
An official website of the Department of Health & Human Services
- Search All AHRQ Sites
- Email Updates

1. Use quotes to search for an exact match of a phrase.
2. Put a minus sign just before words you don't want.
3. Enter any important keywords in any order to find entries where all these terms appear.
- The PSNet Collection
- All Content
- Perspectives
- Current Weekly Issue
- Past Weekly Issues
- Curated Libraries
- Clinical Areas
- Patient Safety 101
- The Fundamentals
- Training and Education
- Continuing Education
- WebM&M: Case Studies
- Training Catalog
- Submit a Case
- Improvement Resources
- Innovations
- Submit an Innovation
- About PSNet
- Editorial Team
- Technical Expert Panel

Developing critical thinking skills for delivering optimal care
Scott IA, Hubbard RE, Crock C, et al. Developing critical thinking skills for delivering optimal care. Intern Med J. 2021;51(4):488-493. doi: 10.1111/imj.15272
Sound critical thinking skills can help clinicians avoid cognitive biases and diagnostic errors. This article describes three critical thinking skills essential to effective clinical care – clinical reasoning, evidence-informed decision-making, and systems thinking – and approaches to develop these skills during clinician training.
Medication use and cognitive impairment among residents of aged care facilities. June 23, 2021
COVID-19 pandemic and the tension between the need to act and the need to know. October 14, 2020
Countering cognitive biases in minimising low value care. June 7, 2017
Scoping review of studies evaluating frailty and its association with medication harm. June 22, 2022
Choosing wisely in clinical practice: embracing critical thinking, striving for safer care. April 6, 2022
An act of performance: exploring residents' decision-making processes to seek help. April 14, 2021
'More than words' - interpersonal communication, cognitive bias and diagnostic errors. August 11, 2021
Decreased incidence of cesarean surgical site infection rate with hospital-wide perioperative bundle. September 29, 2021
Patient harm from cardiovascular medications. August 25, 2021
Analysis of lawsuits related to diagnostic errors from point-of-care ultrasound in internal medicine, paediatrics, family medicine and critical care in the USA. June 24, 2020
Pharmacists reducing medication risk in medical outpatient clinics: a retrospective study of 18 clinics. March 8, 2023
Estimating the economic cost of nurse sensitive adverse events amongst patients in medical and surgical settings. June 16, 2021
Changes in unprofessional behaviour, teamwork, and co-operation among hospital staff during the COVID-19 pandemic. September 28, 2022
Nursing surveillance: a concept analysis May 18, 2022
Delays in diagnosis, treatment, and surgery: root causes, actions taken, and recommendations for healthcare improvement. June 1, 2022
Nurse's Achilles Heel: using big data to determine workload factors that impact near misses. April 14, 2021
Multiple meanings of resilience: health professionals' experiences of a dual element training intervention designed to help them prepare for coping with error. March 31, 2021
Exploring the impact of employee engagement and patient safety. September 14, 2022
Differential diagnosis checklists reduce diagnostic error differentially: a randomised experiment. January 26, 2022
Think twice: effects on diagnostic accuracy of returning to the case to reflect upon the initial diagnosis. September 23, 2020
Associations between healthcare environment design and adverse events in intensive care unit. May 26, 2021
Barriers to accessing nighttime supervisors: a national survey of internal medicine residents. March 17, 2021
Predicting avoidable hospital events in Maryland. December 1, 2021
Pediatric transport safety collaborative: adverse events with parental presence during pediatric critical care transport. November 10, 2021
An observational study of postoperative handoff standardization failures. June 23, 2021
A partially structured postoperative handoff protocol improves communication in 2 mixed surgical intensive care units: findings from the Handoffs and Transitions in Critical Care (HATRICC) prospective cohort study. February 6, 2019
Effect of the surgical safety checklist on provider and patient outcomes: a systematic review. April 27, 2022
Toward the development of the perfect medical team: critical components for adaptation. March 17, 2021
The gaps in specialists' diagnoses. April 11, 2018
Doctors charged with manslaughter in the course of medical practice, 1795-2005: a literature review. July 19, 2006
Transforming the medication regimen review process using telemedicine to prevent adverse events. December 16, 2020
Evaluating the relationship between health information technology and safer-prescribing in the long-term care setting: a systematic review. March 17, 2021
Strategies to prevent missed nursing care: an international qualitative study based upon a positive deviance approach. May 12, 2021
Filling a gap in safety metrics: development of a patient-centred framework to identify and categorise patient-reported breakdowns related to the diagnostic process in ambulatory care. October 27, 2021
The association between nurse staffing and omissions in nursing care: a systematic review. July 11, 2018
Developing a patient safety culture in primary dental care. June 16, 2021
Impact of unacceptable behaviour between healthcare workers on clinical performance and patient outcomes: a systematic review. February 16, 2022
Standardized assessment of medication reconciliation in post-acute care. April 27, 2022
Cognitive biases in surgery: systematic review. March 1, 2023
Reducing failure to rescue rates in a paediatric in-patient setting: a 9-year quality improvement study. November 24, 2021
Interprofessional and intraprofessional communication about older people's medications across transitions of care. May 26, 2021
Diagnostic errors in hospitalized adults who died or were transferred to intensive care. January 17, 2024
Missed nursing care during the COVID-19 pandemic: a comparative observational study. July 21, 2021
Impact of interoperability of smart infusion pumps and an electronic medical record in critical care. September 23, 2020
Evaluation of a second victim peer support program on perceptions of second victim experiences and supportive resources in pediatric clinical specialties using the second victim experience and support tool (SVEST). November 3, 2021
Association between limiting the number of open records in a tele-critical care setting and retract-reorder errors. July 21, 2021
Understanding the second victim experience among multidisciplinary providers in obstetrics and gynecology. May 19, 2021
Care coordination strategies and barriers during medication safety incidents: a qualitative, cognitive task analysis. March 10, 2021
Optimising the delivery of remediation programmes for doctors: a realist review. June 2, 2021
Safety competency: exploring the impact of environmental and personal factors on the nurse's ability to deliver safe care. October 19, 2022
Risk assessment of the acute stroke diagnostic process using failure modes, effects, and criticality analysis. March 1, 2023
Encouraging patients to speak up about problems in cancer care. January 12, 2022
Treatment patterns and clinical outcomes after the introduction of the Medicare Sepsis Performance Measure (SEP-1). May 5, 2021
Patient perceptions of safety in primary care: a qualitative study to inform care. October 13, 2021
Staffing, teamwork and scope of practice: analysis of the association with patient safety in the context of rehabilitation. December 15, 2021
Use of heuristics during the clinical decision process from family care physicians in real conditions. October 6, 2021
Clinical and economic impacts of explicit tools detecting prescribing errors: a systematic review. May 26, 2021
Diagnostic errors in pediatric critical care: a systematic review. April 28, 2021
Emergency departments are higher-risk locations for wrong blood in tube errors. September 29, 2021
TRIAD IX: can a patient testimonial safely help ensure prehospital appropriate critical versus end-of-life care? September 15, 2021
Survey of nurses' experiences applying The Joint Commission's medication management titration standards. November 3, 2021
Clinical predictors for unsafe direct discharge home patients from intensive care units. October 21, 2020
A diagnostic time-out to improve differential diagnosis in pediatric abdominal pain. July 14, 2021
How providers can optimize effective and safe scribe use: a qualitative study. February 1, 2023
Estimation of breast cancer overdiagnosis in a U.S. breast screening cohort. March 16, 2022
Second victim experiences of nurses in obstetrics and gynaecology: a Second Victim Experience and Support Tool Survey December 23, 2020
Improving patient safety in intensive care units in Michigan. June 25, 2008
Perceived patient safety culture in a critical care transport program. July 31, 2013
The impact of health information management professionals on patient safety: a systematic review. December 22, 2021
Developing and aligning a safety event taxonomy for inpatient psychiatry. July 13, 2022
Opioids and falls risk in older adults: a narrative review. May 25, 2022
COVID-19: patient safety and quality improvement skills to deploy during the surge. June 24, 2020
Scoping review of patients' attitudes about their role and behaviours to ensure safe care at the direct care level. August 26, 2020
Mitigating imperfect data validity in administrative data PSIs: a method for estimating true adverse event rates. March 3, 2021
Can patients contribute to enhancing the safety and effectiveness of test-result follow-up? Qualitative outcomes from a health consumer workshop. June 2, 2021
Specificity of computerized physician order entry has a significant effect on the efficiency of workflow for critically ill patients. April 21, 2005
Improving patient care. The cognitive psychology of missed diagnoses. April 21, 2005
Quality of life after maternal near miss: a systematic review. June 2, 2021
Missed nursing care in the critical care unit, before and during the COVID-19 pandemic: a comparative cross-sectional study. June 22, 2022
Accuracy of practitioner estimates of probability of diagnosis before and after testing. May 5, 2021
Medication reconciliation at hospital discharge: a qualitative exploration of acute care nurses' perceptions of their roles and responsibilities. March 23, 2022
The July Effect in podiatric medicine and surgery residency. July 14, 2021
"Good catch, Kiddo"--enhancing patient safety in the pediatric emergency department through simulation. December 9, 2020
How can never event data be used to reflect or improve hospital safety performance? May 19, 2021
Healthcare professionals' encounters with ethnic minority patients: the critical incident approach. June 16, 2021
Medication errors' causes analysis in home care setting: a systematic review. February 9, 2022
Development of a core drug list towards improving prescribing education and reducing errors in the UK. March 2, 2011
What does safety in mental healthcare transitions mean for service users and other stakeholder groups: an open-ended questionnaire study. March 3, 2021
'Doing the best we can': Registered nurses' experiences and perceptions of patient safety in intensive care during COVID-19. September 7, 2022
The critical role of health information technology in the safe integration of behavioral health and primary care to improve patient care. November 10, 2021
The influence of COVID-19 visitation restrictions on patient experience and safety outcomes: a critical role for subjective advocates. July 14, 2021
Development of a multicomponent intervention to decrease racial bias among healthcare staff. July 27, 2022
Prescribing decision making by medical residents on night shifts: a qualitative study. November 9, 2022
Perceptions of providing safe care for frail older people at home: a qualitative study based on focus group interviews with home care staff. November 10, 2021
Pharmacist-led program to improve transitions from acute care to skilled nursing facility care. July 8, 2020
Peer support by interprofessional health care providers in aftermath of patient safety incidents: a cross-sectional study. June 9, 2021
The safety of inpatient health care. January 25, 2023
Provider-patient communication and hospital ratings: perceived gaps and forward thinking about the effects of COVID-19. December 16, 2020
Characteristics of critical incident reporting systems in primary care: an international survey. January 19, 2022
The MedSafer study-electronic decision support for deprescribing in hospitalized older adults: a cluster randomized clinical trial. February 2, 2022
All in Her Head. The Truth and Lies Early Medicine Taught Us About Women's Bodies and Why It Matters Today. March 20, 2024
The racial disparities in maternal mortality and impact of structural racism and implicit racial bias on pregnant Black women: a review of the literature. December 6, 2023
A scoping review exploring the confidence of healthcare professionals in assessing all skin tones. October 4, 2023
Patient safety in palliative care at the end of life from the perspective of complex thinking. August 16, 2023
Only 1 in 5 people with opioid addiction get the medications to treat it, study finds. August 16, 2023
Factors influencing in-hospital prescribing errors: a systematic review. July 19, 2023
Introducing second-year medical students to diagnostic reasoning concepts and skills via a virtual curriculum. June 28, 2023
Context matters: toward a multilevel perspective on context in clinical reasoning and error. June 21, 2023
The good, the bad, and the ugly: operative staff perspectives of surgeon coping with intraoperative errors. June 14, 2023
Explicitly addressing implicit bias on inpatient rounds: student and faculty reflections. June 7, 2023
The time is now: addressing implicit bias in obstetrics and gynecology education. May 17, 2023
Listen to the whispers before they become screams: addressing Black maternal morbidity and mortality in the United States. May 3, 2023
Annual Perspective
Formalizing the hidden curriculum of performance enhancing errors. March 22, 2023
Implicit racial bias, health care provider attitudes, and perceptions of health care quality among African American college students in Georgia, USA. January 18, 2023
Structural racism and impact on sickle cell disease: sickle cell lives matter. January 11, 2023
The REPAIR Project: a prospectus for change toward racial justice in medical education and health sciences research: REPAIR project steering committee. January 11, 2023
Using the Assessment of Reasoning Tool to facilitate feedback about diagnostic reasoning. January 11, 2023
Exploring the intersection of structural racism and ageism in healthcare. December 7, 2022
Calibrate Dx: A Resource to Improve Diagnostic Decisions. October 19, 2022
Improved Diagnostic Accuracy Through Probability-Based Diagnosis. September 28, 2022
Medical malpractice lawsuits involving trainees in obstetrics and gynecology in the USA. September 21, 2022
Skin cancer is a risk no matter the skin tone. But it may be overlooked in people with dark skin. August 17, 2022
Narrowing the mindware gap in medicine. July 20, 2022
From principles to practice: embedding clinical reasoning as a longitudinal curriculum theme in a medical school programme. June 15, 2022
A call to action: next steps to advance diagnosis education in the health professions. June 8, 2022
Does a suggested diagnosis in a general practitioners' referral question impact diagnostic reasoning: an experimental study. April 27, 2022
WebM&M Cases
Analysis of the interprofessional clinical learning environment for quality improvement and patient safety from perspectives of interprofessional teams. March 16, 2022

Connect With Us
Sign up for Email Updates
To sign up for updates or to access your subscriber preferences, please enter your email address below.
Agency for Healthcare Research and Quality
5600 Fishers Lane Rockville, MD 20857 Telephone: (301) 427-1364
- Accessibility
- Disclaimers
- Electronic Policies
- HHS Digital Strategy
- HHS Nondiscrimination Notice
- Inspector General
- Plain Writing Act
- Privacy Policy
- Viewers & Players
- U.S. Department of Health & Human Services
- The White House
- Don't have an account? Sign up to PSNet
Submit Your Innovations
Please select your preferred way to submit an innovation.
Continue as a Guest
Track and save your innovation
in My Innovations
Edit your innovation as a draft
Continue Logged In
Please select your preferred way to submit an innovation. Note that even if you have an account, you can still choose to submit an innovation as a guest.
Continue logged in
New users to the psnet site.
Access to quizzes and start earning
CME, CEU, or Trainee Certification.
Get email alerts when new content
matching your topics of interest
in My Innovations.
What is Critical Thinking in Nursing? (With Examples, Importance, & How to Improve)

Successful nursing requires learning several skills used to communicate with patients, families, and healthcare teams. One of the most essential skills nurses must develop is the ability to demonstrate critical thinking. If you are a nurse, perhaps you have asked if there is a way to know how to improve critical thinking in nursing? As you read this article, you will learn what critical thinking in nursing is and why it is important. You will also find 18 simple tips to improve critical thinking in nursing and sample scenarios about how to apply critical thinking in your nursing career.
What Is Critical Thinking In Nursing?
4 reasons why critical thinking is so important in nursing, 1. critical thinking skills will help you anticipate and understand changes in your patient’s condition., 2. with strong critical thinking skills, you can make decisions about patient care that is most favorable for the patient and intended outcomes., 3. strong critical thinking skills in nursing can contribute to innovative improvements and professional development., 4. critical thinking skills in nursing contribute to rational decision-making, which improves patient outcomes., what are the 8 important attributes of excellent critical thinking in nursing, 1. the ability to interpret information:, 2. independent thought:, 3. impartiality:, 4. intuition:, 5. problem solving:, 6. flexibility:, 7. perseverance:, 8. integrity:, examples of poor critical thinking vs excellent critical thinking in nursing, 1. scenario: patient/caregiver interactions, poor critical thinking:, excellent critical thinking:, 2. scenario: improving patient care quality, 3. scenario: interdisciplinary collaboration, 4. scenario: precepting nursing students and other nurses, how to improve critical thinking in nursing, 1. demonstrate open-mindedness., 2. practice self-awareness., 3. avoid judgment., 4. eliminate personal biases., 5. do not be afraid to ask questions., 6. find an experienced mentor., 7. join professional nursing organizations., 8. establish a routine of self-reflection., 9. utilize the chain of command., 10. determine the significance of data and decide if it is sufficient for decision-making., 11. volunteer for leadership positions or opportunities., 12. use previous facts and experiences to help develop stronger critical thinking skills in nursing., 13. establish priorities., 14. trust your knowledge and be confident in your abilities., 15. be curious about everything., 16. practice fair-mindedness., 17. learn the value of intellectual humility., 18. never stop learning., 4 consequences of poor critical thinking in nursing, 1. the most significant risk associated with poor critical thinking in nursing is inadequate patient care., 2. failure to recognize changes in patient status:, 3. lack of effective critical thinking in nursing can impact the cost of healthcare., 4. lack of critical thinking skills in nursing can cause a breakdown in communication within the interdisciplinary team., useful resources to improve critical thinking in nursing, youtube videos, my final thoughts, frequently asked questions answered by our expert, 1. will lack of critical thinking impact my nursing career, 2. usually, how long does it take for a nurse to improve their critical thinking skills, 3. do all types of nurses require excellent critical thinking skills, 4. how can i assess my critical thinking skills in nursing.
• Ask relevant questions • Justify opinions • Address and evaluate multiple points of view • Explain assumptions and reasons related to your choice of patient care options
5. Can I Be a Nurse If I Cannot Think Critically?


Clinical Nurse Educators' LibGuide
- Keeping up to date This link opens in a new window
- Recent articles from the Journal of Nursing Education and Practice
- Critical thinking and clinical reasoning
- LibGuides Homepage This link opens in a new window
Library support
Library staff can assist you with:
- Literature searching
- Research skills training and support
- EndNote training
- Advice regarding getting published
- Document delivery to obtain full text of journal articles
- And more... see the Library website
Contact or visit your local CLIN Library to find out more about our full range of services and for assistance with your research project.
Some articles on critical thinking in nursing practice
- Fero, L. J., et al. (2009). "Critical thinking ability of new graduate and experienced nurses." Journal of Advanced Nursing 65(1): 139-148. This paper is a report of a study to identify critical thinking learning needs of new and experienced nurses. Concern for patient safety has grown worldwide as high rates of error and injury continue to be reported. In order to improve patient safety, nurses must be able to recognize changes in patient condition, perform independent nursing interventions, anticipate orders and prioritize. Conclusion. Patient safety may be compromised if a nurse cannot provide clinically competent care. Assessments such as the Performance Based Development System can provide information about learning needs and facilitate individualized orientation targeted to increase performance level. © 2008 Blackwell Publishing Ltd.
- Jacob, E., et al. (2018). "Development of an Australian nursing critical thinking tool using a Delphi process." Journal of Advanced Nursing. AIM To develop a critical thinking assessment tool for Australian undergraduate nurses. BACKGROUND Critical thinking is an important skill but difficult to assess in nursing practice. There are often many responses a nurse can make to a clinical problem or situation. Some responses are more correct than others and these decisions have an impact on a patient's care and safety. Differences in a response can relate to the depth of knowledge, experience and critical thinking ability of the individual nurse. DESIGN This study used a Delphi process to develop five clinical case studies together with the most appropriate clinical responses to 25 clinical questions. RESULTS Four rounds of Delphi questions were required to reach consensus on the correct wording and answers for the scenarios. Five case studies have been developed with nursing responses to patient management in rank order from most correct to least correct. CONCLUSION Use of the tool should provide confidence that a nurse has met a certain level of critical thinking ability.
- Ludin, S. M. (2017). "Does good critical thinking equal effective decision-making among critical care nurses? A cross-sectional survey."Intensive and Critical Care Nursing. v. 44 https://doi.org/10.1016/j.iccn.2017.06.002 Background: A critical thinker may not necessarily be a good decision-maker, but critical care nurses are expected to utilise outstanding critical thinking skills in making complex clinical judgements. Studies have shown that critical care nurses' decisions focus mainly on doing rather than reflecting. To date, the link between critical care nurses' critical thinking and decision-making has not been examined closely in Malaysia.
- Simpson, E. and M. Courtney (2002). "Critical thinking in nursing education: literature review." International journal of nursing practice 8(2): 89-98. The need for critical thinking in nursing has been accentuated in response to the rapidly changing health-care environment. Nurses must think critically to provide effective care while coping with the expansion in role associated with the complexities of current health-care systems. This literature review will present a history of inquiry into critical thinking and research to support the conclusion that critical thinking is necessary not only in the clinical practice setting, but also as an integral component of nursing-education programmes to promote the development of nurses' critical-thinking abilities. The aims of this paper are to: (i) review the literature on critical thinking; (ii) examine the dimensions of critical thinking; (iii) investigate the various critical thinking strategies for their appropriateness to enhance critical thinking in nurses; and (iv) examine issues relating to the evaluation of critical-thinking skills in nursing.
- Turner, P. (2005) "Critical thinking in nursing education and practice as defined in the literature". Nursing Education Perspectives 26(5): 272-277. Critical thinking is frequently discussed in nursing education and nursing practice literature. This article presents an analysis of the concept of critical thinking as it applies to nursing, differentiating its use in education and practice literature. Three computerized databases (CINAHL, MEDLINE, and EBSCO) were searched for the years 1981 to 2002, using the keywords critical thinking. References were stratified into two 11-year periods (1981-1991, 1992-2002) to identify changes in the concept over time and integration of the concept differentially into nursing education and nursing practice. A random sample of literature from each stratum was coded for definitions, attributes, surrogate terms, referents, antecedents, and consequences of critical thinking. Critical thinking as a nursing concept has matured since its first appearance in the literature. It is well defined and has clear characteristics. However, antecedents and consequences are not well defined, and many consequences are identical to attributes and surrogate terms. Additional work is needed to clarify the boundaries of the concept of critical thinking in nursing.
Books on critical thinking and clinical reasoning
- << Previous: Recent articles from the Journal of Nursing Education and Practice
- Next: LibGuides Homepage >>
- Last Updated: Feb 8, 2024 2:18 PM
- URL: https://swslhd.libguides.com/CNE
Critical Thinking in Nursing
- First Online: 02 January 2023
Cite this chapter

- Şefika Dilek Güven 3
Part of the book series: Integrated Science ((IS,volume 12))
1079 Accesses
Critical thinking is an integral part of nursing, especially in terms of professionalization and independent clinical decision-making. It is necessary to think critically to provide adequate, creative, and effective nursing care when making the right decisions for practices and care in the clinical setting and solving various ethical issues encountered. Nurses should develop their critical thinking skills so that they can analyze the problems of the current century, keep up with new developments and changes, cope with nursing problems they encounter, identify more complex patient care needs, provide more systematic care, give the most appropriate patient care in line with the education they have received, and make clinical decisions. The present chapter briefly examines critical thinking, how it relates to nursing, and which skills nurses need to develop as critical thinkers.
Graphical Abstract/Art Performance

Critical thinking in nursing.
This painting shows a nurse and how she is thinking critically. On the right side are the stages of critical thinking and on the left side, there are challenges that a nurse might face. The entire background is also painted in several colors to represent a kind of intellectual puzzle. It is made using colored pencils and markers.
(Adapted with permission from the Association of Science and Art (ASA), Universal Scientific Education and Research Network (USERN); Painting by Mahshad Naserpour).
Unless the individuals of a nation thinkers, the masses can be drawn in any direction. Mustafa Kemal Atatürk
This is a preview of subscription content, log in via an institution to check access.
Access this chapter
- Available as PDF
- Read on any device
- Instant download
- Own it forever
- Available as EPUB and PDF
- Compact, lightweight edition
- Dispatched in 3 to 5 business days
- Free shipping worldwide - see info
- Durable hardcover edition
Tax calculation will be finalised at checkout
Purchases are for personal use only
Institutional subscriptions
Bilgiç Ş, Kurtuluş Tosun Z (2016) Birinci ve son sınıf hemşirelik öğrencilerinde eleştirel düşünme ve etkileyen faktörler. Sağlık Bilimleri ve Meslekleri Dergisi 3(1):39–47
Article Google Scholar
Kantek F, Yıldırım N (2019) The effects of nursing education on critical thinking of students: a meta-analysis. Florence Nightingale Hemşirelik Dergisi 27(1):17–25
Ennis R (1996) Critical thinking dispositions: their nature and assessability. Informal Logic 18(2):165–182
Riddell T (2007) Critical assumptions: thinking critically about critical thinking. J Nurs Educ 46(3):121–126
Cüceloğlu D (2001) İyi düşün doğru karar ver. Remzi Kitabevi, pp 242–284
Google Scholar
Kurnaz A (2019) Eleştirel düşünme öğretimi etkinlikleri Planlama-Uygulama ve Değerlendirme. Eğitim yayın evi, p 27
Doğanay A, Ünal F (2006) Eleştirel düşünmenin öğretimi. In: İçerik Türlerine Dayalı Öğretim. Ankara Nobel Yayınevi, pp 209–261
Scheffer B-K, Rubenfeld M-G (2000) A consensus statement on critical thinking in nursing. J Nurs Educ 39(8):352–359
Article CAS Google Scholar
Rubenfeld M-G, Scheffer B (2014) Critical thinking tactics for nurses. Jones & Bartlett Publishers, pp 5–6, 7, 19–20
Gobet F (2005) Chunking models of expertise: implications for education. Appl Cogn Psychol 19:183–204
Ay F-A (2008) Mesleki temel kavramlar. In: Temel hemşirelik: Kavramlar, ilkeler, uygulamalar. İstanbul Medikal Yayıncılık, pp 205–220
Birol L (2010) Hemşirelik bakımında sistematik yaklaşım. In: Hemşirelik süreci. Berke Ofset Matbaacılık, pp 35–45
Twibell R, Ryan M, Hermiz M (2005) Faculty perceptions of critical thinking in student clinical experiences. J Nurs Educ 44(2):71–79
The Importance of Critical Thinking in Nursing. 19 November 2018 by Carson-Newman University Online. https://onlinenursing.cn.edu/news/value-critical-thinking-nursing
Suzanne C, Smeltzer Brenda G, Bare Janice L, Cheever HK (2010) Definition of critical thinking, critical thinking process. Medical surgical nursing. Lippincott, Williams & Wilkins, pp 27–28
Profetto-McGrath J (2003) The relationship of critical thinking skills and critical thinking dispositions of baccalaureate nursing students. J Adv Nurs 43(6):569–577
Elaine S, Mary C (2002) Critical thinking in nursing education: literature review. Int J Nurs Pract 8(2):89–98
Brunt B-A (2005) Critical thinking in nursing: an integrated review. J Continuing Educ Nurs 36(2):60–67
Carter L-M, Rukholm E (2008) A study of critical thinking, teacher–student interaction, and discipline-specific writing in an online educational setting for registered nurses. J Continuing Educ Nurs 39(3):133–138
Daly W-M (2001) The development of an alternative method in the assessment of critical thinking as an outcome of nursing education. J Adv Nurs 36(1):120–130
Edwards S-L (2007) Critical thinking: a two-phase framework. Nurse Educ Pract 7(5):303–314
Rogal S-M, Young J (2008) Exploring critical thinking in critical care nursing education: a pilot study. J Continuing Educ Nurs 39(1):28–33
Worrell J-A, Profetto-McGrath J (2007) Critical thinking as an outcome of context-based learning among post RN students: a literature review. Nurse Educ Today 27(5):420–426
Morrall P, Goodman B (2013) Critical thinking, nurse education and universities: some thoughts on current issues and implications for nursing practice. Nurse Educ Today 33(9):935–937
Raymond-Seniuk C, Profetto-McGrath J (2011) Can one learn to think critically?—a philosophical exploration. Open Nurs J 5:45–51
Download references
Author information
Authors and affiliations.
Nevşehir Hacı Bektaş Veli University, Semra ve Vefa Küçük, Faculty of Health Sciences, Nursing Department, 2000 Evler Mah. Damat İbrahim Paşa Yerleşkesi, Nevşehir, Turkey
Şefika Dilek Güven
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Şefika Dilek Güven .
Editor information
Editors and affiliations.
Universal Scientific Education and Research Network (USERN), Stockholm, Sweden
Nima Rezaei
Rights and permissions
Reprints and permissions
Copyright information
© 2023 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Güven, Ş.D. (2023). Critical Thinking in Nursing. In: Rezaei, N. (eds) Brain, Decision Making and Mental Health. Integrated Science, vol 12. Springer, Cham. https://doi.org/10.1007/978-3-031-15959-6_10
Download citation
DOI : https://doi.org/10.1007/978-3-031-15959-6_10
Published : 02 January 2023
Publisher Name : Springer, Cham
Print ISBN : 978-3-031-15958-9
Online ISBN : 978-3-031-15959-6
eBook Packages : Behavioral Science and Psychology Behavioral Science and Psychology (R0)
Share this chapter
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Publish with us
Policies and ethics
- Find a journal
- Track your research
- - Google Chrome
Intended for healthcare professionals
- Access provided by Google Indexer
- My email alerts
- BMA member login
- Username * Password * Forgot your log in details? Need to activate BMA Member Log In Log in via OpenAthens Log in via your institution

Search form
- Advanced search
- Search responses
- Search blogs
- News & Views
- Margaret McCartney:...
Nurses are critical thinkers
Rapid response to:
Margaret McCartney: Nurses must be allowed to exercise professional judgment
- Related content
- Article metrics
- Rapid responses
Rapid Response:
The characteristic that distinguishes a professional nurse is cognitive rather than psychomotor ability. Nursing practice demands that practitioners display sound judgement and decision-making skills as critical thinking and clinical decision making is an essential component of nursing practice. Nurses’ ability to recognize and respond to signs of patient deterioration in a timely manner plays a pivotal role in patient outcomes (Purling & King 2012). Errors in clinical judgement and decision making are said to account for more than half of adverse clinical events (Tomlinson, 2015). The focus of the nurse clinical judgement has to be on quality evidence based care delivery, therefore, observational and reasoning skills will result in sound, reliable, clinical judgements. Clinical judgement, a concept which is critical to the nursing can be complex, because the nurse is required to use observation skills, identify relevant information, to identify the relationships among given elements through reasoning and judgement. Clinical reasoning is the process by which nurses observe patients status, process the information, come to an understanding of the patient problem, plan and implement interventions, evaluate outcomes, with reflection and learning from the process (Levett-Jones et al, 2010). At all times, nurses are responsible for their actions and are accountable for nursing judgment and action or inaction.
The speed and ability by which the nurses make sound clinical judgement is affected by their experience. Novice nurses may find this process difficult, whereas the experienced nurse should rely on her intuition, followed by fast action. Therefore education must begin at the undergraduate level to develop students’ critical thinking and clinical reasoning skills. Clinical reasoning is a learnt skill requiring determination and active engagement in deliberate practice design to improve performance. In order to acquire such skills, students need to develop critical thinking ability, as well as an understanding of how judgements and decisions are reached in complex healthcare environments.
As lifelong learners, nurses are constantly accumulating more knowledge, expertise, and experience, and it’s a rare nurse indeed who chooses to not apply his or her mind towards the goal of constant learning and professional growth. Institute of Medicine (IOM) report on the Future of Nursing, stated, that nurses must continue their education and engage in lifelong learning to gain the needed competencies for practice. American Nurses Association (ANA), Scope and Standards of Practice requires a nurse to remain involved in continuous learning and strengthening individual practice (p.26)
Alfaro-LeFevre, R. (2009). Critical thinking and clinical judgement: A practical approach to outcome-focused thinking. (4th ed.). St Louis: Elsevier
The future of nursing: Leading change, advancing health, (2010). https://campaignforaction.org/resource/future-nursing-iom-report
Levett-Jones, T., Hoffman, K. Dempsey, Y. Jeong, S., Noble, D., Norton, C., Roche, J., & Hickey, N. (2010). The ‘five rights’ of clinical reasoning: an educational model to enhance nursing students’ ability to identify and manage clinically ‘at risk’ patients. Nurse Education Today. 30(6), 515-520.
NMC (2010) New Standards for Pre-Registration Nursing. London: Nursing and Midwifery Council.
Purling A. & King L. (2012). A literature review: graduate nurses’ preparedness for recognising and responding to the deteriorating patient. Journal of Clinical Nursing, 21(23–24), 3451–3465
Thompson, C., Aitken, l., Doran, D., Dowing, D. (2013). An agenda for clinical decision making and judgement in nursing research and education. International Journal of Nursing Studies, 50 (12), 1720 - 1726 Tomlinson, J. (2015). Using clinical supervision to improve the quality and safety of patient care: a response to Berwick and Francis. BMC Medical Education, 15(103)
Competing interests: No competing interests

- school Campus Bookshelves
- menu_book Bookshelves
- perm_media Learning Objects
- login Login
- how_to_reg Request Instructor Account
- hub Instructor Commons
- Download Page (PDF)
- Download Full Book (PDF)
- Periodic Table
- Physics Constants
- Scientific Calculator
- Reference & Cite
- Tools expand_more
- Readability
selected template will load here
This action is not available.

1.3: Critical Thinking and Clinical Reasoning
- Last updated
- Save as PDF
- Page ID 63335

- Ernstmeyer & Christman (Eds.)
- Chippewa Valley Technical College via OpenRN
Before learning how to use the nursing process, it is important to understand some basic concepts related to critical thinking and nursing practice. Let’s take a deeper look at how nurses think.
Critical Thinking and Clinical Reasoning
Nurses make decisions while providing patient care by using critical thinking and clinical reasoning. Critical thinking is a broad term used in nursing that includes “reasoning about clinical issues such as teamwork, collaboration, and streamlining workflow.” [1] Using critical thinking means that nurses take extra steps to maintain patient safety and don’t just “follow orders.” It also means the accuracy of patient information is validated and plans for caring for patients are based on their needs, current clinical practice, and research.
“Critical thinkers” possess certain attitudes that foster rational thinking. These attitudes are as follows:
- Independence of thought: Thinking on your own
- Fair-mindedness: Treating every viewpoint in an unbiased, unprejudiced way
- Insight into egocentricity and sociocentricity: Thinking of the greater good and not just thinking of yourself. Knowing when you are thinking of yourself (egocentricity) and when you are thinking or acting for the greater good (sociocentricity)
- Intellectual humility: Recognizing your intellectual limitations and abilities
- Nonjudgmental: Using professional ethical standards and not basing your judgments on your own personal or moral standards
- Integrity: Being honest and demonstrating strong moral principles
- Perseverance: Persisting in doing something despite it being difficult
- Confidence: Believing in yourself to complete a task or activity
- Interest in exploring thoughts and feelings: Wanting to explore different ways of knowing
- Curiosity: Asking “why” and wanting to know more
Clinical reasoning is defined as, “A complex cognitive process that uses formal and informal thinking strategies to gather and analyze patient information, evaluate the significance of this information, and weigh alternative actions.” To make sound judgments about patient care, nurses must generate alternatives, weigh them against the evidence, and choose the best course of action. The ability to clinically reason develops over time and is based on knowledge and experience. [3]
The ANA’s Standards of Professional Nursing Practice associated with each component of the nursing process are described below.
Assessment is the first step of the nursing process. The American Nurses Association (ANA) “Assessment” Standard of Practice is defined as, “The registered nurse collects pertinent data and information relative to the health care consumer’s health or the situation.” This includes collecting “pertinent data related to the health and quality of life in a systematic, ongoing manner, with compassion and respect for the wholeness, inherent dignity, worth, and unique attributes of every person, including but not limited to, demographics, environmental and occupational exposures, social determinants of health, health disparities, physical, functional, psychosocial, emotional, cognitive, spiritual/transpersonal, sexual, sociocultural, age-related, environmental, and lifestyle/economic assessments.” [1]
A registered nurse uses a systematic method to collect and analyze patient data. Assessment includes physiological data, as well as psychological, sociocultural, spiritual, economic, and lifestyle data. For example, a nurse’s assessment of a hospitalized patient in pain includes the patient’s response to pain, such as the inability to get out of bed, refusal to eat, withdrawal from family members, or anger directed at hospital staff. Nurses assess patients to gather clues, make generalizations, and diagnose human responses to health conditions and life processes. Patient data is considered either subjective or objective, and it can be collected from multiple sources.
The “Diagnosis” Standard of Practice is defined as, “The registered nurse analyzes the assessment data to determine actual or potential diagnoses, problems, and issues.” [13] A nursing diagnosis is the nurse’s clinical judgment about the client's response to actual or potential health conditions or needs. Nursing diagnoses are the bases for the nurse’s care plan and are different than medical diagnoses.
Outcomes Identification
The “Outcomes Identification” Standard of Practice is defined as, “The registered nurse identifies expected outcomes for a plan individualized to the health care consumer or the situation.” The nurse sets measurable and achievable short- and long-term goals and specific outcomes in collaboration with the patient based on their assessment data and nursing diagnoses.
The “Planning” Standard of Practice is defined as, “The registered nurse develops a collaborative plan encompassing strategies to achieve expected outcomes.” [16] Assessment data, diagnoses, and goals are used to select evidence-based nursing interventions customized to each patient’s needs and concerns. Goals, expected outcomes, and nursing interventions are documented in the patient’s nursing care plan so that nurses, as well as other health professionals, have access to it for continuity of care. [17]
Nursing Care Plans
Creating nursing care plans is a part of the “Planning” step of the nursing process. A nursing care plan is a type of documentation that demonstrates the individualized planning and delivery of nursing care for each specific patient using the nursing process. Registered nurses (RNs) create nursing care plans so that the care provided to the patient across shifts is consistent among health care personnel.
Implementation
The “Implementation” Standard of Practice is defined as, “The nurse implements the identified plan.” Nursing interventions are implemented or delegated with supervision according to the care plan to assure continuity of care across multiple nurses and health professionals caring for the patient. Interventions are also documented in the patient’s electronic medical record as they are completed.
The “Evaluation” Standard of Practice is defined as, “The registered nurse evaluates progress toward attainment of goals and outcomes.” During evaluation, nurses assess the patient and compare the findings against the initial assessment to determine the effectiveness of the interventions and overall nursing care plan. Both the patient’s status and the effectiveness of the nursing care must be continuously evaluated and modified as needed.
Benefits of Using the Nursing Process
Using the nursing process has many benefits for nurses, patients, and other members of the health care team. The benefits of using the nursing process include the following:
- Promotes quality patient care
- Decreases omissions and duplications
- Provides a guide for all staff involved to provide consistent and responsive care
- Encourages collaborative management of a patient’s health care problems
- Improves patient safety
- Improves patient satisfaction
- Identifies a patient’s goals and strategies to attain them
- Increases the likelihood of achieving positive patient outcomes
- Saves time, energy, and frustration by creating a care plan or path to follow
By using these components of the nursing process as a critical thinking model, nurses plan interventions customized to the patient’s needs, plan outcomes and interventions, and determine whether those actions are effective in meeting the patient’s needs. In the remaining sections of this chapter, we will take an in-depth look at each of these components of the nursing process. Using the nursing process and implementing evidence-based practices are referred to as the “science of nursing.” Let’s review concepts related to the “art of nursing” while providing holistic care in a caring manner using the nursing process.
Holistic Nursing Care
The American Nurses Association (ANA) recently updated the definition of nursing as, “Nursing integrates the art and science of caring and focuses on the protection, promotion, and optimization of health and human functioning; prevention of illness and injury; facilitation of healing; and alleviation of suffering through compassionate presence. Nursing is the diagnosis and treatment of human responses and advocacy in the care of individuals, families, groups, communities, and populations in the recognition of the connection of all humanity.”
The ANA further describes nursing is a learned profession built on a core body of knowledge that integrates both the art and science of nursing. The art of nursing is defined as, “Unconditionally accepting the humanity of others, respecting their need for dignity and worth, while providing compassionate, comforting care.”
Nurses care for individuals holistically, including their emotional, spiritual, psychosocial, cultural, and physical needs. They consider problems, issues, and needs that the person experiences as a part of a family and a community as they use the nursing process.
Caring and the Nursing Process
The American Nurses Association (ANA) states, “The act of caring is foundational to the practice of nursing.” Successful use of the nursing process requires the development of a care relationship with the patient. A care relationship is a mutual relationship that requires the development of trust between both parties. This trust is often referred to as the development of rapport and underlies the art of nursing. While establishing a caring relationship, the whole person is assessed, including the individual’s beliefs, values, and attitudes, while also acknowledging the vulnerability and dignity of the patient and family. Assessing and caring for the whole person takes into account the physical, mental, emotional, and spiritual aspects of being a human being. Caring interventions can be demonstrated in simple gestures such as active listening, making eye contact, touching, and verbal reassurances while also respecting and being sensitive to the care recipient’s cultural beliefs and meanings associated with caring behaviors.
- Klenke-Borgmann, L., Cantrell, M. A., & Mariani, B. (2020). Nurse educator’s guide to clinical judgment: A review of conceptualization, measurement, and development. Nursing Education Perspectives, 41 (4), 215-221. ↵
- Powers, L., Pagel, J., & Herron, E. (2020). Nurse preceptors and new graduate success. American Nurse Journal, 15 (7), 37-39. ↵
- “ The Detective ” by paurian is licensed under CC BY 2.0 ↵
- “ In the Quiet Zone… ” by C.O.D. Library is licensed under CC BY-NC-SA 2.0 ↵
- NCSBN. (n.d.). NCSBN clinical judgment model . https://www.ncsbn.org/14798.htm ↵
- American Nurses Association. (2021). Nursing: Scope and standards of practice (4th ed.). American Nurses Association. ↵
- “ The Nursing Process ” by Kim Ernstmeyer at Chippewa Valley Technical College is licensed under CC BY 4.0 ↵
- “Patient Image in LTC.JPG” by ARISE project is licensed under CC BY 4.0 ↵
- American Nurses Association. (n.d.). The nursing process. https://www.nursingworld.org/practice-policy/workforce/what-is-nursing/the-nursing-process/ ↵
- American Nurses Association. (n.d.). The nursing process . https://www.nursingworld.org/practice-policy/workforce/what-is-nursing/the-nursing-process/ ↵
- American Nurses Association. (2021). Nursing: Scope and standards of practice (3rd ed.). American Nurses Association. ↵
- American Nurses Association. (n.d.) The nursing process. https://www.nursingworld.org/practice-policy/workforce/what-is-nursing/the-nursing-process / ↵
- American Nurses Association. (n.d.). The nursing process. https://www.nursingworld.org/practice-policy/workforce/what-is-nursing/the-nursing-process / ↵
- Walivaara, B., Savenstedt, S., & Axelsson, K. (2013). Caring relationships in home-based nursing care - registered nurses’ experiences. The Open Journal of Nursing, 7 , 89-95. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3722540/pdf/TONURSJ-7-89.pdf ↵
- “ hospice-1793998_1280.jpg ” by truthseeker08 is licensed under CC0 ↵
- Watson Caring Science Institute. (n.d.). Watson Caring Science Institute. Jean Watson, PHD, RN, AHN-BC, FAAN, (LL-AAN) . https://www.watsoncaringscience.org/jean-bio/ ↵
The Value of Critical Thinking in Nursing

- How Nurses Use Critical Thinking
- How to Improve Critical Thinking
- Common Mistakes

Some experts describe a person’s ability to question belief systems, test previously held assumptions, and recognize ambiguity as evidence of critical thinking. Others identify specific skills that demonstrate critical thinking, such as the ability to identify problems and biases, infer and draw conclusions, and determine the relevance of information to a situation.
Nicholas McGowan, BSN, RN, CCRN, has been a critical care nurse for 10 years in neurological trauma nursing and cardiovascular and surgical intensive care. He defines critical thinking as “necessary for problem-solving and decision-making by healthcare providers. It is a process where people use a logical process to gather information and take purposeful action based on their evaluation.”
“This cognitive process is vital for excellent patient outcomes because it requires that nurses make clinical decisions utilizing a variety of different lenses, such as fairness, ethics, and evidence-based practice,” he says.
How Do Nurses Use Critical Thinking?
Successful nurses think beyond their assigned tasks to deliver excellent care for their patients. For example, a nurse might be tasked with changing a wound dressing, delivering medications, and monitoring vital signs during a shift. However, it requires critical thinking skills to understand how a difference in the wound may affect blood pressure and temperature and when those changes may require immediate medical intervention.
Nurses care for many patients during their shifts. Strong critical thinking skills are crucial when juggling various tasks so patient safety and care are not compromised.
Jenna Liphart Rhoads, Ph.D., RN, is a nurse educator with a clinical background in surgical-trauma adult critical care, where critical thinking and action were essential to the safety of her patients. She talks about examples of critical thinking in a healthcare environment, saying:
“Nurses must also critically think to determine which patient to see first, which medications to pass first, and the order in which to organize their day caring for patients. Patient conditions and environments are continually in flux, therefore nurses must constantly be evaluating and re-evaluating information they gather (assess) to keep their patients safe.”
The COVID-19 pandemic created hospital care situations where critical thinking was essential. It was expected of the nurses on the general floor and in intensive care units. Crystal Slaughter is an advanced practice nurse in the intensive care unit (ICU) and a nurse educator. She observed critical thinking throughout the pandemic as she watched intensive care nurses test the boundaries of previously held beliefs and master providing excellent care while preserving resources.
“Nurses are at the patient’s bedside and are often the first ones to detect issues. Then, the nurse needs to gather the appropriate subjective and objective data from the patient in order to frame a concise problem statement or question for the physician or advanced practice provider,” she explains.
Top 5 Ways Nurses Can Improve Critical Thinking Skills
We asked our experts for the top five strategies nurses can use to purposefully improve their critical thinking skills.
Case-Based Approach
Slaughter is a fan of the case-based approach to learning critical thinking skills.
In much the same way a detective would approach a mystery, she mentors her students to ask questions about the situation that help determine the information they have and the information they need. “What is going on? What information am I missing? Can I get that information? What does that information mean for the patient? How quickly do I need to act?”
Consider forming a group and working with a mentor who can guide you through case studies. This provides you with a learner-centered environment in which you can analyze data to reach conclusions and develop communication, analytical, and collaborative skills with your colleagues.
Practice Self-Reflection
Rhoads is an advocate for self-reflection. “Nurses should reflect upon what went well or did not go well in their workday and identify areas of improvement or situations in which they should have reached out for help.” Self-reflection is a form of personal analysis to observe and evaluate situations and how you responded.
This gives you the opportunity to discover mistakes you may have made and to establish new behavior patterns that may help you make better decisions. You likely already do this. For example, after a disagreement or contentious meeting, you may go over the conversation in your head and think about ways you could have responded.
It’s important to go through the decisions you made during your day and determine if you should have gotten more information before acting or if you could have asked better questions.
During self-reflection, you may try thinking about the problem in reverse. This may not give you an immediate answer, but can help you see the situation with fresh eyes and a new perspective. How would the outcome of the day be different if you planned the dressing change in reverse with the assumption you would find a wound infection? How does this information change your plan for the next dressing change?
Develop a Questioning Mind
McGowan has learned that “critical thinking is a self-driven process. It isn’t something that can simply be taught. Rather, it is something that you practice and cultivate with experience. To develop critical thinking skills, you have to be curious and inquisitive.”
To gain critical thinking skills, you must undergo a purposeful process of learning strategies and using them consistently so they become a habit. One of those strategies is developing a questioning mind. Meaningful questions lead to useful answers and are at the core of critical thinking .
However, learning to ask insightful questions is a skill you must develop. Faced with staff and nursing shortages , declining patient conditions, and a rising number of tasks to be completed, it may be difficult to do more than finish the task in front of you. Yet, questions drive active learning and train your brain to see the world differently and take nothing for granted.
It is easier to practice questioning in a non-stressful, quiet environment until it becomes a habit. Then, in the moment when your patient’s care depends on your ability to ask the right questions, you can be ready to rise to the occasion.
Practice Self-Awareness in the Moment
Critical thinking in nursing requires self-awareness and being present in the moment. During a hectic shift, it is easy to lose focus as you struggle to finish every task needed for your patients. Passing medication, changing dressings, and hanging intravenous lines all while trying to assess your patient’s mental and emotional status can affect your focus and how you manage stress as a nurse .
Staying present helps you to be proactive in your thinking and anticipate what might happen, such as bringing extra lubricant for a catheterization or extra gloves for a dressing change.
By staying present, you are also better able to practice active listening. This raises your assessment skills and gives you more information as a basis for your interventions and decisions.
Use a Process
As you are developing critical thinking skills, it can be helpful to use a process. For example:
- Ask questions.
- Gather information.
- Implement a strategy.
- Evaluate the results.
- Consider another point of view.
These are the fundamental steps of the nursing process (assess, diagnose, plan, implement, evaluate). The last step will help you overcome one of the common problems of critical thinking in nursing — personal bias.
Common Critical Thinking Pitfalls in Nursing
Your brain uses a set of processes to make inferences about what’s happening around you. In some cases, your unreliable biases can lead you down the wrong path. McGowan places personal biases at the top of his list of common pitfalls to critical thinking in nursing.
“We all form biases based on our own experiences. However, nurses have to learn to separate their own biases from each patient encounter to avoid making false assumptions that may interfere with their care,” he says. Successful critical thinkers accept they have personal biases and learn to look out for them. Awareness of your biases is the first step to understanding if your personal bias is contributing to the wrong decision.
New nurses may be overwhelmed by the transition from academics to clinical practice, leading to a task-oriented mindset and a common new nurse mistake ; this conflicts with critical thinking skills.
“Consider a patient whose blood pressure is low but who also needs to take a blood pressure medication at a scheduled time. A task-oriented nurse may provide the medication without regard for the patient’s blood pressure because medication administration is a task that must be completed,” Slaughter says. “A nurse employing critical thinking skills would address the low blood pressure, review the patient’s blood pressure history and trends, and potentially call the physician to discuss whether medication should be withheld.”
Fear and pride may also stand in the way of developing critical thinking skills. Your belief system and worldview provide comfort and guidance, but this can impede your judgment when you are faced with an individual whose belief system or cultural practices are not the same as yours. Fear or pride may prevent you from pursuing a line of questioning that would benefit the patient. Nurses with strong critical thinking skills exhibit:
- Learn from their mistakes and the mistakes of other nurses
- Look forward to integrating changes that improve patient care
- Treat each patient interaction as a part of a whole
- Evaluate new events based on past knowledge and adjust decision-making as needed
- Solve problems with their colleagues
- Are self-confident
- Acknowledge biases and seek to ensure these do not impact patient care
An Essential Skill for All Nurses
Critical thinking in nursing protects patient health and contributes to professional development and career advancement. Administrative and clinical nursing leaders are required to have strong critical thinking skills to be successful in their positions.
By using the strategies in this guide during your daily life and in your nursing role, you can intentionally improve your critical thinking abilities and be rewarded with better patient outcomes and potential career advancement.
Frequently Asked Questions About Critical Thinking in Nursing
How are critical thinking skills utilized in nursing practice.
Nursing practice utilizes critical thinking skills to provide the best care for patients. Often, the patient’s cause of pain or health issue is not immediately clear. Nursing professionals need to use their knowledge to determine what might be causing distress, collect vital information, and make quick decisions on how best to handle the situation.
How does nursing school develop critical thinking skills?
Nursing school gives students the knowledge professional nurses use to make important healthcare decisions for their patients. Students learn about diseases, anatomy, and physiology, and how to improve the patient’s overall well-being. Learners also participate in supervised clinical experiences, where they practice using their critical thinking skills to make decisions in professional settings.
Do only nurse managers use critical thinking?
Nurse managers certainly use critical thinking skills in their daily duties. But when working in a health setting, anyone giving care to patients uses their critical thinking skills. Everyone — including licensed practical nurses, registered nurses, and advanced nurse practitioners —needs to flex their critical thinking skills to make potentially life-saving decisions.
Meet Our Contributors

Crystal Slaughter, DNP, APRN, ACNS-BC, CNE
Crystal Slaughter is a core faculty member in Walden University’s RN-to-BSN program. She has worked as an advanced practice registered nurse with an intensivist/pulmonary service to provide care to hospitalized ICU patients and in inpatient palliative care. Slaughter’s clinical interests lie in nursing education and evidence-based practice initiatives to promote improving patient care.

Jenna Liphart Rhoads, Ph.D., RN
Jenna Liphart Rhoads is a nurse educator and freelance author and editor. She earned a BSN from Saint Francis Medical Center College of Nursing and an MS in nursing education from Northern Illinois University. Rhoads earned a Ph.D. in education with a concentration in nursing education from Capella University where she researched the moderation effects of emotional intelligence on the relationship of stress and GPA in military veteran nursing students. Her clinical background includes surgical-trauma adult critical care, interventional radiology procedures, and conscious sedation in adult and pediatric populations.

Nicholas McGowan, BSN, RN, CCRN
Nicholas McGowan is a critical care nurse with 10 years of experience in cardiovascular, surgical intensive care, and neurological trauma nursing. McGowan also has a background in education, leadership, and public speaking. He is an online learner who builds on his foundation of critical care nursing, which he uses directly at the bedside where he still practices. In addition, McGowan hosts an online course at Critical Care Academy where he helps nurses achieve critical care (CCRN) certification.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Front Med (Lausanne)
Rethinking clinical decision-making to improve clinical reasoning
Salvatore corrao.
1 Department of Internal Medicine, National Relevance and High Specialization Hospital Trust ARNAS Civico, Palermo, Italy
2 Dipartimento di Promozione della Salute Materno Infantile, Medicina Interna e Specialistica di Eccellenza “G. D’Alessandro” (PROMISE), University of Palermo, Palermo, Italy

Christiano Argano
Associated data.
The original contributions presented in this study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Improving clinical reasoning techniques is the right way to facilitate decision-making from prognostic, diagnostic, and therapeutic points of view. However, the process to do that is to fill knowledge gaps by studying and growing experience and knowing some cognitive aspects to raise the awareness of thinking mechanisms to avoid cognitive errors through correct educational training. This article examines clinical approaches and educational gaps in training medical students and young doctors. The authors explore the core elements of clinical reasoning, including metacognition, reasoning errors and cognitive biases, reasoning strategies, and ways to improve decision-making. The article addresses the dual-process theory of thought and the new Default Mode Network (DMN) theory. The reader may consider the article a first-level guide to deepen how to think and not what to think, knowing that this synthesis results from years of study and reasoning in clinical practice and educational settings.
Introduction
Clinical reasoning is based on complex and multifaceted cognitive processes, and the level of cognition is perhaps the most relevant factor that impacts the physician’s clinical reasoning. These topics have inspired considerable interest in the last years ( 1 , 2 ). According to Croskerry ( 3 ) and Croskerry and Norman ( 4 ), over 40 affective and cognitive biases may impact clinical reasoning. In addition, it should not be forgotten that both the processes and the subject matter are complex.
In medicine, there are thousands of known diagnoses, each with different complexity. Moreover, in line with Hammond’s view, a fundamental uncertainty will inevitably fail ( 5 ). Any mistake or failure in the diagnostic process leads to a delayed diagnosis, a misdiagnosis, or a missed diagnosis. The particular context in which a medical decision is made is highly relevant to the reasoning process and outcome ( 6 ).
More recently, there has been renewed interest in diagnostic reasoning, primarily diagnostic errors. Many researchers deepen inside the processes underpinning cognition, developing new universal reasoning and decision-making model: The Dual Process Theory.
This theory has a prompt implementation in medical decision-making and provides a comprehensive framework for understanding the gamma of theoretical approaches taken into consideration previously. This model has critical practical applications for medical decision-making and may be used as a model for teaching decision reasoning. Given this background, this manuscript must be considered a first-level guide to understanding how to think and not what to think, deepening clinical decision-making and providing tools for improving clinical reasoning.
Too much attention to the tip of the iceberg
The New England Journal of Medicine has recently published a fascinating article ( 7 ) in the “Perspective” section, whereon we must all reflect on it. The title is “At baseline” (the basic condition). Dr. Bergl, from the Department of Medicine of the Medical College of Wisconsin (Milwaukee), raised that his trainees no longer wonder about the underlying pathology but are focused solely on solving the acute problem. He wrote that, for many internal medicine teams, the question is not whether but to what extent we should juggle the treatment of critical health problems of patients with care for their coexisting chronic conditions. Doctors are under high pressure to discharge, and then they move patients to the next stage of treatment without questioning the reason that decompensated the clinical condition. Suppose the chronic condition or baseline was not the fundamental goal of our performance. In that case, our juggling is highly inconsistent because we are working on an intermediate outcome curing only the decompensation phase of a disease. Dr. Bergl raises another essential matter. Perhaps equally disturbing, by adopting a collective “base” mentality, we unintentionally create a group of doctors who prioritize productivity rather than developing critical skills and curiosity. We agree that empathy and patience are two other crucial elements in the training process of future internists. Nevertheless, how much do we stimulate all these qualities? Perhaps are not all part of cultural backgrounds necessary for a correct patient approach, the proper clinical reasoning, and balanced communication skills?
On the other hand, a chronic baseline condition is not always the real reason that justifies acute hospitalization. The lack of a careful approach to the baseline and clinical reasoning focused on the patient leads to this superficiality. We are focusing too much on our students’ practical skills and the amount of knowledge to learn. On the other hand, we do not teach how to think and the cognitive mechanisms of clinical reasoning.
Time to rethink the way of thinking and teaching courses
Back in 1910, John Dewey wrote in his book “How We Think” ( 8 ), “The aim of education should be to teach us rather how to think than what to think—rather improve our minds to enable us to think for ourselves than to load the memory with the thoughts of other men.”
Clinical reasoning concerns how to think and make the best decision-making process associated with the clinical practice ( 9 ). The core elements of clinical reasoning ( 10 ) can be summarized in:
- 1. Evidence-based skills,
- 2. Interpretation and use of diagnostic tests,
- 3. Understanding cognitive biases,
- 4. Human factors,
- 5. Metacognition (thinking about thinking), and
- 6. Patient-centered evidence-based medicine.
All these core elements are crucial for the best way of clinical reasoning. Each of them needs a correct learning path to be used in combination with developing the best thinking strategies ( Table 1 ). Reasoning strategies allow us to combine and synthesize diverse data into one or more diagnostic hypotheses, make the complex trade-off between the benefits and risks of tests and treatments, and formulate plans for patient management ( 10 ).
Set of some reasoning strategies (view the text for explanations).
However, among the abovementioned core element of clinical reasoning, two are often missing in the learning paths of students and trainees: metacognition and understanding cognitive biases.
Metacognition
We have to recall cognitive psychology, which investigates human thinking and describes how the human brain has two distinct mental processes that influence reasoning and decision-making. The first form of cognition is an ancient mechanism of thought shared with other animals where speed is more important than accuracy. In this case, thinking is characterized by a fast, intuitive way that uses pattern recognition and automated processes. The second one is a product of evolution, particularly in human beings, indicated by an analytical and hypothetical-deductive slow, controlled, but highly consuming way of thinking. Today, the psychology of thinking calls this idea “the dual-process theory of thought” ( 11 – 14 ). The Nobel Prize in Economic Sciences awardee Daniel Kahneman has extensively studied the dichotomy between the two modes of thought, calling them fast and slow thinking. “System 1” is fast, instinctive, and emotional; “System 2” is slower, more deliberative, and more logical ( 15 ). Different cerebral zones are involved: “System 1” includes the dorsomedial prefrontal cortex, the pregenual medial prefrontal cortex, and the ventromedial prefrontal cortex; “System 2” encompasses the dorsolateral prefrontal cortex. Glucose utilization is massive when System 2 is performing ( 16 ). System 1 is the leading way of thought used. None could live permanently in a deliberate, slow, effortful way. Driving a car, eating, and performing many activities over time become automatic and subconscious.
A recent brilliant review of Gronchi and Giovannelli ( 17 ) explores those things. Typically, when a mental effort is required for tasks requiring attention, every individual is subject to a phenomenon called “ego-depletion.” When forced to do something, each one has fewer cognitive resources available to activate slow thinking and thus is less able to exert self-control ( 18 , 19 ). In the same way, much clinical decision-making becomes intuitive rather than analytical, a phenomenon strongly affected by individual differences ( 20 , 21 ). Experimental evidence by functional magnetic resonance imaging and positron emission tomography studies supports that the “resting state” is spontaneously active during periods of “passivity” ( 22 – 25 ). The brain regions involved include the medial prefrontal cortex, the posterior cingulate cortex, the inferior parietal lobule, the lateral temporal cortex, the dorsal medial prefrontal cortex, and the hippocampal formation ( 26 ). Findings reporting high-metabolic activity in these regions at rest ( 27 ) constituted the first clear evidence of a cohesive default mode in the brain ( 28 ), leading to the widely acknowledged introduction of the Default Mode Network (DMN) concept. The DMN contains the medial prefrontal cortex, the posterior cingulate cortex, the inferior parietal lobule, the lateral temporal cortex, the dorsal medial prefrontal cortex, and the hippocampal formation. Lower activity levels characterize the DMN during goal-directed cognition and higher activity levels when an individual is awake and involved in the mental processes requiring low externally directed attention. All that is the neural basis of spontaneous cognition ( 26 ) that is responsible for thinking using internal representations. This paradigm is growing the idea of stimulus-independent thoughts (SITs), defined by Buckner et al. ( 26 ) as “thoughts about something other than events originating from the environment” that is covert and not directed toward the performance of a specific task. Very recently, the role of the DMN was highlighted in automatic behavior (the rapid selection of a response to a particular and predictable context) ( 29 ), as opposed to controlled decision making, suggesting that the DMN plays a role in the autopilot mode of brain functioning.
In light of these premises, everyone can pause to analyze what he is doing, improving self-control to avoid “ego-depletion.” Thus, one can actively switch between one type of thinking and the other. The ability to make this switch makes the physician more performing. In addition, a physician can be trained to understand the ways of thinking and which type of thinking is engaged in various situations. This way, experience and methodology knowledge can energize Systems 1 and 2 and how they interact, avoiding cognitive errors. Figure 1 summarizes all the concepts abovementioned about the Dual Mode Network and its relationship with the DMN.

Graphical representation of the characteristics of Dual Mode Network, including the relationship between the two systems by Default Mode Network (view the text for explanations).
Emotional intelligence is another crucial factor in boosting clinical reasoning for the best decision-making applied to a single patient. Emotional intelligence recognizes one’s emotions. Those others label different feelings appropriately and use emotional information to guide thinking and behavior, adjust emotions, and create empathy, adapt to environments, and achieve goals ( 30 ). According to the phenomenological account of Fuchs, bodily perception (proprioception) has a crucial role in understanding others ( 31 ). In this sense, the proprioceptive skills of a physician can help his empathic understanding become elementary for empathy and communication with the patient. In line with Fuchs’ view, empathic understanding encompasses a bodily resonance and mediates contextual knowledge about the patient. For medical education, empathy should help to relativize the singular experience, helping to prevent that own position becomes exclusive, bringing oneself out of the center of one’s own perspective.
Reasoning errors and cognitive biases
Errors in reasoning play a significant role in diagnostic errors and may compromise patient safety and quality of care. A recently published review by Norman et al. ( 32 ) examined clinical reasoning errors and how to avoid them. To simplify this complex issue, almost five types of diagnostic errors can be recognized: no-fault errors, system errors, errors due to the knowledge gap, errors due to misinterpretation, and cognitive biases ( 9 ). Apart from the first type of error, which is due to unavoidable errors due to various factors, we want to mention cognitive biases. They may occur at any stage of the reasoning process and may be linked to intuition and analytical systems. The most frequent cognitive biases in medicine are anchoring, confirmation bias, premature closure, search satisficing, posterior probability error, outcome bias, and commission bias ( 33 ). Anchoring is characterized by latching onto a particular aspect at the initial consultation, and then one refuses to change one’s mind about the importance of the later stages of reasoning. Confirmation bias ignores the evidence against an initial diagnosis. Premature closure leads to a misleading diagnosis by stopping the diagnostic process before all the information has been gathered or verified. Search satisficing blinds other additional diagnoses once the first diagnosis is made posterior probability error shortcuts to the usual patient diagnosis for previously recognized clinical presentations. Outcome bias impinges on our desire for a particular outcome that alters our judgment (e.g., a surgeon blaming sepsis on pneumonia rather than an anastomotic leak). Finally, commission bias is the tendency toward action rather than inaction, assuming that only good can come from doing something (rather than “watching and waiting”). These biases are only representative of the other types, and biases often work together. For example, in overconfidence bias (the tendency to believe we know more than we do), too much faith is placed in opinion instead of gathered evidence. This bias can be augmented by the anchoring effect or availability bias (when things are at the forefront of your mind because you have seen several cases recently or have been studying that condition in particular), and finally by commission bias—with disastrous results.
Novice vs. expert approaches
The reasoning strategies used by novices are different from those used by experts ( 34 ). Experts can usually gather beneficial information with highly effective problem-solving strategies. Heuristics are commonly, and most often successfully, used. The expert has a saved bank of illness scripts to compare and contrast the current case using more often type 1 thinking with much better results than the novice. Novices have little experience with their problems, do not have time to build a bank of illness scripts, and have no memories of previous similar cases and actions in such cases. Therefore, their mind search strategies will be weak, slow, and ponderous. Heuristics are poor and more often unsuccessful. They will consider a more comprehensive range of diagnostic possibilities and take longer to select approaches to discriminate among them. A novice needs specific knowledge and specific experience to become an expert. In our opinion, he also needs special training in the different ways of thinking. It is possible to study patterns, per se as well. It is, therefore, likely to guide the growth of knowledge for both fast thinking and slow one.
Moreover, learning by osmosis has traditionally been the method to move the novice toward expert capabilities by gradually gaining experience while observing experts’ reasoning. However, it seems likely that explicit teaching of clinical reasoning could make this process quicker and more effective. In this sense, an increased need for training and clinical knowledge along with the skill to apply the acquired knowledge is necessary. Students should learn disease pathophysiology, treatment concepts, and interdisciplinary team communication developing clinical decision-making through case-series-derived knowledge combining associative and procedural learning processes such as “Vienna Summer School on Oncology” ( 35 ).
Moreover, a refinement of the training of communicative skills is needed. Improving communication skills training for medical students and physicians should be the university’s primary goal. In fact, adequate communication leads to a correct diagnosis with 76% accuracy ( 36 ). The main challenge for students and physicians is the ability to respond to patients’ individual needs in an empathic and appreciated way. In this regard, it should be helpful to apply qualitative studies through the adoption of a semi-structured or structured interview using face-to-face in-depth interviews and e-learning platforms which can foster interdisciplinary learning by developing expertise for the clinical reasoning and decision-making in each area and integrating them. They could be effective tools to develop clinical reasoning and decision-making competencies and acquire effective communication skills to manage the relationship with patient ( 37 – 40 ).
Clinical reasoning ways
Clinical reasoning is complex: it often requires different mental processes operating simultaneously during the same clinical encounter and other procedures for different situations. The dual-process theory describes how humans have two distinct approaches to decision-making ( 41 ). When one uses heuristics, fast-thinking (system 1) is used ( 42 ). However, complex cases need slow analytical thinking or both systems involved ( 15 , 43 , 44 ). Slow thinking can use different ways of reasoning: deductive, hypothetic-deductive, inductive, abductive, probabilistic, rule-based/categorical/deterministic, and causal reasoning ( 9 ). We think that abductive and causal reasoning need further explanation. Abductive reasoning is necessary when no deductive argument (from general assumption to particular conclusion) nor inductive (the opposite of deduction) may be claimed.
In the real world, we often face a situation where we have information and move backward to the likely cause. We ask ourselves, what is the most plausible answer? What theory best explains this information? Abduction is just a process of choosing the hypothesis that would best explain the available evidence. On the other hand, causal reasoning uses knowledge of medical sciences to provide additional diagnostic information. For example, in a patient with dyspnea, if considering heart failure as a casual diagnosis, a raised BNP would be expected, and a dilated vena cava yet. Other diagnostic possibilities must be considered in the absence of these confirmatory findings (e.g., pneumonia). Causal reasoning does not produce hypotheses but is typically used to confirm or refute theories generated using other reasoning strategies.
Hypothesis generation and modification using deduction, induction/abduction, rule-based, causal reasoning, or mental shortcuts (heuristics and rule of thumbs) is the cognitive process for making a diagnosis ( 9 ). Clinicians develop a hypothesis, which may be specific or general, relating a particular situation to knowledge and experience. This process is referred to as generating a differential diagnosis. The process we use to produce a differential diagnosis from memory is unclear. The hypotheses chosen may be based on likelihood but might also reflect the need to rule out the worst-case scenario, even if the probability should always be considered.
Given the complexity of the involved process, there are numerous causes for failure in clinical reasoning. These can occur in any reasoning and at any stage in the process ( 33 ). We must be aware of subconscious errors in our thinking processes. Cognitive biases are subconscious deviations in judgment leading to perceptual distortion, inaccurate assessment, and misleading interpretation. From an evolutionary point of view, they have developed because, often, speed is more important than accuracy. Biases occur due to information processing heuristics, the brain’s limited capacity to process information, social influence, and emotional and moral motivations.
Heuristics are mind shortcuts and are not all bad. They refer to experience-based techniques for decision-making. Sometimes they may lead to cognitive biases (see above). They are also essential for mental processes, expressed by expert intuition that plays a vital role in clinical practice. Intuition is a heuristic that derives from a natural and direct outgrowth of experiences that are unconsciously linked to form patterns. Pattern recognition is just a quick shortcut commonly used by experts. Alternatively, we can create patterns by studying differently and adequately in a notional way that accumulates information. The heuristic that rules out the worst-case scenario is a forcing mind function that commits the clinician to consider the worst possible illness that might explain a particular clinical presentation and take steps to ensure it has been effectively excluded. The heuristic that considers the least probable diagnoses is a helpful approach to uncommon clinical pictures and thinking about and searching for a rare unrecognized condition. Clinical guidelines, scores, and decision rules function as externally constructed heuristics, usually to ensure the best evidence for the diagnosis and treatment of patients.
Hence, heuristics are helpful mind shortcuts, but the exact mechanisms may lead to errors. Fast-and-frugal tree and take-the-best heuristic are two formal models for deciding on the uncertainty domain ( 45 ).
In the recent times, clinicians have faced dramatic changes in the pattern of patients acutely admitted to hospital wards. Patients become older and older with comorbidities, rare diseases are frequent as a whole ( 46 ), new technologies are growing in a logarithmic way, and sustainability of the healthcare system is an increasingly important problem. In addition, uncommon clinical pictures represent a challenge for clinicians ( 47 – 50 ). In our opinion, it is time to claim clinical reasoning as a crucial way to deal with all complex matters. At first, we must ask ourselves if we have lost the teachings of ancient masters. Second, we have to rethink medical school courses and training ones. In this way, cognitive debiasing is needed to become a well-calibrated clinician. Fundamental tools are the comprehensive knowledge of nature and the extent of biases other than studying cognitive processes, including the interaction between fast and slow thinking. Cognitive debiasing requires the development of good mindware and the awareness that one debiasing strategy will not work for all biases. Finally, debiasing is generally a complicated process and requires lifelong maintenance.
We must remember that medicine is an art that operates in the field of science and must be able to cope with uncertainty. Managing uncertainty is the skill we have to develop against an excess of confidence that can lead to error. Sound clinical reasoning is directly linked to patient safety and quality of care.
Data availability statement
Author contributions.
SC and CA drafted the work and revised it critically. Both authors have approved the submission of the manuscript.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Fastest Nurse Insight Engine
- MEDICAL ASSISSTANT
- Abdominal Key
- Anesthesia Key
- Basicmedical Key
- Otolaryngology & Ophthalmology
- Musculoskeletal Key
- Obstetric, Gynecology and Pediatric
- Oncology & Hematology
- Plastic Surgery & Dermatology
- Clinical Dentistry
- Radiology Key
- Thoracic Key
- Veterinary Medicine
- Gold Membership
Critical Thinking in Nursing Practice
Chapter 15 Critical Thinking in Nursing Practice Objectives • Describe characteristics of a critical thinker. • Discuss the nurse’s responsibility in making clinical decisions. • Discuss how reflection improves clinical decision making. • Describe the components of a critical thinking model for clinical decision making. • Discuss critical thinking skills used in nursing practice. • Explain the relationship between clinical experience and critical thinking. • Discuss the critical thinking attitudes used in clinical decision making. • Explain how professional standards influence a nurse’s clinical decisions. • Discuss the relationship of the nursing process to critical thinking. Key Terms Clinical decision making, p. 196 Concept map, p. 202 Critical thinking, p. 193 Decision making, p. 195 Diagnostic reasoning, p. 196 Evidence-based knowledge, p. 193 Inference, p. 196 Nursing process, p. 197 Problem solving, p. 195 Reflection, p. 202 Scientific method, p. 195 http://evolve.elsevier.com/Potter/fundamentals/ • Review Questions • Case Study with Questions • Audio Glossary • Interactive Learning Activities • Key Term Flashcards • Content Updates Every day you think critically without realizing it. If it’s hot outside, you take off a sweater. If your DVD doesn’t start, you reposition the disc. If you decide to walk the dogs, you change to a pair of walking shoes. These examples involve critical thinking as you face each day and prepare for all possibilities. As a nurse, you will face many clinical situations involving patients, family members, health care staff, and peers. In each situation it is important to try to see the big picture and think smart. To think smart you have to develop critical thinking skills to face each new experience and problem involving a patient’s care with open-mindedness, creativity, confidence, and continual inquiry. When a patient develops a new set of symptoms, asks you to offer comfort, or requires a procedure, it is important to think critically and make sensible judgments so the patient receives the best nursing care possible. Critical thinking is not a simple step-by-step, linear process that you learn overnight. It is a process acquired only through experience, commitment, and an active curiosity toward learning. Clinical Decisions in Nursing Practice Nurses are responsible for making accurate and appropriate clinical decisions. Clinical decision making separates professional nurses from technical personnel. For example, a professional nurse observes for changes in patients, recognizes potential problems, identifies new problems as they arise, and takes immediate action when a patient’s clinical condition worsens. Technical personnel simply follow direction in completing aspects of care that the professional nurse has identified as necessary. A professional nurse relies on knowledge and experience when deciding if a patient is having complications that call for notification of a health care provider or decides if a teaching plan for a patient is ineffective and needs revision. Benner (1984) describes clinical decision making as judgment that includes critical and reflective thinking and action and application of scientific and practical logic. Most patients have health care problems for which there are no clear textbook solutions. Each patient’s problems are unique, a product of the patient’s physical health, lifestyle, culture, relationship with family and friends, living environment, and experiences. Thus as a nurse you do not always have a clear picture of a patient’s needs and the appropriate actions to take when first meeting a patient. Instead you must learn to question, wonder, and explore different perspectives and interpretations to find a solution that benefits the patient. Because no two patients’ health problems are the same, you always apply critical thinking differently. Observe patients closely, gather information about them, examine ideas and inferences about patient problems, recognize the problems, consider scientific principles relating to the problems, and develop an approach to nursing care. With experience you learn to creatively seek new knowledge, act quickly when events change, and make quality decisions for patients’ well-being. You will find nursing to be rewarding and fulfilling through the clinical decisions you make. Critical Thinking Defined Mr. Jacobs is a 58-year-old patient who had a radical prostatectomy for prostate cancer yesterday. His nurse, Tonya, finds the patient lying supine in bed with arms extended along his sides but tensed. When Tonya checks the patient’s surgical wound and drainage device, she notes that the patient winces when she gently places her hands to palpate around the surgical incision. She asks Mr. Jacobs when he last turned onto his side, and he responds, “Not since last night some time.” Tonya asks Mr. Jacobs if he is having incisional pain, and he nods yes, saying, “It hurts too much to move.” Tonya considers the information she has observed and learned from the patient to determine that he is in pain and has reduced mobility because of it. She decides that she needs to take action to relieve Mr. Jacobs’ pain so she can turn him more frequently and begin to get him out of bed for his recovery. In the case example the nurse observes the clinical situation, asks questions, considers what she knows about postoperative pain and risk for immobility, and takes action. The nurse applies critical thinking, a continuous process characterized by open-mindedness, continual inquiry, and perseverance, combined with a willingness to look at each unique patient situation and determine which identified assumptions are true and relevant ( Heffner and Rudy, 2008 ). Critical thinking involves recognizing that an issue (e.g., patient problem) exists, analyzing information about the issue (e.g., clinical data about a patient), evaluating information (reviewing assumptions and evidence) and making conclusions ( Settersten and Lauver, 2004 ). A critical thinker considers what is important in each clinical situation, imagines and explores alternatives, considers ethical principles, and makes informed decisions about the care of patients. Critical thinking is a way of thinking about a situation that always asks “Why?”, “What am I missing?”, “What do I really know about this patient’s situation?”, and “What are my options?” ( Heffner and Rudy, 2008 ; Paul and Heaslip, 1995 ). Tonya knew that pain was likely going to be a problem because the patient had extensive surgery. Her review of her observations and the patient’s report of pain confirmed her knowledge that pain was a problem. Her options include giving Mr. Jacobs an analgesic and waiting until it takes effect so she is able to reposition and make him more comfortable. Once he has less acute pain, Tonya offers to teach Mr. Jacobs some relaxation exercises. You begin to learn critical thinking early in your practice. For example, as you learn about administering baths and other hygiene measures, take time to read your textbook and the nursing literature about the concept of comfort. What are the criteria for comfort? How do patients from other cultures perceive comfort? What are the many factors that promote comfort? The use of evidence-based knowledge, or knowledge based on research or clinical expertise, makes you an informed critical thinker. Thinking critically and learning about the concept of comfort prepares you to better anticipate your patients’ needs, identify comfort problems more quickly, and offer appropriate care. Critical thinking requires cognitive skills and the habit of asking questions, remaining well informed, being honest in facing personal biases, and always being willing to reconsider and think clearly about issues ( Facione, 1990 ). When core critical thinking skills are applied to nursing, they show the complex nature of clinical decision making ( Table 15-1 ). Being able to apply all of these skills takes practice. You also need to have a sound knowledge base and thoughtfully consider what you learn when caring for patients. TABLE 15-1 Critical Thinking Skills SKILL NURSING PRACTICE APPLICATIONS Interpretation Be orderly in data collection. Look for patterns to categorize data (e.g., nursing diagnoses [see Chapter 17 ]). Clarify any data you are uncertain about. Analysis Be open-minded as you look at information about a patient. Do not make careless assumptions. Do the data reveal what you believe is true, or are there other options? Inference Look at the meaning and significance of findings. Are there relationships between findings? Do the data about the patient help you see that a problem exists? Evaluation Look at all situations objectively. Use criteria (e.g., expected outcomes, pain characteristics, learning objectives) to determine results of nursing actions. Reflect on your own behavior. Explanation Support your findings and conclusions. Use knowledge and experience to choose strategies to use in the care of patients. Self-regulation Reflect on your experiences. Identify the ways you can improve your own performance. What will make you believe that you have been successful? Modified from Facione P: Critical thinking: a statement of expert consensus for purposes of educational assessment and instruction. The Delphi report: research findings and recommendations prepared for the American Philosophical Association, ERIC Doc No. ED 315, Washington, DC, 1990, ERIC. Nurses who apply critical thinking in their work are able to see the big picture from all possible perspectives. They focus clearly on options for solving problems and making decisions rather than quickly and carelessly forming quick solutions ( Kataoka-Yahiro and Saylor, 1994 ). Nurses who work in crisis situations such as the emergency department often act quickly when patient problems develop. However, even these nurses exercise discipline in decision making to avoid premature and inappropriate decisions. Learning to think critically helps you care for patients as their advocate, or supporter, and make better-informed choices about their care. Facione and Facione (1996) identified concepts for thinking critically ( Table 15-2 ). Critical thinking is more than just problem solving. It is a continuous attempt to improve how to apply yourself when faced with problems in patient care. TABLE 15-2 Concepts for a Critical Thinker CONCEPT CRITICAL THINKING BEHAVIOR Truth seeking Seek the true meaning of a situation. Be courageous, honest, and objective about asking questions. Open-mindedness Be tolerant of different views; be sensitive to the possibility of your own prejudices; respect the right of others to have different opinions. Analyticity Analyze potentially problematic situations; anticipate possible results or consequences; value reason; use evidence-based knowledge. Systematicity Be organized, focused; work hard in any inquiry. Self-confidence Trust in your own reasoning processes. Inquisitiveness Be eager to acquire knowledge and learn explanations even when applications of the knowledge are not immediately clear. Value learning for learning’s sake. Maturity Multiple solutions are acceptable. Reflect on your own judgments; have cognitive maturity. Modified from Facione N, Facione P: Externalizing the critical thinking in knowledge development and clinical judgment, Nurs Outlook 44(3):129, 1996. Thinking and Learning Learning is a lifelong process. Your intellectual and emotional growth involves learning new knowledge and refining your ability to think, problem solve, and make judgments. To learn, you have to be flexible and always open to new information. The science of nursing is growing rapidly, and there will always be new information for you to apply in practice. As you have more clinical experiences and apply the knowledge you learn, you will become better at forming assumptions, presenting ideas, and making valid conclusions. When you care for a patient, always think ahead and ask these questions: What is the patient’s status now? How might it change and why? Which physiological and emotional responses do I anticipate? What do I know to improve the patient’s condition? In which way will specific therapies affect the patient? What should be my first action? Do not let your thinking become routine or standardized. Instead, learn to look beyond the obvious in any clinical situation, explore the patient’s unique responses to health alterations, and recognize which actions are needed to benefit the patient. With experience you are able to recognize patterns of behavior, see commonalities in signs and symptoms, and anticipate reactions to therapies. Thinking about these experiences allows you to better anticipate each new patient’s needs and recognize problems when they develop. Levels of Critical Thinking in Nursing Your ability to think critically grows as you gain new knowledge in nursing practice. Kataoka-Yahiro and Saylor (1994) developed a critical thinking model ( Fig. 15-1 ) that includes three levels: basic, complex, and commitment. An expert nurse thinks critically almost automatically. As a beginning student you make a more conscious effort to apply critical thinking because initially you are more task oriented and trying to learn how to organize nursing care activities. At first you apply the critical thinking model at the basic level. As you advance in practice, you adopt complex critical thinking and commitment. FIG. 15-1 Critical thinking model for nursing judgment. (Redrawn from Kataoka-Yahiro M, Saylor C: A critical thinking model for nursing judgment, J Nurs Educ 33(8):351, 1994. Modified from Glaser E: An experiment in the development of critical thinking, New York, 1941, Bureau of Publications, Teachers College, Columbia University; Miller M, Malcolm N: Critical thinking in the nursing curriculum, Nurs Health Care 11:67, 1990; Paul RW: The art of redesigning instruction. In Willsen J, Blinker AJA, editors: Critical thinking: how to prepare students for a rapidly changing world, Santa Rosa, Calif, 1993, Foundation for Critical Thinking; and Perry W: Forms of intellectual and ethical development in the college years: a scheme , New York, 1979, Holt, Rinehart, & Winston.) Basic Critical Thinking At the basic level of critical thinking a learner trusts that experts have the right answers for every problem. Thinking is concrete and based on a set of rules or principles. For example, as a nursing student you use a hospital procedure manual to confirm how to insert a Foley catheter. You likely follow the procedure step by step without adjusting it to meet a patient’s unique needs (e.g., positioning to minimize the patient’s pain or mobility restrictions). You do not have enough experience to anticipate how to individualize the procedure. At this level answers to complex problems are either right or wrong (e.g., when no urine drains from the catheter, the catheter tip must not be in the bladder), and one right answer usually exists for each problem. Basic critical thinking is an early step in developing reasoning ( Kataoka-Yahiro and Saylor, 1994 ). A basic critical thinker learns to accept the diverse opinions and values of experts (e.g., instructors and staff nurse role models). However, inexperience, weak competencies, and inflexible attitudes can restrict a person’s ability to move to the next level of critical thinking. Complex Critical Thinking Complex critical thinkers begin to separate themselves from experts. They analyze and examine choices more independently. The person’s thinking abilities and initiative to look beyond expert opinion begin to change. A nurse learns that alternative and perhaps conflicting solutions exist. Consider the case of Mr. Rosen, a 36-year-old man who had hip surgery. The patient is having pain but is refusing his ordered analgesic. His health care provider is concerned that the patient will not progress as planned, delaying rehabilitation. While discussing the importance of rehabilitation with Mr. Rosen, the nurse, Edwin, realizes the patient’s reason for not taking pain medication. Edwin learns that the patient practices meditation at home. As a complex critical thinker, Edwin recognizes that Mr. Rosen has options for pain relief. Edwin decides to discuss meditation and other nonpharmacological interventions with the patient as pain control options and how, when combined with analgesics, these interventions can potentially enhance pain relief. In complex critical thinking each solution has benefits and risks that you weigh before making a final decision. There are options. Thinking becomes more creative and innovative. The complex critical thinker is willing to consider different options from routine procedures when complex situations develop. You learn a variety of different approaches for the same therapy. Commitment The third level of critical thinking is commitment ( Kataoka-Yahiro and Saylor, 1994 ). At this level a person anticipates when to make choices without assistance from others and accepts accountability for decisions made. As a nurse you do more than just consider the complex alternatives that a problem poses. At the commitment level you choose an action or belief based on the available alternatives and support it. Sometimes an action is to not act or to delay an action until a later time. You choose to delay as a result of your experience and knowledge. Because you take accountability for the decision, you consider the results of the decision and determine whether it was appropriate. Critical Thinking Competencies Kataoka-Yahiro and Saylor (1994) describe critical thinking competencies as the cognitive processes a nurse uses to make judgments about the clinical care of patients. These include general critical thinking, specific critical thinking in clinical situations, and specific critical thinking in nursing. General critical thinking processes are not unique to nursing. They include the scientific method, problem solving, and decision making. Specific critical thinking competencies in clinical health care situations include diagnostic reasoning, clinical inference, and clinical decision making. The specific critical thinking competency in nursing involves use of the nursing process. Each of the competencies is discussed in the following paragraphs. General Critical Thinking Scientific Method The scientific method is a way to solve problems using reasoning. It is a systematic, ordered approach to gathering data and solving problems used by nurses, physicians, and a variety of other health care professionals. This approach looks for the truth or verifies that a set of facts agrees with reality. Nurse researchers use the scientific method when testing research questions in nursing practice situations (see Chapter 5 ). The scientific method has five steps: 1 Identifying the problem 2 Collecting data 3 Formulating a question or hypothesis 4 Testing the question or hypothesis 5 Evaluating results of the test or study Consider the following example of the scientific method in nursing practice. A nurse caring for patients who receive large doses of chemotherapy for ovarian cancer sees a pattern of patients developing severe inflammation in the mouth (mucositis) (identifies problem). The nurse reads research articles (collects data) about mucositis and learns that there is evidence to show that having patients keep ice in their mouths (cryotherapy) during the chemotherapy infusion reduces severity of mucositis after treatment. He or she asks (forms question), “Do patients with ovarian cancer who receive chemotherapy have less severe mucositis when given cryotherapy versus standard mouth rinse in the oral cavity?” The nurse then collaborates with colleagues to develop a nursing protocol for using ice with certain chemotherapy infusions. The nurses on the oncology unit collect information that allows them to compare the incidence and severity of mucositis for a group of patients who use cryotherapy versus those who use standard-practice mouth rinse (tests the question). They analyze the results of their project and find that the use of cryotherapy reduced the frequency and severity of mucositis in their patients (evaluating the results). They decide to continue the protocol for all patients with ovarian cancer. Problem Solving You face problems every day such as a computer program that doesn’t function properly or a close friend who has lost a favorite pet. When a problem arises, you obtain information and use it, plus what you already know, to find a solution. Patients routinely present problems in practice. For example, a home care nurse learns that a patient has difficulty taking her medications regularly. The patient is unable to describe what medications she has taken for the last 3 days. The medication bottles are labeled and filled. The nurse has to solve the problem of why the patient is not adhering to or following her medication schedule. The nurse knows that the patient was discharged from the hospital and had five medications ordered. The patient tells the nurse that she also takes two over-the-counter medications regularly. When the nurse asks her to show the medications that she takes in the morning, the nurse notices that she has difficulty reading the medication labels. The patient is able to describe the medications that she is to take but is uncertain about the times of administration. The nurse recommends having the patient’s pharmacy relabel the medications in larger lettering. In addition, the nurse shows the patient examples of pill organizers that will help her sort her medications by time of day for a period of 7 days. Effective problem solving also involves evaluating the solution over time to make sure that it is effective. It becomes necessary to try different options if a problem recurs. From the previous example, during a follow-up visit the nurse finds that the patient has organized her medications correctly and is able to read the labels without difficulty. The nurse obtained information that correctly clarified the cause of the patient’s problem and tested a solution that proved successful. Having solved a problem in one situation adds to a nurse’s experience in practice, and this allows the nurse to apply that knowledge in future patient situations. Decision Making When you face a problem or situation and need to choose a course of action from several options, you are making a decision. Decision making is a product of critical thinking that focuses on problem resolution. Following a set of criteria helps to make a thorough and thoughtful decision. The criteria may be personal; based on an organizational policy; or, frequently in the case of nursing, a professional standard. For example, decision making occurs when a person decides on the choice of a health care provider. To make a decision, an individual has to recognize and define the problem or situation (need for a certain type of health care provider to provide medical care) and assess all options (consider recommended health care providers or choose one whose office is close to home). The person has to weigh each option against a set of personal criteria (experience, friendliness, and reputation), test possible options (talk directly with the different health care providers), consider the consequences of the decision (examine pros and cons of selecting one health care provider over another), and make a final decision. Although the set of criteria follows a sequence of steps, decision making involves moving back and forth when considering all criteria. It leads to informed conclusions that are supported by evidence and reason. Examples of decision making in the clinical area include determining which patient care priority requires the first response, choosing a type of dressing for a patient with a surgical wound, or selecting the best teaching approach for a family caregiver who will assist a patient who is returning home after a stroke. Specific Critical Thinking Diagnostic Reasoning and Inference Once you receive information about a patient in a clinical situation, diagnostic reasoning begins. It is the analytical process for determining a patient’s health problems ( Harjai and Tiwari, 2009 ). Accurate recognition of a patient’s problems is necessary before you decide on solutions and implement action. It requires you to assign meaning to the behaviors and physical signs and symptoms presented by a patient. Diagnostic reasoning begins when you interact with a patient or make physical or behavioral observations. An expert nurse sees the context of a patient situation (e.g., a patient who is feeling light-headed with blurred vision and who has a history of diabetes is possibly experiencing a problem with blood glucose levels), observes patterns and themes (e.g., symptoms that include weakness, hunger, and visual disturbances suggest hypoglycemia), and makes decisions quickly (e.g., offers a food source containing glucose). The information a nurse collects and analyzes leads to a diagnosis of a patient’s condition. Nurses do not make medical diagnoses, but they do assess and monitor patients closely and compare the patients’ signs and symptoms with those that are common to a medical diagnosis. This type of diagnostic reasoning helps health care providers pinpoint the nature of a problem more quickly and select proper therapies. Part of diagnostic reasoning is clinical inference, the process of drawing conclusions from related pieces of evidence and previous experience with the evidence. An inference involves forming patterns of information from data before making a diagnosis. Seeing that a patient has lost appetite and experienced weight loss over the last month, the nurse infers that there is a nutritional problem. An example of diagnostic reasoning is forming a nursing diagnosis such as imbalanced nutrition: less than body requirements (see Chapter 17 ). In diagnostic reasoning use patient data that you gather or collect to logically recognize the problem. For example, after turning a patient you see an area of redness on the right hip. You palpate the area and note that it is warm to the touch and the patient complains of tenderness. You press over the area with your finger; after you release pressure, the area does not blanch or turn white. After thinking about what you know about normal skin integrity and the effects of pressure, you form the diagnostic conclusion that the patient has a pressure ulcer. As a student, confirm your judgments with experienced nurses. At times you possibly will be wrong, but consulting with nurse experts gives you feedback to build on future clinical situations. Often you cannot make a precise diagnosis during your first meeting with a patient. Sometimes you sense that a problem exists but do not have enough data to make a specific diagnosis. Some patients’ physical conditions limit their ability to tell you about symptoms. Some choose to not share sensitive and important information during your initial assessment. Some patients’ behaviors and physical responses become observable only under conditions not present during your initial assessment. When uncertain of a diagnosis, continue data collection. You have to critically analyze changing clinical situations until you are able to determine the patient’s unique situation. Diagnostic reasoning is a continuous behavior in nursing practice. Any diagnostic conclusions that you make will help the health care provider identify the nature of a problem more quickly and select appropriate medical therapies. Clinical Decision Making As in the case of general decision making, clinical decision making is a problem-solving activity that focuses on defining a problem and selecting an appropriate action. In clinical decision making a nurse identifies a patient’s problem and selects a nursing intervention. When you approach a clinical problem such as a patient who is less mobile and develops an area of redness over the hip, you make a decision that identifies the problem (impaired skin integrity in the form of a pressure ulcer) and choose the best nursing interventions (skin care and a turning schedule). Nurses make clinical decisions all the time to improve a patient’s health or maintain wellness. This means reducing the severity of the problem or resolving the problem completely. Clinical decision making requires careful reasoning (i.e., choosing the options for the best patient outcomes on the basis of the patient’s condition and the priority of the problem). Improve your clinical decision making by knowing your patients. Nurse researchers found that expert nurses develop a level of knowing that leads to pattern recognition of patient symptoms and responses ( White, 2003 ). For example, an expert nurse who has worked on a general surgery unit for many years is more likely able to detect signs of internal hemorrhage (e.g., fall in blood pressure, rapid pulse, change in consciousness) than a new nurse. Over time a combination of experience, time spent in a specific clinical area, and the quality of relationships formed with patients allow expert nurses to know clinical situations and quickly anticipate and select the right course of action. Spending more time during initial patient assessments to observe patient behavior and measure physical findings is a way to improve knowledge of your patients. In addition, consistently assessing and monitoring patients as problems occur help you to see how clinical changes develop over time. The selection of nursing therapies is built on both clinical knowledge and specific patient data, including: • The identified status and situation you assessed about the patient, including data collected by actively listening to the patient regarding his or her health care needs. • Knowledge about the clinical variables (e.g., age, seriousness of the problem, pathology of the problem, patient’s preexisting disease conditions) involved in the situation, and how the variables are linked together. • A judgment about the likely course of events and outcome of the diagnosed problem, considering any health risks the patient has; includes knowledge about usual patterns of any diagnosed problem or prognosis. • Any additional relevant data about requirements in the patient’s daily living, functional capacity, and social resources. • Knowledge about the nursing therapy options available and the way in which specific interventions will predictably affect the patient’s situation.
Share this:
- Click to share on Twitter (Opens in new window)
- Click to share on Facebook (Opens in new window)
Related posts:
- Legal Implications in Nursing Practice
- Documentation and Informatics
- Care of Surgical Patients
- Stress and Coping
Stay updated, free articles. Join our Telegram channel
Comments are closed for this page.

Full access? Get Clinical Tree

You are using an outdated browser
Unfortunately Ausmed.com does not support your browser. Please upgrade your browser to continue.
Cultivating Critical Thinking in Healthcare
Published: 06 January 2019

Critical thinking skills have been linked to improved patient outcomes, better quality patient care and improved safety outcomes in healthcare (Jacob et al. 2017).
Given this, it's necessary for educators in healthcare to stimulate and lead further dialogue about how these skills are taught , assessed and integrated into the design and development of staff and nurse education and training programs (Papp et al. 2014).
So, what exactly is critical thinking and how can healthcare educators cultivate it amongst their staff?
What is Critical Thinking?
In general terms, ‘ critical thinking ’ is often used, and perhaps confused, with problem-solving and clinical decision-making skills .
In practice, however, problem-solving tends to focus on the identification and resolution of a problem, whilst critical thinking goes beyond this to incorporate asking skilled questions and critiquing solutions .
Several formal definitions of critical thinking can be found in literature, but in the view of Kahlke and Eva (2018), most of these definitions have limitations. That said, Papp et al. (2014) offer a useful starting point, suggesting that critical thinking is:
‘The ability to apply higher order cognitive skills and the disposition to be deliberate about thinking that leads to action that is logical and appropriate.’
The Foundation for Critical Thinking (2017) expands on this and suggests that:
‘Critical thinking is that mode of thinking, about any subject, content, or problem, in which the thinker improves the quality of his or her thinking by skillfully analysing, assessing, and reconstructing it.’
They go on to suggest that critical thinking is:
- Self-directed
- Self-disciplined
- Self-monitored
- Self-corrective.

Key Qualities and Characteristics of a Critical Thinker
Given that critical thinking is a process that encompasses conceptualisation , application , analysis , synthesis , evaluation and reflection , what qualities should be expected from a critical thinker?
In answering this question, Fortepiani (2018) suggests that critical thinkers should be able to:
- Formulate clear and precise questions
- Gather, assess and interpret relevant information
- Reach relevant well-reasoned conclusions and solutions
- Think open-mindedly, recognising their own assumptions
- Communicate effectively with others on solutions to complex problems.
All of these qualities are important, however, good communication skills are generally considered to be the bedrock of critical thinking. Why? Because they help to create a dialogue that invites questions, reflections and an open-minded approach, as well as generating a positive learning environment needed to support all forms of communication.
Lippincott Solutions (2018) outlines a broad spectrum of characteristics attributed to strong critical thinkers. They include:
- Inquisitiveness with regard to a wide range of issues
- A concern to become and remain well-informed
- Alertness to opportunities to use critical thinking
- Self-confidence in one’s own abilities to reason
- Open mindedness regarding divergent world views
- Flexibility in considering alternatives and opinions
- Understanding the opinions of other people
- Fair-mindedness in appraising reasoning
- Honesty in facing one’s own biases, prejudices, stereotypes or egocentric tendencies
- A willingness to reconsider and revise views where honest reflection suggests that change is warranted.
Papp et al. (2014) also helpfully suggest that the following five milestones can be used as a guide to help develop competency in critical thinking:
Stage 1: Unreflective Thinker
At this stage, the unreflective thinker can’t examine their own actions and cognitive processes and is unaware of different approaches to thinking.
Stage 2: Beginning Critical Thinker
Here, the learner begins to think critically and starts to recognise cognitive differences in other people. However, external motivation is needed to sustain reflection on the learners’ own thought processes.
Stage 3: Practicing Critical Thinker
By now, the learner is familiar with their own thinking processes and makes a conscious effort to practice critical thinking.
Stage 4: Advanced Critical Thinker
As an advanced critical thinker, the learner is able to identify different cognitive processes and consciously uses critical thinking skills.
Stage 5: Accomplished Critical Thinker
At this stage, the skilled critical thinker can take charge of their thinking and habitually monitors, revises and rethinks approaches for continual improvement of their cognitive strategies.
Facilitating Critical Thinking in Healthcare
A common challenge for many educators and facilitators in healthcare is encouraging students to move away from passive learning towards active learning situations that require critical thinking skills.
Just as there are similarities among the definitions of critical thinking across subject areas and levels, there are also several generally recognised hallmarks of teaching for critical thinking . These include:
- Promoting interaction among students as they learn
- Asking open ended questions that do not assume one right answer
- Allowing sufficient time to reflect on the questions asked or problems posed
- Teaching for transfer - helping learners to see how a newly acquired skill can apply to other situations and experiences.
(Lippincott Solutions 2018)
Snyder and Snyder (2008) also make the point that it’s helpful for educators and facilitators to be aware of any initial resistance that learners may have and try to guide them through the process. They should aim to create a learning environment where learners can feel comfortable thinking through an answer rather than simply having an answer given to them.
Examples include using peer coaching techniques , mentoring or preceptorship to engage students in active learning and critical thinking skills, or integrating project-based learning activities that require students to apply their knowledge in a realistic healthcare environment.
Carvalhoa et al. (2017) also advocate problem-based learning as a widely used and successful way of stimulating critical thinking skills in the learner. This view is echoed by Tsui-Mei (2015), who notes that critical thinking, systematic analysis and curiosity significantly improve after practice-based learning .
Integrating Critical Thinking Skills Into Curriculum Design
Most educators agree that critical thinking can’t easily be developed if the program curriculum is not designed to support it. This means that a deep understanding of the nature and value of critical thinking skills needs to be present from the outset of the curriculum design process , and not just bolted on as an afterthought.
In the view of Fortepiani (2018), critical thinking skills can be summarised by the statement that 'thinking is driven by questions', which means that teaching materials need to be designed in such a way as to encourage students to expand their learning by asking questions that generate further questions and stimulate the thinking process. Ideal questions are those that:
- Embrace complexity
- Challenge assumptions and points of view
- Question the source of information
- Explore variable interpretations and potential implications of information.
To put it another way, asking questions with limiting, thought-stopping answers inhibits the development of critical thinking. This means that educators must ideally be critical thinkers themselves .
Drawing these threads together, The Foundation for Critical Thinking (2017) offers us a simple reminder that even though it’s human nature to be ‘thinking’ most of the time, most thoughts, if not guided and structured, tend to be biased, distorted, partial, uninformed or even prejudiced.
They also note that the quality of work depends precisely on the quality of the practitioners’ thought processes. Given that practitioners are being asked to meet the challenge of ever more complex care, the importance of cultivating critical thinking skills, alongside advanced problem-solving skills , seems to be taking on new importance.
Additional Resources
- The Emotionally Intelligent Nurse | Ausmed Article
- Refining Competency-Based Assessment | Ausmed Article
- Socratic Questioning in Healthcare | Ausmed Article
- Carvalhoa, D P S R P et al. 2017, 'Strategies Used for the Promotion of Critical Thinking in Nursing Undergraduate Education: A Systematic Review', Nurse Education Today , vol. 57, pp. 103-10, viewed 7 December 2018, https://www.sciencedirect.com/science/article/abs/pii/S0260691717301715
- Fortepiani, L A 2017, 'Critical Thinking or Traditional Teaching For Health Professionals', PECOP Blog , 16 January, viewed 7 December 2018, https://blog.lifescitrc.org/pecop/2017/01/16/critical-thinking-or-traditional-teaching-for-health-professions/
- Jacob, E, Duffield, C & Jacob, D 2017, 'A Protocol For the Development of a Critical Thinking Assessment Tool for Nurses Using a Delphi Technique', Journal of Advanced Nursing, vol. 73, no. 8, pp. 1982-1988, viewed 7 December 2018, https://onlinelibrary.wiley.com/doi/10.1111/jan.13306
- Kahlke, R & Eva, K 2018, 'Constructing Critical Thinking in Health Professional Education', Perspectives on Medical Education , vol. 7, no. 3, pp. 156-165, viewed 7 December 2018, https://link.springer.com/article/10.1007/s40037-018-0415-z
- Lippincott Solutions 2018, 'Turning New Nurses Into Critical Thinkers', Lippincott Solutions , viewed 10 December 2018, https://www.wolterskluwer.com/en/expert-insights/turning-new-nurses-into-critical-thinkers
- Papp, K K 2014, 'Milestones of Critical Thinking: A Developmental Model for Medicine and Nursing', Academic Medicine , vol. 89, no. 5, pp. 715-720, https://journals.lww.com/academicmedicine/Fulltext/2014/05000/Milestones_of_Critical_Thinking___A_Developmental.14.aspx
- Snyder, L G & Snyder, M J 2008, 'Teaching Critical Thinking and Problem Solving Skills', The Delta Pi Epsilon Journal , vol. L, no. 2, pp. 90-99, viewed 7 December 2018, https://dme.childrenshospital.org/wp-content/uploads/2019/02/Optional-_Teaching-Critical-Thinking-and-Problem-Solving-Skills.pdf
- The Foundation for Critical Thinking 2017, Defining Critical Thinking , The Foundation for Critical Thinking, viewed 7 December 2018, https://www.criticalthinking.org/pages/our-conception-of-critical-thinking/411
- Tsui-Mei, H, Lee-Chun, H & Chen-Ju MSN, K 2015, 'How Mental Health Nurses Improve Their Critical Thinking Through Problem-Based Learning', Journal for Nurses in Professional Development , vol. 31, no. 3, pp. 170-175, viewed 7 December 2018, https://journals.lww.com/jnsdonline/Abstract/2015/05000/How_Mental_Health_Nurses_Improve_Their_Critical.8.aspx
Anne Watkins View profile
Help and feedback, publications.
Ausmed Education is a Trusted Information Partner of Healthdirect Australia. Verify here .
This website is intended for healthcare professionals

- { $refs.search.focus(); })" aria-controls="searchpanel" :aria-expanded="open" class="hidden lg:inline-flex justify-end text-gray-800 hover:text-primary py-2 px-4 lg:px-0 items-center text-base font-medium"> Search
Search menu
Critical thinking: what it is and why it counts. 2020. https://tinyurl.com/ybz73bnx (accessed 27 April 2021)
Faculty of Intensive Care Medicine. Curriculum for training for advanced critical care practitioners: syllabus (part III). version 1.1. 2018. https://www.ficm.ac.uk/accps/curriculum (accessed 27 April 2021)
Guerrero AP. Mechanistic case diagramming: a tool for problem-based learning. Acad Med.. 2001; 76:(4)385-9 https://doi.org/10.1097/00001888-200104000-00020
Harasym PH, Tsai TC, Hemmati P. Current trends in developing medical students' critical thinking abilities. Kaohsiung J Med Sci.. 2008; 24:(7)341-55 https://doi.org/10.1016/S1607-551X(08)70131-1
Hayes MM, Chatterjee S, Schwartzstein RM. Critical thinking in critical care: five strategies to improve teaching and learning in the intensive care unit. Ann Am Thorac Soc.. 2017; 14:(4)569-575 https://doi.org/10.1513/AnnalsATS.201612-1009AS
Health Education England. Multi-professional framework for advanced clinical practice in England. 2017. https://www.hee.nhs.uk/sites/default/files/documents/multi-professionalframeworkforadvancedclinicalpracticeinengland.pdf (accessed 27 April 2021)
Health Education England, NHS England/NHS Improvement, Skills for Health. Core capabilities framework for advanced clinical practice (nurses) working in general practice/primary care in England. 2020. https://www.skillsforhealth.org.uk/images/services/cstf/ACP%20Primary%20Care%20Nurse%20Fwk%202020.pdf (accessed 27 April 2021)
Health Education England. Advanced practice mental health curriculum and capabilities framework. 2020. https://www.hee.nhs.uk/sites/default/files/documents/AP-MH%20Curriculum%20and%20Capabilities%20Framework%201.2.pdf (accessed 27 April 2021)
Jacob E, Duffield C, Jacob D. A protocol for the development of a critical thinking assessment tool for nurses using a Delphi technique. J Adv Nurs.. 2017; 73:(8)1982-1988 https://doi.org/10.1111/jan.13306
Kohn MA. Understanding evidence-based diagnosis. Diagnosis (Berl).. 2014; 1:(1)39-42 https://doi.org/10.1515/dx-2013-0003
Clinical reasoning—a guide to improving teaching and practice. 2012. https://www.racgp.org.au/afp/201201/45593
McGee S. Evidence-based physical diagnosis, 4th edn. Philadelphia PA: Elsevier; 2018
Norman GR, Monteiro SD, Sherbino J, Ilgen JS, Schmidt HG, Mamede S. The causes of errors in clinical reasoning: cognitive biases, knowledge deficits, and dual process thinking. Acad Med.. 2017; 92:(1)23-30 https://doi.org/10.1097/ACM.0000000000001421
Papp KK, Huang GC, Lauzon Clabo LM Milestones of critical thinking: a developmental model for medicine and nursing. Acad Med.. 2014; 89:(5)715-20 https://doi.org/10.1097/acm.0000000000000220
Rencic J, Lambert WT, Schuwirth L., Durning SJ. Clinical reasoning performance assessment: using situated cognition theory as a conceptual framework. Diagnosis.. 2020; 7:(3)177-179 https://doi.org/10.1515/dx-2019-0051
Examining critical thinking skills in family medicine residents. 2016. https://www.stfm.org/FamilyMedicine/Vol48Issue2/Ross121
Royal College of Emergency Medicine. Emergency care advanced clinical practitioner—curriculum and assessment, adult and paediatric. version 2.0. 2019. https://tinyurl.com/eps3p37r (accessed 27 April 2021)
Young ME, Thomas A, Lubarsky S. Mapping clinical reasoning literature across the health professions: a scoping review. BMC Med Educ.. 2020; 20 https://doi.org/10.1186/s12909-020-02012-9
Advanced practice: critical thinking and clinical reasoning
Sadie Diamond-Fox
Senior Lecturer in Advanced Critical Care Practice, Northumbria University, Advanced Critical Care Practitioner, Newcastle upon Tyne Hospitals NHS Foundation Trust, and Co-Lead, Advanced Critical/Clinical Care Practitioners Academic Network (ACCPAN)
View articles
Advanced Critical Care Practitioner, South Tees Hospitals NHS Foundation Trust

Clinical reasoning is a multi-faceted and complex construct, the understanding of which has emerged from multiple fields outside of healthcare literature, primarily the psychological and behavioural sciences. The application of clinical reasoning is central to the advanced non-medical practitioner (ANMP) role, as complex patient caseloads with undifferentiated and undiagnosed diseases are now a regular feature in healthcare practice. This article explores some of the key concepts and terminology that have evolved over the last four decades and have led to our modern day understanding of this topic. It also considers how clinical reasoning is vital for improving evidence-based diagnosis and subsequent effective care planning. A comprehensive guide to applying diagnostic reasoning on a body systems basis will be explored later in this series.
The Multi-professional Framework for Advanced Clinical Practice highlights clinical reasoning as one of the core clinical capabilities for advanced clinical practice in England ( Health Education England (HEE), 2017 ). This is also identified in other specialist core capability frameworks and training syllabuses for advanced clinical practitioner (ACP) roles ( Faculty of Intensive Care Medicine, 2018 ; Royal College of Emergency Medicine, 2019 ; HEE, 2020 ; HEE et al, 2020 ).
Rencic et al (2020) defined clinical reasoning as ‘a complex ability, requiring both declarative and procedural knowledge, such as physical examination and communication skills’. A plethora of literature exists surrounding this topic, with a recent systematic review identifying 625 papers, spanning 47 years, across the health professions ( Young et al, 2020 ). A diverse range of terms are used to refer to clinical reasoning within the healthcare literature ( Table 1 ), which can make defining their influence on their use within the clinical practice and educational arenas somewhat challenging.
The concept of clinical reasoning has changed dramatically over the past four decades. What was once thought to be a process-dependent task is now considered to present a more dynamic state of practice, which is affected by ‘complex, non-linear interactions between the clinician, patient, and the environment’ ( Rencic et al, 2020 ).
Cognitive and meta-cognitive processes
As detailed in the table, multiple themes surrounding the cognitive and meta-cognitive processes that underpin clinical reasoning have been identified. Central to these processes is the practice of critical thinking. Much like the definition of clinical reasoning, there is also diversity with regard to definitions and conceptualisation of critical thinking in the healthcare setting. Facione (2020) described critical thinking as ‘purposeful reflective judgement’ that consists of six discrete cognitive skills: analysis, inference, interpretation, explanation, synthesis and self–regulation. Ross et al (2016) identified that critical thinking positively correlates with academic success, professionalism, clinical decision-making, wider reasoning and problem-solving capabilities. Jacob et al (2017) also identified that patient outcomes and safety are directly linked to critical thinking skills.
Harasym et al (2008) listed nine discrete cognitive steps that may be applied to the process of critical thinking, which integrates both cognitive and meta-cognitive processes:
- Gather relevant information
- Formulate clearly defined questions and problems
- Evaluate relevant information
- Utilise and interpret abstract ideas effectively
- Infer well-reasoned conclusions and solutions
- Pilot outcomes against relevant criteria and standards
- Use alternative thought processes if needed
- Consider all assumptions, implications, and practical consequences
- Communicate effectively with others to solve complex problems.
There are a number of widely used strategies to develop critical thinking and evidence-based diagnosis. These include simulated problem-based learning platforms, high-fidelity simulation scenarios, case-based discussion forums, reflective journals as part of continuing professional development (CPD) portfolios and journal clubs.
Dual process theory and cognitive bias in diagnostic reasoning
A lack of understanding of the interrelationship between critical thinking and clinical reasoning can result in cognitive bias, which can in turn lead to diagnostic errors ( Hayes et al, 2017 ). Embedded within our understanding of how diagnostic errors occur is dual process theory—system 1 and system 2 thinking. The characteristics of these are described in Table 2 . Although much of the literature in this area regards dual process theory as a valid representation of clinical reasoning, the exact causes of diagnostic errors remain unclear and require further research ( Norman et al, 2017 ). The most effective way in which to teach critical thinking skills in healthcare education also remains unclear; however, Hayes et al (2017) proposed five strategies, based on well-known educational theory and principles, that they have found to be effective for teaching and learning critical thinking within the ‘high-octane’ and ‘high-stakes’ environment of the intensive care unit ( Table 3 ). This is arguably a setting that does not always present an ideal environment for learning given its fast pace and constant sensory stimulation. However, it may be argued that if a model has proven to be effective in this setting, it could be extrapolated to other busy clinical environments and may even provide a useful aide memoire for self-assessment and reflective practices.
Integrating the clinical reasoning process into the clinical consultation
Linn et al (2012) described the clinical consultation as ‘the practical embodiment of the clinical reasoning process by which data are gathered, considered, challenged and integrated to form a diagnosis that can lead to appropriate management’. The application of the previously mentioned psychological and behavioural science theories is intertwined throughout the clinical consultation via the following discrete processes:
- The clinical history generates an initial hypothesis regarding diagnosis, and said hypothesis is then tested through skilled and specific questioning
- The clinician formulates a primary diagnosis and differential diagnoses in order of likelihood
- Physical examination is carried out, aimed at gathering further data necessary to confirm or refute the hypotheses
- A selection of appropriate investigations, using an evidence-based approach, may be ordered to gather additional data
- The clinician (in partnership with the patient) then implements a targeted and rationalised management plan, based on best-available clinical evidence.
Linn et al (2012) also provided a very useful framework of how the above methods can be applied when teaching consultation with a focus on clinical reasoning (see Table 4 ). This framework may also prove useful to those new to the process of undertaking the clinical consultation process.
Evidence-based diagnosis and diagnostic accuracy
The principles of clinical reasoning are embedded within the practices of formulating an evidence-based diagnosis (EBD). According to Kohn (2014) EBD quantifies the probability of the presence of a disease through the use of diagnostic tests. He described three pertinent questions to consider in this respect:
- ‘How likely is the patient to have a particular disease?’
- ‘How good is this test for the disease in question?’
- ‘Is the test worth performing to guide treatment?’
EBD gives a statistical discriminatory weighting to update the probability of a disease to either support or refute the working and differential diagnoses, which can then determine the appropriate course of further diagnostic testing and treatments.
Diagnostic accuracy refers to how positive or negative findings change the probability of the presence of disease. In order to understand diagnostic accuracy, we must begin to understand the underlying principles and related statistical calculations concerning sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV) and likelihood ratios.
The construction of a two-by-two square (2 x 2) table ( Figure 1 ) allows the calculation of several statistical weightings for pertinent points of the history-taking exercise, a finding/sign on physical examination, or a test result. From this construct we can then determine the aforementioned statistical calculations as follows ( McGee, 2018 ):
- Sensitivity , the proportion of patients with the diagnosis who have the physical sign or a positive test result = A ÷ (A + C)
- Specificity , the proportion of patients without the diagnosis who lack the physical sign or have a negative test result = D ÷ (B + D)
- Positive predictive value , the proportion of patients with disease who have a physical sign divided by the proportion of patients without disease who also have the same sign = A ÷ (A + B)
- Negative predictive value , proportion of patients with disease lacking a physical sign divided by the proportion of patients without disease also lacking the sign = D ÷ (C + D)
- Likelihood ratio , a finding/sign/test results sensitivity divided by the false-positive rate. A test of no value has an LR of 1. Therefore the test would have no impact upon the patient's odds of disease
- Positive likelihood ratio = proportion of patients with disease who have a positive finding/sign/test, divided by proportion of patients without disease who have a positive finding/sign/test OR (A ÷ N1) ÷ (B÷ N2), or sensitivity ÷ (1 – specificity) The more positive an LR (the further above 1), the more the finding/sign/test result raises a patient's probability of disease. Thresholds of ≥ 4 are often considered to be significant when focusing a clinician's interest on the most pertinent positive findings, clinical signs or tests
- Negative likelihood ratio = proportion of patients with disease who have a negative finding/sign/test result, divided by the proportion of patients without disease who have a positive finding/sign/test OR (C ÷ N1) ÷ (D÷N1) or (1 – sensitivity) ÷ specificity The more negative an LR (the closer to 0), the more the finding/sign/test result lowers a patient's probability of disease. Thresholds <0.4 are often considered to be significant when focusing clinician's interest on the most pertinent negative findings, clinical signs or tests.
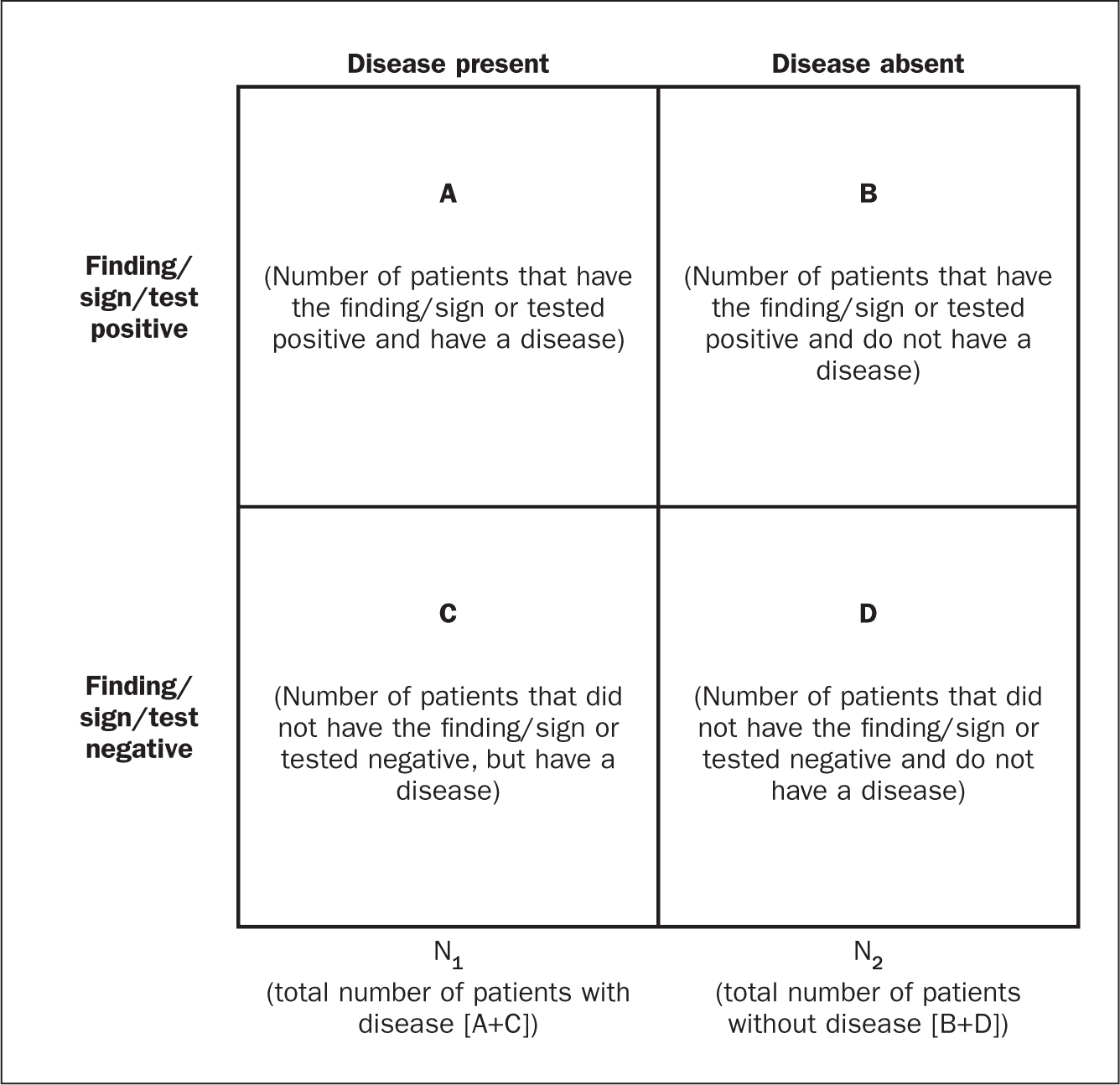
There are various online statistical calculators that can aid in the above calculations, such as the BMJ Best Practice statistical calculators, which may used as a guide (https://bestpractice.bmj.com/info/toolkit/ebm-toolbox/statistics-calculators/).
Clinical scoring systems
Evidence-based literature supports the practice of determining clinical pretest probability of certain diseases prior to proceeding with a diagnostic test. There are numerous validated pretest clinical scoring systems and clinical prediction tools that can be used in this context and accessed via various online platforms such as MDCalc (https://www.mdcalc.com/#all). Such clinical prediction tools include:
- 4Ts score for heparin-induced thrombocytopenia
- ABCD² score for transient ischaemic attack (TIA)
- CHADS₂ score for atrial fibrillation stroke risk
- Aortic Dissection Detection Risk Score (ADD-RS).
Conclusions
Critical thinking and clinical reasoning are fundamental skills of the advanced non-medical practitioner (ANMP) role. They are complex processes and require an array of underpinning knowledge of not only the clinical sciences, but also psychological and behavioural science theories. There are multiple constructs to guide these processes, not all of which will be suitable for the vast array of specialist areas in which ANMPs practice. There are multiple opportunities throughout the clinical consultation process in which ANMPs can employ the principles of critical thinking and clinical reasoning in order to improve patient outcomes. There are also multiple online toolkits that may be used to guide the ANMP in this complex process.
- Much like consultation and clinical assessment, the process of the application of clinical reasoning was once seen as solely the duty of a doctor, however the advanced non-medical practitioner (ANMP) role crosses those traditional boundaries
- Critical thinking and clinical reasoning are fundamental skills of the ANMP role
- The processes underlying clinical reasoning are complex and require an array of underpinning knowledge of not only the clinical sciences, but also psychological and behavioural science theories
- Through the use of the principles underlying critical thinking and clinical reasoning, there is potential to make a significant contribution to diagnostic accuracy, treatment options and overall patient outcomes
CPD reflective questions
- What assessment instruments exist for the measurement of cognitive bias?
- Think of an example of when cognitive bias may have impacted on your own clinical reasoning and decision making
- What resources exist to aid you in developing into the ‘advanced critical thinker’?
- What resources exist to aid you in understanding the statistical terminology surrounding evidence-based diagnosis?
- Open access
- Published: 24 May 2023
Embracing critical thinking to enhance our practice
- Luis Martí-Bonmatí ORCID: orcid.org/0000-0002-8234-010X 1
Insights into Imaging volume 14 , Article number: 97 ( 2023 ) Cite this article
3485 Accesses
1 Citations
2 Altmetric
Metrics details
Miguel de Cervantes, the great Spanish writer, once wrote that those “who read much and walk much, go far and know much" [ 1 ]. The same is true in medicine; reading and gathering experience are the main pillars on which one should develop the knowledge of solving clinical problems in the ever-changing field of healthcare. If properly done, these newly acquired skills will continuously enhance our critical thinking strategies with which we try to identify the best possible improvements in the clinical pathway of radiology. As gaps in knowledge are always present, medicine is rooted in consolidated knowledge based on validated scientific studies and clinical experience reproducibility and accuracy [ 2 ]. This represents our best approach to evidence-based decisions. Medical knowledge must be well-established before it can be considered as the basis for decision making and patients guidance in daily practice.
The practice of critical thinking helps us understand the disease manifestations and the related processes and actions that might be relevant to prevent, diagnose and treat diseases. To critically appraise the way we perform evidence-based practice, we must combine best quality research with clinical expertise. This link between exploration and practice will allow radiologists and related disciplines to impact the way medicine is practiced.
These concepts are the cornerstones of Insights into Imaging , and it is my privilege as editor-in-chief to describe in this editorial how the journal, and each author, can contribute quality through critical thinking, and hence improve the way we practice radiology by re-shaping our understandings.
It is universally recognized that, in medical imaging, strong levels of evidence are needed to assess the results of the different possible actions and to guide decisions (i.e., to demonstrate a sufficient causal relationship between a specific diagnostic criterion and a disease grading, or a given radiological intervention versus another option in a given condition) toward the most effective or safe outcome considering the benefit of patients and value-based healthcare pathways. Consequently, solid levels of evidence are required to assess the results of different possible actions derived from imaging findings. And, in doing so, we continuously generate more data in our diagnostic and therapeutic activities, whether they are processes or outcomes. This new information will then be transformed into new evidence, real world evidence. In this way, the observed relationship between action and outcome generates causality course actions that will improve our understanding of the best clinical pathways, eliminating the many confounding thoughts that we unconsciously carry during the process of learning and implementing our clinical practice.
Socratic inquiry and Skepticism as foundation. Critical thinking can be understood as the process of analyzing and questioning existing and established knowledge with the intention of improving it. Previous knowledge, either eminence- or evidence-based, should continuously be critically reconsidered and reevaluated for the benefit of the patients, as knowledge is always changing in Precision Medicine. In the real world of medical imaging, this critical thinking must be focused on the evaluation of the effectiveness and clinical impact of all those processes in which images are involved, from the acquisition with different modalities to the processing of the data, from the biological correlation of radiomics as an image biomarker to the therapeutic orientation, and finally in image-guided interventional treatments. Developing critical thinking helps to improve any medical discipline by asking ourselves how to establish better and more precise processes based on existing accumulated evidence, how to recognize and control the biases when approaching a clinical problem, and how to adapt the new clinical information in service of the best solutions. Socratic inquiry and a skeptic attitude can be used to consolidate the best knowledge and construct new associations to be more efficient and to approach excellence in our daily work. Critical thinking is therefore necessary to improve both clinical practice and research in radiology, avoiding disruptive uncertainties and wrong assumptions.
These “questioning and solving” skills require learning, practice, and experience [ 3 ], but mainly a recognition of the many uncertainties we do have despite the important scientific advances. Precisely, a good example of the importance of critical thinking is its contribution to Precision Medicine through medical imaging data and information. In daily practice, we should ask ourselves why should we accept a reliable diagnostic method that fails 15% of the time, or an appropriate treatment that is not effective in almost 25% of patients? As scientists, we can improve these clinical decisions in the daily practice. Artificial intelligence (AI) solutions integrating different imaging, clinical, molecular, and genetic data as inputs are being implemented as a suitable pathway to solve clinical problems. The design and methodology of these AI algorithms must allow for their explainability and critical thinking evaluation before they are implemented in clinical practice [ 4 ].
In summary, critical thinking develops evidence-based knowledge, provides continuous improvements, and avoids spurious technical and clinical misconceptions. Insights into Imaging is dedicated to manuscripts with a clear critical approach, focusing on excellence in clinical practice, evidence-based knowledge and causal reasoning in radiology. Science is based on long-lived critiques and authors are encouraged to systematically identify, analyze, and solve problems by identifying inconsistencies and correcting errors.
To foster this, Insights into Imaging welcomes critical thinking papers and will incorporate a new “Critical Relevance Statement” in all their publications, where authors are asked to summarize in one sentence the question they are trying to answer and the improvement they are providing to the issue at hand.
Availability of data and materials
Not applicable.
De Cervantes M (1986) The adventures of don Quixote de la Mancha. New York, Farrar, Straus, Giroux
Martí-Bonmatí L (2021) Evidence levels in radiology: the insights into imaging approach. Insights Imaging 12(1):45. https://doi.org/10.1186/s13244-021-00995-7
Article PubMed PubMed Central Google Scholar
Ho YR, Chen BY, Li CM (2023) Thinking more wisely: using the Socratic method to develop critical thinking skills amongst healthcare students. BMC Med Educ 23(1):173. https://doi.org/10.1186/s12909-023-04134-2
Cerdá-Alberich L, Solana J, Mallol P et al (2023) MAIC-10 brief quality checklist for publications using artificial intelligence and medical images. Insights Imaging 14(1):11. https://doi.org/10.1186/s13244-022-01355-9
Download references
Acknowledgements
To the Insights into Imaging ’s Office for their help in preparing this editorial.
Author information
Authors and affiliations.
Medical Imaging Department and Biomedical Imaging Research Group, Hospital Universitario y Politécnico La Fe and Health Research Institute, Valencia, Spain
Luis Martí-Bonmatí
You can also search for this author in PubMed Google Scholar
Contributions
LBM is the only author.The author have read and approved the final version of the manuscript.
Corresponding author
Correspondence to Luis Martí-Bonmatí .
Ethics declarations
Ethics approval and consent to participate, consent for publication, competing interests.
LMB is the Editor in Chief of Insights into Imaging . He has not taken part in the review or selection process of this article.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Martí-Bonmatí, L. Embracing critical thinking to enhance our practice. Insights Imaging 14 , 97 (2023). https://doi.org/10.1186/s13244-023-01435-4
Download citation
Received : 05 April 2023
Accepted : 24 April 2023
Published : 24 May 2023
DOI : https://doi.org/10.1186/s13244-023-01435-4
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Critical thinking
- Precision medicine
- Reproducibility
- Causal inference
- Departments, units, and programs
- College leadership
- Diversity, equity, and inclusion
- Faculty and staff resources
- LAS Strategic Plan

- Apply to LAS
- Liberal arts & sciences majors
- LAS Insider blog
- Admissions FAQs
- Parent resources
- Pre-college summer programs
Quick Links
Request info
- Academic policies and standing
- Advising and support
- College distinctions
- Dates and deadlines
- Intercollegiate transfers
- LAS Lineup student newsletter
- Programs of study
- Scholarships
- Certificates
- Student emergencies
Student resources
- Access and Achievement Program
- Career services
- First-Year Experience
- Honors program
- International programs
- Internship opportunities
- Paul M. Lisnek LAS Hub
- Student research opportunities
- Expertise in LAS
- Research facilities and centers
- Dean's Distinguished Lecture series
- Alumni advice
- Alumni award programs
- Get involved
- LAS Alumni Council
- LAS@Work: Alumni careers
- Study Abroad Alumni Networks
- Update your information
- Nominate an alumnus for an LAS award
- Faculty honors
- The Quadrangle Online
- LAS News email newsletter archive
- LAS social media
- Media contact in the College of LAS
- LAS Landmark Day of Giving
- About giving to LAS
- Building projects
- Corporate engagement
- Faculty support
- Lincoln Scholars Initiative
- Impact of giving
Why is critical thinking important?
What do lawyers, accountants, teachers, and doctors all have in common?

What is critical thinking?
The Oxford English Dictionary defines critical thinking as “The objective, systematic, and rational analysis and evaluation of factual evidence in order to form a judgment on a subject, issue, etc.” Critical thinking involves the use of logic and reasoning to evaluate available facts and/or evidence to come to a conclusion about a certain subject or topic. We use critical thinking every day, from decision-making to problem-solving, in addition to thinking critically in an academic context!
Why is critical thinking important for academic success?
You may be asking “why is critical thinking important for students?” Critical thinking appears in a diverse set of disciplines and impacts students’ learning every day, regardless of major.
Critical thinking skills are often associated with the value of studying the humanities. In majors such as English, students will be presented with a certain text—whether it’s a novel, short story, essay, or even film—and will have to use textual evidence to make an argument and then defend their argument about what they’ve read. However, the importance of critical thinking does not only apply to the humanities. In the social sciences, an economics major , for example, will use what they’ve learned to figure out solutions to issues as varied as land and other natural resource use, to how much people should work, to how to develop human capital through education. Problem-solving and critical thinking go hand in hand. Biology is a popular major within LAS, and graduates of the biology program often pursue careers in the medical sciences. Doctors use critical thinking every day, tapping into the knowledge they acquired from studying the biological sciences to diagnose and treat different diseases and ailments.
Students in the College of LAS take many courses that require critical thinking before they graduate. You may be asked in an Economics class to use statistical data analysis to evaluate the impact on home improvement spending when the Fed increases interest rates (read more about real-world experience with Datathon ). If you’ve ever been asked “How often do you think about the Roman Empire?”, you may find yourself thinking about the Roman Empire more than you thought—maybe in an English course, where you’ll use text from Shakespeare’s Antony and Cleopatra to make an argument about Roman imperial desire. No matter what the context is, critical thinking will be involved in your academic life and can take form in many different ways.
The benefits of critical thinking in everyday life
Building better communication.
One of the most important life skills that students learn as early as elementary school is how to give a presentation. Many classes require students to give presentations, because being well-spoken is a key skill in effective communication. This is where critical thinking benefits come into play: using the skills you’ve learned, you’ll be able to gather the information needed for your presentation, narrow down what information is most relevant, and communicate it in an engaging way.
Typically, the first step in creating a presentation is choosing a topic. For example, your professor might assign a presentation on the Gilded Age and provide a list of figures from the 1870s—1890s to choose from. You’ll use your critical thinking skills to narrow down your choices. You may ask yourself:
- What figure am I most familiar with?
- Who am I most interested in?
- Will I have to do additional research?
After choosing your topic, your professor will usually ask a guiding question to help you form a thesis: an argument that is backed up with evidence. Critical thinking benefits this process by allowing you to focus on the information that is most relevant in support of your argument. By focusing on the strongest evidence, you will communicate your thesis clearly.
Finally, once you’ve finished gathering information, you will begin putting your presentation together. Creating a presentation requires a balance of text and visuals. Graphs and tables are popular visuals in STEM-based projects, but digital images and graphics are effective as well. Critical thinking benefits this process because the right images and visuals create a more dynamic experience for the audience, giving them the opportunity to engage with the material.
Presentation skills go beyond the classroom. Students at the University of Illinois will often participate in summer internships to get professional experience before graduation. Many summer interns are required to present about their experience and what they learned at the end of the internship. Jobs frequently also require employees to create presentations of some kind—whether it’s an advertising pitch to win an account from a potential client, or quarterly reporting, giving a presentation is a life skill that directly relates to critical thinking.
Fostering independence and confidence
An important life skill many people start learning as college students and then finessing once they enter the “adult world” is how to budget. There will be many different expenses to keep track of, including rent, bills, car payments, and groceries, just to name a few! After developing your critical thinking skills, you’ll put them to use to consider your salary and budget your expenses accordingly. Here’s an example:
- You earn a salary of $75,000 a year. Assume all amounts are before taxes.
- 1,800 x 12 = 21,600
- 75,000 – 21,600 = 53,400
- This leaves you with $53,400
- 320 x 12 = 3,840 a year
- 53,400-3,840= 49,560
- 726 x 12 = 8,712
- 49,560 – 8,712= 40,848
- You’re left with $40,848 for miscellaneous expenses. You use your critical thinking skills to decide what to do with your $40,848. You think ahead towards your retirement and decide to put $500 a month into a Roth IRA, leaving $34,848. Since you love coffee, you try to figure out if you can afford a daily coffee run. On average, a cup of coffee will cost you $7. 7 x 365 = $2,555 a year for coffee. 34,848 – 2,555 = 32,293
- You have $32,293 left. You will use your critical thinking skills to figure out how much you would want to put into savings, how much you want to save to treat yourself from time to time, and how much you want to put aside for emergency funds. With the benefits of critical thinking, you will be well-equipped to budget your lifestyle once you enter the working world.
Enhancing decision-making skills
Choosing the right university for you.
One of the biggest decisions you’ll make in your life is what college or university to go to. There are many factors to consider when making this decision, and critical thinking importance will come into play when determining these factors.
Many high school seniors apply to colleges with the hope of being accepted into a certain program, whether it’s biology, psychology, political science, English, or something else entirely. Some students apply with certain schools in mind due to overall rankings. Students also consider the campus a school is set in. While some universities such as the University of Illinois are nestled within college towns, New York University is right in Manhattan, in a big city setting. Some students dream of going to large universities, and other students prefer smaller schools. The diversity of a university’s student body is also a key consideration. For many 17- and 18-year-olds, college is a time to meet peers from diverse racial and socio-economic backgrounds and learn about life experiences different than one’s own.
With all these factors in mind, you’ll use critical thinking to decide which are most important to you—and which school is the right fit for you.
Develop your critical thinking skills at the University of Illinois
At the University of Illinois, not only will you learn how to think critically, but you will put critical thinking into practice. In the College of LAS, you can choose from 70+ majors where you will learn the importance and benefits of critical thinking skills. The College of Liberal Arts & Sciences at U of I offers a wide range of undergraduate and graduate programs in life, physical, and mathematical sciences; humanities; and social and behavioral sciences. No matter which program you choose, you will develop critical thinking skills as you go through your courses in the major of your choice. And in those courses, the first question your professors may ask you is, “What is the goal of critical thinking?” You will be able to respond with confidence that the goal of critical thinking is to help shape people into more informed, more thoughtful members of society.
With such a vast representation of disciplines, an education in the College of LAS will prepare you for a career where you will apply critical thinking skills to real life, both in and outside of the classroom, from your undergraduate experience to your professional career. If you’re interested in becoming a part of a diverse set of students and developing skills for lifelong success, apply to LAS today!
Read more first-hand stories from our amazing students at the LAS Insider blog .
- Privacy Notice
- Accessibility

COMMENTS
Sound critical thinking skills can help clinicians avoid cognitive biases and diagnostic errors. This article describes three critical thinking skills essential to effective clinical care - clinical reasoning, evidence-informed decision-making, and systems thinking - and approaches to develop these skills during clinician training.
The following are examples of attributes of excellent critical thinking skills in nursing. 1. The ability to interpret information: In nursing, the interpretation of patient data is an essential part of critical thinking. Nurses must determine the significance of vital signs, lab values, and data associated with physical assessment.
Learning to provide safe and quality health care requires technical expertise, the ability to think critically, experience, and clinical judgment. The high-performance expectation of nurses is dependent upon the nurses' continual learning, professional accountability, independent and interdependent decisionmaking, and creative problem-solving abilities.
Critical thinking in nursing is invaluable for safe, effective, patient-centered care. You can successfully navigate challenges in the ever-changing health care environment by continually developing and applying these skills. Images sourced from Getty Images. Critical thinking in nursing is essential to providing high-quality patient care.
The decisions made directly affect patient care outcomes. 1 Bedside nurses, preceptors, and nurse leaders play a pivotal role in the development of critical thinking ability in the clinical setting. The purposes of this article were to explore the concept of critical thinking and to provide nurses with practical strategies to enhance critical ...
Critical thinking is applied by nurses in the process of solving problems of patients and decision-making process with creativity to enhance the effect. It is an essential process for a safe, efficient and skillful nursing intervention. Critical thinking according to Scriven and Paul is the mental active process and subtle perception, analysis ...
Critical thinking is just one skill crucial to evidence based practice in healthcare and education, write Jonathan Sharples and colleagues , who see exciting opportunities for cross sector collaboration Imagine you are a primary care doctor. A patient comes into your office with acute, atypical chest pain. Immediately you consider the patient's sex and age, and you begin to think about what ...
This literature review will present a history of inquiry into critical thinking and research to support the conclusion that critical thinking is necessary not only in the clinical practice setting, but also as an integral component of nursing-education programmes to promote the development of nurses' critical-thinking abilities.
Critical thinking is an integral part of nursing, especially in terms of professionalization and independent clinical decision-making. It is necessary to think critically to provide adequate, creative, and effective nursing care when making the right decisions for practices and care in the clinical setting and solving various ethical issues encountered.
In short, clinical reasoning requires critical thinking skills, abilities and traits which are often not taught in schools and colleges for the health professions. Skilled clinicians systematically analyze their thinking by targeting the elements of clinical reasoning and evaluate their thinking through application of intellectual
Nurses are critical thinkers. The characteristic that distinguishes a professional nurse is cognitive rather than psychomotor ability. Nursing practice demands that practitioners display sound judgement and decision-making skills as critical thinking and clinical decision making is an essential component of nursing practice.
Teaching clinical reasoning is challenging, particularly in the time-pressured and complicated environment of the ICU. Clinical reasoning is a complex process in which one identifies and prioritizes pertinent clinical data to develop a hypothesis and a plan to confirm or refute that hypothesis. Clinical reasoning is related to and dependent on critical thinking skills, which are defined as one ...
Prioritization of patient care should be grounded in critical thinking rather than just a checklist of items to be done. Critical thinking is a broad term used in nursing that includes "reasoning about clinical issues such as teamwork, collaboration, and streamlining workflow.". [1] Certainly, there are many actions that nurses must ...
Critical Thinking and Clinical Reasoning. Nurses make decisions while providing patient care by using critical thinking and clinical reasoning. Critical thinking is a broad term used in nursing that includes "reasoning about clinical issues such as teamwork, collaboration, and streamlining workflow." [1] Using critical thinking means that nurses take extra steps to maintain patient safety ...
Successful nurses think beyond their assigned tasks to deliver excellent care for their patients. For example, a nurse might be tasked with changing a wound dressing, delivering medications, and monitoring vital signs during a shift. However, it requires critical thinking skills to understand how a difference in the wound may affect blood ...
These skills will motivate the trainee to engage in effortful clinical reasoning and critical thinking, as well as to independently formulate and answer key questions necessary to manage patients. Posing questions to learners is a general strategy for assessing and teaching critical thinking in clinical settings.
In countering these shortcomings, clinicians must be able to think critically, interpret and assimilate new knowledge, deal with uncertainty and change behaviour in response to compelling new evidence. Three critical thinking skills underpin effective care: clinical reasoning, evidence-informed decision-making and systems thinking.
Tanner (2006) Clinical Judgement Model was helpful in operationalizing the process of critical thinking and clinical judgment. Tanner states that the clinical judgement of experienced nurses involves four aspects: noticing (gaining a perceptual grasp of the situation), interpreting (developing a sufficient understanding of the situation), responding (deciding on a course of action appropriate ...
Improving clinical reasoning techniques is the right way to facilitate decision-making from prognostic, diagnostic, and therapeutic points of view. However, the process to do that is to fill knowledge gaps by studying and growing experience and knowing some cognitive aspects to raise the awareness of thinking mechanisms to avoid cognitive ...
Kataoka-Yahiro and Saylor (1994) describe critical thinking competencies as the cognitive processes a nurse uses to make judgments about the clinical care of patients. These include general critical thinking, specific critical thinking in clinical situations, and specific critical thinking in nursing. General critical thinking processes are not ...
Critical thinking skills have been linked to improved patient outcomes, better quality patient care and improved safety outcomes in healthcare (Jacob et al. 2017).. Given this, it's necessary for educators in healthcare to stimulate and lead further dialogue about how these skills are taught, assessed and integrated into the design and development of staff and nurse education and training ...
As detailed in the table, multiple themes surrounding the cognitive and meta-cognitive processes that underpin clinical reasoning have been identified. Central to these processes is the practice of critical thinking. Much like the definition of clinical reasoning, there is also diversity with regard to definitions and conceptualisation of critical thinking in the healthcare setting.
The practice of critical thinking helps us understand the disease manifestations and the related processes and actions that might be relevant to prevent, diagnose and treat diseases. To critically appraise the way we perform evidence-based practice, we must combine best quality research with clinical expertise.
The importance of critical thinking can be found across a wide set of disciplines. They are not only used in the humanities but are also important to professionals in the social and behavioral sciences, physical sciences, and STEM—and the list does not end there. At the University of Illinois College of Liberal Arts & Sciences, you'll be ...