- Health Science

Biology Lab Report- Blood Typing Lab
Related documents
Study collections
Add this document to collection(s).
You can add this document to your study collection(s)
Add this document to saved
You can add this document to your saved list
Suggest us how to improve StudyLib
(For complaints, use another form )
Input it if you want to receive answer
Want to create or adapt books like this? Learn more about how Pressbooks supports open publishing practices.
Learning Objectives
- Explain hematocrit, including the significance of values outside of the normal range.
- Determine hematocrit from a blood sample image.
- Explain the ABO and Rh blood groups and their clinical significance.
- Conduct blood typing on a synthetic-blood sample.
- Identify and describe all formed elements in a human blood smear.
- State the relative proportions of formed elements in human blood.
- Demonstrate proficient microscope use.
Blood Composition and Hematocrit
Composition of blood.
Overview of Blood [link opens in new window]
- Proteins (for blood pressure, clotting, and immune functions)
- Water (92% of plasma)
- Electrolytes
- Blood gases
- Red Blood Cells (erythrocytes)
- Platelets (thrombocytes)
- White Blood Cells (leukocytes)
- Definition: The volume—reported as a percentage—of packed elements (mainly red blood cells) in a blood sample.
- Clinical relevance: Provides information about the oxygen-carrying capacity of blood. Low hematocrit means less red blood cells carrying O2.
- Male: ____________%
- Female:____________%

Blood Typing
Blood type refers to the presence or absence of specific molecules, called antigens, on the red blood cell (RBC) RBC surface. Antigens are molecules, such as proteins, lipids, carbohydrates or nucleic acids, that your body can use to differentiate self and non-self. People with different blood types have different antigens on their RBCs.
Antibodies are produced in response to some antigens (non-self), and are generally used by the immune system to recognize and facilitate removal of objects (viruses, bacteria, tumorous cells, etc.) that do not belong in the body.
There are more than 50 blood types in the human population. The most clinically significant are the ABO and Rh(+/-) blood groups.
The ABO Blood Group
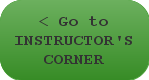
A and B antigens are glycoproteins on the RCC surface. ABO typing does not affect a person’s Rh (+ or -) designation. Figure 2.3 Blood Type
Type A blood: A antigens on cell; anti-B antibodies in plasma
Type B blood: B antigens on cell; anti-A antibodies in plasma
Type AB blood: both A and B antigens on cell; neither anti-A nor anti-B antibodies in plasma
Type O blood: neither A nor B antigens on cell; both anti-A and anti-B antibodies in plasma
If a different type of blood is put into your bloodstream, the blood will agglutinate (clump) and hemolysis (bursting) occurs within the foreign blood cells. Agglutination due to antibodies and antigens is a different process than blood clotting, which involves fibrin and other cascades associated with hemostasis.

Rh Blood Group
Rh antigens are named after the rhesus macaque, a primate with many blood similarities to human. There are many Rh antigens in humans, but the D type of Rh antigen is the most clinically significant. Because of this, in blood typing, sometimes D and Rh are used interchangeably. The Rh factor is grouped with ABO blood group to identify a blood type (example A+, B-, O-).
Type Rh+ (positive) blood: Rh antigens on cell
Type Rh- (negative) blood: no Rh antigens on cell
Unlike ABO blood type, no anti-Rh antibodies are present in Rh- individuals unless they have been exposed to Rh antigens. If Rh+ blood is introduced into an Rh- individual, anti-Rh antibodies will be produced against the Rh(+) blood.
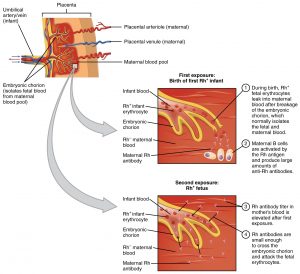
Importance of Rh during Pregnancy
This is a critical consideration in pregnancy for Rh- mothers if the fetus is Rh+. If any of the Rh+ blood enters the mother’s circulation, the mother’s immune system will produce anti-Rh antibodies that will hemolyze her baby’s blood (and any future Rh+ fetuses). This is called hemolytic disease of the newborn or erythroblastosis fetalis. It is prevented with RhoGAM, a dosage of anti-Rh antibodies, given to the mother at 27 weeks and within 72 hours of giving birth in order to destroy any fetal blood cells in her blood so she will not produce her own anti-Rh antibodies. RhoGam antibody dosage is small enough not to hurt fetus, but strong enough to keep mom’s immune system from attacking fetus. See Figure 2.4.
Determining Blood Type
To determine blood types, antiserum is used. The serum contains antibodies that may react with antigens on the RBC surface.
If using anti-A antiserum (contains anti-A antibodies) and the blood sample agglutinates (clumps), this indicates the presence of A antigens.
Which blood types have A antigens? Fill in the type. Type _____ and Type _____
If using anti-B antiserum (contains anti-B antibodies) and the blood sample agglutinates (clumps), this indicates the presence of B antigens.
Which blood types have B antigens? Fill in the type. Type _____ and Type _____
If using anti-Rh (anti-D) antiserum (contains anti-Rh (anti-D) antibodies) and the blood sample agglutinates (clumps), this indicates the presence of Rh antigens.
Which blood type has Rh antigens? Fill in the type. Type _____
Blood Typing Data
Complete the blood typing on your samples and enter your data in Table 2.1.
For each blood sample:
- Place a drop of blood in each of the three depressions of one testing tray. Each depression has a label of A, B, or Rh(D). One tray is used for each blood sample.
- Place a drop of the antiserum that is associated with each depression. For example anti-A antiserum (containing anti-A antibodies) goes into the depression marked A. In that depression, you will be testing to see if the anti-A antibodies agglutinate RBCs with A antigens. Do the same for anti-B and anti-Rh sera into each of their depressions in the tray.
- Stir the combination of the blood and antiserum in each depression with the color coded toothpick. Do not mix toothpicks across depressions.
- Examine the samples for agglutination and fill out your data table to determine the blood type for each sample.
Table 2.1 Blood Typing Data
Human Blood Microscopy and General Microscope Use
In this part of the lab you will use a microscope to examine erythrocytes, leukocytes, and platelets. These three constituents are referred to as the formed elements of blood. Platelets are not considered a cell, as they are enclosed cytoplasmic fragments. A complete blood count with differential is a clinical measure that states the percentages of each blood cell type and is used for various diagnostics such as determining anemia or types of infections or allergic reactions. Erythrocytes are the most numerous blood cell, and then the count of the different leukocytes goes from most to least numerous in this order: neutrophils, lymphocytes, monocytes, eosinophils, and basophils.
Formed Elements of Blood
Erythrocytes (red blood cells).
Erythrocytes
See Figure 2.5 below and notice the numerous, round, pink cells in the background each of the leukocyte images. These are red blood cells (RBCs). Some look like they have a hole in the middle, but this is due to the thin area of the biconcave shape that allows for flexibility and to increase surface area.
Primary function: transport respiratory gases to and from tissues.
Lack a nucleus.
Most abundant of all blood cells.
Contains millions of Hemoglobin molecules: allow for binding of O2 and CO2.
Also called thrombocytes but not technically a cell. They are produced by the fragmentation megakaryocytes that are in bone marrow tissue.
Involved in coagulation: the process of clot formation.
During coagulation, molecules (fibrin) join to form long threads that form a net to trap platelets and plug the wound.
Leukocytes (White Blood Cells)
See Figure 2.5 below.
Only formed elements with a nucleus.
Lacks hemoglobin.
Travel between endothelial cells of capillaries and tissues.
Two types of leukocytes: granular and agranular.

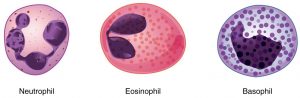
Granulocytes
See Figure 2.6 below.
All have granules in cytoplasm.
- most common WBC
- 1st to arrive at wound/infection site
- release cytotoxins
- capable of phagocytosis
- phagocytize microbes that immune system has coated with antibodies
- decrease inflammatory response at site of wound
- release histamines (cause vasodilation) and heparin (prevents clotting)
- important in allergies
Agranulocytes
Refer back to Figure 2.5
Fewer and less obvious granules in cytoplasm.
- wanderers, patrol body tissue for microbes and worn-out tissue cells
- 2nd to arrive at wound site
- phagocytize dead cells/debris that has accumulated at site of wound/infection
- smallest leukocyte, abundant in bloodstream, occur in lymph nodes and glands
- T-cells: attach to and destroy infected or cancerous cells by releasing cytotoxic molecules and secreting antiviral/proinflammatory molecules
- B-cells: manufacture antibodies that attach to foreign pathogens/cells and help destroy them
- Natural Killer cells: can detect sick, cancerous, and infected cells and release cytotoxic molecules to destroy them
Follow the instructions below for microscope use, and examine a human blood smear. Sketch each of the formed elements of blood as seen in your view.
Microscope Parts and How To Handle Them
There are many different types of microscopes. We shall learn about the compound light microscope. It uses visible light to visualize the specimen, and passes that light through two separate lenses to magnify the image. Compound microscopes have a lot of moving parts and can be damaged and broken through mishandling. A large part of learning how to use the microscope properly involves learning how to avoid damaging it. To do that, you first have to be familiar with the parts.
In Figure 2.7, there are two compound microscopes shown with key parts identified. The one on the left is monocular and the one on the right is binocular. Many of the parts of the two microscopes are in slightly different locations.
When you first sit in front of a microscope, take a moment to find the key parts, especially the knobs for focus, condenser adjustment, and stage control. When viewing a specimen, your eyes will be at the eyepieces (oculars), and if you grab the wrong knob by accident, you can lose your image or damage the microscope.

Eyepiece (Ocular)
The eyepiece contains the eyepiece lens, one of the two lenses doing the magnifying in a compound microscope. If the microscope is binocular, use both eyepieces, adjusting them to ensure they fit the spacing of your eyes. For successful binocular viewing, bring your image into focus with the lowest power objective, while looking through only the non-adjustable ocular. Then while looking only through the adjustable ocular, rotate its focus ring to bring that ocular into clear focus. Now the image should be clear as you look through both oculars.
Carrying arm
When moving a microscope, even if it is just a few inches, always pick it up by the carrying arm. Do not drag the microscope: pick it up. The microscope will have rubber feet that prevent it from sliding, so if you try to drag it, it will shake and vibrate and possibly damage parts. Never pick up the microscope by any part other than the carrying arm. The other parts are generally much more fragile and prone to breaking.
Objective lenses
Most compound light microscopes will contain three to four objective lenses that can be rotated over the slide. Sometimes these lenses are just called objectives. When a particular objective has been fully rotated into position, you will feel a click as that objective locks into place. The objective lens is the second of the two lenses doing the magnifying in a compound microscope, so if it is not snapped into proper position, you will not see the proper image. Each objective lens can usually be unscrewed from its position in the rotating turret that houses it, so be careful you are rotating the turret, not unscrewing an objective. Do not unscrew the objectives from the turret. Each objective lens has a different magnifying power, so the image on your slide will be magnified to lesser or greater extents, depending on which objective lens you have chosen. Each objective’s magnification power will be written somewhere on the side of the objective.
Stage and stage clips
The slide will be held in place on the stage with stage clips that press against the sides of the slide. The clips do not sit above or below the slide. They are spring-loaded to hold the slide edges and lock the slide in place so that the stage controls can move the position of the slide smoothly.
Stage controls
These allow you to move your slide while you are viewing it, but only if the slide is properly clipped in with the stage clips. Find the stage control dials on your microscope before you start viewing your slide. There are two dials—one moves the slide left and right, the other moves the slide up and down. Notice in Figure 2.7, the dials are on top of each other and below the stage on the binocular microscope, however, they are two separate dials and above the stage on the monocular microscope.
Coarse focus
This is the larger of the two focus knobs. Use it with the lowest power objective to get the specimen approximately in focus. After that, only use the fine focus knob, even after you change to a higher-power objective. Notice in Figure 2.7, the binocular microscope fine focus knob is surrounded by the coarse focus knob, however, the monocular microscope coarse focus and fine focus knobs are separated.
This is the smaller of the two focus knobs. This is the focus you will use repeatedly in viewing slides once they are focused with the coarse focus.

Condenser position adjustment
You typically will not need to adjust this knob. It controls how far the light condenser is from the slide, which should be properly adjusted before you use the microscope.
Condenser opening adjustment (not shown in figure)
This opening can be adjusted, usually by rotating a ring around the condenser. Be sure this has not been left closed by a previous user. Experiment with different opening sizes to determine what is best for your specimen.
Iris diaphragm lever
Find the lever under the stage where light passes through to the slide. It opens and closes an iris to let more or less light through the slide. In some specimens there is not much contrast between the colours and shades of the different components being magnified. Changing the view by adjusting the iris can allow you to better see some of the details you are trying to magnify.
Rheostat: Light intensity (not shown in figure)
Rotate this dial to adjust the brightness of the light source. Turn this to its a low setting before looking through the eyepieces. You may need to increase the intensity as you increase the power of your objective. Turn the rheostat all the way down before turning off your microscope.
Lab exercises
Carry out the activities listed below and answer the questions.
- Pick up your microscope and bring it close enough that you can look into it comfortably from where you are sitting with healthy posture. Arrange it so that the stage is facing you and the eyepieces are rotated toward you. What part of the microscope did you grab in order to pick it up and move it?
- Where are the locations of the two stage adjustment knobs on your microscope?
- Where is the location of the coarse focus knob?
- Where is the location of the fine focus knob?
- Is there a condenser opening adjustment ring?
- Find the diaphragm lever. Looking in the hole in the center of the stage, what happens when you move the diaphragm lever in each direction?
- After cleaning a slide as instructed by your professor, place the slide on the stage.
- Take the steps described in the ocular section to obtain clear view through both of your oculars. If you wear glasses, try with and without to determine which is best for you.
- Adjust the condenser opening and iris lever. How does this change your view?
Checking out and storing the microscope
When you finish your microscope work with the blood slide, be prepared to have your instructor check off each of these items before putting away your microscope.
- Turn the rheostat to its dimmest setting.
- Turn off the power, unplug, and wrap the cord around the base.
- Wipe the objective lenses with methanol and lens paper. Notice this is lens paper, not kimwipes. Using any paper other than lens paper can scratch the lens.
- Rotate the objective lens turret so the lowest power objective faces down.
- Wipe the stage clean with a kimwipe and move it to the lowest position.
“Blood Lab” is MODIFIED from:
- Anatomy and Physiology by Open Stax / CC BY 4.0. Download for free at http://cnx.org/contents/[email protected] .
- An Overview of Blood, Anatomy and Physiology by Open Stax / CC BY 4.0. https://cnx.org/contents/[email protected]:IUrEdFyf@10/An-Overview-of-Blood
- UGA Anatomy and Physiology 2 Lab Manual by University System of Georgia / CC BY 4.0
- Human Anatomy and Physiology Lab (BSB 141) by Lumen Learning / CC BY-SA
- A&P Labs. Authored by: Ross Whitwam. Provided by: Mississippi University for Women. Located at: http://www.muw.edu/ . License: CC BY-SA: Attribution-ShareAlike
- Labeled compound light microscope. Authored by: Ross Whitwam. Provided by: Mississippi University for Women. Located at: http://www.muw.edu/ . License: CC BY-SA: Attribution-ShareAlike
Citation notes:
- Hesse, DeLoris; Cozart, Deanna; Szymik, Brett; and Nichols, Rob, “UGA Anatomy and Physiology 2 Lab Manual” (2017). Biological Sciences Open Textbooks. 14. https://oer.galileo.usg.edu/biology-textbooks/14
“Microscope Parts and How to Handle Them” is MODIFIED from:
- Lumen Learning. CC BY-SA https://courses.lumenlearning.com/ap1x9x1/chapter/the-parts-of-a-compound-microscope-and-how-to-handle-them-correctly/
- Labelled compound light microscope. Authored by: Ross Whitwam. Provided by: Mississippi University for Women. Located at: http://www.muw.edu/ . License: CC BY-SA: Attribution-ShareAlike
Anatomy and Physiology 2 Laboratory Manual Copyright © 2019 by Sheryl Shook is licensed under a Creative Commons Attribution 4.0 International License , except where otherwise noted.
Share This Book
- Attributions

- school Campus Bookshelves
- menu_book Bookshelves
- perm_media Learning Objects
- login Login
- how_to_reg Request Instructor Account
- hub Instructor Commons
- Download Page (PDF)
- Download Full Book (PDF)
- Periodic Table
- Physics Constants
- Scientific Calculator
- Reference & Cite
- Tools expand_more
- Readability
selected template will load here
This action is not available.

3.1: Blood Typing Lab
- Last updated
- Save as PDF
- Page ID 138514
- Katherine E. Brent & Sydney Quinn Chizmeshya
Blood Typing
Format: In-person or online
Authors: Katherine E. Brent and Sydney Quinn Chizmeshya
Source: Modified from Classroom Activity on Antibodies . Oxford Sparks.
Time needed: 30-40 minutes total. 15-20 minutes for the activity; 15-20 minutes for the reflection questions
Supplies Needed
- Milk, vinegar, water
- Red gel food coloring
- Eyedroppers or pipettes (5 per group)
- Permanent marker
- Toothpicks or stirrers (6 per group)
- Small containers or sealable test tubes (5 per group)
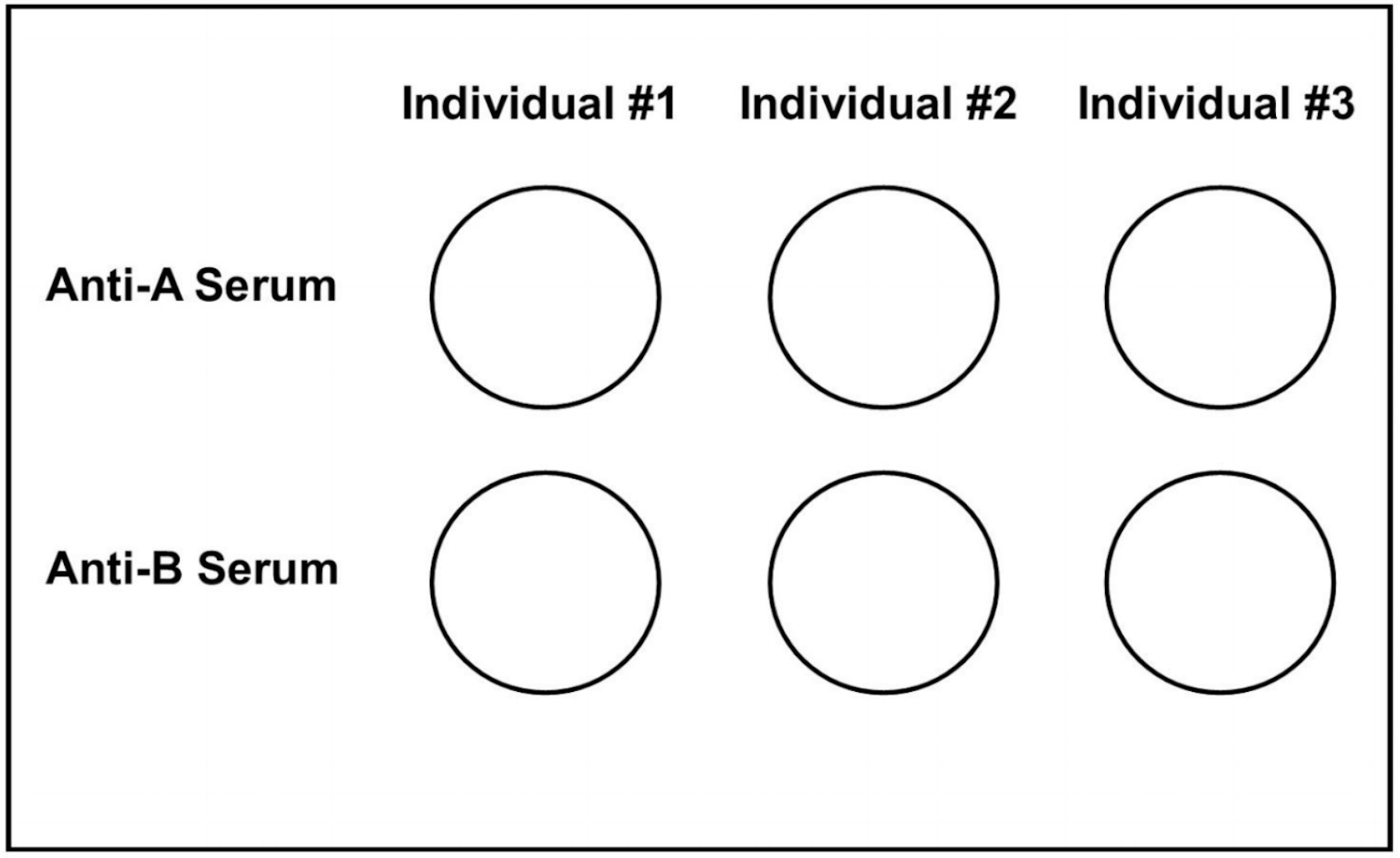
- Blood typing test plate (attached) laminated or placed in a plastic sheet protector (1 per group)
- Student worksheet (attached)
Introduction
In this lab students will perform a blood type test, also called an agglutination assay, on the simulated blood of three individuals. They will observe the agglutination reaction, and determine the blood types of three individuals. Subsequently, students will answer reflection questions about the observations they made during the experiment, as well as consider the inheritance patterns for ABO blood types and what characteristics of this trait are regarded as “Mendelian”.
- Prepare three solutions: vinegar with food coloring, milk with food coloring, and water with food coloring. Slowly add food coloring little by little to ensure that the dye does not coagulate the substance.
- Individual #1: Dyed vinegar (this will simulate Type A blood)
- Individual #2: Dyed milk (this will simulate Type B blood)
- Individual #3: Dyed water (this will simulate Type O blood)
- Anti-A Serum: Milk
- Anti-B Serum: Vinegar
- Five eyedroppers or pipettes
- Six toothpicks or stirrers
- Blood Typing Test Plate (attached) laminated or placed in a plastic sheet protector (1 per group)
- Student worksheets
- Students should use the instructions on their worksheet to complete the lab. When students perform the experiment, they must use each pipette for only the substance it is intended to be used for, as cross-contamination may provide false coagulations.
- Using the pipette for Individual #1, they will pipette several drops of Individual #1’s blood sample into the circles comprising the first column of the laminated blood typing test plate. Individual #2’s sample should be pipetted into to the second column, and Individual #3’s sample pipetted into the third column.
- Using the pipette for Anti-A Serum, pipette several drops of Anti-A serum into each blood sample in the first row of the test plate. Using the pipette for Anti-B Serum, pipette several drops of Anti-B serum into each blood sample in the second row of the test plate.
- Students will stir each sample using a different toothpick for each of the six samples.
- Students will observe each sample to see if it has coagulated (agglutinated) or not, and determine the three individuals’ blood types based on the results.
- Students will complete the reflection questions on their worksheet.
Students will practice observation and problem solving through this lab, as well as review key concepts about Mendelian inheritance and blood typing. Reflection questions are provided on the student worksheet and instructors are encouraged to review some or all of these questions as a class afterwards.
Adapting for Online Learning
1 Not adaptable 2 Possible to adapt 3 Easy to adapt
With clear directions most students could create the artificial blood and serums, as well as complete the experiment, in their home. Instructors could also record a short video showing the experiment for students to watch and reflect on at home.
For Further Exploration
ThePenguinProf. Blood Types: ABO and Rh (with donuts and sprinkles!) https://www.youtube.com/watch?v=L06TJTMVkBo
Wake, Carol. 2005. “ABO/Rh Blood Typing Model: A Problem-Solving Activity.” The American Biology Teacher 67 (3): 158-162.
Arnold, Savittree Rochanasmita, Tussatrin Kruatong, Chanyah Dahsah, and Duongdearn Suwanjinda. 2012. “The Classroom-Friendly ABO Blood Types Kit: Blood Agglutination
Simulation.” Journal of Biological Education 46 (1): 45-51. https://doi.org/10.1080/00219266.2011.556750
Mann, Hayley, Xazmin Lowman, and Malaina Gaddis. 2019. “Chapter 3: Molecular Biology and Genetics.” In Explorations: An Open Invitation to Biological Anthropology, edited by Beth Shook, Katie Nelson, Kelsie Aguilera, and Lara Braff. Arlington, VA: American Anthropological Association. http://explorations.americananthro.org/
Image Attributions
Blood cells human electron microscope by skeeze has been designated under a Pixabay License .
Blood types by Shahinsahar is used under a CC BY-SA 3.0 License .
Blood typing test plate by Katherine E. Brent and Sydney Quinn Chizmeshya original to Explorations Lab and Activities Manual is under a CC BY-NC 4.0 License .
Blood Typing: Worksheet
This lab explores the concepts of Mendelian inheritance using the ABO Blood Group System as an example. Please review the corresponding sections: “Mendelian Genetics” and “Example of Mendelian Inheritance: The ABO Blood Group System” in Explorations Chapter 3: Molecular Biology and Genetics, which will provide the background information to complete the lab exercise.
In this lab, you will be performing a blood type test (agglutination assay) on the simulated blood of three individuals. Subsequently, you will answer reflection questions about the observations you made during the experiment.
As a reminder:
- Blood types in the ABO Blood Group System are A, B, O, and AB.
- A and B alleles are dominant over the O allele, and are codominant with each other. This is because possessing the A or B allele always leads to the production of the corresponding antigen.
- Type A blood with A antigens will coagulate (agglutinate) when they come in contact with anti-A serum (antibodies), but produce anti-B antibodies in a living person, so will not coagulate with anti-B serum.
- Type B blood with B antigens will coagulate (agglutinate) when they come in contact with anti-B serum (antibodies), but produce anti-A antibodies in a living person, so will not coagulate with anti-A serum.
- Type AB blood has both A and B antigens, and will coagulate (agglutinate) when they come in contact with either anti-A or anti-B serum (antibodies). These individuals do not produce anti-A or anti-B antibodies.
- Type O blood produces both anti-A and anti-B antibodies, so it will not coagulate with Anti-A or Anti-B Serum.
Lab Kit Materials
- Individual #1 Blood Sample
- Individual #2 Blood Sample
- Individual #3 Blood Sample
- Anti-A Serum
- Anti-B Serum
- Blood Typing Test Plate laminated or placed in a plastic sheet protector
Instructions
- Using the permanent marker, label each of your five pipettes with one of the substance names (e.g. Individual #1, Anti-A serum). When you perform the experiment, you must ensure that you use each pipette for only the substance it is intended to be used for, as cross-contamination may provide false coagulations.
- Using the pipette for Individual #1, pipette several drops of Individual #1’s blood sample into the circles comprising the first column of the blood typing test plate. Individual #2’s sample should be pipetted into to the second column, and Individual #3’s sample pipetted into the third column.
- Using a different toothpick for each of the six samples, stir each sample.
- Observe each sample to see if it has coagulated (agglutinated) or not.
Reflection Questions
Observe each sample for coagulation. Based on what you see… a. What blood type does Individual #1 have? What is/are the possible genotype(s) for Individual #1? b. What blood type does Individual #2 have? What is/are the possible genotype(s) for Individual #2? c. What blood type does Individual #3 have? What is/are the possible genotype(s) for Individual #3?
Suppose that the three samples are from two parents and their child. a. Which individuals are the parents? Which individual is the child? How do you know? b. What genotype must each individual have for this scenario to be possible? c. Draw a Punnett square using the parents’ genotypes. Circle the genotype that belongs to the child that you have blood typed. d. What is the percent chance that these two parents would have a child with this blood type?
There is one blood type not represented in these samples. a. What blood type is it? b. What would you predict would happen if you added Anti-A serum to this type of blood? c. What would you predict would happen if you added Anti-B serum to this type of blood? d. Why is the genotype that codes for this blood type considered “codominant”?
Is ABO considered a “Mendelian Trait”? a. What is “Mendelian genetics”? How would you identify a trait that follows a pattern of Mendelian genetics? Review the section “Mendelian Genetics” in Chapter 3 to help you. b. How does the ABO blood type system follow the rules of Mendelian Inheritance? c. In what ways is the ABO blood type system more complex than the pea plant traits that Mendel observed?
Blood Typing Test Plate
Global Sites

- 10-Panel Drug Test
- 17-Hydroxyprogesterone
- Acetaminophen
- Acetylcholine Receptor (AChR) Antibody
- Acid-Fast Bacillus (AFB) Testing
- ACTH Stimulation Test
- Activated Clotting Time (ACT)
- Acute Viral Hepatitis Panel
- Adenosine Deaminase
- Adrenocorticotropic Hormone (ACTH)
- Alanine Aminotransferase (ALT)
- Aldosterone and Renin
- ALK Mutation (Gene Rearrangement)
- Alkaline Phosphatase (ALP)
- Allergy Blood Testing
- Alpha-1 Antitrypsin
- Alpha-fetoprotein (AFP) Tumor Marker
- Aminoglycoside Antibiotics
- Amniotic Fluid Testing
- Androstenedione
- Angiotensin-Converting Enzyme (ACE)
- Anti-DNase B
- Anti-Müllerian Hormone
- Anti-MuSK (muscle-specific kinase) Antibodies
- Anti-Saccharomyces cerevisiae Antibodies (ASCA)
- Antibiotic Susceptibility Testing
- Antibody Titer Test
- Anticentromere Antibody
- Antidiuretic Hormone (ADH)
- Antimitochondrial Antibody and AMA M2
- Antineutrophil Cytoplasmic Antibodies (ANCA, MPO, PR3)
- Antinuclear Antibody (ANA)
- Antiphospholipid Antibodies
- Antistreptolysin O (ASO)
- Antithrombin
- APOE Genotyping, Alzheimer Disease
- APOE Genotyping, Cardiovascular Disease
- Arbovirus Testing
- Aspartate Aminotransferase (AST)
- Autoantibodies
- B-cell Immunoglobulin Gene Rearrangement
- Bacterial Wound Culture
- Basic Metabolic Panel (BMP)
- Beta-2 Glycoprotein 1 Antibodies
- Beta-2 Microglobulin Kidney Disease
- Beta-2 Microglobulin Tumor Marker
- Bicarbonate (Total CO2)
- Blood Culture
- Blood Gases
- Blood Ketones
- Blood Smear
Blood Typing
- Blood Urea Nitrogen (BUN)
- BNP and NT-proBNP
- Body Fluid Testing
- Bone Markers
- Bone Marrow Aspiration and Biopsy
- BRCA Gene Testing for Breast and Ovarian Cancer Risk
- Breast Cancer Gene Expression Tests
- C-Reactive Protein (CRP)
- Calprotectin
- CALR Mutation
- Cancer Antigen 19-9
- Carbamazepine
- Carcinoembryonic Antigen (CEA)
- Cardiac Biomarkers
- Cardiac Risk Assessment
- Cardiolipin Antibodies
- Catecholamines
- Celiac Disease Antibody Tests
- Cerebrospinal Fluid (CSF) Testing
- Ceruloplasmin
- Chemistry Panels
- Chickenpox and Shingles Tests
- Chlamydia Testing
- Cholesterol Test
- Cholinesterase Tests
- Chromogranin A
- Chromosome Analysis (Karyotyping)
- Chymotrypsin
- Clopidogrel (CYP2C19 Genotyping)
- Clostridium difficile and C. diff Toxin Testing
- Coagulation Cascade
- Coagulation Factors
- Cold Agglutinins
- Complete Blood Count (CBC)
- Comprehensive Metabolic Panel (CMP)
- Continuous Glucose Monitoring
- Coronavirus (COVID-19) Testing
- Creatine Kinase (CK)
- Creatinine Clearance
- Cryoglobulins
- Cyclic Citrullinated Peptide Antibody
- Cyclosporine
- Cystic Fibrosis (CF) Gene Mutations Testing
- Cytomegalovirus (CMV) Tests
- Dengue Fever Testing
- Des-gamma-carboxy prothrombin (DCP)
- Direct Antiglobulin Test
- Direct LDL Cholesterol
- Drug Abuse Testing
- EGFR Mutation Testing
- Electrolytes and Anion Gap
- Emergency and Overdose Drug Testing
- Epstein-Barr Virus (EBV) Antibody Tests
- Erythrocyte Sedimentation Rate (ESR)
- Erythropoietin
- Estimated Glomerular Filtration Rate (eGFR)
- Estrogen Receptor, Progesterone Receptor Breast Cancer Testing
- Extractable Nuclear Antigen Antibodies (ENA) Panel
- Factor V Leiden Mutation and PT 20210 Mutation
- Fecal Immunochemical Test and Fecal Occult Blood Test
- Fetal Fibronectin (fFN)
- FIP1L1-PDGFRA
- First Trimester Screening
- Follicle-stimulating Hormone (FSH)
- Food Allergy Testing
- Food Sensitivity Test
- Fragile X (FMR1) Genetic Testing
- Fructosamine
- Fungal Tests
- Gamma-Glutamyl Transferase (GGT)
- Gastrointestinal Pathogens Panel
- Genetic Tests for Targeted Cancer Therapy
- Glucose Tests
- Glucose Tests for Gestational Diabetes
- Glucose Tolerance Test
- Gonorrhea Testing
- Growth Hormone
- Haptoglobin
- hCG Tumor Marker
- HDL Cholesterol
- Heavy Metals
- Helicobacter pylori (H. pylori) Testing
- Hemoglobin A1c
- Hemoglobinopathy Evaluation
- Heparin Anti-Xa
- Heparin-induced Thrombocytopenia PF4 Antibody
- Hepatitis A Testing
- Hepatitis B Testing
- Hepatitis C Testing
- Herpes Testing
- High-sensitivity C-reactive Protein (hs-CRP)
- Histone Antibody
- HIV Drug Resistance Testing, Genotype
- HIV Viral Load
- HLA Testing
- Homocysteine
- Human Epididymis Protein 4 (HE4)
- Human Papillomavirus (HPV) Test
- Human T-cell Lymphotropic Virus (HTLV) Testing
- IGRA TB Test
- Immunoglobulins (IgA, IgG, IgM)
- Immunophenotyping by Flow Cytometry
- Immunoreactive Trypsinogen (IRT)
- Influenza Tests
- Inhibin A and Inhibin B Tumor Markers
- Inhibin B in Infertility
- Insulin-like Growth Factor-1 (IGF-1)
- Interleukin-6
- Intrinsic Factor Antibody
- Islet Autoantibodies in Diabetes
- JAK2 Mutation
- Kidney Stone Risk Panel
- Kidney Stone Testing
- KRAS Mutation
- Lactate Dehydrogenase (LD)
- Lactoferrin
- Lactose Tolerance Tests
- LDL Cholesterol
- LDL Particle Testing (LDL-P)
- Legionella Testing
- Levetiracetam
- Lipid Panel
- Lipoprotein (a)
- Liquid Biopsy
- Liver Panel
- Lupus Anticoagulant Testing
- Luteinizing Hormone (LH)
- Lyme Disease Tests
- Lynch Syndrome Genetic Testing
- Marijuana (THC) Testing
- Maternal Serum Screening, Second Trimester
- Measles and Mumps Tests
- Men’s Health Testing
- Metanephrines
- Methotrexate
- Methylmalonic Acid
- Mononucleosis (Mono) Test
- MRSA Screening
- MTHFR Mutation
- Mycophenolic Acid
- Nicotine and Cotinine
- Non-High Density Lipoprotein Cholesterol
- Non-Invasive Prenatal Screening (NIPS)
- Opioid Testing
- Osmolality and Osmolal Gap
- Ova and Parasite Exam
- Pap Smear (Pap Test)
- Parathyroid Hormone (PTH)
- Parietal Cell Antibody
- Partial Thromboplastin Time (PTT, aPTT)
- Parvovirus B19
- Pericardial Fluid Analysis
- Peritoneal Fluid Analysis
- Pharmacogenetic Tests
- Phenobarbital
- Plasma Free Metanephrines
- Platelet Count
- Platelet Function Tests
- Pleural Fluid Testing
- Porphyrin Tests
- Pregnancy Test (hCG)
- Pregnenolone
- Prenatal Group B Strep (GBS) Screening
- Procalcitonin
- Progesterone
- Prostate Specific Antigen (PSA)
- Protein C and Protein S
- Protein Electrophoresis, Immunofixation Electrophoresis
- Prothrombin Time and International Normalized Ratio (PT/INR)
- Red Blood Cell (RBC) Antibody Identification
- Red Blood Cell (RBC) Antibody Screen
- Red Blood Cell Count (RBC)
- Red Cell Indices
- Renal Panel
- Respiratory Pathogens Panel
- Respiratory Syncytial Virus (RSV) Testing
- Reticulocytes
- Rheumatoid Factor (RF)
- Rubella Test
- Salicylates (Aspirin)
- Semen Analysis
- Serum Free Light Chains
- Sex Hormone Binding Globulin (SHBG)
- Shiga toxin-producing Escherichia coli
- Sickle Cell Tests
- Smooth Muscle Antibody (SMA) and F-actin Antibody
- Soluble Mesothelin-Related Peptides
- Soluble Transferrin Receptor
- Sputum Culture, Bacterial
- STD Testing
- Stool Culture
- Stool Elastase
- Strep Throat Test
- Sweat Chloride Test
- Synovial Fluid Analysis
- Syphilis Tests
- T-Cell Receptor Gene Rearrangement
- T3 (Free and Total)
- Tau Protein and Beta Amyloid
- TB Skin Test
- Testosterone
- Theophylline and Caffeine
- Therapeutic Drug Monitoring
- Thiopurine methyltransferase (TPMT)
- Thrombin Time
- Thyroglobulin
- Thyroid Antibodies
- Thyroid Panel
- Thyroid-stimulating Hormone (TSH)
- Total Protein, Albumin-Globulin (A/G) Ratio
- Toxoplasmosis Testing
- Trace Minerals
- Transferrin and Iron-binding Capacity (TIBC, UIBC)
- Trichomonas Testing
- Triglycerides
- Tumor Markers
- Tumor Necrosis Factor (TNF) Inhibitors and TNF Inhibitor Antibodies
- Urine Albumin and Albumin to Creatinine Ratio
- Urine Culture
- Urine Metanephrines
- Urine Protein and Urine Protein to Creatinine Ratio
- Valproic Acid
- Vanillylmandelic Acid (VMA)
- Vitamin B12 and Folate
- Vitamin D Tests
- VLDL Cholesterol
- von Willebrand Factor
- Warfarin Sensitivity Testing
- West Nile Virus Testing
- White Blood Cell (WBC) Differential
- White Blood Cell Count (WBC)
- Whooping Cough (Pertussis) Tests
- Xylose Absorption Test
- Zika Virus Testing
- Zinc Protoporphyrin
- Acidosis and Alkalosis
- Adrenal Insufficiency and Addison Disease
- Alzheimer Disease
- Ankylosing Spondylitis
- Antiphospholipid Syndrome
- Autoimmune Diseases
- Benign Prostatic Hyperplasia
- Bioterrorism Agents
- Bleeding Disorders
- Blood in Urine (Hematuria)
- Bone Marrow Disorders
- Breast Cancer
- Cardiovascular Disease (CVD)
- Celiac Disease
- Cervical Cancer
- Chemical Terrorism Agents
- Chronic Fatigue Syndrome
- Colon Cancer
- Congenital Adrenal Hyperplasia
- Congestive Heart Failure
- Cushing Syndrome
- Cystic Fibrosis
- Deep Vein Thrombosis (DVT)
- Dehydration
- Disseminated Intravascular Coagulation (DIC)
- Down Syndrome
- Ebola Virus Infection
- Endocrine System and Syndromes
- Excessive Clotting Disorders
- Fibromyalgia
- Food and Waterborne Illness
- Fragile X Syndrome
- Fungal Infections
- Gallstones and Gallbladder Disease
- Graves Disease
- Guillain-Barré Syndrome
- Hashimoto Thyroiditis
- Heart Attack and Acute Coronary Syndrome
- Heart Disease
- Hemochromatosis
- Hemoglobin Abnormalities
- HIV Infection and AIDS
- Huntington Disease
- Hypertension
- Hyperthyroidism
- Hypothyroidism
- Infertility
- Inflammatory Bowel Disease
- Insulin Resistance
- Juvenile Rheumatoid Arthritis
- Kidney Disease
- Lactose Intolerance
- Lead Poisoning
- Liver Cancer
- Liver Disease
- Low Platelets
- Low Testosterone in Adult Men
- Lung Cancer
- Lung Diseases
- Lyme Disease
- Lynch Syndrome
- Malabsorption
- Malnutrition
- Meningitis and Encephalitis
- Metabolic Syndrome
- Multiple Myeloma
- Multiple Sclerosis
- Myasthenia Gravis
- Myelodysplastic Syndrome
- Myeloproliferative Neoplasms
- Neural Tube Defects
- Nontuberculous Mycobacteria Infections
- Osteoarthritis
- Osteoporosis
- Ovarian Cancer
- Pancreatic Cancer
- Pancreatic Diseases
- Pancreatic Insufficiency
- Pancreatitis
- Parathyroid Diseases
- Pelvic Inflammatory Disease
- Peptic Ulcer
- Pituitary Disorders
- Polycystic Ovary Syndrome (PCOS)
- Preeclampsia
- Pregnancy: First Trimester (Up to 12 weeks)
- Pregnancy: Preconception
- Pregnancy: Second Trimester (13 to 27 weeks)
- Pregnancy: Third Trimester (28 weeks to delivery)
- Primary Aldosteronism (Conn Syndrome)
- Prostate Cancer
- Protein in Urine (Proteinuria)
- Reactive Arthritis
- Rheumatoid Arthritis
- Sarcoidosis
- Scleroderma
- Septic Arthritis
- Sexually Transmitted Diseases
- Sickle Cell Anemia
- Sjögren Syndrome
- Staph Infections and MRSA
- Testicular Cancer
- Thalassemia
- Thyroid Cancer
- Thyroid Diseases
- Thyroid Nodules
- Travelers' Diseases
- Tuberculosis
- Urinary Tract Infection
- Vaginitis and Vaginosis
- Vitamin B12 and Folate Deficiencies
- Vitamin K Deficiency
- Waldenstrom Macroglobulinemia
- West Nile Virus
- Wilson Disease
- Wound and Skin Infections
- Newborn Screening
- Screening Tests for Infants
- Screening Tests for Children (Ages 2 to 12)
- Screening Tests for Teens (Ages 13-18)
- Screening Tests for Young Adults (Ages 19-29)
- Screening Tests for Adults (Ages 30-49)
- Screening Tests for Adults (50 and Up)
To determine your ABO blood group and Rh type
When you need a transfusion of blood or blood components; when you donate blood at a collection facility or donate an organ, tissue, or bone marrow for transplantation; before or during a woman's pregnancy to determine the risk of Rh incompatibility with the fetus
A sample of blood is drawn from a vein or from the tip of the finger (fingerstick). In newborns, blood from the umbilical cord or a small amount of blood from a heelstick may be used for testing.
You may be able to find your test results on your laboratory's website or patient portal. However, you are currently at Lab Tests Online. You may have been directed here by your lab's website in order to provide you with background information about the test(s) you had performed. You will need to return to your lab's website or portal, or contact your healthcare practitioner in order to obtain your test results.
Lab Tests Online is an award-winning patient education website offering information on laboratory tests. The content on the site, which has been reviewed by laboratory scientists and other medical professionals, provides general explanations of what results might mean for each test listed on the site, such as what a high or low value might suggest to your healthcare practitioner about your health or medical condition.
The reference ranges for your tests can be found on your laboratory report. They are typically found to the right of your results.
If you do not have your lab report, consult your healthcare provider or the laboratory that performed the test(s) to obtain the reference range.
Laboratory test results are not meaningful by themselves. Their meaning comes from comparison to reference ranges. Reference ranges are the values expected for a healthy person. They are sometimes called "normal" values. By comparing your test results with reference values, you and your healthcare provider can see if any of your test results fall outside the range of expected values. Values that are outside expected ranges can provide clues to help identify possible conditions or diseases.
While accuracy of laboratory testing has significantly evolved over the past few decades, some lab-to-lab variability can occur due to differences in testing equipment, chemical reagents, and techniques. This is a reason why so few reference ranges are provided on this site. It is important to know that you must use the range supplied by the laboratory that performed your test to evaluate whether your results are "within normal limits."
For more information, please read the article Reference Ranges and What They Mean .
Blood types are based on the markers (specific carbohydrates or proteins) or antigens on the surface of red blood cells (RBCs) . Two major antigens or surface identifiers on human RBCs are the A and B antigens. Another important surface antigen is called Rh. Blood typing detects the presence or absence of these antigens to determine a person's ABO blood group and Rh type.
People whose red blood cells have A antigens are in blood group A, those with B antigens are group B, those with both A and B antigens are in group AB, and those who do not have either of these markers are in blood group O.
If the Rh protein is present on the red blood cells, a person's blood type is Rh+ (positive); if it is absent, the person's blood is type Rh- (negative).
Our bodies naturally produce antibodies against the A and B antigens that we do not have on our red blood cells. For example, a person who is blood type A will have anti-B antibodies directed against the B antigens on red blood cells and someone who is type B will have anti-A antibodies directed against the A antigens. People with type AB blood have neither of these antibodies, while those with type O blood have both.
The following table indicates the type of antibodies a person is expected to have based on their blood type.
These antibodies are useful for determining a person's blood type and help determine the types of blood that he or she can safely receive (compatibility). If a person who is group A with antibodies directed against the B antigen, for example, were to be transfused with blood that is type B, his or her own antibodies would target and destroy the transfused red blood cells, causing severe, potentially fatal complications. Thus, it is critical to match a person's blood type with the blood that is to be transfused.
Unlike antibodies to A and B antigens, antibodies to Rh are not produced naturally. That is, Rh antibodies develop only after a person who does not have Rh factor on his or her red blood cells (Rh negative) is exposed to Rh positive red blood cells. This can happen during pregnancy or birth when an Rh-negative woman is pregnant with an Rh-positive baby, or sometimes when an Rh-negative person is transfused with Rh-positive blood. In either case, the first exposure to the Rh antigen may not result in a strong response against the Rh positive cells, but subsequent exposures may cause severe reactions.
Blood typing is used to determine an individual's blood group, to establish whether a person is blood group A, B, AB, or O and whether he or she is Rh positive or Rh negative.
Blood typing may be used to:
Similarly, if an Rh-negative individual is transfused with Rh-positive blood, it is likely that the person will produce antibodies against Rh-positive blood. Although this situation does not cause problems for the recipient during the current transfusion, a future transfusion with Rh-positive blood could result in a serious transfusion reaction.
- Determine compatibility between a pregnant woman and her developing baby (fetus). Rh typing is especially important during pregnancy because a mother and her fetus could be incompatible. If the mother is Rh negative but the father is Rh positive, the fetus may be positive for the Rh antigen. As a result, the mother's body could develop antibodies against the Rh antigen. The antibodies may cross the placenta and cause destruction of the baby's red blood cells, resulting in a condition known as hemolytic disease of the fetus and newborn (HDFN) . To prevent development of Rh antibodies, an Rh-negative mother is treated with an injection of Rh immune globulin during her pregnancy and again after delivery if the baby is Rh-positive. The Rh immune globulin binds to and "masks" the fetus's Rh antigen during pregnancy and delivery and prevents the mother from developing antibodies against the Rh antigen.
- Determine the blood group of potential blood donors at a collection facility. Units of blood collected from donors are blood typed and then appropriately labeled so they can be used for people that require a specific ABO group and Rh type.
- Determine the blood group of potential donors and recipients of organs, tissues, or bone marrow , as part of a workup for a transplant procedure. Along with HLA testing , ABO blood typing is used to identify and match organ and tissue transplant donors with recipients who have the same or an acceptable number of matching HLA genes and antigens.
ABO grouping and Rh typing are performed on all donated blood. They are also performed when people require blood transfusion. Conditions or situations that may warrant a transfusion include:
- Severe anemia and conditions causing anemia such as sickle cell disease and thalassemia
- Bleeding during or after surgery
- Injury or trauma
- Excessive blood loss
- Cancer and the effects of chemotherapy
- Bleeding disorders such as hemophilia
Testing is ordered when a woman becomes pregnant to determine whether she is Rh negative or positive. All newborn babies of Rh-negative mothers are typed for ABO and Rh soon after birth to determine if the mother needs to receive Rh immune globulin.
Blood typing may be ordered when a person becomes a candidate for an organ, tissue, or bone marrow transplant, or when a person wishes to become a donor. It is one of the first of many tests used when determining whether a potential donor and recipient are compatible.
Sometimes blood typing may be done as part of the process for determining whether someone could be a blood relative. For more on this, see the article The Universe of Genetic Testing .
The results of blood typing will determine if a person is type A, B, AB, or O and if he or she is Rh negative or positive. The results will tell the healthcare provider what blood or blood components will be safe for the person to receive.
The following table shows what types of blood patients can safely receive, based on their individual blood type.
* These apply for RBC transfusions only; when transfusing plasma products and platelets, the compatible choices are different. (See the article on Transfusion Medicine for more on this.)
Blood typing results will show whether a pregnant woman is Rh positive or negative. This information will indicate whether she may be a candidate for receiving Rh immune globulin, which would prevent her from developing antibodies against her fetus' blood cells.
Typing of donated blood is important because this information allows healthcare practitioners to determine which patients are compatible and can safely receive that blood.
Similarly, when a donor organ, tissue, or bone marrow is compatible with the intended recipient, it is less likely to be rejected in the immediate post-transplant period.
The following table summarizes the approximate distribution of blood groups and types in the U.S. population:
Although Rh incompatibility has more severe consequences, one of the most common causes of hemolytic disease of the fetus and newborn (HDFN) is actually an incompatibility between the mother's and baby's ABO blood groups, not the Rh factor. However, ABO grouping cannot be used to predict whether HDFN will occur because antibodies to the ABO blood groups are naturally occurring.
Besides A and B, many other antigens exist. Having a rare blood type is especially problematic if you need repeated transfusions, as sickle cell anemia and thalassemia patients do. If blood transfusions are not closely matched to blood types of patients, they may suffer transfusion reactions. Such reactions are less likely if donors and recipients are from the same racial or ethnic groups. Molecular testing techniques that analyze a person's genes may be used to predict the presence of unusual or uncommon red cell antigens.
If you need a transfusion, healthcare practitioners at your healthcare facility will determine your blood type before they give you any blood. The only time you would not get a blood type test is in an extreme emergency and there is not enough time to type your blood. In this case, you would receive group O since this blood type does not have any A or B antigens that can potentially cause a hemolytic transfusion reaction. The use of Rh-negative blood depends upon the situation and the supply of O negative blood in the area.
Universal blood donors have type O, Rh negative blood. This means they have no A or B antigens or Rh factor on their red blood cells to which the recipient's antibodies can react. Recipients of their red blood cells have little risk of a hemolytic transfusion reaction due to ABO or Rh incompatibility.
Universal recipients have type AB, Rh positive blood. They recognize A, B and Rh antigens as "self" and can receive red blood cells of any ABO or Rh type with no risk of a serious hemolytic transfusion reaction due to ABO or Rh incompatibility.
Yes, numerous other antigens can be present on the surface of red blood cells. These other RBC blood group antigens include, for example, Kell, Kidd, Duffy, and other Rh antigens. The body does not produce antibodies to these antigens unless it is exposed to these antigens through blood transfusion or during pregnancy. These antibodies are not detected during routine blood typing but may be found with an RBC antibody screen . For more on these antigens and antibodies, see the article on RBC Antibody Identification .
On This Site
Elsewhere on the web.
Sources Used in Current Review
© 2018 AABB. Blood FAQ. Available online at http://www.aabb.org/tm/Pages/bloodfaq.aspx. Accessed October 2018.
© 2018 The American National Red Cross. Understanding Your Blood Type. Available online at https://www.redcrossblood.org/donate-blood/how-to-donate/types-of-blood-donations/blood-types.html. Accessed October 2018.
© 2018 The American National Red Cross. Molecular Testing. Available online at https://www.redcrossblood.org/biomedical-services/blood-diagnostic-testing/molecular-testing.html. Accessed October 2018.
(March 13, 2018) MedlinePlus. Rh Incompatibility. Available online at https://medlineplus.gov/rhincompatibility.html. Accessed October 2018.
Sources Used in Previous Reviews
Pagana, Kathleen D. & Pagana, Timothy J. (© 2006). Mosby's Manual of Diagnostic and Laboratory Test 3rd Edition: Mosby, Elsevier, Saint Louis, MO., Pp. 141-145.
Henry's Clinical Diagnosis and Management by Laboratory Methods. 21st ed. McPherson R, Pincus M, eds. Philadelphia, PA: Saunders Elsevier: 2007, Ch. 34. MedlinePlus Medical Encyclopedia. Blood Typing (Online information, accessed October 2007). Available online at http://www.nlm.nih.gov/medlineplus/ency/article/003345.htm.
(September 2007) National Heart, Lung and Blood Institute. Diseases and Conditions Index: Blood Transfusion (Online information). Available online at http://www.nhlbi.nih.gov/health/dci/Diseases/bt/bt_whatis.html. Accessed November 2007.
(June 2005) Nemours Foundation. Kids Health: What You Need to Know in an Emergency (Online information). Available online at http://kidshealth.org/parent/firstaid_safe/home/healthin.html. Accessed October 2007.
(July 2007) AABB. About Blood and Cellular Therapies: Blood FAQ (Online information). Available online at http://www.aabb.org/Content/About_Blood/FAQ/bloodfaq.htm. Accessed October 2007.
Henry's Clinical Diagnosis and Management by Laboratory Methods. 21st ed. McPherson R, Pincus M, eds. Philadelphia, PA: Saunders Elsevier: 2007, Ch. 34.
(February 5, 2010) MedlinePlus Medical Encyclopedia: Blood Typing (Online information). Available online at http://www.nlm.nih.gov/medlineplus/ency/article/003345.htm. Accessed July 2011.
(July September 20097) National Heart, Lung and Blood Institute. Diseases and Conditions Index. Blood Transfusion (Online information). Available online at http://www.nhlbi.nih.gov/health/dci/Diseases/bt/bt_whatis.html. Accessed July 2011.
(©2011July 2007) AABB. About Blood and Cellular Therapies: Blood FAQ. Available online at http://www.aabb.org/Content/About_Blood/FAQ/bloodfaq.htm. Accessed July 2011.
(©2011) National American Red Cross. Learn About Blood. Available online at http://www.redcrossblood.org/learn-about-blood. Accessed July 2011.
(November 20, 2009) Sandler G. Transfusion Reactions. Medscape Reference. Available online at http://emedicine.medscape.com/article/206885-overview. Accessed July 2011.
(November 4, 2009) Salem L. Rh Incompatibility. Medscape Reference. Available online at http://emedicine.medscape.com/article/797150-overview. Accessed July 2011.
Blood Types. American Red Cross. Available online at http://www.redcrossblood.org/learn-about-blood/blood-types. Copyright 2014. Accessed October 24, 2014.
Testing and Procedures: Blood Transfusion. Mayo Clinic. Available online at http://www.mayoclinic.org/tests-procedures/blood-transfusion/basics/risks/prc-20021256. Last updated April 26, 2012. Accessed October 24, 2014.
Rare Donor Program. Lifeshare Blood Centers. Available online at http://www.lifeshare.org/services/rare-donor-program. Copyright 2014. Accessed October 27, 2014.
Blood Types: Distribution Stats, Interesting Facts. Blood Banker. Available online at http://bloodbanker.com/plasma/plasma-donation/blood-donation-terms/. Accessed October 28, 2014.
(Updated Oct 29, 2014) Gonsorcik V. ABO Grouping. Medscape Reference. Available online at http://emedicine.medscape.com/article/1731198-overview. Accessed October 2014.
(Updated Nov 6, 2013) Gonsorcik V. Rh Typing. Medscape Reference. Available online at http://emedicine.medscape.com/article/1731214-overview. Accessed October 2014.
Ask a Laboratory Scientist
This form enables patients to ask specific questions about lab tests. Your questions will be answered by a laboratory scientist as part of a voluntary service provided by one of our partners, American Society for Clinical Laboratory Science. Please allow 2-3 business days for an email response from one of the volunteers on the Consumer Information Response Team.

- B & T Cells - Clonk's Home Page
- The Immune System in More Detail from Nobelprize.org
- The Immune Response Animation from McGraw-Hill
- Antigenic Determinants (Epitopes) Animation from McGraw-Hill
- Lab Exercise Instructions
- Lab Report Assignment
- Links to images related to the lab
- Additional articles and links that support the lecture material
- Lab #6 : Leukocytes, Antibodies & Blood Typing Lab Exercise INSTRUCTIONS
- Lab #6 : Leukocytes, Antibodies & Blood Typing Lab Report ASSIGNMENT
- Get Started
Learning Lab Collections
- Collections
- Assignments
My Learning Lab:
Forgot my password.
Please provide your account's email address and we will e-mail you instructions to reset your password. For assistance changing the password for a child account, please contact us
You are about to leave Smithsonian Learning Lab.
Your browser is not compatible with site. do you still want to continue.

IMAGES
VIDEO
COMMENTS
Obtain 3 toothpicks per blood slide, use a different color per each well to avoid cross. contamination. Stir each well for 30 seconds. To avoid splattering the simulated blood, do not press too. hard on the typing tray. Let it sit for 2 minutes. Observe each well against a white paper and record the results on the ABO/Rh blood; typing worksheet.
Method: To conduct this lab, we took steps as listed below. 1. Label each blood typing slide: Slide #1: Mr. Smith, Slide #2: Mr. Jones, Slide #3: Mr. Green, Slide #4: Ms. Brown 2. Place three to four drops of Mr. Smith's blood in each of the A, B, and Rh wells of Slide #1 3. Repeat step 2 with Mr. Jones's blood in slide #2 4.
Blood typing lab report part 2 Name: G00971778, G00986239, G01027289, G00661166 Lab: Blood typing Due date:10/26/2020 Purpose The purpose of this lab report is to conclude the blood type as well as if the patient is RH positive or negative. Introduction The human species has 4 different blood types, scientists have categorized them into 4 individual categories, A, B, AB, O.We predict that the ...
A person with type AB blood has. A and B antigens and neither anti-A nor anti-B antibodies. A person with A+ blood has. anti-B antibodies. Rh antigen on the surface of the red blood cells. the A antigen on the surface of the red blood cells. Blood type A- would give which of the following results?
The ABO Blood Group. A and B antigens are glycoproteins on the RCC surface. ABO typing does not affect a person's Rh (+ or -) designation. Figure 2.3 Blood Type. Type A blood: A antigens on cell; anti-B antibodies in plasma. Type B blood: B antigens on cell; anti-A antibodies in plasma. Type AB blood: both A and B antigens on cell; neither ...
This page titled 3.1: Blood Typing Lab is shared under a CC BY-NC 4.0 license and was authored, remixed, and/or curated by Katherine E. Brent & Sydney Quinn Chizmeshya via source content that was edited to the style and standards of the LibreTexts platform; a detailed edit history is available upon request.
Blood typing is performed using "antiserum" - blood that contains specific antibodies. "Anti-A Serum," which contains anti-A antibodies, and "Anti-B Serum," which contains anti-B antibodies, are used in ABO blood typing. To perform a blood typing test, anti-A and anti-B sera are each separately mixed with a drop of sample blood and
Blood types are based on the markers (specific carbohydrates or proteins) or antigens on the surface of red blood cells (RBCs). Two major antigens or surface identifiers on human RBCs are the A and B antigens. Another important surface antigen is called Rh. Blood typing detects the presence or absence of these antigens to determine a person's ...
This is the main page for the Immunology Laboratory Topic of an 8-week introductory college microbiology class. This lab introduces students to leukocytes, antibodies how ABO Rh blood typing works. ADDITIONAL REQUIRED READINGS & ANIMATED LESSONS. The Immunology Lab materials of the Virtual Microbiology Classroom include: IMMUNOLOGY LAB DOCUMENTS.
Lab 2: Blood Typing - Lab Report Brian Melly Lab Partner: Katie Flynn 2/10/20 2. Basic outline and purpose of the laboratory activities. An antigen is a toxin or foreign body that induces an immune response. An antibody is a blood protein that is produced in response to a specific antigen.
The "Bufffy coat" consists of. white blood cells and platelets. White blood cell and platelets make up how much of a centrifuged blood sample. less than 1%. The most abundant WBC in the blood. neutrophil. The least common WBC in the blood. basophil. Study with Quizlet and memorize flashcards containing terms like mature red blood cells are also ...
View Lab - lab report blood typing from BSC 2086C at Florida State College at Jacksonville. BSC 2086C: Anatomy and Physiology II Adil Louski Lab 1: Blood Typing Purpose The purpose of this lab was to ... Assignment 1.docx. Intro to Computing Subject Guide Vol.2.pdf. Datacenter edition of Windows Server 2016 You plan to deploy the following guest.
Q-Chat. valeriegarcia06. Top creator on Quizlet. Study with Quizlet and memorize flashcards containing terms like blood typing is the result of what?, hemagglutination, lab objective and more.
Blood Typing Assignment Lab Report - Copy.docx. San Jacinto Community College. ANATOMY 2302. BLOOD TYPING LAB REPORT.docx. Molloy College. BIO 121. Blood Typing Laboratory Report. Triton College. BIS 241. lab. 4. ABO Rh Blood Typing lab report.pdf. Solutions Available. CUNY College of Staten Island. BIO 150.
Upon completion of this lab exercise students will be able to: Describe the composition of blood plasma . Identify the five types of leukocyte s typically seen in human blood and perform a differential . white blood cell count . Safely obtain a sample of blood by finger-stick to measure hematocrit and determine ABO and . Rh blood types
Fetal anemia. What blood types are dominant & what blood types are recessive? - Dominant: A, B, Rh+. - Recessive: O, Rh-. Agglutination chart. Study with Quizlet and memorize flashcards containing terms like 4 major blood types, 8 blood types, Serum and more.
View Lab - Blood Typing Laboratory Report from BIS 241 at Triton College. Blood Typing Laboratory Report I. Statement of Purpose A. ... Blood Typing Assignment Lab Report - Copy.docx. San Jacinto Community College. ANATOMY 2302. BIOL251 Lab Report 2 York.docx. American Public University. BIOL 251. lab. AP2 Lab 5 Exam Study Guide.pdf. Solutions ...
Blood type activity. Published and Created by: Christine Hunt. 0 Favorites 1 Copy (view) Science Age Levels High School (16 to 18 years old) Discover the importance of knowing about blood groups and how antigens can be used in blood typing. Included is an activity which determines the possible perpetrator of a "crime". Discover the importance ...