulation for improving cardiovascular disease prevention behaviours. Taking a slightly different approach, Protogerou and colleagues examine health-behaviour related self-regulation interventions to reduce risky health behaviour ( Protogerou et al., 2020 ).
Aside from this series of meta-reviews, this special issue also includes narrative reviews complementing the topics covered by the meta-reviews. Alcántara et al. (2020) examine health behaviour self-regulation-related interventions through the lens of the social disparities of health, and so they test the way these factors potentially moderate the effectiveness of behaviour change interventions. Next, Miller et al. (2020) investigate how a developmental perspective is, or is not, considered in the science of behaviour change for self-regulation interventions and provide a strong case for the importance of doing so. As meta-review methodology has advanced so rapidly recently, this special issue also includes one article on how artificial intelligence can be combined with manual systematic searching to support reviewing the existing evidence more efficiently and to enhance the breadth and precision of the meta-analyses found to be eligible when reviewing literature ( Marshall, Johnson, Wang, Rajasekaran, & Wallace, 2020 ).
We conclude this special issue with a series of commentaries on the state of the behaviour change science, and the perspective of funders ( Aklin et al., 2020 ) that further complement the comprehensive overview provided by this special issue as a whole. The commentaries go beyond the implications for future research outlined in the meta-reviews and narrative reviews ( O’Carroll, 2020 ) by e.g. addressing highly topical themes, such as the strong need for improving methods and quality in the area of health behaviour change research ( Byrne, 2020 ), the role of interpersonal differences and environmental factors ( O’Connor, 2020 ), and the interplay between intrapersonal and interpersonal processes ( Rothman, Simpson, Huelsnitz, Jones, & Scholz, 2020 ) as well as the call for taking implementation science into account ( Luszczynska, 2020 ). Finally, the special issue concludes with the perspective of a longstanding editor in chief of Health Psychology Review as the landmark journal for systematic reviews and meta-analyses of the science of behaviour change ( Hagger, 2020 ).
We are convinced that this selection of outstanding articles serves the dual functions of (a) providing a comprehensive overview of the state of the science of behaviour change in terms of knowledge of the role of self-regulatory processes for successful behaviour change interventions and (b) serving as a catalyst for promoting further highest-quality behaviour change interventions addressing the most pressing questions in the science of behaviour change.
Acknowledgments
Role of Funding Sources and Disclosures: This study was supported by the National Institutes of Health (NIH) Science of Behavior Change Common Fund Program through an award administered by the National Institute on Aging (U24AG052175). Karina W. Davidson is a member of the United States Preventive Services Task Force (USPSTF). This article does not represent the views and policies of the USPSTF.
Contributor Information
Karina W. Davidson, Feinstein Institutes for Medical Research, Northwell Health.
Urte Scholz, University of Zurich.
- Abraham C, & Michie S (2008). A taxonomy of behavior change techniques used in interventions . Health Psychology , 27 ( 3 ), 379–387. doi: 10.1037/0278-6133.27.3.379 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Aklin WM, Stoeckel LE, Green PA, Keller C, King JW, Nielsen L, & Hunter C (2020). Commentary: National Institutes of Health (NIH) Science of Behavior Change (SOBC) . Heatlh Psychology Review . doi: 10.1080/17437199.2020.1716383. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Alcántara C, Diaz SV, Giorgio Cosenzo L, Loucks EB, Penedo FJ, & Williams NJ (2020). Social Determinants as Moderators of Health Behaviour Change Interventions: Scientific Gaps and Opportunities . Health Psychology Review . [ PubMed ] [ Google Scholar ]
- Berkman LF, Glass T, Brissette I, & Seeman TE (2000). From social integration to health: Durkheim in the new millennium . Social Science & Medicine , 51 ( 6 ), 843–857. doi: 10.1016/s0277-9536(00)00065-4 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Blackwood D (2016). Taking it to the next level…reviews of systematic reviews . HLA News ( Winter ), 13–15. [ Google Scholar ]
- Byrne M (2020). Gaps and priorities in advancing methods for health behaviour change research . Health Psychology Review . 10.1080/17437199.2019.1707106 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Deutsch R, & Strack F (in press). Changing behavior using the reflective-impulsive model In Hagger MS, Cameron LD, Hamilton K, Hankonen N, & Lintunen T (Eds.), The Handbook of Behavior Change . Cambridge, U.K.: Cambridge University Press. [ Google Scholar ]
- Hagger MS, Moyers S, McAnally K, & McKinley LE (2020). Known knowns and known unknowns on behaviour change interventions and mechanisms of action . Health Psychology Review . doi: 10.1080/17437199.2020.1719184. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Hennessy EA, Johnson BT, Acabchuk RL, McCloskey K, & Stewart-James J (2020). Self-Regulation Mechanisms in Health Behaviour Change: A Systematic Meta-Review of Meta-Analyses, 2006–2017 . Health Psychology Review , 1–142. doi: 10.1080/17437199.2019.1679654 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Knittle K, Heino MTJ, Marques MM, Stenius M, Beattie M, Ehbrecht F, … Hankonen N (2020). The compendium of self-enactable techniques to change and self-manage motivation and behaviour v1. 0 . Nature Human Behaviour . doi: 10.1038/s41562-019-0798-9 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Kok G, Gottlieb NH, Peters GJ, Mullen PD, Parcel GS, Ruiter RA, … Bartholomew LK (2016). A taxonomy of behaviour change methods: an Intervention Mapping approach . Health Psychology Review , 10 ( 3 ), 297–312. doi: 10.1080/17437199.2015.1077155 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Lewis MA, McBride CM, Pollak KI, Puleo E, Butterfield RM, & Emmons KM (2006). Understanding health behavior change among couples: an interdependence and communal coping approach . Social Science & Medicine , 62 ( 6 ), 1369–1380. doi: 10.1016/j.socscimed.2005.08.006 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Luszczynska A (2020). It’s time for effectiveness-implementation hybrid research on behaviour change . Health Psychology Review , 1–5. doi: 10.1080/17437199.2019.1707105 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Marshall IJ, Johnson BT, Wang Z, Rajasekaran S, & Wallace BC (2020). Semi-automated evidence synthesis in health Psychology: Current methods and future potential . Health Psychology Review . doi: 10.1080/17437199.2020. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Michie S, & Abraham C (2004). Interventions to change health behaviours: evidence-based or evidence-inspired? Psychology & Health , 19 ( 1 ), 29–49. doi: 10.1080/0887044031000141199 [ CrossRef ] [ Google Scholar ]
- Michie S, Richardson M, Johnston M, Abraham C, Francis J, Hardeman W, … Wood CE (2013). The behavior change technique taxonomy (v1) of 93 hierarchically clustered techniques: building an international consensus for the reporting of behavior change interventions . Annals of Behavioral Medicine , 46 ( 1 ), 81–95. doi: 10.1007/s12160-013-9486-6 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Miller AL, Lo S, Bauer KW, & Fredericks EM (2020). Considering developmental factors in health-focused self-regulation interventions . Health Psychology Review . doi: 10.1080/17437199.2020.1718530. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Nielsen L, Riddle M, King JW, Aklin WM, Chen W, Clark D, … Weber W (2018). The NIH Science of Behavior Change Program: Transforming the science through a focus on mechanisms of change . Behaviour Research and Therapy , 101 , 3–11. doi: 10.1016/j.brat.2017.07.002 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- O’Carroll RE (2020). Self-regulation interventions - what do we know and where should we go? Health Psychology Review , 1–6. doi: 10.1080/17437199.2019.1709529 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- O’Connor DB (2020). The future of health behaviour change interventions: Opportunities for open science and personality research . Health Psychology Review , 1–10. doi: 10.1080/17437199.2019.1707107 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Pietromonaco PR, & Collins NL (2017). Interpersonal mechanisms linking close relationships to health . The American Psychologist , 72 ( 6 ), 531–542. doi: 10.1037/amp0000129 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Protogerou C, McHugh RK, & Johnson BT (2020). How best to reduce unhealthy risk-taking behaviours? A meta-review of evidence syntheses of interventions using self-regulation principles . Health Psychology Review , 1–30. doi: 10.1080/17437199.2019.1707104 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Rothman AJ, Simpson JA, Huelsnitz CO, Jones RE, & Scholz U (2020). Integrating intrapersonal and interpersonal processes: A key step in advancing the science of behavior change . Health Psychology Review . doi: 10.1080/17437199.2020.1719183. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Ruiter R, Crutzen R, de Leeuw E, & Kok G (in press). Changing behavior using theories at the interpersonal, organizational, community and societal levels In Hagger MS, Cameron LD, Hamilton K, Hankonen N, & Lintunen T (Eds.), The Handbook of Behavior Change . Cambridge, U.K.: Cambridge University Press. [ Google Scholar ]
- Scholz U, Berli C, Lüscher J, & Knoll N (in press). Changing behavior using theories at the interpersonal, organizational, community and societal levels In Hagger MS, Cameron LD, Hamilton K, Hankonen N, & Lintunen T (Eds.), The Handbook of Behavior Change . Cambridge, U.K.: Cambridge University Press. [ Google Scholar ]
- Schuz B (2017). Socio-economic status and theories of health behaviour: Time to upgrade a control variable . British Journal of Health Psychology , 22 ( 1 ), 1–7. doi: 10.1111/bjhp.12205 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Shea BJ, Reeves BC, Wells G, Thuku M, Hamel C, Moran J, … Henry DA (2017). AMSTAR 2: a critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both . BMJ , 358 , j4008. doi: 10.1136/bmj.j4008 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Suls J, Mogavero JN, Falzon L, Pescatello LS, Hennessy EA, & Davidson KW (2020). Health Behaviour Change in Cardiovascular Disease Prevention and Management: Meta-Review of Behaviour Change Techniques to Affect Self-Regulation . Health Psychology Review , 1–23. doi: 10.1080/17437199.2019.1691622 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Sumner JA, Carey RN, Michie S, Johnston M, Edmondson D, & Davidson KW (2018). Using rigorous methods to advance behaviour change science . Nature Human Behaviour , 2 ( 11 ), 797–799. doi: 10.1038/s41562-018-0471-8 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Wilson TE, Hennessy EA, Falzon L, Boyd R, Kronish IM, & Birk JL (2020). Effectiveness of interventions targeting self-regulation to improve adherence to chronic disease medications: A meta-review of meta-analyses . Health Psychology Review , 1–41. doi: 10.1080/17437199.2019.1706615 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
A look at the Texas mental health workforce shortage
A guide to some of the professions that make up the mental health workforce.
/https://static.texastribune.org/media/files/c50e909e094cfdd8d846e56faa07955b/0411%20Texas%20Licensing%20MH%20MC%20TT%2005.jpg)
Sign up for The Brief , The Texas Tribune’s daily newsletter that keeps readers up to speed on the most essential Texas news.
Texas is in the midst of a mental health workforce shortage. But where is the state short?
Today, 246 of Texas’ 254 counties are wholly or partly designated by the federal government as “mental health professional shortage areas,” and that’s in a state where roughly 5 million people do not have health insurance. This has had a particularly dire effect in rural, border, and frontier counties in Texas, as some regions might have only one mental health professional or none.
“If you look at the raw numbers, we don’t have enough providers, even if they were evenly distributed,” said Alison Mohr Boleware, the Hogg Foundation for Mental Health policy director.
A 2023 report from the Health Professions Resource Center, which collects licensure data, shows that while the mental health workforce is growing, it’s not evenly distributed around the state. Also, the workforce is aging fast and typically filled with mostly white, English-only speakers who live in the state’s largest cities.
In Texas, more than 40% of the state’s more than 30 million residents are Hispanic, but its mental health provider population is more than 80% white , according to 2023 data . Also, less than 20% of the state’s 10,440 mental health providers who responded to the 2023 workforce survey said they offer mental health services in a language other than English.
To combat the shortfall, the state’s mental health licensing authority, the Texas Behavioral Health Executive Council , said it is looking more closely at how to meet the demand.
As Boleware notes: “Not everyone needs to see a psychiatrist or a psychologist. We want to make sure people know that they have different options when deciding what level of care they might want.”
Here’s an explanation of the more common job titles in behavioral health and how the shortages stack up, statewide. To practice in Texas, all must pass licensure tests.
Psychiatrist
A psychiatrist is a medical doctor who specializes in mental health, including substance use disorders. Psychiatrists can order or perform lab work, prescribe medications, and provide therapy.
Requirements include a bachelor's degree, a medical school degree then four years of residency.
Psychiatrists often work with individuals who have significant mental illness but can treat a broad spectrum of patients.
In 2023, there were 2,651 psychiatrists in Texas , an increase of 31.7% from 2015, according to the Texas Department of State Health Services. Even so, there are 170 counties that have no licensed psychiatrist. Overall, there are about 11,758 residents for each psychiatrist .
One note. According to the Texas Department of State Health Services, 23% of Texas psychiatrists in 2023 were over 65. The agency estimates that nearly 42% of the Texas psychiatrist workforce will be over 65 within ten years.
Psychologist and psychological associate
Psychologists evaluate a person’s mental health using clinical interviews, evaluations, and testing. They can make diagnoses and provide individual and group therapy. This group cannot prescribe medication.
Psychologists hold a doctoral degree in clinical psychology or another specialty, such as counseling or education, and they can specialize in specific areas of mental health, including child, clinical, developmental, geriatric, and community psychology.
There are 5,138 licensed psychologists and 734 licensed psychological associates in Texas. While the number of licensed psychologists increased by 18.4% since 2015, the number of licensed psychological associates – a mental health professional with a master’s degree instead of a doctoral degree – decreased by 20.2% from the 920 providers in 2015.
This has left 143 counties in the state without a licensed psychologist and 172 without a licensed psychological associate. Metropolitan counties had four times as many licensed psychologists per capita as nonmetropolitan counties.
Within ten years, 40.5% of the Texas licensed psychologist workforce will be over 65.
Social worker
Social workers are often the first point of contact for many people looking for mental health help. They often provide specific services to address a person’s life needs, such as finances, housing, community resources, and government benefits.
A clinical social worker is trained to evaluate a person’s mental health and use therapeutic techniques to help people cope with stressful life events and specific mental health conditions such as depression or anxiety. They cannot prescribe medication.
To become a clinical social worker, one must have a degree in social work, either a master's degree to do clinical work or a bachelor's degree to conduct case management, complete field experience hours, and pass the Texas Social Work Jurisprudence exam and the Texas State Board of Social Workers exam, which the Association of Social Work Boards administers.
There are varying ranks of social workers. Licensed clinical social workers, licensed master social workers, and licensed baccalaureate social workers all have different education and practice requirements.
A licensed clinical social worker is considered the most advanced license and can practice counseling, while licensed master social workers can provide counseling under supervision. A licensed baccalaureate social worker only needs a bachelor’s degree but usually handles non-clinical services like case management and advocacy.
The state has 10,675 licensed clinical social workers, 12,146 licensed master social workers, and 3,236 licensed baccalaureate social workers. However, 91 Texas counties lack access to licensed clinical social workers, 74 counties lack licensed master social workers, and 65 counties lack licensed baccalaureate social workers.
The number of licensed clinical social workers has increased by 49.8% since the 7,126 number was tallied in 2015, and the number of licensed master social workers has increased by 27.7% from 9,508 during the same time period.
Licensed professional counselor
A counselor is trained to evaluate a person’s mental health and engage in counseling as the primary method of treatment. These providers cannot prescribe medication. Counselors are often found in hospitals, clinics, schools, nursing homes, and private practices.
To become a licensed professional counselor, applicants need a master’s degree in a mental health-related field.
There are 25,519 licensed professional counselors in Texas, the most of any mental health profession. Since 2015, there’s been a 47.5% increase in their numbers to 17,303 in 2023.
Despite this increase, 29 counties in Texas still need a licensed professional counselor. Metropolitan counties had 1.8 times as many licensed professional counselors per capita as non-metropolitan counties.
Behavioral Analyst
A behavior analyst provides therapy for individuals, often children, whostruggle to control their emotions. They often train parents, teachers, and others on how to address troubling behavior.
To become a licensed behavioral analyst, an individual must earn an acceptable graduate degree that includes coursework in behavior analysis, complete a defined period of supervised experience, and be certified and comply with the Behavior Analyst Certification Board's professional, ethical, and disciplinary standards and apply for a state-issued license.
This is one of the fastest growing fields. There are 3,467 behavioral analysts in Texas, which is a 62.8% increase from the 2,130 in 2020.
In 2023, there were 140 counties in Texas without behavior analysts and 219 counties without assistant behavior analysts. Per capita, metropolitan counties had 3.8 times as many behavior analysts and four times as many assistant behavior analysts as non-metropolitan counties.
Licensed specialist school psychologist
A school psychologist has an advanced degree in psychology and is trained to make diagnoses, provide individual and group therapy, and work with school staff to ensure mental wellness within the facilities. These providers generally cannot prescribe medication.
Texas has 4,017 licensed school psychology specialists, a 27.6% increase from the 3,148 providers in 2015. In 2023, there were 97 counties without licensed school psychology specialists, most of them in metropolitan areas.
Most licensed school psychology specialists work in public schools, and this provider population is still very young. In 10 years, only 21.6% of the current Texas licensed school psychology specialist workforce will be over 65 years of age.
However, the race and gender dynamics of this provider population have been very rigid. As of 2023, 85.7% of licensed school psychologists were female, and 65.3% of the provider population was classified as White. This reveals that Black, Hispanic, and other races are being underrepresented when compared to the population of Texas.
Marriage and family therapist
Marriage and family therapists are master's degree-level health care professionals trained to provide individual and group counseling. They cannot prescribe medication.
They typically meet one-on-one with couples and families to identify negative behavioral patterns while coming up with successful ways to communicate with one another.
Texas has 3,268 licensed marriage and family therapists, a 22.3% increase from 2,673 in 2015. However, as of last year, 140 counties had no marriage and family therapists.
In the past decade, state lawmakers have tried a variety of methods to increase the number of mental health workers in Texas including the extension of student loan forgiveness, adding more treatment beds in the state hospital system and expanding state hospital capacity.
Last year, lawmakers passed a budget increase for state psychiatric hospital staff and local mental health authorities. They also increased the Loan Repayment Program for Mental Health Professionals funding from $2 million to $28 million.
But neither of these are short-term solutions.
One thing that could help overnight is increasing the amount the Medicaid health insurance program pays providers for mental health services. Medicaid is the federal-state health insurance plan for low-income Texans.
“A lot of providers start out working with Medicaid clients, and then once they see that they won’t be able to support their family or really move up salary-wise, they leave and start doing private work, or they don’t take insurance at all,” said Boleware, with the Hogg Foundation for Mental Health.
Boleware said she believes the state is on the right track to fix the crisis, but it will take some time.
“There are a lot of people working on this issue that have a lot of innovative ideas," she said, "but we have to think about the big picture, long term, rather than getting discouraged by what we are seeing right now.”
Big news: director and screenwriter Richard Linklater ; NPR President and CEO Katherine Maher ; U.S. Rep. Pete Aguilar , D-California; and Luci Baines Johnson will take the stage at The Texas Tribune Festival , Sept. 5–7 in downtown Austin. Buy tickets today!
Texans need truth. Help us report it.
Independent Texas reporting needs your support. The Texas Tribune delivers fact-based journalism for Texans, by Texans — and our community of members, the readers who donate, make our work possible. Help us bring you and millions of others in-depth news and information. Will you support our nonprofit newsroom with a donation of any amount?
Support independent Texas news
Become a member. Join today.
Choose an amount or learn more about membership .
Information about the authors
/https://static.texastribune.org/media/profiles/TEMP_Stephen_Simpson.jpeg)
Stephen Simpson
Mental health reporter.
@Steve55Simpson
/https://static.texastribune.org/media/profiles/Elijah_Nicholson-Messmer.jpeg)
Elijah Nicholson-Messmer
@ElijahMessmer
Learn about The Texas Tribune’s policies , including our partnership with The Trust Project to increase transparency in news.
Explore related story topics
Health care State government Mental health
- Share full article
Advertisement
Supported by
Children With Autism Carry Unique Gut Flora, Study Finds
The research, which builds on previous work, eventually may lead to a more objective diagnostic tool, scientists said.

By Teddy Rosenbluth
The process for diagnosing a child with autism heavily relies on a parent's description of their child’s behavior and a professional’s observations. It leaves plenty of room for human error.
Parents’ concerns may skew how they answer questionnaires. Providers may hold biases, leading them to underdiagnose certain groups . Children may show widely varying symptoms, depending on factors like culture and gender.
A study published Monday in Nature Microbiology bolsters a growing body of research that suggests an unlikely path to more objective autism diagnoses: the gut microbiome.
After analyzing more than 1,600 stool samples from children ages 1 to 13, researchers found several distinct biological “markers” in the samples of autistic children. Unique traces of gut bacteria, fungi, viruses and more could one day be the basis of a diagnostic tool, said Qi Su, a researcher at the Chinese University of Hong Kong and a lead author of the study.
A tool based on biomarkers could help professionals diagnose autism sooner, giving children access to treatments that are more effective at a younger age, he said.
“Too much is left to questionnaires,” said Sarkis Mazmanian, a microbiome researcher at the California Institute of Technology. “If we can get to something we can measure — whatever it is — that’s a huge improvement.”
We are having trouble retrieving the article content.
Please enable JavaScript in your browser settings.
Thank you for your patience while we verify access. If you are in Reader mode please exit and log into your Times account, or subscribe for all of The Times.
Thank you for your patience while we verify access.
Already a subscriber? Log in .
Want all of The Times? Subscribe .

IMAGES
VIDEO
COMMENTS
Conclusion. Health beliefs and behaviors have to be on one accord in order for an individual to live a healthier lifestyle. Your beliefs and attitude regarding health and illness has to be one of an aware and serious nature, or your behaviors will quickly become the gateway to your health deterioration.
Health behaviors, sometimes called health-related behaviors, are actions taken by individuals that affect health or mortality. These actions may be intentional or unintentional, and can promote or detract from the health of the actor or others. Actions that can be classified as health behaviors are many; examples include smoking, substance use ...
Background: Historically, influential models and theories of health behavior employed in aging research view human behavior as determined by conscious processes that involve intentional motives and beliefs. We examine the evolution, strengths, and weaknesses of this approach; then offer a contemporary definition of the mind, provide support for it, and discuss the implications it has for the ...
1. Introduction. Unhealthy behaviors are implicated in up to 40% of premature deaths in the U.S. (Mokdad, Marks, Stroup, & Gerberding, 2004) and contribute to persistent disparities in health (U.S. Department of Health and Human Services, 2015).But public health and behavioral research routinely focuses on single behaviors or small subsets of behaviors with shared functional meanings (e.g ...
Balanced Conceptualizations Mental Health Behavior The report also shows that mental health and illnesses are based on interacting and multiple psychological, biological, and social factors including illness and health. The information presents clear evidence for a relationship to risks of mental illnesses that are related to indicators of poverty and low levels of education.
Health And Behavior Essays. The Link Between Health and Behavior. The interaction between health and behavior is a cyclic phenomenon described by several paradigms related to physical, mental, and social direction. From the point of view of the biopsychosocial model, health is an integral combination of different biological, psychological, and ...
The current issue of Psychology & Health focuses on an important topic for contemporary health psychology, namely health behaviours. Health behaviours have been defined as '. . . overt behavioral patterns, actions and habits that relate to health maintenance, to health restoration and to health improvement' (Gochman, 1997, p. 3).
Essay: Holistic Medicine and the Biopsychosocial Approach. ... Unit 23 Health, Mind, and Behavior. Health, Mind, and Behavior is the twenty-third program in the Discovering Psychology series. This program examines the relationship between mind and body, and some of the ways psychological factors affect our physical health and immune system. ...
Individual response to stressors influences their health. Maladaptive response to stress results in various physical, psychological, and behavioral negative effects. Negative effects of stress on physical health include increased heart rates, sweating, high blood pressure, and long-term development of the cardiac condition. Psychological ...
This essay about the psychological underpinnings of health behavior explores how various theories explain why people engage in health-promoting activities or avoid them. It discusses the Health Belief Model, which centers on personal beliefs about health risks and the perceived balance of benefits versus barriers to taking action.
The interaction between health and behavior is a cyclic phenomenon described by several paradigms related to physical, mental, and social direction. From the point of view of the biopsychosocial model, health is an integral combination of different biological, psychological, and social factors. ... Use our essay writing service and save your ...
Effectively encouraging patients to change their health behavior is a critical skill for primary care physicians. Modifiable health behaviors contribute to an estimated 40 percent of deaths in the ...
In general, behavioral interventions use different ways of thinking, feeling, acting, or relating with others to stimulate a change in a person's behavior to promote their health and well-being. For example, a behavioral intervention could be aimed at modifying something about a person's living environment or diet, with the goal of ...
Health Behavior Theory Essay An individual's attitude towards his health influences his capacity to maintain an optimum level of health, prevent illness or recover from a disease. Understanding patient's attitude towards his condition is the key to establishing an effective health-related program for health promotion, disease prevention and ...
Branches. Health psychology is a specialty area that focuses on how biology, psychology, behavior, and social factors influence health and illness. Other terms such as medical psychology and behavioral medicine are sometimes used interchangeably with the term health psychology. Health and illness are influenced by a wide variety of factors.
Health behaviors are typically conceptualized as potential confounders or mediators of the association between psychological factors and health outcomes (Cohen et al., 2016;Epel et al., 2018 ...
A staggering 129 million Americans have at least one major chronic disease—and 90% of our $4.1 trillion in annual health care spending goes toward treating these physical and mental-health ...
Health and behavior. Health psychology focuses on examining the relationships between behavioral, cognitive, psychophysiological, and social and environmental factors and the establishment, maintenance, and detriment of health. Many behaviors, such as smoking, alcohol and drug use, diet and exercise, and more, can have positive or negative ...
According to Sallis et al. (2008: 466), the four core principles of the ecological perspective model of health behaviour are that: 1. There are multiple influences on specific health behaviours, including factors at the intrapersonal, interpersonal, organizational, community, and public policy levels; 2.
In many cases, caregiving means a complete abdication of a career or of advancement. Anecdotally, paid home health care can precipitate a nightmare of long waits for home health aides and nurses' arrival, the risk of negligence, abusive speech or behavior, victimization, or fast turnover. All this can cause worry, guilt, fear, a distraction ...
Exploring Health Behaviors and Awareness. Introduction Our survey project's main goal was to provide students with a practical chance to apply the fundamental concepts they learned in our public health course to a real-world setting, empowering them. Our focus was on health behaviors and awareness, intending to explore the nuances of how ...
Connor defined health behaviours as activities undertaken for the purpose of preventing or detecting disease or for improving health and wellbeing. 22 Some of the examples include smoking, alcohol ...
The research team, including University of Michigan School of Public Health researcher Scott Roberts, is investigating the ethical and social implications of workplace genetic testing and whether receiving increased risk results promotes health behavior changes and healthcare utilization in employees. The goal is to help guide the future of wGT ...
Chief Medical Correspondent Dr. Sanjay Gupta talks about troubling behaviors demonstrated by President Joe Biden during the recent CNN debate. These include slow responses, trouble finding words ...
The largest neuroimaging study of conduct disorder to date, with funding from NIH, has revealed extensive changes in brain structure among young people with the disorder. The largest difference was a smaller area of the brain's outer layer, known as the cerebral cortex, which is critical for many aspects of behavior, cognition and emotion.
As a youth mental health crisis persists in the US, a new report highlights a significant gap between the level of support that teenagers feel and the amount that parents think their children have.
Health Psychology Review, 10 (3), 297-312. doi: 10.1080/17437199.2015.1077155 [PMC free article] [Google Scholar] Lewis MA, McBride CM, Pollak KI, Puleo E, Butterfield RM, & Emmons KM (2006). Understanding health behavior change among couples: an interdependence and communal coping approach.
Also, less than 20% of the state's 10,440 mental health providers who responded to the 2023 workforce survey said they offer mental health services in a language other than English.
The research, which builds on previous work, eventually may lead to a more objective diagnostic tool, scientists said. By Teddy Rosenbluth The process for diagnosing a child with autism heavily ...
Behavioral Health Services Act - Opportunities for Housing. The BHSA modernizes the MHSA, passed by voters in 2004, to address today's behavioral health system and needs. These reforms expand services to include treatment for people with substance use disorders, prioritize care for individuals with the most serious mental illnesses, provide ...