Case Study 1: A 55-Year-Old Woman With Progressive Cognitive, Perceptual, and Motor Impairments
Information & authors, metrics & citations, view options, case presentation, what are diagnostic considerations based on the history how might a clinical examination help to narrow the differential diagnosis.
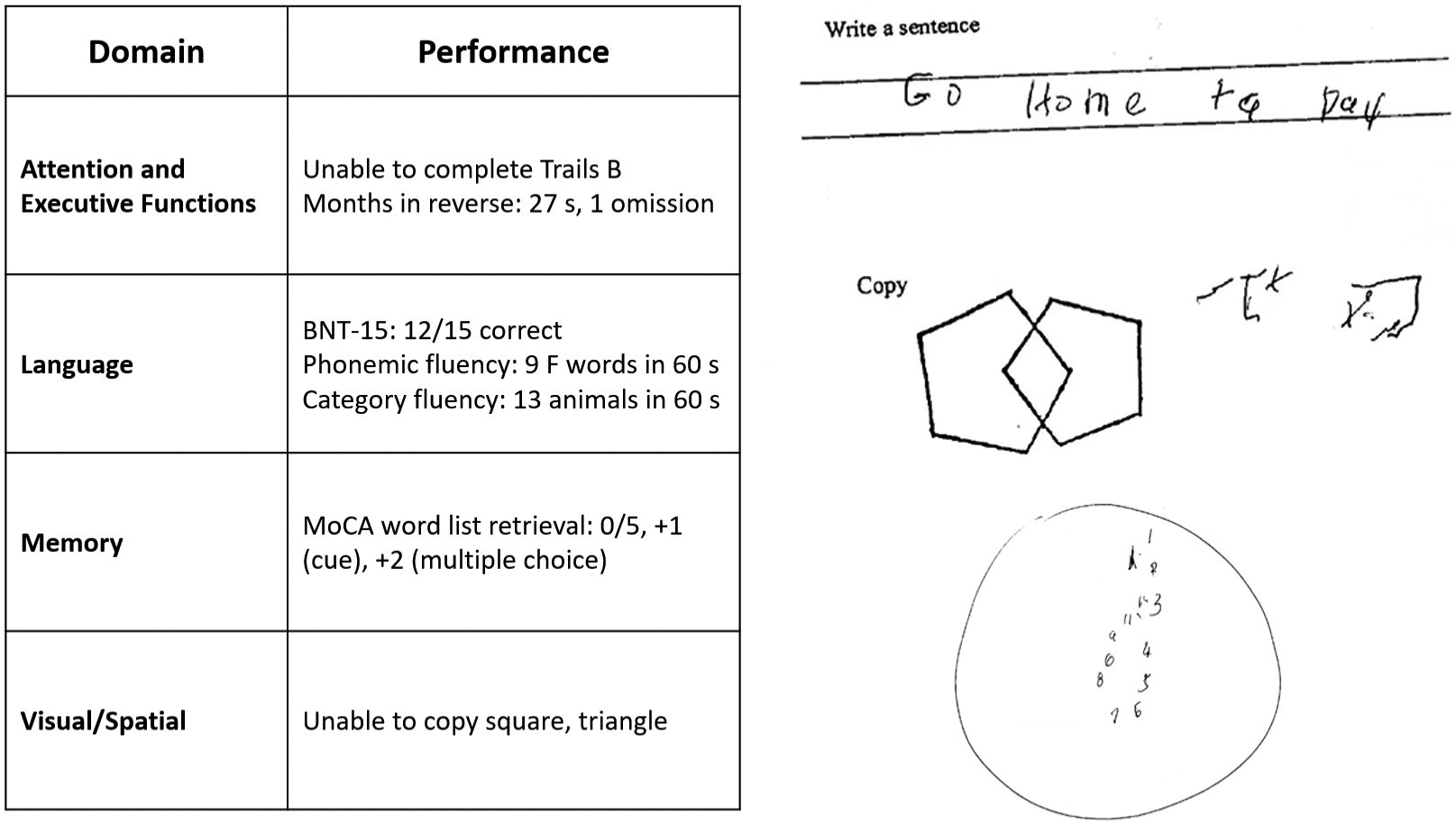

How Does the Examination Contribute to Our Understanding of Diagnostic Considerations? What Additional Tests or Studies Are Indicated?
| Feature | Posterior cortical atrophy | Corticobasal syndrome |
|---|---|---|
| Cognitive and motor features | Visual-perceptual: space perception deficit, simultanagnosia, object perception deficit, environmental agnosia, alexia, apperceptive prosopagnosia, and homonymous visual field defect | Motor: limb rigidity or akinesia, limb dystonia, and limb myoclonus |
| Visual-motor: constructional dyspraxia, oculomotor apraxia, optic ataxia, and dressing apraxia | ||
| Other: left/right disorientation, acalculia, limb apraxia, agraphia, and finger agnosia | Higher cortical features: limb or orobuccal apraxia, cortical sensory deficit, and alien limb phenomena | |
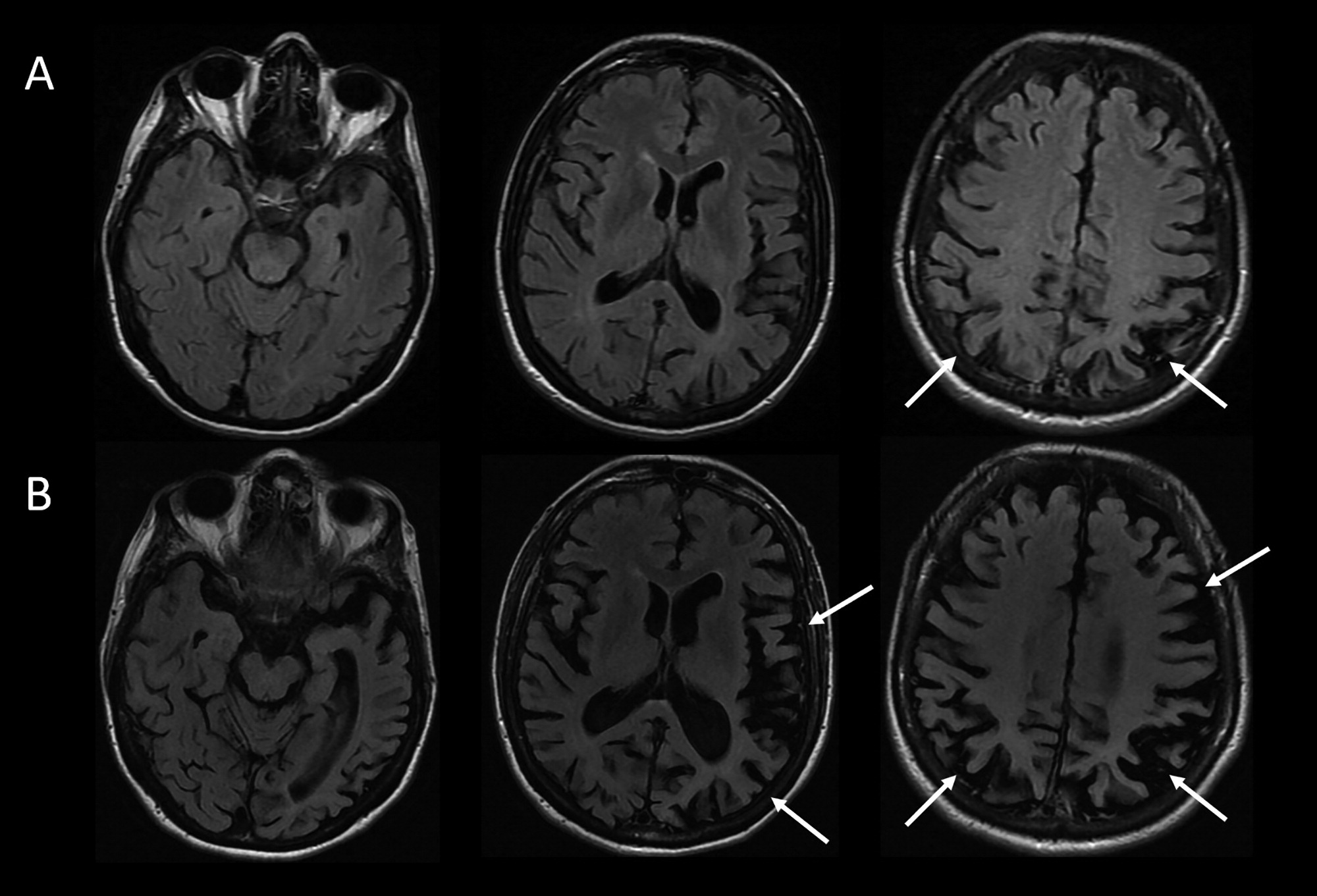
| Imaging features (MRI, FDG-PET, SPECT) | Predominant occipito-parietal or occipito-temporal atrophy, and hypometabolism or hypoperfusion | Asymmetric perirolandic, posterior frontal, parietal atrophy, and hypometabolism or hypoperfusion |
| Neuropathological associations | AD>CBD, LBD, TDP, JCD | CBD>PSP, AD, TDP |
Considering This Additional Data, What Would Be an Appropriate Diagnostic Formulation?
Does information about the longitudinal course of her illness alter the formulation about the most likely underlying neuropathological process, neuropathology.
| Feature | Case of PCA/CBS due to AD | Exemplar case of CBD |
|---|---|---|
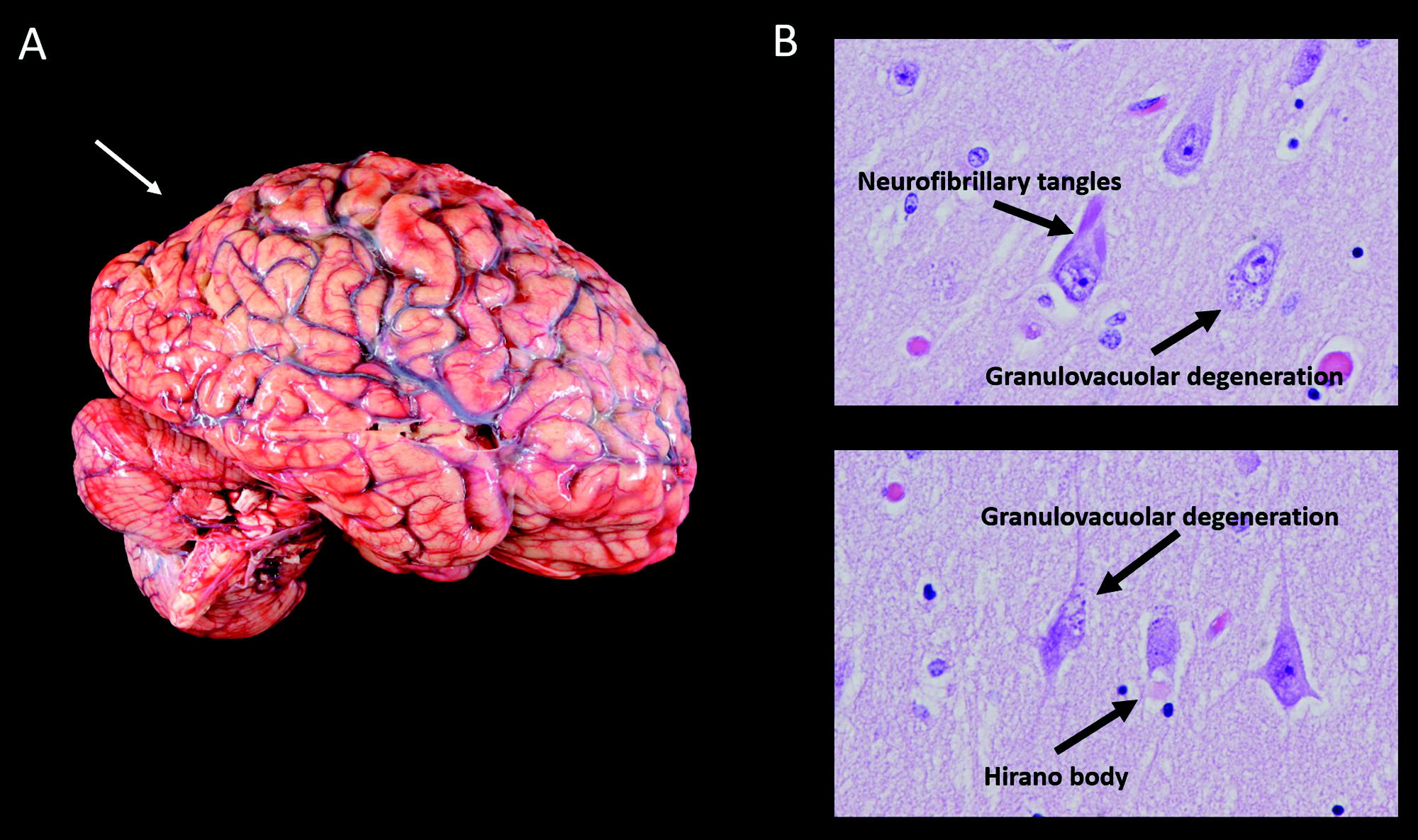
| Macroscopic findings | Cortical atrophy: symmetric, mild | Cortical atrophy: often asymmetric, predominantly affecting perirolandic cortex |
| Substantia nigra: appropriately pigmented | Substantia nigra: severely depigmented | |
| Microscopic findings | Tau neurofibrillary tangles and beta-amyloid plaques | Primary tauopathy |
| No tau pathology in white matter | Tau pathology involves white matter | |
| Hirano bodies, granulovacuolar degeneration | Ballooned neurons, astrocytic plaques, and oligodendroglial coiled bodies | |
| (Lewy bodies, limbic) |
Information
Published in.
- Posterior Cortical Atrophy
- Corticobasal Syndrome
- Atypical Alzheimer Disease
- Network Degeneration
Competing Interests
Funding information, export citations.
If you have the appropriate software installed, you can download article citation data to the citation manager of your choice. Simply select your manager software from the list below and click Download. For more information or tips please see 'Downloading to a citation manager' in the Help menu .
| Format | |
|---|---|
| Citation style | |
| Style | |
To download the citation to this article, select your reference manager software.
There are no citations for this item
View options
Login options.
Already a subscriber? Access your subscription through your login credentials or your institution for full access to this article.
Purchase Options
Purchase this article to access the full text.
PPV Articles - Journal of Neuropsychiatry and Clinical Neurosciences
Not a subscriber?
Subscribe Now / Learn More
PsychiatryOnline subscription options offer access to the DSM-5-TR ® library, books, journals, CME, and patient resources. This all-in-one virtual library provides psychiatrists and mental health professionals with key resources for diagnosis, treatment, research, and professional development.
Need more help? PsychiatryOnline Customer Service may be reached by emailing [email protected] or by calling 800-368-5777 (in the U.S.) or 703-907-7322 (outside the U.S.).
Share article link
Copying failed.
PREVIOUS ARTICLE
Next article, request username.
Can't sign in? Forgot your username? Enter your email address below and we will send you your username
If the address matches an existing account you will receive an email with instructions to retrieve your username
Create a new account
Change password, password changed successfully.
Your password has been changed
Reset password
Can't sign in? Forgot your password?
Enter your email address below and we will send you the reset instructions
If the address matches an existing account you will receive an email with instructions to reset your password.
Your Phone has been verified
As described within the American Psychiatric Association (APA)'s Privacy Policy and Terms of Use , this website utilizes cookies, including for the purpose of offering an optimal online experience and services tailored to your preferences. Please read the entire Privacy Policy and Terms of Use. By closing this message, browsing this website, continuing the navigation, or otherwise continuing to use the APA's websites, you confirm that you understand and accept the terms of the Privacy Policy and Terms of Use, including the utilization of cookies.

Snapsolve any problem by taking a picture. Try it in the Numerade app?
Winningham's Critical Thinking Cases in Nursing
Barbara a preusser, julie s snyder, mariann m harding, patients with multiple disorders - all with video answers.
Section 136
Name Class/Group Date Group Members INSTRUCTIONS All questions apply to this case study. Your responses should be brief and to the point. When asked to provide several answers, list them in order of priority or significance. Do not assume information that is not provided. Please print or write clearly. If your response is not legible, it will be marked as ? and you will need to rewrite it.
As you perform your initial assessment, you note superficial partial-thickness burns on A.N.'s right anterior leg, left anterior and posterior leg, and anterior torso. Shade the affected areas, then using the “rule of nines,” calculate the extent of A.N.'s burn injury.

Because you are concerned about possible smoke inhalation, what signs will you monitor A.N. for?

Interpret A.N.'s laboratory results.
A.N. is undergoing burn fluid resuscitation using the standard Baxter (Parkland) formula. She was admitted at 0400. She weighs 110 pounds. Calculate her fluid requirements, specify the fluids used in the Baxter (Parkland) formula, specify how much will be given, and indicate what time intervals will be used.

A.N. is in severe pain. What is the drug of choice for pain relief following burn injury, and how should it be given?

Because of her significant burn injury, A.N. is at high risk for infection. What measures will you institute to prevent this?
A.N.'s burns are to be treated by the open method with topical application of silver sulfadiazine (Silvadene). When caring for A.N., which interventions will you perform? (Select all that apply.) a. Maintain the room temperature at 85° F (29.4° C). b. Use clean technique when changing A.N.'s dressings. c. Monitor CBC frequently, particularly the white blood cells. d. Do not allow her to bathe for the initial 72 hours following injury. e. Apply a 1 ?16-inch film of medication, covering entire burn. f. Shave all hair within the wound beds.
A.N. has one area of circumferential burns on her right lower leg. What complication is she in danger of developing, and how will you monitor for it?
What interventions will facilitate maintaining A.N.'s peripheral tissue perfusion?
A special burn diet is ordered for A.N. She has always gained weight easily and is concerned about the size of the portions. What diet-related teaching will you provide?

Describe interventions that you could use to assist in meeting A.N.'s nutrition goals.

Case Examples
Examples of recommended interventions in the treatment of depression across the lifespan.

Children/Adolescents
A 15-year-old Puerto Rican female
The adolescent was previously diagnosed with major depressive disorder and treated intermittently with supportive psychotherapy and antidepressants. Her more recent episodes related to her parents’ marital problems and her academic/social difficulties at school. She was treated using cognitive-behavioral therapy (CBT).
Chafey, M.I.J., Bernal, G., & Rossello, J. (2009). Clinical Case Study: CBT for Depression in A Puerto Rican Adolescent. Challenges and Variability in Treatment Response. Depression and Anxiety , 26, 98-103. https://doi.org/10.1002/da.20457
Sam, a 15-year-old adolescent
Sam was team captain of his soccer team, but an unexpected fight with another teammate prompted his parents to meet with a clinical psychologist. Sam was diagnosed with major depressive disorder after showing an increase in symptoms over the previous three months. Several recent challenges in his family and romantic life led the therapist to recommend interpersonal psychotherapy for adolescents (IPT-A).
Hall, E.B., & Mufson, L. (2009). Interpersonal Psychotherapy for Depressed Adolescents (IPT-A): A Case Illustration. Journal of Clinical Child & Adolescent Psychology, 38 (4), 582-593. https://doi.org/10.1080/15374410902976338
© Society of Clinical Child and Adolescent Psychology (Div. 53) APA, https://sccap53.org/, reprinted by permission of Taylor & Francis Ltd, http://www.tandfonline.com on behalf of the Society of Clinical Child and Adolescent Psychology (Div. 53) APA.
General Adults
Mark, a 43-year-old male
Mark had a history of depression and sought treatment after his second marriage ended. His depression was characterized as being “controlled by a pattern of interpersonal avoidance.” The behavior/activation therapist asked Mark to complete an activity record to help steer the treatment sessions.
Dimidjian, S., Martell, C.R., Addis, M.E., & Herman-Dunn, R. (2008). Chapter 8: Behavioral activation for depression. In D.H. Barlow (Ed.) Clinical handbook of psychological disorders: A step-by-step treatment manual (4th ed., pp. 343-362). New York: Guilford Press.
Reprinted with permission from Guilford Press.
Denise, a 59-year-old widow
Denise is described as having “nonchronic depression” which appeared most recently at the onset of her husband’s diagnosis with brain cancer. Her symptoms were loneliness, difficulty coping with daily life, and sadness. Treatment included filling out a weekly activity log and identifying/reconstructing automatic thoughts.
Young, J.E., Rygh, J.L., Weinberger, A.D., & Beck, A.T. (2008). Chapter 6: Cognitive therapy for depression. In D.H. Barlow (Ed.) Clinical handbook of psychological disorders: A step-by-step treatment manual (4th ed., pp. 278-287). New York, NY: Guilford Press.
Nancy, a 25-year-old single, white female
Nancy described herself as being “trapped by her relationships.” Her intake interview confirmed symptoms of major depressive disorder and the clinician recommended cognitive-behavioral therapy.
Persons, J.B., Davidson, J. & Tompkins, M.A. (2001). A Case Example: Nancy. In Essential Components of Cognitive-Behavior Therapy For Depression (pp. 205-242). Washington, D.C.: American Psychological Association. http://dx.doi.org/10.1037/10389-007
While APA owns the rights to this text, some exhibits are property of the San Francisco Bay Area Center for Cognitive Therapy, which has granted the APA permission for use.
Luke, a 34-year-old male graduate student
Luke is described as having treatment-resistant depression and while not suicidal, hoped that a fatal illness would take his life or that he would just disappear. His treatment involved mindfulness-based cognitive therapy, which helps participants become aware of and recharacterize their overwhelming negative thoughts. It involves regular practice of mindfulness techniques and exercises as one component of therapy.
Sipe, W.E.B., & Eisendrath, S.J. (2014). Chapter 3 — Mindfulness-Based Cognitive Therapy For Treatment-Resistant Depression. In R.A. Baer (Ed.), Mindfulness-Based Treatment Approaches (2nd ed., pp. 66-70). San Diego: Academic Press.
Reprinted with permission from Elsevier.
Sara, a 35-year-old married female
Sara was referred to treatment after having a stillbirth. Sara showed symptoms of grief, or complicated bereavement, and was diagnosed with major depression, recurrent. The clinician recommended interpersonal psychotherapy (IPT) for a duration of 12 weeks.
Bleiberg, K.L., & Markowitz, J.C. (2008). Chapter 7: Interpersonal psychotherapy for depression. In D.H. Barlow (Ed.) Clinical handbook of psychological disorders: a treatment manual (4th ed., pp. 315-323). New York, NY: Guilford Press.
Peggy, a 52-year-old white, Italian-American widow
Peggy had a history of chronic depression, which flared during her husband’s illness and ultimate death. Guilt was a driving factor of her depressive symptoms, which lasted six months after his death. The clinician treated Peggy with psychodynamic therapy over a period of two years.
Bishop, J., & Lane , R.C. (2003). Psychodynamic Treatment of a Case of Grief Superimposed On Melancholia. Clinical Case Studies , 2(1), 3-19. https://doi.org/10.1177/1534650102239085
Several case examples of supportive therapy
Winston, A., Rosenthal, R.N., & Pinsker, H. (2004). Introduction to Supportive Psychotherapy . Arlington, VA : American Psychiatric Publishing.
Older Adults
Several case examples of interpersonal psychotherapy & pharmacotherapy
Miller, M. D., Wolfson, L., Frank, E., Cornes, C., Silberman, R., Ehrenpreis, L.…Reynolds, C. F., III. (1998). Using Interpersonal Psychotherapy (IPT) in a Combined Psychotherapy/Medication Research Protocol with Depressed Elders: A Descriptive Report With Case Vignettes. Journal of Psychotherapy Practice and Research , 7(1), 47-55.
- Research article
- Open access
- Published: 27 June 2016
A case series of 223 patients with depersonalization-derealization syndrome
- Matthias Michal 1 ,
- Julia Adler 1 ,
- Jörg Wiltink 1 ,
- Iris Reiner 1 ,
- Regine Tschan 1 ,
- Klaus Wölfling 1 ,
- Sabine Weimert 1 ,
- Inka Tuin 1 ,
- Claudia Subic-Wrana 1 ,
- Manfred E. Beutel 1 &
- Rüdiger Zwerenz 1
BMC Psychiatry volume 16 , Article number: 203 ( 2016 ) Cite this article
42k Accesses
41 Citations
15 Altmetric
Metrics details
Depersonalization-derealization syndrome (DDS) is an underdiagnosed and underresearched clinical phenomenon. In Germany, its administrative prevalence is far below the threshold for orphan diseases, although according to epidemiological surveys the diagnosis should be comparable frequent as anorexia nervosa for instance. Against this background, we carried out a large comprehensive survey of a DDS series in a tertiary mental health center with a specialized depersonalization-derealization clinic. To reveal differential characteristics, we compared the DDS patients, who consulted the specialized depersonalization-derealization clinic, with a group of patients with depressive disorders without comorbid DDS from the regular outpatient clinic of the mental health center.
The sample comprised 223 patients with a diagnosis of depersonalization-derealization-syndrome and 1129 patients with a depressive disorder but without a comorbid diagnosis of DDS. DDS patients were described and compared with depressive outpatients in terms of sociodemographic characteristics, treatment history, treatment wishes, clinical symptomatology, prevailing psychosocial stressors, family history of common mental disorders and history of childhood trauma.
Despite the high comorbidity of DDS patients with depressive disorders and comparable burden with symptoms of depression and anxiety, the clinical picture and course of both patient groups differed strongly. DDS patients were younger, had a significant preponderance of male sex, longer disease duration and an earlier age of onset, a higher education but were more often unemployed. They tended to show more severe functional impairment. They had higher rates of previous or current mental health care utilization. Nearly all DDS patients endorsed the wish for a symptom specific counseling and 70.7 % were interested in the internet-based treatment of their problems. DDS patients had lower levels of self-rated traumatic childhood experiences and current psychosocial stressors. However, they reported a family history of anxiety disorders more often.
In consideration of the selection bias of this study, this case series supports the view that the course of the DDS tends to be long-lasting. DDS patients are severely impaired, utilizing mental health care to a high degree, which nevertheless might not meet their treatment needs, as patients strongly opt for obtaining disorder specific counseling. In view of the size of the problem, more research on the disorder, its course and its optimal treatment is urgently required.
Depersonalization-derealization syndrome as named in the ICD-10 [ 1 ] (or depersonalization-derealization disorder as termed in the DSM-5 [ 2 ] is an underresearched clinical phenomenon [ 3 , 4 ]. Depersonalization-derealization syndrome (DDS) is defined by feeling detached from the own feelings and/or experiences (depersonalization, DP) and/or experiencing objects, people, and/or surroundings as unreal, distant, artificial, and lifeless (derealization, DR) while reality testing remains intact (ICD-10 [ 1 ]). Further, symptoms of depersonalization and derealization are not better explained by another mental disorder or medical condition and the symptoms cause significant impairment (DSM-5 [ 2 ]). The typical DDS patient, reports that the disorder started before age 25, and that the DP/DR symptoms are present all day long since several years [ 5 – 7 ]. Epidemiological surveys suggest that the current prevalence rate of the depersonalization-derealization syndrome is approximately 1 % in the general population [ 5 – 7 ]. However, the disorder is severely underdiagnosed. For example, in the year 2006 the administrative 1-year-prevalence of the ICD-10 diagnosis “depersonalization-derealization syndrome” was as low as 0.007 % according to the registry of a statutory health insurance fund in Germany [ 4 ]. Experts assume this huge diagnostic gap is due to the following reasons: Many clinicians are unfamiliar with the clinical picture and the diagnostic criteria of the disorder. They universally consider symptoms of DP/DR as secondary to a depressive or anxiety disorder, even if these symptoms are all day long present for months and years, or they even misinterpret these symptoms as psychotic although patients are free from any psychotic sings (such as hallucinations, delusions, severe thought disorders, catatonia etc.) [ 3 – 5 , 8 – 10 ]. Moreover, diagnostic awareness is hampered by the patients themselves because many of them are “reluctant to divulge their symptoms out of fears of being thought mad” [ 8 ]. Therefore, it usually takes many years from the initial contact with a mental health service until the right diagnosis is made [ 3 , 4 , 11 ].
The current nosological knowledge about the DDS, as it is reported in the recent version of the DSM-5, is largely based on historic descriptions of the disorder, small case-control studies and two descriptive case series with a total sum of 321 patients from specialized clinics or research units in London (UK) and New York (USA). Concerning the etiology of DDS, it has been found that harm-avoidant temperament was associated with DDS in a cross-sectional study [ 12 ]. Another cross-sectional study comparing healthy controls with 49 DDS patients demonstrated that emotional abuse was associated with severity of DP/DR but not severe forms of childhood maltreatment [ 13 ]. A prospective cohort study found that the only risk factor for severe adult depersonalization at the age of 36 was teacher-estimated childhood anxiety 20 years before. Exposition to environmental risk factors such as socio-economic status, parental death or divorce, and self-reported accidents did not predict later DDS [ 14 ]. From an evolutionary perspective, symptoms of DP/DR are considered as a hard-wired response to severe stress, which is perpetuated according to various disease models of DDS by personality factors such as low capacities of self-regulation (e.g., low self-esteem, low affect tolerance, low cohesiveness of the self) [ 3 , 8 , 15 ]. Previous case series from specialized treatment units in London (UK) and New York (USA) reported a sex ratio of 1:1 or even a slight male preponderance [ 6 ], with an early age of onset usually before age 25, and a high comorbidity with anxiety and depressive disorders [ 6 , 16 ]. Both case series demonstrated that the condition had a high chronicity and tended to be resistant to pharmacological and psychotherapeutic treatments [ 6 , 16 ]. To date, there is no approved medication for the treatment of DDS and there is no randomized controlled trial on the psychotherapeutic treatment of DDS [ 3 ].
As the current disease knowledge of DDS has only a small empirical basis, at least as compared to mental disorders with similar prevalence rates and mental health impact, the principle aim of our study was to support and extend the knowledge about the clinical features of the DDS. For that purpose, we examined a large consecutive outpatient sample of DDS patients from the depersonalization-derealization clinic of our department, which has been established in 2005. Patients usually become aware of the clinic by online research about their main complaints (e.g. “feeling unreal”), they are usually self-referred and they typically seek a second opinion regarding their diagnoses and treatment options.
With our study we aimed to address two main questions. Firstly, we sought to describe the typical clinical features and demographic characteristics of patients with DDS as depicted in our clinical standard assessment. Although our case series study is primarily meant as a descriptive study, we included a comparison group form our outpatient clinic in order to bring out the putative differential characteristics of the DDS patients more clearly. For the latter purpose we used a large comparison group of patients suffering from depression without comorbid DDS. We compared both groups in terms of sociodemographic characteristics, treatment history, treatment wishes, clinical symptomatology, level of disability, prevailing psychosocial stressors, family history of common mental disorders, and severity of childhood trauma. We choose a sample of depressed patients for comparison for several reasons: First, this diagnostic entity represents the largest diagnostic group in our department. Second, depression is the most prevalent comorbid condition of DDS patients [ 6 ]. Third, depression is a well described and popular disorder thus making it easier for clinicians to acknowledge the similar and differential features of the two groups.
We expected that our case series will constitute an important confirmation and extension of the two previous case series and that it will stimulate further studies on the course, mechanisms and treatment of the disorder.
We consecutively included outpatients between January 2010 and December 2013, who consulted the Department of Psychosomatic Medicine and Psychotherapy of the University Medical Center Mainz (Germany). In Germany, Departments of Psychosomatic Medicine and Psychotherapy, usually established at most of all University Medical Centers, are mainly treating patients with depressive disorders, anxiety disorders, somatoform disorders and eating disorders. All patients received a routine psychometric assessment and a clinical interview.
DDS patients who consulted the depersonalization-derealization clinic usually become aware of the clinic by internet research, that is to say, almost all were self-referred. The website of the clinic gives a vivid description of the symptoms and the clinical picture of the disorder. Further, all patients had a short telephone interview with M.M. prior to their consultation, to ensure that they suffer from severe depersonalization/derealization (e.g. as opposed to DP/DR attacks in the context of panic disorder) and to inform them about the focus of the consultation and the therapeutic options of the clinic. Patients from all over Germany were consulting the specialized clinic.
Patients from the comparison group were either self-referred or referred by local physicians and psychotherapist to receive a psychotherapeutic evaluation and treatment recommendations (usually regarding outpatient psychotherapy, inpatient or day clinic psychotherapy). The catchment area of the department is the Rhine-Main-area.
Patients who were treated in the context of the consultation and liaison service (e.g. cancer patients in cancer care units), or who were below age 18 or who had no standardized assessment, or who had no depressive disorder or DDS were excluded.
The sample comprised 223 patients with a definite diagnosis of depersonalization-derealization-syndrome (ICD-10: F48.1 [ 1 ]) and 1129 patients with a depressive disorder (dysthymia F34.1, or unipolar depression F32.x, or F33.x [ 1 ]) but without a comorbid diagnosis of DDS. The latter group will be indicated below as the “Only-Depressed-Group” (ODG). A total of 197 of the 223 patients diagnosed with DDS consulted the depersonalization-derealization clinic of the Department of Psychosomatic Medicine and Psychotherapy of the University Medical Center Mainz, the remaining 26 patients were diagnosed and treated in the general outpatient unit.
Clinical interview
All patients received a full clinical interview of at least 50 min duration by a psychological or medical psychotherapist. Clinical diagnoses of mental disorders were based on the diagnostic criteria for research of the ICD-10 [ 1 ]. The focus of the clinical interview was on the primary presenting problems of the patients and symptom diagnoses. The diagnosis of depersonalization-derealization syndrome was only given, if symptoms of DP/DR were persistent and lasted continuously for at least 1 month and if these symptoms were not better explained by another mental disorder (e.g., unipolar depression, dissociative disorder, anxiety disorder, PTSD) or a medical condition (e.g., seizure disorder). Although the diagnostic criteria of the DDS do not demand specifications about the duration of the symptoms, most clinicians agree that the diagnosis should be only given if the symptoms persist for at least 1 month [ 3 ] (see Additional file 1 for comprehensive information about the diagnostic procedure).
Due to the peculiarities of the clinical interview, personality disorders were underreported in our medical records. This was mainly due to the time restriction of the clinical interview. As each patient received a written report about the diagnostic findings, each diagnosis in the record had to be explained to the patient in advance. The diagnosis of personality disorders was rarely made, as most clinicians believed that informing adequately about the diagnosis of a personality disorder requires more time. Because of this bias of underdiagnosing personality disorders in our records, we did not consider personality disorders in this paper.
Further, clinicians rated the social, occupational, and psychological functioning level of psychological functioning by means of the Global Assessment of Functioning (GAF) scale [ 17 , 18 ]. Lower scores indicate lower levels of functioning. Scores in the range of 51–60 indicate moderate impairment due to symptoms (e.g., flat affect and circumlocutory speech, occasional panic attacks) or moderate difficulty in social, occupational, or school functioning (e.g., few friends, conflicts with peers or co-workers). In Germany, patients with indication for inpatient psychotherapy usually have a current functional level below GAF 50 [ 19 ].
Severity of DP/DR was assessed with the CDS-2, the two-item version of the Cambridge Depersonalization Scale (CDS [ 20 , 21 ]). The CDS-2 comprises the following two items of the CDS [ 22 ]: “My surroundings feel detached or unreal, as if there was a veil between me and the outside world” and “Out of the blue, I feel strange, as if I were not real or as if I were cut off from the world”. The response format of the CDS-2 was adopted from the Patient Health Questionnaire (“Over the last 2 weeks, how often have you been bothered by any of the following problems?/Not at all = 0/Several days = 1/More than half the days = 2/Nearly every day = 3”). The CDS-2 showed high reliability (Cronbach’s Alpha = 0.92) and was able to differentiate patients with clinically significant DP well from other groups (cut-off of CDS-2 ≥ 3, sensitivity = 78.9 %, specificity = 85.7 %). The CDS-2 sum score (range 0–6) correlated strongly ( r = 0.77 [ 22 ]) with depersonalization severity according to a structured clinical interview of depersonalization severity [ 23 ]. Immediately after the CDS-2 items, the patient questionnaire presented the following two questions with a yes/no response: Have you ever consulted a doctor or psychotherapist because of the above symptoms? Do you wish counseling about the above symptoms of depersonalization and derealization?
Severity of depression was measured with the depression module PHQ-9 of the Patient Health Questionnaire [ 24 ]. PHQ-9 scores ≥ 10 identified depressive disorders with a sensitivity of 81 % and a specificity of 82 %. Severity of anxiety was measured with the Generalized Anxiety Disorder-7 (GAD-7). The GAD-7 has seven items depicting various signs of generalized and other anxiety disorders (e.g. PTSD, panic disorder). GAD-7 scores range from 0 to 21, with scores of ≥5, ≥10, and ≥15 representing mild, moderate, and severe anxiety symptom levels [ 25 , 26 ]. The Mini-Social Phobia Inventory (Mini-Spin; [ 27 ]) was used for the measurement of social anxiety. The Mini-Spin has three items, which are rated on a 5-point-Likert scale from 0 = “not at all” to 4 = “extremely”. A cut-off score of 6 (range 0–12) separates individuals with social anxiety disorder from controls with good sensitivity (89 %) and specificity (90 %). Somatic symptoms severity was assessed with the 15 items of the PHQ-15. Scores range between 0–30. Scores above 15 identify individuals with high levels of somatic symptom severity respectively somatization severity [ 28 ]. The overall mental distress level was measured by the Global Severity Index (GSI) of the German version of the short Symptom Check List (SCL-9) [ 29 ]. The range of the GSI is 0 to 4 with higher values reflecting more dysfunction. The ten most common psychosocial stressors (e.g., financial status, family relationships, work, health) were assessed by the corresponding PHQ module on a three-point scale (not bothered = 0, bothered a little =1, bothered a lot =2) [ 30 , 31 ]. We also calculated the sum score of psychosocial stressors (possible range from 0 to 20). Further, we dichotomized the items (“not bothered” or “little bothered” = 0 versus bothered “a lot” = 1) for the use in a regression analysis. The Childhood Trauma Questionnaire (CTQ) is a 28-item self-report inventory for the assessment of the extent of traumatic childhood experiences. The CTQ has a global score and scores for the subscales emotional abuse, physical abuse, sexual abuse, emotional neglect, physical neglect and minimization [ 32 ]. For determining clinically significant levels of traumatization critically cut-points for the subscales have been determined [ 33 , 34 ]: emotional neglect (≥15), sexual abuse (≥8), physical abuse (≥8), physical neglect (≥10), emotional abuse (≥10). Further, patients gave written information about their socioeconomic details, their treatment history and family history.
Statistical analysis
Data were presented as mean ± standard deviation, or age and sex adjusted mean, standard error and 95 % confidence interval, or numbers (n) and percentage. Continuous distributed scores were compared by students T -test. Categorical variables were compared by Chi-square tests. Associations of continuous data were tested by Pearson correlations. Correlations coefficients of the two groups were compared by the Fisher r-to-z transformation, which controls the correlation coefficients for the effect of different sample sizes. In order to control group differences for the effects of age and sex, we applied logistic regression analyses for binary variables and analysis of covariance (ANCOVA) for continuous variables. In order to evaluate the distinctiveness of the symptom dimensions depression, anxiety, social anxiety and DP/DR we performed a principal component analysis with varimax rotation on the pooled items of the CDS-2, PHQ-9, GAD-7 and Mini-Spin. Tests were considered to be significant at a p < 0.05, and all significance tests were two-tailed. Due to the large sample size, the interpretation of the results should focus on effect-sizes rather than p -values. SPSS 22.0 was used for the main statistical analysis and VassarStats for the Fisher r-to-z transformation ( http://vassarstats.net ).
Sociodemographic characteristics
Table 1 shows the sociodemographic characteristics of the sample. The group of DDS patients was of younger age and more often male than the “Only-Depressed-Group” (ODG). There was a significant preponderance of men in the DDS group with a female-to-male ratio of 98 to 125 (≈2 : 3). The DDS patients were living less often in a current partnership, were more often still living with their parents, more often holder of the German citizenship, had a higher educational level, but were more often unemployed.
Comorbid conditions, symptom burden and clinical course
DDS patients had a very high comorbidity with depressive disorders (84.8 %). As compared with ODG, DDS patients had a higher comorbidity with anxiety disorders, whereas somatoform disorders and PTSD were more prevalent in the ODG. The DDS group had more clinical Axis-I disorders than the controls (2.8 ± 1.0 versus 2.3 ± 1.1, T = 6.920, p < 0.0001). Only 21 from 223 DDS-patients (9.4 %) had no comorbid Axis-I disorder. DDS patients had an earlier age of onset and longer disease duration as the ODG (Table 2 ). DDS had its onset in 63.7 % ≤ age 25, in 17.9 % between age 26 and ≤ 40 and in 4.9 % > 40. There was no valid information about the age of onset for 20 DDS patients.
Table 3 shows that after adjustment for age and sex, DDS patients were comparably bothered like the ODG by symptoms of depression (PHQ-9) and anxiety (GAD-7), and they had a similar global severity index (GSI). They had a lower burden with somatic symptoms (PHQ-15) and a slightly lower severity of social anxiety (Mini-Spin). However, severity of depersonalization (CDS-2) strongly separated both patient groups.
In order to evaluate the distinctiveness of the scales we performed a principal component analysis with varimax rotation on the pooled items of the CDS-2, PHQ-9, GAD-7 and Mini-Spin. The Factors were retained in the model based on inspection of the screeplot and eigenvalues > 1. Five factors were identified explaining 61 % of the variance. The items of the CDS-2 were clearly separated from the other scales (data not presented, see Additional file 2 ). Regarding the association of DP/DR with other symptom dimensions we found that the correlation coefficients of the severity of depersonalization (CDS-2) with anxiety (GAD-7, Mini-Spin), depression, general distress (GSI) and somatization were significantly weaker in the DDS group (Table 4 ).
Functional impairment
Both patient groups were markedly impaired by their symptoms (Table 5 ). After adjustment for age and sex, DDS patients endorsed that their symptoms disrupted their work and social life more strongly than ODG, while the impairment of home life was comparable. These differences were in the range of small to medium effect sizes (Cohen’s d 0.24 to 0.28). Clinicians rated the current and 1-year global level of functioning (GAF) of DDS patients significantly lower than those of the ODG. The difference of GAF was in the range of large effect sizes (Cohen’s d 0.54 to 0.67). Overall, the mean GAF of both groups was in the range of serious to moderate impairment of psychological, social and occupational functioning (GAF 50-60). In the DDS group, 35.2 % had a GAF below 50 which, in Germany, is considered as a criterion for inpatient psychotherapy.
Current psychosocial stressors
Overall, DDS patients endorsed being less bothered by psychosocial stressors than the ODG (Table 6 ). In the sex and age adjusted logistic regression model the following stressors were inversely associated with DDS: weight or appearance worries, difficulties with partners, stress at work or school, financial worries, having no one to turn to, as well as recent or past bad events. The same picture emerged regarding the total burden with psychosocial stressors (i.e. the sum score of the scale): 7.7 ± 3.6 in the DDS group versus 9.7 ± 4.0 in the ODG (T = 7.34, p < 0.0001). In the DDS group, there was no correlation between the severity of psychosocial stressors with severity of depersonalization (Pearson correlation between the psychosocial stressor sum score and CDS-2: r = 0.06, p = 0.39). In the ODG, however, CDS-2 correlated significantly with the sum of psychosocial stressors ( r = 0.31, p < 0.0001). The correlations coefficients differed significantly (Fisher r-to-z transformation: z = 3.53, p = 0.0004).
Family history and childhood adversities
In the age and sex adjusted regression analysis, only a FH of any anxiety disorder was significantly associated with DDS (Table 7 ). Regarding childhood adversities, DDS patients showed a similar level of traumatic childhood experiences; only, they endorsed slightly lower levels of physical and sexual abuse than ODG in the age and sex adjusted ANCOVA. Overall, the mean level of traumatic childhood experiences was in the range of minimal to low levels of traumatic childhood experiences (Table 8 ). Based on the critical cut-points of the CTQ [ 33 , 34 ], DDS patients reported the following rates of clinically significant levels of traumatization: Emotional abuse 44.7 %, emotional neglect 35.8 %, physical abuse 12.3 %, physical neglect 15.1 %, and sexual abuse 6.1 %. Altogether, 57.8 % of the DDS patients reported at least one significant traumatic childhood experience and 42.2 % none. In the DDS group, there was no association between severity of childhood traumatic experiences with severity of depersonalization (Pearson correlation of the CTQ total score with CDS-2: r = 0.05, p = 0.44). In the ODG, although weakly, CDS-2 correlated with the CTQ total score ( r = 0.20, p < 0.0001). The correlations coefficients of the two groups differed significantly (Fisher r-to-z transformation, z = 2.07, p = 0.0385).
Treatment history and health care wishes
Overall, DDS had a high treatment rate (Table 9 ). In the age and sex adjusted regression analysis, previous psychiatric inpatient treatment was much more likely in DDS patients than in the comparison group. The vast majority of the DDS patients endorsed firstly that they had previously consulted a doctor or psychotherapist because of DP/DR symptoms (92.7 % ( n = 202) versus 25.3 % ( n = 494)), and secondly that they were interested in DP/DR specific counseling (97.3 % ( n = 213) versus 35.0 % ( n = 446)). Those individuals of the ODG, who endorsed the wish for a DP/DR specific counseling, had higher CDS-2 scores than those denying this question (3.1 ± 1.9 versus 0.9 ± 1.3, T = 20.2, p < 0.0001). Further, DDS patients more often used the internet for searching information about their symptoms and specialists and were much more interested in internet-based treatment approaches.
We investigated a consecutive sample of 223 DDS-patients, who consulted a specialized depersonalization-derealization clinic and compared these patients with a large group of patients with depressive disorders. At the time of the consultation, DDS patients were of younger age, had a significant preponderance of male sex, longer disease duration, an earlier age of onset, and a higher education but they were more often unemployed. Their burden with symptoms of depression and anxiety was comparable, however, they tended to show more severe functional impairment, especially at work/school and in social life. Concerning health care utilization, DDS patients had extraordinary high rates of previous inpatient treatments during the last 12 months (25.6 %) and ongoing outpatient psychotherapy (40.4 %). Despite their high health care utilization, nearly all DDS patients endorsed the wish for a symptom specific counseling (92.7 %) and 70.7 % were interested in an internet-based treatment approach of their problems. With regard to risk factors, DDS patients tended to report lower levels of self-rated traumatic childhood experiences and current psychosocial stressors. However, they more often reported a family history of anxiety disorders. These findings both enhance and extend those of two earlier case series from other countries and health care systems reported by Simeon et al. ([ 16 ]) and Baker et al. ([ 6 ]).
Very similar to the London case series by Baker et al. ([ 6 ]), we found a preponderance of men (125 men to 98 women; Baker et al.: 112 men to 92 women [ 6 ]) and almost the same mean age of onset of 22.9 ± 9.7 years (22.8 ± 11.9 years [ 6 ]). A similar preponderance of male sex has been recently found for clinically significant DP/DR in a representative questionnaire based survey of pupils in the age of 12 to 18 after adjustment for general distress [ 35 ]. The determinants of this putative sex difference in the etiology of DDS warrant further research.
Compared with previous case series, we had a higher proportion of DDS patients reporting an age of onset > 25 years (22.8 %). This finding needs replication, because previous reports assumed that an onset after age of 25 is very rare (less than 5 %) [ 6 , 16 ]. The larger proportion of DDS patients with a late age of onset in our sample may reflect the increasing use of the internet for health research since 2003, as nearly all DDS patients were referred by themselves or “Dr. Google” respectively.
Similar to Simeon et al. ([ 16 ]) and Baker et al. ([ 6 ]) the main comorbid conditions were depressive and anxiety disorders. In the current sample only 9.4 % of the DDS in the current sample had no comorbid Axis-I disorder which is very close to 11 % in the case series of Simeon et al. [ 16 ]. Despite their high comorbidity and equal symptom burden with symptoms of depression and anxiety, the clinical picture and course of both patient groups differed strongly regarding sociodemographic variables, treatment history and treatment wishes, and risk factors. Again, a principal component analysis substantiated clearly the distinctiveness of DP/DR symptoms from anxiety and depression [ 36 ], thus contradicting a commonly held view that symptoms of DP/DR are only a negligible variant of depression and anxiety. The low correlation coefficients of depression or anxiety with DP/DR severity in the DDS group are pointing in the same direction. The much stronger correlation coefficients in the group of the only depressed patients might constitute one reason why many clinicians generally tend to lump together DP/DR symptoms with depression and anxiety. Concerning somatic symptoms severity, DDS patients endorsed significantly less somatic symptoms as compared to the controls. This is in accordance with a recent study, which found that DDS patients endorsed less bodily symptoms of anxiety than pure anxiety patients [ 37 ]. The lower burden by bodily symptoms may reflect DDS patients’ detachment from their body.
Although 57.8 % of the DDS patients reported at least one clinically significant traumatic childhood experience, the overall rate of childhood adversities was rather low among DDS patients and even lower than in the comparison group. In line with previous studies [ 6 , 13 , 14 ] this finding makes it unlikely that traumatic childhood experiences play a crucial role in the etiology of DDS. This highlights an apparent contradiction: Although symptoms of DP/DR are typically reactions to severe stress and trauma (e.g. in the case of PTSD [ 38 ]), DDS is usually not associated with severe forms of childhood traumatization or recent traumatic events. This suggests that for the development of DDS other factors play a superior role as compared to the exposition to severe traumatic events.
There was a high rate of a parental history of anxiety disorders in the DDS group. Akin to the findings of Baker et al. ([ 6 ]), DDS patients had a high rate of psychiatric disorders in a first degree relative (Baker et al.: 30 %; 35.8 % in this sample). This may point to an increased genetic vulnerability of the DDS group on the one hand and on the other hand to an increased environmental risk of being exposed to parents with anxiety disorders [ 39 ].
DDS patients endorsed that they were significantly less bothered by current psychosocial stressors than only depressed patients. This either indicates that they have less psychosocial stressors or that they tend to be less aware how psychosocial factors affect them. The latter interpretation would correspond to our clinical experience. Similar to patients with somatoform disorders, DDS patients initially are often unable to consider psychological problems and interpersonal conflicts as relevant causes, and they are convinced by a physical causation of their symptoms [ 3 ]. Frequently patients assume a brain tumor, an eye disease or drug induced brain damage as the cause of their symptoms and thus initially consult neurologists, ophthalmologists and other somatic specialists before visiting a mental health specialist [ 5 , 40 ]. The lack of any correlation between the severity of DP/DR symptoms with the level of current or past stressors might be interpreted in the same way. Severe depersonalization may constitute a “ceiling” effect, which prevents the patients from seeing relations between stressors and their maladaptive stress-response in form of DP/DR. This reminds strongly to a recent study of 291 DDS patients, which found that despite comparable high levels of anxiety, depersonalization and anxiety correlated only in patients with less severe symptoms of DP/DR but not in patients with very high levels of DP/DR [ 41 ]. That is to say, therapeutic progress would implicate that patients become aware how the DP/DR symptoms wax and wane depending on the level of the mobilized anxieties [ 3 ]. However, in order to test this hypothesis, a longitudinal investigation of these relationships would be necessary.
Making the above considerations, the following major limitations have to be kept in mind. First, our approach implicated a strong selection bias: The DDS-patients were mostly referred by themselves after they have searched the internet for their main complaints, while the comparison group represents patients largely from the near catchment area. This limits the generalizability of our results. For example, we cannot rule out that only DDS patients with a chronic course, poor satisfaction with their current treatment and poor treatment response consulted the depersonalization-derealization clinic of our department. A further bias may constitute the high educational level of the DDS patients. This high educational level could explain the high rate of self-referral among DDS patients coming to a specialized DDS clinic. Highly educated persons may have lower barriers to use the internet for information about health issues. However, the findings concerning chronicity and the high rate of previous health care utilization corresponded well with previous reports from the specialized units in London [ 6 ] and New York [ 16 ]. Secondly, the diagnoses were based on clinical interviews and not on structured clinical interviews as applied in research settings, thus limiting the validity of our diagnoses. However, diagnoses were enhanced by using the diagnostic research criteria of the ICD-10 and by the correlation of the findings with validated rating scales. Thirdly, family history of mental disorders and history of previous treatments was questionnaire based and not corroborated by independent sources.
Conclusions
Keeping the above limitations in mind, we found that DDS patients are severely impaired, are utilizing mental health care to a high degree, which nevertheless might not meet their treatment needs, as the patients are taking strong efforts for obtaining symptom specific counseling. This all may reflect the fact that many clinicians are not familiar with the diagnostic features of DDS and its treatment [ 3 ]. In Germany, a first step towards the improvement of DDS care may constitute the implementation of the guideline recommendations for the diagnosis and treatment of the depersonalization-derealization syndrome, which have been recently published by the Association of the Scientific Medical Societies in Germany [ 42 ]. In view of the size of the problem, much more research on the disorder, its course and its optimal treatment is urgently required.
Abbreviations
ANCOVA, analysis of covariance; CDS-2, 2-item scale of the Cambridge Depersonalization Scale; CTQ, Childhood Trauma Questionnaire; DDS, Depersonalization-derealization syndrome; DP, depersonalization; DR, derealization; DSM-5, 5th edition of the Diagnostic and Statistical Manual of Mental Disorders; FH, family history; GAD-7, Generalized Anxiety Disorder 7-item scale; GAF, Global Assessment of Functioning; GSI, Global Severity Index; Mini-Spin, Mini-Social Phobia Inventory; OGD, Only-Depressed-Group; OR, odds ratio; PHQ-15, Somatic symptom scale from Patient Health Questionnaire; PHQ-9, depression module of the Patient Health Questionnaire; PTSD, Posttraumatic Stress Disorder; SD, standard deviation; SDS, Sheehan Disability Scale; SE, standard error.
WHO. The ICD-10 classification of mental and behavioural disorders: Diagnostic criteria for research. Geneva: World Health Organization; 1993.
Google Scholar
American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders: DSM-5. Washington: American Psychiatric Publishing, Inc.; 2013.
Book Google Scholar
Simeon D: Depersonalization/Derealization Disorder. In Gabbard’s Treatments of Psychiatric Disorders . 5th edition. Edited by Gabbard GO. Washington, DC: American Psychiatric Publishing Inc.; 2014: 459-469.
Michal M, Beutel M, Grobe T. Wie oft wird die Depersonalisations-Derealisationsstörung (ICD-10: F48.1) in der ambulanten Versorgung diagnostiziert? Z Psychosom Med Psychother. 2010;56:74–83.
PubMed Google Scholar
Simeon D, Abugel J. Feeling Unreal: Depersonalization Disorder and the Loss of the Self. Oxford: Oxford University Press; 2006.
Baker D, Hunter E, Lawrence E, Medford N, Patel M, Senior C, Sierra M, Lambert MV, Phillips ML, David AS. Depersonalisation disorder: clinical features of 204 cases. Br J Psychiatry. 2003;182:428–33.
Article PubMed Google Scholar
Medford N, Sierra M, Baker D, David AS. Understanding and treating depersonalisation disorder. Adv Psychiatr Treat. 2005;11:92–100.
Article Google Scholar
Sierra M. Depersonalization: A New Look at a Neglected Syndrome. Cambridge: Cambridge University Press; 2009.
Michal M, Tavlaridou I, Subic-Wrana C, Beutel ME. Fear of going mad - differentiating between neurotic depersonalization-derealization-syndrome and paranoid schizophrenia. Nervenheilkunde. 2012;31:934–7.
Simon AE, Umbricht D, Lang UE, Borgwardt S. Declining transition rates to psychosis: the role of diagnostic spectra and symptom overlaps in individuals with attenuated psychosis syndrome. Schizophr Res. 2014;159:292–8.
Hunter EC, Phillips ML, Chalder T, Sierra M, David AS. Depersonalisation disorder: a cognitive-behavioural conceptualisation. Behav Res Ther. 2003;41:1451–67.
Article CAS PubMed Google Scholar
Simeon D, Guralnik O, Knutelska M, Schmeidler J. Personality factors associated with dissociation: temperament, defenses, and cognitive schemata. Am J Psychiatry. 2002;159:489–91.
Simeon D, Guralnik O, Schmeidler J, Sirof B, Knutelska M. The role of childhood interpersonal trauma in depersonalization disorder. Am J Psychiatry. 2001;158:1027–33.
Lee WE, Kwok CH, Hunter EC, Richards M, David AS. Prevalence and childhood antecedents of depersonalization syndrome in a UK birth cohort. Soc Psychiatry Psychiatr Epidemiol. 2012;47:253–61.
Michal M, Kaufhold J, Overbeck G, Grabhorn R. Narcissistic regulation of the self and interpersonal problems in depersonalized patients. Psychopathology. 2006;39:192–8.
Simeon D, Knutelska M, Nelson D, Guralnik O. Feeling unreal: a depersonalization disorder update of 117 cases. J Clin Psychiatry. 2003;64:990–7.
Saß H, Wittchen H, Zaudig M. Diagnostisches und Statistisches Manual psychischer Störungen: DSM- IV. Göttingen: Hogrefe; 1996.
Hilsenroth MJ, Ackerman SJ, Blagys MD, Baumann BD, Baity MR, Smith SR, et al. Reliability and validity of DSM-IV axis V. Am J Psychiatry. 2000;157:1858–63.
Huber D, Brandl T, Henrich G, Klug G. Ambulant oder stationär? Psychotherapeut. 2002;47:16–23.
Sierra M, Berrios GE. The Cambridge Depersonalization Scale: a new instrument for the measurement of depersonalization. Psychiatry Res. 2000;93:153–64.
Michal M, Sann U, Niebecker M, Lazanowsky C, Kernhof K, Aurich S, Overbeck G, Sierra M, Berrios GE. Die Erfassung des Depersonalisations-Derealisations-Syndroms mit der Deutschen Version der Cambridge Depersonalisation Scale (CDS). Psychother Psychosom Med Psychol. 2004;54:367–74.
Michal M, Zwerenz R, Tschan R, Edinger J, Lichy M, Knebel A, Tuin I, Beutel M. Screening for depersonalization-derealization with two items of the cambridge depersonalization scale. Psychother Psychosom Med Psychol. 2010;60:175–9.
Simeon D, Guralnik O, Schmeidler J. Development of a depersonalization severity scale. J Trauma Stress. 2001;14:341–9.
Löwe B, Kroenke K, Herzog W, Gräfe K. Measuring depression outcome with a brief self-report instrument: sensitivity to change of the Patient Health Questionnaire (PHQ-9). J Affect Disord. 2004;81:61–6.
Löwe B, Decker O, Muller S, Brahler E, Schellberg D, Herzog W, Herzberg PY. Validation and standardization of the Generalized Anxiety Disorder Screener (GAD-7) in the general population. Med Care. 2008;46:266–74.
Spitzer RL, Kroenke K, Williams JBW, Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. 2006;166:1092–7.
Connor KM, Kobak KA, Churchill LE, Katzelnick D, Davidson JR. Mini-SPIN: A brief screening assessment for generalized social anxiety disorder. Depress Anxiety. 2001;14:137–40.
Kroenke K, Spitzer RL, Williams JB, Lowe B. The Patient Health Questionnaire Somatic, Anxiety, and Depressive Symptom Scales: a systematic review. Gen Hosp Psychiatry. 2010;32:345–59.
Prinz U, Nutzinger DO, Schulz H, Petermann F, Braukhaus C, Andreas S. Comparative psychometric analyses of the SCL-90-R and its short versions in patients with affective disorders. BMC Psychiatry. 2013;13:104.
Article PubMed PubMed Central Google Scholar
Klapow J, Kroenke K, Horton T, Schmidt S, Spitzer R, Williams JB. Psychological disorders and distress in older primary care patients: a comparison of older and younger samples. Psychosom Med. 2002;64:635–43.
Spitzer RL, Kroenke K, Williams JB. Validation and utility of a self-report version of PRIME-MD: the PHQ primary care study. Primary Care Evaluation of Mental Disorders. Patient Health Questionnaire. JAMA. 1999;282:1737–44.
Bernstein DP, Fink L. Childhood trauma questionnaire: A retrospective self-report: Manual. San Antonio: Psychological Corporation; 1998.
Walker EA, Unutzer J, Rutter C, Gelfand A, Saunders K, VonKorff M, Koss MP, Katon W. Costs of health care use by women HMO members with a history of childhood abuse and neglect. Arch Gen Psychiatry. 1999;56:609–13.
Subic-Wrana C, Tschan R, Michal M, Zwerenz R, Beutel M, Wiltink J. Kindheitstraumatisierungen, psychische Beschwerden und Diagnosen bei Patienten in einer psychosomatischen Universitätsambulanz [Childhood trauma and its relation to diagnoses and psychic complaints in patients of an psychosomatic university ambulance]. Psychother Psychosom Med Psychol. 2011;61:54–61.
Michal M, Duven E, Giralt S, Dreier M, Müller K, Adler J, Beutel M, Wölfling K. Prevalence and correlates of depersonalization in students aged 12–18 years in Germany. Soc Psychiatry Psychiatr Epidemiol. 2015;50:995–1003.
Michal M, Wiltink J, Till Y, Wild PS, Blettner M, Beutel ME. Distinctiveness and overlap of depersonalization with anxiety and depression in a community sample: results from the Gutenberg Heart Study. Psychiatry Res. 2011;188:264–8.
Nestler S, Jay EL, Sierra M, David AS. Symptom Profiles in Depersonalization and Anxiety Disorders: An Analysis of the Beck Anxiety Inventory. Psychopathology. 2015;48:84–90.
Lanius RA. Trauma-related dissociation and altered states of consciousness: a call for clinical, treatment, and neuroscience research. Eur J Psychotraumatol. 2015;6:27905.
Rutter M, Quinton D. Parental psychiatric disorder: effects on children. Psychol Med. 1984;14:853–80.
Michal M, Lüchtenberg M, Overbeck G, Fronius M. Gestörte visuelle Wahrnehmung beim Depersonalisations-Derealisationssyndrom [Visual Distortions and Depersonalization-Derealization Syndrome]. Klin Monatsbl Augenheilkd. 2006;223:279–84.
Sierra M, Medford N, Wyatt G, David AS. Depersonalization disorder and anxiety: a special relationship? Psychiatry Res. 2012;197:123–7.
Deutsche Gesellschaft für Psychosomatische Medizin und Ärztliche Psychotherapie (DGPM), Deutsches Kollegium für Psychosomatische-Medizin-(DKPM), Deutsche Gesellschaft für Psychiatrie, Psychotherapie, Psychosomatik und Nervenheilkunde (DGPPN), Deutsche Psychoanalytische Vereinigung (DPV), Deutsche Gesellschaft für Verhaltenstherapie (DGVT), Deutsche Gesellschaft für Psychologie (DGPs): Leitlinie: Diagnostik und Behandlung des Depersonalisations-Derealisationssyndroms, Version 1.0 September 2014. AWMF Registernummer 051 - 030. Access http://www.awmf.org/leitlinien/detail/ll/051-030.html . Accessed 1 Feb 2015.
Download references
Acknowledgement
The authors thank Jasmin Schlax for her help with drafting the revisions of the manuscript.
Not applicable.
Availability of the data and materials
The authors confirm that, for approved reasons, access restrictions apply to the data underlying the findings. Due to ethical restrictions, the data cannot be made publicly available (approval of the Ethics Committee of the State Board of Physicians of Rhineland-Palatinate, Mainz, Germany ((837.191.16 (10510)).
Authors’ contributions
MM wrote the first version of the Manuscript; MM, RZ, JW, SW, MEB made the statistical analysis, MM, JA, JW, IR, RT, KW, IT, CS-W, MEB, RZ were involved in the clinical assessment of the patients, all authors contributed substantially to the conception of the study; all authors revised the manuscript critically and all authors gave their approval of the final version of the manuscript.
Competing interests
The authors declare that they have no competing interests.
Consent for publication
Ethics approval and consent to participate.
The study was approved by the Ethics Committee of the State Board of Physicians of Rhineland-Palatinate, Mainz, Germany ((837.191.16 (10510)). According to the approval of the Ethics Committee, there was no need for written consent because the study analyzed clinical data obtained by clinical standard assessment (i.e., not within the context of an epidemiological or clinical study).
Author information
Authors and affiliations.
Department of Psychosomatic Medicine and Psychotherapy, University Medical Center Mainz, Mainz, Germany
Matthias Michal, Julia Adler, Jörg Wiltink, Iris Reiner, Regine Tschan, Klaus Wölfling, Sabine Weimert, Inka Tuin, Claudia Subic-Wrana, Manfred E. Beutel & Rüdiger Zwerenz
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Matthias Michal .

Additional files
Additional file 1:.
Additional information about the diagnostic procedure. (DOC 37 kb)
Additional file 2:
Principal component analysis with varimax rotation of the items of the CDS-2, PHQ-9, GAD-7 and Mini-Spin. (DOCX 21 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License ( http://creativecommons.org/licenses/by/4.0/ ), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated.
Reprints and permissions
About this article
Cite this article.
Michal, M., Adler, J., Wiltink, J. et al. A case series of 223 patients with depersonalization-derealization syndrome. BMC Psychiatry 16 , 203 (2016). https://doi.org/10.1186/s12888-016-0908-4
Download citation
Received : 26 February 2015
Accepted : 20 June 2016
Published : 27 June 2016
DOI : https://doi.org/10.1186/s12888-016-0908-4
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Depersonalization
- Derealization
- Health care utilization
- Childhood trauma
- Parental history of mental disorders
BMC Psychiatry
ISSN: 1471-244X
- General enquiries: [email protected]
- ASH Foundation
- Log in or create an account
- Publications
- Diversity Equity and Inclusion
- Global Initiatives
- Resources for Hematology Fellows
- American Society of Hematology
- Hematopoiesis Case Studies
Case Study: A 78-Year-Old Man With Elevated Leukocytes and Anemia
- Agenda for Nematology Research
- Precision Medicine
- Genome Editing and Gene Therapy
- Immunologic Treatment
- Research Support and Funding
The following case study focuses on finding the optimal treatment for a 78-year-old man. Test your knowledge by reading the question below and making the proper selection.
A 78-year-old man presents with a three-year history of an elevated leukocyte count with recent fatigue and anemia. He has received two red blood cell transfusions in the past two months. His past medical history includes coronary artery disease and hypertension. His physical examination is unremarkable. The patient’s white blood cell (WBC) count is 75,000/uL, hemoglobin is 9.3 g/dL, and platelet count is 71,000/uL with a WBC differential including 60 percent neutrophils, 19 percent lymphocytes, 15 percent monocytes, and 6 percent eosinophils. His bone marrow aspirate shows mild erythroid dysplasia, 1 percent blasts with an increase in monocytes (14 percent) and eosinophils (7 percent). Chromosomal analysis demonstrates 46XY, t(5;12)(q33;p13)[16]; 46,XY[4]. Fluorescence in situ hybridization (FISH) testing for the BCR-ABL translocation and quantitative RT-PCR for the BCR-ABL transcript were both negative. What is the optimal treatment for this patient?
- Decitabine (Dacogen) 20 mg/m 2 daily x five days per month for three months and then re-examine the bone marrow
- Continued observation until further disease progression
- Imatinib (Gleevec) 400 mg once daily
- Standard induction chemotherapy with daunorubicin (50 mg/m 2 daily x three days) and Ara-C (100 mg/m 2 continuous infusion x seven days)
Explanation
Chronic myelomonocytic leukemia (CMML) is considered to be a clonal myeloid stem cell disorder. 1-3 In 2001, the World Health Organization (WHO) classified CMML as a myelodysplastic-myeloproliferative disease with diagnostic criteria including: 1) persistent peripheral blood (PB) monocyte count >1X109/L; 2) absence of the Philadelphia chromosome; 3) < 20 percent blasts in the PB or bone marrow (BM); and 4) dysplasia in one or more hematopoietic cell lineages. 2,3 The subcategory of CMML with eosinophilia was also established and is characterized by a PB eosinophilia of >1500 cells/uL.
Translocation (5;12)(q31-q33;p12-p13) is a recurring cytogenetic abnormality reported in patients with CMML, in particular those with eosinophilia. 4 The t(5;12) translocation results in the fusion of the transmembrane and tyrosine kinase domains of the platelet-derived growth factor receptor-B ( PDGFR-B ) gene on chromosome 5 with the amino-terminal domain of the TEL/ETV6 gene of chromosome 12, a member of the ETS family of transcription factors. 5,6 The resultant aberrant tyrosine kinase activity of this hybrid protein is potentially the transforming event in these cases of CMML. 7-9 The overall incidence of t(5;12) in CMML is unknown but is presumed to be relatively rare. A retrospective analysis by Gunby, et al. demonstrated the translocation in only 1/27 patients with CMML. 10 Others have indicated only 40 to 50 known cases of CMML involving t(5;12) or similar chromosomal abnormalities involving the PDGFR-B loci. 11
Imatinib is a tyrosine kinase inhibitor with potent activity against BCR-ABL in chronic myeloid leukemia. Imatinib also inhibits a number of additional tyrosine kinases including PDGFRA, PDGFRB, and c-kit, providing the basis for its use in CMML involving the t(5;12) translocation. 12-14 Recently, Han, et al. reviewed 13 cases from the literature of myeloproliferative diseases with evidence of PGDFR-B translocations treated with imatinib. 11 An impressive number of complete responses were noted, encouraging further study of this agent in this CMML subgroup.
Given this patient’s age and absence of blastic transformation, intensive induction chemotherapy regimens such as daunorubicin and cytarabine would not be optimal. Such therapies can lead to significant treatment-related mortality in the elderly. The alternative plan of observation alone, while always an option for patients, would not be preferable for this symptomatic patient who has transfusion dependency and fatigue. Finally, hypomethylating agents, including decitabine have recently been evaluated in patients with CMML. 15,16 Overall response rates of 25 percent to 70 percent have been reported, with complete response rates ranging from 12 percent to greater than 60 percent. Although this is a treatment option, given the identification of the t(5;12) translocation, oral imatinib, which is generally well tolerated even in the elderly, is a rational treatment option for this patient.
In summary, CMML associated with t(5;12) translocation is a relatively rare disorder. Responses to imatinib are variable, but this agent offers a unique treatment alternative in a disease with relatively few curative options in the elderly population. Therefore, identifying this translocation, especially in CMML patients presenting with eosinophilia, should be a priority.
- Bennett JM, Catovsky D, Daniel MT, et al. The chronic myeloid leukaemias: guidelines for distinguishing chronic granulocytic, atypical chronic myeloid, and chronic myelomonocytic leukaemia. Proposals by the French-American-British Cooperative Leukaemia Group . Br J Haematol. 1994;87:746-54.
- Elliott MA. Chronic neutrophilic leukemia and chronic myelomonocytic leukemia: WHO defined . Best Pract Res Clin Haematol. 2006;19:571-93.
- Vardiman JW, Harris NL, Brunning RD. The World Health Organization (WHO) classification of the myeloid neoplasms . Blood. 2002;100:2292-302.
- Baranger L, Szapiro N, Gardais J, et al. Translocation t(5;12)(q31-q33;p12-p13): a non-random translocation associated with a myeloid disorder with eosinophilia . Br J Haematol. 1994;88:343-7.
- Golub TR, Barker GF, Lovett M, Gilliland DG. Fusion of PDGF receptor beta to a novel ets-like gene, tel, in chronic myelomonocytic leukemia with t(5;12) chromosomal translocation . Cell. 1994;77:307-16.
- Wlodarska I, Mecucci C, Marynen P, et al. TEL gene is involved in myelodysplastic syndromes with either the typical t(5;12)(q33;p13) translocation or its variant t(10;12)(q24;p13) . Blood. 1995;85:2848-52.
- Carroll M, Tomasson MH, Barker GF, et al. The TEL/platelet-derived growth factor beta receptor (PDGF beta R) fusion in chronic myelomonocytic leukemia is a transforming protein that self-associates and activates PDGF beta R kinase-dependent signaling pathways . Proc Natl Acad Sci USA. 1996;93:14845-50.
- Jousset C, Carron C, Boureux A, et al. A domain of TEL conserved in a subset of ETS proteins defines a specific oligomerization interface essential to the mitogenic properties of the TEL-PDGFR beta oncoprotein . Embo J. 1997;16:69-82.
- Ritchie KA, Aprikyan AA, Bowen-Pope DF, et al. The Tel-PDGFRbeta fusion gene produces a chronic myeloproliferative syndrome in transgenic mice . Leukemia. 1999;13:1790-803.
- Gunby RH, Cazzaniga G, Tassi E, et al. Sensitivity to imatinib but low frequency of the TEL/PDGFRbeta fusion protein in chronic myelomonocytic leukemia . Haematologica. 2003;88:408-15.
- Han X, Medeiros LJ, Abruzzo LV, et al. Chronic myeloproliferative diseases with the t(5;12)(q33;p13): clonal evolution is associated with blast crisis . Am J Clin Pathol. 2006;125:49-56.
- Magnusson MK, Meade KE, Nakamura R, Barrett J, Dunbar CE. Activity of STI571 in chronic myelomonocytic leukemia with a platelet-derived growth factor beta receptor fusion oncogene . Blood. 2002;100:1088-91.
- Carroll M, Ohno-Jones S, Tamura S, et al. CGP 57148, a tyrosine kinase inhibitor, inhibits the growth of cells expressing BCR-ABL, TEL-ABL, and TEL-PDGFR fusion proteins . Blood. 1997;90:4947-52.
- Buchdunger E, Zimmermann J, Mett H, et al. Inhibition of the Abl protein-tyrosine kinase in vitro and in vivo by a 2-phenylaminopyrimidine derivative . Cancer Res. 1996;56:100-4.
- Aribi A, Borthakur G, Ravandi F, et al. Activity of decitabine, a hypomethylating agent, in chronic myelomonocytic leukemia . Cancer. 2007;109:713-7.
- Wijermans PW, Rüter B, Baer MR, et al. Efficacy of decitabine in the treatment of patients with chronic myelomonocytic leukemia (CMML) . Leuk Res. 2008;32:587-91.
Additional Resources
- Han X, Medeiros J, et al. Chronic myeloproliferative diseases with the t(5;12)(q33;p13) . American Journal of Clinical Pathology. 2006;125(1):49-56.
- Elliot M. Chronic neutrophilic leukemia and chronic myelomonocytic leukemia: WHO defined . Best Practice & Research Clinical Haematology. 2006;19(3):571-593.
Case study submitted by Dale Bixby, MD, PhD, of the University of Michigan.
American Society of Hematology. (1). Case Study: A 78-Year-Old Man With Elevated Leukocytes and Anemia. Retrieved from https://www.hematology.org/education/trainees/fellows/case-studies/male-elevated-leukocytes-and-anemia .
American Society of Hematology. "Case Study: A 78-Year-Old Man With Elevated Leukocytes and Anemia." Hematology.org. https://www.hematology.org/education/trainees/fellows/case-studies/male-elevated-leukocytes-and-anemia (label-accessed September 13, 2024).
"American Society of Hematology." Case Study: A 78-Year-Old Man With Elevated Leukocytes and Anemia, 13 Sep. 2024 , https://www.hematology.org/education/trainees/fellows/case-studies/male-elevated-leukocytes-and-anemia .
Citation Manager Formats
Want to create or adapt books like this? Learn more about how Pressbooks supports open publishing practices.
Descriptive Research and Case Studies
Learning objectives.
- Explain the importance and uses of descriptive research, especially case studies, in studying abnormal behavior
Types of Research Methods
There are many research methods available to psychologists in their efforts to understand, describe, and explain behavior and the cognitive and biological processes that underlie it. Some methods rely on observational techniques. Other approaches involve interactions between the researcher and the individuals who are being studied—ranging from a series of simple questions; to extensive, in-depth interviews; to well-controlled experiments.
The three main categories of psychological research are descriptive, correlational, and experimental research. Research studies that do not test specific relationships between variables are called descriptive, or qualitative, studies . These studies are used to describe general or specific behaviors and attributes that are observed and measured. In the early stages of research, it might be difficult to form a hypothesis, especially when there is not any existing literature in the area. In these situations designing an experiment would be premature, as the question of interest is not yet clearly defined as a hypothesis. Often a researcher will begin with a non-experimental approach, such as a descriptive study, to gather more information about the topic before designing an experiment or correlational study to address a specific hypothesis. Descriptive research is distinct from correlational research , in which psychologists formally test whether a relationship exists between two or more variables. Experimental research goes a step further beyond descriptive and correlational research and randomly assigns people to different conditions, using hypothesis testing to make inferences about how these conditions affect behavior. It aims to determine if one variable directly impacts and causes another. Correlational and experimental research both typically use hypothesis testing, whereas descriptive research does not.
Each of these research methods has unique strengths and weaknesses, and each method may only be appropriate for certain types of research questions. For example, studies that rely primarily on observation produce incredible amounts of information, but the ability to apply this information to the larger population is somewhat limited because of small sample sizes. Survey research, on the other hand, allows researchers to easily collect data from relatively large samples. While surveys allow results to be generalized to the larger population more easily, the information that can be collected on any given survey is somewhat limited and subject to problems associated with any type of self-reported data. Some researchers conduct archival research by using existing records. While existing records can be a fairly inexpensive way to collect data that can provide insight into a number of research questions, researchers using this approach have no control on how or what kind of data was collected.
Correlational research can find a relationship between two variables, but the only way a researcher can claim that the relationship between the variables is cause and effect is to perform an experiment. In experimental research, which will be discussed later, there is a tremendous amount of control over variables of interest. While performing an experiment is a powerful approach, experiments are often conducted in very artificial settings, which calls into question the validity of experimental findings with regard to how they would apply in real-world settings. In addition, many of the questions that psychologists would like to answer cannot be pursued through experimental research because of ethical concerns.
The three main types of descriptive studies are case studies, naturalistic observation, and surveys.
Clinical or Case Studies
Psychologists can use a detailed description of one person or a small group based on careful observation. Case studies are intensive studies of individuals and have commonly been seen as a fruitful way to come up with hypotheses and generate theories. Case studies add descriptive richness. Case studies are also useful for formulating concepts, which are an important aspect of theory construction. Through fine-grained knowledge and description, case studies can fully specify the causal mechanisms in a way that may be harder in a large study.
Sigmund Freud developed many theories from case studies (Anna O., Little Hans, Wolf Man, Dora, etc.). F or example, he conducted a case study of a man, nicknamed “Rat Man,” in which he claimed that this patient had been cured by psychoanalysis. T he nickname derives from the fact that among the patient’s many compulsions, he had an obsession with nightmarish fantasies about rats.
Today, more commonly, case studies reflect an up-close, in-depth, and detailed examination of an individual’s course of treatment. Case studies typically include a complete history of the subject’s background and response to treatment. From the particular client’s experience in therapy, the therapist’s goal is to provide information that may help other therapists who treat similar clients.
Case studies are generally a single-case design, but can also be a multiple-case design, where replication instead of sampling is the criterion for inclusion. Like other research methodologies within psychology, the case study must produce valid and reliable results in order to be useful for the development of future research. Distinct advantages and disadvantages are associated with the case study in psychology.
A commonly described limit of case studies is that they do not lend themselves to generalizability . The other issue is that the case study is subject to the bias of the researcher in terms of how the case is written, and that cases are chosen because they are consistent with the researcher’s preconceived notions, resulting in biased research. Another common problem in case study research is that of reconciling conflicting interpretations of the same case history.
Despite these limitations, there are advantages to using case studies. One major advantage of the case study in psychology is the potential for the development of novel hypotheses of the cause of abnormal behavior for later testing. Second, the case study can provide detailed descriptions of specific and rare cases and help us study unusual conditions that occur too infrequently to study with large sample sizes. The major disadvantage is that case studies cannot be used to determine causation, as is the case in experimental research, where the factors or variables hypothesized to play a causal role are manipulated or controlled by the researcher.
Link to Learning: Famous Case Studies
Some well-known case studies that related to abnormal psychology include the following:
- Harlow— Phineas Gage
- Breuer & Freud (1895)— Anna O.
- Cleckley’s case studies: on psychopathy ( The Mask of Sanity ) (1941) and multiple personality disorder ( The Three Faces of Eve ) (1957)
- Freud and Little Hans
- Freud and the Rat Man
- John Money and the John/Joan case
- Genie (feral child)
- Piaget’s studies
- Rosenthal’s book on the murder of Kitty Genovese
- Washoe (sign language)
- Patient H.M.
Naturalistic Observation
If you want to understand how behavior occurs, one of the best ways to gain information is to simply observe the behavior in its natural context. However, people might change their behavior in unexpected ways if they know they are being observed. How do researchers obtain accurate information when people tend to hide their natural behavior? As an example, imagine that your professor asks everyone in your class to raise their hand if they always wash their hands after using the restroom. Chances are that almost everyone in the classroom will raise their hand, but do you think hand washing after every trip to the restroom is really that universal?
This is very similar to the phenomenon mentioned earlier in this module: many individuals do not feel comfortable answering a question honestly. But if we are committed to finding out the facts about handwashing, we have other options available to us.
Suppose we send a researcher to a school playground to observe how aggressive or socially anxious children interact with peers. Will our observer blend into the playground environment by wearing a white lab coat, sitting with a clipboard, and staring at the swings? We want our researcher to be inconspicuous and unobtrusively positioned—perhaps pretending to be a school monitor while secretly recording the relevant information. This type of observational study is called naturalistic observation : observing behavior in its natural setting. To better understand peer exclusion, Suzanne Fanger collaborated with colleagues at the University of Texas to observe the behavior of preschool children on a playground. How did the observers remain inconspicuous over the duration of the study? They equipped a few of the children with wireless microphones (which the children quickly forgot about) and observed while taking notes from a distance. Also, the children in that particular preschool (a “laboratory preschool”) were accustomed to having observers on the playground (Fanger, Frankel, & Hazen, 2012).

It is critical that the observer be as unobtrusive and as inconspicuous as possible: when people know they are being watched, they are less likely to behave naturally. For example, psychologists have spent weeks observing the behavior of homeless people on the streets, in train stations, and bus terminals. They try to ensure that their naturalistic observations are unobtrusive, so as to minimize interference with the behavior they observe. Nevertheless, the presence of the observer may distort the behavior that is observed, and this must be taken into consideration (Figure 1).
The greatest benefit of naturalistic observation is the validity, or accuracy, of information collected unobtrusively in a natural setting. Having individuals behave as they normally would in a given situation means that we have a higher degree of ecological validity, or realism, than we might achieve with other research approaches. Therefore, our ability to generalize the findings of the research to real-world situations is enhanced. If done correctly, we need not worry about people modifying their behavior simply because they are being observed. Sometimes, people may assume that reality programs give us a glimpse into authentic human behavior. However, the principle of inconspicuous observation is violated as reality stars are followed by camera crews and are interviewed on camera for personal confessionals. Given that environment, we must doubt how natural and realistic their behaviors are.
The major downside of naturalistic observation is that they are often difficult to set up and control. Although something as simple as observation may seem like it would be a part of all research methods, participant observation is a distinct methodology that involves the researcher embedding themselves into a group in order to study its dynamics. For example, Festinger, Riecken, and Shacter (1956) were very interested in the psychology of a particular cult. However, this cult was very secretive and wouldn’t grant interviews to outside members. So, in order to study these people, Festinger and his colleagues pretended to be cult members, allowing them access to the behavior and psychology of the cult. Despite this example, it should be noted that the people being observed in a participant observation study usually know that the researcher is there to study them. [1]
Another potential problem in observational research is observer bias . Generally, people who act as observers are closely involved in the research project and may unconsciously skew their observations to fit their research goals or expectations. To protect against this type of bias, researchers should have clear criteria established for the types of behaviors recorded and how those behaviors should be classified. In addition, researchers often compare observations of the same event by multiple observers, in order to test inter-rater reliability : a measure of reliability that assesses the consistency of observations by different observers.
Often, psychologists develop surveys as a means of gathering data. Surveys are lists of questions to be answered by research participants, and can be delivered as paper-and-pencil questionnaires, administered electronically, or conducted verbally (Figure 3). Generally, the survey itself can be completed in a short time, and the ease of administering a survey makes it easy to collect data from a large number of people.
Surveys allow researchers to gather data from larger samples than may be afforded by other research methods . A sample is a subset of individuals selected from a population , which is the overall group of individuals that the researchers are interested in. Researchers study the sample and seek to generalize their findings to the population.
There is both strength and weakness in surveys when compared to case studies. By using surveys, we can collect information from a larger sample of people. A larger sample is better able to reflect the actual diversity of the population, thus allowing better generalizability. Therefore, if our sample is sufficiently large and diverse, we can assume that the data we collect from the survey can be generalized to the larger population with more certainty than the information collected through a case study. However, given the greater number of people involved, we are not able to collect the same depth of information on each person that would be collected in a case study.
Another potential weakness of surveys is something we touched on earlier in this module: people do not always give accurate responses. They may lie, misremember, or answer questions in a way that they think makes them look good. For example, people may report drinking less alcohol than is actually the case.
Any number of research questions can be answered through the use of surveys. One real-world example is the research conducted by Jenkins, Ruppel, Kizer, Yehl, and Griffin (2012) about the backlash against the U.S. Arab-American community following the terrorist attacks of September 11, 2001. Jenkins and colleagues wanted to determine to what extent these negative attitudes toward Arab-Americans still existed nearly a decade after the attacks occurred. In one study, 140 research participants filled out a survey with 10 questions, including questions asking directly about the participant’s overt prejudicial attitudes toward people of various ethnicities. The survey also asked indirect questions about how likely the participant would be to interact with a person of a given ethnicity in a variety of settings (such as, “How likely do you think it is that you would introduce yourself to a person of Arab-American descent?”). The results of the research suggested that participants were unwilling to report prejudicial attitudes toward any ethnic group. However, there were significant differences between their pattern of responses to questions about social interaction with Arab-Americans compared to other ethnic groups: they indicated less willingness for social interaction with Arab-Americans compared to the other ethnic groups. This suggested that the participants harbored subtle forms of prejudice against Arab-Americans, despite their assertions that this was not the case (Jenkins et al., 2012).
Think it Over
Research has shown that parental depressive symptoms are linked to a number of negative child outcomes. A classmate of yours is interested in the associations between parental depressive symptoms and actual child behaviors in everyday life [2] because this associations remains largely unknown. After reading this section, what do you think is the best way to better understand such associations? Which method might result in the most valid data?
clinical or case study: observational research study focusing on one or a few people
correlational research: tests whether a relationship exists between two or more variables
descriptive research: research studies that do not test specific relationships between variables; they are used to describe general or specific behaviors and attributes that are observed and measured
experimental research: tests a hypothesis to determine cause-and-effect relationships
generalizability: inferring that the results for a sample apply to the larger population
inter-rater reliability: measure of agreement among observers on how they record and classify a particular event
naturalistic observation: observation of behavior in its natural setting
observer bias: when observations may be skewed to align with observer expectations
population: overall group of individuals that the researchers are interested in
sample: subset of individuals selected from the larger population
survey: list of questions to be answered by research participants—given as paper-and-pencil questionnaires, administered electronically, or conducted verbally—allowing researchers to collect data from a large number of people
CC Licensed Content, Shared Previously
- Descriptive Research and Case Studies . Authored by : Sonja Ann Miller for Lumen Learning. Provided by : Lumen Learning. License : CC BY-SA: Attribution-ShareAlike
- Approaches to Research. Authored by : OpenStax College. Located at : http://cnx.org/contents/[email protected]:iMyFZJzg@5/Approaches-to-Research . License : CC BY: Attribution . License Terms : Download for free at http://cnx.org/contents/[email protected]
- Descriptive Research. Provided by : Boundless. Located at : https://www.boundless.com/psychology/textbooks/boundless-psychology-textbook/researching-psychology-2/types-of-research-studies-27/descriptive-research-124-12659/ . License : CC BY-SA: Attribution-ShareAlike
- Case Study. Provided by : Wikipedia. Located at : https://en.wikipedia.org/wiki/Case_study . License : CC BY-SA: Attribution-ShareAlike
- Rat man. Provided by : Wikipedia. Located at : https://en.wikipedia.org/wiki/Rat_Man#Legacy . License : CC BY-SA: Attribution-ShareAlike
- Case study in psychology. Provided by : Wikipedia. Located at : https://en.wikipedia.org/wiki/Case_study_in_psychology . License : CC BY-SA: Attribution-ShareAlike
- Research Designs. Authored by : Christie Napa Scollon. Provided by : Singapore Management University. Located at : https://nobaproject.com/modules/research-designs#reference-6 . Project : The Noba Project. License : CC BY-NC-SA: Attribution-NonCommercial-ShareAlike
- Single subject design. Provided by : Wikipedia. Located at : https://en.wikipedia.org/wiki/Single-subject_design . License : CC BY-SA: Attribution-ShareAlike
- Single subject research. Provided by : Wikipedia. Located at : https://en.wikipedia.org/wiki/Single-subject_research#A-B-A-B . License : Public Domain: No Known Copyright
- Pills. Authored by : qimono. Provided by : Pixabay. Located at : https://pixabay.com/illustrations/pill-capsule-medicine-medical-1884775/ . License : CC0: No Rights Reserved
- ABAB Design. Authored by : Doc. Yu. Provided by : Wikimedia. Located at : https://commons.wikimedia.org/wiki/File:A-B-A-B_Design.png . License : CC BY-SA: Attribution-ShareAlike
- Scollon, C. N. (2020). Research designs. In R. Biswas-Diener & E. Diener (Eds), Noba textbook series: Psychology. Champaign, IL: DEF publishers. Retrieved from http://noba.to/acxb2thy ↵
- Slatcher, R. B., & Trentacosta, C. J. (2011). A naturalistic observation study of the links between parental depressive symptoms and preschoolers' behaviors in everyday life. Journal of family psychology : JFP : journal of the Division of Family Psychology of the American Psychological Association (Division 43), 25(3), 444–448. https://doi.org/10.1037/a0023728 ↵
Descriptive Research and Case Studies Copyright © by Meredith Palm is licensed under a Creative Commons Attribution 4.0 International License , except where otherwise noted.
Share This Book
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Soa Chongsonyon Chongsin Uihak
- v.33(3); 2022 Jul 1

Dissociative Identity Disorder in an Adolescent With Nine Alternate Personality Traits: A Case Study
Sang-hun lee.
1 Department of Psychiatry, Jeju National University Hospital, Jeju, Korea
2 Department of Psychiatry, Jeju National University College of Medicine, Jeju, Korea
Duk-Soo Moon
Since dissociative identity disorder (DID) has symptoms similar to schizophrenia, such as auditory hallucinations and delusional thoughts of being controlled, there are difficulties in its differential diagnosis. A 16-year-old adolescent male patient who was previously diagnosed with schizophrenia from a different hospital was admitted to our inpatient psychiatric unit for the evaluation of auditory hallucinations and suicide attempts. Through psychiatric evaluations, it was determined that the patient suffered from identity alternation, dissociation, and amnesia. As for the diagnostic evaluations, the following measures were implemented: a psychiatric interview regarding the diagnostic criteria, mental status examination, laboratory tests, brain imaging studies, electroencephalography, and full psychological test for adolescents, and the self-reported measure of the Adolescent Dissociative Experiences Scale. The patient was diagnosed with DID, and the following treatments were administered: pharmacotherapy, ego state therapy, psychoeducation regarding emotions, trauma-focused psychotherapy including stabilization, and family therapy. Following treatment, in the internal dimensions, the patient was able to recognize the nine alternate identities in charge of his emotions, which established a basis for the potential integration of identities. In the external dimensions, he showed improvements in the aspects of family conflicts and issue of school refusal. This is the first reported case of DID in an adolescent in Korea; it emphasizes the consideration of DID in the differential diagnosis of other mental illnesses such as schizophrenia, bipolar disorder, and posttraumatic stress disorder and expands the treatment opportunities for DID by sharing the procedures of ego state therapy.
INTRODUCTION
Dissociative identity disorder (DID) is characterized by the existence of dissociative identities, disruption of identity and identity alteration, amnesia, depersonalization, and derealization [ 1 ]. Over 80% of patients with DID experience auditory hallucinations, and identity alteration is sometimes similar to the symptoms of other mental illnesses, such as delusional thoughts of being controlled. Since DID shares many of its symptoms with schizophrenia, there are difficulties associated with differential diagnosis, with errors in diagnosis leading to inappropriate treatment [ 2 ]. The patient in this case study had been diagnosed with schizophrenia and depression at a different hospital, with symptoms of auditory hallucinations and suicide attempts and a medical history that included pharmacotherapy and an inpatient treatment program. Afterwards, he was diagnosed with DID with nine alternate personality states (alternate identities, “alter/alters”) at our clinic, underwent two hospitalization at the department of psychiatry’s closed ward, and has significantly improved symptoms through continuous outpatient treatment. This case study is the first reported case of adolescent DID in Korea and is being introduced to emphasize the importance of differential diagnosis between DID and other mental disorders, such as schizophrenia, and to share the specific treatment approach of ego state therapy that had been applied to this case.
CASE REPORT
Patient information.
A 16-year-old male patient visited our outpatient clinic for the evaluation of auditory hallucinations and impulsive behavior of stabbing his mother’s forehead with a knife. The patient was born from a planned pregnancy with no reported medical history during the perinatal or postnatal period. The patient experienced numerous traumatic events starting from his childhood, with both parents engaging in severe conflicts that resulted in a two-way domestic assault over the course of their marriage. The patient recalls his parents fighting before his eyes when he was approximately 5 years old, when his father threw an electric fan at his mother, which knocked her unconscious as it struck her head. He remembers heading to the hospital with his mother in an ambulance, trembling with fear of the possibility of his mother dying from the injury. His parents had divorced when he was about 8 years of age; for a few months following the divorce, the patient kept his eyes closed at all times, except when he was walking on the road or eating his meals. He has been bullied at school since the 1st grade, with most of his school life being spent in solitude. When he was approximately 11 years of age, the patient had witnessed his alcohol-intoxicated mother stabbing herself in the abdomen with a knife in their house. When he was about 13 years of age, the patient spent most of his time playing mobile games at home, excluding the time when he was at school. He had gotten into conflict with his mother regarding this issue, with verbal arguments escalating to the point of his mother throwing and breaking his phone repeatedly on multiple occasions. As the patient quarreled with his mother over his phone, the situation sometimes escalated to the point of his mother strangling the patient’s throat or beating his mother until she had black eyes. When he was about 15 years of age (1 year prior to visiting our clinic), the patient started experiencing auditory hallucinations of three beings talking to him: someone who tells the patient to kill, another who tells the patient to kill himself, and a third one who tries to stop these two beings. The patient killed his pet turtle by chopping it with a knife, and he also caught wild pigeons from the roadside to stab them to death. Reacting to the auditory hallucinations, the patient engaged in self-harm by injuring his thighs with a knife and attempted to commit suicide by jumping from the roof of his school. Subsequently, he visited a different psychiatric clinic and started pharmacotherapy with antipsychotics and antidepressants, from the impressions of schizophrenia and depression. Although the patient faithfully followed the medication regimen, the symptoms of auditory hallucinations did not improve. Six months prior to visiting our clinic, he reacted to a voice that told him to kill a person and tried to stab his friend—who was next to him at the time—with a pen. Due to this incident, he was admitted to a closed ward of a different psychiatric clinic to receive a 2-week inpatient treatment. While the auditory hallucinations seemed to have improved since hospitalization, the patient started hearing auditory hallucinations again, starting from 3 months prior to visiting our clinic. The auditory hallucinations tended to occur when the patient was at crowded places, where the three beings—one male, one female, and one unidentified being—would start talking to him with words such as “Kill. If you do not want to, die.” Despite having increased the dosage of his medication, his auditory hallucinations did not improve to the point where the patient started to leave early from school on more frequent occasions, being unable to eat even a single bite of his school lunch. Two weeks prior to visiting our clinic, the patient’s mother handed the patient a knife as she said, “If you are going to make me suffer so, why don’t you rather just kill me,” while she was intoxicated with alcohol. As they were quarreling with each other, the patient stabbed his mother’s forehead by accident. The patient was given recommendations for receiving treatment at an advanced hospital. The patient visited our outpatient clinic for evaluation and treatment and he was admitted to our inpatient psychiatric unit.
Written informed consent was obtained from the patient and his mother for the publication of data and images included in this article. This case study was reviewed and approved by the Institutional Review Board of the Jeju National University Hospital (IRB no. 2022-03-006).
Clinical findings and diagnostic assessment
At the time of hospitalization at our inpatient psychiatric unit, the patient was a 174 cm-tall male adolescent weighing 88 kg, with greasy hair and poor hygiene, and had no facial expressions and spoke with a dry and monotonous voice. He said that there were three beings inside himself, and that those voices sometimes command him to stab his mother. He also reported that it was not him who stabbed his mother, but the ‘crow monster’ inside himself. He continued by saying that he was a child who could not feel any emotions. For a thorough evaluation of the patient, a psychiatric interview regarding the diagnostic criteria outlined in the Diagnostic and Statistical Manual of Mental Disorders, fifth edition (DSM-5), mental status examination, laboratory tests, brain imaging studies, electroencephalography, and full psychological test for adolescents were administered. Other than hyperprolactinemia (prolactin 67.08 μg/L), there were no noteworthy medical opinions from the laboratory test results. There were also no noteworthy medical opinions based on the brain imaging studies and electroencephalography. Results of the full psychological test for adolescents indicated a Full Scale Intelligence Quotient of 92, and the results of the projective tests suggested no cognitive distortions. In addition, there were no indications of noteworthy aspects from the results of the Minnesota Multiphasic Personality Inventory.
Regarding the ‘three beings within himself’ reported by the patient, it was necessary to have a differential diagnosis for DID. To evaluate for dissociations, the Adolescent Dissociative Experiences Scale (A-DES), which is the adolescent version of the most commonly used measure of dissociation in clinical settings called the Dissociative Experiences Scale (DES), was administered. The DES consists of 28 items measured on the scale of 0–100, each of which is categorized into one of the following four subdimensions: identity confusion/ alteration, absorption, depersonalization/derealization, and amnesia [ 3 , 4 ]. The A-DES consists of 30 items, each measured on a 10-point Likert-type scale; a mean total score of 3.7 in the A-DES was previously found as the standard for ‘significant dissociation’ [ 5 ]. In a study of the A-DES of Turkish adolescents, the mean total score of the A-DES was reported to be 6.2 points for the ‘dissociative disorder’ group, 3.9 points for the ‘posttraumatic stress disorder (PTSD)’ group, and approximately 2.4 points in the ‘non-clinical,’ ‘mood disorders,’ ‘attention deficit hyperactivity disorder,’ and ‘anxiety disorders’ groups [ 6 ]. A study on the validity of the A-DES in Korea reported a mean total score of 2.05 points in the ‘traumatized’ group, which was significantly higher than the score of 0.75 points in the ‘normative’ group [ 7 ].
The patient in this case study had high levels of dissociation based on a mean total score of 6.77 points on the A-DES administered during hospitalization. Regarding the item scores in the patient’s A-DES response, items such as “I have strong feelings that don’t seem like they are mine,” “Something inside of me seems to make me do things that I don’t want to do,” and “I feel like there are different people inside of me” in the identity confusion/alteration subdimension had the highest scores, all of them with 10 points. Items such as “I get confused about whether I have done something or only thought about doing it” and “I can’t figure out if things really happened or if I only dreamed or thought about them” in the amnesia subdimension also had high scores (8–10 points). However, items such as “I find myself standing outside of my body, watching myself as if I were another person” in the depersonalization/derealization subdimension were scored very low at 0 points.
Although the patient reported suffering from auditory hallucinations for almost 1 year, there were no clear observations of disorganized speech or behavior, or the negative symptoms of schizophrenia. The patient experienced disruption of identity characterized by three or more distinct personality states. He had gaps in his recall of specific past memories; childhood trauma experiences were discovered and understood thoroughly during the treatment process. In addition, the patient had multiple occasions when he failed to remember the activities that he had done in person, or was surprised when he discovered evidence of such activities after the fact. The combination of such testing results and clinical features suggests that the patient’s diagnostic impression was closer to that of DID than schizophrenia, which was his previous diagnosis from a different clinic.
Therapeutic intervention
Regarding the treatment for DID, various methods are being implemented, including pharmacotherapy, cognitive behavior therapy, and eye movement desensitization and reprocessing (EMDR) [ 8 ]. One of these methods is ego state therapy, where the clinician comes face-to-face with various ego states within the patient [ 9 ]. Ego state therapy also uses hypnosis as a treatment method and has been combined with trauma processing therapy methods (e.g., EMDR) to be developed into a therapeutic intervention for patients with symptoms of trauma and dissociation [ 10 ]. Ego state therapy aims to promote the proper functioning of a patient’s internal system, which is composed of multiple ego states, by connecting the memory of each state with those of the others, while accepting the differences that exist between the states and respecting the values of reciprocity and cooperativity [ 9 - 11 ]. During the course of two hospitalizations for treatment, the following were administered: psychoeducation regarding emotions, trauma-focused psychotherapy that includes stabilization, and family therapy. In addition, since the patient lacked awareness of his alters and experienced a loss of control, the clinician also utilized ego state therapy to identify and approach the patient’s alters. Pharmacotherapy was administered as an accompanying treatment to control the patient’s underlying symptoms of depression, anxiety, impulsiveness, and aggression (first hospitalization: 200 mg sertraline and 300 mg quetiapine; second hospitalization: 100 mg sertraline and 5 mg aripiprazole).
Follow-up and outcomes
Nine types of alternate identities.
In ego state therapy, the patient was allowed to explore the space of his mind through hypnosis with his eyes closed; the clinician and the patient have named that space the ‘Mind’s Room.’ Inside the Mind’s Room, as described by the patient, was a table, a sofa, three dogs, and 15 trees; on the ceiling, there was a large eye that could observe the inside of the room. There were four doors, each leading to either the ‘Computer Room,’ ‘Jungle,’ ‘Desert,’ or ‘Basement.’ The three alters reported by the patient could be met in the Mind’s Room; as ego state therapy progressed, the other spaces connected to the main room by the four doors were explored, resulting in the discovery of nine total alters ( Table 1 ). Each time a new alter was discovered, the clinician could recognize the identity alteration, as the patient’s facial expression, manner and content of speech, and posture would also be changed simultaneously. There were alters that were aware of each other, but there were also those who had no knowledge of the other until the clinician introduced them to each other. Among these alters, some had been perceived by the patient, whereas others were affecting the patient without the patient knowing their existence. For each of the nine alters, the patient gave names derived from birthstones. According to the patient’s report, excluding ‘Emerald’ who came into existence when he was 4 years old, all alters were created when he was about 15 years old. Centered around ‘Agate,’ who served as the leader, there were dynamic relationships between the alters, with each alter playing a role related to the major emotions of the patient.
Summary of the nine alternate identities
| Name of alternate identity | Emotion(s) expressed by the alternate identity | Characteristics revealed through ego state therapy and the patient’s drawings |
|---|---|---|
| Agate | Void | The patient’s main state; it has become the leader of the other alters through the treatment process and is capable of controlling the other alters. Presence or absence of the horns ( ) can be an indicator of whether the patient is feeling void, or in a state where he is better at feeling emotions. |
| Ri_te | Sorrow | Good at feeling sorrow; when agitated, makes verbal slip-ups that include expletives. When engaging in violent and cruel behavior, it occasionally encourages such behavior from the side. |
| Xandra | Rage | A cynical character, who can be quite fierce at times. In the past, it was always in the shape of a monster resembling a crow; following admission, it became less fierce, and it was discovered that it had a human form. |
| Obsidian | Guilt (sin, fault) | This alter does not feel guilty but makes other alters feel guilty. In this process, its influence grows, which increases the probability of committing a crime. The feeling of guilt was too difficult for this alter; to become numb to guilt, it would repeatedly engage in behaviors that would induce guilt. |
| Tourmaline | Knowledge, disgust | The director who is in charge of the space within the Mind’s Room; has almost all of the information regarding the things that have occurred within the mind. |
| Rose Quartz | Happiness, despair | It had been isolated and exhausted in the desert of Mind’s room; since the beginning of the treatment, it has a good relationship with the others and sits straight. |
| Alex | Love, fear | This alter had thought that the patient was so lonely that it pushed the patient into a love relationship inappropriately with sexual jokes. |
| Emerald | Pure, insanity | Came into existence when the patient was 4 years old and stayed mainly in the basement of the Mind’s Room; although it could leave or enter the space freely, it was completely shut-in when the patient was 10 years old and could no longer leave the Basement. Has a child-like appearance; the facial expression has become brighter since the beginning of the treatment, as the door to the basement had been opened. |
| The Emerald (Emma) | Insanity | The most impulsive and aggressive alter that was hidden inside the pure alter of Emerald. Takes turns with Emerald to change personality within the Mind’s Room. Agate is controlling it since it has insanity and anger for people. |
Therapeutic process inside
At the time of hospitalization, while the patient had some awareness of the beings inside himself, he had lost his sense of control over the auditory hallucinations and the timing of amnesia and/or identity alteration. Through ego state therapy, the patient experienced a detailed inspection and understanding of his own ego states. In a safe treatment space that could be controlled by the clinician, the patient explored the Mind’s Room together with the clinician; when the patient experienced anxiety, stabilization (such as grounding and containment) was used to control the patient’s sense of anxiety. Through this process, the patient increased his awareness of his own states and had more control over himself. Since the patient was fond of drawing, he depicted the Mind’s Room and each of the alters with pictures. Through the treatment process, he organized the changes in his mind by making drawings that captured the characteristics of each alter ( Figs. 1 and and2 2 ).

Self-portraits of the nine alternate identities, drawn by the patient.

The Mind’s Room and its structure, as depicted by the patient. When exploring the Mind’s Room for the first time through ego state therapy—together with the patient, who was in a state of hypnosis—the space had a structure similar to a living room, with actual objects such as a sofa, table, and TV; the alters Alex, Xandra, and Ri-te were in this room. The living room had three doors, each leading to either the Desert, Jungle, or Computer Room. In the Desert, the alters Tourmaline, Obsidian, and Rose Quartz were discovered in order. As treatment progressed, the door to the basement, where the alter Emerald had been locked in, was newly discovered, freeing Emerald from the basement. When Emerald emerged from the basement, all other alters trembled with fear. The clinician believed it was necessary for Emerald—which had been locked away in the basement for a long period of time, as the alter of a young child—to get some rest and care and to be temporarily separated until the other alters’ fear of Emerald had abated. Through hypnotic suggestion, a playroom was created for Emerald.
Prior to treatment, the patient’s alters increased the patient’s sense of confusion by being activated separately, or by confronting each other in the patient’s mind. Through the treatment process, these alters gained awareness of each other’s existence in the patient’s psychic world, understood each other’s positions, and acknowledged the existence of each other. When the patient was faced with difficult decisions, he occasionally found an appropriate measure by having a meeting between the alters; this was different from the past, where the alters would intemperately expose their emotions uncontrollably. As a result, the alters who were alone and isolated in the past became capable of living with each other and started to show signs of communication and understanding between them. The relationship between the alters, which have become intimate and comfortable with each other, has been depicted in the patient’s drawing ( Fig. 3 ).

Patient’s drawing depicting the relationships between the alters in the latter half of the treatment, with their conflicts resolved. Early in the treatment, the alters kept each other in check, quibbling over what was right and wrong in their relationships. The alters’ appearances also had an exclusive and threatening atmosphere, depicted with mostly dark colors, harsh eyes, and sharp lines ( Fig. 1 ). As treatment progressed, the alters understood the position and reason for being of each other and began to be depicted in appearances that were freer and more comfortable within the patient’s control. According to the patient’s explanation, this drawing in Fig. 3 depicts the alter Obsidian, who was always living in seclusion at the Desert, starting to have a good relationship with the other alters. Here, Obsidian is being mischievous with the alter Ri_te, suggesting that male Ri_ te is trying to wear feminine clothing. If this were a dangerous situation, Agate, which is represented as the patient himself, would have intervened to control the situation; Agate stands by and watches the mischievous situation. The patient’s drawing depicts the playful communication between the alters, who used to be isolated in their own situations in the past, gathered in a single room. This describes the relationship between the alters in the latter half of the treatment, with sharp conflicts between them having been resolved.
Since the process of building expertise on ‘acknowledging and making decisions regarding one’s emotions’ is accompanied by heavy responsibilities for the patient, there were moments when the patient wanted to give up his pursuit of the process. During the hospitalization period, a different female patient asked the current patient if they could meet outside the clinic. As the patient was not attracted by the female patient, he wanted to refuse the offer; however, it was difficult for the patient to behave in a manner that matched his emotions. The patient wanted to escape from the burden of such decisions and wished some other alters in his mind to take his place and make the tough decision for him. The patient retreated in his psychic world, telling the clinician that this was unbearable for him. In the absence of the controlling entity, other alters took turns appearing in front of the clinician. The clinician could associate this moment with the formation process of the patient’s alters: when the patient decided that he wanted to escape from difficult emotions, the alters were created to bear the emotions in his place. However, during the treatment process, the patient realized that he cannot delegate all of his decisions to the other alters within his mind and recognized the need to behave autonomously based on the emotions he felt himself. He then communicated his polite yet honest refusal to the female patient. The patient was starting to develop his own capability, so that he no longer had to rely on the alters. The patient, who had let go of his control over emotion regulation since he was afraid of sensing his emotions, has acknowledged through the treatment process the fact that he needs emotions, as well as the ability to control them.
For the patient, whose emotions had been divided into the alters, controlling his emotions meant the same as being able to control his alters. Throughout the treatment process, the patient’s control gradually grew until he had the most influence; over time, the alters could no longer expose themselves at their will and could surface only if the patient allowed them to, in cases of necessity. In this process, the frequency of appearance of the alters decreased over time, and the patients’ sense of confusion was also reduced. At the time of hospitalization, the patient reported that he could not sense emotions, and his emotions were represented by alters. For the patient who had difficulty recognizing his own emotions, it was even more difficult to empathize with the emotions of others. During treatment, the patient had experienced having his emotions understood by the hospital medical staff in a stable relationship and had received education on perceiving and expressing his emotions. Gradually, the patient was able to express his emotions with verbal terms (e.g., anger, depression, and anxiety) rather than expressing them through the activation of his alters. This is considered to be the result of the patient being less afraid of his own emotions due to the novel experience of ‘a sense of security’ in the treatment environment, something that he could not experience in his previous relationships.
Therapeutic process outside
After discharge from the first hospitalization, the patient showed a remarkable decrease in impulsive and aggressive behavior, with a decrease in the frequency of appearance of the alters; however, it was difficult for him to adapt to reality. Sensing the emotions that had been delegating to the alters on his own and determining his behavior accordingly can be considered more difficult for the patient, in a certain sense. The patient’s family members have difficulty empathizing with the patient, who still finds it difficult to adapt to reality, which then worsened the conflict. In this process, a second hospitalization was performed to help the patient with emotional difficulties and adaptation.
If the first hospitalization focused on treating the patient’s internal dimensions, the second admission focused on external dimensions, such as family conflicts and school refusal. By providing psychoeducation on DID to the family, the clinician attempted to help the family understand that symptoms such as dissociation and amnesia were the best means of survival for the patient in his circumstances, rather than an escape mechanism or intentional malingering from the patient. Likewise, through psychoeducation, the patient understood that it was difficult for laypersons, such as the patient’s mother, to understand an illness like DID and that this process could take some time. He realized that his mother’s inability to understand him was, in reality, the consequence of the difficulty she had in understanding the illness. The clinician intervened in the impulsive and hurtful speech between both parties, communicating the presence of sincere worries and love contained within such words and disentangled misunderstandings that had been left unresolved, which had occurred in multiple occasions.
Through family therapy, the family members tried to understand each other’s positions; thus, the conflict between the patient and his mother decreased markedly compared to that in the past. The patient had time to self-reflect on the consequences of his immature behavior and showed a decrease in problematic behaviors. In turn, he was able to return to school and became capable of living in his daily life since his life pattern had been restored. Since he started receiving treatment at our clinic, he had better access to treatment resources, which enabled him to receive financial support for his studies. Despite such improvements, reality remains a series of difficult experiences for the patient, and there are times when he faces surges of anger, depression, and voidness. Through interventions for the patient’s disruption of identity, provided through the two hospitalizations and outpatient treatment, the patient no longer suffered from the external symptoms of abrupt identity disturbance. However, the patient’s inner conflict persisted, along with the feeling of depression caused by the conflict. Nevertheless, the patient chooses to sense such emotions and make judgments himself, rather than delegating the task to the alters in his mind. In a sense, this is even more difficult for the patient, but he is still living his life as he deals with such challenges. The patient is deprived of developmental experiences, has a weak ego function, and is still in his adolescence, that is, he is still immature compared to an adult. In future treatment processes, longterm procedures of ‘working through’ will be even more necessary to promote the continuous growth of the patient’s developmental level and ego functions.
Dissociative identity disorder in Asian culture
There have been four cases of DID reported in Korea, all of which have been adults [ 12 - 14 ]. In Korea, this case study is the first reported case of DID in an adolescent. The prevalence rate of DID is reported to be significantly lower in Asian nations (0%–0.5%), compared to that reported in Western countries of North America and Europe (1%–5%) [ 12 ]. This is considered to be the consequence of previously diagnosing DID mainly as a possession disorder in Asian nations [ 15 ] and the fact that Korean clinicians are not accustomed to the diagnosis of DID [ 16 ]. Specifically, it is important to pay attention to this matter, since undiagnosed DID in Asian nations can be understood as a ‘possession state’ by the patient’s acquaintances, leading the patient to rely on shamanistic interventions rather than appropriate treatment methods, in which the patient may even experience adverse effects.
Trauma and dissociative identity disorder
In systematic ecological research, it has been observed that most DID patients have a history of severe and chronic child abuse [ 17 ]. A high proportion of patients with pathological DID also have a history of childhood trauma [ 18 ]. It has been observed that there is a statistically significant association between trauma, including physical abuse, and symptoms of dissociation [ 19 ]. Insecure attachment relationships also affect the relationship between childhood trauma and symptoms of dissociation in adulthood. This leads to imperfections in the function of resilience (i.e., vulnerability in the functionality of autonomous emotion regulation), which increases the likelihood of dissociative reactions, potentially resulting in the dissociation of identity such as identity alteration [ 20 ].
As such, repeated exposure to trauma, including childhood abuse, are painful experiences that cannot be integrated within the patient [ 18 ]. In this case, where there were many traumatic experiences, dissociation was used as a defense mechanism to protect oneself from painful experiences; by being incapable of sensing emotions, the patient could avoid the agony of such experiences. However, since emotion is an essential component of life, entities were created within the patient’s psychic world to sense the patient’s emotions in his place; therefore, the patient’s alters acquired their characteristic emotions, each being in charge of a major one. During ego state therapy, the alters have voluntarily reported to the clinician that, “We are like vigilantes who had no choice but to mobilize, in order to protect ourselves in a state of anarchy.”
Amnesic barrier in dissociation
Through an amnesic barrier, dissociation can prevent the patient from recognizing major experiences [ 21 ]. The Mind’s Room of this case was separated into different spaces by the four doors found in it. During the ego state therapy, treatment procedures conducted in a specific space were not recognized by the alters that were located in the other spaces. It seems that a dissociative barrier had been embodied in the patient’s psychic world, which prevents the alters from recognizing the existence of each other depending on the characteristic or role of each alter; this is also associated with the symptoms of amnesia commonly observed in patients with dissociation. Depictions in the drawings of the patient in this case study (e.g., his alters and the structure of the Mind’s Room; Figs. 1 1 - -3) 3 ) are considered a useful resource for clinicians who wish to understand the internal dimensions of DID patients.
Differential diagnosis of dissociative identity disorder
Through this case study, the authors emphasize the importance of DID diagnosis, as well as its differential diagnosis from other illnesses. Symptom patterns of DID, which are generally subtle and covert, differ from those portrayed in the media, which are more dramatic or histrionic [ 22 ]. Across studies, patients with DID spend an average of 5–12.4 years in the mental health system before correct diagnosis, receiving an average of 3–4 incorrect diagnosis [ 22 ]. For adolescents with symptoms of mental illness, such as auditory hallucinations, especially those with a history of exposure to traumatic experiences, the differential diagnosis of DID is necessary prior to the diagnosis of schizophrenia. Over 80% of patients with DID report auditory hallucinations [ 2 ], and research also suggests that patients with DID report auditory hallucinations more often than patients with schizophrenia, with both groups being younger than 18 years of age [ 23 ]. Unlike schizophrenia, DID does not have prominent symptoms of formal thought disorders or any negative symptoms [ 24 ]. For an accurate differential diagnosis, it is necessary to check whether the patient has a history of childhood trauma and whether the patient is experiencing symptoms such as amnesia, identity alteration, and dissociative experiences. For the evaluation of dissociative experiences in adolescents, measures such as the A-DES can be helpful.
Patients with DID are sometimes misdiagnosed as bipolar disorder, most commonly as bipolar II disorder. Patients with bipolar disorder are episodic and show slower mood changes; in contrast, patients with DID show rapid and subjective shifts in mood across their dissociative states [ 25 ]. Dissociation can also occur in patients with bipolar disorder; symptoms of dissociation can appear prior to the onset of bipolar disorder and are associated with a worse prognosis and larger numbers of mood swings for patients with bipolar disorder [ 26 ]. In a patient with DID and comorbid bipolar disorder, the bipolar disorder responded to pharmacotherapy, and it was only possible for psychotherapy as treatment for DID to demonstrate its efficacy after the symptoms of bipolar disorder had been controlled; thus, it can be hypothesized that the effectiveness of pharmacotherapy can be used to differentiate the two illnesses [ 27 ].
Since identity alteration observed in DID can be considered to be elaborate displays of trauma-related symptoms (e.g., intrusion and avoidance) that appear in PTSD, the two illnesses have similarities. However, since DID has distinct identities that can be identified at the conscious level (multiple “I” selves), it is different from PTSD [ 1 ].
This case had severe behavioral problems when he lost his sense of control and clearly displayed alterations between different identities during hospitalization. With high scores of dissociation indicated on the A-DES results and reports of ‘relationships with other people being changed without the patient’s knowledge’ during the psychiatric interviews based on the diagnostic criteria of the DSM-5, the patient also reported recurring gaps in the recall of everyday events. The patient reported amnesia for the following: major accidents in the past, parental abuse, and verbal assault toward his parents. Through such evaluative and treatment procedures, the patient was diagnosed with DID, and the influence of other medical conditions, substances, or mental illnesses was ruled out by reviewing the results of the psychiatric evaluation, laboratory tests, brain imaging studies, electroencephalography, and full psychological tests for adolescents. Through such diagnostic procedures, the patient was somewhat relieved, as he started to gain an understanding of his symptoms, which had been causing him a lot of confusion.
DID is occasionally misdiagnosed, making it difficult for patients to receive appropriate treatment. When childhood and adolescent traumatic experiences (e.g., school bullying, chronic abuse and neglect) are present in a patient, similar to that of this case study, the clinician need to be ready to evaluate and treat dissociative disorders. Specifically, for adolescent patients starting to develop symptoms of nonspecific psychotic symptoms including hallucination, it is necessary to have detailed evaluations of their traumatic experiences and dissociation.
Availability of Data and Material
The datasets generated or analyzed during the study are not publicly available due to the copyright and privacy restriction, but are available from the corresponding author on reasonable request.
Conflicts of Interest
The authors have no potential conflicts of interest to disclose.
Author Contributions
Funding Statement
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- My Bibliography
- Collections
- Citation manager
Save citation to file
Email citation, add to collections.
- Create a new collection
- Add to an existing collection
Add to My Bibliography
Your saved search, create a file for external citation management software, your rss feed.
- Search in PubMed
- Search in NLM Catalog
- Add to Search
Common mental disorders in Gestalt therapy treatment: a multiple case study comparing patients with moderate and low integrated personality structures
Affiliations.
- 1 Department for Psychosomatic Medicine and Psychotherapy, University for Continuing Education Krems, Krems, Austria.
- 2 Department Psychotherapy, Bertha von Suttner Private University St. Pölten, St. Pölten, Austria.
- 3 Integrative Gestalttherapie, Österreichischer Arbeitskreis für Gruppentherapie und Gruppendynamik, Vienna, Austria.
- 4 Division of Psychotherapy, Department of Psychology, Paris Lodron University Salzburg, Salzburg, Austria.
- PMID: 38173855
- PMCID: PMC10761483
- DOI: 10.3389/fpsyg.2023.1304726
Introduction: Empowerment is central to self-development and growth in Gestalt therapy. The self evolves through interactions with others, forming self- and object-relations, and ego-functions. Underlying structural functions build the ability to regulate, differentiate, and integrate experiences, leading to self-, and emotion-regulation. Our study examined the self-development of seven clients with prevalent mental health issues and structural challenges, all of whom underwent 30 sessions of Gestalt therapy in a real-world individual therapy context.
Methods: Using a multiple case study approach, we contrasted two client groups: those with moderately integrated and those with low-integrated personality structures, as defined by the operationalised psychodynamic diagnostic manual. Our exploration centered on specific factors of empowerment, therapy processes, and interventions. The study's mixed-method design encompassed quantitative outcome measures (empowerment, wellbeing, psychosocial health, and severity of personality functioning), therapy diaries from both clients and therapists, and semi-structured client interviews about empowering factors in therapy.
Results: Both groups showed positive therapy outcomes on wellbeing, psychosocial health, and empowerment. Specific empowerment-related factors included promoting experiences, relationships, and self-efficacy in the low-integrated group. Support of self-regulation was reported to be essential for successful outcomes in the moderately integrated group. While the therapy processes proceeded similarly in both groups, we observed a strong focus on body awareness-oriented interventions and promotion of verbalisation in the low-integrated group and a relationship-oriented emphasis in the moderately integrated group. Emotional experience linked to positive experience was limited in the low-integrated group, suggesting an impairment of emotional processing, including bodily felt feelings. No change was reported in the level of personality functioning after 30 sessions in both groups.
Discussion: These results underscore the need for tailored therapeutic approaches based on the client's level of personality integration. Future research should probe the long-term effects of therapy and delve deeper into shifts in personality functioning, especially concerning emotional and bodily experiences. In practical terms, therapists should prioritize linking bodily sensations with emotions for clients with low-integrated personalities. For those with moderate integration, the emphasis should be on fostering exploration, awareness, and bolstering self-regulation.
Keywords: Gestalt therapy; common mental health disorders; mixed-methods case study; operationalized psychodynamic diagnostic; outcome; process; psychotherapy.
Copyright © 2023 Kaisler, Fede, Diltsch, Probst and Schaffler.
PubMed Disclaimer
Conflict of interest statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Overview of the study design.…
Overview of the study design. The graph depicts data collection in Gestalt therapy…
Coding system for qualitative data.…
Coding system for qualitative data. The graph displays the coding system of qualitative…
Treatment outcome measures. Overview of…
Treatment outcome measures. Overview of pre-post effect sizes from outcome measures after 15…
Narrative process coding system (NPCS).…
Narrative process coding system (NPCS). The figure shows narrative process coding sequences, relationship…
Emotional expressions co-occur with topics.…
Emotional expressions co-occur with topics. On the left side, emotional expressions are listed…
Similar articles
- Ability to move between self-states and emotional experiencing and processing as predictors of symptomatic change. Fisher H, HaCohen N, Shimshi S, Rand-Lakritz S, Shapira K, Tuval-Mashiach R. Fisher H, et al. Psychol Psychother. 2020 Dec;93(4):723-738. doi: 10.1111/papt.12256. Epub 2019 Oct 21. Psychol Psychother. 2020. PMID: 31637839
- Clients' experiences of one-to-one low-intensity interventions for common mental health problems: An interpretative phenomenological analysis. Amos R, Morris L, Mansell W, Edge D. Amos R, et al. Psychol Psychother. 2019 Dec;92(4):565-583. doi: 10.1111/papt.12200. Epub 2018 Oct 29. Psychol Psychother. 2019. PMID: 30371982 Free PMC article.
- Learning about Aboriginal health and wellbeing at the postgraduate level: novel application of the Growth and Empowerment Measure. Fitzpatrick SA, Haswell MR, Williams MM, Nathan S, Meyer L, Ritchie JE, Jackson Pulver LR. Fitzpatrick SA, et al. Rural Remote Health. 2019 Apr;19(2):4708. doi: 10.22605/RRH4708. Epub 2019 Apr 16. Rural Remote Health. 2019. PMID: 30987426
- Assessing Support for Medicine Decision Making for Youth with ADHD Who Receive Therapy [Internet]. Hogue A, Fisher JH, Dauber S. Hogue A, et al. Washington (DC): Patient-Centered Outcomes Research Institute (PCORI); 2020 Sep. Washington (DC): Patient-Centered Outcomes Research Institute (PCORI); 2020 Sep. PMID: 37672618 Free Books & Documents. Review.
- Psychosocial interventions for self-harm in adults. Hawton K, Witt KG, Taylor Salisbury TL, Arensman E, Gunnell D, Hazell P, Townsend E, van Heeringen K. Hawton K, et al. Cochrane Database Syst Rev. 2016 May 12;2016(5):CD012189. doi: 10.1002/14651858.CD012189. Cochrane Database Syst Rev. 2016. PMID: 27168519 Free PMC article. Review.
- Angus L. (2012). Toward an integrative understanding of narrative and emotion processes in Emotion-focused therapy of depression: implications for theory, research and practice. Psychother. Res. 22, 367–80. 10.1080/10503307.2012.683988 - DOI - PubMed
- Angus L., Levitt H., Hardtke K. (1999). The narrative processes coding system: research applications and implications for psychotherapy practice. J. Clin. Psychol. 55, 1255–1270. 10.1002/(SICI)1097-4679(199910)55:10<1255::AID-JCLP7> 3.0.CO ;2-F - DOI - PubMed
- Ayres L., Kavanaugh K., Knafl K. A. (2003). Within-case and across-case approaches to qualitative data analysis. Qual. Health Res. 13, 871–83. 10.1177/1049732303013006008 - DOI - PubMed
- Bacal H. A., Newman K. M., Vorspohl E. (1994). Objektbeziehungstheorien: Brücken zur Selbstpsychologie. Kraichtal: Friedrich Frommann Verlag Gunther Holzboog.
- Bargghaan D., Harfst T., Dirmaier J., Koch U., Schulz U. (2002). Bericht einer externen Evaluation und Qualitätssicherung der Hardtwaldklinik I, Bad Zwesten, Abteilung Psychotherapie und Psychosomatik. Nr. 1 Analyse von Struktur, Prozess und Outcome 2000–2001. Universitätsklinikum Hamburg-Eppendorf (Hamburg).
Related information
Grants and funding, linkout - more resources, full text sources.
- Europe PubMed Central
- Frontiers Media SA
- PubMed Central

- Citation Manager
NCBI Literature Resources
MeSH PMC Bookshelf Disclaimer
The PubMed wordmark and PubMed logo are registered trademarks of the U.S. Department of Health and Human Services (HHS). Unauthorized use of these marks is strictly prohibited.

IMAGES
VIDEO
COMMENTS
CASE STUDY 98. List 5 pieces of additional information you need to obtain from C.'s mother. ... In the given case, patient C. is a 20-year-old girl who is suffering from type-1 diabetes mellitus. She has returned from a trip to Mexico. She is suffering from high fever, with diarrhea and vomiting. ... System Disorder form - ATI template. Med ...
In burn patients, it is not uncommon to require 5000 kcals a day to meet increased metabolic demands of the body. I would also explain to her that increased protein. is needed for proper healing of burns as well. The benefits of increasing the caloric and protein intake of burn patient are decreasing weight loss, gut atrophy and the risk of sepsis.
ZEL (S#78 iniu rreiter Patients with Multiple Disorders 10 Student Case Study 98 TGA Name C oupe Class/Group _ Group Members Jacken Morgan ggo Domerz Megar Starzoni Cheeses Jugusor - Dayzha Hayden Name Date argel white Scenario You are working in the emergency department (ED) of a community hospital when the ambulance arrives with A.N., a 28-year-old woman who was involved in a house fire.
Oncologic and Hematologic Disorders. Page 411: Case Study 88. Page 415: Case Study 89. Page 419: Case Study 90. Page 423: Case Study 91. ... Patients with Multiple Disorders. Page 461: Case Study 98. Page 469: Case Study 99. Page 475: Case Study 100. Page 481: Case Study 101. Page 487:
The patient's mental status examination included the Montreal Cognitive Assessment (MoCA), a brief global screen of cognition , on which she scored 12/30. There was evidence of dysfunction across multiple cognitive domains . She was fully oriented to location, day, month, year, and exact date.
Video answers for all textbook questions of chapter 15, Patients with Multiple Disorders, Winningham's Critical Thinking Cases in Nursing by Numerade ... INSTRUCTIONS All questions apply to this case study. Your responses should be brief and to the point. When asked to provide several answers, list them in order of priority or significance.
On examination, the patient appeared to be in respiratory distress. The temperature was 35.9°C, the pulse 98 beats per minute, the blood pressure 129/58 mm Hg, the respiratory rate 24 breaths per ...
This case study aims to explore variables associated with a partial or limited treatment response to CBTand illustrate the challenges and variability in CBT treatment for major depressive disorder (MDD) in adolescence. CASE HISTORY AND SYMPTOMATOLOGY The patient was a 15-year-old Puerto Rican adoles-cent female living with both her parents and ...
Study with Quizlet and memorize flashcards containing terms like "An RN is the leader of a team caring for clients with gas-trointestinal (GI) disorders on a medical-surgical unit.The team includes a newly graduated RN who has recently completed hospital orientation, an experienced unlicensed assistive personnel (UAP), and a nursing student. The fol-lowing information about the six assigned ...
The adolescent was previously diagnosed with major depressive disorder and treated intermittently with supportive psychotherapy and antidepressants. ... M.I.J., Bernal, G., & Rossello, J. (2009). Clinical Case Study: CBT for Depression in A Puerto Rican Adolescent. Challenges and Variability in Treatment Response. Depression and Anxiety, 26, 98 ...
Study with Quizlet and memorize flashcards containing terms like Which two of the seven patients would be best to assign to the nurse who has floated from the medical-surgical unit? 1. Ms. B (borderline personality) and Ms. M (manic phase bipolar disorder) 2. Mr. D (major depression) and Ms. G (older patient with dementia)3. Mr. S (disorganized schizophrenia) and Mr. V (suicidal thoughts)4. Mr ...
In this multiple-case study, based on Yin and Campbell ... and (d) met the criteria for a common mental disorder. Patients had to have a common mental disorder operationalised as a PHQ-9 (Kroenke and Spitzer, 2002 ... 77-84. 10.1016/S0920-9964(98)00180-7 [Google Scholar] Damasio A. R. (2011). Selbst ist der Mensch. Körper, Geist und die ...
Background Depersonalization-derealization syndrome (DDS) is an underdiagnosed and underresearched clinical phenomenon. In Germany, its administrative prevalence is far below the threshold for orphan diseases, although according to epidemiological surveys the diagnosis should be comparable frequent as anorexia nervosa for instance. Against this background, we carried out a large comprehensive ...
The following case study focuses on finding the optimal treatment for a 78-year-old man. Test your knowledge by reading the question below and making the proper selection. A 78-year-old man presents with a three-year history of an elevated leukocyte count with recent fatigue and anemia. He has received two red blood cell transfusions in the ...
This case study examines the effect of a tailor-made physiotherapy regimen on an 85-year-old male patient who was suffering from bulbar motor neuron disease (MND) and had a history of stroke and COVID-19. The physiotherapy plan was designed to strategically address the patient's respiratory issues, generalized weakness affecting limb muscles, and speech and swallowing difficulties.
Describes treatment results in 33 8-69 yr old patients with multiple personality disorder with respect to the major identifying characteristic of the condition—the presence of separate personalities within a single individual. Responsiveness to treatment, apparent and stable fusion, follow-up, and reassessment are discussed. Findings show that most Ss reported a better quality of life and ...
Case studies are generally a single-case design, but can also be a multiple-case design, where replication instead of sampling is the criterion for inclusion. Like other research methodologies within psychology, the case study must produce valid and reliable results in order to be useful for the development of future research.
1. Introduction. Neurological disorders encompass a wide range of conditions that affect the nervous system, including the brain, spinal cord, and peripheral nerves [].These disorders can be debilitating, leading to significant impairments in motor function, cognition, behaviour, and overall quality of life [].Traditional treatment options for neurological disorders often provide limited ...
Study with Quizlet and memorize flashcards containing terms like Ms. B is a 68-year-old woman admitted to the medical unit through the emergency department (ED) after being hit in the abdomen by an automobile while walking home. An 18-gauge IV catheter was inserted in the left forearm, and normal saline was started at 100 mL/hr. *ED vital signs* were blood pressure, 118/80 mm Hg; heart rate ...
The patient in this case study had been diagnosed with schizophrenia and depression at a different hospital, with symptoms of auditory hallucinations and suicide attempts and a medical history that included pharmacotherapy and an inpatient treatment program. ... Lee JS, Nam JH. A case of multiple personality disorder. Ment Health Res. 1995; 14: ...
Methods: Using a multiple case study approach, we contrasted two client groups: those with moderately integrated and those with low-integrated personality structures, as defined by the operationalised psychodynamic diagnostic manual. Our exploration centered on specific factors of empowerment, therapy processes, and interventions.