An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Int J Environ Res Public Health


Food-Borne Disease Prevention and Risk Assessment
“Food-borne Disease Prevention and Risk Assessment” is a Special Issue of the International Journal of Environmental Research and Public Health on understanding how food-borne disease is still a global threat to health today and to be able to target strategies to reduce its prevalence. Despite decades of government and industry interventions, food-borne disease remains unexpectedly high in both developed and developing nations. For instance, the Centers for Disease Control and Prevention (CDC) estimates that one in six persons in the United States suffers from gastroenteritis each year, with up to 3000 fatalities arising from consumption of contaminated food [ 1 ]. According to the WHO Initiative to Estimate the Global Burden of Food-borne Diseases, 31 global hazards caused 600 million food-borne illnesses and 420,000 deaths in 2010; diarrheal disease agents were the leading cause of these in most regions caused by Salmonella, but Taenia solium , hepatitis A virus, and aflatoxin were also significant causes of food-borne illness [ 2 , 3 ]. The global burden of food-borne disease by these 31 hazards was 33 (95% UI 25–46) million Disability Adjusted Life Years (DALYs) in 2010; 40% of the food-borne disease burden was among children under five years of age. Since we know that most food-borne diseases are preventable, these are astonishing figures for the 21st century. We are familiar with some of the underlying conditions: unsafe water used for the cleaning and processing of food, poor food-production processes, inadequate storage, and food-handling practices including infected food workers and cross-contamination of food. These can be coupled with inadequate or poorly enforced regulatory standards and industry compliance. However, knowledge of these is not enough. Making advances in prevention and control practices requires a suite of interlinked actions from improvements in the investigation of complaints and illnesses to finding the root cause of outbreaks; applying rapid and accurate identification of the hazards present; determining the conditions in which pathogens grow and multiply in order to eliminate or reduce these numbers; developing targeted intervention strategies; understanding human behavior with respect to food processing and its preparation; producing effective educational and training programs; evaluating the risks of existing and modified food production and preparation practices; predicting how effective potential interventions would be, and introducing effective and enforceable codes of practice for the different harvesting, processing, and preparing industry components. The human element is now known to be critical in applying safe practices to prevent food-borne illnesses, but it is much more difficult to influence for positive change, both from the culture of an organization and individual backgrounds and preferences. This issue is a modest attempt to explore some of these efforts through five publications.
Most agents causing food-borne illness have been identified over the last 145 years, starting from the pioneering work of Robert Koch who identified the cause of anthrax, tuberculosis and cholera. He also dismissed the then-current concept of spontaneous generation, used agar as a base for growing bacteria, and proposed his four postulates: (1) the organism must always be present, in every case of the disease; (2) the organism must be isolated from a host containing the disease and grown in pure culture; (3) samples of the organism taken from pure culture must cause the same disease when inoculated into a healthy, susceptible animal in the laboratory; (4) the organism must be isolated from the inoculated animal and must be identified as the same original organism first isolated from the originally diseased host. Over time, however, the rigid application of these postulates probably hindered research into the discovery of new agents, particularly viruses which initially could not be seen or isolated in culture. Today, nucleic acid-based microbial detection methods have made Koch’s original postulates less relevant, because these methods make it possible to identify microbes associated with a disease, even if they are non-culturable. Prions are another class of agents that do not fit into the classical infectious disease agent being misfolded proteins with the ability to transmit their misfolded shape onto normal variants of the same protein to cause transmissible neurodegenerative diseases in humans and some animals. Thus, a challenge today is to be prepared to identify and characterize new infectious agents which can arise from unexpected sources. This applies to coronaviruses which have recently been brought to the public’s attention where humans have been infected from animal sources. These include severe acute respiratory syndrome coronavirus (SARS-CoV), for which bats are a major reservoir of many strains, and other strains have been identified in palm civets; Middle East respiratory syndrome-related coronavirus (MERS-CoV), is a species of coronavirus which also has reservoirs in bats, and but has spread to camels and from there to humans, particularly camel handlers; and the current COVID-19 virus pandemic affecting millions of people worldwide, which likely originated from wet markets in Wuhan, China, where domestic and wild animals are slaughtered for customers; however, significantly, bats may also be the primary reservoir.
This background makes the paper of Wen, Sun, Li, He and Tsai [ 4 ], Avian Influenza—Factors Affecting Consumers’ Purchase Intentions toward Poultry Products , all the more relevant for those seeing increasing links between animals and human diseases. Influenza viruses, belong to the Orthomyxoviridae, a different family from the coronaviruses; yet, strains of both of these infect humans and animals, and some can be transmitted from animals to humans; these include the H1N1 avian influenza (swine flu) of 2009, which killed between 151,000 and 575,000 people worldwide) and H5N1, strain (popularly known as the bird flu) which had pandemic potential. In particular, poultry production and sales have led to the spread of H5N1 and other avian influenza viruses [ 5 ]. This strain was first isolated from a goose in China in 1996 and it spread throughout Asia and Europe over the next decade with associations of wild birds and poultry. Large sums of money were spent in order to eliminate this disease despite the relatively few associated human illnesses and deaths worldwide, and most Europeans who had limited exposure to H5N1 feared any new viruses such as the avian flu and avoided uncooked chicken products [ 6 ]. Poultry production dropped 25-30% in many Asian countries, including China. A subsequent avian influenza strain, A H7N9, also caused human infections although the number of human cases transmitted by this strain was more limited than for H5N1. Nevertheless, populations in Asia and particularly China have been sensitized to the potential risks of human infections and economic damage from news’ reports of avian influenza. The paper of Wen et al. [ 4 ] focuses on the purchase intentions consumers in Guangzhou, China, during recurring reports of this epidemic. Avian influenza A H7N9 virus had not previously been seen in either animals or people until it was found in March 2013 in China. However, since then, infections in both humans and birds have been observed, and the disease is of concern because most patients have become severely ill. Most of the cases of human infection with this avian H7N9 virus were associated with recent exposure to live poultry or potentially contaminated environments, especially markets where live birds have been sold. This virus does not appear to transmit easily from person to person, and sustained human-to-human transmission has not been reported. However, according to the Food and Agriculture Organization (FAO) [ 7 ], case-control studies suggest contact with poultry or a visit to a live poultry market in the two weeks prior to disease onset was a significant risk factor. Cases have been reported in humans who visited live bird markets, slaughtered poultry or pigeons, transported poultry, and brought live poultry into their homes. As of December 2019, the number of confirmed human cases and deaths was 1568 and 616, respectively, and 26 live markets in 15 Chinese provinces tested positive for the virus, mainly in chicken samples [ 8 ]. Thus, it is understandable that Chinese purchasers of recently slaughtered poultry should have concerns for their health, and they would consider avoiding purchasing any chicken products.
Wen et al. [ 4 ] found, unsurprisingly, that from a risk perception perspective, the more consumers believed purchasing chicken products was a risk during a period of this avian influenza outbreak, the more they reduced their purchase of chicken products, since they had low levels of trust in the quality of chicken meat. Since the public receives most of its information on avian influenza and its relationship to human illness, animal diseases and food contamination, through the mass media as it is narrated and shown to consumers, will influence and change their willingness to purchase chicken products. The authors recommended that government provides accurate information on the public health system to ensure the stable and healthy development of the poultry meat products or consumers, and to rebut any misleading media reports. However, this depends on how much trust the people are willing to place on government agencies. As Bánáti [ 6 ] indicates, there was distrust in the past in industry and government oversight of the food supply developed because of food scares such mad cow disease, dioxin in pork, melamine in pet and baby food, and now more recently in outbreaks of avian influenza, and the current COVID-19 pandemic. Although coronaviruses, particularly COVID-19, are not food-borne, the worldwide public may be overly cautious about any food they purchase and wet markets in Asia may see a drop in attendance at least until such pandemics are over. It would be interesting to explore how long anxiety over food purchases occur after this pandemic is over, but it seems the longer they last through media coverage, the more the concern will remain.
The second paper in this series, entitled Cognitive Biases of Consumers’ Risk Perception of Food-borne Diseases in China: Examining Anchoring Effect by Shan, Wang, Wu and Tsai [ 9 ], also focuses on the perception of risks of food-borne illness in China. The authors indicate that the home is the place where the largest number of food-borne illness cases occur in China, and one of the reasons for this is that many consumers are not aware of their vulnerability to such illnesses and they underestimate their risk. This seems to be opposite to the findings of Wen et al. [ 4 ] where consumers are very concerned about avian influenza transmission, but the contrast can be explained because there is virtually no media coverage of food-borne illnesses at home. Because consumers seem to have limited knowledge of the risks, the authors propose that they tend to use an anchoring strategy on which to base their food-borne disease prevention and control decisions. The authors argue that since consumers are not always rational in making decisions, they often adjust their judgments on their subjective understanding and their initial reference information (called the initial anchor). However, other factors such as an uncertain external environment and limited knowledge make consumers unsure of the extent to which they can adjust their estimates. These limitations in information processing result in biased anchoring results, which they call the “anchoring effect”. The authors postulate that because Chinese citizens have limited scientific literacy compared with those in developed countries, Chinese consumers should have significant cognitive biases including the anchoring effect. Although there are few reports on whether there is an anchoring effect in consumers’ risk perception of food-borne disease, previous studies of other diseases have confirmed that there is indeed an anchoring effect, such as overestimating the risks of breast cancer. To test whether or not consumers’ limited knowledge results in a significant anchoring effect, the authors collected survey data from 375 consumers in Wuxi, Jiangsu Province. A questionnaire obtained information on how much the respondents knew about food-borne diseases and how they could be prevented. Based on the approximate national food-borne disease prevalence rate of 15% of the population, in this study 30% and 5% food-borne disease prevalence were selected as high and low anchor values, respectively. This experimenter-provided anchor value, a history of food-borne disease, and familiarity with those diseases were found to be important factors influencing the respondents’ anchoring effect. They found that when more information was provided to the respondents in the study (considered as a short-term intervention), their risk perception was improved to some extent, but there were still anchoring biases. As a result, Shan et al. [ 9 ] argue that short-term interventions would not substantially change consumers’ anchoring effect, and there is a need for stronger and more long-term interventions. They recommend that government should play an active role in publicity and education aimed at the public about food-borne diseases. Specifically, the prevalence and scientific context about different food-borne diseases should be disseminated to consumers through various media, such as the internet, television, and radio, to warn consumers of the objective risks of these diseases. Therefore, they argue that improving consumers’ risk perception of food-borne disease is critical to the long-term prevention of illness from these risks. They concluded that government should strengthen active monitoring, publicity, and education about food-borne disease, so that individuals are more knowledgeable scientifically to improve their perception in making judgments about risks of food-borne disease. However, knowledge alone may not be enough. Da Cunha et al. [ 10 ] found that education is not as effective as training in school food handlers in Brazil. Rossi et al. [ 11 ] observed that although food handlers have knowledge of microbiological risks, their risk perception has a weak association with food safety knowledge. They stated that, unfortunately, food handlers demonstrate an awareness of food safety, but they generally fail to translate that knowledge into safe practices because of their optimistic bias. Optimistic bias is a psychological phenomenon in which people believe they are less likely to experience adverse events than others, such as in home-prepared meals. This concern also applies to consumers eating out; they can incorporate a sense of affection and identity to a place, associating it with making their own meals at home, and do not identify the risk of food-borne disease while eating at those restaurants [ 12 ]. Like food handlers, consumers have a feeling of overconfidence in the restaurant they eat with their optimistic bias. This result reinforces the need for governments and health agencies to protect the health of the population. Wildemann [ 13 ] also points out that although food-borne illnesses contribute substantially to the overall burden of disease, including hospitalizations, economic loss, and death, in contrast to food safety experts, the public usually perceives food-borne diseases as low risk. This distinguishes the differences in the perception of the risk between experts and the public. Wildemann [ 13 ] lists many qualitative factors affecting risk perception and evaluation. These include mild symptoms vs. potential fatal consequences or delayed adverse effects; dread or low concern for a certain disease; reversibility of the effects of the disease (e.g., long-term sequelae, reduced quality of life, or rapid recovery); previous history of the disease in the family or community; existing health of the individual, e.g., immunocompromised; familiarity of the agents or disease and understanding its means of transmission; increasing or decreasing public concern; exposure and impact controllable; risk determined by personal actions or mistakes made by others; trust in institutions; much or little media attention to the concern. Rosati and Saba [ 14 ] found that the concern about food risks was found to be statistically significantly dependent on the perception of risk to the individual. Usually, food-borne illness will not evoke outrage among lay people because they are perceived as voluntary, controllable, visible, and familiar. This means that most individuals perceive the threats of food-borne diseases as low, although food can pose significant risks. In particular, food-borne illness originating in the home is perceived as familiar and controllable.
For Wuxi consumers and, by extrapolation, for Chinese residents on the whole, there should be a low perceived risk even though the prevalence of food-borne disease in China is as high as 15%. This is similar to the percentage in the USA (17%) where, according to Scallan et al. [ 1 ], one in six persons is estimated to suffer from food-borne illness each year. Wildemann [ 13 ] emphasizes among the factors associated with increased concern are high media attention, and any risk message and its originator are crucial components for informing the public what actions to take of any food-borne disease concern; she emphasizes that if the public does not consider the source credible, it will be difficult to convey the message and effect long-term changes in attitude. This seems to be consistent with a long-term-held anchoring effect described by Shan et al. [ 9 ]. Credibility has two dimensions: expertise and trustworthiness. Expertise refers to the knowledge in a specific area and trustworthiness to the reliability of the message content. Trust depends on three factors: knowledge expertise, honesty concerning the completeness of the provided information, and whether the concerns of the consumers are taken seriously or not by the risk message originator [ 14 ]. Therefore, trust plays a major role in the credibility and acceptance of an institution to influence the processing of risk information and potential changes in consumer behavior. Involving the media during the whole process may enhance the trust of the public in food safety policy. All this information questions whether it is possible, without extensive government media campaigns and perhaps a scare factor like avian influenza in a population, to substantially change attitudes and behaviors towards food safety through reducing the anchoring effect. Unfortunately, although food scares draw public attention, they can also create false or misleading information that has to be countered by the experts [ 6 ], and the public may become polarized between being ultra-protective of personal and family health to a cavalier attitude to throw caution to the wind, as seems to be the case in the current COVID-19 pandemic.
The discussion on perception and communication of risk and how translate government polices into changed behavior takes us to the third paper in this issue, that of Farias, Akutsu, Botelho, and Zandonadi [ 15 ] discussing Good Practices in Home Kitchens: Construction and Validation of an Instrument for Household Food-Borne Disease Assessment and Prevention . The purpose of the study was to develop and validate an instrument to evaluate Brazilian home kitchens’ good practices. the rationale for this was for food preparers at home to avoid food-borne diseases illnesses by adopting preventive actions throughout the home food production chain. Although governments regulate food safety practices in commercial food production and food service establishments, there are no regulations on how to control food preparation and handling in the home. From the work of Rossi et al. [ 11 ] and Shan et al. [ 9 ], consumers may have an optimistic bias that creates an anchoring effect to fix consumers’ the risks associated with food-borne illness. Therefore, there needs to be more information on how to reduce food-borne domestic cases through improving food handling practices. After the instrument was developed, the content was validated using the Delphi technique with independent food hygiene and food safety specialists, and a focus group for validation of the criteria. The study showed that consumers in Brazil tend not to perceive themselves, or someone in their family, to be susceptible to food-borne illness; rank their risk of food-borne illness lower than that of others; and/or do not follow all recommended food safety practices, and, consequently, they do not take sufficient precautions to prevent illnesses from occurring. The authors found that food was prepared in the home where there were heavily contaminated areas in the kitchen (refrigerator handles, tap handles, sink drain areas, dishcloths, and sponges) because it is unusual for these surfaces to be frequently washed or cleaned. Additionally, raw or unwashed foods were constantly touched during meal preparation. The authors state that because there is limited guidance for home food preparers, the use of an such an instrument helps evaluate the level of food safety at home, and identifies unsafe practices in food handling for targeted prevention and control strategies though improving consumer knowledge about food and waterborne diseases and their consequence. Farias et al. [ 15 ] certainly developed a method to comprehensively understand the risk of home food preparation in a Brazilian community and presumably would have global value for helping to reduce risks that have led to the annual estimate of 600 million food-borne illnesses worldwide [ 3 ]. Similar studies have been done in the past such as that of Redmond and Griffith [ 16 ] who said that knowledge, attitudes, intentions, and self-reported practices do not correspond to observed behaviors, suggesting that observational studies provide a more realistic indication of the food hygiene actions actually used in domestic food preparation. Only an improvement in consumer food-handling behavior is likely to reduce the risk and incidence of food-borne disease. So, the question remains that unless food preparers are motivated, it may be very hard to change perceptions of risk of illness to themselves or who they serve. As Collins [ 17 ] pointed out 23 years ago, only 50% of consumers were concerned about food safety, partly because of lifestyle changes affecting food behavior, with an increasing number of women in the workforce, limited commitment to food preparation, and a greater number of single heads of households. Then, as now, it may be that consumers appear to be more interested in convenience and saving time than in proper food handling and preparation. Fischer et al. [ 18 ] showed that while most consumers are knowledgeable about the importance of cross-contamination and heating in preventing the occurrence of food-borne illness, this knowledge is not necessarily translated into behavior. Potentially risky behaviors were observed in the domestic food preparation environment with errors like participants allowing raw meat juices to come in contact with the final meal. The authors stated that procedural food safety knowledge (i.e., knowledge proffered after general open questions) was a better predictor of efficacious bacterial reduction than declarative food safety knowledge (i.e., knowledge proffered after formal questioning). This suggests that motivation to prepare safe food was a better indicator of actual behavior than knowledge about food safety per se . Byrd-Bredbenner et al. [ 19 ] point out that adding food safety cues to food packages may be particularly effective given that nearly half of consumers indicate they commonly read cooking instructions on food packages. Moreover, some especially “teachable moments” are after publicized food-borne illness outbreaks or recalls, before major holidays, during the perinatal period, and after being diagnosed with an immune-compromising condition. However, providing food safety information for those at increased risk of poor food-borne illness outcome often is not part of standard clinical practice among health professionals, and role models like athletes do not always demonstrate good food safety practices.
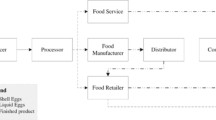
The fourth paper takes the reader from understanding risk perception and risk communication strategies for prevention of food-borne illnesses in homes and restaurants to reviewing mathematical models to help risk managers in making decisions for reducing food-borne disease, in this case the beef industry. Risk assessments have been promoted to address specific issues with the impact of chemical contaminants in the health and environmental fields for over 70 years, but a standardized risk-based food safety management approach was only recommended and adopted by the Codex Alimentarius Commission of the World Health Organization (WHO) in the last 21 years [ 20 ]. This Commission defined risk analysis as comprising risk assessment, risk management, and risk communication, and all types of contaminants were considered, including microbiological ones which have specific modeling challenges in that pathogens can increase and decrease over the production, transport, storage, and preparation of foods. Microbiological risk assessment is a scientific evaluation that aims to provide an estimation of a risk considering the probability and the severity of health effects caused by a bacterial, viral or parasitic hazard in order to support decision-making processes. The Joint FAO/WHO Expert Meetings on Microbiological Risk Assessment (JEMRA) began in 2000 in response to requests from the Codex Alimentarius Commission and FAO and WHO Member Countries and the increasing need for risk-based scientific advice on microbiological food safety issues. Quantitative microbiological risk assessments (QMRAs) aim at determining the existing public health risk associated with biological hazards in a food using mathematical equations to estimate the change of microbial load after each processing step and then to compare the efficiency of different risk reduction measures [ 21 ]. Model inputs are generated by collecting data or soliciting experts. QMRA models comprise four steps: hazard identification, exposure assessment, hazard characterization, and risk characterization. QRMAs enable experts to estimate the risk to which the population may be exposed, evaluate possible risk mitigation strategies, and generate knowledge for the better management of risks associated with contamination events. The assessment involves measuring known microbial pathogens or indicators and running a Monte Carlo simulation throughout different steps in the food chain to estimate the risk of transfer from the food to the consumer. If a dose–response model is available for the microbe, it would be used to estimate the probability of infection.
The present study of Tesson, Federighi, Cummins, Mota, Guillou, and Boué [ 22 ], entitled A Systematic Review of Beef Meat Quantitative Microbial Risk Assessment Models , was to conduct a critical analysis of beef QMRAs to help identify present and future contamination challenges in beef production. The authors’ review was comprehensive with 67 publications selected, but the focus was limited to studies in western countries and for a limited number of pathogens, mainly Enterohemorrhagic Escherichia coli (EHEC) and Salmonella spp. The authors concluded from the QMRAs that there were sufficient public health risks associated with beef meat consumption that specific risk mitigation strategies must be put in place. Because it was difficult to compare the different models used in each study, it was not possible to rank risk mitigation strategies by study in terms of effectiveness or hazards in terms of priority. Nevertheless, the authors highlighted the major risk mitigation strategies. For instance, those for EHEC and Salmonella should have a priority on the reduction of their prevalence before slaughter, e.g., the shedding condition of the animal, and the reduction of cross-contamination on the product, e.g., pathogen dispersion during dehiding, and to a lesser effect during evisceration and splitting; this would be followed by rapid chilling of the carcass to prevent growth of these pathogens and to lessen contamination of the final beef products during fabrication. Because there are limited data on the potential for cross-contamination during transportation from the farm to the slaughterhouse or during holding in the lairage, this step in beef production is difficult to model without a high degree of uncertainty. However, because it is known that lessening the length of the transit and lairage time has been observed to reduce the stress in cattle, in combination of good cleaning procedures for transport trucks and at the lairage, shedding and cross-contamination of enteric pathogens can be reduced by these actions. As a result, it is not necessary to model the whole farm-to-fork chain when trying to address specific risk management questions. In contrast, the authors argue that the strategies to control Listeria monocytogenes should focus on storage steps at retail and at home with information to the consumer, instead of emphasizing all the efforts on the slaughterhouse. Figure 5 in the publication is a useful summary of the most critical points raised in each of the 67 studies with a breakdown by Farm (prevalence of pathogens in cattle feces and hide coats; shedding time), Processing (dehiding and chilling), Retail and Consumer (storage temperature); Consumer (cooking preference and host susceptibility).
The authors conclude that QMRA is a very powerful tool providing valuable insights to assist managers make decisions to reduce the risk of infections arising from consumption of pathogens in beef, but they agree that models can only provide estimations with a level of accuracy that depends on quality and consistency of data for input into these models. Where there are data gaps in the meat production chain from farm to fork, surveys and targeted research should be encouraged to generate the missing information, but data extraction from some of the farm-to-fork steps may be difficult or even almost impossible. Therefore, proposed risk mitigation interventions for these steps may be unrealistic and hence the hazard can remain. However, if the need is great, persistence can achieve positive results. For instance, data gaps were explored to understand why deli meats sliced and packaged in the deli were contaminated with Listeria monocytogenes five to seven times more frequently than deli meats sliced and packaged by a processor [ 23 ]. Extensive testing and observations of worker behavior showed that these deli meats tended not to contain added inhibitors; resident L. monocytogenes were present in niches in equipment and spread through cross-contamination from food contact and non-food contact surfaces; and there was lack of adequate sanitation; inadequate temperature control; and inappropriate glove/hand issues. This information was used to create a “virtual deli” model and to generate six baseline situations and 22 scenarios by the U.S. Department of Health and Human Services; Center for Food Safety and Applied Nutrition, Food and Drug Administration and the U.S. Department of Agriculture Food Safety and Inspection Service [ 24 , 25 , 26 ]. Overall, the virtual deli model indicated that the greatest risk was from contamination present in an incoming chub of a product that permitted growth of Listeria . Even products that did not permit growth could still be a significant contributor to listeriosis, from environmental contamination and subsequent cross-contamination to other products. Important environmental factors contributing to risks were worker behaviors, the slicer construction and its maintenance, trash handling, and cleanup operations. The level of contamination at retail delis was found to directly affect the risk, where a two-fold decrease in contamination would result in a 20% reduction in illnesses. The simulation showed that if all deli meat products would have growth inhibitors coupled with appropriate control of temperature and storage time at the consumer’s home there would be fewer cases of listeriosis attributable to deli meats.
In another study, to acquire useful data for the consumer phase of a typical QMRA in the Netherlands, Chardon and Swart [ 27 ] designed a food consumption and food handling survey that was specifically aimed at obtaining quantitative data at the consumer level, typically not otherwise available. For a broad spectrum of food products, the survey covered the following topics: processing status at retail, consumer storage, preparation, and consumption. The final result was a coherent quantitative consumer phase food survey and parameter estimates for food handling and consumption practices in the Netherlands, including variation over individuals and uncertainty estimates. For instance, the survey showed that an average 40% of the fresh meat was stored in the refrigerator, 44% was stored in the freezer, and 18% of the dried sausages and 30% of the eggs were stored at room temperature. The mean storage time in the refrigerator was between 2 and 3 days for fresh meat and fresh meat products and about 4 days for cooked meat products and pâté. For understanding the risks of cross-contamination, 66% of chicken breasts were cut at home, and home-cut ingredients were added to 72% of precut lettuce. When meat and lettuce were prepared at the same time, 52% of the meat was cut before cutting the lettuce. Fortunately, rare and raw preparations of meat products were preferred by only 1 to 5% of the respondents; medium and done cooked food was the preference of the vast majority of those surveyed. However, 8% of respondents consumed steak tartare raw. However, more detailed information is needed on consumer preferences. For instance, products can be fresh or deep-frozen, meat cuts can be intact or consist of combined meat pieces, and beef can be mechanically tenderized with needles; not all these differences are known or acknowledged by consumers for food safety concerns.
It is not always necessary to conduct a full QRMA to achieve a risk management goal for meat production. Pointon et al. [ 28 ] used qualitative risk assessments and expert opinion to develop a framework for profiling and managing risks associated with red meat-borne food safety hazards. Inputs included known ruminant food-borne pathogens Clostridium perfringens , Campylobacter jejuni , enterohemorrhagic Escherichia coli and Salmonella spp.; increase the shedding and transmission of pathogens by co-mingling of animals, as well as intensive rearing methods and stress (such as starvation and transport). The risk profile showed that there were low-risk ratings for pathogens in raw meats (products with a terminal cooking step) and for cooked cured meats. Uncooked comminuted fermented meats (UCFM) were ranked as low risk when the process was adequate enough to inactivate the expected loading of pathogens on incoming raw ingredients. Risk ratings were higher for L. monocytogenes in ready-to-eat meat products, for Salmonella in kebabs and for enterohemorrhagic E. coli and Salmonella in UCFM where the process was not adequate to inactivate these hazards in raw materials.
QMRAs can be combined with the use of the Codex Alimentarius’ newly adopted risk management metrics to improve public health outcomes. By estimating the food safety objective (the maximum frequency and/or concentration of a hazard in a food at the time of consumption) and the performance objective (the maximum frequency and/or concentration of a hazard in a food at a specified step in the food chain before the time of consumption), risk managers will have a better understanding of the appropriate level of protection (ALOP) from microbial hazards for public health protection. Crouch et al. [ 29 ] explored such a combination that allows identification of an ALOP and evaluation of corresponding metrics at appropriate points in the meat food chain with the example of a Monte Carlo QMRA for Clostridium perfringens in ready-to-eat and partially cooked meat and poultry products. For demonstration purposes, the QMRA model was applied specifically to hot dogs produced and consumed in the United States. Evaluation of the cumulative uncertainty distribution for illness rate allows a specification of an ALOP that, with defined confidence, corresponds to current industry practices; ALOPs considered were 13–21 C. perfringens illnesses per million servings of hot dogs where the prevalence of the pathogen in hot dog servings would be 0.72–1.76%.
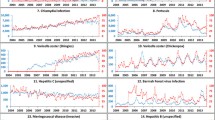
The last of the five papers in this Issue, Prevention and Control of Food-borne Diseases in Middle-East North African Countries: Review of National Control Systems is by Faour-Klingbeil and Todd [ 30 ] who discuss how a region, in this case Middle-East North African (MENA) countries, tackles prevention and control of food-borne diseases, where for the most part there are limited industry and governmental scientific and economic resources. Most of this region is arid with limited rainfall that impacts agriculture and much of the food has to be imported. The 14 WHO global subregions have considerably different burdens of food-borne disease, with the greatest falling on the subregions in Africa, followed by the subregions in South-East Asia and the Eastern Mediterranean subregion because of adverse environmental and economic conditions. More specifically, one reason why some parts of the world suffer more from food and waterborne diseases is that the public health structure may be compromised, and their prevention and control strategies, including their regulatory standards, local enforcement, educational programs, surveillance and epidemiological information systems, and applied research towards advanced technologies, are less well developed [ 31 ]. The WHO Eastern Mediterranean Region contains most of the MENA countries with an estimated 100 million people living in this region suffering from food-borne illness, mainly from nontyphoidal Salmonella, E. coli , norovirus, and Campylobacter [ 3 ]. Despite most of these countries having similar cultures, there are great economic disparities among them with Yemen and Palestinian Gaza existing in extreme poverty at one end compared Gulf countries flush with oil revenues at the other. Several MENA countries have had histories of civil wars, some on-going as in Libya, Syria and Yemen. Over the years, many of these countries have the interest, but not the will to modernize their food safety oversight systems. The authors suggest that they should manage their national food safety programs based on risk analysis with an integrated farm-to-table approach [ 32 ], and use the Codex Alimentarius Commission (CAC) working principles, and the Procedural Manual [ 19 ], and Guidelines for National Food Control Systems (NFCS) comprising of Laws and regulations; Food control management; Inspection services; Food monitoring and epidemiological Data; and Communication, information, education, and training as recommended by the FAO [ 33 , 34 ].
There is great diversity in these countries for the establishment and effectiveness of food safety legislation. For example, the Saudi Food and Drug Authority (SFDA) was established in 2003 as an independent body directly reporting to the Prime Minister with the responsibility to regulate, oversee, and control food, drug, medical devices, and the Gulf Standardization Organization (GSO) was established within the Gulf countries with the aim to harmonize the Standards and Technical Regulations of member countries based on Codex Alimentarius and in efforts to meet the requirements the Technical Barriers to Trade (TBT) and the Sanitary and Phytosanitary (SPS) Measures Agreement under the World Trade Organization (WTO). In contrast, Lebanon is still working on the legislation required to enter the WTO while facing many challenges of sectarian and political turmoil, the failure of economic growth, and massive influx of refugees from Syria. Lebanon passed its food safety law as late as 2016 after drafts had been discussed as early as 2004, with a view to establish public governance of food safety. Before the publication of the 2016 Food Safety Law, there were nine government agencies dealing with food safety, but there was no coordination among them [ 35 ]. The Food Safety Lebanese Commission (FSLC) was given responsibilities under the Law to build-up the system of food safety and sub-systems in all the ministries and organizations, and to establish by-laws and policies that would be implemented under the Council of Ministers. The FSLC was also tasked with developing education and training of professionals through academic institutions for the food industry, setting up the means for well-trained inspectors to monitor the food supply and accreditations for new laboratories. The challenge for the FSLC will be for its recommendations to be accepted by existing food safety agencies and at the cabinet level, especially today under conditions of civil unrest and economic hardship. These issues are not unique to Lebanon where weak governments combined with powerful external lobbyists can delay or minimize effective prevention and control measures for food safety. Another example is in Palestine, where the current food safety legislations are not harmonized with international standards [ 30 ].
Priority for food safety sometimes only occurs after a number of food scares are sufficient to mobilize the public to demand change. It was not until January 2017 when the Egyptian Parliament established the National Food Safety Authority (NFSA) to exclusively assume the responsibilities and jurisdiction of all ministries, public institutions, government agencies, and municipalities in relation to supervision over the handling of foodstuff with the aim to improve the regulatory oversight and efficiency in the food system. This is one step beyond the Lebanese FSLC, which has to collaborate with other agencies. Nevertheless, an agency having been given complete authority does not necessarily translate into safer food for the residents of Egypt or for products exported to other countries. Although the United Arab Emirates (UAE) has a federal law on food safety passed in 2016, food safety control in the emirates of Dubai and Sharjah is managed at the municipal level, and Dubai has established an international reputation for hosting the annual Dubai International Food Safety Conferences well before the law was promulgated. For the most part, food-borne diseases in the Eastern Mediterranean Region are still generally not well understood because of the ineffective food-borne illness surveillance and many illness cases are perceived as mild and self-limiting or unverified due to gaps in detection, surveillance and reporting by authorities. This partly reflects on the commitment of agencies to support sufficient numbers of qualified inspectors and testing laboratories to monitor the food supply. Where surveillance exists, reportable diseases in many of these countries tend to include food poisoning as a catch-all rather than list specific food-borne diseases, and the agent is not necessarily required to be identified during an investigation.
PulseNet Middle East was established in 2006 with 10 countries in the Eastern Mediterranean Region participating for molecular surveillance of food-borne infectious diseases using pulsed-field gel electrophoresis (PFGE), but it has yet to play a large role in identifying agents and factors contributing to illness, and recalling contaminated products in the Region. Since Whole Genomic Sequencing (WGS) has largely taken over from PFGE testing in Western nations, it remains to be seen if MENA countries can utilize molecular surveillance more effectively for improving food safety for the public. Even if a country has the capability to use WGS, it may not be effective unless linked to an overall surveillance and management structure such as a National Food Control System [ 30 ]. Aggressive closure of food facilities by inspectors, sometimes in collaboration with the local police force, can occur after publicly-reported food poisonings, or violations identified during an inspection, such as ‘eating spoiled foods’ to be used as deterrents for perceived compliance failures. During these closures, owners are forced financially to let go their employees temporarily. Unfortunately, these limited investigations often fail to determine the source of causative agents or to recommend educational advice to avoid future to risk behavior. Fines can also be imposed on the owners of these facilities which may be encouraged as an important source of revenue for cash-strapped public health agencies. It is difficult to ascertain the burden of food-borne diseases in many Middle Eastern countries especially when rural areas may see less inspection than in urban centers, and these are more likely to be underestimated than in western nations. As the authors state, inspection activities in the majority of the countries follow a reactive approach relying on end-products sampling, focusing on sanitation, personal hygiene, food labels instead of risk-based preventive approaches.
Governments in MENA countries tend not to be directly involved in promoting food safety training, and where these exist, they are the responsibility of the private sector, or are sponsored by non-governmental organizations, for programs like understanding and developing targeted hazard analysis critical control point (HACCP) plans. A driver for training for safe food is more linked to satisfying importers in other countries. The 2011 U.S. Food Safety Modernization Act [ 36 ] gives the Food and Drug Administration the authority to require exporters to the United States to satisfy certain criteria before they are allowed to export products, such as requiring that high-risk imported foods be accompanied by a credible third party certification or other assurance of compliance as a condition of entry into the U.S. High-risk products include those implicated in food-borne illnesses such as sesame-seed based tahini and other seed products, nuts, berries as well as meat and dairy foods. The authors conclude that there has to be more research and scientific outputs to understand the local food chain systems, to strengthen the food-borne disease surveillance systems, and to further develop capacity building programs to build NFCS using a risk-based approach to prevention and control of food-borne disease.
Several countries in the MENA region have made substantial efforts in improving their food safety systems and in some cases, in unifying the food control activities under one central agency. However, many challenges are still encountered due to ineffective surveillance systems, lack of communication among stakeholders, and limited, sometimes absent, food control functions along the food supply chain. MENA countries have limited capacity to enforce the law and implement food safety policies on a large scale and foster inter-communications among stakeholders.
These guidelines provide information for government agencies to assist in the development of national food control systems (NFCS) and to promote effective collaboration between stakeholders involved in the management and control of food safety and quality. However, different risk management decisions could be made at national levels according to different criteria and different ranges of risk management options.
In conclusion, these five papers add to our knowledge of how to understand why preventing and controlling food-borne illness is so difficult. Consumers and the public in general react to broadcast news and nowadays social media, as well as their base culture, for setting their anchoring of how they perceive risks of illness from eating specific food items. Food scares and epidemics/pandemics often reset perceptions which may last for many years depending on how much coverage the public is exposed to. The science through risk assessments and epidemiological investigations can weigh the risks of food-borne illness to a population to help governments and industry react appropriately with interventions and advice, but how much is absorbed and acted on by the public depends on the following factors: (1) trust in the responsible agency or company; (2) the acceptable level of risk communication for lay audiences; (3) the variety of communication approaches, and the duration of the messages over an extended period of time.
Systematic foodborne disease prevention and risk management based on infection mechanisms
- Published: 15 March 2024
Cite this article

- Ran Liu 1 &
- Lindu Zhao ORCID: orcid.org/0000-0003-4902-3679 1
75 Accesses
Explore all metrics
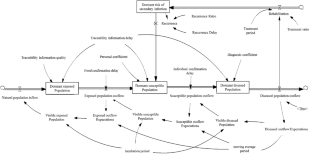
A dynamic system with 3 levels of risk management was developed to prevent the spread of foodborne diseases in populations while considering secondary infections. The effects of factors such as information quality, time delay and periodicity were compared. The results indicated that the infection mechanism of foodborne diseases exacerbated the severity of epidemics. This severity manifested as a greater number of dormant and visible populations at each stage. The risk of susceptible and exposed populations was significantly amplified during infection, which promotes the probability of dormant populations transforming into diseased populations. The infection mechanism reduced the risk of infection in the population. An increase in the time delay and periodicity increased the risk of foodborne disease, while an increase in information quality reduced the risk. By preventing infections, reducing information delay times and cycle times, and improving information quality, the prevalence of foodborne diseases can be controlled or prevented.
A dynamic system with 3 levels: exposed, susceptible and diseased population.
Emphasize the secondary infection.
Distinguish the influence of time-delay, periodic and information quality factors.
This is a preview of subscription content, log in via an institution to check access.
Access this article
Price includes VAT (Russian Federation)
Instant access to the full article PDF.
Rent this article via DeepDyve
Institutional subscriptions
Similar content being viewed by others

Software and Data Bases: Use and Application
A Markov chain model for quantifying consumer risk in food supply chains
Using internet search queries for infectious disease surveillance: screening diseases for suitability
Data availability.
The data that support the findings of this study are available from the corresponding author upon reasonable request.
The setting of the time range was mainly based on the population change equation. This article set the incidence function of the sudden increase in the disease after the 40th period. Therefore, the setting value of the total research time needed to be greater than 40 periods, but above the 40th period, the setting was modified. A certain range had no essential influence on the conclusion.
The setting of the population base to 0 was to better respond to the characteristics of sudden diseases, that is, there has been a sudden increase in such diseases before, so the population base of each disease stage was 0; however, from a mathematical perspective, the adjustment for base population had no essential impact on the conclusions.
These basic parameters could be modified within a certain range without affecting the main conclusion. To ensure that the simulation results were valid, the setting of each parameter was mainly based on the function setting of the main equations in the appendix. Under the condition of ensuring that the function was meaningful, modifying the parameters would not change the research conclusion.
The setting of the population base to 0 was to better respond to the characteristics of sudden diseases, that is, there has been a sudden increase in such diseases before, so the population base of each disease stage was 0; however, from a mathematical perspective, the adjustment for the base population had no essential impact on the conclusions.
Augustin, J. C., Kooh, P., Bayeux, T., et al. (2020). Contribution of foods and poor food-handling practices to the burden of food-borne infectious diseases in France. Foods , 9 (1644), 1644.
Article PubMed PubMed Central Google Scholar
Bertolini, M., Bevilacqua, M., & Massini, R. (2006). FMECA approach to product traceability in the food industry. Food Control , 2 (17), 137–145. https://doi.org/10.1016/j.foodcont.2004.09.013
Bisht, A., Kamble, M. P., Choudhary, P., et al. (2021). A surveillance of food borne disease outbreaks in India: 2009–2018. Food Control , 121 , 107630.
Article Google Scholar
Cai, Y., Lian, X., Peng, Z., et al. (2019). Spatiotemporal transmission dynamics for influenza disease in a heterogenous environment. Nonlinear Analysis: Real World Applications , 46 , 178–194.
MathSciNet Google Scholar
Cao, M., & Zhang, Q. (2011). Supply chain collaboration: Impaction collaborative advantage and firm performance. Journal of Operations Management , 29 (3), 163–180.
Chang, L., Duan, M., Sun, G., et al. (2020). Cross-diffusion-induced patterns in an SIR epidemic model on complex networks. Chaos: An Interdisciplinary Journal of Nonlinear Science , 30 (1), 013147.
Article MathSciNet Google Scholar
Chen, J., Chen, L., Liao, N., et al. (2021). Practice and consideration of foodborne disease surveillance in Zhejiang Province. Chinese Journal of Food Hygiene , 33 (01), 47–52.
CAS Google Scholar
Czarnecki, D. (2014). The Incidence of Melanoma is increasing in the susceptible young Australian population. Acta dermato-venereologica , 94 (5), 539–411.
Article MathSciNet PubMed Google Scholar
Fitzgibbon, W. E., Morgan, J. J., Webb, G. F., et al. (2020). Analysis of a reaction–diffusion epidemic model with asymptomatic transmission. Journal of Biological Systems , 28 (03), 561–587.
Article MathSciNet CAS Google Scholar
Ge, Y. (2021). Quality control in food supply chain with dynamic quality characteristics. Journal of Control and Decision . https://doi.org/10.1080/23307706.2021.1960646 .
Huang, C., Zhang, H., Cao, J., et al. (2019). Stability and Hopf bifurcation of a delayed prey–predator model with disease in the predator. International Journal of Bifurcation and Chaos , 29 (07), 1950091.
Article ADS MathSciNet Google Scholar
Kermack, W. O., & Mckendrick, A. G. (1927). A contribution to the mathematical theory of epidemics. Mathematical Physical and Engineering Sciences , 115 (772), 700–721.
Google Scholar
Lai, Y. H., Chung, Y. A., Wu, Y. C., et al. (2020). Disease burden from foodborne illnesses in Taiwan, 2012–2015. Journal of the Formosan Medical Association , 119 (9), 1372–1381.
Article PubMed Google Scholar
Li, C. H., Tsai, C. C., & Yang, S. Y. (2014). Analysis of epidemic spreading of an SIRS model in complex heterogeneous networks. Communications in Nonlinear Science and Numerical Simulation , 19 (04), 1042–1054.
Loukieh, M., Mouannes, E., Abou, J. C., et al. (2018). Street foods in Beirut city: An assessment of the food safety practices and of the microbiological quality. Journal of Food Safety , 38 (3), 1–11.
Machiela, M. J., & Chanock, S. J. (2015). Dlink a web-based application for exploring population-specific haplotype structure and linking correlated alleles of possible functional variants. Bioinformatics , 31 (21), 3555–3557.
Article CAS PubMed PubMed Central Google Scholar
>Nayak, R. (2016). P. Waterson (Ed.), ‘When Food kills’: A socio-technical systems analysis of the UK Pennington 1996 and 2005 E. Coli O157 Outbreak reports. Safety Science 86 36–47.
Ozdemir, Berna, C., & Dotto, G. P. (2017). Racial differences in cancer susceptibility and survival: More than the color of the skin? Trends in Cancer , 3 (3), 181–207.
Park, J. M., Kim, J. M., Hong, J. W., et al. (2020). Introduction of highly effective proactive food safety management programs into food distribution channels: For safe food labeling and safe advertisements. Journal of Food Safety , 40 (2), 1–12.
Petrignani, M., Verhoef, L., Vennema, H., et al. (2014). Underdiagnosis of food-borne hepatitis A, the Netherlands, 2008–2010. Emerging Infectious Diseases , 20 , 596–602.
Pogreba-Brown, K., Austhof, E., Armstrong, A., et al. (2020). Chronic gastrointestinal and joint-related sequelae associated with common foodborne illnesses: A scoping review. Foodborne Pathogens and Disease , 17 (2), 67–86.
Prajogo, D., & Olhager, J. (2012). Supply chain integration and performance: The effects of long-term relationships, information technology and sharing, and logistics integration. International Journal of Production Economics , 135 (1), 514–522.
Rihan, F. A., Al-Mdalla, Q. M., Alsakaji, H. J., et al. (2019). A fractional-order epidemic model with time-delay and nonlinear incidence rate. Chaos, Solitons, and Fractals , 126 (3), 97–105.
Ruey, S., Chen, C., Yan, B., et al. (2008). Using RFID technology in food produce traceability. WSEAS Transactions on Information Science and Applications , 5 (11), 1551–1560.
Scalia, G. L., Nasca, A., Corona, O., et al. (2017). An innovative shelf-life model based on smart logistic unit for an efficient management of the perishable food supply chain. Journal of Food Process Engineering , 40 (1), 1–13.
Shashi, C., Rajwinder, S., Piera, C., et al. (2018). Food cold chain management: From a structured literature review to a conceptual framework and research agenda. The International Journal of Logistics Management , 29 (3), 792–821.
Song, L., Yu, Z., & He, Q. (2023). Evolutionary game theory and simulations based on doctor and patient medical malpractice. Plos One , 18 (3), e0282434.
Sundstrom, K. (2018). Cost of illness for five major foodborne illnesses and sequelae in Sweden. Applied Health Economics and Health Policy , 16 (2), 243–257.
Syahrul, F., Wahyuni, C. U., Notobroto, H. B., et al. (2020). Transmission media of foodborne diseases as an Index prediction of Diarrheagenic Escherichia coli: Study at Elementary School, Surabaya, Indonesia. International Journal of Environmental Research and Public Health , 17 (21), 8227.
Tack, D. M., Ray, L., Griffin, P. M., et al. (2020). Preliminary incidence and trends of infections with pathogens transmitted commonly through food-foodborne diseases active surveillance network, 10 U.S. Sites, 2016–2019. Mmwr. Morbidity and Mortality Weekly Report , 69 (17), 509–514.
Taylor, D. A. (2011). Laws, regulations and policy: New food safety law brings opportunities amid hurdles. Environmental Health Perspectives, 119 (3), A119. https://doi.org/10.2307/41203198
Ushadevi, N., Vidyasagar, P., & Arshinder, K. (2015). A case study to explore influence of traceability factors on Australian food supply chain performance. Procedia - Social and Behavioral Sciences , 15 (189), 17–32.
Van, C., Le, D., Sommen, S. Y. C., et al. (2017). Estimated annual numbers of food-borne pathogen–associated illnesses, hospitalizations, and deaths, France, 2008–2013. Emerging Infectious Diseases , 23 , 1486–1492.
Verhoef, L., Hewitt, J., Barclay, L., et al. (2015). Norovirus genotype profiles associated with food-borne transmission, 1999–2012. Emerging Infectious Diseases , 21 , 592–599.
Walsh, C., & Leva, M. C. (2019). A review of human factors and food safety in Ireland. Safety Science , 119 , 399–411.
Wang, J., Wu, X., Guo, C., et al. (2018). An empirical study on the transparency of food safety logistics in China: A sampling survey based on 151 food logistics enterprises in 31 provinces. Science and Technology Management Research , 38 (23), 219–227. https://doi.org/10.3969/j.issn.1000-7695.2018.23.032
Wang, Y., Cao, J., Alsaedi, A., et al. (2017). Edge-based SEIR dynamics with or without infectious force in latent period on random networks. Communications in Nonlinear Science and Numerical Simulation , 45 , 35–54.
Wolfert, J., Verdouw, C. N., Verloop, C. M., et al. (2010). Organizing information integration in architecture food: A method based on a service-oriented architecture and living lab approach. Computers & Electronics in Agriculture , 70 (2), 389–405.
Yan, S., Zhang, Y., Ma, J., et al. (2018). An edge-based SIR model for sexually transmitted diseases on the contact network. Journal of Theoretical Biology , 439 , 216–225.
Article ADS MathSciNet PubMed Google Scholar
Yu, J. H., & Fu, R. (2015). Study on application of food safety management in cold chain logistics process based on HACCP. Logistics Technology , 34 (15), 45–47.
Yu, W., Lv, Y., Hu, C., et al. (2018). Research of an emergency medical system for mass casualty incidents in Shanghai, China: A system dynamics model. Patient Preference and Adherence , 12 , 207–222.
Zhang, B., Lin, J., & Liu, R. (2016). Factors affecting the food firm’s intention to control quality safety in China: The moderating effect of government regulation. Chinese Management Studies , 10 (2), 256–271.
Download references
Acknowledgements
For useful feedback on previous versions, we thank the editor and reviewers.This work is partially supported by the National Natural Science Foundation of China (No. 71390333), the National Key Technology RD Program of China during the 12th Five-Year Plan Period (No. 2013BAD19B05). The authors also gratefully acknowledge the helpful comments and suggestions of the reviewers, which have improved the presentation.
This work is partially supported by the National Natural Science Foundation of China (No. 71390333), the National Key Technology RD Program of China during the 12th Five-Year Plan Period (No. 2013BAD19B05).
Author information
Authors and affiliations.
Institute of Systems Engineering, School of Economics and Management, Southeast University, Nanjing, 210096, China
Ran Liu & Lindu Zhao
You can also search for this author in PubMed Google Scholar
Contributions
All authors contributed to the study conception and design, material preparation, data collection, methodology, analysis and investigation.
Corresponding author
Correspondence to Lindu Zhao .
Ethics declarations
Ethics approval and consent to participate.
Not applicable. This manuscript does not report on or involve the use of any animal or human data or tissue.
Consent to publish
Not applicable. This manuscript does not contain data from any individual person.
Conflict of interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
Reprints and permissions
About this article
Liu, R., Zhao, L. Systematic foodborne disease prevention and risk management based on infection mechanisms. Environ Dev Sustain (2024). https://doi.org/10.1007/s10668-024-04732-0
Download citation
Received : 14 October 2022
Accepted : 03 March 2024
Published : 15 March 2024
DOI : https://doi.org/10.1007/s10668-024-04732-0
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Foodborne diseases
- Infection mechanism
- Risk management
- Information traceability
- System dynamics
- Find a journal
- Publish with us
- Track your research

An official website of the United States government
Here’s how you know
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
Food Safety and Inspection Service
- News & Events
- Food Safety
- Science & Data

Foodborne Illness and Disease
What is foodborne illness.
Foodborne illness is a preventable public health challenge that causes an estimated 48 million illnesses and 3,000 deaths each year in the United States. It is an illness that comes from eating contaminated food. The onset of symptoms may occur within minutes to weeks and often presents itself as flu-like symptoms, as the ill person may experience symptoms such as nausea, vomiting, diarrhea, or fever. Because the symptoms are often flu-like, many people may not recognize that the illness is caused by harmful bacteria or other pathogens in food.
Everyone is at risk for getting a foodborne illness. However, some people are at greater risk for experiencing a more serious illness or even death should they get a foodborne illness. Those at greater risk are infants, young children, pregnant women and their unborn babies, older adults, and people with weakened immune systems (such as those with HIV/AIDS, cancer, diabetes, kidney disease, and transplant patients.) Some people may become ill after ingesting only a few harmful bacteria; others may remain symptom free after ingesting thousands.
How Do Bacteria Get in Food?
Microorganisms may be present on food products when you purchase them. For example, plastic-wrapped boneless chicken breasts and ground meat were once part of live chickens or cattle. Raw meat, poultry, seafood, and eggs are not sterile. Neither is fresh produce such as lettuce, tomatoes, sprouts, and melons.
Thousands of types of bacteria are naturally present in our environment. Microorganisms that cause disease are called pathogens. When certain pathogens enter the food supply, they can cause foodborne illness. Not all bacteria cause disease in humans. For example, some bacteria are used beneficially in making cheese and yogurt.
Foods, including safely cooked and ready-to-eat foods, can become cross-contaminated with pathogens transferred from raw egg products and raw meat, poultry, and seafood products and their juices, other contaminated products, or from food handlers with poor personal hygiene. Most cases of foodborne illness can be prevented with proper cooking or processing of food to destroy pathogens.
Learn more about Pathogens
The Danger Zone
Bacteria multiply rapidly between 40 °F and 140 °F. To keep food out of this "Danger Zone," keep cold food cold and hot food hot .
- Store food in the refrigerator (40 °F or below) or freezer (0 °F or below).
- Cook all raw beef, pork, lamb and veal steaks, chops, and roasts to a minimum internal temperature of 145 °F as measured with a food thermometer before removing meat from the heat source. For safety and quality, allow meat to rest for at least three minutes before carving or consuming. For reasons of personal preference, consumers may choose to cook meat to higher temperatures.
- Cook all raw ground beef, pork, lamb, and veal to an internal temperature of 160 °F as measured with a food thermometer.
- Cook all poultry to a safe minimum internal temperature of 165 °F as measured with a food thermometer.
- Maintain hot cooked food at 140 °F or above.
- When reheating cooked food, reheat to 165 °F.
Learn more about food safety.
In Case of Foodborne Illness
Follow these general guidelines:
- Preserve the evidence. If a portion of the suspect food is available, wrap it securely, mark "DANGER" and freeze it. Save all the packaging materials, such as cans or cartons. Write down the food type, the date, other identifying marks on the package, the time consumed, and when the onset of symptoms occurred. Save any identical unopened products.
- Seek treatment as necessary. If the victim is in an "at risk" group, seek medical care immediately. Likewise, if symptoms persist or are severe (such as bloody diarrhea, excessive nausea and vomiting, or high temperature), call your doctor.
- Call the local health department if the suspect food was served at a large gathering, from a restaurant or other food service facility, or if it is a commercial product.
- Call the USDA Meat and Poultry Hotline at 1-888-MPHotline (1-888-674-6854) if the suspect food is a USDA-inspected product and you have all the packaging.
What Are Foodborne Pathogens?
There are different bacteria and pathogens that can cause foodborne illness.
Public Health Partners
Resources for sharing information or reporting foodborne illness.
Outbreaks: Response & Prevention
FSIS collaborates with CDC, FDA and APHIS for response and prevention efforts.
Foodborne Bacteria Table
Featured factsheets & resources.

Slow Cookers and Food Safety

Cleanliness Helps Prevent Foodborne Illness

Leftovers and Food Safety
Start your search, popular topics.
- Skip to main content
- Skip to FDA Search
- Skip to in this section menu
- Skip to footer links

The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
U.S. Food and Drug Administration
- Search
- Menu
- Science & Research (Food)
- Social and Behavioral Science Research (Food)
Consumer Research on Foodborne Illness
Below are research abstracts of consumer research studies conducted or supported by the Center for Food Safety and Applied Nutrition.
The FDA Food Safety Survey: A Data Resource
The U.S. Food and Drug Administration (FDA) Food Safety Survey is a single-stage, random-digit-dialing tracking survey of a nationally representative sample of American consumers. Data were collected in 1988, 1993, 1998, 2001, 2006, and 2010 with sample sizes of 3,202, 1,620, 2,001, 4,482, 4,539, and 4,568, respectively. The purpose of the survey is to track American consumers’ knowledge, behavior, and perceptions on a number of food-safety related topics. These topics include 1) perception of individual and societal risk related to food consumption, 2) food handling, 3) food product safety label understanding and usage, 4) consumption of potentially risky foods, 5) attitude toward new food technologies, 6) perception, knowledge, and experience with foodborne illness, 7) food safety knowledge sources, and 8) consumers’ experience with food allergies. In addition, each wave queries consumers on recent FDA food safety advisories and other topics of current interest to the FDA. The available demographic information includes gender, age, education, race/ethnicity, household size, health status, region, and household income. [Contact: Amy Lando ]
Consumers’ Use of Personal Electronic Devices in the Kitchen. 2018. Amy M. Lando, Michael C. Bazaco and Yi Chen. Journal of Food Protection.
Smartphones, tablets, and other personal electronic devices have become ubiquitous in Americans’ daily lives. These devices are used by people throughout the day, including while preparing food. For example, a device may be used to look at recipes and therefore be touched multiple times during food preparation. Previous research has indicated that cell phones can harbor bacteria, including opportunistic human pathogens such as Staphylococcus and Klebsiella spp. This investigation was conducted with data from the 2016 Food Safety Survey (FSS) and from subsequent focus groups to determine the frequency with which consumers use personal electronic devices in the kitchen while preparing food, the types of devices used, and hand washing behaviors after handling these devices. The 2016 FSS is the seventh wave of a repeated cross-sectional survey conducted by the U.S. Food and Drug Administration in collaboration with the U.S. Department of Agriculture. The goal of the FSS is to evaluate U.S. adult consumer attitudes, behaviors, and knowledge about food safety. The FSS included 4,169 adults that were contacted using a dual-frame (land line and cell phone interviews) random-digit-dial sampling process. The personal electronics module was the first of three food safety topics discussed by each of eight consumer focus groups, which were convened in four U.S. cities in fall 2016. Results from the 2016 FSS revealed that of those individuals who use personal electronic devices while cooking, only about one third reported washing hands after touching the device and before continuing cooking. This proportion is significantly lower than that for self-reported hand washing behaviors after touching risky food products such as raw eggs, meat, chicken, or fish. Results from the focus groups highlight the varied usage of these devices during food preparation and the related strategies consumers are using to incorporate personal electric devices into their cooking routines. [Contact: Amy Lando ]
Mapping Sources of Food Safety Information for U.S. Consumers: Findings From a National Survey 2016. Xiaoli Nan, Linda Verrill, and Jarim Kim. Health Communication.
This research examines the sources from which U.S. consumers obtain their food safety information. It seeks to determine differences in the types of information sources used by U.S. consumers of different sociodemographic background, as well as the relationships between the types of information sources used and food safety risk perceptions. Analyzing the 2010 Food Safety Survey (N = 4,568) conducted by the U.S. Food and Drug Administration, we found that age, gender, education, and race predicted the use of different sources for food safety information. Additionally, use of several information sources predicted perceived susceptibility to foodborne illnesses and severity of food contamination. Implications of the findings for food safety risk communication are discussed. [Contact: Linda Verrill ]
Importance of Cohorts in Analyzing Trends in Safe At-Home Foodhandling Practices. 2015. Mario Teisl, Amy M. Lando, Alan S. Levy, and Caroline L. Noblet. Food Control 62: 381-389.
Safe in-home food preparation is the last line of defense for preventing foodborne illness. The Food Safety Survey assessing consumers' food handling behavior has been conducted every 3-5 years (1993, 1998, 2001, 2006, 2010) using a random digit telephone sample of United States adult consumers. Sample sizes ranged from 1620 to 4547. A previous analysis of this data has examined trends in safe food handling (as measured by washing hands and/or cutting boards after touching/cutting raw meat or chicken and by washing hands after cracking eggs). We continue and expand this analysis by modeling the unique effects of age, survey period (year) and birth cohort on safe food handling. We find that age, period, and cohort effects are relevant in measuring changes in food handling behavior; however, the effects are not similar in size or apparent mediating process. The strongest effect is period, followed by age and cohort. Thus it appears contemporaneous changes in information activity can make relatively large short-run improvements, whereas changes in one's maturation and accumulated experience have quadratic effects, and the unique shared experience of cohort leaves its own definite long-lasting imprint. We propose that the birth cohort effects can be explained by the food safety environment during young adulthood. Those who were young adults in two critical time periods – before 1940 when there were widespread foodborne infections and immediately after the 1993 outbreak of Escherichia coli O157:H7 – have better food handling behaviors. [Contact: Amy Lando ]
Self-Reported Hand Washing Behaviors and Foodborne Illness: A Propensity Score Matching Approach. 2014. Mir Ali, Linda Verrill, and Yuanting Zhang. Journal of Food Protection 77(3):352-358.
Hand washing is a simple and effective but easily overlooked way to reduce cross-contamination and the transmission of foodborne pathogens. In this study, we used the propensity score matching methodology to account for potential selection bias to explore our hypothesis that always washing hands before food preparation tasks is associated with a reduction in the probability of reported foodborne illness. Propensity score matching can simulate random assignment to a condition so that pretreatment observable differences between a treatment group and a control group are homogenous on all the covariates except the treatment variable. Using the U.S. Food and Drug Administration's 2010 Food Safety Survey, we estimated the effect of self-reported hand washing behavior on the probability of self-reported foodborne illness. Our results indicate that reported washing of hands with soap always before food preparation leads to a reduction in the probability of reported foodborne illness. [Contact: Linda Verrill ]
Consumer Vegetable and Fruit Washing Practices in the United States, 2006 and 2010. 2012. Linda Verrill, Amy M. Lando, and Kellie M. O'Connell. Food Protection Trends 32(4):164-172.
Vegetables and fruits may become contaminated with pathogens anywhere along the farm-to-plate continuum. There-fore, the FDA recommends that vegetables and fruits that have not already been washed be washed by the consumer before slicing or consuming them. The FDA included in its 2006 and 2010 Food Safety Survey a series of questions about purchasing and washing of strawberries, tomatoes, cantaloupes, and bagged, pre-cut lettuce. The Food Safety Survey is a telephone survey tracking consumers' knowledge, attitudes and behaviors related to food safety. In 2006, of those who buy these products, 98% wash strawberries, 97% wash tomatoes, 57% wash cantaloupes and 54% wash bagged pre-cut lettuce. Overall, for both years, more women than men wash cantaloupes, and more men than women wash bagged pre-cut lettuce. Cantaloupe washing declined from 2006 to 2010 for men, while lettuce washing increased for women in the same period. Targeted education campaigns should emphasize the importance of washing produce, especially fruits with hard rinds. [Contact: Linda Verrill ]
Trends in Ownership and Usage of Food Thermometers in the United States, 1998 through 2010. 2012. Amy M. Lando and Cary C. Chen. Journal of Food Protection 75(3):556-562.
Food safety research has shown that the use of a food thermometer is the best way to ensure that meat, poultry, and other foods reach an internal temperature sufficient to destroy foodborne pathogens. The 1998, 2001, 2006, and 2010 Food Safety Surveys were used to analyze changes in food thermometer ownership and usage for roasts, chicken parts, and hamburgers in the United States. A probit regression model was used to evaluate differing trends in ownership across demographic subgroups, and probit models with sample selection were used to evaluate differing trends in food thermometer usage for roasts, chicken parts, and hamburgers. The Food Safety Surveys are nationally representative telephone surveys tracking consumers' food safety attitudes and behaviors. Findings from these surveys indicate that the percentage of consumers who own food thermometers has increased from 49% in 1998 to 70% in 2010 (P < 0.05). The use of food thermometers has also increased over this time period but varies by food type. Of those who own food thermometers, a higher percentage reported using thermometers for roasts (76% in 1998 and 82% in 2010, P < 0.05) than for chicken parts (33% in 1998 and 53% in 2010, P < 0.05) and hamburgers (14% in 1998 and 23% in 2010, P < 0.05). The results also show that men, non-Hispanic whites, those with some college education or higher, those with higher incomes, and those 65 years and older were more likely to own food thermometers. After controlling for food thermometer ownership, those aged 18 to 29 years were more likely to use a food thermometer for roasts and chicken parts than those aged 65 to 101 years. The results suggest that educational programs encouraging food thermometer usage should focus first on food thermometer ownership. [Contact: Amy Lando ]
Trends in U.S. Consumers’ Safe Handling and Consumption of Food and Their Risk Perceptions, 1988 through 2010. 2011. Sara B. Fein, Amy M. Lando, Alan S. Levy, Mario F. Teisl, and Caroline Noblet. Journal of Food Protection 74(9):1513-1523 .
Although survey results measuring the safety of consumers’ food handling and risky food consumption practices have been published for over 20 years, evaluation of trends is impossible because the designs of published studies are not comparable. The Food Safety Surveys used comparable methods to interview U.S. adults by telephone in 1988, 1993, 2001, 2006, and 2010 about food handling (i.e., cross-contamination prevention) and risky consumption practices (eating raw or undercooked foods from animals) and perceived risk from foodborne illness. Sample sizes ranged from 1,620 to 4,547. Responses were analyzed descriptively, and four indices measuring meat, chicken, and egg cross-contamination, fish cross-contamination, risky consumption, and risk perceptions were analyzed using generalized linear models. The extent of media coverage of food safety issues was also examined. We found a substantial improvement in food handling and consumption practices and an increase in perceived risk from foodborne illness between 1993 and 1998. All indices were stable or declined between 1998 and 2006. Between 2006 and 2010, the two safe food handling practice indices increased significantly, but risk perceptions did not change, and safe consumption declined. Women had safer food handling and consumption practices than men. The oldest and youngest respondents and those with the highest education had the least safe food handling behaviors. Changes in safety of practices over the survey years are consistent with the change in the number of media stories about food safety in the periods between surveys. This finding suggests that increased media attention to food safety issues may raise awareness of food safety hazards and increase vigilance in food handling by consumers. [Contact: Amy Lando ]
Developing Consumer-focused Risk Communication Strategies Related to Food Terrorism. 2011. Sara Eggers, Linda Verrill, Cory M. Bryant, and Sarah L. Thorne. International Journal of Food Safety, Nutrition and Public Health 4(1):45-62.
Risk communication strategies related to food terrorism (FT) threats should reflect an in-depth understanding of consumers’ perceptions, priorities, and information needs related to those threats. To support development of communication strategies, we used a mental models approach to risk communication method to design, conduct and analyse 50 semi-structured telephone interviews with US adults. Interviewees generally lacked well-defined mental models specific to FT, and, instead, drew on their perceptions of terrorism in general, accidental contamination, product recalls, and emergency preparedness. Assessments of their personal threat of FT were influenced by their beliefs about the nature of terrorism, their confidence in government and the food system to prevent and respond to terrorism threats, and their personal control over food choices. These qualitative research results support guidance for developing and implementing consumer-focused FT risk communications strategies. [Contact: Linda Verrill ]
Awareness and Knowledge of Methylmercury in Fish in the United States. 2011. Amy M. Lando, and Yuanting Zhang. Environmental Research 111(3):442-450.
In the 1970s several states in the Great Lakes region became concerned about mercury contamination in lakes and rivers and were the first to issue local fish consumption advisories. In 2001, the Food and Drug Administration (FDA) advised pregnant women, nursing mothers, young children, and women who may become pregnant not to consume shark, swordfish, king mackerel, and tilefish and recommended that these women not exceed 12 ounces of other fish per week. In 2004, FDA reissued this advice jointly with the U.S. Environmental Protection Agency (EPA) and modified it slightly to provide information about consumption of canned tuna and more details about consumption of recreationally caught fish. Though several studies have examined consumers’ awareness of the joint FDA and EPA advisory as well as different state advisories, few used representative data. We examined the changes in awareness and knowledge of mercury as a problem in fish using the pooled nationally representative 2001 and 2006 Food Safety Surveys (FSS) with sample sizes of 4482 in 2001 and 2275 in 2006. Our results indicated an increase in consumers’ awareness of mercury as a problem in fish (69% in 2001 to 80% in 2006, p<.001). In our regression models, we found that in both years, parents having children less than 5 years of age were more aware of mercury in fish and knowledgeable about the information contained in the national advisories about mercury in fish (p<.01) than other adults. In both 2001 and 2006, women of childbearing age (aged 18–45) were less aware and knowledgeable about this information than other women. However, women of all age groups had larger gains in awareness and knowledge than their male counterparts during this time. Participants’ race, education, income, region, fish preparation experiences, having a foodborne illness in the past year, and risk perceptions about the safety of food were significant predictors of their awareness and knowledge. [Contact: Amy Lando ]
Food Safety Perceptions and Practices of Older Adults. 2011. Amy L. Anderson, Linda A. Verrill, and Nadine R. Sahyoun. Public Health Reports 126:220-227.
Older adults are considered more vulnerable to foodborne illness due to lowered immune function. We compared the food safety perceptions and practices of older and younger adults and determined associations with demographic characteristics. We focused on 1,317 participants ≥60 years of age from the U.S. Food and Drug Administration’s 2006 Food Safety Survey, a telephone survey of a nationally representative sample of American consumers. We used data on participants ≥60 years of age to compare younger and older adults, and used Pearson’s Chi-square tests to determine whether perceptions and practices differed by age, gender, level of education, living arrangement, and race/ethnicity. We conducted multiple logistic regression analysis to assess relationships of demographic characteristics and food safety perceptions with food safety practices of older adults. We found that adults ≥60 years of age were more likely to follow recommended food safety practices than those <60 years of age. Sixty-six percent of adults ≥60 years of age reported eating potentially hazardous foods in the past year compared with 81% of adults <60 years of age. Among people ≥60 years of age, women, those with less education, and nonwhite individuals generally had better food safety practices and a greater awareness of food safety risk. These findings suggest that certain subsets of the older adult population are less likely to follow recommended food safety practices and, thus, are at greater risk of foodborne illness. Food safety education for older adults should target men and those with more education and higher incomes. [Contact: Linda Verrill ]
Practice-specific risk perceptions and self-reported food safety practices. 2008. Alan S. Levy, Conrad J. Choinière, and Sara B. Fein. Risk Analysis 28(3):749-761.
The relationship between risk perception and risk avoidance is typically analyzed using self-reported measures. However, in domains such as driving or food handling, the validity of responses about usual behavior is threatened because people think about the situations in which they are self-aware, such as when they encounter a hazard. Indeed, researchers have often noted a divergence between what people say about their behavior and how they actually behave. Thus, in order to draw conclusions about risk perceptions and risk avoidance from survey data, it is important to identify particular cognitive elements, such as those measured by questions about risk and safety knowledge, risk perceptions, or information search behavior, which may be effective antecedents of self-reported safety behavior. It is also important to identify and correct for potential sources of bias that may exist in the data. The authors analyze the Food and Drug Administration's 1998 Food Safety Survey to determine whether there are consistent cognitive antecedents for three types of safe food practices: preparation, eating, and cooling of foods. An assessment of measurement biases shows that endogeneity of food choices affects reports of food preparation. In addition, response bias affects reports of cooling practices as evidenced by its relation to knowledge and information search, a pattern of cognitive effects unique to cooling practices. After correcting for these biases, results show that practice-specific risk perceptions are the primary cognitive antecedents of safe food behavior, which has implications for the design of effective education messages about food safety. [Contact: Amy Lando ]
Consumer Decisions on Storage of Packaged Foods. 2007. Amy M. Lando, and Sara B. Fein. Food Protection Trends 27(5): 307-313.
We investigate the causes of consumer uncertainty regarding storage of packaged foods by examining the characteristics of the consumers, the type of food products and packaging, and the where the product was stored at purchase. Consumers’ self-reported refrigeration practices from the 1998 Food Safety Survey are analyzed descriptively and by logistic regression. Eleven percent of the 2,001 respondents reported difficulty during the past three months in deciding whether to refrigerate a packaged food. When consumers do have difficulty, it is likely that the products either are new to them or need to be stored in an unexpected way. The most likely to report uncertainty about whether to refrigerate were people of middle age and people likely to be more attuned to food safety issues – those who have some college or higher education, who look at many sources of food information, and who thought that a household member had a recent foodborne illness. The results suggest that additional education may be needed to inform consumers about proper refrigeration and that storage information on packages is particularly important for foods that are stored at room temperature until opened but that then need refrigeration. [Contact: Amy Lando ]
Awareness and Perceived Risk of Pesticide and Antibiotic Residues in Food: Socioeconomic Variations Among US Consumers. 2006. Steven T. Yen, Kimberly L. Jensen, and Chung-Tung J. Lin. Food Protection Trends 26(9): 654-661.
We investigate American consumers’ awareness and perceived risk of pesticide and antibiotic residues in food, and how socioeconomic characteristics affect the awareness and risk perception. Based on a 2001 national telephone survey, we employ a statistical approach that accommodates correlations between the two issues and the fact that perceived risk was collected in the survey only from those who were aware of a given issue. Most individuals have heard of pesticide residues but only some have heard of antibiotic residues, though the latter were perceived as a more serious food safety problem than the former. Awareness of one residue problem is associated with a lower perceived risk of the other problem. Income, age, college-or-more education, and being the main meal preparers are related to more awareness of the two issues. Awareness of pesticide residues is lower among Hispanics and blacks, while awareness of antibiotic residues is lower among blacks. Among those who had heard of pesticide residues, the perceived risk of the residues was higher with higher income and being a Midwest resident and lower with a larger number of adults in the household, being a female, older, Hispanic or black, and being a main meal preparer in the household. Among those who had heard of antibiotic residues, the perceived risk of the residues was higher with higher income and being a Hispanic and lower being a female or black. Results also suggest that our statistical approach is worth considering in future research of similar topics. [Contact: Chung-Tung Lin ]
Awareness of Foodborne Pathogens Among US Consumers. 2005. Chung-Tung J. Lin, Kimberly L. Jensen, and Steven T. Yen. Food Quality and Preference 16(5): 401-412.
Each year in the United States, microbial pathogens cause millions of cases of foodborne disease and result in many hospitalizations and deaths. Effective consumer education programs to promote safer food handling practices and other averting behaviors may benefit from consumer awareness of microbial pathogens. This paper investigates US consumers’ awareness of four major microbial pathogens (Salmonella, Campylobacter, Listeria and Escherichia coli) as food safety problems, using a multivariate probit model. The awareness varies among pathogens and the variations appear to be related to differences in the number and severity of illnesses associated with these pathogens. Our findings suggest that awareness of microbial pathogens is associated with food safety perceptions, awareness of potentially risky foods and substances associated with potential food safety hazards, food safety related behaviors, and demographics. There are differentiated effects of variables on awareness of the four pathogens. [Contact: Chung-Tung Lin ]
Consumers' Assessment of the Food Safety Problem for Meals Prepared at Home and Reactions to Food Safety Labeling. 2001. Brian Roe, Mario F. Teisl, Alan S. Levy, Kevin Boyle, Mark L Messonnier, T. Lynn Riggs, Melissa J. Herrmann, and Felicia M. Newman. Journal of Food Products Marketing 6(4):9-26.
To identify if differences in food safety risk can be effectively and credibly communicated, we conducted eight focus groups. This article summarizes these focus groups and reports how consumers frame the issues surrounding the food safety problem and how consumers react to label-based communications of food safety characteristics. We find consumers have broad, moderate food safety concerns, a wide but spotty understanding of food borne illness prevention and consequences, and a healthy skepticism concerning food safety claims. We identity two forms of labeling that show promise with regard to consumer acceptance and credibility in communicating brand-level and package-level differences in the risk of food borne illness and discuss implications for consumer valuation of such differences. [Contact: Amy Lando ]
Foodborne Illness: Perceptions, Experience, and Preventive Behaviors in the United States. 1995. Sara B. Fein, Chung-Tung J. Lin, and Alan S. Levy. Journal of Food Protection 58(12):1405-1411.
Data from national telephone surveys conducted in 1988 and 1993 were used to describe consumer perceptions of foodborne illness. The 1993 data were also used to assess the relationship between the perception that a foodborne illness had recently been experienced and awareness, concern, knowledge, and behavior related to food safety. Respondents described foodborne disease primarily as a minor illness without fever that occurs within a day of eating contaminated food prepared in a restaurant. However, several common pathogens have latency period longer than a day, and experts on foodborne disease estimate that most cases of foodborne illness originate from foods prepared at home. In both surveys, people 18 to 39 years of age were more likely than those in other age groups to believe they had experienced a foodborne illness. In 1993, people with at least some college education were more likely to believe they had experienced foodborne illness than were people with less education. People who believed they had experienced foodborne illness had greater awareness of foodborne microbes and concern about food safety issues, were more likely to eat raw protein foods from animals, and were less likely to practice safe food handling than were those who did not perceive that they had experienced such an illness. [Contact: Chung-Tung Lin ]
Prevalence of Selected Food Consumption and Preparation Behaviors Associated with Increased Risks of Food-borne Disease. 1995. Karl C. Klontz, Babgaleh B. Timbo, Sara Fein, and Alan S. Levy. Journal of Food Protection 58(8):927-930.
Although not well quantified, a portion of food-borne illness results from voluntary behaviors that are entirely avoidable, such as eating raw foods of animal origin or engaging in unsafe food preparation practices. A telephone survey of 1,620 respondents was conducted to assess the prevalence of selected self-reported food consumption and preparation behaviors associated with increased risks of food-borne illness and the demographic characteristics related to such behaviors. The percentages of survey respondents who reported consuming raw foods of animal origin were 53%, raw eggs; 23%, undercooked hamburgers; 17%, raw clams or oysters; and 8%, raw sushi or ceviche. A fourth of the respondents said that after cutting raw meat or chicken, they use the cutting board again without cleaning it. Safer food consumption and preparation behaviors were consistently reported by persons who were female, were at least 40 years old, and had a high school education or less. These findings suggest that risky food consumption and preparation behaviors are common in the United States and that educational campaigns aimed at changing these behaviors may need to be targeted to specific groups of persons. [Contact: Amy Lando ]
Consumer Knowledge of Foodborne Microbial Hazards and Food-Handling Practices. 1995. Sean F. Altekruse, Debra A. Street, Sara B. Fein, and Alan S. Levy. Journal of Food Protection 59(3)287-294.
A national telephone survey was conducted of 1,620 randomly selected U.S. residents who spoke English, were at least 18 years old, and resided in households with kitchen facilities. Respondents were interviewed about their recognition of foodborne pathogens, foods at risk for transmitting infection, knowledge of safe food handling, and food handling practices. One-third of the respondents who prepared meals reported unsafe food hygiene practices: e.g., they did not wash hands or take precautions to prevent cross-contamination from raw meat. Unsafe practices were reported more often by men, persons 18 to 29 years of age and occasional food preparers than by women, persons 30 years old or older, and frequent food preparers. Respondents who identified a food vehicle for Salmonella spp. were more likely to report washing their hands and cleaning cutting boards after preparing raw meat and poultry. The results raise concerns about consumer food-handling practices. The influence of food safety training, food-handling experience, and age on food-handling practices should be studied further. Awareness of a food vehicle for Salmonella spp., for example, may indicate knowledge of the etiology of foodborne disease that promotes safe food handling. Understanding the factors associated with safe food handling will assist in development of effective safe-food instruction programs. [Contact: Amy Lando ]
- Patient Care & Health Information
- Diseases & Conditions
- Food poisoning
Food poisoning, a type of foodborne illness, is a sickness people get from something they ate or drank. The causes are germs or other harmful things in the food or beverage.
Symptoms of food poisoning often include upset stomach, diarrhea and vomiting. Symptoms usually start within hours or several days of eating the food. Most people have mild illness and get better without treatment.
Sometimes food poisoning causes severe illness or complications.
Products & Services
- A Book: Mayo Clinic Book of Home Remedies
Symptoms vary depending on what is causing the illness. They may begin within a few hours or a few weeks depending on the cause.
Common symptoms are:
- Upset stomach.
- Diarrhea with bloody stools.
- Stomach pain and cramps.
Less often food poisoning affects the nervous system and can cause severe disease. Symptoms may include:
- Blurred or double vision.
- Loss of movement in limbs.
- Problems with swallowing.
- Tingling or numbness of skin.
- Changes in sound of the voice.
When to see a doctor
Infants and children.
Vomiting and diarrhea can quickly cause low levels of body fluids, also called dehydration, in infants and children. This can cause serious illness in infants.
Call your child's health care provider if your child's symptoms include vomiting and diarrhea and any of the following:
- Unusual changes in behavior or thinking.
- Excessive thirst.
- Little or no urination.
- Diarrhea that lasts more than a day.
- Vomiting often.
- Stools that have blood or pus.
- Stools that are black or tarry.
- Severe pain in the stomach or rectum.
- Any fever in children under 2 years of age.
- Fever of 102 degrees Fahrenheit (38.9 degrees Celsius) or higher in older children.
- History of other medical problems.
Adults should see a health care provider or get emergency care if the following occur:
- Nervous system symptoms, such as blurry vision, muscle weakness and tingling of skin.
- Changes in thinking or behavior.
- Fever of 103 degrees Fahrenheit (39.4 degrees Celsius).
- Diarrhea that lasts more than three days.
- Symptoms of dehydration — excessive thirst, dry mouth, little or no urination, severe weakness, dizziness, or lightheadedness.
There is a problem with information submitted for this request. Review/update the information highlighted below and resubmit the form.
From Mayo Clinic to your inbox
Sign up for free and stay up to date on research advancements, health tips, current health topics, and expertise on managing health. Click here for an email preview.
Error Email field is required
Error Include a valid email address
To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
Thank you for subscribing!
You'll soon start receiving the latest Mayo Clinic health information you requested in your inbox.
Sorry something went wrong with your subscription
Please, try again in a couple of minutes
Many germs or harmful things, called contaminants, can cause foodborne illnesses. Food or drink that carries a contaminant is called "contaminated." Food can be contaminated with any of the following:
- Parasites that can live in the intestines.
- Poisons, also called toxins.
- Bacteria that carry or make toxins.
- Molds that make toxins.
Understanding terms
The term "food poisoning" is commonly used to describe all foodborne illnesses. A health care provider might use these terms to be more specific:
- "Foodborne illnesses" means all illnesses from any contaminated food or beverage.
- "Food poisoning" means illness specifically from a toxin in food. Food poisoning is a type of foodborne illness.
How food becomes contaminated
Food can be contaminated at any point from the farm or fishery to the table. The problem can begin during growing, harvesting or catching, processing, storing, shipping, or preparing.
Food can be contaminated any place it's handled, including the home, because of:
- Poor handwashing. Feces that remains on the hands after using the toilet can contaminate food. Other contaminants can be transferred from hands during food preparation or food serving.
- Not disinfecting cooking or eating areas. Unwashed knives, cutting boards or other kitchen tools can spread contaminants.
- Improper storage. Food left out for too long at room temperature can become contaminated. Food stored in the refrigerator for too long can spoil. Also, food stored in a refrigerator or freezer that is too warm can spoil.
Common causes
The following table shows common causes of foodborne illnesses, the time from exposure to the beginning of symptoms and common sources of contamination.
Other sources
Bacteria that cause foodborne illnesses can also be found in swimming pools, lakes, ponds, rivers and seawater. Also, some bacteria, such as E. coli, may be spread by exposure to animals carrying the disease.
Risk factors
Anyone can get food poisoning. Some people are more likely to get sick or have more-serious disease or complications. These people include:
- Infants and children.
- Pregnant people.
- Older adults.
- People with weakened immune systems due to another disease or treatments.
Complications
In most healthy adults, complications are uncommon. They can include the following.
Dehydration
The most common complication is dehydration. This a severe loss of water and salts and minerals. Both vomiting and diarrhea can cause dehydration.
Most healthy adults can drink enough fluids to prevent dehydration. Children, older adults, and people with weakened immune systems or other illnesses may not be able to replace the fluids they've lost. They are more likely to become dehydrated.
People who become dehydrated may need to get fluids directly into the bloodstream at the hospital. Severe dehydration can cause organ damage, other severe disease and death if not treated.
Complications of systemic disease
Some contaminants can cause more widespread disease in the body, also called systemic disease or infection. This is more common in people who are older, have weakened immune systems or other medical conditions. Systemic infections from foodborne bacteria may cause:
- Blood clots in the kidneys. E. coli can result in blood clots that block the kidneys' filtering system. This condition, called hemolytic uremic syndrome, results in the sudden failure of the kidneys to filter waste from the blood. Less often, other bacteria or viruses may cause this condition.
- Bacteria in the bloodstream. Bacteria in the blood can cause disease in the blood itself or spread disease to other parts of the body.
- Meningitis. Meningitis is inflammation that may damage the membranes and fluid surrounding the brain and spinal cord.
- Sepsis. Sepsis is an overreaction of the immune system to systemic disease that damages the body's own tissues.
Pregnancy complications
Illness from the listeria bacteria during pregnancy can result in:
- Miscarriage or stillbirth.
- Sepsis in the newborn.
- Meningitis in the newborn.
Rare complications
Rare complications include conditions that may develop after food poisoning, including:
- Arthritis. Arthritis is swelling, tenderness or pain in joints.
- Irritable bowel syndrome. Irritable bowel syndrome is a lifelong condition of the intestines that causes pain, cramping and irregular bowel movements.
- Guillain-Barre syndrome. Guillain-Barre syndrome is an immune system attack on nerves that can result in tingling, numbness and loss of muscle control.
- Breathing difficulties. Rarely, botulism can damage nerves that control the muscles involved in breathing.
To prevent food poisoning at home:
- Handwashing. Wash your hands with soap and water for at least 20 seconds. Do this after using the toilet, before eating, and before and after handling food.
- Wash fruits and vegetables. Rinse fruits and vegetables under running water before eating, peeling or preparing.
- Wash kitchen utensils thoroughly. Wash cutting boards, knives and other utensils with soapy water after contact with raw meats or unwashed fruits and vegetables.
- Don't eat raw or undercooked meat or fish. Use a meat thermometer to make sure meat is cooked enough. Cook whole meats and fish to at least 145 F (63 C) and let rest for at least three minutes. Cook ground meat to at least 160 F (71 C). Cook whole and ground poultry to at least 165 F (74 C).
- Refrigerate or freeze leftovers. Put leftovers in covered containers in the refrigerator right after your meal. Leftovers can be kept for 3 to 4 days in the refrigerator. If you don't think you'll eat them within four days, freeze them right away.
- Cook leftovers safely. You can safely thaw frozen food three ways. You can microwave it. You can move it to the refrigerator to thaw overnight. Or you can put the frozen food in a leakproof container and put it in cold water on the counter. Reheat leftovers until the internal temperature reaches 165 degrees Fahrenheit (74 degrees Celsius).
- Throw it out when in doubt. If you aren't sure if a food has been prepared, served or stored safely, discard it. Even if it looks and smells fine, it may not be safe to eat.
- Throw out moldy food. Throw out any baked foods with mold. Throw out moldy soft fruits and vegetables, such as tomatoes, berries or peaches. And throw away any nuts or nut products with mold. You can trim away mold from firm foods with low moisture, such as carrots, bell peppers and hard cheeses. Cut away at least 1 inch (2.5 centimeters) around the moldy part of the food.
- Clean your refrigerator. Clean the inside of the refrigerator every few months. Make a cleaning solution of 1 tablespoon (15 milliliters) of baking soda and 1 quart (0.9 liters) of water. Clean visible mold in the refrigerator or on the door seals. Use a solution of 1 tablespoon (15 milliliters) of bleach in 1 quart (0.9 liters) of water.
Safety for at-risk people
Food poisoning is especially serious during pregnancies and for young children, older adults and people with weakened immune systems. These illnesses may be life-threatening. These individuals should avoid the following foods:
- Raw or undercooked meat, poultry, fish, and shellfish.
- Raw or undercooked eggs or foods that may contain them, such as cookie dough and homemade ice cream.
- Raw sprouts, such as alfalfa, bean, clover and radish sprouts.
- Unpasteurized juices and ciders.
- Unpasteurized milk and milk products.
- Soft cheeses, such as feta, brie and Camembert; blue-veined cheese; and unpasteurized cheese.
- Refrigerated pates and meat spreads.
- Uncooked hot dogs, luncheon meats and deli meats.
- Foodborne germs and illnesses. U.S. Centers for Disease Control and Prevention. https://www.cdc.gov/foodsafety/foodborne-germs.html. Accessed Nov. 7, 2022.
- Definition & facts of food poisoning. National Institute of Diabetes and Digestive and Kidney Diseases. https://www.niddk.nih.gov/health-information/digestive-diseases/food-poisoning/definition-facts. Accessed Nov. 7, 2022.
- Symptoms & causes of food poisoning. National Institute of Diabetes and Digestive and Kidney Diseases. https://www.niddk.nih.gov/health-information/digestive-diseases/food-poisoning/symptoms-causes. Accessed Nov. 7, 2022.
- LaRocque R. Causes of acute infectious diarrhea and other foodborne illnesses in resource-rich settings. https://www.uptodate.com/contents/search. Accessed Nov. 7, 2022.
- Bennett JE, et al. Mandell, Douglas, and Bennett's Principles and Practice of Infectious Diseases. 9th ed. Elsevier; 2020. https://www.clinicalkey.com. Accessed Nov. 7, 2022.
- Schmitt BD. Pediatric Telephone Protocols: Office Version. 17th ed. American Academy of Pediatrics; 2021.
- Fever. American College of Emergency Physicians. https://www.emergencyphysicians.org/article/know-when-to-go/fever. Accessed Nov. 30, 2022.
- Bacteria and viruses. FoodSafety.gov. U.S. Department of Health and Human Services. https://www.foodsafety.gov/food-poisoning/bacteria-and-viruses. Accessed Nov. 16, 2022.
- Kellerman RD, et al. Foodborne illnesses. In: Conn's Current Therapy 2022. Elsevier; 2022. https://www.clinicalkey.com. Accessed Nov. 13, 2022.
- Goldman L, et al., eds. Giardiasis. Goldman-Cecil Medicine. 26th ed. Elsevier; 2020. https://www.clinicalkey.com. Accessed Nov. 13, 2022.
- Diagnosis of food poisoning. National Institute of Diabetes and Digestive and Kidney Diseases. https://www.niddk.nih.gov/health-information/digestive-diseases/food-poisoning/diagnosis. Accessed Nov. 7, 2022.
- LaRocque R. Approach to the adult with acute diarrhea in resource-rich settings. https://www.uptodate.com/contents/search. Accessed Nov. 7, 2022.
- Treatment for food poisoning. National Institute of Diabetes and Digestive and Kidney Diseases. https://www.niddk.nih.gov/health-information/digestive-diseases/food-poisoning/treatment. Accessed Nov. 7, 2022.
- Eating, diet and nutrition for food poisoning. National Institute of Diabetes and Digestive and Kidney Diseases. https://www.niddk.nih.gov/health-information/digestive-diseases/food-poisoning/eating-diet-nutrition. Accessed Nov. 20, 2022.
- Four steps to food safety: Clean, separate, cook, chill. U.S. Centers for Disease Control and Prevention. https://www.cdc.gov/foodsafety/keep-food-safe.html. Accessed Nov. 7, 2022.
- Leftovers and food safety. U.S. Department of Agriculture. https://www.fsis.usda.gov/food-safety/safe-food-handling-and-preparation/food-safety-basics/leftovers-and-food-safety. Accessed Nov. 20, 2022.
- Foods that can cause food poisoning. U.S. Centers for Disease Control and Prevention. https://www.cdc.gov/foodsafety/foods-linked-illness.html. Accessed Nov. 20, 2022.
- Molds on food: Are they dangerous? Food Safety and Inspection Service. U.S. Department of Agriculture. https://www.fsis.usda.gov/food-safety/safe-food-handling-and-preparation/food-safety-basics/molds-food-are-they-dangerous Accessed Dec. 1, 2022.
News from Mayo Clinic
- Mayo Clinic Minute: Tips for safer picnics May 26, 2023, 03:00 p.m. CDT
- Mayo Clinic Minute: Does one moldy berry spoil the whole bunch? March 09, 2023, 03:30 p.m. CDT
- Mayo Clinic Minute: Food recalls and sickness July 11, 2022, 04:00 p.m. CDT
- Symptoms & causes
- Diagnosis & treatment
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
Your gift holds great power – donate today!
Make your tax-deductible gift and be a part of the cutting-edge research and care that's changing medicine.
Disclaimer: Early release articles are not considered as final versions. Any changes will be reflected in the online version in the month the article is officially released.
Volume 30, Number 6—June 2024
Research Letter
Foodborne disease outbreaks linked to foods eligible for irradiation, united states, 2009–2020.
Suggested citation for this article
Food irradiation can reduce foodborne illnesses but is rarely used in the United States. We determined whether outbreaks related to Campylobacter , Salmonella , Escherichia coli , and Listeria monocytogenes were linked to irradiation-eligible foods. Of 482 outbreaks, 155 (32.2%) were linked to an irradiation-eligible food, none of which were known to be irradiated.
Food irradiation has been studied globally for decades and is a safe, effective means of reducing foodborne illness–causing pathogens, sterilizing insects, delaying ripening or sprouting, and extending shelf life ( 1 , 2 ). The US Food and Drug Administration has approved various foods for irradiation, including meat, poultry, fresh shell eggs, and spices ( 2 ) ( Appendix Table). However, irradiation has not been widely adopted in the United States because of large fixed costs and the perception of consumer unwillingness to purchase irradiated food ( 3 ). Estimates of the amount of irradiated food available in the United States are scarce, but as of 2010, approximately one third of spices consumed and <0.1% of imported fruit, vegetables, and meats were irradiated ( 3 ).
Campylobacter , Salmonella , Escherichia coli , and Listeria monocytogenes are among the most common bacterial foodborne pathogens causing illnesses, hospitalizations, and death in the United States ( 4 ) and can be neutralized by irradiation at sufficient doses ( 5 ). We identified outbreaks caused by these pathogens and linked to irradiation-eligible foods; then, we determined whether any of the foods had been irradiated.
In the United States, the Foodborne Disease Outbreak Surveillance System (FDOSS) collects information from state, local, and territorial health departments about foodborne disease outbreaks. The National Outbreak Reporting System, launched in 2009, reports information gathered by FDOSS, including food processing methods such as shredding, pasteurizing, or irradiation. We searched for foodborne disease outbreaks reported and finalized through FDOSS and the National Outbreak Reporting System as of February 4, 2022, for which the date of first illness onset occurred during 2009–2020 and a confirmed pathogen was Campylobacter , Salmonella , E. coli , or Listeria monocytogenes. A foodborne disease outbreak was defined as > 2 illnesses linked to a common exposure with evidence suggesting a food source. FDOSS variables we examined included method of processing, food vehicle, Interagency Food Safety Analytics Collaboration (IFSAC) food category, and the number of estimated primary illnesses, hospitalizations, and deaths. We grouped outbreaks by IFSAC category and irradiation approval status (eligible, some foods eligible, not yet eligible, or undetermined) ( Appendix Table). We conducted a literature review to identify outbreaks not captured through FDOSS. We obtained foods approved for irradiation for pathogen reduction and approval years from the Code of Federal Regulations 21 Part 179 ( Appendix Table).
In FDOSS, we identified 2,153 foodborne outbreaks during 2009–2020 caused by Campylobacter , Salmonella , E. coli , or Listeria monocytogenes . Of those, 482 (22.4%) included information regarding processing methods other than unknown or a missing value; none had irradiation listed as a processing method. Of the 482 outbreaks, 155 (32.2%) were linked to a food eligible for irradiation when the onset of the first reported illness occurred; those outbreaks resulted in 3,512 illnesses, 463 hospitalizations, and 10 deaths ( Appendix Table). The most common sources were chicken (52 outbreaks), beef (31), and eggs (29), comprising 72% (112/155) of outbreaks linked to irradiation-eligible foods.
During our literature search, we identified 1 outbreak linked to food that might have included an irradiated ingredient. During 2009–2010, Salmonella enterica serotype Montevideo was found in imported pepper used in ready-to-eat salami ( 6 ). Some of the manufacturer’s pepper was reportedly irradiated, but some was not. Whether the implicated product contained irradiated pepper is unclear. Irradiation was not reported as a processing method for the outbreak in FDOSS. After consultation with the Centers for Disease Control and Prevention outbreak investigation team, we determined there was insufficient evidence to link that outbreak to irradiated pepper.
The illnesses, hospitalizations, and deaths associated with outbreaks linked to irradiation-eligible foods might have been prevented or reduced had these foods been irradiated. Irradiation has repeatedly been proposed as a strategy to reduce foodborne disease outbreaks ( 5 , 7 , 8 ). Irradiation typically eliminates a large proportion of pathogenic microorganisms. The efficacy of irradiation depends on factors like temperature and water content ( 9 ). Food may become contaminated after irradiation. Irradiation can be a useful tool in improving food safety complementary to existing food safety practices. Consumer demand for irradiated foods may be increased through education ( 10 ).
The first limitation of our study is that IFSAC food categories do not always correspond to food groups approved for irradiation by the US Food and Drug Administration ( Appendix Table); therefore, misclassification of irradiation approval status might have occurred for some foods. Reporting of outbreaks to FDOSS is voluntary, and processing method information was frequently missing, so irradiation might have been underreported or unrecognized by public health partners because of limited knowledge of irradiation or unfamiliarity with labeling. For outbreaks with multiple etiologies including a pathogen other than the 4 of interest, irradiation might not have reduced those pathogens.
We identified 155 Campylobacter , Salmonella , E. coli , or Listeria monocytogenes outbreaks with a known method of processing that were linked to irradiation-eligible foods during 2009–2020; none of the implicated foods were reported as irradiated. These results suggest that some outbreaks could be prevented or mitigated through irradiation. Prioritizing food irradiation efforts, particularly for chicken, beef, and eggs, could substantially reduce outbreaks and illnesses.
Dr. Zlotnick is an Oak Ridge Institute for Science and Education Fellow at the Centers for Disease Control and Prevention, Atlanta. Her work focuses on the prevention of zoonotic disease originating in food or animal contact.
Acknowledgments
We thank Michelle Canning, Laura Gieraltowski, Lane Highbarger, and Jacqueline Roshelli Baker for their assistance.
This project was supported in part by an appointment to the Research Participation Program at the Centers for Disease Control and Prevention administered by the Oak Ridge Institute for Science and Education through an interagency agreement between the US Department of Energy and the Centers for Disease Control and Prevention.
- High-dose irradiation: wholesomeness of food irradiated with doses above 10 kGy. Report of a Joint FAO/IAEA/WHO Study Group. World Health Organ Tech Rep Ser . 1999 ; 890 : i – vi, 1–197 . PubMed Google Scholar
- Food and Drug Administration . Food irradiation: what you need to know. 2022 [ cited 2022 Jun 23 ]. https://www.fda.gov/food/buy-store-serve-safe-food/food-irradiation-what-you-need-know
- Ferrier P . Irradiation of produce imports: small inroads, big obstacles. 2011 [ cited 2022 June 27 ]. https://www.ers.usda.gov/amber-waves/2011/june/irradiation-of-produce-imports
- Scallan E , Hoekstra RM , Angulo FJ , Tauxe RV , Widdowson MA , Roy SL , et al. Foodborne illness acquired in the United States—major pathogens. Emerg Infect Dis . 2011 ; 17 : 7 – 15 . DOI PubMed Google Scholar
- Tauxe RV . Food safety and irradiation: protecting the public from foodborne infections. Emerg Infect Dis . 2001 ; 7 ( Suppl ): 516 – 21 . DOI PubMed Google Scholar
- Gieraltowski L , Julian E , Pringle J , Macdonald K , Quilliam D , Marsden-Haug N , et al. Nationwide outbreak of Salmonella Montevideo infections associated with contaminated imported black and red pepper: warehouse membership cards provide critical clues to identify the source. Epidemiol Infect . 2013 ; 141 : 1244 – 52 . DOI PubMed Google Scholar
- Osterholm MT , Norgan AP . The role of irradiation in food safety. N Engl J Med . 2004 ; 350 : 1898 – 901 . DOI PubMed Google Scholar
- Gunther NW IV , Abdul-Wakeel A , Scullen OJ , Sommers C . The evaluation of gamma irradiation and cold storage for the reduction of Campylobacter jejuni in chicken livers. Food Microbiol . 2019 ; 82 : 249 – 53 . DOI PubMed Google Scholar
- World Health Organization . Safety and nutritional adequacy of irradiated food. Geneva: World Health Organization; 1994 [ cited 2022 Nov 16 ]. https://iris.who.int/handle/10665/39463
- Ablan M , Low MSF , Marshall KE , Devchand R , Koehler L , Hume H , et al. Focus groups exploring U.S. adults’ knowledge, attitudes, and practices related to irradiation as a food safety intervention, 2021. Food Prot Trends . 2023 ; 43 : 448 – 56 .
Suggested citation for this article : Zlotnick M, Eisenstein T, Robyn MP, Marshall KE. Foodborne disease outbreaks linked to foods eligible for irradiation, United States, 2009–2020. Emerg Infect Dis. 2024 Jun [ date cited ]. https://doi.org/10.3201/eid3006.230922
DOI: 10.3201/eid3006.230922
Table of Contents – Volume 30, Number 6—June 2024
Please use the form below to submit correspondence to the authors or contact them at the following address:
Marta Zlotnick, Centers for Disease Control and Prevention, 1600 Clifton Rd NE, Mail Stop H24-11, Atlanta, GA 30329-4018, USA
Comment submitted successfully, thank you for your feedback.
There was an unexpected error. Message not sent.
Exit Notification / Disclaimer Policy
- The Centers for Disease Control and Prevention (CDC) cannot attest to the accuracy of a non-federal website.
- Linking to a non-federal website does not constitute an endorsement by CDC or any of its employees of the sponsors or the information and products presented on the website.
- You will be subject to the destination website's privacy policy when you follow the link.
- CDC is not responsible for Section 508 compliance (accessibility) on other federal or private website.
Metric Details
Article views: 431.
Data is collected weekly and does not include downloads and attachments. View data is from .
What is the Altmetric Attention Score?
The Altmetric Attention Score for a research output provides an indicator of the amount of attention that it has received. The score is derived from an automated algorithm, and represents a weighted count of the amount of attention Altmetric picked up for a research output.
A third of US food outbreaks and 3,500 illnesses tied to non-irradiated eligible food

Manjurul / iStock
Of 482 US foodborne outbreaks caused by four common bacteria from 2009 to 2022, 32.2%—involving more than 3,500 sick people and 10 deaths—were linked to a food that could have undergone pathogen-neutralizing irradiation but did not, researchers from the Centers for Disease Control and Prevention reported yesterday in Emerging Infectious Diseases .
The investigators identified foodborne disease outbreaks reported to the Foodborne Disease Outbreak Surveillance System (FDOSS) and the National Outbreak Reporting System through February 2022. For outbreaks to be included in the study, the first illness had to have been reported from 2009 to 2020 and be tied to Campylobacter , Salmonella , Escherichia coli , or Listeria monocytogenes.
The team also reviewed the literature to identify outbreaks that FDOSS didn't capture. An outbreak was defined as at least two illnesses associated with common exposure to a food.
Food irradiation has been proven to be a safe, effective way to reduce foodborne illness–causing pathogens, sterilize insects, delay ripening or sprouting, and lengthen shelf life, the study authors said.
"The US Food and Drug Administration has approved various foods for irradiation, including meat, poultry, fresh shell eggs, and spices," they wrote. "However, irradiation has not been widely adopted in the United States because of large fixed costs and the perception of consumer unwillingness to purchase irradiated food."
Outbreaks led to 10 deaths
FDOSS listed 2,153 foodborne outbreaks caused by one of the four bacteria. Of those, 482 (22.4%) contained information on processing methods, none of which listed irradiation.
Estimates of the amount of irradiated food available in the United States are scarce, but as of 2010, approximately one third of spices consumed and <0.1% of imported fruit, vegetables, and meats were irradiated.
A total of 155 of 482 (32.2%) foodborne outbreaks involved an irradiation-eligible food that wasn't irradiated. The outbreaks resulted in 3,512 illnesses, 463 hospitalizations, and 10 deaths. The most common bacterial sources were chicken (52 outbreaks), beef (31), and eggs (29), which made up 72% of outbreaks tied to foods that could have been irradiated.
" Campylobacter , Salmonella , Escherichia coli , and Listeria monocytogenes are among the most common bacterial foodborne pathogens causing illnesses, hospitalizations, and death in the United States and can be neutralized by irradiation at sufficient doses," the researchers wrote.
"Estimates of the amount of irradiated food available in the United States are scarce, but as of 2010, approximately one third of spices consumed and <0.1% of imported fruit, vegetables, and meats were irradiated," they added.
Irradiation of commonly contaminated foods
Irradiation destroys large proportions of pathogens, but food may become contaminated after irradiation, the authors said. "Irradiation can be a useful tool in improving food safety complementary to existing food safety practices," they wrote. "Consumer demand for irradiated foods may be increased through education."
The team noted that outbreak reporting to FDOSS is voluntary, and processing method information is often not listed, so public health officials may not have reported or recognized outbreaks because they had limited knowledge of irradiation or weren't familiar with labeling practices.
"For outbreaks with multiple etiologies including a pathogen other than the 4 of interest, irradiation might not have reduced those pathogens," they wrote.
In summary, "These results suggest that some outbreaks could be prevented or mitigated through irradiation," the researchers concluded. "Prioritizing food irradiation efforts, particularly for chicken, beef, and eggs, could substantially reduce outbreaks and illnesses."
Related news
2023 e coli outbreak in kids in utah traced to untreated irrigation water.

Study cites role of age, sex in antibiotic-resistant infections

European data highlight resistance in zoonotic, indicator bacteria

CDC announces E coli outbreak tied to raw milk cheese, more charcuterie Salmonella cases

This week's top reads
Wastewater testing finds h5n1 avian flu in 9 texas cities.
Wastewater detections began in early March, and so far sequencing hasn't found any mutations linked to human adaptation.

CDC launches new influenza A wastewater dashboard; states report more H5N1 in dairy herds
The tracker will help with surveillance, but it doesn't distinguish the influenza A subtype or determine the source of the virus.

USDA experiments suggest H5N1 not viable in properly cooked ground beef
Federal officials said it's unclear if dairy cow outbreaks are peaking, and they haven't made much headway testing farm workers for avian flu virus.


Feds announces assistance for US farmers affected by H5N1 avian flu
The assistance is meant to both improve on-site biosecurity and address financial losses connected to lost milk production in herds affected by H5N1.

USDA confirms 3 more H5N1 outbreaks in dairy herds
Of the three newly confirmed outbreaks, two are in Michigan and one is in Idaho.
WHO describes MERS cluster in Saudi Arabia
The index case-patient, who died from his infection, shared a hospital room with the second patient identified.
Study: Before vaccines, 44% of COVID-19 patients in ICU died
The overall case-hospitalization rate among patients was 5.7%.

Global meta-analysis estimates 43% rate of multidrug resistance in COVID patients
A total of 76% of patients were prescribed antibiotics.
Data: Heart-failure patients have 82% better odds of living longer if vaccinated against COVID
Vaccinated patients also had a 47% lower risk of hospitalization for heart failure and a 13% reduced risk of infection over 6 months.

Hospital COVID patients 35% more likely to die than flu patients last winter, study suggests
The results should be interpreted in the context of twice as many hospitalizations for COVID than flu during the study period, the authors say.

Our underwriters
Unrestricted financial support provided by.

- Antimicrobial Resistance
- Chronic Wasting Disease
- All Topics A-Z
- Resilient Drug Supply
- Influenza Vaccines Roadmap
- CIDRAP Leadership Forum
- Roadmap Development
- Coronavirus Vaccines Roadmap
- Antimicrobial Stewardship
- Osterholm Update
- Newsletters
- About CIDRAP
- CIDRAP in the News
- Our Director
- Osterholm in the Press
- Shop Merchandise

What is pasteurization? A dairy expert explains how it protects against foodborne illness, including avian flu
Associate Research Professor of Food Science, Penn State
Disclosure statement
Kerry Elizabeth Kaylegian receives funding from USDA.
Penn State provides funding as a founding partner of The Conversation US.
View all partners
Recent reports that the H5N1 avian flu virus has been found in cow’s milk have raised questions about whether the U.S. milk supply is safe to drink. According to the federal Food and Drug Administration, the answer is yes, as long as the milk is pasteurized .
Nonetheless, raw (unpasteurized) milk sales are up , despite health experts’ warning that raw milk could contain high levels of the virus , along with many other pathogens.
As an extension food scientist in a state where raw milk sales are legal , I provide technical support to help processors produce high-quality, safe dairy foods. I also like to help people understand the confusing world of pasteurization methods on their milk labels, and why experts strongly discourage consuming raw milk and products made from it.
What can make milk unsafe
Dairy products, like many foods, have inherent risks that can cause a variety of illnesses and even death. Our milk comes from animals that graze outdoors and live in barns. Milk is picked up from the farm in tanker trucks and delivered to the processing plant. These environments offer numerous opportunities for contamination by pathogens that cause illness and organisms that make food spoil.
For example, listeria monocytogenes comes from environmental sources like soil and water. Mild infections with listeriosis cause flu-like symptoms. More serious cases are, unfortunately, too common and can cause miscarriages in pregnant women and even death in extreme cases .
Other pathogens commonly associated with dairy animals and raw milk include E. coli , which can cause severe gastrointestinal infections and may lead to kidney damage; Campylobacter , the most common cause of diarrheal illness in the U.S.; and Salmonella , which cause abdominal pain, diarrhea and other symptoms.
Keeping beverages safe with heat
In the 1860s, French microbiologist Louis Pasteur discovered that heating wine and beer killed the organisms that caused spoilage, which then was a significant problem in France.
This heating process, which became known as pasteurization, was adopted in the U.S. prior to World War II, at a time when milk was responsible for 25% of all U.S. outbreaks of foodborne illnesses . In 1973, the federal government required that all milk sold across state lines in the U.S. had to be pasteurized, and in 1987, it banned interstate sales of raw milk .
Pasteurization heats every particle of a food to a specific temperature for a continuous length of time in order to kill the most heat-resistant pathogen associated with that product. Different organisms have different responses to heat, so controlled scientific studies are required to determine what length of time at a given temperature will kill a specific organism.
Since 1924, pasteurization in the U.S. has been guided by the Grade “A” Pasteurized Milk Ordinance , a federal guidance document that is updated every two years to reflect current science and has been adopted by all 50 states . Pasteurization equipment in the U.S. must meet stringent requirements that include sanitary design, safety controls and material standards.

Pasteurization methods
Dairy processors can choose among several different types of pasteurization. When executed properly, all of these methods produce the same result: pathogen-free milk. Processors may treat milk beyond minimum times or temperatures to provide an extra margin of safety, or to reduce bacteria that can cause milk to spoil, thus increasing the product’s shelf life.
Vat pasteurizers , also known as batch pasteurizers, often are used by smaller-scale processors who handle limited volumes. The milk is pumped into a temperature-controlled tank with a stirrer, heated to a minimum of 145 degrees Fahrenheit (63 Celsius) and held there continuously for 30 minutes. Then it is cooled and pumped out of the vat.
The most common method used for commercial milk is high-temperature short-time pasteurization , which can treat large volumes of milk. The milk is pumped through a series of thin plates at high speed to reach a minimum temperature of 161 F (71 C). Then it travels through a holding tube for 15 seconds, and the temperature is checked automatically for safety and cooled.
The most complex and expensive systems are ultra-pasteurizers and ultra-high-temperature pasteurizers , which pasteurize milk in just a few seconds at temperatures above 285 F (140 C). This approach destroys many spoilage organisms, giving the milk a significantly longer shelf life than with other methods, although sometimes products made this way have more of a “cooked” flavor.
Ultra-high-temperature products are processed in a sterile environment and packaged in sterile packaging, such as lined cartons and pouches. They can be shelf-stable for up to a year before they are opened. Ultra-high-temperature packaging makes taking milk to school for lunch safe for kids every day.
Avian flu in milk
The detection of avian flu virus fragments in milk is a new challenge for the dairy industry. Scientists do not have a full picture of the risks to humans but are learning.
Research so far has shown that virus particles end up in the milk of infected cows, but that pasteurization will inactivate the virus . However, the FDA is advising consumers not to drink raw milk because there is limited information about whether it may transmit avian flu .
The agency also is urging producers not to manufacture or sell raw milk or raw milk products, including cheese, made with milk from cows showing symptoms of illness.
It’s never a good time to get a foodborne illness, and this is the beginning of ice cream season . At a time when avian flu is showing up in new species and scientists are still learning about how it is transmitted, I agree with the FDA that raw milk poses risks not worth taking.
- Avian flu H5N1
- Food safety
- Dairy products
- US agriculture
- Significant Terms
- Foodborne illness

Case Management Specialist

Lecturer / Senior Lecturer - Marketing

Assistant Editor - 1 year cadetship

Executive Dean, Faculty of Health

Lecturer/Senior Lecturer, Earth System Science (School of Science)
A .gov website belongs to an official government organization in the United States.
A lock ( ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
- How It Spreads
- Norovirus Statistics
- Communication Resources
- Lab Testing
- Reporting & Surveillance
- Food Safety
- Foodborne outbreaks
Norovirus Facts and Stats
- Norovirus is the leading cause of vomiting and diarrhea from acute gastroenteritis among people of all ages in the United States.
Each year, there are about 2,500 reported norovirus outbreaks in the United States.
- Norovirus causes 58% of foodborne illnesses acquired in the United States.

Norovirus is the leading cause of vomiting and diarrhea from acute gastroenteritis among people of all ages in the United States. Gastroenteritis is the inflammation of the stomach and intestines.
Norovirus is also the leading cause of foodborne illness in the United States. It causes 58% of foodborne illnesses acquired in the United States.
Annual number of illnesses and associated outcomes
Each year in the United States, norovirus causes on average:
- 900 deaths, mostly among adults aged 65 and older
- 109,000 hospitalizations
- 465,000 emergency department visits, mostly in young children
- 2,270,000 outpatient clinic visits annually, mostly in young children
- 19 to 21 million illnesses
Economic impact
Each year, foodborne norovirus illness in the United States costs about $2 billion, mainly due to lost productivity and healthcare expenses.
Who is affected
Norovirus is responsible for nearly 1 million pediatric medical care visits annually.
People more likely to have an outpatient or emergency department visit than people of other ages:
- Children under 5 years old
- Adults 85 years and older
By 5 years of age:
- 1 in 110,000 will die from norovirus
- 1 in 160 will be hospitalized
- 1 in 40 will go to the emergency department
- 1 in 7 will go to an outpatient clinic
U.S. outbreaks
- Norovirus outbreaks occur throughout the year but are most common from November to April.
- In years when there is a new strain of the virus, there can be 50% more norovirus illness.
- Most outbreaks occur when infected people spread the virus to others through direct contact (such as caring for them, sharing food, or eating utensils with them).
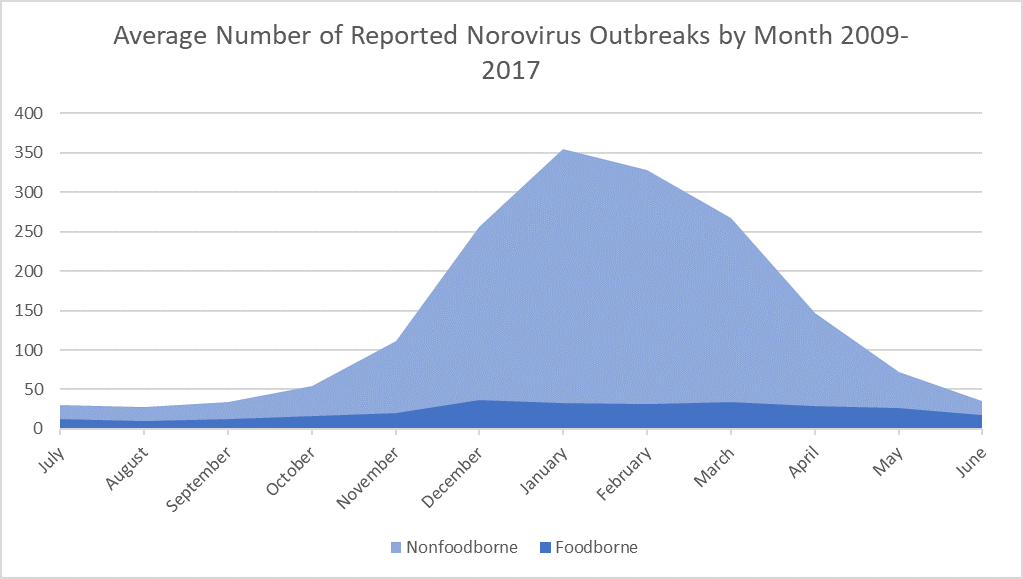
Norovirus Outbreaks
Norovirus worldwide
Worldwide, norovirus causes about 1 out of every 5 cases of acute gastroenteritis that leads to diarrhea and vomiting.
Worldwide, norovirus annually causes on average:
- 685 million total cases of acute gastroenteritis
- 200 million cases in children under 5 years old
- 50,000 child deaths, mostly in developing countries
Norovirus illness is a problem in both low-income and high-income countries. Every year, norovirus is estimated to cost $60 billion worldwide due to healthcare costs and lost productivity.
Global outbreaks
Globally, norovirus is the leading cause of acute gastroenteritis outbreaks.
Outbreaks are usually more common in cooler winter months. They typically occur from November to April in countries above the equator; and from May to September in countries below the equator. However, in places closer to the equator, norovirus may be less seasonal.
- Since 2002, GII.4 viruses (genogroup II genotype 4) have caused the majority of norovirus outbreaks worldwide.
- However, non-GII.4 viruses, such as GII.17 and GII.2, have temporarily replaced GII.4 viruses in several Asian countries.
- Between 2002 and 2012, new GII.4 viruses emerged about every 2 to 4 years, but since 2012, the same virus (GII.4 Sydney) has been the dominant strain worldwide. Often, but not always, these new strains lead to a global increase in norovirus outbreaks.
What CDC is doing
CDC works with many global partners to identify the burden of acute gastroenteritis caused by norovirus and to prevent norovirus outbreaks.
- CDC Estimates of Foodborne Illness in the United States
- Global Burden of Norovirus and Prospects for Vaccine Development
- WHO Estimates of the Global Burden of Foodborne Diseases | PLOS
- Global Burden of Norovirus & Prospects for Vaccine Development | PLOS
Norovirus is the leading cause of vomiting and diarrhea, and foodborne illness in the United States. Always wash your hands and handle food well.
For Everyone
Public health.
- Today's news
- Reviews and deals
- Climate change
- 2024 election
- Fall allergies
- Health news
- Mental health
- Sexual health
- Family health
- So mini ways
- Unapologetically
- Buying guides
Entertainment
- How to Watch
- My watchlist
- Stock market
- Biden economy
- Personal finance
- Stocks: most active
- Stocks: gainers
- Stocks: losers
- Trending tickers
- World indices
- US Treasury bonds
- Top mutual funds
- Highest open interest
- Highest implied volatility
- Currency converter
- Basic materials
- Communication services
- Consumer cyclical
- Consumer defensive
- Financial services
- Industrials
- Real estate
- Mutual funds
- Credit cards
- Balance transfer cards
- Cash back cards
- Rewards cards
- Travel cards
- Online checking
- High-yield savings
- Money market
- Home equity loan
- Personal loans
- Student loans
- Options pit
- Fantasy football
- Pro Pick 'Em
- College Pick 'Em
- Fantasy baseball
- Fantasy hockey
- Fantasy basketball
- Download the app
- Daily fantasy
- Scores and schedules
- GameChannel
- World Baseball Classic
- Premier League
- CONCACAF League
- Champions League
- Motorsports
- Horse racing
- Newsletters
New on Yahoo
- Privacy Dashboard
What is pasteurization? A dairy expert explains how it protects against foodborne illness, including avian flu
Recent reports that the H5N1 avian flu virus has been found in cow’s milk have raised questions about whether the U.S. milk supply is safe to drink. According to the federal Food and Drug Administration, the answer is yes, as long as the milk is pasteurized .
Nonetheless, raw (unpasteurized) milk sales are up , despite health experts’ warning that raw milk could contain high levels of the virus , along with many other pathogens.
As an extension food scientist in a state where raw milk sales are legal , I provide technical support to help processors produce high-quality, safe dairy foods. I also like to help people understand the confusing world of pasteurization methods on their milk labels, and why experts strongly discourage consuming raw milk and products made from it.
What can make milk unsafe
Dairy products, like many foods, have inherent risks that can cause a variety of illnesses and even death. Our milk comes from animals that graze outdoors and live in barns. Milk is picked up from the farm in tanker trucks and delivered to the processing plant. These environments offer numerous opportunities for contamination by pathogens that cause illness and organisms that make food spoil.
For example, listeria monocytogenes comes from environmental sources like soil and water. Mild infections with listeriosis cause flu-like symptoms. More serious cases are, unfortunately, too common and can cause miscarriages in pregnant women and even death in extreme cases .
Other pathogens commonly associated with dairy animals and raw milk include E. coli , which can cause severe gastrointestinal infections and may lead to kidney damage; Campylobacter , the most common cause of diarrheal illness in the U.S.; and Salmonella , which cause abdominal pain, diarrhea and other symptoms.
Keeping beverages safe with heat
In the 1860s, French microbiologist Louis Pasteur discovered that heating wine and beer killed the organisms that caused spoilage, which then was a significant problem in France.
This heating process, which became known as pasteurization, was adopted in the U.S. prior to World War II, at a time when milk was responsible for 25% of all U.S. outbreaks of foodborne illnesses . In 1973, the federal government required that all milk sold across state lines in the U.S. had to be pasteurized, and in 1987, it banned interstate sales of raw milk .
Pasteurization heats every particle of a food to a specific temperature for a continuous length of time in order to kill the most heat-resistant pathogen associated with that product. Different organisms have different responses to heat, so controlled scientific studies are required to determine what length of time at a given temperature will kill a specific organism.
Since 1924, pasteurization in the U.S. has been guided by the Grade “A” Pasteurized Milk Ordinance , a federal guidance document that is updated every two years to reflect current science and has been adopted by all 50 states . Pasteurization equipment in the U.S. must meet stringent requirements that include sanitary design, safety controls and material standards.
Pasteurization methods
Dairy processors can choose among several different types of pasteurization. When executed properly, all of these methods produce the same result: pathogen-free milk. Processors may treat milk beyond minimum times or temperatures to provide an extra margin of safety, or to reduce bacteria that can cause milk to spoil, thus increasing the product’s shelf life.
Vat pasteurizers , also known as batch pasteurizers, often are used by smaller-scale processors who handle limited volumes. The milk is pumped into a temperature-controlled tank with a stirrer, heated to a minimum of 145 degrees Fahrenheit (63 Celsius) and held there continuously for 30 minutes. Then it is cooled and pumped out of the vat.
The most common method used for commercial milk is high-temperature short-time pasteurization , which can treat large volumes of milk. The milk is pumped through a series of thin plates at high speed to reach a minimum temperature of 161 F (71 C). Then it travels through a holding tube for 15 seconds, and the temperature is checked automatically for safety and cooled.
The most complex and expensive systems are ultra-pasteurizers and ultra-high-temperature pasteurizers , which pasteurize milk in just a few seconds at temperatures above 285 F (140 C). This approach destroys many spoilage organisms, giving the milk a significantly longer shelf life than with other methods, although sometimes products made this way have more of a “cooked” flavor.
Ultra-high-temperature products are processed in a sterile environment and packaged in sterile packaging, such as lined cartons and pouches. They can be shelf-stable for up to a year before they are opened. Ultra-high-temperature packaging makes taking milk to school for lunch safe for kids every day.
Avian flu in milk
The detection of avian flu virus fragments in milk is a new challenge for the dairy industry. Scientists do not have a full picture of the risks to humans but are learning.
Research so far has shown that virus particles end up in the milk of infected cows, but that pasteurization will inactivate the virus . However, the FDA is advising consumers not to drink raw milk because there is limited information about whether it may transmit avian flu .
The agency also is urging producers not to manufacture or sell raw milk or raw milk products, including cheese, made with milk from cows showing symptoms of illness.
It’s never a good time to get a foodborne illness, and this is the beginning of ice cream season . At a time when avian flu is showing up in new species and scientists are still learning about how it is transmitted, I agree with the FDA that raw milk poses risks not worth taking.
This article is republished from The Conversation , a nonprofit, independent news organization bringing you facts and trustworthy analysis to help you make sense of our complex world. It was written by: Kerry E. Kaylegian , Penn State
Food expiration dates don’t have much science behind them – a food safety researcher explains another way to know what’s too old to eat
Louis Pasteur’s scientific discoveries in the 19th century revolutionized medicine and continue to save the lives of millions today
Is the FDA being Grinch-like in raising concerns about raw cookie dough?
Kerry Elizabeth Kaylegian receives funding from USDA.
Recommended Stories
Raw milk's popularity is surging. here's why experts say that's dangerous..
Despite the current outbreak of bird flu among dairy cattle, sales of raw milk continue to rise — and experts say there are no benefits that outweigh the risks of illness from untreated dairy.
Bird flu: The latest on U.S. spread, the safety of milk and new federal funding to prevent outbreaks
Everything you need to know about the spread of avian influenza, aka bird flu, in the U.S. and new federal funding.
What to know about bird flu found in milk, Trump trial witness gives damning testimony and a Beyoncé documentary trailer drops
The stories you need to start your day: What to know about bird flu in milk, the NBA playoffs and more in today’s edition of The Yodel newsletter
More people prefer cow's milk over plant-based milks, new Yahoo/YouGov poll finds. Here's what nutritionists think about that.
Whole milk and 2% cow’s milk emerged as the top choices of milk, beating out plant-based milk.
Secondhand Rolex sales surge in 'underdeveloped' US market
Luxury watch prices are moderating on the secondary market, but retailers like Watches of Switzerland see demand continuing to outpace supply.
Why companies are turning to internal hackathons
One way to do that is by running an internal hackathon around a theme and having employees attack a problem together. Brandon Kessler, CEO and co-founder at DevPost, a company that helps customers organize and manage internal and external hackathons, says that he’s seen how hackathons help companies encourage their employees to solve big problems. “Without question, innovation and collaboration are the two key value props when it comes to running internal hackathons, and almost everyone wants both,” Kessler told TechCrunch.
NBA playoffs: Pacers vs. Knicks Game 7 updates, score, highlights, analysis
One team will go on to the Eastern Conference finals. The other will go home.
The big questions JPMorgan investors have for Jamie Dimon
Attendees at JPMorgan's annual investor day Monday will be listening for answers to some key questions. A top concern is how much longer Jamie Dimon plans to run the largest US bank.
Manchester City wins historic 4th consecutive Premier League title
Man City discarded West Ham and did what no other club had ever done in the 124-year history of English soccer.
'My skin felt smoother and brighter': Shoppers in their 50s rave about this vitamin C serum — and it's on sale for $12
This elixir may help smooth fine lines and more, according to 22,000+ five-star fans.
I’m rooting for Melinda French Gates to fix tech's broken ‘brilliant jerk’ culture
On Monday, Melinda French Gates resigned from the philanthropy organization she ran with ex-husband Bill Gates. French Gates will leave next month with an additional $12.5 billion, she said. The Gates Foundation famously works on projects to help impoverished people, especially in developing countries, such as fighting malaria, polio or improving sanitation.
'Hides the pooch': This loose but 'not sloppy loose' button-down is on sale for just $23
Lightweight and flattering, Amazon's No. 1 bestselling top will get plenty of play in your summer rotation.
Dow at 40,000: Why stocks still have 'plenty of room to run'
Wall Street pros say there's more room to grow with stock markets around record highs.
Overpacker? Bring these genius foldable hangers — they're just under $1 each right now
If you like having vacay-outfit options, you may need to bring some hangers along — these doodads are here to help.
Trading stocks all day and all night might be an 'inevitability' for investors
Around-the-clock stock trading is likely the future, executives at several trading platforms say, thanks to increased demand from international markets and a new generation of investors who expect constant online access.
Score big savings on Hoka hiking boots during REI's Anniversary Sale
If you’re in the market for new hiking boots, now is the perfect time to take advantage of the incredible deals at REI's Anniversary Sale.
Housing experts revise mortgage rate forecasts for remainder of 2024
Experts are revising their forecasts about mortgage rates and home prices for the rest of the year.
Markets brace for Nvidia earnings: What to know this week
A crucial earnings report from AI leader Nvidia greets a stock market that hit new records last week.
Mortgage rates today, May 19, 2024: Rates inch down but remain high overall
These are today's mortgage rates. Rates are ticking down, but it could be months before we see drastic decreases. Lock in your rate today.
Report: Fanatics files lawsuit against Cardinals rookie WR Marvin Harrison Jr. for breach of contract
Marvin Harrison Jr., Fanatics said, “rejected or ignored every request” from the company while refusing to fulfill obligations of their contract that was signed last May.

Hidden costs of food-borne illnesses: Impacts on productivity and economic growth
F ood-borne illnesses are a significant public health concern that affects millions of people worldwide each year. While the immediate health consequences are well-known, the broader impacts on productivity and economic growth are often overlooked. This article sheds light on the hidden costs associated with food-borne illnesses and emphasises the need for proactive measures to mitigate their impact on productivity and economic growth.
The toll on productivity
Food-borne illnesses can have a severe impact on productivity, both at an individual and societal level. When employees fall ill due to contaminated food, they often experience symptoms such as nausea, vomiting, and diarrhea, which can lead to absenteeism and reduced work performance. This not only affects the affected individuals but also disrupts workflow and productivity within organisations. Moreover, outbreaks of food-borne illnesses can lead to temporary closures of businesses, further exacerbating the economic consequences.
Economic implications
The economic consequences of food-borne illnesses are far-reaching. First and foremost, the healthcare costs associated with treating individuals affected by food-borne illnesses can be substantial. These costs include medical consultations, hospitalisations, medications, and laboratory tests. Additionally, the indirect costs, such as lost productivity and wages, can have a significant impact on individuals and their families.
Furthermore, food-borne illness outbreaks can tarnish the reputation of businesses and entire industries. Consumer confidence in food products may decline, leading to reduced demand and sales. This can have long-lasting effects on the affected businesses, resulting in financial losses, layoffs, and even closures. The economic impact extends beyond the immediate industry, affecting suppliers, distributors, and other related sectors.
The role of prevention
Prevention is key to reducing the burden of food-borne illnesses on productivity and economic growth. Governments, regulatory agencies, and food manufacturers must prioritise food safety measures throughout the entire food supply chain. This includes implementing and enforcing strict hygiene practices, conducting regular inspections, and ensuring proper food handling and storage.
Education and awareness campaigns are also crucial in empowering individuals to make informed choices about food safety. By promoting safe food handling practices, proper cooking techniques, and the importance of purchasing from reputable sources, consumers can play an active role in safeguarding their health and supporting the economy.
Collaboration and knowledge sharing
Addressing the impact of food-borne illnesses on productivity and economic growth requires collaboration among various stakeholders. Governments, businesses, and public health agencies should work together to share information, best practices, and research findings. This collaboration can help identify emerging food safety risks, develop effective prevention strategies, and enhance surveillance systems to detect and respond to outbreaks promptly.
Specific scenarios, illustrations, and policies
1. Scenario: Salmonella outbreak in the United States
Illustration: In 2018, a widespread Salmonella outbreak linked to contaminated eggs affected multiple states in the United States. The outbreak resulted in hundreds of reported cases of illness and hospitalisations.
Policy response: In response to the outbreak, the U.S. Food and Drug Administration (FDA) implemented stricter regulations and inspections for egg producers. The FDA also collaborated with state health departments to investigate the source of contamination and implement control measures to prevent future outbreaks.
2. Scenario: Listeria outbreak in African soft cheeses
Illustration: Imported soft cheeses from various African countries were found to be contaminated with Listeria monocytogenes, leading to outbreaks of Listeriosis in the United States. The outbreak resulted in several deaths and severe illnesses.
Policy response: The FDA issued import alerts and increased surveillance on imported soft cheeses from Africa. The agency worked closely with African authorities to improve food safety practices and enhance testing protocols to prevent further contamination.
3. Scenario: Vibrio outbreak in Asian seafood
Illustration: Consumption of raw or undercooked fish and shellfish from Asia led to outbreaks of Vibrio parahaemolyticus infections in the United States. The outbreaks resulted in numerous cases of gastrointestinal illness and hospitalisations.
Policy response: The FDA implemented stricter import regulations for seafood from Asia, including increased testing and inspection protocols. The agency also collaborated with Asian authorities to improve seafood safety practices and enhance monitoring of seafood exports.
4. Scenario: Economic impact on international relations
Illustration: The occurrence of food-borne illness outbreaks in Africa, Asia, and sub-Saharan countries has led to trade restrictions and strained international relations. Importing countries, including the United States, have imposed bans or increased scrutiny on food products from these regions, affecting trade and diplomatic relations.
Policy response: Governments in affected regions have implemented stricter food safety regulations and invested in improving food handling and processing practices. They have also worked with international partners to enhance surveillance systems, conduct joint inspections, and share best practices to regain consumer confidence and restore trade relationships.
Nigerian example
Illustration: In Nigeria, there have been instances of food-borne illness outbreaks, such as cholera outbreaks linked to contaminated water and street food. These outbreaks have resulted in significant health burdens and economic losses.
Policy response: The Nigerian government has taken steps to address food-borne illnesses, including strengthening food safety regulations, improving sanitation practices, and increasing public awareness about safe food handling. The government has also collaborated with international organisations and neighbouring countries to enhance surveillance and control measures to prevent and respond to outbreaks effectively.
These specific scenarios and policy responses, including the example from Nigeria, highlight the importance of addressing food-borne illnesses and their impact on productivity, economic growth, and international relations. By implementing stringent food safety measures, conducting thorough inspections, and fostering collaboration between nations, we can mitigate the economic consequences of food-borne illnesses and maintain strong international trade relationships. It is crucial for governments, regulatory agencies, and food manufacturers to prioritise food safety to protect public health, support economic growth, and promote harmonious international relations.
Dolapo Ologunde, founder and CEO of Creacion Cakes Co, sent this from the United Kingdom.
READ ALSO FROM NIGERIAN TRIBUNE
- Skip to main content
- Skip to footer
AgriLife Today
Texas A&M AgriLife's digital magazine and newsroom
Fight to eradicate malaria takes associate professor to Equatorial Guinea
Giri athrey says science is the best hope for infectious disease solutions at home and abroad.
May 16, 2024 - by Susan Himes

Giri Athrey, Ph.D., understands the significance of a single mosquito bite.
“There is an anecdote that George Washington was struck with malaria at age 17, but managed to recover,” he said. “How different would history be if he had succumbed to malaria?”
While Athrey is an avian geneticist and associate professor in the Texas A&M College of Agriculture and Life Sciences Department of Poultry Science , he also spends a lot of time thinking about malaria and ways to prevent mosquito-borne diseases. Athrey is also an associate professor of quantitative genetics and functional genomics and a member of the graduate faculty of entomology .
Malaria elimination project
A passion of Athrey’s is his involvement in the Bioko Island Malaria Elimination Project , BIMEP. The project works to eradicate malaria in Equatorial Guinea.
BIMEP was started in 2004. Athrey began working with them in 2010, and in 2021 assumed the role of technical adviser, making him the main person for molecular entomology and surveillance. Since 2004, the project has led to a 97% overall reduction in the rate of malaria transmission by mosquitoes on Bioko Island.
The work he conducts overseas is based on successes pioneered in the U.S. and elsewhere. Discoveries he makes in Equatorial Guinea are also highly applicable to controlling mosquito-borne vectors at home into the future, Athrey said.
His research related to BIMEP focuses on mosquitoes and the critical role molecular entomology can play in understanding and combating vector-borne diseases and contributing to improving public health outcomes in malaria-affected regions.
“It’s very meaningful work, and it’s very impactful work,” he said. “I spent five years as a postdoctoral associate working on malaria genomics. I was emotionally invested in the work and had put a lot of energy into this research, so I wanted to continue doing it even when I became faculty.”
Work that impacts people
While the Athrey lab works on applying genomics to improve poultry, a global food source, he views his work on malaria as also impacting the same beneficiaries – people. There is a significant overlap in the lab and computational methods used between these fields. And there are often lessons and serendipitous insights when working on two entirely different models.

“In our lab we are interested in using crossing experiments coupled with next-generation sequencing approaches to unravel the genetic basis of complex traits,” he said.
The lab characterizes sequence variation in genes and regulatory elements underlying traits. This work has great importance in a variety of contexts including understanding disease resistance or host-seeking behaviors in disease vectors.
The research is also applicable to many countries dealing with mosquito-transmitted diseases.
Malaria and other mosquito-borne diseases impact the world
Mosquito-borne diseases affect people worldwide — including in Texas and across the U.S., Athrey said. Infected people and animals can also infect non-infected mosquitoes, which in turn infect other people and animals.
West Nile virus is the most prominent arthropod-borne or arbovirus and is the leading cause of mosquito-borne disease in the U.S. West Nile can infect not just humans but birds, horses and other animals.
Other mosquito-borne viral illnesses/diseases seen in Texas include: St. Louis encephalitis, Eastern equine encephalitis, Western equine encephalitis, California encephalitis, dengue fever, Zika and Chikungunya.
Besides health impacts, including potential death and long-term health issues, these mosquito-borne diseases can have tremendous economic impacts.
Athrey feels a personal and professional calling to help with global issues affecting mankind.
Growing up in India, he was familiar with the impact of food insecurity and infectious disease. His work with poultry and malaria answers his need to address both these issues.
The two things people need for building a foundation in life are food and health, he said. That led him to ask himself what he could do to help address those issues.
“For me, it was science,” he said. “Science equals solutions.”
Infectious diseases can make what should be a normal life into a terrible life or cut it short altogether, he said.

“If you read some of the historical accounts of some African regions, there’s sicknesses like river blindness,” Athrey said. “That is terrifying to imagine that disease existed. There would be entire villages of blind people from infectious disease.”
Malaria field work
Athrey has made several trips to the African nation since 2020.
“I just go into the field mentally prepared because we have to get the maximum out of the amount of time we’re there,” Athrey said of his eight-to-10-day trips to Equatorial Guinea, the last one in November. On that trip, he carried out a week-long training program at the national lab in Baney, but also used the opportunity to perform field collections for continuing genomics studies.
There is a limited window each evening to gather female Anopheles mosquitoes — the only mosquito species that spreads malaria.
“So, we would carry out a training and capacity building program in the day, and from 6:30 p.m. to midnight collect samples,” he said.
It can be exhausting work with little sleep, but Athrey said he looks forward to it.
And as much as Athrey values his time in Equatorial Guinea, he is always eager to return home to be with his family, which includes a middle-schooler.
Once the samples are back in the U.S. at Texas A&M for the diagnostic work, lab tech Mark Mattine works on them.
“These samples are invaluable for our research, offering insights that could lead to breakthroughs in understanding mosquito behavior and malaria transmission dynamics,” Athrey explained.
The data generated by Athrey’s lab is mission-critical because it is used to determine how to continue the mosquito control programs, he said.

“Because we’re always on a deadline when it gets here, Mark has to manage his time carefully to keep it churning,” Athrey said. “He works really hard and is an important contributor to what we’re able to do.”
“The capability to do some of the testing and research we’re doing hasn’t previously existed in Equatorial Guinea,” he said. “But things are beginning to change with the opening of the state-of-the-art Baney Laboratory and the training program that has been created to start preparing scientists to do some of the work there.”
Athrey plans to return in late summer to see how the process is going.
“BIMEP is a real success story because it’s one of the best run programs in Africa, and it’s run by competent and good people,” Athrey said. “It’s a privilege to work with all the expertise that comes there, including people from the University of Washington and the London School of Tropical Medicine and Hygiene.
“It’s very fulfilling work, and it is making a difference for people there,” he said. “I just feel fortunate that there is a chance to improve people’s lives by doing this kind of work.”

Media Inquiries
Laura Muntean , media relations coordinator [email protected] 601.248.1891
Are you interested in this content, need high resolution photos or assistance getting connected with an expert to learn more? Please contact our media relations team at [email protected] .
You May Also Like

Mosquito season: How to control and prevent bites

$8 million grant establishes multi-agency program to mitigate vector-borne diseases
Western gulf center of excellence gains ground against vector-borne diseases.
A member of Texas A&M AgriLife
Texas A&M AgriLife Extension Service | Texas A&M AgriLife Research | Texas A&M Forest Service | Texas A&M Veterinary Medical Diagnostic Lab | College of Agriculture & Life Sciences
Texas A&M AgriLife
Phone: (979) 803-1287 [email protected]
More Information
- Resources for Press and Media
- Story Suggestion
Find Us on Social Media
About texas a&m university.

IMAGES
COMMENTS
"Food-borne Disease Prevention and Risk Assessment" is a Special Issue of the International Journal of Environmental Research and Public Health on understanding how food-borne disease is still a global threat to health today and to be able to target strategies to reduce its prevalence. Despite decades of government and industry interventions, food-borne disease remains unexpectedly high in ...
Foodborne diseases are reflected in several targets of Sustainable Developmental Goal 3 and are a priority area within the Organization's work. Activities include research and independent scientific assessments of food-related hazards, foodborne disease awareness programs, and helping to promote food safety through national health-care programs.
Around the world unsafe food is known to cause more than 200 acute and chronic diseases. In 2015, WHO published the first-ever estimates of global burden of foodborne diseases, which indicated that the 31 hazards examined were responsible for 600 million cases of foodborne diseases in 2010, resulting in 33 million disability-adjusted life years (DALYs), including 420 000 deaths worldwide.
Among all illnesses related to solved foodborne outbreaks, 6% occurred in children under 5 and 18% occurred in adults over 65 years, age groups at higher risk for severe illness. When compared with Salmonella or STEC infections, a higher proportion of solved multistate foodborne outbreaks of Listeria infections were in adults over 65 (43%).
What is a foodborne disease outbreak? A foodborne disease outbreak occurs when two or more people develop a similar illness after ingesting the same contaminated food or drink (WHO, 2008). In some countries, only one case of a rare but severe foodborne disease - like botulism or chemical intoxication - is also considered an outbreak.
The marginal contribution of this article to existing research is mainly reflected in three aspects: (1) Based on the classic infectious disease model, a diffusion mechanism for foodborne diseases was designed, and at the same time, combined with the susceptible-infected-recovered-immune (SIRM) model, a systematic model was established on how ...
Versions Notes. "Food-borne Disease Prevention and Risk Assessment" is a Special Issue of the International Journal of Environmental Research and Public Health on understanding how food-borne disease is still a global threat to health today and to be able to target strategies to reduce its prevalence. Despite decades of government and ...
These estimates are known as the attribution of foodborne illness. By estimating the burden of foodborne illness and attributing illnesses to specific food sources, CDC, regulatory agencies, industry, consumer groups, and others can better target prevention measures and improve food safety in the United States.
Foodborne Illness: Pathogens and Diseases. June 2019. In book: Research Trends in Food Technology and Nutrition Vol-8 (pp.1-20) Chapter: First. Publisher: AkiNik Publications. Authors: Ena Gupta ...
Foodborne diseases are an important public health burden in the United States. First, we estimate that 31 of the most important known agents of foodborne disease found in foods consumed in the United States each year cause 9.4 million illnesses, 55,961 hospitalizations, and 1,351 deaths. Second, not all agents of foodborne disease are known or ...
Foodborne Bacteria Table. Contaminated water, raw or unpasteurized milk, and raw or undercooked meat, poultry, or shellfish. Diarrhea (sometimes bloody), cramping, abdominal pain, and fever that appear 2 to 5 days after eating; may last 7 days. May spread to bloodstream and cause a life- threatening infection.
National burden of foodborne disease (FBD) studies are essential to establish food safety as a public health priority, rank diseases, and inform interventions. In recent years, various countries have taken steps to implement them. Despite progress, the current burden of disease landscape remains scattered, and researchers struggle to translate ...
1-14 days, usually at least 1 week. Diarrhea (usually watery), loss of appetite, substantial loss of weight, stomach cramps, nausea, vomiting, fatigue. May be remitting and relapsing over weeks to ...
When two or more people get the same illness from the same contaminated food or drink, the event is called a foodborne illness outbreak. FDA investigates outbreaks to control them, so more people ...
The 2016 FSS is the seventh wave of a repeated cross-sectional survey conducted by the U.S. Food and Drug Administration in collaboration with the U.S. Department of Agriculture. The goal of the ...
Overview. Food poisoning, a type of foodborne illness, is a sickness people get from something they ate or drank. The causes are germs or other harmful things in the food or beverage. Symptoms of food poisoning often include upset stomach, diarrhea and vomiting. Symptoms usually start within hours or several days of eating the food.
Research Letter Foodborne Disease Outbreaks Linked to Foods Eligible for Irradiation, United States, 2009-2020 Marta Zlotnick , Taylor Eisenstein, Misha Park Robyn, and Katherine E. Marshall ... the Centers for Disease Control and Prevention, or the authors' affiliated institutions. Use of trade names is for identification only and does not ...
Abstract. Foodborne disease (also referred to as foodborne illness or food poisoning) is any illness that results from the consumption of contaminated food, contaminated with pathogenic bacteria, viruses, or parasites. The economic costs associated with foodborne disease can be severe on people, food companies, and country reputation.
A dairy expert explains how it protects against foodborne illness, including avian flu. Kerry E. Kaylegian, Penn State. Before World War II, pathogens in milk accounted for 1 in 4 cases of ...
Food irradiation has been studied globally for decades and is a safe, effective means of reducing foodborne illness-causing pathogens, sterilizing insects, delaying ripening or sprouting, and extending shelf life (1,2).The US Food and Drug Administration has approved various foods for irradiation, including meat, poultry, fresh shell eggs, and spices (Appendix Table).
Of 482 US foodborne outbreaks caused by four common bacteria from 2009 to 2022, 32.2%—involving more than 3,500 sick people and 10 deaths—were linked to a food that could have undergone pathogen-neutralizing irradiation but did not, researchers from the Centers for Disease Control and Prevention reported yesterday in Emerging Infectious Diseases.
Research so far has shown that virus particles end up in the milk of infected cows, ... It's never a good time to get a foodborne illness, and this is the beginning of ice cream season. At a ...
By Coral Beach on May 15, 2024. Research funded in part by the CDC has shown that food irradiation could reduce the number of foodborne outbreaks caused by pathogens. For the project, researchers ...
Norovirus is also the leading cause of foodborne illness in the United States. It causes 58% of foodborne illnesses acquired in the United States. Annual number of illnesses and associated outcomes. Each year in the United States, norovirus causes on average: 900 deaths, mostly among adults aged 65 and older. 109,000 hospitalizations
Research so far has shown that virus particles end up in the milk of infected cows, ... It's never a good time to get a foodborne illness, and this is the beginning of ice cream season. At a ...
Food-borne illnesses can have a severe impact on productivity, both at an individual and societal level. ... best practices, and research findings. This collaboration can help identify emerging ...
His research related to BIMEP focuses on mosquitoes and the critical role molecular entomology can play in understanding and combating vector-borne diseases and contributing to improving public health outcomes in malaria-affected regions. "It's very meaningful work, and it's very impactful work," he said. ...