Home Blog Design How to Design a Winning Poster Presentation: Quick Guide with Examples & Templates

How to Design a Winning Poster Presentation: Quick Guide with Examples & Templates

How are research posters like High School science fair projects? Quite similar, in fact.
Both are visual representations of a research project shared with peers, colleagues and academic faculty. But there’s a big difference: it’s all in professionalism and attention to detail. You can be sure that the students that thrived in science fairs are now creating fantastic research posters, but what is that extra element most people miss when designing a poster presentation?
This guide will teach tips and tricks for creating poster presentations for conferences, symposia, and more. Learn in-depth poster structure and design techniques to help create academic posters that have a lasting impact.
Let’s get started.
Table of Contents
- What is a Research Poster?
Why are Poster Presentations important?
Overall dimensions and orientation, separation into columns and sections, scientific, academic, or something else, a handout with supplemental and contact information, cohesiveness, design and readability, storytelling.
- Font Characteristics
- Color Pairing
- Data Visualization Dimensions
- Alignment, Margins, and White Space
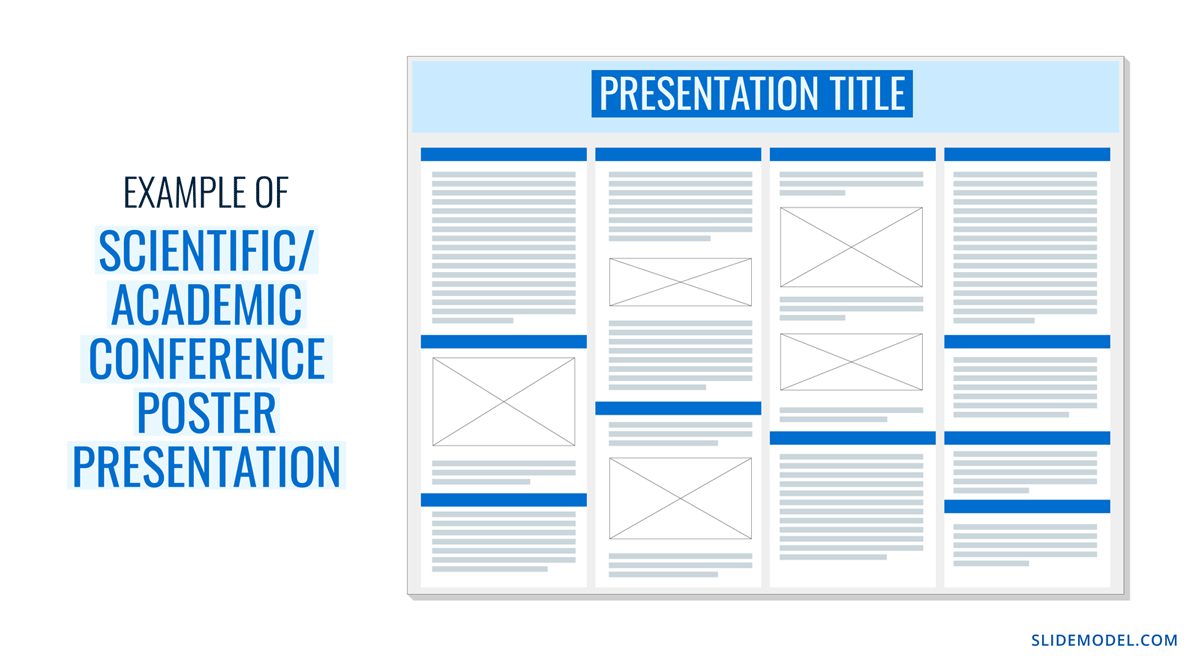
Scientific/Academic Conference Poster Presentation
Digital research poster presentations, slidemodel poster presentation templates, how to make a research poster presentation step-by-step, considerations for printing poster presentations, how to present a research poster presentation, final words, what is a research poster .
Research posters are visual overviews of the most relevant information extracted from a research paper or analysis. They are essential communication formats for sharing findings with peers and interested people in the field. Research posters can also effectively present material for other areas besides the sciences and STEM—for example, business and law.
You’ll be creating research posters regularly as an academic researcher, scientist, or grad student. You’ll have to present them at numerous functions and events. For example:
- Conference presentations
- Informational events
- Community centers
The research poster presentation is a comprehensive way to share data, information, and research results. Before the pandemic, the majority of research events were in person. During lockdown and beyond, virtual conferences and summits became the norm. Many researchers now create poster presentations that work in printed and digital formats.
Let’s look at why it’s crucial to spend time creating poster presentations for your research projects, research, analysis, and study papers.
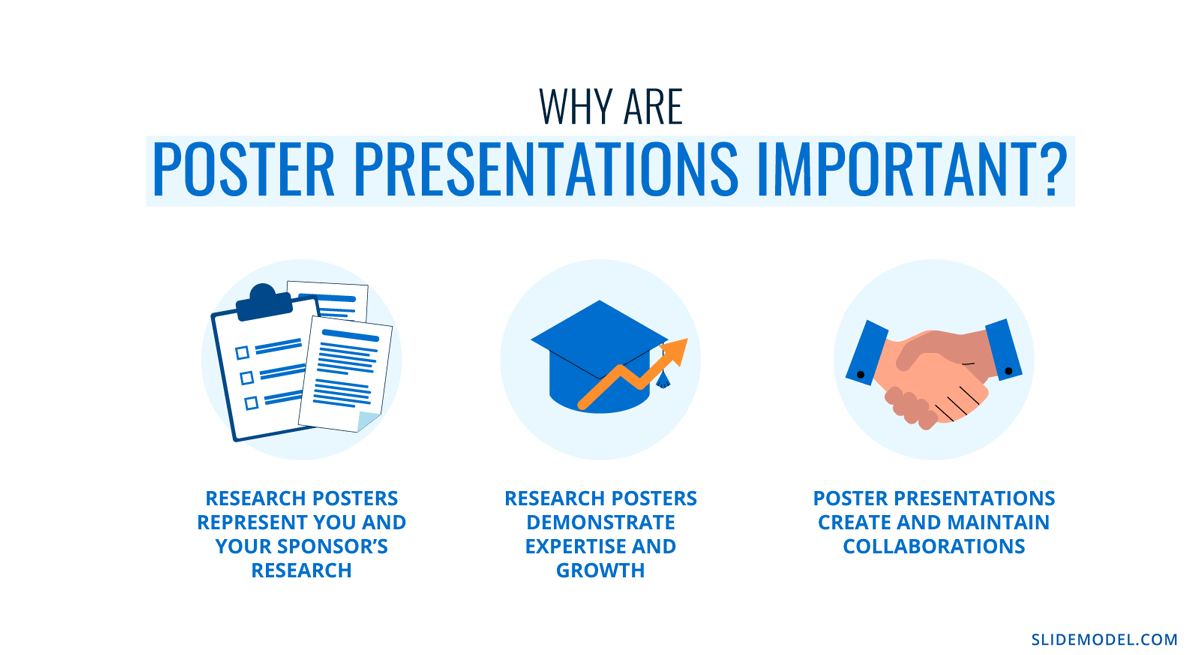
Research posters represent you and your sponsor’s research
Research papers and accompanying poster presentations are potent tools for representation and communication in your field of study. Well-performing poster presentations help scientists, researchers, and analysts grow their careers through grants and sponsorships.
When presenting a poster presentation for a sponsored research project, you’re representing the company that sponsored you. Your professionalism, demeanor, and capacity for creating impactful poster presentations call attention to other interested sponsors, spreading your impact in the field.
Research posters demonstrate expertise and growth
Presenting research posters at conferences, summits, and graduate grading events shows your expertise and knowledge in your field of study. The way your poster presentation looks and delivers, plus your performance while presenting the work, is judged by your viewers regardless of whether it’s an officially judged panel.
Recurring visitors to research conferences and symposia will see you and your poster presentations evolve. Improve your impact by creating a great poster presentation every time by paying attention to detail in the poster design and in your oral presentation. Practice your public speaking skills alongside the design techniques for even more impact.
Poster presentations create and maintain collaborations
Every time you participate in a research poster conference, you create meaningful connections with people in your field, industry or community. Not only do research posters showcase information about current data in different areas, but they also bring people together with similar interests. Countless collaboration projects between different research teams started after discussing poster details during coffee breaks.
An effective research poster template deepens your peer’s understanding of a topic by highlighting research, data, and conclusions. This information can help other researchers and analysts with their work. As a research poster presenter, you’re given the opportunity for both teaching and learning while sharing ideas with peers and colleagues.
Anatomy of a Winning Poster Presentation
Do you want your research poster to perform well? Following the standard layout and adding a few personal touches will help attendees know how to read your poster and get the most out of your information.
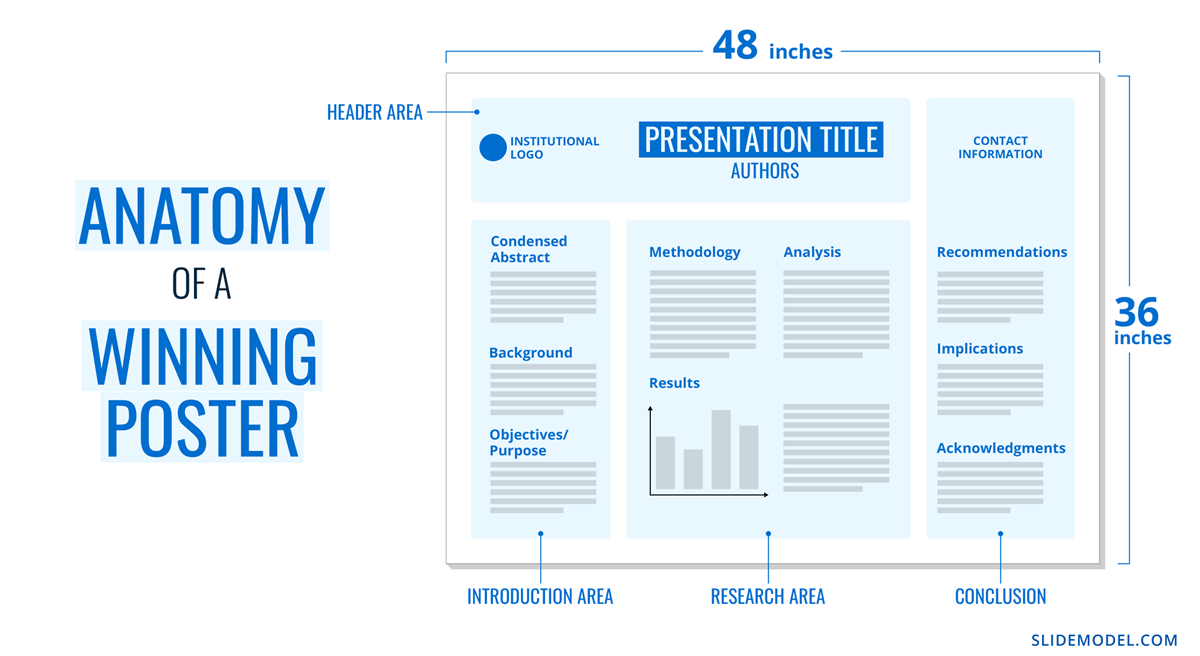
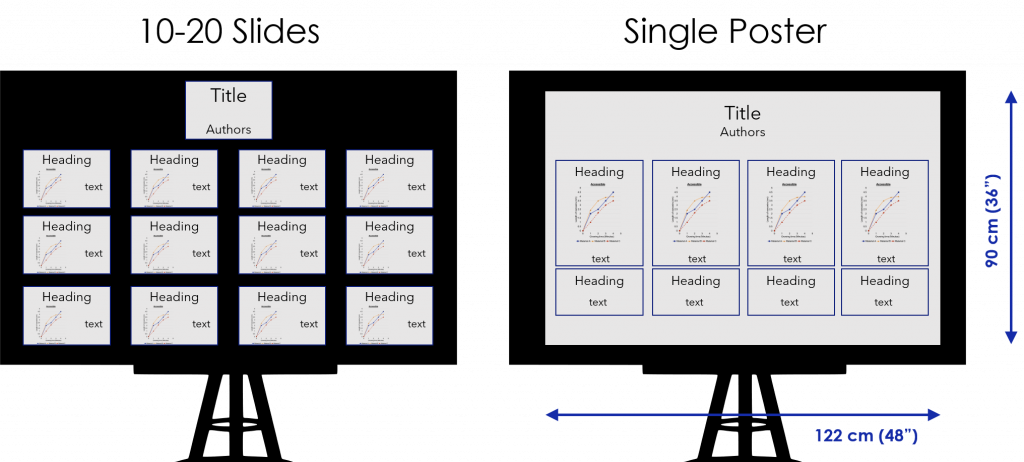
The overall size of your research poster ultimately depends on the dimensions of the provided space at the conference or research poster gallery. The poster orientation can be horizontal or vertical, with horizontal being the most common. In general, research posters measure 48 x 36 inches or are an A0 paper size.
A virtual poster can be the same proportions as the printed research poster, but you have more leeway regarding the dimensions. Virtual research posters should fit on a screen with no need to scroll, with 1080p resolution as a standard these days. A horizontal presentation size is ideal for that.
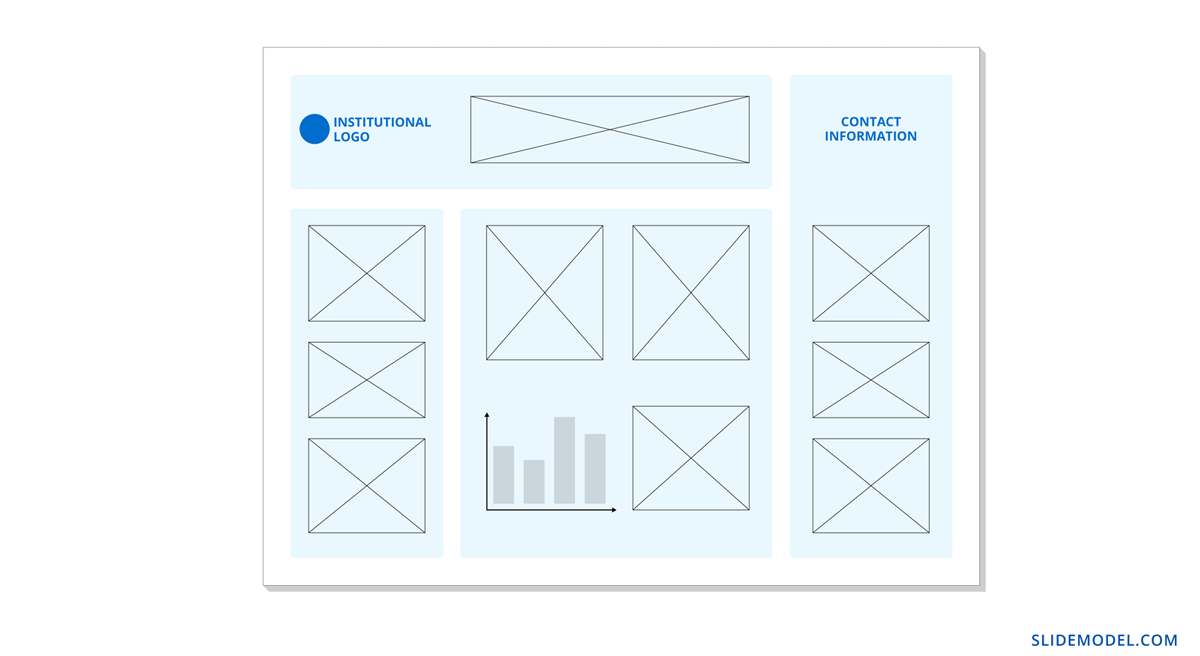
A research poster presentation has a standard layout of 2–5 columns with 2–3 sections each. Typical structures say to separate the content into four sections; 1. A horizontal header 2. Introduction column, 3. Research/Work/Data column, and 4. Conclusion column. Each unit includes topics that relate to your poster’s objective. Here’s a generalized outline for a poster presentation:
- Condensed Abstract
- Objectives/Purpose
- Methodology
- Recommendations
- Implications
- Acknowledgments
- Contact Information
The overview content you include in the units depends on your poster presentations’ theme, topic, industry, or field of research. A scientific or academic poster will include sections like hypothesis, methodology, and materials. A marketing analysis poster will include performance metrics and competitor analysis results.
There’s no way a poster can hold all the information included in your research paper or analysis report. The poster is an overview that invites the audience to want to find out more. That’s where supplement material comes in. Create a printed PDF handout or card with a QR code (created using a QR code generator ). Send the audience to the best online location for reading or downloading the complete paper.
What Makes a Poster Presentation Good and Effective?
For your poster presentation to be effective and well-received, it needs to cover all the bases and be inviting to find out more. Stick to the standard layout suggestions and give it a unique look and feel. We’ve put together some of the most critical research poster-creation tips in the list below. Your poster presentation will perform as long as you check all the boxes.
The information you choose to include in the sections of your poster presentation needs to be cohesive. Train your editing eye and do a few revisions before presenting. The best way to look at it is to think of The Big Picture. Don’t get stuck on the details; your attendees won’t always know the background behind your research topic or why it’s important.
Be cohesive in how you word the titles, the length of the sections, the highlighting of the most important data, and how your oral presentation complements the printed—or virtual—poster.
The most important characteristic of your poster presentation is its readability and clarity. You need a poster presentation with a balanced design that’s easy to read at a distance of 1.5 meters or 4 feet. The font size and spacing must be clear and neat. All the content must suggest a visual flow for the viewer to follow.
That said, you don’t need to be a designer to add something special to your poster presentation. Once you have the standard—and recognized—columns and sections, add your special touch. These can be anything from colorful boxes for the section titles to an interesting but subtle background, images that catch the eye, and charts that inspire a more extended look.
Storytelling is a presenting technique involving writing techniques to make information flow. Firstly, storytelling helps give your poster presentation a great introduction and an impactful conclusion.
Think of storytelling as the invitation to listen or read more, as the glue that connects sections, making them flow from one to another. Storytelling is using stories in the oral presentation, for example, what your lab partner said when you discovered something interesting. If it makes your audience smile and nod, you’ve hit the mark. Storytelling is like giving a research presentation a dose of your personality, and it can help turning your data into opening stories .
Design Tips For Creating an Effective Research Poster Presentation
The section above briefly mentioned how important design is to your poster presentation’s effectiveness. We’ll look deeper into what you need to know when designing a poster presentation.
1. Font Characteristics
The typeface and size you choose are of great importance. Not only does the text need to be readable from two meters away, but it also needs to look and sit well on the poster. Stay away from calligraphic script typefaces, novelty typefaces, or typefaces with uniquely shaped letters.
Stick to the classics like a sans serif Helvetica, Lato, Open Sans, or Verdana. Avoid serif typefaces as they can be difficult to read from far away. Here are some standard text sizes to have on hand.
- Title: 85 pt
- Authors: 65 pt
- Headings: 36 pt
- Body Text: 24 pt
- Captions: 18 pt
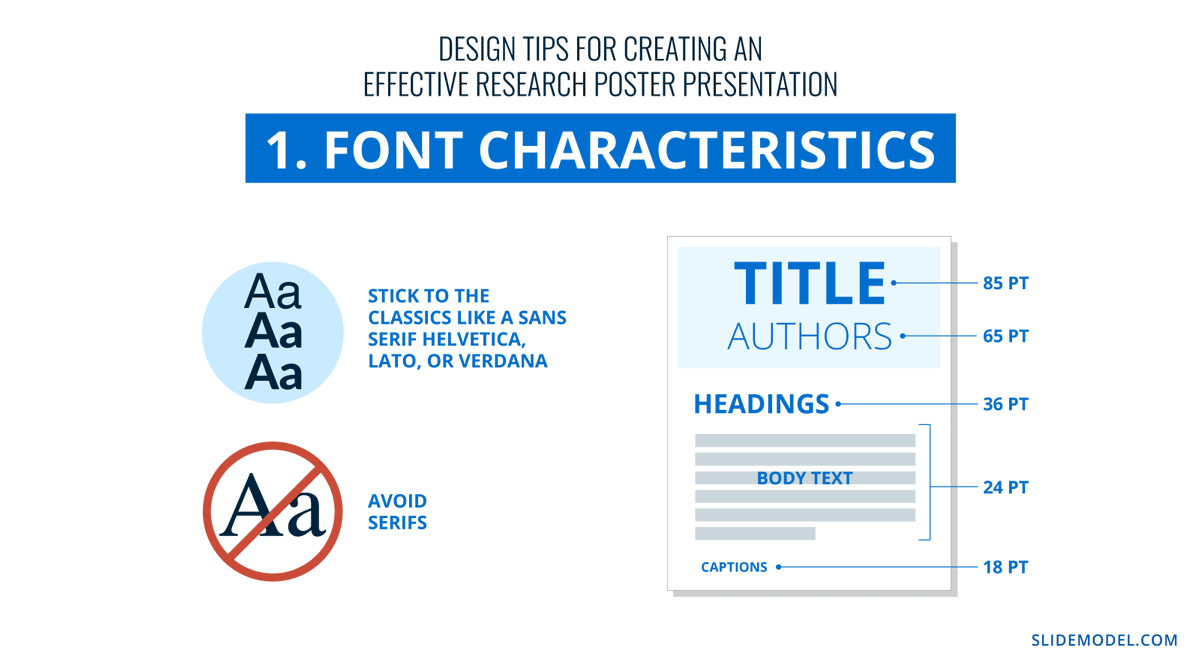
If you feel too prone to use serif typefaces, work with a font pairing tool that helps you find a suitable solution – and intend those serif fonts for heading sections only. As a rule, never use more than 3 different typefaces in your design. To make it more dynamic, you can work with the same font using light, bold, and italic weights to put emphasis on the required areas.
2. Color Pairing
Using colors in your poster presentation design is a great way to grab the viewer’s attention. A color’s purpose is to help the viewer follow the data flow in your presentation, not distract. Don’t let the color take more importance than the information on your poster.
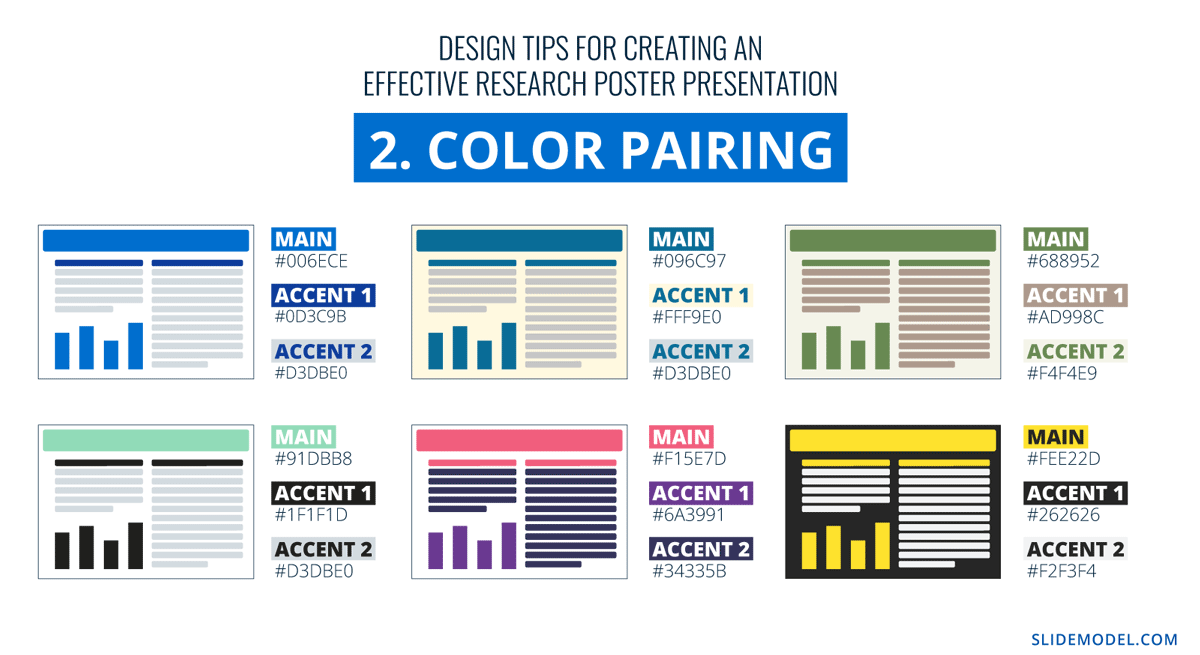
Choose one main color for the title and headlines and a similar color for the data visualizations. If you want to use more than one color, don’t create too much contrast between them. Try different tonalities of the same color and keep things balanced visually. Your color palette should have at most one main color and two accent colors.
Black text over a white background is standard practice for printed poster presentations, but for virtual presentations, try a very light gray instead of white and a very dark gray instead of black. Additionally, use variations of light color backgrounds and dark color text. Make sure it’s easy to read from two meters away or on a screen, depending on the context. We recommend ditching full white or full black tone usage as it hurts eyesight in the long term due to its intense contrast difference with the light ambiance.
3. Data Visualization Dimensions
Just like the text, your charts, graphs, and data visualizations must be easy to read and understand. Generally, if a person is interested in your research and has already read some of the text from two meters away, they’ll come closer to look at the charts and graphs.
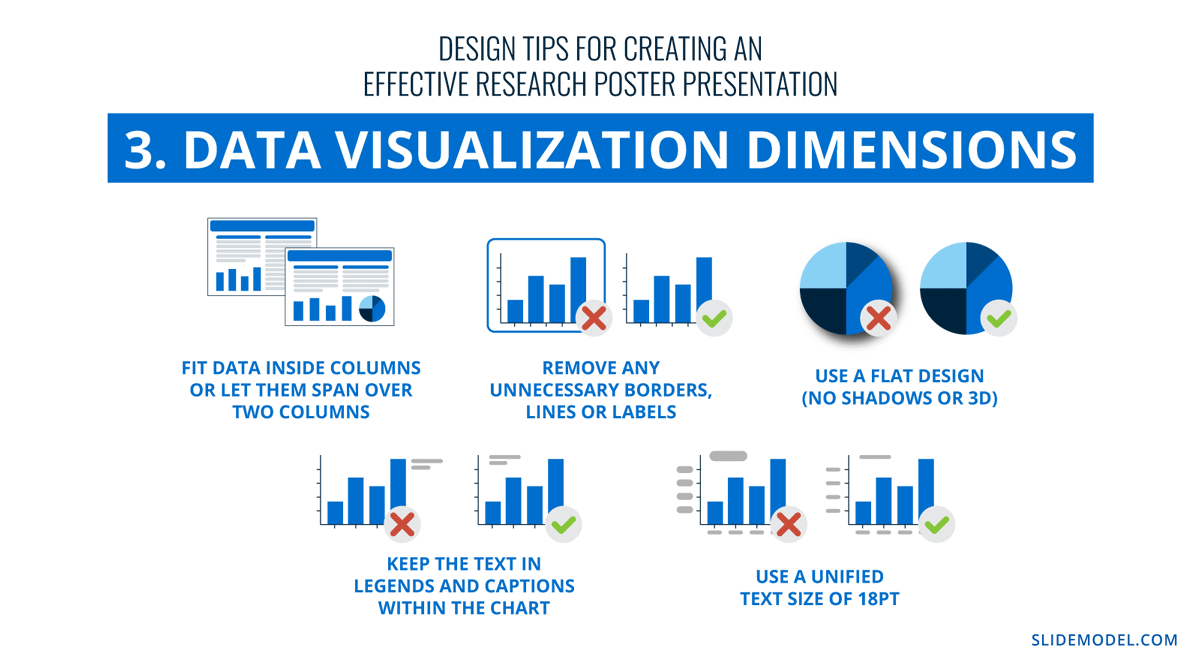
Fit data visualizations inside columns or let them span over two columns. Remove any unnecessary borders, lines, or labels to make them easier to read at a glance. Use a flat design without shadows or 3D characteristics. The text in legends and captions should stay within the chart size and not overflow into the margins. Use a unified text size of 18px for all your data visualizations.
4. Alignment, Margins, and White Space
Finally, the last design tip for creating an impressive and memorable poster presentation is to be mindful of the layout’s alignment, margins, and white space. Create text boxes to help keep everything aligned. They allow you to resize, adapt, and align the content along a margin or grid.
Take advantage of the white space created by borders and margins between sections. Don’t crowd them with a busy background or unattractive color.
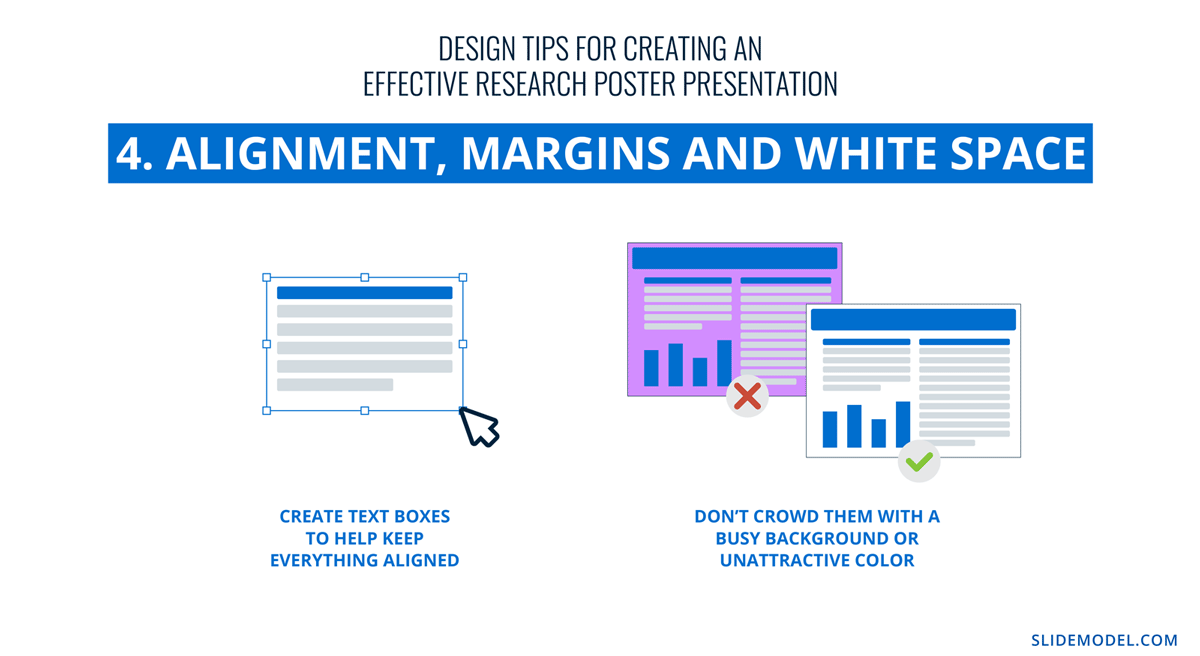
Calculate margins considering a print format. It is a good practice in case the poster presentation ends up becoming in physical format, as you won’t need to downscale your entire design (affecting text readability in the process) to preserve information.
There are different tools that you can use to make a poster presentation. Presenters who are familiar with Microsoft Office prefer to use PowerPoint. You can learn how to make a poster in PowerPoint here.
Poster Presentation Examples
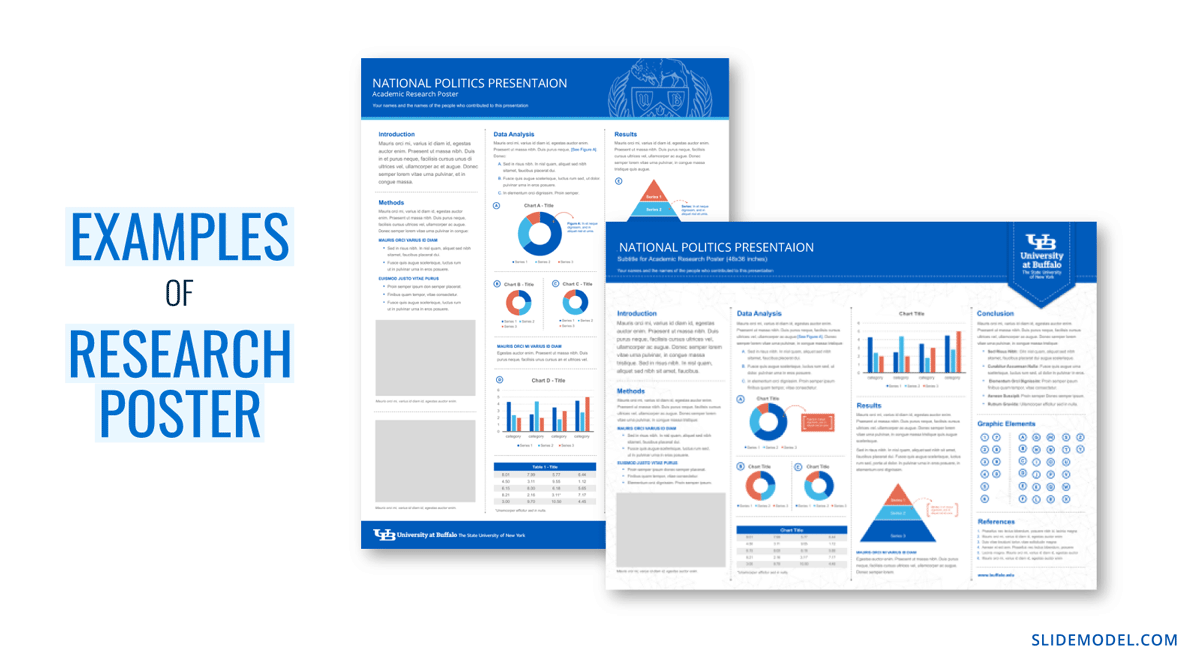
Before you start creating a poster presentation, look at some examples of real research posters. Get inspired and get creative.
Research poster presentations printed and mounted on a board look like the one in the image below. The presenter stands to the side, ready to share the information with visitors as they walk up to the panels.
With more and more conferences staying virtual or hybrid, the digital poster presentation is here to stay. Take a look at examples from a poster session at the OHSU School of Medicine .
Use SlideModel templates to help you create a winning poster presentation with PowerPoint and Google Slides. These poster PPT templates will get you off on the right foot. Mix and match tables and data visualizations from other poster slide templates to create your ideal layout according to the standard guidelines.
If you need a quick method to create a presentation deck to talk about your research poster at conferences, check out our Slides AI presentation maker. A tool in which you add the topic, curate the outline, select a design, and let AI do the work for you.
1. One-pager Scientific Poster Template for PowerPoint
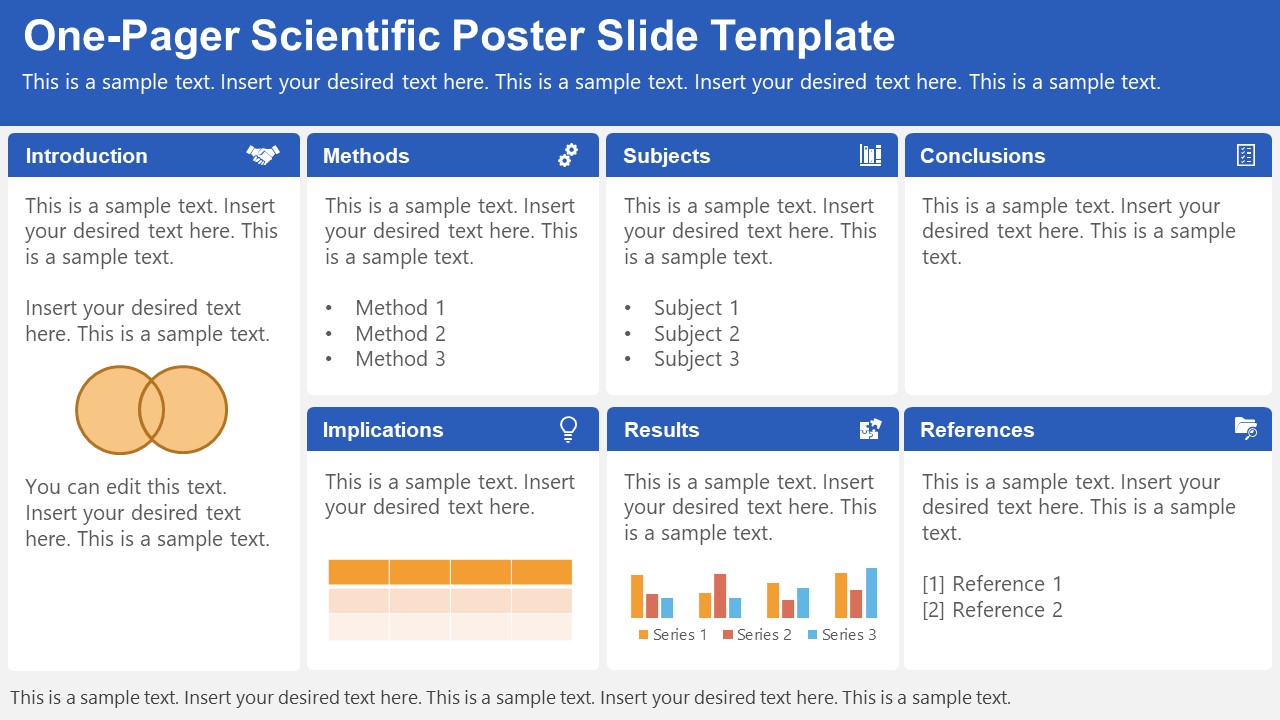
A PowerPoint template tailored to make your poster presentations an easy-to-craft process. Meet our One-Pager Scientific Poster Slide Template, entirely editable to your preferences and with ample room to accommodate graphs, data charts, and much more.
Use This Template
2. Eisenhower Matrix Slides Template for PowerPoint
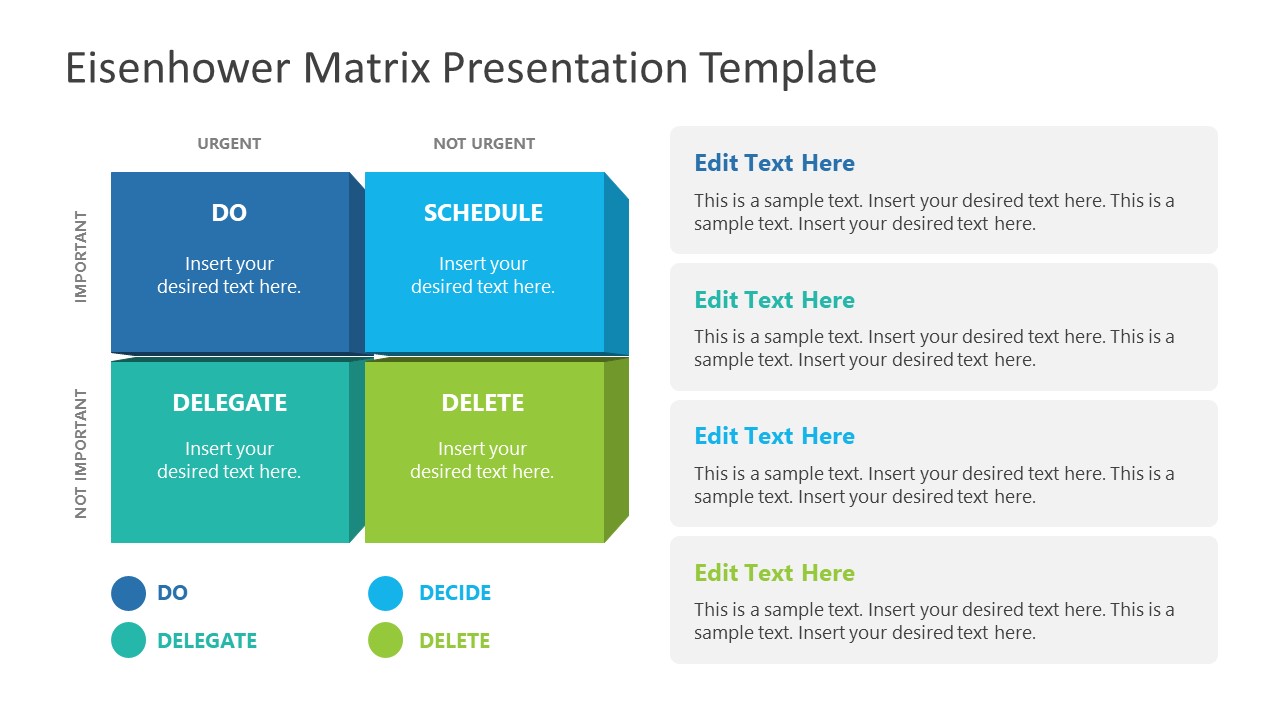
An Eisenhower Matrix is a powerful tool to represent priorities, classifying work according to urgency and importance. Presenters can use this 2×2 matrix in poster presentations to expose the effort required for the research process, as it also helps to communicate strategy planning.
3. OSMG Framework PowerPoint Template
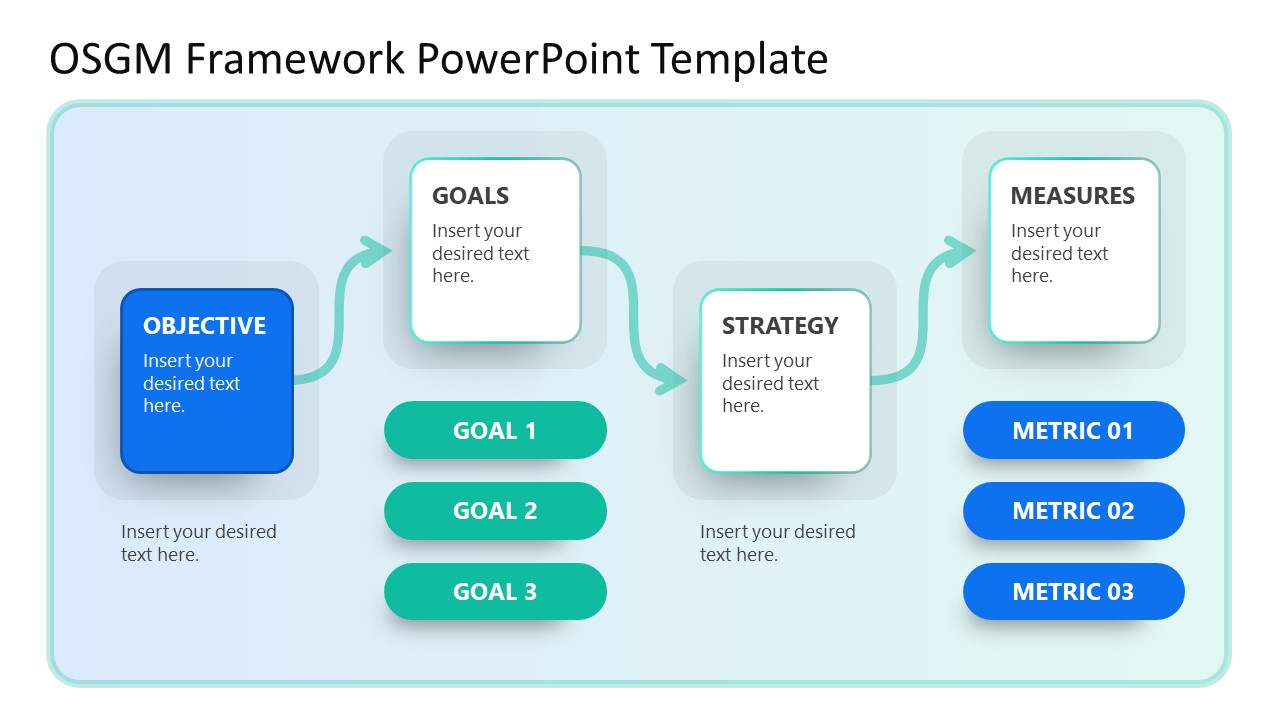
Finally, we recommend presenters check our OSMG Framework PowerPoint template, as it is an ideal tool for representing a business plan: its goals, strategies, and measures for success. Expose complex processes in a simplified manner by adding this template to your poster presentation.
Remember these three words when making your research poster presentation: develop, design, and present. These are the three main actions toward a successful poster presentation.
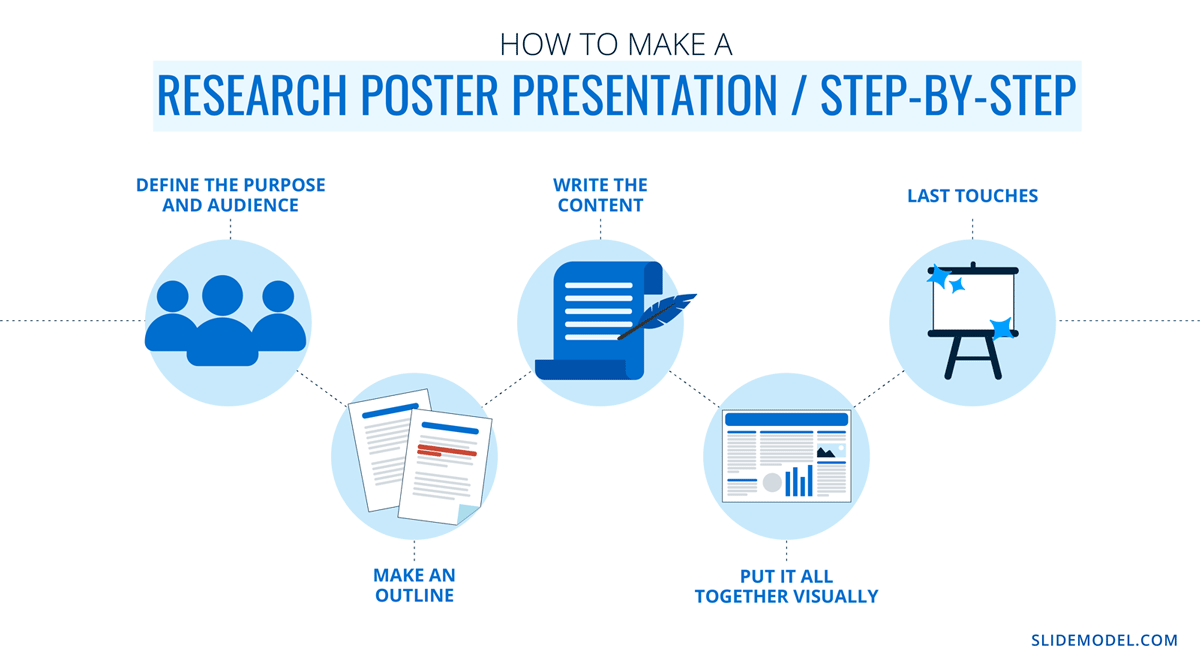
The section below will take you on a step-by-step journey to create your next poster presentation.
Step 1: Define the purpose and audience of your poster presentation
Before making a poster presentation design, you’ll need to plan first. Here are some questions to answer at this point:
- Are they in your field?
- Do they know about your research topic?
- What can they get from your research?
- Will you print it?
- Is it for a virtual conference?
Step 2: Make an outline
With a clear purpose and strategy, it’s time to collect the most important information from your research paper, analysis, or documentation. Make a content dump and then select the most interesting information. Use the content to draft an outline.
Outlines help formulate the overall structure better than going straight into designing the poster. Mimic the standard poster structure in your outline using section headlines as separators. Go further and separate the content into the columns they’ll be placed in.
Step 3: Write the content
Write or rewrite the content for the sections in your poster presentation. Use the text in your research paper as a base, but summarize it to be more succinct in what you share.
Don’t forget to write a catchy title that presents the problem and your findings in a clear way. Likewise, craft the headlines for the sections in a similar tone as the title, creating consistency in the message. Include subtle transitions between sections to help follow the flow of information in order.
Avoid copying/pasting entire sections of the research paper on which the poster is based. Opt for the storytelling approach, so the delivered message results are interesting for your audience.
Step 4: Put it all together visually
This entire guide on how to design a research poster presentation is the perfect resource to help you with this step. Follow all the tips and guidelines and have an unforgettable poster presentation.
Moving on, here’s how to design a research poster presentation with PowerPoint Templates . Open a new project and size it to the standard 48 x 36 inches. Using the outline, map out the sections on the empty canvas. Add a text box for each title, headline, and body text. Piece by piece, add the content into their corresponding text box.
Transform the text information visually, make bullet points, and place the content in tables and timelines. Make your text visual to avoid chunky text blocks that no one will have time to read. Make sure all text sizes are coherent for all headings, body texts, image captions, etc. Double-check for spacing and text box formatting.
Next, add or create data visualizations, images, or diagrams. Align everything into columns and sections, making sure there’s no overflow. Add captions and legends to the visualizations, and check the color contrast with colleagues and friends. Ask for feedback and progress to the last step.
Step 5: Last touches
Time to check the final touches on your poster presentation design. Here’s a checklist to help finalize your research poster before sending it to printers or the virtual summit rep.
- Check the resolution of all visual elements in your poster design. Zoom to 100 or 200% to see if the images pixelate. Avoid this problem by using vector design elements and high-resolution images.
- Ensure that charts and graphs are easy to read and don’t look crowded.
- Analyze the visual hierarchy. Is there a visual flow through the title, introduction, data, and conclusion?
- Take a step back and check if it’s legible from a distance. Is there enough white space for the content to breathe?
- Does the design look inviting and interesting?
An often neglected topic arises when we need to print our designs for any exhibition purpose. Since A0 is a hard-to-manage format for most printers, these poster presentations result in heftier charges for the user. Instead, you can opt to work your design in two A1 sheets, which also becomes more manageable for transportation. Create seamless borders for the section on which the poster sheets should meet, or work with a white background.
Paper weight options should be over 200 gsm to avoid unwanted damage during the printing process due to heavy ink usage. If possible, laminate your print or stick it to photographic paper – this shall protect your work from spills.
Finally, always run a test print. Gray tints may not be printed as clearly as you see them on screen (this is due to the RGB to CMYK conversion process). Other differences can be appreciated when working with ink jet plotters vs. laser printers. Give yourself enough room to maneuver last-minute design changes.
Presenting a research poster is a big step in the poster presentation cycle. Your poster presentation might or might not be judged by faculty or peers. But knowing what judges look for will help you prepare for the design and oral presentation, regardless of whether you receive a grade for your work or if it’s business related. Likewise, the same principles apply when presenting at an in-person or virtual summit.
The opening statement
Part of presenting a research poster is welcoming the viewer to your small personal area in the sea of poster presentations. You’ll need an opening statement to pitch your research poster and get the viewers’ attention.
Draft a 2 to 3-sentence pitch that covers the most important points:
- What the research is
- Why was it conducted
- What the results say
From that opening statement, you’re ready to continue with the oral presentation for the benefit of your attendees.
The oral presentation
During the oral presentation, share the information on the poster while conversing with the interested public. Practice many times before the event. Structure the oral presentation as conversation points, and use the poster’s visual flow as support. Make eye contact with your audience as you speak, but don’t make them uncomfortable.
Pro Tip: In a conference or summit, if people show up to your poster area after you’ve started presenting it to another group, finish and then address the new visitors.
QA Sessions
When you’ve finished the oral presentation, offer the audience a chance to ask questions. You can tell them before starting the presentation that you’ll be holding a QA session at the end. Doing so will prevent interruptions as you’re speaking.
If presenting to one or two people, be flexible and answer questions as you review all the sections on your poster.
Supplemental Material
If your audience is interested in learning more, you can offer another content type, further imprinting the information in their minds. Some ideas include; printed copies of your research paper, links to a website, a digital experience of your poster, a thesis PDF, or data spreadsheets.
Your audience will want to contact you for further conversations; include contact details in your supplemental material. If you don’t offer anything else, at least have business cards.
Even though conferences have changed, the research poster’s importance hasn’t diminished. Now, instead of simply creating a printed poster presentation, you can also make it for digital platforms. The final output will depend on the conference and its requirements.
This guide covered all the essential information you need to know for creating impactful poster presentations, from design, structure and layout tips to oral presentation techniques to engage your audience better .
Before your next poster session, bookmark and review this guide to help you design a winning poster presentation every time.

Like this article? Please share
Cool Presentation Ideas, Design, Design Inspiration Filed under Design
Related Articles
Filed under Design • January 11th, 2024
How to Use Figma for Presentations
The powerful UI/UX prototyping software can also help us to craft high-end presentation slides. Learn how to use Figma as a presentation software here!

Filed under Design • December 28th, 2023
Multimedia Presentation: Insights & Techniques to Maximize Engagement
Harnessing the power of multimedia presentation is vital for speakers nowadays. Join us to discover how you can utilize these strategies in your work.
Filed under Google Slides Tutorials • December 15th, 2023
How to Delete a Text Box in Google Slides
Discover how to delete a text box in Google Slides in just a couple of clicks. Step-by-step guide with images.
Leave a Reply
Customize Your Path
Filters Applied
Customize Your Experience.
Utilize the "Customize Your Path" feature to refine the information displayed in myRESEARCHpath based on your role, project inclusions, sponsor or funding, and management center.
Poster and oral presentations
Need assistance with poster presentations?
Get help with poster presentations.
Contact the Research Navigators:
- Email: [email protected]
Poster and oral presentations are typically delivered to academic colleagues at conferences or congresses. Here are some best practices and resources to help develop the content and visuals for a high-impact poster, and plan and practice memorable oral presentations.
The "Related Resources" on this page can be used to tap into Duke’s hub of templates, guides, and services to support researchers developing their presentations.
The Duke Medical Center Library has tips for things to keep in mind before working through the development of a poster presentation, and the Duke University Libraries' Center for Data and Visualization Sciences recorded a talk on preparing effective academic posters .
- Just like with any other publication, the specifications from the conference should be read and understood – there are often size limits or font requirements to keep in mind.
- A good title is critical for posters since presenters get just a few seconds to attract conference goers who are passing by. Make sure the title briefly and memorably portrays the most interesting or central finding of the work.
- Energy should be focused on a solid abstract, as the poster is simply a blown-up visualization of that summary.
- Less is more in poster design. Rather than shrinking fonts to fit the commentary, the commentary should be shrunk to fit the space on the poster, while retaining a readable font and plenty of white space.
The Thompson Writing Program has great general guidance on oral presentations, summarized throughout this page. There are several training opportunities listed in this page's "Related Resources" that can help researchers at all stages to hone their presentation skills.
- Preparing for an oral presentation will take the majority of a researcher's time. The goal of the talk should be fully understood as typically no more than 3-5 key points will be covered in a presentation; the audience and the time allotted should be carefully considered.
- Consideration of “guideposts” for the audience should be given. It is especially important in oral deliveries that information is organized in to meaningful blocks for the audience. Transitions should be emphasized during the presentation.
- Rather than creating a word-for-word speech, researchers should create a plan for each section, idea or point. By reading written points, delivery can be kept fresh.
- To engage audiences, it is a good idea to make strongest points first, and in a memorable way. While background and introduction sections are common in academic presentations, they are often already known to the audience.
The Duke Medical Center Library has tutorials, best practices for general design, and strategies for a high-impact poster presentations. Bass Connections also provides guidance on poster design.
Some important things to keep in mind are:
- Keeping posters simple and focusing on two things: Strong visualizations and small blocks of supporting text. Remember the audience; they will be standing a few feet away. Make sure the content is visible from afar.
- Follow brand guidelines from Duke or Duke School of Medicine . When representing Duke at a conference, it is best practice to align the presentation with institutional standards, including appropriate logos and color schemes.
- Avoid violating copyright protections. Include only images created specifically for this purpose, or use stock photography provided by Duke or other vendors.
- Visualizing data tells the story. The Center for Data and Visualization Sciences has workshops, consultations and other resources to ensure that graphical representations of data are effective.
- Poster presentations can be designed using a variety of software (PowerPoint, Illustrator, Keynote, Inkscape), and templates. When choosing software or templates, consideration should be given to accessibility and understanding by everyone involved in creating the presentation.
- Contact information, citations and acknowledgements: On posters, key articles may be noted or images needing references included. For oral and poster presentations, key contributors should be recognized. Funding sources should also be mentioned on posters and in oral presentations.
- A link or QR code should be included for supplemental materials, citations, movies, etc.
- Before a poster is printed, someone with fresh eyes should review it! Reprinting posters is costly and can take time. There are many options for printing, some on paper and some on fabric, with production times varying. The Medical Center Library has some local options to suggest.
- Practicing in a space that is similar to the actual presentation is a good idea, and doing so within the allotted time. Finishing early to allow good Q&A is also a good idea.
- Family, trusted friends, or colleagues can be great test audiences, and can provide valuable feedback.
- Preparation and practice should be started early and repeated often.
- If it is an important address, researchers may want to videotape a rehearsal run to review and improve performance.
- If a presentation is being digitized, release or permission forms may be needed. Duke has resources available via Scholarworks.
- Once a poster session or oral presentation has been completed, researchers should be sure to add it to their CV or biosketch.
University Library, University of Illinois at Urbana-Champaign

Research Posters : Oral Presentations
- Elements of a poster
- Step by step
- Visualizations & images
- Illinois logo
- Archiving - Grad Students
- More Resources
- Oral Presentations
- 2024 Undergraduate Research Symposium This link opens in a new window
TIPS FOR ORAL PRESENTATIONS
- How to give a great oral presentation
- Ten Simple Rules for Making Good Oral Presentations
- Top 15 tips to give a good oral presentation
- Designing PowerPoint Slides for a Scientific Presentation
The Speaking Center
The Library offers speaking consultation and practice at the The Speaking Center . Schedule an appointment with us and practice giving your presentation.
CONSIDERING YOUR CONTENT
I have been accepted to present an oral presentation at the Symposium; how do I upload my talk? All oral presentation rooms are equipped with PC laptops (no Apple Mac's) so be sure the format of your presentation is compatible with PCs. In general, we recommend that students save their presentations in two formats: the first being a .PPT (Microsoft PowerPoint) file, and the back-up being a .PDF (Adobe Acrobat) file. Please bring these files on a portable drive (flash drive, etc.) to your oral presentation panel and be sure to show up early to allow enough time to download it to the computer prior to the start of the session.
- Think of, or research, an attention grabber: a story, fact or statistic, or other interesting piece of information that will help draw in the audience right away and frame the talk in a minute or less.
- Focus only on the 3 most important points. Introduce them at the beginning, and repeat them at the very end.
- Have 2-3 specifics/particular points that fall within each of the three categories, and, if possible, also have a brief story or example to illustrate each main point.
- Write out transitions between major points and examples (and practice them) so your speech will flow better. Example: “So far we’ve discussed [x], but on the other end of the spectrum is this other important aspect, [y].”
- Be gender neutral. Even though it may not technically be grammatically correct, today it is acceptable in formal presentations in most contexts to use “they” and “them” instead of she/he, him/her.
- Try, if you can, to incorporate a bit of tasteful humor. It shouldn’t be forced; it needs to fit in with the rest of the speech and feel natural to be funny. Don’t be afraid to improvise during your talk, if you can do so comfortably.
- Have someone else read your speech, or alternately, practice your presentation in front of them – so they can critique the content and delivery.
PRESENTATION DELIVERY
1. Practice and prepare. Practice in front of a mirror. Take a video or audio recording of yourself. Rehearse the presentation in your head when you are unable to rehearse it aloud. With the right amount of practice and preparation, the words will flow more easily on presentation day. Don’t strive for absolute perfection, though: too much rehearsal may make you come across stiff and stifled, not natural.
2. When practicing, pay attention to your voice inflections, including which words and syllables you will emphasize. Be deliberate. Your voice inflections and emphases will affect your audience members’ interpretation, comprehension, and retention of the material.
3. Know how you are going to stand, gesture, and move your body. Practice walking around a bit – moving toward your audience and back towards the screen/lectern, for example. Try to face your audience at all times, and look around the room at individual audience members as much as possible. Make the audience feel like you are directly addressing them. While some movement is fine and can complement your style, be careful not to walk or pace too much; this can be distracting.
4. Wear comfortable professional clothing and comfortable shoes. You will not want to be distracted because you are uncomfortable.
5. Be early. If you are running late, you will be more nervous and have less time to prepare yourself mentally.
6. On the day of the talk, take 10-15 minutes before your presentation to relax, do some deep breathing, and keep your mind off of the presentation for a bit. You want to be relaxed during your presentation.
7. Be confident! Be passionate! Be energetic! You’ve got this. Don’t expect to be perfect, but if you have practiced and you are confident, it will show and make for a great presentation.
- << Previous: More Resources
- Next: 2024 Undergraduate Research Symposium >>
- Last Updated: Apr 9, 2024 12:09 PM
- URL: https://guides.library.illinois.edu/poster

Preparing oral and poster presentations for conferences
As a PhD student, attending conferences is an exciting part of academic life. Conferences are a chance to share your research findings, learn novel ideas or techniques and travel, whether that is locally, further afield or even internationally. A crucial aspect to conference attending is conveying your research to the wider scientific community, through either a poster or oral presentation.
Preparing your research to present at a conference is a balance. You need to include the same details as you would put in a paper or report, but make it concise to fit reasonably in a poster format, or within a specific talk length, such as 10 minutes. When writing a talk or poster for a specific conference, investigating the style and content of previous years abstracts may help to peg yours at a suitable level. Before you start, check the conference guidelines on oral presentation outlines, poster size, and orientation. Although most conferences allow A0 portrait posters, some are different and it’s advisable to check this before writing.
Preparing your poster
Generally, posters follow a bullet point style divided into four main sections:
- Introduction or Background
- Discussion or Conclusions.
However, there are some other areas of the poster that need attention too.
Firstly, a snappy title is a must. The title must cover the basic outline of the study, yet be intriguing, making the viewer want to read on. The title must be considered during abstract preparation, as whatever you name your abstract will be your poster title. Author names and affiliations sit below the title; the order of this can be important but must be agreed by your research group before poster publication.
The introduction covers the background details of the research involved, using current literature and references. The aims and objectives of the research must be in the introduction, and generally sits well at the end just before the method section to give a sense of flow.
Methods covers obviously what you did to achieve your results. It’s good to be aware of any ethical approval gained for the study, and noting participant numbers, genders and ages, statistical methods used and any chemical in their full unabbreviated names initially, with subsequent references to the ingredients by the standard abbreviations. If the method is tricky to explain, a diagram or photo may help to illustrate, and it is not necessary to repeat the methods in words.
The results section needs to cover all relevant findings. Tables or figures can really help show data, so be imaginative! You’ll need to include statistical p-values to show significances. Finally, the discussion or conclusion section highlights the key findings from your results in punchy language as a ‘take home message’. These need to be clear and concise, covering the exact findings and if possible the relevance of findings to the study and scientific community as a whole.
Oral presentations
For oral presentations the same headings should be followed, with clear simple slides. Keep the number of slides to a minimum to keep the length of the talk on track. A good guideline is around one slide per minute. Set the scene with a clear introduction to the work, indicating the relevance of the study to the general scientific community. Highlight the study aims and objectives, and unlike a poster, you may want to include a hypothesis for further clarity. Diagrams may also help to describe methodology, and helps to keep audience attention as they must listen to you fully to understand the technique.
Results can also be shown on graphs and figures; be careful with tables, as these can appear daunting to the viewer, unless you clearly highlight the numbers or significances of importance to your work. Throughout the results section explain what each experiment or figure means, what is the finding? This will help you lead directly into the conclusions, and you can repeat the key findings already covered in the results, and give a clear take home message to your audience.
And finally...
Whether you’re giving a poster or a talk at a conference, be confident. Who knows your work better than you? This will help you tackle any questions and comments posed, and give you a chance to meet fellow researchers and possible future collaborators. Project your voice, face your audience and above all enjoy yourself!
Dr Caroline Withers
Poster Presentations
Poster presentations (pdf), considering the audience.
As with any presentation, you should consider who is likely to be listening. In some cases, your audience is going to be people who know a fair bit about your topic or discipline. In other cases, such as a poster session for a family weekend, you are likely to get some people who know the topic, but also many more people who are just curious about the research that is going on. You should plan to adapt based on the person with whom you are interacting. Ask yourself: what does this person likely know and what will they want to know?
Preparing a Pitch
You should plan for having a short (about 2 minutes) summary overview of the project that can give a listener a taste of what you did. You can use that time to answer three big questions:
- What is the topic?
- What did you find? Or What are the results?
- Why is this important?
People will ask follow-up questions if they are interested in learning more or if they are confused about something you said. Think of this pitch as an appetizer: you want to whet someone’s appetite to learn more about your topic, but that small bite may be sufficient for some people.
When thinking about the pitch, keep in mind that you do not need to verbally address every component of the poster in your first remarks. You should, however, be prepared to talk about each component if asked. You should never read directly from the poster to the audience!
Posters with a Partner
If you worked on your project with another person, you should both be prepared to give the basic pitch. You may have parts of the project that each of you is more comfortable talking about in detail, but each of you should know the fundamentals in case you are asked. Then, you can pass off a question to the other person if necessary.
Preparing for Questions
You should anticipate questions from the people who view your poster. One part of your preparation can be brainstorming the likely questions and then practicing answering those questions. If you are presenting your poster at a professional meeting with other people from the discipline, you can expect more technical or content questions than if you are presenting to a more general audience. Some likely general questions you may get are:
- What made you interested in this topic?
- Why was this approach/tool/theory the most appropriate for your project?
- Where do you go from here with this research?
- What was the most interesting/surprising/challenging part of this project?
- How does this project relate to other work you are doing?
Regardless of the question, it’s ok to take a breath and focus before you start to answer. Your response should be focused and succinct as well as appropriate for the audience. If you aren’t sure what someone is asking, ask for clarification!
Ideally, the poster session will give you an opportunity to engage in a dialogue about your work. In fact, that’s one of the main draws of posters as a way to disseminate research findings.
Interacting with Your Poster
You and your poster are a team, working together to present your ideas. Once your poster is mounted, you should position yourself so that you are close to your poster but not blocking it from passersby, especially the title. Additionally:
- You should feel free to move as necessary to show different parts of the poster.
- Gesture to the relevant parts of the poster. You should use your whole hand to point toward something rather than just pointing a finger. Graphs and other data are excellent parts of a poster for gesturing. Avoid turning your back on your audience to gesture. Use the arm closest to the poster to gesture so you are not gesturing across your body or turning.
- Avoid standing with your arms crossed or otherwise looking defensive both while talking and while waiting for an audience. Closed off body language makes you appear less welcoming for someone to approach.
- Don’t forget to smile. Even if you are feeling nervous, you can “fake it ‘til you make it” by adopting a smile and acting confident.
Office / Department Name
Oral Communication Center
Contact Name
Amy Gaffney
Oral Communication Center Director

Help us provide an accessible education, offer innovative resources and programs, and foster intellectual exploration.
Site Search
Posters & Oral Presentations
Good scientific research involves a sound methodology and a novel idea that can be tested simply and repeatedly to give valid, trustworthy results. However, even the most clinically significant research is useless if it is not communicated successfully. Scientific ideas are novel, sometimes simple in theory, but most always complex in technique. These attributes of research make it necessary to use all available means of presentation. The most common media for scientists to communicate with the general public is primary journal articles. However, posters and oral presentations are also affective because they allow scientists to be in direct contact with their audience. This provides both parties an opportunity to ask pertinent questions to add clarity to the work being presented.
A poster is an exciting way for scientists to present their research. It, just as a primary research article, includes all aspects of the scientific method. A title that is brief, but specific, an abstract, an introduction, material and methods, results, and a conclusion are some headings that can appear on a poster. Also, references and acknowledgments are sometimes are included. A poster is different from a written manuscript or an oral presentation because it is mostly graphical. As such, it is important to design a poster that is visually pleasing by focusing on charts, graphs, and pictures and minimizing lengthy introductions and discussions. Highlighting all significant information with the use of bullets is essential because if further explanation is needed the audience will simply ask for it.
Oral presentations are yet another avenue for scientists to share their findings with the world. Although it can be challenging to present years of works within fifteen minutes, oral presentations can be a rewarding experience because you are the only one front of an audience whose attention you know have. Of course this emphasizes the need to speak clearly and concisely with choice words that engross the audience. Again, just as with written manuscript and posters the format of oral presentations can also vary, but essentially it must include logical, easy-to-understand events that are presented in a matter with respect to the scientific method.
Electronic Resources
Poster Presentation http://www.ncsu.edu/project/posters
This is an excellent site that covers all aspects of a poster presentation from creating a poster to presenting one. It also provides several examples with critiques for each sample. Lastly, it has a quick reference page with helpful tips for delivering a successful poster presentation.
Oral Presentation http://www.kumc.edu/SAH/OTEd/jradel/Preparing_talks/103.html
This site is cited by the NIH and is quite useful when designing an oral presentation. It addresses all aspects of a scientific talk from planning and preparing to practicing and presenting. It is brief and easy to follow with helpful tips on how to prepare for the question/answer session.
Document Resources
Scientific Poster: Tips, Significance, Design, Templates and Presentation
This document provides tips and temples for designing a poster presentation. It also discusses the significance of a poster presentation and includes a section that gives advice on how to present successfully.
Oral Presentations: Tips, Significance, Design, Guidelines & Presentation
This document provides tips and guidelines for designing an oral presentation. It also discusses the significance of an oral presentation and includes a section that gives advice on how to present successfully.
- Interlibrary Loan and Scan & Deliver
- Course Reserves
- Purchase Request
- Collection Development & Maintenance
- Current Negotiations
- Ask a Librarian
- Instructor Support
- Library How-To
- Research Guides
- Research Support
- Study Rooms
- Research Rooms
- Partner Spaces
- Loanable Equipment
- Print, Scan, Copy
- 3D Printers
- Poster Printing
- OSULP Leadership
- Strategic Plan
Research Posters and Presentations
- Poster Sections
- Day of Presentation
Science Librarian

1. Think of, or research, an attention grabber: a story, fact or statistic, or other interesting piece of information that will help draw in the audience right away and frame the talk in a minute or less.
2. Focus only on the 3 most important points. Introduce them at the beginning, and repeat them at the very end.
3. Have 2-3 specifics/particular points that fall within each of the three categories, and, if possible, also have a brief story or example to illustrate each main point.
4. Write out transitions between major points and examples (and practice them) so your speech will flow better. Example: “So far we’ve discussed [x], but on the other end of the spectrum is this other important aspect, [y].”
5. Be gender neutral. Even though it may not technically be grammatically correct, today it is acceptable in formal presentations in most contexts to use “they” and “them” instead of she/he, him/her.
6. Try, if you can, to incorporate a bit of tasteful humor. It shouldn’t be forced; it needs to fit in with the rest of the speech and feel natural to be funny. Don’t be afraid to improvise during your talk, if you can do so comfortably.
7. Have someone else read your speech, or alternately, practice your presentation in front of them – so they can critique the content and delivery.
1. Practice and prepare. Practice in front of a mirror. Take a video or audio recording of yourself. Rehearse the presentation in your head when you are unable to rehearse it aloud. With the right amount of practice and preparation, the words will flow more easily on presentation day. Don’t strive for absolute perfection, though: too much rehearsal may make you come across stiff and stifled, not natural.
2. When practicing, pay attention to your voice inflections, including which words and syllables you will emphasize. Be deliberate. Your voice inflections and emphases will affect your audience members’ interpretation, comprehension, and retention of the material.
3. Know how you are going to stand, gesture, and move your body. Practice walking around a bit – moving toward your audience and back towards the screen/lectern, for example. Try to face your audience at all times, and look around the room at individual audience members as much as possible. Make the audience feel like you are directly addressing them. While some movement is fine and can complement your style, be careful not to walk or pace too much; this can be distracting.
4. Wear comfortable professional clothing and comfortable shoes. You will not want to be distracted because you are uncomfortable.
5. Be early. If you are running late, you will be more nervous and have less time to prepare yourself mentally.
6. On the day of the talk, take 10-15 minutes before your presentation to relax, do some deep breathing, and keep your mind off of the presentation for a bit. You want to be relaxed during your presentation.
7. Be confident! Be passionate! Be energetic! You’ve got this. Don’t expect to be perfect, but if you have practiced and you are confident, it will show and make for a great presentation.
- << Previous: Design
- Next: Day of Presentation >>
- Last Updated: Oct 19, 2022 1:34 PM
- URL: https://guides.library.oregonstate.edu/researchposters

Contact Info
121 The Valley Library Corvallis OR 97331–4501
Phone: 541-737-3331
Services for Persons with Disabilities
In the Valley Library
- Oregon State University Press
- Special Collections and Archives Research Center
- Undergrad Research & Writing Studio
- Graduate Student Commons
- Tutoring Services
- Northwest Art Collection
Digital Projects
- Oregon Explorer
- Oregon Digital
- ScholarsArchive@OSU
- Digital Publishing Initiatives
- Atlas of the Pacific Northwest
- Marilyn Potts Guin Library
- Cascades Campus Library
- McDowell Library of Vet Medicine

An Emergency Physician’s Path pp 551–555 Cite as
Preparing Oral and Poster Presentations
- Kimberly M. Rathbun 5
- First Online: 02 March 2024
A poster or oral presentation is a great way to share your research project and get feedback. Designing a poster or preparing an oral presentation should be done within the guidelines set forth by the conference. Traditional posters and oral presentations convey the same information in different formats. When presenting your study, you should know all the details of the project and be able to field any questions from the audience.
This is a preview of subscription content, log in via an institution .
Buying options
- Available as PDF
- Read on any device
- Instant download
- Own it forever
- Available as EPUB and PDF
- Compact, lightweight edition
- Dispatched in 3 to 5 business days
- Free shipping worldwide - see info
Tax calculation will be finalised at checkout
Purchases are for personal use only
Suggested Readings
Barker E, Phillips V. Creating conference posters: structure, form and content. J Perioper Pract. 2021;31(7–8):296–9.
PubMed PubMed Central Google Scholar
Gundogan B, Koshy K, Kurar L, Whitehurst K. How to make an academic poster. Ann Med Surg (Lond). 2016;11:69–71.
Article PubMed Google Scholar
Naegle KM. Ten simple rules for effective presentation slides. PLoS Comput Biol. 2021;17(12):e1009554.
Article CAS PubMed PubMed Central Google Scholar
Download references
Author information
Authors and affiliations.
Department of Emergency Medicine, AU/UGA Medical Partnership, Athens, GA, USA
Kimberly M. Rathbun
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Kimberly M. Rathbun .
Editor information
Editors and affiliations.
Emergency Medicine, Penn State Milton S. Hershey Medical Center, Hershey, PA, USA
Robert P. Olympia
Elizabeth Barrall Werley
Jeffrey S. Lubin
MD Anderson Cancer Center at Cooper, Cooper Medical School of Rowan University, Camden, NJ, USA
Kahyun Yoon-Flannery
Rights and permissions
Reprints and permissions
Copyright information
© 2023 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter.
Rathbun, K.M. (2023). Preparing Oral and Poster Presentations. In: Olympia, R.P., Werley, E.B., Lubin, J.S., Yoon-Flannery, K. (eds) An Emergency Physician’s Path. Springer, Cham. https://doi.org/10.1007/978-3-031-47873-4_79
Download citation
DOI : https://doi.org/10.1007/978-3-031-47873-4_79
Published : 02 March 2024
Publisher Name : Springer, Cham
Print ISBN : 978-3-031-47872-7
Online ISBN : 978-3-031-47873-4
eBook Packages : Medicine Medicine (R0)
Share this chapter
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Publish with us
Policies and ethics
- Find a journal
- Track your research

Want to create or adapt books like this? Learn more about how Pressbooks supports open publishing practices.
21 Poster Presentations
Read time: 8 minutes
This section will outline how to communicate your scientific research in the format of a poster presentation, and provide guidance on designing your poster.
Sections in this chapter
Environment and audience, poster vs. talk, verbal aspect, poster design, virtual posters.
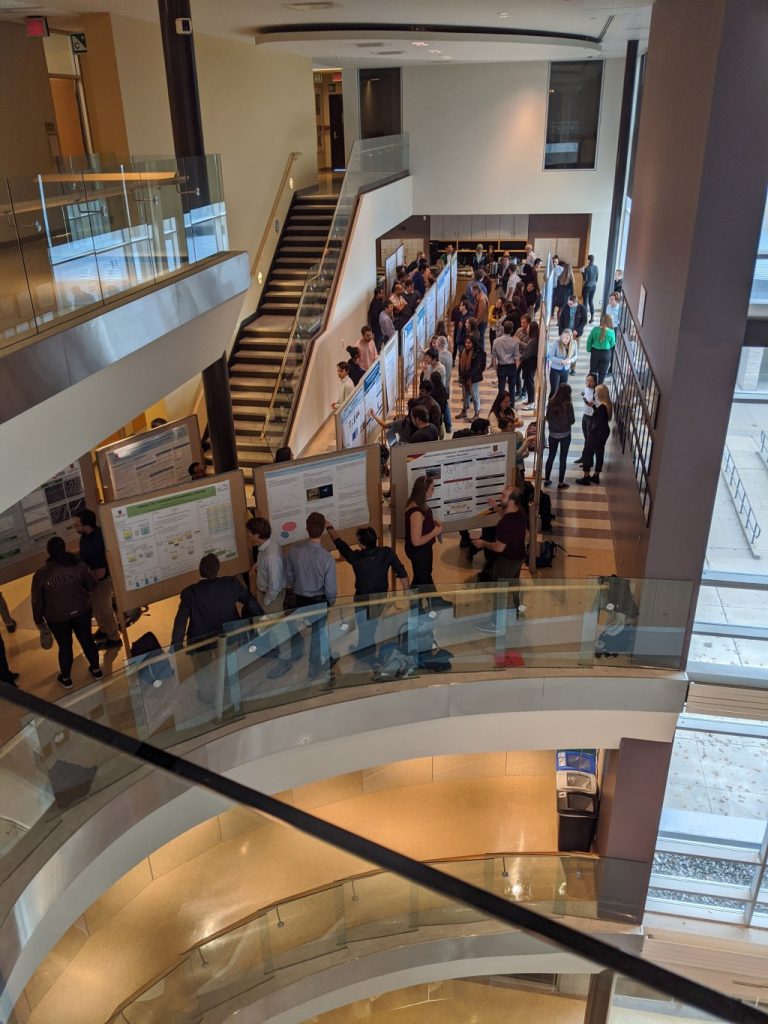
Many conferences have poster presentation sessions along with oral presentations. The poster presentation is a format introduced into the American Chemical Society meetings in the 1970s. This format allows more people the opportunity to present their work since many posters can be scheduled for the same time period and in one large room.
The format of a poster presentation allows for a one-on-one and in-depth discussion between the presenter and viewer. For this reason, poster sessions are often combined with social mixers, where people can walk around and browse the posters.
Theoretically, the poster audience is more broad and diverse, since many disciplines present in one large room. For this reason, your poster should be readable or understandable in less than 5 minutes by someone not in your field, who has only general knowledge of the research area. People browse posters and look for something that interests them, and on average spend around 90 seconds viewing a single poster. However, the people who actually attend your poster will likely be those who are interested in your work or work in a similar area.
Attaching business cards and one-page copies of your poster allow viewers to contact you later and get the information without having to take notes.
Table 21.1. Differences between posters and oral presentations (talks)
Posters are mostly non-verbal and visual, so most of this chapter will discuss poster design. However, the verbal aspect of the poster presentation is where many presenters struggle! The most common mistake is for presenters to launch into a detailed overview of the slides, starting at the introduction and working their way through the poster all the way to the acknowledgements. Even a 5-minute overview is too long at a poster! The issue with this approach is that the viewer cannot listen to you and think critically at the same time, and they lose the autonomy of exploring your visuals at their own pace. Follow these tips for a successful poster presentation:
- If someone shows interest in your poster, smile and introduce yourself, then wait.
- If they start to intently view your poster, let them do this silently without interruption.
- If they turn to you, ask if they would like a short overview of your work.
- Start with the key finding, from your conclusion, and state it in a single sentence.
- Then move on to your motivation and methods and details about the results.
- Make sure to pause and make eye contact, which will let viewers ask questions.
- Ask your viewer questions to gauge their interest and background, and encourage discussion
- Point to relevant things on your poster as you present.
There are some aspects of etiquette to giving poster presentations. First of all, you should be at your poster during the specified times. Socializing with friends should be a lower priority, so if your lab members are hanging around your poster you can politely ask them to give you some space. Stay tuned to social cues from your viewer, and let them view the poster silently if they seem to want that. Lastly, consider waiting until after the presentation for drinks.
Format and Size
Posters should be concise, organized, and self-explanatory: the best way to achieve this is to have a central and obvious message. Beyond that, a poster should be easy to view from 1-2 meters away, which means you should limit text to short paragraphs (<20 lines) or bullet points. Remember that you are not writing a full paper! Any text should be in a simple Sans-Serif typeface ( e.g., Arial, Verdana, Calibri) with adequate spacing, and large enough to easily read. Consider using a different font style for the title and headings than the main text. Follow this guide for minimum text sizes:
Title 100 pt (Verdana, bold)
Authors 36 pt (Arial, bold)
Headings 54 pt (Verdana, bold)
Main text 32 pt (Arial)
References 28 point (Arial)
Instead of text, use figures, graphs, and charts to visually communicate of your work. Make sure the text labels and axes are large enough to easily read, following the guide above.
Check the conference website for instructions on the acceptable dimensions for posters. The typically allowed dimensions are 90 cm (36”) high x 122 cm (48”) wide. There are two ways to create your poster (Figure 21.1): 1) print 12-20 regular slides on 8.5″ x 11″ pieces of paper, and arrange them; 2) create a single large poster sheet, either printed on paper or fabric, to fill the whole space.
Posters have all the components of a paper, organized into sections. These sections are not always separate on your poster (see below ‘Layout’), but they should be present in one way or another. See Table 21.2. for a list of sections and their descriptions.
Table 21.2. Poster sections
Sections in your poster are outlined by headings. Instead of using section titles like “Introduction”, use descriptive headings that tell the viewer the key message of the section (Table 21.3).
Table 21.3. Replacing poster headings with descriptive headings
Layout & design.
A thoughtful layout will provide a natural flow that guides people through your poster. It is best to arrange your poster in blocks of columns, so that the audience reads from left to right, top to bottom using “reader’s gravity”. You can number each section block or heading to help the reader to follow the flow of the material.
Posters with symmetric layouts and plenty of ‘white space’ are more visually pleasing, and can also help with flow. Also, place graphics and text to create a symmetrical balance.
Instead of headings like “Introduction”, use descriptive headings to clearly communicate your main points. A lack of headings, plus an asymmetric layout of the material, makes it difficult for the viewer to follow the flow or find a particular section of the poster.
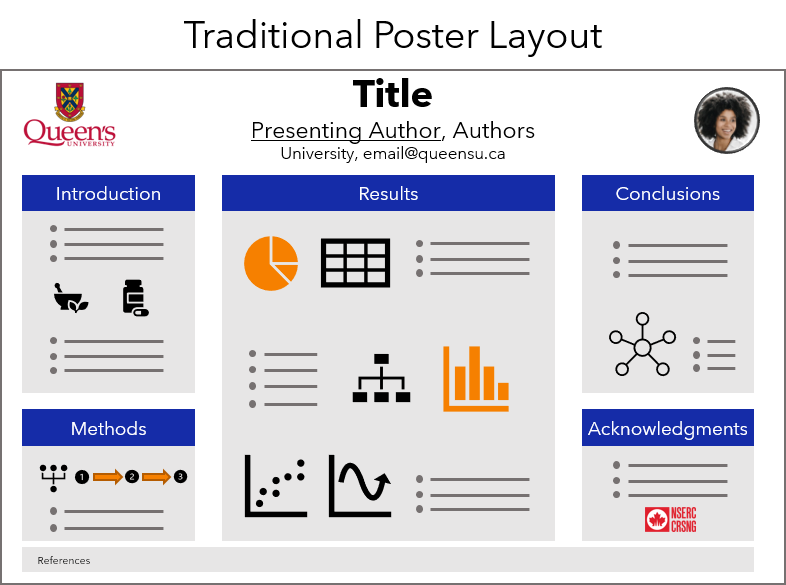
A popular traditional poster format (see Figure 21.2) has a landscape layout and three columns: 1) Introduction and Methods, 25% width; 2) Results arena, 50% Width; 3) Conclusions and Acknowledgements, 25% width. A more modern landscape layout (Figure 21.3) was designed by Mike Morrison , [1] which features a large takeaway sidebar with the key message, and a QR code that links to the paper or a website. This modern poster format also works well in a portrait format (Figure 21.4).

Stick to a theme of 2 or 3 colours, using an accessible colour scheme , and be consistent with the use of colours that have meaning (e.g., in legends). Don’t be afraid to use b right colours to attract attention, but if you overuse them you will wear out readers’ eyes. For the body of your poster, use a light coloured background and dark coloured text. Dark backgrounds with light letters can become tiring to read but are often used for headings.
Don’t start from scratch
There are many poster templates available online! Here are some PowerPoint templates and guides:
BetterPosters.blogspot.com landscape template
BetterPosters.blogspot.com portrait template
BetterPosters.blogspot.com Twitter template
Queen’s Chemistry Landscape Poster Template
Queen’s Chemistry Portrait Poster Template
Online conferences and symposia are becoming more common, including virtual poster sessions. Virtual posters can have animations, videos, and audio narration. These posters can take many formats, but one common format is for the RSC Poster Day on Twitter. They published this guide to creating a version of your poster on Twitter, and how to identify your work using the right hashtag ( e.g., #RSCOrganic, #RSCAnalytical).
Here are some links to the 2020 winners of #RSCPoster Day.
Super excited to share my research on the use of electrochemistry as a tool for drug detection in complex matrices as a #comicsforscience for my first #RSCPoster #RSCAnalytical #RSCPhys #electrochem @DennanyChem @PamelaAllanChem @CarnegieUni @StrathChem @StrathForensics pic.twitter.com/ISzJ55Hbqh — Kelly Brown (@kellybrown_94) March 3, 2020
Excited to share my first #RSCPoster and looking forward to interact with all the #chemtweeps to discuss magnetic photocatalysis 🧲💡 #RSCCat #RSCNano #RSCMat pic.twitter.com/XzwxnIYJyh — Julio Terra, Ph.D. (@_julioterra) March 3, 2020
Here we go again! NEON can deny, oops I mean no-one can deny Hydrogen's BRIGHT future for renewable energy! Here is my fun twist on my LIGHT weight hydrogen storage for mobile fuel cell applications research at @lborouniversity @LboroScience #RSCEnergy #RSCPoster pic.twitter.com/8DzRUHobiA — Lizzie Ashton (@LizzieRAshton) March 3, 2020
- " Critique: The Morrison billboard poster ", Zen Faulkes, April 11, 2019, Better Posters. Accessed 2020-08-31 ↵
Principles of Scientific Communication Copyright © 2020 by Amanda Bongers and Donal Macartney is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License , except where otherwise noted.
Share This Book
Argonne National Laboratory
Planning your oral/poster presentation.
STEM experts routinely present posters and deliver oral presentations at various points throughout their careers. Presentations give researchers a chance to share their work with different groups of people, which increases the visibility of their work and can also inspire collaboration and constructive feedback.
One advantage that presentations have over written communication is that they allow communication to happen as a direct, two-way exchange. During a presentation, the audience is right there in front of you. You can ask audience members questions, visually gauge their level of understanding/interest, and get feedback from them.
But with these benefits comes a new set of challenges, the foremost being time constraints. As a speaker, you are limited by the time allotted for your presentation and by the limited attention span of your audience. And just as you can see your audience, your audience now can see you. This means that you, the speaker, must pay special attention to the additional visual information that audiences now have access to, such as your appearance, your tone of voice, and visual aids like PowerPoint slides.
Presentations, like reports, require careful planning and attention to detail. Brainstorming, the spontaneous process of generating ideas, is often the first step in planning a presentation. After brainstorming ideas, and writing them down, you should review these ideas and filter out extraneous ones until you are left with those that are most important. Ideas are relevant if they: (1) explain the purpose of your presentation, (2) make sense to your audience, and (3) explain or support your goals.
After brainstorming and identifying the ideas that are most relevant to your presentation goals, these ideas must then be organized in a logical pattern. We do this by creating an outline. The main purpose of an outline is to organize your ideas within a structure that gives your audience easy access to them.
As with a science report, a presentation outline can take on various formats, including a traditional bulleted outline, a diagram, a storyboard, or even a grid of sticky notes that you can rearrange. Regardless of how you choose to craft your outline, in the end, all outlines should include the key takeaway messages and evidence to support them, all organized within a logical structure. You should also make note of the tables and/or figures you would want to include in your presentation, as well as any external references.
You can adapt parts of your science report or project report to suit your presentation outline; however the presentation outline should NOT mirror your report or report outline. Due to time constraints, presenters must be more selective in their presentations than in their reports when deciding which details to include.
Review Your Ideas
During or following your brainstorming session, review the ideas you have come up with and select those that best: (1) explain the purpose of your presentation, (2) are pertinent to your audience, and (3) define or support your goals.
Your purpose
The reason for the presentation. Are you trying to summarize, analyze, evaluate, argue/persuade, etc.? Use this information to define the layout of your poster or slide presentation.
Your audience
Consider what your audience would find most interesting about your research project, what they already know about your topic and what they may not know. This information will tell you where to start your presentation and what attention-grabbing opening statement to use on your audience (also see Engaging your Audience ).
Decide on your message(s). What are the 2–3 main points that you want your audience to remember? Focus your presentation around these takeaways.
- Research & Faculty
- Offices & Services
- Information for:
- Faculty & Staff
- News & Events
- Contact & Visit
- Quick Facts
- Survey Summary
- Gender Neutral Restrooms
- Undergraduate Study
- Biomedical Engineering (BS)
- ABET Objectives & Outcomes
- Combined BS/MS Program
- Career Resources
- Research Opportunities
- Summer Research Grants in BME
- Special Programs
- Student Awards
- Student Organizations and Professional Societies
- Graduate Study
- Biomedical Engineering (MS)
- Curriculum & Requirements
- Biomedical Engineering (PhD)
- PhD Timeline
- Courses Collapse Courses Submenu
- Biomechanics
- Biomaterials and Regenerative Engineering
- Cell and Molecular Engineering
- Imaging and Biophotonics
- Medical Devices and Instrumentation
- Neural Engineering
- Research Areas
- Affiliate Centers & Institutes
- Faculty Start-ups
- Core Faculty
- Administrative Faculty
- Courtesy Faculty
- Teaching Faculty
- Adjunct Faculty
- Advisory Board
- News Archive
- BME Seminar Series
- Past Seminar Speakers Collapse Past Seminar Speakers Submenu
- Careers in the Department
- Faculty Openings
- Other Opportunities
- Student Resources
- Faculty & Staff Resources
- Purchasing Procedures
- Reserve a Room
- Templates for Oral and Poster Presentations
- Travel Reimbursement Procedure
- Visitor Travel Reimbursement Procedure
- Northwestern Engineering
Resources Templates for Oral and Poster Presentations
Oral presentation template
Poster presentation template
More in this section
- Engineering Home
- BME Department
Contact Info
Department of Biomedical Engineering M c Cormick School of Engineering and Applied Science 2145 Sheridan Road Evanston, IL 60208 Phone: 847-467-1213 Fax: 847-491-4928 Email Department
Customer Reviews
Free research poster powerpoint templates.

About our free research poster templates
Easy to use and customize.
▪ Change colors with one click ▪ Most standard US and international poster sizes. ▪ Support for all PowerPoint versions ▪ Only basic PowerPoint skills required ▪ Fully customizable ▪ Instructions included with the poster templates. ▪ Online video tutorials ▪ Configured to print professionally ▪ Additional layouts included in each template
40 color schemes built-in to every research poster template
Five reasons to print your poster with us >, professionally designed research poster templates.
QUICK FIND POSTER TEMPLATES American standard poster sizes (inches) 30x40 | 36x48 | 36x56 | 36x60 | 36x72 | 36x96 | 42x60 | 42x72 | 42x90 | 44x44 | 48x48 | 48x72 | 48x96 | Trifold | Virtual International common poster sizes (centimeters) 91x122 | 70x100 | 100x140 | 100x100 | 100x200 | A0 | A1 | Virtual IMPORTANT Check the requirements of your conference before you download and work on a poster template. If you need further assistance, our phone support is available and free. We are here to provide the best service you can ask for.
Step-by-Step Tutorials
This series of short videos and animated tutorials will walk you through the research poster-making process, answering the most common questions along the way.
Need further poster template assistance? 510.649.3001
Free powerpoint poster templates for research poster presentations.
Poster template design: Aragon Standard poster sizes in inches (Height x Width) - Click on a size to download 36x48 | 36x56 | 36x60 | 36x72 | 36x96 | 42x60 | 42x72 | 42x90 | 44x44 | 30x40 | 48x48 | 48x72 | 48x96 | Trifold | Virtual - Standard Screen (4:3 Ratio) | Virtual - Wide Screen (16:9 Ratio) Standard poster sizes in centimeters (Height x Width) - Click on a size to download 122x91 | 100x70 | 140x100 | 100x100 | 200x100 | A0 | A1 ► View Samples ► Learn how to customize the template colors

Poster template design: Beaumont Standard poster sizes in inches (Height x Width) - Click on a size to download 36x48 | 36x56 | 36x60 | 36x72 | 36x96 | 42x60 | 42x72 | 42x90 | 44x44 | 30x40 | 48x48 | 48x72 | 48x96 | Trifold | Virtual - Standard Screen (4:3 Ratio) | Virtual - Wide Screen (16:9 Ratio) Standard poster sizes in centimeters (Height x Width) - Click on a size to download 122x91 | 100x70 | 140x100 | 100x100 | 200x100 | A0 | A1 ► View Samples ► Learn how to customize the template colors

Poster template design: Newfield Standard poster sizes in inches (Height x Width) - Click on a size to download 36x48 | 36x56 | 36x60 | 36x72 | 36x96 | 42x60 | 42x72 | 42x90 | 44x44 | 30x40 | 48x48 | 48x72 | 48x96 | Trifold | Virtual - Standard Screen (4:3 Ratio) | Virtual - Wide Screen (16:9 Ratio) Standard poster sizes in centimeters (Height x Width) - Click on a size to download 122x91 | 100x70 | 140x100 | 100x100 | 200x100 | A0 | A1 ► View Samples ► Learn how to customize the template colors
Poster template design: Winchester Standard poster sizes in inches (Height x Width) - Click on a size to download 36x48 | 36x56 | 36x60 | 36x72 | 36x96 | 42x60 | 42x72 | 42x90 | 44x44 | 30x40 | 48x48 | 48x72 | 48x96 | Trifold | Virtual - Standard Screen (4:3 Ratio) | Virtual - Wide Screen (16:9 Ratio) Standard poster sizes in centimeters (Height x Width) - Click on a size to download 122x91 | 100x70 | 140x100 | 100x100 | 200x100 | A0 | A1 ► View Samples ► Learn how to customize the template colors

Poster template design: Lockwood Standard poster sizes in inches (Height x Width) - Click on a size to download 36x48 | 36x56 | 36x60 | 36x72 | 36x96 | 42x60 | 42x72 | 42x90 | 44x44 | 30x40 | 48x48 | 48x72 | 48x96 | Trifold | Virtual - Standard Screen (4:3 Ratio) | Virtual - Wide Screen (16:9 Ratio) Standard poster sizes in centimeters (Height x Width) - Click on a size to download 122x91 | 100x70 | 140x100 | 100x100 | 200x100 | A0 | A1 ► View Samples ► Learn how to customize the template colors
Poster template design: Kensington Standard poster sizes in inches (Height x Width) - Click on a size to download 36x48 | 36x56 | 36x60 | 36x72 | 36x96 | 42x60 | 42x72 | 42x90 | 44x44 | 30x40 | 48x48 | 48x72 | 48x96 | Trifold | Virtual - Standard Screen (4:3 Ratio) | Virtual - Wide Screen (16:9 Ratio) Standard poster sizes in centimeters (Height x Width) - Click on a size to download 122x91 | 100x70 | 140x100 | 100x100 | 200x100 | A0 | A1 ► View Samples ► Learn how to customize the template colors

Poster template design: Stone A new, simplified concept for better poster design Standard poster sizes in inches (Height x Width) - Click on a size to download 36x48 | 36x56 | Trifold | Virtual - Standard Screen (4:3 Ratio) | Virtual - Wide Screen (16:9 Ratio) Standard poster sizes in centimeters (Height x Width) - Click on a size to download A0 ► View Samples ► Learn how to customize the template colors
Poster template design: Marquee Standard poster sizes in inches (Height x Width) - Click on a size to download 36x48 | 36x56 | 36x60 | 36x72 | 36x96 | 42x60 | 42x72 | 42x90 | 44x44 | 30x40 | 48x48 | 48x72 | 48x96 | Trifold | Virtual - Standard Screen (4:3 Ratio) | Virtual - Wide Screen (16:9 Ratio) Standard poster sizes in centimeters (Height x Width) - Click on a size to download 122x91 | 100x70 | 140x100 | 100x100 | 200x100 | A0 | A1 ► View Samples ► Learn how to customize the template colors
Poster template design: Winston Standard poster sizes in inches (Height x Width) - Click on a size to download 36x48 | 36x56 | Trifold | Virtual - Standard Screen (4:3 Ratio) | Virtual - Wide Screen (16:9 Ratio) Standard poster sizes in centimeters (Height x Width) - Click on a size to download A0 ► View Samples ► Learn how to customize the template colors

Poster template design: Chamberlain Standard poster sizes in inches (Height x Width) - Click on a size to download 36x48 | 36x56 | 36x60 | 36x72 | 36x96 | 42x60 | 42x72 | 42x90 | 44x44 | 30x40 | 48x48 | 48x72 | 48x96 | Trifold | Virtual - Standard Screen (4:3 Ratio) | Virtual - Wide Screen (16:9 Ratio) Standard poster sizes in centimeters (Height x Width) - Click on a size to download 122x91 | 100x70 | 140x100 | 100x100 | 200x100 | A0 | A1 ► View Samples ► Learn how to customize the template colors

Poster template design: Forrest Standard poster sizes in inches (Height x Width) - Click on a size to download 36x48 | 36x56 | 36x60 | 36x72 | 36x96 | 42x60 | 42x72 | 42x90 | 44x44 | 30x40 | 48x48 | 48x72 | 48x96 | Trifold | Virtual - Standard Screen (4:3 Ratio) | Virtual - Wide Screen (16:9 Ratio) Standard poster sizes in centimeters (Height x Width) - Click on a size to download 122x91 | 100x70 | 140x100 | 100x100 | 200x100 | A0 | A1 ► View Samples ► Learn how to customize the template colors

DIGITAL POSTER PRESENTATION HANDOUTS
Free with a printed poster order.
A feature-packed alternative to traditional paper poster handouts

Instant QR Code Generator
Add functionality to your poster! Share a link to a page, your email or additional info on the web. It's easy, free and further connects your audience!
Professional Trifold Poster Boards
Ready to use out of the box. Great solution for tabletop 36x48 Trifold poster presentations. Price includes printing, mounting and free Ground FedEx shipping.
Poster Font Size Checker
A convenient way to visualize what size the text will be on your printed poster. Wondering how big the fonts will be on your poster? Download and print this PDF on your desktop printer.
Quick access to ALT code symbols
Click here to choose from over 350 easy to copy and use ALT code symbols.
Fabric Research Posters
Say goodbye to poster tubes with a professional fabric poster you can pack in your luggage! With our crease-resistant EasyTravel™ fabric your presentation will look professional, sharp, and will pack nicely in your carry-on.
Simplify Your Group’s Poster-Ordering Process
Join our free service designed to help you coordinate your group’s poster orders, get discounted rates and customized special features not normally available for standard orders.
Links to university corporate identity (Logo) pages
List of corporate identity pages where you can download university logos to use with your poster presentation. Help your fellow researchers. Good quality logos for use in printed research posters are difficult to find online. If you have a link to the identity page of your university, email it to us and we will add it to our list for others to use.
UC Berkeley Texas A&M UCLA Columbia Medical Center Stanford University
Adelphi University Duke University UPENN Bradley University ENMU
UNC Chapel Hill Northwestern University Magnet recognition Seal Howard University University of Houston
Drexel University Carlow University UNLV UNR UFL
TUFTS George Mason U. St. Scholastica College Mount Royal University Penn State
Yale University University of Wisconsin SD School of Mines USC GATECH
STARTER POWERPOINT POSTER TEMPLATES
Standard size research poster templates in inches use these starter poster templates as a starting point for your own poster designs, thumbnails of posters are shown in proportion to each others’ sizes based on a 48 inch (height) x 96 inch (width) display area, 36” tall x 48” wide .
STARTER 36x48 POWERPOINT POSTER TEMPLATE The 36x48 scientific poster template size is one of the smaller sizes and also one of the most common. It is very suitable for scientific posters with low to moderate amount of text and graphics. The 36x48 research poster template can also be printed at the following sizes without distortion or any necessary adjustments: 36x48 (Standard), 42x56, 48x64, 30x40
Trifold (tabletop)
STARTER TRIFOLD POWERPOINT POSTER TEMPLATE These free PowerPoint poster templates are designed for a standard 3x4 foot poster presentation to be mounted on a standard Trifold poster board. This research poster template should be printed only at the following size: 36x48 (Standard Trifold) This poster template is for a standard Trifold board presentation. You can use it with poster boards available at office-supply stores or our professional ready-to-use Trifold poster presentation product. Are you looking for a larger MonsterBoard template? Use this PowerPoint MonsterBoard template.
36” Tall x 56” Wide
STARTER 36x56 POWERPOINT POSTER TEMPLATE This free PowerPoint poster template is designed for a standard 3x4.5 foot poster presentation. This PowerPoint research poster template is for a medium size poster. It is suitable for most poster presentations. It can accommodate moderate to large amounts of content. This scientific poster template can be printed at the following sizes: 36x56 (Standard), 42x65.3, 48x74.6
36” Tall x 60” Wide
STARTER 36x60 POWERPOINT POSTER TEMPLATE This free PowerPoint poster template is designed for a standard 3x5 foot poster presentation. This is also one of the standard sizes. It is used mostly when the height of the presentation board is only three feet and there is more content to present that can fit in a 48x36 poster. This scientific poster template can be printed at the following sizes: 36x60 (Standard), 42x70, 48x80
36” Tall x 72” Wide
STARTER 36x72 POWERPOINT POSTER TEMPLATE This free PowerPoint poster template is designed for a standard 3x6 foot poster presentation. The same as the above scientific poster template, only wider by a foot. Again, it depends on how much content you need to present. This scientific poster template can be printed at the following sizes: 36x72 (Standard), 42x84, 48x96
36” Tall x 96” Wide
STARTER 36x96 POWERPOINT POSTER TEMPLATE This free PowerPoint poster template is designed for a standard 3x8 foot poster presentation. It’s the widest one you can use on a three foot tall presentation board. It has five columns. This scientific poster template can be printed at the following sizes: 96x36 (Standard), 24x64
42” Tall x 60” Wide
STARTER 42x60 POWERPOINT POSTER TEMPLATE This free PowerPoint poster template is designed for a standard 3.5x5 foot poster presentation. This PowerPoint research poster template is suitable for most poster presentations. It can accommodate moderate to large amounts of content. This scientific poster template can be printed at the following sizes: 42x60 (Standard), 36x51.42, 48x68.57
42” Tall x 72” Wide
STARTER 42x72 POWERPOINT POSTER TEMPLATE This free PowerPoint poster template is designed for a standard 3.5x6 foot poster presentation. This PowerPoint research poster template is for a medium size poster. It is suitable for most poster presentations. It can accommodate moderate to large amounts of content. This scientific poster template can be printed at the following sizes: 42x72 (Standard), 36x61.70, 48x82.28
42” Tall x 90” Wide
STARTER 42x90 POWERPOINT POSTER TEMPLATE This free PowerPoint poster template is designed for a standard 3.5x7.5 foot poster presentation. This PowerPoint research poster template is for a large size poster. It is suitable for most poster presentations. It can accommodate moderate to large amounts of content. This scientific poster template can be printed at the following sizes: 42x90 (Standard), 36x77.14, 44x94.28
44” Tall x 44” Wide
STARTER 44x44 POWERPOINT POSTER TEMPLATE This free PowerPoint poster template is designed for a standard 3.7 x 3.7 foot poster presentation. This PowerPoint research poster template is for a medium size poster. It is suitable for many poster presentations. It can accommodate moderate amounts of content. This scientific poster template can be printed at the following sizes: 44x44 (Standard), 36x36, 42x42, 48x48
48” Tall x 72” Wide
STARTER 48x72 POWERPOINT POSTER TEMPLATE This free PowerPoint poster template is designed for a standard 4x6 foot poster presentation. This PowerPoint research poster template is for a medium/large size poster. It is suitable for most poster presentations. It can accommodate moderate to large amounts of content. This scientific poster template can be printed at the following sizes: 48x72 (Standard), 24x36, 42x63
48” Tall x 48” Wide
STARTER 48x72 POWERPOINT POSTER TEMPLATE This free PowerPoint poster template is designed for a standard 4x4 foot poster presentation. This scientific poster template is a good size for limited available spaces without compromising room for content. This research poster template can be printed at the following sizes: 48x48 (Standard), 36x36, 24x24, 42x42
48” Tall x 96” Wide
STARTER 48x96 POWERPOINT POSTER TEMPLATE This free PowerPoint poster template is designed for a standard 4x8 foot poster presentation. This poster template is for the largest size poster usually allowed in conferences. It can accommodate a lot of content. You can use this template if you also have a large number of photos, tables, charts, and text. This scientific poster template can be printed at the following sizes: 48x96 (Standard), 24x48, 42x84, 36x72
40” Tall x 30” Wide
STARTER 40x30 POWERPOINT POSTER TEMPLATE This free PowerPoint poster template is designed for a standard 40x30 inch poster presentation. This vertical poster template can accommodate a moderate amount of content. It can accommodate several photos, tables, charts, and a decent amount of text. This scientific poster template can be printed at the following sizes: 40x30 (Standard), 48x36, 56x42
Free PowerPoint poster templates in metric sizes (cm) for international poster conferences
Thumbnails of posters are shown in proportion to each others’ sizes based on a 200 cm (height) x 100 cm (width) display area, 91 wide x 122 tall.
STARTER 91cmX122cm POWERPOINT POSTER TEMPLATE This free PowerPoint poster template is designed for a standard metric 91 cm by 122 cm scientific poster presentation for international poster sessions. This PowerPoint poster template is essentially a vertical version of a standard 48x36 inch poster presentation. This scientific poster template can be printed at the following sizes: 91 cm x122 cm (Standard 36x48 inches), 76x102 cm
70 Wide x 100 Tall
STARTER 70cmX100cm POWERPOINT POSTER TEMPLATE This free PowerPoint poster template is designed for a standard metric 70 cm by 100 cm scientific poster presentation for international poster sessions. This PowerPoint poster template is for a small size poster poster presentation commonly used at international conferences. This scientific poster template can be printed at the following sizes: 70 cm x100 cm (Standard 27.5x39.37 inches), 100x143 cm
100 Wide x 140 Tall
STARTER 100cmX140cm POWERPOINT POSTER TEMPLATE This free PowerPoint poster template is designed for a standard metric 100 cm by 140 cm scientific poster presentation for international poster sessions. This PowerPoint poster template is for a small size poster poster presentation commonly used at international conferences. This scientific poster template can be printed at the following sizes: 100 cm x140 cm (Standard 39.37x55.12 inches)
1 Meter x 1 Meter
STARTER 100cmX100cm POWERPOINT POSTER TEMPLATE This free PowerPoint poster template is designed for a standard metric 1 meter by 1 meter scientific poster presentation for international or domestic poster sessions. This template is commonly required at the Keystone Symposia research poster conferences. This scientific poster template can be printed at the following size: 100 cm x 100 cm (Standard 39 x 39 inches). Any square size up to 121 x 121 cm
100 Wide x 200 Tall
STARTER 100cmX200cm POWERPOINT POSTER TEMPLATE This free PowerPoint poster template is designed for a standard metric 1 meter by 2 meter scientific poster presentation for international or domestic poster sessions. This scientific poster template can be printed at the following size: 100 cm x 200 cm (Standard 39 x 78 inches)
STARTER A0 POWERPOINT POSTER TEMPLATE This free PowerPoint poster template is designed for a standard metric A0 scientific poster presentation at a 841mm x 1189mm size for international or domestic poster sessions. This scientific poster template can be printed at the following size: 46.81 inches x 33.11 inches
STARTER A1 POWERPOINT POSTER TEMPLATE This free PowerPoint poster template is designed for a standard metric A1 scientific poster presentation at a 594mm x 841mm poster size for international or domestic poster sessions. This scientific poster template can be printed at the following size: 23.39 inches x 33.11 inches
VIRTUAL POSTER PRESENTATION
STARTER POSTER TEMPLATES These free PowerPoint poster templates are designed for screen presentations at virtual meetings Virtual - Standard Screen (4:3 Ratio) Virtual - Wide Screen (16:9 Ratio)
Virtual poster sessions for conferences and meetings of all sizes
If you are a meeting organizer we can help you set up a virtual poster session, free yourself from managing poster submissions and provide your meeting's attendees with a versatile presentation platform that will meet all your requirements.
Five good reasons to print your poster with PosterPresentations.com
Amazingly fast printing: Experience amazingly fast printing with us! If you place your poster order between Monday and Friday before 3pm Eastern time (noon Pacific time), we'll ship it out the same day. You can expect your delivery within one, two, or three business days. Plus, if you give us an additional two business days, we'll provide free shipping! Top-Quality Materials: We take pride in using the finest materials available in the industry. Our prints are produced on high-quality photographic papers, vinyls, and exquisite fabrics. In fact, we were the pioneers of fabric printing for research posters in the USA back in 2008. Reliable Customer Support: Rest assured that we don't simply print whatever you send us. We ensure that your files are optimized for the best possible printing results. If we notice any issues, we'll promptly inform you. Your presentation matters as much to us as it does to you. Competitive Pricing with No Surprises: As a professional, you'll find our prices to be competitive, and we never add unexpected last-minute fees. Furthermore, expedited printing is always included at no extra cost. For students, our prices are among the lowest nationwide. Group Discounts Available: Place a group order with us and not only will you enjoy free shipping, but also discounts that can beat most of our competitors. Feel free to reach out to us at 510.649.3001 for more information.
PosterPresentations.com 2117 Fourth Street STE C Berkeley California 94710 USA
Copyright © 2024

Poster Printing
Research paper posters
Fabric posters
Trifold poster boards
Rollup banners
Dry-erase whiteboards
PowerPoint poster templates
Poster-making tutorials
Google Slides support
Terms and Privacy
Poster design services
New Services
Virtual poster meetings
- Virtual poster handouts
Oratory Club
Public Speaking Helpline
Poster Vs Oral Presentation: Which Is Best In 2023?
When it comes to presenting information or research, there are two popular options: posters or oral presentations. Choosing between the two can be a tough decision, but fear not! We’re here to help you explore the key differences and find the best fit for your needs. So, let’s dive in and compare the advantages of each approach.
First up, we have posters. These visual displays offer a great way to showcase your work creatively. With posters, you can utilize eye-catching graphics, images, and charts to capture your audience’s attention. Plus, posters allow for easy interaction, as viewers can take their time to study the content at their own pace.
On the other hand, we have oral presentations, which involve speaking in front of an audience to convey your research findings. Oral presentations enable you to engage directly with your peers, expressing your ideas, and answering questions on the spot. They offer a dynamic platform for showcasing your public speaking skills and establishing your expertise.
Now that we’ve introduced both options, let’s delve deeper into the specific merits of each one—poster presentations and oral presentations. By examining the distinct features of these approaches, we can help you make an informed decision that best suits your needs and preferences. So, let’s weigh the pros and cons and find the perfect medium for your next presentation.
When deciding between a poster and an oral presentation, there are several key features to consider.
1. Visual Impact: Posters offer a visual representation of information, while oral presentations allow for direct engagement.
2. Audience Interaction: With posters, viewers can leave comments or ask questions. For oral presentations, immediate feedback is possible.
3. Versatility: Posters can be displayed for extended periods, while oral presentations allow for dynamic delivery.
4. Time Management: Posters can be viewed at any time, while oral presentations have a set duration.
5. Communication Style: Posters rely on visuals, while oral presentations include spoken words and gestures.
Consider these features to determine which format will best suit your needs.

Table of Contents
Key Takeaways: Poster vs Oral Presentation
- Posters are visual displays of information, while oral presentations involve speaking to an audience.
- Posters allow for more creativity in design and visual appeal.
- Oral presentations provide an opportunity for direct interaction and engagement with the audience.
- Posters are often used in conferences or exhibitions, while oral presentations are common in classrooms or professional settings.
- Both formats have their benefits and can be effective in communicating information.
Comparing Poster vs Oral Presentation
In today’s fast-paced world, effective communication is key. Whether it’s presenting research findings, sharing ideas, or conveying information, there are various methods to choose from. Two popular options are posters and oral presentations. In this article, we will explore the differences and similarities between these two formats, to help you make an informed decision on which method is better suited for your needs.
Overview of Posters
Posters are a visual medium for presenting information. They typically consist of a combination of text, images, graphs, and charts. Posters are often used in academic and scientific settings, such as conferences or research symposiums, to showcase research findings or present complex data. They offer a concise and visually appealing way to convey information to a large audience.
Creating a poster involves careful consideration of the layout, design elements, and content. The goal is to effectively communicate the main points of the research or topic in a visually appealing manner. Posters can be displayed on walls or presentation boards, allowing viewers to engage with the information at their own pace.
Overview of Oral Presentations
Oral presentations, on the other hand, involve the delivery of information through spoken words. This format is commonly used in academic, professional, and educational settings. Instead of relying solely on visual aids, oral presentations allow presenters to verbally explain their research or ideas, often supported by slides or visual aids.
An oral presentation typically follows a structured format, with an introduction, body, and conclusion. Presenters are expected to articulate their thoughts clearly, provide engaging explanations, and convey their message effectively. This format allows for direct interaction with the audience through questions, discussions, and feedback.
Key Features Compared
When comparing posters and oral presentations, there are several key features to consider. Let’s explore each of these features in detail and compare the two methods.
Content Delivery
In terms of content delivery, posters and oral presentations offer different approaches. Posters rely heavily on visuals and concise written information to convey the main points. Viewers can read the content at their own pace and spend more time analyzing the information presented. On the other hand, oral presentations focus on verbal communication, allowing presenters to provide more in-depth explanations and engage directly with the audience.
Engagement and Interaction
Posters provide a more self-paced experience for viewers. They can spend as much time as needed to absorb the information, making them suitable for passive engagement. However, posters lack the interactive element that oral presentations offer. Oral presentations allow for real-time interaction, such as question-and-answer sessions or audience feedback, creating a more dynamic and engaging experience.
Presentation Skills
Both posters and oral presentations require distinct presentation skills. Creating an effective poster involves designing an aesthetically appealing layout, using clear and concise language, and organizing information in a logical manner. Oral presentations, on the other hand, require strong public speaking skills, the ability to engage the audience, and effective use of visual aids. Each format requires different skill sets and preparation.
User Experience
The user experience for both posters and oral presentations can vary depending on various factors. For posters, viewers have the flexibility to study the content at their own pace, review specific details, and focus on areas of interest. However, posters may lack the personal touch and direct interaction that oral presentations provide.
In oral presentations, the audience can benefit from real-time explanations, engagement, and the opportunity to ask questions. This format allows for a more dynamic and interactive user experience. However, some audience members may feel overwhelmed by the fast pace or struggle to fully grasp the information presented in the moment.
Pros and Cons
- Visually appealing and engaging.
- Provides a concise overview of research or information.
- Allows viewers to study and analyze content at their own pace.
- Lacks direct interaction and engagement with the audience.
- May require a large amount of space for display.
- Can be challenging to condense complex information into a limited space.
Oral Presentations
- Allows for direct interaction and engagement with the audience.
- Enables presenters to provide in-depth explanations and clarify misunderstandings.
- Creates a dynamic and engaging experience for both presenters and audience members.
- Requires strong public speaking skills and presentation preparation.
- May limit the amount of information that can be covered within a given time frame.
- Relies heavily on the presenter’s ability to convey the message effectively.
Price Comparison
When it comes to cost, posters are generally more affordable compared to oral presentations. Creating a poster requires minimal resources, such as printing costs, design software, and materials for display. On the other hand, oral presentations may involve additional expenses, such as travel costs for attending conferences or professional presentation software.
Comparison Table
Here is a comparison table that highlights the key features of posters and oral presentations:
| Feature | Posters | Oral Presentations | |————————-|—————————————|————————————-| | Content Delivery | Relies on visuals and concise text | Verbal explanations and visual aids | | Engagement and Interaction | Passive engagement for viewers | Real-time interaction with audience | | Presentation Skills | Design and organization | Public speaking and visual aid usage |
Which is Better – Poster vs Oral Presentation
In conclusion, the choice between posters and oral presentations ultimately depends on various factors, such as the nature of the content, audience preferences, and available resources. Both formats have their strengths and limitations, and the decision should be based on the specific goals and circumstances of the presentation.
When choosing between posters and oral presentations, consider the level of audience engagement desired, the complexity of the information being conveyed, and the presentation skills of the presenter. While posters offer a visually appealing and self-paced experience, oral presentations provide real-time interaction and the opportunity for in-depth explanations.
In summary, posters are ideal when conveying concise information visually and when passive engagement is desired. On the other hand, oral presentations are best suited for interactive discussions, in-depth explanations, and audience engagement. Ultimately, the choice between posters and oral presentations should be based on the specific goals and requirements of the presentation.
Three reasons to choose posters:
- Visually engaging and can effectively communicate concise information.
- Allows for self-paced studying and analysis of the content.
- Minimal cost and resource requirements compared to oral presentations.
Frequently Asked Questions
When it comes to presenting information, two common formats are posters and oral presentations. Here are answers to some frequently asked questions about these two formats and their differences.
1. Which format is better for presenting information, a poster or an oral presentation?
Both formats have their advantages, and the choice depends on the context and purpose of the presentation. Posters are visually appealing and allow viewers to absorb information at their own pace. They are great for displaying complex data or visuals and can be easily referenced. Oral presentations, on the other hand, allow for direct interaction with the audience and the opportunity to convey information with enthusiasm and charisma. They are more dynamic and can often be more engaging for the audience. Ultimately, it’s important to consider the specific goals of your presentation and choose the format that aligns best with those objectives.
2. What are the main differences between a poster and an oral presentation?
The main difference is the way information is delivered. In a poster, the content is static and can be absorbed visually. Viewers can interpret the information at their own pace and refer back to it when needed. An oral presentation, on the other hand, involves a live performance where the presenter delivers information verbally. This format allows for direct interaction with the audience, the use of visual aids, and the ability to adapt the delivery based on audience reactions. Another difference is the level of preparation required. Posters typically require more time for design and visual arrangement, while oral presentations require more time rehearsing and practicing engaging delivery.
3. Are there any advantages to using a poster instead of an oral presentation?
Yes, there are several advantages to using a poster. Posters are highly visual and can convey complex information in an easily digestible manner. They allow viewers to study the content at their own pace and can be used as reference material even after the presentation. Posters are also ideal for situations where there is limited time for presentations or if the presenter prefers a more hands-off approach. Additionally, posters can be displayed in public areas even after the event, reaching a wider audience and serving as a long-lasting visual representation of the topic.
4. Can an oral presentation be more engaging than a poster?
Yes, an oral presentation can often be more engaging than a poster. Oral presentations allow for direct interaction with the audience, enabling the presenter to capture their attention and convey information using gestures, voice modulation, and visual aids. Presenters can also adapt their delivery based on audience reactions and engage the audience through questions, discussions, or interactive activities. Additionally, the live nature of an oral presentation allows for the presenter’s enthusiasm and passion for the topic to shine through, making it more memorable and impactful for the audience.
5. Can a poster and an oral presentation be used together?
Absolutely! Combining a poster and an oral presentation can be a powerful way to enhance the impact of your message. By creating a visually appealing poster that provides an overview of the topic, you can effectively capture the audience’s attention. Then, during the oral presentation, you can dive deeper into the content, providing additional insights, anecdotes, and engaging the audience in an interactive discussion. This combination allows for the best of both worlds, offering the visual appeal and reference value of a poster, along with the dynamic engagement of an oral presentation.

Poster Presenting Tips : Cal NERDS’ Student Research Poster Presenting Tips
So, to sum it all up, when it comes to presenting information, there are two main options: posters and oral presentations. Posters are like visual aids that can help you explain your ideas with pictures, graphs, and text. On the other hand, oral presentations involve speaking to an audience and sharing your thoughts and information out loud.
Both methods have their advantages and disadvantages. Posters can be a great way to showcase your creativity and make your ideas visual. They allow your audience to take their time and study the information on their own. However, they might not provide enough explanation and can limit your ability to interact with your audience.
Oral presentations, on the other hand, give you a chance to engage with your audience directly. You can use your voice, gestures, and expressions to convey your message. However, they require more preparation and can be nerve-wracking for some people.
In the end, the best method for presenting information depends on your personal style and the situation. If you’re a visual person who likes to express yourself through images and graphs, posters might be your go-to. If you enjoy speaking and connecting with others, oral presentations might be a better fit.
Remember, it’s not about picking a winner between the two, but rather about choosing the method that works best for you and effectively communicates your ideas. So, whether you choose to create a poster or give an oral presentation, embrace the opportunity to share your knowledge and let your creativity shine!
Similar Posts
What are the types of online presentations.
There are two types of online presentations: live presentations and recorded presentations. Live presentations are delivered in real-time, while recorded presentations are pre-recorded and made available for on-demand viewing. Online presentations offer a convenient and flexible way to share information, engage with an audience, and deliver a compelling message. They can be used for various…
What Are The Principles Of A Strong Presentation?
Are you tired of giving lackluster presentations that fail to captivate your audience? Do you want to learn the secrets to delivering a strong and impactful presentation? Look no further! In this article, we will explore the principles of a strong presentation that will leave your audience engaged and inspired. Whether you are a seasoned…

Best Budget Projectors for Presentations
The best budget projector for presentations is [insert name of projector]. With its affordable price and high-quality performance, it is the perfect choice for delivering captivating presentations. Whether you are a student, professional, or business owner, this projector offers excellent brightness and clarity, making your visuals stand out. Its compact and lightweight design ensures easy…
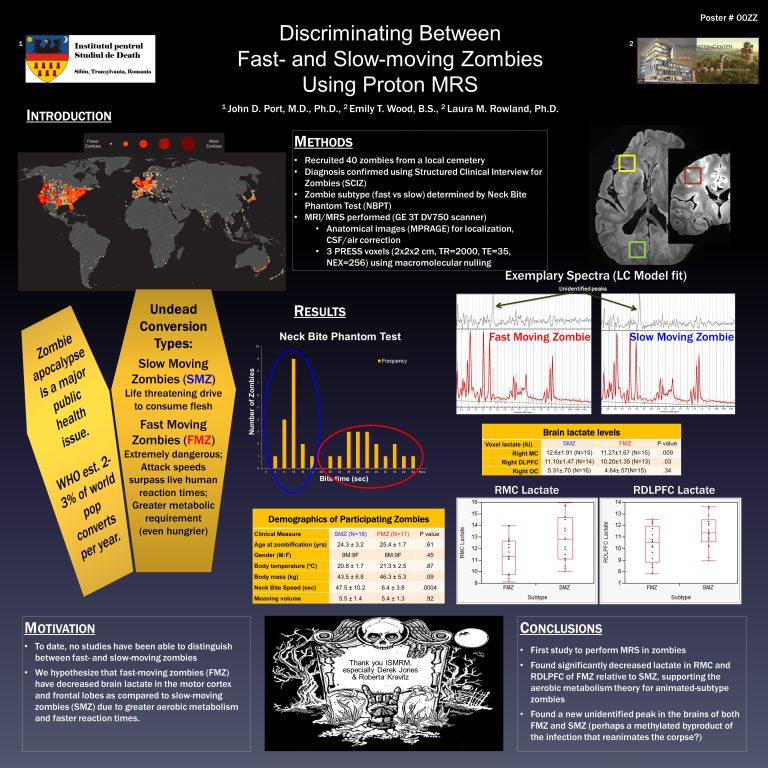
What is the Digital Poster?
A digital poster is a visual display that uses digital technology to present information, images, and videos. It is an innovative and interactive form of visual communication that allows businesses to showcase their products or services in a dynamic and engaging way. With increasing advancements in digital signage and display technology, digital posters have become…
How to Own The Stage in Presentation?
To own the stage in a presentation, maintain a confident presence, engage the audience through storytelling, and deliver a clear message with enthusiasm. A powerful and engaging presentation captures the attention and interest of the audience, leaving a lasting impression. By mastering the art of stage presence and incorporating effective communication techniques, you can create…
How To End A Presentation?
Are you tired of ending your presentations with a whimper instead of a bang? Do you want to leave a lasting impression on your audience and make them remember your key message? Look no further! In this article, we will dive into the art of ending a presentation with impact. From powerful closing statements to…
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Br J Gen Pract
- v.70(Suppl 1); June 2020

Oral and Poster Presentations
- Br J Gen Pract. 2020 Jun; 70(Suppl 1): bjgp20X710465.
Preventative health screening community events, a mechanism to target minority ethnic populations in improving primary care utilisation to improve health outcomes
Preventative medicine has become a central focus in primary care provision, with greater emphasis on education and access to health care screening. The Department of Health reports existing health inequalities and inequalities in access within ethnic minority groups. Studies assessing the value of community engagement in primary care have reported variable outcomes in term of subsequent service utilisation.
To consider the benefit of community-based health screening checks to improve access and health outcomes in minority ethnic groups.
An open community health screening event ( n = 43), to allow targeted screening within an ethnic minority population. Screening included BP, BMI, BM and cholesterol. Results were interpreted by a healthcare professional and counselling was provided regarding relevant risk factors. Post-event feedback was gathered to collate participant opinion and views.
Seventy-nine per cent of participants were from ethnic minority backgrounds: 64% were overweight or obese and 53% of participants were referred to primary care for urgent review following abnormal findings. All those referred would not have accessed healthcare without the event referral. All (100%) participants believed it improved health education and access to health care.
This study clearly demonstrates the value of targeted community-led screening and education events in public health promotion. There was a significant benefit in providing community-based screening. There is a need for a longitudinal analysis to determine the impact on health outcomes and long-term access to healthcare provision.
Bringing together child health professionals and dental experts to tackle oral health in children
In the UK, poor oral health among children continues to be a major public health concern. Primary care professionals are encouraged to take a proactive approach in engaging parents and carers to develop better oral health practices for their children. Unfortunately, research has shown that patients are often exposed to inconsistent and at worst conflicting advice.
To increase the confidence of primary care professionals in their knowledge surrounding preventative oral health and ensure the delivery of consistent and proactive oral health advice.
A local dentist and dental health educator were invited to a general practice multidisciplinary meeting to deliver an educational session on oral health advice for children. Qualitative and quantitative data in form of a questionnaire was collected to analyse the impact of the education session.
The meeting was attended by 15 healthcare professionals including GPs, paediatricians, a community mental health representative, and a school nurse. There were 78% of attendees who reported that they had never received any formal teaching on oral health care prior to this session. Qualitative data highlighted specific gaps in knowledge, while confidence ratings suggest significant improvement in confidence of attendees in their knowledge of oral health in children.
Achieving good oral health for all children requires the support of a wide range of healthcare professionals. Further education sessions such as this encourages joint learning and relationship building between professionals and influences behaviour to improve child health care as part of making every contact count. The emerging Primary Care Networks provide an excellent setting to deliver this education.
The annual dementia review: exploring current practice in primary care
Dementia is a global public health challenge, the significant consequences of which are recognised in global and national health policies. Despite approaches to improve the implementation of evidence-based dementia care in primary care and the inclusion of indicators for dementia in the Quality and Outcomes Framework (QOF), there is consistent evidence that people with dementia and their family carers lack access to care which meets their needs.
This study aims to explore current practice regarding the annual dementia review in primary care by investigating: 1) what ‘should’ be happening in annual dementia reviews; 2) how dementia reviews are delivered in a sample of general practices; 3) the barriers and facilitators to the implementation of evidence-based care in dementia reviews; and 4) the experience of these reviews from the perspectives of people with dementia and their informal carer(s).
Qualitative methods will be used. In the first stage, semi-structured interviews with national and regional experts in dementia policy and healthcare will be used to explore what ‘should’ be happening in an annual dementia review. In the second stage, interviews with primary healthcare team members will explore how annual dementia reviews are delivered in a sample of practices in North East England. Interviews with people with dementia and their carers will then be used to explore how reviews are experienced by service users. Thematic analysis will be used to analyse data.
Key themes from the first stage will be presented and their implications in primary care discussed.
The research plan for the second stage will be presented.
Resilience in advanced cancer caregiving
Family caregivers of advanced cancer patients are at risk for developing mental disorders. Despite this risk, the majority seem to adapt well, and throughout the caregiving period, their trajectory is characterised by healthy functioning. However, GPs struggle with making timely assessments of caregivers at risk for mental dysfunction, since they often fail to seek medical help for themselves and the appropriate research about resilience in cancer caregivers is scarce. Moreover, research is hampered by the lack of a universal definition or theoretical framework.
To propose a comprehensive definition and framework for further research in family caregiving for advanced cancer patients.
Inspired by the hermeneutic methodology, reviews and concept analyses on resilience following a potentially traumatic event were searched and analysed. Conforming to the hermeneutic methodology, article collection from PubMed, EMBASE, CINAHL, and PsycInfo was followed by analysis and was stopped when saturation was reached. Elements consistently arising from the definitions of resilience were listed and the theoretical frameworks were compared.
The APA definition: ‘ resilience is the process of adapting well in the face of adversity, trauma or threats ’ and Bonanno’s framework ‘ temporal elements of resilience ’ are proposed.
There is a need for studies on resilience in caregivers of advanced cancer patients. Resilience is context-dependent, hence, study results cannot be transferred as such from one clinical situation to another. Furthermore, conceptual ambiguities hinder the interpretation and comparison of study results. For further research on resilience in caregivers of advanced cancer patients, we suggest the APA definition of resilience and Bonanno’s framework.
Dermatology in primary care: an audit of the proportion of patients who present to general practice with a dermatological problem that could be self-managed
A considerable proportion of GPs’ workload is dermatological. It is important to investigate what common skin conditions encountered in primary care can be self-managed, in an effort to alleviate the burden on primary care.
The purpose of the audit was to identify the proportion of consultations that are dermatological in nature and analyse potential for self-management by patients.
Data was collected using the patient electronic record system (EMIS) in general practice. A search was made for all consultations from the 17 April to 15 May 2019, which included all new presenting complaints that were dermatological in nature. The criteria for self-management included advising over the counter (OTC) medication or reassurance. On the other hand, a case was deemed not self-manageable if prescription only medication (POM) was prescribed or if a referral to dermatology was made.
There were a total of 2175 consultations, where 246 (11.31%) cases were dermatological. Of the 246, 80 cases (32.5%) could be self-managed. There were 46 different dermatological presenting complaints of which the 5 most common included: rash (51 cases), dermatitis (44 cases), acne vulgaris (13 cases), moles (12 cases), dry skin (11 cases). None of the acne or moles cases could be self-managed, whereas 23%, 68.2%, 72.7% of rashes, dermatitis, and dry skin cases, respectively, could be self-managed.
Certain dermatological conditions have more potential for self-management than others. Research into teledermatology as a means of addressing patient concern and providing clinical information is important in order to reduce unnecessary consultations.
Improving access to appointments at Laurie Pike Health Centre
Rising demand makes it increasingly difficult for patients to access appointments. Laurie Pike Health Centre (LPHC) operates a predominantly same-day booking policy in order to manage appointment requests from its 18 000 patients. We sought to quantify the number of requests, in order to estimate the unmet demand.
1) To estimate the met and unmet demand for same-day appointments; 2) To assess how capacity for same-day appointments compares to demand; 3) To analyse how well LPHC is utilising its available appointment slots.
We created a data collection tool to count the total number of patient requests by type. We grouped types into four categories: 1) medical appointment requests; 2) sick notes and results requests; 3) other appointment requests (such as healthcare assistant, nurse); and 4) admin/other. Category-specific percentages were applied to call log data to estimate the number of appointment requests per category. Capacity was measured by counting the total number of same-day GP/advanced nurse practitioner (ANP) appointment slots. Consultation records for GP/ANP appointments were analysed to assess the appropriateness of the booking.
Estimated average demand for same-day GP/ANP appointments was 222 per day. Average same-day capacity was 112 slots. After introducing pharmacist and video consultations, average capacity increased to 194 slots per day, a shortfall of 28 appointments. Consultation records indicated that 41% of GP/ANP appointments could have been seen by other practitioners; for example, musculoskeletal practitioners (14%).
GP/ANP appointments alone cannot meet patient demand but a diversified workforce might. Alongside this, efforts to improve care navigation may free up to 41% of GP/ANP appointment slots.
The development of palliative care education and training for GPs in Yangon, Myanmar: a workshop success
Palliative care is an important but often overlooked component of primary care. In Myanmar, early emergence of palliative care is being seen, however no formal community-based services yet exist. Present challenges include resource scarcity and inadequate education and training.
Our goal was to improve understanding and approach towards palliative care by GPs in Yangon.
An initial survey was performed among 42 GPs in Yangon, Mandalay, and Meiktila in March 2019 demonstrating a gap in current training needs and willingness by GPs for this to be improved. A 2-day workshop, the first ever of its kind, was subsequently designed and held for 20 local GPs, consisting of interactive seminars delivered in Burmese.
Improvement in knowledge and confidence were used as measures of success. A true/false-style quiz was distributed pre- and post-workshop demonstrating a mean total score improvement of 15%. Self-reported confidence rating scores regarding confidence when: 1) managing palliative patients; 2) providing holistic care; and 3) breaking bad news, increased by a mean of 25%.
The greatest outcome from this workshop, by far, was the enthusiasm and awareness it generated, support was even gained from the President of the Myanmar Medical Association despite his initial reservations about developing this area. Ultimately, the workshop behaved as an advocate for the introduction of a regular palliative care lecture into the local Diploma in Family Medicine curriculum; it also spurred a group of GPs to further this work and turn the workshop into a regular teaching event.
What influences Roma women attending NHS cervical screening? Knowledge, fear, and passive consent
Recent immigration from Eastern Europe poses new challenges in engaging with women eligible to have smears. The Roma population have low socioeconomic status, low educational status, and a life expectancy 10 years lower than other EU citizens. An audit of smear uptake in four ‘Deep End’ Sheffield practices identified as having >1000 registered Roma Slovak patients, demonstrated smear uptakes between 53% to 40%, all of which are below the Sheffield CCG average of 73.5%.
To establish the barriers, facilitators and attitudes of Roma women towards accessing the NHS cervical screening.
Semi-structured interviews were recorded, transcribed, and analysed thematically using an iterative, with independent verification of emergent themes. Interviews continued to data saturation. Interviews were carried out in the patient’s home or a community centre, facilitated by a trained interpreter.
Sixteen women who self-identified as Roma, were interviewed. The overarching themes of ‘language discordance’, ‘poor educational attainment’, and ‘passivity in receiving care’, influenced the women’s likelihood of smear uptake or the need for screening. These emergent themes underpinned a longstanding distrust of the role of the state in relation to the health needs of the community.
It is vital that we develop and evaluate appropriate interventions to increase smear uptake in migrant and other vulnerable populations. There is a need for the UK to adapt screening programmes to maximise uptake within ‘hard to reach’ groups, such as the ‘Roma’, who are likely to be at the highest risk of cancer and late presentation of the disease.
General practice is ‘different’: qualitative study of acculturation experiences of East Staffordshire general practice specialty trainees
Undergraduate medical education and postgraduate foundation training are largely secondary care based. General practice trainees also spend nearly half of their training in hospital rotations. Little is known about factors that support effective transition into general practice specialty training or belongingness experiences throughout training.
To explore the reported experiences of general practice trainee transition into general practice, training in hospital settings, and views of the future.
Semi-structured interviews with 18 purposively selected trainees plus observation and stakeholder discussions by a visiting Sri Lankan general practice trainee attending the vocational training scheme in a participant observer role.
Mastering core skills of general practice, undergraduate and early experience in general practice during specialty training, and general practice trainer guidance and role modelling facilitated transition. A reduced sense of belongingness during hospital rotations impacted on training and work. Building bridging social connections, personal agency initiatives to bring general practice relevance into hospital training, and secondary care affiliative behaviours were adaptive strategies. Allocation to more general practice relevant duties was thought to create value within the hospital team. General practice trainees are thriving with the support of general practice trainers and colleagues, vocational training scheme, and good work/life balance. International graduates require additional support in specific areas.
Adequate support towards transition into general practice and fostering belongingness in hospital settings is important due to the wider impact on training, patient care, and primary/secondary care integration. We propose a theoretical explanation based on Wenger’s social learning model, which may have useful practical implications.
A primary care network analysis: natural communities of general practices in London
Primary care networks (PCNs) are a new organisational hierarchy introduced in the NHS Long Term Plan with wide-ranging responsibilities. The vision is that they represent ‘natural’ communities of general practices with boundaries that make sense to practices, other healthcare providers, and local communities.
Our study aims to identify natural communities of general practices based on patient registration patterns, using network analysis methods and unsupervised clustering to create catchments for these communities.
Patients resident in and attending GP practices in London were identified from Hospital Episode Statistics from 2017 to 2018. We used a series of novel methods for unsupervised graph clustering. A cosine similarity matrix was constructed representing similarities between each general practice to each other, based on registration of patients in each Lower Super Output Area (LSOA). Unsupervised graph partitioning using Markov Multiscale Community Detection was conducted to identify communities of general practices. Catchments were assigned to each PCN based on the majority attendance from an LSOA.
In total 3 428 322 unique patients attended 1334 GPs in general practices LSOAs in London. The model grouped 1291 general practices (96.8%) and 4721 LSOAs (97.6%), into 165 mutually exclusive PCNs. The median PCN list size was 53 490 and a median of 70.1% of patients attended a general practice within their allocated PCN, ranging from 44.6% to 91.4%.
With PCNs expected to take a role in population health management and with community providers expected to reconfigure around them, it is vital we recognise how PCNs represent their communities. This method may be used by policymakers to understand the populations and geography shared between networks.
Workforce Race Equality Standard survey in general practice: Lewisham 2019
The NHS Workforce Race Equality Standard (WRES) was introduced in 2015 and is mandatory for NHS trusts. Nine indicators have been created to evaluate the experiences of black and minority ethnic (BME) staff compared with the rest of the workforce. The trust data published showed a poor experience of BME staff compared with non BME staff.
To introduce the concept of WRES into general practice and create a baseline from which improvement can be made. A diverse workforce will better serve its population and this will improve health outcomes.
We conducted a survey among all general practice staff members, clinicians, and non-clinicians and asked open-ended questions built around four WRES indicators most applicable to general practice, over a 6-week period in August and September 2019.
We collected 151 responses out of a total workforce of around 550. The response rate between clinicians and non-clinicians was equal 50.6% versus 49.4%. The distribution of non BME staff 51% versus BME staff 49% mirrors the diverse population of Lewisham. 54% of BME staff experienced bullying from patients, their relatives, and members of the public. 25% experienced bullying from a colleague or staff member in the workplace and 22% of BME staff changed jobs as a result of this.
BME staff in general practice report high levels of racism, especially from service users. In 22% this led to a career change. A zero-tolerance policy needs to be enforced and a multi-pronged approach is required to address this.
‘Would you like to join the NHS Organ Donor Register?’ A general practice feasibility study
A shortage of organ donors exists in the UK and targeting family consent is key for increasing donation consent rates. Registration on the NHS Organ Donor Register (NHS ODR) facilitates this, as it guides families on their loved ones donation preference. In general practice, an opportunity to register is provided, however only to new patients. To improve access to registration opportunities, an intervention was designed where general practice staff asked their patients if they wished to register as an organ donor.
To assess an organ donation registration intervention for feasibility and acceptability in a UK general practice setting.
One general practice, in Luton, UK, conducted the intervention for 3 months (April to July 2018). Training was held in March 2018, and leaflets and posters were displayed for the 3-month period. An embedded experimental mixed-methods design was used, with data collected via SystmONE questionnaires, surveys and focus groups.
The intervention was found to be feasible and acceptable to conduct with some patients by some staff members. During the 3 months, patients were asked in 12.4% of face-to-face consultations ( n =812). Nurses and healthcare assistants were more able to conduct the intervention than doctors. Lack of time, telephone consultations, and it not being appropriate were the most common reasons for not asking. Finally, 244 patients joined the NHS ODR; 30.4% of those asked.
This study demonstrates that general practice could be a feasible location in which an intervention designed to increase NHS ODR registration could be conducted
An exploration of stakeholders’ perceptions of the extent to which the individual and collective views of patients with long-term conditions and their carers are heard and used to inform commissioning decisions within primary care
Involving patients and carers in decisions that influence the delivery of health services is a statutory requirement across the NHS. However, current evidence suggests a gap exists between the theory, legislation and policy intentions and their practical implementation.
This research aimed to identify the nature and extent of that perceived gap.
Adopting a mixed-methods approach using questionnaires and semi-structured interviews, stakeholders’ perceptions were explored regarding the extent to which the views of patients with long-term conditions and their carers are heard and used within primary care, across four clinical commissioning groups. Descriptive statistics were used to analyse the quantitative data; thematic analysis was applied to explore the qualitative data.
Data analysis demonstrated considerable difference between patients’ and carers’ perceptions and those of healthcare professionals regarding how well involvement is implemented. Three key themes emerged that were perceived to influence the effectiveness of involvement. These related to the need for effective communication of relevant, accessible information that meets people’s requirements; the need to take account of individuals’ expectations, ability, motivation, assumptions, and previous experience; and the need for organisations to provide effective systems and processes, including adequate time and focused training to support involvement, in addition to robust monitoring and evaluation of the extent to which outputs from involvement influence commissioning decisions.
The literature suggests that no existing framework addresses all three key themes. Therefore, a revised framework for involvement was developed, informed by the three key themes, that can be tested across a larger sample and different healthcare settings.
Identification and management of frailty in English primary care: a qualitative study of national policy
Policymakers are directing attention to addressing the needs of an ageing population. Since 2017, general practices in England have been contractually required to identify and code ‘frailty’ as a new clinical concept and, in doing so, support targeted management for this population with the aim of improving outcomes. However, embedding frailty policies into routine practice is not without challenges and little is currently known about the success or otherwise of the programme.
To explore the implementation of a national policy on frailty identification and management in English primary care.
Semi-structured interviews were conducted with GPs ( n = 10), nurses ( n = 6), practice managers ( n = 3) and health advisors ( n = 3). Normalisation Process Theory (NPT) and System Thinking provided sensitizing frameworks to support data collection and analysis.
Primary care professionals were starting to use the concept of frailty to structure care both within practices and across organisations, however, there was widespread concern about the challenge of providing expanded care for the identified needs within existing resources. Concerns were also expressed around how best to identify the frail subpopulation and the limitations of current tools for this, and there was a professional reticence to use the term ‘frailty’ with patients.
Findings suggest that additional focused resources and the development of a stronger evidence base are essential to facilitate professional engagement in policies to improve the targeted coding and management of frailty in primary care.
Study design of the Fasting In diabetes Treatment (FIT) trial: a randomised, controlled, assessor blinded intervention trial which examines the effect of intermittent use of a fasting mimicking diet in patients with type 2 diabetes
Caloric restriction is an effective way to treat type 2 diabetes (DM2). However, chronic restriction of food intake is difficult to sustain. Intermittent total fasting exerts similar metabolic effects, but may be even more challenging for most patients. A fasting mimicking diet (FMD) was designed to achieve the metabolic benefits of total fasting, despite considerable calorie content. The effects of a FMD in DM2 patients are still unknown.
To determine the effect of intermittent use (5 consecutive days a month during a year) of a FMD in DM2 patients on metabolic parameters and DM2 medication use compared to usual care.
One hundred DM2 patients from general practices in the Netherlands with a BMI ≥ 27 kg/m 2 , treated with lifestyle advice only or metformin, will be randomised to receive the FMD plus usual care or usual care only. Primary outcomes are HbA1c and DM2 medication dosage. Secondary outcomes are anthropometrics, blood pressure, plasma lipid profiles, quality of life, treatment satisfaction, metabolomics, microbiome, MRI (for example, cardiac function and fat distribution), cost-effectiveness, and feasibility in clinical practice.
The first 70 patients are included. Follow up will be completed in April 2021.
Our results will show whether monthly cycles of a FMD are feasible in clinical practice, if they improve metabolic parameters and/or reduce the need for medication in DM2 and if this is a cost-effective intervention.
Emergency Admission Risk Prediction (EARP) tools in primary care to reduce emergency admissions to hospital: clash of evidence and practice
Policy initiatives have incentivised use of EARP tools in primary care to reduce emergency admissions. A recently published trial in South Wales found that EARP increased emergency admissions and emergency department attendances without clear benefits. This cost the NHS an additional £76 per patient per year. But the use of EARP in primary care across the UK was unknown.
To assess implementation and facilitators use of EARP tools in primary care across the UK.
Structured email survey of 235 UK primary care commissioners across the UK.
There were 148 (87%) of 171 responders (73%) who reported that EARP tools were available in their areas. We identified 39 different EARP tools in use. Access to EARP tools varied widely by country: Northern Ireland (100%), Scotland (91%), England (76%) and Wales (14%). Promotion by NHS commissioners, and engagement of clinical leaders and practice managers were identified as the most important factors in encouraging use of EARP tools. Research evidence was seen as less important. Nearly 40% of areas using EARP reported that they had revised services as a result, but few reported use of EARP for service evaluation.
Though EARP tools are widely available in primary care, new evidence shows that they are counter-productive. We estimate that by delaying the dissemination of EARP for evaluation NHS Wales saved >£200 million per year. We encourage further research and discussion about next steps in use of EARP tools in emergency admission prevention in the UK.
Anticipatory care planning for older adults: a trans-jurisdictional feasibility study
As the population of older adults’ increases, the complexity of care required to support those who choose to remain in the community has also increased. Anticipatory Care Planning (ACP) through earlier identification of healthcare needs is evidenced to improve quality of life, decrease the number of aggressive futile interventions, and even to prolong life.
To determine the feasibility of a cluster randomised trial to evaluate the implementation and outcomes of Anticipatory Care Planning (ACP) in primary care to assist older adults identified as at risk for functional decline by developing a personalised support plan.
GP practices were randomised into control/intervention groups stratified by jurisdiction [Northern Ireland (UK) and the Republic of Ireland (RoI)], and by setting (urban and rural). Participants were included if they were a) aged ≥70 years, b) 2 or more chronic medical conditions, c) 4 or more prescribed medications. The Anticipatory Care Plan consisted of home visits where the study nurse discussed patients’ goals and plans. An action plan was put in place following consultation with patient’s GPs and study Pharmacist.
Eight primary care practices participated; four in the UK and four in the RoI. Sample n = 64. Data was collected pertaining to patient quality of life, mental health, healthcare utilisation, costs, perception of person-centred care, and the use of potentially inappropriate medication.
Unique insights relating to the trans-jurisdictional delivery of healthcare services in the UK and RoI were observed which has implications on service delivery for older adults.
Vitamin D deficiency is associated with increased risk of postural hypotension in older men: a cross-sectional analysis from The British Regional Heart Study
There is growing interest in the role of vitamin D in extra-skeletal health, including postural hypotension. Postural hypotension is found in 1 in 5 community-dwelling adults aged 60 years and above. It increases risk of falls, fractures, cardiovascular disease and all-cause mortality. Better understanding of the aetiology of postural hypotension may help yield more effective treatment options than those that are currently available.
The aim of this study was to investigate the association between circulating vitamin D, parathyroid hormone and postural hypotension.
This was a cross-sectional analysis of 3620 community-dwelling men living in the UK (mean age 68.6 years; standard deviation 5.5 years). Vitamin D status (nmol/L) was categorised as sufficient (≥50), insufficient (≥25 – <50), or deficient (<25). Parathyroid hormone levels were categorised by quintiles. Postural hypotension was defined by consensus criteria as a decrease in systolic blood pressure ≥20 mmHg and/or diastolic blood pressure ≥10 mmHg that occurred within three minutes of standing.
Compared to sufficient levels of vitamin D, vitamin D deficiency increased risk of postural hypotension that specifically occurred within one minute of standing (OR 1.51, 95% CI = 1.06 to 2.15) in multinomial, multiple logistic regression. Neither vitamin D insufficiency, nor elevated parathyroid hormone, were associated with postural hypotension.
In this study, vitamin D deficiency was associated with increased risk of postural hypotension. Further research may help clarify whether treating vitamin D deficiency can reduce the degree of postural hypotension, or if preventing the progression to vitamin D deficiency can reduce the incidence of postural hypotension.
How can referrals of patients who are obese to the local exercise referral scheme be increased? A UK based primary care quality improvement study
Obesity is classified as a body mass index (BMI) >30kg/m 2 and contributes to poor health outcomes in the UK. In 2017–18, obesity resulted in 711,000 hospital admissions. The National Institute for Health and Care Excellence (NICE) recommends GPs educate patients who are obese and refer them to exercise programmes. Our practice, Brierley Park Medical Centre, (NHS Mansfield and Ashfield CCG) is in a 4 th decile most deprived region of North Nottinghamshire (UK) and serves a population of 9,288. The local exercise referral scheme (ERS) allows clinicians to refer patients to the local gym for a reduced fee at the point of access.
To calculate and increase the number of adult patients who are obese in our practice who are referred to the local ERS.
The number of adult obese patients who were referred to the local ERS scheme from October 2018 to September 2019 was calculated. An intervention comprising internal system alerts, GP education utilising Making Every Contact Count framework and targeted patient group text alerts was designed and delivered. Pre (cycle 1) and post (cycle 2) intervention data from November to February were generated and compared.
In total, 2766 adult obese patients (29.8% of practice population) were identified: 16 (0.2%) patients were referred to ERS during cycle 1.96 (1%) patients were referred during cycle 2.
The interventions that we have designed and implemented have increased the number of referrals to ERS and may be applied to similar primary care settings.
Evaluating interprofessional education: initial learning from a domestic abuse conference
The importance of multi-agency working to identify, prevent and reduce domestic abuse is widely recognised. Interprofessional learning opportunities can provide a supportive learning environment for multi-agency practitioners to explore and develop collaborative approaches to improve health outcomes for vulnerable children, young people and their families.
Participants drawn from Kent GP trainees, student Health Visitors, School Nurses, Midwives, Social Workers, student Teachers and Special Educational Needs Coordinators (SENCOs), and postgraduate Police Officers attended this sixth annual conference.
To enable participants to understand why domestic abuse is a serious public health issue; identify indicators of domestic violence and abuse; identify opportunities for safe enquiry and know how to respond; critically reflect on ethical, legal, professional and interprofessional challenges for practitioners; and reflect on and explore opportunities for inter-professional working.
Multi-disciplinary educators delivered formal presentations and facilitated interprofessional workshops.
Data from anonymised pre- and post- conference questionnaires distributed on the day, included quantitative questions using a Likert scale 1–5 and open and closed qualitative questions.
In total, 75 out of a possible 121 participants completed both questionnaires (62%). The above aims were all met. In all questions participants gave higher scores after the conference indicating increased levels of knowledge and confidence. The qualitative comments highlighted the learning benefits from interprofessional group work. 100% (average score 4.5) agreed that facilitators fostered a supportive learning environment.
The conference provided a highly valued opportunity for useful interprofessional learning about domestic abuse. Results indicated that it increased participants’ knowledge and confidence about their own and others’ roles and responsibilities.
What do patients want? A qualitative exploration of patients’ needs and expectations regarding online access to their primary care record
Primary care records have traditionally served the needs and demands of clinicians rather than those of the patient. GP contracts in England state practices must promote and offer registered patients online access to their primary care record and research has shown benefits to both patients and clinicians of doing so. Despite this, we know little about patients’ needs and expectations regarding online access.
To explore patients’ views about accessing online primary care records and to find out how patients would like to interact with their records and what support they may need.
Interviews and focus groups with a sample of 50 patients from a variety of socio-demographic backgrounds who were either; eligible for the NHS Health Check; had multimorbidities or were carers. Thematic analysis of data identified major themes impacting upon patients’ wishes and needs as well as highlighting population-specific issues.
Participants highlighted a wide range of views about the benefits and drawbacks of accessing their records online. The majority of participants indicated that they would be more likely to access their online primary care record if improvements were made to the design, reliability and functionality of existing online record services. Carers found accessing online records particularly useful.
Consultation with patients and carers about their experiences of accessing online records; support needs and preferred functions can provide useful insights to inform the future design of online record services.
MULTIPAP Study: Improving healthcare for patients with multimorbidity
The steady rise in multimorbidity entails serious consequences for our populations, challenges healthcare systems, and calls for specific clinical approaches of proven effectiveness. The MULTIPAP Study comprises three sequential projects (MULTIPAP and MULTIPAP Plus RCTs, and the MULTIPAP Cohort). Results of MULTIPAP RCT are presented.
To evaluate the effectiveness of a complex, patient-centred intervention in young-old patients with multimorbidity and polypharmacy.
Pragmatic cluster-randomised clinical trial in a primary healthcare setting. GPs were randomly allocated to either conventional care or the MULTIPAP intervention based on the Ariadne Principles with two components: GPs e-training (that is, eMULTIPAP addresses specific, key concepts on multimorbidity, polypharmacy and shared decision-making) and GP–patient-centred interview. Young-old patients aged 65–74 years with multimorbidity and polypharmacy were included. Main outcome: difference in the Medication Appropriateness Index (MAI) after 6-month follow-up between groups. Secondary outcomes: MAI, quality of life, patient perception, health services use, treatment adherence and cost-effectiveness after 12-month follow-up.
117 GPs from 38 Spanish primary health care recruited 593 patients randomly assigned to the intervention/control groups. Difference in MAI scores between groups in the intention-to-treat analysis after 6 months’ follow-up: −2.42 (−4.27 to −0.59), P = 0.009 (adjusted difference in mean MAI score −1.81(−3.35 to −0.27), P = 0.021). Secondary outcomes: not significant, including quality of life (adjusted difference in mean EQ-5D-5L (VAS) 2.94 (−1.39 to 7.28), P = 0.183, EQ-5D-5L (index) −0.006(−0.034 to 0.022), P = 0.689).
The intervention significantly improved medication appropriateness. The observed quality of life improvement was not significant. GPs e-training in multimorbidity has shown to be feasible and well accepted by the professionals. Future studies may test whether this format facilitates implementation.
GPs’ experience of safeguarding in care homes: what do they see and what do they do?
Abuse of older people in care homes is an on-going problem. GPs, as the most frequent practitioner group visiting care homes, have an important role in detecting and reporting abuse. However, there is little research about GPs’ experiences of working in care homes and how they work to safeguard residents.
To explore the challenges experienced by GPs working in this unique environment and how these impact on safeguarding.
An online survey collected qualitative data about GPs’ experiences as visiting professionals to care homes, with an emphasis on safeguarding. A thematic analysis identified key themes.
In total, 58 completed surveys were returned, with a range of practitioner experience represented (1–30 years). Approximately 70% were GP partners, with the remainder salaried and locum doctors. Over one third reported they had witnessed signs of definite or possible abuse within care homes. Emerging themes related to the complex care home context, in which residents had multiple health needs and GPs had to build multiple relationships with managers, carers, families, and residents. Difficulties in accessing information were reported; residents could not always provide information, GPs had to rely on others for information, and rarely had access to electronic records.
GP work in care homes is a complex and skilled role, in which GPs encounter evidence of poor care and abuse. Key themes in respect of barriers and facilitators of good care were highlighted. The reliance on others for information and the need to build relationships with staff/managers may raise tensions in respect of safeguarding practice.
If GPs who teach medical students were assisted to be good role models might this influence the medical career the students choose?
Most patients are cared for in the community by GPs, and workforce planning for the UK NHS suggests that 50% of medical school graduates need to train as GPs. While there is pressure on medical schools to provide more student teaching in general practice, general practice must be prepared for this increase in workload and teachers should have appropriate training.
This study examined the influence that teachers as role models can have on the development and career choices of medical students and whether GPs who teach medical students might benefit from assistance in developing positive attributes.
A literature search was carried out. Relevant papers were those that examined the influence of a doctor as teacher role model for medical students, both in assisting in professional development and clinical skills, and in influencing career choice.
The review identified eleven papers. There was evidence of association between a student having an influential role model as teacher and choosing specialty training in that area, although evidence of a causative connection is less convincing. A recurring theme is the recommendation that teachers should be aware of the influence they can have as role models, both positive and negative.
As medical student teaching moves into general practice GPs who teach will need to be helped to understand and develop positive role model attributes, to promote general practice as an attractive career to the students. Further research needs to identify the extent of assistance required and whether medical schools are prepared for this extra responsibility.
Quantifying empathy levels among UK undergraduate medical students: an online survey
Empathy is a key health care concept and refers to care that incorporates understanding of patient perspective’s, shared decision making, and consideration of the broader context in which illness is experience. Evidence suggests experiences of doctor empathy correlate with improved health outcomes and patient satisfaction. It has also been linked to job satisfaction, and mental wellbeing for doctors. To date, there is a paucity of evidence on empathy levels among medical students. This is critical to understand given that it is a key point at which perceptions and practices of empathy in the longer term might be formed.
To quantify the level of empathy among UK undergraduate medical students
An anonymised cross-sectional online survey was distributed to medical students across three universities. The previously validated Davis’s Interpersonal Reactivity Index was used to quantify empathy. The survey also collected information on age, sex, ethnicity, year of medical school training and included a free-text box for ‘any other comments’.
Data analysis is currently underway with high response rates. Mean empathy scores by age, sex, year of study and ethnic group are presented. A correlation analysis will examine associations between age and year of study, and mean empathy sores.
These data will help to provide a better understanding of empathy levels to inform the provision of future empathy training and medical school curriculum design. Given previous evidence linking experiences of empathy to better health outcomes, the findings may also be significant to future patient care
Patients’, healthcare providers’, and health insurance employees’ preferences for knee and hip osteoarthritis care: a discrete choice experiment
Despite the wide range of treatment options for knee and hip osteoarthritis (KHOA), suboptimal care, low uptake and low adherence to treatment is widely seen. We need to gain insight into preferences for KHOA treatment.
To determine patients’, healthcare providers’ and healthcare insurance employees’ preferences for existing health care for KHOA.
A survey containing a discrete choice experiment (DCE) was conducted. Patients with KHOA, healthcare providers (orthopaedists and GPs), and insurance employees had to choose scenarios that differed in six attributes: waiting times, out of pocket costs, travel distance, involved healthcare providers during consultation, length of consultation and access to specialist equipment. A (panel latent class) conditional logit model was used to determine the relative importance of the attributes and trade-offs that responders made, and to explore preference heterogeneity.
A total of 648 patients completed the DCE. All six attributes played a significant role in patients’ choices. On average, out of pocket costs were deemed undesirable by patients. A GP with an orthopaedist during the consultation was preferred compared to a GP alone. Healthcare providers ( n = 76) and insurance employees ( n = 150) showed similar preferences, with respect to out of pockets costs being valued less important. Latent class analysis identified four classes of patients varying in their preferences.
Patients prefer less out of pocket costs and a GP with an orthopedists during consultation for KHOA care. Four subgroups of patients were identified that vary in preferences for KHOA care. These subgroups could provide opportunities to improve uptake, adherence and effectiveness of KHOA care.
Chest discomfort at night and risk of acute coronary syndrome: cross-sectional study of telephone conversations
During telephone triage it is difficult to assign the adequate urgency to patients with chest discomfort. Considering the time of calling could be helpful.
To assess the risk of acute coronary syndrome (ACS) in certain time periods and whether sex influences this risk.
Cross-sectional study of 1,655 recordings of telephone conversations of patients who called the out-of-hours services primary care (OHS-PC) for chest discomfort. Call time, patient characteristics, symptoms, medical history and urgency allocation of the triage conversations were collected. The final diagnosis of each call was retrieved at the patient’s general practice. Absolute numbers of patients with and without ACS were plotted and risks per hour were calculated. The risk ratio of ACS at night (0 am to 9 am) was calculated by comparing to the risk at other hours, and was adjusted for gender and age.
The mean age of callers was 58.9 (SD ± 19.5) years, 55.5% were women and in total, 199 (12.0%) had an ACS. The crude risk ratio for an ACS at night was 1.80 (CI = 1.39 to 2.34, P <0.001); 2.33 (1.68 to 3.22, P <0.001) for men, and 1.29 (0.83 to 1.99, P = 0.256) for women. The adjusted risk ratio for ACS of all people at night was 1.82 (1.07 to 3.10, P = 0.039).
Patients calling the OHS-PC for chest discomfort between 0–9 am have almost twice a higher risk of ACS than those calling other hours, a phenomenon more evident in men than in women. At night, dispatching ambulances more ‘straightaway’ could be considered for these patients with chest discomfort.
Missed acute coronary syndrome during telephone triage at out-of-hours primary care: lessons from a case-control study
Serious adverse events (SAE) at out-of-hours services in primary care (OHS-PC) are rare. It most often concerns missed acute coronary syndromes (ACS). Root cause analyses highlighted errors in the triage process, but these analyses are hampered by hindsight bias.
To compare triage calls at the OHS-PC of missed ACS with matched controls with chest discomfort but without a missed ACS; and to assess predictors of missed ACS.
A case-control study with triage recordings of calls of a missed ACS registered between 2013–2017. Controls were from the same period. Cases were matched 1:8 with controls based on age and gender. Clinical, patient and call characteristics were assessed, and 15 expert GPs rated the triage safety and quality, being blinded to the final diagnosis. We applied conditional logistic regression analysis.
Fifteen missed ACS calls and 120 matched control calls were included. Cases used less cardiovascular medication (38.5% versus 64.1%, P = 0.05), and more often experienced retrosternal chest pain (63.3% versus 24.7%, P = 0.02) than controls. Consultation of the supervising GP (86.7% versus 49.2%, P = 0.02) occurred more often in cases than controls. Experts rated the triage of cases more often as ‘poor’ (33.3% versus 10.9%, P = 0.001), and ‘unsafe’ (73.3% versus 22.5%, P <0.001) than that of controls.
It seems nearly impossible to differentiate missed ACS at the OHS-PC from others with chest discomfort based on symptom presentation.
The Moving Healthcare Professionals Programme
Healthcare professionals (HCPs) are estimated to see nearly 500 000 patients during their career. Evidence demonstrates that one in four patients would be more active if advised by their GP. However, there is a lack of engagement between HCPs and patients regarding the benefits of physical activity (PA). PA is not discussed with 80% of patients, with 75% of GPs feeling they lack knowledge to advise their patients.
Moving Healthcare Professionals Programme (MHPP) aims include increasing awareness and skills in PA for prevention and management of ill health; changing clinical practice in the promotion of activity; and evaluating impact to identify ‘what works’.
GPs were recruited as Physical Activity Clinical Champions (PACCs) to deliver peer-to-peer training to HCPs nationally. Additionally, relationships were developed with undergraduate medical schools to embed PA into curriculum. A PA advice pad was developed as a local GP pilot, while the ‘Moving Medicine’ online resource was created.
Over 22 000 HCPs were trained to date, with evaluation demonstrating an increase in knowledge, skills and confidence, and over 18 000 completions of our eLearning modules. PA coverage was expanded across the undergraduate curriculum at multiple medical schools, while feedback on the e-advice pad pilot has informed a further digital pilot. Additionally, there were >3000 monthly users of ‘Moving Medicine’.
This work demonstrated scope for significant improvements in HCP engagement in multiple clinical settings. Working with GPs has proved crucial to this success across various workstreams, with their participation a continued focus moving into Phase 2.
A qualitative evaluation of a prescribing e-learning package for general practice
The GMC PRACtiCe study identified a 1 in 20 error rate in prescriptions issued in general practice and identified a need for further training in prescribing. As a result, an e-Learning prescribing package was designed and launched to healthcare professionals through the Royal College of General Practitioners in January 2014.
This part of the study explored the longer-term impact on prescribing knowledge, attitudes and behaviours of practitioners completing the eLearning prescribing package.
On completion of the e-Learning package, participants were asked to indicate their willingness to be contacted for a telephone interview. Semi-structured interviews were conducted which were audio recorded, transcribed verbatim and analysed using thematic analysis, aided by NVivo. Interviewees were invited to enter a prize draw to win Stockley’s Drug Interaction textbook (provided courtesy of the Royal Pharmaceutical Society).
Of the 120 participants who expressed an interest in being followed up for interview, seven prescribers were interviewed in 2014 and 2015. Reasons for completing the course were explored, and interviewees gave examples of changes made to their prescribing practice as a result of completing the e-Learning. This included the adoption of specific strategies to enhance safe practice, and enacting enhanced vigilance in key areas such as renal function monitoring. Some changes to the course content and presentation were also recommended.
These interviews have highlighted the potential for using e-Learning for prescribing training and to achieve long-term changes in prescribing practice. However, further work is needed to generate substantive evidence of its impact on prescribing.
Awareness and use of online appointment booking in general practice: analysis of GP Patient Survey data
General practices are required to provide online booking to patients in line with policy to digitise access. However, uptake of online booking by patients is currently low and there is little evidence about awareness and use by different patient groups.
To examine variability in awareness and use of online appointment booking in general practice.
Secondary analysis of two questions from the GP Practice Survey data (2018) asking about awareness and use of online booking of appointments. Multivariable logistic regression was used to examine associations with age, gender, ethnicity, deprivation, the presence of a long-term condition, long-term sickness and being deaf.
In total, 43.3% (277 278/647 064) of responders reported being aware of being able to book appointments online, while only 15% (93 671/641 073) reported doing so. There was evidence of variation by all factors considered, with strong deprivation gradients in both awareness and use (for example, most versus least deprived quintile OR for use: 0.63 (95% CI = 0.61 to 0.65). There was a reduction in awareness and use in patients >75 years of age. Patients with long-term conditions were more aware and more likely to use online booking.
While over 40% of patients know that they can book appointment online, the number that actually do so is far lower. With the constant push for online services within the NHS and the roll out of the NHS app, practices should be aware that not all patient groups will book appointments online and that other routes of access need to be maintained to avoid widening health inequalities.
Interpreter costs across clinical commissioning groups in England 2017–2018: a cross sectional survey using ‘freedom of information’ requests
Professional interpreters are considered to be the gold standard when meeting the needs of patients with limited English proficiency (LEP) in primary care. The models by which CCGs supply interpreting services (IS) vary. Many CCGs use external commercial IS, while other CCGs commission ‘not for profit’ services such as the Advocacy and Interpreting Service in Tower Hamlets, the Sussex Interpreting Service, and the decommissioned Sheffield Community Access and Interpreting Service. Research on comparative costs and needs of the LEP population is lacking.
To compare the costs of interpreting services between CCG’s in England.
A cross-sectional study involving CCGs in England. A standardised request was sent to 195 CCGs inviting comment on how much the CCG spent (2017–2018) on IS. The data were plotted against a number of demographic variables ( https://fingertips.phe.org.uk ) and analysed using regression analysis.
Survey response rate: 86% of CCGs ( n = 169). Of those CCGs who responded, 39% ( n = 66) did not hold IS cost data. NHS England spent £2 951 348.16 for IS services for the year 2017–2018. A positive correlation was noted with increased cost of interpreting services when plotted against increasing percentage BME or percentage birth to non-UK parents. However, there were wide variations around correlation of best fit indicating variation in spending between CCGs for similar populations.
Inter CCG variation in correlations between demographic variables and expenditure suggests further research is needed to determine how to optimise and resource safe and equitable IS across the UK population.
Determinants of primary care workforce variation in England
The General Practice Forward View (GPFV) outlined how the government plans to attain a strengthened model of general practice. A key component of this proposal is an expansion of the workforce by employing a varied range of practitioners, in other words ‘skill mix’. A significant proportion of this investment focuses on increasing the number of ‘new’ roles such as clinical pharmacists, physiotherapists, physician associates, and paramedics.
The aim of this study is to examine what practice characteristics are associated with the current employment of these ‘new’ roles.
The study uses practice level workforce data (2015–2019), publicly available from NHS Digital. The authors model FTE of specific workforce groups (for example, advanced nurse) as a function of deprivation, practice rurality, patient demographics (total list size and percentage of patients aged >65 years) and FTEs from other staff groups.
Although analysis is ongoing, initial estimation suggests that the employment of ‘new’ roles has occurred in larger practices (in terms of list size), in practices with a higher proportion of patients living in deprived areas and practices with a larger proportion of patients aged >65 years. FTE for advanced nurses is negatively associated with GP FTE.
A negative correlation between advanced nurse FTE and GP FTE is potentially suggestive of substitution between roles, deliberate or otherwise. For example, practices may employ ‘new’ roles if they are unable to recruit GPs or they may recruit staff to free up GP time. Further work is needed to confirm these findings and to explore the reasons behind practice employment decisions.
Motivating factors behind skill mix change: results from a practice managers’ survey in England
The expansion of the primary care workforce by employing a varied range of practitioners (‘skill mix’) is a key component of the General Practice Forward View (GPFV). The extent of skill mix change and where that has occurred has been examined using publicly available practice level workforce data. However, such data does not provide information regarding specific motivating factors behind employment decisions for individual practices nor future workforce plans.
To identify key motivating factors behind practice workforce decisions and their future workforce plans.
An online questionnaire was sent to practice managers in England. Data collection is ongoing; however, 1000 practices have responded to the survey so far. The questionnaire was composed of questions related to current workforce, motivating factors behind employment decisions, planned future workforce changes, financial assistance with employing staff (for example, HEE or CCG funding) and ideal workforce.
Early results indicate that practices that have employed physician associates have done so to increase appointment availability (78% of practices) and release GP time (68%). Sixty-six per cent of practices who have employed pharmacists have received some form of financial assistance with 21% of practices still receiving assistance. When asked to construct an ideal workforce, ‘new’ roles accounted for 20% of that workforce on average, which is a significantly larger proportion than those roles currently account for.
Although data collection and analysis are ongoing, the results of the survey provide novel insights into the underlying motivating factors behind employment decisions, specifically for new roles such as pharmacists, PAs and paramedics.
Time for change? A comparative analysis of GPs’ opinions on appointment length
The research on the benefits, disadvantages and factors that affect appointment length in general practice is fragmented. There is a need to draw the evidence together and who better to assess this than those on the front line.
To investigate GPs’ opinions on appointment length, including the factors that affect appointment length, its impact on doctors and the validity of increasing appointment length.
A questionnaire was sent to six general practices in Bristol and was completed by 30 GPs (response rate = 100%). Analysis of current appointment length, satisfaction and the ideal length was undertaken, alongside thoughts about the advantages and disadvantages of longer appointments. Ethical approval was successfully sought from Student Research Ethics Committee.
Most doctors have 10-minute appointments ( n = 29); however, 90% ( n = 27) wished for 15 minutes. Appointments overrunning was described as a constant problem and resulting in stress. Longer appointments were due to multiple problems in a single consultation, mental health and multimorbidity. There did not appear to be any variation in viewpoints with practices, clinician experience and session length. The benefits of a longer appointment were a greater ability to deal with complex conditions, improved decision making, stress reduction and time to talk about interventions. However, 93.3% ( n = 28) of doctors were concerned that there would be less appointments available if appointment lengths increased.
Most doctors would like longer appointments. In light of the concern about appointment availability, there needs to be research into whether this would substantiate.
In situ deteriorating patient simulation in general practice
GP practices have limited access to medical emergency training and basic life support is often taught out of context as a skills-based event.
To develop and evaluate a whole team integrated simulation-based education, to enhance learning, change behaviours and provide safer care.
Phase 1: 10 practices piloted a 3-hour programme delivering 40 minutes BLS and AED skills and 2-hour deteriorating patient simulation. Three scenarios where developed: adult chest pain, child anaphylaxis and baby bronchiolitis. An adult simulation patient and relative were used and a child and baby manikin. Two facilitators trained in coaching and debriefing used the 3D debriefing model. Phase 2: 12 new practices undertook identical training derived from Phase 1, with pre- and post-course questionnaires. Teams were scored on: team working, communication, early recognition and systematic approach. The team developed action plans derived from their learning to inform future response. Ten of the 12 practices from Phase 2 received an emergency drill within 6 months of the original session. Three to four members of the whole team integrated training, attended the drill, but were unaware of the nature of the scenario before. Scoring was repeated and action plans were revisited to determine behaviour changes.
Every emergency drill demonstrated improved scoring in skills and behaviour.
A combination of: in situ GP simulation, appropriately qualified facilitators in simulation and debriefing, and action plans developed by the whole team suggests safer care for patients experiencing a medical emergency.
GP views on the routine identification of older people living with frailty in primary care
To meet the challenges of an ageing population, the updated 2017/18 NHS GP contract requires primary care providers to use evidence-based frailty identification tools to risk-stratify all patients aged >65 years. Those patients flagged as moderately or severely frail should be clinically reviewed and if severe frailty is confirmed, providers have been asked to consider offering relevant interventions, with the overall aim of enabling these patients to live well for longer. However, there is limited knowledge about how this frailty contractual requirement is being operationalised in primary care.
To improve understanding of the barriers and facilitators GPs encounter when routinely identifying, risk-stratifying and providing interventions for people living with frailty in primary care.
This was a two-part study: an initial survey via online questionnaire, with participants selected by maximum variation sampling to be followed up with a semi-structured telephone interview. All GPs working in the East Midlands region (Derbyshire, Leicestershire, Lincolnshire, Nottinghamshire, and Northamptonshire) were eligible to take part. The online questionnaire was analysed using descriptive statistics. Interview transcripts were analysed using framework analysis to identify key themes.
In total, 188 GPs responded to the survey. Eighteen GPs were interviewed. Four themes were identified: 1) beliefs about stratification and pro-active identification of frailty; 2) frailty stratification tools; 3) managing complexity, resources and models of care; and 4) drivers of GP behaviour.
The study findings will inform the further development of NHS England policy on the frailty contractual requirement for primary care providers.
Healthcare professionals’ perspectives on lung cancer screening in the UK: a qualitative study
Lung cancer screening with low-dose CT has been shown to decrease mortality. Low lung cancer survival rates in the UK, driven primarily by late-stage presentation, provide the impetus for implementing screening. Nascent guidance on screening in the UK recommends primary care case-finding. However, the potential impact and acceptability on primary care, and the opportunistic utilisation of other case-finding routes such as pharmacies, smoking cessation services and respiratory clinics, have not been fully explored.
To explore healthcare professionals’ views and perspectives about lung cancer screening and their preparedness and willingness to be involved in its implementation.
A qualitative study was carried out with semi-structured interviews conducted with GPs, pharmacists and staff from smoking cessation services within Southwark and Lambeth and from respiratory clinics in Guy’s and St. Thomas’ NHS Trust in London in 2018. Sixteen participants were interviewed, and the interview transcripts were analysed thematically.
Participants described lung cancer screening as an important diagnostic tool for capturing lung cancer at an earlier stage and in increasing survivorship. However, the majority expressed a lack of awareness and understanding, uncertainty and concerns about the validity of screening, its misuse and the potential impact on their patients and workload.
Study participants had mixed opinions about lung cancer screening and expressed their concerns about its implementation. Addressing these concerns by providing resources and effective and detailed guidelines for their use may lead to greater engagement and willingness to be involved in lung cancer screening.
Achieving better quality care in general practice: are incentives the answer?
The introduction of financial incentives, such as the quality and outcomes framework (QOF), historically lead to improvements in standardising practice. However, with shifting demands on healthcare providers, are these schemes still enough to drive high-quality care?
To explore current incentives, intrinsic and extrinsic, their role and effectiveness in improving quality of care and how they are perceived by GPs.
Mixed methods study using two systematic literature reviews including 44 papers and 18 semi-structured interviews with GPs.
In the literature, QOF was associated with reduced socioeconomic inequalities, decreased mortality and improved outcomes. However, the absence of control groups and the simultaneous analysis of multiple indicators complicates the findings. GPs agreed with the literature and viewed financial incentives as beneficial, however, they felt the key driver in providing good-quality care was their intrinsic motivation. Financial incentives were found to contribute to depersonalised care, diluted provision of non-incentivised activities and hindered overall practice. The results from the second literature review were in keeping with the views of the participants. They illustrated the importance of managing factors contributing to physician burnout, reduced performance, and low job satisfaction, which can result in the provision of low-quality care.
Financial incentives have the potential to induce behaviour change, however, their use in quality improvement is limited when used alone. If used in an environment that nurtures intrinsic motivation, healthcare providers will be more driven to achieve a higher quality of care and will be better able to cope with shifting demands.
2017 Cancer Prevalence Dashboard for London
As cancer incidence increases and survival improves, the number of people living with a cancer diagnosis is increasing. People living with cancer have 50% more contact with GPs 15 months after diagnosis than a population of similar age, sex and locality; 70% have another long-term condition.
To aid service providers’ understanding of the cancer prevalent population by creating a publicly available visualisation tool that both describes patients’ demographics and length of time lived with cancer, and compares counts of nationally registered cancer survivors to GP-maintained registers.
Using National Cancer Registration and Analysis Service (NCRAS) data, prevalence rates and counts were generated for London patients diagnosed 1995–2017 and alive 31 December 2017, overall and for lower-level geographies. GP-recorded Quality and Outcomes Framework (QOF) prevalence at Clinical Commissioning Group (CCG) level was compared to NCRAS counts for the same period.
On 31 December 2017, 231 740 (2.6%) people were living with cancer in London; 33% were diagnosed 5–9 years prior and 31% were diagnosed ≥10 years prior. Prevalence was higher in women ( P <0.001) and dramatically increased with age for London ( P <0.001); >12% of >75 year olds were living with a cancer diagnosis in every lower-level geography. Completeness of GP QOF cancer registers against NCRAS prevalence counts ranged from 75–108% across CCGs.
Local understanding of the cancer prevalent population is needed, with a concerted effort to interpret large discrepancies between QOF and NCRAS registers, which may arise from differences in coding practice. Ensuring patients are identified in primary care is a first key step to managing cancer as a long-term condition.
How do you diagnose asthma? A multiple case study design to understand and explain current use of national guidelines by primary care clinicians
Clinical guidelines for asthma are available to UK clinicians but implementation is not straightforward. Diagnostic and treatment inadequacy contribute to patient morbidity and mortality and lack of adherence to guidelines is a component of this.
This qualitative study sought to explore and understand the use of asthma guidelines by primary care clinicians in two geographically bounded regions of Wales.
Multiple case study design was used. Data was collected using semi-structured interviews with a purposively sampled group of clinical staff from GP practices. Interview transcripts were thematically analysed to produce a detailed picture of practice.
Asthma care in the studied areas operated as a social network of clinicians who often used guidelines as boundary objects. Practice and local service design was influenced and dependent on regular input from local secondary care providers. Clinicians looked to British Thoracic Society and Scottish Intercollegiate Guideline Network (BTS/SIGN) 2016 guidelines. There was limited use of National Institute for Health and Care Excellence (NICE) 2017 guidelines. Barriers to guideline recommended diagnostic asthma care included: lack of acceptability, financial costs and disempowerment of nursing staff.
The findings from this study replicate and reinforce the findings of previous work. It is striking and concerning that the thematic outcomes of this study bear a strong resemblance to that which was demonstrated over a decade ago. The guideline-implementation gap in asthma diagnostics will likely persist unless there is significant restructuring, financial investment and greater empowerment of nursing staff in primary care.
The prevalence of musculoskeletal presentations in general practice: an epidemiological study
It is estimated that 28.9% (17.8 million) of the UK population live with a musculoskeletal (MSK) condition. They are a major cause of morbidity, and a significant reason for presentation to primary care.
The primary aim of this study was to determine the prevalence of MSK conditions presenting for consultation in general practice. The secondary aim was to determine specifically which MSK conditions present most frequently in general practice.
A total of 545 consultations were reviewed at an urban community general practice, which included evaluating morning consultations over a 1-week period taken from each of January, April, July and October 2018. This encompassed all morning consultations from all GPs present. The number of MSK consultations were recorded and, within that, the different presentations and their management plan.
A total of 115 of all consultations were regarding an MSK presentation yielding an overall prevalence of 21.1%. The commonest MSK presentations included the lumbosacral spine (18.3%) and the knee (17.4%). Re-presentations of original condition accounted for 73.9% of all MSK consultations. Steroid injections were administered in 33% of knee related consultations.
This study demonstrates that MSK presentations account for a large proportion of GP workload. There are no current mandatory training requirements in orthopaedics as part of the GP curriculum. Structured MSK education for GPs is important and would reduce the burden of re-presentations, particularly that of the lumbosacral spine and knee. Competency in joint injection is also a valuable skill for GPs.
A scoping review of community holistic interventions for older people with multimorbidity
In many areas, new regional community-based services have been established to provide holistic care to patients with high physical, mental and social needs. Older people represent a group with multimorbidity and high healthcare needs that may benefit from holistic care, although uncertainty remains whether such an approach is effective.
To review evidence for community holistic interventions in older people with multimorbidity.
The authors screened studies referenced by an earlier Cochrane Review and Academy of Medical Sciences report, both of which looked at interventions and populations more broadly, and their own searches of Medline, EMBASE, trial registration databases and hand-searching of journals since 2015. The authors included controlled community-based studies of holistic interventions with data for people aged at least 60 years.
Studies found (five published, two ongoing) were heterogeneous. The only significant improvement relating to physical or mental outcomes occurred in self-rated health scores, seen in two studies. One consisting entirely of diabetics showed developing a self-management plan improved self-rated health ( P = 0.023), and Mental Component Summary ( P = 0.03). The other used a multidisciplinary-team-guided personal care plan and found self-rated overall health improved ( P = 0.02). Three studies looked at service usage, only one seeing a benefit, and only in the second year.
Community-based holistic interventions for people with multimorbidity tended to focus on disease management or medication modification, and resulted in few significant benefits, almost entirely in self-rated health measures. Research into interventions focused on those with the highest needs, for example, multimorbidity with frailty; high number of comorbidities may be more likely to demonstrate meaningful benefits.
Continuing professional development for GPs in Myanmar: a pilot programme
The quality of general practice in Myanmar is currently highly variable. No formalised system of revalidation yet exists and so engagement with continuing professional development (CPD) activities and motivation to further one’s own knowledge is sporadic.
To train GPs in three key areas; 1) recording CPD activities and maintaining a portfolio logbook; 2) reflecting on learning; and 3) what a future formalised CPD credit system may involve.
Sixty-one GPs were recruited in March 2019 and given training on the above. Logbooks were issued, which were completed by the GPs while attending a simultaneous 3-month ‘GP CPD Refresher’ course, organised by the GP Society of Myanmar. The logbooks were then marked and individualised feedback given before issuing CPD accredited certificates.
All GPs agreed the pilot helped them to better understand how to maintain a CPD logbook and the importance of doing so (retention rate = 67%). All GPs also reported they would now be more likely to continue to keep a portfolio. Finally, all GPs surveyed felt a credit reward system, used as tangible evidence of CPD participation, would positively influence their future engagement with CPD.
Improving general practice is a key component in helping Myanmar develop its healthcare system; one step required is making engagement with CPD compulsory for the revalidation of clinicians. This pilot has highlighted existing inadequacies within current training of GPs, as well as the potential benefits of implementing a CPD credit reward system.
Antibiotic resistance of uropathogenic Escherichia coli and ESBL prevalence in general practice patients over 10 years
Bacterial susceptibility to antibiotics changes over time. Knowledge of the susceptibility is important for antibiotic treatment guidelines in general practices.
To determine the antibiotic-susceptibility of E. coli from uncomplicated UTI among women in general practices in the Netherlands and to compare the results with those collected in 2004 and 2009.
Urine samples were collected from women with symptoms of uncomplicated UTI, in 30 sentinel GP practices of the Nivel Primary Care database. Patient characteristics, E. coli susceptibility and ESBL prevalence were analysed.
In total, 689 samples were collected. E. coli was the most isolated uropathogen (83%). Antibiotic susceptibility was stable over time except for ciprofloxacin (96%, 97% and 94% in 2004, 2009 and 2014, respectively; P <0.05). The susceptibility to co-amoxiclav was 88%, 87% and 92% in 2004, 2009 and 2014, respectively. The prevalence of ESBL producing E. coli increased from 0.1% in 2004, to 2.2% in 2014 ( P <0.05). Susceptibility for co-trimoxazole was the highest in the West (88%) and the lowest in the North (72%, P = 0.021). Ciprofloxacin susceptibility was related to antibiotic use in the past 3 months (97% no use versus 90% use, P = 0.002) and those aged >70 years ( P = 0.005). In 2014, prescription of fosfomycin increased compared to 2009 (14.3% versus 5.6%) at the expense of co-amoxiclav, co-trimoxazole and ciprofloxacin ( P <0.05).
The antibiotic susceptibility percentages to the agents tested were stable over the 10-year period, except for ciprofloxacin as was the prevalence of ESBL producing E. coli . Surveillance with regular intervals is warranted.
Cancer treatment decisions for people living with dementia: experiences of family carers
Dementia and cancer are both diseases associated with older age. The National Cancer Data Audit in England found that 4.4% of people diagnosed with cancer also had cognitive impairment. Decisions about cancer treatment can be very complex when someone already has dementia. Often someone’s closest relative may be asked to make decisions on their behalf. Little is known about the psychosocial impact that this has on carers, or what their support needs are during this time.
To explore the experiences of family carers who have been involved in making cancer treatment decisions on behalf of a relative with dementia, in particular identifying challenges and support needs.
The authors are conducting semi-structured interviews with carers of people with dementia who have been involved in making decisions about cancer treatment on their behalf. Data is being thematically analysed using an inductive approach. Two researchers will independently verify themes.
The authors expect to have completed 14–18 interviews and will report their preliminary findings. Family carers experience many difficulties in the context of cancer and dementia, including lack of support when coping with the aftereffects of cancer treatment, lack of awareness among healthcare professionals regarding the authority granted by a lasting power of attorney and the anxiety created by feeling responsible for identifying cancer recurrence.
This study will highlight that supporting someone with dementia through cancer treatment, and having to make decisions about it on their behalf, creates unique challenges for carers. Currently there is a significant lack of support for those facing this distressing experience.
Exploring patient preference regarding interpreter use in primary care
Effective communication is considered an essential component of delivering health care. Trained, professional interpreters are the gold standard for overcoming language barriers with those with limited English proficiency (LEP). However, LEP patients often use unqualified interpreters such as family members and friends. Existing literature explores the rationale behind choosing different interpreters, but rarely from the patient perspective.
To explore the patient perspective on the type of interpreter best suited for primary care consultations.
Participants self-identified as having LEP were recruited from four GP practices in areas of Sheffield with high proportions of black and minority ethnic (BME) residents. The participants were from Urdu-, Arabic-, or Romani-speaking ethnic groups. Semi-structured interpreted interviews were recorded, transcribed, and analysed thematically with independent verification of emergent themes. Interviews continued to data saturation.
All participants expressed a preference for face-to-face interpreters. Urdu and Arabic participants highlighted the importance of using an interpreter with the same dialect; Roma participants were passionate about the need for qualified Roma interpreters. Most participants also identified trust and sex as important factors. However, interpreter preference varied between participants: some valued the continuity of family members, whereas others favoured the professionalism and linguistic accuracy associated with qualified interpreters.
This study identified conflicts between patient preferences and guidance for healthcare professionals; all of the participants disliked telephone interpreting, and many recognised the benefits of untrained interpreters. The study highlights the complexities of interpreter preference in primary care and suggests that the decision should be flexible, and patient centred.
A case study evaluation of a community multidisciplinary team in South East England using a mixed-method approach
Community multidisciplinary teams (MDTs) represent a model of integrated care comprising health, social care, and the voluntary sector where members work collaboratively to coordinate care for those patients most at risk.
The evaluation will answer the question, ‘What are the enablers and what are the restrictors to the embedding of the case study MDT into the routine practice of the health and social care teams involved in the project?’
The MDT was evaluated using a mixed-method approach with normalisation process theory as a methodological tool. Both quantitative and qualitative data were gathered through a questionnaire consisting of the NoMAD survey followed by free-form questions.
The concepts of the MDT were generally clear, and participants could see the potential benefits of the programme, though this was found to be lower in GPs. Certain professionals, particularly mental health and nursing professionals, found it difficult to integrate the MDT into normal working patterns because of a lack of resources. Participants also felt there was a lack of training for MDT working. A lack of awareness of evidence supporting the programme was shown particularly within management, GP, and nursing roles.
Specific recommendations have been made in order to improve the MDT under evaluation. These include adjustments to IT systems and meeting documentation, continued education as to the purpose of the MDT, and the engagement of GPs to enable better buy-in. Recommendations were made to focus the agenda with specialist attendance when necessary, and to expand the MDT remit, particularly in mental health and geriatrics.
Opioid crisis in primary care? An audit of high-dose opioid prescribing at Bangholm GP Practice
Opioids are effective analgesics for acute and palliative pain, but there is no evidence base for long-term pain relief. They also carry considerable risks such as overdose and dependence. Despite this, they are increasingly prescribed for chronic pain. In the UK, opioid prescribing more than doubled between 1998 and 2018.
An audit at Bangholm GP Practice to understand the scale of high-strength opioid prescribing. The aim of the audit was to find out if indications, length of prescription, discussion, and documentation at initial consultation and review process were consistent with best-practice guidelines.
A search on Scottish Therapeutics Utility for patients prescribed an average daily dose of opioid equivalent ≥50 mg morphine between 1 July 2019 and 1 October 2019, excluding methadone, cancer pain, or palliative prescriptions. The Faculty of Pain Medicine’s best-practice guidelines were used.
Demographics: 60 patients (37 females), average age 62, 28% registered with repeat opioid prescription, 38% comorbid depression. Length of prescription: average 6 years, 57% >5 years, 22% >10 years. Opioid: 52% tramadol, 23% on two opioids. Indications: back pain (42%), osteoarthritis (12%), fibromyalgia (10%). Initial consultation: 7% agreed outcomes, 35% follow-up documented. Review: 56% 4-week, 70% past year.
Opioid prescribing guidelines are not followed. The significant issues are: long-term prescriptions for chronic pain, especially back pain; new patients registering with repeat prescriptions; and no outcomes of treatment agreed, a crucial message is the goal is pain management rather than relief. Changes have been introduced at the practice: a patient information sheet, compulsory 1-month review for new patients on opioids, and in-surgery pain referrals.
Inequalities in suicide rates associated with deprivation in England from 2004 to 2019
Although addressing inequality has been a public and political priority for decades, inequalities in health, wealth, and other societal domains persist in England. In Ireland, rates of suicide are twice as high in the most deprived decile of society compared with the least deprived. Trends in the association between deprivation and suicide in England are unclear.
To describe the relationship between deprivation and suicide in England in 2019 and analyse trends in this relationship over time.
Data on rate of suicide and Index of Multiple Deprivation (IMD) for each local authority in England for 2018 and 2004 were obtained from the Office for National Statistics’ publicly available databases. The mean suicide rate for each quintile of deprivation was calculated, and means compared using ANOVA. The correlation coefficients between IMD and suicide rate were calculated for both 2004 and 2019. Steiger’s test was used to compare coefficients over time.
In 2019, the suicide rate in the least deprived quintile was 8.7 per 100 000 person-years, compared with 8.3 in 2004. This increased across each quintile to 11.1 suicides per 100 000 person-years in the most deprived quintile in 2019 (ANOVA: P <0.001), and to 11.7 in 2004 (ANOVA: P <0.001). The correlation coefficient between IMD and suicide rate in 2004 was 0.43, compared with 0.33 in 2019. Steiger’s test demonstrated no significant difference between coefficients over time ( P = 0.16).
Suicide is associated with deprivation in England. Despite significant research and policy effort, there has been no improvement in this association between 2004 and 2019.
Blood tests in general practice: the use of routine data to characterise venous blood testing in North West London, 2016–2018
Laboratory testing is an integral diagnostic tool, contributing to 70% of diagnoses in the NHS today. Its use has been steadily increasing despite estimates that ≤40% of blood tests ordered are unnecessary. Understanding blood-testing patterns is a fundamental step to tackling overuse.
To characterise the volume, type, and per patient frequency (PPF) of venous blood testing reported in general practice in North West London, 2016–2018.
Following ethics clearance, aggregate data of blood tests reported in general practice in North West London between 2016 and 2018 were extracted from the Discover database. Non-venous blood test codes and codes not used within the designated time period were excluded. Codes reporting the same analyte were aggregated. Overall volume and PPF were calculated per analyte.
Three hundred and thirty-six individual analytes were reported and grouped into 35 recognised panels or groupings. Blood testing increased by 16.5% over the 3-year period. Full blood count, urea and electrolytes, liver function tests, and lipid profile accounted for 80.4% of all venous blood tests. Requests for HbA1c increased by 52.8% and non-HDL cholesterol by 148.7%, whereas glucose decreased by 13.3% and urea by 15.7%. The PPF remained unchanged over the 3-year period at 1.29 blood tests per person per year. The coagulation assay had the highest PPF at 3.0.
Routine general practice data revealed important trends in blood testing. Trends uncovered can inform innovative and targeted solutions to reduce unnecessary blood testing.
Management of gout and adherence to current guidelines in general practice surgery
Gout is one of the most common inflammatory joint diseases in the UK managed by GPs. The recent (2017) guideline of the British Society for Rheumatology (BSR) changed the recommendation for urate-lowering therapy (ULT) and now advises it after the first episode of gout, whereas it previously recommended after the second one. Moreover, the BSR now also recommends screening and management of risk factors of gout.
To audit contemporary management of gout and adherence to the new BSR guideline in a large GP practice.
The audit identified all patients diagnosed with gout between 1 July 2017 and 1 May 2019. Pharmacological gout management, lifestyle advice, and management of risk factors were assessed, including body mass index (BMI), systemic blood pressure (BP), and HbA1c.
The audit included 104 patients, 26.9% female, mean age 63.8 years at the age of diagnosis. Uric acid was raised in all patients (mean 469 um/L). Most patients (68%) had abnormal BMI (mean 30.4), whereas BP, cholesterol, and HbA1C were normal in the majority of patients (in 78%, 75%, and 90%, respectively); however, all of these parameters were normal in just 17% of patients. Lifestyle advice was given to 46 (44.2%) patients while allopurinol was prescribed, and overall in 21 (20.2%) patients. More patients were managed with colchicine (40.2%) and naproxen (56.7%).
Most patients diagnosed with a first gout attack have risk factors of gout and require their management. Overall, allopurinol is prescribed in a fifth of patients, which may be related to patients’ preferences, strict adherence to lifestyle modification only, or presence of contraindications to allopurinol. This requires, however, further assessment.
Evaluation of a novel anxiety and trauma intervention at the Edinburgh Fringe
Anxiety and psychological trauma are common presentations in general practice and may lead to long-term prescribing and/or time-consuming talking therapies.
To assess the efficacy and acceptability of short ‘Gazetherapy’ interventions.
‘The Anxiety Experiment’ was delivered as a show at the Edinburgh Fringe Festival from 1–25 August 2019. Gazetherapy interventions were explained using props to describe polyvagal theory and cranial nerve and cerebellar/hippocampus anatomy and function. BabyGaze (reducing anxiety in the moment), da Vinci Gaze (attenuating stress), and Accessory Gaze (resolving simple trauma) were delivered to audiences of between six and 51 people during <10 minutes of the 50-minute presentation. Subjects were given a card bearing a QR code to link to an online survey containing validated short screening questionnaires: GAD-2 for probable anxiety disorder and PC-PTSD for probable post-traumatic stress disorder (PTSD).
Efficacy: 73 (9.8%) attendees completed the survey, of whom 39% screened positive for anxiety and 26% screened positive for PTSD. Those screening negative in both tests (52%) were designated a control group, with 36% of them feeling better after the presentation. Fifty-nine per cent of probable anxiety ‘cases’ and 68% of probable PTSD cases felt better after the presentation; none felt worse. Acceptability: 95% reported a ‘definite’ or ‘probable’ intent to use the techniques in the future, with 5% (all non-cases) stating that they probably would not. No responder said they would definitely not use the techniques.
The acceptability and effectiveness of a new therapeutic approach were demonstrated by presenting them in a show at the Edinburgh Fringe.
Appropriate secondary prevention of stroke and transient ischaemic attack with antithrombotics: an audit in general practice
Stroke is a major cause of death and disability worldwide. Major advances have occurred in secondary prevention of stroke/transient ischaemic attack (TIA) during the past three decades. Primary care is a critical point of contact with patients in the implementation of secondary prevention, with the majority of patients with past stroke/TIA being managed in the community.
To assess current practice at the New Queen Street and Stanground Surgeries, Peterborough, in reference to the National Institute for Health and Care Excellence guidelines on secondary prevention of stroke/TIA.
An audit at the above practices was undertaken by searching the SystmOne computer system for adult patients with previous stroke/TIA (311), excluding those with haemorrhagic stroke and those on aspirin. The patient records of the remaining group (37) were investigated to find whether they were on appropriate antithrombotic therapy and, if not, why.
Of post-stroke/TIA patients, 234/236 were receiving antithrombotic therapy unless contraindicated. For those not on antithrombotics, risk of bleeding was the reason given in 10/13 of cases, though many of these patients did not have active bleeding (exact number unclear due to poor documentation). In 2/13 cases there was no documented reason given and informed dissent in one of the 13 cases.
It was found that both practices implemented the guidelines to a satisfactory degree. However, to further improve secondary prevention outreach, bleeding risk should be assessed using a tool such as S2TOP-BLEED before withholding antithrombotic therapy, as, on balance, antithrombotic therapy may still be preferable. In addition, accurate and detailed documentation of the indications/contraindications to anticoagulation is paramount for such assessment.
A pilot project on the management of osteoporosis in primary care: results of the audit cycle
Osteoporosis is a major public health problem with the ageing population in the UK. However, there is no known national algorithm for the management of osteoporosis in primary care. Therefore, a treatment pathway was developed in secondary care for patients in the community.
This audit cycle investigates whether patients at a GP practice with a population of 14 000 have been appropriately identified, coded as osteoporosis, treated, and have followed the recommended pathway.
A search of the practice clinical system was undertaken for three groups of patients coded as: patients currently on the existing osteoporosis register; patients with a code of ‘osteoporosis’ or ‘fragility fracture’ but not prescribed an osteoporosis treatment; and patients currently prescribed an osteoporosis treatment with no coding for ‘osteoporosis’ or ‘fragility fracture’. The words ‘osteoporosis’, ‘fragility fracture’, ‘QOF’, and all individual drug names were used in the search engine.
The completed audit cycle shows an increase in the proportion of patients following the local guidelines pathway, from 75% in 2018 to 81% in 2019, emphasising the importance of having a guideline for GPs to follow in order to optimise treatment and prevent future fragility fractures.
This is a pilot project to assess the ability to identify patients who have osteoporosis and review their treatment pathway. The results are promising as the analysed data indicate that GP practice lists can be used to identify and treat high-risk patients for osteoporosis and assess the adherence to the pathway. Using the pathway, GPs can more efficiently diagnose and manage patients.
Should diverticulitis be managed in primary care? An audit on the management of diverticulitis in primary care.
The prevalence of diverticulosis and acute diverticulitis is increasing in developed countries. For those with diverticulosis the lifetime risk of developing acute diverticulitis is about 4–25%. Mild, uncomplicated diverticulitis can be, and often is, managed safely in a primary care setting, avoiding unnecessary admission.
To evaluate management of suspected diverticulitis in primary care against standards set by the National Institute for Health and Care Excellence (NICE) and review admission rates following primary care management.
An electronic search on EMIS Web using Read codes ‘diverticulitis’, ‘diverticulosis’, and ‘diverticular disease’, with a specified period of 2017–2019. All consultations with suggestions of an infective flare of diverticular disease were included in the study. Clinical data from the consultations were extracted and retrospectively audited.
A total of 64 patients were identified with diverticular disease or diverticulosis. Of those, 42% ( n = 27) presented to primary care with presenting complaints suspicious of diverticulitis. A total of 64 consultations were reviewed, as several patients presented more than once in the study period. Of the consultations reviewed, 12.5% ( n = 8) resulted in referral to the surgical assessment unit. Antibiotics were prescribed after 68.4% ( n = 39) of consultations. Bloods for inflammatory markers were performed after 19.3% ( n = 11) of consultations. Only 3.5% ( n = 2) of patients were reviewed within the recommended 48-hour timeframe. Only 3.5% ( n = 2) of patients subsequently deteriorated and required admission.
The management of diverticulitis in this primary care centre is not fully concordant with NICE guidelines. There is a need to improve adherence, in particular antibiotic regimen when deciding to prescribe antibiotics.
Multiple risk behaviour intervention to prevent depression in primary care
Primary care is the ideal setting for promotion and prevention intervention. Multiple risk behaviour interventions present several advantages over single-risk lifestyle interventions. Multiple risk behaviour interventions could be easily implemented in primary care to prevent non-communicable disease and depression.
To test the effectiveness of a multiple risk behaviour intervention to promote Mediterranean diet, physical activity, and/or smoking cessation in people attending Spanish primary health care with incidence of depression and symptoms of depression.
This was a secondary analysis of the EIRA study that aims to test the effectiveness of a multiple risk behaviour intervention to promote healthy lifestyles. Twenty-six primary care centres were randomised to receive multiple risk behaviour intervention or usual care. The multiple risk behaviour intervention included individual sessions, group sessions, communitarian activities, and SMS reception. Participants were followed for 10–14 months. The primary outcomes of this study were incidence of depression and reductions of depressive symptoms.
Three thousand and sixty-seven participants were included. Females accounted for 45.13% and 93.88% were Spanish. Age varied between 45 and 75 years old. The effectiveness of the intervention will be calculated using the Patient Health Questionnaire (PHQ-9) and the Composite International Diagnostic Interview (CIDI) depression section. Linear and logistic regression will be used to create predictive models.
Primary care is the most accessible service in the health system for patients. Hence primary care is the ideal setting for health education, promotion, and prevention interventions. This study will provide high-quality evidence about the effectiveness of multiple risk behaviour interventions over depression prevention.
Association between screen-time and school performance of secondary school children in Karachi, Pakistan
Electronic media are playing a negative role in people’s lives and yet people are unaware of the hazardous effect.
To show that screen-time of >1 hour had detrimental associations with school performance.
A population-based, cross-sectional survey of 363 students, mean age 14.2 years (grades 5–8), from both government and private-sector schools in Karachi was conducted. A total of 363 students (210 males [57.9%] and 153 females [42.1%]) were included in the study. Of these students, 193 (53.2%) belonged to government schools and 173 (46.8%) to private schools. A questionnaire form was filled in. Weekday, weekend television, and video game screen-time was looked at. The main outcome was self-report of school performance (grades A, B, and C). Ordinal logistic regression analysis was used to test the independent effects of each variable, adjusting for demographics, child personality, and parenting style.
Television content measurement showed that 69 (19%) students watched sports channels regularly while 30 (8.3%) and 3 (0.8%) watched educational and action programmes, respectively. The viewers of entertainment TV programmes (268 [73.8%]) and news programmes (159 [43.8%]) were in the majority. In terms of school grades, 154 students (42.4%) attained grade A, 180 students (49.6%) scored grade B, and 29 (8%) obtained grade C. Data showed no association between increased screen-time of ≤1 hour (weekdays as well as weekends) with poor school performance ( P =0.46 and P =0.58, respectively).
Screen-time of ≤1 hour does not have any detrimental associations with poor school performance.
Revolutionising participants’ health and wellbeing through neuro-reprogramming via the Slimpod ® app: a randomised controlled trial
Obesity is a global pandemic that threatens the health of the population and the sustainability of publicly funded health care. This randomised controlled trial addresses the gap in the literature surrounding unconscious persuasion and its use in weight loss and weight management. The Slimpod ® tool is unlike any of those currently available on the market. Using breakthrough research in ‘nudge’ thinking, it is designed to retrain an adult’s habitual and emotional response to foodstuffs. This therapeutic model allows unconscious thought to be shaped into a manner more consistent with a healthy lifestyle. Candidates can then take control of their eating behaviours to induce a holistic state of wellbeing.
To assess the effectiveness of an audio unconscious-persuasion weight loss/weight management intervention (Slimpod ® ) compared with audio relaxation (control).
Eighty-two overweight adults were randomised to intervention ( n = 41) and control groups ( n = 41). Weight was assessed at trial commencement, mid-trial (12 weeks), and trial end (24 weeks). Secondary outcomes were assessed using the Eating Self-Efficacy Scale (ESES), Exercise Confidence Scale (ECS), and Quality of Life Index Generic Version III (QLI-G3) at the start and end of the trial.
Reports found a statistically significant difference in mean weight loss between intervention group (1.7 kg at 12 weeks and 4.3 kg at 24 weeks) versus control (0.6 kg and 1.2 kg respectively) at P <0.001. ESES scores showed greater self-efficacy ( P = 0.008) in intervention at 24 weeks. No significant differences in ESES negative affect sub-scale score or ECS were observed.
Slimpod ® was effective at reducing weight and increasing eating self-efficacy in overweight adults.
Evaluating the relational continuity of care of four GP practices, one of which uses personalised lists
Continuity of care is a fading type of care because GPs are working more flexibly and at reduced working hours. The GP Contract gave a financial incentive to provide prompt GP appointments, but to the detriment of continuity of care. Increased patient demand for appointments has seemingly led to patients favouring ‘any’ appointment with a GP rather than ‘an appointment with the same GP’. Continuity of care in general practice is associated with greater patient satisfaction and is the preferred type of care for patients with chronic disease or psychological problems. In the Northeast of England there is a multi-partner GP practice that operates a true personalised list system. Other GP practices in the area do offer a degree of continuity of care, but this has not been measured.
To measure and compare the relational continuity of care index of four matched GP practices, one of which operates a personalised list.
A written protocol enabled the authors to extract comparable anonymised data from four GP practices over a year (January to December 2019). Two standardised indexes of continuity of care (UPC and SLICC) were calculated and compared.
Continuity of care was consistently higher with personalised lists. UPC index results show that all GP practices provide surprisingly high continuity of care, albeit not with patients’ assigned GPs. Higher monthly UPC scores versus overall scores indicate patients are receiving continuity of care in relation to their condition.
Continuity of care is still observed in GP practices that do not have personalised lists.
Decision making on clinical care choices including end-of-life decision making for older adults in an acute care setting
The Scottish Government’s vision for older people is that ‘Older people are valued as an asset; their voices are heard and they are supported to enjoy full and positive lives.’ In the health and social care setting in Scotland it is increasingly recognised that there is a need for careful planning of care for older patients with complex comorbidities, and that this should involve the patient where possible via a process of shared decision making (SDM).
To establish what future planning for healthcare decision making and end-of-life care was undertaken in the care of the older patients in a secondary care facility, and how much they participate in this process.
An audit was conducted across four wards in the care of the older patient setting in a hospital for older patients in Scotland. Over a 2-week period, all patients’ charts ( n = 82) were reviewed, and evidence was examined on whether the following documents were in place: a do not resuscitate order; an escalation of medical care plan; and an assessment of capacity/incapacity.
The majority of patients (55%) had a resuscitation plan in place. An Incapacity Statement was also in place for the majority of patients who required it (90%). The escalation of medical care plan was only completed for a minority of patients, mainly those on the palliative care ward.
Plans for decision making around resuscitation were reasonably well developed. However, planning for other, more complex, future medical care needs was less well defined or explored with older patients.

Guidelines for Oral and Poster Presentations
Guidelines for oral and poster presentations.
Oral presentations
Please follow the guidelines below when preparing your oral presentation.
- You should use the same title submitted with your abstract.
- Provide appropriate context to ensure an international audience can follow your paper content.
- You should provide content that clearly addresses the theme of the session in which you are participating.
- You must allow time for questions within your assigned time slot so please take note of papers duration below.
- You should provide 1-2 key take home messages on the final slide.
- The language of the congress is English.
Duration of oral presentation
Each 90 minute session will include up to 5 paper presentations. Each presentation should be no longer than 14-15 minutes to ensure that there is sufficient time for Q&A. Please be mindful of time when preparing your paper as session Chairs will stick rigorously to time.
Preparation of oral presentation
- We strongly recommend that slides are prepared in PowerPoint. Other software packages are acceptable as long as the presentation is in PDF and complies with the widescreen (16:9) format.
- There is no requirement to submit your presentation ahead of time. All presentations must be brought to the symposium venue on a USB-key.
- Presenters may not use their own laptops for presenting – however you may bring a tablet / iPad onstage with you and read from it if needed.
Scientific posters
- Include an abstract on your poster to ensure viewers can follow it.
- Demonstrate how your poster clearly addresses the congress or session themes.
Display of your poster
- Posters are exhibited in DCU our Congress Venue and will be available for informal browsing. In addition, there will be poster sessions scheduled within the Congress for individual discussion with the authors throughout the conference. Posters will also be hosted digitally on an app / online programme.
- Specific poster requirements will be communicated in Spring 2024.
Congress Secretariat
35 th International Geographical Congress – Dublin 2024 c/o Keynote PCO, Suite 26, Anglesea House, 63 Carysfort Ave., Blackrock, Co Dublin, A94 FF63, Ireland T: + 353 1 400 3626 E: [email protected]
Useful Links
Privacy & Cookie Policy
Congress Organisers

This site uses cookies. By continuing to browse the site, you are agreeing to our use of cookies.
Cookie and Privacy Settings
We may request cookies to be set on your device. We use cookies to let us know when you visit our websites, how you interact with us, to enrich your user experience, and to customize your relationship with our website.
Click on the different category headings to find out more. You can also change some of your preferences. Note that blocking some types of cookies may impact your experience on our websites and the services we are able to offer.
These cookies are strictly necessary to provide you with services available through our website and to use some of its features.
Because these cookies are strictly necessary to deliver the website, refuseing them will have impact how our site functions. You always can block or delete cookies by changing your browser settings and force blocking all cookies on this website. But this will always prompt you to accept/refuse cookies when revisiting our site.
We fully respect if you want to refuse cookies but to avoid asking you again and again kindly allow us to store a cookie for that. You are free to opt out any time or opt in for other cookies to get a better experience. If you refuse cookies we will remove all set cookies in our domain.
We provide you with a list of stored cookies on your computer in our domain so you can check what we stored. Due to security reasons we are not able to show or modify cookies from other domains. You can check these in your browser security settings.
We also use different external services like Google Webfonts, Google Maps, and external Video providers. Since these providers may collect personal data like your IP address we allow you to block them here. Please be aware that this might heavily reduce the functionality and appearance of our site. Changes will take effect once you reload the page.
Google Webfont Settings:
Google Map Settings:
Google reCaptcha Settings:
Vimeo and Youtube video embeds:
- CROI 2024 Important Dates and Deadlines
- CROI Foundation
- Scientific Program Committee
- Policies, Website, and Copyrights
- Funding and Grant Support
- Illustrations of HIV, HCV, and SARS-CoV-2 Viruses
- Abstract Guidelines and Submission
- CROI 2024 Abstract Categories
- People-First Language and the Use of Appropriate Terminology
- Frequently Asked Questions
- Invited Presenters
- Themed Discussion Guidelines
Oral Abstract Presentation Guidelines
- Letter Of Invitation (For Visa And Other Purposes)
- Who Can Attend
- Media Accreditation and Registration
- CROI 2024 List of Hotels
- Affiliated and Proximate Activities
- New Investigator Scholarship
- International Investigator Scholarship
- Community Educator and Mentor Scholarships
- CROI 2024 Program
- CROI 2024 Resources
- Continuing Medical Education (CME)
- Resources From Prior Years
- Abstracts and ePoster Archive
- CROI Issues of TAM TM
Oral Abstract Sessions include leading-edge research in HIV, hepatitis viruses, SARS-CoV-2, mpox , and their related conditions. During these 2 -hour sessions, speakers present their research . The Oral Abstract Sessions are divided into two 1-hour segments, as described below. 2 combined question-and-answer sessions are held and moderated by experts in the field. Moderators introduce p resenters and facilitate audience discussion during the live question-and-answer periods.
See Also: Important Dates | Abstract Submission | Themed Discussion Guidelines | Poster Presentation Guidelines | Registration | Embargo Policy | FAQs
CROI Slide Template: Download the optional slide template here .
Title Slide: A title slide prepopulated with your name, institution, and financial disclosures will be provided when you submit your final slides in the Speaker Ready Room at CROI.
Note: The CROI presentation software can only accept PowerPoint slides (eg no Keynote or other slide programs).
GENERAL INFORMATION FOR ORAL PRESENTERS AND MODERATORS
Presentation development and slide submission .
- Presentation Length: In general, Oral abstract presenters are asked to prepare an 8-minute presentation. An optimal 8-minute presentation has 8 content slides not including the 1 title slide provided. The session moderators will cut off presentations longer than 8 minutes.
- Presentation Contents: Refer to the Guidelines for Presentation Development below for slide format and details on content to be included or excluded in presentations
- Final Slide Submission: The final version of the presentation slides must be submitted in the Speaker Ready Room at CROI (refer to the conference program for location) 24 hours before the start of the session . The presentation you upload in the Speaker Ready Room will be projected in the session room from a central location, not from a laptop at the podium. Bring your notes with you, as there is no notes preview at the podium for your presentation.
Check-In on Session Day
Presenters and moderators should check in at the front of the session room (near the podium) 10 minutes before the start of the session. The first group of presenters will then be seated on the stage. Following the first segment, the second group will be seated on the stage.
Session Flow
Oral sessions generally have 8 presentations, sometimes 9. Many attendees move from session to session; THEREFORE, IT IS ESSENTIAL THAT EACH PRESENTATION IS KEPT TO TIME. Before the session begins, Presenter Group 1 and the Oral Session Moderators take the stage. Regardless of the number of presentations, sessions will follow the same general flow:
1. Oral Session Moderators: Welcome and introduce Presenter Group 1 (5 minutes). Oral moderators introduce each speaker before their presentation.
2. Presenter Group 1
- Presenter 1 (8-minute presentation, no Q&A)
- Presenter 2 (8-minute presentation, no Q&A)
- Presenter 3 (8-minute presentation, no Q&A)
- Presenter 4 (8-minute presentation, no Q&A)
3. Group Q&A 1: Audience Questions and Answers for Presenter Group 1. Priority will be given to questions from the microphone in the sessions, with an option to submit questions electronically.
4. Transition: Presenter Group 1 leaves the stage, and Presenter Group 2 joins the stage
5. Oral Session Moderators: Introduce Presenter Group 2 (5 minutes). Oral moderators introduce each speaker before their presentation.
6. Presenter Group 2:
- Presenter 5 (8-minute presentation, no Q&A)
- Presenter 6 (8-minute presentation, no Q&A)
- Presenter 7 (8-minute presentation, no Q&A)
- Presenter 8 (8-minute presentation, no Q&A)
7. Group Q&A 2: Audience Questions and Answers for Presenter Group 2 , moderated by the Oral Session Moderators. If time remains (and at the discretion of the moderators), additional questions may be posed to Presenter Group 1
8. Oral Session Moderators: Wrap up the session with thanks to the audience and presenters
GUIDELINES FOR PRESENTATION DEVELOPMENT
Slide format .
- Slide Template: You are welcome to use the CROI Slide Template (optional) for a professional look that is consistent with the CROI branding
- Title Slide: A prepopulated title slide is provided for you. See above.
- Format: When preparing your presentation, note that high-definition (HD) projectors will be used for all CROI sessions. Please apply widescreen formatting when preparing your slides (aspect ratio 16:9; resolution 1920 x 1080)
- Font Size: For content slides, it is generally recommended to have a font size of 26 to 32 (based on Arial font) for text. This provides for around 7 lines of text, including a header. Details should be visible from the back of a large ballroom (avoid overly detailed figures or large blocks of text)
- Embedded Videos: Please test any embedded videos in the Speaker Ready room prior presentation.
Trade Names
Trade names for drugs should not be used in presentations. Refer to drugs and products by their nonproprietary names.
Acknowledgments of Support and Contributors
Acknowledgments of support may be included in the oral presentation of the abstract at CROI.
Sex Stratification and Other Demographic Variables
Presentations from randomized trials and cohorts should follow the ICMJE guidelines, including reporting of study designs (eg, prospective, observational, randomized, double-blind, STROBE, CONSORT, or others), statistical methods, and outcomes by demographic variables. For human clinical or epidemiologic studies, the presentation should provide sex-stratified results or identify who was included if it includes only a single population. Presentations of preclinical data including the use of cell lines and animal studies should include the sex of the animals or the sex of the source of the cell lines. If data are not available on sex (as assigned at birth) or gender (where gender is relevant to the study results), this should be identified as a limitation in the study.
See: ICMJE Preparing for Submission
Use of People-First Language and Appropriate Terminology
See: Appropriate Terminology
Presentations Describing New Compounds
Please be sure to include information sufficient to allow for meaningful review of compound data; this can include isolation, activity, chemical structure, mechanism of action, toxic effects, and pharmacologic data. The chemical or molecular structure must be shown in the presentation (it need not be part of the abstract or be published in the Abstract eBook).
PUBLICATION OR PRESENTATION PRIOR TO CROI
If study data are accepted for publication or presentation after the abstract submission to CROI, and that publication or presentation is expected to take place before CROI, the presenting author must contact CROI at [email protected] to provide details as soon as the presentation is accepted for review, presentation, or publication in another venue or outlet. Please be aware that although publication in these circumstances will not necessarily prevent presentation of the research at CROI, our strong preference is that any additional publication or presentation happen either simultaneous to or following presentation at CROI. Requests to publish or present research accepted for presentation at CROI prior to its presentation at CROI will be evaluated on a case-by-case basis. Failure to notify the conference promptly regarding plans to publish or present a CROI-accepted abstract prior to CROI may result in the removal of the study from the conference program.
- ASH Foundation
- Log in or create an account
- Publications
- Diversity Equity and Inclusion
- Global Initiatives
- American Society of Hematology
- ASH Annual Meeting & Exposition
- Schedule and Program
Oral and Poster Sessions
- Agenda for Nematology Research
- Precision Medicine
- Genome Editing and Gene Therapy
- Immunologic Treatment
- Research Support and Funding
The following information is preliminary and subject to change. All times are listed in Pacific time.
Abstracts selected for oral and poster presentations represent important, novel research in the field of hematology and are considered the best of thousands submitted for the ASH annual meeting. now available online and in the ASH annual meeting app .

See the schedule at-a-glance for specific session dates and times.
Simultaneous Oral Abstract Sessions
These sessions feature 15-minute presentations of high-scoring abstracts. Sessions on related topics are scheduled near one another to make it easy to move between rooms and hear individual presentations of interest. Both in-person and virtual attendees will be able to watch the oral abstract sessions as they are presented live.
Poster Sessions
Poster presenters will display a physical copy of their poster in the poster hall on either Saturday, Sunday, or Monday during the ASH annual meeting. Posters will also be made available on the virtual event platform both in the form of a short Power Point presentation with accompanying audio narration and as a static image. Poster presenters will be available in-person to answer questions and discuss their research during designated presentation times. There will also be a “Contact the Author” button on each poster presentation page on the virtual event platform to submit questions to the authors directly.
audio presentations of annual meeting posters
Download the free PosterCast app to stream audio explanations of posters as you view them. While you are in the poster hall, simply scan the QR code on a participating poster or use the keypad to enter the poster number. This resource is particularly valuable when posters are unattended by presenters.
Download for iOS | Download for Android

Oral Presentations
Talks are limited to 15 minutes, with 5 minutes for questions.
Slides should be submitted to the conference organizers by 5PM on Friday, April 19th.
Presenters will have an opportunity to test their slides during the check-in period (8AM - 9AM).
Poster Presentations
Posters should be no larger than 48 inches tall and 60 inches wide.
Posters should be set up during the registration period (8AM - 9AM) and will remain up all day.
2024 Presentation Guidelines
(scroll down for poster guidelines)
For Oral Presentations
Authors making oral presentations must submit a full paper to the ICSD organizers by August 1, 2023, or risk losing their presentation slot. We will begin accepting full papers on June 1, 2024, via an Oral Presentations Airtable Form. Full papers will be reviewed by the Scientific Committee and used to inform the presentation order. It is optional to also have your paper published as a conference proceeding (not peer-reviewed); check the box to opt-out as you prefer.
Papers must meet the following guidelines:
- Papers cannot be longer than 9 pages including figures and tables, excluding bibliographies.
- The top of the page should include the paper title, a list of all the authors and their affiliations (Ex. John Doe, Professor, University of Illinois), and full contact details for the corresponding author (email, phone number, and mailing address).
- Text should be in 11 point Arial font and single-spaced.
- Citations should follow the Chicago Manual of Style and use footnotes.
- A template of a full paper format is available to download.
**Important: We encourage you to incorporate feedback you receive at the event into your paper. You will have the opportunity to submit an updated manuscript after the event.**
To submit your paper, please login to your Google Workspace account. Please respond to the required questions in the Google Form and upload your paper, selecting if you wish to have your paper published in the conference proceedings. You will have a chance to update your title and authors if necessary. Please note, once you’ve completed your submission, you cannot go back and edit it . You may email us if there are corrections needed. If you have any questions, please write to [email protected] .
All oral presenters will present virtually. Each will be given 10 minutes to present their work and an additional 5 minutes for Q&A, for a total of 15 minutes. Presenters will be able to share their screens for a slide presentation, but this is not required. Presentations will be done on Zoom Webinar. Almost all presentation software is compatible with Zoom, however videos are not recommended as the quality will be poor and there may be technical difficulties with sound. You will have to share your own screen and advance your own slides. More guidance on how presenters will connect through Zoom will be provided in August. The full program will be announced by mid-August, and we will do our utmost to accommodate presenters’ time zones.
For Poster Presentations
Authors making poster presentations must submit their posters to the ICSD organizers by August 1, 2024, or risk losing their presentation slot. We will begin accepting posters on June 1, 2024, via a Poster Presentations Airtable Form .
This year’s posters will be displayed in our online virtual event poster gallery on this ICSD conference website. Once the event is live, all posters will be available to view.
To submit your poster, please login to your Google Workspace account. Please respond to the required questions in the Google Form and upload your poster. You will have a chance to update your title and authors if necessary. Please note, once you’ve completed your submission, you cannot go back and edit it . You may email us if there are corrections needed. If you have any questions, please write to [email protected] .
Poster presentations must meet the following guidelines:
- All posters must be uploaded as a one page PDF.
- Poster presentations cannot be larger than 5MB.
- A presentation sample/template is available for download should you require assistance. You are not required to use this layout (but you are required to keep it to one page ).
- While participants will be able to zoom in or out on your poster, we suggest using at minimum Arial 17 point font for readability.
- There are no required dimensions for the posters, just the 5MB file size restriction.
Should you have any additional questions, please visit our FAQ or email us at [email protected] .
University to Celebrate Student Scholarship April 24

The University of Scranton will hold the 24th Annual Celebration of Student Scholars during the afternoon of Wednesday, April 24 in the Loyola Science Center.
Over 120 students are expected to present more than 90 displays, showcasing their outstanding and unique scholarly work. Under the guidance of faculty mentors, undergraduate and graduate students have worked throughout the year, and in some instances longer, to produce the high-quality scholarly endeavors that will be on display.
The showcase of work will include poster presentations, demonstrations, and oral presentations. Posters will be on display from 12 p.m. to 3 p.m. and the schedule of oral presentations will be announced in the coming days.
Everyone from the University community, as well as family members, alumni, and the general public are invited to walk through, learn more about the students’ research, and celebrate our outstanding student scholars.
The Celebration of Student Scholars is coordinated by The Office of Research Support and Sponsored Programs. For more information, please contact Brooke Leonard at 570.941.7653.

- Today's news
- Reviews and deals
- Climate change
- 2024 election
- Fall allergies
- Health news
- Mental health
- Sexual health
- Family health
- So mini ways
- Unapologetically
- Buying guides
Entertainment
- How to Watch
- My Portfolio
- Stock Market
- Biden Economy
- Stocks: Most Actives
- Stocks: Gainers
- Stocks: Losers
- Trending Tickers
- World Indices
- US Treasury Bonds
- Top Mutual Funds
- Highest Open Interest
- Highest Implied Volatility
- Stock Comparison
- Advanced Charts
- Currency Converter
- Basic Materials
- Communication Services
- Consumer Cyclical
- Consumer Defensive
- Financial Services
- Industrials
- Real Estate
- Mutual Funds
- Credit Cards
- Balance transfer cards
- Cash-back cards
- Rewards cards
- Travel cards
- Personal Loans
- Student Loans
- Car Insurance
- Options 101
- Good Buy or Goodbye
- Options Pit
- Yahoo Finance Invest
- Fantasy football
- Pro Pick 'Em
- College Pick 'Em
- Fantasy baseball
- Fantasy hockey
- Fantasy basketball
- Download the app
- Daily fantasy
- Scores and schedules
- GameChannel
- World Baseball Classic
- Premier League
- CONCACAF League
- Champions League
- Motorsports
- Horse racing
- Newsletters
New on Yahoo
- Privacy Dashboard
Yahoo Finance
Biohaven showcases innovative neuroscience portfolio with 20 presentations at the 2024 american academy of neurology (aan) annual meeting and provides other business updates.
Biohaven's first-in-class Molecular Degrader of Extracellular Proteins (MoDE™) technology targeting IgG removal, BHV-1300, was selected for an oral presentation at AAN highlighting its novel mechanism of action and the latest preclinical data demonstrating rapid, robust, and selective target removal
Biohaven announces it will present safety and IgG lowering data from its ongoing single ascending dose (SAD) study of BHV-1300 at the company's annual R&D day at the Yale Innovation Summit in New Haven, Connecticut on May 29, 2024
Safety, tolerability, and target engagement data showing the differentiated profile of BHV-7000 as a potential best-in-class Kv7 activator will be presented as both oral and poster presentations; the Phase 2/3 focal epilepsy program is now enrolling patients
AAN Abstract of Distinction awarded to BHV-2100, which demonstrated potent reversal of pain in preclinical models and favorable initial safety and pharmacokinetic data in Phase 1 studies, highlighting the potential for TRPM3 antagonism as a novel nonopioid target to treat pain and migraine
Oral and poster presentations of troriluzole as a novel glutamate modulating agent with favorable pharmacokinetics, safety, and outcomes data in the potential treatment of neurologic and neuropsychiatric disorders
Biohaven announces the Data Monitoring Committee for its Phase 3 trial in obsessive-compulsive disorder convened in the second quarter to review the interim analysis and informed the Company that the study may continue
Additional efficacy and safety data regarding troriluzole in spinocerebellar ataxia will also be presented in both oral and poster format
Poster presentation of RESILIENT Phase 3 study design with taldefgrobep alfa in spinal muscular atrophy; study completed enrollment and topline results anticipated in the second half of 2024
Biohaven announces the FDA granted "rare pediatric disease" designation for taldefgrobep alfa thereby providing the potential to receive a priority review voucher (PRV) if ultimately approved for the indication of spinal muscular atrophy
Other presentations and posters include development of the PARCOMS, a new outcome measure for Parkinson's disease clinical trials, application of machine learning in video assessment of gait, and data demonstrating a reduced risk for Parkinson's disease in patients taking anti-inflammatory agents
Three oral presentations and 6 poster presentations from the Biohaven Clinical and Health Outcomes group describe the development and validation of novel scales and natural history studies in support of troriluzole and BHV-8000 development programs, the impact of immune-modulating therapy in Parkinson's disease, the burden of illness in focal epilepsy and KCNQ2-DEE (BHV-7000), and the application of AI machine learning technology to quantify patient mobility with troriluzole in spinocerebellar ataxia
DENVER, CO and NEW HAVEN, Conn. , April 13, 2024 /PRNewswire/ -- Biohaven Ltd. (NYSE: BHVN) announced today that 20 abstracts, including 8 oral presentations and 12 posters, will be featured this weekend starting April 13 th at the 2024 American Academy of Neurology (AAN) Annual Meeting, taking place in Denver, Colorado . The presentations highlight Biohaven's leadership in neuroscience and extensive development programs evaluating novel therapies to treat neurological diseases, with abstracts covering programs that include Kv7 ion channel modulation, molecular degraders of extracellular protein (MoDEs), TRPM3 antagonism, TYK2/JAK1 inhibition, glutamate modulation, and myostatin inhibition.
Irfan Qureshi , M.D., Chief Medical Officer of Biohaven, commented, "The research being presented at the AAN Annual Meeting emphasizes Biohaven's commitment to developing new therapeutic options across a range of neurological diseases. By targeting novel mechanisms of action, differentiated from currently available treatments and other therapies in development, and following innovative science, Biohaven continues to strive for better treatments for people living with neurological disorders. We are particularly honored that the AAN Science Committee selected our BHV-2100 (TRPM3) abstract as an AAN Abstract of Distinction, recognizing it as the top abstract in the pain category. Following the completion of Phase 1 studies in the first half of 2024, we look forward to initiating a Phase 2 study with BHV-2100 in migraine in the second half of the year and are excited by the potential for this novel nonopioid approach to treat pain."
Vlad Coric M.D ., Chief Executive Officer and Chairman of Biohaven, added, "Our leadership in neuroscience research is on full display at the AAN Annual Meeting with the breadth and depth of clinical, epidemiological, and preclinical programs highlighted in our scientific presentations. Central nervous system (CNS) disorders continue to represent one of the highest unmet medical needs facing our society and we must act urgently to bring better treatments to patients and improve clinical outcomes. We believe that the next generation of therapies for CNS disorders will include MoDEs for autoimmune disorders, ion channel modulation for epilepsy, migraine and other pain disorders, immune modulation for neurodegenerative disorders including Parkinson's and Alzheimer's diseases, myostatin targeting drugs for neuromuscular disorders and glutamate modulating agents for neuropsychiatric disorders. I am so proud of the team at Biohaven who are working tirelessly to alleviate the burden of these devastating disorders."
The complete list of Biohaven's accepted abstract titles is below. Full abstracts can be viewed online at https://index.mirasmart.com/AAN2024/ .
Oral Presentations:
Novel Bispecific Degrader BHV-1300 Achieves Rapid, Robust, and Selective IgG Reduction in Preclinical Models Including Nonhuman Primates
BHV-2100, a First-in-class TRPM3 Antagonist for the Treatment of Pain (AAN Abstract of Distinction)
Characterization of BHV-7000: A Novel Kv7.2/7.3 Activator for the Treatment of Seizures
Association of Anti-inflammatory Therapy Use with the Incidence of Parkinson's Disease: A Person-Time Analysis Among Patients with Autoimmune Diseases
Re-weighting MDS-UPDRS Motor Items for Optimal Sensitivity to Parkinson's Disease Progression in Untreated Patients Using Parkinson's Progression Markers Initiative Data
Population Pharmacokinetic Modeling of Riluzole After Administration of a Next Generation Prodrug Troriluzole
Next Generation Prodrug Troriluzole: Increased Bioavailability of Riluzole with No Food Effect in Healthy Subjects
Matching-adjusted Indirect Comparison of Troriluzole Versus Untreated Natural History Cohort in Spinocerebellar Ataxia
Poster Presentations:
Phase 1 Study Evaluating the Safety and Tolerability of BHV-7000, a Novel, Selective Kv7.2/7.3 Potassium Channel Activator, in Healthy Adults
Novel, Selective Kv7.2/7.3 Potassium Channel Activator, BHV-7000, Demonstrates Dose-dependent Pharmacodynamic Effects on EEG Parameters in Healthy Adults
Determinants of Health-related Quality of Life of Patients with Focal Epilepsy: A Systematic Literature Review
Functional Impairments in Patients with KCNQ2-DEE: Associations Among Key Clinical Features
The Phase 3 RESILIENT Study: Taldefgrobep Alfa in Spinal Muscular Atrophy
Re-weighting MDS-UPDRS Part II Items for Optimal Sensitivity to Parkinson's Disease Progression Using Parkinson's Progression Markers Initiative Natural History Data
Safety, Tolerability, and Pharmacokinetics of Single and Multiple Rising Doses of a Next Generation Prodrug Troriluzole in Healthy Subjects
Troriluzole Exhibits Favorable Hepatic Safety Profile Across a Diverse Range of Disorders
No Clinically Relevant Effects of Hepatic Impairment on the Pharmacokinetics of a Next Generation Prodrug Troriluzole
Automated Video-based Characterization of Movement Quality in a Phase III Clinical Trial of Troriluzole in Subjects with Spinocerebellar Ataxia
Psychometric Validation of the Modified-functional Scale for the Assessment and Rating of Ataxia
Development of a Novel Composite Measure (SCACOMS) to Assess Disease Progression in Spinocerebellar Ataxia
Posters and presentations will be available on the Posters and Presentations page after the conference at www.biohaven.com .
About Biohaven Biohaven is a biopharmaceutical company focused on the discovery, development, and commercialization of life-changing treatments in key therapeutic areas, including immunology, neuroscience, and oncology. The company is advancing its innovative portfolio of therapeutics, leveraging its proven drug development experience and multiple proprietary drug development platforms. Biohaven's extensive clinical and preclinical programs include Kv7 ion channel modulation for epilepsy and mood disorders; extracellular protein degradation for immunological diseases; TRPM3 antagonism for migraine and neuropathic pain; TYK2/JAK1 inhibition for neuroinflammatory disorders; glutamate modulation for OCD and SCA; myostatin inhibition for neuromuscular and metabolic diseases, including SMA and obesity; and antibody recruiting, bispecific molecules and antibody drug conjugates for cancer.
Forward-looking Statements This news release includes forward-looking statements within the meaning of the Private Securities Litigation Reform Act of 1995. The use of certain words, including "continue", "plan", "will", "believe", "may", "expect", "anticipate" and similar expressions, is intended to identify forward-looking statements. Investors are cautioned that any forward-looking statements, including statements regarding the future development, timing and potential marketing approval and commercialization of development candidates, are not guarantees of future performance or results and involve substantial risks and uncertainties. Actual results, developments and events may differ materially from those in the forward-looking statements as a result of various factors including: the expected timing, commencement and outcomes of Biohaven's planned and ongoing clinical trials; the timing of planned interactions and filings with the FDA; the timing and outcome of expected regulatory filings; complying with applicable U.S. regulatory requirements; the potential commercialization of Biohaven's product candidates; the potential for Biohaven's product candidates to be first in class therapies; and the effectiveness and safety of Biohaven's product candidates. Additional important factors to be considered in connection with forward-looking statements are described in Biohaven's filings with the Securities and Exchange Commission, including within the sections titled "Risk Factors" and "Management's Discussion and Analysis of Financial Condition and Results of Operations". The forward-looking statements are made as of the date of this news release, and Biohaven does not undertake any obligation to update any forward-looking statements, whether as a result of new information, future events or otherwise, except as required by law.
Investor Contact: Jennifer Porcelli Vice President, Investor Relations [email protected] 201-248-0741
Media Contact: Mike Beyer Sam Brown Inc. [email protected] 312-961-2502
MoDE is a trademark of Biohaven Therapeutics Ltd.
Biohaven AAN 2024 Oral & Poster Presentations:
Functional Impairments in Patients with KCNQ2-DEE: Associations Among Key Clinical Features Sunday 4/14/24: 8:00-9:00 P1- Poster Session 1 Colorado Convention Center – Exhibit Hall B-E
The Phase 3 RESILIENT Study: Taldefgrobep Alfa in Spinal Muscular Atrophy Sunday 4/14/24: 11:45 - 12:45 P2 - Poster Session 2 Colorado Convention Center - Exhibit Hall
Association of Anti-inflammatory Therapy Use with the Incidence of Parkinson's Disease: A Person-Time Analysis Among Patients with Autoimmune Diseases Sunday 4/14/24: 1:00-3:00 (1:24-1:36) S2 – Movement Disorders: Epidemiology and Clinical Aspects Colorado Convention Center- Mile High 4CD
Re-weighting MDS-UPDRS Motor Items for Optimal Sensitivity to Parkinson's Disease Progression in Untreated Patients Using Parkinson's Progression Markers Initiative Data Sunday 4/14/24: 1:00-3:00 (1:36-1:48) S2 – Movement Disorders: Epidemiology and Clinical Aspects Colorado Convention Center- Mile High 4CD
Population Pharmacokinetic Modeling of Riluzole After Administration of a Next Generation Prodrug Troriluzole Sunday 4/14/24: 1:00 - 3:00 (2:12-2:24) S3 - General Neurology 1 Colorado Convention Center - Four Seasons 2/3
Next Generation Prodrug Troriluzole: Increased Bioavailability of Riluzole with No Food Effect in Healthy Subjects Sunday 4/14/24: 3:30 - 5:30 (4:30-4:42) S5 - ALS and CMT: New Therapeutic Approaches Colorado Convention Center - Four Seasons 1
BHV-2100, A First-In-Class TRPM3 Antagonist for the Treatment of Pain Monday 4/15/24: 11:15-12:15 (11:27-11:39) S13 – Pain Research Colorado Convention Center 605
Troriluzole Exhibits Favorable Hepatic Safety Profile Across a Diverse Range of Disorders Monday 4/15/24: 11:45 - 12:45 P4 - Poster Session 4 Colorado Convention Center - Exhibit Hall
Safety, Tolerability, and Pharmacokinetics of Single and Multiple Rising Doses of a Next Generation Prodrug Troriluzole in Healthy Subjects Monday 4/15/24: 11:45 - 12:45 P4 - Poster Session 4 Colorado Convention Center - Exhibit Hall
No Clinically Relevant Effects of Hepatic Impairment on the Pharmacokinetics of a Next Generation Prodrug Troriluzole Monday 4/15/24: 11:45 - 12:45 P4 - Poster Session Colorado Convention Center - Exhibit Hall
Automated Video-based Characterization of Movement Quality in a Phase III Clinical Trial of Troriluzole in Subjects with Spinocerebellar Ataxia Tuesday 4/16/24: 8:00-9:00 P6- Poster Session 6 Colorado Convention Center – Exhibit Hall
Psychometric Validation of the Modified-functional Scale for the Assessment and Rating of Ataxias Tuesday 4/16/24: 11:45-12:45 P7 – Poster Session 7 Colorado Convention Center – Exhibit Hall
Development of a Novel Composite Measure (SCACOMS) to Assess Disease Progression in Spinocerebellar Ataxia Tuesday 4/16/24: 11:45-12:45 P7 - Poster Session 7 Colorado Convention Center – Exhibit Hall
Phase 1 Study Evaluating the Safety and Tolerability of BHV-7000, a Novel, Selective Kv7.2/7.3 Potassium Channel Activator, in Healthy Adults Tuesday 4/16/24: 5:30 - 6:30 P8 - Poster Session 8 Colorado Convention Center - Exhibit Hall
Tuesday 4/16/24: 5:30 - 6:30 P8 - Poster Session 8 Colorado Convention Center - Exhibit Hall
Determinants of Health-related Quality of Life of Patients with Focal Epilepsy: A Systematic Literature Review Wednesday 4/17/24: 8:00-9:00 P9- Poster Session 9 Colorado Convention Center – Exhibit Hall
Characterization of BHV-7000: A Novel Kv7/2/7.3 Activator for the Treatment of Seizures Wednesday 4/17/24: 1:00-3:00 (2:00-2:12) S29- Epilepsy Diagnostics and Therapeutics Colorado Convention Center 605
Matching-adjusted Indirect Comparison of Troriluzole Versus Untreated Natural History Cohort in Spinocerebellar Ataxia Wednesday 4/17/24: 3:30-5:30 (5:06-5:18) S35 – Movement Disorders: Hyperkinetic Movement Disorders Colorado Convention Center – Four Seasons 4
Re-weighting MDS-UPDRS Part II Items for Optimal Sensitivity to Parkinson's Disease Progression Using Parkinson's Progression Markers Initiative Natural History Data Wednesday 4/17/24: 5:30-6:30 P11 – Poster Session 11 Colorado Convention Center – Exhibit Hall
Novel Bispecific Degrader BHV-1300 Achieves Rapid, Robust, and Selective IgG Reduction in Preclinical Models Including Nonhuman Primates Thursday 4/18/24: 1:00 - 3:00 (1:36-1:48) S43 - General Neurology 2 Colorado Convention Center - 108/110/112
View original content to download multimedia: https://www.prnewswire.com/news-releases/biohaven-showcases-innovative-neuroscience-portfolio-with-20-presentations-at-the-2024-american-academy-of-neurology-aan-annual-meeting-and-provides-other-business-updates-302115939.html
SOURCE Biohaven Ltd.

IMAGES
VIDEO
COMMENTS
Step 3: Write the content. Write or rewrite the content for the sections in your poster presentation. Use the text in your research paper as a base, but summarize it to be more succinct in what you share. Don't forget to write a catchy title that presents the problem and your findings in a clear way.
Poster and oral presentations are typically delivered to academic colleagues at conferences or congresses. Here are some best practices and resources to help develop the content and visuals for a high-impact poster, and plan and practice memorable oral presentations. The "Related Resources" on this page can be used to tap into Duke's hub of ...
5. Be early. If you are running late, you will be more nervous and have less time to prepare yourself mentally. 6. On the day of the talk, take 10-15 minutes before your presentation to relax, do some deep breathing, and keep your mind off of the presentation for a bit. You want to be relaxed during your presentation. 7.
b. A poster should be self-sustaining i. The poster should be able to stand alone. A good poster contains just enough information to be understandable. The presenter can always fill in the gaps if requested by a viewer. c. Posters speak, but you speak better i. Once you have an audience, you will begin an oral presentation. ii.
Oral presentations. For oral presentations the same headings should be followed, with clear simple slides. Keep the number of slides to a minimum to keep the length of the talk on track. A good guideline is around one slide per minute. Set the scene with a clear introduction to the work, indicating the relevance of the study to the general ...
Gesture to the relevant parts of the poster. You should use your whole hand to point toward something rather than just pointing a finger. Graphs and other data are excellent parts of a poster for gesturing. Avoid turning your back on your audience to gesture. Use the arm closest to the poster to gesture so you are not gesturing across your body ...
Posters & Oral Presentations. Good scientific research involves a sound methodology and a novel idea that can be tested simply and repeatedly to give valid, trustworthy results. However, even the most clinically significant research is useless if it is not communicated successfully. Scientific ideas are novel, sometimes simple in theory, but ...
1. Think of, or research, an attention grabber: a story, fact or statistic, or other interesting piece of information that will help draw in the audience right away and frame the talk in a minute or less. 2. Focus only on the 3 most important points. Introduce them at the beginning, and repeat them at the very end. 3.
A poster or oral presentation is a great way to share your research project and get feedback. Designing a poster or preparing an oral presentation should be done within the guidelines set forth by the conference. Traditional posters and oral presentations convey the same information in different formats.
Poster presentations allow the author to meet and speak informally with interested viewers, facilitating a greater exchange of ideas and networking opportunities than with oral presentations. Poster presentations often are the first opportunities for young investigators to present their work at important scientific meetings and preparatory for ...
While there may be some differences in things to consider when making a poster or putting together powerpoint slides for an oral presentation, the following considerations and tips for the presentation aspect can apply to either poster or oral presentations: General Tips for Presentations: MARCH 21 2020 // #UBCMURC Define Your Purpose
Many conferences have poster presentation sessions along with oral presentations. The poster presentation is a format introduced into the American Chemical Society meetings in the 1970s. This format allows more people the opportunity to present their work since many posters can be scheduled for the same time period and in one large room.
Brainstorm. Presentations, like reports, require careful planning and attention to detail. Brainstorming, the spontaneous process of generating ideas, is often the first step in planning a presentation. After brainstorming ideas, and writing them down, you should review these ideas and filter out extraneous ones until you are left with those ...
Templates for Oral and Poster Presentations; Contact Info. Department of Biomedical Engineering M c Cormick School of Engineering and Applied Science 2145 Sheridan Road Evanston, IL 60208 Phone: 847-467-1213 Fax: 847-491-4928 Email Department. Northwestern Seal.
This free PowerPoint poster template is designed for a standard 4x4 foot poster presentation. This scientific poster template is a good size for limited available spaces without compromising room for content. This research poster template can be printed at the following sizes: 48x48 (Standard), 36x36, 24x24, 42x42.
Add headers if necessary to clarify the structure of your poster, and add everything else that is needed, such as literature, acknowledgements. Ensure that author name(s) and affiliation are on the poster. 7) Review, revise, optimize. Ask your co-authors and/or colleagues to comment on a draft version of your poster.
Mechanical and Industrial Engineering Department. P.O. Box 173800 Bozeman, MT 59717-3800 Tel: (406) 994-2203 Fax: (406) 994-6292 Location: 220 Roberts
Presentation Deadlines and Upload Instructions. First authors should submit their PowerPoint slide presentations on ASCO's Speaker Center by the following deadlines: Oral Abstracts: Preliminary slides for review by your discussant and session chair - May 13, 2024, by 11:59 PM ET. Rapid Oral Abstracts: Preliminary slides for review by your ...
A Comparison: Poster vs Oral Presentation. When deciding between a poster and an oral presentation, there are several key features to consider. 1. Visual Impact: Posters offer a visual representation of information, while oral presentations allow for direct engagement. 2.
Oral and Poster Presentations. ... Training was held in March 2018, and leaflets and posters were displayed for the 3-month period. An embedded experimental mixed-methods design was used, with data collected via SystmONE questionnaires, surveys and focus groups. ... Multi-disciplinary educators delivered formal presentations and facilitated ...
Please follow the guidelines below when preparing your oral presentation. Include an abstract on your poster to ensure viewers can follow it. Provide appropriate context to ensure an international audience can follow your paper content. Demonstrate how your poster clearly addresses the congress or session themes. Display of your poster.
Presentation Length: In general, Oral abstract presenters are asked to prepare an 8-minute presentation. An optimal 8-minute presentation has 8 content slides not including the 1 title slide provided. The session moderators will cut off presentations longer than 8 minutes. Presentation Contents: Refer to the Guidelines for Presentation ...
audio presentations of annual meeting posters. Download the free PosterCast app to stream audio explanations of posters as you view them. While you are in the poster hall, simply scan the QR code on a participating poster or use the keypad to enter the poster number. This resource is particularly valuable when posters are unattended by presenters.
Oral Presentations Talks are limited to 15 minutes, with 5 minutes for questions. ... Poster Presentations Posters should be no larger than 48 inches tall and 60 inches wide. Posters should be set up during the registration period (8AM - 9AM) and will remain up all day. California Institute of Technology. 1200 East California Boulevard.
Authors making poster presentations must submit their posters to the ICSD organizers by August 1, 2024, or risk losing their presentation slot. We will begin accepting posters on June 1, 2024, via a Poster Presentations Airtable Form. This year's posters will be displayed in our online virtual event poster gallery on this ICSD conference website.
The showcase of work will include poster presentations, demonstrations, and oral presentations. Posters will be on display from 12 p.m. to 3 p.m. and the schedule of oral presentations will be announced in the coming days.
Oral Presentation Oral Presentation 1 and Oral Presentation 2. Journal of the International Society of Physical and Rehabilitation Medicine. 6(4) ... Favorite; PDF; Permissions Free. Table of Contents Outline | Back to Top Poster presentations Poster presentations Part 1, Poster presentations Part 2 and Poster presentations Part 3.
Three oral presentations and 6 poster presentations from the Biohaven Clinical and Health Outcomes group describe the development and validation of novel scales and natural history studies in support of troriluzole and BHV-8000 development programs, the impact of immune-modulating therapy in Parkinson's disease, the burden of illness in focal ...
Biohaven Ltd. (NYSE: BHVN) announced today that 20 abstracts, including 8 oral presentations and 12 posters, will be featured this weekend starting April 13th at the 2024 American Academy of ...