

The Future of Peer Review
- Peer Review
Essential Science Conversations
February 2023
- Transcript (PDF, 84KB)
- Related resources (PDF, 110KB)
Many recent changes, coming from the White House, the academy, and advances in technology, have raised questions about the future of peer review. Is peer review worth saving? Should peer review processes be revised? How should reviewers’ work be recognized? Join us for an Essential Science Conversation on The Future of Peer Review.
This program does not offer CE credit.
Joanne Davila, PhD
Professor of psychology, Stony Brook University.
Craig Rodriguez-Seijas, PhD
Assistant professor of psychology, University of Michigan.
Jessica Schleider, PhD
Assistant professor of psychology, Stony Brook University.
Jasper Simons, MA
Chief publishing officer, APA.
Mitch Prinstein, PhD
Chief Science Officer, APA.
More in this series
The number of publications among graduate school/faculty applicants, or among those applying for tenure and promotion seems to have increased considerably
September 18, 2024 Live Webinar
Physical activity benefits mental and physical health, yet participation rates are declining.
May 2024 On Demand Webinar
Discussing AI's impact on psychological research: potential to replace human participants, unintended consequences, peer review challenges, and ethical considerations.
April 2024 On Demand Webinar
Panel discusses strategies to combat stigma across clinical, research, educational, and community settings.
March 2024 On Demand Webinar
- Current Students
Half-million-dollar grant will create peer review and science communication curriculum for grad students
- By Elise Proulx
- 3 min. read ▪ Published August 29
- Share on LinkedIn
- Share on Facebook
- Share on X (Twitter)
The ability to critically evaluate scientific literature is crucial for graduate students as they start their careers in science.
However, a lack of systematic training can hamper students’ future ability to review the work of others in their field.
“Reviewing scientific literature and analyzing literature is a huge part of graduate student education,” says Sarah Klass , a postdoctoral fellow in the Keasling Lab at UC Berkeley and the Joint Bioenergy Institute and the lead recipient of a $499,992, two-year grant from the National Science Foundation (NSF). “But there’s no formal education” on how to do it, Klass continues.
To attempt to remedy this disconnection, Klass and her partners will use the NSF grant to fund a new curriculum that will immerse graduate students in the sciences in the “principles and practices of peer review and science communication with a heavy emphasis on building practical skills.” Peer review is the system in which multiple experts review scientific papers to ensure quality before publication.
The team will spend the first year developing a curriculum. The second year, UC Berkeley grad students will put it to the test. The grant team, which will also include UC Berkeley School of Public Health professor Stefano M. Bertozzi and a to-be-determined team of UC Berkeley graduate students, will collect data on impact and effectiveness.
The proposed curriculum builds upon the success that the journal Rapid Reviews\Infectious Diseases ( RR\ID ) has had in making rigorous peer review faster and more efficient, partially by training UC Berkeley undergraduate students. RR\ID is an open-access journal that prioritizes rapid and efficient peer review alongside offering student training and mentoring and supporting the democratization of academic publishing through partnerships with a dozen academic institutions in low- and middle-income countries that will be established over the next three years. Bertozzi is the journal’s editor-in-chief
“As part of UC Berkeley Undergraduate Research Apprentice Program, RR\ID editors have offered a workshop allowing undergraduates to participate in research projects with faculty members for academic credit, focusing on topics of special interest,” the grant application reads. “The aim is to familiarize undergraduate students with contemporary scientific and academic research, peer review processes, and publication standards, particularly concerning infectious diseases.”
The new curriculum project will pilot a curriculum for a training program that will initially involve STEM graduate students enrolled at UC Berkeley, specializing in a broad spectrum of fields related to infectious diseases, data science, public health, engineering, and basic biological and chemical sciences. “By providing graduate students with the necessary tools and insights to critically evaluate scientific literature and review preprints, our goal is to improve graduate student research/literature comprehension and engagement with their respective STEM fields,” the team said.
“We are trying to teach good peer review skills to graduate students so they can help enable the rapid dissemination of scientifically vetted literature that can have an immediate impact on people’s lives,” says Klass.
“Above all, the intellectual discourse that needs to happen around science is closed off and isolated,” says Hildy Fong Baker, executive director of the UC Berkeley Center for Global Public Health and managing director of the project. “We are creating an avenue for people to be part of an ecosystem at the beginning of their careers.”
The course materials created during the two-year grant period will eventually be available to all via open access to encourage other institutions to adopt and adapt the curriculum worldwide.
People of BPH found in this article include:
- Stefano Bertozzi Professor, Health Policy and Management
More in category “School News”:
Meet our new faculty: xiudi li, alum melissa stafford jones on her career developing meaningful policy approaches in public health, uc berkeley school of public health welcomes inaugural cohort of impact fellows, new alumni association co-presidents are ready to foster engagement and make an impact.
Log in using your username and password
- Search More Search for this keyword Advanced search
- Latest content
- Current issue
- For authors
- New editors
- BMJ Journals
You are here
- Online First
- They are still children: a scoping review of conditions for positive engagement in elite youth sport
- Article Text
- Article info
- Citation Tools
- Rapid Responses
- Article metrics
- http://orcid.org/0000-0001-5244-6416 Stuart G. Wilson 1 ,
- http://orcid.org/0009-0000-1865-0915 Mia KurtzFavero 1 ,
- http://orcid.org/0000-0002-4616-2617 Haley H. Smith 1 ,
- http://orcid.org/0000-0003-1377-0234 Michael F Bergeron 2 ,
- http://orcid.org/0000-0002-3242-599X Jean Côté 1
- 1 School of Kinesiology & Health Studies , Queen's University , Kingston , Ontario , Canada
- 2 Performance Health , WTA Women’s Tennis Association , St. Petersburg , Florida , USA
- Correspondence to Dr Stuart G. Wilson; Stuart.wilson{at}queensu.ca
Objective The objective of this study is to characterise the key factors that influence positive engagement and desirable developmental outcomes in sport among elite youth athletes by summarising the methods, groups and pertinent topical areas examined in the extant published research.
Design Scoping review.
Data sources We searched the databases SPORTDiscus, APA PsycINFO, Web of Science and Sports Medicine & Education Index for peer-reviewed, published in English articles that considered the factors influencing positive developmental outcomes for athletes under 18 years competing at a national and/or international level.
Results The search returned 549 articles, of which 43 met the inclusion criteria. 16 studies used a qualitative approach, 14 collected quantitative data, 2 adopted mixed methods and 11 were reviews. Seven articles involved athletes competing in absolute skill contexts (ie, against the best athletes of any age) while the majority involved athletes competing in relative skill contexts (ie, against the best in a specific age or developmental group). The studies described the characteristics of the athletes, as well as their training, relationships with others, social and physical environments, and/or their overall developmental pathways.
Conclusion Existing research on positive engagement in elite youth sport aligned with and mapped onto established models of positive development in youth sport more generally. Our findings further support that, while certain youth athletes may demonstrate extraordinary performance capabilities, they are still children who benefit from positive engagement prompted and reinforced by developmentally appropriate and supportive activities, relationships and environments.
- Psychology, Sports
- Athletic Performance
Data availability statement
Data are available on reasonable request.
https://doi.org/10.1136/bjsports-2024-108200
Statistics from Altmetric.com
Request permissions.
If you wish to reuse any or all of this article please use the link below which will take you to the Copyright Clearance Center’s RightsLink service. You will be able to get a quick price and instant permission to reuse the content in many different ways.
X @SGWilsonQU, @mia_jkf, @hale_smith, @DrMBergeron_01, @jeancote46
Contributors SGW is the guarantor. JC and MFB conceived of the project. SGW, MK, HHS and JC designed and conducted the review. SGW, MK and JC drafted the paper, and all authors contributed to editing and revising the paper.
Funding This research was supported by a Research Grant from the International Olympic Committee (IOC) and an Insight Grant from the Social Sciences and Humanities Research Council of Canada (SSHRC Grant # 435-2020-0094).
Competing interests None declared.
Provenance and peer review Not commissioned; externally peer reviewed.
Read the full text or download the PDF:
Peer reviewers wanted: Help colleagues grow their teaching skills
Corie Farnsley Aug 26, 2024

Annual peer review of teaching training workshop is Sept. 24
Is this you?
- You have a talent for teaching, guiding, mentoring or serving.
- You have a heart for building up those around you.
- You are seeking opportunities to serve your colleagues while helping the Indiana University School of Medicine continue to provide world-class medical education for learners.
If yes, clear your schedule from 3 to 4:30 p.m. Tuesday, Sept. 24, and learn how you can get involved in peer review of teaching.
The annual Academy of Teaching Scholars session, Giving Great Teaching Feedback: How to Conduct a Peer Review of Teaching , is the first (required) step for becoming a peer reviewer. During this online session, you will learn to provide effective feedback to colleagues that can inspire change and improve learner experiences in the classroom, operating room, labs and clinical settings.
Who should attend
- Anyone interested in conducting peer reviews of teaching; the course is required for new reviewers
- Veteran reviewers who would like to refresh their skills and knowledge of peer review best practices
- Faculty who are interested in serving their school and peers on a flexible schedule can learn about important best practices and receive the resources they need to provide effective feedback.
- Faculty who wish to be promoted, gain tenure, earn awards, join honor societies or simply improve their teaching effectiveness should undergo multiple peer reviews of their teaching over the course of their time at IU School of Medicine. In addition to learner evaluations, peer reviews of teaching help faculty members documenting a holistic review of their teaching efforts. Faculty peer reviewers are an essential resource for fellow colleagues and for the school as a whole.
“Becoming a better educator requires one being open to feedback from both learners and peers,” said Matthew Holley, PhD, assistant dean for faculty affairs and professional development and the director of both the Academy of Teaching Scholars and the Peer Review of Teaching programs. “Using the feedback from a peer review, educators can spend time reflecting upon their work — acknowledging their strengths but also their potential areas for growth. By serving as a peer reviewer, you play an important role in the growth and development of educators.”
What the session will cover
- The administrative process IU School of Medicine uses to manage peer reviews
- The steps you should take to ensure an effective review
- The various reasons why faculty undergo review and how to adjust reviews to meet faculty needs
- Resources to efficiently conduct a peer review
- Examples of established reviewers' experiences conducting and completing reviews
Participants and session leaders will conduct a mini peer review as a group during the session.
Growth is never by mere chance; it is the result of forces working together.
James Cash Penney
Corie Farnsley
Corie is communications generalist for Indiana University School of Medicine Faculty Affairs and Professional Development (FAPD). She focuses on telling the story of FAPD by sharing information about the many opportunities the unit provides for individuals’ professional development, the stories behind how these offerings help shape a broad culture of faculty vitality, and ultimately the impact IU School of Medicine faculty have on the future of health. She is a proud IU Bloomington School of Journalism alumna who joined the IU School of Medicine team in 2023 with nearly 25 years of communications and marketing experience.
- Open access
- Published: 24 August 2024
The impact of religious spiritual care training on the spiritual health and care burden of elderly family caregivers during the COVID-19 pandemic: a field trial study
- Afifeh Qorbani 1 ,
- Shahnaz Pouladi 2 ,
- Akram Farhadi 3 &
- Razieh Bagherzadeh 2
BMC Nursing volume 23 , Article number: 584 ( 2024 ) Cite this article
98 Accesses
Metrics details
Family caregiving is associated with many physical and psychological problems for caregivers, but the effect of spiritual support on reducing their issues during a crisis is also the subject of research. The study aims to examine the impact of religious spiritual care training on the spiritual health and care burdens of elderly family caregivers during the COVID-19 pandemic.
The randomized controlled field trial involved 80 Iranian family caregivers in Bushehr City, who were selected by convenience sampling based on the inclusion criteria and divided into experimental (40 people) and control (40 people) groups by simple random sampling in 2021 and 2022. Data collection was conducted using spiritual health and care burden questionnaires using the Porsline software. The virtual intervention included spiritual and religious education. Four virtual sessions were held offline over two weeks. The first session was to get to know the participants and explain the purpose, The second session focused on the burden of care, the third on empowerment, and the fourth on mental health and related issues. In the control group, daily life continued as usual during the study.
Mean changes in existential health (3.40 ± 6.25) and total spiritual health (5.05 ± 11.12) increased in the intervention group and decreased in the control group. There were statistically significant differences between the two groups for existential health (t = 3.78, p = 0.001) and spiritual health (t = 3.13, p = 0.002). Cohen’s d-effect sizes for spiritual health and caregiving burden were 0.415 and 0.366, respectively. There was no statistically significant difference in mean changes in religious health ( p = 0.067) or caregiving burden ( p = 0.638) between the two intervention and control groups.
Given that the religious-spiritual intervention had a positive effect on existential health and no impact on religious health or care burden, it is recommended that comprehensive planning be undertaken to improve the spiritual health of family caregivers to enable them to better cope with critical situations such as a COVID-19 pandemic.
Trial registration
IRCT code number IRCT20150529022466N16 and trial ID number 48,021. (Registration Date2020/06/28)
Peer Review reports
With the global outbreak of COVID-19 on January 12, 2020, and the highly contagious nature of this virus, the World Health Organization issued protocols for limiting community interactions worldwide [ 1 ]. While individuals of all ages are susceptible to COVID-19, The high incidence of infection in older people, the greater severity of the disease, and the increased mortality are significant challenges in implementing appropriate preventive measures and future strategies to protect against this disease in the geriatric population [ 2 , 3 ]. According to the US Centers for Disease Control and Prevention, 31% of COVID-19 cases, 45% of hospitalizations, 53% of intensive care unit admissions, and 80% of COVID-19-related deaths in the United States occur in the elderly [ 4 ].
During the COVID-19 crisis, elderly people required various forms of assistance, including telephone and digital visits, with most of these services provided by family members [ 5 ], Park (2021) reported that long-term caregivers (> 1 year) had more negative somatic physical symptoms (headaches, body aches, and abdominal discomfort), worse mental health, and more significant fatigue than non-caregivers [ 6 ]. Family caregivers can only provide up to 80% of the required care to seniors with Multiple chronic conditions in the community, and they are also responsible for the majority of the costs and shoulder the related burden. This increased reliance on family caregivers has, in turn, heightened their care burden. The burden of care is a significant issue globally, with millions of individuals taking on caregiving responsibilities for their loved ones. The care burden encompasses various dimensions, including time-dependent, evolving, physical, social, and emotional aspects, making it a complex and highly individualized concept [ 7 ]. It often results from a negative imbalance between caregiving responsibilities and other obligations [ 8 ].
In Iran, like in many other countries, this burden can have profound implications on caregivers’ physical, emotional, and financial well-being. By introducing the concept of spiritual health into the discourse, we aim to shed light on a potentially overlooked aspect that could provide additional support and resilience to caregivers. Statistics indicate that caregivers who report a strong sense of spiritual well-being often exhibit lower levels of stress, anxiety, and depression, highlighting the importance of addressing this dimension in caregiving research. The existing literature on caregiver burden focuses mainly on caregiving’s physical and emotional aspects. While these studies provide valuable insights, there is a noticeable gap in understanding the role of spiritual health in mitigating the burden of care. Further exploration is needed to investigate how spiritual well-being can influence the overall caregiving experience and contribute to the well-being of the caregiver and the care recipient. In Iranians’ religious and national culture, the elderly hold a revered position and are highly respected. Reflecting on this cultural perspective, the Prophet of Islam stated, that respecting older people of my community is the same as respecting me [ 9 ]. This cultural context is evident in the fact that 86.4% of elderly individuals in Iran, according to statistics from the welfare organization, live with their children and spouses [ 10 ]. However, when caregiving responsibilities increase, they can overshadow the multiple health dimensions of the older people’s family members, including physical, psychological, social, and spiritual aspects. Coping strategies, such as spiritual-religious approaches, are often employed to manage the challenges [ 11 ].
There are two dimensions to spiritual health: religious and existential. Religious health refers to how a person understands his or her spiritual well-being when connected to a higher power. Conversely, existential health centers on an individual’s capacity for adaptation to their being, the societal landscape, and the broader environment [ 12 ]. In the past, the significance of spirituality in effectively managing stress was often underestimated; however, recent years have seen increased attention from researchers [ 11 , 13 , 14 ]. It is important to note that the understanding of spirituality is influenced by culture and religion, and its implications may vary for different individuals [ 15 ]. The current research gap lies in the lack of comprehensive studies that assess the intersection of spiritual health and care burden in the Iranian caregiving landscape. While some research exists on the broader topic of spirituality and health, there is a need for targeted investigations that consider the unique cultural and religious factors that shape the Iranian perspective on caregiving. Understanding these nuances can provide valuable insights into how spiritual care practices can be effectively integrated into support systems for caregivers in Iran. To the best of our knowledge, no previous study has investigated the impact of religious-spiritual care training on the spiritual health and care burden of family caregivers of older people during the COVID-19 pandemic. Given the critical role of nurses as caregivers for family and elderly health along with their supportive function [ 16 ], it is essential to identify caregivers at risk during critical situations and address their spiritual needs as part of community-oriented care. The study aimed to examine the impact of religious spiritual care training on the spiritual health and caregiving burden of older family carers during the COVID-19 pandemic. By thoroughly exploring the relationship between spiritual health and the caregiving burden of older family carers, we aim to identify potential strategies and interventions that can improve the well-being of caregivers and the overall quality of care provided to care recipients in Iran.
Study design
This study utilized a randomized controlled field trial design. The choice of a field randomized controlled trial for this study provides a rigorous and systematic approach to evaluating the effectiveness of a spiritual health intervention on care burden among Iranian caregivers. This design ensures internal validity, generalizability, and ethical soundness, thereby strengthening the overall quality of the research findings.
Participants and data collection
Participants were selected from the home care department of the comprehensive rehabilitation service center for the elderly in Mohammadieh, Bushehr City (affiliated with the welfare organization), and four comprehensive urban health centers in Bushehr Port, specifically Kheybar, Quds, Meraj, and Shohada centers. The inclusion criteria encompass caring for elderly individuals who showed a degree of dependence in at least one of their six daily activities, as defined by Katz’s criteria for activities of daily living (ADL). Additionally, caregivers had to possess literacy skills (reading and writing), with at least six months having elapsed since the commencement of their caregiving responsibilities. Furthermore, inclusion criteria require a family relationship between caregivers and elderly individuals in their care, cohabitation with older people, and delivering at least 40 h of care per week. Caregivers had to be at least 18-year-old Shia Muslims. The exclusion criteria dictated that the caregivers be excluded from the study under certain conditions, including the death of either the caregiver or the elderly individual during the study, refusal to continue participation in the study, the presence of neurological and psychiatric diseases, or the use of neuropsychiatric drugs, self-reported drug or alcohol addiction, or prior involvement in a spiritual-religious educational program related to elderly care.
Sample size
Based on the effect sizes observed in the studies by Hosseini et al. (2016) [ 17 ], Mahdavi et al. (2016) [ 18 ], and Moeini et al. (2012) [ 19 ], with a Type I error rate of 0.50 and a power of 80%, and using the G Power 3.1.9.2 software, the required sample size for the two-group test was approximately 80 individuals, with 40 participants in each group. Eligible elderly family caregivers were selected from available candidates and randomly assigned to either the test or control group (Fig. 1 ). Randomization was done using Random Allocation software and by a person who did not know the participants and did not know their characteristics.
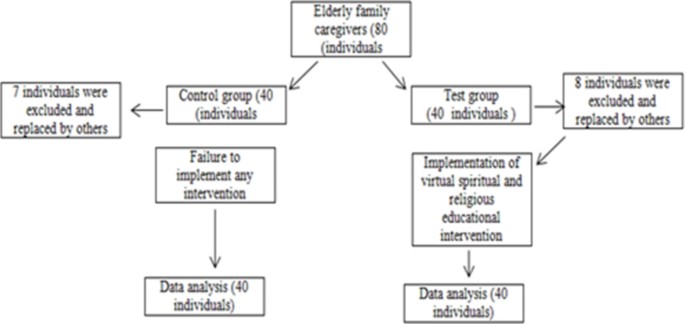
Consort diagram
Instruments
The data collection instruments used in this study consisted of a demographic information form, along with the spiritual health questionnaire developed by Paloutzian and Ellison (1982) and the care burden questionnaire designed by Novak and Guest (1989).
Demographic information form
This form collected information about the caregiver, including age, number of children, family relationship to older people, level of education, occupation, income, and type of housing.
Spiritual health questionnaire (Paloutzian and Ellison, 1982)
The Spiritual Health Questionnaire, developed by Paloutzian and Ellison in 1982, is widely used to assess an individual’s spiritual well-being and beliefs. This questionnaire consists of 20 items that explore different aspects of spirituality, including beliefs, practices, values, and experiences. Participants are asked to respond to statements about spirituality on a six-point Likert scale, with responses to agree strongly or to disagree strongly. This questionnaire includes two subscales: (1) Religious well-being (10 items): This subscale assesses how an individual’s religious beliefs, values, and practices contribute to their overall well-being and sense of purpose. (2) Existential well-being (10 items): This subscale focuses on the individual’s sense of meaning, purpose, and connection to something greater than themselves, regardless of religious affiliation. Each subscale receives a score from 10 to 60. The spiritual health score is the sum of these two subscales and ranges from 20 to 120. In Iran, during the research conducted by Parvizi et al. (2000), the reliability of this questionnaire using Cronbach’s alpha coefficient was 0.82 [ 20 ]. In Hamdami et al.‘s research (2015), Cronbach’s alpha coefficient of the total spiritual health score was 0.79 [ 21 ].
Care burden questionnaire (Novak and Guest, 1989)
The Care Burden Questionnaire, developed by Novak and Guest in 1989, is a widely used instrument for assessing the burden experienced by caregivers who provide care to individuals with chronic illnesses or disabilities. Caregivers are asked to respond to a series of statements concerning caregiving burden on a Likert scale, with response options typically ranging from 1 (Strongly Disagree) to 5 (Strongly Agree). The maximum score that can be attained on this questionnaire is 96, while the minimum score is 0. The questionnaire includes five sub-scales designed to capture a specific aspect of the burden. These include time demands, emotional stress, social isolation, financial strain, and conflicts with other responsibilities. In Iran, in the study of Abbasi et al. (2013), the Cronbach’s alpha coefficient of this questionnaire was 0.90, and its subscales ranged from 0.72 to 0.82 [ 22 ].
Baseline test
Before the intervention, research sessions were initially scheduled to occur in person; however, the coronavirus pandemic rendered it impractical to conduct face-to-face training sessions. As a result, spiritual and religious training was carried out online without impacting b behavioral therapy (CBT) and stress management techniques. It was structured to address the emotional, social, and physical dimensions of caregiver burden while simultaneously fostering coping strategies and self-care practices. The intervention framework was informed by existing research on caregiver interventions, CBT, and stress management. Studies have shown the effectiveness of psychoeducational programs in reducing caregiver burden and enhancing well-being. The incorporation of CBT techniques aimed to help caregivers identify and reframe negative thought patterns, while stress management strategies were included to help caregivers better cope with stressors.
In the test group, the intervention took the form of spiritual care based on the model of Richards and Bergin, which was aligned with Islamic teachings. This model featured six key steps: First, caregivers were guided to pay attention to spiritual-cultural sensitivities. Second, they were trained to establish an open and secure spiritual relationship. Third, potential ethical challenges were addressed. Fourth, caregivers conducted a religious and spiritual assessment of clients. The fifth step involved defining suitable goals for spiritual therapy, and the final step focused on properly implementing spiritual interventions [ 23 ]. The educational sessions covered various dimensions of the care burden, including physical, mental, social, and financial elements, as well as facets of spiritual health, which included the religious dimension (about communication with a transcendent higher power) and the existential dimension (encompassing communication with oneself, creation, and all living beings). These educational sessions were delivered via pre-recorded video presentations developed by a specialist in geriatric nursing and religious education. Participants engaged in four virtual sessions offline, conducted through WhatsApp social messenger, with two sessions held per week. Each session involved the following activities: (1) Following up on the previous session’s topics; (2) providing feedback to participants; (3) summarizing and outlining previous topics to create a connection between the topics discussed; and (4) offering explanations and summaries related to the new session’s topic. One month after the end of the intervention, test and control group participants completed the Mental Health Questionnaire and the Carer’s Burden Questionnaire again. The control group continued with their daily lives as usual throughout the study. Upon its conclusion, the educational materials on spirituality and its various concepts, which had been shared via WhatsApp Messenger, were made available in alignment with the ethical principles that govern such research. The educational content for the sessions was developed by a multidisciplinary team consisting of a nurse psychiatrist, a gerontologist, and a Specialist in Quran and Hadith. The educational content was designed and compiled by the research team to improve practical skills, stress management, self-care, and communication, based on the model of Richards and Bergin and according to the teachings of Islam and the Shia religion. To ensure the accuracy and reliability of the content, the educational materials underwent a rigorous review process involving experts from diverse fields, including caregiving, psychology, and Quranic and Hadith sciences. Feedback from caregivers and pilot testing were also used to refine and validate the content before implementation. A pilot study was conducted to test the intervention’s feasibility, acceptability, and initial effectiveness. The pilot study involved a small group of caregivers who received the intervention, and their feedback was used to refine the program before full implementation. All contributors implementing the intervention received comprehensive training on the educational content and intervention protocols. These trainings were followed daily by viewing the participants’ WhatsApp to receive educational content and listening to audio files, making daily phone calls, and asking them questions over the phone to understand the content and express their questions. The intervention was implemented by a team of trained healthcare professionals, including a social gerontologist, a nursing gerontologist, and a medical-surgical nursing student with a master’s degree. They all had relevant qualifications and expertise in mental health and caregiving support. Potential challenges for implementers could include caregiver resistance, emotional distress, not receiving training materials on time, or difficulty engaging participants. The plan for dealing with such situations included regular monitoring of caregiver progress, open communication, and flexibility in the delivery of sessions. For participants who required more specialized training or support beyond the scope of the intervention, referrals were made through telephone communication with the training session facilitators. Response data from the instruments, such as the Care Burden Questionnaire and other assessment measures, were collected through self-report questionnaires and standardized rating scales administered by trained assessors. Caregivers were asked to respond based on their experiences before and after the intervention. To handle ambiguities in the response data, assessors were trained to clarify any uncertainties or ambiguities in the questions with caregivers. This involved providing clear explanations, and examples, and ensuring that caregivers understood the questions before responding. A specific post-intervention assessment time point was established to standardize the time after the intervention for all participants. This time point was determined based on the intervention duration and the optimal timeframe for assessing the intervention’s impact on caregiver burden based on past studies [ 24 , 25 ]. Caregivers were scheduled for the post-intervention assessment at this standardized time point to ensure consistency across all participants.
Ethical considerations
This study originated from a master’s thesis in internal surgical nursing at the Faculty of Midwifery Nursing, Bushehr University of Medical Sciences, with an ethics code number of IR.BPUMS.REC.1399.042. It is also registered with the Clinical Trial Centre of Iran under IRCT20150529022466N16. The caregivers were furnished with comprehensive information about the study, encompassing its objective, methodology, potential hazards and advantages, confidentiality protocols, and their entitlement to withdraw from the study at any point. Informed consent was obtained from all participants before they participated in the study. Measures were taken to ensure the confidentiality of participants’ personal information and data collected during the study. Participants were assured that their responses would be anonymized, stored securely, and only accessed by authorized research staff.
Data analysis
Due to the peak of the Corona pandemic and the closing of universities in person, the possibility of consulting statistics professors and performing data analysis was delayed for eight months. The data collected during the study were analyzed using SPSS version 19 software. The Shapiro-Wilk test was used to check the distribution of the data. An independent t-test, or Mann-Whitney test, was used to compare quantitative demographic variables between two groups. A Chi-squared or Fisher’s exact test was used to compare qualitative demographic variables between groups. To test the hypotheses above, a paired t-test was employed to ascertain the mean of the primary variables in question, before and after the intervention in each group. An independent t-test was utilized to determine the mean of the variables between groups, and Cohen’s d was calculated as the effect size. Independent t-tests were conducted to compare the mean scores of the changes. The significance level was assumed to be less than 0.05 in all cases.
No statistically significant differences were detected between the groups in terms of demographic variables, suggesting group homogeneity ( p > 0.05) (Tables 1 and 2 ). Regarding spiritual health, within the intervention group, the post-test average score for total spiritual health was significantly higher than the pre-test score ( p = 0.007), in contrast within the control group, the post-test average score was considerably lower than the pre-test score ( p = 0.003). No statistically significant differences were observed between the two groups in terms of mean posttest spiritual health scores (Table 3 ) still, changes in overall spiritual health increased in the intervention group and decreased in the control group, with statistically significant differences between the two groups ( p = 0.002) (Table 4 ). The Cohen’s d effect size for the difference in spiritual health between the intervention and control groups was 0.415, indicating a moderate effect of the intervention (Table 3 ). Within-group analysis showed no statistically significant differences between pre-and post-test scores for total care burden in either group. Furthermore, no statistically significant differences between the two groups were observed in terms of average care burden scores ( p < 0.05) (Table 5 ). Likewise, the average changes in care burden scores between the intervention and control groups showed no statistically significant differences ( p < 0.05) (Table 6 ). The Cohen’s d effect size for the difference in caregiving burden between the intervention and control groups was 0.366, indicating a moderate effect of the intervention on caregiving burden, although not statistically significant (Table 5 ).
This study aimed to evaluate the impact of religious spiritual care training on the spiritual health and care burden experienced by elderly family caregivers in Bushehr during the COVID-19 pandemic. The findings of this study suggest that a religious and spiritual intervention approach can effectively promote existential health and overall spiritual well-being. However, it was observed that this approach did not yield a notable impact on religious health or care burden. The Scores for existential health and overall spiritual health increased in the intervention group after the training, while they decreased in the control group. The mean change in religious health scores between the two groups did not reach statistical significance. These findings are consistent with the study conducted by Sayyadi et al. (2018) [ 26 ], who also observed an increase in spiritual health following a religious psychotherapy intervention. In this study, most family caregivers in the experimental and control groups initially demonstrated moderate to high levels of spiritual health. Similarly, Sayyadi et al. (2018) found higher spiritual health scores in medical and nursing students compared to other student populations. To explain and interpret the consistent findings regarding the positive effects of spiritual health on caregivers in the study by Sayyadi et al. and the current study on the impact of religious spiritual care training on elderly family caregivers, we can consider several factors that may contribute to these findings: (1) Spiritual health is often associated with providing a sense of support, purpose and coping mechanisms during challenging times. Caregivers facing the stress and demands of caregiving may benefit from a solid spiritual foundation to help them navigate their roles and find meaning in their experiences. Studies may have highlighted the role of spiritual health as a resource for caregivers to cope with the emotional and psychological challenges they face. (2) Spiritual health can help to build resilience and foster hope in individuals, including caregivers. By nurturing their spiritual well-being, caregivers may develop a sense of resilience that enables them to cope with adversity and maintain a positive outlook. Studies may have observed the positive impact of spiritual health on caregivers’ resilience and hope, leading to improved well-being and outcomes. (3) Spiritual health is often linked to personal growth and making sense of one’s experiences [ 27 ]. Caregivers possessing a robust spiritual foundation may engage in meaning-making processes, facilitating the discovery of purpose and significance within their caregiving journey. Studies may have underscored the role of spiritual health in promoting personal growth and facilitating meaning-making among caregivers. These factors, alongside the consistent focus on spiritual health across studies, provide a robust framework for understanding the positive impact of spiritual health on caregivers. Recognizing the importance of spiritual well-being within the broader context of caregiver health, and integrating interventions that specifically address spiritual needs, can contribute to improved outcomes and well-being for caregivers. This is supported by the findings of both Sayyadi et al. and the present study. It is important to note that the religious health scores did not increase after the intervention in the current study. The intervention, centered on religious and spiritual care training, had a significant impact on both existential well-being and overall spiritual health. The caregiver survey of palliative care patients will likely target different aspects of spiritual well-being, such as hope and general well-being. In interpreting these results, it is essential to consider the unique components of each intervention and how they may have influenced different aspects of spiritual health. On the other hand, Casalerio et al. (2024) in the study: Promoting Spiritual Coping of Family Caregivers of an Adult Relative with Severe Mental Illness: Development and Test of a Nursing Intervention, reported that the spiritual and religious intervention for caregivers increased their spiritual health dimension and their religious dimension [ 28 ]. These contrasting religious findings with the current study suggest that the effectiveness of religious and spiritual interventions may vary depending on the specific focus and approach of the intervention. Caregivers’ responses to such interventions may be influenced by factors such as the nature of the caring role, the context of the carer’s condition, and individual preferences regarding spirituality and religiosity. Further research and tailored interventions may be needed to address the diverse spiritual needs of caregivers in different care contexts.
Regarding the care burden, the results of the current study demonstrated no statistically significant differences in the average care burden scores within and between the groups. This result contrasts with previous studies by Polat et al. (2024), Xavier et al. (2023) [ 13 , 29 ], Partovirad et al. (2024) [ 11 ], Hekmatpour and colleagues (2018) [ 30 ], Shoghi et al. (2018) [ 31 ], which showed reductions in the care burden following intervention models and the current study care burden result align with previous studies by Khalili et al. (2024) [ 32 ], Salmoirago-Blotcher et al. (2016) [ 33 ], and Karadag Arli (2017) [ 34 ]. One of the reasons why the present study did not show the same effect of spiritual and religious interventions in reducing caregiver burden as similar studies have shown is probably due to the high caregiver burden in the relevant situation. In the present study, caregiver burden had increased due to the conditions of the Corona pandemic, and reducing caregiver burden may require more extended, and more social interventions. One potential explanation for the lack of reduction in care burden scores in the current study is the influence of social interaction theory and attachment theory. These theoretical frameworks emphasize the significance of the dynamic interplay between caregiver and care recipient, particularly highlighting the role of mutual appreciation and non-violent communication in mitigating caregiver burden [ 35 ]. The physical and mental conditions of care recipients, coupled with their inability to engage in appropriate interactions with caregivers during the COVID-19 crisis, may have intensified the care burden. Furthermore, a review of similar studies reveals that most interventions aimed at reducing care burden were conducted over longer periods than our study. These studies typically involved a higher number of sessions, ranging from 8 to 12 (e.g., Mohammadi and Babaei (2018) [ 36 ], Rahgooy et al. (2018) [ 37 ], Sotoudeh et al. (2018) [ 38 ] and Salehinejad et al. (2017) [ 39 ] Consequently, the shorter duration and fewer sessions in our study may have limited the effectiveness of the intervention in reducing the care burden. Additionally, the limitations imposed by social distancing measures may have exacerbated the needs of elderly individuals, leading to an increased caregiver burden. Furthermore, a review of similar studies reveals that most interventions aimed at reducing care burden were conducted over more extended periods than our study. These studies typically involved a higher number of sessions, ranging from 8 to 12 (e.g., Mohammadi and Babaei (2018) [ 30 ], Rahgooy et al. (2018) [ 32 ], Sotoudeh et al. (2018) [ 39 ] and Salehinejad et al. Consequently, the shorter duration and fewer sessions in our study may have limited the effectiveness of the intervention in reducing the care burden.
Limitations
This study had limitations. The limitations imposed by the pandemic, including the need for social distancing, made it impossible to conduct face-to-face training sessions and deprived participants and carers of the opportunity for close, face-to-face communication during the spiritual and religious intervention. This limitation may have affected the participants’ internal beliefs, emotions, and motivations. The restrictions imposed by the pandemic, through the utilization of routine telephone communications and collaboration with pertinent academic staff, exemplify adaptability and ingenuity in maintaining communication with participants. This multi-channel approach may have helped to ensure continued engagement and support for participants throughout the intervention. Despite the challenges posed by the lack of face-to-face communication, the study managed to keep participants engaged through alternative means. The regular phone calls and coordination with the professors may have fostered a sense of connection and support, potentially enhancing participants’ overall experience and engagement with the intervention. The lack of face-to-face interaction during the spiritual and religious intervention may have limited the depth of participants’ engagement and the impact on their internal beliefs and motivations. This limitation could affect the validity of the study findings, as face-to-face communication is often crucial for building trust and rapport in interventions of this nature. The short duration of the intervention and the constraints imposed by the pandemic may have limited the generalizability of the study results. Further research utilizing more extended intervention periods and more diverse participant groups may enhance the generalizability of the findings to a broader population. Utilizing virtual platforms for interactive sessions and group discussions could facilitate the replication of the advantages of face-to-face communication and cultivate a sense of community among participants. Conducting long-term follow-up studies to track the sustained effects of spiritual and religious interventions on caregiver burden could provide valuable insights into the lasting impact and effectiveness of the intervention over time.
Based on the study, the results were mixed. The religious and spiritual intervention was effective in improving existential health and overall spiritual health but did not have a significant impact on religious health and caregiving burden. The training in religious and spiritual care was determined to be effective in enhancing the existential well-being of elderly family caregivers, as evidenced by an increase in their sense of meaning, purpose, and fulfillment in the caregiving role. The intervention demonstrated effectiveness in improving caregivers’ overall spiritual health, suggesting positive outcomes in terms of emotional well-being, connectedness, and resilience. Notwithstanding the favorable outcomes in existential and general spiritual well-being, the intervention did not demonstrate a notable impact on religious well-being and caregiver burden, underscoring domains that may warrant further investigation and the development of alternative intervention strategies. It is crucial to recognize the intricate nature of caregiving dynamics and the various ways in which spirituality and religion can impact the well-being of caregivers. The result of the study indicates that integrating religious and spiritual care training could effectively enhance the existential and holistic spiritual well-being of elderly family caregivers. Practitioners and caregivers can utilize this intervention to foster a greater sense of meaning and spiritual well-being within the caregiving context. In addition, the study highlights the importance of personalized interventions that consider individual differences in spiritual beliefs and coping strategies. In conclusion, while the religious and spiritual intervention showed promising results in improving certain aspects of the spiritual health of elderly family caregivers in Bushehr, further research is needed to address the nuances of religious health and care burden. By carefully considering these key findings and implications, practitioners and researchers can tailor interventions to better support caregivers’ holistic well-being in the face of challenges such as the COVID-19 pandemic.
Data availability
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
Na Zhu DZ, Wang W, Li X, Yang B, Song J, Zhao X, Huang B, Shi W, Lu R, Niu P, Zhan F. A novel coronavirus from patients with pneumonia in China, 2019. 2020:727–33. https://www.nejm.org/doi/pdf/ https://doi.org/10.1056/NEJMoa2001017
Dhama K, Patel SK, Kumar R, Rana J, Yatoo MI, Kumar A, et al. Geriatric population during the COVID-19 pandemic: problems, considerations, exigencies, and beyond. Front Public Health. 2020;8:574198. https://doi.org/10.3389/fpubh.2020.574198
Article PubMed PubMed Central Google Scholar
Zhang J, Wang J, Liu H, Wu C. Association of dementia comorbidities with caregivers’ physical, psychological, social, and financial burden. BMC Geriatr. 2023;23(1):60. https://doi.org/10.1186/s12877-023-03774-9
Shahid ZKR, McClafferty B, Kepko D, Ramgobin D, Patel R. COVID-19 and older adults: what we know. J Am Geriatr Soc. 2020;68(5):926–9. https://doi.org/.1111/jgs.16472 . Epub 2020 Apr 20. PMID: 32255507; PMCID: PMC7262251.
Moradi M, Navab E, Sharifi F, Namadi B, Rahimidoost M. The effects of the COVID-19 pandemic on the elderly: a systematic review. J Salmand: Iran J Ageing. 2021;16(1):2–29. https://doi.org/10.3389/fpubh.2020.574198
Article Google Scholar
Park SS. Caregivers’ mental health and somatic symptoms during COVID-19. J Gerontol B Psychol Sci Soc Sci. 2021;76(4). https://doi.org/10.1093/geronb/gbaa121 . PMID: 32738144; PMCID: PMC7454918.
Malmir S, Navipour H, Negarandeh R. Exploring challenges among Iranian family caregivers of seniors with multiple chronic conditions: a qualitative research study. BMC Geriatr. 2022;22(1):270. https://doi.org/10.1186/s12877-022-02881-3
Phillips R, Durkin M, Engward H, Cable G, Iancu M. The impact of caring for family members with mental illnesses on the caregiver: a scoping review. Health Promot Int. 2023;38(3). https://doi.org/10.1093/heapro/daac049 . PMID: 35472137; PMCID: PMC10269136.
jaafari zadeh H, SmS K, rahgozar M. Health care status of elderly people with disabilities in District 13 of Tehran Municipality and their problems. Journal of Urmia Nursing And Midwifery Faculty. 2006;4(2):67–81.
Nafei ARV, Ghafori R, Khalvati M, Eslamian A, Sharifi D, et al. Death anxiety and related factors among older adults in Iran: findings from a National Study. Salmand Iran J Ageing. 2024;19(1):144–57. https://doi.org/10.32598/sija.2023.1106.1
Partovirad M, Rizi S, Amrollah Majdabadi Z, Mohammadi F, Hosseinabadi A, Nikpeyma N. Assessing the relationship between spiritual intelligence and care burden in family caregivers of older adults with chronic diseases. 2024. https://doi.org/10.21203/rs.3.rs-4343106/v1
Davarinia Motlagh Quchan A, Mohammadzadeh F, Mohamadzadeh Tabrizi Z, Bahri N. The relationship between spiritual health and COVID-19 anxiety among nurses: a national online cross-sectional study. Sci Rep. 2024;14(1):16356. https://doi.org/10.1038/s41598-024-67523-7
Article CAS PubMed PubMed Central Google Scholar
Türkben Polat H, Kiyak S. Spiritual well-being and care burden in caregivers of patients with breast cancer in Turkey. J Relig Health. 2023;62(3):1950–63. https://doi.org/10.1007/s10943-022-01695-2 . Epub 2022 Dec 5. PMID: 36469230; PMCID: PMC9734401.
Article PubMed Google Scholar
Francesco Chirico KB, Batra R, Ferrari G, Crescenzo P. Spiritual well-being and burnout syndrome in healthcare: asystematic review. School of Medicine Faculty Publications. 2023;15(3). https://doi.org/10.19204/2023/sprt2
Rezaei H, Niksima SH, Ghanei Gheshlagh R. Burden of care in caregivers of Iranian patients with chronic disorders: a systematic review and meta-analysis. Health Qual Life Outcomes. 2020;18(1):261. https://doi.org/10.1186/s12955-020-01503-z . PMID: 32746921; PMCID: PMC7398060.
Kurtgöz A, Edis EK. Spiritual care from the perspective of family caregivers and nurses in palliative care: a qualitative study. BMC Palliat Care. 2023;22(1):161. https://doi.org/10.1186/s12904-023-01286-2
Hosseini MA, Mohammadzaheri S, Fallahi Khoshkenab, Mohammadi Shahbolaghi M, Reza Soltani F, Sharif Mohseni M. Effect of mindfulness program on caregivers’ strain on Alzheimer’s disease caregivers. Salmand: Iran J Ageing. 2016;11(3):448–55. https://doi.org/10.21859/sija-1103448
Mahdavi B, Fallahi-Khoshknab M, Mohammadi F, Hosseini MA, Haghi M. Effects of spiritual group therapy on caregiver strain in-home caregivers of the elderly with Alzheimer’s disease. Arch Psychiatr Nurs. 2017;31(3):269–73. https://doi.org/10.1016/j.apnu.2016.12.003
Moeini M, Ghasemi TMG, Yousefi H, Abedi HJIjon, Research M. The effect of spiritual care on the spiritual health of patients with cardiac ischemia. 2012;17(3):195. https://pubmed.ncbi.nlm.nih.gov/23833611/
Parvizi S, Allahbakhshian M, Jafarpour allavi M, Haghani H. The relationship between spiritual health and quality of life in multiple sclerosis patients. Zahedan J Res Med Sci. 2000;12(3):29–33. https://civilica.com/doc/963361/
Google Scholar
Hamdami M, GHasemi jovineh R, Zahrakar K, Karimi K. The role of spiritual health and mindfulness in students’ psychological capital. Res Med Educ. 2015;8(2):2736. https://doi.org/10.18869/acadpub.rme.8.2.27
Abbasi A, Ashraf Rezaei N, Asayesh H, Shariati A, Rahmani H, Molaei E, et al. Relationship between caregiving pressure and coping skills of caregivers of patients undergoing hemodialysis. Urmia School Nurs Midwifery. 2011;10(4):533–9.
Pouladi S ss, Bahreyni M, Bagherzadeh R. The effect of spiritual-religious psychotherapy on self-concept and sense of coherence in cancer patients of Bushehr City, 2017–2018. Bushehr University of Medical Sciences.
Modarres MAS. Effect of religion-based spirituality education on happiness of postmenopausal women: an interventional study. Health Spiritual Med Ethics. 2021;8(1):44–54. https://doi.org/10.29252/jhsme.8.1.44
Jahdi F, mA B, Mahani M, Behboudi Moghaddam Z. The effect of prenatal group care on the empowerment of pregnant women. Payesh. 2014;13(2):229–34.
Sayyadi M, Sayyad S, Vahabi A, Vahabi B, Noori B, Amani M. Evaluation of the spiritual health level and its related factors in the students of Sanandaj Universities, 2015. Shenakht J Psychol Psychiatry. 2019;6(1):1–10. https://doi.org/10.22122/cdj.v6i3.332
Koburtay TJD, Aljafari A. Religion, spirituality, and well-being: a systematic literature review and futuristic agenda. Bus Ethics Environ Responsib. 2023;32(1):41–57. https://doi.org/10.1111/beer.12478
Casaleiro TMH, Caldeira S. Promoting spiritual coping of family caregivers of an adult relative with severe mental illness development and test of a nursing intervention. Healthcare. 2024;12(13). https://doi.org/10.3390/healthcare12131247
Xavier FT, Esperandio MRG. Spirituality and caregiver burden of people with intellectual disabilities: an empirical study. Int J Latin Am Religions. 2023;7(1):17–35. https://doi.org/10.1007/s41603-023-00196-8
Hekmatpour DB, EM.Dehkordi LM. The effect of patient care education on the burden of care and the quality of life of caregivers of stroke patients. Multidisciplinary Healthc. 2019;12(2):7–11. https://doi.org/10.2147/JMDH.S232970 . PMID: 30936715; PMCID: PMC6430991.
Shoghi MN, Seyedfatemi., Shahbazi B. M S. The effect of family-center empowerment model(FCEM) on the care burden of the patient of children diagnosed with cancer. 2019;20(6):1757–68. https://doi.org/10.31557/APJCP.2019.20.6.1757
Khalili Z, Habibi E, Kamyari N, Tohidi S, Yousofvand V. Correlation between spiritual health, anxiety, and sleep quality among cancer patients. Int J Afr Nurs Sci. 2024;20:100668. https://doi.org/10.1016/j.ijans.2024.100668
Salmoirago-Blotcher EFG, Leung K, Volturo G, Boudreaux E, Crawford S, et al. An exploration of the role of religion/spirituality in the promotion of physicians’ well-being in emergency medicine. Prev Med Rep. 2016;1(3):189–95. https://doi.org/10.1016/j.pmedr.2016.01.009 . PMID: 27419014; PMCID: PMC4929145.
Karadag Arli SBA, Erisik E. An investigation of the relationship between nurses’ views on spirituality and spiritual care and their level of burnout. J Holist Nurs. 2017;35(3):214–20. https://doi.org/10.1177/0898010116652974 . Epub 2016 May 30. PMID: 27241132.
Jafari M, Alipour F, Raheb G, Mardani M. Perceived stress and burden of care in elderly caregivers: the moderating role of resilience Salmand. Iran J Ageing. 2022;17(1):62–75. https://doi.org/10.32598/sija.2021.2575.2
Mohammadi F, Babaie M. The impact of participation in support groups on spiritual health and care burden of elderly patients with Alzheimer’s family caregivers. Iran J Ageing. 2012;12(19):29–37. https://salmandj.uswr.ac.ir/article-1-374-en.html
Rahgooy AF, Sojoudi M. T. Investigating the effect of the empowerment program on the care burden of mothers with children with phenylketonuria and the level of phenylalanine in the children’s serum. TEHRAN: University of Rehabilitation Sciences and Social Welfare; 2016.
Sotoudeh RPS, Alavi M. The effect of a family-based training program on the care burden of family caregivers of patients undergoing hemodialysis. Iran J Nurse Midwifery Res. 2019;24(2):144. https://doi.org/10.4103/ijnmr.IJNMR_93_18 . PMID: 30820227; PMCID: PMC6390430.
Salehi Nejad S, Azami M, Motamedi F, Bahaadinbeigy K, Sedighi B, Shahesmaili A. The effect of web-based information intervention in caregiving burden in caregivers of patients with dementia. J J Health Biomedical Inf. 2017;4(3):181–91. https://www.sid.ir/fa/VEWSSID/J_pdf/3007513960302.pdf
Download references
Acknowledgements
We would like to express our gratitude to the Student Research Committee, the Persian Gulf Martyrs Hospital’s Clinical Research Development Center, and all the elderly caregivers who participated in this research, as their contributions were invaluable.
Research expenses by the vice president of research and the student research committee of Bushehr University of Medical Sciences, Iran, have been paid.
Author information
Authors and affiliations.
Bushehr University of Medical Sciences, Bushehr, Islamic Republic of Iran
Afifeh Qorbani
Nursing and Midwifery Faculty of Bushehr, University of Medical Sciences, Bushehr, Islamic Republic of Iran
Shahnaz Pouladi & Razieh Bagherzadeh
Persian Gulf Tropical Medicine Research Center, Persian Gulf Biomedical Sciences Research Institute, Bushehr University of Medical Sciences, Bushehr, Islamic Republic of Iran
Akram Farhadi
You can also search for this author in PubMed Google Scholar
Contributions
AQ: Student. Author of the article. SH: Supervisor, the editor, preparation of educational packages. AF.: Consultant professor, the editor, preparation of educational packages. RB: Consultant professor of statistics department, the editor.
Corresponding author
Correspondence to Shahnaz Pouladi .
Ethics declarations
Ethical approval and consent to participate.
The research has an ethics code number of IR.BPUMS.REC.1399.042 from the Research Vice-Chancellor of Bushehr University of Medical Sciences. All study participants provided written informed consent.
Consent for publication
Not Applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/ .
Reprints and permissions
About this article
Cite this article.
Qorbani, A., Pouladi, S., Farhadi, A. et al. The impact of religious spiritual care training on the spiritual health and care burden of elderly family caregivers during the COVID-19 pandemic: a field trial study. BMC Nurs 23 , 584 (2024). https://doi.org/10.1186/s12912-024-02268-2
Download citation
Received : 29 May 2024
Accepted : 16 August 2024
Published : 24 August 2024
DOI : https://doi.org/10.1186/s12912-024-02268-2
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Caregiver burden
- Spirituality
BMC Nursing
ISSN: 1472-6955
- General enquiries: [email protected]
- Open access
- Published: 28 August 2024
Transforming simulation in healthcare to enhance interprofessional collaboration leveraging big data analytics and artificial intelligence
- Salman Yousuf Guraya 1
BMC Medical Education volume 24 , Article number: 941 ( 2024 ) Cite this article
10 Altmetric
Metrics details
Simulation in healthcare, empowered by big data analytics and artificial intelligence (AI), has the potential to drive transformative innovations towards enhanced interprofessional collaboration (IPC). This convergence of technologies revolutionizes medical education, offering healthcare professionals (HCPs) an immersive, iterative, and dynamic simulation platform for hands-on learning and deliberate practice. Big data analytics, integrated in modern simulators, creates realistic clinical scenarios which mimics real-world complexities. This optimization of skill acquisition and decision-making with personalized feedback leads to life-long learning. Beyond clinical training, simulation-based AI, virtual reality (VR), and augmented reality (AR) automated tools offer avenues for quality improvement, research and innovation, and team working. Additionally, the integration of VR and AR enhances simulation experience by providing realistic environments for practicing high-risk procedures and personalized learning. IPC, crucial for patient safety and quality care, finds a natural home in simulation-based education, fostering teamwork, communication, and shared decision-making among diverse HCP teams. A thoughtful integration of simulation-based medical education into curricula requires overcoming its barriers such as professional silos and stereo-typing. There is a need for a cautious implantation of technology in clinical training without overly ignoring the real patient-based medical education.
Peer Review reports
Simulation in healthcare, powered by big data analytics (BDA) and artificial intelligence (AI), stands at the forefront of transformative innovations with a promise to facilitating interprofessional collaboration (IPC). This convergence of technologies towards educational philosophies not only revolutionizes medical training but also enhances the quality of care and patient safety in an IPC climate for an efficient delivery of healthcare system [ 1 ]. Simulation in healthcare showcases a controlled, versatile, and safe environment for healthcare professionals (HCPs) from diverse disciplines to engage in hands-on learning with deliberate practice [ 2 ]. Learners are engrossed in immersive, iterative, and interactive climate which can nurture opportunities for the acquisition of transferable psychomotor and cognition-based skills [ 3 ]. A simulated environment nurtures the real jest of life-long learning where learners can be trained by deliberate practice till the acquisition of their skills.
BDA, embedded in modern cutting-edge simulators, can utilize enormous healthcare data for clinical training and skills acquistion [ 4 ]. For instance, Bateman and Wood employed Amazon’s Web Service to accumulate a complete human genomic scaffold including 140 million individual base pairs by adopting an advanced hashing algorithm [ 5 ]. Later, a BDA platform successfully matched patients’ data of children in hospital to their whole-genome sequencing for the management of potentially incurable clinical conditions [ 6 ]. From another perspective, leveraging clinical scenarios with realism, BDA can be a valuable tool in reflecting the complexities of the real-world medical practice. This data-driven approach diligently mimics the variability and inconsistency encountered in real clinical settings, preparing HCPs for diverse patient encounters and crisis management. Artificial intelligence (AI) with its machine learning algorithm (MLA) and natural language processing (NLP) further fortifies the impact of simulation by enabling adaptive learning experiences [ 7 ]. Moreover, AI-powered patient simulators with automated interfaces can demonstrate high fidelity realistic physiological responses such as pulse, blood pressure, breathing patterns, and facial expressions to allow learners to practice decision-making in lifelike scenarios. By analyzing simulation data, institutions can identify trends, best practices, and areas for improvement, ultimately enhancing patient outcomes and advancing medical knowledge.
Applications of BDA harness the experimental usage of electronic health records, medical imaging, genetic information, and patients’ demographics. By aggregating and analyzing this data, simulation platforms can create realistic scenarios that can be used by learners for clinical reasoning and critical decision-making. Additionally, MLA and NLP have the ability to predict disease prognosis, treatment efficacy, and unwanted outcomes, thereby offering a reliable hub for interactive and immersive learning for HCPs [ 8 ]. MLA and NLP encourage adaptive learning experiences by analyzing learner interactions and performance in real-time. This unique opportunity of acquiring skills mastery with personalized feedback either by simulator, peer, or facilitator makes simulation a master-class educational and training tool for all HCPs. For instance, if a learner consistently makes errors in decision-making or a procedural skill, a smart simulator can tailor further exercises to provide targeted practice opportunities for individual learners.
Clinical training is interposed at the crossroads of adopting AI, virtual reality (VR), and augmented reality (AR) technologies. Beyond training, simulation-driven medical education holds immense potential for quality improvement and research in healthcare [ 9 ]. VR and AR technologies offer immersive experiences that simulate clinical settings with unprecedented realism. VR headsets transform learners into a cyber space where they deal with animations, digital images, and a host of other exercises in virtual climate [ 10 ]. AR overlays digital information onto the physical world, allowing learners to visualize anatomical structures, medical procedures, or patient data in real-time. Moreover, VR and AR can be used to perform high risk medical procedures till the complete acquisition of skill mastery. Such opportunity is not possible due to threats to patient safety and limited time for learners’ training in real-world workplaces [ 11 ]. At the same time, the mapping of learners’ needs with the curriculum is possible only in simulated environment where learners’ expectations can be tailored to meet their learning styles [ 11 ]. AI, VR, and AR technologies in healthcare simulators essentially empower learners to develop clinical expertise, enhance patient care, and drive innovations in healthcare delivery.
An example of integration of AI, NP, ML, and certain other algorithms in simulation is the sepsis management of a virtual patient being managed by a team of HCPs from different healthcare disciplines. A patient presents with fever, confusion, and rapid breathing in the emergency room. AI platform creates a detailed medical record of the patient with past hospital visits, medications, allergies, and baseline health metrics. AI simulates patient’s symptoms in real-time with tachycardia, tachypnea, hypotension, and fever. The trainees interview the virtual patient and AI responds, using NLP, by providing coherent and contextually appropriate answers. The trainees order a set of tests, including blood cultures, a complete blood count, and lactate levels. AI presents realistic test results where blood cultures show a bacterial infection, leukocytosis, and elevated lactate levels. Based on the diagnosis of sepsis, the trainees plan treatment which typically includes oxygen, broad-spectrum antibiotics, and intravenous fluid. AI then adjusts the patient condition based on the trainees’ actions which may lead to improvement in clinical parameters. However, a delayed treatment could lead to worsening symptoms such as septic shock. Furthermore, AI can introduce complications if initial treatments were ineffective or if the trainees commit errors. Thereupon, AI provides real-time feedback on the trainees’ decisions which can highlight missed signs, suggest alternative diagnostic tests, or recommend adjustments to treatment plans. Lastly, AI would generate a summary report of the performance with a breakdown of diagnostic accuracy, treatment efficacy, and adherence to clinical guidelines. MLAs analyze patterns in patient data to assist in diagnosis. In this context, decision trees and neural networks of MLAs analyze vast datasets of patient records to create realistic virtual patients with diverse medical histories and clinical conditions.
There has been a proliferation of empirical research about the powerful role of IPC in medical education [ 12 , 13 ]. IPC fosters shared decision-making, role identification and negotiations, team coherence, and mitigates potential errors [ 14 ]. Through simulated scenarios, HCPs learn to navigate interdisciplinary challenges, appreciate each other’s roles, and develop a shared approach to patient care. Additionally, simulation in healthcare faces the challenges of costs, access, development, and ethical considerations. Nevertheless, the integration of simulation, BDA, VR, AR, and AI heralds a new era of IPC in healthcare, where learning, practice, and innovation converge to shape the future of medicine.
The overarching goal of all healthcare systems focuses on patient safety as reiterated by the World Health Organization (WHO) sustainable development goals [ 15 ]. General Medical Council, Irish Medical Council, Canada MEDs, Accreditation Council for Graduate Medical Education, and EmiatesMEDS are also in agreement with WHO and, in this context, IPC can potentially enhance the quality of care and patient safety [ 16 ]. Though the role of IPC is widely accepted, there is a lukewarm response from medical institutions about its integration into the existing curricula. Professional silos, stereotyping, bureaucratic inertia, and resistant mindsets are some of the deterring factors [ 17 ]. In the era of simulation in healthcare, IPC can be efficiently embedded into this technology-powered educational tool for impactful collaborative teamwork. By harnessing the technological power of VR, AR, and AI, simulation platforms can leverage the indigenous advantage of IPC in clinical training. Once skills acquisition is accomplished in the simulated platform, its recreation in the real world would be a seamless transition of transferable skills.
To sum up, despite an exponential growth in the use of technology-driven simulation in healthcare, educators should be mindful of its careful integration in medical curricula. Clinical training on real patients cannot be replaced by any strategy or tool regardless of its perceived efficiency or effectiveness. Bearing in mind the learning styles of our learners with a preference toward fluid than crystalloid verbal comprehension and fluid reasoning, technology-driven simulation plays a vital role in medical education. A thoughtful integration of simulation pitched at certain courses and modules spiraled across the curriculum will enhance the learning experience of medical and health sciences students and HCPs [ 18 ].
Data availability
No datasets were generated or analysed during the current study.
Choudhury A, Asan O. Role of artificial intelligence in patient safety outcomes: systematic literature review. JMIR Med Inf. 2020;8(7):e18599.
Article Google Scholar
Higgins M, Madan CR, Patel R. Deliberate practice in simulation-based surgical skills training: a scoping review. J Surg Educ. 2021;78(4):1328–39.
Watts PI, McDermott DS, Alinier G, Charnetski M, Ludlow J, Horsley E, et al. Healthcare simulation standards of best practiceTM simulation design. Clin Simul Nurs. 2021;58:14–21.
Chrimes D, Moa B, Zamani H, Kuo M-H, editors. Interactive healthcare big data analytics platform under simulated performance. 2016 IEEE 14th Intl Conf on Dependable, Autonomic and Secure Computing, 14th Intl Conf on Pervasive Intelligence and Computing, 2nd Intl Conf on Big Data Intelligence and Computing and Cyber Science and Technology Congress (DASC/PiCom/DataCom/CyberSciTech); 2016: IEEE.
Bateman A, Wood M. Cloud computing. Oxford University Press; 2009. p. 1475.
Twist GP, Gaedigk A, Miller NA, Farrow EG, Willig LK, Dinwiddie DL, et al. Constellation: a tool for rapid, automated phenotype assignment of a highly polymorphic pharmacogene, CYP2D6, from whole-genome sequences. NPJ Genomic Med. 2016;1(1):1–10.
Winkler-Schwartz A, Bissonnette V, Mirchi N, Ponnudurai N, Yilmaz R, Ledwos N, et al. Artificial intelligence in medical education: best practices using machine learning to assess surgical expertise in virtual reality simulation. J Surg Educ. 2019;76(6):1681–90.
Li WT, Ma J, Shende N, Castaneda G, Chakladar J, Tsai JC, et al. Using machine learning of clinical data to diagnose COVID-19: a systematic review and meta-analysis. BMC Med Inf Decis Mak. 2020;20:1–13.
Google Scholar
Caffò AO, Tinella L, Lopez A, Spano G, Massaro Y, Lisi A, et al. The drives for driving simulation: a scientometric analysis and a selective review of reviews on simulated driving research. Front Psychol. 2020;11:917.
Hsieh M-C, Lee J-J. Preliminary study of VR and AR applications in medical and healthcare education. J Nurs Health Stud. 2018;3(1):1.
Forgione A, Guraya SY. The cutting-edge training modalities and educational platforms for accredited surgical training: a systematic review. J Res Med Sci. 2017;22(1):51.
Sulaiman N, Rishmawy Y, Hussein A, Saber-Ayad M, Alzubaidi H, Al Kawas S, et al. A mixed methods approach to determine the climate of interprofessional education among medical and health sciences students. BMC Med Educ. 2021;21:1–13.
Guraya SY, David LR, Hashir S, Mousa NA, Al Bayatti SW, Hasswan A, et al. The impact of an online intervention on the medical, dental and health sciences students about interprofessional education; a quasi-experimental study. BMC Med Educ. 2021;21:1–11.
Wei H, Corbett RW, Ray J, Wei TL. A culture of caring: the essence of healthcare interprofessional collaboration. J Interprof Care. 2020;34(3):324–31.
Organization WH. Global patient safety action plan 2021–2030: towards eliminating avoidable harm in health care. World Health Organization; 2021.
Guraya SS, Umair Akhtar M, Sulaiman N, David LR, Jirjees FJ, Awad M, et al. Embedding patient safety in a scaffold of interprofessional education; a qualitative study with thematic analysis. BMC Med Educ. 2023;23(1):968.
Supper I, Catala O, Lustman M, Chemla C, Bourgueil Y, Letrilliart L. Interprofessional collaboration in primary health care: a review of facilitators and barriers perceived by involved actors. J Public Health. 2015;37(4):716–27.
Guraya SS, Guraya SY, Al-Qahtani MF. Developing a framework of simulation-based medical education curriculum for effective learning. Med Educ. 2020;24(4):323–31.
Download references
Acknowledgements
Not applicable.
Author information
Authors and affiliations.
Vice Dean College of Medicine, University of Sharjah, Sharjah, United Arab Emirates
Salman Yousuf Guraya
You can also search for this author in PubMed Google Scholar
Contributions
This is a sole author manuscript. Salman Guraya conceived, prepraed, revieweed, revised, and finalized this editorial artcile.
Corresponding author
Correspondence to Salman Yousuf Guraya .

Ethics declarations
Ethics approval and consent to participate, consent for publication.
Not applicable as this is an editorial article.
Competing interests
Corresponding author is a senior editorial board memeber of the BMC Medical Education.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/ .
Reprints and permissions
About this article
Cite this article.
Guraya, S.Y. Transforming simulation in healthcare to enhance interprofessional collaboration leveraging big data analytics and artificial intelligence. BMC Med Educ 24 , 941 (2024). https://doi.org/10.1186/s12909-024-05916-y
Download citation
Received : 06 May 2024
Accepted : 14 August 2024
Published : 28 August 2024
DOI : https://doi.org/10.1186/s12909-024-05916-y
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Big data analytics
- Augmented reality
- Virtual reality
- Artificial intelligence
- Medical education
BMC Medical Education
ISSN: 1472-6920
- General enquiries: [email protected]
- Open access
- Published: 26 August 2024
The impact of surge capacity enhancement training for nursing managers on hospital disaster preparedness and response: an action research study
- Alireza Shafiei 1 ,
- Narges Arsalani 2 ,
- Mehdi Beyrami Jam 3 &
- Hamid Reza Khankeh ORCID: orcid.org/0000-0002-9532-5646 4
BMC Emergency Medicine volume 24 , Article number: 153 ( 2024 ) Cite this article
42 Accesses
Metrics details
Introduction
Hospitals as the main providers of healthcare services play an essential role in the management of disasters and emergencies. Nurses are one of the important and influential elements in increasing the surge capacity of hospitals. Accordingly, the present study aimed to assess the effect of surge capacity enhancement training for nursing managers on hospital disaster preparedness and response.
All nursing managers employed at Motahari Hospital in Tehran took part in this interventional pre- and post-test action research study. Ultimately, a total of 20 nursing managers were chosen through a census method and underwent training in hospital capacity fluctuations. The Iranian version of the “Hospital Emergency Response Checklist” was used to measure hospital disaster preparedness and response before and after the intervention.
The overall hospital disaster preparedness and response score was 184 (medium level) before the intervention and 216 (high level) after the intervention. The intervention was effective in improving the dimensions of hospital disaster preparedness, including “command and control”, “triage”, “human resources”, “communication”, “surge capacity”, “logistics and supply”, “safety and security”, and “recovery”, but had not much impact on the “continuity of essential services” component.
The research demonstrated that enhancing the disaster preparedness of hospitals can be achieved by training nursing managers using an action research approach. Encouraging their active participation in identifying deficiencies, problems, and weaknesses related to surge capacity, and promoting the adoption and implementation of suitable strategies, can enhance overall hospital disaster preparedness.
Peer Review reports
Hospitals, as the main providers of healthcare services, play an essential role in managing and reducing the suffering of injured people in emergencies and disasters [ 26 ]. Most of the definitive, life-saving and emergency care for injured people are carried out in hospitals. Therefore, the preparedness of hospitals is essential in moderating and decreasing the negative health consequences of disasters [ 29] . From an international perspective, the Sendai Framework for Disaster Risk Reduction 2015–2030 and World Health Organization (WHO), highlights the need for disaster preparedness and risk reduction measures in hospitals [ 30 , 31 ]. Based on WHO, the preparedness and well-trained hospital personnel is the main factor in minimizing the casualties and damages resulting from disasters. Therefore, assessing and improving hospitals’ capacity and preparedness for disasters is a crucial first step toward effective disaster response and achieving the objectives outlined in the Sendai Framework 2015–2030 [ 30 , 32 ].
In Iran, efforts to enhance hospitals’ disaster preparedness began in the winter of 2009 with the creation of the National Hospital Disaster Preparedness Plan (NHDPP) by the Health Research Center on Disasters at the University of Social Welfare and Rehabilitation Sciences. This initiative, serving as a national guideline, received backing from the Secretariat of the Disaster Health Working Group in the Ministry of Health and was communicated to all hospitals across the country [ 1 ]. Furthermore, in the third phase of Iran’s hospital accreditation program, criteria for disaster risk management were added in the form of seven standards and thirty-seven measurements, directly addressing the hospital’s preparedness and response to emergencies and disasters [ 2 ].
To effectively address disasters, a hospital needs a thorough preparedness strategy, necessary tools, equipment, sufficient space, skilled staff, and, in essence, enough surge capacity [ 33 ]. Surge capacity refers to the ability to acquire additional resources during a disaster or emergency. It is the ability to provide quickly the usual functions beyond the increased demand for experienced staff, medical care, and social health services. Surge capacity has three core components including staff, stuff, and structures [ 3 ].
Nurses are one of the major groups of healthcare providers in hospitals(staff) [ 4 ]. They have the most contact with patients and provide the most care [ 5 ]. Along with other disaster management teams, they also play crucial roles in planning, education and training, response, and recovery for hospital disaster preparedness [ 6 , 7 ].
Experiences have shown that training and exercises before the occurrence of disasters can significantly increase the ability of people to face critical situations such as natural disasters [ 4 , 6 ]. Therefore, providing effective disaster training for nurses has a crucial role in increasing hospital preparedness and capacity for response to disasters. Previous studies have demonstrated inadequate training for nurses on preparedness and response to emergencies and disasters [ 2 , 4 , 5 , 6 ]. Moreover, despite numerous investigations assessing the preparedness of Iranian hospitals for disasters [ 8 , 9 , 10 ], to the best of our knowledge, only a limited number of interventional studies have explored the impact of disaster training for nurses on enhancing hospital disaster preparedness in Iran. Hence, recognizing the crucial contributions of nurses to the development of hospital capacity, this research aimed to examine the effects of training of surge capacity enhancement for the nursing managers on the emergency and disaster preparedness of Motahari Hospital in Iran.
Study design and settings
The current investigation utilized a pretest-posttest interventional design, conducted at Shahid Motahari Burn Hospital, affiliated with Iran University of Medical Sciences in Tehran, Iran. This hospital is the first and only main and specialized center providing medical services to burn patients in the center of the country and plays an essential role in the management of the injured during disasters and emergencies, especially fires.
Population and sampling
Aligned with the study’s goals, we employed a census sampling method to select all nursing managers at Shahid Motahari Hospital in Tehran. The eligibility criteria encompassed individuals within the nursing profession, such as nursing managers, supervisors, and head nurses, who held a minimum of a bachelor’s degree and possessed a minimum of one year of managerial experience. Those who expressed unwillingness to participate in the study were excluded.
The data was collected using the Persian version of the Hospital Emergency Response Checklist developed by Khankeh et al. (2013) [ 34 ]. The checklist was used to estimate the current state of preparedness of hospitals and healthcare centers. The original version of this tool was formulated by the World Health Organization [ 35 ]. The checklist measures 9 key components including command and control (7 items), triage (10 items), human resources (15 items), communication (9 items), surge capacity (13 items), logistics and supply management (10 items), safety and security (10 items), continuity of essential services (8 items) and post-disaster recovery (8 items). The reliability and validity of the Persian version of the tool have been confirmed by Karimian et al. (2013) [ 14 ]. They confirmed the validity of the tool (CVI = 0.86) and its reliability with Cronbach’s alpha of 0.83. The items in the checklist are rated on a 3-point scale (1 = due for review, 2 = in progress, and 3 = completed).
Moreover, the hospital surge capacity guideline was used to examine the current situation, weaknesses, problems, and target actions and develop a hospital surge capacity training program. This guidance was formulated by the Health in Emergency and Disaster Research Center at the University of Social Welfare and Rehabilitation Sciences and approved and disseminated by the Iranian Ministry of Health [ 34 ].
Intervention
This intervention study adopted a participatory action research approach as the participants were involved in problem identification and intervention to improve the process. Research in action is a type of study used by people to change unfavorable situations into relatively favorable situations and finally improve procedures in their workplace [ 11 ]. Action research is a type of study that attempts to learn and understand purposeful interventions meant to bring about desired changes in the organizational environment [ 12 ]. Action research simultaneously promotes problem-solving and expands scientific knowledge, as well as strengthens the skills of research participants [ 13 ].
In general, in action research, participants are involved in all stages of the research, from identifying the problem and collecting the data to planning, implementation, and evaluation. The engagement of participants in all stages of the research will encourage their participation in the research procedure and make them interested in the research topic [ 7 ].
This study adopted Streubert Speziale and Carpenter’s five-step action research method [ 7 ]. These steps include (1) defining the problem (explaining the current situation), (2) collecting, analyzing, and interpreting data, (3) planning, (4) implementing, and (5) evaluating. In this research, nurses actively engaged in elucidating the issue, gathering and analyzing data related to hospital surge capacity, devising and executing capacity-enhancing strategies based on their training, and assessing these measures to enhance hospital disaster preparedness and response.
To collect the data, the required permits were obtained from the hospital managers and officials. Besides, some instructions about the research procedure and data gathering were provided in a briefing session for the participants. The researcher and the participants made the required arrangements and plans for conducting the training intervention. In the next step, the items on the instruments (the Hospital Emergency Response Checklist) were completed by the participants(pre-test). When completing the checklist, the officials and managers of the hospital were also interviewed to better identify the problems and challenges related to the surge capacity. After that, topics and concepts related to increasing surge capacity and hospital disaster preparedness were taught to the participants during a two-day workshop, and they did round table exercises. Following the National Hospital Emergency Preparedness and Response Instructions [ 1 ], the content of the workshop included hospital risk and hazard assessment, incident command system, early warning system, response plan, and enhancing hospital capacity in response to emergencies and disasters with emphasis on solving problems and weaknesses identified in the pre-intervention stage. After completing the training workshop, the participants were given a six-month opportunity to carry out interventions and transfer the training to other staff and nurses. During this period, the participants and other members of the disaster risk management committee attended meetings held every two weeks. In these meetings, the necessary actions for the next two weeks were set, and the officials to manage each action were specified. In addition, in each meeting, the extent to which the goals of the previous meeting were achieved and the reasons for not fulfilling them were discussed. Finally, the items in the Hospital Emergency Response Checklist were completed for the second time (post-test) and the collected data was analyzed.
Ethical considerations
To comply with ethical protocols, this research project was approved with the code of ethics of the Ethics Committee of the University of Rehabilitation Sciences and Social Health. Moreover, informed consent was obtained from all the participants. The participants completed the checklists anonymously and, they were assured that their participation was voluntary and had no impact on their evaluation procedure.
The participants in this study were 20 nursing managers and supervisors at Motahari Burn Hospital in Iran. The study participants had an average age of 38 years (30 to 52 years old) and an average work experience of 16 years (4 to 25 years). Most of the participants were female (15 persons), married (18 persons), had a bachelor’s degree (12 persons), and had served in managerial positions (9 persons). Table No. 1 Shows other demographic characteristics of the participants. The surge capacity enhancement strategies that were recognized and put into practice by the participants throughout the study(6 months) included: 1- Executing a memorandum with retired personnel and reactivating them when necessary, Executing a memorandum with the Iran University of Medical Sciences to hire students if needed, drafting instructions for requesting staff from the relevant authorities such as the Emergency Operations Center (EOC) of the Ministry of Health, in the realm of enhancing “staff” capacity. 2- Preparing and reserving medications and essential equipment for a minimum duration of 72 h, signing a memorandum with other hospitals and nearby health centers to provide equipment in emergencies, and also creating more water storage volume to be used in emergencies and disasters, in the realm of enhancing “stuff” capacity. 3- Identifying suitable non-clinical and clinical spaces in the Motahhari Hospital to place beds and admit patients during disasters and emergencies, concluding an agreement with a school near the hospital to provide physical space for the hospital, creating a new rehabilitation department in the hospital, enlarging the space of the emergency department in the realm of increasing “space” capacity. And, 4- developing plans and instructions necessary to manage the risk of emergencies and disasters, doing training and practice in the hospital, in the realm of enhancing “system” capacity. The data showed that hospital disaster preparedness was at an average level (184) before the intervention and reached the optimal level (216) after the intervention. Also, the results also demonstrated that, except for “continuity of essential services”, the intervention improved the hospital’s disaster preparedness score across all dimensions. Most notably, the intervention enhanced “surge capacity” by 10 units and “staff” by 6 units. For detailed information on the intervention’s effects on hospital preparedness dimensions, please refer to Table No. 2 .
This study aimed to examine how providing action research training to nursing managers enhances surge capacity and contributes to improving hospital disaster preparedness. Many hospitals may face numerous challenges due to inadequate preparedness in the face of disasters and the increased demand for healthcare services [ 36 , 37 ]. The results of this study indicated that implementing the surge capacity enhancement intervention for nursing managers and officials led to a 32-unit improvement in disaster preparedness at Motahari Hospital. This improvement was expected because surge capacity is one of the most important components of hospital disaster preparedness and response.
Regarding the impact of the intervention on enhancing hospital disaster preparedness, various studies have been conducted in Iran, each employing distinct approaches to bolster preparedness.
In a study conducted by Karimiyan et al. (2013), it was found that hospital preparedness training aligned with the national plan significantly enhanced the hospital’s preparedness to address emergencies and disasters [ 14 ]. Delshad et al. (2015) showed early warning system training improved the preparedness of Motahari Hospital in emergencies and disasters [ 15 ]. Also, Salawati et al. (2014) in another study, examined the effect of teaching and applying non-structural hospital safety principles for nurses on the preparedness of medical departments of several private and public hospitals in Tehran during disasters [ 16 ]. The findings indicated that the safety score of two non-structural and functional parts of the hospital safety index increased after the intervention. The authors concluded that teaching and applying non-structural safety principles to nurses improves hospital safety and preparedness [ 16 ].
Like numerous other hospitals in Iran [ 17 , 18 , 19 ], Motahari Hospital’s disaster preparedness status was assessed as moderate before the intervention. Nevertheless, some studies have indicated inadequacies in the preparedness level of the examined hospital. For example, both the investigation conducted by Hekmatkhah et al. [ 20 ] and that of Ojaghi et al. [ 21 ] revealed insufficient preparedness in the hospitals under examination.
The current study demonstrated that enhancing the hospital’s response capacity and hospital’s disaster preparedness across various components can be achieved through capacity-building training for nursing managers through action research. The greatest effect of the intervention in this study was on “surge capacity” and the “human resource” dimension(staff). This outcome can be primarily attributed to instructing the hospital surge capacity-building principles for participants in the training workshop. Additionally, due to steps were taken to augment capacity in terms of “human resources”, “medication, and equipment”. Two studies conducted in Iran have identified a shortage of human resources and equipment as a primary factor contributing to the limited preparedness of hospitals in dealing with disasters [ 22 , 23 ]. In this research, the re-employment of retired employees and the use of university students were among the most important strategies that were adopted to increase the hospital capacity and preparedness in the human resource dimension. Similarly, Dowlati et al. (2021) reported that the preparation of a list of employers from other hospitals and medical centers, including clinics and health students, is one of the most important strategies to increase the capacity of hospital staff to respond to chemical, biological, and nuclear hazards and disasters [ 38 ].
The results of this study show that the intervention improved the hospital preparedness scores in the “triage” and “command and control” dimensions. In this context, the educational intervention on triage by Rahmati and colleagues enhances the preparedness of the emergency department, as highlighted in their study [ 24 ]. Also, Delshad et al. conducted a study where actions such as designating an external location for triage and formulating a strategy for the postponement of elective surgeries contributed to an improvement in the hospital preparedness score [ 15 ].
The results of this study emphasize that enhancing hospital preparedness can be achieved through conducting a needs assessment, recognizing gaps within the organization as identified by study participants, and effectively communicating and raising awareness among hospital managers. In this context, Karimian et al. (2013) underscored the importance of providing additional training for officials, managers, and hospital staff concerning emergency preparedness and response in hospitals [ 14 ].
The data in the present study indicated the intervention had a smaller impact on the components of “continuity of essential services”, “logistics and supply”, and “safety and security” compared to other components of hospital preparedness. Perhaps one of the main reasons was the restricted timeframe of the study and limited financial resources to carry out capacity-building and preparedness measures in these dimensions. As stated earlier, measures to increase the surge capacity and improve preparedness were formulated and followed up during the meetings of the emergency and disaster risk committees. Since these meetings were held every two weeks, the 6-month timeframe of the study did not leave an opportunity to carry out measures to improve the mentioned components. Furthermore, the limited financial resources can be considered one of the main reasons for not carrying out the actions planned by the committee. The findings of the “logistics” and “essential services” are consistent with the findings of the study by Ingrassia et al. (2016). This study showed that hospital preparedness in these dimensions was poor [ 25 ]. The findings concerning the " logistics and supply” as well as the “countiniuty of essential services “dimensions in this research align with the outcomes observed in Ingrassia et al.‘s (2016) study, highlighting the inadequate preparedness of the hospital in these aspects [ 25 ].
Limitations
The study was constrained by a limited duration of 6 months and insufficient financial resources, restricting the ability to implement further measures to enhance hospital preparedness. Future investigations could overcome these limitations by extending the study period to at least one year and ensuring adequate financial resources. Furthermore, as this study solely assessed the impact of the intervention on the disaster preparedness level of a single hospital, statistical analysis could not be conducted due to the absence of mean and standard deviation data. The alterations were solely presented descriptively.
This study examined the effect of surge capacity training using an action research plan on disaster preparedness and response at Shahid Motahari Hospital in Tehran. The results showed that surge capacity enhancement training for nursing managers and officials increased their sensitivity to the importance of hospital emergency preparedness and response. Furthermore, their proactive involvement in recognizing capacities, deficiencies, problems, and weaknesses with appropriate tools and taking measures to address them can improve hospital emergency preparedness and response. The findings indicated that senior managers within the hospital can instigate changes through the provision of financial backing and the implementation of mandatory protocols.
Data availability
The datasets that were used and/or analyzed during the current study are available from the corresponding author upon reasonable request.
HamidReza Khankeh. Hospital Disaster preparedness: National Program. Iran: Publications of University of Welfare and Rehabilitation Sciences; 2013.
Google Scholar
Abbasabadi M, Khankeh H, Mosadegh Rad AM. Designing of disaster risk management accreditation standards in iranians hospitals. Int J Qual Health Care. 2018;30(suppl2):45–6.
Article Google Scholar
Kaji A, Koenig KL, Bey T. Surge capacity for healthcare systems: a conceptual framework. Acad Emerg Med. 2006;13(11):1157–9.
Article PubMed Google Scholar
Al Harthi M, Al Thobaity A, Al Ahmari W, Almalki M. Challenges for nurses in disaster management: a scoping review. Risk Manage Healthc Policy. 2020:2627–34.
Imani Eea. Awareness of nurses about crisis management and related factors. J Health Care. 2011;13(4):10–8.
Al Thobaity A, Plummer V, Williams B. What are the most common domains of the core competencies of disaster nursing? A scoping review. Int Emerg Nurs. 2017;31:64–71.
Al Thobaity A, Alamri S, Plummer V, et al. Exploring the necessary disaster plan components in Saudi Arabian hospitals. Int J Disaster Risk Reduct. 2019;41:101–316.
Janati A, Sadeghi-Bazargani H, Hasanpoor E, Sokhanvar M, HaghGoshyie E, Salehi A. Emergency response of Iranian hospitals against disasters: a practical framework for improvement. Disaster Med Public Health Prep. 2018;12:166–71.
Hosseini S, Izadfar A, Rajabzadeh R, Sadeghi M, Sadeghi A. Assessing the levels of preparedness against disaster of the hospitals in North Khorasan; Iran, in 2016. J Biol Todays World. 2017;6:191–5.
Naser WN, Ingrassia PL, Aladhrae S, Abdulraheem WA. A study of hospital disaster preparedness in South Yemen. Prehosp Disaster Med. 2018;33:133–8.
UNDERSTANDING PARTICIPATORY ACTION RESEARCH: CM. A QUALITATIVE RESEARCH METHODOLOGY OPTION. Can J Action Res. 2012;13(2):34–50.
Braa K, Vidgen RT. Interpretation, intervention and reduction in the organizational laboratory: a framework for in-context information systems research. Inf Organ. 1999;9(1):25–47.
Hult M, Lennung S. Towards a definition of action research: a note and bibliography. J Manage Stud. 1980;17:241–50.
Karimiyan A, Khankeh H, Dalvandi A. Effect of hospital preparedness principles based on a national plan on readiness to respond to disasters in Shahid Motahari Tehran, 2013. Tehran: university of social welfare and rehabilitation sciences; 2013.
Delshad Ve. Early warning system and disaster preparedness in Motahari Hospital. J Res Dev Nurs Midwifery. 2015;12(2):51–8.
Salevaty J, Khankeh HR, Dalvandi A, Delshad V. The impact of nurses training and applying functional and nonstructural hospital safety in preparedness of Razi and day hospitals in disasters based on Hospital Safety Index. 2015.
Bazyar J, Pourvakhshoori N, Safarpour H, Farrokhi M, Khankeh HR, Daliri S, et al. Hospital disaster preparedness in Iran: a systematic review and meta-analysis. Iran J Public Health. 2020;49(5):837.
PubMed PubMed Central Google Scholar
Kazemzadeh M, Shafiei E, Jahangiri K, Yousefi K, Sahebi A. The preparedness of hospital emergency departments for responding to disasters in Iran; a systematic review and meta-analysis. Archives of Academic Emergency Medicine. 2019;7(1).
Amiri Me. Preparedness of Affiliated hospitals of universities in North of Iran to confront disasters. Hosp J. 2013;12(1):19–28.
Hekmatkhah A, Rahimi H, Kamali Aghdam M, Taghavi Shahri M, Sadeghifar J, Hamouzadeh P. Assessing the preparedness rate againest earthquake risk in hospitals affiliated to urmia university of medical sciences 2011. J Urmia Nurs Midwifery Fac. 2012;10(2):0.
Ojaghi S, Nourizadeh S, MAHBOUBI M, Khazaei A, NAJAFI GA. Disaster crisis handling preparedness level of hospitals in Kermanshah. 2009.
Mahdaviazad H, Abdolahifar GR. Assessing hospital disaster preparedness in Shiraz, Iran 2011: teaching versus private hospitals. Am J Disaster Med. 2013;8(1):65–73.
Djalali A, Castren M, Khankeh H, Gryth D, Radestad M, Öhlen G, et al. Hospital disaster preparedness as measured by functional capacity: a comparison between Iran and Sweden. Prehosp Disaster Med. 2013;28(5):454–61.
Rahmati H, Azmoon M, Kalantari Meibodi M, Zare N. Effects of triage education on knowledge, practice and qualitative index of emergency room staff: a quasi-interventional study. Bull Emerg Trauma. 2013;1:69–75.
Ingrassia PL, Mangini M, Azzaretto M, Ciaramitaro I, Costa L, Burkle JF, et al. Hospital Disaster preparedness in Italy: a preliminary study utilizing the World Health Organization Hospital Emergency Response Evaluation Toolkit. Minerva Anestesiol. 2016;82(12):1259–66.
PubMed Google Scholar
Ardalan A, Kandi M, Talebian MT, Khankeh H, Masoumi G, Mohammadi R, Maleknia S, Miadfar J, Mobini A, Mehranamin S. Hospitals safety from disasters in IR iran: the results from assessment of 224 hospitals. PLoS currents. 2014 Feb 28;6.
Asefzadeh S, Rajaee R, Ghamari F, Kalhor R, Gholami S. Preparedness of Iranian hospitals against disasters. Biotechnology and Health Sciences. 2016;3(3):1-6.
Khankeh He. Management of health care in the event of natural disasters. Quarterly rehabilitation. 2006;7(2).
Krajewski MJ, Sztajnkrycer M, Baez AA. Hospital disaster preparedness in the United States: new issues, new challenges. The internet journal of Rescue and Disaster Medicine. 2005;4(2):22-5.
UNISDR U, editor Sendai framework for disaster risk reduction 2015–2030. Proceedings of the 3rd United Nations World Conference on DRR, Sendai, Japan; 2015.
Hospital Safety Index: Guide for Evaluators. Geneva, Switzerland: World Health Organization; 2008. Available at: http://www.paho.org/english/dd/ ped/SafeHosEvaluatorGuideEng.pdf, Accessed April 2014.
Djalali A, Castren M, Khankeh H, Gryth D, Radestad M, Öhlen G, et al. Hospital disaster preparedness as measured by functional capacity: a comparison between Iran and Sweden. Prehospital and disaster medicine. 2013;28(5):454-61.
Vahedparast H, Ravanipour M, Hajinezhad F, Kamali F, Gharibi T, Bagherzadeh R. Assessing Hospital Disaster Preparedness of Bushehr province. Iranian South Medical Journal. 2013 Mar 1;16(1).
Khankeh H. Risk assessment tools and health capabilities indicators of specialized in disaster. University of Welfare and Rehabilitation Sciences: Publications of University of Welfare and Rehabilitation Sciences; 2013.
Sorensen B, Zane R, Wante B, Rao M, Bortolin M, Rockenschaub G. Hospital emergency response checklist: an all-hazards tool for hospital administrators and emergency managers. 2011. World Health Organ. 2013.
Shabanikiya H, Jafari M, Gorgi HA, Seyedin H, Rahimi A. Developing a practical toolkit for evaluating hospital preparedness for surge capacity in disasters. International journal of disaster risk reduction. 2019; 34:423-8.
Pourhosseini SS, Ardalan A, Mehrolhassani MH. Key aspects of providing healthcare services in the disaster response stage. Iranian journal of public health. 2015;44(1):111.
Dowlati M, Seyedin H, Moslehi S. Hospital preparedness measures for biological hazards: a systematic review and meta-synthesis. Disaster medicine and public health preparedness. 2021;15(6):790-803.
Download references
Acknowledgements
The authors would like to express their acknowledgments to the staff at the Department of Postgraduate Studies in the University of Social Welfare and Rehabilitation Sciences and appreciate the sincere cooperation of hospital managers, officials, and staff of Shahid Motahhari Hospital for their contributions to conducting this research project.
This study was conducted as part of a master’s thesis at the University of Social Welfare and Rehabilitation Sciences.
Author information
Authors and affiliations.
Department of Nursing, University of Welfare and Rehabilitation Sciences, Tehran, Iran
Alireza Shafiei
Iranian Research Center on Aging, Department of Nursing, University of Social Welfare and Rehabilitation Sciences, Tehran, Iran
Narges Arsalani
Department of Pre-Hospital Medical Emergencies, School of Paramedical, Qazvin University of Medical Sciences, Qazvin, Iran
Mehdi Beyrami Jam
Health in Emergency and Disaster Research Center, University of Social Welfare and Rehabilitation Sciences, Tehran, Iran
Hamid Reza Khankeh
You can also search for this author in PubMed Google Scholar
Contributions
ASH, HKH design of the study, MB, ASH and NA collect and analysed the data and ASH, MB, HKH preparation of the manuscript.
Corresponding author
Correspondence to Hamid Reza Khankeh .
Ethics declarations
Ethics approval and consent to participate.
This study was approved by the University of Social Welfare and Rehabilitation Sciences(USWRS) Research Ethics Committees with the Code of Ethics USWR.REC.1392.93. Also, the institutional review board of USWRS approved all the methods and steps for this study. Hence, all procedures were conducted in compliance with the appropriate guidelines and regulations, and written informed consent was obtained from study participants. They were informed that their involvement in the research was entirely voluntary, and they had the freedom to withdraw from the study at any point if they chose to do so.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Shafiei, A., Arsalani, N., Beyrami Jam, M. et al. The impact of surge capacity enhancement training for nursing managers on hospital disaster preparedness and response: an action research study. BMC Emerg Med 24 , 153 (2024). https://doi.org/10.1186/s12873-024-00930-1
Download citation
Received : 07 October 2023
Accepted : 03 January 2024
Published : 26 August 2024
DOI : https://doi.org/10.1186/s12873-024-00930-1
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Disaster preparedness
- Surge capacity
- Action research
BMC Emergency Medicine
ISSN: 1471-227X
- General enquiries: [email protected]
Journal of Materials Chemistry A
Nanostructured dyfeo 3 photocatalyst: an authentic and effective approach for remediation of industrial and pharmaceutical wastewater.
The persistent issue of water contamination by industrial dyes and pharmaceutical residues has created an urgent need for advanced photocatalytic materials to effectively address environmental remediation. Despite ongoing research, developing novel photocatalysts with ideal band structures, high quantum yields, and strong stability remains a considerable challenge. In this study, we report the synthesis and detailed characterization of nanostructured dysprosium orthoferrite (DyFeO 3 ) nanoparticles, designed with a porous architecture featuring an average pore size of 3.41 nm and a surface area of 23.25 m 2 /g to enhance photocatalytic efficiency under solar irradiation. Using Inverse Fast Fourier Transform (FFT) analysis on selected areas of TEM images, we gained deeper insights into the formation and internal structure of these nanoparticles. DyFeO 3 nanoparticles exhibit a direct band gap of 2.1 eV, making them particularly effective for solar light absorption. Comprehensive spectroscopic analyses, including Mott-Schottky measurements and valence band XPS, confirmed their n-type semiconducting nature and revealed an electronic band structure that supports efficient oxygen reduction and oxidation reactions. Additionally, time-resolved photoluminescence spectroscopy demonstrated a charge carrier lifetime of 2.43 ns, indicating efficient separation and transport of photogenerated charge carriers. The photocatalytic performance of DyFeO 3 was evaluated through degradation experiments using two model pollutants: Rhodamine B (RhB) and Levofloxacin (LFX). The nanoparticles successfully degraded both the colored RhB and the colorless LFX, eliminating concerns of dye sensitization. Furthermore, the presence of DyFeO 3 significantly reduced the activation energy for RhB degradation from 55.87 kJ mol -1 K -1 to 34.58 kJ mol -1 K -1 and for LFX from 38.4 kJ mol -1 K -1 to 34.1 kJ mol -1 K -1 , demonstrating their catalytic efficiency. With apparent quantum yield values of 28.94% for RhB and 32.83% for LFX, these nanoparticles demonstrate exceptional solar energy harvesting capabilities. The high degradation efficiency, quantum yield, and stability of the single-structured DyFeO 3 nanoparticles underscore their potential for large-scale applications in photocatalytic and environmental remediation technologies.
Supplementary files
- Supplementary information PDF (1956K)
Transparent peer review
To support increased transparency, we offer authors the option to publish the peer review history alongside their article.
View this article’s peer review history
Article information
Download citation, permissions.
M. Tarek, F. Yasmeen and M. A. Basith, J. Mater. Chem. A , 2024, Accepted Manuscript , DOI: 10.1039/D4TA04728A
To request permission to reproduce material from this article, please go to the Copyright Clearance Center request page .
If you are an author contributing to an RSC publication, you do not need to request permission provided correct acknowledgement is given.
If you are the author of this article, you do not need to request permission to reproduce figures and diagrams provided correct acknowledgement is given. If you want to reproduce the whole article in a third-party publication (excluding your thesis/dissertation for which permission is not required) please go to the Copyright Clearance Center request page .
Read more about how to correctly acknowledge RSC content .
Social activity
Search articles by author.
This article has not yet been cited.
Advertisements
- Technical Support
- Find My Rep
You are here
Review of Educational Research
Preview this book.
- Description
- Aims and Scope
- Editorial Board
- Abstracting / Indexing
- Submission Guidelines
The Review of Educational Research ( RER , quarterly, begun in 1931; approximately 640 pp./volume year) publishes critical, integrative reviews of research literature bearing on education. Such reviews should include conceptualizations, interpretations, and syntheses of literature and scholarly work in a field broadly relevant to education and educational research. RER encourages the submission of research relevant to education from any discipline, such as reviews of research in psychology, sociology, history, philosophy, political science, economics, computer science, statistics, anthropology, and biology, provided that the review bears on educational issues. RER does not publish original empirical research unless it is incorporated in a broader integrative review. RER will occasionally publish solicited, but carefully refereed, analytic reviews of special topics, particularly from disciplines infrequently represented.
The Review of Educational Research publishes critical, integrative reviews of research literature bearing on education. Such reviews should include conceptualizations, interpretations, and syntheses of literature and scholarly work in a field broadly relevant to education and educational research. RER encourages the submission of research relevant to education from any discipline, such as reviews of research in psychology, sociology, history, philosophy, political science, economics, computer science, statistics, anthropology, and biology, provided that the review bears on educational issues. RER does not publish original empirical research, and all analyses should be incorporated in a broader integrative review. RER will occasionally publish solicited, but carefully refereed, analytic reviews of special topics, particularly from disciplines infrequently represented. The following types of manuscripts fall within the journal’s purview:
Integrative reviews pull together the existing work on an educational topic and work to understand trends in that body of scholarship. In such a review, the author describes how the issue is conceptualized within the literature, how research methods and theories have shaped the outcomes of scholarship, and what the strengths and weaknesses of the literature are. Meta-analyses are of particular interest when they are accompanied by an interpretive framework that takes the article beyond the reporting of effect sizes and the bibliographic outcome of a computer search.
Theoretical reviews should explore how theory shapes research. To the extent that research is cited and interpreted, it is in the service of the specification, explication, and illumination of a theory. Theoretical reviews and integrative reviews have many similarities, but the former are primarily about how a theory is employed to frame research and our understandings, and refer to the research as it relates to the theory.
Methodological reviews are descriptions of research design, methods, and procedures that can be employed in literature reviews or research in general. The articles should highlight the strengths and weaknesses of methodological tools and explore how methods constrain or open up opportunities for learning about educational problems. They should be written in a style that is accessible to researchers in education rather than methodologists.
Historical reviews provide analyses that situate literature in historical contexts. Within these reviews, explanations for educational phenomena are framed within the historical forces that shape language and understanding.
Commissioned reviews and thematic issues. The editors may commission and solicit authors to review areas of literature. In all other respects, commissioned reviews are subject to the same review process as submitted reviews. The editors also encourage readers to propose thematic topics for special issues and, as potential guest editors, to submit plans for such issues.
In addition to review articles, RER will occasionally publish notes and responses which are short pieces of no more than 1,200 words on any topic that would be of use to reviewers of research. Typically, they point out shortcomings and differences in interpretation in RER articles and policy.
The standards and criteria for review articles in RER are the following:
1. Quality of the Literature. Standards used to determine quality of literature in education vary greatly. Any review needs to take into account the quality of the literature and its impact on findings. Authors should attempt to review all relevant literature on a topic (e.g., international literature, cross-disciplinary work, etc.).
2. Quality of Analysis. The review should go beyond description to include analysis and critiques of theories, methods, and conclusions represented in the literature. This analysis should also examine the issue of access—which perspectives are included or excluded in a body of work? Finally, the analysis should be reflexive—how does the scholars’ framework constrain what can be known in this review?
3. Significance of the Topic. The review should seek to inform and/or illuminate questions important to the field of education. While these questions may be broad-based, they should have implications for the educational problems and issues affecting our national and global societies.
4. Impact of the Article. The review should be seen as an important contribution and tool for the many different educators dealing with the educational problems and issues confronting society.
5. Advancement of the Field. The review should validate or inform the knowledge of researchers and guide and improve the quality of their research and scholarship.
6. Style. The review must be well written and conform to style of the Publication Manual of the American Psychological Association (6th edition). Authors should avoid the use of unexplained jargon and parochialism.
7. Balance and Fairness. The review should be careful not to misrepresent the positions taken by others, or be disrespectful of contrary positions.
8. Purpose. Any review should be accessible to the broad readership of RER. The purpose of any article should be to connect the particular problem addressed by the researcher(s) to a larger context of education.
We also encourage all authors interested in submitting a manuscript to RER to read our Editorial Vision for more information on our publication aims.
| Pennsylvania State University, USA | |
| The Pennsylvania State University, USA | |
| The Pennsylvania State University, USA | |
| The Pennsylvania State University, USA |
| Florida Atlantic University, USA | |
| Pennsylvania State University, USA | |
| Purdue University, USA | |
| University of Southern California, USA | |
| Arizona State University, USA | |
| Texas State University, USA | |
| Pennsylvania State University, USA | |
| Arizona State University, USA | |
| University of Arizona, USA | |
| University of North Carolina, Greensboro, USA | |
| University of Arizona, USA | |
| University of Illinois, Chicago, USA |
| University of California, Berkley | |
| University of Maryland, USA | |
| University at Buffalo - SUNY, USA | |
| University of Pennsylvania, USA | |
| Pennsylvania State University, USA | |
| Boston University, USA | |
| Columbia University, USA | |
| University of Colorado Boulder, USA | |
| University of California, Santa Cruz, USA | |
| Rutgers University, USA | |
| Ohio State University, USA | |
| University of North Carolina, USA | |
| University of Quebec, Canada | |
| Colorado State University, USA | |
| University of Colorado Boulder, USA | |
| Arizona State University, USA | |
| University of North Carolina, USA | |
| University of California, Berkeley | |
| Indiana University, USA | |
| University at Buffalo - SUNY, USA | |
| Brigham Young University, USA | |
| Pennsylvania State University, USA | |
| University of California, Riverside, USA | |
| Arizona State University,USA | |
| San Jose State University, USA | |
| University of Illinois, USA | |
| Texas Christian University, USA | |
| Vanderbilt University, USA | |
| University of Florida, USA | |
| University of Massachusets, Amherst, USA | |
| University of Twente, Netherlands | |
| University of Illinois, USA | |
| Rutgers University, USA | |
| University of Kiel, Germany | |
| University of Nebraska - Lincoln, USA | |
| College of Education, University of Florida, USA | |
| University of Pittsburgh, USA | |
| University of Texas-Austin, USA | |
| American Institutes for Research, USA | |
| University of California, Riverside, USA | |
| University of Tennessee, USA | |
| Boston College, USA | |
| Harvard University, USA | |
| Harvard University, USA | |
| Mathematica, USA | |
| University of Utah, USA | |
| Ben-Gurion University of the Negev, Israel | |
| University of Washington, USA | |
| University of California, Santa Barbara, USA | |
| University of Cincinnati, USA | |
| University of Vermont, USA | |
| University of Melbourne, Australia | |
| Texas State University, USA | |
| Hunter College, USA | |
| Arizona State University, USA | |
| University of Michigan,USA | |
| University of Connecticut, USA | |
| University of Pennsylvania, USA |
- Academic Search - Premier
- Academic Search Alumni Edition
- Academic Search Elite
- Clarivate Analytics: Current Contents - Physical, Chemical & Earth Sciences
- EBSCO: MasterFILE Elite
- EBSCO: MasterFILE Premier
- EBSCO: Professional Development Collection
- EBSCO: Sales & Marketing Source
- EBSCOhost: Current Abstracts
- ERIC (Education Resources Information Center)
- Educational Research Abstracts Online (T&F)
- Higher Education Abstracts
- MasterFILE Select - EBSCO
- ProQuest Education Journals
- Social SciSearch
- Social Sciences Citation Index (Web of Science)
- Teacher Reference Center
- Wilson Education Index/Abstracts
Manuscript submission guidelines can be accessed on Sage Journals .
- Read Online
- Sample Issues
- Current Issue
- Email Alert
- Permissions
- Foreign rights
- Reprints and sponsorship
- Advertising
Individual Subscription, Combined (Print & E-access)
Institutional Subscription, E-access
Institutional Subscription & Backfile Lease, E-access Plus Backfile (All Online Content)
Institutional Subscription, Print Only
Institutional Subscription, Combined (Print & E-access)
Institutional Subscription & Backfile Lease, Combined Plus Backfile (Current Volume Print & All Online Content)
Institutional Backfile Purchase, E-access (Content through 1998)
Individual, Single Print Issue
Institutional, Single Print Issue
To order single issues of this journal, please contact SAGE Customer Services at 1-800-818-7243 / 1-805-583-9774 with details of the volume and issue you would like to purchase.
- AERA Open Editors
- AERJ Editors
- EEPA Editors
- ER Issues and Archives
- JEBS Editors
- JSTOR Online Archives
- RER Editors
- RRE Editors
- AERA Examination and Desk Copies
- Mail/Fax Book Order Form
- International Distribution
- Books & Publications
- Merchandise
- Search The Store
- Online Paper Repository
- i-Presentation Gallery
- Research Points
- AERA Journal Advertising Rate Cards
- Publications Permissions
- Publications FAQs











IMAGES
VIDEO
COMMENTS
Many recent changes, coming from the White House, the academy, and advances in technology, have raised questions about the future of peer review. Is peer review worth saving? Should peer review processes be revised? How should reviewers' work be recognized? Join us for an Essential Science Conversation on The Future of Peer Review.
"But there's no formal education" on how to do it, Klass continues. To attempt to remedy this disconnection, Klass and her partners will use the NSF grant to fund a new curriculum that will immerse graduate students in the sciences in the "principles and practices of peer review and science communication with a heavy emphasis on ...
Review of Education is an official BERA journal publishing educational research from throughout the world, and papers on topics of international interest. ... This study reviews the literature through a bibliometric analysis of 387 peer-reviewed papers on this topic published between 2000 and 2024, followed by a synthesis of the top-cited ...
Educational settings in professional health education establishments significantly shape students' academic, social, and emotional experiences. These environments encompass physical, psychological, and social infrastructures of programs or institutions, which jointly influence learning and development. This study analyzed the educational environment at Prince Nora University in Saudi Arabia, a ...
Design Scoping review. Data sources We searched the databases SPORTDiscus, APA PsycINFO, Web of Science and Sports Medicine & Education Index for peer-reviewed, published in English articles that considered the factors influencing positive developmental outcomes for athletes under 18 years competing at a national and/or international level.
If yes, clear your schedule from 3 to 4:30 p.m. Tuesday, Sept. 24, and learn how you can get involved in peer review of teaching. The annual Academy of Teaching Scholars session, Giving Great Teaching Feedback: How to Conduct a Peer Review of Teaching, is the first (required) step for becoming a peer reviewer. During this online session, you ...
Studying medicine is a multi-dimensional process involving acquiring medical knowledge, clinical skills, and professional attitudes. Previous research has found that emotions play a significant role in this process [1, 2].Different types of emotions are important in an academic context, influencing performance on assessments and evaluations, reception of feedback, exam scores, and overall ...
The disruption of health and medical education by the COVID-19 pandemic made educators question the effect of online setting on students' learning, motivation, self-efficacy and preference. In light of the health care staff shortage online scalable education seemed relevant. Reviews on the effect of online medical education called for high quality RCTs, which are increasingly relevant with ...
Peer Review reports. Background. With the global outbreak of COVID-19 on January 12, 2020, ... were made available in alignment with the ethical principles that govern such research. The educational content for the sessions was developed by a multidisciplinary team consisting of a nurse psychiatrist, a gerontologist, and a Specialist in Quran ...
Flipped teaching is an interactive learning strategy that actively engages students in the learning process. Students have an active role in flipped teaching as they independently prepare for the class. Class time is dedicated to discussion and learning activities. Thus, it is believed that flipped teaching promotes students' critical thinking, communication, application of knowledge in real ...
Cynthia DiCarlo, PhD was awarded the 2024 National Association of Early Childhood Teacher Educators (NAECTE) Foundation Established Career Early Teacher Educator Research Grant Award Winner. Dr. DiCarlo was selected as the top-scoring application after the review by a team of NAECTE peer reviewers for her project "Child Sustained Attention in One-Year-Olds."
Simulation in healthcare, empowered by big data analytics and artificial intelligence (AI), has the potential to drive transformative innovations towards enhanced interprofessional collaboration (IPC). This convergence of technologies revolutionizes medical education, offering healthcare professionals (HCPs) an immersive, iterative, and dynamic simulation platform for hands-on learning and ...
The research demonstrated that enhancing the disaster preparedness of hospitals can be achieved by training nursing managers using an action research approach. ... Peer Review reports. Introduction. Hospitals, ... the educational intervention on triage by Rahmati and colleagues enhances the preparedness of the emergency department, as ...
Despite ongoing research, developing novel photocatalysts with ideal band structures, high quantum yields, and strong stability remains a considerable challenge. ... we offer authors the option to publish the peer review history alongside their article. View this article's peer review history. Article information. DOI ... Education in Chemistry;
Review of Educational Research. Impact Factor: 8.3 5-Year Impact Factor: 16.4. Journal Homepage. Submit Paper. The Review of Educational Research (RER) publishes critical, integrative reviews of research literature bearing on education, including conceptualizations, interpretations, and syntheses of literature and scholarly work in a field ...
The Review of Educational Research ( RER, quarterly, begun in 1931; approximately 640 pp./volume year) publishes critical, integrative reviews of research literature bearing on education. Such reviews should include conceptualizations, interpretations, and syntheses of literature and scholarly work in a field broadly relevant to education and ...
The Review of Educational Research ( RER, bimonthly, begun in 1931) publishes critical, integrative reviews of research literature bearing on education. Such reviews should include conceptualizations, interpretations, and syntheses of literature and scholarly work in a field broadly relevant to education and educational research.
Review of Educational Research (RER) publishes critical, integrative reviews of research literature bearing on education. Such reviews should include conceptualizations, interpretations, and syntheses of literature and scholarly work in a field. RER encourages the submission of research relevant to education from any discipline, such as reviews ...
The Journal of the European Association for Research on Learning and Instruction (EARLI) Educational Research Review is an international journal addressed to researchers and various agencies interested in the review of studies and theoretical papers in education at any level. The journal accepts …. View full aims & scope. Learn more about EARLI.
Rebecca D. Silverman. Kristin Keane. Elena Darling-Hammond. Saurabh Khanna. Preview abstract. Educational technology is ubiquitous, and educational technology interventions often target literacy. However, there is insufficient information about the effects of these interventions on literacy outcomes in elementary school.
The style guide for the Review of Educational Research and all AERA journals is the Publication Manual of the American Psychological Association, ... The manuscript submission and peer review procedure is unchanged. On acceptance of your article, you will be asked to let Sage know directly if you are choosing Sage Choice.
The Review of Educational Research is a bimonthly peer-reviewed review journal published by SAGE Publications on behalf of the American Educational Research Association.It was established in 1931 and covers all aspects of education and educational research.The journal's co-editors are Mildred Boveda, Karly Sarita Ford, Erica Frankenberg, and Francesca López (Pennsylvania State University).
The Journal of the European Association for Research on Learning and Instruction (EARLI). Educational Research Review is an international journal addressed to researchers and various agencies interested in the review of studies and theoretical papers in education at any level. The journal accepts high quality articles that are solving educational research problems by using a review approach.
Examining Race in LatCrit: A Systematic Review of Latinx Critical Race Theory in Education. This systematic review includes 125 peer-reviewed education-research articles that employ a LatCrit framework (from a search including articles published from 1995 to 2020). The author examines how the literature utilizes LatCrit and advances ideas about ...
Abstract. The underrepresentation and underperformance of men of color relative to women of color within institutions of higher education have been extensively studied the past 20 years. The purpose of this study is to understand trends in how this research has ... xml GET ACCESS.
The Review of Educational Research is a bimonthly peer-reviewed review journal published by SAGE Publications on behalf of the American Educational Research Association. It was established in 1931 and covers all aspects of education and educational research.
Review of Educational Research | Citations: 3,241 | The Review of Educational Research (RER, quarterly, begun in 1931; approximately 640 pp./volume year) publishes critical, integrative reviews of ...
Peer-Review Check - Option #1 - OneSearch (library website) OneSearch. This method works if you have the title of an article. Paste the title of the article in the search blank (ONESEARCH) on the library website. If the journal that this article was published in a blue icon and PEER REVIEWED label will appear in the results.
Review of Educational Research Fall 1998, Vol. 68, No. 3, pp. 249-276 Peer Assessment Between Students in Colleges and Universities Keith Topping University of Dundee A definition and typology of peer assessment between students in higher education is proposed, and the theoretical underpinnings of the method are discussed.
Review of Research in Education (RRE), published annually, provides a forum for analytic research reviews on selected education topics of significance to the field.Each volume addresses a topic of broad relevance to education and learning, and publishes articles that critically examine diverse literatures and bodies of knowledge across relevant disciplines and fields.