- Research article
- Open access
- Published: 10 April 2021

The role of artificial intelligence in healthcare: a structured literature review
- Silvana Secinaro 1 ,
- Davide Calandra 1 ,
- Aurelio Secinaro 2 ,
- Vivek Muthurangu 3 &
- Paolo Biancone 1
BMC Medical Informatics and Decision Making volume 21 , Article number: 125 ( 2021 ) Cite this article
164k Accesses
313 Citations
28 Altmetric
Metrics details
Background/Introduction
Artificial intelligence (AI) in the healthcare sector is receiving attention from researchers and health professionals. Few previous studies have investigated this topic from a multi-disciplinary perspective, including accounting, business and management, decision sciences and health professions.
The structured literature review with its reliable and replicable research protocol allowed the researchers to extract 288 peer-reviewed papers from Scopus. The authors used qualitative and quantitative variables to analyse authors, journals, keywords, and collaboration networks among researchers. Additionally, the paper benefited from the Bibliometrix R software package.
The investigation showed that the literature in this field is emerging. It focuses on health services management, predictive medicine, patient data and diagnostics, and clinical decision-making. The United States, China, and the United Kingdom contributed the highest number of studies. Keyword analysis revealed that AI can support physicians in making a diagnosis, predicting the spread of diseases and customising treatment paths.
Conclusions
The literature reveals several AI applications for health services and a stream of research that has not fully been covered. For instance, AI projects require skills and data quality awareness for data-intensive analysis and knowledge-based management. Insights can help researchers and health professionals understand and address future research on AI in the healthcare field.
Peer Review reports
Artificial intelligence (AI) generally applies to computational technologies that emulate mechanisms assisted by human intelligence, such as thought, deep learning, adaptation, engagement, and sensory understanding [ 1 , 2 ]. Some devices can execute a role that typically involves human interpretation and decision-making [ 3 , 4 ]. These techniques have an interdisciplinary approach and can be applied to different fields, such as medicine and health. AI has been involved in medicine since as early as the 1950s, when physicians made the first attempts to improve their diagnoses using computer-aided programs [ 5 , 6 ]. Interest and advances in medical AI applications have surged in recent years due to the substantially enhanced computing power of modern computers and the vast amount of digital data available for collection and utilisation [ 7 ]. AI is gradually changing medical practice. There are several AI applications in medicine that can be used in a variety of medical fields, such as clinical, diagnostic, rehabilitative, surgical, and predictive practices. Another critical area of medicine where AI is making an impact is clinical decision-making and disease diagnosis. AI technologies can ingest, analyse, and report large volumes of data across different modalities to detect disease and guide clinical decisions [ 3 , 8 ]. AI applications can deal with the vast amount of data produced in medicine and find new information that would otherwise remain hidden in the mass of medical big data [ 9 , 10 , 11 ]. These technologies can also identify new drugs for health services management and patient care treatments [ 5 , 6 ].
Courage in the application of AI is visible through a search in the primary research databases. However, as Meskò et al. [ 7 ] find, the technology will potentially reduce care costs and repetitive operations by focusing the medical profession on critical thinking and clinical creativity. As Cho et al. and Doyle et al. [ 8 , 9 ] add, the AI perspective is exciting; however, new studies will be needed to establish the efficacy and applications of AI in the medical field [ 10 ].
Our paper will also concentrate on AI strategies for healthcare from the accounting, business, and management perspectives. The authors used the structured literature review (SLR) method for its reliable and replicable research protocol [ 11 ] and selected bibliometric variables as sources of investigation. Bibliometric usage enables the recognition of the main quantitative variables of the study stream [ 12 ]. This method facilitates the detection of the required details of a particular research subject, including field authors, number of publications, keywords for interaction between variables (policies, properties and governance) and country data [ 13 ]. It also allows the application of the science mapping technique [ 14 ]. Our paper adopted the Bibliometrix R package and the biblioshiny web interface as tools of analysis [ 14 ].
The investigation offers the following insights for future researchers and practitioners:
bibliometric information on 288 peer-reviewed English papers from the Scopus collection.
Identification of leading journals in this field, such as Journal of Medical Systems, Studies in Health Technology and Informatics, IEEE Journal of Biomedical and Health Informatics, and Decision Support Systems.
Qualitative and quantitative information on authors’ Lotka’s law, h-index, g-index, m-index, keyword, and citation data.
Research on specific countries to assess AI in the delivery and effectiveness of healthcare, quotes, and networks within each region.
A topic dendrogram study that identifies five research clusters: health services management, predictive medicine, patient data, diagnostics, and finally, clinical decision-making.
An in-depth discussion that develops theoretical and practical implications for future studies.
The paper is organised as follows. Section 2 lists the main bibliometric articles in this field. Section 3 elaborates on the methodology. Section 4 presents the findings of the bibliometric analysis. Section 5 discusses the main elements of AI in healthcare based on the study results. Section 6 concludes the article with future implications for research.
Related works and originality
As suggested by Zupic and Čater [ 15 ], a research stream can be evaluated with bibliometric methods that can introduce objectivity and mitigate researcher bias. For this reason, bibliometric methods are attracting increasing interest among researchers as a reliable and impersonal research analytical approach [ 16 , 17 ]. Recently, bibliometrics has been an essential method for analysing and predicting research trends [ 18 ]. Table 1 lists other research that has used a similar approach in the research stream investigated.
The scientific articles reported show substantial differences in keywords and research topics that have been previously studied. The bibliometric analysis of Huang et al. [ 19 ] describes rehabilitative medicine using virtual reality technology. According to the authors, the primary goal of rehabilitation is to enhance and restore functional ability and quality of life for patients with physical impairments or disabilities. In recent years, many healthcare disciplines have been privileged to access various technologies that provide tools for both research and clinical intervention.
Hao et al. [ 20 ] focus on text mining in medical research. As reported, text mining reveals new, previously unknown information by using a computer to automatically extract information from different text resources. Text mining methods can be regarded as an extension of data mining to text data. Text mining is playing an increasingly significant role in processing medical information. Similarly, the studies by dos Santos et al. [ 21 ] focus on applying data mining and machine learning (ML) techniques to public health problems. As stated in this research, public health may be defined as the art and science of preventing diseases, promoting health, and prolonging life. Using data mining and ML techniques, it is possible to discover new information that otherwise would be hidden. These two studies are related to another topic: medical big data. According to Liao et al. [ 22 ], big data is a typical “buzzword” in the business and research community, referring to a great mass of digital data collected from various sources. In the medical field, we can obtain a vast amount of data (i.e., medical big data). Data mining and ML techniques can help deal with this information and provide helpful insights for physicians and patients. More recently, Choudhury et al. [ 23 ] provide a systematic review on the use of ML to improve the care of elderly patients, demonstrating eligible studies primarily in psychological disorders and eye diseases.
Tran et al. [ 2 ] focus on the global evolution of AI research in medicine. Their bibliometric analysis highlights trends and topics related to AI applications and techniques. As stated in Connelly et al.’s [ 24 ] study, robot-assisted surgeries have rapidly increased in recent years. Their bibliometric analysis demonstrates how robotic-assisted surgery has gained acceptance in different medical fields, such as urological, colorectal, cardiothoracic, orthopaedic, maxillofacial and neurosurgery applications. Additionally, the bibliometric analysis of Guo et al. [ 25 ] provides an in-depth study of AI publications through December 2019. The paper focuses on tangible AI health applications, giving researchers an idea of how algorithms can help doctors and nurses. A new stream of research related to AI is also emerging. In this sense, Choudhury and Asan’s [ 26 ] scientific contribution provides a systematic review of the AI literature to identify health risks for patients. They report on 53 studies involving technology for clinical alerts, clinical reports, and drug safety. Considering the considerable interest within this research stream, this analysis differs from the current literature for several reasons. It aims to provide in-depth discussion, considering mainly the business, management, and accounting fields and not dealing only with medical and health profession publications.
Additionally, our analysis aims to provide a bibliometric analysis of variables such as authors, countries, citations and keywords to guide future research perspectives for researchers and practitioners, as similar analyses have done for several publications in other research streams [ 15 , 16 , 27 ]. In doing so, we use a different database, Scopus, that is typically adopted in social sciences fields. Finally, our analysis will propose and discuss a dominant framework of variables in this field, and our analysis will not be limited to AI application descriptions.
Methodology
This paper evaluated AI in healthcare research streams using the SLR method [ 11 ]. As suggested by Massaro et al. [ 11 ], an SLR enables the study of the scientific corpus of a research field, including the scientific rigour, reliability and replicability of operations carried out by researchers. As suggested by many scholars, the methodology allows qualitative and quantitative variables to highlight the best authors, journals and keywords and combine a systematic literature review and bibliometric analysis [ 27 , 28 , 29 , 30 ]. Despite its widespread use in business and management [ 16 , 31 ], the SLR is also used in the health sector based on the same philosophy through which it was originally conceived [ 32 , 33 ]. A methodological analysis of previously published articles reveals that the most frequently used steps are as follows [ 28 , 31 , 34 ]:
defining research questions;
writing the research protocol;
defining the research sample to be analysed;
developing codes for analysis; and
critically analysing, discussing, and identifying a future research agenda.
Considering the above premises, the authors believe that an SLR is the best method because it combines scientific validity, replicability of the research protocol and connection between multiple inputs.
As stated by the methodological paper, the first step is research question identification. For this purpose, we benefit from the analysis of Zupic and Čater [ 15 ], who provide several research questions for future researchers to link the study of authors, journals, keywords and citations. Therefore, RQ1 is “What are the most prominent authors, journal keywords and citations in the field of the research study?” Additionally, as suggested by Haleem et al. [ 35 ], new technologies, including AI, are changing the medical field in unexpected timeframes, requiring studies in multiple areas. Therefore, RQ2 is “How does artificial intelligence relate to healthcare, and what is the focus of the literature?” Then, as discussed by Massaro et al. [ 36 ], RQ3 is “What are the research applications of artificial intelligence for healthcare?”.
The first research question aims to define the qualitative and quantitative variables of the knowledge flow under investigation. The second research question seeks to determine the state of the art and applications of AI in healthcare. Finally, the third research question aims to help researchers identify practical and theoretical implications and future research ideas in this field.
The second fundamental step of the SLR is writing the research protocol [ 11 ]. Table 2 indicates the currently known literature elements, uniquely identifying the research focus, motivations and research strategy adopted and the results providing a link with the following points. Additionally, to strengthen the analysis, our investigation benefits from the PRISMA statement methodological article [ 37 ]. Although the SLR is a validated method for systematic reviews and meta-analyses, we believe that the workflow provided may benefit the replicability of the results [ 37 , 38 , 39 , 40 ]. Figure 1 summarises the researchers’ research steps, indicating that there are no results that can be referred to as a meta-analysis.
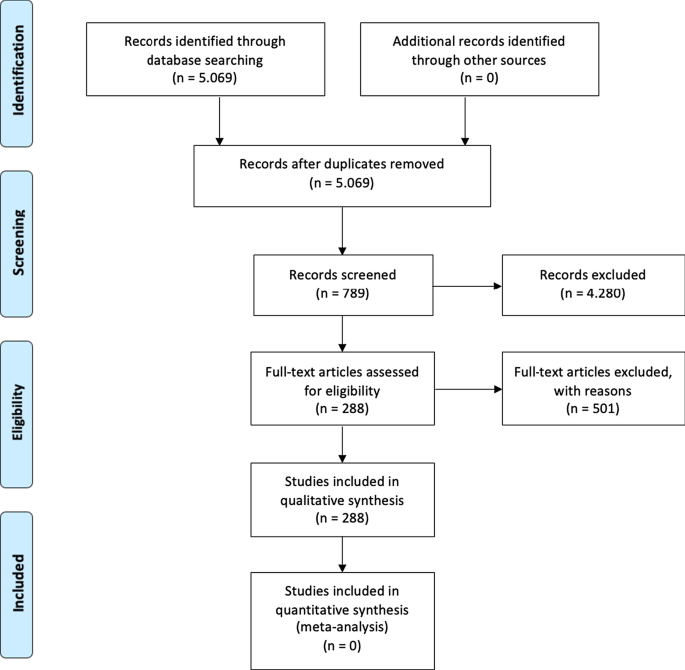
Source : Authors’ elaboration on Liberati et al. [ 37 ]
PRISMA workflow.
The third step is to specify the search strategy and search database. Our analysis is based on the search string “Artificial Intelligence” OR “AI” AND “Healthcare” with a focus on “Business, Management, and Accounting”, “Decision Sciences”, and “Health professions”. As suggested by [ 11 , 41 ] and motivated by [ 42 ], keywords can be selected through a top-down approach by identifying a large search field and then focusing on particular sub-topics. The paper uses data retrieved from the Scopus database, a multi-disciplinary database, which allowed the researchers to identify critical articles for scientific analysis [ 43 ]. Additionally, Scopus was selected based on Guo et al.’s [ 25 ] limitations, which suggest that “future studies will apply other databases, such as Scopus, to explore more potential papers” . The research focuses on articles and reviews published in peer-reviewed journals for their scientific relevance [ 11 , 16 , 17 , 29 ] and does not include the grey literature, conference proceedings or books/book chapters. Articles written in any language other than English were excluded [ 2 ]. For transparency and replicability, the analysis was conducted on 11 January 2021. Using this research strategy, the authors retrieved 288 articles. To strengthen the study's reliability, we publicly provide the full bibliometric extract on the Zenodo repository [ 44 , 45 ].
The fourth research phase is defining the code framework that initiates the analysis of the variables. The study will identify the following:
descriptive information of the research area;
source analysis [ 16 ];
author and citation analysis [ 28 ];
keywords and network analysis [ 14 ]; and
geographic distribution of the papers [ 14 ].
The final research phase is the article’s discussion and conclusion, where implications and future research trends will be identified.
At the research team level, the information is analysed with the statistical software R-Studio and the Bibliometrix package [ 15 ], which allows scientific analysis of the results obtained through the multi-disciplinary database.
The analysis of bibliometric results starts with a description of the main bibliometric statistics with the aim of answering RQ1, What are the most prominent authors, journal keywords and citations in the field of the research study?, and RQ2, How does artificial intelligence relate to healthcare, and what is the focus of the literature? Therefore, the following elements were thoroughly analysed: (1) type of document; (2) annual scientific production; (3) scientific sources; (4) source growth; (5) number of articles per author; (6) author’s dominance ranking; (7) author’s h-index, g-index, and m-index; (8) author’s productivity; (9) author’s keywords; (10) topic dendrogram; (11) a factorial map of the document with the highest contributions; (12) article citations; (13) country production; (14) country citations; (15) country collaboration map; and (16) country collaboration network.
Main information
Table 3 shows the information on 288 peer-reviewed articles published between 1992 and January 2021 extracted from the Scopus database. The number of keywords is 946 from 136 sources, and the number of keywords plus, referring to the number of keywords that frequently appear in an article’s title, was 2329. The analysis period covered 28 years and 1 month of scientific production and included an annual growth rate of 5.12%. However, the most significant increase in published articles occurred in the past three years (please see Fig. 2 ). On average, each article was written by three authors (3.56). Finally, the collaboration index (CI), which was calculated as the total number of authors of multi-authored articles/total number of multi-authored articles, was 3.97 [ 46 ].
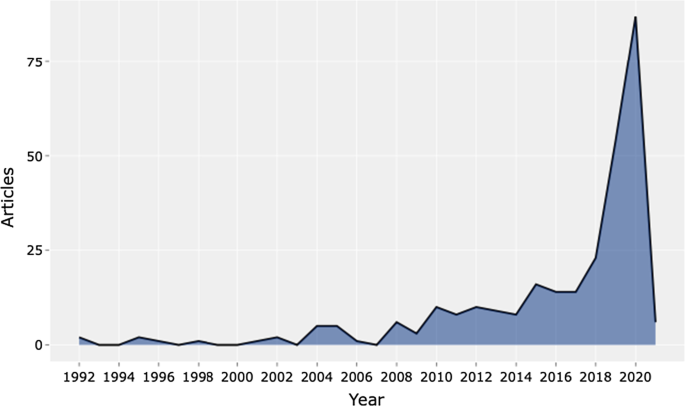
Source : Authors’ elaboration
Annual scientific production.
Table 4 shows the top 20 sources related to the topic. The Journal of Medical Systems is the most relevant source, with twenty-one of the published articles. This journal's main issues are the foundations, functionality, interfaces, implementation, impacts, and evaluation of medical technologies. Another relevant source is Studies in Health Technology and Informatics, with eleven articles. This journal aims to extend scientific knowledge related to biomedical technologies and medical informatics research. Both journals deal with cloud computing, machine learning, and AI as a disruptive healthcare paradigm based on recent publications. The IEEE Journal of Biomedical and Health Informatics investigates technologies in health care, life sciences, and biomedicine applications from a broad perspective. The next journal, Decision Support Systems, aims to analyse how these technologies support decision-making from a multi-disciplinary view, considering business and management. Therefore, the analysis of the journals revealed that we are dealing with an interdisciplinary research field. This conclusion is confirmed, for example, by the presence of purely medical journals, journals dedicated to the technological growth of healthcare, and journals with a long-term perspective such as futures.
The distribution frequency of the articles (Fig. 3 ) indicates the journals dealing with the topic and related issues. Between 2008 and 2012, a significant growth in the number of publications on the subject is noticeable. However, the graph shows the results of the Loess regression, which includes the quantity and publication time of the journal under analysis as variables. This method allows the function to assume an unlimited distribution; that is, feature can consider values below zero if the data are close to zero. It contributes to a better visual result and highlights the discontinuity in the publication periods [ 47 ].
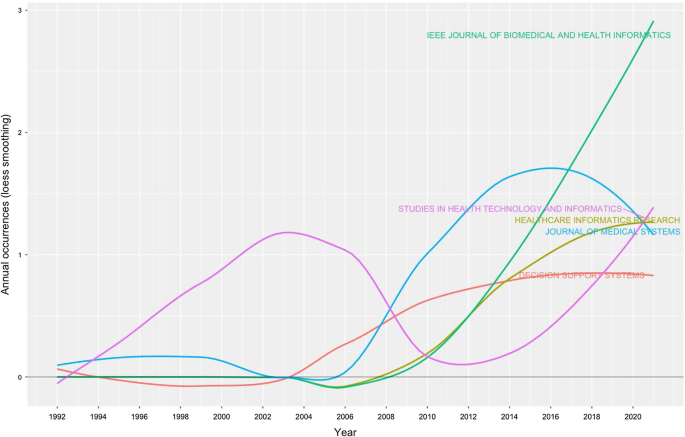
Source growth. Source : Authors’ elaboration
Finally, Fig. 4 provides an analytical perspective on factor analysis for the most cited papers. As indicated in the literature [ 48 , 49 ], using factor analysis to discover the most cited papers allows for a better understanding of the scientific world’s intellectual structure. For example, our research makes it possible to consider certain publications that effectively analyse subject specialisation. For instance, Santosh’s [ 50 ] article addresses the new paradigm of AI with ML algorithms for data analysis and decision support in the COVID-19 period, setting a benchmark in terms of citations by researchers. Moving on to the application, an article by Shickel et al. [ 51 ] begins with the belief that the healthcare world currently has much health and administrative data. In this context, AI and deep learning will support medical and administrative staff in extracting data, predicting outcomes, and learning medical representations. Finally, in the same line of research, Baig et al. [ 52 ], with a focus on wearable patient monitoring systems (WPMs), conclude that AI and deep learning may be landmarks for continuous patient monitoring and support for healthcare delivery.
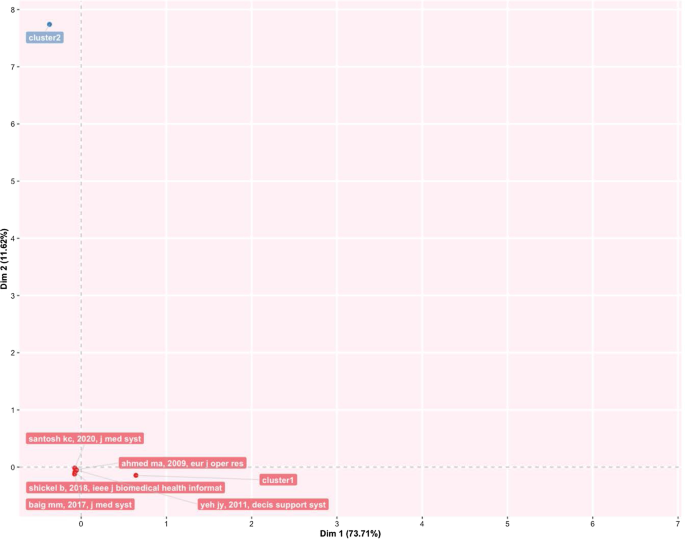
Factorial map of the most cited documents.
This section identifies the most cited authors of articles on AI in healthcare. It also identifies the authors’ keywords, dominance factor (DF) ranking, h-index, productivity, and total number of citations. Table 5 identifies the authors and their publications in the top 20 rankings. As the table shows, Bushko R.G. has the highest number of publications: four papers. He is the editor-in-chief of Future of Health Technology, a scientific journal that aims to develop a clear vision of the future of health technology. Then, several authors each wrote three papers. For instance, Liu C. is a researcher active in the topic of ML and computer vision, and Sharma A. from Emory University Atlanta in the USA is a researcher with a clear focus on imaging and translational informatics. Some other authors have two publications each. While some authors have published as primary authors, most have published as co-authors. Hence, in the next section, we measure the contributory power of each author by investigating the DF ranking through the number of elements.
Authors’ dominance ranking
The dominance factor (DF) is a ratio measuring the fraction of multi-authored articles in which an author acts as the first author [ 53 ]. Several bibliometric studies use the DF in their analyses [ 46 , 54 ]. The DF ranking calculates an author’s dominance in producing articles. The DF is calculated by dividing the number of an author’s multi-authored papers as the first author (Nmf) by the author's total number of multi-authored papers (Nmt). This is omitted in the single-author case due to the constant value of 1 for single-authored articles. This formulation could lead to some distortions in the results, especially in fields where the first author is entered by surname alphabetical order [ 55 ].
The mathematical equation for the DF is shown as:
Table 6 lists the top 20 DF rankings. The data in the table show a low level of articles per author, either for first-authored or multi-authored articles. The results demonstrate that we are dealing with an emerging topic in the literature. Additionally, as shown in the table, Fox J. and Longoni C. are the most dominant authors in the field.
Authors’ impact
Table 7 shows the impact of authors in terms of the h-index [ 56 ] (i.e., the productivity and impact of citations of a researcher), g-index [ 57 ] (i.e., the distribution of citations received by a researcher's publications), m-index [ 58 ] (i.e., the h-index value per year), total citations, total paper and years of scientific publication. The H-index was introduced in the literature as a metric for the objective comparison of scientific results and depended on the number of publications and their impact [ 59 ]. The results show that the 20 most relevant authors have an h-index between 2 and 1. For the practical interpretation of the data, the authors considered data published by the London School of Economics [ 60 ]. In the social sciences, the analysis shows values of 7.6 for economic publications by professors and researchers who had been active for several years. Therefore, the youthfulness of the research area has attracted young researchers and professors. At the same time, new indicators have emerged over the years to diversify the logic of the h-index. For example, the g-index indicates an author's impact on citations, considering that a single article can generate these. The m-index, on the other hand, shows the cumulative value over the years.
The analysis, also considering the total number of citations, the number of papers published and the year of starting to publish, thus confirms that we are facing an expanding research flow.
Authors’ productivity
Figure 5 shows Lotka’s law. This mathematical formulation originated in 1926 to describe the publication frequency by authors in a specific research field [ 61 ]. In practice, the law states that the number of authors contributing to research in a given period is a fraction of the number who make up a single contribution [ 14 , 61 ].
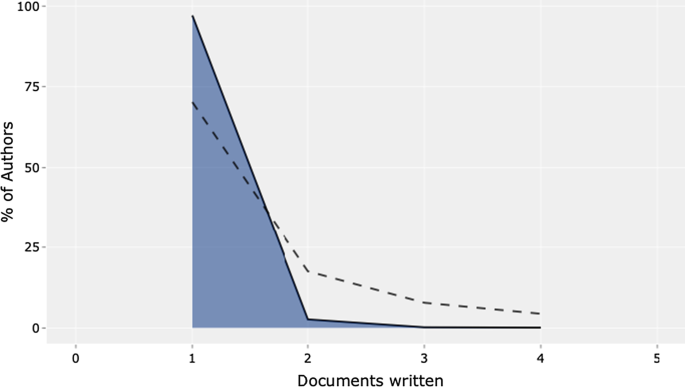
Lotka’s law.
The mathematical relationship is expressed in reverse in the following way:
where y x is equal to the number of authors producing x articles in each research field. Therefore, C and n are constants that can be estimated in the calculation.
The figure's results are in line with Lotka's results, with an average of two publications per author in a given research field. In addition, the figure shows the percentage of authors. Our results lead us to state that we are dealing with a young and growing research field, even with this analysis. Approximately 70% of the authors had published only their first research article. Only approximately 20% had published two scientific papers.
Authors’ keywords
This section provides information on the relationship between the keywords artificial intelligence and healthcare . This analysis is essential to determine the research trend, identify gaps in the discussion on AI in healthcare, and identify the fields that can be interesting as research areas [ 42 , 62 ].
Table 8 highlights the total number of keywords per author in the top 20 positions. The ranking is based on the following elements: healthcare, artificial intelligence, and clinical decision support system . Keyword analysis confirms the scientific area of reference. In particular, we deduce the definition as “Artificial intelligence is the theory and development of computer systems able to perform tasks normally requiring human intelligence, such as visual perception, speech recognition, decision-making, and translation between languages” [ 2 , 63 ]. Panch et al. [ 4 ] find that these technologies can be used in different business and management areas. After the first keyword, the analysis reveals AI applications and related research such as machine learning and deep learning.
Additionally, data mining and big data are a step forward in implementing exciting AI applications. According to our specific interest, if we applied AI in healthcare, we would achieve technological applications to help and support doctors and medical researchers in decision-making. The link between AI and decision-making is the reason why we find, in the seventh position, the keyword clinical decision support system . AI techniques can unlock clinically relevant information hidden in the massive amount of data that can assist clinical decision-making [ 64 ]. If we analyse the following keywords, we find other elements related to decision-making and support systems.
The TreeMap below (Fig. 6 ) highlights the combination of possible keywords representing AI and healthcare.
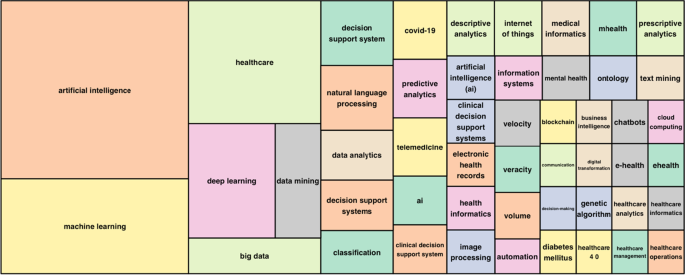
Keywords treemap.
The topic dendrogram in Fig. 7 represents the hierarchical order and the relationship between the keywords generated by hierarchical clustering [ 42 ]. The cut in the figure and the vertical lines facilitate an investigation and interpretation of the different clusters. As stated by Andrews [ 48 ], the figure is not intended to find the perfect level of associations between clusters. However, it aims to estimate the approximate number of clusters to facilitate further discussion.
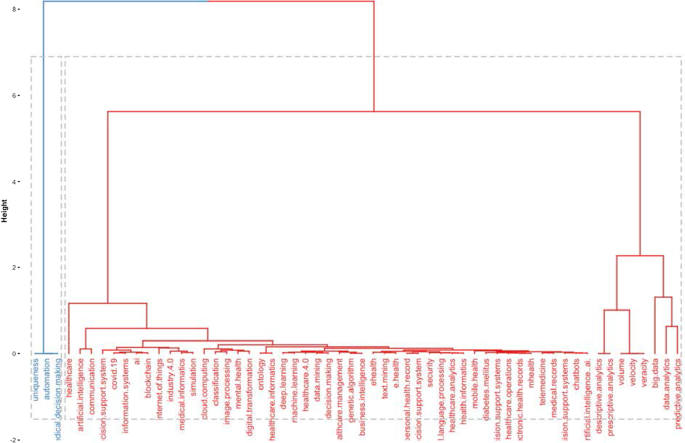
Topic dendrogram.
The research stream of AI in healthcare is divided into two main strands. The blue strand focuses on medical information systems and the internet. Some papers are related to healthcare organisations, such as the Internet of Things, meaning that healthcare organisations use AI to support health services management and data analysis. AI applications are also used to improve diagnostic and therapeutic accuracy and the overall clinical treatment process [ 2 ]. If we consider the second block, the red one, three different clusters highlight separate aspects of the topic. The first could be explained as AI and ML predictive algorithms. Through AI applications, it is possible to obtain a predictive approach that can ensure that patients are better monitored. This also allows a better understanding of risk perception for doctors and medical researchers. In the second cluster, the most frequent words are decisions , information system , and support system . This means that AI applications can support doctors and medical researchers in decision-making. Information coming from AI technologies can be used to consider difficult problems and support a more straightforward and rapid decision-making process. In the third cluster, it is vital to highlight that the ML model can deal with vast amounts of data. From those inputs, it can return outcomes that can optimise the work of healthcare organisations and scheduling of medical activities.
Furthermore, the word cloud in Fig. 8 highlights aspects of AI in healthcare, such as decision support systems, decision-making, health services management, learning systems, ML techniques and diseases. The figure depicts how AI is linked to healthcare and how it is used in medicine.
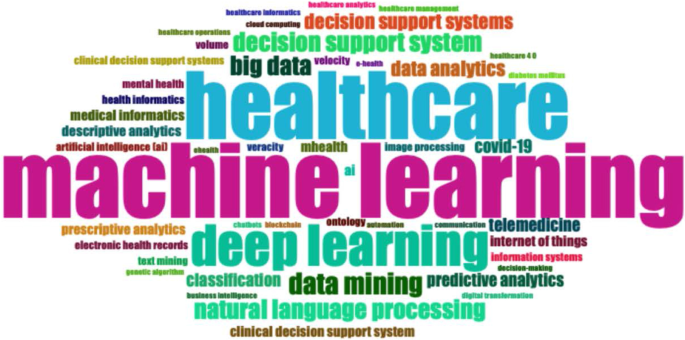
Word cloud.
Figure 9 represents the search trends based on the keywords analysed. The research started in 2012. First, it identified research topics related to clinical decision support systems. This topic was recurrent during the following years. Interestingly, in 2018, studies investigated AI and natural language processes as possible tools to manage patients and administrative elements. Finally, a new research stream considers AI's role in fighting COVID-19 [ 65 , 66 ].
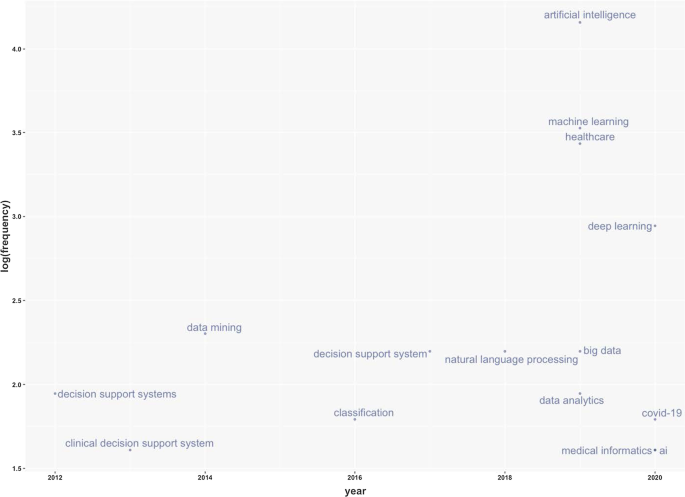
Keywords frequency.
Table 9 represents the number of citations from other articles within the top 20 rankings. The analysis allows the benchmark studies in the field to be identified [ 48 ]. For instance, Burke et al. [ 67 ] writes the most cited paper and analyses efficient nurse rostering methodologies. The paper critically evaluates tangible interdisciplinary solutions that also include AI. Immediately thereafter, Ahmed M.A.'s article proposes a data-driven optimisation methodology to determine the optimal number of healthcare staff to optimise patients' productivity [ 68 ]. Finally, the third most cited article lays the groundwork for developing deep learning by considering diverse health and administrative information [ 51 ].
This section analyses the diffusion of AI in healthcare around the world. It highlights countries to show the geographies of this research. It includes all published articles, the total number of citations, and the collaboration network. The following sub-sections start with an analysis of the total number of published articles.
Country total articles
Figure 9 and Table 10 display the countries where AI in healthcare has been considered. The USA tops the list of countries with the maximum number of articles on the topic (215). It is followed by China (83), the UK (54), India (51), Australia (54), and Canada (32). It is immediately evident that the theme has developed on different continents, highlighting a growing interest in AI in healthcare. The figure shows that many areas, such as Russia, Eastern Europe and Africa except for Algeria, Egypt, and Morocco, have still not engaged in this scientific debate.
Country publications and collaboration map
This section discusses articles on AI in healthcare in terms of single or multiple publications in each country. It also aims to observe collaboration and networking between countries. Table 11 and Fig. 10 highlight the average citations by state and show that the UK, the USA, and Kuwait have a higher average number of citations than other countries. Italy, Spain and New Zealand have the most significant number of citations.
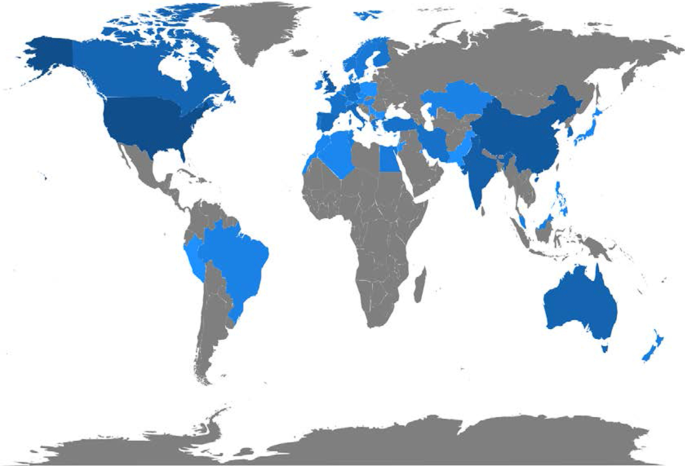
Articles per country.
Figure 11 depicts global collaborations. The blue colour on the map represents research cooperation among nations. Additionally, the pink border linking states indicates the extent of collaboration between authors. The primary cooperation between nations is between the USA and China, with two collaborative articles. Other collaborations among nations are limited to a few papers.
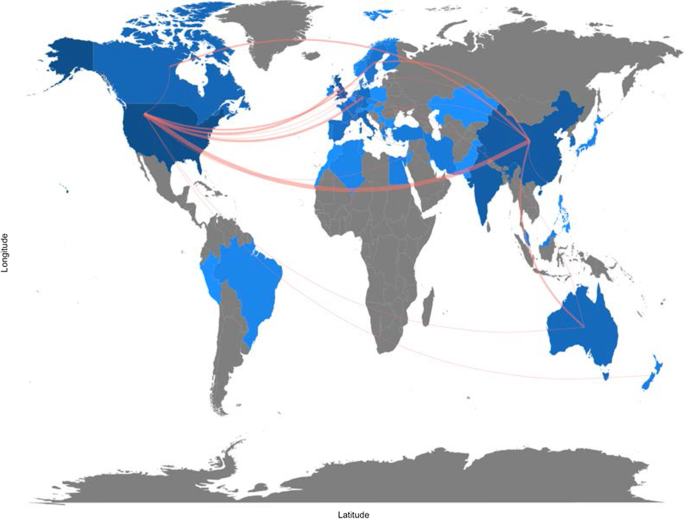
Collaboration map.
Artificial intelligence for healthcare: applications
This section aims to strengthen the research scope by answering RQ3: What are the research applications of artificial intelligence for healthcare?
Benefiting from the topical dendrogram, researchers will provide a development model based on four relevant variables [ 69 , 70 ]. AI has been a disruptive innovation in healthcare [ 4 ]. With its sophisticated algorithms and several applications, AI has assisted doctors and medical professionals in the domains of health information systems, geocoding health data, epidemic and syndromic surveillance, predictive modelling and decision support, and medical imaging [ 2 , 9 , 10 , 64 ]. Furthermore, the researchers considered the bibliometric analysis to identify four macro-variables dominant in the field and used them as authors' keywords. Therefore, the following sub-sections aim to explain the debate on applications in healthcare for AI techniques. These elements are shown in Fig. 12 .
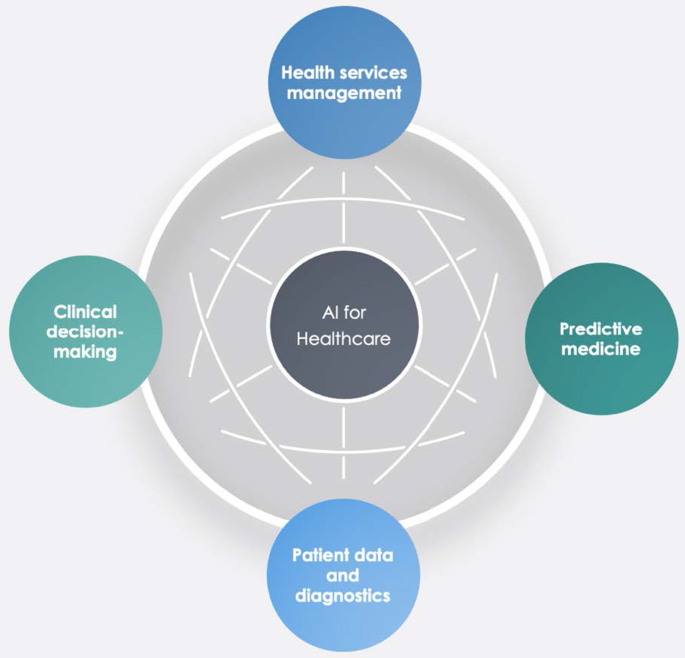
Dominant variables for AI in healthcare.
Health services management
One of the notable aspects of AI techniques is potential support for comprehensive health services management. These applications can support doctors, nurses and administrators in their work. For instance, an AI system can provide health professionals with constant, possibly real-time medical information updates from various sources, including journals, textbooks, and clinical practices [ 2 , 10 ]. These applications' strength is becoming even more critical in the COVID-19 period, during which information exchange is continually needed to properly manage the pandemic worldwide [ 71 ]. Other applications involve coordinating information tools for patients and enabling appropriate inferences for health risk alerts and health outcome prediction [ 72 ]. AI applications allow, for example, hospitals and all health services to work more efficiently for the following reasons:
Clinicians can access data immediately when they need it.
Nurses can ensure better patient safety while administering medication.
Patients can stay informed and engaged in their care by communicating with their medical teams during hospital stays.
Additionally, AI can contribute to optimising logistics processes, for instance, realising drugs and equipment in a just-in-time supply system based totally on predictive algorithms [ 73 , 74 ]. Interesting applications can also support the training of personnel working in health services. This evidence could be helpful in bridging the gap between urban and rural health services [ 75 ]. Finally, health services management could benefit from AI to leverage the multiplicity of data in electronic health records by predicting data heterogeneity across hospitals and outpatient clinics, checking for outliers, performing clinical tests on the data, unifying patient representation, improving future models that can predict diagnostic tests and analyses, and creating transparency with benchmark data for analysing services delivered [ 51 , 76 ].
Predictive medicine
Another relevant topic is AI applications for disease prediction and diagnosis treatment, outcome prediction and prognosis evaluation [ 72 , 77 ]. Because AI can identify meaningful relationships in raw data, it can support diagnostic, treatment and prediction outcomes in many medical situations [ 64 ]. It allows medical professionals to embrace the proactive management of disease onset. Additionally, predictions are possible for identifying risk factors and drivers for each patient to help target healthcare interventions for better outcomes [ 3 ]. AI techniques can also help design and develop new drugs, monitor patients and personalise patient treatment plans [ 78 ]. Doctors benefit from having more time and concise data to make better patient decisions. Automatic learning through AI could disrupt medicine, allowing prediction models to be created for drugs and exams that monitor patients over their whole lives [ 79 ].
- Clinical decision-making
One of the keyword analysis main topics is that AI applications could support doctors and medical researchers in the clinical decision-making process. According to Jiang et al. [ 64 ], AI can help physicians make better clinical decisions or even replace human judgement in healthcare-specific functional areas. According to Bennett and Hauser [ 80 ], algorithms can benefit clinical decisions by accelerating the process and the amount of care provided, positively impacting the cost of health services. Therefore, AI technologies can support medical professionals in their activities and simplify their jobs [ 4 ]. Finally, as Redondo and Sandoval [ 81 ] find, algorithmic platforms can provide virtual assistance to help doctors understand the semantics of language and learning to solve business process queries as a human being would.
Patient data and diagnostics
Another challenging topic related to AI applications is patient data and diagnostics. AI techniques can help medical researchers deal with the vast amount of data from patients (i.e., medical big data ). AI systems can manage data generated from clinical activities, such as screening, diagnosis, and treatment assignment. In this way, health personnel can learn similar subjects and associations between subject features and outcomes of interest [ 64 ].
These technologies can analyse raw data and provide helpful insights that can be used in patient treatments. They can help doctors in the diagnostic process; for example, to realise a high-speed body scan, it will be simpler to have an overall patient condition image. Then, AI technology can recreate a 3D mapping solution of a patient’s body.
In terms of data, interesting research perspectives are emerging. For instance, we observed the emergence of a stream of research on patient data management and protection related to AI applications [ 82 ].
For diagnostics, AI techniques can make a difference in rehabilitation therapy and surgery. Numerous robots have been designed to support and manage such tasks. Rehabilitation robots physically support and guide, for example, a patient’s limb during motor therapy [ 83 ]. For surgery, AI has a vast opportunity to transform surgical robotics through devices that can perform semi-automated surgical tasks with increasing efficiency. The final aim of this technology is to automate procedures to negate human error while maintaining a high level of accuracy and precision [ 84 ]. Finally, the -19 period has led to increased remote patient diagnostics through telemedicine that enables remote observation of patients and provides physicians and nurses with support tools [ 66 , 85 , 86 ].
This study aims to provide a bibliometric analysis of publications on AI in healthcare, focusing on accounting, business and management, decision sciences and health profession studies. Using the SLR method of Massaro et al. [ 11 ], we provide a reliable and replicable research protocol for future studies in this field. Additionally, we investigate the trend of scientific publications on the subject, unexplored information, future directions, and implications using the science mapping workflow. Our analysis provides interesting insights.
In terms of bibliometric variables, the four leading journals, Journal of Medical Systems , Studies in Health Technology and Informatics , IEEE Journal of Biomedical and Health Informatics , and Decision Support Systems , are optimal locations for the publication of scientific articles on this topic. These journals deal mainly with healthcare, medical information systems, and applications such as cloud computing, machine learning, and AI. Additionally, in terms of h-index, Bushko R.G. and Liu C. are the most productive and impactful authors in this research stream. Burke et al.’s [ 67 ] contribution is the most cited with an analysis of nurse rostering using new technologies such as AI. Finally, in terms of keywords, co-occurrence reveals some interesting insights. For instance, researchers have found that AI has a role in diagnostic accuracy and helps in the analysis of health data by comparing thousands of medical records, experiencing automatic learning with clinical alerts, efficient management of health services and places of care, and the possibility of reconstructing patient history using these data.
Second, this paper finds five cluster analyses in healthcare applications: health services management, predictive medicine, patient data, diagnostics, and finally, clinical decision-making. These technologies can also contribute to optimising logistics processes in health services and allowing a better allocation of resources.
Third, the authors analysing the research findings and the issues under discussion strongly support AI's role in decision support. These applications, however, are demonstrated by creating a direct link to data quality management and the technology awareness of health personnel [ 87 ].
The importance of data quality for the decision-making process
Several authors have analysed AI in the healthcare research stream, but in this case, the authors focus on other literature that includes business and decision-making processes. In this regard, the analysis of the search flow reveals a double view of the literature. On the one hand, some contributions belong to the positivist literature and embrace future applications and implications of technology for health service management, data analysis and diagnostics [ 6 , 80 , 88 ]. On the other hand, some investigations also aim to understand the darker sides of technology and its impact. For example, as Carter [ 89 ] states, the impact of AI is multi-sectoral; its development, however, calls for action to protect personal data. Similarly, Davenport and Kalakota [ 77 ] focus on the ethical implications of using AI in healthcare. According to the authors, intelligent machines raise issues of accountability, transparency, and permission, especially in automated communication with patients. Our analysis does not indicate a marked strand of the literature; therefore, we argue that the discussion of elements such as the transparency of technology for patients is essential for the development of AI applications.
A large part of our results shows that, at the application level, AI can be used to improve medical support for patients (Fig. 11 ) [ 64 , 82 ]. However, we believe that, as indicated by Kalis et al. [ 90 ] on the pages of Harvard Business Review, the management of costly back-office problems should also be addressed.
The potential of algorithms includes data analysis. There is an immense quantity of data accessible now, which carries the possibility of providing information about a wide variety of medical and healthcare activities [ 91 ]. With the advent of modern computational methods, computer learning and AI techniques, there are numerous possibilities [ 79 , 83 , 84 ]. For example, AI makes it easier to turn data into concrete and actionable observations to improve decision-making, deliver high-quality patient treatment, adapt to real-time emergencies, and save more lives on the clinical front. In addition, AI makes it easier to leverage capital to develop systems and facilities and reduce expenses at the organisational level [ 78 ]. Studying contributions to the topic, we noticed that data accuracy was included in the debate, indicating that a high standard of data will benefit decision-making practitioners [ 38 , 77 ]. AI techniques are an essential instrument for studying data and the extraction of medical insight, and they may assist medical researchers in their practices. Using computational tools, healthcare stakeholders may leverage the power of data not only to evaluate past data ( descriptive analytics ) but also to forecast potential outcomes ( predictive analytics ) and to define the best actions for the present scenario ( prescriptive analytics ) [ 78 ]. The current abundance of evidence makes it easier to provide a broad view of patient health; doctors should have access to the correct details at the right time and location to provide the proper treatment [ 92 ].
Will medical technology de-skill doctors?
Further reflection concerns the skills of doctors. Studies have shown that healthcare personnel are progressively being exposed to technology for different purposes, such as collecting patient records or diagnosis [ 71 ]. This is demonstrated by the keywords (Fig. 6 ) that focus on technology and the role of decision-making with new innovative tools. In addition, the discussion expands with Lu [ 93 ], which indicates that the excessive use of technology could hinder doctors’ skills and clinical procedures' expansion. Among the main issues arising from the literature is the possible de-skilling of healthcare staff due to reduced autonomy in decision-making concerning patients [ 94 ]. Therefore, the challenges and discussion we uncovered in Fig. 11 are expanded by also considering the ethical implications of technology and the role of skills.
Implications
Our analysis also has multiple theoretical and practical implications.
In terms of theoretical contribution, this paper extends the previous results of Connelly et al., dos Santos et al, Hao et al., Huang et al., Liao et al. and Tran et al. [ 2 , 19 , 20 , 21 , 22 , 24 ] in considering AI in terms of clinical decision-making and data management quality.
In terms of practical implications, this paper aims to create a fruitful discussion with healthcare professionals and administrative staff on how AI can be at their service to increase work quality. Furthermore, this investigation offers a broad comprehension of bibliometric variables of AI techniques in healthcare. It can contribute to advancing scientific research in this field.
Limitations
Like any other, our study has some limitations that could be addressed by more in-depth future studies. For example, using only one research database, such as Scopus, could be limiting. Further analysis could also investigate the PubMed, IEEE, and Web of Science databases individually and holistically, especially the health parts. Then, the use of search terms such as "Artificial Intelligence" OR "AI" AND "Healthcare" could be too general and exclude interesting studies. Moreover, although we analysed 288 peer-reviewed scientific papers, because the new research topic is new, the analysis of conference papers could return interesting results for future researchers. Additionally, as this is a young research area, the analysis will be subject to recurrent obsolescence as multiple new research investigations are published. Finally, although bibliometric analysis has limited the subjectivity of the analysis [ 15 ], the verification of recurring themes could lead to different results by indicating areas of significant interest not listed here.
Future research avenues
Concerning future research perspectives, researchers believe that an analysis of the overall amount that a healthcare organisation should pay for AI technologies could be helpful. If these technologies are essential for health services management and patient treatment, governments should invest and contribute to healthcare organisations' modernisation. New investment funds could be made available in the healthcare world, as in the European case with the Next Generation EU programme or national investment programmes [ 95 ]. Additionally, this should happen especially in the poorest countries around the world, where there is a lack of infrastructure and services related to health and medicine [ 96 ]. On the other hand, it might be interesting to evaluate additional profits generated by healthcare organisations with AI technologies compared to those that do not use such technologies.
Further analysis could also identify why some parts of the world have not conducted studies in this area. It would be helpful to carry out a comparative analysis between countries active in this research field and countries that are not currently involved. It would make it possible to identify variables affecting AI technologies' presence or absence in healthcare organisations. The results of collaboration between countries also present future researchers with the challenge of greater exchanges between researchers and professionals. Therefore, further research could investigate the difference in vision between professionals and academics.
In the accounting, business, and management research area, there is currently a lack of quantitative analysis of the costs and profits generated by healthcare organisations that use AI technologies. Therefore, research in this direction could further increase our understanding of the topic and the number of healthcare organisations that can access technologies based on AI. Finally, as suggested in the discussion section, more interdisciplinary studies are needed to strengthen AI links with data quality management and AI and ethics considerations in healthcare.
In pursuing the philosophy of Massaro et al.’s [ 11 ] methodological article, we have climbed on the shoulders of giants, hoping to provide a bird's-eye view of the AI literature in healthcare. We performed this study with a bibliometric analysis aimed at discovering authors, countries of publication and collaboration, and keywords and themes. We found a fast-growing, multi-disciplinary stream of research that is attracting an increasing number of authors.
The research, therefore, adopts a quantitative approach to the analysis of bibliometric variables and a qualitative approach to the study of recurring keywords, which has allowed us to demonstrate strands of literature that are not purely positive. There are currently some limitations that will affect future research potential, especially in ethics, data governance and the competencies of the health workforce.
Availability of data and materials
All the data are retrieved from public scientific platforms.
Tagliaferri SD, Angelova M, Zhao X, Owen PJ, Miller CT, Wilkin T, et al. Artificial intelligence to improve back pain outcomes and lessons learnt from clinical classification approaches: three systematic reviews. NPJ Digit Med. 2020;3(1):1–16.
Article Google Scholar
Tran BX, Vu GT, Ha GH, Vuong Q-H, Ho M-T, Vuong T-T, et al. Global evolution of research in artificial intelligence in health and medicine: a bibliometric study. J Clin Med. 2019;8(3):360.
Article PubMed Central Google Scholar
Hamid S. The opportunities and risks of artificial intelligence in medicine and healthcare [Internet]. 2016 [cited 2020 May 29]. http://www.cuspe.org/wp-content/uploads/2016/09/Hamid_2016.pdf
Panch T, Szolovits P, Atun R. Artificial intelligence, machine learning and health systems. J Glob Health. 2018;8(2):020303.
Article PubMed PubMed Central Google Scholar
Yang X, Wang Y, Byrne R, Schneider G, Yang S. Concepts of artificial intelligence for computer-assisted drug discovery | chemical reviews. Chem Rev. 2019;119(18):10520–94.
Article CAS PubMed Google Scholar
Burton RJ, Albur M, Eberl M, Cuff SM. Using artificial intelligence to reduce diagnostic workload without compromising detection of urinary tract infections. BMC Med Inform Decis Mak. 2019;19(1):171.
Meskò B, Drobni Z, Bényei E, Gergely B, Gyorffy Z. Digital health is a cultural transformation of traditional healthcare. Mhealth. 2017;3:38.
Cho B-J, Choi YJ, Lee M-J, Kim JH, Son G-H, Park S-H, et al. Classification of cervical neoplasms on colposcopic photography using deep learning. Sci Rep. 2020;10(1):13652.
Article CAS PubMed PubMed Central Google Scholar
Doyle OM, Leavitt N, Rigg JA. Finding undiagnosed patients with hepatitis C infection: an application of artificial intelligence to patient claims data. Sci Rep. 2020;10(1):10521.
Shortliffe EH, Sepúlveda MJ. Clinical decision support in the era of artificial intelligence. JAMA. 2018;320(21):2199–200.
Article PubMed Google Scholar
Massaro M, Dumay J, Guthrie J. On the shoulders of giants: undertaking a structured literature review in accounting. Account Auditing Account J. 2016;29(5):767–801.
Junquera B, Mitre M. Value of bibliometric analysis for research policy: a case study of Spanish research into innovation and technology management. Scientometrics. 2007;71(3):443–54.
Casadesus-Masanell R, Ricart JE. How to design a winning business model. Harvard Business Review [Internet]. 2011 Jan 1 [cited 2020 Jan 8]. https://hbr.org/2011/01/how-to-design-a-winning-business-model
Aria M, Cuccurullo C. bibliometrix: an R-tool for comprehensive science mapping analysis. J Informetr. 2017;11(4):959–75.
Zupic I, Čater T. Bibliometric methods in management and organization. Organ Res Methods. 2015;1(18):429–72.
Secinaro S, Calandra D. Halal food: structured literature review and research agenda. Br Food J. 2020. https://doi.org/10.1108/BFJ-03-2020-0234 .
Rialp A, Merigó JM, Cancino CA, Urbano D. Twenty-five years (1992–2016) of the international business review: a bibliometric overview. Int Bus Rev. 2019;28(6):101587.
Zhao L, Dai T, Qiao Z, Sun P, Hao J, Yang Y. Application of artificial intelligence to wastewater treatment: a bibliometric analysis and systematic review of technology, economy, management, and wastewater reuse. Process Saf Environ Prot. 2020;1(133):169–82.
Article CAS Google Scholar
Huang Y, Huang Q, Ali S, Zhai X, Bi X, Liu R. Rehabilitation using virtual reality technology: a bibliometric analysis, 1996–2015. Scientometrics. 2016;109(3):1547–59.
Hao T, Chen X, Li G, Yan J. A bibliometric analysis of text mining in medical research. Soft Comput. 2018;22(23):7875–92.
dos Santos BS, Steiner MTA, Fenerich AT, Lima RHP. Data mining and machine learning techniques applied to public health problems: a bibliometric analysis from 2009 to 2018. Comput Ind Eng. 2019;1(138):106120.
Liao H, Tang M, Luo L, Li C, Chiclana F, Zeng X-J. A bibliometric analysis and visualization of medical big data research. Sustainability. 2018;10(1):166.
Choudhury A, Renjilian E, Asan O. Use of machine learning in geriatric clinical care for chronic diseases: a systematic literature review. JAMIA Open. 2020;3(3):459–71.
Connelly TM, Malik Z, Sehgal R, Byrnes G, Coffey JC, Peirce C. The 100 most influential manuscripts in robotic surgery: a bibliometric analysis. J Robot Surg. 2020;14(1):155–65.
Guo Y, Hao Z, Zhao S, Gong J, Yang F. Artificial intelligence in health care: bibliometric analysis. J Med Internet Res. 2020;22(7):e18228.
Choudhury A, Asan O. Role of artificial intelligence in patient safety outcomes: systematic literature review. JMIR Med Inform. 2020;8(7):e18599.
Forliano C, De Bernardi P, Yahiaoui D. Entrepreneurial universities: a bibliometric analysis within the business and management domains. Technol Forecast Soc Change. 2021;1(165):120522.
Secundo G, Del Vecchio P, Mele G. Social media for entrepreneurship: myth or reality? A structured literature review and a future research agenda. Int J Entrep Behav Res. 2020;27(1):149–77.
Dal Mas F, Massaro M, Lombardi R, Garlatti A. From output to outcome measures in the public sector: a structured literature review. Int J Organ Anal. 2019;27(5):1631–56.
Google Scholar
Baima G, Forliano C, Santoro G, Vrontis D. Intellectual capital and business model: a systematic literature review to explore their linkages. J Intellect Cap. 2020. https://doi.org/10.1108/JIC-02-2020-0055 .
Dumay J, Guthrie J, Puntillo P. IC and public sector: a structured literature review. J Intellect Cap. 2015;16(2):267–84.
Dal Mas F, Garcia-Perez A, Sousa MJ, Lopes da Costa R, Cobianchi L. Knowledge translation in the healthcare sector. A structured literature review. Electron J Knowl Manag. 2020;18(3):198–211.
Mas FD, Massaro M, Lombardi R, Biancuzzi H. La performance nel settore pubblico tra misure di out-put e di outcome. Una revisione strutturata della letteratura ejvcbp. 2020;1(3):16–29.
Dumay J, Cai L. A review and critique of content analysis as a methodology for inquiring into IC disclosure. J Intellect Cap. 2014;15(2):264–90.
Haleem A, Javaid M, Khan IH. Current status and applications of Artificial Intelligence (AI) in medical field: an overview. Curr Med Res Pract. 2019;9(6):231–7.
Paul J, Criado AR. The art of writing literature review: what do we know and what do we need to know? Int Bus Rev. 2020;29(4):101717.
Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JPA, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med. 2009;6(7):e1000100.
Biancone PP, Secinaro S, Brescia V, Calandra D. Data quality methods and applications in health care system: a systematic literature review. Int J Bus Manag. 2019;14(4):p35.
Secinaro S, Brescia V, Calandra D, Verardi GP, Bert F. The use of micafungin in neonates and children: a systematic review. ejvcbp. 2020;1(1):100–14.
Bert F, Gualano MR, Biancone P, Brescia V, Camussi E, Martorana M, et al. HIV screening in pregnant women: a systematic review of cost-effectiveness studies. Int J Health Plann Manag. 2018;33(1):31–50.
Levy Y, Ellis TJ. A systems approach to conduct an effective literature review in support of information systems research. Inf Sci Int J Emerg Transdiscipl. 2006;9:181–212.
Chen G, Xiao L. Selecting publication keywords for domain analysis in bibliometrics: a comparison of three methods. J Informet. 2016;10(1):212–23.
Falagas ME, Pitsouni EI, Malietzis GA, Pappas G. Comparison of PubMed, Scopus, Web of Science, and Google Scholar: strengths and weaknesses. FASEB J. 2007;22(2):338–42.
Article PubMed CAS Google Scholar
Sicilia M-A, Garcìa-Barriocanal E, Sànchez-Alonso S. Community curation in open dataset repositories: insights from zenodo. Procedia Comput Sci. 2017;1(106):54–60.
Secinaro S, Calandra D, Secinaro A, Muthurangu V, Biancone P. Artificial Intelligence for healthcare with a business, management and accounting, decision sciences, and health professions focus [Internet]. Zenodo; 2021 [cited 2021 Mar 7]. https://zenodo.org/record/4587618#.YEScpl1KiWh .
Elango B, Rajendran D. Authorship trends and collaboration pattern in the marine sciences literature: a scientometric Study. Int J Inf Dissem Technol. 2012;1(2):166–9.
Jacoby WG. Electoral inquiry section Loess: a nonparametric, graphical tool for depicting relationships between variables q. In 2000.
Andrews JE. An author co-citation analysis of medical informatics. J Med Libr Assoc. 2003;91(1):47–56.
PubMed PubMed Central Google Scholar
White HD, Griffith BC. Author cocitation: a literature measure of intellectual structure. J Am Soc Inf Sci. 1981;32(3):163–71.
Santosh KC. AI-driven tools for coronavirus outbreak: need of active learning and cross-population train/test models on multitudinal/multimodal data. J Med Syst. 2020;44(5):93.
Shickel B, Tighe PJ, Bihorac A, Rashidi P. Deep EHR: a survey of recent advances in deep learning techniques for electronic health record (EHR) analysis. IEEE J Biomed Health Inform. 2018;22(5):1589–604.
Baig MM, GholamHosseini H, Moqeem AA, Mirza F, Lindén M. A systematic review of wearable patient monitoring systems—current challenges and opportunities for clinical adoption. J Med Syst. 2017;41(7):115.
Kumar S, Kumar S. Collaboration in research productivity in oil seed research institutes of India. In: Proceedings of fourth international conference on webometrics, informetrics and scientometrics. p. 28–1; 2008.
Gatto A, Drago C. A taxonomy of energy resilience. Energy Policy. 2020;136:111007.
Levitt JM, Thelwall M. Alphabetization and the skewing of first authorship towards last names early in the alphabet. J Informet. 2013;7(3):575–82.
Saad G. Exploring the h-index at the author and journal levels using bibliometric data of productive consumer scholars and business-related journals respectively. Scientometrics. 2006;69(1):117–20.
Egghe L. Theory and practise of the g-index. Scientometrics. 2006;69(1):131–52.
Schreiber M. A modification of the h-index: the hm-index accounts for multi-authored manuscripts. J Informet. 2008;2(3):211–6.
Engqvist L, Frommen JG. The h-index and self-citations. Trends Ecol Evol. 2008;23(5):250–2.
London School of Economics. 3: key measures of academic influence [Internet]. Impact of social sciences. 2010 [cited 2021 Jan 13]. https://blogs.lse.ac.uk/impactofsocialsciences/the-handbook/chapter-3-key-measures-of-academic-influence/ .
Lotka A. The frequency distribution of scientific productivity. J Wash Acad Sci. 1926;16(12):317–24.
Khan G, Wood J. Information technology management domain: emerging themes and keyword analysis. Scientometrics. 2015;9:105.
Oxford University Press. Oxford English Dictionary [Internet]. 2020. https://www.oed.com/ .
Jiang F, Jiang Y, Zhi H, Dong Y, Li H, Ma S, et al. Artificial intelligence in healthcare: past, present and future. Stroke Vasc Neurol. 2017;2(4):230–43.
Calandra D, Favareto M. Artificial Intelligence to fight COVID-19 outbreak impact: an overview. Eur J Soc Impact Circ Econ. 2020;1(3):84–104.
Bokolo Anthony Jnr. Use of telemedicine and virtual care for remote treatment in response to COVID-19 pandemic. J Med Syst. 2020;44(7):132.
Burke EK, De Causmaecker P, Berghe GV, Van Landeghem H. The state of the art of nurse rostering. J Sched. 2004;7(6):441–99.
Ahmed MA, Alkhamis TM. Simulation optimization for an emergency department healthcare unit in Kuwait. Eur J Oper Res. 2009;198(3):936–42.
Forina M, Armanino C, Raggio V. Clustering with dendrograms on interpretation variables. Anal Chim Acta. 2002;454(1):13–9.
Wartena C, Brussee R. Topic detection by clustering keywords. In: 2008 19th international workshop on database and expert systems applications. 2008. p. 54–8.
Hussain AA, Bouachir O, Al-Turjman F, Aloqaily M. AI Techniques for COVID-19. IEEE Access. 2020;8:128776–95.
Agrawal A, Gans JS, Goldfarb A. Exploring the impact of artificial intelligence: prediction versus judgment. Inf Econ Policy. 2019;1(47):1–6.
Chakradhar S. Predictable response: finding optimal drugs and doses using artificial intelligence. Nat Med. 2017;23(11):1244–7.
Fleming N. How artificial intelligence is changing drug discovery. Nature. 2018;557(7707):S55–7.
Guo J, Li B. The application of medical artificial intelligence technology in rural areas of developing countries. Health Equity. 2018;2(1):174–81.
Aisyah M, Cockcroft S. A snapshot of data quality issues in Indonesian community health. Int J Netw Virtual Organ. 2014;14(3):280–97.
Davenport T, Kalakota R. The potential for artificial intelligence in healthcare. Future Healthc J. 2019;6(2):94–8.
Mehta N, Pandit A, Shukla S. Transforming healthcare with big data analytics and artificial intelligence: a systematic mapping study. J Biomed Inform. 2019;1(100):103311.
Collins GS, Moons KGM. Reporting of artificial intelligence prediction models. Lancet. 2019;393(10181):1577–9.
Bennett CC, Hauser K. Artificial intelligence framework for simulating clinical decision-making: a Markov decision process approach. Artif Intell Med. 2013;57(1):9–19.
Redondo T, Sandoval AM. Text Analytics: the convergence of big data and artificial intelligence. Int J Interact Multimed Artif Intell. 2016;3. https://www.ijimai.org/journal/bibcite/reference/2540 .
Winter JS, Davidson E. Big data governance of personal health information and challenges to contextual integrity. Inf Soc. 2019;35(1):36–51.
Novak D, Riener R. Control strategies and artificial intelligence in rehabilitation robotics. AI Mag. 2015;36(4):23–33.
Tarassoli SP. Artificial intelligence, regenerative surgery, robotics? What is realistic for the future of surgery? Ann Med Surg (Lond). 2019;17(41):53–5.
Saha SK, Fernando B, Cuadros J, Xiao D, Kanagasingam Y. Automated quality assessment of colour fundus images for diabetic retinopathy screening in telemedicine. J Digit Imaging. 2018;31(6):869–78.
Gu D, Li T, Wang X, Yang X, Yu Z. Visualizing the intellectual structure and evolution of electronic health and telemedicine research. Int J Med Inform. 2019;130:103947.
Madnick S, Wang R, Lee Y, Zhu H. Overview and framework for data and information quality research. J Data Inf Qual. 2009;1:1.
Chen X, Liu Z, Wei L, Yan J, Hao T, Ding R. A comparative quantitative study of utilizing artificial intelligence on electronic health records in the USA and China during 2008–2017. BMC Med Inform Decis Mak. 2018;18(5):117.
Carter D. How real is the impact of artificial intelligence? Bus Inf Surv. 2018;35(3):99–115.
Kalis B, Collier M, Fu R. 10 Promising AI Applications in Health Care. 2018;5.
Biancone P, Secinaro S, Brescia V, Calandra D. Management of open innovation in healthcare for cost accounting using EHR. J Open Innov Technol Market Complex. 2019;5(4):99.
Kayyali B, Knott D, Van Kuiken S. The ‘big data’ revolution in US healthcare [Internet]. McKinsey & Company. 2013 [cited 2020 Aug 14]. https://healthcare.mckinsey.com/big-data-revolution-us-healthcare/ .
Lu J. Will medical technology deskill doctors? Int Educ Stud. 2016;9(7):130–4.
Hoff T. Deskilling and adaptation among primary care physicians using two work innovations. Health Care Manag Rev. 2011;36(4):338–48.
Picek O. Spillover effects from next generation EU. Intereconomics. 2020;55(5):325–31.
Sousa MJ, Dal Mas F, Pesqueira A, Lemos C, Verde JM, Cobianchi L. The potential of AI in health higher education to increase the students’ learning outcomes. TEM J. 2021. ( In press ).
Download references
Acknowledgements
The authors are grateful to the Editor-in-Chief for the suggestions and all the reviewers who spend a part of their time ensuring constructive feedback to our research article.
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Author information
Authors and affiliations.
Department of Management, University of Turin, Turin, Italy
Silvana Secinaro, Davide Calandra & Paolo Biancone
Ospedale Pediatrico Bambino Gesù, Rome, Italy
Aurelio Secinaro
Institute of Child Health, University College London, London, UK
Vivek Muthurangu
You can also search for this author in PubMed Google Scholar
Contributions
SS and PB, Supervision; Validation, writing, AS and VM; Formal analysis, DC and AS; Methodology, DC; Writing; DC, SS and AS; conceptualization, VM, PB; validation, VM, PB. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Davide Calandra .
Ethics declarations
Ethical approval and consent to participate.
Not applicable.
Consent for publication
Competing interests.
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Secinaro, S., Calandra, D., Secinaro, A. et al. The role of artificial intelligence in healthcare: a structured literature review. BMC Med Inform Decis Mak 21 , 125 (2021). https://doi.org/10.1186/s12911-021-01488-9
Download citation
Received : 24 December 2020
Accepted : 01 April 2021
Published : 10 April 2021
DOI : https://doi.org/10.1186/s12911-021-01488-9
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Artificial intelligence
- Patient data
BMC Medical Informatics and Decision Making
ISSN: 1472-6947
- General enquiries: [email protected]
Information
- Author Services
Initiatives
You are accessing a machine-readable page. In order to be human-readable, please install an RSS reader.
All articles published by MDPI are made immediately available worldwide under an open access license. No special permission is required to reuse all or part of the article published by MDPI, including figures and tables. For articles published under an open access Creative Common CC BY license, any part of the article may be reused without permission provided that the original article is clearly cited. For more information, please refer to https://www.mdpi.com/openaccess .
Feature papers represent the most advanced research with significant potential for high impact in the field. A Feature Paper should be a substantial original Article that involves several techniques or approaches, provides an outlook for future research directions and describes possible research applications.
Feature papers are submitted upon individual invitation or recommendation by the scientific editors and must receive positive feedback from the reviewers.
Editor’s Choice articles are based on recommendations by the scientific editors of MDPI journals from around the world. Editors select a small number of articles recently published in the journal that they believe will be particularly interesting to readers, or important in the respective research area. The aim is to provide a snapshot of some of the most exciting work published in the various research areas of the journal.
Original Submission Date Received: .
- Active Journals
- Find a Journal
- Proceedings Series
- For Authors
- For Reviewers
- For Editors
- For Librarians
- For Publishers
- For Societies
- For Conference Organizers
- Open Access Policy
- Institutional Open Access Program
- Special Issues Guidelines
- Editorial Process
- Research and Publication Ethics
- Article Processing Charges
- Testimonials
- Preprints.org
- SciProfiles
- Encyclopedia

Article Menu

- Subscribe SciFeed
- Recommended Articles
- Google Scholar
- on Google Scholar
- Table of Contents
Find support for a specific problem in the support section of our website.
Please let us know what you think of our products and services.
Visit our dedicated information section to learn more about MDPI.
JSmol Viewer
Recent advances of artificial intelligence in healthcare: a systematic literature review.

1. Introduction
2. literature review methodology, 3. classification framework for analysis, 3.1. healthcare activities using ai, 3.2. advantages and drawbacks for the healthcare sector, 3.3. ethical issues about ai, 3.4. social sustainability and ai, 3.5. ai in hospital management, 3.6. ai and machine learning in disease diagnosis, 3.7. ai and machine learning in remote patient monitoring, 4. discussion, 5. conclusions, author contributions, institutional review board statement, informed consent statement, data availability statement, conflicts of interest.
- Aerts, A.; Bogdan-Martin, D. Leveraging data and AI to deliver on the promise of digital health. Int. J. Med. Inform. 2021 , 150 , 104456. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Ali, O.; Abdelbaki, W.; Shrestha, A.; Elbasi, E.; Alryalat, M.A.A.; Dwivedi, Y.K. A systematic literature review of artificial intelligence in the healthcare sector: Benefits, challenges, methodologies, and functionalities. J. Innov. Knowl. 2023 , 8 , 100333. [ Google Scholar ] [ CrossRef ]
- Li, B.H.; Hou, B.C.; Yu, W.T.; Lu, X.B.; Yang, C.W. Applications of artificial intelligence in intelligent manufacturing: A review. Front. Inf. Technol. Electron. Eng. 2017 , 18 , 86–96. [ Google Scholar ] [ CrossRef ]
- Kaplan, A.; Haenlein, M. Rulers of the world, unite! The challenges and opportunities of artificial intelligence. Bus. Horiz. 2020 , 63 , 37–45. [ Google Scholar ] [ CrossRef ]
- Chien, C.F.; Dauzere-Peres, S.; Huh, W.T.; Jang, Y.J.; Morrison, J.R. Artificial intelligence in manufacturing and logistics systems: Algorithms, applications, and case studies. Int. J. Prod. Res. 2020 , 58 , 2730–2731. [ Google Scholar ] [ CrossRef ]
- Kumar, P.; Sharma, S.K.; Dutot, V. Artificial intelligence (AI)-enabled CRM capability in healthcare: The impact on service innovation. Int. J. Inf. Manag. 2023 , 69 , 102598. [ Google Scholar ] [ CrossRef ]
- Aiken, R.M.; Epstein, R.G. Ethical guidelines for AI in education: Starting a conversation. Int. J. Artif. Intell. Educ. 2000 , 11 , 163–176. [ Google Scholar ]
- Bansal, A.; Padappayil, R.P.; Garg, C.; Singal, A.; Gupta, M.; Klein, A. Utility of artificial intelligence amidst the COVID 19 pandemic: A review. J. Med. Syst. 2020 , 44 , 156. [ Google Scholar ] [ CrossRef ]
- Chee, M.L.; Ong, M.E.H.; Siddiqui, F.J.; Zhang, Z.; Lim, S.L.; Ho, A.F.W.; Liu, N. Artificial intelligence applications for COVID-19 in intensive care and emergency settings: A systematic review. Int. J. Environ. Res. Public Health 2021 , 18 , 4749. [ Google Scholar ] [ CrossRef ]
- Minz, A.; Mahobiya, C. MR Image Classification Using ad Boost for Brain Tumor Type. In Proceedings of the IEEE 7th International Advance Computing Conference, Hyderabad, India, 5–7 January 2017; pp. 701–705. [ Google Scholar ]
- Ribbens, A.; Hermans, J.; Maes, F.; Vandermeulen, D.; Suetens, P. Unsupervised segmentation, clustering, and group wise registration of heterogeneous populations of brain MR images. IEEE Trans. Med. Imaging 2014 , 33 , 201–224. [ Google Scholar ] [ CrossRef ]
- Strachna, O.; Asan, O. Reengineering Clinical Decision Support Systems for Artificial Intelligence. In Proceedings of the IEEE International Conference on Healthcare Informatics, Oldenburg, Germany, 30 November–3 December 2020; pp. 1–3. [ Google Scholar ]
- Comito, C.; Falcone, D.; Forestiero, A. Current Trends and Practices. In Smart Health Monitoring and Clinical Decision Support. In Proceedings of the IEEE International Conference on Bioinformatics and Biomedicine, Seoul, Republic of Korea, 16–19 December 2020; pp. 2577–2584. [ Google Scholar ]
- Bernardini, M.; Romeo, L.; Frontoni, E.; Amini, M.R. A semi-supervised multitask learning approach for predicting short-term kidney disease evolution. IEEE J. Biomed. Health Inform. 2021 , 25 , 3983–3994. [ Google Scholar ] [ CrossRef ]
- Yu, H.; Zhou, Z. Optimization of IoT-based artificial intelligence assisted telemedicine health analysis system. IEEE Access 2021 , 9 , 85034–85048. [ Google Scholar ] [ CrossRef ]
- Chen, Z. An AI-Based heart failure treatment adviser system. IEEE J. Transl. Eng. Health Med. 2018 , 6 , 1–10. [ Google Scholar ] [ CrossRef ]
- Dhieb, N.; Ghazzai, H.; Besbes, H.; Massoud, Y. A Secure AI-Driven architecture for automated insurance systems: Fraud detection and risk measurement. IEEE Access 2020 , 8 , 58546–58558. [ Google Scholar ] [ CrossRef ]
- Merhi, M.I. An evaluation of the critical success factors impacting artificial intelligence implementation. Int. J. Inf. Manag. 2022 , 69 , 102545. [ Google Scholar ] [ CrossRef ]
- Sqalli, M.T.; Al-Thani, D. AI-Supported Health Coaching Model for Patients with Chronic Diseases. In Proceedings of the 16th International Symposium on Wireless Communication Systems, Oulu, Finland, 27–30 August 2019; pp. 452–456. [ Google Scholar ]
- Zhou, L. A rapid, accurate and machine-agnostic segmentation and quantification method for CT-Based COVID-19 diagnosis. IEEE Trans. Med. Imaging 2020 , 39 , 2638–2652. [ Google Scholar ] [ CrossRef ]
- Tobore, I.; Li, J.; Yuhang, L.; Al-Handarish, Y.; Kandwal, A.; Nie, Z.; Wang, L. Deep learning intervention for health care challenges: Some biomedical domain considerations. JMIR mHealth uHealth 2019 , 7 , e11966. [ Google Scholar ] [ CrossRef ]
- Kitsios, F.; Kamariotou, M. Information Systems Strategy and Strategy-as-Practice: Planning Evaluation in SMEs. In Proceedings of the Americas Conference on Information Systems (AMCIS2019), Cancun, Mexico, 15–17 August 2019; pp. 1–10. [ Google Scholar ]
- Wahl, B.; Cossy-Gantner, A.; Germann, S.; Schwalbe, N.R. Artificial intelligence (AI) and global health: How can AI contribute to health in resource-poor settings? BMJ Glob. Health 2018 , 3 , e000798. [ Google Scholar ] [ CrossRef ] [ Green Version ]
- Kaur, A.; Garg, R.; Gupta, P. Challenges Facing AI and Big Data for Resource Poor Healthcare System. In Proceedings of the 2nd International Conference on Electronics and Sustainable Communication Systems, Coimbatore, India, 4–6 August 2021; pp. 1426–1433. [ Google Scholar ]
- Goodarzian, F.; Ghasemi, P.; Gunasekaren, A.; Taleizadeh, A.A.; Abraham, A. A sustainable-resilience healthcare network for handling COVID-19 pandemic. Ann. Oper. Res. 2021 , 312 , 761–825. [ Google Scholar ] [ CrossRef ]
- Pee, L.G.; Pan, S.; Cui, L. Artificial intelligence in healthcare robots: A social informatics study of knowledge embodiment. J. Assoc. Inf. Sci. Technol. 2019 , 70 , 351–369. [ Google Scholar ] [ CrossRef ]
- Maduri, P.K.; Dewangan, Y.; Yadav, D.; Chauhan, S.; Singh, K. IoT Based Patient Health Monitoring Portable Kit. In Proceedings of the 2nd International Conference on Advances in Computing, Communication Control and Networking, Greater Noida, India, 18–19 December 2020; pp. 513–516. [ Google Scholar ]
- Hossen, M.S.; Karmoker, D. Predicting the Probability of COVID-19 Recovered in South Asian Countries Based on Healthy Diet Pattern Using a Machine Learning Approach. In Proceedings of the 2nd International Conference on Sustainable Technologies for Industry 4.0, Dhaka, Bangladesh, 19–20 December 2020; pp. 1–6. [ Google Scholar ]
- Dharani, N.; Krishnan, G. ANN Based COVID-19 Prediction and Symptoms Relevance Survey and Analysis. In Proceedings of the 5th International Conference on Computing Methodologies and Communication, Erode, India, 8–10 April 2021; pp. 1805–1808. [ Google Scholar ]
- Duan, L.; Street, W.N.; Xu, E. Health-care information systems: Data mining methods in the creation of a clinical recommender system. Enterp. Inf. Syst. 2011 , 5 , 169–181. [ Google Scholar ] [ CrossRef ]
- Antoniou, Z.C.; Panayides, A.S.; Pantzaris, M.; Constantinides, A.G.; Pattichis, C.S.; Pattichis, M.S. Real-Time adaptation to time-varying constraints for medical video communications. IEEE J. Biomed. Health Inform. 2018 , 22 , 1177–1188. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Liu, J.; Ma, J.; Li, J.; Huang, M.; Sadiq, N.; Ai, Y. Robust watermarking algorithm for medical volume data in internet of medical things. IEEE Access 2020 , 8 , 93939–93966. [ Google Scholar ] [ CrossRef ]
- Xie, X.; Zang, Z.; Ponzoa, J.M. The information impact of network media, the psychological reaction to the COVID-19 pandemic, and online knowledge acquisition: Evidence from Chinese college students. J. Innov. Knowl. 2020 , 5 , 297–305. [ Google Scholar ] [ CrossRef ]
- Gunasekeran, D.V.; Tseng, R.M.W.W.; Tham, Y.C.; Wong, T.Y. Applications of digital health for public health responses to COVID-19: A systematic scoping review of artificial intelligence, telehealth and related technologies. NPJ Digit. Med. 2021 , 4 , 40. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Charan, S.; Khan, M.J.; Khurshid, K. Breast Cancer Detection in Mammograms using Convolutional Neural Network. In Proceedings of the International Conference on Computing, Mathematics and Engineering Technologies, Sukkur, Pakistan, 3–4 March 2018; pp. 1–5. [ Google Scholar ]
- Woo, Y.; Andres, P.T.C.; Jeong, H.; Shin, C. Classification of Diabetic Walking through Machine Learning: Survey Targeting Senior Citizens. In Proceedings of the International Conference on Artificial Intelligence in Information and Communication, Jeju Island, Republic of Korea, 20–23 April 2021; pp. 435–437. [ Google Scholar ]
- Deng, Y. A new framework to reduce doctor’s workload for medical image annotation. IEEE Access 2019 , 7 , 107097–107104. [ Google Scholar ] [ CrossRef ]
- Khan, M.; Mehran, M.T.; Haq, Z.U.; Ullah, Z.; Naqvi, S.R.; Ihsan, M.; Abbass, H. Applications of artificial intelligence in COVID-19 pandemic: A comprehensive review. Expert Syst. Appl. 2021 , 185 , 115695. [ Google Scholar ] [ CrossRef ]
- Chen, X.; Xie, H.; Zou, D.; Hwang, G. Application and theory gaps during the rise of Artificial Intelligence in Education. Comput. Educ. Artif. Intell. 2020 , 1 , 100002. [ Google Scholar ] [ CrossRef ]
- Johnson, M.; Albizri, A.; Harfouche, A.A.; Fosso-Wamba, W. Integrating human knowledge into artificial intelligence for complex and ill-structured problems: Informed artificial intelligence. Int. J. Inf. Manag. 2022 , 64 , 10247. [ Google Scholar ] [ CrossRef ]
- Webster, J.; Watson, R.T. Analyzing the Past to Prepare for the Future: Writing a Literature Review. MIS Q. 2002 , 26 , xiii–xxiii. [ Google Scholar ]
- Kamboj, S.; Rahman, Z. Marketing capabilities and firm performance: Literature review and future research agenda. Int. J. Product. Perform. Manag. 2015 , 64 , 1041–1067. [ Google Scholar ] [ CrossRef ]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. BMJ 2009 , 339 , b2535. [ Google Scholar ] [ CrossRef ] [ Green Version ]
- Abbas, Z.; Raza, S.; Ejaz, K. Systematic reviews and their role in evidence—Informed health care. J. Pak. Med. Assoc. 2008 , 58 , 461–467. [ Google Scholar ]
- Kitsios, F.; Kamariotou, M.; Talias, M.A. Corporate sustainability strategies and decision support methods: A bibliometric analysis. Sustainability 2020 , 12 , 521. [ Google Scholar ] [ CrossRef ] [ Green Version ]
- Kitsios, F.; Kamariotou, M. Artificial intelligence and business strategy towards digital transformation: A research agenda. Sustainability 2021 , 13 , 2025. [ Google Scholar ] [ CrossRef ]
- Mahdi, S.S.; Battineni, G.; Khawaja, M.; Allana, R.; Siddiqui, M.K.; Agha, D. How does artificial intelligence impact digital healthcare initiatives? A review of AI applications in dental healthcare. Int. J. Inf. Manag. Data Insights 2023 , 3 , 100144. [ Google Scholar ] [ CrossRef ]
- Vishwakarma, L.P.; Singh, R.K.; Mishra, R.; Kumari, A. Application of artificial intelligence for resilient and sustainable healthcare system: Systematic literature review and future research directions. Int. J. Prod. Res. 2023 , 1–23. [ Google Scholar ] [ CrossRef ]
- Siala, H.; Wang, Y. SHIFTing artificial intelligence to be responsible in healthcare: A systematic review. Soc. Sci. Med. 2022 , 296 , 114782. [ Google Scholar ] [ CrossRef ]
- Jahan, R.; Tripathi, M.M. Brain Tumor Detection using Machine Learning in MR Images. In Proceedings of the 10th IEEE International Conference on Communication Systems and Network Technologies, Bhopal, India, 18–19 June 2021; pp. 664–668. [ Google Scholar ]
- Ladgham, A.; Torkhani, G.; Sakly, A.; Mtibaa, A. Modified Support Vector Machines for MR Brain Images Recognition. In Proceedings of the International Conference on Control, Decision and Information Technologies, Hammamet, Tunisia, 6–8 May 2013; pp. 32–35. [ Google Scholar ]
- Rong, G.; Mendez, A.; Assi, E.B.; Zhao, B.; Sawan, M. Artificial intelligence in healthcare: Review and prediction case studies. Engineering 2020 , 6 , 291–301. [ Google Scholar ] [ CrossRef ]
- Wu, F.; Wu, T.; Yuce, M.R. Design and Implementation of a Wearable Sensor Network System for IoT-Connected Safety and Health Applications. In Proceedings of the 5th World Forum on Internet of Things, Limerick, Ireland, 15–18 April 2019; pp. 87–90. [ Google Scholar ]
- Gandhi, M.; Singh, V.K.; Kumar, V. IntelliDoctor—AI Based Medical Assistant. In Proceedings of the 5th International Conference on Science Technology Engineering and Mathematics, Chennai, India, 14–15 March 2019; pp. 162–168. [ Google Scholar ]
- Jaiman, V.; Urovi, V. A consent model for blockchain-based health data sharing platforms. IEEE Access 2020 , 8 , 143734–143745. [ Google Scholar ] [ CrossRef ]
- Zheng, X.; Mukkamala, R.R.; Vatrapu, R.; Ordieres-Mere, J. Blockchain-Based Personal Health Data Sharing System using Cloud Storage. In Proceedings of the 20th International Conference on e-Health Networking, Applications and Services, Ostrava, Czech Republic, 17–20 September 2018; pp. 1–6. [ Google Scholar ]
- Thakkar, B.A.; Hasan, M.I.; Desai, M.A. Health Care Decision Support System for Swine Flu Prediction using Naïve Bayes Classifier. In Proceedings of the International Conference on Advances in Recent Technologies in Communication and Computing, Kottayam, Kerala, India, 16–17 October 2010; pp. 101–105. [ Google Scholar ]
- Moein, M.; Davarpanah, M.; Montazeri, M.A.; Ataei, M. Classifying Ear Disorders using Support Vector Machines. In Proceedings of the 2nd International Conference on Computational Intelligence and Natural Computing, Wuhan, China, 13–14 September 2010; pp. 321–324. [ Google Scholar ]
- Nimmagadda, S.L.; Nimmagadda, S.K.; Dreher, H. Multidimensional Data Warehousing & Mining of Diabetes & Food-Domain Ontologies for e-Health. In Proceedings of the 9th IEEE International Conference on Industrial Informatics, Lisbon, Portugal, 26–29 July 2011; pp. 682–687. [ Google Scholar ]
- Bennett, C.; Doub, T.; Bragg, A.; Luellen, J.; Regenmorter, C.V.; Lockman, J.; Reiserer, R. Data Mining Session-Based Patient Reported Outcomes (PROs) in Mental Health Setting: Toward Data-Driven Clinical Decision Support and Personalized Treatment. In Proceedings of the 1st International Conference on Healthcare Informatics, Imaging and Systems Biology, San Jose, CA, USA, 26–29 July 2011. [ Google Scholar ]
- Seebock, P. Unsupervised identification of disease marker candidates in retinal OCT imaging data. IEEE Trans. Med. Imaging 2019 , 38 , 1037–1047. [ Google Scholar ] [ CrossRef ] [ PubMed ] [ Green Version ]
- McGregor, C. Health Analytics as a Service with Artemis Cloud: Service Availability. In Proceedings of the 42nd Annual International Conference of the IEEE Engineering in Medicine & Biology Society, Montreal, QC, Canada, 20–24 July 2020; pp. 5644–5648. [ Google Scholar ]
- Albu, A. From Logical Inference to Decision Trees in Medical Diagnosis. In Proceedings of the E-Health and Bioengineering Conference, Sinaia, Romania, 22–24 June 2017; pp. 65–68. [ Google Scholar ]
- Patii, N.; Iyer, B. Health Monitoring and Tracking System for Soldiers using Internet of Things (IoT). In Proceedings of the International Conference on Computing, Communication and Automation, Greater Noida, India, 5–6 May 2017; pp. 1347–1352. [ Google Scholar ]
- Yang, G. IoT-based remote pain monitoring system: From device to cloud platform. IEEE J. Biomed. Health Inform. 2018 , 22 , 1711–1719. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Ciprian, C.; Masychev, K.; Ravan, M.; Reilly, J.P.; Maccrimmon, D. A machine learning approach using effective connectivity to predict response to clozapine treatment. IEEE Trans. Neural Syst. Rehabil. Eng. 2020 , 28 , 2598–2607. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Zhou, R.; Zhang, X.; Wang, X.; Yang, G.; Guizani, N.; Du, X. Efficient and traceable patient health data search system for hospital management in smart cities. IEEE Internet Things J. 2021 , 8 , 6425–6436. [ Google Scholar ] [ CrossRef ]
- Hassan, T.; Hameed, A.; Nisar, S.; Kamal, N.; Hasan, O. Al-Zahrawi: A telesurgical robotic system for minimal invasive surgery. IEEE Syst. J. 2016 , 10 , 1035–1045. [ Google Scholar ] [ CrossRef ]
- Rahman, M.A.; Abualsaud, K.; Barnes, S.; Rashid, M.; Abdullah, S.M. A Natural User Interface and Blockchain-Based in-Home Smart Health Monitoring System. In Proceedings of the IEEE International Conference on Informatics, IoT, and Enabling Technologies, Doha, Qatar, 2–5 February 2020; pp. 262–266. [ Google Scholar ]
- Sakkos, D.; Mccay, K.D.; Marcroft, C.; Embleton, N.D.; Chattopadhyay, S.; Ho, E.S.L. Identification of abnormal movements in infants: A deep neural network for body part-based prediction of cerebral palsy. IEEE Access 2021 , 9 , 94281–94292. [ Google Scholar ] [ CrossRef ]
- Kumar, S.; Raut, R.D.; Narkhede, B.E. A proposed collaborative framework by using artificial intelligence-internet of things (AI-IoT) in COVID-19 pandemic situation for healthcare workers. Int. J. Healthc. Manag. 2020 , 13 , 337–345. [ Google Scholar ] [ CrossRef ]
- Khan, M.; Yaseen, Q.; Mumtaz, A.; Saleem, A.; Ishaq, S.; Udeen, H. Severe Analysis of Cardiac Disease Detection using the Wearable Device by Artificial Intelligence. In Proceedings of the International Conference for Innovation in Technology, Bangalore, India, 6–8 November 2020; pp. 1–8. [ Google Scholar ]
- Chauhan, T.; Rawat, S.; Malik, S.; Singh, P. Supervised and Unsupervised Machine Learning Based Review on Diabetes Care. In Proceedings of the 7th International Conference on Advanced Computing and Communication Systems, Coimbatore, India, 19–20 March 2021; pp. 581–585. [ Google Scholar ]
- Ahmed, I.; Jeon, G.; Piccialli, F. A Deep-Learning-based smart healthcare system for patient’s discomfort detection at the edge of Internet of Things. IEEE Internet Things J. 2021 , 8 , 10318–11032. [ Google Scholar ] [ CrossRef ]
- Wu, H.; Bowers, D.M.; Huynh, T.T.; Souvenir, R. Biomedical Video Denoising using Supervised Manifold Learning. In Proceedings of the IEEE 10th International Symposium on Biomedical Imaging, San Francisco, CA, USA, 7–11 April 2013; pp. 1244–1247. [ Google Scholar ]
- Zhang, Y. Collaborative unsupervised domain adaptation for medical image diagnosis. IEEE Trans. Image Process. 2020 , 29 , 7834–7844. [ Google Scholar ] [ CrossRef ]
- Azghadi, M.R. Hardware implementation of deep network accelerators towards healthcare and biomedical applications. IEEE Trans. Biomed. Circuits Syst. 2020 , 14 , 1138–1159. [ Google Scholar ] [ CrossRef ]
- Yanhong, F.; Bin, W.; Fengjuan, H.; Wenqiang, T. Research on Teleoperation Surgery Simulation System Based on Virtual Reality. In Proceedings of the 11th World Congress on Intelligent Control and Automation, Shenyang, China, 29 June–4 July 2014; pp. 5830–5834. [ Google Scholar ]
- Shim, S.; Ji, D.; Lee, S.; Choi, H.; Hong, J. Compact bone surgery robot with a high-resolution and high-rigidity remote center of motion mechanism. IEEE Trans. Biomed. Eng. 2020 , 67 , 2497–2506. [ Google Scholar ] [ CrossRef ]
- Gayathri, B.M.; Sumathi, C.P. Mamdani Fuzzy Inference System for Breast Cancer Risk Detection. In Proceedings of the International Conference on Computational Intelligence and Computing Research, Tamil Nadu, India, 10–12 December 2015; pp. 1–6. [ Google Scholar ]
- Katarya, R.; Srinivas, P. Predicting Heart Disease at Early Stages using Machine Learning: A Survey. In Proceedings of the International Conference on Electronics and Sustainable Communication Systems, Coimbatore, India, 2–4 July 2020; pp. 302–305. [ Google Scholar ]
- Harinishree, M.S.; Aditya, C.R.; Sachin, D.N. Detection of Breast Cancer using Machine Learning Algorithms—A Survey. In Proceedings of the 5th International Conference on Computing Methodologies and Communication, Erode, India, 8–10 April 2021; pp. 1598–1601. [ Google Scholar ]
- Amrane, M.; Oukid, S.; Gagaoua, I.; Ensari, T. Breast Cancer Classification using Machine Learning. In Proceedings of the Electric Electronics, Computer Science, Biomedical Engineerings’ Meeting, Istanbul, Turkey, 18–19 April 2018; pp. 1–4. [ Google Scholar ]
- Murray, M.; Macedo, M.; Glynn, C. Delivering Health Intelligence for Healthcare Services. In Proceedings of the 1st International Conference on Digital Data Processing, London, UK, 15–17 November 2019; pp. 88–91. [ Google Scholar ]
- Wong, D.L.T. An integrated wearable wireless vital signs biosensor for continuous inpatient monitoring. IEEE Sens. J. 2020 , 20 , 448–462. [ Google Scholar ] [ CrossRef ]
- Sasubilli, S.M.; Kumar, A.; Dutt, V. Machine Learning Implementation on Medical Domain to Identify Disease Insights using TMS. In Proceedings of the International Conference on Advances in Computing and Communication Engineering, Las Vegas, NV, USA, 22–24 June 2020; pp. 1–4. [ Google Scholar ]
- Razaak, M.; Martini, M.G.; Savino, K. A study on quality assessment for medical ultrasound video compressed via HEVC. IEEE J. Biomed. Health Inform. 2014 , 18 , 1552–1559. [ Google Scholar ] [ CrossRef ] [ Green Version ]
- Roa, D.; Bautista, J.; Rodríguez, N.; Villamil, M.P.; Jimenez, A.; Bernal, O. Data Mining: A New Opportunity to Support the Solution of Public Health Issues in Colombia. In Proceedings of the 6th Colombian Computing Congress, Manizales, Colombia, 4–6 May 2011; pp. 1–6. [ Google Scholar ]
- Rawte, V.; Anuradha, G. Fraud Detection in Health Insurance using Data Mining Techniques. In Proceedings of the International Conference on Communication, Information & Computing Technology, Mumbai, India, 15–17 January 2015; pp. 1–5. [ Google Scholar ]
- Daltayanni, M.; Wang, C.; Akella, R. A Fast-Interactive Search System for Healthcare Services. In Proceedings of the Annual SRII Global Conference, San Jose, CA, USA, 24–27 July 2012; pp. 525–534. [ Google Scholar ]
- Gangopadhyay, A.; Chen, S. Health Care Fraud Detection with Community Detection Algorithms. In Proceedings of the International Conference on Smart Computing, St. Louis, MO, USA, 18–20 May 2016; pp. 1–5. [ Google Scholar ]
- Anbarasi, M.S.; Dhivya, S. Fraud Detection using Outlier Predictor in Health Insurance Data. In Proceedings of the International Conference on Information Communication and Embedded Systems, Chennai, India, 23–24 February 2017; pp. 1–6. [ Google Scholar ]
- Thorntonl, D.; Capelleveen, G.; Poe, M. Outlier-based health insurance fraud detection for U.S. Medicaid data. Int. J. Enterp. Inf. Syst. 2015 , 27 , 684–694. [ Google Scholar ]
- Yang, W.S.; Hwang, S.Y. A hybrid approach for fraud detection in health insurance. Expert Syst. Appl. 2014 , 31 , 56–68. [ Google Scholar ] [ CrossRef ]
- Bagde, P.R.; Chaudhari, M.S. Analysis of fraud detection mechanism in health insurance using statistical data mining techniques. Int. J. Comput. Sci. Inf. Technol. 2016 , 7 , 925–926. [ Google Scholar ]
- Jumelle, A.K.L. Ethical Assessment in e-Health. In Proceedings of the 16th International Conference on e-Health Networking, Applications and Services, Natal, Brazil, 15–18 October 2014; pp. 262–268. [ Google Scholar ]
- Paranjape, K.; Schinkel, M.; Panday, R.N.; Car, J.; Nanayakkara, P. Introducing artificial intelligence training in medical education. JMIR Med. Educ. 2019 , 5 , e16048. [ Google Scholar ] [ CrossRef ]
- Torner, J.; Skouras, S.; Molinuevo, J.L.; Gispert, J.D.; Alpiste, F. Multipurpose virtual reality environment for biomedical and health applications. IEEE Trans. Neural Syst. Rehabil. Eng. 2019 , 27 , 1511–1520. [ Google Scholar ] [ CrossRef ]
- Gupta, A.; Cecil, J.; Pirela-Cruz, M.; Ramanathan, P. A virtual reality enhanced cyber-human framework for orthopedic surgical training. IEEE Syst. J. 2019 , 13 , 3501–3512. [ Google Scholar ] [ CrossRef ]
- Rahman, M.M.; Khatun, F.; Uzzaman, A.; Sami, S.I.; Bhuiyan, M.A.A.; Kiong, T.S. A comprehensive study of artificial intelligence and machine learning approaches in confronting the coronavirus (COVID-19) pandemic. Int. J. Health Serv. 2021 , 51 , 446–461. [ Google Scholar ] [ CrossRef ]
- Ling, Y.; An, Y.; Liu, M.; Hu, X. An Error Detecting and Tagging Framework for Reducing Data Entry Errors in Electronic Medical Records (EMR) System. In Proceedings of the International Conference on Bioinformatics and Biomedicine, Shanghai, China, 18–21 December 2013; pp. 249–254. [ Google Scholar ]
- Hasan, M.; Fukuda, A.; Maruf, R.I.; Yokota, F.; Ahmed, A. Errors in Remote Healthcare System: Where, How and by Whom? In Proceedings of the TENCON 2017—2017 IEEE Region 10 Conference, Penang, Malaysia, 5–8 November 2017; pp. 170–175. [ Google Scholar ]
- Goldberg, S.I. A Weighty Problem: Identification, Characteristics and Risk Factors for Errors in EMR Data. In Proceedings of the AMIA Annual Symposium Proceedings, Washington, DC, USA, 13–17 November 2010; pp. 251–255. [ Google Scholar ]
- Madanan, M.; Zulkefli, N.A.M.; Velayudhan, N.C. Designing a Hybrid Artificial Intelligent Clinical Decision Support System using Artificial Neural Network and Artificial Bee Colony for Predicting Heart Failure Rate. In Proceedings of the International Conference on Computer Communication and Informatics, Coimbatore, India, 19–22 July 2021; pp. 1–7. [ Google Scholar ]
- Aljaaf, A.J.; Al-Jumeily, D.; Hussain, A.J.; Fergus, P.; Al-Jumaily, M.; Abdel-Aziz, K. Toward an Optimal Use of Artificial Intelligence Techniques within a Clinical Decision Support System. In Proceedings of the Science and Information Conference, London, UK, 28–30 July 2015; pp. 548–554. [ Google Scholar ]
- Kusano, T.; Paliyawan, P.; Harada, T.; Thawonmas, R. Towards Adaptive Motion Gaming AI with Player’s Behavior Modeling for Health Promotion. In Proceedings of the 6th Global Conference on Consumer Electronics, Nagoya, Japan, 24–27 October 2017; pp. 1–2. [ Google Scholar ]
- Srivastava, B.; Rossi, F. Rating AI systems for bias to promote trustable applications. IBM J. Res. Dev. 2019 , 63 , 51–59. [ Google Scholar ] [ CrossRef ]
- Lim, A.K.; Thumper, C. Opportunities and Challenges of Internet-Based Health Interventions in the Future Internet. In Proceedings of the 12th International Conference on Information Technology—New Generations, Las Vegas, NV, USA, 13–15 April 2015; pp. 567–573. [ Google Scholar ]
- Mohr, D.C.; Cuijpers, P.; Lehman, K. Supportive accountability: A model for providing human support to enhance adherence to eHealth interventions. J. Med. Internet Res. 2011 , 13 , 30e. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Tsang, K.C.H.; Pinnock, H.; Wilson, A.M.; Shah, S.A. Application of Machine Learning to Support Self-Management of Asthma with mHealth. In Proceedings of the 42nd Annual International Conference of the IEEE Engineering in Medicine & Biology Society, Montreal, QC, Canada, 20–24 July 2020; pp. 5673–5677. [ Google Scholar ]
- Floridi, L.; Cowls, J.; Beltrametti, M.; Chatila, R.; Chazerand, P.; Dignum, V.; Vayena, E. AI4People—An ethical framework for a good AI society: Opportunities, risks, principles, and recommendations. Minds Mach. 2018 , 28 , 689–707. [ Google Scholar ] [ CrossRef ] [ PubMed ] [ Green Version ]
- Scott, B.K.; Miller, G.T.; Fonda, S.J.; Yeaw, R.E.; Gaudaen, J.C.; Pavliscsak, H.H.; Pamplin, J.C. Advanced digital health technologies for COVID-19 and future emergencies. Telemed. E-Health 2020 , 26 , 1226–1233. [ Google Scholar ] [ CrossRef ]
- Schwalbe, N.; Wahl, B. Artificial intelligence and the future of global health. Lancet 2020 , 395 , 1579–1586. [ Google Scholar ] [ CrossRef ]
- Secinaro, S.; Calandra, D.; Secinaro, A.; Muthurangu, V.; Biancone, P. The role of artificial intelligence in healthcare: A structured literature review. BMC Med. Inform. Decis. Mak. 2021 , 21 , 125. [ Google Scholar ] [ CrossRef ]
- Morley, J.; Machado, C.C.; Burr, C.; Cowls, J.; Joshi, I.; Taddeo, M.; Floridi, L. The ethics of AI in health care: A mapping review. Soc. Sci. Med. 2020 , 260 , 113172. [ Google Scholar ] [ CrossRef ]
- Sood, S.K.; Rawat, K.S.; Kumar, D. A visual review of artificial intelligence and Industry 4.0 in healthcare. Comput. Electr. Eng. 2022 , 101 , 107948. [ Google Scholar ] [ CrossRef ]
- Jobin, A.; Ienca, M.; Vayena, E. The global landscape of AI ethics guidelines. Nat. Mach. Intell. 2019 , 1 , 389–399. [ Google Scholar ] [ CrossRef ] [ Green Version ]
- Zerka, F. Blockchain for privacy preserving and trustworthy distributed machine learning in multi-centric medical imaging (C-DistriM). IEEE Access 2020 , 8 , 183939–183951. [ Google Scholar ] [ CrossRef ]
- Peters, D.; Vold, K.; Robinson, D.; Calvo, R.A. Responsible AI—Two frameworks for ethical design practice. IEEE Trans. Technol. Soc. 2020 , 1 , 34–47. [ Google Scholar ] [ CrossRef ]
- Wang, S. Big data privacy in biomedical research. IEEE Trans. Big Data 2020 , 6 , 296–308. [ Google Scholar ] [ CrossRef ]
- Jameel, T.; Ali, R.; Toheed, I. Ethics of Artificial Intelligence: Research Challenges and Potential Solutions. In Proceedings of the 3rd International Conference on Computing, Mathematics and Engineering Technologies, Sukkur, Pakistan, 29–30 January 2020; pp. 1–6. [ Google Scholar ]
- Richie, C. Environmentally sustainable development and use of artificial intelligence in health care. Bioethics 2022 , 36 , 547–555. [ Google Scholar ] [ CrossRef ]
- Bryson, J.J. Patiency is not a virtue: The design of intelligent systems and systems of ethics. Ethics Inf. Technol. 2018 , 20 , 15–26. [ Google Scholar ] [ CrossRef ] [ Green Version ]
- Esmaeilzadeh, P. Use of AI-based tools for healthcare purposes: A survey study from consumers’ perspectives. BMC Med. Inform. Decis. Mak. 2020 , 20 , 170. [ Google Scholar ] [ CrossRef ]
- Shaban-Nejad, A.; Michalowski, M.; Brownstein, J.S.; Buckeridge, D.L. Guest editorial explainable AI: Towards fairness, accountability, transparency and trust in healthcare. IEEE J. Biomed. Health Inform. 2021 , 25 , 2374–2375. [ Google Scholar ] [ CrossRef ]
- Chun, R. Ethical character and virtue of organizations: An empirical assessment and strategic implications. J. Bus. Ethics 2005 , 57 , 269–284. [ Google Scholar ] [ CrossRef ]
- Song, S.Y.; Kim, Y.K. Theory of virtue ethics: Do consumers’ good traits predict their socially responsible consumption? J. Bus. Ethics 2018 , 152 , 1159–1175. [ Google Scholar ] [ CrossRef ]
- Chatterjee, S.; Sarker, S.; Fuller, M. A deontological approach to designing ethical collaboration. J. Assoc. Inf. Syst. 2009 , 10 , 138–169. [ Google Scholar ] [ CrossRef ] [ Green Version ]
- Audi, R. Virtue ethics as a resource in business. Bus. Ethics Q. 2012 , 22 , 273–291. [ Google Scholar ] [ CrossRef ] [ Green Version ]
- Unberath, M.; Ghobadi, K.; Levin, S.; Hinson, J.; Hager, G.D. Artificial Intelligence-Based Clinical Decision Support for COVID-19—Where Art Thou? Adv. Intell. Syst. 2020 , 2 , 2000104. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Chakrabarty, S.; Bass, A.E. Comparing virtue, consequentialist, and deontological ethics-based corporate social responsibility: Mitigating microfinance risk in institutional voids. J. Bus. Ethics 2015 , 126 , 487–512. [ Google Scholar ] [ CrossRef ]
- Vaishya, R.; Javaid, M.; Khan, I.H.; Haleem, A. Artificial Intelligence (AI) applications for COVID-19 pandemic. Diabetes Metab. Syndr. Clin. Res. Rev. 2020 , 14 , 337–339. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Rigby, M.J. Ethical dimensions of using artificial intelligence in health care. AMA J. Ethics 2019 , 21 , 121–124. [ Google Scholar ]
- Van der Schaar, M.; Alaa, A.M.; Floto, A.; Gimson, A.; Scholtes, S.; Wood, A.; Ercole, A. How artificial intelligence and machine learning can help healthcare systems respond to COVID-19. Mach. Learn. 2021 , 110 , 1–14. [ Google Scholar ] [ CrossRef ]
- Combs, C.D.; Combs, P.F. Emerging roles of virtual patients in the age of AI. AMA J. Ethics 2019 , 21 , E153–E159. [ Google Scholar ]
- Yu, K.H.; Beam, A.L.; Kohane, I.S. Artificial intelligence in healthcare. Nat. Biomed. Eng. 2018 , 2 , 719–731. [ Google Scholar ] [ CrossRef ]
- Powell, J. Trust Me, I’m a chatbot: How artificial intelligence in health care fails the turing test. J. Med. Internet Res. 2019 , 21 , e16222. [ Google Scholar ] [ CrossRef ]
- Abràmoff, M.D.; Leng, T.; Ting, D.S.; Rhee, K.; Horton, M.B.; Brady, C.J.; Chiang, M.F. Automated and computer-assisted detection, classification, and diagnosis of diabetic retinopathy. Telemed. E-Health 2020 , 26 , 544–550. [ Google Scholar ] [ CrossRef ] [ Green Version ]
- McCall, B. COVID-19 and artificial intelligence: Protecting health-care workers and curbing the spread. Lancet Digit. Health 2020 , 2 , e166–e167. [ Google Scholar ] [ CrossRef ]
- Lee, D.; Yoon, S.N. Application of artificial intelligence-based technologies in the healthcare industry: Opportunities and challenges. Int. J. Environ. Res. Public Health 2021 , 18 , 271. [ Google Scholar ] [ CrossRef ]
- Lee, S.; Lee, D. Healthcare wearable devices: An analysis of key factors for continuous use intention. Serv. Bus. 2020 , 14 , 503–531. [ Google Scholar ] [ CrossRef ]
- Yoon, S.; Lee, D. Artificial Intelligence and Robots in Healthcare: What are the Success Factors for Technology-based ServiceEncounters? Int. J. Healthc. Manag. 2019 , 12 , 218–225. [ Google Scholar ] [ CrossRef ]
- Chen, J.; See, K.C. Artificial intelligence for COVID-19: Rapid review. J. Med. Internet Res. 2020 , 22 , e21476. [ Google Scholar ] [ CrossRef ]
- Katiyar, S.; Farhana, A. Artificial Intelligence in e-Health: A Review of Current Status in Healthcare and Future Possible Scope of Research. J. Comput. Sci. 2022 , 18 , 928–939. [ Google Scholar ] [ CrossRef ]
- Kumar, Y.; Koul, A.; Singla, R.; Ijaz, M.F. Artificial intelligence in disease diagnosis: A systematic literature review, synthesizing framework and future research agenda. J. Ambient Intell. Humaniz. Comput. 2023 , 14 , 8459–8486. [ Google Scholar ] [ CrossRef ]
- Singh, A.; Mehta, J.C.; Anand, D.; Nath, P.; Pandey, B.; Khamparia, A. An intelligent hybrid approach for hepatitis disease diagnosis: Combining enhanced k-means clustering and improved ensemble learning. Expert Syst. 2021 , 38 , e12526. [ Google Scholar ] [ CrossRef ]
- Gulati, K.; Nayak, K.M.; Priya, B.S.; Venkatesh, B.; Satyam, Y.; Chahal, D. An Examination of How Robots, Artificial Intelligence, and Machinery Learning are Being Applied in the Medical and Healthcare Industries. Int. J. Recent Innov. Trends Comput. Commun. 2022 , 10 , 298–305. [ Google Scholar ] [ CrossRef ]
- Calton, B.; Abedini, N.; Fratkin, M. Telemedicine in the time of coronavirus. J. Pain Symptom Manag. 2020 , 60 , e12–e14. [ Google Scholar ] [ CrossRef ]
- Srivastava, S.; Pant, M.; Agarwal, R. Role of AI techniques and deep learning in analyzing the critical health conditions. Int. J. Syst. Assur. Eng. Manag. 2020 , 11 , 350–365. [ Google Scholar ] [ CrossRef ]
- Xu, Y.; Wang, T.; Chen, Z.; Jin, L.; Wu, Z.; Yan, J.; He, N. The point-of-care-testing of nucleic acids by chip, cartridge and paper sensors. Chin. Chem. Lett. 2021 , 32 , 3675–3686. [ Google Scholar ] [ CrossRef ]
Click here to enlarge figure
| Authors | Year | Methodology |
|---|---|---|
| Mahdi et al. [ ] | 2023 | In areas where AI is now playing a substantial role in clinical dentistry, this study attempts to systematically review that role. |
| Vishwakarma et al. [ ] | 2023 | The purpose of this study is to comprehend how AI helps create a robust and sustainable healthcare system. |
| Ali et al. [ ] | 2023 | This paper gives a thorough analysis of scholarly works on the use of AI in the healthcare industry. A total of 180 articles have been examined to present a classification framework based on four dimensions: AI-enabled healthcare benefits, challenges, methodologies, and functionalities. |
| Siala and Wang [ ] | 2022 | This paper suggests a responsible AI initiative framework that includes five key themes for AI solution developers, healthcare professionals, and policy makers by combining pertinent knowledge from AI governance and ethics. These themes include inclusivity, fairness, inclusivity, sustainability, and transparency. A total of 253 papers were extracted from two databases. |
| The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
Share and Cite
Kitsios, F.; Kamariotou, M.; Syngelakis, A.I.; Talias, M.A. Recent Advances of Artificial Intelligence in Healthcare: A Systematic Literature Review. Appl. Sci. 2023 , 13 , 7479. https://doi.org/10.3390/app13137479
Kitsios F, Kamariotou M, Syngelakis AI, Talias MA. Recent Advances of Artificial Intelligence in Healthcare: A Systematic Literature Review. Applied Sciences . 2023; 13(13):7479. https://doi.org/10.3390/app13137479
Kitsios, Fotis, Maria Kamariotou, Aristomenis I. Syngelakis, and Michael A. Talias. 2023. "Recent Advances of Artificial Intelligence in Healthcare: A Systematic Literature Review" Applied Sciences 13, no. 13: 7479. https://doi.org/10.3390/app13137479
Article Metrics
Article access statistics, further information, mdpi initiatives, follow mdpi.

Subscribe to receive issue release notifications and newsletters from MDPI journals
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Review Article
- Published: 10 October 2018
Artificial intelligence in healthcare
- Kun-Hsing Yu ORCID: orcid.org/0000-0001-9892-8218 1 ,
- Andrew L. Beam 1 &
- Isaac S. Kohane 1 , 2
Nature Biomedical Engineering volume 2 , pages 719–731 ( 2018 ) Cite this article
43k Accesses
1441 Citations
109 Altmetric
Metrics details
- Computational models
- Machine learning
- Predictive medicine
Artificial intelligence (AI) is gradually changing medical practice. With recent progress in digitized data acquisition, machine learning and computing infrastructure, AI applications are expanding into areas that were previously thought to be only the province of human experts. In this Review Article, we outline recent breakthroughs in AI technologies and their biomedical applications, identify the challenges for further progress in medical AI systems, and summarize the economic, legal and social implications of AI in healthcare.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
24,99 € / 30 days
cancel any time
Subscribe to this journal
Receive 12 digital issues and online access to articles
92,52 € per year
only 7,71 € per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
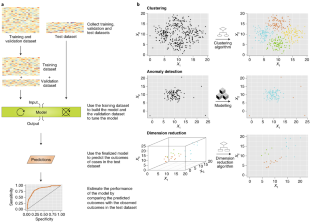
Similar content being viewed by others
A short guide for medical professionals in the era of artificial intelligence

The potential for artificial intelligence to transform healthcare: perspectives from international health leaders
Guiding principles for the responsible development of artificial intelligence tools for healthcare.
Simonite, T. Google’s AI eye doctor gets ready to go to work in India. WIRED (6 August 2017).
Lee, R., Wong, T. Y. & Sabanayagam, C. Epidemiology of diabetic retinopathy, diabetic macular edema and related vision loss. Eye Vis. 2 , 17 (2015).
Article Google Scholar
Lin, D. Y., Blumenkranz, M. S., Brothers, R. J. & Grosvenor, D. M. The sensitivity and specificity of single-field nonmydriatic monochromatic digital fundus photography with remote image interpretation for diabetic retinopathy screening: a comparison with ophthalmoscopy and standardized mydriatic color photography. Am. J. Ophthalmol. 134 , 204–213 (2002).
Article PubMed Google Scholar
Zheng, Y., He, M. & Congdon, N. The worldwide epidemic of diabetic retinopathy. Indian J. Ophthalmol. 60 , 428–431 (2012).
Article PubMed PubMed Central Google Scholar
Gulshan, V. et al. Development and validation of a deep learning algorithm for detection of diabetic retinopathy in retinal fundus photographs. JAMA 316 , 2402–2410 (2016).
Poplin, R. et al. Prediction of cardiovascular risk factors from retinal fundus photographs via deep learning. Nat. Biomed. Eng. 2 , 158–164 (2018).
Abràmoff, M. D., Lavin, P. T., Birch, M., Shah, N. & Folk, J. C. Pivotal trial of an autonomous AI-based diagnostic system for detection of diabetic retinopathy in primary care offices. NPJ Digit. Med. 1 , 39 (2018).
Russell, S. J. & Norvig, P. Artificial Intelligence: A Modern Approach (Prentice Hall, New Jersey, 2010).
Krizhevsky, A., Sutskever, I. & Hinton, G. E. in Advances in Neural Information Processing Systems 1097–1105 (Curran Associates, Nevada, 2012).
Lewis-Kraus, G. The great A.I. awakening. The New York Times Magazine (14 December 2016).
Kundu, M., Nasipuri, M. & Basu, D. K. Knowledge-based ECG interpretation: a critical review. Pattern Recognit. 33 , 351–373 (2000).
Jha, S. & Topol, E. J. Adapting to artificial intelligence: radiologists and pathologists as information specialists. JAMA 316 , 2353–2354 (2016).
Golub, T. R. et al. Molecular classification of cancer: class discovery and class prediction by gene expression monitoring. Science 286 , 531–537 (1999).
Article CAS PubMed Google Scholar
Wang, Y. et al. Gene selection from microarray data for cancer classification—a machine learning approach. Comput. Biol. Chem. 29 , 37–46 (2005).
Article PubMed CAS Google Scholar
Yu, K. H. et al. Predicting ovarian cancer patients’ clinical response to platinum-based chemotherapy by their tumor proteomic signatures. J. Proteome Res. 15 , 2455–2465 (2016).
Article CAS PubMed PubMed Central Google Scholar
Yu, K. H. et al. Omics AnalySIs System for PRecision Oncology (OASISPRO): a web-based omics analysis tool for clinical phenotype prediction. Bioinformatics 34 , 319–320 (2017).
Article CAS PubMed Central Google Scholar
Check Hayden, E. The automated lab. Nature 516 , 131–132 (2014).
Miller, R. A. Medical diagnostic decision support systems–past, present, and future: a threaded bibliography and brief commentary. J. Am. Med. Inform. Assoc. 1 , 8–27 (1994).
Musen, M. A., Middleton, B. & Greenes, R. A. in Biomedical Informatics (eds Shortliffe, E. H. & Cimino, J. J.) 643–674 (Springer, London, 2014).
Shortliffe, E. Computer-Based Medical Consultations: MYCIN Vol. 2 (Elsevier, New York, 2012).
Chapter Google Scholar
Szolovits, P., Patil, R. S. & Schwartz, W. B. Artificial intelligence in medical diagnosis. Ann. Intern. Med. 108 , 80–87 (1988).
de Dombal, F. T., Leaper, D. J., Staniland, J. R., McCann, A. P. & Horrocks, J. C. Computer-aided diagnosis of acute abdominal pain. Br. Med. J. 2 , 9–13 (1972).
Shortliffe, E. H. et al. Computer-based consultations in clinical therapeutics: explanation and rule acquisition capabilities of the MYCIN system. Comput. Biomed. Res. 8 , 303–320 (1975).
Barnett, G. O., Cimino, J. J., Hupp, J. A. & Hoffer, E. P. DXplain. An evolving diagnostic decision-support system . JAMA 258 , 67–74 (1987).
Miller, R. A., McNeil, M. A., Challinor, S. M., Masarie, F. E. Jr & Myers, J. D. The INTERNIST-1/QUICK MEDICAL REFERENCE Project — status report. Western J. Med. 145 , 816–822 (1986).
Berner, E. S. et al. Performance of four computer-based diagnostic systems. N. Engl. J. Med. 330 , 1792–1796 (1994).
Szolovits, P. & Pauker, S. G. Categorical and probabilistic reasoning in medical diagnosis. Artif. Intell. 11 , 115–144 (1978).
Deo, R. C. Machine learning in medicine. Circulation 132 , 1920–1930 (2015).
Yu, K. H. & Snyder, M. Omics profiling in precision oncology. Mol. Cell. Proteomics 15 , 2525–2536 (2016).
Roberts, K. et al. Biomedical informatics advancing the national health agenda: the AMIA 2015 year-in-review in clinical and consumer informatics. J. Am. Med. Inform. Assoc. 24 , 185–190 (2017).
Cloud AutoML ALPHA (Google Cloud); https://cloud.google.com/automl/
Goodfellow, I., Bengio, Y., Courville, A. & Bengio, Y. Deep Learning 1 (MIT Press, Cambridge, 2016).
Google Scholar
Gill, N. S. Overview and applications of artificial neural networks. Xenonstack https://www.xenonstack.com/blog/data-science/artificial-neural-networks-applications-algorithms/ (2017).
TOP500 List – November 2006 (TOP500); https://www.top500.org/list/2006/11/
Beam, A. L. & Kohane, I. S. Translating artificial intelligence into clinical care. JAMA 316 , 2368–2369 (2016).
Kamentsky, L. et al. Improved structure, function and compatibility for CellProfiler: modular high-throughput image analysis software. Bioinformatics 27 , 1179–1180 (2011).
Ching, T. et al. Opportunities and obstacles for deep learning in biology and medicine. J. R. Soc. Interface 15 , 20170387 (2018).
Tomczak, K., Czerwinska, P. & Wiznerowicz, M. The Cancer Genome Atlas (TCGA): an immeasurable source of knowledge. Contemp. Oncol. 19 , 68–77 (2015).
Sudlow, C. et al. UK biobank: an open access resource for identifying the causes of a wide range of complex diseases of middle and old age. PLoS Med. 12 , e1001779 (2015).
Ljosa, V., Sokolnicki, K. L. & Carpenter, A. E. Annotated high-throughput microscopy image sets for validation. Nat. Methods 9 , 637 (2012).
Williams, E. et al. The image data resource: a bioimage data integration and publication platform. Nat. Methods 14 , 775–781 (2017).
DesRoches, C. M. et al. Electronic health records in ambulatory care–a national survey of physicians. N. Engl. J. Med. 359 , 50–60 (2008).
Hsiao, C. J. et al. Office-based physicians are responding to incentives and assistance by adopting and using electronic health records. Health Aff. 32 , 1470–1477 (2013).
Esteva, A. et al. Dermatologist-level classification of skin cancer with deep neural networks. Nature 542 , 115–118 (2017).
Beck, A. H. et al. Systematic analysis of breast cancer morphology uncovers stromal features associated with survival. Sci. Transl. Med. 3 , 108ra113 (2011).
Yu, K. H. et al. Predicting non-small cell lung cancer prognosis by fully automated microscopic pathology image features. Nat. Commun. 7 , 12474 (2016).
Shademan, A. et al. Supervised autonomous robotic soft tissue surgery. Sci. Transl. Med. 8 , 337ra364 (2016).
Reed, J. C. Chest Radiology: Plain Film Patterns and Differential Diagnoses (Elsevier Health Sciences, Philadelphia, 2010).
Lodwick, G. S., Haun, C. L., Smith, W. E., Keller, R. F. & Robertson, E. D. Computer diagnosis of primary bone tumors: a preliminary report. Radiology 80 , 273–275 (1963).
van Ginneken, B., Setio, A. A., Jacobs, C. & Ciompi, F. Off-the-shelf convolutional neural network features for pulmonary nodule detection in computed tomography scans. In IEEE 12th International Symposium Biomedical Imaging (ISBI) 286–289 (IEEE, 2015).
Lakhani, P. & Sundaram, B. Deep learning at chest radiography: automated classification of pulmonary tuberculosis by using convolutional neural networks. Radiology 284 , 574–582 (2017).
Wang, X. et al. ChestX-ray8: hospital-scale chest X-ray database and benchmarks on weakly-supervised classification and localization of common thorax diseases. Preprint at https://arxiv.org/abs/1705.02315 (2017).
Yao, L. et al. Learning to diagnose from scratch by exploiting dependencies among labels. Preprint at https://arxiv.org/abs/1710.10501 (2017).
Rajpurkar, P. et al. CheXNet: radiologist-level pneumonia detection on chest X-rays with deep learning. Preprint at https://arxiv.org/abs/1711.05225 (2017).
Samala, R. K. et al. Mass detection in digital breast tomosynthesis: deep convolutional neural network with transfer learning from mammography. Med. Phys. 43 , 6654–6666 (2016).
Arevalo, J., González, F. A., Ramos-Pollán, R., Oliveira, J. L. & Lopez, M. A. G. Convolutional neural networks for mammography mass lesion classification. In IEEE 37th Annual International Conference of the Engineering in Medicine and Biology Society (EMBC) 797–800 (IEEE, 2015).
510(k) Premarket Notification (FDA, 2017); https://www.accessdata.fda.gov/scripts/cdrh/cfdocs/cfpmn/pmn.cfm?ID=K163253
Marr, B. First FDA approval for clinical cloud-based deep learning in healthcare. Forbes (20 January 2017).
Rigel, D. S., Friedman, R. J., Kopf, A. W. & Polsky, D. ABCDE—an evolving concept in the early detection of melanoma. Arch. Dermatol. 141 , 1032–1034 (2005).
Thomas, L. et al. Semiological value of ABCDE criteria in the diagnosis of cutaneous pigmented tumors. Dermatology 197 , 11–17 (1998).
Ercal, F., Chawla, A., Stoecker, W. V., Lee, H. C. & Moss, R. H. Neural network diagnosis of malignant melanoma from color images. IEEE Trans. Biomed. Eng. 41 , 837–845 (1994).
Wolf, J. A. et al. Diagnostic inaccuracy of smartphone applications for melanoma detection. JAMA Dermatol. 149 , 422–426 (2013).
Panwar, N. et al. Fundus photography in the 21st century — a review of recent technological advances and their implications for worldwide healthcare. Telemed. J. E. Health 22 , 198–208 (2016).
American Diabetes Association. 10. Microvascular complications and foot care. Diabetes Care 40 , 88–98 (2017).
Menke, A., Casagrande, S., Geiss, L. & Cowie, C. C. Prevalence of and trends in diabetes among adults in the United States, 1988–2012. JAMA 314 , 1021–1029 (2015).
Abràmoff, M. D. et al. Improved automated detection of diabetic retinopathy on a publicly available dataset through integration of deep learning. Investigative Opthalmology Visual Sci. 57 , 5200–5206 (2016).
Rorke, L. B. Pathologic diagnosis as the gold standard. Cancer 79 , 665–667 (1997).
Lakhani, S. R. & Ashworth, A. Microarray and histopathological analysis of tumours: the future and the past? Nat. Rev. Cancer 1 , 151–157 (2001).
Rubegni, P. et al. Automated diagnosis of pigmented skin lesions. Int. J. Cancer 101 , 576–580 (2002).
Stang, A. et al. Diagnostic agreement in the histopathological evaluation of lung cancer tissue in a population-based case-control study. Lung Cancer 52 , 29–36 (2006).
Yu, K. H. et al. Association of omics features with histopathology patterns in lung adenocarcinoma. Cell Syst. 5 , 620–627 (2017).
Litjens, G. et al. Deep learning as a tool for increased accuracy and efficiency of histopathological diagnosis. Sci. Rep. 6 , 26286 (2016).
Bejnordi, B. E. et al. Machine learning detection of breast cancer lymph node metastases. JAMA 318 , 2199–2210 (2017).
Cireşan, D. C., Giusti, A., Gambardella, L. M. & Schmidhuber, J. in Medical Image Computing and Computer-Assisted Intervention — MICCAI 2013 (eds Mori, K. et al.) 411–418 (Springer, Berlin, Heidelberg, 2013).
Manak, M. S. et al. Live-cell phenotypic-biomarker microfluidic assay for the risk stratification of cancer patients via machine learning. Nat. Biomed. Eng. https://doi.org/10.1038/s41551-018-0285-z (2018).
Robboy, S. J. et al. Pathologist workforce in the United States: I. Development of a predictive model to examine factors influencing supply. Arch. Pathol. Lab. Med. 137 , 1723–1732 (2013).
Litjens, G. et al. A survey on deep learning in medical image analysis. Med. Image Anal. 42 , 60–88 (2017).
Quang, D., Chen, Y. & Xie, X. DANN: a deep learning approach for annotating the pathogenicity of genetic variants. Bioinformatics 31 , 761–763 (2015).
Quang, D. & Xie, X. DanQ: a hybrid convolutional and recurrent deep neural network for quantifying the function of DNA sequences. Nucleic Acids Res. 44 , e107 (2016).
Article PubMed PubMed Central CAS Google Scholar
DePristo, M. & Poplin, R. DeepVariant: highly accurate genomes with deep neural networks. Google AI Blog https://research.googleblog.com/2017/12/deepvariant-highly-accurate-genomes.html (2017).
Poplin, R. et al. Creating a universal SNP and small indel variant caller with deep neural networks. Preprint at https://www.biorxiv.org/content/early/2016/12/14/092890 (2018).
Kamps, R. et al. Next-generation sequencing in oncology: genetic diagnosis, risk prediction and cancer classification. Int. J. Mol. Sci. 18 , 308 (2017).
Article PubMed Central CAS Google Scholar
He, Z. & Yu, W. Stable feature selection for biomarker discovery. Comput. Biol. Chem. 34 , 215–225 (2010).
Zhang, Z. et al. Three biomarkers identified from serum proteomic analysis for the detection of early stage ovarian cancer. Cancer Res. 64 , 5882–5890 (2004).
Wallden, B. et al. Development and verification of the PAM50-based Prosigna breast cancer gene signature assay. BMC Med. Genomics 8 , 54 (2015).
Sweeney, T. E., Wong, H. R. & Khatri, P. Robust classification of bacterial and viral infections via integrated host gene expression diagnostics. Sci. Transl. Med. 8 , 346ra391 (2016).
Article CAS Google Scholar
Huang, T., Hoffman, B., Meschino, W., Kingdom, J. & Okun, N. Prediction of adverse pregnancy outcomes by combinations of first and second trimester biochemistry markers used in the routine prenatal screening of Down syndrome. Prenat. Diagn. 30 , 471–477 (2010).
PubMed Google Scholar
Mook, S. et al. Metastatic potential of T1 breast cancer can be predicted by the 70-gene MammaPrint signature. Ann. Surg. Oncol. 17 , 1406–1413 (2010).
Farina, D. et al. Man/machine interface based on the discharge timings of spinal motor neurons after targeted muscle reinnervation. Nat. Biomed. Eng. 1 , 0025 (2017).
Altman, R. B. Artificial intelligence (AI) systems for interpreting complex medical datasets. Clin. Pharmacol. Ther. 101 , 585–586 (2017).
Cai, X. et al. Real-time prediction of mortality, readmission, and length of stay using electronic health record data. J. Am. Med. Inform. Assoc. 23 , 553–561 (2016).
Makar, M., Ghassemi, M., Cutler, D. M. & Obermeyer, Z. Short-term mortality prediction for elderly patients using medicare claims data. Int. J. Mach. Learn. Comput. 5 , 192–197 (2015).
Ng, T., Chew, L. & Yap, C. W. A clinical decision support tool to predict survival in cancer patients beyond 120 days after palliative chemotherapy. J. Palliat. Med. 15 , 863–869 (2012).
Delen, D., Oztekin, A. & Kong, Z. J. A machine learning-based approach to prognostic analysis of thoracic transplantations. Artif. Intell. Med. 49 , 33–42 (2010).
Churpek, M. M. et al. Predicting cardiac arrest on the wards: a nested case-control study. Chest 141 , 1170–1176 (2012).
Churpek, M. M. et al. Multicenter development and validation of a risk stratification tool for ward patients. Am. J. Respir. Crit. Care Med. 190 , 649–655 (2014).
Lundberg, S. M. et al. Explainable machine-learning predictions for the prevention of hypoxaemia during surgery. Nat. Biomed. Eng. https://doi.org/10.1038/s41551-018-0304-0 (2018).
Li, X. et al. Digital health: tracking physiomes and activity using wearable biosensors reveals useful health-related information. PLoS Biol. 15 , e2001402 (2017).
Majumder, S., Mondal, T. & Deen, M. J. Wearable sensors for remote health monitoring. Sensors 17 , 130 (2017).
Article PubMed Central Google Scholar
Pastorino, M., Arredondo, M., Cancela, J. & Guillen, S. Wearable sensor network for health monitoring: the case of Parkinson disease. J. Phys. Conf. Ser. 450 , 012055 (2013).
Mercer, K., Li, M., Giangregorio, L., Burns, C. & Grindrod, K. Behavior change techniques present in wearable activity trackers: a critical analysis. JMIR Mhealth Uhealth 4 , e40 (2016).
Takacs, J. et al. Validation of the Fitbit One activity monitor device during treadmill walking. J. Sci. Med. Sport 17 , 496–500 (2014).
Yang, R., Shin, E., Newman, M. W. & Ackerman, M. S. When fitness trackers don’t ‘fit’: end-user difficulties in the assessment of personal tracking device accuracy. In Proceedings of the 2015 ACM International Joint Conference on Pervasive and Ubiquitous Computing 623–634 (ACM, 2015).
Endeavour Partners. Inside wearables: how the science of human behavior change offers the secret to long-term engagement. Medium https://blog.endeavour.partners/inside-wearable-how-the-science-of-human-behavior-change-offers-the-secret-to-long-term-engagement-a15b3c7d4cf3 (2017).
Herz, J. C. Wearables are totally failing the people who need them most. Wired (11 June 2014).
Clawson, J., Pater, J. A., Miller, A. D., Mynatt, E. D. & Mamykina, L. No longer wearing: investigating the abandonment of personal health-tracking technologies on Craigslist. In Proceedings of the 2015 ACM International Joint Conference on Pervasive and Ubiquitous Computing 647–658 (ACM, 2015).
Wheeler, M. J. Overview on robotics in the laboratory. Ann. Clin. Biochem. 44 , 209–218 (2007).
Moustris, G. P., Hiridis, S. C., Deliparaschos, K. M. & Konstantinidis, K. M. Evolution of autonomous and semi-autonomous robotic surgical systems: a review of the literature. Int. J. Med. Robot . 7 , 375–392 (2011).
Gomes, P. Surgical robotics: reviewing the past, analysing the present, imagining the future. Robot. Comput. Integr. Manuf. 27 , 261–266 (2011).
Majdani, O. et al. A robot-guided minimally invasive approach for cochlear implant surgery: preliminary results of a temporal bone study. Int. J. Comput. Assist. Radiol. Surg. 4 , 475–486 (2009).
Elek, R. et al. Recent trends in automating robotic surgery. In 2016 IEEE 20th Jubilee International Conference on Intelligent Engineering Systems (INES) 27–32 (IEEE, 2016).
Liew, C. The future of radiology augmented with artificial intelligence: a strategy for success. Eur. J. Radiol. 102 , 152–156 (2018).
Jones, L., Golan, D., Hanna, S. & Ramachandran, M. Artificial intelligence, machine learning and the evolution of healthcare: a bright future or cause for concern? Bone Joint Res. 7 , 223–225 (2018).
Obermeyer, Z. & Emanuel, E. J. Predicting the future — big data, machine learning, and clinical medicine. N. Engl. J. Med. 375 , 1216–1219 (2016).
Krause, J. et al. Grader variability and the importance of reference standards for evaluating machine learning models for diabetic retinopathy. Ophthalmology 125 , 1264–1272 (2018).
Rebholz-Schuhmann, D. et al. The CALBC silver standard corpus for biomedical named entities—a study in harmonizing the contributions from four independent named entity taggers. In LREC 568–573 (2010).
Kirby, J. C. et al. PheKB: a catalog and workflow for creating electronic phenotype algorithms for transportability. J. Am. Med. Inform. Assoc. 23 , 1046–1052 (2016).
Simonyan, K., Vedaldi, A. & Zisserman, A. Deep inside convolutional networks: visualising image classification models and saliency maps. Preprint at https://arxiv.org/abs/1312.6034 (2013).
Ribeiro, M. T., Singh, S. & Guestrin, C. “Why should I trust you?”: explaining the predictions of any classifier. Preprint at https://arxiv.org/abs/1602.04938 (2016).
LeCun, Y., Bengio, Y. & Hinton, G. Deep learning. Nature 521 , 436–444 (2015).
Boulanger-Lewandowski, N., Bengio, Y. & Vincent, P. Modeling temporal dependencies in high-dimensional sequences: application to polyphonic music generation and transcription. Preprint at https://arxiv.org/abs/1206.6392 (2012).
Zoph, B. & Le, Q. V. Neural architecture search with reinforcement learning. Preprint at https://arxiv.org/abs/1611.01578 (2016).
Lee, L. M. & Gostin, L. O. Ethical collection, storage, and use of public health data: a proposal for a national privacy protection. JAMA 302 , 82–84 (2009).
Narayan, S., Gagné, M. & Safavi-Naini, R. Privacy preserving EHR system using attribute-based infrastructure. In Proceedings of the 2010 ACM Workshop on Cloud Computing Security Workshop 47–52 (ACM, 2010).
Dolin, R. H. et al. HL7 Clinical Document Architecture, Release 2. J. Am. Med. Inform. Assoc. 13 , 30–39 (2006).
Mandl, K. D. & Kohane, I. S. Escaping the EHR trap—the future of health IT. N. Engl. J. Med. 366 , 2240–2242 (2012).
Mandel, J. C., Kreda, D. A., Mandl, K. D., Kohane, I. S. & Ramoni, R. B. SMART on FHIR: a standards-based, interoperable apps platform for electronic health records. J. Am. Med. Inform. Assoc. 23 , 899–908 (2016).
All eyes are on AI. Nat. Biomed. Eng . 2 , 139 (2018).
Yu, K. H. & Kohane I. S. Framing the challenges of artificial intelligence in medicine. BMJ Qual. Safety https://doi.org/10.1136/bmjqs-2018-008551 (2018).
Dignum, V. Ethics in artificial intelligence: introduction to the special issue. Ethics Inf. Technol . 20 , 1–3 (2018).
Price, I. & Nicholson, W. Artificial Intelligence in Health Care: Applications and Legal Implications (Univ. Michigan Law School, 2017).
Mukherjee, S. A.I. versus M.D. What happens when diagnosis is automated? The New Yorker (3 April 2017).
Del Beccaro, M. A., Jeffries, H. E., Eisenberg, M. A. & Harry, E. D. Computerized provider order entry implementation: no association with increased mortality rates in an intensive care unit. Pediatrics 118 , 290–295 (2006).
Longhurst, C. A. et al. Decrease in hospital-wide mortality rate after implementation of a commercially sold computerized physician order entry system. Pediatrics 126 , 14–21 (2010).
Carspecken, C. W., Sharek, P. J., Longhurst, C. & Pageler, N. M. A clinical case of electronic health record drug alert fatigue: consequences for patient outcome. Pediatrics 131 , 1970–1973 (2013).
Ash, J. S., Berg, M. & Coiera, E. Some unintended consequences of information technology in health care: the nature of patient care information system-related errors. J. Am. Med. Inform. Assoc. 11 , 104–112 (2004).
Lehman, C. D. et al. Diagnostic accuracy of digital screening mammography with and without computer-aided detection. JAMA Intern. Med. 175 , 1828–1837 (2015).
Koppel, R. et al. Role of computerized physician order entry systems in facilitating medication errors. JAMA 293 , 1197–1203 (2005).
Middleton, B. et al. Enhancing patient safety and quality of care by improving the usability of electronic health record systems: recommendations from AMIA. J. Am. Med. Inform. Assoc. 20 , 2–8 (2013).
Gottlieb, S. Twitter (12 April 2018); https://twitter.com/SGottliebFDA/status/984378648781312002
Digital Health Software Precertification (Pre-Cert) Program (FDA); https://www.fda.gov/MedicalDevices/DigitalHealth/DigitalHealthPreCertProgram/default.htm
Estrin, D. & Sim, I. Open mHealth architecture: an engine for health care innovation. Science 330 , 759–760 (2010).
Shortliffe, E. H. Computer programs to support clinical decision making. JAMA 258 , 61–66 (1987).
Armbruster, D. A., Overcash, D. R. & Reyes, J. Clinical chemistry laboratory automation in the 21st century—amat victoria curam (victory loves careful preparation). Clin. Biochem. Rev. 35 , 143–153 (2014).
Rosenfeld, L. A golden age of clinical chemistry: 1948–1960. Clin. Chem. 46 , 1705–1714 (2000).
Kuperman, G. J. et al. Medication-related clinical decision support in computerized provider order entry systems: a review. J. Am. Med. Inform. Assoc. 14 , 29–40 (2007).
Glassman, P. A., Simon, B., Belperio, P. & Lanto, A. Improving recognition of drug interactions: benefits and barriers to using automated drug alerts. Med. Care 40 , 1161–1171 (2002).
FDA permits marketing of artificial intelligence algorithm for aiding providers in detecting wrist fractures. https://www.fda.gov/newsevents/newsroom/pressannouncements/ucm608833.htm (FDA, 2018).
Haenssle, H. A. et al. Man against machine: diagnostic performance of a deep learning convolutional neural network for dermoscopic melanoma recognition in comparison to 58 dermatologists. Ann. Oncol. 29 , 1836–1842 (2018).
Simonyan, K. & Zisserman, A. Very deep convolutional networks for large-scale image recognition. Preprint at https://arxiv.org/abs/1409.1556 (2014).
Murphy, K. P. & Bach F. Machine Learning: A Probabilistic Perspective (MIT Press, Cambridge, 2012).
Download references
Acknowledgements
K.-H.Y. is supported by a Harvard Data Science Postdoctoral Fellowship. I.S.K. was supported in part by the NIH grant OT3OD025466. Figure 4 was generated by using the computational infrastructure supported by the AWS Cloud Credits for Research, the Microsoft Azure Research Award, and the NVIDIA GPU Grant Programme.
Author information
Authors and affiliations.
Department of Biomedical Informatics, Harvard Medical School, Boston, MA, USA
Kun-Hsing Yu, Andrew L. Beam & Isaac S. Kohane
Boston Children’s Hospital, Boston, MA, USA
Isaac S. Kohane
You can also search for this author in PubMed Google Scholar
Contributions
K.-H.Y. conceived and designed the article, performed the literature review and wrote and revised the manuscript. A.L.B. and I.S.K. edited the manuscript. I.S.K. supervised the work.
Corresponding author
Correspondence to Isaac S. Kohane .
Ethics declarations
Competing interests.
Harvard Medical School (K.-H.Y.) submitted a provisional patent application on digital pathology profiling to the United States Patent and Trademark Office (USPTO).
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Reprints and permissions
About this article
Cite this article.
Yu, KH., Beam, A.L. & Kohane, I.S. Artificial intelligence in healthcare. Nat Biomed Eng 2 , 719–731 (2018). https://doi.org/10.1038/s41551-018-0305-z
Download citation
Received : 12 December 2017
Accepted : 05 September 2018
Published : 10 October 2018
Issue Date : October 2018
DOI : https://doi.org/10.1038/s41551-018-0305-z
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
This article is cited by
Machine learning algorithms for predicting covid-19 mortality in ethiopia.
- Melsew Setegn Alie
- Yilkal Negesse
- Dereje Senay Merawi
BMC Public Health (2024)
Second opinion machine learning for fast-track pathway assignment in hip and knee replacement surgery: the use of patient-reported outcome measures
- Andrea Campagner
- Frida Milella
- Federico Cabitza
BMC Medical Informatics and Decision Making (2024)
Medical image fusion based on machine learning for health diagnosis and monitoring of colorectal cancer
- Yifeng Peng
- Haijun Deng
BMC Medical Imaging (2024)
Machine learning-enabled prediction of prolonged length of stay in hospital after surgery for tuberculosis spondylitis patients with unbalanced data: a novel approach using explainable artificial intelligence (XAI)
- Parhat Yasin
- Yasen Yimit
- Mayidili Nijiati
European Journal of Medical Research (2024)
Personalized prediction of mortality in patients with acute ischemic stroke using explainable artificial intelligence
Quick links.
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
- Computer Science and Engineering
- Artificial Intelligence
Artificial Intelligence in Healthcare
- October 2019
- Journal of Drug Delivery and Therapeutics 9(5-s)
- CC BY-NC 4.0

- Koringa College of Pharmacy

- Koringa college of pharmacy
Discover the world's research
- 25+ million members
- 160+ million publication pages
- 2.3+ billion citations
- Yahya Saleh
- J CARDIOTHORAC SURG

- S Sheik Asraf
- Jins K Abraham

- Miss. Isha Anand Bhagat
- Miss. Komal Gajanan Wankhede
- Mr. Navoday Atul Kopawar
- Prof. Dipali A. Sananse
- Sergey A. Smirnov

- J DRUG DELIV SCI TEC
- Naitik Jariwala

- Ketki Gatade

- Recruit researchers
- Join for free
- Login Email Tip: Most researchers use their institutional email address as their ResearchGate login Password Forgot password? Keep me logged in Log in or Continue with Google Welcome back! Please log in. Email · Hint Tip: Most researchers use their institutional email address as their ResearchGate login Password Forgot password? Keep me logged in Log in or Continue with Google No account? Sign up
IEEE Account
- Change Username/Password
- Update Address
Purchase Details
- Payment Options
- Order History
- View Purchased Documents
Profile Information
- Communications Preferences
- Profession and Education
- Technical Interests
- US & Canada: +1 800 678 4333
- Worldwide: +1 732 981 0060
- Contact & Support
- About IEEE Xplore
- Accessibility
- Terms of Use
- Nondiscrimination Policy
- Privacy & Opting Out of Cookies
A not-for-profit organization, IEEE is the world's largest technical professional organization dedicated to advancing technology for the benefit of humanity. © Copyright 2024 IEEE - All rights reserved. Use of this web site signifies your agreement to the terms and conditions.
Advancements in Artificial Intelligence for Health: A Rapid Review of AI-Based Mental Health Technologies Used in the Age of Large Language Models
- Conference paper
- First Online: 23 August 2024
- Cite this conference paper

- Johana Cabrera Medina ORCID: orcid.org/0000-0002-5444-688X 6 , 7 &
- Rodrigo Rojas Andrade ORCID: orcid.org/0000-0002-0096-2432 6 , 7
Part of the book series: Lecture Notes in Computer Science ((LNBI,volume 14848))
Included in the following conference series:
- International Work-Conference on Bioinformatics and Biomedical Engineering
This paper aims to explore the advancements of AI technologies in mental health by conducting a rapid review of recent scientific literature and mass media outputs. The study focuses on identifying AI technologies used in mental health, outlining the types of interventions benefiting from these technologies, evaluating the scientific evidence on their safety and effectiveness, and assessing the existence of normative frameworks that ensure their ethical use.
Employing a rapid review methodology, this research scrutinizes scientific studies and media reports selected based on explicit relevance to AI and mental health. The review integrates both scientific and grey evidence, providing a comprehensive overview of the current state and potential of AI applications in mental health care. The findings reveal significant utilization of AI in mental health diagnostics, treatment planning, and therapeutic interventions, facilitated by tools such as natural language processing, machine learning algorithms, and integrated AI systems, such as robots. The study also highlights the ethical, safety, and regulatory challenges emerging from the massive use of AI in this field, reflecting the need for stringent oversight and continuous evaluation.
This is a preview of subscription content, log in via an institution to check access.
Access this chapter
Subscribe and save.
- Get 10 units per month
- Download Article/Chapter or eBook
- 1 Unit = 1 Article or 1 Chapter
- Cancel anytime
- Available as PDF
- Read on any device
- Instant download
- Own it forever
- Available as EPUB and PDF
- Compact, lightweight edition
- Free shipping worldwide - see info
Tax calculation will be finalised at checkout
Purchases are for personal use only
Institutional subscriptions
The authors disclose that they have used ChatGPT 4 for organizing, translating, and structuring the information for a better understanding of the information developed. The authors disclose that the content of this paper is accurate and original.
Joksimovic, S., Ifenthaler, D., Marrone, R., De Laat, M., Siemens, G.: Opportunities of artificial intelligence for supporting complex problem-solving: findings from a scoping review. Comput. Educ. Artif. Intell. 4 , 100138 (2023). https://doi.org/10.1016/j.caeai.2023.100138
European Parliament. What is artificial intelligence and how is it used?. https://www.europarl.europa.eu/topics/en/article/20200827STO85804/what-is-artificial-intelligence-and-how-is-it-used . Accessed 06 Mar 2024
International Business Machines Corporation. What is artificial intelligence (AI)?. https://www.ibm.com/topics/artificial-intelligence . Accessed 06 Mar 2024
Cannataro, M., Guzzi, P.H., Agapito, G., Zucco, C., Milano, M.: Artificial Intelligence in Bioinformatics: From Omics Analysis to Deep Learning and Network Mining. 1st edn. ISBN 9780128229521 (2022)
Google Scholar
Alowais, S.A., et al.: Revolutionizing healthcare: the role of artificial intelligence in clinical practice. BMC Med. Educ. 23 , 689 (2023). https://doi.org/10.1186/s12909-023-04698-z
Article Google Scholar
Kizza, J.M.: Artificial intelligence: ethical and social problems of large language models and the future of technology. In: Kizza, J.M. (ed.) Ethical and Secure Computing: A Concise Module, pp. 275–285. Springer International Publishing, Cham (2023). https://doi.org/10.1007/978-3-031-31906-8_13
Hendrycks, D., Mazeika, M., Woodside, T.: An Overview of Catastrophic AI Risks (2023). http://arxiv.org/abs/2306.12001 , https://doi.org/10.48550/arXiv.2306.12001
OPEN AI. CHATGPT. https://openai.com/chatgpt . Accessed 06 Mar 2024
Cabrera, J., Loyola, M.S., Magaña, I., Rojas, R.: Ethical dilemmas, mental health, artificial intelligence, and LLM-based Chatbots. In: Rojas, I., Valenzuela, O., Rojas Ruiz, F., Herrera, L.J., and Ortuño, F. (eds.) Bioinformatics and Biomedical Engineering, pp. 313–326. Springer Nature Switzerland, Cham (2023). https://doi.org/10.1007/978-3-031-34960-7_22
Clarke, V., Braun, V.: Thematic analysis. J. Posit. Psychol. 12 , 297–298 (2017). https://doi.org/10.1080/17439760.2016.1262613
Cecula, P., et al.: Applications of artificial intelligence to improve patient flow in mental health inpatient units - Narrative literature review. Heliyon 7 (6), e07351 (2021). https://doi.org/10.1016/j.heliyon.2021.e07351
Graham, S., et al.: Artificial Intelligence for Mental Health and Mental Illnesses: an Overview. Curr. Psychiatry Rep. 21 (11), 116 (2019). https://doi.org/10.1007/s11920-019-1094-0
Straw, I., Callison-Burch, C.: Artificial Intelligence in mental health and the biases of language based models. PLoS ONE 15 (10), e0239693 (2020). https://doi.org/10.1371/journal.pone.0239693
Smrke, U., Mlakar, I., Lin, S.M., Musil, B., Plohl, N.: Language, speech, and facial expression features for artificial intelligence-based cancer survivors’ depression: scoping meta-review. JMIR Mental Health 8 (3), e21135 (2021). https://doi.org/10.2196/21135
Abd-Alrazaq, A., AlSaad, R., Shuweihdi, F., Ahmed, A., Aziz, S., Sheikh, J.: Systematic review and meta-analysis of performance of wearable artificial intelligence in detecting and predicting depression. NPJ Digital Med. 6 , 14 (2023). https://doi.org/10.1038/s41746-023-00614-3
Thenral, M., Annamalai, A.: Telepsychiatry and the role of artificial intelligence in mental health in post-COVID-19 India: a scoping review on opportunities. Indian J. Psychol. Med. 42 (5S), 53S-59S (2020). https://doi.org/10.1177/0253717620959592
Chowdhury, M., Cervantes, E.G., Chan, W.Y., Seitz, D.P.: Use of machine learning and artificial intelligence methods in geriatric mental health research involving electronic health record or administrative claims data: a systematic review. Front. Psychiatry 12 , 625875 (2021). https://doi.org/10.3389/fpsyt.2021.625875
Abd-alrazaq, A., et al.: Wearable artificial intelligence for anxiety and depression: scoping review. J. Med. Internet Res. 25 (1), e26273 (2023). https://doi.org/10.2196/26273
CBS NEWS. Mental health chatbots powered by artificial intelligence providing support. https://www.cbsnews.com/news/mental-health-chatbots-powered-by-artificial-intelligence-providing-support-60-minutes-transcript/ . Accessed 7 Apr 2024
News Medical Life Science. Five ways AI can help to deal with the mental health crisis. https://www.news-medical.net/news/20231028/Five-ways-AI-can-help-to-deal-with-the-mental-health-crisis.aspx . 28 Oct 2023
National Law Review. Incorporating AI to address mental health challenges in K-12 students. https://natlawreview.com/article/incorporating-ai-address-mental-health-challenges-k-12-students . Accessed 9 Apr 2024
Berkeley Articles. Can artificial intelligence help human mental health? https://greatergood.berkeley.edu/article/item/can_artificial_intelligence_help_human_mental_health . Accessed 24 Jan 2024
Forbes. AI in mental health: Opportunities and challenges in developing intelligent digital therapies. https://www.forbes.com/sites/bernardmarr/2023/07/06/ai-in-mental-health-opportunities-and-challenges-in-developing-intelligent-digital-therapies/?sh=5f282af85e10 . Accessed 6 Jul 2023
Tomorrow’s News Today. First clinically-trialed AI app designed for digital therapy. https://www.tomorrowsworldtoday.com/artificial-intelligence/first-clinically-trialed-ai-app-designed-for-digital-therapy/ . Accessed 23 April 2024
Darmoth News. Phone app uses AI to detect depression from facial cues. https://home.dartmouth.edu/news/2024/02/phone-app-uses-ai-detect-depression-facial-cues . Accessed 27 Feb 2024
Yahoo Finance. Qualifacts announces the launch of Qualifacts® iQ Behavioral Health Artificial Intelligence (AI) Solution ahead of NatCon24. https://finance.yahoo.com/news/qualifacts-announces-launch-qualifacts-iq-130200003.html . Accessed 11 Apr 2024
Daily Bruin. Student-led Bruincare initiative uses AI to enhance mental health support services. https://dailybruin.com/2024/04/04/student-led-bruincare-initiative-uses-ai-to-enhance-mental-health-support-services . Accessed 5 Apr 2024
WHO News. WHO unveils a digital health promoter harnessing generative AI for public health. https://www.who.int/news/item/02-04-2024-who-unveils-a-digital-health-promoter-hardessing-generative-ai-for-public-health , Accessed 2 Apr 2024
Here’s the continuation and completion of the reference list in Springer LNCS format for the rest of the cited internet news media articles:
Fox 13. Artificial intelligence tackling mental health suicide prevention among veterans. https://www.fox13news.com/news/artificial-intelligence-tackling-mental-health-suicide-prevention-among-veterans , 10 Nov 2023
MIT Technology Review. A chatbot helped more people access mental-health services. https://www.technologyreview.com/2024/02/05/1087690/a-chatbot-helped-more-people-access-mental-health-services . February 5, 2024
TIME. Can AI chatbots ever replace human therapists? https://time.com/6320378/ai-therapy-chatbots /, October 4, 2023
Forbes. 4 AI therapy options reviewed: Do they work? https://www.forbes.com/health/mind/ai-therapy/ , December 6, 2023
APA News. AI is changing every aspect of psychology. Here’s what to watch for. https://www.apa.org/monitor/2023/07/psychology-embracing-ai , July 1, 2023
Forbes. Workers using AI technology taking mental health into their own hands. https://www.forbes.com/sites/bryanrobinson/2023/09/02/workers-taking-wellness-into-their-own-hands-using-ai-backed-mental-health/?sh=390066aa5ee4 , September 2, 2023
FOX. Mental health app ‘Together by Renee’ using artificial intelligence to assist doctors. https://www.fox35orlando.com/news/ai-mental-health-app . November 8, 2023
Keck School of Medicine of USC. New AI-driven initiative could optimize brain stimulation for treatment-resistant depression. https://keck.usc.edu/news/new-ai-driven-initiative-could-optimize-brain-stimulation-for-treatment-resistant-depression/ . February 14, 2024
Education Week. Emotional intelligence and AI together can help lessen the student mental health crisis. https://www.edweek.org/leadership/opinion-emotional-intelligence-and-ai-together-can-help-lessen-the-student-mental-health-crisis/2024/01 . January 4, 2024
Very Well Health. Artificial intelligence (AI) to diagnose and treat autism. https://www.verywellhealth.com/artificial-intelligence-to-treat-autism-4706533 . August 8, 2023
Cardoso, J.R., Pereira, L.M., Iversen, M.D., Ramos, A.L.: What is gold standard and what is ground truth? Dental Press J. Orthod. 19 , 27–30 (2014). https://doi.org/10.1590/2176-9451.19.5.027-030.ebo
Download references
Author information
Authors and affiliations.
School of Psychology, Faculty of Humanities, University of Santiago de Chile, Santiago, Chile
Johana Cabrera Medina & Rodrigo Rojas Andrade
Nucleus of Innovation and Project Operations, School of Psychology (PSINOP), Santiago, Chile
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Johana Cabrera Medina .
Editor information
Editors and affiliations.
Department of Computer Architecture, CITIC-UGR - University of Granada, Granada, Granada, Spain
Ignacio Rojas
Francisco Ortuño
Fernando Rojas
Luis Javier Herrera
Department of Applied Mathematics, University of Granada, Granada, Granada, Spain
Olga Valenzuela
Rights and permissions
Reprints and permissions
Copyright information
© 2024 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this paper
Cite this paper.
Medina, J.C., Andrade, R.R. (2024). Advancements in Artificial Intelligence for Health: A Rapid Review of AI-Based Mental Health Technologies Used in the Age of Large Language Models. In: Rojas, I., Ortuño, F., Rojas, F., Herrera, L.J., Valenzuela, O. (eds) Bioinformatics and Biomedical Engineering. IWBBIO 2024. Lecture Notes in Computer Science(), vol 14848. Springer, Cham. https://doi.org/10.1007/978-3-031-64629-4_26
Download citation
DOI : https://doi.org/10.1007/978-3-031-64629-4_26
Published : 23 August 2024
Publisher Name : Springer, Cham
Print ISBN : 978-3-031-64628-7
Online ISBN : 978-3-031-64629-4
eBook Packages : Computer Science Computer Science (R0)
Share this paper
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Publish with us
Policies and ethics
- Find a journal
- Track your research
Click through the PLOS taxonomy to find articles in your field.
For more information about PLOS Subject Areas, click here .
Loading metrics
Open Access
Peer-reviewed
Research Article
The state of artificial intelligence in medical research: A survey of corresponding authors from top medical journals
Contributed equally to this work with: Michele Salvagno, Alessandro De Cassai
Roles Conceptualization, Data curation, Methodology, Writing – original draft, Writing – review & editing
Affiliation Department of Intensive Care, Hôpital Universitaire de Bruxelles (HUB), Brussels, Belgium
Roles Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Writing – original draft, Writing – review & editing
* E-mail: [email protected] , [email protected] (AC)
Affiliation Sant’Antonio Anesthesia and Intensive Care Unit, University Hospital of Padua, Padua, Italy
Roles Writing – original draft, Writing – review & editing
Roles Visualization, Writing – original draft, Writing – review & editing
Affiliations Department of Mathematical Modelling and Artificial Intelligence, National Aerospace University “Kharkiv Aviation Institute”, Kharkiv, Ukraine, Ubiquitous Health Technologies Lab, University of Waterloo, Waterloo, Canada
Affiliation Department of Clinical Sciences and Community Health, Università degli Studi di Milano, Milan, Italy
Affiliation Department of Anesthesiology and Critical Care Medicine, Johns Hopkins University School of Medicine, Baltimore, MD, United States of America
Roles Supervision, Writing – original draft, Writing – review & editing
- Michele Salvagno,
- Alessandro De Cassai,
- Stefano Zorzi,
- Mario Zaccarelli,
- Marco Pasetto,
- Elda Diletta Sterchele,
- Dmytro Chumachenko,
- Alberto Giovanni Gerli,
- Razvan Azamfirei,
- Fabio Silvio Taccone

- Published: August 23, 2024
- https://doi.org/10.1371/journal.pone.0309208
- Peer Review
- Reader Comments
Natural Language Processing (NLP) is a subset of artificial intelligence that enables machines to understand and respond to human language through Large Language Models (LLMs)‥ These models have diverse applications in fields such as medical research, scientific writing, and publishing, but concerns such as hallucination, ethical issues, bias, and cybersecurity need to be addressed. To understand the scientific community’s understanding and perspective on the role of Artificial Intelligence (AI) in research and authorship, a survey was designed for corresponding authors in top medical journals. An online survey was conducted from July 13 th , 2023, to September 1 st , 2023, using the SurveyMonkey web instrument, and the population of interest were corresponding authors who published in 2022 in the 15 highest-impact medical journals, as ranked by the Journal Citation Report. The survey link has been sent to all the identified corresponding authors by mail. A total of 266 authors answered, and 236 entered the final analysis. Most of the researchers (40.6%) reported having moderate familiarity with artificial intelligence, while a minority (4.4%) had no associated knowledge. Furthermore, the vast majority (79.0%) believe that artificial intelligence will play a major role in the future of research. Of note, no correlation between academic metrics and artificial intelligence knowledge or confidence was found. The results indicate that although researchers have varying degrees of familiarity with artificial intelligence, its use in scientific research is still in its early phases. Despite lacking formal AI training, many scholars publishing in high-impact journals have started integrating such technologies into their projects, including rephrasing, translation, and proofreading tasks. Efforts should focus on providing training for their effective use, establishing guidelines by journal editors, and creating software applications that bundle multiple integrated tools into a single platform.
Citation: Salvagno M, Cassai AD, Zorzi S, Zaccarelli M, Pasetto M, Sterchele ED, et al. (2024) The state of artificial intelligence in medical research: A survey of corresponding authors from top medical journals. PLoS ONE 19(8): e0309208. https://doi.org/10.1371/journal.pone.0309208
Editor: Sanaa Kaddoura, Zayed University, UNITED ARAB EMIRATES
Received: November 22, 2023; Accepted: August 8, 2024; Published: August 23, 2024
Copyright: © 2024 Salvagno et al. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Data Availability: All relevant data are within the manuscript and its Supporting Information files.
Funding: The author(s) received no specific funding for this work.
Competing interests: The authors have declared that no competing interests exist.
Introduction
Artificial intelligence (AI) and machine learning systems are advanced computer systems designed to emulate human cognitive functions and perform a wide range of tasks independently. The giant leaps these systems provide are the possibility to learn and solve problems through autonomous decision-making if an adequate initial database is provided [ 1 ]. Natural Language Processing (NLP) represents a field within AI focused on enabling machines to understand, interpret, and respond to human language meaningfully.
One intriguing advancement within the realm of AI is the development of Large Language Models (LLMs), which are a subset of NLP technologies. They are characterized by billions of parameters, which allows them to process and generate human-like text, understanding and producing language across a wide range of topics and styles.Generative chatbots, like ChatGPT(Generative Pre-trained Transformer), Microsoft Copilot, or Google Gemini,enhance these models and offer an easy-to-use interface. These LLMs excel in natural language processing and text generation, making them invaluable for diverse applications. Specifically, they have been used in medical research for estimating adverse effects and predicting mortality in clinical settings [ 2 – 4 ], as well as in scientific writing and publishing [ 5 ]. Finally, domain-specific or fine-tuned modelsare models that undergo additional training on a specialized dataset and are tailored to specific areas of expertise. This allows these models to develop a deeper understanding of terminology, concepts, and contexts, making them more adept at handling tasks ina specific field.
Potential applications of AI, and more precisely LLMs, in scientific production, are vast and multi-faceted. These applications range from automated abstract generation to enhancing the fluency of English prose for non-native speakers and even streamlining the creation of exhaustive literature reviews [ 6 , 7 ]. However, AI output is far from being perfect, as AI hallucination has been well described and documented in the current literature [ 8 , 9 ]. Additional concerns include ethical, copyright, transparency, and legal issues, the risk of bias, plagiarism, lack of originality, limited knowledge, incorrect citations, cybersecurity issues, and the risk of infodemics [ 9 ].
In light ofAI’s novel application in scientific production, it remains unclear to what extent the scientific community understands its inherent potentials, limitations, and potential applications. To address this, the authors designed a survey to examine the level of familiarity, understanding, and perspectives among contributing authors in premier medical journals regarding the role and impact of artificial intelligence in top scientific research and authorship. We hypothesize that, given the novelty of large language models (LLMs), researchers might not be familiar with their use and may not have implemented them in their daily practice.
Survey design
An online survey in this study was conducted using the SurveyMonkey web instrument ( https://www.surveymonkey.com , SurveyMonkey Inc., San Mateo, California, USA). The survey protocol (P2023/262) was approved by the Hospitalo-FacultaireErasme–ULB ethical commission(Comitéd’Ethiquehospitalo-facultaireErasme–ULB, chairman: Prof. J.M. Boeynaems) on July 11 th , 2023.
Two members of the survey team (M.S. and A.D.C.) performed a bibliographic search on April 19, 2023, on PubMed and Scopus, to retrieve any validated questionnaire on the topic using the following search string: [((Artificial Intelligence) OR (ChatGPT) OR (ChatBot)) AND ((scientific production) OR (scientific writing)) AND (survey)]. No existing surveys on the specific topic were found.
Therefore, the research team constructed the questionnaire under the BRUSO acronym to create a well-constructed survey [ 10 ]. The survey consisted of 20 single-choice, multiple-choice, and open-ended questions investigating individuals’ perceptions of using Artificial Intelligence (AI) in scientific production and content. The full list of questions is available for consultation in English ( S1 Appendix Content 1, Survey Questionnaire in English).
Population of interest
The population of interest in this survey consisted of corresponding authors who published in 2022 in the 15 highest-impact medical journals ( S2 Appendix Content 2), as ranked by the Journal Citation Report from Clarivate. In this survey, we used the Journal Impact Factor (JIF) as a benchmark to target leading publications in the research field. Originally developed by Eugene Garfield in the 1960s, the JIF is frequently employed as a proxy for a journal’s relative importance within its discipline. It is calculated by dividing the number of citations in a given year to articles published in the preceding two years by the total number of articles published in those two years. The focus on the corresponding authors aimed to access a segment of the research community that is potentially at the forefront of research publishing and scientific production. For this survey, only the email addresses of the corresponding authors listed in the manuscript were sought and collected. Whenmultiple emails were listed as corresponding, only the first email for each article was collected.When no email addresses were found, no further steps were taken to retrieve them.No differentiation was made regarding the type of published article, except for excluding memorial articles dedicated to deceased colleagues. All other articles were included. The authenticity of the email addresses or their correspondence with the author’s name was not verified. As a result, it was not possible to calculate the a priori sample size.
Survey distribution plan
To enhance the survey’s effectiveness, a pretest was performed in two phases. In the first phase, the survey team reviewed the entire survey, with particular attention to the flow and the order of the questions to avoid issues with “skip” or “branch” logic. The time required to complete the survey was estimated to be around four minutes. In the second phase,the survey was distributed for validation to a small subset of participants, which included researchers working at the Erasme Hospital, to identify any issues before distributing it to the general population of interest. Their answers were not included in the final data analysis.
UsingSurveyMonkey’s email distribution feature, the survey link was disseminated to all collected email addresses of the corresponding authors. To minimize the ratio of non-responders, reminder emails were sent one, two, and three weeks after the initial contact, with a final reminder sent one month later. Responses were collected from July 13 th , 2023, to September 1 st , 2023. SurveyMonkey’s web instrument automatically identifies respondents and non-respondents through personalized links, allowing for targeted reminders to only those who had not yet completed the survey. This system also automatically prevents duplicate responses.
Statistical analysis
Descriptive statistics was used to provide an overview of the dataset. Depending on the nature of the variables the results are reported either as percentages or as medians with interquartile range (IQR). Comparison among percentages were performed with the chi-square test with a p-values significance threshold at 0.05. All statistical analyses were performed using Jamovi (Jamovi, Sydney, NSW Australia, Version 2.3) and GraphPad Prism (GraphPad Software, Boston, Massachusetts USA,Version 10).
A total of 4,302 email addresses for inclusion in the survey were collected from the list of journals in the appendix. Survey data were collected from 13 th July to 1 st September 2023. Following the initial email outreach and four subsequent reminders, 222 emails bounced back, and 142 recipients actively opted out of participating.Of those who opened the survey link, 266 respondents answered the initial questions. However, some immediately declined to continue, resulting in 236(5.5% of the emails sent) participants who started the survey and were included in the final analysis upon response.
The geographical distribution and demographic data of 229 respondents are depicted in Table 1 ,.The United States and the United Kingdom were most prominently represented, accounting for 57 (24.9%) and 41 (17.9%) of respondents, respectively. In total, English-speaking nations (USA, UK, Canada, and Australia) accounted for 124 (54.1%) of respondents.
- PPT PowerPoint slide
- PNG larger image
- TIFF original image
https://doi.org/10.1371/journal.pone.0309208.t001
The role of 229 responders is represented in Fig 1 . Physicians, research academics and research clinicians were equally represented, with 64 (27.9%), 65 (28.4%) and 67 (29.2%) responders, respectively. The other responders declared not to be classified as the aforementioned and explained themselves mainly as journalists, students, veterinarians, editors, and pharmacists.
Proportion of respondents in various professional roles as a percentage of the total respondent pool.
https://doi.org/10.1371/journal.pone.0309208.g001
Most of the respondents to this question reported moderate 93 (40.6%) or little 60 (26.2%) familiarity with AI tools. Only 13 (5.7%) indicated extensive familiarity.Following questions up to Q14 were answered by all participants except for the 10 individuals (4.4%) who indicated no prior knowledge of AI (resulting in their automatic exclusion from answering those specific questions). Notably, 9 (69.2%)out of 13 with extensive familiarity reported AI tool usage, compared to lower rates among 20 out of 93 (21.5%)with moderate and 5 out of 60 (8.3%)minimal familiarity (p < 0.001).
More than half of 229 respondents (130, 55%) published their first medical article over 15 years ago, while 31 (13.5%) did so within the last five years. The median Scopus H-index among respondents was 24 (IQR 13–42). No statistically significant correlations were identified between H-index, AI familiarity and AI usage (p > 0.05).
Only 2 participants (< 1%), reported receiving specific training in AI for scientific production. Despite this, 55 (24.02%) out of 229 responders usedAI tools in scientific content creation.Of these, the majority (67.3%) used ChatGPT. Interestingly, among participants from the US(n = 57), a notable difference exists between those who have used AI for scientific production(n = 8, 14%) and those who have not (n = 49, 86%).Those who published the first medical article more than 15 years ago, also declared to have ever used AI tools for scientific production in a lesser amount than the ones who published the first medical article less than 15 years ago(23/130 [17.7%] vs. 32/99 [32.3%], p = 0.01).
As shown in Fig 2 , besides ChatGPT, among the 55 responders who have already published using the aid of AI during the scientific production,Microsoft Bing and Google Bard were used by 8 (14.5%) and 2 (3.6%) of respondents, respectively. Other large language models comprised 5.0% of the usage. Various software tools, including image creation and meta-analysis assistant tools, were also reported to be used by 7 (12.7%) and 6 (10.9%), respectively. Other AI tools reported are mainly Grammarly, Image Analysis tools, and plagiarism-checking tools.
The Y-axis lists the AI tools reported by respondents, while the X-axis shows their stated usage as a percentage. The total percentage exceeds 100% as respondents could report using multiple tools. LLM: Large Language Models; AI: Artificial Intelligence.
https://doi.org/10.1371/journal.pone.0309208.g002
When the 55 respondents who already used AI tools were asked about the primary applications of AI, 55.6% reported using AI for rephrasing text, 33.3% for translation, and 37.78% for proofreading. The rate of AI usage for language translation was consistent across English and non-English-speaking countries (94.4% vs 92.4%,p = 0.547). Additional applications such as draft writing, idea generation, and information synthesis were each noted by 24.4% of respondents.
In the survey, 8 of the 51 who answered this question (15.7%) admitted to using a chatbot for scientific work without acknowledgment.By contrast, 27 (11.9%)out of 226 are certain they will employ some form of Artificial Intelligence in future scientific production. The complete set of responses is summarized in Table 2 .
https://doi.org/10.1371/journal.pone.0309208.t002
The primary challenges associated with utilizing AI in scientific research are outlined in Table 3 .
https://doi.org/10.1371/journal.pone.0309208.t003
The medical fields that respondents anticipate will gain the most from AI applications are Big Data Management and Automated Radiographic Report Generation. Additionalareas are detailed in Table 4 .
https://doi.org/10.1371/journal.pone.0309208.t004
When asked about their ability to distinguish between text written by a human and text generated by AI, 7 (3.1%) out of 226 respondents believed they could always tell the difference. Meanwhile, 120 (53.1%) felt they could only sometimes discern the difference. A total of 59 (26%)were uncertain, and a small fraction, 3 (1.3%), reported it is never possible to distinguish between the two.
Over 80% of respondents (n = 226) do not foresee AI supplanting the role of medical researchers in the future, with 81 (35.8%)strongly disagreeing and 106 (46.9%)disagreeing. A small fraction, 10 responders (4.4%), either somewhat or strongly agree that AI could take on the role of medical researchers. Meanwhile, 29 (12.8%)remain uncertain. By contrast, when it comes to the impact on clinical physicians,among the 226 responders to this last question, 177(78.3%) anticipate that AI will partially alter the nature of their work within the next two decades. A minority of 18 responders (8.0%) foresee no change at all, and a very small fraction, 2 (0.9%), predict a complete transformation in the role of clinical physicians. To conclude, 14 (6.0%)are still unsure about the future impact of AI on clinical practice.
The present study aimed to explore the perceptions and utilization of Artificial Intelligence (AI) tools in scientific production among corresponding authors who published in the 15 most-impacted factor medical journals in 2022.
Familiarity and training in AI
Intriguingly, this survey indicated that less than 1% of respondents had undergone formal training specifically designed for the application of AI in scientific research. This highlights a critical need for educational programs tailored to empower researchers with the necessary skills for effective AI utilization. The dearth of formal training may also contribute to the observed "limited" to "moderate" familiarity with AI concepts and tools among most survey participants, without a difference among ages and genders.Generally, AI tools are user-friendly and straightforward, requiring no specialized skills for basic usage. This could account for the lack of a significant difference between younger and older users.However, even though the basic use appears straightforward, a lack of comprehension may lead individuals to commit unnoticed errors with these tools, stemming from an unawareness of their own knowledge gaps [ 11 ].
Although beyond the primary focus of this study, we find it noteworthy to comment on the responses concerning the Scopus H-index. This score remains a subject of debate and is fraught with limitations, including self-citation biases, equal attribution regardless of author order and academic age,as well as gender-based disparities other than topic-specific biases. In our survey, the responders presented a median H-index of 24 (IQR 13–42), without statistically significant correlationsbetween H-index values and the variables of interest. Remarkably, two respondents indicated a lack of interest in monitoring their H-index. One respondent, a journal editor, expressed outright indifference with the remark "Who cares", probably echoing a sentiment that could be ascribed to Nobel Laureate Tu Youyou, whose current relatively low Scopus H-index of 16 belies her groundbreaking work on artemisinin, a treatment for malaria that has saved millions of lives.
Applications of AI in scientific production
The survey results underscore a paradoxical relationship between familiarity with AI concepts and its actual utilization in scientific production. While many respondents indicated a “limited” to “moderate” familiarity with AI, around 25% reported employing AI tools in their research endeavors. This suggests that while the theoretical understanding of AI might be limited among the surveyed population, its practical applications are cautiously being explored. It is plausible that the rapid advancements in AI, coupled with its increasing accessibility, have allowed researchers to experiment with these tools without necessarily delving deep into the underlying algorithms and principles.Notably, the preponderance of the surveyed gravitated toward ChatGPT, suggesting a proclivity for natural language processing applications. Indeed, ChatGPT could assist scientists in scientific production in several ways [ 12 ].
The principal tasks for which AI was employed encompassed rephrasing, translation, and proofreading functions. AI tools, especially natural language processing models like ChatGPT, can significantly improve the fluency and coherence of scientific texts, especially for non-native English speakers. This is crucial in the globalized world of scientific research, where effective communication can determine the reach and impact of a study. Interestingly, the rates of AI use for language translation were quite similar between English-speaking and non-English-speaking countries, at 94.4% and 92.4%, respectively. This is unexpected since English is often the preferred language for communication in scientific fields, diminishing the perceived need for translation tools. Several factors could explain this trend. First, these countries have a high proportion of expatriates, leading to many non-native English speakers in the workforce. One limitation of our study is that we did not inquire about the respondents’ countries of origin, so we cannot provide further insights. Another possible explanation could be the selectivity of our respondent pool, which may not be sufficiently representative to show a difference in this variable.Nevertheless, ifthe predominant use of AI for tasks such as rephrasing, translation, and proofreading underscores its potential to enhance the quality of research output, it is essential to strike a balance to ensure that the essence and originality of the research are maintained in the pursuit of linguistic perfection.
This pattern intimates that, in its current stage, AI is predominantly perceived as a facilitator for enhancing the textual quality of scholarly work, rather than as an instrument for novel research ideation or data analysis. In response to this evolving landscape, academic journals, for example, JAMA and Nature, have issued guidelines concerning the judicious use of large language models (LLMs) and generative chatbots [ 13 , 14 ]. Such guidelines often stipulate authors’ need to disclose any AI-generated content explicitly, including the specification of the AI model or tool deployed.
While the survey highlighted the use of LLMs predominantly in textual enhancements, the potential of other AI in data analysis still needs to be explored among the respondents. Indeed, LLM and NLP, in general, currently have a very weak theoretical basis for data prediction.Nevertheless, longitudinal electronic health record (EHR) data have been effectively tokenized and modeled using transformer approaches, to integrate different patient measurements, as reported in the field of Intensive Care Medicine [ 15 ], even if this field is still insufficiently explored. Advanced AI algorithms can process vast datasets, identify patterns, and even accurately predict future trends, often beyond human capabilities. For instance, in biomedical research, numerous machine learning applications tailored to specific tasks or domains can assist in analyzing complex genomic data, predicting disease outbreaks, or modeling the effects of potential drugs. As indicated by the survey, the limited utilization of AI in these areas may be due to the lack of specialized training or apprehensions about the reliability of AI-generated insights.
Future prospects
Most respondents were optimistic about the future role of AI in scientific production, with nearly 12% stating they would "surely" use AI in the future. This optimism towards integrating AI in scientific production can be attributed to the numerous advancements and breakthroughs in AI in recent years. As AI models become more sophisticated, their potential applications in research expand, ranging from data analysis and visualization to hypothesis generation and experimental design. The increasing availability of open-source AI tools and platforms makes it more accessible for researchers to incorporate AI into their work, even without extensive technical expertise.
However, most respondents (> 80%) did not believe that AI would replace medical researchers, suggesting a balanced view that AI will serve as a complementary tool rather than a replacement for human expertise. The sentiment that AI will augment rather than replace human expertise aligns with the broader perspective in the AI community, often termed “augmented intelligence” [ 16 ]. This perspective emphasizes the synergy between human intuition and AI’s computational capabilities. While AI can handle vast amounts of data and rapidly perform complex calculations, human researchers bring domain expertise, critical thinking, and ethical considerations [ 17 ]. This combination can lead to more robust and comprehensive research outcomes [ 16 , 18 ].
Moreover, the evolving landscape of AI in research also presents opportunities for interdisciplinary collaboration [ 19 ]. As AI becomes more integrated into scientific research, there will be a growing need for collaboration between AI specialists and domain experts. Such collaborations can ensure that AI tools are developed and applied in contextually relevant and scientifically rigorous ways. This interdisciplinary approach can lead to novel insights and innovative solutions to complex research challenges.
Ethical and technical concerns
This survey identified a wide range of concerns regarding the integration of Artificial Intelligence (AI) into the realm of scientific research. Among these, content inaccuracies emerged as the most salient, flagged by over 80% of respondents. The risks associated with AI-generated content include creating ostensibly accurate but factually erroneous data, such as fabricated bibliographic references, a phenomenon described as "Artificial Intelligence Hallucinations"[ 20 ]. It has already been proposed that the Dunning-Kruger effect serves as a pertinent framework to consider the actual vs. the perceived competencies that exist regarding the application of AI in research [ 21 ]. Furthermore,the attitudes and expectations surrounding such technologies, just one year following the release of OpenAI’s ChatGPT, can be aptly illustrated by the Gartner Hype Cycle [ 22 ]. Consequently, it is imperative that content generated by AI algorithms, even translations, undergo rigorous validation by subject matter experts.
Moreover, the rapid evolution of AI models, especially deep learning architectures, has created ’black box’ systems where the decision-making process is not transparent [ 23 ]. This opacity can further exacerbate researchers’ trust issues towards AI-generated content. The lack of interpretability can hinder the widespread adoption of AI in scientific research, as researchers might be hesitant to rely on tools they need to understand fully. Efforts are being made in the AI community to develop more interpretable and explainable AI models, but the balance between performance and transparency remains a challenge [ 24 ].
Beyond the ethical implications, another emerging concern is the potential for AI to perpetuate existing biases in the training data or continue "citogenesis"[ 25 ], which represents an insidious form of error propagation within the scientific corpus [ 26 ]. If AI models are trained on biased datasets, they can produce skewed or discriminatory results, leading to flawed conclusions and the perpetuation of systemic inequalities in research. This is particularly concerning in social sciences and medicine, where biased conclusions can have far-reaching implications [ 27 ]. For this reason, researchers must be aware of these pitfalls and advocate for the usage of data that is as unbiased and representative as possible in training AI models. The full spectrum of potential negative outcomes remains largely unquantified. Furthermore, using AI complicates the attribution of accountability, particularly in clinical settings. Ethical concerns, echoed by most of our respondents, coexist with legal considerations [ 28 ].
Additionally, integrating AI into scientific research raises data privacy and security questions [ 29 ]. As AI models often require vast amounts of data for continued training,there is the risk of submitted sensitive information being unintentionally exposed or misused during the process.This is one of the main reasons why several AI companies recently came out with enterprise and on-premise software versions.Such measures are especially pertinent in medical research, where patient data confidentiality is paramount [ 23 , 30 ]. Ensuring robust data encryption and adhering to stringent data handling protocols becomes crucial when incorporating AI into the research workflow.
Various policy options have been tabled to govern the use of AI in the production and editing of scholarly texts. These range from a complete prohibition on using AI-generated content in academic manuscripts to mandates for clear disclosure of AI contributions within the text and reference sections [ 31 ]. Notably, accrediting AI systems as authors appear to be universally rejected.Given these challenges, the concerns identified are legitimate and necessitate comprehensive investigation, particularly as AI technologies continue to advance and diversify in application.
A collaborative approach that includes AI experts, ethicists, policymakers, and researchers is crucial to manage the ethical and technical complexities and fully leverage AI in a responsible and effective manner. Furthermore, it is advisable for journal editors to establish clear guidelines for AI use, as some have already begun [ 14 ], including mandating the disclosure of AI involvement in the research process. Strict policies should be implemented to safeguard the data utilized by AI systems. Human oversight is necessary to interpret the data and results produced by AI. Additionally, an independent group should assess the impact of AI on research outcomes and ethical issues.
Lastly, attention must be paid to the energy consumption of AI systems and their consequent carbon footprint, which can be considerable, especially in the case of large-scale computational models [ 32 ]. AI and machine learning models, particularly those utilizing deep learning, require extensive computational resources and use significant amounts of electricity. To minimize this footprint, researchers should focus on optimizing AI algorithms to increase their energy efficiency and employ these systems only when absolutely necessary. It is essential for researchers to consider the environmental impact of their AI usage, treating ecological sustainability as a critical factor in today’s world.
Future in healthcare
The advent of AI in healthcare is rapidly evolving, and our responders anticipate Big Data Management [ 33 ] and Automated Radiographic Report Generation [ 34 ] to be the most impactful areas influenced by AI applications in the next few years. These results underline the growing recognition of AI’s transformative potential in these domains [ 35 ]. Indeed, the current healthcare landscape generates massive amounts of data from diverse sources, including electronic health records, diagnostic tests, and patient monitoring systems [ 36 ]. AI-powered analytics tools could revolutionize how we understand and interpret this data, thus aiding in more accurate diagnosis and personalized treatment protocols. Similarly, medical imaging studies require considerable time and expertise for interpretation, representing a potential bottleneck in clinical workflow. Automated systems powered by AI can analyze images and rapidly generate reports with a speed and consistency that could vastly improve throughput and possibly contribute to improved patient outcomes, bolstering the assumption that AI-assisted radiologists work better and faster [ 37 ]. By contrast, these systems have been demonstrated to generate more incorrect positive results compared to radiology reports, especially when dealing with multiple or smaller-sized target findings [ 38 ]. Despite these and other limitations such as privacy security concerns, computer-aided diagnosis is promising and could impact several specialties [ 39 ]. In the market, there are already various user-friendly and easy-to-use mobile apps available, designed for healthcare professionals as well as patients, that offer quick access to artificial intelligence tools for obtaining potential diagnoses.Nevertheless, AI currently lacks the precision and capability to make clinical diagnoses, and thus cannot be a substitute for a doctor.
Finally, the development of AI in diagnosis and drug development was also highly rated in the survey. These results mirror current research trends, where AI has been applied for early disease detection and drug discovery processes, significantly cutting down time and costs. Even so, the essential human interaction between patient and clinician remains a core aspect of medical care, making it unlikely that AI will soon replace the need for in-person connection [ 40 ]. Our survey respondents echo this sentiment, as the majority believe clinical doctors will only be partially replaced by technological advancements. Interestingly, in the open-ended responses, among the others, we found this comment “Humans do not want an AI-doctor”. Even though literature tells us that AI could be more empathetic than human doctors [ 41 ], for the moment, everyone agrees.
Limitations
While this study provides valuable insights into the understanding and utilization of Artificial Intelligence (AI) in scientific research, there are some noteworthy limitations. First, the study sample focuses exclusively on corresponding authors from high-impact medical journals. Although this allows us to capture perspectives from researchers at the forefront of scientific advancements, it may limit the generalizability of our findings to the broader scientific and medical community, including early-career researchers and students. Future surveys should aim to include a more diverse range of participants for a fuller picture.
Second, the survey had a low response rate. Physicians are generally challenging to be involved in survey research, and web-based surveys often yield lower participation rates [ 42 ]. Additionally, the accuracy of the email addresses is not guaranteed in email surveys, as evidenced by the emails that were bounced back, likely due to outdated or incorrect institutional email addresses. Nevertheless, although we didn’t conduct an a priori sample size calculation, our aim was to collect responses from at least 300 participants to obtain a substantial perspective on the subject.
Third, the data was gathered through an online survey, which might introduce selection bias as those who are more comfortable with technology and AI may have been more inclined to participate.
Fourth, there was no verification process for the authenticity of the email addresses used in our study, which leaves room for potential inaccuracies in the data collected.
Conclusions
This survey revealed varying degrees of familiarity with AI tools among researchers, with many in high-impact journals beginning to integrate AI into their work. The majority of respondents were from the USA and UK, with 54.1% from English-speaking countries. Only 5.7% indicated extensive familiarity with AI, and 24% used AI tools in scientific content creation, predominantly ChatGPT. Despite low training rates in AI (less than 1%), its use is gradually becoming more prevalent in scientific research and authorship.
Supporting information
S1 appendix. survey questionnaire..
https://doi.org/10.1371/journal.pone.0309208.s001

S2 Appendix. List of the leading 15 medical journals by impact factor.
https://doi.org/10.1371/journal.pone.0309208.s002
- View Article
- PubMed/NCBI
- Google Scholar
- 14. Artificial Intelligence (AI) | Nature Portfolio n.d. https://www.nature.com/nature-portfolio/editorial-policies/ai (accessed April 15, 2024).
- 25. 978: Citogenesis ‐ explain xkcd n.d. https://www.explainxkcd.com/wiki/index.php/978:_Citogenesis (accessed September 3, 2023).
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- My Bibliography
- Collections
- Citation manager
Save citation to file
Email citation, add to collections.
- Create a new collection
- Add to an existing collection
Add to My Bibliography
Your saved search, create a file for external citation management software, your rss feed.
- Search in PubMed
- Search in NLM Catalog
- Add to Search
Innovation and challenges of artificial intelligence technology in personalized healthcare
Affiliations.
- 1 International School, Beijing University of Posts and Telecommunications, Bei Jing, 100876, China.
- 2 Department of Ophthalmology, The Second Norman Bethune Hospital of Jilin University, Changchun, 130000, China.
- 3 Department of Ophthalmology, The Second Norman Bethune Hospital of Jilin University, Changchun, 130000, China. [email protected].
- PMID: 39152194
- PMCID: PMC11329630
- DOI: 10.1038/s41598-024-70073-7
As the burgeoning field of Artificial Intelligence (AI) continues to permeate the fabric of healthcare, particularly in the realms of patient surveillance and telemedicine, a transformative era beckons. This manuscript endeavors to unravel the intricacies of recent AI advancements and their profound implications for reconceptualizing the delivery of medical care. Through the introduction of innovative instruments such as virtual assistant chatbots, wearable monitoring devices, predictive analytic models, personalized treatment regimens, and automated appointment systems, AI is not only amplifying the quality of care but also empowering patients and fostering a more interactive dynamic between the patient and the healthcare provider. Yet, this progressive infiltration of AI into the healthcare sphere grapples with a plethora of challenges hitherto unseen. The exigent issues of data security and privacy, the specter of algorithmic bias, the requisite adaptability of regulatory frameworks, and the matter of patient acceptance and trust in AI solutions demand immediate and thoughtful resolution .The importance of establishing stringent and far-reaching policies, ensuring technological impartiality, and cultivating patient confidence is paramount to ensure that AI-driven enhancements in healthcare service provision remain both ethically sound and efficient. In conclusion, we advocate for an expansion of research efforts aimed at navigating the ethical complexities inherent to a technology-evolving landscape, catalyzing policy innovation, and devising AI applications that are not only clinically effective but also earn the trust of the patient populace. By melding expertise across disciplines, we stand at the threshold of an era wherein AI's role in healthcare is both ethically unimpeachable and conducive to elevating the global health quotient.
Keywords: Artificial intelligence; Data security; Healthcare; Remote patient care; Virtual assistant chatbots.
© 2024. The Author(s).
PubMed Disclaimer
Conflict of interest statement
The authors declare no competing interests.
Similar articles
- Reimagining Healthcare: Unleashing the Power of Artificial Intelligence in Medicine. Iqbal J, Cortés Jaimes DC, Makineni P, Subramani S, Hemaida S, Thugu TR, Butt AN, Sikto JT, Kaur P, Lak MA, Augustine M, Shahzad R, Arain M. Iqbal J, et al. Cureus. 2023 Sep 4;15(9):e44658. doi: 10.7759/cureus.44658. eCollection 2023 Sep. Cureus. 2023. PMID: 37799217 Free PMC article. Review.
- Challenges and strategies for wide-scale artificial intelligence (AI) deployment in healthcare practices: A perspective for healthcare organizations. Esmaeilzadeh P. Esmaeilzadeh P. Artif Intell Med. 2024 May;151:102861. doi: 10.1016/j.artmed.2024.102861. Epub 2024 Mar 30. Artif Intell Med. 2024. PMID: 38555850
- Generative AI in healthcare: an implementation science informed translational path on application, integration and governance. Reddy S. Reddy S. Implement Sci. 2024 Mar 15;19(1):27. doi: 10.1186/s13012-024-01357-9. Implement Sci. 2024. PMID: 38491544 Free PMC article. Review.
- ARTIFICIAL INTELLIGENCE IN MEDICAL PRACTICE: REGULATIVE ISSUES AND PERSPECTIVES. Pashkov VM, Harkusha AO, Harkusha YO. Pashkov VM, et al. Wiad Lek. 2020;73(12 cz 2):2722-2727. Wiad Lek. 2020. PMID: 33611272 Review.
- Unraveling the Ethical Enigma: Artificial Intelligence in Healthcare. Jeyaraman M, Balaji S, Jeyaraman N, Yadav S. Jeyaraman M, et al. Cureus. 2023 Aug 10;15(8):e43262. doi: 10.7759/cureus.43262. eCollection 2023 Aug. Cureus. 2023. PMID: 37692617 Free PMC article. Review.
- Esteva, A., Kuprel, B. & Novoa, R. A. Dermatologist-level classification of skin cancer with deep neural networks. Oncologie19(11–12), 407–408 (2017). - PMC - PubMed
- Wiriyathammabhum, P. et al. Computer vision and natural language processing: Recent approaches in multimedia and robotics. ACM Comput. Surveys49(4), 1–44 (2017).10.1145/3009906 - DOI
- Gulshan, V. et al. Development and validation of a deep learning algorithm for detection of diabetic retinopathy in retinal fundus photographs. Jama-J. Am. Med. Assoc.316(22), 2402–2410 (2016).10.1001/jama.2016.17216 - DOI - PubMed
- Susymary, J. & Deepalakshmi, P. Machine learning for precision medicine forecasts and challenges when incorporating non omics and omics data. Intell. Decis. Technol.-Netherlands15(1), 69–85 (2021).
- Aggarwal, A. et al. Artificial intelligence-based chatbots for promoting health behavioral changes: Systematic review. J. Med. Internet Res.25, e40789 (2023). 10.2196/40789 - DOI - PMC - PubMed
Publication types
- Search in MeSH
Grants and funding
- No. 82171053/National Natural Science Foundation of China
- 81570864/National Natural Science Foundation of China
LinkOut - more resources
Full text sources.
- Nature Publishing Group
- PubMed Central
- MedlinePlus Health Information
Research Materials
- NCI CPTC Antibody Characterization Program

- Citation Manager
NCBI Literature Resources
MeSH PMC Bookshelf Disclaimer
The PubMed wordmark and PubMed logo are registered trademarks of the U.S. Department of Health and Human Services (HHS). Unauthorized use of these marks is strictly prohibited.

- Assets Blogs Podcasts Affiliate Partners FinTech Resources Startup Valuation Training Program Career Accelerator
- Hire Engineers
- Startup Valuation
- Training Program
- Career Accelerator
AI for Hospitals: Can Artificial Intelligence Help Healthcare
Discover how AI is transforming healthcare. Explore its potential to enhance patient care, improve diagnosis, and streamline hospital operations.

Introduction
The average time an American waits in the Emergency Department to see a physician, advanced practice registered nurse (APRN), or physician assistant was 35.7 minutes in 2021. Meanwhile, one percent (that is roughly 1,331 visits) of ED visits had waited four to six hours before being seen. What if that time could be reduced by the implementation of AI? Imagine the doors it would open and the lives AI could potentially save.
Healthcare is at a pivotal juncture, with hospitals around the world grappling with challenges such as increasing patient loads, rising costs, and the ever-present risk of human error. Amid these pressures, Artificial Intelligence (AI) is emerging as a powerful tool that could transform the way healthcare is delivered. AI is poised to revolutionize healthcare by enhancing efficiency by reducing wait times, improving diagnostic accuracy, and elevating patient care to new heights.
The benefits AI offers range from operational efficiency to personalized treatment . Nonetheless, we must consider the challenges and ethical dilemmas that come with its adoption. By understanding the full scope of AI’s capabilities and limitations, healthcare leaders can make informed decisions about integrating this technology into their institutions.
The Role of AI in Healthcare
Artificial Intelligence (AI) refers to the simulation of human intelligence processes by machines, particularly computer systems. These processes include the acquisition of information and rules for using the information (learning), using rules to reach approximate or definite conclusions (reasoning), and self-correction.
In healthcare, AI is increasingly being utilized to analyze complex medical data, enhance decision-making , and automate routine processes. Artificial Intelligence can mimic human cognitive functions, assist healthcare professionals in diagnosing diseases, develop treatment plans, and improve patient outcomes.
AI is being leveraged in hospitals across the globe to address some of the most critical challenges in healthcare. Here are some of the key areas where AI is making a significant impact:
- AI-Driven Imaging : AI-powered imaging tools are revolutionizing radiology and pathology by enhancing the accuracy and speed of diagnoses. For example, AI algorithms can analyze medical images to detect abnormalities such as tumors, fractures, or lesions with high precision. In some cases, these tools have been shown to perform on par with or even exceed the diagnostic capabilities of human radiologists.
- Pattern Recognition : AI’s ability to recognize patterns in complex datasets is being used to identify early signs of diseases, such as cancer or cardiovascular conditions before symptoms become apparent. This enables earlier interventions and improves patient outcomes.
- AI in Genomics : AI is playing a critical role in genomics by analyzing genetic data to identify mutations and predict disease risks. This information is then used to create personalized treatment plans tailored to an individual’s genetic makeup, leading to more effective and targeted therapies.
- Tailored Treatment Plans : AI systems can also analyze patient data, including medical history, lifestyle, and current health status, to recommend personalized treatment plans. This approach helps in optimizing treatment effectiveness while minimizing side effects.
- Scheduling and Resource Management : AI is being used to optimize hospital operations by predicting patient admissions, managing staff schedules, and ensuring that resources such as beds and medical equipment are used efficiently. By reducing bottlenecks and improving workflow, AI helps hospitals provide better care while lowering costs.
- Reducing Patient Wait Times : AI-driven systems can predict peak times and patient influx , allowing hospitals to allocate resources more effectively and reduce wait times for patients. As a result, patient satisfaction improves while the overall quality of care is enhanced.
- Patient Engagement : AI-powered virtual health assistants are being used to engage patients by providing them with information, reminders, and guidance on managing their health conditions. These assistants can answer questions, schedule appointments, and even monitor patients’ symptoms, helping to ensure continuous care outside of the hospital setting.
- Remote Monitoring : AI-enabled devices and applications allow for remote monitoring of patients with chronic conditions, such as diabetes or heart disease. These tools collect and analyze real-time data, alerting healthcare providers to potential issues before they become critical. This proactive approach helps in managing conditions more effectively and reducing hospital readmissions.
Benefits of AI Integration in Healthcare
We know what AI can do for us now, but we already have medical practitioners, so what advantages does the integration of AI bring to the table?
Improved Accuracy
One of the most significant benefits of AI in healthcare is its ability to reduce diagnostic errors, which are a leading cause of patient harm. By analyzing large datasets with precision, AI systems can identify patterns and anomalies that might be missed by human eyes.
For instance, AI-driven imaging tools have been shown to detect early-stage cancers, such as breast and lung cancer, with remarkable accuracy, often outperforming human radiologists. Moreover, AI can integrate data from multiple sources—such as lab results, medical imaging, and patient records—to provide a more comprehensive view, aiding clinicians in making more informed and accurate diagnoses.
Efficiency Gains
AI is also transforming hospital operations by automating routine tasks and optimizing workflows. For example, AI-powered scheduling systems can predict patient volumes and optimize staff allocation, ensuring that the right resources are available at the right time.
This leads to significant efficiency gains, reducing patient wait times, and improving the overall patient experience. Additionally, AI can help manage supply chains by predicting inventory needs and preventing shortages or overstock, ultimately leading to cost savings and better resource allocation. By streamlining these operations, hospitals can focus more on patient care and less on administrative tasks.
Enhanced Patient Care
Plus, AI contributes to more personalized and proactive patient care by leveraging data to tailor treatment plans to individual patients. AI algorithms can analyze a patient’s genetic information, medical history, and lifestyle factors to recommend the most effective treatments, reducing the trial-and-error approach often seen in traditional medicine.
Moreover, AI-driven tools can monitor patients in real-time, alerting healthcare providers to any changes in a patient’s condition that may require immediate attention. This proactive approach helps in preventing complications and improving patient outcomes. AI also plays a role in mental health care by offering personalized therapy through chatbots and virtual assistants, providing continuous support to patients outside of clinical settings.
Data-Driven Insights
The vast amount of data generated in hospitals—ranging from patient records to medical research—holds immense potential for improving healthcare outcomes. AI excels at analyzing big data, identifying trends , and predicting future healthcare needs. For example, AI can analyze epidemiological data to predict outbreaks of infectious diseases, enabling hospitals and public health agencies to prepare and respond more effectively.
In a clinical setting, AI can predict patient outcomes based on historical data, helping healthcare providers to make better treatment decisions and allocate resources more effectively. Additionally, AI-driven predictive analytics can help in identifying at-risk populations, allowing for targeted interventions and preventive measures. These data-driven insights are invaluable in creating more efficient, effective, and responsive healthcare systems .
Challenges and Limitations
Despite its possible benefits, some setbacks must be addressed first. Implementors must first consider data privacy, the possibility of biases, and integration challenges .
AI algorithms are only as good as the data they are trained on. If the data used to develop these algorithms is biased or unrepresentative, the AI can produce biased outcomes , leading to disparities in healthcare.
If an AI system is trained on data predominantly from one demographic group, it may perform poorly when applied to patients from different backgrounds, resulting in suboptimal treatment recommendations. To mitigate this risk, it is crucial to ensure that AI models are trained on diverse and representative datasets and that ongoing monitoring is in place to identify and correct any biases that may emerge.
Another significant challenge is the integration of AI into existing hospital technologies and workflows. Hospitals often rely on a patchwork of legacy systems that may not be compatible with modern AI technologies. Integrating AI requires significant effort to ensure interoperability, which can be both time-consuming and costly.
Similarly, hospital staff may need to be retrained to use AI systems effectively. Ensuring a smooth integration process involves careful planning, collaboration between IT teams and healthcare professionals, and the development of user-friendly interfaces that complement rather than complicate existing workflows.
Lastly, the implementation of AI in hospitals comes with significant costs , which can be a barrier to widespread adoption, particularly in resource-limited settings. Developing, deploying, and maintaining AI systems requires substantial investment in infrastructure, software, and training. Not to mention, the cost of AI technologies can create a digital divide, where well-funded hospitals in wealthy regions can afford cutting-edge AI solutions, while those in less affluent areas may struggle to keep up.
This disparity can lead to unequal access to the benefits of AI in healthcare, exacerbating health inequities. Addressing this challenge requires efforts to reduce the costs of AI technologies, explore scalable solutions for lower-income settings, and ensure that the benefits of AI are accessible to all patients, regardless of where they receive care.
Monetary and cultural problems aside, ethical considerations relating to both patients and healthcare providers.
One of the foremost challenges in adopting AI in hospitals is ensuring the privacy and security of patient data. AI systems rely on vast amounts of sensitive medical information to function effectively, making data protection a critical concern.
However, the integration of AI introduces new vulnerabilities, such as the potential for data breaches or unauthorized access to patient records. Hospitals must comply with stringent regulations that govern the privacy of patients, making sure data is encrypted and anonymized.
While AI systems can analyze data and provide recommendations with incredible speed and accuracy, the final decision in patient care often carries significant moral and ethical weight. For example, an AI might suggest a particular treatment plan based on data, but this recommendation may conflict with the preferences of the patient or the clinical judgment of the healthcare provider.
The challenge lies in determining when to rely on AI’s recommendations and when human judgment should take precedence.
AI algorithms, especially those based on deep learning, can be highly complex and opaque, making it difficult for healthcare providers to understand how certain conclusions or recommendations are reached.
This lack of transparency, often referred to as the “black box” problem, can undermine trust in AI systems and make it challenging to justify their use in patient care. To address this issue, there is a growing emphasis on developing AI systems that are explainable—where the reasoning behind AI decisions is clear and understandable to human users.
There is the concern that AI could replace certain roles, leading to job displacement and a loss of the human touch in healthcare. The ethical challenge here is to strike a balance where AI enhances, rather than diminishes, the role of healthcare professionals . This involves ensuring that AI is seen as a tool that supports and augments human skills, rather than a replacement.
Case Studies and Real-world Examples
Looking to successful AI implementation in healthcare systems around the world allows to us to see what AI brings to the table.
Radiology has been one of the most impactful areas for AI implementation, with AI algorithms being used to analyze medical images such as X-rays, MRIs, and CT scans to detect conditions like tumors, fractures, and other abnormalities.
Institutions such as the Mayo Clinic and the University of California, San Francisco (UCSF) have successfully integrated AI into their radiology departments. In these, we see how AI has significantly improved the accuracy and efficiency of radiological diagnoses, often detecting abnormalities that may be missed by human radiologists. This has led to earlier detection of diseases, improved patient outcomes, and enhanced diagnostic throughput, allowing radiologists to focus on more complex cases.
What do we learn from these implementations?
- Collaboration is Key : Successful AI implementations underscore the importance of collaboration between AI developers, healthcare professionals, and IT teams.
- Training and Adaptation : Comprehensive training programs are essential to help healthcare professionals understand and effectively use AI tools.
- Data Quality and Diversity Matter : The effectiveness of AI systems is heavily dependent on the quality and diversity of the data they are trained on.
- Ethical Considerations and Transparency : Transparency and ethical guidelines are critical for maintaining trust in AI systems.
- Scalability and Continuous Improvement : Successful AI implementations are designed with scalability in mind, allowing for expansion as the hospital’s needs evolve.
Conclusions
The future of AI in healthcare holds exciting possibilities, with emerging technologies like AI-driven drug discovery and robotics in surgery poised to further revolutionize patient care. As we’ve explored, AI offers significant benefits in enhancing diagnostic accuracy, operational efficiency, and personalized care .
However, challenges such as data privacy, algorithmic bias, and the integration of AI into existing systems must be carefully managed. Moreover, ethical considerations, including transparency, accountability, and the impact on healthcare professionals, are paramount to ensuring AI’s responsible use.
The potential of AI to transform healthcare is immense, but it must be approached with caution and ethical foresight. As AI continues to advance, healthcare leaders are encouraged to proactively explore its possibilities while addressing the challenges head-on. This will allow healthcare to harness the power of AI to create a more efficient, equitable, and patient-centered system.
How is AI helping doctors in medical diagnosis?
AI is revolutionizing healthcare by assisting doctors in medical diagnosis through advanced machine learning algorithms that analyze patient data, medical images, and lab results. These AI-driven tools enhance accuracy, reduce diagnostic errors, and provide personalized treatment recommendations, enabling more effective patient care.
What are the benefits of AI in Electronic Health Records (EHR)?
AI in electronic health record (EHR) systems is transforming healthcare by automating data entry, improving patient record management, and providing predictive analytics. This leads to enhanced efficiency, reduced administrative burden, and better patient outcomes, as healthcare providers can access comprehensive, real-time patient data for informed decision-making.
Who are the leading providers of AI technology in healthcare?
Leading providers of AI technology in healthcare include companies like IBM Watson, Google Health, and Siemens Healthineers. These organizations are at the forefront of developing AI solutions for diagnostics, personalized medicine, and automated health systems, driving innovation across the medical field.
How is the AI market in healthcare expected to grow?
The AI market in healthcare is rapidly expanding, driven by advancements in AI applications such as drug discovery, robotics in surgery, and machine learning in patient care. As AI continues to prove its value in improving healthcare efficiency and patient outcomes, the industry is poised for significant growth, making healthcare a major AI industry.
Hire Top 1% Engineers
Trending articles, eugenia shevchenko on the prospect of remote employment, gaper.io features b-labs about achieving sustainable goals, hiring tech talent amid covid-19 crisis here’s a surefire way to hire top 1% vetted engineers, cynthia shares about remote work at stix – only on gaper.io, gaper shares scott’s perspective on the future of remote employment, looking for top talent, next article.

Innovative Python-based business ventures to launch in 2024
Hire top 1% engineers for your startup in 24 hours.
Top quality ensured or we work for free

Gaper.io @2023 All rights reserved.
Leading Marketplace for Software Engineers
Subscribe to receive latest news, discount codes & more
Stay updated with all that’s happening at Gaper
Official websites use .gov
A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS
A lock ( ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
Health Equity and Ethical Considerations in Using Artificial Intelligence in Public Health and Medicine
COMMENTARY — Volume 21 — August 22, 2024
Irene Dankwa-Mullan, MD, MPH 1 ( View author affiliations )
Suggested citation for this article: Dankwa-Mullan I. Health Equity and Ethical Considerations in Using Artificial Intelligence in Public Health and Medicine. Prev Chronic Dis 2024;21:240245. DOI: http://dx.doi.org/10.5888/pcd21.240245 .
PEER REVIEWED
Introduction
Background on ai in public health and medicine, the importance of promoting health equity and addressing bias in ai applications, sources and risk of bias, ethical considerations in the use of artificial intelligence, challenges and opportunities, acknowledgments, author information.
What is already known on this topic?
Artificial intelligence (AI) is increasingly used in health care for diagnostics, predictive analytics, and personalized medicine, but it can exacerbate health disparities and ethical concerns if not carefully managed.
What is added by this report?
This commentary highlights the multifaceted approach and strategies to promote health equity and ethical use of AI, emphasizing community engagement, inclusive data practices, and transparent algorithms.
What are the implications for public health practice?
Implementing these strategies can ensure that AI benefits all populations equitably, enhancing trust and effectiveness in public health interventions and medical care.
This commentary explores the critical roles of health equity and ethical considerations in the deployment of artificial intelligence (AI) in public health and medicine. As AI increasingly permeates these fields, it promises substantial benefits but also poses risks that could exacerbate existing disparities and ethical challenges. This commentary delves into the current integration of AI technologies, underscores the importance of ethical social responsibility, and discusses the implications for practice and policy. Recommendations are provided to ensure AI advancements are leveraged responsibly, promoting equitable health outcomes and adhering to rigorous ethical standards across all populations.
The integration of artificial intelligence (AI) in public health and medicine is revolutionizing how health care and public health professionals approach health care delivery, disease prediction, population health, and patient care management (1). As these technologies evolve, they offer unprecedented opportunities for expanding precision health, enhancing efficiency, and optimizing effectiveness in health services (2). However, this integration also prompts critical discussions of the ethical use of AI and the imperative to ensure health equity. This commentary explores how AI is reshaping public health and medicine, concerns about bias, ethical challenges, and the importance of incorporating an equity lens in its deployment.
AI’s potential to transform health is immense, from improving diagnostic accuracy to personalizing treatment plans and predicting disease trends (2). Yet, as we stand on the brink of this technological revolution, it is crucial to address the ethical implications and ensure that these advancements benefit all sections of society equitably. The misuse or unethical application of AI can lead to increased disparities and further exacerbate adverse outcomes for socially and economically disadvantaged populations.
This commentary not only discusses the current applications and benefits of AI but also emphasizes the critical need to maintain a balance between innovation and ethical responsibilities. The commentary explores the historical context of technological transitions in health, examines the effect of AI on health equity, and provides actionable insights and recommendations to guide practitioners, policymakers, researchers, and developers. The aim is to foster a health care environment that not only embraces technological advancements but also upholds the highest standards of equity and ethical practice.
Historical perspective
The integration of technology in health care is not a novel concept. AI was initially described in the 1950s as expert computer systems that could mimic human intelligence (2). These systems were followed in the 2000s by the emergence of computer vision and machine learning (2). Even though researchers continued to explore AI technologies with the evolution of data, the rapid advancement and adoption of AI has come to represent a transformative shift in the landscape. Technological innovations such as the electronic health record (EHR) and medical imaging revolutionized medical diagnostics and patient record management (2). Today, AI builds on these foundational advancements by offering more sophisticated tools for data analysis and clinical decision-making.
Current trends
AI is now being used across various facets of public health and medicine, substantially altering how health professionals engage with their patients, communities, and health data. Two key areas where AI is making a mark are diagnostic algorithms and predictive analytics (2). For example, AI algorithms are being increasingly used to diagnose diseases from imaging scans — with higher accuracy and speed than human radiologists (3). In predictive analytics, AI can forecast outbreaks of diseases (4), hospital readmission rates (5), and a patient’s risk of developing chronic illnesses (6) by analyzing vast datasets. In this era of precision medicine, AI can help in tailoring medical treatments to individual genetic profiles, potentially improving outcomes and minimizing side effects (7). Public health surveillance, disease forecasting, and epidemic modeling are increasingly becoming important areas for integration of AI-based tools (6). These applications showcase a few of AI’s potential to enhance the efficacy and precision of public health and clinical decision-making. However, they also bring to light the need for a robust framework to manage these technologies responsibly.
Transition challenges
As the public health and health care sectors navigate their way through digital transformation, several challenges emerge. These include technology challenges, widening knowledge gaps, and overall hesitance and resistance to change. For example, integrating AI into any existing public health or health care infrastructure requires substantial technology upgrades, a robust data architecture, and staff training. Apart from providing upgrades, gaps in understanding AI technologies among health care providers can hinder their effective implementation. In addition to that, adapting to AI-driven methods requires changes in established workflows and practices, which often meet with resistance from traditional health care providers. As AI continues to evolve, the health care industry must not only keep pace with these technological changes but also anticipate future developments. Addressing these challenges head-on will be essential for leveraging AI to improve health outcomes while ensuring that such technologies are used ethically and equitably.
The potential of AI to transform public health and medicine is immense. Yet, as health professionals harness these technologies, they must also consider the implications on health equity and ethical practices. Health equity in the context of AI applications refers to the fair and just distribution of health technologies and their benefits (8). It ensures that all individuals have access to the same high-quality health care services, regardless of their socioeconomic status, race, sex or gender, ethnicity, disability status, or geographic location (8). The deployment of AI diagnostic tools for diabetic retinopathy primarily in well-resourced health care settings or among populations with insurance coverage exemplifies an unfair distribution of technology. This approach disproportionately benefits people with greater economic means and access while potentially excluding socially or economically disadvantaged populations that may have a higher prevalence of disease but lack the resources or insurance necessary to access such advanced diagnostic tools. Equity is the absence of systematic disparities in health, or in the social determinants of health, between groups with different levels of underlying social advantage such as wealth, power, privilege, and prestige (9). For AI to be truly transformative, it must not only advance health care and outcomes but do so in a way that bridges existing health disparities rather than widening them.
One of the most noteworthy concerns with AI is the risk of bias in algorithms, which can inadvertently perpetuate existing health disparities. AI bias is a general concept that refers to the fact that an AI system has been designed in a way that makes the system’s decisions or use unfair (10). These AI data biases often arise from various sources, including the processes of data access, collection, acquisition, preparation, processing, development, and validation (11). Bias can also arise from the processes through which scientific evidence is generated, from lack of research diversity and from inadequate data governance. AI models are typically trained on available data, which may not adequately represent racial and ethnic minority groups or other populations that are medically underserved (11). For example, Obermeyer et al discovered that commercial algorithms, which use cost as a proxy for illness, exhibit racial bias by inadequately identifying the health needs of Black patients compared with White patients despite similar levels of chronic illnesses (12). Training data can also reflect historical biases in treatment and access to care for socially disadvantaged populations, leading AI to replicate these injustices (12). Finally, many AI tools are so-called black boxes — in which decision-making processes are not transparent — making it difficult to assess and rectify biases (13). These are some of the problems that underscore the need for meticulous oversight and corrective measures in the development and deployment of AI technologies to ensure they serve all populations equitably.
Even though addressing AI biases has primarily focused on algorithms, external sources of AI bias exist. They include experience and expertise, exclusion, environment, empathy, and evidence (14).
Experience and expertise bias
Experience and expertise bias refers to the skew introduced by the varying levels of expertise among individuals involved in developing AI systems (14). This bias can manifest in several ways including:
- Training data quality: The quality of the training data can be influenced by the expertise of those who collect, label, and input the data. Inconsistent or incorrect labeling due to lack of expertise can lead to a biased model (2,11,15).
- Algorithm development: The design and tuning of algorithms require a high level of expertise. Inadequate expertise can result in models that do not generalize well across diverse populations (2).
- Clinical implementation: Varying levels of familiarity with AI tools among health care providers can affect how these tools are implemented and interpreted, potentially leading to biased outcomes (2,14,16).
Exclusion bias
Exclusion bias occurs when certain groups are systematically left out of the data collection and analysis processes (14). This bias can result in AI systems that do not accurately represent or serve the entire population. Some examples are:
- Data missingness: When data are missing or incomplete for groups within a dataset, the AI system may not learn patterns relevant to these groups, leading to poorer performance for them compared with other groups (2,11).
- Underrepresentation: Exclusion of certain demographic groups in clinical trials or datasets can cause AI to be less effective or even harmful to these groups (2,11).
- Access to care: AI tools developed without considering socially or economically marginalized populations might not address the unique barriers these groups face in accessing health care (2,11).
Environment bias
Environment bias arises from the socio-environmental context in which data are collected and used (14). This bias can include the following:
- Social determinants of health: Factors such as income, education, and living conditions can influence health outcomes and need to be adequately represented in datasets (2,11).
- Physical environment: Geographic and environmental factors (eg, urban vs rural settings) can affect health outcomes and must be considered to avoid biased AI predictions (2,11).
- Integration of environmental factors: Ensuring that environmental variables are incorporated into AI models can help in understanding and mitigating health disparities.
Empathy bias
Empathy bias refers to the challenge of incorporating human experiences and subjective elements that are difficult to quantify into AI systems (14). This bias includes:
- Quantitative versus qualitative data: AI systems primarily rely on quantitative data, which can miss nuanced human experiences that affect health outcomes.
- Patient preferences: Empathy bias can occur when AI systems do not consider patient preferences, values, and unique circumstances, leading to recommendations that are misaligned with patient needs (14).
- Human stories: Integrating personal stories and experiences into AI models can enhance their relevance and fairness, although this factor presents a complex challenge.
Evidence bias
Evidence bias involves the processes through which scientific evidence is generated, disseminated, and translated into practice (14). This bias can affect the overall reliability and applicability of AI systems. Examples include:
- Research funding: How research is funded can introduce biases, as funding priorities may not align with the needs of all populations.
- Publication bias: There is often a bias toward publishing positive results, which can skew the evidence base that AI systems rely on.
- Translation to practice: The way evidence is translated into clinical guidelines and policies can introduce biases if it does not consider the diversity of patient populations and contexts.
AI is not a monolithic entity; rather, it comprises various interconnected technologies and data inputs of intricate stacks playing a distinct role, contributing to the overall functionality, outputs, and intelligence of the system. To enhance clarity and understanding about sources of biases, it is beneficial to conceptualize the stack of interconnected technologies and inputs ( Table ). Biases that occur during the development of AI tools or models were mapped to specific points in the stack, to identify their origins and implement targeted strategies to address them ( Table ).
To mitigate the risk of bias and promote health equity in AI, several strategic actions are recommended. These actions include collecting data from diverse population groups to ensure AI systems are well-informed and represent the variability in human health; developing AI with explainable outcomes to allow users to understand and trust decisions and ensure accountability in AI-driven processes; continuously monitoring AI systems for biased outcomes; and adjusting algorithms accordingly to ensure they remain equitable over time.
Specific proposed strategies for addressing bias follow.
Addressing experience and expertise bias
- Diverse expert teams: Assemble multidisciplinary teams with diverse expertise, including data scientists, clinicians, ethicists, and social scientists, to inform, develop, and evaluate AI systems.
- Continuous training: Provide ongoing education and training for health care providers on AI technologies to ensure they are proficient in using and interpreting AI tools.
- Standardized protocols: Develop and adhere to standardized protocols for data collection, labeling, and algorithm development to minimize variability due to different levels of expertise.
Addressing exclusion bias
- Inclusive data collection: Ensure datasets include diverse demographic groups by actively recruiting underrepresented populations in data collection efforts.
- Equity audits: Conduct regular equity audits of AI systems to identify and address any exclusion of populations.
- Accessible AI solutions: Design AI tools with accessibility in mind, ensuring that they cater to the needs of socially and economically marginalized populations and do not perpetuate existing barriers to care.
Addressing environment bias
- Integration of social determinants: Include social determinants of health (eg, income, education, housing) in AI models to provide a more holistic understanding of health outcomes.
- Geospatial analysis: Use geospatial analysis to incorporate environmental factors such as air quality, water access, and neighborhood characteristics into health data.
- Contextual adaptation: Adapt AI models to local contexts, ensuring that they account for regional variations in social and environmental factors that affect health.
Addressing empathy bias
- Incorporation of qualitative data: Combine quantitative data with qualitative insights from patient interviews, focus groups, and patient narratives to capture a full picture of health experiences.
- Patient-centered design: Engage patients in the design and development of AI systems to ensure that their preferences, values, and experiences are reflected in the models.
- Ethical review boards: Establish ethical review boards that include patient representatives to oversee the development and deployment of AI tools, ensuring they align with patient needs and ethical standards.
Addressing evidence bias
- Diversification of funding: Advocate for diverse funding sources to support research that addresses the health needs of varied populations, avoiding biases introduced by funding priorities.
- Transparent reporting: Encourage transparent reporting of all research findings, including negative results, to build a comprehensive and unbiased evidence base.
- Inclusive guidelines: Develop clinical guidelines that are inclusive and consider the diverse patient populations and contexts in which they will be applied.
These strategies illustrate that while biases in the development and deployment of AI present challenges to health equity, with careful planning and ethical consideration AI also offers substantial opportunities to enhance health care for all. By prioritizing equity in the design and implementation of AI, public health professionals and medical practitioners can use these powerful tools to not only improve health outcomes but also ensure these improvements are shared across all segments of the population.
Ethical frameworks
The deployment of AI in health necessitates adherence to established ethical frameworks designed to guide clinical practice and technological development (18,19). These frameworks typically emphasize principles that must be carefully considered when integrating AI into health care settings (18,19). Principles of beneficence and nonmaleficence ensure that AI technologies benefit patients and do not cause harm, whether through error, bias, or misuse (18,19). Another ethical AI principle is preserving patient autonomy by maintaining transparency and consent in AI interactions (18,19). Fairness and justice principles ensure that AI-driven tools do not create or exacerbate inequalities but rather promote equitable access to health care services (18,19).
Privacy and confidentiality
With AI’s ability to process vast amounts of personal data, safeguarding patient privacy and confidentiality becomes paramount (18,19). These safeguards involve several key concerns about data security, informed consent, and misuse of data. It is critical to implement robust security measures to protect health data against unauthorized access and breaches (18,19). In addition, for populations with limited English proficiency, it is important to make sure informed consent forms are reviewed and explained to patients or translated. In this digital age, we can consider refining consent forms and including concise language for patients on how their data will be used in AI systems to inform their care. Finally, as part of ensuring privacy and confidentiality and limiting potential misuse, we should encourage collecting only data that are necessary for a specific AI application.
Decision-making
AI’s role in clinical decision-making, public health interventions, and population health management introduces complexities in the extent of human oversight and the transparency of AI decisions. To ensure human oversight, we should establish guidelines for human oversight in AI-driven decisions, ensuring that machines augment rather than replace human judgment. To maintain trust and accountability, it is also important to develop AI systems whose actions can be understood and explained to practitioners and patients. Finally, determining how responsibilities and liabilities are shared among AI developers, health professionals, and institutions when AI is used in patient care is a complex and critical component of integrating AI into health care systems. This component involves understanding the roles and obligations of each partner to ensure patient safety, legal compliance, and ethical standards are upheld. Developers are responsible for creating accurate, reliable, and safe AI tools. Health care providers using AI tools must be adequately trained and responsible for interpreting AI outputs correctly, making final clinical decisions based on a combination of AI insights, patient values, and their professional judgment. Public health professionals must be guided by the principles of responsibility and ethics to enhance the ability to analyze data, predict health trends, and implement effective interventions to ensure the well-being of individuals and communities. Institutions need to establish policies and provide oversight to monitor AI performance, ensuring compliance with legal and ethical standards.
Community engagement
Involving diverse communities in the AI development lifecycle is essential for its ethical application in public health and medicine. This approach ensures that AI systems are developed with a comprehensive understanding of the unique needs and challenges faced by various populations. Benefits of community engagement include enhanced relevance of the AI system to address the actual needs and preferences of the population, leading to better outcomes, and an increased trust and acceptance, with likelihood of successful implementation of the AI system (20).
The ethical integration of AI in health care and public health presents both challenges and opportunities. For example, AI can potentially streamline workflows and enhance diagnostic accuracy, but it also raises issues such as the potential for dehumanization in care and reduced patient–provider interactions (17). By addressing these ethical considerations proactively, working partners in public health and medicine can leverage AI to improve population health and health care outcomes while maintaining a commitment to ethical practice. As we delve into the transformative potential of AI in public health and medicine, it becomes increasingly apparent that while AI offers substantial benefits for health care efficiency and effectiveness, it also introduces substantial ethical and equity challenges.
To promote health equity and ethical AI use in public health and medicine, it is recommended to develop inclusive AI policies, enhance ethical frameworks, and ensure transparency and accountability ( Figure ). Investing in public and professional education about AI, fostering community engagement, and integrating social determinants of health into AI models are essential. Additionally, diverse funding for research and evidence, continuous monitoring and evaluation of AI systems, and interdisciplinary collaboration are crucial strategies to ensure AI technologies are fair, equitable, and beneficial for all populations ( Figure ) .
To advance public health and medicine responsibly, it is also imperative that partners work collaboratively to ensure that AI technologies not only meet the highest standards of innovation but also adhere to ethical and equitable practices. By implementing these recommendations, health care and public health professionals can leverage AI to enhance health care outcomes while safeguarding against potential inequalities and ethical transgressions.
This comprehensive approach ensures that AI serves as a tool for positive change, propelling public health and medicine into a future where technology and human values are aligned to promote the well-being of all individuals.
The author received no external financial support for the research, authorship or publication of this article. The author declares no potential conflicts of interest with respect to the research, authorship or publication of this article. No copyrighted material, surveys, instruments, or tools were used in the research described in this article.
Corresponding Author: Irene Dankwa-Mullan, MD, MPH, Department of Health Policy and Management, Milken Institute School of Public Health, The George Washington University, 2175 K Street NW, Washington, DC 20037 ( [email protected] ).
Author Affiliations: 1 Department of Health Policy and Management, Milken Institute School of Public Health, The George Washington University, Washington, District of Columbia.
- Alowais SA, Alghamdi SS, Alsuhebany N, Alqahtani T, Alshaya AI, Almohareb SN, et al. . Revolutionizing healthcare: the role of artificial intelligence in clinical practice. BMC Med Educ . 2023;23(1):689. PubMed doi:10.1186/s12909-023-04698-z
- Roski J, Chapman W, Heffner J, Trivedi R, Del Fiol G, Kukafka R, et al. . Chapter 3: How artificial intelligence is changing health and health care. In: Matheny M, Israni ST, Ahmed M, Whicher D, eds. Artificial Intelligence in Health Care: The Hope, the Hype, the Promise, the Peril . The National Academies Press; 2019:65–98.
- Rajpurkar P, Chen E, Banerjee O, Topol EJ. AI in health and medicine. Nat Med . 2022;28(1):31–38. PubMed doi:10.1038/s41591-021-01614-0
- Zeng D, Cao Z, Neill DB. Artificial intelligence–enabled public health surveillance — from local detection to global epidemic monitoring and control. Artif Intell Med . 2021:437–453.
- Romero-Brufau S, Wyatt KD, Boyum P, Mickelson M, Moore M, Cognetta-Rieke C. Implementation of artificial intelligence-based clinical decision support to reduce hospital readmissions at a regional hospital. Appl Clin Inform . 2020;11(4):570–577. PubMed doi:10.1055/s-0040-1715827
- Rashid J, Batool S, Kim J, Wasif Nisar M, Hussain A, Juneja S, et al. . An augmented artificial intelligence approach for chronic diseases prediction. Front Public Health . 2022;10:860396. PubMed doi:10.3389/fpubh.2022.860396
- Johnson KB, Wei WQ, Weeraratne D, Frisse ME, Misulis K, Rhee K, et al. . Precision medicine, AI, and the future of personalized health care. Clin Transl Sci . 2021;14(1):86–93. PubMed doi:10.1111/cts.12884
- Gurevich E, El Hassan B, El Morr C. Equity within AI systems: what can health leaders expect? Healthc Manage Forum . 2023;36(2):119–124. PubMed doi:10.1177/08404704221125368
- Braveman P, Gruskin S. Defining equity in health. J Epidemiol Community Health . 2003;57(4):254–258. PubMed doi:10.1136/jech.57.4.254
- Schwartz R, Vassilev A, Greene K, Perine L, Burt A, Hall P. Special Publication 1270: Towards a Standard for Identifying and Managing Bias in Artificial Intelligence . National Institutes of Standards and Technology. March 2022. Accessed May 29, 2024. https://nvlpubs.nist.gov/nistpubs/SpecialPublications/NIST.SP.1270.pdf
- Nazer LH, Zatarah R, Waldrip S, Ke JXC, Moukheiber M, Khanna AK, et al. . Bias in artificial intelligence algorithms and recommendations for mitigation. PLOS Digit Health . 2023;2(6):e0000278. PubMed doi:10.1371/journal.pdig.0000278
- Obermeyer Z, Powers B, Vogeli C, Mullainathan S. Dissecting racial bias in an algorithm used to manage the health of populations. Science . 2019;366(6464):447–453. PubMed doi:10.1126/science.aax2342
- Mann H. Do all AI systems need to be explainable?. Stanford Social Innovation Review. November 15, 2023. Accessed July 10, 2024. https://ssir.org/articles/entry/do_ai_systems_need_to_be_explainable
- Dankwa-Mullan I, Weeraratne D. Artificial intelligence and machine learning technologies in cancer care: addressing disparities, bias, and data diversity. Cancer Discov . 2022;12(6):1423–1427. PubMed doi:10.1158/2159-8290.CD-22-0373
- Yang J, Soltan AAS, Eyre DW, Yang Y, Clifton DA. An adversarial training framework for mitigating algorithmic biases in clinical machine learning. NPJ Digit Med . 2023;6(1):55. PubMed doi:10.1038/s41746-023-00805-y
- Chen Y, Clayton EW, Novak LL, Anders S, Malin B. Human-centered design to address biases in artificial intelligence. J Med Internet Res . 2023;25:e43251. PubMed doi:10.2196/43251
- Ferrara E. Fairness and bias in artificial intelligence: a brief survey of sources, impacts, and mitigation strategies. Sci. 2024;6(1):3.
- Mennella C, Maniscalco U, De Pietro G, Esposito M. Ethical and regulatory challenges of AI technologies in healthcare: a narrative review. Heliyon . 2024;10(4):e26297. PubMed doi:10.1016/j.heliyon.2024.e26297
- Dankwa-Mullan I, Scheufele EL, Matheny M, Quintana Y, Chapman W, Jackson G, et al. . A proposed framework on integrating health equity and racial justice into the artificial intelligence development lifecycle. J Health Care Poor Underserved . 2021;32(2):300–317.
- Rajamani G, Rodriguez Espinosa P, Rosas LG. Intersection of health informatics tools and community engagement in health-related research to reduce health inequities: scoping review. J Particip Med . 2021;13(3):e30062. PubMed doi:10.2196/30062
| Interconnected stack of AI technologies | Points where biases can occur | Reference |
|---|---|---|
| • Experience and expertise bias • Exclusion bias • Environment bias • Empathy bias • Evidence bias | Dankwa-Mullan and Weeraratne (14) | |
| Data collection: gathering raw data from various sources (eg, sensors, user inputs, patient-reported outcomes, electronic health records and administrative claims databases, community health–related and social surveys, public health surveys, clinical trials, research data) | • Data sampling bias: Occurs when the data collected are not representative of the population of focus, leading to skewed insights. • Historical bias Biases present in historical data can be perpetuated. For example, if past hiring practices favored certain demographic characteristics, a model trained on this data might continue to favor these characteristics. | Roski et al (2); Nazer et al (11) |
| Data preparation and preprocessing: cleaning, transforming, and structuring data for analysis | • Data cleaning bias: Bias can be introduced during the data cleaning process if certain data points are disproportionately removed or altered. For example, removing outliers might inadvertently exclude data on minority groups. • Feature selection bias: Occurs when choosing features that reflect existing prejudices or systemic biases. For example, using zip code as a feature in credit scoring might unintentionally introduce racial and/or socioeconomic bias. | Roski et al (2); Nazer et al (11) |
| Feature engineering: Creating relevant features from raw data to improve model performance | • Human bias in feature selection: The selection and creation of features can reflect the biases of the individuals involved in the process. For example, selecting features that favor certain groups over others: frequency of health care visits or access to specialists care can favor people with better access, and variables that measure engagement with digital health tools can favor younger or more tech-savvy populations. • Overfitting specific biases: Creating features that overfit the training data might capture and reinforce biases present in that data. | Chen et al (16) |
| Model selection: Choosing the appropriate algorithms and models for the task | • Algorithmic bias: Some algorithms might inherently favor certain patterns or demographic groups, which may lead to algorithmic bias. For example, decision trees might create splits that disproportionately affect certain demographics. • Inherent biases in model architecture: Certain model architectures may have biases based on their design. For example, linear models might fail to capture complex patterns in data related to underrepresented groups. | Roski et al (2); Nazer et al (11) |
| Model training: Training the model using prepared data | • Training data bias: Bias in the training data can lead to biased model outcomes. For example, if the training data contains biased labels, the model will learn and reproduce those biases. • Overfitting and underfitting: Overfitting to biased training data can exacerbate biases (by tailoring the model too closely to the training data), while underfitting might fail to capture important nuances, leading to a lack of fairness. | Roski et al (2); Yang et al (15) |
| Model evaluation and validation: Using metrics and validation techniques to assess the model’s performance | • Validation set bias: Bias in the evaluation process can arise if the validation set is not representative or if biased metrics are used to assess performance. In other words, if the validation set is not representative, it can lead to misleading performance metrics. For example, evaluating a model on a biased subset might indicate good performance while hiding biases. • Metric selection bias: This bias results from choosing evaluation metrics that do not capture fairness aspects. For example, using accuracy alone might ignore disparities in model performance across different groups. | Roski et al (2) |
| Model deployment: Integrating the trained model into production environments | • Deployment context bias: The deployment context can introduce bias if the model is used in a different environment than it was trained for, affecting its performance and fairness. The environment in which the model is deployed might differ from the training environment, introducing bias. For example, a model trained in one geographical area might not perform well in another. • Real-world feedback loop bias: As the model interacts with the real world, it might receive biased feedback, reinforcing existing biases. For example, a recommendation system might continue to favor popular items, ignoring niche interests. | Ferrara (17) |
| Monitoring and maintenance: Continuously monitoring model performance and making updates | • Drift in data distribution: As models are used over time, changes in data distributions can introduce new biases, and feedback loops can reinforce existing biases. Over time, the data distribution might change, leading to biases if the model is not updated. For example, shifts in consumer behavior can render an e-commerce model biased if it remains static. • Ongoing feedback bias: Continuous feedback loops can reinforce existing biases. For example, if a model’s recommendations are followed by users, the resulting data might further entrench those recommendations. | Roski et al (2); Ferrara (17) |
The opinions expressed by authors contributing to this journal do not necessarily reflect the opinions of the U.S. Department of Health and Human Services, the Public Health Service, the Centers for Disease Control and Prevention, or the authors’ affiliated institutions.

- My Favorites
You have successfully logged in but...
... your login credentials do not authorize you to access this content in the selected format. Access to this content in this format requires a current subscription or a prior purchase. Please select the WEB or READ option instead (if available). Or consider purchasing the publication.
OECD Artificial Intelligence Papers
Initial policy considerations for generative artificial intelligence.
The OECD engages in comprehensive research and analysis to deepen insights into the transformative power of artificial intelligence (AI) and its implications for economies and societies. The OECD Artificial Intelligence Papers series draws on comprehensive evidence-base to identify trends and developments and delve into an extensive array of AI-related subjects. This includes opportunities and challenges in AI governance, the impact of AI across policy domains including labour markets, education and healthcare, ethical considerations in AI design and deployment, and new frontiers such as generative AI. This collection encompasses OECD policy papers as well as working papers.

- Science and Technology
- Social Issues/Migration/Health
- ISSN: 3005348X (online)
- https://doi.org/10.1787/dee339a8-en
- Subscribe to the RSS feed Subscribe to the RSS feed
Generative artificial intelligence (AI) creates new content in response to prompts, offering transformative potential across multiple sectors such as education, entertainment, healthcare and scientific research. However, these technologies also pose critical societal and policy challenges that policy makers must confront: potential shifts in labour markets, copyright uncertainties, and risk associated with the perpetuation of societal biases and the potential for misuse in the creation of disinformation and manipulated content. Consequences could extend to the spreading of mis- and disinformation, perpetuation of discrimination, distortion of public discourse and markets, and the incitement of violence. Governments recognise the transformative impact of generative AI and are actively working to address these challenges. This paper aims to inform these policy considerations and support decision makers in addressing them.
- Click to access:
- Click to download PDF - 3.27MB PDF

Cite this content as:
Author(s) Philippe Lorenz, Karine Perset and Jamie Berryhill
18 Sept 2023
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Elsevier - PMC COVID-19 Collection

The rise of artificial intelligence in healthcare applications
1 Sonohaler, Copenhagen, Denmark
Kaveh Memarzadeh
2 ChemoMetec, Lillerød, Denmark
Big data and machine learning are having an impact on most aspects of modern life, from entertainment, commerce, and healthcare. Netflix knows which films and series people prefer to watch, Amazon knows which items people like to buy when and where, and Google knows which symptoms and conditions people are searching for. All this data can be used for very detailed personal profiling, which may be of great value for behavioral understanding and targeting but also has potential for predicting healthcare trends. There is great optimism that the application of artificial intelligence (AI) can provide substantial improvements in all areas of healthcare from diagnostics to treatment. It is generally believed that AI tools will facilitate and enhance human work and not replace the work of physicians and other healthcare staff as such. AI is ready to support healthcare personnel with a variety of tasks from administrative workflow to clinical documentation and patient outreach as well as specialized support such as in image analysis, medical device automation, and patient monitoring. In this chapter, some of the major applications of AI in healthcare will be discussed covering both the applications that are directly associated with healthcare and those in the healthcare value chain such as drug development and ambient assisted living.
2.1. The new age of healthcare
Big data and machine learning are having an impact on most aspects of modern life, from entertainment, commerce, and healthcare. Netflix knows which films and series people prefer to watch, Amazon knows which items people like to buy when and where, and Google knows which symptoms and conditions people are searching for. All this data can be used for very detailed personal profiling, which may be of great value for behavioral understanding and targeting but also has potential for predicting healthcare trends. There is great optimism that the application of artificial intelligence (AI) can provide substantial improvements in all areas of healthcare from diagnostics to treatment. There is already a large amount of evidence that AI algorithms are performing on par or better than humans in various tasks, for instance, in analyzing medical images or correlating symptoms and biomarkers from electronic medical records (EMRs) with the characterization and prognosis of the disease [1] .
The demand for healthcare services is ever increasing and many countries are experiencing a shortage of healthcare practitioners, especially physicians. Healthcare institutions are also fighting to keep up with all the new technological developments and the high expectations of patients with respect to levels of service and outcomes as they know it from consumer products including those of Amazon and Apple [2] . The advances in wireless technology and smartphones have provided opportunities for on-demand healthcare services using health tracking apps and search platforms and have also enabled a new form of healthcare delivery, via remote interactions, available anywhere and anytime. Such services are relevant for underserved regions and places lacking specialists and help reduce costs and prevent unnecessary exposure to contagious illnesses at the clinic. Telehealth technology is also relevant in developing countries where the healthcare system is expanding and where healthcare infrastructure can be designed to meet the current needs [3] . While the concept is clear, these solutions still need substantial independent validation to prove patient safety and efficacy.
The healthcare ecosystem is realizing the importance of AI-powered tools in the next-generation healthcare technology. It is believed that AI can bring improvements to any process within healthcare operation and delivery. For instance, the cost savings that AI can bring to the healthcare system is an important driver for implementation of AI applications. It is estimated that AI applications can cut annual US healthcare costs by USD 150 billion in 2026. A large part of these cost reductions stem from changing the healthcare model from a reactive to a proactive approach, focusing on health management rather than disease treatment. This is expected to result in fewer hospitalizations, less doctor visits, and less treatments. AI-based technology will have an important role in helping people stay healthy via continuous monitoring and coaching and will ensure earlier diagnosis, tailored treatments, and more efficient follow-ups.
The AI-associated healthcare market is expected to grow rapidly and reach USD 6.6 billion by 2021 corresponding to a 40% compound annual growth rate [4] .
2.1.1. Technological advancements
There have been a great number of technological advances within the field of AI and data science in the past decade. Although research in AI for various applications has been ongoing for several decades, the current wave of AI hype is different from the previous ones. A perfect combination of increased computer processing speed, larger data collection data libraries, and a large AI talent pool has enabled rapid development of AI tools and technology, also within healthcare [5] . This is set to make a paradigm shift in the level of AI technology and its adoption and impact on society.
In particular, the development of deep learning (DL) has had an impact on the way we look at AI tools today and is the reason for much of the recent excitement surrounding AI applications. DL allows finding correlations that were too complex to render using previous machine learning algorithms. This is largely based on artificial neural networks and compared with earlier neural networks, which only had 3–5 layers of connections, DL networks have more than 10 layers. This corresponds to simulation of artificial neurons in the order of millions.
There are numerous companies that are frontrunners in this area, including IBM Watson and Google’s Deep Mind. These companies have shown that their AI can beat humans in selected tasks and activities including chess, Go, and other games. Both IBM Watson and Google’s Deep Mind are currently being used for many healthcare-related applications. IBM Watson is being used to investigate for diabetes management, advanced cancer care and modeling, and drug discovery, but has yet to show clinical value to the patients. Deep Mind is also being looked at for applications including mobile medical assistant, diagnostics based on medical imaging, and prediction of patient deterioration [6] , [7] .
Many data and computation-based technologies have followed exponential growth trajectories. The most known example is that of Moore’s law, which explains the exponential growth in the performance of computer chips. Many consumer-oriented apps have experienced similar exponential growth by offering affordable services. In healthcare and life science, the mapping of the human genome and the digitization of medical data could result in a similar growth pattern as genetic sequencing and profiling becomes cheaper and electronic health records and the like serve as a platform for data collection. Although these areas may seem small at first, the exponential growth will take control at some point. Humans are generally poor at understanding exponential trends and have a tendency to overestimate the impact of technology in the short-term (e.g. 1 year) while underestimating the long-term (e.g. 10 years) effect.
2.1.2. Artificial intelligence applications in healthcare
It is generally believed that AI tools will facilitate and enhance human work and not replace the work of physicians and other healthcare staff as such. AI is ready to support healthcare personnel with a variety of tasks from administrative workflow to clinical documentation and patient outreach as well as specialized support such as in image analysis, medical device automation, and patient monitoring.
There are different opinions on the most beneficial applications of AI for healthcare purposes. Forbes stated in 2018 that the most important areas would be administrative workflows, image analysis, robotic surgery, virtual assistants, and clinical decision support [8] . A 2018 report by Accenture mentioned the same areas and also included connected machines, dosage error reduction, and cybersecurity [9] . A 2019 report from McKinsey states important areas being connected and cognitive devices, targeted and personalized medicine, robotics-assisted surgery, and electroceuticals [10] .
In the next sections, some of the major applications of AI in healthcare will be discussed covering both the applications that are directly associated with healthcare and other applications in the healthcare value chain such as drug development and ambient assisted living (AAL).
2.2. Precision medicine
Precision medicine provides the possibility of tailoring healthcare interventions to individuals or groups of patients based on their disease profile, diagnostic or prognostic information, or their treatment response. The tailor-made treatment opportunity will take into consideration the genomic variations as well as contributing factors of medical treatment such as age, gender, geography, race, family history, immune profile, metabolic profile, microbiome, and environment vulnerability. The objective of precision medicine is to use individual biology rather than population biology at all stages of a patient’s medical journey. This means collecting data from individuals such as genetic information, physiological monitoring data, or EMR data and tailoring their treatment based on advanced models. Advantages of precision medicine include reduced healthcare costs, reduction in adverse drug response, and enhancing effectivity of drug action [11] . Innovation in precision medicine is expected to provide great benefits to patients and change the way health services are delivered and evaluated.
There are many types of precision medicine initiatives and overall, they can be divided into three types of clinical areas: complex algorithms, digital health applications, and “omics”-based tests.
Complex algorithms: Machine learning algorithms are used with large datasets such as genetic information, demographic data, or electronic health records to provide prediction of prognosis and optimal treatment strategy.
Digital health applications : Healthcare apps record and process data added by patients such as food intake, emotional state or activity, and health monitoring data from wearables, mobile sensors, and the likes. Some of these apps fall under precision medicine and use machine learning algorithms to find trends in the data and make better predictions and give personalized treatment advice.
Omics-based tests : Genetic information from a population pool is used with machine learning algorithms to find correlations and predict treatment responses for the individual patient. In addition to genetic information, other biomarkers such as protein expression, gut microbiome, and metabolic profile are also employed with machine learning to enable personalized treatments [12] .
Here, we explore selected therapeutic applications of AI including genetics-based solutions and drug discovery.
2.2.1. Genetics-based solutions
It is believed that within the next decade a large part of the global population will be offered full genome sequencing either at birth or in adult life. Such genome sequencing is estimated to take up 100–150 GB of data and will allow a great tool for precision medicine. Interfacing the genomic and phenotype information is still ongoing. The current clinical system would need a redesign to be able to use such genomics data and the benefits hereof [13] .
Deep Genomics, a Healthtech company, is looking at identifying patterns in the vast genetic dataset as well as EMRs, in order to link the two with regard to disease markers. This company uses these correlations to identify therapeutics targets, either existing therapeutic targets or new therapeutic candidates with the purpose of developing individualized genetic medicines. They use AI in every step of their drug discovery and development process including target discovery, lead optimization, toxicity assessment, and innovative trial design.
Many inherited diseases result in symptoms without a specific diagnosis and while interpreting whole genome data is still challenging due to the many genetic profiles. Precision medicine can allow methods to improve identification of genetic mutations based on full genome sequencing and the use of AI.
2.2.2. Drug discovery and development
Drug discovery and development is an immensely long, costly, and complex process that can often take more than 10 years from identification of molecular targets until a drug product is approved and marketed. Any failure during this process has a large financial impact, and in fact most drug candidates fail sometime during development and never make it onto the market. On top of that are the ever-increasing regulatory obstacles and the difficulties in continuously discovering drug molecules that are substantially better than what is currently marketed. This makes the drug innovation process both challenging and inefficient with a high price tag on any new drug products that make it onto the market [14] .
There has been a substantial increase in the amount of data available assessing drug compound activity and biomedical data in the past few years. This is due to the increasing automation and the introduction of new experimental techniques including hidden Markov model based text to speech synthesis and parallel synthesis. However, mining of the large-scale chemistry data is needed to efficiently classify potential drug compounds and machine learning techniques have shown great potential [15] . Methods such as support vector machines, neural networks, and random forest have all been used to develop models to aid drug discovery since the 1990s. More recently, DL has begun to be implemented due to the increased amount of data and the continuous improvements in computing power. There are various tasks in the drug discovery process where machine learning can be used to streamline the tasks. This includes drug compound property and activity prediction, de novo design of drug compounds, drug–receptor interactions, and drug reaction prediction [16] .
The drug molecules and the associated features used in the in silico models are transformed into vector format so they can be read by the learning systems. Generally, the data used here include molecular descriptors (e.g., physicochemical properties) and molecular fingerprints (molecular structure) as well as simplified molecular input line entry system (SMILES) strings and grids for convolutional neural networks (CNNs) [17] .
2.2.2.1. Drug property and activity prediction
The properties and activity on a drug molecule are important to know in order to assess its behavior in the human body. Machine learning-based techniques have been used to assess the biological activity, absorption, distribution, metabolism, and excretion (ADME) characteristics, and physicochemical properties of drug molecules ( Fig. 2.1 ). In recent years, several libraries of chemical and biological data including ChEMBL and PubChem have become available for storing information on millions of molecules for various disease targets. These libraries are machine-readable and are used to build machine learning models for drug discovery. For instance, CNNs have been used to generate molecular fingerprints from a large set of molecular graphs with information about each atom in the molecule. Neural fingerprints are then used to predict new characteristics based on a given molecule. In this way, molecular properties including octanol, solubility melting point, and biological activity can be evaluated as demonstrated by Coley et al. and others and be used to predict new features of the drug molecules [18] . They can then also be combined with a scoring function of the drug molecules to select for molecules with desirable biological activity and physiochemical properties. Currently, most new drugs discovered have a complex structure and/or undesirable properties including poor solubility, low stability, or poor absorption.

Machine learning opportunities within the small molecule drug discovery and development process.
Machine learning has also been implemented to assess the toxicity of molecules, for instance, using DeepTox, a DL-based model for evaluating the toxic effects of compounds based on a dataset containing many drug molecules [19] . Another platform called MoleculeNet is also used to translate two-dimensional molecular structures into novel features/descriptors, which can then be used in predicting toxicity of the given molecule. The MoleculeNet platform is built on data from various public databases and more than 700,000 compounds have already been tested for toxicity or other properties [20] .
2.2.2.2. De novo design through deep learning
Another interesting application of DL in drug discovery is the generation of new chemical structures through neural networks ( Fig. 2.2 ). Several DL-based techniques have been proposed for molecular de novo design. This also includes protein engineering involving the molecular design of proteins with specific binding or functions.

Illustration of the generative artificial intelligence concept for de novo design. Training data of molecular structures are used to emit new chemical entities by sampling.
Here, variational autoencoders and adversarial autoencoders are often used to design new molecules in an automated process by fitting the design model to large datasets of drug molecules. Autoencoders are a type of neural network for unsupervised learning and are also the tools used to, for instance, generate images of fictional human faces. The autoencoders are trained on many drug molecule structures and the latent variables are then used as the generative model. As an example, the program druGAN used adversarial autoencoders to generate new molecular fingerprints and drug designs incorporating features such as solubility and absorption based on predefined anticancer drug properties. These results suggest a substantial improvement in the efficiency in generating new drug designs with specific properties [21] . Blaschke et al. also applied adversarial autoencoders and Bayesian optimization to generate ligands specific to the dopamine type 2 receptor [22] . Merk et al. trained a recurrent neural network to capture a large number of bioactive compounds such as SMILES strings. This model was then fine-tuned to recognize retinoid X and peroxisome proliferator-activated receptor agonists. The identified compounds were synthesized and demonstrated potent receptor modulatory activity in in vitro assays [23] .
2.2.2.3. Drug–target interactions
The assessment of drug–target interactions is an important part of the drug design process. The binding pose and the binding affinity between the drug molecule and the target have an important impact on the chances of success based on the in silico prediction. Some of the more common approaches involve drug candidate identification via molecular docking, for prediction and preselection of interesting drug–target interactions.
Molecular docking is a molecular modeling approach used to study the binding and complex formation between two molecules. It can be used to find interactions between a drug compound and a target, for example a receptor, and predicts the conformation of the drug compound in the binding site of the target. The docking algorithm then ranks the interactions via scoring functions and estimates binding affinity. Popular commercial molecular docking tools include AutoDock, DOCK, Glide, and FlexX. These are rather simple and many data scientists are working on improving the prediction of drug–target interaction using various learning models [24] . CNNs are found useful as scoring functions for docking applications and have demonstrated efficient pose/affinity prediction for drug–target complexes and assessment of activity/inactivity. For instance, Wallach and Dzamba build AtomNet, a deep CNN to predict the bioactivity of small molecule drugs for drug discovery applications. The authors showed that AtomNet outperforms conventional docking models in relation to accuracy with an AUC (area under the curve) of 0.9 or more for 58% of the targets [25] .
Current trends within AI applications for drug discovery and development point toward more and more models using DL approaches. Compared with more conventional machine learning approaches, DL models take a long time to train because of the large datasets and the often large number of parameters needed. This can be a major disadvantage when data is not readily available. There is therefore ongoing work on reducing the amount of data required as training sets for DL so it can learn with only small amounts of available data. This is similar to the learning process that takes place in the human brain and would be beneficial in applications where data collection is resource intensive and large datasets are not readily available, as is often the case with medicinal chemistry and novel drug targets. There are several novel methods being investigated, for instance, using a one-shot learning approach or a long short-term memory approach and also using memory augmented neural networks such as the differentiable neural computer [17] .
2.3. Artificial intelligence and medical visualization
Interpretation of data that appears in the form of either an image or a video can be a challenging task. Experts in the field have to train for many years to attain the ability to discern medical phenomena and on top of that have to actively learn new content as more research and information presents itself. However, the demand is ever increasing and there is a significant shortage of experts in the field. There is therefore a need for a fresh approach and AI promises to be the tool to be used to fill this demand gap.
2.3.1. Machine vision for diagnosis and surgery
Computer vision involves the interpretation of images and videos by machines at or above human-level capabilities including object and scene recognition. Areas where computer vision is making an important impact include image-based diagnosis and image-guided surgery.
2.3.1.1. Computer vision for diagnosis and surgery
Computer vision has mainly been based on statistical signal processing but is now shifting more toward application of artificial neural networks as the choice for learning method. Here, DL is used to engineer computer vision algorithms for classifying images of lesions in skin and other tissues. Video data is estimated to contain 25 times the amount of data from high-resolution diagnostic images such as CT and could thus provide a higher data value based on resolution over time. Video analysis is still premature but has great potential for clinical decision support. As an example, a video analysis of a laparoscopic procedure in real time has resulted in 92.8% accuracy in identification of all the steps of the procedure and surprisingly, the detection of missing or unexpected steps [26] .
A notable application of AI and computer vision within surgery technology is to augment certain features and skills within surgery such as suturing and knot-tying. The smart tissue autonomous robot (STAR) from the Johns Hopkins University has demonstrated that it can outperform human surgeons in some surgical procedures such as bowel anastomosis in animals. A fully autonomous robotic surgeon remains a concept for the not so near future but augmenting different aspects of surgery using AI is of interest to researchers. An example of this is a group at the Institute of Information Technology at the Alpen-Adria Universität Klagenfurt that uses surgery videos as training material in order to identify a specific intervention made by the surgeon. For example, when an act of dissection or cutting is performed on the patient’s tissues or organs, the algorithm recognizes the likelihood of the intervention as well as the specific region in the body [27] . Such algorithms are naturally based on the training on many videos and could be proven very useful for complicated surgical procedures or for situations where an inexperienced surgeon is required to perform an emergency surgery. It is important that surgeons are actively engaged in the development of such tools ensuring clinical relevance and quality and facilitating the translation from the lab to the clinical sector.
2.3.2. Deep learning and medical image recognition
The word “Deep” refers to the multilayered nature of machine learning and among all DL techniques, the most promising in the field of image recognition has been the CNNs. Yann LeCun, a prominent French computer scientist introduced the theoretical background to this system by creating LeNET in the 1980s, an automated handwriting recognition algorithm designed to read cheques for financial systems. Since then, these networks have shown significant promise in the field of pattern recognition.
Similar to radiologists that during the medical training period have to learn by constantly correlating and relating their interpretations of radiological images to the ground truth, CNNs are influenced by the human visual cortex, where image recognition is initiated by the identification of the many features of the image. Furthermore, CNNs require a significant amount of training data that comes in the form of medical images along with labels for what the image is supposed to be. At each hidden layer of training, CNNs can adjust the applied weights and filters (characteristics of regions in an image) to improve the performance on the given training data.
Briefly and very simply ( Fig. 2.3 ), the act of convolving an image with various weights and creating a stack of filtered images is referred to as a convolutional layer, where an image essentially becomes a stack of filtered images. Pooling is then applied to all these filtered images, where the original stack of images becomes a smaller representation of themselves and all negative values are removed by a rectified linear unit (ReLU). All these operations are then stacked on top of one another to create layers, sometimes referred to as Deep stacking. This process can be repeated multiple times and each time the image gets filtered more and relatively smaller. The last layer is referred to as a fully connected layer where every value assigned to all layers will contribute to what the results will be. If the system produces an error in this final answer, the gradient descent can be applied by adjusting the values up and down to see how the error changes relative to the right answer of interest. This can be achieved by an algorithm called back propagation that signifies “learning from mistakes.” After learning a new capability from the existing data, this can be applied to new images and the system can classify the images in the right category (Inference), similar to how a radiologist operates [28] .

The various stages of convolutional neural networks at work.
2.3.3. Augmented reality and virtual reality in the healthcare space
Augmented and virtual reality (AR and VR) can be incorporated at every stage of a healthcare system. These systems can be implemented at the early stages of education for medical students, to those training for a specific specialty and experienced surgeons. On the other hand, these technologies can be beneficial and have some negative consequences for patients.
In this section, we will attempt to cover each stage and finally comment on the usefulness of these technologies.
2.3.3.1. Education and exploration
Humans are visual beings and play is one of the most important aspects of our lives. As children the most important way for us to learn was to play. Interaction with the surroundings allowed us to gain further understanding of the world and provided us with the much-needed experience. The current educational system is limited and for interactive disciplines such as medicine this can be a hindrance. Medicine can be visualized as an art form and future clinicians are the artist. These individuals require certain skills to fulfill the need for an ever-evolving profession. Early in medical school, various concepts are taught to students without them ever experiencing these concepts in real life. So game-like technologies such as VR and AR could enhance and enrich the learning experience for future medical and health-related disciplines [29] . Medical students could be provided with and taught novel and complicated surgical procedures, or learn about anatomy through AR without ever needing to interact or involve real patients at an early stage or without ever needing to perform an autopsy on a real corpse. These students will of course be interacting with real patients in their future careers, but the goal would be to initiate the training at an earlier stage and lowering the cost of training at a later stage.
For today’s training specialists, the same concept can be applied. Of course, human interaction should be encouraged in the medical field but these are not always necessary and available when an individual is undergoing a certain training regimen. The use of other physical and digital cues such as haptic feedback and photorealistic images and videos can provide a real simulation whereby learning can flourish and the consequences and cost of training are not drastic ( Fig. 2.4 ).

Virtual reality can help current and future surgeons enhance their surgical abilities prior to an actual operation. (Image obtained from a video still, OSSOR VR).
In a recent study [30] , two groups of surgical trainees were subjected to different methods for Mastoidectomy, where one group ( n =18) would go through the standard training path and the other would train on a freeware VR simulator [the visible ear simulator (VES)]. At the end of the training, a significant improvement in surgical dissection was observed for those who trained with VR. For real-life and precise execution, AR would be more advantageous in healthcare settings. By wearing lightweight headsets (e.g., Microsoft HoloLens or Google Glass) that project relevant images or video onto the regions of interest, the user can focus on the task without ever being distracted by moving their visual fields away from the region of interest.
2.3.3.2. Patient experience
Humans interact with their surroundings with audiovisual cues and utilize their limbs to engage and move within this world. This seemingly ordinary ability can be extremely beneficial for those who are experiencing debilitating conditions that limit movement or for individuals who are experiencing pain and discomfort either from a chronic illness or as a side effect of a treatment. A recent study, looking at the effect of immersive VR for patients who had suffered from chronic stroke patients, found this technology to be contributing positively to the state of patients. During the VR experience, the patients are asked to grab a virtual ball and throw it back into the virtual space [31] . For these patients, this immersive experience could act as a personal rehabilitation physiotherapist who engages their upper limb movement multiple times a day, allowing for possible neuroplasticity and a gradual return of normal motor function to these regions.
For others, these immersive technologies could help cope with the pain and the discomfort of their cancer or mental health condition. A study has shown that late-stage adult cancer patients can use this technology with minimum physical discomfort and in return benefit from an enhanced relaxed state, entertainment, and a much-needed distraction [32] . These immersive worlds provide a form of escapism with their artificial characters and environments, allowing the individual to interact and explore the surrounding while receiving audiovisual feedback from the environment, much like all the activities of daily living.
2.4. Intelligent personal health records
Personal health records have historically been physician-oriented and often have lacked patient-related functionalities. However, in order to promote self-management and improve the outcomes for patients, a patient-centric personal health record should be implemented. The goal is to allow ample freedom for patients to manage their conditions, while freeing up time for the clinicians to perform more crucial and urgent tasks.
2.4.1. Health monitoring and wearables
For millennia individuals relied on physicians to inform them about their own bodies and to some extent, this practice is still applied today. However, the relatively new field of wearables is changing this. Wearable health devices (WHDs) are an upcoming technology that allow for constant measurement of certain vital signs under various conditions. The key to their early adoption and success is their application flexibility—the users are now able to track their activity while running, meditating, or when underwater. The goal is to provide individuals with a sense of power over their own health by allowing them to analyze the data and manage their own health. Simply, WHDs create individual empowerment ( Fig. 2.5 ).

Health outcome of a patient depends on a simple yet interconnected set of criteria that are predominantly behavior dependent.
At first look, a wearable device might look like an ordinary band or watch; however, these devices bridge the gap between multiple scientific disciplines such as biomedical engineering, materials science, electronics, computer programming, and data science, among many others [33] . It would not be an exaggeration to refer to them as ever-present digital health coaches, as increasingly it is encouraged to wear them at all times in order to get the most out of your data. Garmin wearables are a good example of this, with a focus on being active, they cover a vast variety of sports and provide a substantial amount of data on their Garmin connect application where users can analyze and observe their daily activities. These are increasingly accompanied by implementation of gamification.
Gamification refers to utilization of game design elements for nongame-related applications. These elements are used to motivate and drive users to reach their goals [34] . On wearable platforms, data gathered from daily activities can serve as competition between different users on the platform. Say, that your average weekly steps are around 50,000 steps. Here, based on specific algorithms, the platform places you on a leaderboard against individuals whose average weekly steps are similar to yours or higher, with the highest ranking member exceeding your current average weekly steps. As a result of this gamified scenario, the user can push themselves to increase their daily activities in order to do better on the leaderboard and potentially lead a healthier life. While the gamification aspect of wearables and their application could bring benefits, evidence of efficacy is scarce and varies widely with some claiming that the practice might bring more harm than good.
Remote monitoring and picking up on early signs of disease could be immensely beneficial for those who suffer from chronic conditions and the elderly. Here, by wearing a smart device or manual data entry for a prolonged period, individuals will be able to communicate to their healthcare workers without the need of disrupting their daily lives [35] . This is a great example of algorithms collaborating with healthcare professionals to produce an outcome that is beneficial for patients.
2.4.2. Natural language processing
Natural language processing (NLP) relates to the interaction between computers and humans using natural language and often emphasizes on the computer’s ability to understand human language. NLP is crucial for many applications of big data analysis within healthcare, particularly for EMRs and translation of narratives provided by clinicians. It is typically used in operations such as extraction of information, conversion of unstructured data into structured data, and categorization of data and documents.
NLP makes use of various classifications to infer meaning from unstructured textual data and allows clinicians to work more freely using language in a “natural way” as opposed to fitting sequences of text into input options to serve the computer. NLP is being used to analyze data from EMRs and gather large-scale information on the late-stage complications of a certain medical condition [26] .
There are many areas in healthcare in which NLP can provide substantial benefits. Some of the more immediate applications include [36]
- 1. Efficient billing: extracting information from physician notes and assigning medical codes for the billing process.
- 2. Authorization approval: Using information from physician notes to prevent delays and administrative errors.
- 3. Clinical decision support: Facilitate decision-making for members of healthcare team upon need (for instance, predicting patient prognosis and outcomes).
- 4. Medical policy assessment: compiling clinical guidance and formulation appropriate guidelines for care.
One application of NLP is disease classification based on medical notes and standardized codes using International Statistical Classification of Diseases and Related Health Problems (ICD). ICD is managed and published by the WHO and contains codes for diseases and symptoms as well as various findings, circumstances, and causes of disease. Here is an illustrative example of how an NLP algorithm can be used to extract and identify the ICD code from a clinical guidelines description. Unstructured text is organized into structured data by parsing for relevant clauses followed by classification of ICD-10 codes based on frequency of occurrence. The NLP algorithm is run at various thresholds to improve classification accuracy and the data is aggregated for the final output ( Fig. 2.6 ).

Example of ICD-10 mapping from a clinical guidelines’ description [36] .
2.4.3. Integration of personal records
Since the introduction of EMRs, there have been large databases of information on each patient, which collectively can be used to identify healthcare trends within different disease areas. The EMR databases contain the history of hospital encounters, records of diagnoses and interventions, lab test, medical images, and clinical narratives. All these datasets can be used to build predictive models that can help clinicians with diagnostics and various treatment decision support. As AI tools mature it will be possible to extract all kinds of information such as related disease effects and correlations between historical and future medical events [37] . The only data often missing is data from in between interventions and between hospital visits when the patient is well or may not be showing symptoms. Such data could help to construct an end-to-end model of both “health” and “disease” for studying long-term effects and further disease classifications.
Although the applications of AI for EMRs are still quite limited, the potential for using the large databases to detect new trends and predict health outcomes is enormous. Current applications include data extraction from text narratives, predictive algorithms based on data from medical tests, and clinical decision support based on personal medical history. There is also great potential for AI to enable integration of EMR data with various health applications. Current AI applications within healthcare are often standalone applications, these are often used for diagnostics using medical imaging and for disease prediction using remote patient monitoring [38] . However, integrating such standalone applications with EMR data could provide even greater value by adding personal medical data and history as well as a large statistical reference library to make classifications and predictions more accurate and powerful. EMR providers such as Cerner, Epic, and Athena are beginning to add AI functionality such as NLP in their systems making it easier to access and extract data held in their libraries [39] . This could facilitate the integration of, for instance, Telehealth and remote monitoring applications with EMR data and the data integration transfer could even go both ways including the addition of remote monitoring data in the EMR systems.
There are many EMR providers and systems globally. These use various operating systems and approaches with more than a thousand EMR providers operating in the United States alone. Integration of EMR records on their own poses a great challenge and interoperability of these systems is important to obtain the best value from the data. There are various international efforts in gathering EMR data across countries including Observational Health Data Science and Informatics (OHDSI), who have consolidated 1.26 billion patient records from 17 different countries [40] . Various AI methods have been used to extract, classify, and correlate data from EMRs but most generally make use of NLP, DL, and neural networks.
DeepCare is an example of an AI-based platform for end-to-end processing of EMR data. It uses a deep dynamic memory neural network to read and store experiences and in memory cells. The long short-term memory of the system models the illness trajectory and healthcare processes of users via a time-stamped sequence of events and in this way allows capturing long-term dependencies [41] . Using the stored data, the framework of DeepCare can model disease progression, support intervention recommendation, and provide disease prognosis based on EMR databases. Studying data from a cohort of diabetic and mental health patients it was demonstrated that DeepCare could predict the progression of disease, optimal interventions, and assessing the likelihood for readmission [37] .
2.5. Robotics and artificial intelligence-powered devices
There are numerous areas in healthcare where robots are being used to replace human workforce, augment human abilities, and assist human healthcare professionals. These include robots used for surgical procedures such as laparoscopic operations, robotic assistants for rehabilitation and patient assistance, robots that are integrated into implants and prosthetic, and robots used to assist physicians and other healthcare staff with their tasks. Some of these devices are being developed by several companies especially for interacting with patients and improving the connection between humans and machines from a care perspective. Most of the robots currently under development have some level of AI technology incorporated for better performance with regard to classifications, language recognition, image processing, and more.
2.5.1. Minimally invasive surgery
Although many advances have been seen in the area surrounding surgery measured by the outcomes of surgical procedures, the main practice of surgery still remains a relatively low-tech procedure for the most part using hand tools and instruments for “cutting and sewing.” Conventional surgery relies greatly on sensing by the surgeon, where touching allows them to distinguish between tissues and organs and often requires open surgery. There is an ongoing transformation within surgical technology and focus has especially been placed in reducing the invasiveness of surgical procedure by minimizing incisions, reducing open surgeries, and using flexible tools and cameras to assist the surgery [42] . Such minimally invasive surgery is seen as the way forward, but it is still in an early phase with many improvements to be made to make it “less of a big deal” for patients and reduce time and cost. Minimal invasive surgery requires different motor skills compared with conventional surgery due to the lower tactile feedback when relying more on tools and less on direct touching. Sensors that provide the surgeon with finer tactile stimuli are under development and make use of tactile data processing to translate the sensor input into data or stimuli that can be perceived by the surgeon. Such tactile data processing typically makes use of AI, more specifically artificial neural networks to enhance the function of this signal translation and the interpretation of the tactile information [43] . Artificial tactile sensing offers several advantages compared with physical touching including a larger reference library to compare sensation and standardization among surgeons with respect to quantitative features, continuous improvement, and level of training.
An example where artificial tactile sensing has been used includes screening of breast cancer, as a replacement for clinical breast examination to complement medical imaging techniques such as x-ray mammography and MRI. Here, the artificial tactile sensing system was built on data from reconstruction of mechanical tissue measurements using a pressure sensor as reference data. During training of the neural network, the weight of the input data adjusts according to the desired output [44] . The tactile sensory system can detect mass calcifications inside the breast tissue based on palpation of different points of the tissue and comparing with different reference data, and subsequently determine whether there are any significant abnormalities in the breast tissue. Artificial tactile sensing has also been used for other applications including assessment of liver, brain, and submucosal tumors [45] .
2.5.2. Neuroprosthetics
Our species has always longed for an eternal life, in the ancient Vedic tradition there exists a medicinal drink that provides “immortality” for those who drink it. The Rig Veda, which was written some 5000 years ago, comments: “We drank soma, we became immortal, we came to the light, we found gods.” This is similar in ancient Persian culture, where a similar legendary drink is called Hoama in the Zoroastrain sacred book, Avesta [46] , [47] . This longing for “enhancement” and “augmentation” has always been with us, and in the 21st century we are gradually beginning to move towards making some past myths into reality. In this section, we will cover some recent innovations that can utilize AI to assist and allow humans to function better. Most research in this area is to assist individuals with preexisting conditions and have not been implemented in normal functioning humans for the sake of human augmentation; however, this can perhaps change in the coming years.
Neuroprosthetics are defined as devices that help or augment the subject’s own nervous system, in both forms of input and output. This augmentation or stimulation often occurs in the form of an electrical stimulation to overcome the neurological deficiencies that patients experience.
These debilitating conditions can impair hearing, vision, cognitive, sensory or motor skills, and can lead to comorbidities. Indeed, movement disorders such as multiple sclerosis or Parkinson’s are progressive conditions that can lead to a painful and gradual decline in the above skills while the patient is always conscious of every change. The recent advances in brain machine interfaces (BMIs) have shown that a system can be employed where the subjects’ intended and voluntary goal-directed wishes (electroencephalogram, EEG) can be stored and learned when a user “trains” an intelligent controller (an AI). This period of training allows for identification of errors in certain tasks that the user deems incorrect, say that on a computer screen, a square is directed to go left and instead it goes to right and also in a situation where the BMI is connected to a fixed robotic hand, the subject directs the device to go up and the signals are interpreted as a down movement. Correct actions are stored, and the error-related brain signals are registered by the AI to correct for future actions. Because of this “reinforcement learning,” the system can potentially store single to several control “policies,” which allow for patient personalization [48] . This is rather similar to the goals of the company Neuralink which aims to bring the fields of material science, robotics, electronics, and neuroscience together to try and solve multifaceted health problems [49] .
While in its infancy and very exploratory, this field will be immensely helpful for patients with neurodegenerative diseases who will increasingly rely on neuroprostheses throughout their lives.
2.6. Ambient assisted living
With the aging society, more and more people live through old age with chronic disorders and mostly manage to live independently up to an old age. Data indicates that half of people above the age of 65 years have a disability of some sort, which constitutes over 35 million people in the United States alone. Most people want to preserve their autonomy, even at an old age, and maintain control over their lives and decisions [50] . Assistive technologies increase the self-dependencies of patients, encouraging user participation in Information and Communication Technology (ICT) tools to provide remote care services type assistance and provide information to the healthcare professionals. Assistive technologies are experiencing rapid growth, especially among people aged 65–74 years [51] . Governments, industries, and various organizations are promoting the concept of AAL, which enables people to live independently in their home environment. AAL has multiple objectives including promoting a healthy lifestyle for individuals at risk, increasing the autonomy and mobility of elderly individuals, and enhancing security, support, and productivity so people can live in their preferred environment and ultimately improve their quality of life. AAL applications typically collect data through sensors and cameras and apply various artificially intelligent tools for developing an intelligent system [52] . One way of implementing AAL is using smart homes or assistive robots.
2.6.1. Smart home
A smart home is a normal residential home, which has been augmented using different sensors and monitoring tools to make it “smart” and facilitate the lives of the residents in their living space. Other popular applications of AAL that can be a part of a smart home or used as an individual application include remote monitoring, reminders, alarm generation, behavior analysis, and robotic assistance.
Smart homes can be useful for people with dementia and several studies have investigated smart home applications to facilitate the lives of dementia patients. Low-cost sensors in an Internet of Things (IoT) architecture can be a useful way of detecting abnormal behavior in the home. For instance, sensors are placed in different areas of the house including the bedroom, kitchen, and bathroom to ensure safety. A sensor can be placed on the oven and detect the use of the cooker, so the patient is reminded if it was not switched off after use. A rain sensor can be placed by the window to alert the patient if the window was left open during rain. A bath sensor and a lamp sensor can be used in the bathroom to ensure that they are not left on [53] .
The sensors can transmit information to a nearby computing device that can process the data or upload them to the cloud for further processing using various machine learning algorithms, and if necessary, alert relatives or healthcare professionals ( Fig. 2.7 ). By daily collection of patient data, activities of daily living are defined over time and abnormalities can be detected as a deviation from the routine. Machine learning algorithms used in smart home applications include probabilistic and discriminative methods such as Naive Bayes classifier and Hidden Markov Model, support vector machine, and artificial neural networks [54] .

Process diagram of a typical smart home or smart assistant setup.
In one example, Markov Logic Network was used for activity recognition design to model both simple and composite activities and decide on appropriate alerts to process patient abnormality. The Markov Logic Network used handles both uncertainty modeling and domain knowledge modeling within a single framework, thus modeling the factors that influence patient abnormality [55] . Uncertainty modeling is important for monitoring patients with dementia as activities conducted by the patient are typically incomplete in nature. Domain knowledge related to the patient’s lifestyle is also important and combined with their medical history it can enhance the probability of activity recognition and facilitate decision-making. This machine learning-based activity recognition framework detected abnormality together with contextual factors such as object, space, time, and duration for decision support on suitable action to keep the patient safe in the given environment. Alerts of different importance are typically used for such decision support and can, for instance, include a low-level alarm when the patient has forgotten to complete a routine activity such as switching off the lights or closing the window and a high-level alarm if the patient has fallen and requires intervention by a caretaker. One of the main aims of such activity monitoring approaches, as well as other monitoring tools, is to support healthcare practitioners in identifying symptoms of cognitive functioning or providing diagnosis and prognosis in a quantitative and objective manner using a smart home system [56] . There are various other assistive technology devices for people with dementia including motion detectors, electronic medication dispensers, and robotic devices for tracking.
2.6.2. Assistive robots
Assistive robots are used to support the physical limitations of the elderly and dysfunctional people and help them by assisting in daily activities and acting as an extra pair of hands or eyes. Such assistive robots can help in various activities such as mobility, housekeeping, medication management, eating, grooming, bathing, and various social communications. An assistive robot named RIBA with human-type arms was designed to help patients with lifting and moving heavy things. It has been demonstrated that the robot is able to carry the patient from the bed to a wheelchair and vice versa. Instructions can be provided to RIBA either by using tactile sensors using a method known as tactile guidance to teach by showing [57] .
The MARIO project (Managing active and healthy Aging with use of caring Service robots) is another assistive robot which has attracted a lot of attention. The project aims to address the problems of loneliness, isolation, and dementia, which are commonly observed with elderly people. This is done by performing multifaceted interventions delivered by service robots. The MARIO Kompaï companion robot was developed with the objective to provide real feelings and emotions to improve acceptance by dementia patients, to support physicians and caretakers in performing dementia assessment tests, and promote interactions with the end users. The Kompaï robot used for the MARIO project was developed by Robosoft and is a robot containing a camera, a Kinect motion sensor, and two LiDAR remote sensing systems for navigation and object identification [58] . It further includes a speech recognition system or other controller and interface technologies, with the intention to support and manage a wide range of robotic applications in a single robotic platform similar to apps for smartphones. The robotic apps include those focused on cognitive stimulation, social interaction, as well as general health assessment. Many of these apps use AI-powered tools to process the data collected from the robots in order to perform tasks such as facial recognition, object identification, language processing, and various diagnostic support [59] .
2.6.3. Cognitive assistants
Many elderly people experience a decline in their cognitive abilities and have difficulties in problem-solving tasks as well as maintaining attention and accessing their memory. Cognitive stimulation is a common rehabilitation approach after brain injuries from stroke, multiple sclerosis or trauma, and various mild cognitive impairments. Cognitive stimulation has been demonstrated to decrease cognitive impairment and can be trained using assistive robots.
Virtrael is one of such cognitive stimulation platforms and serves to assess, stimulate, and train various cognitive skills that experience a decline in the patient. The Virtrael program is based on visual memory training and the project is carried out by three different key functionalities: configuration, communication, and games. The configuration mode allows an administrator to match the patient with a therapist and the therapist to configure the program for the patient. The communication tool allows communication between the patient and the therapist and between patients., The games are intended to train cognitive skills of the patient including memory, attention, and planning ( Fig. 2.8 ) [60] .

Example of games used for training cognitive skills of patients [60] .
2.6.4. Social and emotional stimulation
One of the first applications of assistive robots and a commonly investigated technology is companion robots for social and emotional stimulation. Such robots assist elderly patients with their stress or depression by connecting emotionally with the patient with enhanced social interaction and assistance with various daily tasks. The robots vary from being pet-like robots to more peer-like and they are all interactive and provide psychological and social effects. The robotic pet PARO, a baby seal robot, is the most widely used robotic pet and carries various sensors to sense touch, sounds, and visual objects [61] . Another robot is the Mario Kampäi mentioned earlier, which focuses on assisting elderly patients with dementia, loneliness, and isolation. Yet, another companion robot Buddy, by Blue Frog Robotics, assists elderly patients by helping with daily activities such as reminders about medication and appointments, as well as using motion sensors to detect falls and physical inactivity. Altogether, studies investigating cognitive stimulation seem to demonstrate a decrease in the rate of cognitive decline and progression of dementia.
2.7. The artificial intelligence can see you now
AI is increasingly becoming an integral part of all our lives. From smartphones to cars and more importantly our healthcare. This technology will continue to push boundaries and certain norms that have been dormant and accepted as the status quo for hundreds of years, will now be directly challenged and significantly augmented.
2.7.1. Artificial intelligence in the near and the remote
We believe that AI has an important role to play in the healthcare offerings of the future. In the form of machine learning, it is the primary capability behind the development of precision medicine, widely agreed to be a sorely needed advance in care. Although early efforts at providing diagnosis and treatment recommendations have proven challenging, we expect that AI will ultimately master that domain as well. Given the rapid advances in AI for imaging analysis, it seems likely that most radiology and pathology images will be examined at some point by a machine. Speech and text recognition are already employed for tasks like patient communication and capture of clinical notes, and their usage will increase.
The greatest challenge to AI in these healthcare domains is not whether the technologies will be capable enough to be useful, but rather ensuring their adoption in daily clinical practice. For widespread adoption to take place, AI systems must be approved by regulators, integrated with EHR systems, standardized to a sufficient degree that similar products work in a similar fashion, taught to clinicians, paid for by public or private payer organizations, and updated over time in the field. These challenges will ultimately be overcome, but they will take much longer to do so than it will take for the technologies themselves to mature. As a result, we expect to see limited use of AI in clinical practice within 5 years and more extensive use within 10 years.
It also seems increasingly clear that AI systems will not replace human clinicians on a large scale, but rather will augment their efforts to care for patients. Over time, human clinicians may move toward tasks and job designs that draw on uniquely human skills like empathy, persuasion, and big-picture integration. Perhaps the only healthcare providers who will risk their careers over time may be those who refuse to work alongside AI.
2.7.2. Success factors for artificial intelligence in healthcare
A review by Becker [62] suggests that AI used in healthcare can serve clinicians, patients, and other healthcare workers in four different ways. Here, we will use these suggestions as inspirations and will expand on their contribution toward a successful implementation of AI in healthcare: ( Fig. 2.9 )
- 1. Assessment of disease onset and treatment success.
- 2. Management or alleviation of complications.
- 3. Patient-care assistance during a treatment or procedure.
- 4. Research aimed at discovery or treatment of disease.

The likely success factors depend largely on the satisfaction of the end users and the results that the AI-based systems produce.
2.7.2.1. Assessment of condition
Prediction and assessment of a condition is something that individuals will demand to have more control over in the coming years. This increase in demand is partly due to a technology reliable population that has grown to learn that technological innovation will be able to assist them in leading healthy lives. Of course, while not all answers lie in this arena, it is an extremely promising field.
Mood and mental health-related conditions are immensely important topic in today’s world and for good reason. According to the WHO, one in four people around the world experiences such conditions and as a result can accelerate their path toward ill-health and comorbidities. Recently, machine learning algorithms have been developed to detect words and intonations of an individual’s speech that may indicate a mood disorder. Using neural networks, an MIT-based lab has conducted research onto the detection of early signs of depression using speech. According to the researchers, the “model sees sequences of words/speaking style” and decides whether these emerging patterns are likely to be seen in individuals with and without depression [63] . The technique employed by the researchers is often referred to as a sequence modeling, where model sequences of audio and text from patients with and without depression are fed to the system and as these accumulate, various text patterns could be paired with audio signals. For example, words such as “low”, “blue,” and “sad” can be paired with more monotone and flat audio signals. Additionally, the speed and the length of pauses can play a major role in detection of individuals experiencing depression. An example of this can be seen in Fig. 2.10 where within a period of 60 seconds and based on the tone and words used, it is possible to measure an estimated emotion.

Early detection of certain mood conditions can be predicted by analyzing the trend, tone of voice, and speaking style of individuals.
2.7.2.2. Managing complications
The general feeling of being unwell and its various complications that accompany mild illnesses are usually well tolerated by patients. However, for certain conditions, it is categorically important to manage these symptoms as to prevent further development and ultimately alleviate more complex symptoms. A good example for this can be seen in the field of infectious diseases. In a study published in the journal of trauma and acute care surgery, researchers think that by understanding the microbiological niches (biomarkers) of trauma patients, we could hold the key to future wound infections and therefore can allow healthcare workers to take the necessary arrangements to prevent the worst outcome [64] . Machine learning techniques can also contribute toward the prediction of serious complications such as neuropathy that could arise for those suffering from type 2 diabetes or early cardiovascular irregularities. Furthermore, the development of models that can help clinicians detect postoperative complications such as infections will contribute toward a more efficient system [65] .
2.7.2.3. Patient-care assistance
Patient-care assistance technologies can improve the workflow for clinicians and contribute toward patient’s autonomy and well-being. If each patient is treated as an independent system, then based on the variety of designated data available, a bespoke approach can be implemented. This is of utmost importance for the elderly and the vulnerable in our societies. An example of this could be that of virtual health assistants that remind individuals to take their required medications at a certain time or recommend various exercise habits for an optimal outcome. The field of Affective Computing can contribute significantly in this arena. Affective computing refers to a discipline that allows the machine to process, interpret, simulate, and analyze human behavior and emotions. Here, patients will be able to interact with the device in a remote manner and access their biometric data, all the while feeling that they are interacting with a caring and empathetic system that truly wants the best outcome for them. This setting can be applied both at home and in a hospital setting to relieve work pressure from healthcare workers and improve service.
2.7.2.4. Medical research
AI can accelerate the diagnosis process and medical research. In recent years, an increasing number of partnerships have formed between biotech, MedTech, and pharmaceutical companies to accelerate the discovery of new drugs. These partnerships are not all based on curiosity-driven research but often out of necessity and need of society. In a world where certain expertise is rare, research costs high and effective treatments for certain conditions are yet to be devised, collaboration between various disciplines is key. A good example of this collaboration is seen in a recent breakthrough for antibiotic discovery, where the researchers devised/trained a neural network that actively “learned” the properties of a vast number of molecules in order to identify those that inhibit the growth of E. coli , a Gram negative bacterial species that is notoriously hard to kill [66] . Another example is the recent research carried out regarding the pandemic of COVID-19 all around the world. Predictive Oncology, a precision medicine company has announced that they are launching an AI platform to accelerate the production of new diagnostics and vaccines, by using more than 12,000 computer simulations per machine. This is combined with other efforts to employ DL to find molecules that can interact with the main proteases (M pro or 3CL pro ) of the virus, resulting in the disruption of the replication machinery of the virus inside the host [67] , [68] .
2.7.3. The digital primary physician
As you walk into the primary care physician’s room, you are greeted by the doctor. There is an initial eye to eye contact, then an exchange of pleasantries follows. She further asks you about your health and how she can be of help. You, the patient, have multiple medical problems: previous presence of sciatica, snapping hip syndrome, high cholesterol, an above-average blood pressure, and chronic sinusitis. However, because of the limited time that you have with the doctor, priorities matter [69] . You categorize your own conditions and tend to focus on the most important to you, the chronic sinusitis. The doctor asks you multiple questions about the condition and as you are explaining your symptoms, she types it all in your online record, does a quick examination, writes a prescription, and says to come back in 6 weeks for further examination. For your other conditions, you probably need to book a separate appointment unless you live in a country that designates more than 20 minutes per patient.
The above scenario is the normal routine in most countries. However, despite the helpfulness of the physician, it is not an ideal system and it is likely that if you were in the position of the above patient, you will walk away dissatisfied with the care received. The frustration with such systems has led to an immense pressure on the health workers and needs to be addressed. Today, there are numerous health-related applications that utilize and combine the power of AI with that of a remote physician to answer some of the simple questions that might not warrant a physical visit to the doctors.
2.7.3.1. Artificial intelligence prequalification (triage)
Prior to having access to an actual doctor, trained AI bots can qualify whether certain symptoms warrant an actual conversation with a physician. Many questions are asked of the patient and based on each response; the software encourages the user to take specific actions. These questions and answers are often vigorously reviewed by medical professionals at each stage to account for accuracy. In important cases, a general response of “You should see a doctor” is given and the patient is directed to book an appointment with a primary care physician.
2.7.3.2. Remote digital visits
The unique selling point for these recent innovations is that they allow remote video conversations between the patient and the physician. Normally, the patient books an appointment for a specific time, often during the same day. This provides them with ample time to provide as much information as possible for the physician responsible to review and carefully analyze the evidence before talking to the patient. The information can be in the form of images, text, video, and audio. This is extremely encouraging and creative as many people around the world lack the time and resources to visit a physician and allows remote work for the physician.
2.7.3.3. The future of primary care
In a recent study, when asked about the future of AI on primary care, while acknowledging its potential benefits, most practitioners were extremely skeptical regarding it playing a significant role in the future of the profession. One main pain point refers to the lack of empathy and the ethical dilemma that can occur between AI and patients [70] . While this might be true for today, it is naive to assume that this form of technology will remain dormant and will not progress any further. Humanity prefers streamlining and creative solutions that are effective and take less out of our daily lives. Combine this with the ever-increasing breakthroughs in the field of smart healthcare materials [71] and AI, one could envisage patients managing most of their own conditions at home and when necessary get in touch with a relevant healthcare worker who will refer them to more specialized physicians who could tend to their needs. It is also very important to note that at the time of an epidemic, an outbreak, natural or manmade disaster, or simply when the patient is away from their usual dwelling, a technology that allows humans to remotely interact and solve problems will have to become a necessity. At the time of writing (Early 2020), the threat of a SARS-COV-2 epidemic looms over many countries and is expanding at an unprecedented rate. World experts speculate that the infection rate is high and has the potential to remain within a population and cause many fatalities in many months to come. It is therefore essential to promote remote healthcare facilities/technologies and to have permanent solutions in place to save lives in order to reduce any unnecessary burden or risk on both healthcare workers and patients alike.

IMAGES
COMMENTS
Artificial intelligence (AI) is a powerful and disruptive area of computer science, with the potential to fundamentally transform the practice of medicine and the delivery of healthcare. In this review article, we outline recent breakthroughs in the application of AI in healthcare, describe a roadmap to building effective, reliable and safe AI ...
1. Introduction. Artificial intelligence (AI) is defined as the intelligence of machines, as opposed to the intelligence of humans or other living species [1], [2].AI can also be defined as the study of "intelligent agents"—that is, any agent or device that can perceive and understand its surroundings and accordingly take appropriate action to maximize its chances of achieving its ...
This paper explores artificial intelligence's evolving role in healthcare, focusing on its application in hospitals and clinics. In consideration of the extensive scope of this study, we employed a meticulous approach in selecting references, focusing primarily on works published within reputable journals over the past five years.
This paper evaluated AI in healthcare research streams using the SLR method [].As suggested by Massaro et al. [], an SLR enables the study of the scientific corpus of a research field, including the scientific rigour, reliability and replicability of operations carried out by researchers.As suggested by many scholars, the methodology allows qualitative and quantitative variables to highlight ...
This paper presents a systematic review of the role of Artificial Intelligence (AI) in healthcare, highlighting its a pplications and challenges. AI technologies, including machine learning,
Respiratory Research (2024) Artificial intelligence (AI) is poised to broadly reshape medicine, potentially improving the experiences of both clinicians and patients. We discuss key findings from ...
1. Introduction1.1. Background. The emergence of artificial intelligence (AI) within healthcare holds much promise. AI in healthcare helps to enhance patient diagnoses, improve prevention and treatment, increase cost-efficiency, and serve as a way to provide equitable access and treatment for all [1, 2].The term AI innovation refers to the creation of new knowledge, tools, and ideas [3] using ...
Artificial intelligence (AI) has the potential to transform care delivery by improving health outcomes, patient safety, and the affordability and accessibility of high-quality care. AI will be ...
The advancements in artificial intelligence (AI) have provided a wealth of opportunities for clinical practice and healthcare. Large language models (LLMs), such as BERT, GPT, and LaMDA have experienced exponential growth, with some now containing over a trillion parameters. 1 This growth in AI capabilities allows for seamless integration between different types of data and has led to ...
VOL. 388 NO. 13. Artificial intelligence (AI) has gained recent public prominence with the release of deep-learning models that can generate anything from art to term papers with minimal human ...
The implementation of artificial intelligence (AI) is driving significant transformation inside the administrative and clinical workflows of healthcare organizations at an accelerated rate. This modification highlights the significant impact that AI has on a variety of tasks, especially in health procedures relating to early detection and diagnosis. Papers done in the past imply that AI has ...
Artificial intelligence is gradually changing the landscape of healthcare and biomedical research. In the Aravind Eye Care System in India, ophthalmologists and computer scientists are working ...
SUBMIT PAPER. Healthcare Management Forum. Journal indexing and metrics. JOURNAL HOMEPAGE. ... The Dartmouth summer research project on artificial intelligence. Artificial intelligence: past, present, and future. 1956. ... Artificial Intelligence in Health Care Sector and Future Scope.
Abstract. Artificial intelligence is to reduce human cognitive functions. It is bringing an approach to healthcare, powdered by increasing the availability of healthcare data and rapid progress of ...
Artificial intelligence (AI) has become a rapidly growing field with the potential to revolutionize many industries, including healthcare. Integrating AI into healthcare has the potential to transform patient care and disease management, leading to improved outcomes and reduced costs. Our research explores the various applications of AI in healthcare, including predictive analytics, medical ...
AI and robotics in health care using artificial intelligence develops quickly, especially for early detection and diagnostic application. 3 Ai is becoming more powerful at the same time. It enables them to do what humans perform — often more efficiently, easily, and at reduced cost. ... The research type of this paper includes five journals 1 ...
Artificial Intelligence (AI) has emerged as a transformative technology with immense potential in the field of medicine. ... we identified and included a subset of 52 papers that were directly relevant to our research, including four on cardiology, three on ... Li H., Ma S., Wang Y. Artificial intelligence in healthcare: Past, present and ...
Academics and practitioners are paying increasing attention to service automation and taking advantage of the tremendous opportunities offered by artificial intelligence (AI). The requirement to deliver effective services has greatly increased interest in this topic. In the current study, we examined how AI is being used in healthcare. We searched the Scopus database for articles to obtain a ...
In recent years, artificial intelligence (AI) technologies have greatly advanced and become a reality in many areas of our daily lives. In the health care field, numerous efforts are being made to implement the AI technology for practical medical treatments. With the rapid developments in machine learning algorithms and improvements in hardware ...
The results of the present research, demonstrate that Artificial Intelligence is catalyzing transformative advancements in mental health care, facilitating a diverse array of interventions tailored to meet specific clinical challenges and therapeutic targets.
Research topics. Artificial Intelligence (AI) is a novel topic based on already known knowledge, which has several healthcare implications. Due to its continuous growth, there is the potential for a structured literature review (SLR) investigating how AI can contribute to healthcare implementation. 5069 results.
Natural Language Processing (NLP) is a subset of artificial intelligence that enables machines to understand and respond to human language through Large Language Models (LLMs)‥ These models have diverse applications in fields such as medical research, scientific writing, and publishing, but concerns such as hallucination, ethical issues, bias, and cybersecurity need to be addressed.
As the burgeoning field of Artificial Intelligence (AI) continues to permeate the fabric of healthcare, particularly in the realms of patient surveillance and telemedicine, a transformative era beckons. This manuscript endeavors to unravel the intricacies of recent AI advancements and their profound …
Therefore, this paper aims to introduce the current research and application status of AI technology in health care and discuss the issues that need to be resolved. Keywords: Further, various attempts have been made to develop and commercialize AI-based medical devices.
Artificial Intelligence (AI) is increasingly being used at different stages of teaching and learning, from kindergarten to university education, to enhance the learning and development of learners. Research has proven that AI can perform multiple roles aimed at effectively facilitating learning and improving performance.
The Role of AI in Healthcare. Artificial Intelligence (AI) ... The vast amount of data generated in hospitals—ranging from patient records to medical research—holds immense potential for improving healthcare outcomes. AI excels at analyzing big data, identifying trends, and predicting future healthcare needs. For example, AI can analyze ...
Figure. Multifaceted approach for ethical and equitable implementation of artificial intelligence (AI) in public health and medicine. [A text version of this figure is available.]. To advance public health and medicine responsibly, it is also imperative that partners work collaboratively to ensure that AI technologies not only meet the highest standards of innovation but also adhere to ethical ...
The complexity and rise of data in healthcare means that artificial intelligence (AI) will increasingly be applied within the field. Several types of AI are already being employed by payers and providers of care, and life sciences companies. The key categories of applications involve diagnosis and treatment recommendations, patient engagement ...
The OECD Artificial Intelligence Papers series draws on comprehensive evidence-base to identify trends and developments and delve into an extensive array of AI-related subjects. ... healthcare and scientific research. However, these technologies also pose critical societal and policy challenges that policy makers must confront: potential shifts ...
The AI-associated healthcare market is expected to grow rapidly and reach USD 6.6 billion by 2021 corresponding to a 40% compound annual growth rate [4]. 2.1.1. Technological advancements. There have been a great number of technological advances within the field of AI and data science in the past decade.