- Patient Care & Health Information
- Diseases & Conditions
Syphilis is an infection caused by bacteria. Most often, it spreads through sexual contact. The disease starts as a sore that's often painless and typically appears on the genitals, rectum or mouth. Syphilis spreads from person to person through direct contact with these sores. It also can be passed to a baby during pregnancy and childbirth and sometimes through breastfeeding.
After the infection happens, syphilis bacteria can stay in the body for many years without causing symptoms. But the infection can become active again. Without treatment, syphilis can damage the heart, brain or other organs. It can become life-threatening.
Early syphilis can be cured, sometimes with a single shot of medicine called penicillin. That's why it's key to get a health care checkup as soon as you notice any symptoms of syphilis. All pregnant people should get tested for syphilis at their first prenatal checkup too.

Products & Services
- A Book: Mayo Clinic Family Health Book, 5th Edition

- Primary syphilis
Primary syphilis causes painless sores (chancres) on the genitals, rectum, tongue or lips. The disease can be present with the appearance of a single chancre (shown here on a penis) or many.
Syphilis develops in stages. The symptoms vary with each stage. But the stages may overlap. And the symptoms don't always happen in the same order. You may be infected with syphilis bacteria without noticing any symptoms for years.
The first symptom of syphilis is a small sore called a chancre (SHANG-kur). The sore is often painless. It appears at the spot where the bacteria entered your body. Most people with syphilis develop only one chancre. Some people get more than one.
The chancre often forms about three weeks after you come in contact with syphilis bacteria. Many people who have syphilis don't notice the chancre. That's because it's usually painless. It also may be hidden within the vagina or rectum. The chancre heals on its own within 3 to 6 weeks.
Secondary syphilis
You may get a rash while the first chancre heals or a few weeks after it heals.
A rash caused by syphilis:
- Often is not itchy.
- May look rough, red or reddish-brown.
- Might be so faint that it's hard to see.
The rash often starts on the trunk of the body. That includes the chest, stomach area, pelvis and back. In time, it also could appear on the limbs, the palms of the hands and the soles of the feet.
Along with the rash, you may have symptoms such as:
- Wartlike sores in the mouth or genital area.
- Muscle aches.
- Sore throat.
- Tiredness, also called fatigue.
- Weight loss.
- Swollen lymph nodes.
Symptoms of secondary syphilis may go away on their own. But without treatment, they could come and go for months or years.
Latent syphilis
If you aren't treated for syphilis, the disease moves from the secondary stage to the latent stage. This also is called the hidden stage because you have no symptoms. The latent stage can last for years. Your symptoms may never come back. But without treatment, the disease might lead to major health problems, also called complications.
Tertiary syphilis
After the latent stage, up to 30% to 40% of people with syphilis who don't get treatment have complications known as tertiary syphilis. Another name for it is late syphilis.
The disease may damage the:
- Blood vessels.
- Bones and joints.
These problems may happen many years after the original, untreated infection.
Syphilis that spreads
At any stage, untreated syphilis can affect the brain, spinal cord, eyes and other body parts. This can cause serious or life-threatening health problems.
Congenital syphilis
Pregnant people who have syphilis can pass the disease to their babies. Unborn babies can become infected through the organ that provides nutrients and oxygen in the womb, called the placenta. Infection also can happen during birth.
Newborns with congenital syphilis might have no symptoms. But without fast treatment, some babies might get:
- Sores and rashes on the skin.
- A type of discolored skin and eyes, called jaundice.
- Not enough red blood cells, called anemia.
- Swollen spleen and liver.
- Sneezing or stuffed, drippy nose, called rhinitis.
- Bone changes.
Later symptoms may include deafness, teeth problems and saddle nose, a condition in which the bridge of the nose collapses.
Babies with syphilis also can be born too early. They may die in the womb before birth. Or they could die after birth.
When to see a doctor
Call a member of your health care team if you or your child has any symptoms of syphilis. These could include any unusual discharge, a sore or a rash, especially in the groin area.
Also get tested for syphilis if you:
- Have had sexual contact with someone who might have the disease.
- Have another sexually transmitted disease such as HIV .
- Are pregnant.
- Regularly have sex with more than one partner.
- Have unprotected sex, meaning sex without a condom.
- Mayo Clinic Minute: Signs and symptoms of syphilis
Vivien Williams: Syphilis is a sexually transmitted infection caused by the bacterium Treponema pallidum. Dr. Stacey Rizza, an infectious diseases specialist at Mayo Clinic, says syphilis affects men and women and can present in various stages.
Stacey Rizza, M.D.: Primary syphilis causes an ulcer, and this sometimes isn't noticed because it's painless and can be inside the vagina or on the cervix…after a few weeks, two months, they can get secondary syphilis, which is a rash.
Vivien Williams: It may then progress to latent stage syphilis and, finally, the most serious stage: tertiary. Pregnant women are not immune to syphilis. Congenital syphilis can lead to miscarriage, stillbirth or infant deaths. That's why all pregnant women should be screened. Syphilis is preventable and treatable. As for prevention, Dr. Rizza recommends barrier protection during sex.
Dr. Rizza: And that's during oral sex, anal sex, vaginal sex — using condoms, dental dams and any other barrier protection.
Vivien Williams: For the Mayo Clinic News Network, I'm Vivien Williams.
More Information
There is a problem with information submitted for this request. Review/update the information highlighted below and resubmit the form.
From Mayo Clinic to your inbox
Sign up for free and stay up to date on research advancements, health tips, current health topics, and expertise on managing health. Click here for an email preview.
Error Email field is required
Error Include a valid email address
To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
Thank you for subscribing!
You'll soon start receiving the latest Mayo Clinic health information you requested in your inbox.
Sorry something went wrong with your subscription
Please, try again in a couple of minutes
The cause of syphilis is a bacterium called Treponema pallidum. The most common way syphilis spreads is through contact with an infected person's sore during vaginal, oral or anal sex.
The bacteria enter the body through minor cuts or scrapes in the skin or in the moist inner lining of some body parts.
Syphilis is contagious during its primary and secondary stages. Sometimes it's also contagious in the early latent period, which happens within a year of getting infected.
Less often, syphilis can spread by kissing or touching an active sore on the lips, tongue, mouth, breasts or genitals. It also can be passed to babies during pregnancy and childbirth and sometimes through breastfeeding.
Syphilis can't be spread through casual contact with objects that an infected person has touched.
So you can't catch it by using the same toilet, bathtub, clothing, eating utensils, doorknobs, swimming pools or hot tubs.
Once cured, syphilis doesn't come back on its own. But you can become infected again if you have contact with someone's syphilis sore.
Risk factors
The risk of catching syphilis is higher if you:
- Have unprotected sex.
- Have sex with more than one partner.
- Live with HIV , the virus that causes AIDS if untreated.
The chances of getting syphilis also are higher for men who have sex with men. The higher risk may be linked, in part, with less access to health care and less use of condoms among this group. Another risk factor for some people in this group includes recent sex with partners found through social media apps.
Complications
Without treatment, syphilis can lead to damage throughout the body. Syphilis also raises the risk of HIV infection and can cause problems during pregnancy. Treatment can help prevent damage. But it can't repair or reverse damage that's already happened.
Small bumps or tumors
Rarely in the late stage of syphilis, bumps called gummas can form on the skin, bones, liver or any other organ. Most often, gummas go away after treatment with medicine called antibiotics.
Neurological problems
Syphilis can cause many problems with the brain, its covering or the spinal cord. These issues include:
- Meningitis, a disease that inflames the protective layers of tissue around the brain and spinal cord.
- Confusion, personality changes or trouble focusing.
- Symptoms that mimic dementia, such as loss of memory, judgment and decision-making skills.
- Not being able to move certain body parts, called paralysis.
- Trouble getting or keeping an erection, called erectile dysfunction.
- Bladder problems.
Eye problems
Disease that spreads to the eye is called ocular syphilis. It can cause:
- Eye pain or redness.
- Vision changes.
Ear problems
Disease that spreads to the ear is called otosyphilis. Symptoms can include:
- Hearing loss.
- Ringing in the ears, called tinnitus.
- Feeling like you or the world around you is spinning, called vertigo.
Heart and blood vessel problems
These may include bulging and swelling of the aorta — the body's major artery — and other blood vessels. Syphilis also may damage heart valves.
HIV infection
Syphilis sores on the genitals raise the risk of catching or spreading HIV through sex. A syphilis sore can bleed easily. This provides an easy way for HIV to enter the bloodstream during sex.
Pregnancy and childbirth complications
If you're pregnant, you could pass syphilis to your unborn baby. Congenital syphilis greatly raises the risk of miscarriage, stillbirth or your newborn's death within a few days after birth.
There is no vaccine for syphilis. To help prevent the spread of syphilis, follow these tips:
- Have safe sex or no sex. The only certain way to avoid contact with syphilis bacteria is not to have sex. This is called abstinence. If a person is sexually active, safer sex means a long-term relationship in which you and your partner have sex only with each other, and neither of you is infected. Before you have sex with someone new, you should both get tested for syphilis and other sexually transmitted infections (STIs).
- Use a latex condom. Condoms can lower your risk of getting or spreading syphilis. But condoms work only if they cover an infected person's syphilis sores. Other types of birth control do not lower your risk of syphilis.
- Be careful with alcohol and stay away from street drugs. Drinking too much alcohol or taking drugs can get in the way of your judgment. Either can lead to unsafe sex.
- Do not douche. It can remove some of the healthy bacteria that's usually in the vagina. And that might raise your risk of getting STIs .
- Breastfeed with caution. Syphilis can pass from a parent to a baby during breastfeeding if sores are on one or both breasts. This can happen when the baby or pumping equipment touches a sore. To keep that from happening, pump or hand-express breastmilk from the breast with sores. Do so until the sores heal. If your pump touches a sore, get rid of the milk you just pumped.
Partner notification and preventive treatment
If tests show that you have syphilis, your sex partners need to know so that they can get tested. This includes your current partners and any others you've had over the last three months to 1 year. If they're infected, they can then get treatment.
After you learn you have syphilis, your local health department may contact you. A department employee talks with you about private ways to let your partners know that they've been exposed to syphilis. You can ask the department to do this for you without revealing your identity to your partners.
Or you can contact your partners along with a department employee or simply tell your partners yourself. This free service is called partner notification. It can help limit the spread of syphilis. The practice also steers those at risk toward counseling and the right treatment.
And since you can get syphilis more than once, partner notification lowers your risk of getting infected again.
Screening tests for pregnant people
You can be infected with syphilis and not know it. And the disease can have deadly effects on unborn babies. For this reason, health officials recommend that all pregnant people be tested for the disease.
- Syphilis — CDC detailed fact sheet. Centers for Disease Control and Prevention. https://www.cdc.gov/std/syphilis/stdfact-syphilis-detailed.htm. Accessed April 27, 2023.
- Sexually transmitted infections treatment guidelines, 2021: Syphilis. Centers for Disease Control and Prevention. https://www.cdc.gov/std/treatment-guidelines/syphilis.htm. Accessed April 27, 2023.
- Hicks CB, et al. Syphilis: epidemiology, pathophysiology, and clinical manifestations in patients without HIV. https://www.uptodate.com/contents/search. Accessed April 27, 2023.
- Syphilis. Merck Manual Professional Version. https://www.merckmanuals.com/professional/infectious-diseases/sexually-transmitted-diseases-stds/syphilis. Accessed April 27, 2023.
- Hicks CB, et al. Syphilis: Treatment and monitoring. https://www.uptodate.com/contents/search. Accessed April 27, 2023.
- Hicks CB, et al. Syphilis: Screening and diagnostic testing. https://www.uptodate.com/contents/search. Accessed April 27, 2023.
- Syphilis — CDC basic fact sheet. Centers for Disease Control and Prevention. https://www.cdc.gov/std/syphilis/stdfact-syphilis.htm. Accessed April 27, 2023.
- Loscalzo J, et al., eds. Syphilis. In: Harrison's Principles of Internal Medicine. 21st ed. McGraw Hill; 2022. https://accessmedicine.mhmedical.com. Accessed July 14, 2019.
- AskMayoExpert. Syphilis (adult). Mayo Clinic; 2021.
- Sexually transmitted infections. Office on Women's Health. http://womenshealth.gov/publications/our-publications/fact-sheet/sexually-transmitted-infections.html. Accessed April 27, 2023.
- Tosh PK (expert opinion). Mayo Clinic. May 1, 2023.
- Cáceres CF, et al. Syphilis in men who have sex with men: advancing research and human rights. The Lancet Global Health. 2021; doi:10.1016/S2214-109X(21)00269-2.
- How can partner services programs help me and my patients? Centers for Disease Control and Prevention. https://www.cdc.gov/hiv/clinicians/screening/partner-notification.html. Accessed April 28, 2023.
- Penicillin allergy FAQ. American Academy of Allergy, Asthma & Immunology. https://www.aaaai.org/tools-for-the-public/conditions-library/allergies/penicillin-allergy-faq. Accessed April 28, 2023.
- Just diagnosed? Next steps after testing positive for gonorrhea or chlamydia. Centers for Disease Control and Prevention. https://www.cdc.gov/std/prevention/NextSteps-GonorrheaOrChlamydia.htm. Accessed May 1, 2023.
News from Mayo Clinic
- Newborns diagnosed with syphilis at alarming rates Feb. 19, 2024, 03:30 p.m. CDT
- Mayo Clinic Minute: Syphilis surge is cause for concern Feb. 03, 2024, 12:00 p.m. CDT
- Syphilis: A rising community presence Aug. 01, 2022, 04:30 p.m. CDT
- Symptoms & causes
- Diagnosis & treatment
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
Make twice the impact
Your gift can go twice as far to advance cancer research and care!
Syphilis – CDC Basic Fact Sheet
Electron micrograph of Treponema pallidum on cultures of cotton-tail rabbit epithelium cells

A primary vulvar syphilitic chancre due to Treponema pallidum bacteria

A penile chancre located on the proximal penile shaft: primary syphilitic infection

Gummatous lesions on the dorsal surface of the left hand

Secondary syphilitic papulosquamous rash on the torso and upper body

Secondary syphilitic lesions on the face

Secondary syphilis presenting pigmented macules and papules on the skin

Secondary syphilitic lesions of vagina

This was a case of congenital syphilis resulting in the death of this newborn infant

This newborn presented with symptoms of congenital syphilis that included lesions on the soles of both feet

Interstitial keratitis

Peg-shaped, notched central incisors (Hutchinson teeth)

Osteoperiostitis of the tibia ("saber shins")

Clutton joints
Signs and symptoms of primary syphilis
Signs and symptoms of secondary syphilis, latent syphilis, signs and symptoms of tertiary syphilis.
Loss of anal and bladder sphincter control
Dorsal column loss (loss of vibration and proprioception/position sense)
Romberg sign.
Behavioral changes
Memory impairment
Altered mood
Argyll-Robertson pupils.
HIV coinfection
Primary syphilis: larger, painful multiple ulcers.
Secondary syphilis: genital ulcers more common and higher titers with rapid plasma reagin (RPR) testing and Venereal Disease Research Laboratory (VDRL) testing.
Possibly more rapid progression to neurosyphilis. [ 18 ]
Serologic responses to infection may be atypical. [ 34 ]
Signs and symptoms of congenital syphilis
Identification of syphilis in the mother
Adequacy of maternal treatment
Presence of clinical, laboratory, or radiographic evidence of syphilis in the infant (testing should include paired maternal and neonatal nontreponemal serologic titers using the same test, preferably conducted at the same laboratory).
Peg-shaped central incisors, notched at the apex (Hutchinson teeth)
Eighth cranial nerve deafness
Frontal bossing of the skull
Anterior bowing of the shins (Saber shins)
Saddle nose deformity
Clutton joints (symmetric painless knee swelling).
Initial investigations for acquired syphilis
Treponemal enzyme immunoassay (EIA)
T pallidum particle agglutination assay (TPPA)
T pallidum haemagglutination assay (TPHA)
Fluorescent antibody absorption (FTA-ABS)
Immunocapture assay (ICA).
EIA: 3 weeks
TPPA: 4-6 weeks
TPHA: 4-6 weeks.
RPR: 4 weeks
VDRL: 4 weeks.
Other initial investigations for acquired syphilis
Emerging investigations, further investigations for acquired syphilis.
CSF white blood cell (WBC) count >10 cells/mm³ (10 × 10⁶ cells/L)
CSF protein >50 mg/dL (0.50 g/L)
A positive CSF VDRL test.
Initial investigations for congenital syphilis
Further investigations for congenital syphilis.
An abnormal physical exam that is consistent with congenital syphilis (e.g., nonimmune hydrops, conjugated or direct hyperbilirubinemia or cholestatic jaundice or cholestasis, hepatosplenomegaly, rhinitis, skin rash, or pseudoparalysis of an extremity) or
A serum quantitative nontreponemal serologic titer that is fourfold higher than the mother's titer (e.g., maternal titer = 1:2, neonatal titer ≥1:8 or maternal titer = 1:8, neonatal titer ≥1:32) or
A positive dark-field test or PCR of placenta, cord, lesions or body fluids, or a positive silver stain of the placenta or cord.
The mother was not treated, was inadequately treated, or has no documentation of having received treatment or
The mother was treated with erythromycin or other nonpenicillin regimen or
The mother received treatment <4 weeks before delivery.
Infants and children ages ≥1 month with reactive serologic tests for syphilis.
sexual contact with an infected person
The risk of acquiring syphilis after sex with someone with primary or secondary syphilis is between 30% and 60%. [ 17 ]
men who have sex with men (MSM)
At higher risk, particularly if they are also HIV coinfected, use illicit drugs such as methamphetamine, or have multiple, casual sexual partners. [ 21 ] [ 22 ]
In 2021, almost half (46.5%) of all reported cases of primary and secondary syphilis in the US occurred in MSM. [ 12 ]
illicit drug use
Association due to the exchange of sex for money or drugs, particularly crack cocaine. [ 23 ]
commercial sex workers
Multiple sexual partners.
A risk factor for all STIs.
Important in syphilis epidemiology. [ 21 ]
people with HIV or other STIs
Suggests unprotected sexual intercourse, which increases the risk of STIs.
All patients who have an STI should have syphilis screening, as should patients at higher risk of STIs, irrespective of where they are seen.
syphilis during pregnancy (risk for congenital syphilis)
The fetus acquires the infection from the infected mother. Inadequate treatment of maternal syphilis accounts for up to one-third of congenital syphilis cases. [ 24 ]
This may result in miscarriage, stillbirth, or neonatal death. [ 3 ]
Screening for syphilis at the first prenatal visit aims to identify and treat asymptomatic infected women, thus preventing transplacental transmission. [ 25 ] The Centers for Disease Control and Prevention recommends repeating syphilis screening at 28 weeks' gestation and at delivery for women at high risk of syphilis infection. Risk factors for syphilis infection during pregnancy include commercial sex work, a history of substance misuse, sex with multiple partners, late entry into prenatal care (i.e., first visit during the second trimester or later) or no prenatal care, unstable housing or homelessness, and imprisonment of the woman or her partner. [ 8 ]
Initially a macule, developing into a papule and then ulcerating to form a chancre. Image
Classically appears in the anogenital area 14 to 21 days after exposure (primary infection).
Usually indurated, solitary, and painless. Image
May not always be noticed by the patient and examining physician, and it heals spontaneously.
Atypically may be multiple and painful. Coinfection with genital herpes or chancroid may cause painful ulceration. HIV coinfection may be associated with multiple ulcers.
Erosions on the genitalia may also occur in secondary syphilis. Image
Moderately enlarged, rubbery regional lymphadenopathy associated with the classical syphilitic ulcer (chancre) in primary infection.
Generalized lymphadenopathy may occur with secondary syphilis.
Symmetric macular, papular, or maculopapular rash in secondary syphilis. Image
Often widespread with mucous membrane involvement. Image
May desquamate.
Usually nonitchy, over the trunk, palms, soles, and scalp.
In dark-skinned patients may cause pruritus.
May accompany a history of constitutional symptoms such as fever and malaise.
Onset is usually 6 to 12 weeks after exposure.
Up to 25% of people who have untreated secondary syphilis develop relapsing episodes of rash and fever. [ 9 ] [ 17 ]
Rash also occurs in congenital syphilis.
Such as fever, malaise, myalgia, fatigue, and arthralgia with secondary syphilis.
May be mistaken for primary HIV infection or another intercurrent viral illness.
As a result of cardiovascular syphilis (tertiary disease), which may lead to heart failure.
May also be a constitutional symptom in secondary syphilis.
A sign of early congenital syphilis (occurring <2 years of age).
Discharge may be purulent and bloody.
Usually associated with other signs of disseminated infection (rash, mucous membrane ulceration).
May develop in secondary syphilis.
Slightly raised, or flat, round, or oval papules covered by gray exudates.
A sign of secondary syphilis.
May be present within moist areas of the perineum.
May be mistaken for genital warts.
Possible signs of neurosyphilis. [ 66 ]
Brain involvement in tertiary syphilis causes a range of syndromes, including cognitive and motor impairment, which are sometimes grouped under the broad term "general paresis".
Visual impairment may be a presenting feature of syphilitic iritis or uveitis, occurring in secondary infection.
Bilaterally small, irregular pupils, which do not constrict when exposed to bright light, but do constrict in response to accommodation.
A feature of tabes dorsalis occurring in tertiary syphilis.
Dorsal column loss is a feature of tabes dorsalis, occurring in tertiary syphilis.
Possible sign of cardiovascular syphilis (tertiary disease).
Diastolic murmur at the left sternal edge indicates aortic regurgitation, which may be due to aortitis caused by cardiovascular syphilis.
A sign of gummatous syphilis (also known as benign tertiary syphilis).
Affects skin and visceral organs.
The destructive gumma may gradually replace normal tissue.
Signs of congenital syphilis. [ 67 ]
Signs of early congenital syphilis.
May occur in early congenital syphilis (occurring <2 years of age).
This rash may be similar to the rash of secondary syphilis in adults. It may also be more widespread, bullous or papulonecrotic, or desquamating.
Initially the rash may be a vesicular rash with small blisters appearing on the palms and plantar surfaces of the feet. An erythematous or maculopapular rash, which is often copper-colored, may subsequently appear on the face, palms, and plantar surfaces of the feet. The rash may also affect the mouth, genitalia, and anus. Images
A sign of late congenital syphilis (occurring >2 years of age).
Due to neonatal osteochondritis in congenital syphilis. Image
Including frontal bossing, high cranium, and saddle nose.
Hutchinson teeth (peg-shaped incisors, notched at the apex), mulberry molars dome-shaped with small cusps at the apex.
Poorly mineralized teeth. Image
Necrotizing funisitis (inflammation of the umbilical cord) is virtually diagnostic of congenital syphilis. Usually found in preterm infants who are stillborn, or die within a few weeks of birth.
The umbilical cord has a specific appearance known as the "barberpole" cord as a result of inflammation of the matrix of the umbilical cord. [ 37 ]
May coexist with genital ulceration.
Occurs in both primary and secondary infection.
In secondary infection the mouth ulcers (snail track ulcers) will usually be coexistent with other symptoms or signs, such as rash, fever.
Latent syphilis is defined as positive serology in the absence of clinical features of syphilis.
Ulcers in primary syphilis may not be noticed by the patient and examining physician.
Possible sign of tertiary disease with brain involvement.
May indicate neurologic involvement.
May occur with neck stiffness.
May be a presenting feature of syphilitic iritis or uveitis, occurring in secondary infection.
The eighth cranial nerve is the most commonly affected cranial nerve in neurosyphilis.
Hearing loss may be a symptom and a sign of both early and late neurosyphilis.
Deafness may also occur as a result of late congenital syphilis (occurring >2 years of age).
Suggest neurologic involvement.
Occurs with nephrotic syndrome that may develop due to vasculitis in secondary syphilis.
May indicate hepatitis, due to vasculitis in secondary syphilis.
Sign of neurosyphilis.
Usually affecting lower limbs.
May occur in all forms of neurosyphilis.
As a result of cardiovascular syphilis (tertiary disease).
Aortic aneurysm caused by syphilis almost always affects the thoracic aorta (usually the ascending part of the thoracic aorta), resulting in heart failure.
Lesions in gummatous syphilis may cause organomegaly, and become infiltrative or destructive.
May occur as a result of gummatous syphilis.
May include a wide range of problems such as seizures, meningitis, obstructive hydrocephalus, and cranial nerve palsies.
coiled spirochete bacterium with a corkscrew appearance and motility
Performed to identify Treponema pallidum .
Can provide a definitive diagnosis of syphilis, but is not usually available outside specialist settings.
The lesion is cleansed and abraded with a gauze pad until serous exudates appear, which are collected onto a glass slide for microscopic analysis.
A single negative result does not exclude infection; ideally 3 negative examinations on different days are required.
Primary syphilis: sensitivity of dark-field microscopy is 74% to 86%, specificity is 85% to 100%. [ 5 ] [ 6 ] [ 39 ]
Secondary syphilis: dark-field microscopy may be positive from ulcerative anogenital lesions.
Gummata in tertiary syphilis have few, if any, identifiable T pallidum organisms.
Congenital syphilis: test suspicious lesions (e.g., bullous rash or nasal discharge). [ 8 ]
A treponemal serology test.
A patient with a positive treponemal test result will remain positive for life. Therefore, a positive result alone cannot distinguish between an active infection or past (treated) infection.
The most common approach is to use a treponemal test as the initial serologic test, followed by a nontreponemal test to confirm diagnosis and provide evidence of active disease or reinfection (i.e., a "reverse sequence screening algorithm"). [ 40 ]
False-positive results may occur with other nonsexually transmitted treponemal infection (e.g., yaws, pinta, bejel).
False-negative results may occur in incubating and early primary syphilis. It usually takes 3 weeks for an EIA IgG/IgM test to become positive after infection with Treponema pallidum .
EIA is the test generally used for screening. [ 10 ]
Primary syphilis: EIA sensitivity 82% to 100%, and specificity 97% to 100%. [ 68 ]
Secondary syphilis: EIA sensitivity is 100%. [ 68 ]
Late latent syphilis: EIA sensitivity is 98% to 100%. [ 68 ]
A patient with a positive treponemal test result will remain positive for life. Therefore, a positive result alone cannot distinguish between an active or past (treated) infection.
Primary syphilis: TPPA sensitivity is 85% to 100%, and specificity is 98% to 100%. [ 69 ] [ 70 ]
Secondary and late latent syphilis: TPPA sensitivity is 98% to 100%. [ 70 ]
FTA-ABS is used less often than TPHA and TPPA because it is less specific.
LIA serologic tests (e.g., INNO-LIA syphilis test) can be used to confirm syphilis infection following initial serologic treponemal testing. A single LIA test can confirm infection, making it more convenient than traditional methods of serologic confirmation (which usually require multiple assays). Studies evaluating the performance of LIA tests for syphilis infection have demonstrated higher sensitivity and specificity compared with FTA-ABS and TPHA serology tests. [ 49 ] [ 50 ]
A nontreponemal serology test.
Provides a quantitative measure of disease activity and can be used to monitor treatment response (RPR titers decrease or become nonreactive with effective treatment).
Despite adequate treatment, some patients maintain a persisting low level positive antibody titer (known as a serofast reaction). [ 44 ]
False positives may occur due to the presence of a variety of medical conditions (e.g., pregnancy, autoimmune disorders, and infections).
A false-negative test may occasionally occur in an undiluted specimen (the prozone phenomenon).
Primary syphilis: RPR sensitivity is 70% to 73%. [ 5 ] [ 71 ]
Secondary syphilis: RPR sensitivity is 100%. [ 71 ]
Preferred test over the serum Venereal Disease Research Laboratory test.
Congenital syphilis: include paired maternal and neonatal nontreponemal serologic titers using the same test, preferably conducted at the same laboratory. [ 8 ]
The Food and Drug Administration (FDA) has issued a warning of false-positive RPR results linked to COVID-19 vaccination. RPR false reactivity has been observed in some individuals for at least 5 months following the vaccine. The issue has been identified in the Bio-Rad BioPlex 2200 Syphilis Total & RPR test kit. It is not yet known if other RPR tests are affected similarly. For healthcare professionals who use the Bio-Rad BioPlex 2200 Syphilis Total & RPR test kit, the FDA recommends performing confirmatory testing for all reactive results. In patients previously treated for syphilis who received a COVID-19 vaccine, and whose clinical presentation and epidemiologic considerations do not support syphilis reinfection, reactive RPR results obtained from the BioPlex 2200 Syphilis Total & RPR test kit should be confirmed using an RPR test from a different manufacturer. [ 45 ]
Provides a quantitative measure of disease activity and can be used to monitor treatment response (VDRL titers decrease or become nonreactive with effective treatment).
Primary syphilis: VDRL sensitivity is 44% to 76%. [ 5 ]
VDRL is positive in 77% of cases of late latent syphilis. [ 5 ]
VDRL sensitivity in secondary syphilis is 100%. [ 71 ]
WBC count >10 cells/mm³; CSF protein >50 mg/dL; CSF VDRL positive; CSF TPHA/TPPA/FTA-ABS positive
Indicated for any patient with clinical evidence of neurologic involvement (e.g., cranial nerve dysfunction, meningitis, stroke, acute or chronic altered mental status, or loss of vibration sense).
Indicated if syphilis of unknown duration exists in the presence of HIV coinfection.
Indicated in any child with congenital syphilis and neurologic symptoms or signs. [ 8 ]
An elevated CSF WBC count and positive CSF Venereal Disease Research Laboratory (VDRL) suggests neurologic involvement. [ 31 ]
Some patients with neurosyphilis have an isolated elevated CSF WBC count and negative rapid plasma reagin/VDRL.
Neurosyphilis is unlikely at CSF Treponema pallidum hemagglutination assay (TPHA)/ T pallidum particle agglutination assay (TPPA) titers <1:320.
A nonreactive CSF-TPHA test result usually excludes neurosyphilis.
possible widened thoracic aorta, aortic calcification
May detect possible thoracic aortic aneurysm or aortic calcification.
Required in people with symptoms or signs of aortic regurgitation, heart failure, or aortic aneurysm.
may show evidence of heart failure, aortic regurgitation, or thoracic aortic aneurysm
Required if cardiovascular syphilis is strongly suspected (e.g., a patient has symptoms or signs of aortic regurgitation, heart failure, or aortic aneurysm).
usually normal
Performed before lumbar puncture to exclude elevated intracranial pressure, to ensure that a lumbar puncture procedure will be safe.
Elevated intracranial pressure is rarely caused by syphilis itself.
positive or negative
All patients with syphilis should be tested for HIV.
In geographic areas in which the prevalence of HIV is high, patients who have syphilis should be retested for HIV after 3 months, even if the first HIV test result is negative, and be offered HIV pre-exposure prophylaxis (PrEP). [ 8 ]
All infants and children at risk for congenital syphilis should be tested for HIV. [ 8 ]
may show hepatomegaly, ascites, hydrops fetalis, intrauterine growth retardation
Should be performed on all pregnant women with syphilis or suspected of having syphilis.
Presence of fetal or placental syphilis indicates a greater risk of treatment failure for congenital syphilis. [ 65 ]
may show anemia, thrombocytopenia, leukopenia, possible neutrophilia
Performed in infants with possible congenital syphilis.
may demonstrate osteochondritis
May be indicated in infants with suspected congenital syphilis. [ 8 ]
Performed if osteochondritis suspected.
aspartate aminotransferase and alanine aminotransferase may be elevated
Performed if clinical findings suggestive of liver involvement (e.g., hepatomegaly).
may detect deafness
Performed if clinically indicated.
may detect hearing deficit
Neurosyphilis may involve cranial nerves (particularly the 8th cranial nerve).
osseous lesions
Might aid diagnosis of congenital syphilis in stillborn infants. [ 8 ]
T pallidum PCR has been shown to have moderate sensitivity (70% to 80%) and high specificity >90% in the diagnosis of primary or secondary syphilis, when compared with adequate reference tests (e.g., serology, dark-field microscopy). [ 51 ]
The Centers for Disease Control and Prevention considers PCR testing a valid method for diagnosing primary, secondary, and congenital syphilis, and its use is likely to increase. [ 8 ] [ 52 ]
positive; however, a positive result for treponemal antibodies alone does not distinguish between current, past, or treated infection
POC syphilis testing has been assessed in the setting of high-risk regions, where rapid and early diagnosis may be more important than accuracy. Several clinical trials have shown promise and POC testing has been recommended as part of the Pan American Health Organization strategy to diagnose and treat syphilis. [ 53 ] [ 54 ]
Genital herpes
Differentiating Signs/Symptoms
There may be a history of fever, genital blisters or sores, and lymphadenopathy with first episode herpes simplex.
The patient may describe previous episodes of genital ulceration.
On physical exam there are typically multiple, painful vesicular or ulcerative lesions on or around the genitals or rectum.
Differentiating Tests
If lesions are present, clinical diagnosis should be confirmed by swabbing lesions for herpes simplex virus (HSV) culture or HSV polymerase chain reaction (PCR). [ 8 ]
Because of the higher sensitivity of PCR, this is the preferred test when available. [ 8 ]
Glycoprotein G-based type-specific serology may be indicated in certain patient groups and can differentiate between infection with HSV-1 and HSV-2. [ 8 ]
Characterized by painful genital ulcers and painful inguinal lymphadenopathy. Lesions of primary syphilis are typically not painful.
Usually occurs in discrete outbreaks.
On physical exam there may be an erythematous papule, pustule, or painful ulcer, as well as painful unilateral inguinal lymphadenopathy (bubo formation), which may rupture.
Haemophilus ducreyi is identified on specialist culture medium, which is not widely commercially available and has a sensitivity of <80%. [ 72 ]
Polymerase chain reaction testing is up to 100% sensitive but is not universally approved. [ 72 ] [ 73 ]
Therefore a positive diagnosis of chancroid is suggested by the presence of one or more painful genital ulcers with no evidence of syphilis or herpes simplex virus. [ 8 ] Regional lymphadenopathy is also confirmatory, if present. [ 8 ]
Primary HIV infection
Not preceded by genital ulceration.
However, genital ulceration may be present at the same time as primary HIV infection and the rash associated with the ulceration.
Laboratory tests positive for HIV, including antigen (P24 antigen) tests.
Other acute viral exanthems
Laboratory tests positive for specific virus.
Skin lesions are usually pruritic.
Typical distribution: interdigital, wrists, nipples, ankles, buttocks.
Diagnosis is usually clinical, but skin scrapings and microscopy for Sarcoptes scabiei may be performed.
Skin lesions are usually absent on palms and plantar aspects of feet.
Not associated with signs of systemic infection.
Diagnosis is usually clinical.
Skin biopsy can be undertaken to confirm diagnosis.
Lichen planus
Skin lesions are usually absent on palms and plantar aspect of feet.
Genital warts
Pink lumps, in genital and/or perianal skin and mucous membranes. Not necessarily confined to opposing membranes.
Not associated with other signs of secondary syphilis (rash, constitutional symptoms, generalized lymphadenopathy).
Exclusion of syphilis (negative syphilis serology).
Alzheimer dementia
Progressive dementia.
No specific differentiating symptoms and signs compared with neurosyphilis.
Less likely to have a history of possible signs and symptoms of earlier stages of syphilis infection.

Vascular dementia
Multi-infarct dementia often associated with other evidence of arteriopathy.
Syphilis infection is often asymptomatic but highly transmissible
If untreated, it causes in-utero mortality and considerable morbidity many years after initial infection
Treatment of syphilis in the early stage of infection is curative and aims to halt disease progression and eliminate further transmission of infection
Syphilis is an important facilitator of HIV transmission.
Asymptomatic patients who are at risk of syphilis infection [ 1 ] [ 74 ]
Pregnant women [ 8 ] [ 29 ] [ 62 ] [ 63 ] [ 75 ]
Blood donors. [ 76 ]
Screening tests
Screening in sti clinic, prenatal screening, screening low-risk asymptomatic population, screening for hiv and other stis, treatment approach, without neurosyphilis, neurosyphilis, infection in pregnancy, coinfection with hiv, congenital syphilis.
Presence of clinical, laboratory, or radiographic evidence of syphilis in the infant (testing should include paired maternal and neonatal non-treponemal serological titres using the same test, preferably conducted at the same laboratory).
Potential adverse effects of therapy
Primary Options
penicillin G benzathine
2.4 million units intramuscularly as a single dose
Secondary Options
100 mg orally twice daily for 14 days
Empiric therapy may be considered in those with suspected early infection (a rash or ulceration) before results of serology are available. Empiric therapy may be appropriate if there are concerns regarding re-attendance. The benefits of empiric therapy (prompt therapy) and risks (potentially unnecessary treatment) should be discussed with the patient.
Intramuscular benzathine penicillin G as a single dose is given. If the patient is allergic to penicillin and is not pregnant, oral doxycycline may be offered.
Sexual contacts of patients with confirmed syphilis should be screened and offered presumptive treatment if follow-up may be problematic.
intramuscular benzathine penicillin G
primary/secondary/early latent syphilis (nonpregnant): 2.4 million units intramuscularly as a single dose; primary/secondary/early latent syphilis (pregnant): 2.4 million units intramuscularly as a single dose, may repeat in 1 week; late-latent/tertiary syphilis with normal cerebrospinal fluid examination: 2.4 million units intramuscularly once weekly for 3 weeks
The first-line treatment for primary, secondary, and early latent syphilis (without neurosyphilis) is intramuscular benzathine penicillin G as a single dose. [ 8 ] Note that the dose may be split and administered at two discrete injection sites.
The first-line treatment of late latent and tertiary (gummatous, cardiovascular, psychiatric manifestations, late neurosyphilis) syphilis with normal cerebrospinal fluid (CSF) examination is intramuscular benzathine penicillin G (once weekly for 3 weeks).
All patients who have tertiary syphilis should undergo cerebrospinal fluid examination before treatment is started. Patients with abnormal CSF findings should be treated with a neurosyphilis regimen. [ 8 ]
Pregnant women should receive penicillin-based treatment according to their stage of syphilis. For pregnant women with primary, secondary, or early latent syphilis, certain evidence suggests that administering two injections of intramuscular benzathine penicillin G, rather than one, can help prevent congenital syphilis. Pregnant women with late latent or tertiary syphilis with normal CSF examination should receive three injections of intramuscular benzathine penicillin G, as per the guidance for nonpregnant individuals. [ 8 ]
Most clinicians treat HIV-positive and HIV-negative individuals with the same penicillin regimens, according to the stage of syphilis. [ 8 ]
Antibiotic therapy for cardiovascular syphilis does not reverse cardiovascular disease, which may continue to progress after treatment. Discussion with a cardiologist is advised.
40-60 mg orally once daily for 3 days; start 24 hours before penicillin
Corticosteroid therapy may be considered to minimize the risk of Jarisch-Herxheimer reaction in nonpregnant patients with neurosyphilis. [ 10 ] However, evidence of effectiveness is unclear and it is not routinely recommended in the US.
Jarisch-Herxheimer reaction is an acute febrile illness that can occur within the first 24 hours after initiation of antibiotic treatment for syphilis. Symptoms include acute fever, headache, and myalgia, usually occurring in patients with early syphilis. [ 8 ]
oral doxycycline
100 mg orally twice daily for 14 days (primary/secondary/early latent syphilis) or 28 days (late latent/tertiary syphilis with normal cerebrospinal fluid examination)
If the patient is allergic to penicillin, the first-line treatment in nonpregnant patients is oral doxycycline.
Adherence and patient compliance may influence treatment outcome if oral therapy is administered.
Patients who are allergic to penicillin, with primary or secondary syphilis and HIV coinfection, should receive antibiotic therapy as recommended for penicillin-allergic, HIV-negative patients. [ 8 ]
40-60 mg orally once daily for 3 days; start 24 hours before doxycycline
Corticosteroid therapy may be considered to minimize the risk of Jarisch-Herxheimer reaction in nonpregnant patients with neurosyphilis. [ 10 ] However, evidence of effectiveness is unclear and it is not routinely recommended in the US.
desensitization
Penicillin desensitization is recommended for all patients with penicillin hypersensitivity in pregnancy. The evidence for the use of nonpenicillin regimens is relatively weak. [ 8 ]
Penicillin allergy skin testing identifies patients at high risk for penicillin reactions. Skin reagents used should include major and minor allergens. [ 97 ] Those who are skin-test negative can receive penicillin therapy. However, some clinicians perform desensitization without skin testing, particularly if the skin reagents for both minor and major determinants of penicillin allergy are not available.
Acute desensitization can be performed in patients who have a positive skin test to one of the penicillin determinants, and should be performed in a hospital setting. Oral or intravenous desensitization can be performed, and is usually completed in 4 hours, following which the first dose of penicillin is administered. [ 98 ]
postdesensitization intramuscular benzathine penicillin G
primary/secondary/early latent syphilis: 2.4 million units intramuscularly as a single dose, may repeat in 1 week; late-latent/tertiary syphilis with normal cerebrospinal fluid examination: 2.4 million units intramuscularly once weekly for 3 weeks
Desensitization is usually completed in 4 hours, following which the first dose of penicillin is administered. [ 98 ]
Pregnant women should receive penicillin-based treatment according to their stage of syphilis. For pregnant women with primary, secondary, or early latent syphilis, certain evidence suggests that administering two injections of intramuscular benzathine penicillin G, rather than one, can help prevent congenital syphilis. Pregnant women with late latent or tertiary syphilis with normal cerebrospinal fluid examination should receive three injections of intramuscular benzathine penicillin G, as per the guidance for nonpregnant individuals. [ 8 ]
adults with neurosyphilis
intravenous aqueous penicillin G
penicillin G sodium
18-24 million units/day intravenously given in divided doses every 4 hours (or by continuous infusion) for 10-14 days
Central nervous system involvement can occur at any stage of syphilis and can range from asymptomatic meningeal involvement to dementia and sensory neuropathy. [ 18 ] First-line treatment for neurosyphilis is intravenous aqueous penicillin G. [ 8 ]
Pregnant women should receive penicillin-based treatment according to their stage of syphilis.
Most clinicians treat HIV-positive and HIV-negative patients with the same penicillin regimens, according to the stage of syphilis. [ 8 ]
subsequent intramuscular benzathine penicillin G
2.4 million units intramuscularly once weekly for 1-3 weeks
Some specialists administer benzathine penicillin G once weekly for up to 3 weeks after the intravenous aqueous penicillin G regimen for neurosyphilis has been completed.
This ensures the duration of treatment is comparable with that of late syphilis in the absence of neurosyphilis. [ 8 ]
intramuscular procaine penicillin G plus oral probenecid
penicillin G procaine
2.4 million units intramuscularly once daily for 10-14 days
500 mg orally four times daily for 10-14 days
Second-line treatment for neurosyphilis is intramuscular procaine penicillin G plus oral probenecid.
Most clinicians treat HIV-positive and HIV-negative patients with the same penicillin regimens according to the stage of syphilis.
Pregnant women should receive penicillin-based treatment according to their stage of syphilis. [ 8 ]
with penicillin allergy
Penicillin desensitization is recommended for all patients with neurosyphilis who have penicillin hypersensitivity. The evidence for the use of nonpenicillin regimens is relatively weak. [ 8 ]
postdesensitization penicillin G
subsequent postdesensitization intramuscular benzathine penicillin G
Some specialists administer benzathine penicillin G once weekly for up to 3 weeks after the treatment regimen for neurosyphilis has been completed (only if first-line intravenous therapy was chosen as the initial therapy).
high-dose oral doxycycline
200 mg orally twice daily for 28 days
The evidence for the use of nonpenicillin regimens is relatively weak. However, high-dose doxycycline is used by some clinicians in this situation. [ 7 ] [ 18 ]
congenital syphilis
neonate: confirmed proven or highly probable congenital syphilis
intravenous aqueous penicillin G or intramuscular procaine penicillin G
100,000 to 150,000 units/kg/day intravenously, administered as 50,000 units/kg/dose every 12 hours during the first 7 days of life and then every 8 hours thereafter for a total of 10 days
50,000 units/kg intramuscularly once daily for 10 days
All neonates born to mothers who have reactive nontreponemal and treponemal tests results should be evaluated with a quantitative nontreponemal serologic test (rapid plasma reagin tests [RPR] or Venereal Disease Research Laboratory [VDRL]) performed on the neonate's serum. The nontreponemal test performed on the neonate should be the same type of nontreponemal test performed on the mother. [ 8 ]
Confirmed proven or highly probable syphilis includes any neonate with: an abnormal physical exam that is consistent with congenital syphilis (e.g., nonimmune hydrops, conjugated or direct hyperbilirubinemia or cholestatic jaundice or cholestasis, hepatosplenomegaly, rhinitis, skin rash, or pseudoparalysis of an extremity); a serum quantitative nontreponemal serologic titer that is fourfold (or greater) higher than the mother's titer at delivery (e.g., maternal titer = 1:2, neonatal titer ≥1:8 or maternal titer = 1:8, neonatal titer ≥1:32); or a positive darkfield test or polymerase chain reaction (PCR) of placenta, cord, lesions, or body fluids or a positive silver stain of the placenta or cord. [ 8 ]
First-line treatment of confirmed proven or highly probable congenital syphilis is intravenous aqueous penicillin G or intramuscular procaine penicillin G. [ 8 ] [ 100 ]
Discussion with an obstetric specialist and neonatologist is recommended. Subsequently, close clinical and serologic follow-up by a pediatric specialist is recommended.
Neonates with reactive nontreponemal tests should be followed up to ensure that the nontreponemal test returns to negative. [ 8 ]
Neonates with a penicillin allergy or those who develop an allergic reaction presumed secondary to penicillin should be desensitized and treated with penicillin. [ 8 ] The evidence for the use of nonpenicillin regimens is relatively weak.
Skin testing is not possible in neonates with congenital syphilis as the procedure has not been standardized in this age group. [ 8 ]
neonate: possible congenital syphilis
intravenous aqueous penicillin G or intramuscular procaine penicillin G or intramuscular benzathine penicillin G
50,000 units/kg intramuscularly as a single dose
All neonates born to mothers who have reactive nontreponemal and treponemal test results should be evaluated with a quantitative nontreponemal serologic test (rapid plasma reagin [RPR] or Venereal Disease Research Laboratory [VDRL]) performed on the neonate's serum. The nontreponemal test performed on the neonate should be the same type of nontreponemal test performed on the mother.
Possible congenital syphilis includes any neonate who has a normal physical exam and a serum quantitative nontreponemal serologic titer equal to or less than fourfold of the maternal titer at delivery (e.g., maternal titer = 1:8, neonatal titer ≤1:16) and one of the following: the mother was not treated, was inadequately treated, or has no documentation of having received treatment; the mother was treated with erythromycin or a regimen other than those recommended by the Centers for Disease Control and Prevention (i.e., a nonpenicillin G regimen); the mother received the recommended regimen but treatment was initiated <30 days before delivery. [ 8 ]
Treatment of possible congenital syphilis is intravenous aqueous penicillin G, intramuscular procaine penicillin G, or intramuscular benzathine penicillin G. [ 8 ] [ 100 ]
Single-dose benzathine penicillin G may be used if follow up is certain and the following investigations are normal: cerebrospinal fluid analysis for VDRL test, cell count, and protein; complete blood count including differential and platelet count; and long-bone radiographs. [ 8 ] Single-dose benzathine penicillin G may also be considered if the risk of untreated maternal syphilis is considered low and the neonate's nontreponemal test is nonreactive. If the mother had untreated early syphilis at the time of delivery, the neonate is at increased risk for congenital syphilis and the 10-day course of aqueous penicillin G should be considered, even if investigations are normal, nontreponemal test is nonreactive, and follow-up is assured. [ 8 ]
neonate: congenital syphilis less likely
Congenital syphilis is less likely in any neonate who has a normal physical exam and a serum quantitative nontreponemal serologic titer equal or less than fourfold of the maternal titer at delivery (e.g., maternal titer = 1:8, neonatal titer ≤1:16) and both of the following are true: the mother was treated during pregnancy, treatment was appropriate for the infection stage, and the treatment regimen was initiated ≥30 days before delivery; the mother has no evidence of reinfection or relapse. [ 8 ]
Recommended treatment is with intramuscular benzathine penicillin G. [ 8 ]
If the mother's nontreponemal titers decreased at least fourfold after therapy for early syphilis, or remained stable for low-titer, latent syphilis (e.g., VDRL test <1:2 or RPR <1:4), an alternative approach is to provide close serologic follow-up every 2-3 months for 6 months. [ 8 ]
neonate: congenital syphilis unlikely
observation
Congenital syphilis is unlikely if the neonate has a normal physical exam and a serum quantitative nontreponemal serologic titer equal to or less than fourfold of the maternal titer at delivery and both of the following are true: the mother's treatment was adequate before pregnancy; and the mother's nontreponemal serologic titer remained low and stable (i.e., serofast) before and during pregnancy and at delivery (e.g., VDRL test ≤1:2 or RPR ≤1:4). [ 8 ]
No treatment is required. However, neonates with reactive nontreponemal tests should be followed up to ensure that the nontreponemal test returns to negative. [ 8 ]
Intramuscular benzathine penicillin G may be considered, particularly if the neonate has a reactive nontreponemal test and follow up is not certain. [ 8 ]
infant or child
intravenous aqueous penicillin G or intramuscular benzathine penicillin G
200,000 to 300,000 units/kg/day intravenously, administered as 50,000 units/kg/dose every 4-6 hours for 10 days
50,000 units/kg intramuscularly once weekly for up to 3 weeks, maximum 2.4 million units/dose
Infants and children ages ≥1 month who have reactive serologic tests for syphilis (e.g., serum rapid plasma reagin reactive, serum treponemal enzyme immunoassay reactive, or serum Treponema pallidum particle agglutination reactive) should be examined thoroughly for clinical manifestations of congenital syphilis. [ 8 ] Maternal records should be reviewed for evidence of maternal infection. Maternal serologic tests may have been negative in cases of extremely early or incubating syphilis. [ 8 ]
Evaluation should include: cerebrospinal fluid analysis for Venereal Disease Research Laboratory test, cell count, and protein; complete blood count, including differential and platelet count; and other tests if clinically indicated (e.g., long-bone x-rays, chest x-ray, liver enzymes, neuroimaging, auditory brain-stem response). [ 8 ]
Infants and children with clinical manifestations of congenital syphilis or abnormal evaluation should be treated with intravenous aqueous penicillin G. A single dose of intramuscular benzathine penicillin G may be considered after the 10-day treatment course of intravenous aqueous penicillin G to provide a more comparable duration as treatment for late syphilis. [ 8 ]
Infants and children with no clinical manifestations of congenital syphilis and normal evaluation (including normal cerebrospinal fluid evaluation) may be treated with up to 3 weekly doses of intramuscular benzathine penicillin G. [ 8 ]
Infants and children ages >1 month with acquired primary or secondary syphilis should be managed by a pediatric infectious disease specialist and evaluated for sexual abuse. [ 8 ] See Sexual abuse and assault .
Infants and children with a penicillin allergy or those who develop an allergic reaction presumed secondary to penicillin should be desensitized and treated with penicillin. [ 8 ] Skin testing may be used in children ages ≥2 years. The evidence for the use of nonpenicillin regimens is relatively weak.
Azithromycin
Ceftriaxone, primary prevention, secondary prevention.
People exposed within 90 days preceding diagnosis of primary, secondary, or early latent syphilis in a sexual partner should be treated presumptively, on the basis that they may be infected even if seronegative. It is estimated that 30% to 60% of sexual partners of people with early syphilis will develop the infection. [ 17 ]
People exposed more than 90 days before diagnosis of primary, secondary, or early latent syphilis in a sexual partner should be treated presumptively if syphilis serology is not available immediately and if follow-up may be problematic.
Treatment of long-term sexual partners of patients with latent syphilis is dependent on clinical evaluation and serology results.
For primary syphilis: exposure 3 months before treatment, plus duration of symptoms.
For secondary syphilis: 6 months plus duration of symptoms.
For early latent syphilis: 1 year.
Follow-Up Overview
Natural course of infection
Serology test results
Jarisch-Herxheimer reaction
Occurs within the first 24 hours after antibiotic therapy due to the rapid killing of treponemes.
Characterized by acute fever, headache, and myalgia, usually in patients with early syphilis. [ 8 ]
The likelihood of reaction is high in early syphilis but low in late syphilis. However, all patients should be advised of a possible reaction prior to receiving antibiotic treatment.
In pregnant women, Jarisch-Herxheimer reaction may cause fetal distress and premature labor. [ 8 ]
Treatment is supportive with oral fluids, acetaminophen, and nonsteroidal anti-inflammatory drugs.
Corticosteroid therapy may be considered to minimize the risk of a Jarisch-Herxheimer reaction in nonpregnant patients with cardiovascular syphilis or neurosyphilis. [ 10 ] However, the evidence of effectiveness is unclear and it is not routinely recommended in the US.
allergic reaction to penicillin
May arise in patients not previously known to be allergic.
In patients with penicillin allergy, alternative treatment options may be offered, dependent on the stage of syphilis.
Penicillin allergy skin testing and desensitization may be required (e.g., in the treatment of pregnant women).
Penicillin-allergic responses may include urticaria, angioedema, and anaphylaxis.
Treatment of allergic reaction is determined by the severity of the reaction.
asymptomatic progression of disease
Organ-specific complications can occur in untreated infection of unknown duration.
Specialist opinion should be sought depending on the nature of the complication (e.g., ophthalmology specialist opinion for ocular infection, cardiovascular specialist opinion for aortic regurgitation).
HIV infection
Syphilis facilitates the acquisition of HIV. [ 17 ]
iatrogenic procaine reaction
Occurs when intramuscular procaine penicillin G (e.g., used to treat neurosyphilis) is mistakenly administered intravenously.
Patients may develop penicillin allergic responses, including anaphylactic shock. [ 23 ]
Key Articles
Stoltey JE, Cohen SE. Syphilis transmission: a review of the current evidence. Sex Health. 2015 Apr;12(2):103-9. [Abstract] [Full Text]
British Association for Sexual Health and HIV (BASHH). UK national guidelines on the management of syphilis. December 2015 [internet publication]. [Full Text]
World Health Organization. Guidelines for the treatment of Treponema pallidum (syphilis). 2016 [internet publication]. [Full Text]
Workowski KA, Bachmann LH, Chan PA, et al. Sexually transmitted infections treatment guidelines, 2021. MMWR Recomm Rep. MMWR Recomm Rep. 2021 Jul 23;70(4):1-187. [Abstract] [Full Text]
World Health Organization. WHO guideline on syphilis screening and treatment for pregnant women. 2017 [internet publication]. [Full Text]
Referenced Articles
1. Stoltey JE, Cohen SE. Syphilis transmission: a review of the current evidence. Sex Health. 2015 Apr;12(2):103-9. [Abstract] [Full Text]
2. Baughn RE, Musher DM. Secondary syphilitic lesions. Clin Microbiol Rev. 2005 Jan;18(1):205-16. [Abstract] [Full Text]
3. Newman L, Kamb M, Hawkes S, et al. Global estimates of syphilis in pregnancy and associated adverse outcomes: analysis of multinational antenatal surveillance data. PLoS Med. 2013;10(2):e1001396. [Abstract] [Full Text]
4. British Association for Sexual Health and HIV (BASHH). UK national guidelines on the management of syphilis. December 2015 [internet publication]. [Full Text]
5. Goh BT. Syphilis in adults. Sex Transm Infect. 2005 Dec;81(6):448-52. [Abstract] [Full Text]
6. O'Byrne P, MacPherson P. Syphilis. BMJ. 2019 Jun 28;365:l4159. [Erratum in: Syphilis. BMJ. 2019 Jul 19;366:l4746.] [Abstract] [Full Text]
7. World Health Organization. Guidelines for the treatment of Treponema pallidum (syphilis). 2016 [internet publication]. [Full Text]
8. Workowski KA, Bachmann LH, Chan PA, et al. Sexually transmitted infections treatment guidelines, 2021. MMWR Recomm Rep. MMWR Recomm Rep. 2021 Jul 23;70(4):1-187. [Abstract] [Full Text]
9. Ghanem KG, Ram S, Rice PA. The modern epidemic of syphilis. N Engl J Med. 2020 Feb 27;382(9):845-54. [Abstract]
10. British Association for Sexual Health and HIV (BASHH). UK national guidelines on the management of syphilis. December 2015 [internet publication]. [Full Text]
11. World Health Organization. Report on global sexually transmitted infection surveillance, 2018. 2018 [internet publication]. [Full Text]
12. Centers for Disease Control and Prevention. Sexually transmitted disease surveillance, 2021. Apr 2023 [internet publication]. [Abstract] [Full Text]
13. Edmondson DG, Hu B, Norris SJ. Long-term in vitro culture of the syphilis spirochete Treponema pallidum subsp. pallidum. mBio. 2018 Jun 26;9(3). [Abstract] [Full Text]
14. Lee V, Kinghorn G. Syphilis: an update. Clin Med (Lond). 2008 Jun;8(3):330-3. [Abstract] [Full Text]
15. Stoltey JE, Cohen SE. Syphilis transmission: a review of the current evidence. Sex Health. 2015 Apr;12(2):103-9. [Abstract] [Full Text]
16. Centers for Disease Control and Prevention. Transmission of primary and secondary syphilis by oral sex - Chicago, Illinois, 1998-2002. MMWR Morb Mortal Wkly Rep. 2004 Oct 22;53(41):966-8. [Abstract] [Full Text]
17. French P. Syphilis. BMJ. 2007 Jan 20;334(7585):143-7. [Abstract]
18. Ropper AH. Neurosyphilis. N Engl J Med. 2019 Oct 3;381(14):1358-63. [Abstract]
19. Clark EG, Danbolt N. The Oslo study of the natural course of untreated syphilis. Med Clin North Am. 1964;48:613-21.
20. Chaudhary PM, Roninson IB. Activation of MDR1 (P-glycoprotein) gene expression in human cells by protein kinase C agonists. Oncol Res. 1992;4(7):281-90. [Abstract]
21. Peterman TA, Heffelfinger JD, Swint EB, et al. The changing epidemiology of syphilis. Sex Transm Dis. 2005 Oct;32(10 suppl):S4-10. [Abstract]
22. Centers for Disease Control and Prevention. Outbreak of syphilis among men who have sex with men - Southern California, 2000. MMWR Morb Mortal Wkly Rep. 2001 Feb 23;50(7):117-20. [Abstract]
23. Janier M, Unemo M, Dupin N, et al. 2020 European guideline on the management of syphilis. J Eur Acad Dermatol Venereol. 2021 Mar;35(3):574-88. [Abstract]
24. Keuning MW, Kamp GA, Schonenberg-Meinema D, et al. Congenital syphilis, the great imitator-case report and review. Lancet Infect Dis. 2020 Jul;20(7):e173-9. [Abstract]
25. Saloojee H, Velaphi S, Goga Y, et al. The prevention and management of congenital syphilis: an overview and recommendations. Bull World Health Organ. 2004 Jun;82(6):424-30. [Abstract] [Full Text]
26. National Institute for Health and Care Excellence. Recommendations on reducing sexually transmitted infections. Jun 2022 [internet publication]. [Full Text]
27. Holmes KK, Levine R, Weaver M. Effectiveness of condoms in preventing sexually transmitted infections. Bull World Health Organ. 2004 Jun;82(6):454-61. [Abstract]
28. Tobian AA, Serwadda D, Quinn TC, et al. Male circumcision for the prevention of HSV-2 and HPV infections and syphilis. N Engl J Med. 2009 Mar 26;360(13):1298-309. [Abstract] [Full Text]
29. US Preventive Services Task Force. Syphilis infection in pregnant women: screening. Sept 2018 [internet publication]. [Full Text]
30. Molina JM, Charreau I, Chidiac C, et al. Post-exposure prophylaxis with doxycycline to prevent sexually transmitted infections in men who have sex with men: an open-label randomised substudy of the ANRS IPERGAY trial. Lancet Infect Dis. 2018 Mar;18(3):308-17. [Abstract] [Full Text]
31. Brown DL, Frank JE. Diagnosis and management of syphilis. Am Fam Physician. 2003 Jul 15;68(2):283-90. [Abstract]
32. Rompalo AM, Lawlor J, Seaman P, et al. Modification of syphilitic genital ulcer manifestations by coexistent HIV infection. Sex Transm Dis. 2001 Aug;28(8):448-54. [Abstract] [Full Text]
33. Lafond RE, Lukehart SA. Biological basis for syphilis. Clin Microbiol Rev. 2006 Jan;19(1):29-49. [Abstract] [Full Text]
34. Tucker JD, Li JZ, Robbins GK, et al. Ocular syphilis among HIV-infected patients: a systematic analysis of the literature. Sex Trans Infect. 2011 Feb;87(1):4-8. [Abstract]
35. Rottingen JA, Cameron DW, Garnett GP. A systematic review of the epidemiologic interactions between classic sexually transmitted diseases and HIV: how much is really known? Sex Transm Dis. 2001 Oct;28(10):579-97. [Abstract]
36. Centers for Disease Control and Prevention. Sexually transmitted disease (STDs): syphilis & MSM fact sheet. 22 July 2021 [internet publication]. [Full Text]
37. Fojaco RM, Hensley GT, Moskowitz L. Congenital syphilis and necrotizing funisitis. JAMA. 1989 Mar 24-31;261(12):1788-90. [Abstract]
38. Hammerschlag MR, Guillén CD. Medical and legal implications of testing for sexually transmitted infections in children. Clin Microbiol Rev. 2010 Jul;23(3):493-506. [Abstract] [Full Text]
39. Wheeler HL, Agarwal S, Goh BT. Dark ground microscopy and treponemal serological tests in the diagnosis of early syphilis. Sex Transm Infect. 2004 Oct;80(5):411-4. [Abstract]
40. Centers for Disease Control and Prevention. Sexually transmitted diseases: syphilis. CDC fact sheet (detailed). 10 August 2021 [internet publication]. [Full Text]
41. Centers for Disease Control and Prevention (CDC). Discordant results from reverse sequence syphilis screening - five laboratories, United States, 2006-2010. MMWR Morb Mortal Wkly Rep. 2011 Feb 11;60(5):133-7. [Abstract] [Full Text]
42. Park IU, Fakile YF, Chow JM, et al. Performance of treponemal tests for the diagnosis of syphilis. Clin Infect Dis. 2019 Mar 5;68(6):913-18. [Abstract] [Full Text]
43. Pope V. Use of treponemal tests to screen for syphilis. Infect Med. 2004;21:399-402.
44. Seña AC, Wolff M, Behets F, et al. Rate of decline in nontreponemal antibody titers and seroreversion after treatment of early syphilis. Sex Transm Dis. 2017 Jan;44(1):6-10. [Abstract] [Full Text]
45. US Food and Drug Administration. Possible false RPR reactivity with BioPlex 2200 Syphilis Total & RPR test kit following a COVID-19 vaccine - letter to clinical laboratory staff and health care providers. Dec 2021 [internet publication]. [Full Text]
46. Smith G, Holman RP. The prozone phenomenon with syphilis and HIV-1 co-infection. South Med J. 2004 Apr;97(4):379-82. [Abstract]
47. Kingston AA, Vujevich J, Shapiro M, et al. Seronegative secondary syphilis in 2 patients coinfected with human immunodeficiency virus. Arch Dermatol. 2005 Apr;141(4):431-3. [Abstract]
48. British Association for Sexual Health and HIV (BASHH). BASHH national guideline on the management of sexually transmitted infections and related conditions in children and young people 2021. 2021 [internet publication]. [Full Text]
49. Lam TK, Lau HY, Lee YP, et al. Comparative evaluation of the INNO-LIA syphilis score and the MarDx Treponema pallidum immunoglobulin G Marblot test assays for the serological diagnosis of syphilis. Int J STD AIDS. 2010 Feb;21(2):110-3. [Abstract]
50. Hagedorn HJ, Kraminer-Hagedorn A, de Bosschere K, et al. Evaluation of INNO-LIA syphilis assay as a confirmatory test for syphilis. J Clin Microbiol. 2002 Mar;40(3):973-8. [Abstract] [Full Text]
51. Gayet-Ageron A, Lautenschlager S, Ninet B, et al. Sensitivity, specificity and likelihood ratios of PCR in the diagnosis of syphilis: a systematic review and meta-analysis. Sex Transm Infect. 2013 May;89(3):251-6. [Abstract]
52. Gayet-Ageron A, Sednaoui P, Lautenschlager S, et al. Use of Treponema pallidum PCR in testing of ulcers for diagnosis of primary syphilis. Emerg Infect Dis. 2015 Jan;21(1):127-9. [Abstract] [Full Text]
53. Shahrook S, Mori R, Ochirbat T, et al. Strategies of testing for syphilis during pregnancy. Cochrane Database Syst Rev. 2014 Oct 29;(10):CD010385. [Abstract] [Full Text]
54. Pan American Health Organization (PAHO). Guidance on syphilis testing in Latin America and the Caribbean: improving uptake, interpretation, and quality of testing in different clinical settings. 2015. 2015 [internet publication]. [Full Text]
55. Luger AF, Schmidt BL, Kaulich M. Significance of laboratory findings for the diagnosis of neurosyphilis. Int J STD AIDS. 2000 Apr;11(4):224-34. [Abstract]
56. Lavi R, Yarnitsky D, Rowe JM, et al. Standard vs atraumatic Whitacre needle for diagnostic lumbar puncture: a randomized trial. Neurology. 2006 Oct 24;67(8):1492-4. [Abstract]
57. Arendt K, Demaerschalk BM, Wingerchuk DM, et al. Atraumatic lumbar puncture needles: after all these years, are we still missing the point? Neurologist. 2009 Jan;15(1):17-20. [Abstract]
58. Nath S, Koziarz A, Badhiwala JH, et al. Atraumatic versus conventional lumbar puncture needles: a systematic review and meta-analysis. Lancet. 2018 Mar 24;391(10126):1197-204. [Abstract]
59. Rochwerg B, Almenawer SA, Siemieniuk RAC, et al. Atraumatic (pencil-point) versus conventional needles for lumbar puncture: a clinical practice guideline. BMJ. 2018 May 22;361:k1920. [Abstract] [Full Text]
60. Ahmed SV, Jayawarna C, Jude E. Post lumbar puncture headache: diagnosis and management. Postgrad Med J. 2006 Nov;82(973):713-6. [Abstract] [Full Text]
61. Arevalo-Rodriguez I, Ciapponi A, Roqué i Figuls M, et al. Posture and fluids for preventing post-dural puncture headache. Cochrane Database Syst Rev. 2016 Mar 7;(3):CD009199. [Abstract] [Full Text]
62. American College of Obstetricians and Gynecologists. ACOG Committee Opinion No. 752: prenatal and perinatal human immunodeficiency virus testing. Obstet Gynecol. 2018 Sep;132(3):e138-42. [Abstract] [Full Text]
63. National Institute for Health and Care Excellence (UK). Antenatal care. 19 August 2021 [internet publication]. [Full Text]
64. Simundic AM, Bölenius K, Cadamuro J, et al. Joint EFLM-COLABIOCLI recommendation for venous blood sampling. Clin Chem Lab Med. 2018;56(12):2015-38. [Abstract]
65. Hollier LM, Harstad TW, Sanchez PJ, et al. Fetal syphilis: clinical and laboratory characteristics. Obstet Gynecol. 2001 Jun;97(6):947-53. [Abstract]
66. Ropper AH. Neurosyphilis. N Engl J Med. 2019 Oct 3;381(14):1358-63. [Abstract]
67. Arnesen L, Serruya S, Duran P. Gestational syphilis and stillbirth in the Americas: a systematic review and meta-analysis. Rev Panam Salud Publica. 2015 Jun;37(6):422-9. [Abstract] [Full Text]
68. Cole M, Perry K. MHRA 04109: ten syphilis EIAs. UK: HSMO; 2004.
69. Creegan L, Bauer HM, Samuel MC, et al. An evaluation of the relative sensitivities of the venereal disease research laboratory test and the Treponema Pallidum particle agglutination test among patients diagnosed with primary syphilis. Sex Transm Dis. 2007 Dec;34(12):1016-18. [Abstract]
70. Manavi K, Young H, McMillan A. The sensitivity of syphilis assays in detecting different stages of early syphilis. Int J STD AIDS. 2006 Nov;17(11):768-71. [Abstract]
71. Cantor A, Nelson HD, Daeges M, et al. Screening for syphilis in nonpregnant adolescents and adults: systematic review to update the 2004 US Preventive Services Task Force recommendation [Internet]. Rockville (MD): Agency for Healthcare Research and Quality (US); 2016 Jun. Report No: 14-05213-EF-1. [Abstract] [Full Text]
72. Lewis DA. Chancroid: clinical manifestations, diagnosis, and management. Sex Transm Infect. 2003 Feb;79(1):68-71. [Abstract] [Full Text]
73. Patterson K, Olsen B, Thomas C, et al. Development of a rapid immunodiagnostic test for Haemophilus ducreyi. J Clin Microbiol. 2002 Oct;40(10):3694-702. [Abstract] [Full Text]
74. US Preventive Services Task Force. Syphilis infection in nonpregnant adults and adolescents: screening. Sep 2022 [internet publication] [Full Text]
75. World Health Organization. WHO guideline on syphilis screening and treatment for pregnant women. 2017 [internet publication]. [Full Text]
76. World Health Organization. Screening donated blood for transfusion-transmissible infections: recommendations. 2009 [internet publication]. [Abstract] [Full Text]
77. Tucker JD, Bu J, Brown LB, et al. Accelerating worldwide syphilis screening through rapid testing: a systematic review. Lancet Infect Dis. 2010 Jun;10(6):381-6. [Abstract]
78. World Health Organization. The use of rapid syphilis tests. 2006 [internet publication]. [Full Text]
79. Young H. Guidelines for serological testing for syphilis. Sex Transm Infect. 2000 Oct;76(5):403-5. [Abstract]
80. Centers for Disease Control and Prevention. Recommendations for partner services programs for HIV infection, syphilis, gonorrhea, and chlamydial infection. MMWR Recomm Rep. 2008 Nov 7;57(RR-9):1-83;quiz CE1-4. [Abstract] [Full Text]
81. World Health Organization. WHO guideline on self-care interventions for health and well-being, 2022 revision. Jun 2022 [internet publication]. [Full Text]
82. Lin JS, Eder ML, Bean SI. Screening for syphilis infection in pregnant women: updated evidence report and systematic review for the US Preventive Services Task Force. JAMA. 2018 Sep 4;320(9):918-25. [Abstract] [Full Text]
83. World Health Organization, Department of Reproductive Health and Research. The global elimination of congenital syphilis: rationale and strategy for action. 2007 [internet publication]. [Full Text]
84. Menezes EV, Yakoob MY, Soomro T, et al. Reducing stillbirths: prevention and management of medical disorders and infections during pregnancy. BMC Pregnancy Childbirth. 2009 May 7;9(suppl 1):S4. [Abstract] [Full Text]
85. Hawkes SJ, Gomez GB, Broutet N. Early antenatal care: does it make a difference to outcomes of pregnancy associated with syphilis? A systematic review and meta-analysis. PLoS One. 2013;8(2):e56713. [Abstract] [Full Text]
86. Blencowe H, Cousens S, Kamb M, et al. Lives Saved Tool supplement detection and treatment of syphilis in pregnancy to reduce syphilis related stillbirths and neonatal mortality. BMC Public Health. 2011 Apr 13;11(suppl 3):S9. [Abstract] [Full Text]
87. Chen XS, Peeling RW, Yin YP, Mabey D. Improving antenatal care to prevent adverse pregnancy outcomes caused by syphilis. Future Microbiol. 2011 Oct;6(10):1131-4. [Abstract]
88. Hawkes S, Matin N, Broutet N, et al. Effectiveness of interventions to improve screening for syphilis in pregnancy: a systematic review and meta-analysis. Lancet Infect Dis. 2011 Sep;11(9):684-91. [Abstract]
89. Munkhuu B, Liabsuetrakul T, Chongsuvivatwong V, et al. One-stop service for antenatal syphilis screening and prevention of congenital syphilis in Ulaanbaatar, Mongolia: a cluster randomized trial. Sex Transm Dis. 2009 Nov;36(11):714-20. [Abstract]
90. World Health Organization. WHO guideline on syphilis screening and treatment for pregnant women. 2017 [internet publication]. [Full Text]
91. Stoner BP. Current controversies in the management of adult syphilis. Clin Infect Dis. 2007 Apr 1;44(suppl 3):S130-46. [Abstract] [Full Text]
92. Parkes R, Renton A, Meheus A, et al. Review of current evidence and comparison for effective syphilis treatment in Europe. Int J STD AIDS. 2004 Feb;15(2):73-88. [Abstract]
93. Hook EW 3rd, Martin DH, Stephens J, et al. A randomized, comparative pilot study of azithromycin versus benzathine penicillin G for treatment of early syphilis. Sex Transm Dis. 2002 Aug;29(8):486-90. [Abstract]
94. Riedner G, Rusizoka M, Todd J, et al. Single-dose azithromycin versus penicillin G benzathine for the treatment of early syphilis. N Engl J Med. 2005 Sep 22;353(12):1236-44. [Abstract] [Full Text]
95. Lukehart SA, Godornes C, Molini BJ, et al. Macrolide resistance in Treponema pallidum in the United States and Ireland. N Engl J Med. 2004 Jul 8;351(2):154-8. [Abstract] [Full Text]
96. World Health Organization. Guidelines for the treatment of Treponema pallidum (syphilis). 2016 [internet publication]. [Full Text]
97. Ansotegui IJ, Melioli G, Canonica GW, et al. IgE allergy diagnostics and other relevant tests in allergy, a World Allergy Organization position paper. World Allergy Organ J. 2020 Feb;13(2):100080. [Abstract] [Full Text]
98. Chastain DB, Hutzley VJ, Parekh J, et al. Antimicrobial desensitization: a review of published protocols. Pharmacy (Basel). 2019 Aug 9;7(3):112. [Abstract] [Full Text]
99. World Health Organization. WHO guideline on syphilis screening and treatment for pregnant women. 2017 [internet publication]. [Full Text]
100. Walker GJ, Walker D, Molano Franco D, et al. Antibiotic treatment for newborns with congenital syphilis. Cochrane Database Syst Rev. 2019 Feb 15;(2):CD012071. [Abstract] [Full Text]
101. Liang Z, Chen YP, Yang CS, et al. Meta-analysis of ceftriaxone compared with penicillin for the treatment of syphilis. Int J Antimicrob Agents. 2016 Jan;47(1):6-11. [Abstract]
102. Liu HY, Han Y, Chen XS, et al. Comparison of efficacy of treatments for early syphilis: A systematic review and network meta-analysis of randomized controlled trials and observational studies. PLoS One. 2017 Jun 28;12(6):e0180001. [Abstract] [Full Text]
103. Faculty of Sexual and Reproductive Healthcare. Barrier methods for contraception and STI prevention. August 2015 [internet publication]. [Full Text]
104. Ng BE, Butler LM, Horvath T, et al. Population-based biomedical sexually transmitted infection control interventions for reducing HIV infection. Cochrane Database Syst Rev. 2011 Mar 16;(3):CD001220. [Abstract] [Full Text]
105. de Walque D, Dow WH, Nathan R, et al. Incentivising safe sex: a randomised trial of conditional cash transfers for HIV and sexually transmitted infection prevention in rural Tanzania. BMJ Open. 2012 Feb 8;2(1):e000747. [Abstract] [Full Text]
106. British Association for Sexual Health and HIV (BASHH). BASHH National Guideline on the Management of Sexually Transmitted Infections and Related Conditions in Children and Young People 2021. 2021 [internet publication]. [Full Text]
Published by
Centers for Disease Control and Prevention
World Health Organization
International Union against Sexually Transmitted Infections
British Association for Sexual Health and HIV
International Union against Sexually Transmitted Infections
National Institute for Health and Care Excellence (UK)
Faculty of Sexual and Reproductive Healthcare (UK)
Topic last updated: 2024-04-12
Juan C. Salazar , MD, MPH, FAAP
Professor and Chair
Department of Pediatrics
University of Connecticut School of Medicine
Physician in Chief
Connecticut Children's
Acknowledgements :
Dr Juan C. Salazar would like to gratefully acknowledge Adriana R. Cruz, Jairo M. Montezuma-Rusca, Nicholas Bennett, Patrick French, and Nooshin Barmania, previous contributors to this topic. We would also like to acknowledge our infectious diseases expert panel member, Dr Elisabeth Adderson, for her contribution to this topic.
Peer Reviewers
Robert A. Larsen , MD
Associate Professor of Medicine
University of Southern California
Keck School of Medicine
Los Angeles
William Rodriguez , MD
Assistant Professor of Medicine
Harvard Medical School
Director of Research
Global Health Delivery Project
Harvard School of Public Health
Jennifer Handforth , MB ChB, MRCPCH, DTM&H
Consultant Paediatrician
Croydon University Hospital
- Summary of Recommendation
- USPSTF Assessment of Magnitude of Net Benefit
- Practice Considerations
- Reaffirmation of Previous USPSTF Recommendation
- Supporting Evidence
- Research Needs and Gaps
- Recommendations of Others
- Article Information
See the Practice Considerations section for information on increased risk. USPSTF indicates US Preventive Services Task Force.
USPSTF indicates US Preventive Services Task Force.
eFigure. US Preventive Services Task Force (USPSTF) Grades and Levels of Evidence
- USPSTF Review: Screening for Syphilis Infection in Nonpregnant Adults and Adolescents JAMA Research Letter September 27, 2022 This systematic review to support the 2022 US Preventive Services Task Force Recommendation Statement on screening for syphilis infection summarizes published evidence on the benefits and harms of screening for syphilis infection in asymptomatic, nonpregnant adults and adolescents at increased risk for syphilis infection. Michelle L. Henninger, PhD; Sarah I. Bean, MPH; Jennifer S. Lin, MD, MCR
- The Critical Need to Modernize Syphilis Screening JAMA Editorial September 27, 2022 Susan Tuddenham, MD, MPH; Khalil G. Ghanem, MD, PhD
- Patient Information: Screening for Syphilis JAMA JAMA Patient Page September 27, 2022 This JAMA Patient Page summarizes the US Preventive Services Task Force’s recent recommendations on screening for syphilis infection in adults and adolescents who are at increased risk for syphilis infection. Jill Jin, MD, MPH
- A Man With Asymptomatic Ulcerated White Plaques on the Soft Palate JAMA JAMA Clinical Challenge February 28, 2023 A man in his 60s had irregular gray-white ulcers with a surrounding erythema on the soft palate, uvula, and tonsils that did not improve with oral cefuroxime. He reported sexual contact with 1 male partner over the prior 6 months; history and physical examination findings were otherwise unremarkable. What is the diagnosis and what would you do next? Shuni Ying, MD; Sheng Li, MD; Jianjun Qiao, MD, PhD
- Patient Information: Syphilis JAMA JAMA Patient Page May 16, 2023 This JAMA Patient Page describes syphilis, its signs and symptoms, diagnosis, and treatment. Shiwei Zhou, MD; Rishi Chanderraj, MD
- Screening for Syphilis in Nonpregnant Adults and Adolescents JAMA Network Open Editorial September 27, 2022 Ronnie M. Gravett, MD; Jeanne Marrazzo, MD, MPH
- Resurgence of Syphilis in the US—USPSTF Reaffirms Screening Guidelines JAMA Dermatology Editorial November 1, 2022 Erin H. Amerson, MD; Herbert B. Castillo Valladares, MD, MHS; Kieron S. Leslie, MD
See More About
Select your interests.
Customize your JAMA Network experience by selecting one or more topics from the list below.
- Academic Medicine
- Acid Base, Electrolytes, Fluids
- Allergy and Clinical Immunology
- American Indian or Alaska Natives
- Anesthesiology
- Anticoagulation
- Art and Images in Psychiatry
- Artificial Intelligence
- Assisted Reproduction
- Bleeding and Transfusion
- Caring for the Critically Ill Patient
- Challenges in Clinical Electrocardiography
- Climate and Health
- Climate Change
- Clinical Challenge
- Clinical Decision Support
- Clinical Implications of Basic Neuroscience
- Clinical Pharmacy and Pharmacology
- Complementary and Alternative Medicine
- Consensus Statements
- Coronavirus (COVID-19)
- Critical Care Medicine
- Cultural Competency
- Dental Medicine
- Dermatology
- Diabetes and Endocrinology
- Diagnostic Test Interpretation
- Drug Development
- Electronic Health Records
- Emergency Medicine
- End of Life, Hospice, Palliative Care
- Environmental Health
- Equity, Diversity, and Inclusion
- Facial Plastic Surgery
- Gastroenterology and Hepatology
- Genetics and Genomics
- Genomics and Precision Health
- Global Health
- Guide to Statistics and Methods
- Hair Disorders
- Health Care Delivery Models
- Health Care Economics, Insurance, Payment
- Health Care Quality
- Health Care Reform
- Health Care Safety
- Health Care Workforce
- Health Disparities
- Health Inequities
- Health Policy
- Health Systems Science
- History of Medicine
- Hypertension
- Images in Neurology
- Implementation Science
- Infectious Diseases
- Innovations in Health Care Delivery
- JAMA Infographic
- Law and Medicine
- Leading Change
- Less is More
- LGBTQIA Medicine
- Lifestyle Behaviors
- Medical Coding
- Medical Devices and Equipment
- Medical Education
- Medical Education and Training
- Medical Journals and Publishing
- Mobile Health and Telemedicine
- Narrative Medicine
- Neuroscience and Psychiatry
- Notable Notes
- Nutrition, Obesity, Exercise
- Obstetrics and Gynecology
- Occupational Health
- Ophthalmology
- Orthopedics
- Otolaryngology
- Pain Medicine
- Palliative Care
- Pathology and Laboratory Medicine
- Patient Care
- Patient Information
- Performance Improvement
- Performance Measures
- Perioperative Care and Consultation
- Pharmacoeconomics
- Pharmacoepidemiology
- Pharmacogenetics
- Pharmacy and Clinical Pharmacology
- Physical Medicine and Rehabilitation
- Physical Therapy
- Physician Leadership
- Population Health
- Primary Care
- Professional Well-being
- Professionalism
- Psychiatry and Behavioral Health
- Public Health
- Pulmonary Medicine
- Regulatory Agencies
- Reproductive Health
- Research, Methods, Statistics
- Resuscitation
- Rheumatology
- Risk Management
- Scientific Discovery and the Future of Medicine
- Shared Decision Making and Communication
- Sleep Medicine
- Sports Medicine
- Stem Cell Transplantation
- Substance Use and Addiction Medicine
- Surgical Innovation
- Surgical Pearls
- Teachable Moment
- Technology and Finance
- The Art of JAMA
- The Arts and Medicine
- The Rational Clinical Examination
- Tobacco and e-Cigarettes
- Translational Medicine
- Trauma and Injury
- Treatment Adherence
- Ultrasonography
- Users' Guide to the Medical Literature
- Vaccination
- Venous Thromboembolism
- Veterans Health
- Women's Health
- Workflow and Process
- Wound Care, Infection, Healing
Others Also Liked
- Download PDF
- X Facebook More LinkedIn
- CME & MOC
US Preventive Services Task Force. Screening for Syphilis Infection in Nonpregnant Adolescents and Adults : US Preventive Services Task Force Reaffirmation Recommendation Statement . JAMA. 2022;328(12):1243–1249. doi:10.1001/jama.2022.15322
Manage citations:
© 2024
- Permissions
Screening for Syphilis Infection in Nonpregnant Adolescents and Adults : US Preventive Services Task Force Reaffirmation Recommendation Statement
- Editorial The Critical Need to Modernize Syphilis Screening Susan Tuddenham, MD, MPH; Khalil G. Ghanem, MD, PhD JAMA
- Editorial Screening for Syphilis in Nonpregnant Adults and Adolescents Ronnie M. Gravett, MD; Jeanne Marrazzo, MD, MPH JAMA Network Open
- Editorial Resurgence of Syphilis in the US—USPSTF Reaffirms Screening Guidelines Erin H. Amerson, MD; Herbert B. Castillo Valladares, MD, MHS; Kieron S. Leslie, MD JAMA Dermatology
- Research Letter USPSTF Review: Screening for Syphilis Infection in Nonpregnant Adults and Adolescents Michelle L. Henninger, PhD; Sarah I. Bean, MPH; Jennifer S. Lin, MD, MCR JAMA
- JAMA Patient Page Patient Information: Screening for Syphilis Jill Jin, MD, MPH JAMA
- JAMA Clinical Challenge A Man With Asymptomatic Ulcerated White Plaques on the Soft Palate Shuni Ying, MD; Sheng Li, MD; Jianjun Qiao, MD, PhD JAMA
- JAMA Patient Page Patient Information: Syphilis Shiwei Zhou, MD; Rishi Chanderraj, MD JAMA
Importance Syphilis is a sexually transmitted infection that can progress through different stages (primary, secondary, latent, and tertiary) and cause serious health problems if left untreated. Reported cases of primary and secondary syphilis in the US increased from a record low of 2.1 cases per 100 000 population in 2000 and 2001 to 11.9 cases per 100 000 population in 2019. Men account for the majority of cases (83% of primary and secondary syphilis cases in 2019), and rates among women nearly tripled from 2015 to 2019.
Objective To reaffirm its 2016 recommendation, the US Preventive Services Task Force (USPSTF) commissioned a reaffirmation evidence update focusing on targeted key questions evaluating the performance of risk assessment tools and the benefits and harms of screening for syphilis in nonpregnant adolescents and adults.
Population Asymptomatic, nonpregnant adolescents and adults who have ever been sexually active and are at increased risk for syphilis infection.
Evidence Assessment Using a reaffirmation process, the USPSTF concludes with high certainty that there is a substantial net benefit of screening for syphilis infection in nonpregnant persons who are at increased risk for infection.
Recommendation The USPSTF recommends screening for syphilis infection in persons who are at increased risk for infection. (A recommendation)
See the Summary of Recommendation figure.
Syphilis is a sexually transmitted infection (STI) that can progress through different stages (primary, secondary, latent, and tertiary) and cause serious health problems if left untreated. 1 Tertiary syphilis, which occurs in approximately one-third of latent syphilis cases, can affect multiple organ systems. 2 Syphilis can attack the nervous system (neurosyphilis) and visual system (ocular syphilis) at any stage of disease, resulting in movement disorders, sensory deficits, dementia, paralysis, visual changes, or blindness. 1 Syphilis infection also increases the risk for acquiring or transmitting HIV infection. 1 , 3
Primary and secondary syphilis are the most infectious stages of the disease. Reported cases of primary and secondary syphilis in the US increased from a record low of 2.1 cases per 100 000 population in 2000 and 2001 to 11.9 cases per 100 000 population in 2019. Men account for the majority of cases (83% of primary and secondary syphilis cases in 2019), and rates among women nearly tripled from 2015 to 2019. Men who have sex with men are disproportionately affected, accounting for a majority (57%) of all primary and secondary syphilis cases among men in 2019. 4 The overall rate of primary and secondary syphilis among men who have sex with men was 106 times the rate among men who only have sex with women and 168 times the rate among women. 5 Primary and secondary syphilis rates are highest among Black adolescents and adults, nearly 5 times the rate among White adolescents and adults. Elevated rates have also been reported in Hispanic adolescents and adults, Native American/Alaska Native adolescents and adults, and Native Hawaiian/Pacific Islander adolescents and adults. 4 These disparities are primarily driven by social conditions such as poverty, low education levels, and poor access to quality health care, which disproportionately affect communities of color and make it harder to maintain sexual health. Differences in sexual network characteristics also play a role in disparities. Sexually active people may be more likely to become infected in communities with higher STI rates. 6 - 10
Syphilis infection can be passed from a pregnant person to the fetus, causing neonatal morbidity and mortality. 1 The USPSTF addresses screening for syphilis in pregnant persons in a separate recommendation statement. 11
In 2016, the US Preventive Services Task Force (USPSTF) reviewed the evidence for screening for syphilis infection in nonpregnant adolescents and adults and issued an A recommendation for persons who are at increased risk. 12 The USPSTF has decided to use a reaffirmation deliberation process to update this recommendation. The USPSTF uses the reaffirmation process for well-established, evidence-based standards of practice in current primary care practice for which only a very high level of evidence would justify a change in the grade of the recommendation. 13 In its deliberation of the evidence, the USPSTF considers whether the new evidence is of sufficient strength and quality to change its previous conclusions about the evidence.
Using a reaffirmation process, the USPSTF concludes with high certainty that there is a substantial net benefit of screening for syphilis infection in nonpregnant persons who are at increased risk for infection.
See the Table for more information on the USPSTF recommendation rationale and assessment and the eFigure in the Supplement for information on the recommendation grade. See the Figure for a summary of the recommendation for clinicians. For more details on the methods the USPSTF uses to determine the net benefit, see the USPSTF Procedure Manual. 13
This recommendation applies to asymptomatic, nonpregnant adolescents and adults who have ever been sexually active and are at increased risk for syphilis infection.
In this recommendation statement, sex and gender as well as race and ethnicity terminology are based on how study participants were reported in reviewed studies. This recommendation is inclusive of all persons at increased risk for syphilis.
The USPSTF recommends screening for syphilis in persons who are at increased risk for infection. When deciding which persons to screen for syphilis, clinicians should consider the prevalence of infection in the communities they serve, as well as other sociodemographic and behavioral factors that may be associated with increased risk of syphilis infection. For example, prevalence of syphilis is higher in men, men who have sex with men, persons with HIV infection, young adults, and persons with a history of incarceration, sex work, or military service. 9 , 10 A substantial percentage of heterosexual syphilis transmission occurs among persons who use illicit drugs, particularly methamphetamine. 14 , 15 Diagnosis of another STI may signal that a person is having condomless sex, which increases their risk of syphilis infection. 16 Higher infection rates in persons of some racial and ethnic groups have been reported and are primarily a reflection of a combination of factors, including social determinants of health (eg, disparities of income, low educational achievement, and unstable housing), 6 differential health insurance coverage or access to quality health care, 6 and differences in sexual network characteristics (eg, individuals living in communities with a high prevalence of STIs have an increased chance of encountering an infected partner). 7 Local prevalence rates may change over time, so clinicians should be aware of the latest data and trends for their specific population and geographic area, which are available through their state and local health departments and Centers for Disease Control and Prevention (CDC) surveillance. 9 , 10 , 17
Although direct evidence on screening in nonpregnant persons who are not at increased risk for syphilis infection is lacking, based on the established test performance characteristics of current screening tests and the low prevalence rate of syphilis in this population, the yield of screening is likely low. 9 , 10 Therefore, screening in this population may result in high false-positive rates and overtreatment.
Current syphilis screening tests rely on detection of antibodies rather than direct detection of the organism that causes syphilis, Treponema pallidum . A traditional screening algorithm is a 2-step process involving an initial nontreponemal test (eg, Venereal Disease Research Laboratory [VDRL] or rapid plasma reagin [RPR] test) followed by a confirmatory treponemal antibody detection test (eg, T pallidum particle agglutination [TP-PA] test). 18 A more recently developed reverse sequence algorithm uses an automated treponemal test (eg, enzyme-linked or chemiluminescence immunoassay) for the initial screening, followed by a nontreponemal test for reactive samples. 18 Discordant results in the reverse sequence are resolved with a second confirmatory treponemal test, preferably testing for different antigens than the initial test. 9 Most laboratories perform traditional screening 19 ; however, the automated processes used in reverse sequence may be appropriate for high-volume laboratories or areas where populations may be at higher risk for late-stage latent disease that traditional screening may miss. 20
Rapid point-of-care (POC) testing for antibodies to T pallidum can provide quick on-site results (typically within 5 to 30 minutes); however, initial real-world data show sensitivity may be low. 21
Optimal screening frequency for persons who are at increased risk for syphilis infection is not well established. Men who have sex with men or persons with HIV infection may benefit from screening at least annually or more frequently (eg, every 3 to 6 months) if they continue to be at high risk. 9 , 10 , 16
The effectiveness of parenteral penicillin G for the treatment of primary, secondary, and latent syphilis is well established. Dosage and the length of treatment depend on the stage and symptoms of the infection. Clinicians are encouraged to refer to the CDC’s STI Treatment Guidelines for the most up-to-date treatment guidance. 16
The USPSTF did not review evidence on screening for syphilis in persons with HIV infection or taking HIV preexposure prophylaxis if screening was part of disease management. The CDC provides recommendations for these circumstances and other specific groups. The CDC also describes management and follow-up considerations, including interventions to decrease transmission and reinfection. 16
The CDC provides fact sheets, treatment guidelines, and national and state surveillance data for syphilis ( https://www.cdc.gov/std ). It also provides guidance for clinicians on providing quality STI clinical services ( https://www.cdc.gov/mmwr/volumes/68/rr/rr6805a1.htm ).
The National Academies of Sciences, Engineering, and Medicine provides a comprehensive systems-based approach for prevention and control of STIs ( https://nap.nationalacademies.org/catalog/25955/sexually-transmitted-infections-adopting-a-sexual-health-paradigm ).
The Community Preventive Services Task Force has issued several recommendations on the prevention of HIV/AIDS, other STIs, and teen pregnancy. The Community Guide discusses interventions that have been efficacious in school settings and for men who have sex with men ( https://www.thecommunityguide.org/topic/hiv-stis-and-teen-pregnancy ).
The USPSTF has issued a separate recommendation for screening for syphilis infection in pregnant persons 11 as well as screening recommendations for other STIs, including hepatitis B, 22 hepatitis C, 23 genital herpes, 24 HIV, 25 and chlamydia and gonorrhea. 26 The USPSTF has also issued a recommendation on behavioral counseling for all sexually active adolescents and for adults who are at increased risk for STIs. 27
This recommendation is a reaffirmation of the USPSTF 2016 recommendation statement. In 2016, the USPSTF reviewed the evidence for syphilis screening in nonpregnant adolescents and adults and found convincing evidence that the benefits of screening substantially outweighed the harms (A recommendation). 12 In the current update, the USPSTF found no new substantial evidence that could change its recommendation and, therefore, reaffirms its recommendation to screen for syphilis in nonpregnant adolescents and adults who are at increased risk of infection.
To reaffirm its recommendation, the USPSTF commissioned a reaffirmation evidence update. The aim of evidence updates that support the reaffirmation process is to identify if there is new and substantial evidence sufficient enough to change the prior recommendation. 13 The reaffirmation update focuses on targeted key questions evaluating the performance of risk assessment tools and the benefits and harms of screening for syphilis in nonpregnant adolescents and adults. The review also included a more limited literature search comparing testing algorithms and the accuracy of rapid POC tests. Because the USPSTF previously determined that treatments for these infections are effective and well established, this review did not include a review of treatments.
Test accuracy can vary based on disease stage. A literature review showed the sensitivity of commonly used nontreponemal tests, such as RPR and VDRL, ranged from 61% to 78% for detecting primary and late latent syphilis. Sensitivity of these nontreponemal tests for detecting secondary and early latent syphilis ranged from 85% to 100%. Sensitivity of preferred treponemal tests ranged from 82% to 100% across the spectrum of disease. Specificity of preferred treponemal tests for detecting primary syphilis ranged from 94% to 100%. 9 , 10
There is limited evidence directly comparing the traditional and reverse sequence algorithms. A recent 2020 narrative study reviewed 69 articles summarizing the pros and cons of the 2 algorithms. Findings showed that the nontreponemal test in the traditional algorithm may have decreased sensitivity for detecting primary and latent syphilis. The automated tests used in the reverse sequence algorithm allows for faster processing but may have higher false-positive rates than the traditional algorithm. The study concluded that the traditional algorithm may be more appropriate for smaller laboratories with lower volumes of testing because performing manual nontreponemal screening assays would not significantly affect workflow. Alternatively, the reverse algorithm may be more suitable for either larger laboratories where automated testing processes can improve workflow and efficiency or for smaller laboratories serving higher-risk populations. 20
A 2020 systematic review evaluated rapid POC test performance in laboratory and real-world settings. The study found that the pooled sensitivity from the laboratory evaluations (n = 5) was 98.5% (95% CI, 92.1%-100%), while pooled specificity was 95.9% (95% CI, 81.5%-100.0%). The pooled sensitivity for prospective studies (n = 10) was 87.7% (95% CI, 71.8%-97.2%), while pooled specificity was 96.7% (95% CI, 91.9%-99.2%). However, in 2 of these prospective studies, the sensitivity was only 50%. Differences in testing protocols, training, and specimen collection (eg, sera vs whole-blood samples) are potential factors explaining the inconsistency in test performance between laboratory and real-world POC testing. 21
The USPSTF reviewed 1 fair-quality study (n = 361) that evaluated an online calculator for predicting syphilis within the next 3 months in high-risk individuals seeking STI testing or treatment in Peru. The model with the greatest area under the curve (0.69) included the risk factors current HIV infection, history of syphilis infection, number of male sex partners in past 3 months, and sex role for anal sex (receptive or insertive) in the prior 3 months. 28
The USPSTF reviewed 1 fair-quality Australian cohort study (n = 117 387) examining trends in syphilis testing and detection among sexually active men who have sex with men (68% HIV-negative). During an 8-year follow-up period, the proportion of men tested for syphilis annually increased significantly among both HIV-negative (n = 97 895) and HIV-positive (n = 19 492) men (48% to 91% in HIV-negative men and 42% to 77% in HIV-positive men; P <.001 for trend). Syphilis was detected in 2799 HIV-negative men (3%) and 1032 HIV-positive men (5%). The proportion of early latent infections detected increased from 27% to 44% in HIV-negative men and from 23% to 45% in HIV-positive men ( P < .001 for trend), while the proportion of secondary infections decreased from 24% to 19% ( P = .03 for trend) and from 45% to 26% ( P < .001 for trend) in HIV-positive and negative men, respectively. This study demonstrated that screening in men who have sex with men was associated with greater detection of early asymptomatic syphilis and a decrease in secondary syphilis, suggesting that screening is likely to have interrupted the progression of syphilis. 29
No studies reported the effectiveness of screening on acquisition or transmission of other STIs or other complications such as tertiary syphilis or neurosyphilis. No studies directly addressed effective screening intervals in the included populations.
The effectiveness of penicillin G for the treatment of primary, secondary, and latent syphilis is well established and was not reviewed for this recommendation update. 16
The USPSTF reviewed 1 fair-quality, pre-post design study (n = 1097) examining emotional stress associated with rapid POC STI testing. Participants considered to be in high-risk groups completed a questionnaire assessing emotional stress prior to and after testing for HIV, hepatitis C, and syphilis. Factors associated with increased stress included history of injection drug use, Black race, less than a high school education, and single marital status. The study did not compare changes in the levels of emotional stress pretesting vs posttesting. 30
A draft version of this recommendation statement was posted for public comment on the USPSTF website from February 15 to March 14, 2022. The USPSTF clarified factors driving disparities in syphilis prevalence among certain populations in the Importance and Practice Considerations sections. The USPSTF clarified preferred screening tests by the CDC as well as test performance of different screening tests in the Practice Considerations and Supporting Evidence sections. Additional risk behaviors were added to the Practice Considerations section to further help identify persons who would benefit from screening. Last, the USPSTF clarified harms in the Table .
Studies are needed that provide more information on the following.
Validated risk assessment tools, feasible for use in primary care, that will more accurately identify populations at increased risk of infection who would benefit most from screening.
Direct evidence evaluating the benefits and harms of screening for syphilis in adolescents.
Factors driving demographic, geographic, and occupational health disparities and effective prevention strategies that may improve health inequities.
Optimal screening intervals for all high-risk populations.
Effectiveness of rapid POC testing in real-world settings compared with laboratory-based testing.
The CDC recommends at least annual screening for syphilis in sexually active men who have sex with men, with confirmatory testing for individuals with reactive serology. The CDC recommends that persons with HIV infection who are sexually active be screened at the first HIV evaluation and at least annually thereafter. Men who have sex with men and persons with HIV infection may benefit from more frequent screening (eg, every 3 to 6 months) based on individual risk behaviors and local epidemiology. The CDC also recommends opt-out syphilis screening in correctional facilities based on the local area and institutional prevalence. 16 The American College of Obstetricians and Gynecologists does not recommend routine screening for syphilis in persons who are not pregnant. 31 The HIV Medicine Association (part of the Infectious Diseases Society of America) recommends that all patients with HIV infection be screened for syphilis on initiation of care and periodically thereafter, depending on risk. 32 The recommendation of the American Academy of Family Physicians is similar to the USPSTF guidelines for screening for syphilis in persons at increased risk. 33 , 34
Corresponding Author: Carol M. Mangione, MD, MSPH, David Geffen School of Medicine, University of California, Los Angeles, 10940 Wilshire Blvd, Ste 700, Los Angeles, CA 90024 ( [email protected] ).
Accepted for Publication: August 17, 2022.
The US Preventive Services Task Force (USPSTF) members: Carol M. Mangione, MD, MSPH; Michael J. Barry, MD; Wanda K. Nicholson, MD, MPH, MBA; Michael Cabana, MD, MA, MPH; David Chelmow, MD; Tumaini Rucker Coker, MD, MBA; Esa M. Davis, MD, MPH; Katrina E. Donahue, MD, MPH; Carlos Roberto Jaén, MD, PhD, MS; Martha Kubik, PhD, RN; Li Li, MD, PhD, MPH; Gbenga Ogedegbe, MD, MPH; Lori Pbert, PhD; John M. Ruiz, PhD; James Stevermer, MD, MSPH; John B. Wong, MD.
Affiliations of The US Preventive Services Task Force (USPSTF) members: University of California, Los Angeles (Mangione); Harvard Medical School, Boston, Massachusetts (Barry); University of North Carolina at Chapel Hill (Nicholson, Donahue); Albert Einstein College of Medicine, New York, New York (Cabana); Virginia Commonwealth University, Richmond (Chelmow); University of Washington, Seattle (Coker); University of Pittsburgh, Pittsburgh, Pennsylvania (Davis); The University of Texas Health Science Center, San Antonio (Jaén); George Mason University, Fairfax, Virginia (Kubik); University of Virginia, Charlottesville (Li); New York University, New York, New York (Ogedegbe); University of Massachusetts Medical School, Worcester (Pbert); University of Arizona, Tucson (Ruiz); University of Missouri, Columbia (Stevermer); Tufts University School of Medicine, Boston, Massachusetts (Wong).
Author Contributions: Dr Mangione had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. The USPSTF members contributed equally to the recommendation statement.
Conflict of Interest Disclosures: Authors followed the policy regarding conflicts of interest described at https://www.uspreventiveservicestaskforce.org/Page/Name/conflict-of-interest-disclosures . All members of the USPSTF receive travel reimbursement and an honorarium for participating in USPSTF meetings.
Funding/Support: The USPSTF is an independent, voluntary body. The US Congress mandates that the Agency for Healthcare Research and Quality (AHRQ) support the operations of the USPSTF.
Role of the Funder/Sponsor: AHRQ staff assisted in the following: development and review of the research plan, commission of the systematic evidence review from an Evidence-based Practice Center, coordination of expert review and public comment of the draft evidence report and draft recommendation statement, and the writing and preparation of the final recommendation statement and its submission for publication. AHRQ staff had no role in the approval of the final recommendation statement or the decision to submit for publication.
Disclaimer: Recommendations made by the USPSTF are independent of the US government. They should not be construed as an official position of AHRQ or the US Department of Health and Human Services.
Additional Contributions: We thank Brandy Peaker, MD, MPH (AHRQ), who contributed to the writing of the manuscript, and Lisa Nicolella, MA (AHRQ), who assisted with coordination and editing.
Additional Information: The US Preventive Services Task Force (USPSTF) makes recommendations about the effectiveness of specific preventive care services for patients without obvious related signs or symptoms. It bases its recommendations on the evidence of both the benefits and harms of the service and an assessment of the balance. The USPSTF does not consider the costs of providing a service in this assessment. The USPSTF recognizes that clinical decisions involve more considerations than evidence alone. Clinicians should understand the evidence but individualize decision-making to the specific patient or situation. Similarly, the USPSTF notes that policy and coverage decisions involve considerations in addition to the evidence of clinical benefits and harms. Published by JAMA®—Journal of the American Medical Association under arrangement with the Agency for Healthcare Research and Quality (AHRQ). ©2022 AMA and United States Government, as represented by the Secretary of the Department of Health and Human Services (HHS), by assignment from the members of the United States Preventive Services Task Force (USPSTF). All rights reserved.
- Register for email alerts with links to free full-text articles
- Access PDFs of free articles
- Manage your interests
- Save searches and receive search alerts
Clinical presentation and serological diagnosis of syphilis reinfection in men living with HIV: a retrospective cohort study
Affiliations.
- 1 Department of Dermatology, University Hospital Zurich, University of Zurich, Zurich, Switzerland.
- 2 Division of Infectious Diseases and Hospital Epidemiology, University Hospital Zurich, Zurich, Switzerland.
- 3 Department of Public Health, University of Zurich, Zurich, Switzerland.
- 4 Department of Dermatology, University Hospital Zurich, University of Zurich, Zurich, Switzerland [email protected].
- PMID: 34475233
- DOI: 10.1136/sextrans-2020-054923
Objectives: Studies on the characteristics of syphilis reinfection are scarce despite increasing numbers and proportions of cases. We aimed to gain insights into the clinical and serological presentation of reinfected men living with HIV and to evaluate diagnostic criteria for syphilis reinfection.
Methods: We conducted a retrospective cohort study of 259 HIV-positive men diagnosed with syphilis between January 1999 and September 2015 at the University Hospital Zurich. We compared patients with a single syphilis infection (n = 109) to patients with reinfections (n = 150).
Results: The two groups matched in age, sexual orientation and numbers of other STIs. Reinfected patients more often presented with latent syphilis than patients with a single syphilis episode (41.9% vs 8.9%; p<0.001). Although generally high venereal diseases research laboratory (VDRL) or rapid plasma reagin (RPR) titres (median 1:32) were seen in reinfected patients, 19.4% had titres ≤1:8. Treponema pallidum passive particle agglutination (TPPA) titres were significantly higher (1:81 840 vs 1:10 240; p<0.001), while IgM values were significantly lower (1.27 vs 3.5; p<0.001) in syphilis reinfections than in first infections. The TPPA increased ≥fourfold in >92.3% of reinfected patients.
Conclusions: Our data highlight the paramount importance of regularly screening patients at risk as syphilis reinfections in men living with HIV are more likely to be latent infections, that is, without symptoms. As non-treponemal tests might be biologically false-positive (up to a titre of 1:8) due to various conditions, a ≥fourfold increase of the TPPA might be considered as optional criterion for the diagnosis of syphilis reinfections. This could be especially valuable for diagnosing reinfected latent stage patients.
Keywords: diagnosis; diagnostic techniques and procedures; serology; syphilis.
© Author(s) (or their employer(s)) 2022. No commercial re-use. See rights and permissions. Published by BMJ.
- HIV Infections* / complications
- Reinfection
- Retrospective Studies
- Syphilis Serodiagnosis
- Syphilis* / complications
- Syphilis* / diagnosis
- Syphilis* / epidemiology
- Treponema pallidum
Achieve Mastery of Medical Concepts
Study for medical school and boards with lecturio.
USMLE Step 1 | USMLE Step 2 | COMLEX Level 1 | COMLEX Level 2 | ENARM | NEET
Syphilis (Clinical)
Syphilis Syphilis Syphilis is a bacterial infection caused by the spirochete Treponema pallidum pallidum (T. p. pallidum), which is usually spread through sexual contact. Syphilis has 4 clinical stages: primary, secondary, latent, and tertiary. Syphilis is a bacterial infection caused by the spirochete Spirochete Treponema is a gram-negative, microaerophilic spirochete. Owing to its very thin structure, it is not easily seen on Gram stain, but can be visualized using dark-field microscopy. This spirochete contains endoflagella, which allow for a characteristic corkscrew movement. Treponema Treponema pallidum Treponema pallidum The causative agent of venereal and non-venereal syphilis as well as yaws. Treponema subspecies pallidum (T. pallidum) , which is usually spread through sexual contact. Syphilis Syphilis Syphilis is a bacterial infection caused by the spirochete Treponema pallidum pallidum (T. p. pallidum), which is usually spread through sexual contact. Syphilis has 4 clinical stages: primary, secondary, latent, and tertiary. Syphilis has 4 clinical stages: primary, secondary, latent, and tertiary. Primary syphilis Primary Syphilis Syphilis begins with a chancre Chancre The primary sore of syphilis, a painless indurated, eroded papule, occurring at the site of entry of the infection. Syphilis , a painless ulcer on the genitals. Progression to secondary syphilis Secondary Syphilis Syphilis manifests as a generalized maculopapular Maculopapular Dermatologic Examination rash Rash Rocky Mountain Spotted Fever , which includes the palms and soles. The development of tertiary syphilis Tertiary Syphilis Syphilis can cause severe neurologic ( neurosyphilis Neurosyphilis Infections of the central nervous system caused by treponema pallidum which present with a variety of clinical syndromes. The initial phase of infection usually causes a mild or asymptomatic meningeal reaction. The meningovascular form may present acutely as brain infarction. The infection may also remain subclinical for several years. Late syndromes include general paresis; tabes dorsalis; meningeal syphilis; syphilitic optic atrophy; and spinal syphilis. General paresis is characterized by progressive dementia; dysarthria; tremor; myoclonus; seizures; and argyll-robertson pupils. Syphilis ), cardiovascular, and/or gummatous disease. The diagnosis is through both treponemal and nontreponemal testing. Penicillin Penicillin Rheumatic Fever G is the antibiotic of choice. The duration of management varies based on the stage of the disease.
Last updated: Mar 4, 2024
Clinical Presentation
Differential diagnosis.
Share this concept:
Epidemiology [3,11,12]
- Worldwide annual new cases: approximately 6.3 million
- Worldwide case rate: 17‒18 per 100,000
- Highest prevalence Prevalence The total number of cases of a given disease in a specified population at a designated time. It is differentiated from incidence, which refers to the number of new cases in the population at a given time. Measures of Disease Frequency in the WHO Western Pacific region: 93 cases per 100,000
- Second highest prevalence Prevalence The total number of cases of a given disease in a specified population at a designated time. It is differentiated from incidence, which refers to the number of new cases in the population at a given time. Measures of Disease Frequency in WHO African region: 47 cases per 100,000
- WHO Americas region: 34 cases per 100,000 population
- Incidence Incidence The number of new cases of a given disease during a given period in a specified population. It also is used for the rate at which new events occur in a defined population. It is differentiated from prevalence, which refers to all cases in the population at a given time. Measures of Disease Frequency in the United States is rising.
- Men > women, particularly in men who have sex Sex The totality of characteristics of reproductive structure, functions, phenotype, and genotype, differentiating the male from the female organism. Gender Dysphoria with men (MSM)
- Most common age group: 20–29 years old
- Increased prevalence Prevalence The total number of cases of a given disease in a specified population at a designated time. It is differentiated from incidence, which refers to the number of new cases in the population at a given time. Measures of Disease Frequency in minorities
- Note: Syphilis Syphilis Syphilis is a bacterial infection caused by the spirochete Treponema pallidum pallidum (T. p. pallidum), which is usually spread through sexual contact. Syphilis has 4 clinical stages: primary, secondary, latent, and tertiary. Syphilis increases the rate of HIV HIV Anti-HIV Drugs acquisition by 2‒5 times.
- Treponema pallidum Treponema pallidum The causative agent of venereal and non-venereal syphilis as well as yaws. Treponema subsp. pallidum (T. pallidum)
- Gram-negative spirochete Spirochete Treponema is a gram-negative, microaerophilic spirochete. Owing to its very thin structure, it is not easily seen on Gram stain, but can be visualized using dark-field microscopy. This spirochete contains endoflagella, which allow for a characteristic corkscrew movement. Treponema (spiral-shaped)
- Human to human: T. pallidum has very limited ability to survive outside the body.
- Bacteria Bacteria Bacteria are prokaryotic single-celled microorganisms that are metabolically active and divide by binary fission. Some of these organisms play a significant role in the pathogenesis of diseases. Bacteriology may enter through genital, anorectal, or oral sites.
- Transmission rate: Approximately ⅓ of sexual contacts develop the disease.
- Via direct contact during primary or secondary syphilis Secondary Syphilis Syphilis with a syphilitic sore, mucous patch Patch Nonpalpable lesion > 1 cm in diameter Generalized and Localized Rashes , condyloma Condyloma Sexually transmitted form of anogenital warty growth caused by the human papillomaviruses. Male Genitourinary Examination latum, or rash Rash Rocky Mountain Spotted Fever
- Sharing needles with an infected person
- Bacterial entry into the fetus through the placenta Placenta A highly vascularized mammalian fetal-maternal organ and major site of transport of oxygen, nutrients, and fetal waste products. It includes a fetal portion (chorionic villi) derived from trophoblasts and a maternal portion (decidua) derived from the uterine endometrium. The placenta produces an array of steroid, protein and peptide hormones (placental hormones). Placenta, Umbilical Cord, and Amniotic Cavity
- Transmission rate: 60%‒80% from an infected mother to a fetus
- Patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship with a sex Sex The totality of characteristics of reproductive structure, functions, phenotype, and genotype, differentiating the male from the female organism. Gender Dysphoria partner with primary, secondary, or early latent syphilis Latent syphilis The stage of syphilis that occurs following the primary (chancre) and secondary stages. The patient is asymptomatic at the latent stage but remains seropositive for the spirochete. Syphilis
- Sexually active MSM
- People living with HIV HIV Anti-HIV Drugs
- Unprotected sexual contact
- Multiple sex Sex The totality of characteristics of reproductive structure, functions, phenotype, and genotype, differentiating the male from the female organism. Gender Dysphoria partners
- Work in the sex Sex The totality of characteristics of reproductive structure, functions, phenotype, and genotype, differentiating the male from the female organism. Gender Dysphoria trade
- History of incarceration Incarceration Inguinal Canal: Anatomy and Hernias
- Men < 29 years of age
- Late or no prenatal care Prenatal care Prenatal care is a systematic and periodic assessment of pregnant women during gestation to assure the best health outcome for the mother and her fetus. Prenatal care prevents and identifies maternal and fetal problems that adversely affect the pregnancy outcome. Prenatal Care
- Maternal drug use
- Inadequate treatment of syphilis Syphilis Syphilis is a bacterial infection caused by the spirochete Treponema pallidum pallidum (T. p. pallidum), which is usually spread through sexual contact. Syphilis has 4 clinical stages: primary, secondary, latent, and tertiary. Syphilis during pregnancy Pregnancy The status during which female mammals carry their developing young (embryos or fetuses) in utero before birth, beginning from fertilization to birth. Pregnancy: Diagnosis, Physiology, and Care
Pathophysiology [11‒13]
- Allows tissue invasion
- Facilitates dissemination
- Able to move in thick substances (e.g., connective tissue Connective tissue Connective tissues originate from embryonic mesenchyme and are present throughout the body except inside the brain and spinal cord. The main function of connective tissues is to provide structural support to organs. Connective tissues consist of cells and an extracellular matrix. Connective Tissue: Histology )
- Assists with dissemination
- Protective coating
- Comes from the host
- Prevents phagocytosis Phagocytosis The engulfing and degradation of microorganisms; other cells that are dead, dying, or pathogenic; and foreign particles by phagocytic cells (phagocytes). Innate Immunity: Phagocytes and Antigen Presentation and immune recognition Immune Recognition Yaws, Bejel, and Pinta
- T. pallidum adheres to skin Skin The skin, also referred to as the integumentary system, is the largest organ of the body. The skin is primarily composed of the epidermis (outer layer) and dermis (deep layer). The epidermis is primarily composed of keratinocytes that undergo rapid turnover, while the dermis contains dense layers of connective tissue. Skin: Structure and Functions or mucosal membranes → hyaluronidase Hyaluronidase Bacteroides production → tissue invasion
- The organism coats itself in the host’s fibronectin Fibronectin Glycoproteins found on the surfaces of cells, particularly in fibrillar structures. The proteins are lost or reduced when these cells undergo viral or chemical transformation. They are highly susceptible to proteolysis and are substrates for activated blood coagulation factor VIII. The forms present in plasma are called cold-insoluble globulins. Connective Tissue: Histology → prevents recognition and phagocytosis Phagocytosis The engulfing and degradation of microorganisms; other cells that are dead, dying, or pathogenic; and foreign particles by phagocytic cells (phagocytes). Innate Immunity: Phagocytes and Antigen Presentation by the immune system Immune system The body’s defense mechanism against foreign organisms or substances and deviant native cells. It includes the humoral immune response and the cell-mediated response and consists of a complex of interrelated cellular, molecular, and genetic components. Primary Lymphatic Organs → development of the chancre Chancre The primary sore of syphilis, a painless indurated, eroded papule, occurring at the site of entry of the infection. Syphilis (initial ulcerative lesion)
- Eventual local immune control → resolution of chancre Chancre The primary sore of syphilis, a painless indurated, eroded papule, occurring at the site of entry of the infection. Syphilis
- During the primary period, some spirochetes Spirochetes An order of slender, flexuous, helically coiled bacteria, with one or more complete turns in the helix. Treponema move into local lymph nodes Lymph Nodes They are oval or bean shaped bodies (1 – 30 mm in diameter) located along the lymphatic system. Lymphatic Drainage System: Anatomy .
- Spirochetes Spirochetes An order of slender, flexuous, helically coiled bacteria, with one or more complete turns in the helix. Treponema multiply and disseminate through the bloodstream → invade other organs and tissues
- Host immune-inflammatory response → systemic clinical manifestations
Related videos
Syphilis Syphilis Syphilis is a bacterial infection caused by the spirochete Treponema pallidum pallidum (T. p. pallidum), which is usually spread through sexual contact. Syphilis has 4 clinical stages: primary, secondary, latent, and tertiary. Syphilis is a multistage disease. Patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship can present at any stage, and infected individuals may not exhibit symptoms for years.
Primary syphilis Primary Syphilis Syphilis [1,3,5,11‒13,15]
- Initial: localized infection
- Incubation Incubation The amount time between exposure to an infectious agent and becoming symptomatic. Rabies Virus period is approximately 10–90 days (average, 3 weeks).
- Symptoms may go unnoticed.
- Begins as a firm, red papule Papule Elevated lesion Generalized and Localized Rashes
- Becomes a firm ulcer (typically 1‒2 cm in diameter) with raised, indurated borders
- Posterior pharynx Pharynx The pharynx is a component of the digestive system that lies posterior to the nasal cavity, oral cavity, and larynx. The pharynx can be divided into the oropharynx, nasopharynx, and laryngopharynx. Pharyngeal muscles play an integral role in vital processes such as breathing, swallowing, and speaking. Pharynx: Anatomy
- Lips Lips The lips are the soft and movable most external parts of the oral cavity. The blood supply of the lips originates from the external carotid artery, and the innervation is through cranial nerves. Lips and Tongue: Anatomy
- Heals spontaneously in 3–6 weeks (regardless of treatment)
- Note: Because these lesions are painless , and often occur in areas that are hard to see, the patient may not notice them.
- Palpable, rubbery lymph nodes Lymph Nodes They are oval or bean shaped bodies (1 – 30 mm in diameter) located along the lymphatic system. Lymphatic Drainage System: Anatomy
- Usually inguinal

Primary, painless chancre of syphilis ( T. pallidum infection)
Secondary syphilis Secondary Syphilis Syphilis [1,3,5,11‒13,15]
- Systemic disease that develops 2–12 weeks after the primary infection Primary infection Herpes Simplex Virus 1 and 2
- Lasts 4–8 weeks
- Fever Fever Fever is defined as a measured body temperature of at least 38°C (100.4°F). Fever is caused by circulating endogenous and/or exogenous pyrogens that increase levels of prostaglandin E2 in the hypothalamus. Fever is commonly associated with chills, rigors, sweating, and flushing of the skin. Fever
- Malaise Malaise Tick-borne Encephalitis Virus
- Myalgias Myalgias Painful sensation in the muscles. Tick-borne Encephalitis Virus
- Anorexia Anorexia The lack or loss of appetite accompanied by an aversion to food and the inability to eat. It is the defining characteristic of the disorder anorexia nervosa. Anorexia Nervosa
- Weight loss Weight loss Decrease in existing body weight. Bariatric Surgery
- Nausea Nausea An unpleasant sensation in the stomach usually accompanied by the urge to vomit. Common causes are early pregnancy, sea and motion sickness, emotional stress, intense pain, food poisoning, and various enteroviruses. Antiemetics
- Tender (may be very mild)
- Affected nodes usually are in the axillary, cervical, inguinal, and femoral regions.
- Nonpruritic
- Macular, papular, or nodular
- Scaly or smooth
- Red, reddish-brown, or copper Copper A heavy metal trace element with the atomic symbol cu, atomic number 29, and atomic weight 63. 55. Trace Elements color
- Involves the trunk, extremities, palms, and soles
- White erosions Erosions Corneal Abrasions, Erosion, and Ulcers
- May be seen in the mouth (buccal or lingual mucosa) or genital regions
- Grayish-white color
- Wart-like lesions
- Mostly seen around the anus and vagina Vagina The vagina is the female genital canal, extending from the vulva externally to the cervix uteri internally. The structures have sexual, reproductive, and urinary functions and a rich blood supply, mainly arising from the internal iliac artery. Vagina, Vulva, and Pelvic Floor: Anatomy (near the location of the primary chancre Chancre The primary sore of syphilis, a painless indurated, eroded papule, occurring at the site of entry of the infection. Syphilis , in warm, moist areas)
- More severe, ulcerating skin Skin The skin, also referred to as the integumentary system, is the largest organ of the body. The skin is primarily composed of the epidermis (outer layer) and dermis (deep layer). The epidermis is primarily composed of keratinocytes that undergo rapid turnover, while the dermis contains dense layers of connective tissue. Skin: Structure and Functions lesions
- Seen in immunocompromised immunocompromised A human or animal whose immunologic mechanism is deficient because of an immunodeficiency disorder or other disease or as the result of the administration of immunosuppressive drugs or radiation. Gastroenteritis patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship (e.g., HIV HIV Anti-HIV Drugs )
- Alopecia Alopecia Alopecia is the loss of hair in areas anywhere on the body where hair normally grows. Alopecia may be defined as scarring or non-scarring, localized or diffuse, congenital or acquired, reversible or permanent, or confined to the scalp or universal; however, alopecia is usually classified using the 1st 3 factors. Alopecia (hair loss): can be in a diffuse or a “moth-eaten” pattern
- GI infiltration and/or ulcerations
- Proctitis Proctitis Inflammation of the mucous membrane of the rectum, the distal end of the large intestine. Chronic Granulomatous Disease
- Periostitis Periostitis Inflammation of the periosteum. The condition is generally chronic, and is marked by tenderness and swelling of the bone and an aching pain. Acute periostitis is due to infection, is characterized by diffuse suppuration, severe pain, and constitutional symptoms, and usually results in necrosis. Reactive Arthritis
- Synovitis Synovitis Inflammation of the synovial membrane. Rheumatoid Arthritis
- Nephrotic syndrome Nephrotic syndrome Nephrotic syndrome is characterized by severe proteinuria, hypoalbuminemia, and peripheral edema. In contrast, the nephritic syndromes present with hematuria, variable loss of renal function, and hypertension, although there is sometimes overlap of > 1 glomerular disease in the same individual. Nephrotic Syndrome
- Acute nephritis
- Renal failure Renal failure Conditions in which the kidneys perform below the normal level in the ability to remove wastes, concentrate urine, and maintain electrolyte balance; blood pressure; and calcium metabolism. Renal insufficiency can be classified by the degree of kidney damage (as measured by the level of proteinuria) and reduction in glomerular filtration rate. Crush Syndrome
- Keratitis Keratitis Inflammation of the cornea. Herpes Simplex Virus 1 and 2
- Anterior uveitis Uveitis Uveitis is the inflammation of the uvea, the pigmented middle layer of the eye, which comprises the iris, ciliary body, and choroid. The condition is categorized based on the site of disease; anterior uveitis is the most common. Diseases of the Uvea
- Posterior uveitis Posterior Uveitis Diseases of the Uvea
- Optic neuritis Optic neuritis Inflammation of the optic nerve. Commonly associated conditions include autoimmune disorders such as multiple sclerosis, infections, and granulomatous diseases. Clinical features include retro-orbital pain that is aggravated by eye movement, loss of color vision, and contrast sensitivity that may progress to severe visual loss, an afferent pupillary defect (Marcus-Gunn pupil), and in some instances optic disc hyperemia and swelling. Inflammation may occur in the portion of the nerve within the globe (neuropapillitis or anterior optic neuritis) or the portion behind the globe (retrobulbar neuritis or posterior optic neuritis). Cranial Nerve Palsies
- Hearing loss Hearing loss Hearing loss, also known as hearing impairment, is any degree of impairment in the ability to apprehend sound as determined by audiometry to be below normal hearing thresholds. Clinical presentation may occur at birth or as a gradual loss of hearing with age, including a short-term or sudden loss at any point. Hearing Loss
- Tinnitus Tinnitus A nonspecific symptom of hearing disorder characterized by the sensation of buzzing, ringing, clicking, pulsations, and other noises in the ear. Objective tinnitus refers to noises generated from within the ear or adjacent structures that can be heard by other individuals. The term subjective tinnitus is used when the sound is audible only to the affected individual. Tinnitus may occur as a manifestation of cochlear diseases; vestibulocochlear nerve diseases; intracranial hypertension; craniocerebral trauma; and other conditions. Cranial Nerve Palsies
- Vertigo Vertigo Vertigo is defined as the perceived sensation of rotational motion while remaining still. A very common complaint in primary care and the ER, vertigo is more frequently experienced by women and its prevalence increases with age. Vertigo is classified into peripheral or central based on its etiology. Vertigo

Diffuse cutaneous lesions on the palms of a patient with secondary syphilis

Generalized maculopapular rash on the trunk of a patient with secondary syphilis

Condyloma lata in a patient with secondary syphilis
Latent syphilis Latent syphilis The stage of syphilis that occurs following the primary (chancre) and secondary stages. The patient is asymptomatic at the latent stage but remains seropositive for the spirochete. Syphilis [1,3,5,11‒13,15]
- Period between secondary and tertiary syphilis Tertiary Syphilis Syphilis during which the disease lays dormant
- Positive serologic test with no visible signs or symptoms
- Early: < 1‒2 years after initial infection
- Late: > 1‒2 years after initial infection
- May last months to years (often decades)
- The disease can resolve, relapse Relapse Relapsing Fever with skin Skin The skin, also referred to as the integumentary system, is the largest organ of the body. The skin is primarily composed of the epidermis (outer layer) and dermis (deep layer). The epidermis is primarily composed of keratinocytes that undergo rapid turnover, while the dermis contains dense layers of connective tissue. Skin: Structure and Functions /mucosal lesions (i.e., recurrent secondary disease), or progress to tertiary syphilis Tertiary Syphilis Syphilis .
Tertiary syphilis Tertiary Syphilis Syphilis [1,3,5,10‒15]
- Seen in 33% of untreated cases
- Occurs 1–30 years after the initial infection
- Headache Headache The symptom of pain in the cranial region. It may be an isolated benign occurrence or manifestation of a wide variety of headache disorders. Brain Abscess
- Nausea Nausea An unpleasant sensation in the stomach usually accompanied by the urge to vomit. Common causes are early pregnancy, sea and motion sickness, emotional stress, intense pain, food poisoning, and various enteroviruses. Antiemetics and vomiting Vomiting The forcible expulsion of the contents of the stomach through the mouth. Hypokalemia
- Neck stiffness Neck Stiffness Meningitis
- Photophobia Photophobia Abnormal sensitivity to light. This may occur as a manifestation of eye diseases; migraine; subarachnoid hemorrhage; meningitis; and other disorders. Photophobia may also occur in association with depression and other mental disorders. Migraine Headache
- Focal neurologic deficits Neurologic Deficits High-Risk Headaches
- Cranial nerve deficits
- Seizures Seizures A seizure is abnormal electrical activity of the neurons in the cerebral cortex that can manifest in numerous ways depending on the region of the brain affected. Seizures consist of a sudden imbalance that occurs between the excitatory and inhibitory signals in cortical neurons, creating a net excitation. The 2 major classes of seizures are focal and generalized. Seizures
- Endarteritis → stroke
- Meningomyelitis → spastic weakness, paresthesia, muscular atrophy Atrophy Decrease in the size of a cell, tissue, organ, or multiple organs, associated with a variety of pathological conditions such as abnormal cellular changes, ischemia, malnutrition, or hormonal changes. Cellular Adaptation
- Chronic progressive meningoencephalitis Meningoencephalitis Encephalitis → cerebral atrophy Cerebral Atrophy Subdural Hemorrhage
- Mood disturbances
- Psychiatric disease (e.g., depression, mania Mania A state of elevated excitement with over-activity sometimes accompanied with psychotic symptoms (e.g., psychomotor agitation, inflated self esteem and flight of ideas). It is often associated with mental disorders (e.g., cyclothymic disorder; and bipolar diseases). Bipolar Disorder , psychosis)
- Memory Memory Complex mental function having four distinct phases: (1) memorizing or learning, (2) retention, (3) recall, and (4) recognition. Clinically, it is usually subdivided into immediate, recent, and remote memory. Psychiatric Assessment impairment
- Dysarthria Dysarthria Disorders of speech articulation caused by imperfect coordination of pharynx, larynx, tongue, or face muscles. This may result from cranial nerve diseases; neuromuscular diseases; cerebellar diseases; basal ganglia diseases; brain stem diseases; or diseases of the corticobulbar tracts. The cortical language centers are intact in this condition. Wilson Disease
- Pupillary abnormalities can occur but are rare.
- Demyelination Demyelination Multiple Sclerosis of the dorsal columns Dorsal Columns Posterior Cord Syndrome and the dorsal roots
- Ataxia Ataxia Impairment of the ability to perform smoothly coordinated voluntary movements. This condition may affect the limbs, trunk, eyes, pharynx, larynx, and other structures. Ataxia may result from impaired sensory or motor function. Sensory ataxia may result from posterior column injury or peripheral nerve diseases. Motor ataxia may be associated with cerebellar diseases; cerebral cortex diseases; thalamic diseases; basal ganglia diseases; injury to the red nucleus; and other conditions. Ataxia-telangiectasia
- Stabbing (“lightning-like”) pain Pain An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons. Pain: Types and Pathways in the back and legs
- Loss of vibratory sense and proprioception Proprioception Sensory functions that transduce stimuli received by proprioceptive receptors in joints, tendons, muscles, and the inner ear into neural impulses to be transmitted to the central nervous system. Proprioception provides sense of stationary positions and movements of one’s body parts, and is important in maintaining kinesthesia and postural balance. Neurological Examination
- Loss of reflexes
- Paresthesia
- Charcot joints
- Urine retention and incontinence
- Argyll Robertson pupils (pupils accommodate but do not react to light)
- A consequence of vasculitis Vasculitis Inflammation of any one of the blood vessels, including the arteries; veins; and rest of the vasculature system in the body. Systemic Lupus Erythematosus in the vasa vasorum Vasa vasorum Nutrient blood vessels which supply the walls of large arteries or veins. Arteries: Histology
- Aortitis Aortitis Inflammation of the wall of the aorta. Ankylosing Spondylitis
- Aortic aneurysm Aortic aneurysm An abnormal balloon- or sac-like dilatation in the wall of aorta. Thoracic Aortic Aneurysms and aortic root dilation Aortic root dilation Aortic Regurgitation → aortic regurgitation Regurgitation Gastroesophageal Reflux Disease (GERD)
- Coronary artery Coronary Artery Truncus Arteriosus narrowing
- Soft, solitary, granulomatous lesions with central necrosis Necrosis The death of cells in an organ or tissue due to disease, injury or failure of the blood supply. Ischemic Cell Damage
- Variable Variable Variables represent information about something that can change. The design of the measurement scales, or of the methods for obtaining information, will determine the data gathered and the characteristics of that data. As a result, a variable can be qualitative or quantitative, and may be further classified into subgroups. Types of Variables in size
- Destructive (leaves scars)
- Occurs on skin Skin The skin, also referred to as the integumentary system, is the largest organ of the body. The skin is primarily composed of the epidermis (outer layer) and dermis (deep layer). The epidermis is primarily composed of keratinocytes that undergo rapid turnover, while the dermis contains dense layers of connective tissue. Skin: Structure and Functions , bones, or organs
- Bone Bone Bone is a compact type of hardened connective tissue composed of bone cells, membranes, an extracellular mineralized matrix, and central bone marrow. The 2 primary types of bone are compact and spongy. Bones: Structure and Types involvement may cause deep, boring pain Pain An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons. Pain: Types and Pathways (worse at night).

A gumma on the palate of a patient with tertiary syphilis
Screening Screening Preoperative Care [7]
Screening Screening Preoperative Care asymptomatic individuals every 3‒12 months is recommended in individuals at high risk for disease. These individuals include:
- Individuals with a sex Sex The totality of characteristics of reproductive structure, functions, phenotype, and genotype, differentiating the male from the female organism. Gender Dysphoria partner with early syphilis Syphilis Syphilis is a bacterial infection caused by the spirochete Treponema pallidum pallidum (T. p. pallidum), which is usually spread through sexual contact. Syphilis has 4 clinical stages: primary, secondary, latent, and tertiary. Syphilis
- Individuals with HIV HIV Anti-HIV Drugs
- Multiple partners
- Sex Sex The totality of characteristics of reproductive structure, functions, phenotype, and genotype, differentiating the male from the female organism. Gender Dysphoria without condoms Condoms A sheath that is worn over the penis during sexual behavior in order to prevent pregnancy or spread of sexually transmitted disease. Nonhormonal Contraception
- Sex Sex The totality of characteristics of reproductive structure, functions, phenotype, and genotype, differentiating the male from the female organism. Gender Dysphoria with individuals with other sexually transmitted infections Infections Invasion of the host organism by microorganisms or their toxins or by parasites that can cause pathological conditions or diseases. Chronic Granulomatous Disease ( STIs STIs Sexually transmitted infections (STIs) or sexually transmitted diseases (STDs) are infections that spread either by vaginal intercourse, anal sex, or oral sex. Symptoms and signs may include vaginal discharge, penile discharge, dysuria, skin lesions (e.g., warts, ulcers) on or around the genitals, and pelvic pain. Some infections can lead to infertility and chronic debilitating disease. Sexually Transmitted Infections (STIs) )
- Commercial sex Sex The totality of characteristics of reproductive structure, functions, phenotype, and genotype, differentiating the male from the female organism. Gender Dysphoria work
Pregnant patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship :
- All should be screened at the initial patient encounter.
- Individuals at high risk should have repeat screening Screening Preoperative Care at 28‒32 weeks of gestation and again at delivery.
General approach [2‒5]
It is difficult to diagnose syphilis Syphilis Syphilis is a bacterial infection caused by the spirochete Treponema pallidum pallidum (T. p. pallidum), which is usually spread through sexual contact. Syphilis has 4 clinical stages: primary, secondary, latent, and tertiary. Syphilis . However, specific labs and the correlation Correlation Determination of whether or not two variables are correlated. This means to study whether an increase or decrease in one variable corresponds to an increase or decrease in the other variable. Causality, Validity, and Reliability of history and examination results can lead to a diagnosis.
- Treponemal tests (TTs): detect antibodies Antibodies Immunoglobulins (Igs), also known as antibodies, are glycoprotein molecules produced by plasma cells that act in immune responses by recognizing and binding particular antigens. The various Ig classes are IgG (the most abundant), IgM, IgE, IgD, and IgA, which differ in their biologic features, structure, target specificity, and distribution. Immunoglobulins: Types and Functions specific for T. pallidum
- Nontreponemal tests (NTTs): detect antibodies Antibodies Immunoglobulins (Igs), also known as antibodies, are glycoprotein molecules produced by plasma cells that act in immune responses by recognizing and binding particular antigens. The various Ig classes are IgG (the most abundant), IgM, IgE, IgD, and IgA, which differ in their biologic features, structure, target specificity, and distribution. Immunoglobulins: Types and Functions against anticardiolipin, lecithin Lecithin A complex mixture of phospholipids; glycolipids; and triglycerides; with substantial amounts of phosphatidylcholines; phosphatidylethanolamines; and phosphatidylinositols, which are sometimes loosely termed as 1, 2-diacyl-3-phosphocholines. Lecithin is a component of the cell membrane and commercially extracted from soybeans and egg yolk. The emulsifying and surfactant properties are useful in food additives and for forming organogels (gels). Fatty Acids and Lipids , and cholesterol Cholesterol The principal sterol of all higher animals, distributed in body tissues, especially the brain and spinal cord, and in animal fats and oils. Cholesterol Metabolism , which are released from damaged host cells
- Confirming the diagnosis typically requires a positive result on both treponemal and nontreponemal tests.
- Screening Screening Preoperative Care test (1st): NTT
- Confirmatory test (2nd): TT
- Screening Screening Preoperative Care test (1st): TT
- Confirmatory test (2nd): NTT
- Will result in more false positives than the traditional approach
- Those with very early disease
- The 15%‒25% of patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship with late or latent syphilis Latent syphilis The stage of syphilis that occurs following the primary (chancre) and secondary stages. The patient is asymptomatic at the latent stage but remains seropositive for the spirochete. Syphilis whose NTTs become nonreactive over time
- Patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship should also be tested for other STIs STIs Sexually transmitted infections (STIs) or sexually transmitted diseases (STDs) are infections that spread either by vaginal intercourse, anal sex, or oral sex. Symptoms and signs may include vaginal discharge, penile discharge, dysuria, skin lesions (e.g., warts, ulcers) on or around the genitals, and pelvic pain. Some infections can lead to infertility and chronic debilitating disease. Sexually Transmitted Infections (STIs) .
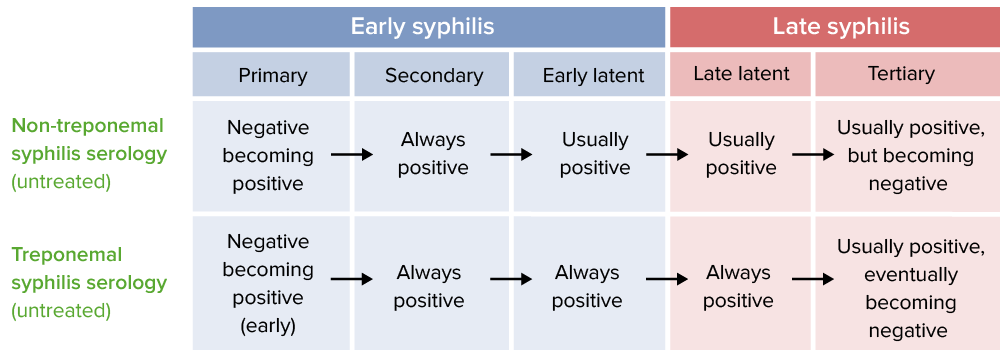
Reactivity of serological tests by stage of syphilis
Nontreponemal testing [5]
- Tests are sensitive but not specific.
- Detects IgG IgG The major immunoglobulin isotype class in normal human serum. There are several isotype subclasses of igg, for example, igg1, igg2a, and igg2b. Hypersensitivity Pneumonitis or IgM IgM A class of immunoglobulin bearing mu chains (immunoglobulin mu-chains). Igm can fix complement. The name comes from its high molecular weight and originally being called a macroglobulin. Immunoglobulins: Types and Functions antilipid antibodies Antibodies Immunoglobulins (Igs), also known as antibodies, are glycoprotein molecules produced by plasma cells that act in immune responses by recognizing and binding particular antigens. The various Ig classes are IgG (the most abundant), IgM, IgE, IgD, and IgA, which differ in their biologic features, structure, target specificity, and distribution. Immunoglobulins: Types and Functions
- Takes 1‒4 weeks after chancre Chancre The primary sore of syphilis, a painless indurated, eroded papule, occurring at the site of entry of the infection. Syphilis appears to become reactive → will miss early-phase primary syphilis Primary Syphilis Syphilis
- May become nonreactive ( false negative False negative An FN test result indicates a person does not have the disease when, in fact, they do. Epidemiological Values of Diagnostic Tests ) in late neurosyphilis Neurosyphilis Infections of the central nervous system caused by treponema pallidum which present with a variety of clinical syndromes. The initial phase of infection usually causes a mild or asymptomatic meningeal reaction. The meningovascular form may present acutely as brain infarction. The infection may also remain subclinical for several years. Late syndromes include general paresis; tabes dorsalis; meningeal syphilis; syphilitic optic atrophy; and spinal syphilis. General paresis is characterized by progressive dementia; dysarthria; tremor; myoclonus; seizures; and argyll-robertson pupils. Syphilis (especially tabes dorsalis Tabes dorsalis Parenchymatous neurosyphilis marked by slowly progressive degeneration of the posterior columns, posterior roots, and ganglia of the spinal cord. The condition tends to present 15 to 20 years after the initial infection and is characterized by lightning-like pains in the lower extremities, urinary incontinence; ataxia; severely impaired position and vibratory sense, abnormal gait, optic atrophy; Argyll-Robertson pupils, hypotonia, hyperreflexia, and trophic joint degeneration. Syphilis )
- Rapid plasma Plasma The residual portion of blood that is left after removal of blood cells by centrifugation without prior blood coagulation. Transfusion Products reagin ( RPR RPR Treponema ) test: 1st choice
- Best initial test for CSF analysis CSF analysis Meningitis
- Test of choice for neurosyphilis Neurosyphilis Infections of the central nervous system caused by treponema pallidum which present with a variety of clinical syndromes. The initial phase of infection usually causes a mild or asymptomatic meningeal reaction. The meningovascular form may present acutely as brain infarction. The infection may also remain subclinical for several years. Late syndromes include general paresis; tabes dorsalis; meningeal syphilis; syphilitic optic atrophy; and spinal syphilis. General paresis is characterized by progressive dementia; dysarthria; tremor; myoclonus; seizures; and argyll-robertson pupils. Syphilis
- Toluidine red unheated serum test ( TRUST Trust Confidence in or reliance on a person or thing. Conflict of Interest ): used less frequently [16,17]
- Qualitative (reactive or nonreactive)
- Tests provide titer levels.
- Results are used to follow titers → monitor treatment response
- Pregnancy Pregnancy The status during which female mammals carry their developing young (embryos or fetuses) in utero before birth, beginning from fertilization to birth. Pregnancy: Diagnosis, Physiology, and Care
- Viral infections Infections Invasion of the host organism by microorganisms or their toxins or by parasites that can cause pathological conditions or diseases. Chronic Granulomatous Disease
- Rheumatic fever Rheumatic fever Acute rheumatic fever (ARF) is an autoimmune inflammatory process that usually follows Streptococcal pharyngitis. Acute rheumatic fever usually occurs 2-4 weeks after an untreated infection and affects the heart, skin, joints, and nervous system. Rheumatic Fever
- Systemic lupus erythematosus Systemic lupus erythematosus Systemic lupus erythematosus (SLE) is a chronic autoimmune, inflammatory condition that causes immune-complex deposition in organs, resulting in systemic manifestations. Women, particularly those of African American descent, are more commonly affected. Systemic Lupus Erythematosus
Treponemal testing [5,17]
- Tests that detect antibodies Antibodies Immunoglobulins (Igs), also known as antibodies, are glycoprotein molecules produced by plasma cells that act in immune responses by recognizing and binding particular antigens. The various Ig classes are IgG (the most abundant), IgM, IgE, IgD, and IgA, which differ in their biologic features, structure, target specificity, and distribution. Immunoglobulins: Types and Functions to Treponema Treponema Treponema is a gram-negative, microaerophilic spirochete. Owing to its very thin structure, it is not easily seen on Gram stain, but can be visualized using dark-field microscopy. This spirochete contains endoflagella, which allow for a characteristic corkscrew movement. Treponema antigens
- Even after treatment, treponemal antibody titers are positive for life.
- Reported as “reactive” or “nonreactive”
- Does not distinguish between an active and a prior, treated infection
- Typically, becomes positive 5‒15 days after appearance of the chancre Chancre The primary sore of syphilis, a painless indurated, eroded papule, occurring at the site of entry of the infection. Syphilis
- Can be done on CSF to evaluate for neurosyphilis Neurosyphilis Infections of the central nervous system caused by treponema pallidum which present with a variety of clinical syndromes. The initial phase of infection usually causes a mild or asymptomatic meningeal reaction. The meningovascular form may present acutely as brain infarction. The infection may also remain subclinical for several years. Late syndromes include general paresis; tabes dorsalis; meningeal syphilis; syphilitic optic atrophy; and spinal syphilis. General paresis is characterized by progressive dementia; dysarthria; tremor; myoclonus; seizures; and argyll-robertson pupils. Syphilis
- Less specific than the CSF-VDRL test
- Expensive, time-consuming, and difficult to read
- Microhemagglutination assay for T. pallidum ( MHA-TP MHA-TP Treponema ); in Europe: T. pallidum haemagglutination test (TPHA)
- T. pallidum particle agglutination test ( TPPA TPPA Syphilis )
- T. pallidum enzyme immunoassay Enzyme immunoassay HIV Infection and AIDS ( TP-EIA TP-EIA Syphilis )
- Chemiluminescence immunoassay Chemiluminescence Immunoassay Syphilis ( CIA CIA Syphilis )
- Prior treated syphilis: In a patient with a history of prior treated syphilis; the patient will require no further treatment (unless there is a reexposure).
- Untreated syphilis: Those without a history of treatment for syphilis require treatment. Unless there is medical history indicating a recent infection, previously untreated patients should be treated as having syphilis of unknown duration or late latent syphilis. [1]
- False positive treponemal test: can be seen in African immigrants with exposure to endemic treponematoses (e.g., yaws, pinta).
Direct methods [5]
Definitive tests using obtained specimens (such as exudates from mucosal lesions). However, use is limited since the tests are not routinely available.
- A microscopy technique illuminating specimens against a dark background.
- Motile spirochetes Spirochetes An order of slender, flexuous, helically coiled bacteria, with one or more complete turns in the helix. Treponema are seen.
- Must be performed immediately after specimen collection
- Sensitivity is < 50% (high false negative False negative An FN test result indicates a person does not have the disease when, in fact, they do. Epidemiological Values of Diagnostic Tests rate).
- Direct fluorescent antibody Direct Fluorescent Antibody A form of fluorescent antibody technique utilizing a fluorochrome conjugated to an antibody, which is added directly to a tissue or cell suspension for the detection of a specific antigen. Congenital TORCH Infections (DFA) testing
- Recommended over darkfield microscopy if using direct methods
- Low sensitivity in blood
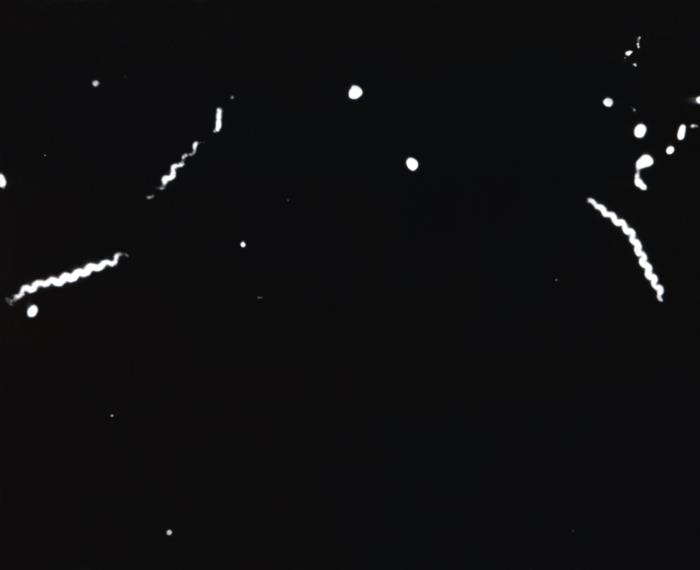
Darkfield microscopy of T. pallidum : Corkscrew-shaped bacteria are seen.
CSF assessment [2,5,6]
- Tests are better at excluding neurosyphilis Neurosyphilis Infections of the central nervous system caused by treponema pallidum which present with a variety of clinical syndromes. The initial phase of infection usually causes a mild or asymptomatic meningeal reaction. The meningovascular form may present acutely as brain infarction. The infection may also remain subclinical for several years. Late syndromes include general paresis; tabes dorsalis; meningeal syphilis; syphilitic optic atrophy; and spinal syphilis. General paresis is characterized by progressive dementia; dysarthria; tremor; myoclonus; seizures; and argyll-robertson pupils. Syphilis rather than diagnosing it.
- TT (TPHA, MHA-TP MHA-TP Treponema , or TPPA TPPA Syphilis )
- NTT (preferably VDRL VDRL Treponema , owing to its better sensitivity than RPR RPR Treponema in CSF)
- Total protein Total protein Liver Function Tests
- Number of mononuclear cells or WBCs
- Neurologic, ocular, and/or otic/auricular findings
- Tertiary syphilis Tertiary Syphilis Syphilis
- Treatment failure in any stage
- Have RPR RPR Treponema or VDRL VDRL Treponema titers ≥ 1:32
- Have a CD4+ count ≤ 350/ mm MM Multiple myeloma (MM) is a malignant condition of plasma cells (activated B lymphocytes) primarily seen in the elderly. Monoclonal proliferation of plasma cells results in cytokine-driven osteoclastic activity and excessive secretion of IgG antibodies. Multiple Myeloma 3
- Have detectable plasma Plasma The residual portion of blood that is left after removal of blood cells by centrifugation without prior blood coagulation. Transfusion Products HIV RNA HIV RNA HIV Infection and AIDS
- Are not on antiretroviral therapy Antiretroviral therapy Antiretroviral therapy (ART) targets the replication cycle of the human immunodeficiency virus (HIV) and is classified based on the viral enzyme or mechanism that is inhibited. The goal of therapy is to suppress viral replication to reach the outcome of undetected viral load. Anti-HIV Drugs
- Consider in follow-up of late syphilis Syphilis Syphilis is a bacterial infection caused by the spirochete Treponema pallidum pallidum (T. p. pallidum), which is usually spread through sexual contact. Syphilis has 4 clinical stages: primary, secondary, latent, and tertiary. Syphilis patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship treated with alternative regimens (e.g., doxycycline)
General management for syphilis Syphilis Syphilis is a bacterial infection caused by the spirochete Treponema pallidum pallidum (T. p. pallidum), which is usually spread through sexual contact. Syphilis has 4 clinical stages: primary, secondary, latent, and tertiary. Syphilis [2–6,9]
- Bactericidal Bactericidal Penicillins levels should be maintained for 7‒10 days (longer with late syphilis Syphilis Syphilis is a bacterial infection caused by the spirochete Treponema pallidum pallidum (T. p. pallidum), which is usually spread through sexual contact. Syphilis has 4 clinical stages: primary, secondary, latent, and tertiary. Syphilis ).
- Long-acting penicillin Penicillin Rheumatic Fever G benzathine is the treatment of choice.
- Typical dose: 2.4 million units (provides treponemicidal levels for up to 21 days)
- Offer HIV HIV Anti-HIV Drugs preexposure prophylaxis Prophylaxis Cephalosporins to those who test negative.
- In geographic areas with high prevalence Prevalence The total number of cases of a given disease in a specified population at a designated time. It is differentiated from incidence, which refers to the number of new cases in the population at a given time. Measures of Disease Frequency of HIV HIV Anti-HIV Drugs , offer preexposure prophylaxis Prophylaxis Cephalosporins and retest for HIV HIV Anti-HIV Drugs in 3 months (if initial result is negative).
- Screening Screening Preoperative Care for other STIs STIs Sexually transmitted infections (STIs) or sexually transmitted diseases (STDs) are infections that spread either by vaginal intercourse, anal sex, or oral sex. Symptoms and signs may include vaginal discharge, penile discharge, dysuria, skin lesions (e.g., warts, ulcers) on or around the genitals, and pelvic pain. Some infections can lead to infertility and chronic debilitating disease. Sexually Transmitted Infections (STIs)
- Offer vaccination Vaccination Vaccination is the administration of a substance to induce the immune system to develop protection against a disease. Unlike passive immunization, which involves the administration of pre-performed antibodies, active immunization constitutes the administration of a vaccine to stimulate the body to produce its own antibodies. Vaccination for hepatitis B Hepatitis B Hepatitis B virus (HBV) is a partially double-stranded DNA virus, which belongs to the Orthohepadnavirus genus and the Hepadnaviridae family. Most individuals with acute HBV infection are asymptomatic or have mild, self-limiting symptoms. Chronic infection can be asymptomatic or create hepatic inflammation, leading to liver cirrhosis and hepatocellular carcinoma (HCC). Hepatitis B Virus , if appropriate.
- Full neurologic exam
- CSF assessment
- Cranial nerve exam
- Ocular slit-lamp exam
- Ophthalmologic exam
- CSF assessment is recommended by some expert guidelines.
- Presumptively treat all partners from the past 90 days.
- Secondary syphilis Secondary Syphilis Syphilis : Test all partners from within the past 6 months; treat based on results.
- Early latent syphilis Latent syphilis The stage of syphilis that occurs following the primary (chancre) and secondary stages. The patient is asymptomatic at the latent stage but remains seropositive for the spirochete. Syphilis : Test all partners from within the past 12 months; treat based on results.
- Test all partners from the past 1 year; treat based on results.
- Test all long-term sex Sex The totality of characteristics of reproductive structure, functions, phenotype, and genotype, differentiating the male from the female organism. Gender Dysphoria partners; treat based on results.
- All lesions are healed (if present).
- 2 weeks after completion of treatment
- Individuals with HIV HIV Anti-HIV Drugs are monitored more frequently.
- Patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship with late syphilis Syphilis Syphilis is a bacterial infection caused by the spirochete Treponema pallidum pallidum (T. p. pallidum), which is usually spread through sexual contact. Syphilis has 4 clinical stages: primary, secondary, latent, and tertiary. Syphilis should also be tested at 24 months.
- Consider CSF assessment.
- Compare titers to initial baseline levels to assess treatment response.
- < 4-fold decrease in NTT titers lasting 6‒12 months after treatment
- Persistent low antibody titers ≤ 4 at 1–2 years after treatment
Early syphilis Syphilis Syphilis is a bacterial infection caused by the spirochete Treponema pallidum pallidum (T. p. pallidum), which is usually spread through sexual contact. Syphilis has 4 clinical stages: primary, secondary, latent, and tertiary. Syphilis management
For primary, secondary, or early latent syphilis Latent syphilis The stage of syphilis that occurs following the primary (chancre) and secondary stages. The patient is asymptomatic at the latent stage but remains seropositive for the spirochete. Syphilis , the following antibiotics can be used:
- Penicillin Penicillin Rheumatic Fever G benzathine 2.4 million units IM once
- If penicillin Penicillin Rheumatic Fever G benzathine is not available: procaine Procaine A local anesthetic of the ester type that has a slow onset and a short duration of action. It is mainly used for infiltration anesthesia, peripheral nerve block, and spinal block. Local Anesthetics penicillin Penicillin Rheumatic Fever 600,000 units IM daily for 10‒14 days
- Includes pregnant patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship and those with HIV HIV Anti-HIV Drugs
- For individuals with penicillin Penicillin Rheumatic Fever allergies Allergies A medical specialty concerned with the hypersensitivity of the individual to foreign substances and protection from the resultant infection or disorder. Selective IgA Deficiency , consider desensitization and/or skin Skin The skin, also referred to as the integumentary system, is the largest organ of the body. The skin is primarily composed of the epidermis (outer layer) and dermis (deep layer). The epidermis is primarily composed of keratinocytes that undergo rapid turnover, while the dermis contains dense layers of connective tissue. Skin: Structure and Functions testing prior to starting an alternative agent.
- Doxycycline (best-studied alternative) 100 mg by mouth twice a day for 14 days
- Ceftriaxone Ceftriaxone A broad-spectrum cephalosporin antibiotic and cefotaxime derivative with a very long half-life and high penetrability to meninges, eyes and inner ears. Cephalosporins 1 g IM or IV once daily for 10‒14 days
- Tetracycline Tetracycline A naphthacene antibiotic that inhibits amino Acyl tRNA binding during protein synthesis. Drug-Induced Liver Injury 500 mg by mouth 4 times daily for 14 days
- Amoxicillin Amoxicillin A broad-spectrum semisynthetic antibiotic similar to ampicillin except that its resistance to gastric acid permits higher serum levels with oral administration. Penicillins 3 g + probenecid Probenecid The prototypical uricosuric agent. It inhibits the renal excretion of organic anions and reduces tubular reabsorption of urate. Probenecid has also been used to treat patients with renal impairment, and, because it reduces the renal tubular excretion of other drugs, has been used as an adjunct to antibacterial therapy. Gout Drugs 500 mg twice daily for 14 days
- Azithromycin Azithromycin A semi-synthetic macrolide antibiotic structurally related to erythromycin. It has been used in the treatment of Mycobacterium avium intracellulare infections, toxoplasmosis, and cryptosporidiosis. Macrolides and Ketolides (should be considered only as a last resort owing to resistance Resistance Physiologically, the opposition to flow of air caused by the forces of friction. As a part of pulmonary function testing, it is the ratio of driving pressure to the rate of air flow. Ventilation: Mechanics of Breathing ): 2 g by mouth once
- Erythromycin Erythromycin A bacteriostatic antibiotic macrolide produced by streptomyces erythreus. Erythromycin a is considered its major active component. In sensitive organisms, it inhibits protein synthesis by binding to 50s ribosomal subunits. This binding process inhibits peptidyl transferase activity and interferes with translocation of amino acids during translation and assembly of proteins. Macrolides and Ketolides (a possibility per the WHO, but not recommended by US, UK, or European guidelines): 500 mg 4 times daily for 14 days
- Azithromycin Azithromycin A semi-synthetic macrolide antibiotic structurally related to erythromycin. It has been used in the treatment of Mycobacterium avium intracellulare infections, toxoplasmosis, and cryptosporidiosis. Macrolides and Ketolides and erythromycin Erythromycin A bacteriostatic antibiotic macrolide produced by streptomyces erythreus. Erythromycin a is considered its major active component. In sensitive organisms, it inhibits protein synthesis by binding to 50s ribosomal subunits. This binding process inhibits peptidyl transferase activity and interferes with translocation of amino acids during translation and assembly of proteins. Macrolides and Ketolides do not cross the placenta Placenta A highly vascularized mammalian fetal-maternal organ and major site of transport of oxygen, nutrients, and fetal waste products. It includes a fetal portion (chorionic villi) derived from trophoblasts and a maternal portion (decidua) derived from the uterine endometrium. The placenta produces an array of steroid, protein and peptide hormones (placental hormones). Placenta, Umbilical Cord, and Amniotic Cavity well, so they are poor choices in pregnant women.
- Doxycycline is teratogenic and is contraindicated.
Late syphilis Syphilis Syphilis is a bacterial infection caused by the spirochete Treponema pallidum pallidum (T. p. pallidum), which is usually spread through sexual contact. Syphilis has 4 clinical stages: primary, secondary, latent, and tertiary. Syphilis management [2,5,6,9]
For late-latent syphilis Syphilis Syphilis is a bacterial infection caused by the spirochete Treponema pallidum pallidum (T. p. pallidum), which is usually spread through sexual contact. Syphilis has 4 clinical stages: primary, secondary, latent, and tertiary. Syphilis , tertiary syphilis Tertiary Syphilis Syphilis , or syphilis Syphilis Syphilis is a bacterial infection caused by the spirochete Treponema pallidum pallidum (T. p. pallidum), which is usually spread through sexual contact. Syphilis has 4 clinical stages: primary, secondary, latent, and tertiary. Syphilis of unknown duration, the following regimen is used:
- Penicillin Penicillin Rheumatic Fever G benzathine 2.4 million units IM once per week for 3 weeks (i.e., on days 1, 8, and 15)
- If penicillin Penicillin Rheumatic Fever G benzathine is not available: procaine Procaine A local anesthetic of the ester type that has a slow onset and a short duration of action. It is mainly used for infiltration anesthesia, peripheral nerve block, and spinal block. Local Anesthetics penicillin Penicillin Rheumatic Fever 600,000–1.2 million units IM once daily for 17‒21 days
- Doxycycline 100 mg by mouth twice daily for 21‒30 days
- Ceftriaxone Ceftriaxone A broad-spectrum cephalosporin antibiotic and cefotaxime derivative with a very long half-life and high penetrability to meninges, eyes and inner ears. Cephalosporins 2 g IV or IM daily for 10‒14 days
Neurosyphilis Neurosyphilis Infections of the central nervous system caused by treponema pallidum which present with a variety of clinical syndromes. The initial phase of infection usually causes a mild or asymptomatic meningeal reaction. The meningovascular form may present acutely as brain infarction. The infection may also remain subclinical for several years. Late syndromes include general paresis; tabes dorsalis; meningeal syphilis; syphilitic optic atrophy; and spinal syphilis. General paresis is characterized by progressive dementia; dysarthria; tremor; myoclonus; seizures; and argyll-robertson pupils. Syphilis [2,5,6,9,10,14]
- Invasion of T. pallidum into the CSF is common in primary and secondary syphilis Secondary Syphilis Syphilis , but the clinical significance of this is unclear.
- Patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship with ocular and/or otologic findings should be treated for neurosyphilis Neurosyphilis Infections of the central nervous system caused by treponema pallidum which present with a variety of clinical syndromes. The initial phase of infection usually causes a mild or asymptomatic meningeal reaction. The meningovascular form may present acutely as brain infarction. The infection may also remain subclinical for several years. Late syndromes include general paresis; tabes dorsalis; meningeal syphilis; syphilitic optic atrophy; and spinal syphilis. General paresis is characterized by progressive dementia; dysarthria; tremor; myoclonus; seizures; and argyll-robertson pupils. Syphilis regardless of CSF findings.
- 3‒4 million units IV every 4 hours OR
- Continuous infusion
- Procaine Procaine A local anesthetic of the ester type that has a slow onset and a short duration of action. It is mainly used for infiltration anesthesia, peripheral nerve block, and spinal block. Local Anesthetics penicillin Penicillin Rheumatic Fever G 2.4 million units IM once daily for 10‒14 days PLUS
- Probenecid Probenecid The prototypical uricosuric agent. It inhibits the renal excretion of organic anions and reduces tubular reabsorption of urate. Probenecid has also been used to treat patients with renal impairment, and, because it reduces the renal tubular excretion of other drugs, has been used as an adjunct to antibacterial therapy. Gout Drugs 500 mg by mouth 4 times daily for 10‒14 days
- Alternative regimen: ceftriaxone Ceftriaxone A broad-spectrum cephalosporin antibiotic and cefotaxime derivative with a very long half-life and high penetrability to meninges, eyes and inner ears. Cephalosporins 2 g IV once daily for 10‒14 days
- Serial neurologic examinations every 6 months
- Consider CSF assessment (especially if treated with an alternative regimen).
Jarisch–Herxheimer reaction Jarisch–Herxheimer Reaction Syphilis [9]
- Caused by an immune response to the antigens released by dying spirochetes Spirochetes An order of slender, flexuous, helically coiled bacteria, with one or more complete turns in the helix. Treponema
- Rigors Rigors Fever
- Rise in temperature
- Increased respiratory rate Respiratory rate The number of times an organism breathes with the lungs (respiration) per unit time, usually per minute. Pulmonary Examination
- Hypotension Hypotension Hypotension is defined as low blood pressure, specifically Hypotension
- Occurs within 24 hours
- Resolves within 12–24 hours
- Seen in 10%–35% of cases
- Antipyretics (e.g., acetaminophen Acetaminophen Acetaminophen is an over-the-counter nonopioid analgesic and antipyretic medication and the most commonly used analgesic worldwide. Despite the widespread use of acetaminophen, its mechanism of action is not entirely understood. Acetaminophen , aspirin Aspirin The prototypical analgesic used in the treatment of mild to moderate pain. It has anti-inflammatory and antipyretic properties and acts as an inhibitor of cyclooxygenase which results in the inhibition of the biosynthesis of prostaglandins. Aspirin also inhibits platelet aggregation and is used in the prevention of arterial and venous thrombosis. Nonsteroidal Antiinflammatory Drugs (NSAIDs) , ibuprofen Ibuprofen A nonsteroidal anti-inflammatory agent with analgesic properties used in the treatment of rheumatism and arthritis. Nonsteroidal Antiinflammatory Drugs (NSAIDs) )
- IV fluids IV fluids Intravenous fluids are one of the most common interventions administered in medicine to approximate physiologic bodily fluids. Intravenous fluids are divided into 2 categories: crystalloid and colloid solutions. Intravenous fluids have a wide variety of indications, including intravascular volume expansion, electrolyte manipulation, and maintenance fluids. Intravenous Fluids
- Chancroid Chancroid Chancroid is a highly transmissible STD caused by Haemophilus ducreyi. The disease presents with painful ulcer(s) on the genital tract (termed chancroid or “soft chancre”). Up to 50% of patients will develop painful inguinal lymphadenopathy. Chancroid : STI STI Sexually transmitted infections (STIs) are infections that spread either by vaginal intercourse, anal sex, or oral sex. Symptoms and signs may include vaginal discharge, penile discharge, dysuria, skin lesions (e.g., warts, ulcers) on or around the genitals, and pelvic pain. Some infections can lead to infertility and chronic debilitating disease. Sexually Transmitted Infections (STIs) caused by Haemophilus ducreyi Haemophilus ducreyi A species of Haemophilus that appears to be the pathogen or causative agent of the sexually transmitted disease, chancroid. Haemophilus . Patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship develop painful, necrotizing genital ulcers and inguinal lymphadenopathy Inguinal Lymphadenopathy Lymphadenopathy . Diagnosis is usually clinical, but PCR PCR Polymerase chain reaction (PCR) is a technique that amplifies DNA fragments exponentially for analysis. The process is highly specific, allowing for the targeting of specific genomic sequences, even with minuscule sample amounts. The PCR cycles multiple times through 3 phases: denaturation of the template DNA, annealing of a specific primer to the individual DNA strands, and synthesis/elongation of new DNA molecules. Polymerase Chain Reaction (PCR) and cultures can help to confirm. Management is with macrolide antibiotics.
- Donovanosis Donovanosis Donovanosis (also known as granuloma inguinale) is an STD caused by Klebsiella granulomatis and is mainly seen in tropical regions. The condition is characterized by chronic, progressive, ulcerating disease mostly affecting the genital region. Donovanosis : STI STI Sexually transmitted infections (STIs) are infections that spread either by vaginal intercourse, anal sex, or oral sex. Symptoms and signs may include vaginal discharge, penile discharge, dysuria, skin lesions (e.g., warts, ulcers) on or around the genitals, and pelvic pain. Some infections can lead to infertility and chronic debilitating disease. Sexually Transmitted Infections (STIs) caused by Klebsiella Klebsiella Klebsiella are encapsulated gram-negative, lactose-fermenting bacilli. They form pink colonies on MacConkey agar due to lactose fermentation. The main virulence factor is a polysaccharide capsule. Klebsiella pneumoniae is the most important pathogenic species. Klebsiella granulomatis . Donovanosis Donovanosis Donovanosis (also known as granuloma inguinale) is an STD caused by Klebsiella granulomatis and is mainly seen in tropical regions. The condition is characterized by chronic, progressive, ulcerating disease mostly affecting the genital region. Donovanosis is also known as granuloma inguinale Granuloma inguinale Donovanosis (also known as granuloma inguinale) is an STD caused by Klebsiella granulomatis and is mainly seen in tropical regions. The condition is characterized by chronic, progressive, ulcerating disease mostly affecting the genital region. Donovanosis . The progressive, nodular genital lesions can form into painless ulcerations and cause tissue damage. Lymphadenopathy Lymphadenopathy Lymphadenopathy is lymph node enlargement (> 1 cm) and is benign and self-limited in most patients. Etiologies include malignancy, infection, and autoimmune disorders, as well as iatrogenic causes such as the use of certain medications. Generalized lymphadenopathy often indicates underlying systemic disease. Lymphadenopathy is uncommon. Diagnosis is confirmed with microscopic findings of Donovan bodies Donovan Bodies Donovanosis from the lesion. Management involves antibiotics, such as macrolides Macrolides Macrolides and ketolides are antibiotics that inhibit bacterial protein synthesis by binding to the 50S ribosomal subunit and blocking transpeptidation. These antibiotics have a broad spectrum of antimicrobial activity but are best known for their coverage of atypical microorganisms. Macrolides and Ketolides , tetracyclines Tetracyclines Tetracyclines are a class of broad-spectrum antibiotics indicated for a wide variety of bacterial infections. These medications bind the 30S ribosomal subunit to inhibit protein synthesis of bacteria. Tetracyclines cover gram-positive and gram-negative organisms, as well as atypical bacteria such as chlamydia, mycoplasma, spirochetes, and even protozoa. Tetracyclines , and trimethoprim-sulfamethoxazole.
- Lymphogranuloma venereum Lymphogranuloma venereum Subacute inflammation of the inguinal lymph glands caused by certain immunotypes of Chlamydia trachomatis. It is a sexually transmitted disease in the U.S. But is more widespread in developing countries. It is distinguished from granuloma venereum, which is caused by calymmatobacterium granulomatis. Chlamydial Infections : STI STI Sexually transmitted infections (STIs) are infections that spread either by vaginal intercourse, anal sex, or oral sex. Symptoms and signs may include vaginal discharge, penile discharge, dysuria, skin lesions (e.g., warts, ulcers) on or around the genitals, and pelvic pain. Some infections can lead to infertility and chronic debilitating disease. Sexually Transmitted Infections (STIs) caused by 3 strains of Chlamydia trachomatis Chlamydia trachomatis Type species of Chlamydia causing a variety of ocular and urogenital diseases. Chlamydia . Patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship may have a small, transient, painless genital ulcer followed by lymphadenopathy Lymphadenopathy Lymphadenopathy is lymph node enlargement (> 1 cm) and is benign and self-limited in most patients. Etiologies include malignancy, infection, and autoimmune disorders, as well as iatrogenic causes such as the use of certain medications. Generalized lymphadenopathy often indicates underlying systemic disease. Lymphadenopathy ( bubo Bubo Yersinia pestis/Plague ). Diagnosis is clinical, though PCR PCR Polymerase chain reaction (PCR) is a technique that amplifies DNA fragments exponentially for analysis. The process is highly specific, allowing for the targeting of specific genomic sequences, even with minuscule sample amounts. The PCR cycles multiple times through 3 phases: denaturation of the template DNA, annealing of a specific primer to the individual DNA strands, and synthesis/elongation of new DNA molecules. Polymerase Chain Reaction (PCR) testing can help with confirmation. Management involves tetracyclines Tetracyclines Tetracyclines are a class of broad-spectrum antibiotics indicated for a wide variety of bacterial infections. These medications bind the 30S ribosomal subunit to inhibit protein synthesis of bacteria. Tetracyclines cover gram-positive and gram-negative organisms, as well as atypical bacteria such as chlamydia, mycoplasma, spirochetes, and even protozoa. Tetracyclines or erythromycin Erythromycin A bacteriostatic antibiotic macrolide produced by streptomyces erythreus. Erythromycin a is considered its major active component. In sensitive organisms, it inhibits protein synthesis by binding to 50s ribosomal subunits. This binding process inhibits peptidyl transferase activity and interferes with translocation of amino acids during translation and assembly of proteins. Macrolides and Ketolides .
- Genital herpes Genital Herpes Genital herpes infections are common sexually transmitted infections caused by herpes simplex virus (HSV) type 1 or 2. Primary infection often presents with systemic, prodromal symptoms followed by clusters of painful, fluid-filled vesicles on an erythematous base, dysuria, and painful lymphadenopathy. Labial and Genital Herpes : a common STI STI Sexually transmitted infections (STIs) are infections that spread either by vaginal intercourse, anal sex, or oral sex. Symptoms and signs may include vaginal discharge, penile discharge, dysuria, skin lesions (e.g., warts, ulcers) on or around the genitals, and pelvic pain. Some infections can lead to infertility and chronic debilitating disease. Sexually Transmitted Infections (STIs) caused by HSV HSV Herpes simplex virus (HSV) is a double-stranded DNA virus belonging to the family Herpesviridae. Herpes simplex virus commonly causes recurrent infections involving the skin and mucosal surfaces, including the mouth, lips, eyes, and genitals. Herpes Simplex Virus 1 and 2 type 1 Type 1 Spinal Muscular Atrophy or 2. Prodromal symptoms often precede clusters of painful, fluid-filled vesicles Vesicles Female Genitourinary Examination on an erythematous base, which eventually form ulcers that can coalesce. Lymphadenopathy Lymphadenopathy Lymphadenopathy is lymph node enlargement (> 1 cm) and is benign and self-limited in most patients. Etiologies include malignancy, infection, and autoimmune disorders, as well as iatrogenic causes such as the use of certain medications. Generalized lymphadenopathy often indicates underlying systemic disease. Lymphadenopathy , dysuria Dysuria Painful urination. It is often associated with infections of the lower urinary tract. Urinary tract infections (UTIs) , and severe neuralgia can occur. The diagnosis is generally clinical but confirmed with PCR PCR Polymerase chain reaction (PCR) is a technique that amplifies DNA fragments exponentially for analysis. The process is highly specific, allowing for the targeting of specific genomic sequences, even with minuscule sample amounts. The PCR cycles multiple times through 3 phases: denaturation of the template DNA, annealing of a specific primer to the individual DNA strands, and synthesis/elongation of new DNA molecules. Polymerase Chain Reaction (PCR) and serologic testing. Management includes antiviral Antiviral Antivirals for Hepatitis B therapy.
- Genital warts Warts Benign epidermal proliferations or tumors; some are viral in origin. Female Genitourinary Examination (also called condylomata acuminata Condylomata Acuminata Condylomata acuminata are a clinical manifestation of genital HPV infection. Condylomata acuminata are described as raised, pearly, flesh-colored, papular, cauliflower-like lesions seen in the anogenital region that may cause itching, pain, or bleeding. Condylomata Acuminata (Genital Warts) ): a human papillomavirus Human papillomavirus Human papillomavirus (HPV) is a nonenveloped, circular, double-stranded DNA virus belonging to the Papillomaviridae family. Humans are the only reservoir, and transmission occurs through close skin-to-skin or sexual contact. Human papillomaviruses infect basal epithelial cells and can affect cell-regulatory proteins to result in cell proliferation. Papillomavirus (HPV) ( HPV HPV Human papillomavirus (HPV) is a nonenveloped, circular, double-stranded DNA virus belonging to the Papillomaviridae family. Humans are the only reservoir, and transmission occurs through close skin-to-skin or sexual contact. Human papillomaviruses infect basal epithelial cells and can affect cell-regulatory proteins to result in cell proliferation. Papillomavirus (HPV) ) infection causing a range of mucocutaneous findings, including broad-based smooth or velvety papules or rough verrucous or fungating plaques, in the anogenital region. The diagnosis is clinical. Management may include cytodestructive therapy ( podophyllotoxin Podophyllotoxin A lignan (lignans) found in podophyllin resin from the roots of podophyllum plants. It is a potent spindle poison, toxic if taken internally, and has been used as a cathartic. It is very irritating to skin and mucous membranes, has keratolytic actions, has been used to treat warts and keratoses, and may have antineoplastic properties, as do some of its congeners and derivatives. Molluscum Contagiosum ), immune-mediated therapy ( imiquimod Imiquimod A topically-applied aminoquinoline immune modulator that induces interferon production. It is used in the treatment of external genital and perianal warts, superficial carcinoma, basal cell; and actinic keratosis. Hypertrophic and Keloid Scars ), or surgical therapy.
Practical application in the clinic (checklist for patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship presenting with a genital ulcer): [4]
- Take a careful medical and sexual history.
- Examination of the genital, anal, and oral areas
- Syphilis Syphilis Syphilis is a bacterial infection caused by the spirochete Treponema pallidum pallidum (T. p. pallidum), which is usually spread through sexual contact. Syphilis has 4 clinical stages: primary, secondary, latent, and tertiary. Syphilis ( PCR PCR Polymerase chain reaction (PCR) is a technique that amplifies DNA fragments exponentially for analysis. The process is highly specific, allowing for the targeting of specific genomic sequences, even with minuscule sample amounts. The PCR cycles multiple times through 3 phases: denaturation of the template DNA, annealing of a specific primer to the individual DNA strands, and synthesis/elongation of new DNA molecules. Polymerase Chain Reaction (PCR) from lesion and serologic TT and/or NTT)
- Herpes simplex Herpes Simplex A group of acute infections caused by herpes simplex virus type 1 or type 2 that is characterized by the development of one or more small fluid-filled vesicles with a raised erythematous base on the skin or mucous membrane. It occurs as a primary infection or recurs due to a reactivation of a latent infection. Congenital TORCH Infections virus Virus Viruses are infectious, obligate intracellular parasites composed of a nucleic acid core surrounded by a protein capsid. Viruses can be either naked (non-enveloped) or enveloped. The classification of viruses is complex and based on many factors, including type and structure of the nucleoid and capsid, the presence of an envelope, the replication cycle, and the host range. Virology ( nucleic acid amplification Nucleic acid amplification Laboratory techniques that involve the in-vitro synthesis of many copies of DNA or RNA from one original template. Septic Arthritis test (NAAT) from lesion)
- Consider other ulcerative diseases, including lymphogranuloma venereum Lymphogranuloma venereum Subacute inflammation of the inguinal lymph glands caused by certain immunotypes of Chlamydia trachomatis. It is a sexually transmitted disease in the U.S. But is more widespread in developing countries. It is distinguished from granuloma venereum, which is caused by calymmatobacterium granulomatis. Chlamydial Infections , chancroid Chancroid Chancroid is a highly transmissible STD caused by Haemophilus ducreyi. The disease presents with painful ulcer(s) on the genital tract (termed chancroid or “soft chancre”). Up to 50% of patients will develop painful inguinal lymphadenopathy. Chancroid , and donovanosis Donovanosis Donovanosis (also known as granuloma inguinale) is an STD caused by Klebsiella granulomatis and is mainly seen in tropical regions. The condition is characterized by chronic, progressive, ulcerating disease mostly affecting the genital region. Donovanosis .
- Provide same-day treatment for syphilis Syphilis Syphilis is a bacterial infection caused by the spirochete Treponema pallidum pallidum (T. p. pallidum), which is usually spread through sexual contact. Syphilis has 4 clinical stages: primary, secondary, latent, and tertiary. Syphilis and/or HSV HSV Herpes simplex virus (HSV) is a double-stranded DNA virus belonging to the family Herpesviridae. Herpes simplex virus commonly causes recurrent infections involving the skin and mucosal surfaces, including the mouth, lips, eyes, and genitals. Herpes Simplex Virus 1 and 2 based on history, point-of-care testing, and clinical findings.
- Screen for other STIs STIs Sexually transmitted infections (STIs) or sexually transmitted diseases (STDs) are infections that spread either by vaginal intercourse, anal sex, or oral sex. Symptoms and signs may include vaginal discharge, penile discharge, dysuria, skin lesions (e.g., warts, ulcers) on or around the genitals, and pelvic pain. Some infections can lead to infertility and chronic debilitating disease. Sexually Transmitted Infections (STIs) .
- Address safe sex Sex The totality of characteristics of reproductive structure, functions, phenotype, and genotype, differentiating the male from the female organism. Gender Dysphoria , abstinence during and after treatment, and partner treatment.
- Adjust management based on test results when they become available.
- Centers for Disease Control and Prevention. (2021). Sexually transmitted infections treatment guidelines, 2021: syphilis. Retrieved August 8, 2022, from https://www.cdc.gov/std/treatment-guidelines/syphilis.htm
- Centers for Disease Control and Prevention. (2022). Syphilis—CDC detailed fact sheet. Retrieved August 8, 2022, from https://www.cdc.gov/std/syphilis/stdfact-syphilis-detailed.htm
- World Health Organization. (2016). WHO guidelines for the treatment of Treponema pallidum (syphilis). Retrieved August 8, 2022, from https://www.who.int/publications/i/item/9789241549714
- World Health Organization. (2021). Guidelines for the management of symptomatic sexually transmitted infections. Retrieved August 8, 2022, from https://www.who.int/publications/i/item/9789240024168
- Janier, M., Unemo, M., Dupin, N., et al. (2020). 2020 European guideline on the management of syphilis. https://onlinelibrary.wiley.com/doi/full/10.1111/jdv.16946
- Kingston, M., French, P., Higgins, S., et al. (2015). UK national guidelines on the management of syphilis 2015. International Journal of STD & AIDS. https://journals.sagepub.com/doi/10.1177/0956462415624059?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub%20%200pubmed
- US Preventive Services Task Force. (2022). Recommendation statement: screening for syphilis infection in nonpregnant adults and adolescents. Retrieved November 30, 2022, from https://www.uspreventiveservicestaskforce.org/uspstf/recommendation/syphilis-infection-nonpregnant-adults-adolescents-screening
- Hicks, C., Clement, M. (2020). Syphilis: screening and diagnostic testing. UpToDate. Retrieved January 18, 2021, from https://www.uptodate.com/contents/syphilis-screening-and-diagnostic-testing
- Hicks, C., Clement, M. (2020). Syphilis: treatment and monitoring. UpToDate. Retrieved January 18, 2021, from https://www.uptodate.com/contents/syphilis-treatment-and-monitoring
- Marra, C. (2020). Neurosyphilis. UpToDate. Retrieved January 18, 2021, from https://www.uptodate.com/contents/neurosyphilis
- Hicks, C., Clement, M. (2020). Syphilis: epidemiology, pathophysiology, and clinical manifestations in patients without HIV. UpToDate. Retrieved January 18, 2021, from https://www.uptodate.com/contents/syphilis-epidemiology-pathophysiology-and-clinical-manifestations-in-patients-without-hiv
- Chandrasekar, P. H. (2017). Syphilis. Medscape. Retrieved February 19, 2021, from https://emedicine.medscape.com/article/229461-overview
- Tudor, M. E., Al Aboud, A. M., Gossman, W. G. (2020). Syphilis. StatPearls. Retrieved February 19, 2021, from https://www.ncbi.nlm.nih.gov/books/NBK534780/
- Ha, T., Taki, P., and Dubensky, L. (2020). Neurosyphilis. StatPearls. Retrieved February 19, 2021, from https://www.ncbi.nlm.nih.gov/books/NBK540979/
- Morris, S. R. (2020). Syphilis. MSD Manual Professional Version. Retrieved February 19, 2021, from https://www.msdmanuals.com/professional/infectious-diseases/sexually-transmitted-diseases-stds/syphilis
- Gu, W. M., Yang, Y., Wang, Q. Z., Pan, B. S., Guo, W., Wu, L., Hu, W. Z., Yang, S., Song, B. B., Zhang, C. Y. (2013). Comparing the performance of traditional non-treponemal tests on syphilis and non-syphilis serum samples. International Journal of STD & AIDS, 24(12), 919–925. https://doi.org/10.1177/0956462413491399
- Henao-Martínez, A. F., Johnson, S. C. (2014). Diagnostic tests for syphilis: new tests and new algorithms. Neurology Clinical Practice, 4(2), 114–122. https://doi.org/10.1212/01.CPJ.0000435752.17621.48
Study with Lecturio for
Medical School
Nursing School
- Data Privacy
- Terms and Conditions
- Legal Information
USMLE™ is a joint program of the Federation of State Medical Boards (FSMB®) and National Board of Medical Examiners (NBME®). MCAT is a registered trademark of the Association of American Medical Colleges (AAMC). NCLEX®, NCLEX-RN®, and NCLEX-PN® are registered trademarks of the National Council of State Boards of Nursing, Inc (NCSBN®). None of the trademark holders are endorsed by nor affiliated with Lecturio.
Create your free account or log in to continue reading!
Sign up now and get free access to Lecturio with concept pages, medical videos, and questions for your medical education.
Log in to your account
User Reviews
Get Premium to test your knowledge
Lecturio Premium gives you full access to all content & features
Get Premium to watch all videos
Verify your email now to get a free trial.
Create a free account to test your knowledge
Lecturio Premium gives you full access to all contents and features—including Lecturio’s Qbank with up-to-date board-style questions.

An official website of the United States government
Here’s how you know
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock A locked padlock ) or https:// means you’ve safely connected to the .gov website. Share sensitive information only on official, secure websites.
Syphilis Is a Public Health Priority
As a sexually transmitted infection (STI), syphilis is a public health threat in the United States, and it has reached a crisis level. Cases of syphilis in the U.S. have reached their highest levels since the 1950s, and, heartbreakingly, cases of syphilis among newborns have gone up more than tenfold over the past 10 years. So, this STI Awareness Week , I joined partners across the country to raise awareness of syphilis and congenital syphilis and what individuals, clinicians, and organizations can do to reduce it.
Syphilis is a serious infection. If untreated, it can damage the heart and brain and can cause blindness, deafness, and paralysis. When transmitted and not treated during pregnancy, it can cause miscarriage, lifelong medical issues, and even infant death. It is curable with antibiotics, and screening, early diagnosis and treatment are essential to preventing complications and transmission.
Sadly, prevention and treatment services are not getting to all those who need them. For example, according to a recent Centers for Disease Control and Prevention(CDC) report , 9 in 10 cases of congenital syphilis could have been prevented with timely testing and adequate treatment during pregnancy in 2022. Testing and treatment gaps were present in the majority of cases across all races, ethnicities, and U.S. Census Bureau regions.
In response to this crisis, the U.S. Department of Health and Human Services (HHS) formed a multi-agency National Syphilis and Congenital Syphilis Syndemic Task Force. The goal of the task force is to leverage federal resources to improve prevention and treatment of syphilis, while also reducing health inequities.
The task force has undertaken numerous actions, including raising awareness of this crisis, conducting briefings with external partners to identify and maximize collaboration opportunities, convening workshops to address disparities and focus on research strategies, and working with agencies to issue funding flexibility letters to grantees for syphilis care.
As we continue to implement these and other strategies, here are just some of the steps we can all take:
- Individuals—Have open and honest conversations with your clinician and partner(s) about sexual health and sexually transmitted infections (STIs). Find out if syphilis and other STI tests are for you, and, if you need treatment for an STI, work with your sex partners to make sure they receive treatment as well
- Pregnant people—See a clinician as soon as possible if you think you are pregnant to be sure that you and your baby are healthy during your pregnancy. Ask your clinician about getting tested for syphilis at your first visit and, if you have syphilis, get treatment as quickly as possible and also talk with your partner(s) about treatment.
- Clinicians—Collect a sexual history with all of your patients as part of routine health care and look for ways to reduce stigma and create a welcoming clinical environment. Test your patients for syphilis and other STIs as recommended by CDC. You can access STI treatment guidelines on CDC.gov to ensure appropriate treatment and care. If you need to learn more about syphilis, please utilize the National STD Curriculum and reach out to the STD Clinical Consultation Network if you need help managing your patients. The National Network of STD Clinical Prevention Training Centers can help provide education about syphilis and other STIs too.
- Organizations—Continue to spread the word that syphilis is preventable and treatable and amplify efforts to reduce the STI-related stigma that prevents many people from accessing the medical care they need.
Please join me in raising awareness of syphilis and other STIs by sharing this information with your networks, this STI Awareness week and beyond.
Together, we can bend the syphilis curve and its associated complications. I look forward to reaching our goals for syphilis and other STIs together.
Sign Up for Email Updates
Receive the latest updates from the Secretary, Blogs, and News Releases
Subscribe to RSS
Receive latest updates

Related Blog Posts

OCR Celebrates Women’s History Month

Black History Month; Recognizing Contributions and Continuing the Fight Against Health Inequities

Happy National Hispanic Heritage Month - Latinos: Driving Prosperity, Power and Progress in America
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List

Syphilis Infections, Reinfections and Serological Response in a Large Italian Sexually Transmitted Disease Centre: A Monocentric Retrospective Study
Valentina marchese.
1 Unit of Infectious and Tropical Diseases, Department of Clinical and Experimental Sciences, ASST Spedali Civili di Brescia and University of Brescia, 25123 Brescia, Italy
2 Unit of Infectious and Tropical Diseases, ASST Spedali Civili di Brescia, 25123 Brescia, Italy
Giorgio Tiecco
Samuele storti, melania degli antoni, stefano calza.
3 Unit of Biostatistics and Bioinformatics, Department of Molecular and Translational Medicine, University of Brescia, 25123 Brescia, Italy
Maurizio Gulletta
Francesca viola, emanuele focà, alberto matteelli, francesco castelli, eugenia quiros-roldan, associated data.
Data presented in this manuscript are available from the corresponding authors on reasonable request.
Background: Syphilis infection does not confer definitive and protective immunity against reinfection, and crucial aspects of repeated episodes of syphilis are far from being understood, especially among people living with HIV (PLWH). Methods: In order to explore the burden of syphilis in a large cohort of HIV-negative patients and PLWH, this retrospective study describes the demographics, clinical presentation and treatment outcome of patients with syphilis treated at our clinic from 2013 to 2021. Results: Within the study period, 1859 syphilis episodes (827, 44.5% first infections and 1032, 55.5% reinfections) were recorded. A total of 663 patients, of whom 347 (52%) had PLWH, were considered. Syphilis was mostly diagnosed in males (77%) and European (79%) patients. More than half of syphilis episodes were recorded during the late latent stage (64%) or during follow-up/screening visits for other diseases, while symptomatic stages led to a diagnosis in almost half of HIV-negative patients ( p < 0.001). PLWH with syphilis infection were predominantly homo/bisexual ( p < 0.001). A significantly higher rate of syphilis reinfection was observed in PLWH, who also demonstrated a higher range of subsequent episodes. The serofast state was found to be similar at the 6- and 12-month follow-up visits. The multivariate analysis carried out in the HIV-positive group showed that an RPR titre >1:16 was an independent predictor for serological non-response. Conclusions: Syphilis reinfections are predominantly diagnosed in HIV-positive MSM. The high rate of asymptomatic presentation among PLWH supports the role of periodical syphilis screening. In PLWH, the only baseline factor associated with an increased risk of non-response was an RPR titre >1:16, while assessment at 12 months after treatment increased the possibility of detecting a serological response, indicating that PLWH have a slower serological response to treatment.
1. Background
Syphilis is one of the oldest sexually transmitted diseases, for which curative and inexpensive treatment is available [ 1 ]. However, the annual rate of primary and secondary syphilis has risen in recent years, both in Europe and the USA [ 2 ]. In Italy, the estimated notification rate is 2.5/100,000, and syphilis disproportionately affects men, with an overall gender ratio of 7:1 (male-to-female) in 2018 [ 3 ]. Previous Italian national data (1991–2017) confirm the major burden in males, demonstrating that they account for 91% of all primary or secondary cases and 65% of latent syphilis [ 4 ].
During the last two years of the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) pandemic, community containment and social distancing measures might have affected the circulation of STDs [ 5 ]. However, few and controversial data are available. A recent monocentric study carried out in Italy has shown that despite the lockdown and the fear of SARS-CoV-2 infection, risky sexual activity has not diminished; likewise, the risk of syphilis remains, raising concern for community health [ 6 ].
Syphilis is frequently encountered among people living with HIV (PLWH), with a non-uniquely defined prevalence; in Europe, the rate of HIV and syphilis coinfection (either known or newly diagnosed) is 24% overall and may reach 35% when specifically considering the bisexual population and other men who have sex with men (MSM) [ 2 , 7 ]. Moreover, syphilis facilitates both HIV transmission and HIV acquisition, and with the consolidation of the evidence that a stable virological suppression of plasmatic HIV-RNA does not lead to HIV transmission (U = U or undetectable = untransmittable), this bond is intended to last [ 1 ]. Coinfection is dangerous because HIV infection may modulate the clinical presentation and the serologic response to syphilis treatment [ 7 ]. PLWH with a syphilis infection seem to have a higher risk of developing neurosyphilis and mount an abnormal serological response [ 8 , 9 ]. Many diagnostic and therapeutic challenges remain, as there are currently no controlled trials focused on syphilis–HIV coinfection management. Standard HIV care should always include regular syphilis serology, but new models for testing and prevention will be crucial next steps in controlling this coinfection [ 10 ].
Syphilis infection does not lead to immunity against reinfection, making repeated episodes of syphilis a concrete reality, especially in MSM with a high rate of partner change [ 11 ]. Moreover, data regarding serological response in patients with syphilis reinfection are discordant, and crucial aspects of the interpretation of non-treponemal test trends are far from being resolved [ 1 ]. The non-uniquely defined serological response in syphilis reinfections, together with the altered immunologic response in PLWH, represents a challenge for clinicians.
In order to explore the burden of syphilis in a large cohort of HIV-negative patients and PLWH, this retrospective study describes the demographics, clinical presentation and treatment outcomes of patients with syphilis treated at our clinic from 2013 to 2021. It also aims at assessing possible factors associated with serological response to treatment for syphilis reinfections among PLWH, for whom a higher frequency of reinfection was recorded during the study period. We also aimed to assess relevant factors associated with a serological response to treatment and syphilis reinfection among our HIV/syphilis coinfected population.
2. Materials and Methods
2.1. study population and setting.
The study was conducted at the Department of Infectious Disease of the ASST Spedali Civili, Brescia, Italy. In 2021, our department provided care to 3841 PLWH and hosted a clinic for sexually transmitted diseases (STDs) as part of the Italian Sentinel Surveillance System.
We retrospectively evaluated all cases of syphilis reported by our clinic to the Italian Sentinel Syphilis Surveillance System from January 2013 to December 2021, matching them with our electronic health record system. Incomplete or uncertain records were excluded. The study population was split into 2 groups: the HIV-positive group and HIV-negative group or control group, according to the presence of HIV/syphilis coinfection. All cases of syphilis (first diagnosis or reinfection), either among PLWH or HIV-negative patients aged >18 years, were included.
2.2. Data Collection
Demographic and clinical/laboratory characteristics were collected from medical records. The variables included sex, age, area of origin according to the United Nations (UN) classification [ 12 ], sexual orientation, HIV infection and, among PLWH, HIV viral load and lymphocyte CD4+ T-cell count. For detected cases, data regarding clinical classification (primary, secondary, tertiary, early latent, late latent or neurosyphilis) and reasons for testing were collected (screening for PLWH, pregnancy, other STDs or partner tracing or presence of symptoms). Incomplete or uncertain cases were excluded. Moreover, only records with at least one follow-up consultation at 6 and/or 12 months after treatment, reporting signs or symptoms and non-treponemal test results were included to assess the serological response to treatment.
2.3. Clinical Management
We considered indirect methods to assess a syphilis diagnosis; TPHA (Treponema pallidum haemagglutination assay) as a treponemal test and RPR (rapid plasma reagin) as a non-treponemal test were the principally used assays. PLWH underwent syphilis screening at their first HIV clinical evaluation with both treponemal and non-treponemal tests. Patients with positive results received the appropriate supervised treatment. Screening was repeated annually (with an RPR test being used only in previously treated patients), or earlier in the case of reported symptoms or at-risk sexual intercourse. A thorough anamnesis and physical examination were performed in the case of a syphilis diagnosis to assess its stage, even performing a lumbar puncture according to current ongoing guidelines if needed [ 13 ]. All patients received appropriate treatment (mostly benzathine penicillin or doxycycline in the case of allergy). In HIV-negative individuals, indications for testing for syphilis infection in Italy include clinical suspicion, contact with syphilis, pregnant women and risk factors for sexually transmitted diseases. Follow-up visits were scheduled at 6 months and 12 months after treatment. During these visits, clinicians assessed risk factors for syphilis re-exposure and serological data were obtained to monitor the RPR titre trends. Patients with a serological non-response or a serofast status were asked for risk factors, and in doubtful cases, a new treatment was given.
2.4. Definitions
A first syphilis case was defined as a patient with positive treponemal and non-treponema tests without a previous history of treated syphilis infection whether in combination with clinical signs of syphilis or not. Reinfection was defined in patients having more than 2 diagnoses of syphilis infection during the study period in the case of having been previously diagnosed as having syphilis, having received adequate treatment and having demonstrated a seroreversion from negative to positive or a ≥4-fold increase in non-treponemal titre. Patients with undocumented treatment during the study period and patients with missing, incomplete or uncertain data were excluded from the study.
In accordance with the current literature, we considered patients with a complete seroreversion in RPR titres (from positive to negative) or with a ≥4-fold decline in nontreponemal antibody titres as serological responders [ 13 , 14 ]. Patients who, after an effective treatment, showed a ≤4-fold titre decline were defined as serological non-responders, whereas patients with a persistently reactive RPR titre despite adequate treatment and an initial ≥4-fold decline were defined as serofast.
2.5. Ethical Aspects
The study protocol received ethical approval from the Ethics Committee of the province of Brescia (code number NP 4847). All data were collected and analysed according to current Italian laws for the management of sensitive data and principles of the Declaration of Helsinki. The standard clinical practice at all healthcare services included providing thorough information and receiving verbal consent to any of the offered practices.
2.6. Statistical Analysis
Descriptive analysis of the characteristics of the two cohorts at baseline was performed. The median values and interquartile ranges (IQRs) were used to describe numerical variables, while the counts and percentages were employed for qualitative variables. A chi-square (χ2) test with p -values computed using Monte–Carlo simulations (B = 2000) or the Wilcoxon–Mann–Whitney test were used to compare the groups for categorical or continuous variables, respectively.
The number of reinfections was modelled using a generalised linear model (GLM) with a negative binomial family. The results are reported as incidence rate ratio (IRR) estimates and corresponding 95% confidence intervals (CIs 95%). Serological non-responses or serofast statuses were modelled as binary outcomes in a longitudinal setting using generalised linear mixed models (GLMMs) with a binomial family (also known as logistic regression). The results are reported as odds ratios (ORs) and corresponding 95% confidence intervals (CIs 95%). All tests were two-sided (apart from χ2), and a 5% significance level was assumed.
3.1. Prevalence of Syphilis Episodes in the Study Period
In the study period, 1859 syphilis episodes were recorded. A total of 827 patients were diagnosed with a first episode of syphilis infection (44.5%) and divided according to their HIV infection status ( Table 1 ). Between 2019 and 2021, we observed a decrease in first syphilis infection diagnoses among HIV-negative subjects. Approximately 1032 (55.5%) syphilis reinfections were recorded, especially in the HIV-positive population.
Number of first syphilis infections and reinfections per year during the study period.
Approximately 164 (19.8%) records regarding first syphilis infections were incomplete. Thus, 95 (11%) HIV-negative and 69 (8%) HIV-positive patients were excluded due to missing data ( Figure 1 ), whereas 650 (63%) subsequent episodes of syphilis infection were excluded due to patients being lost to follow-up. As shown in Figure 1 , 61 HIV-negative and 209 HIV-positive patients had at least 1 new episode of syphilis during the follow-up visits at 6 and/or 12 months. A total of 54 and 328 episodes of syphilis reinfection were recorded among HIV-negative and HIV-positive patients, respectively.

Study design (Ep. = episodes).
3.2. Demographic and Clinical Characteristics of Included Patients
The study included 663 patients, 316 (48%) HIV-negative and 347 (52%) HIV-positive patients with a median CD4 count of 295.5 cells/mcL (range 4 to 1038). As shown in Table 2 , syphilis was mostly diagnosed in males (508, 77%) with a median age of 39 years old (IQR, 12–83 years). Most patients were of European origin (522, 79%) and self-declared a homo/bisexual orientation (299, 45%). More than half of syphilis episodes were recorded during the late latent stage (424, 64%), followed by the secondary (107, 16%), primary (63, 10%) and early latent (53, 8%) stages. Neurosyphilis was observed in 16 (2%) episodes. Most syphilis episodes (426, 64%) were detected during follow-up/screening visits for other diseases (HIV, other STIs or partner tracing), whereas (237) 36% were detected due to the appearance of symptoms (skin rash, chancre or neurologic symptoms).
Demographic characteristics of the study population.
We found statistical differences between the HIV-positive group and the control group in several aspects of the demographic analysis. PLWH with syphilis infection were predominantly (260, 75%) homo/bisexual ( p < 0.001), while most heterosexuals with syphilis (184, 58%) were in the control group. Almost half (163, 53%) of HIV-negative syphilis infections were diagnosed during symptomatic stages, while, considering the longer median follow-up (88.9 months, p < 0.001), PLWH were diagnosed mainly with syphilis (278, 80%) due to screening/follow-up reasons during asymptomatic stages ( p < 0.001). Regarding syphilis reinfection, a significantly higher rate ( p < 0.001) was observed in the HIV-positive group (209, 60%), who had a higher rate of subsequent episodes (1 to 7), whereas sporadic (61, 19%) episodes of syphilis reinfections were recorded in the control group.
Among PLWH, the logistic regression model to assess factors associated with the number of syphilis reinfections showed a protective association with age (IRR 0.65, 95% CI 0.47–0.91 for range 40–50 years, p = 0.011 and IRR 0.55, 95% CI 0.35–0.86, p = 0.009 for age > 50 years), while being homosexual/bisexual increased the risk of syphilis reinfections (IRR 1.52, 95% CI 1.09, 2.18, p = 0.017). In our model, gender, geographical origin and CD4 nadir were not associated with an increased risk of syphilis reinfection in PLWH ( Table 3 ).
Generalised linear model to assess factors associated with the number of syphilis reinfections among PLWH.
1 IRR = incidence rate ratio, CI = confidence interval.
3.3. Serological Response to Treatment in Syphilis Reinfection
Among the patients with syphilis reinfection effectively treated according to their syphilis stage, no significant statistical difference was observed in the serological response between PLWH and HIV-negative patients at 6-month and 12-month follow-up visits ( p = 0.2 at 6 months, p = 0.1 at 12 months). Among PLWH, the serologic response and seroreversion rate increased over time, while the serological non-response rate decreased during the follow-up assessment at 6 and 12 months after treatment. Conversely, the serofast status rate was found to be similar at both the 6- and at 12-month follow-up in PLWH, without any significant difference with the control group ( Table 4 ).
Serological response to treatment after syphilis reinfection at 6- and 12-month follow-up (SNR = serological non-response).
Multivariate analysis was performed considering syphilis reinfection in the HIV-positive group. In our study, an RPR titre > 1:16 was an independent predictor (OR 2.26, 95% CI 1.14–4.51, p = 0.020) of serological non-response, regardless of sex, age, CD4 cell count at diagnosis or HIV viral load ( Table 5 ). On the other hand, a follow-up evaluation at 12 months rather than earlier (6 months) statistically reduced the risk of serological non-response in PLWH (OR 0.38, 95% CI 0.22–0.65, p < 0.001). Among all the risk factors considered, none was statistically associated with the serofast state ( Table 5 ).
Risk factors associated with a serological non-response and a serofast status in syphilis reinfection among people living with HIV.
1 CI = confidence interval.
4. Discussion
This was a large monocentric retrospective study including over 1800 episodes of syphilis infection describing a cohort of 663 people diagnosed with a first syphilis infection, dividing them into two groups according to their HIV status and focusing on serological response in syphilis reinfection among PLWH. As previously described, syphilis infection and homo/bisexual orientation were also often accompanied by HIV coinfection in our cohort [ 14 ]. Furthermore, the introduction of successful antiretroviral therapy and the general assumption among PLWH of U = U have induced an alarming decline in the adoption of safe sexual behaviours [ 10 ].
During the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) pandemic, community containment and social distancing measures might have affected the circulation of STDs. A recent monocentric study showed that despite the lockdown and the fear of SARS-CoV-2 infection, risky sexual activity has not diminished, nor has unprotected sexual intercourse among the increasing number of PrEP users (pre-exposure prophylaxis). Thus, the occurrence of syphilis has continued unabated [ 6 , 15 ]. However, in a COVID-19-prioritised era, an inevitably downscaled number of individuals seeking medical attention might also partially justify possible incidence reductions in STD diagnoses [ 16 ]. In our centre, a statistical difference was found in the annual trend of syphilis reinfections among HIV-positive and HIV-negative patients. The minimal non-significant decrease in diagnoses of syphilis among PLWH observed during 2020 and 2021 is also in line with the maintained continuum of care in PLWH with few missed visits, but with a reduction in new HIV diagnoses observed in our centre during the SARS-CoV-2 pandemic [ 17 , 18 ]. Interestingly, national epidemiological data report a 20% reduction in latent syphilis diagnoses in 2020 compared to 2019, and a 5% reduction in primary and secondary syphilis [ 19 ]. Further studies are needed to clarify the link between lockdown and sexual habits and the risk for syphilis.
Syphilis infection does not lead to immunity against reinfection, and repeated episodes of syphilis occur predominantly in PLWH, especially in an asymptomatic form, highlighting the crucial role of periodical screening [ 20 , 21 ]. In our centre, PLWH are screened for syphilis at least annually, regardless of their symptoms or risk factors, allowing for an earlier diagnosis and intercepting repeated episodes. In our cohort, syphilis reinfections in PLWH ranged from one to seven episodes. It is known that MSM with HIV infection present high rates of syphilis coinfection and reinfection [ 22 ]. In particular, MSM report a syphilis reinfection rate higher than one in five men (71/323; 22%), while in PLWH, approximately 21.8% of coinfected patients experience a reinfection [ 23 , 24 ]. The higher percentage of syphilis among HIV-negative females with respect to HIV-positive females (44% vs. 4%) in our cohort reflects an occasional diagnosis of syphilis during the pregnancy screening programs.
A recent study with a large cohort showed that factors associated with more than one episode of syphilis were sex (male) (OR = 4.28), age (OR = 1.02), homosexual/bisexual orientation (OR = 2.29) and absence of STI symptoms at the time of syphilis diagnosis (OR = 1.70) [ 25 ]. The extent of sexually risky behaviour over time is the strongest risk factor for repeated syphilis episodes when compared to other indicators (antiretroviral regimen or immunological status) [ 26 ]. The identification of at-risk adults and adolescents is crucial to improve syphilis screening strategies, as recommended by the latest USPSTF (US Preventive Services Task Force) statements [ 27 , 28 , 29 ]. While the interpretation of the indirect methods for syphilis diagnosis is relatively straightforward in patients without a prior history of syphilis, it becomes more complex in the case of reinfections, as treponemal antibodies mostly remain positive for their entire life cycle, tests lack sensitivity in early infection (as well as when patients are contagious), and non-treponemal titres often lead to difficult-to-interpret serological responses after treatment [ 29 ].
Although there are no controlled clinical trials focused on optimising the treatment of syphilis, all our patients were treated following literature recommendations based on laboratory results, expert opinions, clinical cases and experience [ 30 ]. HIV infection did not influence the treatment regimen used and, in line with the most recent literature reviews, no additional antibiotic doses were used in the case of anomalous serologic responses [ 31 , 32 ].
The main finding of our study regards the serological response to treatment in syphilis reinfections; no significant statistical difference was observed in the serological response between PLWH and HIV-negative patients. Like other authors, we were unable to find an association between the CD4 count, HIV viral load and serological response [ 33 , 34 , 35 ]. Serological response to treatment in coinfection syphilis/HIV is controversial as unusual serologic responses might be recorded [ 36 ]. However, our results are consistent with the current literature, since the majority of PLWH infected with syphilis achieved an adequate serologic response [ 36 ]. PLWH may just take longer to reach an adequate serologic response after treatment [ 36 ]; in our study, seroreversion and serological non-response rates in PLWH raised and decreased, respectively, over time. HIV-related immunodeficiency was hypothesised as the cause of this controversial response [ 37 ]. In our study, an apparently overall better serological response was found in PLWH; the primary explanation for this is that PLWH are chronically evaluated in our centre with scheduled visits every 6 months. This increases the detection rate of syphilis infection at earlier stages, which is linked to a better serological response [ 38 ].
A decline in the serofast status rate over time was not confirmed in our analysis. However, there is a paucity of information about the serofast status in the literature. In a recent analysis, HIV coinfection was associated with a slower serological cure, and while just 37% seroreverted within a year, more than 60% still had a positive RPR after 1 year of follow-up [ 39 ]. Here, the serofast status rate was found to be similar at 6 and 12 months, but this does not mean that this trend must be confirmed in a more prolonged observational study (at a hypothetical 18-month or 24-month follow-up visit). In our clinical practice, patients with a serofast status or a serological non-response after treatment are asked about risk factors for new syphilis exposure and, in doubtful cases, a new treatment is given. It is univocally stated that neither the choice of therapy nor the posology (single dose vs. three doses of intramuscular benzathine benzylpenicillin) in PLWH has any influence on the serofast state in early syphilis [ 40 ].
The risk factors for serofast status in HIV coinfection are only partially understood, especially in the case of syphilis reinfections [ 40 ]. As previously described, in our analysis, the serofast state in subsequent episodes of syphilis infection was not statistically associated with gender, age, CD4 at diagnosis or HIV-RNA or RPR titre in PLWH [ 41 ]. Curiously, baseline RPR titres ≤ 1:16, CD4 counts < 350 cells/µL, untreated HIV infection and a previous syphilis history are considered predictors for persistent non-treponemal titres [ 42 , 43 ].
Lastly, the multivariate analysis carried out among syphilis reinfections in PLWH showed that both a high RPR titre (>1:16) and an earlier follow-up evaluation (6 months rather than 12 months) after appropriate treatment are independent risk factors for serological non-response. In PLWH, repeated episodes of syphilis are associated with higher non-treponemal titres, influencing the serological outcome after treatment, whereas an adequate titre response is generally obtained earlier in HIV-negative people [ 37 ]. In addition, patients with a lower baseline RPR titre during syphilis infection seem to require a longer period to achieve a serological response (252 days for RPR titre ≤1:8, 78 days for RPR titres from 1:16 to 1:32 and 53 days for RPR titres ≥1:64, respectively; p < 0.001). It is unlikely that an earlier evaluation (at 6 months after treatment) is associated with complete seroreversion [ 39 ]. Although RPR is routinely used to monitor for a syphilis reinfection, our results suggest a possible role of a high RPR titre (>1:16) as a predictor of serological non-response. The ab initio role of the RPR titre in syphilis management is controversial, and further studies are needed to confirm our finding.
The findings of our study should be seen in light of some limitations. First, it goes without saying that retrospective studies are subject to innate bias. The data were collected retrospectively from the patients’ electronic medical records, and in some cases, they were lacking. Second, the study was carried out in a single healthcare centre, and the conclusions drawn might not be representative of the general population. In our database, data for sexual risk behaviours were not always recorded, and a proportion of patients, especially in the HIV-negative group, were lost to follow-up, reducing the number of evaluable data on treatment response. Lastly, 24-month follow-up visits are routinely scheduled in our centre, but the available data were not sufficient to be considered in this study. Nonetheless, the study’s main strength is the large sample size and the comparability between the HIV-positive group and the control group. Moreover, a single health centre study ensures a unique interpretation of the most recent guidelines, resulting in a specific and shared way of treating patients and scheduling follow-up visits. Our findings should, therefore, be confirmed by further studies.
5. Conclusions
Syphilis rates have continued to rise in recent years. To control this epidemic, patients at risk must follow up with periodical screening, and tests must be correctly interpreted to provide appropriate treatment. Interpretations of syphilis serology can be challenging, and misinterpretation may result in undertreatment or overtreatment. HIV infection status should not be considered a factor influencing the choice of treatment or altering the interpretation of the serological results, even in the case of repeated episodes of syphilis. Regarding the serological response to treatment, PLWH probably need more time to obtain an adequate response, once more confirming the importance of chronic follow-up both to assess the response to treatment and to track reinfection earlier.
Acknowledgments
Not applicable.
Funding Statement
This paper was supported with an unconditional grant from GILEAD.
Author Contributions
E.Q.-R.: Conceptualization and supervision; V.M., G.T. and E.Q.-R.: Methodology and original draft preparation; S.C.: formal statistical analysis; F.V.: Data curation; M.G.: Data collection and supervision; V.M., G.T., S.S., M.D.A., S.C., M.G., F.V., E.F., A.M., F.C. and E.Q.-R.: software, validation, investigation, resources, and writing—review & editing. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki and approved by the Ethics Committee of or Hospital (code number NP 4847).
Informed Consent Statement
Data availability statement, conflicts of interest.
The authors declare no conflict of interest.
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.

IMAGES
VIDEO
COMMENTS
Tertiary (late) syphilis is slowly progressive and may affect any organ. The disease is generally not thought to be infectious at this stage. Manifestations may include the following: Impaired balance, paresthesias, incontinence, and impotence. Focal neurologic findings, including sensorineural hearing and vision loss.
Syphilis is a systemic bacterial infection caused by the spirochete Treponema pallidum. Due to its many protean clinical manifestations, it has been named the "great imitator and mimicker." The origin of syphilis has been controversial and under great debate, and many theories have been postulated regarding this.
The rash often starts on the trunk of the body. That includes the chest, stomach area, pelvis and back. In time, it also could appear on the limbs, the palms of the hands and the soles of the feet. Along with the rash, you may have symptoms such as: Wartlike sores in the mouth or genital area. Hair loss.
If you are pregnant and have syphilis, you can give the infection to your unborn baby. Having syphilis can lead to a low-birth-weight-baby. It can make it more likely you will deliver your baby too early or stillborn (a baby born dead). To protect your baby, you should receive syphilis testing at least once during your pregnancy. Receive ...
Introduction. Syphilis is caused by the bacterium Treponema pallidum subspecies pallidum. 1 This motile, gram-negative spirochete can be transmitted both sexually and from mother to child, and can invade virtually any organ or structure in the human body. The disease, which should be considered systemic throughout, is characterised by overlapping clinical stages and a relapsing and remitting ...
Neurosyphilis. Can occur at any stage of syphilis. Early manifestations (months to years after infection) Cranial nerve dysfunction, meningitis, stroke, AMS, hearing or vision changes. Otosyphilis - hearing loss w/wo tinnitus. Ocular - range of visual symptoms. Late manifestations (10-30 years after infection) Tabes dorsalis and general ...
Introduction. Syphilis is caused by the bacterium Treponema pallidum subspecies pallidum. 1 This motile, gram-negative spirochete can be transmitted both sexually and from mother to child, and can invade virtually any organ or structure in the human body. The disease, which should be considered systemic throughout, is characterised by overlapping clinical stages and a relapsing and remitting ...
Diagnosis and treatment of syphilis are challenging because of its variable clinical presentation and course and the lack of definitive tests of cure after treatment. This review of the most recent literature on the epidemiology, clinical manifestations, current diagnosis, and treatment of syphilis is focused toward clinicians who treat patients with this disease. Syphilis coinfection with ...
by positive syphilis serology with no clinical manifestations. Latent syphilis is often divided into two phases: early latent syphilis is defined as infection for less than two years while late latent syphilis is the presence of the disease for two years or more. Sexual transmission typically occurs during primary, secondary or early latent ...
Syphilis remains common worldwide, and since the late 1990s infectious early syphilis has re-emerged as an important disease in western Europe, including the United Kingdom. 1 The clinical presentation of both early and late syphilis is diverse, and patients may present to a wide range of services and clinicians, including general practitioners. Until recently many doctors will have had ...
Some studies suggest that infection with HIV may affect the clinical presentation of syphilis, as atypical or multiple genital lesions are more apparent, and accelerated progression of syphilis may be seen in people with advanced immunosuppression. 16,17,19-22 Primary or secondary syphilis also may cause a transient decrease in CD4 T lymphocyte ...
Syphilis is an infectious disease caused by the spirochete bacterium Treponema pallidum. It can be transmitted sexually, during pregnancy and via blood transfusion. ... With syphilis infections rising, it is essential to be aware of the clinical presentation and management, as syphilis has a safe, effective and curative treatment. However, if ...
The clinical presentation of syphilis does not differ between pregnant and nonpregnant women. Primary syphilis is characterized by one or more indurated chancres at the site of inoculation, which ...
common in the United States and affects the initial presentation, disease course, diagnosis, and treatment of syphilis. Of particular consequence is the effect of human immunodeficiency virus on the clinical diagnosis, prevalence, and course of neurosyphilis, one of the most serious consequences of syphilis infection. Mayo Clin Proc. 2007;82(9 ...
Syphilis infection causes an ulceration in the mucous membrane, thus greatly increasing the risk of also acquiring or transmitting HIV. By the end of 2019, 1,059,784 individuals in the United States and dependent areas were living with HIV. ... The clinical presentation of untreated syphilis varies according to its stage. These 4 stages are ...
Clinical features of secondary syphilis typically appear 4 to 8 weeks after primary syphilis infection, but they may also occur up to 6 months later. The presentation of secondary syphilis is diverse. Hematogenous dissemination in secondary syphilis affects different organs.
Importance Syphilis is a sexually transmitted infection that can progress through different stages (primary, secondary, latent, and tertiary) and cause serious health problems if left untreated. Reported cases of primary and secondary syphilis in the US increased from a record low of 2.1 cases per 100 000 population in 2000 and 2001 to 11.9 cases per 100 000 population in 2019.
1.2.3. Clinical Presentation. The natural history of syphilis is characterized by the cyclical alternation of symptomatic and asymptomatic periods. The first year after infection is the early stage of syphilis, which is divided into primary, secondary, and transient stages.
We aimed to gain insights into the clinical and serological presentation of reinfected men living with HIV and to evaluate diagnostic criteria for syphilis reinfection. Methods: We conducted a retrospective cohort study of 259 HIV-positive men diagnosed with syphilis between January 1999 and September 2015 at the University Hospital Zurich.
Clinical Presentation. Syphilis Syphilis Syphilis is a bacterial infection caused by the spirochete Treponema pallidum pallidum (T. p. pallidum), which is usually spread through sexual contact. Syphilis has 4 clinical stages: primary, secondary, latent, and tertiary. Syphilis is a multistage disease. Patients Patients Individuals participating in the health care system for the purpose of ...
From 2012 to 2021, congenital syphilis cases increased by 755% 2 . In the United States, in 2022 alone, there were 3,755 cases of congenital syphilis. According to the CDC, 88% of congenital syphilis cases in 2022 could have been prevented with timely screening and treatment 2. Notably, two in five infants with congenital syphilis were born to ...
Syphilis is a serious infection. If untreated, it can damage the heart and brain and can cause blindness, deafness, and paralysis. When transmitted and not treated during pregnancy, it can cause miscarriage, lifelong medical issues, and even infant death. It is curable with antibiotics, and screening, early diagnosis and treatment are essential ...
Moreover, HIV infection may modulate the clinical presentation and the clinical and serologic response to syphilis treatment [3,4,5,6]. In 2017, the annual rate of primary and secondary syphilis in the United States was 11% higher than in 2016: more than 60% of infected individuals were MSM, of whom 46% were people living with HIV infection ...
Congenital syphilis, a preventable and deadly disease, has witnessed an alarming resurgence in the US in recent years, posing a vital public health challenge. Historically, effective prevention and treatment strategies led to a decline in congenital syphilis, and some believed that it could be eradicated. However, inadequate prenatal care, limited access to healthcare services, and gaps in ...
meeting April 12, 2024. 1 Landgren O, Gormley N, Turley D, Owen RG, Rawstron A, Paiva B, Barnett D, Arroz M, Wallace P, Durie B, Yuan C, Dogan A, Stetler-Stevenson M, Marti GE. Flow cytometry ...
syphilis, the clinical manifestations of syphilis are similar to those observed in people without HIV. Some studies suggest that infection with HIV may affect the clinical presentation of syphilis, as atypical or multiple genital lesions are more apparent, and accelerated progression of syphilis may be seen in people with advanced ...
sk factors among a selection of high-risk MSM without symptomatic urethritis attending a men's health clinic in Johannesburg, South Africa. Methods A cross-sectional study was conducted in 2022. Enrolled clients self-reported demographic, sexual behavioral risks, and clinical information. Client or clinician-collected rectal and pharyngeal swabs were tested for Neisseria gonorrhoeae, Chlamydia ...
Syphilis is a multisystem infection caused by the spirochete Treponema pallidum. ... The clinical presentation varies and is determined by the structures involved and duration of infection. The absence of gold-standard tests and the broad clinical features contribute to difficulties in diagnosis. The laboratory diagnosis of neurosyphilis ...
Cutaneous leishmaniasis (CL) is a neglected tropical skin disease, caused by the protozoan parasite Leishmania (L.). It is endemic to 90 countries and causes >200,000 new infections each year. In Ethiopia, CL is mainly caused by L. aethiopica and can present in different clinical forms: localised cutaneous leishmaniasis (LCL); mucocutaneous leishmaniasis (MCL), where the mucosa of the nose and ...
Coinfection is dangerous because HIV infection may modulate the clinical presentation and the serologic response to syphilis treatment . PLWH with a syphilis infection seem to have a higher risk of developing neurosyphilis and mount an abnormal serological response [8,9]. Many diagnostic and therapeutic challenges remain, as there are currently ...