Log in using your username and password
- Search More Search for this keyword Advanced search
- Latest content
- Supplements
- BMJ Journals More You are viewing from: Google Indexer

You are here
- Volume 7, Issue 6
- What India can learn from globally successful malaria elimination programmes
- Article Text
- Article info
- Citation Tools
- Rapid Responses
- Article metrics
- Sachin Sharma 1 ,
- Reena Verma 1 ,
- Bhawna Yadav 1 ,
- Amit Kumar 1 ,
- Manju Rahi 2 ,
- http://orcid.org/0000-0002-3305-0034 Amit Sharma 1 , 3
- 1 ICMR-National Institute of Malaria Research , New Delhi , Delhi , India
- 2 Division of Epidemiology and Communicable Diseases , Indian Council of Medical Research , Delhi , Delhi , India
- 3 International Centre for Genetic Engineering and Biotechnology , New Delhi , Delhi , India
- Correspondence to Dr Manju Rahi; drmanjurahi{at}gmail.com ; Dr Amit Sharma; directornimr{at}gmail.com
India is targeting malaria elimination by 2030. Understanding and adopting the strategies employed by countries that have successfully eliminated malaria can serve as a crucial thrust in this direction for a geographically diverse country like India. This analysis is based on extensive literature search on malaria elimination policies, strategies and programmes adopted by nine countries (China, El Salvador, Algeria, Argentina, Uzbekistan, Paraguay, Sri Lanka, Maldives and Armenia) which have attained malaria-free status over the past decade. The key points which India can learn from their journey are mandatory time-bound response in the form of case reporting and management, rapid vector control response, continuous epidemiological and entomological surveillance, elevated community participation, more training and capacity building, private sector involvement, use of quality diagnostics, cross-border collaborations, inclusion of prevention of re-establishment programmes into the elimination plans, higher investment in research, and uninterrupted funds for successful implementation of malaria elimination programmes. These learnings would help India and other South Asian countries steer their programmes by devising tailor-made strategies for their own regions.
Data availability statement
All data relevant to the study are included in the article or uploaded as supplementary information.
This is an open access article distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited, appropriate credit is given, any changes made indicated, and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/ .
https://doi.org/10.1136/bmjgh-2022-008431
Statistics from Altmetric.com
Request permissions.
If you wish to reuse any or all of this article please use the link below which will take you to the Copyright Clearance Center’s RightsLink service. You will be able to get a quick price and instant permission to reuse the content in many different ways.
SUMMARY BOX
By 2021, 40 countries have been certified by the WHO as malaria-free. There are 85 malaria-endemic countries, with an estimated 241 million cases in 2020.
India continues to show a sustained decline in overall malaria but faces several challenges in its malaria elimination journey.
An overview of malaria elimination strategies which were central to the success achieved by nine countries in the past decade is presented here. Some of these can be emulated by India and other South Asian countries to overcome the challenges in their elimination drive.
Barriers to smooth adoption of these strategies in the Indian programme have also been described.
Introduction
The 2021 World Malaria Report (WMR) estimated 241 million cases with approximately 0.63 million malaria deaths from 85 malaria-endemic countries ( figure 1 ). Most of the deaths were reported in children under 5 years of age (~77%) and majority were in African nations (~96%). By 2021, 40 countries have been certified by the World Health Organization (WHO) as malaria-free, 1 two (Malaysia and the Islamic Republic of Iran) have achieved zero indigenous case status, and Azerbaijan and Tajikistan have applied for certification. 2 The world’s 11 highest malaria burden countries (India being one of them), accounting for 70% of global cases, have adopted the WHO’s High Burden to High Impact initiative to formulate a country-led response for malaria elimination. 3
- Download figure
- Open in new tab
- Download powerpoint
World map depicting country-wise contribution of global malaria cases in 2020 and WHO-certified malaria-free countries so far. 1 2
India is slated for malaria elimination by 2030. 4 It contributed 83% of the estimated malaria cases and 82% of malaria deaths in South-East Asia Region (SEAR) in 2020, according to the 2021 WMR. Plasmodium falciparum and P. vivax are the major prevalent parasites in India. The country contributed 51% of the global P. vivax cases in 2016, when the country launched the National Framework for Malaria Elimination, outlining the goals, strategies, guidelines and time-bound targets to eliminate malaria in India by 2030. 4 Through concerted efforts, India has managed to sustain the decline in overall burden, with 186 532 cases and 93 deaths reported in 2020 by India’s national programme ( figure 2 ). Malaria endemicity in India is heterogeneous, with the highest endemicity regions being tribal and forested areas of the country. Analysis of epidemiological data from 2000 to 2019 revealed that forested districts contributed ~32% of malaria cases and 42% of mortality due to malaria, while harbouring ~6.6% of the country’s population. 5 The different topographies, climatic conditions and ecosystems support breeding and survival of Anopheles species. The major challenges towards malaria elimination in India are large population size, population movement across regions of different endemicities (the risk of parasite carriers moving from high endemic to low endemic areas), undetected asymptomatic and subpatent malaria cases, multiple vectors, threat of drug and insecticide resistance, shortage of skilled human resources, lack of reporting from the private sector, and unplanned expansion of urban and semi-urban areas. These factors add to the complexity of malaria transmission and make malaria elimination challenging in India.
Reported number of malaria cases and deaths in India and species-wise break-up of cases in India in the last 10 years (2011–2020). Data source: Directorate of the National Centre for Vector Borne Diseases Control, Government of India, and WHO World Malaria Report 2021. 2
Several countries share the above challenges associated with malaria control and prevention but have successfully eliminated malaria. Here, we have selected nine countries as they have successfully eliminated malaria in the last decade (2011–2021). We chose these countries for the reason that in these 10 years the most impactful interventions, namely insecticide impregnated bed nets, rapid diagnostics and artemisinin-based drug therapy, were deployed and they made a major dent in the burden of malaria in endemic countries. 6 Moreover, molecular surveillance of parasites and systematic periodic vector surveillance studies were established as the monitoring mechanisms during this decade itself. Additionally, some of these countries share a similar ecological and epidemiological scenario, such as the dominance of P. vivax cases in Sri Lanka and the southern part of India.
Therefore, we feel that studying these countries’ practices and policies would be insightful for Indian malaria programme managers and malariologists. For example, the diverse mosquito species that caused malaria in Maldives and Uzbekistan and their elimination strategies for vector control could be additional lessons for India. Environmental engineering methods as adopted by Argentina could be helpful in tackling forest malaria in India. El Salvador had successful strategies for active surveillance of migrant populations searching for employment. In India, the migrant population is a threat for reintroducing malaria in states which have reached almost zero indigenous cases. The strategy of Algeria in combating P. falciparum and the involvement of non-governmental organisations (NGOs) and private sectors in Sri Lanka and Paraguay could be inspiring strategies for India to imbibe. It is essential to reach population groups even in the hard-to-reach and conflict-ridden areas to achieve elimination. In this regard, India could learn from Sri Lanka’s elimination drive even during a civil war. If we consider China, its population size is similar to India. Also, its battle, like India, has been a long one but successful, and therefore these countries’ strategies in eliminating malaria are a great learning lesson for us.
We also realise that it is difficult to emulate all the strategies and practices of the victorious countries due to diversity in the epidemiological and entomological picture and the different population scale in India. However, we believe that India can imbibe many of the best practices followed by these countries by closely studying the factors and influences behind the successful elimination of malaria, and if possible replicate them at the appropriate level in India. In this paper, we have analysed the strategies/policies used by these countries in their fight against malaria and have listed them in the following sections, which can serve as torchbearers for India.
Key strategies adopted by some selected countries
In 2021, China, in the WHO Western Pacific Region (WHO WPR), was declared malaria-free after reporting the last indigenous malaria case in 2016 7 —this was a culmination of efforts of over ~70 years. P. vivax was the major parasite species of concern in China. At the time of transition of their programme from control to elimination in 2011, P. vivax malaria cases (2118 cases) were ~1.5 times of P. falciparum (1269 cases). 8 The policies and strategies which became the cornerstone of malaria elimination programme in China were the following: (1) In 1967, China launched a national effort called ‘the 523 project’, which resulted in the discovery of the artemisinin group of highly effective antimalarial drugs, which are the most potent antimalarial drugs to date. (2) Within the control strategy of malaria, mass drug administration (MDA) was used on a large scale (1973–1983). (3) During the decline phase (1981–2000), the country implemented the strategy of environmental management as well as protective measures for exposed population {early distribution of insecticide impregnated bednets and indoor residual spray (IRS) for vector control}, and then a foci-based response (2000-2009) to reduce the high burden of malaria in different provinces by stratification based on transmission risk and incidence. Under this phase they also introduced the National Malaria Elimination Action Plan that combined surveillance and response with real-time reporting. 9–11 (4) During the malaria elimination phase (2011–2020), the country adopted local, tailor-made, pragmatic approaches with deployment of the ‘1-3-7’ surveillance strategy, which meant prompt reporting of confirmed cases within a day to a web-based national case reporting system, further investigation within 3 days and genome sequencing to distinguish imported and indigenous cases, treatment within 3 days, and foci response and adopted reactive case detection (RACD) within 7 days to prevent further transmission. 12 Imported malaria was tackled by the ‘1-3-7’ strategy and by the collaborative approaches of health professionals at the border, with polymerase chain reaction (PCR) as an additional diagnostic tool used by the reference laboratories at the counties. For prevention of re-establishment (POR), they restructured the 1-3-7 approach to 3-3-7, where the diagnosis of case is completed within 3 days, reconfirmation and epidemiological investigation are done within another 3 days, and foci investigation and response completion is done within 7 days after diagnosis. Additionally, China in 2017 initiated a subnational malaria elimination drive for individual provinces which was in tandem with the WHO 2017 Malaria Elimination Programme. They invested in building systems such as the National Institute of Parasitic Diseases and the Chinese Center for Disease Control and Prevention (China CDC), supported by capacity building and web-based reporting system at the grass-roots level. They also collaborated with the Global Fund to Fight AIDS, Tuberculosis and Malaria (GFATM), which contributed to global malaria elimination efforts through collaborative projects which created an opportunity for mutual learning. 12
El Salvador
In 2021, El Salvador became the first country in the Central America of the WHO Region of the Americas (WHO AMR) to be certified as malaria-free. The last indigenous malaria case of P. falciparum in El Salvador was reported in 1995, while the last P. vivax cases were reported in 2016. 13 The key programmatic activities which possibly paved the way for elimination were the following: (1) geographical stratification using altitude and slide positivity rate data; (2) decentralisation for diagnosis facilities and data reporting; (3) weekly reporting systems and analysis; (4) computerised malaria information system; (5) decision on MDA and IRS at the local and regional level; (6) mandatory reporting by the private sector and (7) outbreak response on detection of two or more cases. 14
In 2019, Algeria, in the WHO African Region (AFR), was declared malaria-free by the WHO, with the last case of indigenous malaria reported in 2015. P. falciparum was the dominant parasite species. Geographical information system (GIS) mapping to identify imported cases of malaria, epidemiological surveys around each positive case and entomological surveillance to document the movement of mosquito vectors helped in curtailing imported malaria. 15
Argentina, in the WHO AMR, was certified by the WHO as a malaria-free country in 2019. In this South American country, the last indigenous case was reported in 2010. The most prevalent parasites in the country were P. falciparum and P. vivax . The key elements were IRS including at border areas, collaboration between border countries, prompt IRS by brigades on diagnosis of a malaria case and surveillance within the 500 meter radius of the identified case. Management of estuaries as breeding sites via infrastructural development and reintroduction of vertical vegetation, removal of green algae, and IRS with dichloro-diphenyl-trichloroethane (DDT) were especially helpful. 16
Uzbekistan, in the WHO European Region (WHO EUR), was declared malaria-free in 2018. The last locally acquired malaria case in Uzbekistan was reported in 2010. Both P. falciparum and P. vivax infections were prevalent in the country. Private sector involvement, supervised treatment for P. vivax cases, MDA, larvivorous fish Gambusia for vector control, and annual surveys to identify and liquidate water bodies acting as mosquito breeding grounds helped the country achieve malaria-free status in 2018. 17
Paraguay, in the WHO AMR, was declared malaria-free by the WHO in 2018, with the last indigenous case reported in 2011. 18 P. falciparum was the major reported parasite. Reporting of cases within 24 hours of detection and timely treatment, investigation of outbreaks within 24 hours of a case, GIS and establishment of a behavioural change communications plan for at-risk populations were some of the key steps.
Sri Lanka, which belongs to the WHO SEAR, was declared malaria-free in 2016, with the last case of indigenous P. vivax infection reported in 2012. 19 20 P. vivax and P. falciparum were the most prevalent parasites. Some of the crucial steps taken were the following: (1) the ‘1, 2, 3 approach’ that is confirmation within 24 hours (1 day) of malaria case by either a public or a private facility, investigation within 48 hours (2 days) and RACD within 72 hours (3 days); (2) close and periodic follow-up upto one year to tackle the resurgence of P. vivax cases in malaria camps and prevention of relapse due to lack of treatment compliance by directly observed primaquine (PQ) treatment was adopted 20 21 ; (3) public–private partnerships; (4) mobile clinics and (5) stringent vigilance on imported malaria, which is key to POR of malaria in Sri Lanka. 22 23 Despite facing a civil war, Sri Lanka achieved the elimination of malaria. The realisation that malaria is deadly but can be prevented and cured, the motivation and cooperation of conflicting groups to work with the government to protect the populations, and the involvement of neutral organisations played crucial roles. 24
Maldives became the first country within the WHO SEAR to eliminate malaria in 2015. The last case of indigenous P. vivax was reported in 1984, after which the reported cases were only from imported malaria. There are a total of 1200 islands in Maldives with large forested areas, out of which 198 are habitable. Important interventions which helped the country were the following: (1) hospital boat, called Golden Ray , which was equipped with medicines moved between the islands to treat patients (2) epidemiological and entomological surveys along with efforts to wipe out malaria vectors and (3) vigilance of imported malaria cases and vectors. 25
Armenia, in the WHO EUR, attained malaria-free status in 2011. The country reported its last indigenous case in 2009. P. vivax was the dominant parasite species and P. falciparum was via imported malaria. Mandatory notification, hospitalisation (in no later than 1–3 days), treatment of asymptomatic cases by supervised treatment, prophylaxis among military personnel and follow-up of patients for a period of 3 years for monitoring relapses were important steps. 26 27
Current challenges to India’s malaria elimination programme
India has managed to sustain the decline in overall malaria burden, but some of the significant current challenges which make malaria intractable in India are the following:
Incomplete understanding of the actual burden of malaria as the private sector is not involved in data reporting, although it caters to the healthcare needs of a large section of the population in India.
Inaccessible and remote areas of India are malaria-endemic (with persistent malaria), and providing health services to these communities becomes extremely difficult especially during monsoon and post-monsoon (transmission seasons) when these areas are cut off from the usual mode of communication and transportation.
Uncertain contribution of asymptomatic and low-density malaria infections to continued transmission of malaria.
Inadequate coverage and use of vector control products due to huge target population and time lag in replacements through a single channel of national control programme.
Cross-border malaria and internal migration.
Substantial burden of P. vivax malaria and weak mitigation policies and tools, such as missed diagnosis by the current methods, poor compliance to PQ’s 2-week course and lack of monitoring of relapses.
Emergence of drug and insecticide resistance in India’s neighbouring countries and border areas poses a threat of introduction of resistant parasites and vectors in the country.
Lack of skilled human resource in the national programme has been a long-standing challenge and more so with the integration of malaria programme with the general health services. Grass-root-level workers and healthcare staff are shared between several healthcare schemes and programmes and malaria may not be given the prioritisation it needs, more so when the target to report the last indigenous case is 2027 and elimination certification by 2030.
Lessons India can learn in its programme to accelerate malaria elimination
The national strategies for malaria elimination in the nine countries were mainly based on WHO guidelines and included intensified surveillance, vector control programmes, early diagnosis, rigorous case investigations, free and prompt treatment of patients based on malaria cases, and follow-ups. The key strategies of the nine countries are summarised in table 1 .
- View inline
Countries certified as malaria-free by the WHO from 2011 to 2021 and their key elimination strategies
India, in its national programme for malaria elimination, has all the major and essential elements well documented, and perhaps most of the steps are in the right direction to make malaria elimination possible. Additionally, certain strategies/policies/activities of the successful countries can be emulated in the following facets of the Indian elimination programme:
Strengthening of surveillance
Time-bound response by countries, such as the 1-3-7 strategy of China and the 1, 2, 3 strategy of Sri Lanka: a strong surveillance system was the most important pillar that played a crucial role in malaria elimination for most countries. The pivotal strategy, which could be adopted in our context, could be similar to those used in China and Sri Lanka. This will need to be supported by a strong web-based system that connects the public and private sectors at the level of healthcare to a central portal system. In India, at present, there is no time-bound strategy for mitigation of malaria cases on detection of a case. Hence, adopting some time frame would be useful in early management and thus in curtailing transmission. 28
Modernisation of surveillance system, that is, digital near real-time surveillance and smart surveillance systems: in China, a smart web-based health information system called the Chinese information system for disease control and prevention used time-bound alert Short Message Service (SMS) for follow-up and control measures. El Salvador also used computerised management information system to overcome delays in manual reporting system. 14 29 Such strong real-time surveillance and data-based decision making at the local level were also applied in Uzbekistan and Maldives. Countries like China and El Salvador overcame barriers by integrating digital technology and mobile SMS systems in their malaria elimination programme. Although surveillance has been strengthened in the malaria elimination drive in India, it still needs to be more inclusive and comprehensive. Therefore, this is the right time for India to adopt smart digital tools for surveillance, 30 and discussions at the national malaria elimination programme have already begun in this direction. Following the same, the ICMR-National Institute of Malaria Research has developed a Malaria Dashboard that is ready for data reporting, collation, visualisation and research. Case-based and foci-based examinations are much required, particularly in low transmission areas to achieve elimination in India. 31 Hence, implementation of a robust surveillance system (digital methods such as electronic dashboards) is very important. 30 32 It is therefore an opportunity for India to revamp its surveillance strategies from the archaic paper-based and aggregated systems to near real-time, digital and technology-backed integrated systems. 33 Such changes may fasten the process of malaria elimination.
Annual Parasite Index (API)-based stratification: India has stratified the states and districts (unit of implementation) based on their API. The subnational plan for elimination, although adopted by India, is yet to be fully deployed to certify states as malaria-free as and when they achieve this status.
Focus on high transmission areas: India, in its national strategic plan, has focused on high-burden endemic regions. Regular process monitoring, innovative research and prompt translation in policy along with increased community mobilisation will play an important role in reducing malaria cases.
Involvement of the private sector in reporting of malaria case data: Sri, Lanka, El Salvador and Paraguay have led by example and allowed active involvement of the private sector in the mainstream of malaria surveillance and management. In India, participation of the private sector is crucial because it provides 60%–70% of healthcare. The inclusion of this sector in India is in the nascent stages as there is no concrete roadmap towards this aim. We have suggested ways to involve the private sector in our previous work. 34 Additionally, India could gain insights from the national programmes of Sri Lanka, El Salvador and Paraguay which have actively involved private providers. India has made malaria a notifiable disease in 31 states, but it is only an initial step towards tackling under-reporting and underestimation of malaria burden in the country. Rapid diagnostics as field diagnostics have been the cornerstone of early identification and thus timely management of cases. Over-the-counter availability of rapid diagnostic tests (RDTs) in the commercial sector can empower people to self-diagnosis and reporting to the healthcare system. 34
Use of molecular tools of diagnosis and national reference laboratories
Prompt and accurate diagnosis of malaria cases, including the hidden burden of asymptomatic and subpatent infections, is important as it will help in treatment and thus cessation of transmission. Adoption of molecular methods for diagnosis in the national programme would be a way forward. The WHO recommends microscopy as the gold standard and RDT as field diagnostics. Use of molecular tools like PCR and loop-mediated isothermal amplification for RACD, as adopted by China, was useful in the identification and resolution of all malaria cases. India suffers from considerable burden of low-density infections which escape detection by routine diagnostics. 31 The development of field-friendly, point-of-care/collection molecular tests could help bring out the burden and management of subpatent malaria. 35 District-level healthcare facilities have been empowered in terms of infrastructure and expertise owing to the COVID-19 pandemic and these can be co-opted for diagnosis of submicroscopic malaria. 36 37 In India, the barrier to adopting molecular tools in its routine programme would be the prohibitive cost of infrastructure and training of the laboratory workforce. However, countries like China and Sri Lanka have shown the way that it is possible to use these more sensitive tools as routine diagnostics. The establishment of the National Reference Laboratory for quality assurance was adopted by China, El Salvador, Uzbekistan, Paraguay and Armenia. Having such central hub that connects all states and district-level laboratories can step up India’s centralized diagnostic structure.
India, in its national guidelines, has a special emphasis on P. vivax elimination. The foreseeable barriers for India are poor compliance of PQ treatment, inadequate follow-up of patients with P. vivax malaria, cross-border and migration issues. Compliance to antimalarials, especially for P. vivax malaria, which needs 14-day treatment with PQ is a daunting challenge in India. Almost half of India’s malaria burden is P. vivax malaria. It is widely acknowledged that it will be difficult to achieve elimination of P. vivax as compared with P. falciparum . Adoption of single-day treatment with tafenoquine may be considered by India after due regulatory consideration. 38 The issue of compliance can be overcome if the P. vivax antimalarial therapy is administered as directly observed treatment (DOT). We could follow the Sri Lankan example which to tackle the P. vivax resurgence in army camps adopted PQ directly observed treatment for infected army personnel. 20 21 El Salvador and Uzbekistan supervised the PQ treatment. Similarly, Armenia had also introduced DOTs for both P. falciparum and P. vivax control in their national programme. Good compliance to 14-day radical treatment with primaquine along with estimation of glucose-6-phosphate dehydrogenase (G6PD) deficiency in the population, addressing low-density infections and tackling asymptomatics will play pivotal role in P. vivax elimination.
Follow-up of P. vivax cases to capture relapse cases: P. vivax malaria is characterised by latent hypnozoites which can get activated in variable durations. Therefore, it is important to follow these cases so as to capture relapse cases and treat them on time. In the national guidelines of Sri Lanka, El Salvador, Armenia, Algeria and Maldives, at least 6 months to 1 year of follow-up was practised.
Cross-border malaria: countries which have achieved malaria elimination have robust mitigation strategies against imported malaria. Cross-country cooperation is at the centre of the elimination programme. Strict surveillance of cross-border transmission as embraced by China, Algeria, El Salvador, Sri Lanka, Armenia, Paraguay and Uzbekistan with deployment of mobile teams and examination of travellers from malaria-endemic countries through RACD could be possible steps which need induction in our control guidelines. India has porous borders with many neighbouring malaria-endemic countries and also poses a threat to the neighbouring countries which are at the cusp of elimination such as Bhutan. 39 Therefore, India should institute strong parasite and vector surveillance programmes to curtail exchange. Cross-border malaria issues have been handled well by China, Algeria, El Salvador, Sri Lanka, Armenia, Paraguay and Uzbekistan by intense surveillance of migrants and travellers.
Internal migration: El Salvador had carried out active surveillance and chloroquine+primaquine (CQ+PQ) single-dose prophylaxis for migrant populations in employments such as cotton production, coffee fields or factories. 13 In India, the interstate movement of people is high for employment, tourism and other purposes. Special attention is needed in areas where malaria elimination status has progressed from control to pre-elimination phase. For example, the state of Punjab has shown a drastic decline in the number of malaria cases. 40 However, there is always a risk of re-establishment owing to the constant influx of migrant labourers for construction/agriculture activities in the state. This mobile population is very often from malaria-endemic states such as Bihar, Chhattisgarh and Jharkhand and thus could act as reservoirs for the parasite resulting in re-establishment of infection. Thus, India could also consider devising plans for screening, treating and reporting of malaria cases among such migrant populations.
Many malaria elimination demonstration projects have successfully shown that adopting certain strategies can dent the malaria endemicity situation. One of the programmes, the Comprehensive Case Management Plan (CCMP), has been adopted by the government of Odisha as the Durgama Anchalare Malaria Nirakarana (DAMaN) programme for mitigation of malaria in inaccessible areas and has contributed to a remarkable decline in malaria. Biannual screening of malaria in mass surveys and subsequent treatment has been adopted as a programme strategy in this state’s malaria plan. 41
In order to implement public–private partnerships, Indian policy makers should devise a well-defined strategy to work locally and focally at panchayat/district levels with emphasis on common platform for reporting, regular communication and assessment of progress.
Vector control and management of resistance
Robust vector surveillance using smart tools: China, Algeria and Sri Lanka adopted a robust vector surveillance with the use of GIS and spatiotemporal analysis. Similar to these platforms, a web-based database of vector surveillance should be adopted in India.
Insecticide resistance management (IRM): Resistance to routinely used insecticides (DDT and some synthetic pyrethroids) has been reported in the malaria-endemic areas of India. Frequency of insecticide resistance should be monitored at sentinel sites periodically. IRM with rotational or mosaic pattern with insecticides of different mechanisms of action has been deployed by Sri Lanka. Focal IRS in areas such as plantations, factories and along countries’ border with high endemicity regions have been adopted by China, Sri Lanka and El Salvador. Environmental engineering methods were adopted by Argentina. All these strategies and tools could be useful to India with its diverse geographical regions. Laboratory studies conducted in India are indicative that newer tools like attractive toxic sugar baits (ATSBs) could be a promising vector control. 42
Integrated vector management (IVM): IRM and IVM, although discussed in India, are not holistically implemented. In Maldives, elimination of malaria vectors was one of the key contributing factors to maintaining a malaria-free status since 1984. El Salvador and Armenia implemented water management projects to reduce mosquito breeding sites and also planted neem trees to prevent mosquitoes in the surrounding areas. India should consider IVM as an umbrella vector management programme.
Role of partners
Currently, the different partners and stakeholders in India are working in silos towards the common goal of malaria elimination. There is a lack of cohesion at the central level and thus at the peripheral levels. Experiences of other countries can be leveraged on using the strengths of partner organisations and taking them in the fold of the national programme. Sri Lanka’s successful elimination was achieved despite facing a civil war. Indian policy makers could involve NGOs, private partners and voluntary collaborative network, as adopted by Sri Lanka, El Salvador, Armenia, Paraguay and Algeria, to enhance successful deployment of all components of malaria elimination. Involvement of intersectoral ministries and uninterrupted funding were adopted in Sri Lanka to eliminate the disease. National and international partners are crucial to achieving malaria elimination, especially for overcoming the last-mile challenges. 39
Prevention of re-establishment strategies
POR of malaria transmission in a malaria-free country is a daunting task. After elimination, active case detection (ACD) with mobile malaria clinics is still maintained in Sri Lanka. Algeria has taken stern steps in quickly identifying any imported malaria, followed by appropriate POR actions. Obligatory notification and reporting of malaria and timely epidemiological investigation of each imported case and focus are followed by Paraguay, Uzbekistan, El Salvador and Maldives. These activities would need to be undertaken by the states which have eliminated malaria to prevent its re-establishment from other states. India would need robust alert systems and prompt surveillance and diagnostics to mitigate the threat of imported malaria, as done by other countries.
Domestic funding and sustained political commitment
In addition to global and international funding {GFATM, World Bank, President’s Malaria Initiative (PMI)/United States Agency for International Development (USAID)}, China, Sri Lanka, Algeria, Armenia, Uzbekistan and El Salvador allotted heavy domestic funding for malaria elimination. 2 In India, the national programme is mainly funded by the Government of India, but the Global Fund is the major financial source for procurement of long-lasting insecticidal nets (LLINs) in India. From 2016 to 2018, ~80% (~40 million) of the LLINs distributed in the country were procured by the Global Fund financial resources. Political and financial commitment from the government is vital to maintain the momentum of the malaria elimination programme in India. 43 India needs to pledge substantial funds for sustenance of the national programme for malaria elimination and beyond. Provision of funds in the scenario of withdrawal of the Global Fund also needs to be created.
Promoting research
Research and Development (R&D) need constant thrust as the limitations of the currently available tools can hinder the achievement of malaria elimination, and threats like drug and vector resistance need investment in research to discover newer tools. Malaria-free countries have invested in research to identify the most optimum strategies, tools and operations. China invested in R&D and artemisinin derivatives have been the cornerstone of malaria treatment. In 1967, the CDC Division of Parasitic Diseases was set up in San Salvador. 44 Efforts should be put in to develop and validate non-histidine-rich protein (non-HRP) 2/3-based RDTs, feasibility of a single dose of tafenoquine for P. vivax malaria 38 , field-friendly molecular tools, and robust research to assess the impact of climate change on malaria transmission. 45 Research into the possible zoonotic transmission of malaria parasites in India should also be considered. Innovative approaches to mosquito control like ATSB, 42 insecticide impregnated clothing, hammocks etc could be explored to address the challenges associated with forest malaria, 5 outdoor biting and insecticide resistance. Concerted efforts have been initiated in this direction by a nodal research body of the Government of India. 46 Consolidation and implementation of the research findings into policy and practice would provide the necessary thrust to malaria elimination in India. However, poor investment and lack of priority to continue research once elimination is near or achieved can derail research programmes on promising tools. Advocacy for continued and breakthrough research needs to be made at the highest level.
India’s track record in elimination of other infectious diseases
Despite enormous population and diverse geographical conditions, India has successfully eliminated polio (2014), 47 smallpox (1977) 48 and guinea worm disease (2000) 49 50 and is possibly on track to eliminate tuberculosis by 2025.
India was certified polio-free in 2014. Considering the scale at which the polio vaccination drive was conducted, it can be considered as one of the biggest success stories. However, the path was not easy for India. The challenges ranged from arranging logistics for a large population and reaching even the hard-to-reach areas, building trust, changing perceptions and convincing the communities to accept vaccines amidst anti-vaccine movements. 51 This was achieved by enhanced communication within the community, by involving local representatives and religious leaders, and by providing basic health packages to address immediate concerns regarding other health issues. Screening of migrant and mobile populations and international travellers played a crucial role in identifying potential sources of continued transmission. In addition to government officials, several partners worked collectively in the polio elimination drive. Defining the role and accountability of each of the public and private stakeholder was also done to avoid redundancy in the tasks performed. Further, the accuracy of data was monitored to get reliable information on disease prevalence. The need for training healthcare workers was identified and addressed by capacity building and repeated trainings. 52
As India is hurtling towards malaria elimination, it is the most appropriate time to review and assess the strategies and practices by countries that have been successful in achieving malaria elimination. The same can be tailored according to India and neighbouring South Asian countries as they share several commonalities in the context of environmental conditions, vectors, parasites, community behaviour and health infrastructures. These shared features could be the basis of cross-learnings and can help India and others steer their malaria elimination programme.
Ethics statements
Patient consent for publication.
Not required.
Acknowledgments
We acknowledge Bhabani Shankar Muduli and Mansi Arora for their contribution and help in generating the world map depicting country-wise contribution to global malaria cases (figure 1).
- ↵ Countries and territories certified malaria-free by who . Available: https://www.who.int/teams/control-of-neglected-tropical-diseases/yaws/diagnosis-and-treatment/global-malaria-programme [Accessed 16 Dec 2021 ].
- World Health Organization
- ↵ High burden to high impact: a targeted malaria response. , 2021 . Available: https://www.who.int/publications-detail-redirect/WHO-CDS-GMP-2018.25 [Accessed 17 Dec 2021 ].
- India CO for, Organization WH
- ↵ World malaria report 2020. 2021 . Available: https://www.who.int/publications-detail-redirect/9789240015791 [Accessed 17 Dec 2021 ].
- Yin J-hai ,
- Yang M-ni ,
- Zhou S-sen ,
- Zhou S , et al
- Ruktanonchai NW , et al
- Beiersmann C , et al
- Huang F , et al
- Liang X-H ,
- Lu S-N , et al
- ↵ Malaria elimination in El Salvador: a historical and epidemiological perspective . Available: https://www.path.org/resources/malaria-elimination-in-el-salvador-a-historical-and-epidemiological-perspective/ [Accessed 17 Dec 2021 ].
- Burton RA ,
- Chévez JER ,
- Sauerbrey M , et al
- Nasir SMI ,
- Amarasekara S ,
- Wickremasinghe R , et al
- Alba Soto C
- Razakov SA ,
- Shakhgunova GS
- ↵ Paraguay now malaria-free . Available: https://www.downtoearth.org.in/news/health/paraguay-now-malaria-free-60829 [Accessed 16 Dec 2021 ].
- Abeyasinghe RR ,
- Galappaththy GNL ,
- Smith Gueye C , et al
- Fernando SD ,
- Rodrigo C ,
- de Silva N , et al
- Premaratne R ,
- Wickremasinghe R ,
- Ranaweera D , et al
- Gosling R ,
- Abeyasinghe R
- Fernando D ,
- Wijeyaratne P ,
- Hounsell KG ,
- Sadiq T , et al
- ↵ Asia Ro for S-E, organization WH. Malaria-free Maldives. who regional office for south-east Asia , 2016 . Available: https://apps.who.int/iris/handle/10665/250397 [Accessed 17 Dec 2021 ].
- Grigorian G ,
- Solkhomonian L
- Davidyants VA ,
- Kondrashin AV ,
- Vanyan AV , et al
- Sturrock HJW ,
- Cotter C , et al
- Herrera S ,
- Ochoa-Orozco SA ,
- González IJ , et al
- Gahtori R , et al
- Pal Bhowmick I ,
- Chouhan A , et al
- Saroha P , et al
- Baharia RK ,
- Das P , et al
- Singh K , et al
- ↵ Monthly malaria information system (MMIS): national center for vector borne diseases control (NCVBDC) . Available: https://nvbdcp.gov.in/index1.php?lang=1&level=1&sublinkid=5879&lid=3957 [Accessed 17 Dec 2021 ].
- Ghosal J , et al
- ↵ Laboratory evaluation of the efficacy of boric acid containing toxic sugar baits against Anopheles culicifacies, an. stephensi and Aedes aegypti mosquitoes . Available: https://www.jvbd.org/preprintarticle.asp?id=331414;type=0 [Accessed 2 Jan 2022 ].
- ↵ Malaria : National Center for Vector Borne Diseases Control (NCVBDC) . Available: https://nvbdcp.gov.in/index1.php?lang=1&level=1&sublinkid=5784&lid=3689 [Accessed 29 Dec 2021 ].
- Caminade C ,
- Rocklov J , et al
- Vashishtha VM
- ↵ Guinea Worm Eradication Programme (GWEP) : National Centre for Disease Control (NCDC) . Available: https://ncdc.gov.in/index1.php?lang=1&level=1&sublinkid=142&lid=73 [Accessed 24 Feb 2022 ].
- Bellatin A ,
- Rao S , et al
Handling editor Seye Abimbola
Contributors MR and AS conceived the idea and framed the manuscript. SS wrote the initial draft. RV, BY and AK did review of literature, analysis and graphics. All authors read and approved the manuscript.
Funding The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Map disclaimer The inclusion of any map (including the depiction of any boundaries therein), or of any geographic or locational reference, does not imply the expression of any opinion whatsoever on the part of BMJ concerning the legal status of any country, territory, jurisdiction or area or of its authorities. Any such expression remains solely that of the relevant source and is not endorsed by BMJ. Maps are provided without any warranty of any kind, either express or implied.
Competing interests None declared.
Provenance and peer review Not commissioned; externally peer reviewed.
Read the full text or download the PDF:
WHO World Malaria Report 2020: India continues to make Impressive Gains in reduction of Malaria Burden India the only high endemic country which has reported a decline of 17.6% in 2019 over 2018 India has sustained Annual Parasitic Incidence (API) of less than one since 2012
The World Malaria Report (WMR) 2020 released by WHO, which gives the estimated cases for malaria across the world, based on mathematical projections, indicates that India has made considerable progress in reducing its malaria burden. India is the only high endemic country which has reported a decline of 17.6% in 2019 as compared to 2018. The Annual Parasitic Incidence (API) reduced by 27.6% in 2018 compared to 2017 and by 18.4% in 2019 as compared to 2018. India has sustained API less than one since year 2012.
India has also contributed to the largest drop in cases region-wide, from approximately 20 million to about 6 million. The percentage drop in the malaria cases was 71.8% and deaths was 73.9% between 2000 to 2019.
India achieved a reduction of 83.34% in malaria morbidity and 92% in malaria mortality between the year 2000 (20,31,790 cases, 932 deaths) and 2019 (3,38,494 cases, 77 deaths), thereby achieving Goal 6 of the Millennium Development Goals (50-75% decrease in case incidence between 2000 and 2019).
Figure 1: Epidemiological trends of Malaria in India (2000-2019) Pv; Plasmodium Vivax & pf; Plasmodium Falciparum
Decrease in incidence of Malaria cases is also exhibited in the year-on-year tally. The cases and fatalities have declined significantly by 21.27% and 20% in the year 2019 (3,38,494 cases, 77 deaths) as compared to 2018 (4,29,928 cases, 96 deaths). The total number of malaria cases reported in 2020, till October, (1,57,284) has further decreased by 45.02 percent as compared to corresponding period of 2019 (2,86,091).
Malaria Elimination efforts were initiated in the country in 2015 and were intensified after the launch of National Framework for Malaria Elimination (NFME) in 2016 by the Ministry of Health and Family Welfare. National Strategic Plan for Malaria Elimination (2017-22) was launched by the Health Ministry in July, 2017 which laid down strategies for the next five years.
Figure 2: Epidemiological situation of Malaria in India (2015 – 2019)
The first two years saw a 27.7% decline in cases and 49.5% reduction in fatalities; 11,69,261 cases and 385 deaths in 2015to 8,44,558 cases and 194 deaths in 2017.
States of Odisha, Chhattisgarh, Jharkhand, Meghalaya and Madhya Pradesh disproportionately accounted for nearly 45.47 percent (1,53,909 cases out of India’s 3,38,494 cases) of malaria cases and 70.54 percent (1,10,708 cases out of India’s 1,56,940 cases) of falciparum Malaria cases in 2019. 63.64% (49 out of 77) of malaria deaths were also reported from these states.
Due to the efforts made by the Government of India in provision of microscopes, rapid diagnostics Long Lasting Insecticidal Nets (LLINs) – about 5 crores have been distributed in 7 North-East States, Chhattisgarh, Jharkhand, Madhya Pradesh and Odisha up to 2018-19 and another 2.25 crore LLINs are being supplied/distributed during current financial year to high burden areas leading to reduction in endemicity in these otherwise very high endemic states. Additional procurement of 2.52 crore LLINs is initiated.Use of LLINs has been accepted by the community at large and has been one of the main contributors to the drastic malaria decline in the country.
Decline of API in HBHI (High Burden High Impact) Regions of India (2016-2019)
WHO has initiated the High Burden to High Impact (HBHI) initiative in 11 high malaria burden countries, including India. Implementation of “High Burden to High Impact (HBHI)” initiative has been started in four states i.e. West Bengal and Jharkhand, Chhattisgarh and Madhya Pradesh in July, 2019. A key strategy to reignite progress is the “High burden to high impact” (HBHI) response, catalyzed in 2018 by WHO and the RBM Partnership to End Malaria continued to make impressive gains in India, with 18% reductions in cases and 20% reductions in death respectively, over the last 2 years.
Malaria has been made notifiable in 31 states/UTs (Andhra Pradesh, Arunachal Pradesh, Assam, Chhattisgarh, Goa, Gujarat, Haryana, Himachal Pradesh, Jammu & Kashmir, Jharkhand, Karnataka, Kerala, Madhya Pradesh, Manipur, Mizoram, Nagaland, Odisha, Punjab, Rajasthan, , Sikkim, Tamil Nadu, Telangana, Tripura Uttar Pradesh, Uttarakhand, West Bengal, Pudducherry Chandigarh, Daman & Diu, D&N Haveli and Lakshadweep) and decline has been observed in the hitherto high endemic states. Percentage of decline in the year 2019 as compared to 2018 is as follows: Odisha – 40.35%, Meghalaya- 59.10%, Jharkhand – 34.96%, Madhya Pradesh –36.50% and Chhattisgarh –23.20%.
The figures and trends between last two decades clearly show the drastic decline in malaria. The malaria elimination target of 2030 looks achievable building on the Union Government’s strategic interventions in this regard.
GIS maps – Shrinking malaria endemicity (District level)
HFW/World Malaria Report/2ndDecember2020/1
BRIEF RESEARCH REPORT article
Malaria elimination: situation analysis of cases in india, the state of madhya pradesh in central india, and district mandla of madhya pradesh.

- 1 Malaria Elimination Demonstration Project, Mandla, Madhya Pradesh, India
- 2 Indian Council of Medical Research, National Institute of Malaria Research, New Delhi, India
- 3 Department of Health Services, Government of Madhya Pradesh, Mandla, Madhya Pradesh, India
- 4 Directorate General of Health Services, Government of Madhya Pradesh, Bhopal, Madhya Pradesh, India
- 5 Foundation for Disease Elimination and Control of India (FDEC India), Mumbai, Maharashtra, India
- 6 Sun Pharmaceutical Industries Ltd., Mumbai, India
India contributed approximately 66% of the malaria cases in the WHO South-East Asia region in 2022. In India, approximately 44% of cases have been reported to be disproportionately contributed by approximately 27 districts. 1 A comparative analysis of reported malaria cases between January 2017 and December 2022 was performed in Mandla district, which is the site of a model malaria elimination demonstration project (MEDP) in Madhya Pradesh (MP), India. Compared to 2017, the decrease in malaria cases in Mandla from 2018 to 2022 was higher than MP and the rest of the country. The reduction of cases was significant in 2018, 2019, and 2021 ( p < 0.01) (Mandla vs. MP) and was highly significant during 2018–2022 ( p < 0.001) (Mandla vs. India). Robust surveillance and real-time data-based decisions accompanied by appropriate management, operational controls, and independent reviews, all designed for resource optimisation, were the reasons for eliminating indigenous malaria in Mandla district. The increase in infection rates during the months immediately following rains suggests that surveillance, vector control, and case management efforts should be specifically intensified for eliminating imported and indigenous cases in the near-elimination districts to work towards achieving the national elimination goal of 2030.
Introduction
Malaria remains one of the most important public health problems globally, with an estimated 249 million cases and 608,000 malaria-attributable deaths reported in 2022. Approximately 94% of global malaria cases are contributed by African countries, while 2% of cases are contributed by countries in the World Health Organization (WHO) South-East Asia (SEA) region. India accounted for approximately 66% of the malaria cases in the WHO SEA region in 2022 ( 1 ).
During the COVID-19 pandemic between 2019 and 2020, the global burden of malaria increased by 6%, primarily due to the disruption of anti-malarial activities. In comparison, India was the only High Burden High Impact (HBHI) country that reported a 46% decrease in malaria cases between 2019 and 2020. However, there was a 50% decrease in the distribution of insecticide-treated bed nets in India in 2020 ( 2 ).
In India, approximately 44% of the reported malaria cases and 43% deaths are disproportionately contributed by approximately 27 tribal-dominated districts that comprise 5% of the country's population. Among these cases, 57.3% are identified as Plasmodium falciparum infections ( 3 ).
India had set the target to achieve zero indigenous malaria cases in 26 low-to-moderate endemic malaria states/Union Territories (UTs) by 2022 and eliminate malaria throughout the country by 2027. The proposed strategies included strengthening malaria surveillance, establishing the mechanism for early case detection and prompt treatment, distribution and promotion of the use of long-lasting insecticidal nets (LLIN), effective indoor residual sprays (IRS), capacity-building of community healthcare service providers, and inter-sectorial coordination. The 2022 target of zero indigenous cases was achieved by only two states/UTs of Puducherry and Lakshadweep, with Chandigarh and newly formed UT of Ladakh reporting only two cases each in 2022 ( 3 , 4 ).
Inaccessible terrains, dense forest covers, perennial streams, poor socioeconomic indicators, poor health-seeking behavior, and inadequate health infrastructure are the significant challenges for malaria elimination in tribal-dominated areas of India. People living in these malaria-endemic areas have poor access to formal health facilities. Unqualified healthcare providers and traditional faith healers are often the first points of contact in the rural tribal areas, which is the primary cause of delay in prompt diagnosis and radical treatment ( 5 ).
In 2017, the MEDP was launched as a public–private partnership project between the Government of Madhya Pradesh (MP), Indian Council of Medical Research (ICMR), and Foundation for Disease Elimination and Control (FDEC) of India—a corporate social responsibility (CSR) subsidiary of Sun Pharmaceutical Industries Ltd.—to demonstrate that malaria elimination is possible in hard-to-reach, hilly, forested, and tribal-dominated areas. The MEDP's malaria operational elimination plan used the T4 (Track fever, Test fever, Treat malaria, and Track treatment) strategy, monitoring of vector control interventions, Mass Screening and Treatment (MSaT), needs-assessment followed by capacity-building, regular monitoring, and supervision for data-driven decision-making to ensure best outcomes of the resources deployed for the project ( 6 – 9 ).
The MEDP also estimated the burden of sub-microscopic malaria infection and the importation of cases into the district. From September 2017 to March 2021, for a total of 43 months of field operations, the MEDP achieved a 91% reduction in indigenous malaria cases with 10 consecutive months of zero transmission of indigenous malaria cases ( 10 ).
In the MEDP, the key interventions added to complement the interventions of the national programme included: (1) robust active surveillance using the T4 strategy, (2) periodic mass survey and treatment adopting the stratified clustered random sampling method, (3) molecular diagnosis of a subset of samples to estimate the burden of low-density malaria infection and asymptomatic cases, (4) supervised and quality-assured IRS and LLIN distribution for vector control efforts, (5) regular capacity-building of healthcare providers, (6) innovative information education communication/behavior change communication (IEC BCC) campaigns, and (7) robust reviews and accountability frameworks.
The present situation analysis was conducted to track malaria elimination progress in Mandla district post-MEDP and to highlight how the lessons learned could help achieve the national malaria elimination goal.
This study presents the situation analysis of the reported malaria cases between January 2017 and December 2022 in Mandla district. It compares them with the reported cases in MP and India during the same period. In Mandla, the monthly malaria prevalence data were collected from the MEDP data repository, which included the active and passive cases detected using rapid diagnostic tests (RDTs), microscopic examination of blood smears, and data provided by the District Malaria Office. During the study period, the total reported malaria cases of Mandla district were classified into two groups, namely indigenous and imported cases. Annual malaria prevalence data from the state of MP and India were obtained from the official website of the National Center for Vector Borne Disease Control (NCVBDC). The annual per cent decline in malaria cases, along with a 95% confidence interval, was estimated from 2017 as a reference year. The Chi-squared test was used to compare percentage change over multiple time points between Mandla vs. MP and India. The statistical analysis was performed using R for Windows version 4.3.2. The monthly trend of malaria cases during the MEDP (January 2017–March 2021) and the post-MEDP (April 2021–December 2022) period in Mandla district is presented in Figure 1 . The comparison of the annual per cent decline in malaria cases over multiple time points between Mandla district, the state of MP, and the country is shown in Table 1 .
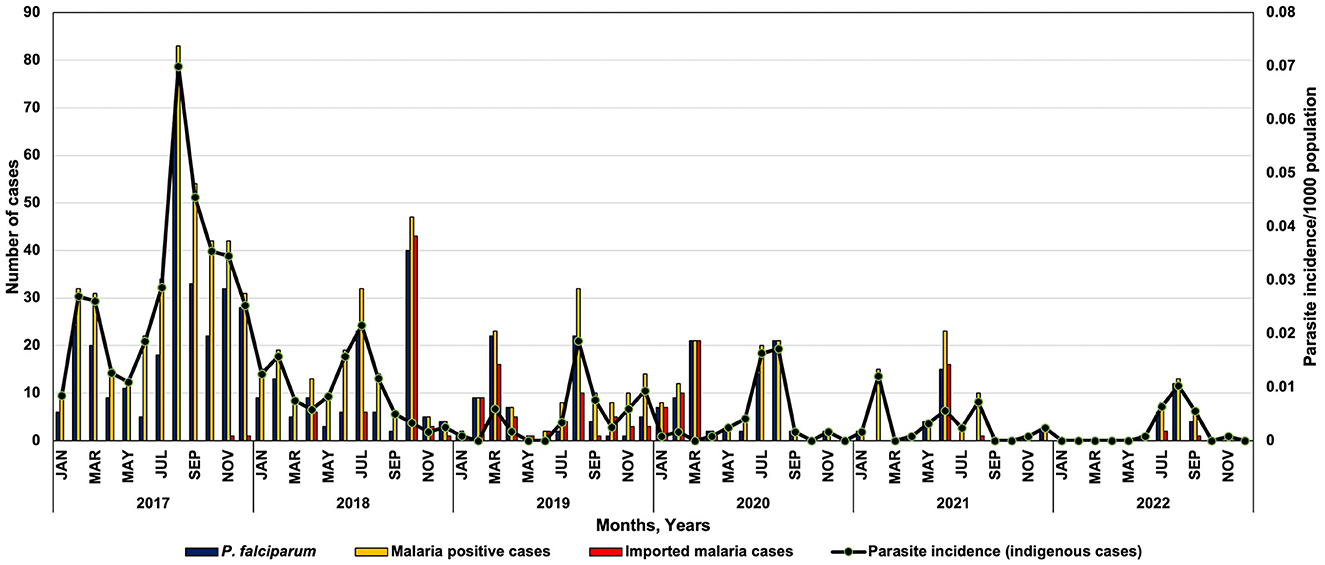
Figure 1 . Monthly trend of Plasmodium falciparum , malaria cases and parasite incidence in district Mandla during 2017–2022.
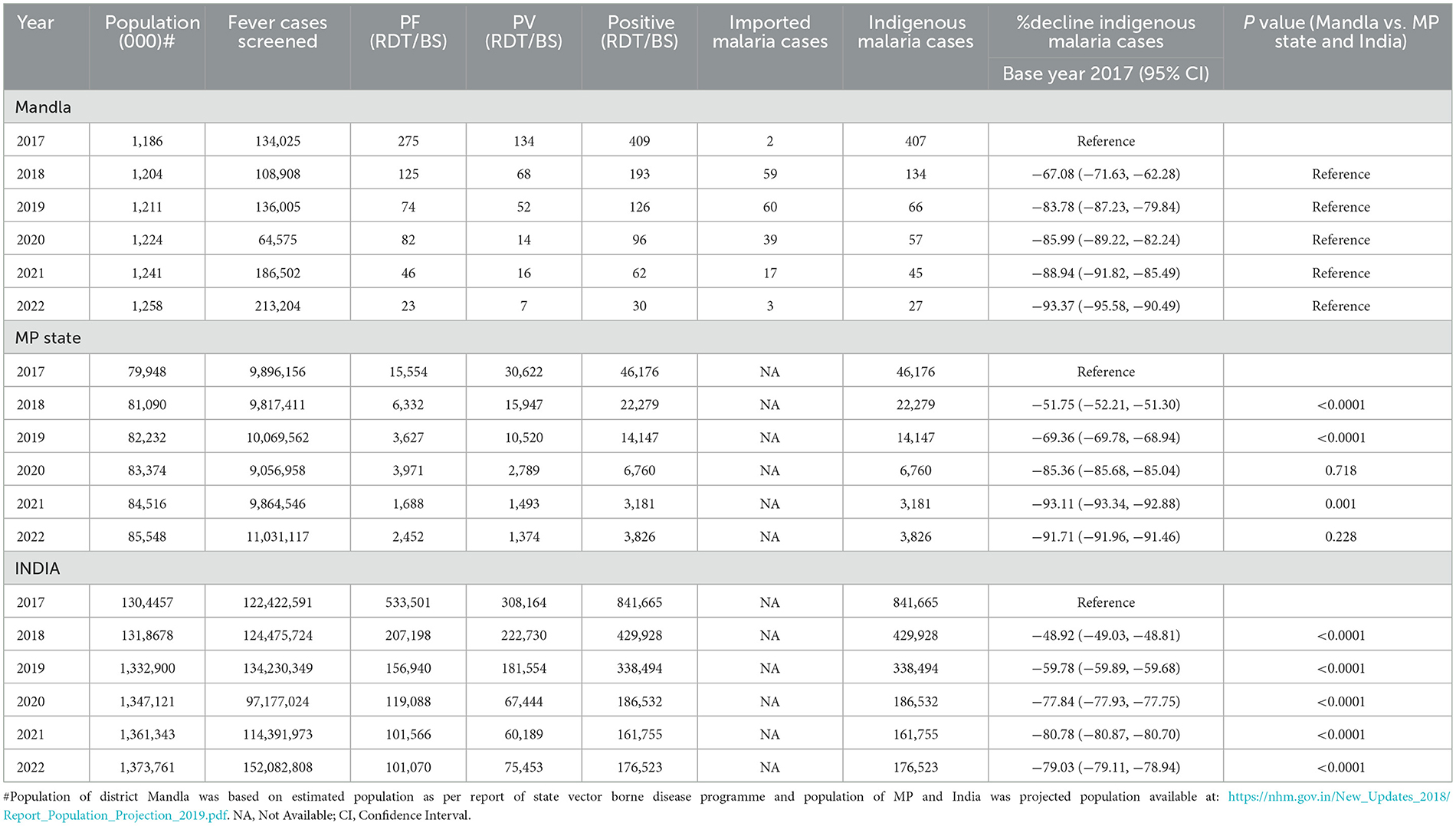
Table 1 . Situation analysis of malaria cases during 2017 and 2022 in district Mandla, Madhya Pradesh and India.
Mandla district is located at the geo-coordinates of 22° 38' 25.476” N latitude and 80° 30' 48.384 E longitude. This district is among the tribal dominant and hilly forested districts in the state of MP. Approximately 58% of the population belonged to the ethnic tribal groups, mainly “ Gond” and “ Baiga” (Particularly Vulnerable Tribal Group). The transmission dynamics of malaria in the district is seasonal, and Anopheles culicifacies is the main malaria vector that breeds in perennial streams ( 11 ).
In reference to 2017 as the base year, the per cent decrease in malaria cases in Mandla district was 67.08%, 83.78%, 85.99%, 88.94%, and 93.37% from 2018 to 2022. At the state level, in MP, the percent decrease in malaria cases during this period was 51.75%, 69.36%, 85.36%, 93.11%, and 91.71%, respectively. Similarly, during the same period in India, the per cent decrease in malaria cases was 48.92%, 59.78%, 77.84%, 80.78%, and 79.03%, respectively ( Table 1 ).
Further analysis revealed that the per cent decrease in malaria cases in Mandla from 2018 to 2022, in reference to the year 2017, was significantly higher than MP during 2018 and 2019. The decrease was significantly higher in district Mandla than in the entire country from 2018 to 2022.
It should be noted that the data on malaria cases from district Mandla were obtained using active surveillance, passive surveillance, data from health camps, primary health centers, community health centers, district hospitals, and the sentinel surveillance network, which included registered public and private practitioners in the district. In comparison, the state and country data come solely from public (government) sources.
The monthly trend of P. falciparum malaria cases and parasite incidence/1,000 population showed a seasonal variation in the distribution of Plasmodium species in Mandla district. Most of the P. vivax cases were reported from March to August, showing peaks between June and August and then dominated by P. falciparum cases from September with peaks from October to December ( Figure 1 ).
Mandla district reported malaria cases throughout 2017 and 2018. Zero indigenous malaria cases were reported for 3 months each in 2019, 2020, and 2021, and there were zero indigenous malaria cases for seven months in 2022. Compared to the years 2017–2020, where there were two distinct peaks of malaria in February–March and July–September, there was only one peak with much lower intensity in the July–September months of 2021 and 2022. The month-wise trend at the state and country level could not be analyzed due to the non-availability of seasonal data in the public domain.
The comprehensive surveillance strategy provided a robust estimate of malaria cases in Mandla district as compared to the rest of the state and the country. The MEDP also implemented MSaT to diagnose and treat the asymptomatic malaria cases during 2018–2020 and adopted the stratified clustered sampling method based on the malaria endemicity ( 12 ). Therefore, the Mandla malaria estimates were a true “total” burden of malaria as compared to the state of MP and the rest of the country. Furthermore, a higher rate of decline in malaria cases was observed during the year 2022. Most of the malaria cases were reported during the monsoon season (June–September), along with zero reported indigenous malaria cases in the consecutive 8 months of the post-intervention period of the MEDP between 2021 and 2022.
Based on the findings from the malaria elimination project in Mandla district, the significant reduction in malaria cases over 4 years is attributable to robust (active and passive) surveillance using digital tools, the T4 strategy, active monitoring of vector control interventions, periodic capacity-building of the healthcare providers, regular community mobilization, MSaT, and molecular diagnosis of a subset of samples to estimate the burden of low-density malaria infection and asymptomatic cases. The institution of appropriate management and operational controls, along with frequent internal and external reviews, contributed to prompt actions and responses based on the real-time data ( 10 , 11 , 13 , 14 ). These protocols ensured the best outcomes of human, commodity, and financial resources used for the elimination project.
The MEDP regularly monitored and supervised vector control interventions in the district. The regular use of LLINs in the community increased from 34% (95% CI: 33.74–34.26) in 2017 to 47% (95% CI: 46.80–47.19) in 2019, and this difference was significant statistically ( p < 0.0001). The spraying quality of the IRS improved from 47.8% in 2017 to 88.6% in 2019, and the improvement in satisfaction with the IRS by the community increased from 66.8% to 90.5% within the same period ( 15 – 17 ).
Alphacypermethrin was used in LLIN and IRS in Mandla. As part of the MEDP, the insecticide susceptibility tests were conducted periodically during 2017, 2018, and 2019 to regularly monitor insecticide resistance to the vector species. The results showed that alphacypermethrin was possibly resistant to the Anopheles culicifacies in 2017 and further developed resistance in the year 2019 ( 15 ).
The strategies used in the MEDP can serve as a guide to develop and/or refine the district-specific malaria elimination operational plans by treating the district as an operational unit as has been already proposed by NCVBDC. In addition, linking data from each district through digital systems for robust surveillance, effective supply chain management, and real-time data analysis and reporting would be highly useful for programme managers and policy makers ( 18 ).
Two additional noteworthy observations from the MEDP study that are critical to malaria elimination are: (1) the finding of 1.51% of sub-microscopic infections in the community, detected through the diagnostic PCR method, and (2) the prevalence of asymptomatic malaria that was found to be 0.98% during the mass survey conducted by the MEDP from 2018 to 2020. Based on this information, the national programme should consider testing a subset of cases using sensitive PCR methods to determine sub-microscopic infection and conduct periodic mass surveys to identify and treat asymptomatic cases during the elimination phase ( 19 ).
The incidence data for Mandla, where indigenous transmission of malaria was interrupted several times during the conduct of the project, indicates that intensified surveillance, case management, and vector control efforts immediately after rains would lead to the elimination of infections, whether they are imported or are indigenous. Additionally, the gradual increase in the malaria-free months from 2019 to 2022 indicates that the gains achieved throughout the MEDP were progressive and sustained in the district. We firmly believe that the sustained gains were attributed to robust real-time internal and external reviews as part of the programme's management and operational controls.
Robust surveillance would provide information on individuals requiring treatment, including imported cases. Molecular diagnostic tests would help determine the burden of sub-microscopic/sub-RDT and asymptomatic infections. IRS and LLINs, together with minor engineering, should be deployed simultaneously, followed by an independent assessment of the households for the use of LLINs and IRS. Internal and external data quality reviews should be conducted for accountability at operational, human resource, supply chain, and scientific levels required for elimination goals.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Author contributions
MS: Conceptualization, Data curation, Formal analysis, Writing—original draft. PB: Writing—review & editing. HR: Conceptualization, Writing—original draft, Writing—review & editing. RS: Writing—review & editing. HJ: Writing—review & editing. AA: Writing—review & editing. AL: Conceptualization, Supervision, Writing—original draft, Writing—review & editing.
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This study was funded by the Foundation for Disease Elimination and Control (FDEC) of India.
Conflict of interest
AL was employed by Sun Pharmaceutical Industries Ltd.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. ^ 27 high-burden districts - Lawngtlai, Lunglei, Mamit and Saiha (Mizoram); Dhalai, Gomati, Khowai, North Tripura, South Tripura (Tripura); South Garo Hills (Meghalaya); Gadchiroli (Maharashtra); Kolkata (West Bengal); Kalahandi, Kandhamal, Korapur, Malkangiri, Rayadgada (Odisha); Bastar, Bijapur, Dantewada Kanker, Kondagaon Narayanpur, Sukma (Chattisgarh); Khunti, West Singhbhum (Jharkhand); Nicobars (Andman and Nicobar).
1. WHO World Malaria Report . (2023). Available online at: https://www.who.int/teams/global-malaria-programme/reports/world-malaria-report-2023~ (accessed January 22, 2024).
Google Scholar
2. WHO World Malaria Report. Geneva: WHO (2022). p. 293.
3. NVBDCP Malaria Situation in India . (2023). Available online at: https://nvbdcp.gov.in/index4.php?lang=1andlevel=0andlinkid=564andlid=3867 (accessed June 20, 2023).
4. NVBDCP National Framework for Elimination of Malaria in India 2016-30 . (2016). Available online at: http://nvbdcp.gov.in/Doc/National-framework-for-malaria-elimination-in-India-2016%E2%80%932030.pdf (accessed January 22, 2024).
5. Sharma RK, Thakor HG, Saha KB, Sonal GS, Dhariwal AC, Singh N. Malaria situation in India with special reference to tribal areas. Indian J Med Res. (2015) 141:537–45. doi: 10.4103/0971-5916.159510
PubMed Abstract | Crossref Full Text | Google Scholar
6. Rajvanshi H, Bharti PK, Nisar S, Jain Y, Jayswar H, Mishra AK, et al. Study design and operational framework for a community-based Malaria Elimination Demonstration Project (MEDP) in 1233 villages of district Mandla, Madhya Pradesh. Malar J. (2020) 19:1–12. doi: 10.1186/s12936-020-03458-4
7. Rajvanshi H, Saha KB, Shukla MM, Nisar S, Jayswar H, Mishra AK, et al. Assessment of ASHA for knowledge, diagnosis and treatment on malaria in Mandla district of Madhya Pradesh as part of the malaria elimination demonstration project. Malar J. (2021) 20:1–8. doi: 10.1186/s12936-021-03610-8
8. Rajvanshi H, Nisar S, Bharti PK, Jayswar H, Mishra AK, Sharma RK, et al. Significance of training, monitoring and assessment of malaria workers in achieving malaria elimination goal of Malaria Elimination Demonstration Project. Malar J. (2021) 20:1–12. doi: 10.1186/s12936-020-03534-9
9. Singh MP, Rajvanshi H, Nisar S, Singh A, Jayswar H, Singh S, et al. A comparative assessment of the community frontline health workers for their knowledge and practices of malaria diagnosis and treatment in three contiguous districts Mandla, Balaghat, and Dindori of Madhya Pradesh, India. Malar J. (2023) 22:62. doi: 10.1186/s12936-023-04492-8
10. Bharti PK, Rajvanshi H, Nisar S, Jayswar H, Saha KB, Shukla MM, et al. Demonstration of indigenous malaria elimination through Track-Test-Treat-Track (T4) strategy in a malaria elimination demonstration project in Mandla, Madhya Pradesh. Malar J. (2020) 19:1–12. doi: 10.1186/s12936-020-03402-6
11. Singh MP, Rajvanshi H, Bharti PK, Jayswar H, Singh S, Mehra RK, et al. Evaluation of the model malaria elimination strategy in Mandla district along with its neighbouring districts: a time series analysis from 2008 to 2020. Malar J. (2023) 22:45. doi: 10.1186/s12936-023-04477-7
12. Singh A, Rajvanshi H, Singh MP, Bhandari S, Nisar S, Poriya R, et al. Mass screening and treatment (MSaT) for identifying and treating asymptomatic cases of malaria-malaria elimination demonstration project (MEDP), Mandla, Madhya Pradesh. Malar J. (2022) 21:395. doi: 10.1186/s12936-022-04423-z
13. Pradhan S, Pradhan MM, Dutta A, Shah NK, Joshi PL, Pradhan K, et al. Improved access to early diagnosis and complete treatment of malaria in Odisha, India. PLoS ONE. (2019) 14:e0208943. doi: 10.1371/journal.pone.0208943
14. Rajvanshi H, Singh MP, Bharti PK, Sahu RS, Anvikar A. Science of malaria elimination: using knowledge of bottlenecks and enablers from the Malaria Elimination Demonstration Project in Central India for eliminating malaria in the Asia Pacific region. Front Public Health. (2024) 11:1303095. doi: 10.3389/fpubh.2023.1303095
15. Mishra AK, Bharti PK, Vishwakarma A, Nisar S, Rajvanshi H, Sharma RK, et al. A study of malaria vector surveillance as part of the Malaria Elimination Demonstration Project in Mandla, Madhya Pradesh. Malar J. (2020) 19:1–13. doi: 10.1186/s12936-020-03517-w
16. Rajvanshi H, Mishra K, Bharti PK, Sandhibigraha D, Nisar S, Jayswar H, et al. Learnings from two independent malaria elimination demonstration projects in India. Trans R Soc Trop Med Hyg. (2021) 115:1229–33. doi: 10.1093/trstmh/trab148
17. Mishra AK, Nisar S, Rajvanshi H, Bharti PK, Saha KB, Shukla MM, et al. Improvement of Indoor Residual Spraying and Long-Lasting Insecticidal Net services through structured monitoring and supervision as part of the Malaria Elimination Demonstration Project in Mandla, Madhya Pradesh. Malar J. (2021) 20:1–12. doi: 10.1186/s12936-021-03639-9
18. Rajvanshi H, Bharti PK, Nisar S, Jayswar H, Mishra AK, Sharma RK, et al. A model for malaria elimination based on learnings from the Malaria Elimination Demonstration Project, Mandla district, Madhya Pradesh. Malar J. (2021) 20:1–15. doi: 10.1186/s12936-021-03607-3
19. Singh A, Singh MP, Bhandari S, Rajvanshi H, Nisar S, Telasey V, et al. Significance of nested PCR testing for the detection of low-density malaria infection amongst febrile patients from the Malaria Elimination Demonstration Project in Mandla, Madhya Pradesh, India. Malar J. (2022) 21:341. doi: 10.1186/s12936-022-04355-8
Keywords: malaria elimination, MEDP, monitoring and accountability frameworks, robust surveillance, situation analysis, tribal malaria
Citation: Singh MP, Bharti PK, Rajvanshi H, Sahu RS, Jayswar H, Anvikar AR and Lal AA (2024) Malaria elimination: situation analysis of cases in India, the state of Madhya Pradesh in central India, and district Mandla of Madhya Pradesh. Front. Public Health 12:1363736. doi: 10.3389/fpubh.2024.1363736
Received: 31 December 2023; Accepted: 11 March 2024; Published: 09 April 2024.
Reviewed by:
Copyright © 2024 Singh, Bharti, Rajvanshi, Sahu, Jayswar, Anvikar and Lal. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY) . The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Altaf A. Lal, altaf.lal@gmail.com ; altaf.lal@sunpharma.com
† Present address: Harsh Rajvanshi, Asia Pacific Leaders Malaria Alliance (APLMA), Singapore, Singapore
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Cookies on GOV.UK
We use some essential cookies to make this website work.
We’d like to set additional cookies to understand how you use GOV.UK, remember your settings and improve government services.
We also use cookies set by other sites to help us deliver content from their services.
You have accepted additional cookies. You can change your cookie settings at any time.
You have rejected additional cookies. You can change your cookie settings at any time.
- International
- International aid and development
- Health in developing countries
Battling malaria in India
How a DFID supported health programme in rural India is helping to raise awareness of malaria prevention and treatment among vulnerable tribal communities

A health worker runs a malaria diagnosis test on an elderly woman. Picture: DFID
Update: This case study was updated in November 2012
Milu Jani lives in Labangi, a small village in a remote area of Western Odisha - one of the poorest states in India. The village is around 3 hours from the nearest district town of Angul and part of the journey needs to be done on foot. There is no health centre, no electricity and no school in the village. Milu works as a forest guard at the Satakosia wildlife reserve, earning a mere 90 rupees (£1.20) a day.
Like most villagers, Milu has lost a loved one to malaria. His eyes tear up as he recalls his father’s death last winter. Milu’s father fell ill with a high fever and was tragically diagnosed with malaria only a day before his death, leaving no time for proper treatment. Malaria can be treated effectively with drugs, but treatment is most effective when administered within 24 hours of the onset of fever. Odisha accounts for a quarter of India’s malaria cases amd 16% of its malaria deaths.
Milu knew mosquito bites can cause malaria but didn’t know the deadly mosquitos were breeding in the water pools around the village. After his father passed away, Milu met a local health worker who explained the risks of malaria and how to prevent his family from becoming ill with this deadly disease.
Getting healthcare to rural communities
The DFID supported state health programme in Odisha trains health workers to help raise awareness of malaria prevention and treatment among vulnerable tribal communities like Milu’s. Health workers like Suhasini Behera in Milu’s village are trained in the use of diagnostic tests and how to administer appropriate medicines. They also distribute bednets and promote the proper use of nets to prevent malaria.
“It was not easy to convince people to use bed nets,” Suhasini says. “People feared the nets were poisonous as there had been reports of rashes and itching from the insecticide” - misconceptions that she sought to dispel while visiting their homes.
By working with the community to raise awareness of malaria, Suhasini and her fellow health workers help to prevent people from contracting malaria and help the villagers to understand how to access treatment.
Bednets - a simple prevention tool
DFID’s support to the Odisha state health programme has helped Milu and his family purchase bednets that will prevent them from contracting malaria in the future. By subsidising the cost of the nets, DFID enabled poor families like Milu’s to purchase two bednets for only 20 rupees (25p). The nets are treated with insecticide and last up to five years.

Milu Jani and his family under their new bednet.
Milu’s mother is content with her new net. “I always had disturbed sleep due to the mosquitoes. This new net has brought me a lot of comfort and I also use it for my afternoon nap”.
Milu is equally satisfied. “Malaria was a huge problem in our area. Now everyone in the village is using a net. I have lost my father but now I can keep my family safe from malaria”.
The DFID supported Odisha state health programme distributed 4.3 million bed nets to villages between 2009 and 2012, integrated with education and awareness activities of health workers. The programme has trained nearly 39,000 health workers to use diagnostic tests, give medicines and distribute bed nets.
DFID support has helped provide an extra 240,000 bed nets to young expectant mothers and tribal children to prevent anaemia and malaria-related deaths between 2010 and 2012. The fact that most women sleep with their newborn under the treated bednet has helped reduce deaths in children due to Malaria. DFID’s technical support has also helped the state government establish evidence required for assessing and up-scaling malaria initiatives.
Odisha has recorded a 24% decline in malaria cases and 60% decline in reported deaths in 2011 compared to 2010. The total number of reported malaria deaths declined from 247 to 100 between 2010 and 2011.
Related content
Is this page useful.
- Yes this page is useful
- No this page is not useful
Help us improve GOV.UK
Don’t include personal or financial information like your National Insurance number or credit card details.
To help us improve GOV.UK, we’d like to know more about your visit today. We’ll send you a link to a feedback form. It will take only 2 minutes to fill in. Don’t worry we won’t send you spam or share your email address with anyone.
We have updated our terms and conditions and privacy policy Click "Continue" to accept and continue with ET HealthWorld
We use cookies to ensure best experience for you
We use cookies and other tracking technologies to improve your browsing experience on our site, show personalize content and targeted ads, analyze site traffic, and understand where our audience is coming from. You can also read our privacy policy , We use cookies to ensure the best experience for you on our website.
By choosing I accept, or by continuing being on the website, you consent to our use of Cookies and Terms & Conditions .
- Leaders Speak
- Brand Solutions
- Malaria elimination from the tribes of India: The final frontier
More than 90% of India’s 161,516 reported malaria cases in 2021 were concentrated in just 8 states, all of which have significant tribal populations. The tribal districts that report malaria represent only 8.6% of the country’s population but account for 50% of total malaria cases and 30% of all malaria deaths.
- ETHealthWorld
- Updated On Aug 19, 2022 at 08:54 AM IST

- Published On Aug 19, 2022 at 08:54 AM IST
All Comments
By commenting, you agree to the Prohibited Content Policy
Find this Comment Offensive?
- Foul Language
- Inciting hatred against a certain community
- Out of Context / Spam
Join the community of 2M+ industry professionals
Subscribe to our newsletter to get latest insights & analysis., download ethealthworld app.
- Get Realtime updates
- Save your favourite articles
- swati piramal
- sarthak das
- tribal health collaborative
- ministry of home affairs
- Malaria elimination
- World Mosquito. Day
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- My Account Login
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Open access
- Published: 02 May 2024
Active self-treatment of a facial wound with a biologically active plant by a male Sumatran orangutan
- Isabelle B. Laumer 1 ,
- Arif Rahman 2 ,
- Tri Rahmaeti 2 ,
- Ulil Azhari 3 ,
- Hermansyah 4 ,
- Sri Suci Utami Atmoko 5 &
- Caroline Schuppli 1
Scientific Reports volume 14 , Article number: 8932 ( 2024 ) Cite this article
66k Accesses
6014 Altmetric
Metrics details
Although self-medication in non-human animals is often difficult to document systematically due to the difficulty of predicting its occurrence, there is widespread evidence of such behaviors as whole leaf swallowing, bitter pith chewing, and fur rubbing in African great apes, orangutans, white handed gibbons, and several other species of monkeys in Africa, Central and South America and Madagascar. To the best of our knowledge, there is only one report of active wound treatment in non-human animals, namely in chimpanzees. We observed a male Sumatran orangutan ( Pongo abelii ) who sustained a facial wound. Three days after the injury he selectively ripped off leaves of a liana with the common name Akar Kuning ( Fibraurea tinctoria ), chewed on them, and then repeatedly applied the resulting juice onto the facial wound. As a last step, he fully covered the wound with the chewed leaves. Found in tropical forests of Southeast Asia, this and related liana species are known for their analgesic, antipyretic, and diuretic effects and are used in traditional medicine to treat various diseases, such as dysentery, diabetes, and malaria. Previous analyses of plant chemical compounds show the presence of furanoditerpenoids and protoberberine alkaloids, which are known to have antibacterial, anti-inflammatory, anti-fungal, antioxidant, and other biological activities of relevance to wound healing. This possibly innovative behavior presents the first systematically documented case of active wound treatment with a plant species know to contain biologically active substances by a wild animal and provides new insights into the origins of human wound care.
Similar content being viewed by others

Microdosing with psilocybin mushrooms: a double-blind placebo-controlled study

Adults who microdose psychedelics report health related motivations and lower levels of anxiety and depression compared to non-microdosers

Nicotine pouches: a review for the dental team
Introduction.
In the early 1960s Jane Goodall first described the presence of whole leaves in the feces of chimpanzees ( Pan troglodytes ) at Gombe Stream, Tanzania 1 . By the late 1990s, this behavior, now called whole leaf swallowing, was documented at several African great ape study sites, along with bitter pith chewing, and demonstrated to have therapeutic, anti-parasitic functions 2 . Since then, various forms of self-medication have been observed in wild great apes (e.g., 2 , 3 , 4 , 5 , 6 ). Some of the most detailed evidence for animal self-medication comes from research in primates (e.g., 1 , 2 , 3 , 4 , 5 , 6 , 7 , 8 , 9 , 10 , 11 , 12 ).
Animal self-medication is now divided into five categories 2 , 4 : (1) sick behaviors, such as anorexia; (2) avoidance behaviors, such as avoiding e.g. feces, contaminated food or water; (3) prophylactic behaviors, such as routine consumption of foods with preventive or health maintenance effects; (4) therapeutic behaviors, defined by the ingestion of a small amount of a biologically active or toxic substance with no or little nutritional value for the curative treatment of a disease or its symptoms, and; (5) therapeutic topical application of pharmacologically active plants onto the body for the treatment of external health conditions or placement of such species in the nest as a fumigant or insect repellent 13 . Several of these behaviors can be found in wild apes 2 .
While sick and avoidance behavior (category 1 and 2) can be regularly observed in non-human animals (e.g. 14 ), self-medication in the form of ingestion of specific plant parts (prophylactic and therapeutic behavior, category 3 and 4) is widespread, albeit exhibited at low frequencies (e.g., 15 , but see 16 ). So far, leaf swallowing has been reported in chimpanzees ( Pan sp. ; e.g., 7 , 9 , 16 , 17 ), bonobos ( Pan paniscus 3 ), gorillas (e.g. Gorilla beringei graueri 18 ), and in only one Asian ape species, the white-handed gibbon ( Hylobates lar ) 19 . Another study reported the consumption of plant species directly related to the occurrence of parasite infections in individual orangutans ( Pongo sp. ), but not correlated with the plant’s distribution in the environment 20 . Another therapeutic self-medicative behavior seen in chimpanzees is bitter pith chewing of Vernonia amygdalina to treat worm infection 8 , 10 , 13 . Despite the plant’s year-round availability, the behavior is highly seasonal, peaking during the rainy season when worm infections also peak 8 , 13 . Interestingly, as Vernonia amygdalina is not evenly distributed in their home range, the apes often need to actively adapt their usual travel routes to gain access to the plant 13 .
Among Bornean orangutans ( Pongo pygmaeus ) there are several reports proposing the intentional ingestion of specific plant species also used in ethnomedicine for their medicinally active properties. In Sabah, Malaysia, a 4- to 5-year-old severely wounded female Bornean orangutan was observed eating ginger leaves and stem (Zingiberaceae) 21 . Ginger is known as a traditional medical plant against inflammation with antibacterial, antiviral, antifungal properties 22 , 23 , 24 , 25 . In 7 years of observation, no other individual, except two flanged males was ever observed feeding on the same ginger species at that study site. The researchers concluded that the juvenile may have attempted to treat itself with these plants. Another study, which interviewed 13 traditional healers from Central Kalimantan, showed that Bornean orangutans feed on the same plant parts from two plant species ( Uncaria gambir Roxb and Pternandra galeata Ridl ), used by traditional healers for treating internal illness, tumors, and haemorrhage 26 . Additionally, they observed a female Bornean orangutan selectively choosing young leaves of Mezzetia sp. , the pulp of Dyera lowii and Ilex cymosa , and leaves of Belang Handipek ( Scolopia macrophylla) 27 . This plant combination is used in ethnomedicine as a prevention against fatigue 27 . Despite these reports, overall, evidence of plant consumption for self-medication in orangutans is still limited.
Reports of the topical application of plants or insects to one’s own body (category 5) are found in a limited number of taxa, but the evidence for medicinal benefits remain mostly anecdotal (e.g. 28 , 29 , 30 , 31 , 32 , 33 , 34 , 35 , 36 , 37 , 38 ). However, there is growing evidence for the application of biologically active plant compounds to the skin in orangutans. At Sabangau peat swamp forest in Central Kalimantan, two adult female and one adolescent female Bornean orangutans were observed chewing leaves of Dracaena cantleyi for three to five minutes and then rubbing the resulting green-white lather onto their arms and legs for up to 35 min 11 . Ten years later, a follow-up study confirmed the same behavior in six additional adult females and one flanged male of the same population (the lather was similarly applied and massaged into the skin for up to 45 min 6 ). The behavior appeared to be intentional as only specific body parts were treated, the behavior was repeated several times until the hair was fully wet and the entire process took a considerable amount of time 6 , 11 . Orangutans were never observed ingesting the leaves 6 . Dracaena cantleyi is a medicinal plant used by indigenous people for several medical treatments including sore muscles, joint or bone pain 6 , pain after a stroke 6 and swelling 11 . Indeed, pharmacological analyses revealed that Dracaena cantleyi inhibits TNFα-induced inflammatory cytokine production thereby acting as an anti-inflammatory agent 6 .
There are some brief anecdotal mentions of chimpanzees using leaves (plant species unknown) to wipe blood from their wounds 39 , 40 . Active wound treatment with a substance has only recently been documented for the first time in a great ape species. Chimpanzees of the Rekambo community ( Pan troglodytes troglodytes ) in the Loango National Park, Gabon, were observed applying insects to their own wounds (n = 19) and to the wounds of conspecifics (n = 3) 5 . The five adult males, one adult female, and one juvenile female applied the insects in the same sequence: they caught a dark-colored, winged insect approximately 5 mm in size (unidentified at the time of publication), immobilized it by squeezing it between the lips, then applied the insect to the wound moving it with their mouth or finger, then removed it. The last two steps were usually repeated several times. Further research is needed to investigate the efficiency of this behavior. Active wound treatment has also been described in a captive capuchin monkey, that was observed grooming her vaginal area and four of her own wounds with a sugar-coated tool 41 . However, as the authors noted that the capuchin was used to having her wounds treated with an antibacterial salve topically applied by caregivers.
We here report for the first time active wound treatment with a known biologically active plant substance by a male Sumatran orangutan in the wild, and discuss the hypothesis that this may be a form of self-medication to treat a wound and possibly prevent infection and accelerate wound healing.
The observations took place in the Suaq Balimbing research area (N 3° 02.873′, E97° 25.013′), a part of the Gunung Leuser National Park in South Aceh, Indonesia. The research area is approximately 350 ha and consists mainly of peat swamp forest. Since 1994, the wild Sumatran orangutans ( Pongo abelii ) at Suaq have been the subjects of non-invasive, almost exclusively observational research.

Subject information
A male Sumatran orangutan named Rakus was first observed in March 2009. At that time, Rakus was an unflanged male (i.e., adult but without secondary sexual characteristics 42 ) and was estimated to be born in the late 1980s. He is either a resident to the area or a frequent visitor 43 , 44 , 45 . Rakus went through a secondary growth spurt in 2021 and has been a fully flanged male since August 2021.
Data collection procedure
Data on orangutans at Suaq Balimbing are collected using all-day focal follows. Data collection starts when an individual is found or when they leave their night nest in the morning until they build a new night nest in the evening. Data is collected at two-minute intervals following standardized protocols for orangutan behavioural observations. Furthermore, all rare behaviors are described in detail on an all-occurrence basis in the notes section of the data sheets.
Rakus was a focal individual from June 22 (on the day this fresh wound was first noted) to June 26, from June 28 to 30, on July 5, July 19, and August 5, 2022. The wound treatment data was collected on June 25, 2022, and described in detail in the notes section of the data sheets. Unfortunately, no photos or videos were taken of the wound treatment.
We took detailed pictures of the plant specimen that was used by the orangutan to ensure reliable identification (see Fig. 2 ). However, due to a lack of the necessary permits, we were unable to collect and store a physical sample of the specimen. The pictures of the specimen were compared to the site’s detailed picture-based herbarium which was established at the beginning of the research activities at Suaq Balimbing via samples collected at the site in partnership with the National Herbarium of Indonesia and the National University of Indonesia (UNAS).
Ethical guidelines
The data collection in wild orangutans was strictly observational and collected without any interaction with the study animals. The research protocols were approved by the Ministry of research and technology (RISTEK; research permit no. 152/SIP/FRP/SM/V/2012 and following) and complied with the legal requirements of Indonesia.
On June 22, 2022, our research team (including UA) first noticed that Rakus had a fresh wound on his right flange (see Fig. 1 , see movie S1 ) and inside his mouth, first visible when he emitted a long call; see movie S2 ). How he got the wound is unknown, however typically flanged males acquire these kinds of wounds during fights with other flanged males. Vocal evidence of a fight between orangutan males was reported earlier on the same day of this observation.

Process of wound healing. Rakus fed on and later applied the masticated leaves of Fibraurea tinctoria to his facial wound on June 25. On June 26 he was again observed feeding on Fibraurea tinctoria leaves (see photo). By June 30 the wound was closed and by August 25 was barely visible anymore.
On June 25 at 11:16, Rakus started feeding on the stem and the leaves of the liana of Fibraurea tinctoria (see Fig. 2 ), also known as ‘Akar Kuning’ (for other synonyms and classification of the plant, please see SI, Table S1 ), which is part of the orangutans’ diet in this area. The liana is rarely eaten (0.3% of all feeding scans, n = 390′000), but 47 out of a total of the 132 orangutans on which we have collected feeding data were observed consuming its leaves, fruits, or parts of the stem. Thirteen minutes after Rakus had started feeding on the liana, he began chewing the leaves without swallowing them and using his fingers to apply the plant juice from his mouth directly onto his facial wound. This behavior was repeated several times and lasted seven minutes. After this period, at 11:36, flies of an unknown species appeared on the wound. Rakus then smeared the entire wound with the plant pulp until the red flesh was fully covered with the green leaf material. He then continued feeding on this plant for a total of 34 min. The next day (June 26), but not on any other of the following observation days (June 28, 29, 30; July 5, 19, 20), he ate leaves of Fibraurea tinctoria again for two minutes (pictures (Figs. 1 and 2 ) and one video (see movie S1 ) were taken on June 26th while he was feeding on Fibraurea tinctoria ).

Left: Pictures of Fibraurea tinctoria leaves. The length of the leaves is between 15 to 17 cm. Right: Rakus feeding on Fibraurea tinctoria leaves (photo taken on June 26, the day after applying the plant mesh to the wound).
Observations over the following days did not show any signs of the wound becoming infected (see photos taken on June 26 and 28; Fig. 1 ) and by June 30 the facial wound was already closed (see Fig. 1 and movie S1 ). By July 19, 2022, the wound appeared to have fully healed and only a faint scar remained (see Fig. 1 ).
Furthermore, UA (who collected the focal data) noted that Rakus rested more than usual after being wounded, which may positively affect wound healing as growth hormone release, protein synthesis and cell division are increased during sleep 46 , 47 . When considering the percentage of time spent resting (based on 2-min interval activity scans) between January 30, 2021 (since then he has been considered a flanged male; this is important to consider, as flanged males in general rest more than unflanged males 12 , 48 ) to February 22, 2023, we noticed that resting time increased after being wounded (June 22, 2022, to July 20, 2022; mean = 33 ± 17.2%) compared to the time before (January 30, 2021, to November 8, 2021; mean = 14.8 ± 7.4%) and that resting time decreased again after the wound had closed (August 5, 2022, to February 22, 2023; mean = 23.6 ± 12.9%; see SI, Figure S1 ). He spent more than 50% the day resting after he was found with the fresh wound (June 23, 2022; 52.2% of resting), the day after wound treatment (June 26, 2023; 51%), and four days after treatment (June 29, 2023; 54.3%; see SI, Fig. S1 ).
To the best of our knowledge, this study is the first systematic documentation of the putative active wound treatment with a biologically active plant substance in great apes and other non-human species. In this study, the flanged male orangutan Rakus was observed to selectively detach, chew, and repeatedly apply the chewed leave juice directly on his three-day-old facial wound for several minutes and covered the entire wound with a chewed-up leaf mash. Additionally, Rakus rested more when the wound was fresh compared to before and after wounding.
The treatment of human wounds was most likely first mentioned in a medical manuscript that dates back to 2200 BC, which included cleaning, making plasters and bandaging of wounds 49 . One of the earliest known wound care products used by the Sumerians, Greek, Mayans and Egyptians were oil, herbs, maggots, beer, vinegar, wine, green paint containing copper and honey 49 , 50 .
Fibraurea tinctoria , has other generic names such as Akar Kuning (Central Kalimantan), Akar Palo (Aceh), and Yellow Root (East Kalimantan 51 ). It is an evergreen, climbing plant in the family Menispermaceae, with a broad distribution across Mainland China, Indonesia, Malaysia, Thailand, Vietnam and other areas of Southeast Asia 52 , 53 , and is known for its analgesic, antipyretic, antidote, and diuretic effects, and is used in traditional medicine to treat condition such as dysentery, diabetes, and malaria 51 , 54 , 55 . All plant parts have been reported to be used for these medical applications, including leaves, stems, roots and bark 54 .
Pharmacological analysis of the plant’s chemical compounds shows the presence of furanoditerpenoids 56 , a special group of diterpenoids composed of one or more aromatic furan rings (with four carbon atoms and one oxygen), which are reported to have antibacterial, anti-inflammatory, anti-fungal, antioxidant, and anticarcinogenic biological activities 55 , 56 . Fibraurea tinctoria also has a high concentration of protoberberine alkaloids, which have anti-inflammatory, analgesic, anticonvulsant, antiamnesic, narcotic, antiarrhythmic, antihemorrhagic, hypotensive, antioxidant, antitumoral, antidiuretic, antiulcer, and muscle relaxant properties 57 . It also contains jatrorrhizine (antidiabetic, antimicrobial, antiprotozoal, anticancer, and hypolipidemic properties; reviewed in 58 ) and palmatine (anticancer, antioxidation, anti-inflammatory, antibacterial, antiviral properties; reviewed in 59 , 60 ). Among 38 plants used in ethnomedicine and grown in South Vietnam, Fibraurea tinctoria showed the highest activity tested for antimalarial effects 61 . It has also been shown that the leaves and stems of Fibraurea tinctoria inhibit the growth of several bacteria species, including Bacillus cereus , Staphylococcus aureus, and Escherichia coli 53 , 62 . Fibraurea tinctoria also showed a significant anti-inflammatory effect in reducing mouse paw edema 55 .
Like all self-medication behavior in non-human animals, the case reported in this study raises questions about how intentional these behaviors are and how they emerge. Similar to plant ointment behavior in Bornean orangutans 6 , 11 , the behavior of the Sumatran flanged male orangutan reported here appeared to be intentional as (I) he selectively treated his facial wound on his right flange with the plant juice (and no other body parts), (II) the behavior was repeated several times, not only plant juice but later also more solid plant material was applied until the wound was fully covered and (III) the entire process took a considerable amount of time. It is possible, that wound treatment with Fibraurea tinctoria emerges through accidental individual innovation 63 . Individuals may accidentally touch their wounds while feeding on Fibraurea tinctoria and thus unintentionally apply the plant’s juice to their wounds. As Fibraurea tinctoria has potent analgesic effects, individuals may feel an immediate pain release, causing them to repeat the behavior several times and subsequently apply solid plant matter possibly to also cover the wound as a protection against flies (as the case reported here suggests). Immature orangutans rely on observational social learning for the acquisition of their skill repertoires 64 and recent evidence suggests that social learning continues into adulthood 65 . Therefore, given that it occurs frequent enough and in social contexts, wound treatment with Fibraurea tinctoria may also spread socially from individual to individual.
However, up to date, in 21 years and 28′000 observation hours, we never observed any other orangutans at Suaq using Fibraurea tinctoria to treat their wounds. On the one hand, this may be due to the fact that we rarely encounter injured orangutans at Suaq. Due to high food availability, high social tolerance between orangutans and relatively stable social hierarchies (each area is usually inhabited by a dominant male and several females 66 ), there are few physical fights. However, during the time of this study, there was no clearly dominant male present in the research area. Rakus had just gone through his secondary sexual development in the year before the incident and, as a newly flanged male, he seemed to try to establish himself as the new dominant local male which is reflected in our behavioral data collected during this time. As a result of that, Rakus was involved in several long-call battles 66 and physical altercations with other flanged males that were resident in and around the area at that time. On the other hand, it may be that wound treatment with Fibraurea tinctoria has so far been absent in the behavioral repertoire of the Suaq orangutan population. Like all adult males in the area, Rakus was not born in Suaq (his origin is unknown). Orangutan males disperse from their natal area during/after puberty over long distances to either establish a new home range in another area (mostly as dominant flanged male) or are moving between other’s home ranges (as unflanged males or flanged males) 67 . Therefore, any adult male in an area does not originate from the area 67 . Thus, as of now, it is impossible to find out where the males come from. Therefore, it is possible that the behavior is shown by more individuals in his natal population.
Of the few injured orangutans that we observed at Suaq so far, we observed one other instance of possible wound soothing/treatment behavior. Flanged male named Pluto repeatedly put his injured finger into the water of a pitcher plant. The water may have had a cooling effect that could eventually relieve pain or help clean the wound.
Taken together, chemical analyzes of the properties of the Fibraurea tinctoria and the orangutan's particular goal-oriented behavior are consistent with the hypothesis that the process of preparing and applying herbal ointments may be a form of self-medication that reduces pain, prevents inflammation, and accelerates wound healing. The present study may thus present the first report of active wound management with a biological active substance in a great ape species and provides new insights into the existence of self-medication in our closest relatives and in the evolutionary origins of wound medication more broadly. As forms of active wound treatment are not just a human universal but can also be found in both African and Asian great apes, it is possible that there exists a common underlying mechanism for the recognition and application of substances with medical or functional properties to wounds and that our last common ancestor already showed similar forms of ointment behavior.
Data availability
The data of this study consist of detailed pictures of the wounded orangutan and the specimen used by the orangutan to treat the wound. All data are provided in the manuscript.
Wrangham, R. W. & Goodall, J. Understanding Chimpanzees 22–37 (Harvard University Press, 1989).
Google Scholar
Huffman, M. in Mahale Chimpanzees—50 Years of Research Chimpanzee Self-Medication: A Historical Perspective of the Key Findings Vol. 50, 340–353 (Cambridge University Press, 2015).
Fruth, B. et al. New Evidence for Self-Medication in Bonobos: Manniophyton fulvum Leaf-and Stemstrip-Swallowing from LuiKotale, Salonga National Park, DR Congo. Am. J. Primatol. 76 , 146–158 (2014).
Article PubMed Google Scholar
Huffman, M. Encyclopedia of Animal Behavior Vol. 2, 696–702 (Elsevier, 2019).
Book Google Scholar
Mascaro, A., Southern, L. M., Deschner, T. & Pika, S. Application of insects to wounds of self and others by chimpanzees in the wild. Curr. Biol. 32 , R112–R113 (2022).
Article CAS PubMed Google Scholar
Morrogh-Bernard, H. et al. Self-medication by orang-utans ( Pongo pygmaeus ) using bioactive properties of Dracaena cantleyi. Sci. Rep. 7 , 16653 (2017).
Article ADS CAS PubMed PubMed Central Google Scholar
Huffman, M., Pebsworth, P., Bakuneeta, C., Gotoh, S. & Bardi, M. Macro-habitat comparison of host-parasite ecology in two populations of chimpanzees in the Budongo forest, Uganda and the Mahale Mountains, Tanzania. In Primate Parasite Ecology: The Dynamics of Host-Parasite Relationships . Cambridge University Press, Cambridge, 311–330 (2009).
Huffman, M. A., Gotoh, S., Izutsu, D., Koshimizu, K. & Kalunde, M. S. Further obervations on the use of the medicinal plant, Vernonia amygdalina (Del). By a wild chimpanzee, its possible effect on parasote load, and its phytochemistry. Afr. Study Monogr. 14 , 227–240 (1993).
Huffman, M. A., Gotoh, S., Turner, L. A., Hamai, M. & Yoshida, K. Seasonal trends in intestinal nematode infection and medicinal plant use among chimpanzees in the Mahale Mountains, Tanzania. Primates 38 , 111–125 (1997).
Article Google Scholar
Huffman, M. A. & Seifu, M. Observations on the illness and consumption of a possibly medicinal plant Vernonia amygdalina (Del), by a wild chimpanzee in the Mahale Mountains National Park, Tanzania. Primates 30 , 51–63 (1989).
Morrogh-Bernard, H. C. Fur-rubbing as a form of self-medication in Pongo pygmaeus. Int. J. Primatol. 29 , 1059–1064 (2008).
Morrogh-Bernard, H. C. et al. Orangutan activity budgets and diet. In Orangutans: Geographic Variation in Behavioral Ecology and Conservation , 119–133 (2009).
Huffman, M. A. Primate self-medication, passive prevention and active treatment-a brief review. Int. J. Multidiscip. Stud. https://doi.org/10.31357/ijms.v3i2.2794 (2016).
Case, T. I., Stevenson, R. J., Byrne, R. W. & Hobaiter, C. The animal origins of disgust: Reports of basic disgust in nonhuman great apes. Evol. Behav. Sci. 14 , 231 (2020).
Huffman, M. A. Current evidence for self-medication in primates: A multidisciplinary perspective. Am. J. Phys. Anthropol. Off. Publ. Am. Assoc. Phys. Anthropol. 104 , 171–200 (1997).
Mclennan, M. R. & Huffman, M. A. High frequency of leaf swallowing and its relationship to intestinal parasite expulsion in “Village” chimpanzees at Bulindi, Uganda. Am. J. Primatol. 74 , 642–650 (2012).
Fowler, A., Koutsioni, Y. & Sommer, V. Leaf-swallowing in Nigerian chimpanzees: Evidence for assumed self-medication. Primates 48 , 73–76 (2007).
Yamagiwa, J., Basabose, A. K., Kaleme, K. & Yumoto, T. Diet of Grauer’s gorillas in the montane forest of Kahuzi, Democratic Republic of Congo. Int. J. Primatol. 26 , 1345–1373 (2005).
Barelli, C. & Huffman, M. A. Leaf swallowing and parasite expulsion in Khao Yai white-handed gibbons ( Hylobates lar ), the first report in an Asian ape species. Am. J. Primatol. 79 , e22610 (2017).
Foitová, I., Jarkovský, J., Dušek, L. & Koptíková, J. Relationship between plant prevalence in the orangutan diet and their coincidence with parasite presence. In Report to Foundation UMI-Saving of Pongidae (2006).
Kanamori, T., Kuze, N., Bernard, H., Malim, T. P. & Kohshima, S. Fatality of a wild Bornean orangutan ( Pongo pygmaeus morio ): Behavior and death of a wounded juvenile in Danum Valley, North Borneo. Primates 53 , 221–226 (2012).
Jamaluddin, A. W. & Lestari, A. Effectiveness of Ginger Ointment ( Zingiber officinale roscoe ) on Incision Wound Healing in White Rats ( Rattus norvegicus ). Jurnal Riset Veteriner Indonesia (J. Indones. Veterinary Res.). https://doi.org/10.20956/jrvi.v5i1.13060 (2021).
Onyiba, C. I. A systematic review of garlic and ginger as medicinal spices against viral infections. Extensive Rev. 2 , 32–44 (2022).
Abdalla, W. E. & Abdallah, E. M. Antibacterial activity of ginger ( Zingiber Officinale Rosc.) rhizome: A mini review. Int. J. Pharmacogn. Chin. Med 2 , 000142 (2018).
Wang, H. & Ng, T. B. An antifungal protein from ginger rhizomes. Biochem. Biophys. Res. Commun. 336 , 100–104 (2005).
Panda, A. & Gunawan, Y. E. Linking zoopharmacognocy with ethnomedication, an evidence base from Sebangau National Park, Central Kalimantan Indonesia. J. Trop. Life Sci. 8 , 323–329 (2018).
Panda, A., Djohan, T., Artama, W. & Priyowidodo, D. in IOP Conference Series: Earth and Environmental Science. 012055 (IOP Publishing).
Clayton, D. H. & Wolfe, N. D. The adaptive significance of self-medication. Trends Ecol. Evol. 8 , 60–63 (1993).
Cimadom, A. et al. Darwin’s finches treat their feathers with a natural repellent. Sci. Rep. 6 , 34559 (2016).
Craig, A. Anting in Afrotropical birds: A review. Ostrich 70 , 203–207 (1999).
Nero, R. & Hatch, D. Common Grackles anting with marigold flowers. Blue Jay 42 (1984).
Potter, E. F. Anting in wild birds, its frequency and probable purpose. Auk 87 , 692–713 (1970).
Simmons, K. A review of the anting-behaviour of passerine birds. Br. Birds 50 , 401–424 (1957).
VanderWerf, E. A. ‘Elepaio “anting” with a garlic snail and a Schinus fruit. J. Field Ornithol. 76 , 134–137 (2005).
Weldon, P. J. et al. Anointing chemicals and hematophagous arthropods: Responses by ticks and mosquitoes to citrus (Rutaceae) peel exudates and monoterpene components. J. Chem. Ecol. 37 , 348–359 (2011).
Wenny, D. Three-striped Warbler ( Basileuterus tristriatus ) “anting" with a Caterpillar. In The Wilson Bulletin , 128–131 (1998).
Baker, M. Fur Rubbing: Use of Medicinal Plants by Capuchin Monkeys (Cebus capucinus) (Wiley Online Library, 1996).
Martínez, J., Zenteno-Ruiz, F., Moya, L., Carvajal, P. & Wallace, R. Fur rubbing behaviour in free ranging Beni titi monkeys ( Plecturocebus modestus ) in Bolivia. Neotrop. Primates 25 , 44–48 (2019).
Van Lawick-Goodall, J. Advances in the Study of Behavior Vol. 3, 195–249 (Elsevier, 1971).
Köhler, W. The Mentality of Apes (JSTOR, 1925).
Westergaard, G. & Fragaszy, D. Self-treatment of wounds by a capuchin monkey ( Cebus apella ). Hum. Evol. 2 , 557–562 (1987).
Rodman, P. S. Orangutans, sexual dimorphism in a solitary species. In Primate Societies , 146–154 (1987).
Galdikas, B. M. Orangutan reproduction in the wild. In Reproductive biology of the great apes: Comparative and biomedical perspectives , 281–300 (1981).
Dunkel, L. P. et al. Variation in developmental arrest among male orangutans: A comparison between a Sumatran and a Bornean population. Front. Zool. 10 , 1–11 (2013).
Van Schaik, C. P. & Van Hooff, J. Toward an understanding of the orangutan’s social system. In Great ape societies , 3–15 (1996).
Sassin, J. et al. Human growth hormone release: Relation to slow-wave sleep and sleep-waking cycles. Science 165 , 513–515 (1969).
Article ADS CAS PubMed Google Scholar
Smith, T. J. et al. Impact of sleep restriction on local immune response and skin barrier restoration with and without “multinutrient” nutrition intervention. J. Appl. Physiol. 124 , 190–200 (2018).
Van Schaik, C. P., Van Noordwijk, M. A. & Vogel, E. R. Ecological sex differences in wild orangutans. In Orangutans: Geographic Variation in Behavioral Ecology and Conservation , 49–64 (2009).
Shah, J. B. The history of wound care. J. Am. Coll. Certif. Wound Spec. 3 , 65–66 (2011).
Hobson, D. W. et al. The first cut is the deepest: The history and development of safe treatments for wound healing and tissue repair. Int. J. Toxicol. 35 , 491–498 (2016).
Fikriah, I. & Sawitri, E. In vivo antimalarial effect of yellow root stem ( Fibraurea tinctoria Lour) on Plasmodium berghei . Syst. Rev. Pharmacy 11 , 380 (2020).
CAS Google Scholar
Wu, M., Su, C., Chang, L. & Lee, C. A pharmacognostical study of Chinese drug huang-teng. The roots and stems of Fibraurea tinctoria Lour. Yao xue xue bao = Acta pharmaceutica Sinica 9 , 233–241 (1962).
CAS PubMed Google Scholar
Chac, L. D., Hoi, Q. V. & Thinh, B. B. Chemical composition and antimicrobial activity of the Essential oil of Fibraurea tinctoria . Chem. Nat. Compd. 59 , 597–599 (2023).
Article CAS Google Scholar
Purwaningsih, I., Maksum, I. P., Sumiarsa, D. & Sriwidodo, S. A review of Fibraurea tinctoria and its component, berberine, as an antidiabetic and antioxidant. Molecules 28 , 1294 (2023).
Article CAS PubMed PubMed Central Google Scholar
Su, C.-R. et al. Anti-inflammatory activities of furanoditerpenoids and other constituents from Fibraurea tinctoria . Bioorg. Med. Chem. 16 , 9603–9609 (2008).
Bao, H., Zhang, Q., Ye, Y. & Lin, L. Naturally occurring furanoditerpenoids: Distribution, chemistry and their pharmacological activities. Phytochem. Rev. 16 , 235–270. https://doi.org/10.1007/s11101-016-9472-2 (2017).
Leitao da-Cunha, E. V., Fechine, I. M., Guedes, D. N., Barbosa-Filho, J. M. & Sobral da Silva, M. in The Alkaloids: Chemistry and Biology Vol. 62 (ed G. A. Cordell) 1–75 (Academic Press, 2005).
Zhong, F. et al. Jatrorrhizine: a review of sources, pharmacology, pharmacokinetics and toxicity. Front. Pharmacol. 12 , 783127 (2022).
Article PubMed PubMed Central Google Scholar
Long, J. et al. Palmatine: A review of its pharmacology, toxicity and pharmacokinetics. Biochimie 162 , 176–184 (2019).
Keawpradub, N., Dej-adisai, S. & Yuenyongsawad, S. Antioxidant and cytotoxic activities of Thai medicinal plants named Khaminkhruea: Arcangelisia flava , Coscinium blumeanum and Fibraurea tinctoria . Songklanakarin J. Sci. Technol 27 , 455–467 (2005).
Nguyen-Pouplin, J. et al. Antimalarial and cytotoxic activities of ethnopharmacologically selected medicinal plants from South Vietnam. J. Ethnopharmacol. 109 , 417–427 (2007).
Galappathie, S. et al. Comparative antimicrobial activity of South East Asian plants used in Bornean folkloric medicine. J. Herbal Med. 4 , 96–105 (2014).
van Schaik, C. P. et al. The reluctant innovator: Orangutans and the phylogeny of creativity. Philos. Trans. R. Soc. B Biol. Sci. 371 , 20150183 (2016).
Schuppli, C. et al. Observational social learning and socially induced practice of routine skills in immature wild orang-utans. Anim Behav. 119 , 87–98 (2016).
Mörchen, J. et al. Migrant orangutan males use social learning to adapt to new habitat after dispersal. Front. Ecol. Evol. https://doi.org/10.3389/fevo.2023.1158887 (2023).
Spillmann, B., Willems, E. P., van Noordwijk, M. A., Setia, T. M. & van Schaik, C. P. Confrontational assessment in the roving male promiscuity mating system of the Bornean orangutan . Behav. Ecol. Sociobiol. 71 , 1–11 (2017).
Nietlisbach, P. et al. Heavily male-biased long-distance dispersal of orang-utans (genus: Pongo), as revealed by Y-chromosomal and mitochondrial genetic markers. Mol. Ecol. 21 , 3173–3186 (2012).
Download references
Acknowledgements
The research at Suaq is funded by the Max Planck Institute of Animal Behavior, the University of Zurich, the SUAQ Foundation, Stiftung Mensch und Tier Freiburg im Breisgau, and by a Freigeist Grant of the Volkswagen Stiftung to CS. We acknowledge all students, volunteers and local field assistants involved in the collection of standard behavioural data at Suaq. We gratefully acknowledge the Indonesian State Ministry for Research and Technology Badan Riset dan Inovasi Nasional (BRIN), Departement Dalam Negri, the Sumatran Orangutan Conservation Program (SOCP), Yayasan Ekosistem Lestari (YEL), the local government in South Aceh, the Balai Besar Taman Nasional Gunung Leuser (TNGL) in Medan and Tapak Tuan, and the Director General Departemen Kehutanan (PHKA) for their permission and support to conduct this research. We also thank the Fakultas Biologi Universitas Nasional (UNAS) in Jakarta for their collaboration and support, in particular, Tatang Mitra Setia.
Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and affiliations.
Development and Evolution of Cognition Research Group, Max Planck Institute of Animal Behavior, Konstanz, Germany
Isabelle B. Laumer & Caroline Schuppli
Department of Biology, Graduate Program, Faculty of Biology and Agriculture, Universitas Nasional, Jakarta, 12520, Indonesia
Arif Rahman & Tri Rahmaeti
SUAQ Project, Medan, Indonesia
Ulil Azhari
Yayasan Ekosistem Lestari (YEL), Medan, Indonesia
Fakultas Biologi, Universitas Nasional, Jakarta, Indonesia
Sri Suci Utami Atmoko
You can also search for this author in PubMed Google Scholar
Contributions
IBL wrote the manuscript. UA collected the data and took photos and videos. AR helped obtaining detailed accounts of the observed behavior and commented on the manuscript. TR helped to obtain detailed accounts of the observed behavior, translated the focal follow protocol from Indonesian to English and commented on the manuscript. H and SSUA commented on the manuscript. CS reviewed and edited the manuscript text.
Corresponding author
Correspondence to Isabelle B. Laumer .
Ethics declarations
Competing interests.
The authors declare no competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Supplementary information 1..
Supplementary Video 1.
Supplementary Video 2.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Laumer, I.B., Rahman, A., Rahmaeti, T. et al. Active self-treatment of a facial wound with a biologically active plant by a male Sumatran orangutan. Sci Rep 14 , 8932 (2024). https://doi.org/10.1038/s41598-024-58988-7
Download citation
Received : 19 December 2023
Accepted : 05 April 2024
Published : 02 May 2024
DOI : https://doi.org/10.1038/s41598-024-58988-7
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Animal self-medication
- Therapeutic topical application
- Phytotherapy
- Ethnomedicine
By submitting a comment you agree to abide by our Terms and Community Guidelines . If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing: Anthropocene newsletter — what matters in anthropocene research, free to your inbox weekly.
- Perspective
- Open access
- Published: 06 May 2024
Leveraging malaria vaccines and mRNA technology to tackle the global inequity in pharmaceutical research and production towards disease elimination
- Floriano Amimo ORCID: orcid.org/0000-0003-1460-9522 1
Malaria Journal volume 23 , Article number: 136 ( 2024 ) Cite this article
1 Altmetric
Metrics details
Malaria vaccine introduction in endemic countries is a game-changing milestone in the fight against the disease. This article examines the inequity in the global pharmaceutical research, development, manufacturing, and trade landscape. The role of inequity in hindering progress towards malaria elimination is explored. The analysis finds that transformational changes are required to create an equity-enabling environment. Addressing the inequity is critical to maximizing the public health impact of vaccines and attaining sustainability. Avenues to catalyze progress by leveraging malaria vaccines and messenger ribonucleic acid (mRNA) technology are discussed.
The World Health Organization (WHO) recommends childhood malaria immunization with RTS,S/AS01 (RTS,S) and R21/Matrix-M (R21) in endemic countries [ 1 , 2 ]. These pre-erythrocytic virus-like particle vaccines are valuable assets in the fight against malaria with the potential to accelerate progress towards disease elimination, a longstanding global target that has, nevertheless, remained elusive for many African countries. Prior research has shown that 384.7 (uncertainty interval [UI]: 311.7–496.5) cases per 1000, 1.0 (UI: 0.7–1.6) resistant cases per 1000, and 1.1 (UI: 0.8–1.5) deaths per 1000 could be averted with the deployment of a vaccine efficacy of 40% for 10 years [ 3 ].
The introduction of vaccines in endemic countries, therefore, has the potential to revert recent unsatisfactory trends in key indicators, particularly in the context of the coronavirus disease 2019 (COVID-19) pandemic and antimicrobial resistance. Yet inequitable reliance on imported medicines by national malaria control programmes (NMCPs) in Africa may affect the supply, availability, and accessibility of the vaccines and reduce their potential public health impact on the continent.
This article examines the inequity in the global pharmaceutical landscape, from research to trade. It takes an in-depth look at the central but often neglected issues that hamper malaria elimination and eradication while delving into avenues to effectively tackle them. Drawing on current research, it first addresses inequity in essential medicines manufacturing and trade and subsequently examines hindrances to progress in research and development (R&D) in Africa. In each of these two domains, the analysis explores the factors underlying the chronic hurdles and the risks that the resulting inequity poses to the population health and sustainability of NMCPs on the continent. It moreover surveys the challenges facing the policy, strategic, regulatory, and implementation frameworks put in place to address the difficulties. Implications of the recent advances in mRNA-based therapeutics ushered in by the COVID-19 pandemic are explored.
Manufacturing and trade
Reliance on imported medicines has traditionally been a major weakness of malaria control efforts in Africa. About 96–95.4% and 75.7–74.5% of global malaria deaths in 2021–2022 occurred in the WHO African Region (AFR) and among children younger than 5 years (U5) in the region, respectively [ 7 , 12 , 13 ]. Yet the continent has to import medicines to protect itself against the disease. Only 5% and < 1% of the medicines and vaccines Africa consumes and 3% and 0.1–0.2% of the global supply are produced on the continent, respectively [ 9 , 10 , 14 ]. The reliance on imported drugs also affects artemisinin derivatives used for artemisinin-based combination therapy (ACT). These are currently strongly recommended by the WHO as the cornerstone for malaria case management based on high-certainty evidence—artemether-lumefantrine, artesunate-amodiaquine, artesunate-mefloquine, dihydroartemisinin-piperaquine, artesunate-sulfadoxine-pyrimethamine (SP) (ASP)—as well as artesunate-pyronaridine [ 4 ]. Most of these ACT medicines are produced outside the continent, mostly in India [ 5 ] (see Fig. 1 ). This inequitable reliance on imported essential medicines perpetuates the vulnerability of national anti-malarial efforts to disruptions and shocks of global supply chains and systems, as observed at the height of the COVID-19 pandemic. This creates important risks to population health and global health security, thus acting as a structural obstacle to malaria elimination and eradication.
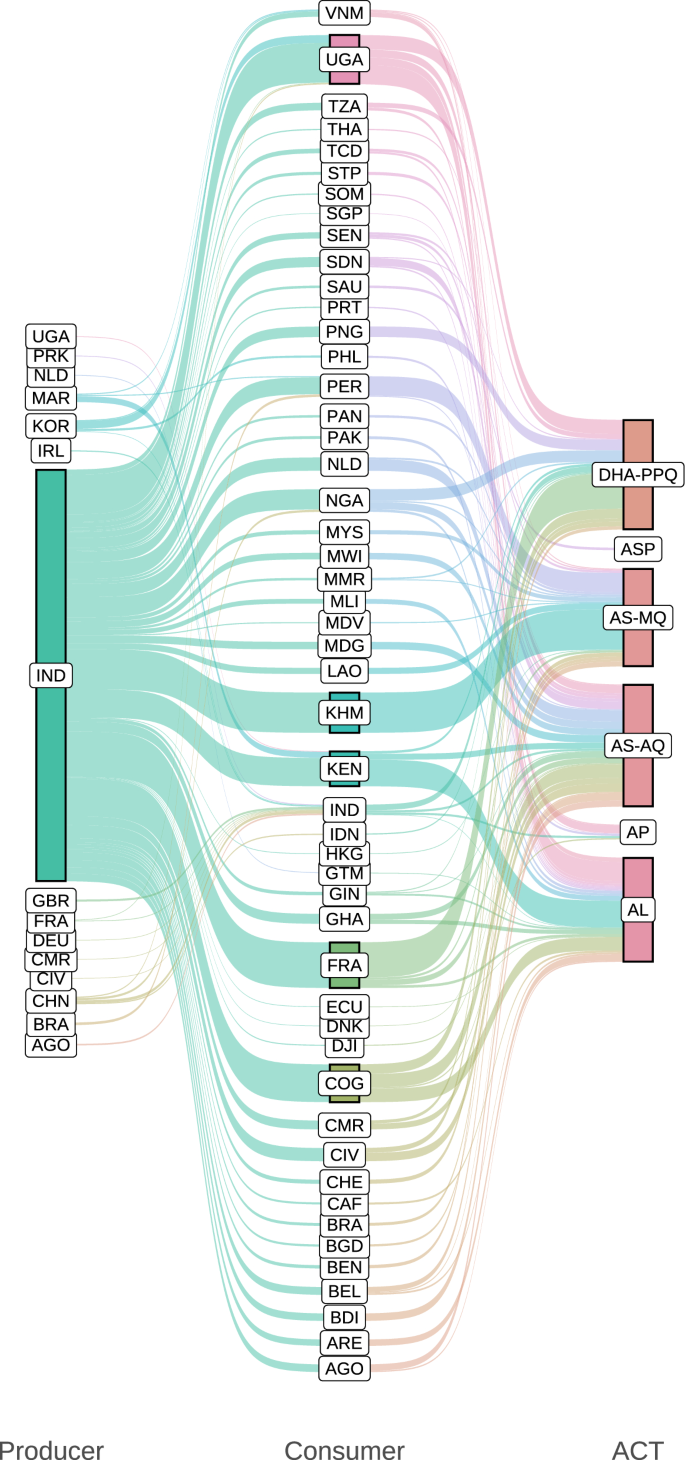
Most artemisinin-based combinations used in malaria-endemic African countries are produced outside the continent. The size of each leftmost and central node and each flow on the left and right side is proportional to the quantity of ACT medicines exported and imported by each producer and consumer country, respectively. The size of each rightmost node represents the quantity of each drug combination shipped. The colour of each left side and right side flow, as well as the leftmost and central nodes, represents each producer and consumer country, respectively. The colour of the rightmost nodes represents each drug combination. Producer and Consumer denote exporter and importer countries or territories represented by ISO 3166-1 alpha-3 codes, respectively. ACT medicines used for artemisinin-based combination therapy, AL artemether-lumefantrine, AP artesunate-pyronaridine, AS-AQ artesunate-amodiaquine, AS-MQ artesunate-mefloquine, ASP artesunate-SP, DHA-PPQ dihydroartemisinin-piperaquine. Data sources: [ 4 , 5 ]
Regional and global efforts to boost local pharmaceutical production (LPP) in Africa have yielded inconsequential results. This is despite the adoption of the Pharmaceutical Manufacturing Plan for Africa (PMPA, aimed at catalyzing LPP to improve public health outcomes) in 2007 and the endorsement of its Business Plan (BP, aimed at providing approaches to accelerate the implementation of the PMPA) in 2012 [ 15 , 16 , 17 ]. Global inequity in drug manufacturing is also being observed with the malaria vaccines. For instance, to date, there are 18 million doses of malaria vaccines available for priority allocation in selected African countries [ 18 ]. How many of these available vaccines were manufactured in an African country? Data shows that all doses of Mosquirix, the trade name of RTS,S, used in Kenya as of 16 September 2023 were imported from Belgium [ 5 ]. This is even though some African countries have some capacity to produce vaccines nationally (Fig. 2 ). This status quo implies that with the expected increase in the supply of malaria vaccines as the cost decreases over time might come further reliance of African countries on imported medical products (MPs).
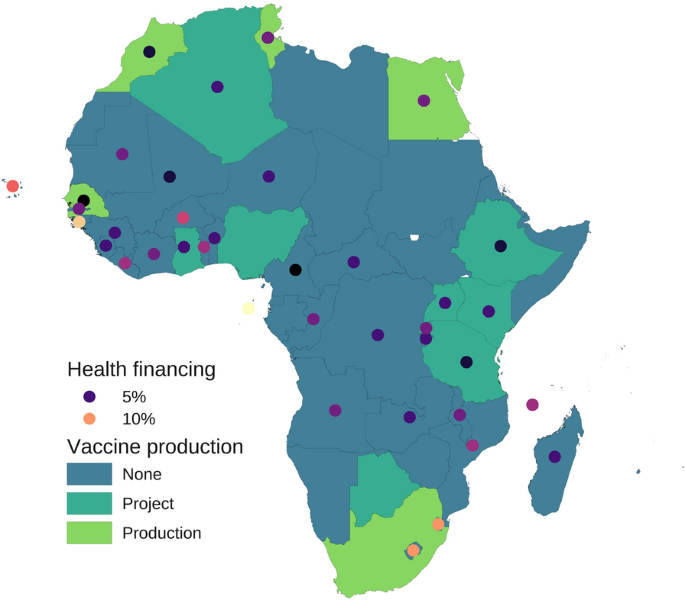
Geospatial distribution of vaccine production and health financing in Africa. Vaccine production categories shown with surface colour for each country are as follows: Production, countries with active vaccine manufacturing facilities and projects; Project, countries with vaccine manufacturing projects; None, countries without vaccine manufacturing facilities or projects. The colour of each dot is proportional to government health financing measured as the geometric mean of central government health spending as a share of general government expenditure in 2019–2021; the variation in colour intensity between or beyond the two values shown in the legend represents the corresponding variation in government health financing. Most countries do not comply with the Abuja Declaration of 2001 to allocate ≥ 15% of their annual budget to improve the health sector. Investment in vaccine manufacturing without compliance with the Abuja Declaration may result in an important diversion of government funds from the health sector, as suggested by the inverse association between the vaccine production status and government health financing observed in the current analysis (η 2 [H] = 0.17). Data sources: [ 6 , 7 , 8 , 9 , 10 , 11 ]
The COVID-19 pandemic has raised attention to the necessity to produce medicines locally or regionally and even catalyzed processes that could otherwise have taken longer to materialize. Modular mRNA production facilities have been developed by pharmaceutical companies to improve affordability and scale up accessibility of mRNA-based technologies for LPP in low- and middle-income countries (LMICs) [ 19 , 20 ]. The first such a facility (‘‘BioNTainer’’, a platform for mRNA production) was set up in Kigali, Rwanda, in 2023. Just as COVID-19 ushered in the era of mRNA therapeutics and was a catalyst to install some capability for LPP in Africa, the roll-out and introduction of RTS,S and R21 on the continent could thus be leveraged to boost and scale up such LPP capability to meet the demands and accelerate attainment of universal malaria immunization coverage. However, whether, when, or how that will be attained hinges on the solidity and stability of investment in scientific, management, and financing capabilities and practices on the continent (see domain ‘‘Research and development’’). If the hindrances associated with the human component are tackled effectively and sustainably, then these facilities could become an important asset that the continent could leverage to expand its capability to produce sustainably malaria vaccines to reduce the importation and associated public health consequences.
The Framework for Action (FFA) developed by the Partnerships for African Vaccine Manufacturing (PAVM, spearheaded by the Africa Centers for Disease Control and Prevention, established by the African Union (AU) in 2021), approved by the AU in 2022, aims to enable the continent to meet 60% of its vaccine needs through local production by 2040 in the context of AU Agenda 2063 [ 10 ]. Ensuring that the PAVM-FFA does not face the same difficulties that the PMPA (adopted in 2007) and other valuable strategic and higher-level mechanisms and frameworks faced is a major challenge. Current data on the indicators established by the PMPA-BP [ 16 ]—e.g., (i) proportion of pharmaceutical market supplied by African-based manufacturers, (ii) proportion of substandard MPs in the market, (iii) number of companies achieving WHO prequalification, among others—show negligible progress. The reliance on imported medicines continues to date (see data above and Fig. 1 ). The percentage of substandard and falsified (SF) medicines was estimated at 5–40% and 19–50% in several countries on the continent and in the Sahel countries in 2018, respectively [ 21 ]. Furthermore, it was only in 2022 that the first African-based manufacturer, Universal Corporation Limited (Kenya), received WHO prequalification to produce SP [ 22 ]. This is an essential medicine used in the chemoprevention of malaria in pregnancy (intermittent preventive treatment in pregnancy [IPTp]) and childhood (seasonal malaria chemoprevention [SMC] and perennial malaria chemoprevention [PMC]) and as a partner drug for ACT with ASP (also see Fig. 1 ). It can be seen that the PMPA, despite its noble aspirations, has delivered little impact to date.
Major hurdles to these and related mechanisms and frameworks typically reside in their implementation. The rampant epidemics of corruption and mismanagement in most of the continent [ 23 , 24 ] weaken not only public financing of critical infrastructure and services, but also regulatory frameworks, labour productivity, enforcement of rules, and other prerequisites for competitive LPP and trade [ 25 , 26 , 27 , 28 , 29 ]. The placement of unqualified or less qualified professionals in critical positions [ 30 ], a manifestation of these epidemics, lessens the impact of capacity building. Government non-compliance, e.g., with the Abuja Declaration of 2001 [ 6 ] (see Fig. 2 ), also a consequence of mismanagement [ 24 ], compounds the difficulties. These epidemics hinder, e.g., cross-border trade of active pharmaceutical ingredients (APIs) and sustainability of pharmaceutical investments. Thus, corruption and mismanagement are the key barriers to LPP and trade, although the nexus might not always be obvious without a rigorous analysis. Progress tracking is another challenge. An important improvement in PAVM-FFA compared to PMPA-BP is that the former has short-, medium-, and long-term key performance indicator targets [ 10 ], whereas the latter has monitoring and evaluation (M&E) indicators without targets [ 16 ]. However, for both PAVM-FFA and PMPA-BP, no baseline survey was conducted for their indicators, and research funding (e.g., to assess medicine quality) is scanty (see domain ‘‘Research and development’’). As a result, data, e.g., on compliance with pharmacopoeia requirements, is limited on the continent [ 21 ], thereby complicating the M&E of, e.g., the percentage of SF medicines nationally over time. These difficulties are far from new but are typically neglected by efforts aiming to advance LPP and trade in Africa.
Ensuring different outcomes and impacts for PAVM-FFA requires transformation, not simply incremental changes, including in business and governance practices not only across the continent but also in global organizations. A rigorous study of the root causes of chronic non-compliance by AU member states with their regulations and commitments is needed to allow its effective tackling. It is critical to leverage regional, continental, and global initiatives and organizations, e.g., the African Continental Free Trade Area (AfCFTA), World Trade Organization (WTO), United Nations Industrial Development Organization, and WHO, to reduce duplication of efforts, minimize costs, enforce compliance, overcome supply chain barriers, and ensure sustainability. Reform of the international system is necessary to strengthen the capacity of regional, continental, and global organizations to ensure the cost–benefit and sustainability of international investments and strategies to more effectively support LPP and trade in Africa. Doing so could contribute to reducing greatly historical inequities in pharmaceutical manufacturing and trade (as well as R&D). This could allow countries that most need anti-malarial drugs to produce and purchase them locally or regionally and thus remove a major obstacle to malaria elimination and eradication (Fig. 1 ).
In 2022, the WTO temporarily waived the Trade-Related Aspects of Intellectual Property Rights (TRIPS) agreement on MPs for COVID-19, given the exceptional circumstances of the pandemic [ 31 ]. This measure provided a critical facility for the international transfer of knowledge and technology for LPP of MPs for the prevention, diagnosis, and treatment of COVID-19. Given the epidemiological and economic burden of malaria in the AFR [ 12 , 13 , 32 , 33 ], a similar measure could be warranted to boost LPP and accelerate progress towards a world free of malaria. To ensure sustainability and maximize impact, any TRIPS agreement waiver on anti-malarial MPs should be coupled with adequate measures to: (i) incentivize local and international drug innovation and R&D (see domain ‘‘Research and development’’), (ii) strengthen local and continental regulatory, surveillance, and quality assurance capabilities, and (iii) boost continental trade of raw materials and APIs by leveraging the AfCFTA. Making access to TRIPS agreement waivers and similar initiatives conditional on each country’s commitment and progress on these fundamental prerequisites is critical to attaining the transformational changes needed to catalyze advancement in disease control. Failure to do so could complicate the political likelihood or feasibility of a TRIPS agreement waiver for anti-malarial MPs and similar initiatives, e.g., a pandemic treaty.
Transfer of manufacturing plants to endemic countries, an asymmetric initiative, may not on its own be sustainable. African countries need to transform into an environment that disincentivizes corruption and mismanagement. This is a necessary condition to attain a competitive LPP and trade to more effectively combat their major causes of death and suffering, e.g., malaria, towards disease elimination and eradication.
Research and development
What is the contribution of African higher education (HE) institutions to R&D to tackling the continent’s reliance on imported medicines and technology? In most of the continent, HE is not the hub for generating research, knowledge, and innovation but a neglected and underfunded sector, with research itself largely regarded as an appendage, rather than the core, of the academic work stream. Despite the commitment of AU member states in 2007 to allocate ≥ 1% of their gross domestic product in R&D [ 34 ], the continent’s public funding for R&D at 0.42% by 2019 remains one of the poorest, if not the poorest globally, just 25% of the global average of 1.7% [ 35 , 36 ]. Most, if not all, of these countries, including those approved for RTS,S priority allocation, do not comply with the Abuja Declaration of 2001 to allocate ≥ 15% of their annual budget to improve the health sector [ 6 , 37 ]. Among those with a combined share of global malaria mortality in 2021–2022 > 50% [ 12 , 13 ], the average government health financing in 2019–2021 was ≤ 5% in the Democratic Republic of the Congo, the Niger, as well as Tanzania, with little difference in several other countries on the continent (see Fig. 2 ). Rarely can R&D for health take place in such a setting.
These chronic difficulties and failures of governance cannot be tackled without institutional strengthening and eradication of the rampant epidemics of corruption and mismanagement in most of the continent [ 23 , 24 ]. These epidemics are also rampant in HE, affecting, e.g., research fund availability and allocation [ 25 , 38 ]. Successive HE reforms implemented in Africa have failed to solve these and other core issues hindering academic R&D despite gains in other domains [ 39 ]. Poor regulatory frameworks, chronic non-compliance, inconsistent enforcement of rules, and other deficiencies have undermined the realization of the potential of reforms to tackle the root causes of the weaknesses, thereby hampering HE performance. As a result, the global inequity in R&D has lingered. For instance, even after attaining advanced academic qualifications, most African researchers remain stuck in less prominent author list positions in peer-reviewed scientific publications (in the middle) [ 40 ].
Thus, African researchers end up having a limited role in the global research priority-setting, funding allocation, cutting-edge pre-clinical research, new trial designs, setting up of trial networks, and vaccine R&D, thereby weakening the African clinical trial ecosystem [ 41 ] and the scientific productivity and competitiveness of the continent. For instance, promising research by researchers from HE institutions in Australia, New Zealand, and Japan on mRNA malaria vaccine did not involve any African researchers or academic institutions [ 42 ]. In the last 10 years, Africa filed < 1% of global vaccine patents [ 10 ]. This creates a feedback loop, thus perpetuating inequity in pharmaceutical R&D and the reliance on imported medicines and technology. Indeed, even the mRNA clinical trials ongoing in Africa, e.g., for human immunodeficiency virus (HIV, mRNA-1644, Rwanda and South Africa), are typically not spearheaded by African academic, pharmaceutical, or research organizations, but by companies based in higher-income countries [ 43 ].
In the context of chronically limited local R&D, technology importation, that is, transfer, has emerged as an avenue to accelerate tackling inequity. mRNA technology transfer initiatives have been put in motion by development partners to advance R&D in LMICs. These initiatives include the mRNA Technology Transfer Programme established around Afrigen in South Africa in 2021 by the WHO and Medicines Patent Pool to provide technology development, training, and transfer to partners in LMICs [ 44 ]. The Bill & Melinda Gates Foundation has invested or allocated approximately ≥ US$135 million in mRNA research and vaccine manufacturing technology, including $60 million allocated to Quantoom Biosciences (based in Belgium), $5 million to the Institut Pasteur de Dakar (IPD, Senegal), and $5 million to Biovac (South Africa) [ 45 ]. These initiatives are necessary to advance mRNA technology to pave the way for its use to develop medicines for major causes of death and suffering in Africa, such as malaria. They could also contribute to accelerating the reduction of the reliance of African countries on imported medicines. However, the initiatives do not include solutions to address the underlying problems [ 23 , 24 , 38 ] that created the need for technology transfer, such as meager research and innovation in academic institutions in most of the continent. Also, there is an important differential in funding and asymmetry in roles between Europe-based Quantoom Biosciences and Africa-based IPD and Biovac. For instance, Univercells (based in Belgium), a parent company of Quantoom Biosciences, developed a low-cost mRNA research and manufacturing technology that IPD and Biovac are expected to acquire [ 45 ]. This implies that only a part of the funds allocated to African R&D institutes may be used for R&D by them, as the other may have to be ‘‘allocated back’’ to companies from higher-income countries. Thus, these shifts in R&D can deepen inequity rather than tackle it.
Investing in establishing and strengthening research infrastructures and capabilities in HE institutions across Africa similar to those that generated the mRNA technology in higher-income countries could be more impactful and sustainable than simply transferring a mature technology for development and production. An overview of the settings under which the science that led to the mRNA technology emerged and developed can illustrate this. Building on prior work by other researchers since the discovery of deoxyribonucleic acid (DNA) by Johann Friedrich Miescher (University of Tübingen) in 1869 [ 46 ], Watson and Crick (both, University of Cambridge) in the 1950s formulated the current structure of DNA (double helix) [ 47 ]. These researchers made such a contribution working under a solid research infrastructure not dominated by corruption and mismanagement. Such a research infrastructure also allowed expansion and deepening of the understanding of nucleic acids in the subsequent decades. This allowed Karikó and Weissman (both, University of Pennsylvania), since the 1990s, to gradually unlock the therapeutic potential of mRNA—until they finally discovered that using Pseudouridine (Ψ) instead of Uridine (U) could prevent the inflammatory response and increase protein production—thus paving the way for nucleoside-modified mRNA (modRNA) therapeutics [ 48 ]. Even so, a successful mRNA vaccine was not developed until after additional research and funding, including $25 million allocated by the Defense Advanced Research Projects Agency in 2013 to Moderna [ 49 ]. In 2020–2021, as the world was under the COVID-19 global public health emergency, leveraging the accumulated science of nucleic acids, Pfizer/BioNTech and Moderna delivered the first mRNA vaccines [ 50 , 51 ].
It can be seen that the game-changing discoveries that led to the mRNA technology, from Miescher to Karikó and Weissman, took place mostly at universities, which are neglected in most of Africa. Also, it took decades for the results of academic research (nucleic acids) to deliver results with pharmaceutical or clinical applicability (modRNA COVID-19 vaccines). Indeed, even malaria vaccines have been in R&D for at least eight decades. Since at least the 1940s, researchers have been attempting to induce protective immunity to malaria parasites using, e.g., killed or inactivated sporozoites, before RTS,S and R21 (that target the Plasmodium falciparum circumsporozoite protein and, to a lesser extent, the hepatitis B virus surface antigen) became the first and second approved human antiparasitic vaccines in 2021 and 2023, respectively [ 2 , 52 , 53 ]. Thus, substantive funding needs to be allocated continuously to HE institutions for research if game-changing solutions for public health challenges are to be observed on the continent. Sustainability is paramount. Otherwise, if AFR continues to neglect its HE, then even to fight against malaria (a preventable and curable disease whose approximately 3/4 of attributable deaths globally occur in its U5 [ 7 ]) the continent may have to continue relying on imported medicines and technology. Given the complexity of the biology of P. falciparum [ 54 , 55 ], even the mRNA technology transfer, on its own, not coupled with a solid investment in HE on the continent and institutional strengthening, may not be the panacea for meager R&D, at least not as expected.
Creating an R&D infrastructure capable of replicating or surpassing the successes that resulted in the mRNA technology cannot happen under the current academic and research governance and financing systems in Africa. Thus, if the current and future technology transfer or similar initiatives are to tackle the chronic reliance by African countries on imported medicines and technology, they need to invest equally or more in transformational change to address the root causes of the chronic hindrances to progress, not only the consequences. Eradication of the neglected epidemics of corruption and mismanagement on the continent is the most sustainable pathway to accelerate the attainment of equity in pharmaceutical R&D towards malaria elimination and eradication.
Conclusions
Transformation is needed in governance practices throughout the continent and in global organizations, as well as in the pharmaceutical landscape, from research to trade. Tackling inequitable reliance on imported medicines and technology requires solid and stable investment to establish and strengthen research infrastructures and capabilities in academic institutions on the continent. These are a necessary condition to create a sustainable environment capable of enabling endemic countries to boost innovation and LPP. Removing these major structural obstacles in the fight against malaria is critical to ensuring progress in eliminating and eradicating the disease. If these hindrances are tackled effectively and sustainably, the momentum created by malaria vaccine introduction and technological advancements ushered in by the COVID-19 pandemic could be a catalyst for bettering local research, development, and production of medicines. Lessons learned on malaria could then be translated to other vaccine-preventable diseases that, despite having effective vaccines, continue to burden the continent.
Availability of data and materials
The datasets used in the current study are publicly available and can be efficiently extracted from the sources cited in the article. The processed data that were presented in the main text and/or used to draw the graphs are available from the corresponding author upon reasonable request. The data analysis was performed using R version 4.3.0. Data and code sharing will require a Materials Transfer Agreement (MTA).
Abbreviations
Artemisinin-based combination therapy
African Continental Free Trade Area
WHO African Region
Active pharmaceutical ingredient
Artesunate-SP
African Union
Business plan
Coronavirus disease 2019
Deoxyribonucleic acid
Framework for action
Higher education
Institut Pasteur de Dakar
Low- and middle-income country
Local pharmaceutical production
Monitoring and evaluation
Nucleoside-modified mRNA
Medical product
Messenger ribonucleic acid
National Malaria Control Programme
Partnerships for African Vaccine Manufacturing
Pharmaceutical Manufacturing Plan for Africa
- R21/Matrix-M
Substandard and falsified
Sulfadoxine-pyrimethamine
Trade-Related Aspects of Intellectual Property Rights
Children younger than 5 years
Uncertainty interval
World Health Organization
World Trade Organization
WHO. Malaria vaccine: WHO position paper – March 2022. Wkly Epidemiol Rec. 2022;97:60–78.
World Health Organization. WHO recommends R21/Matrix-M vaccine for malaria prevention in updated advice on immunization. Geneva: World Health Organization; 2023.
Google Scholar
Hamilton A, Haghpanah F, Hasso-Agopsowicz M, Frost I, Lin G, Schueller E, et al. Modeling of malaria vaccine effectiveness on disease burden and drug resistance in 42 African countries. Commun Med (Lond). 2023;3:144.
Article PubMed PubMed Central Google Scholar
World Health Organization. WHO guidelines for malaria. Geneva: World Health Organization; 2023.
Volza. Global export import trade data of 209+ countries. Rehoboth BCH: Volza; 2023.
Organisation of African Unity. Abuja declaration on HIV/AIDS, tuberculosis and other related infectious diseases. Abuja; 2001.
Amimo F. Malaria vaccination: hurdles to reach high-risk children. BMC Med. 2024;22:111.
Georgieva K. Support for Africa’s vaccine production is good for the world: robust and reliable vaccine capacity in Africa is a global public good, deserving of global support. Washington: International Monetary Fund; 2022.
Gavi, The Vaccine Alliance. Expanding sustainable vaccine manufacturing in Africa: priorities for support. Geneva: Gavi, the Vaccine Alliance; 2022.
Africa Centres for Disease Control and Prevention. Partnerships for African Vaccine Manufacturing (PAVM) Framework for Action. Addis Ababa: Africa Centres for Disease Control and Prevention; 2022.
WHO. What is Africa’s vaccine production capacity? Brazzaville: World Health Organization Regional Office for Africa; 2021.
WHO. World malaria report 2022. Geneva: World Health Organization; 2022.
WHO. World malaria report 2023. Geneva: World Health Organization; 2023.
WHO. Inside Africa’s drive to boost medicines and vaccine manufacturing. Addis Ababa: World Health Organization – Ethiopia; 2021.
African Union. Pharmaceutical manufacturing plan for Africa. Addis Ababa; 2007.
African Union Commission (AUC) – United Nations Industrial Development Organization (UNIDO). Pharmaceutical manufacturing plan for Africa business plan. Addis Ababa: African Union; 2012.
Byaruhanga J. The pharmaceutical manufacturing plan for Africa. Midrand: African Union Development Agency-New Partnership for Africa’s Development (AUDA-NEPAD); 2020.
WHO. First malaria vaccine supply allocations May 2023: explanation of process and outcomes. Geneva: World Health Organization; 2023.
BioNTech. BioNTech achieves milestone at mRNA-based vaccine manufacturing site in Rwanda. Mainz: BioNTech; 2023.
Quantoom Biosciences. Etherna Immunotherapies and Quantoom Biosciences announce a strategic collaboration for the development of a novel RNA production system. Niel and Brussels: Quantoom Biosciences; 2021.
United Nations Office on Drugs and Crime. Trafficking in medical products in the Sahel: transnational organized crime threat assessment – Sahel. Vienna: United Nations Office on Drugs and Crime; 2023.
Book Google Scholar
Medicines for Malaria Venture. First African-manufactured medicine to prevent malaria in pregnant women and infants quality-approved by WHO. Geneva: MMV; 2022.
Transparency International. Corruption perceptions index 2023. Berlin: Transparency International; 2024.
Adeboye T, Economic and Social Council; United Nations, Economic Commission For Africa. Underdevelopment and natural resource abundance in Africa. ECA meeting of the Committee on Natural Resources and Science and Technology. Addis Ababa; 1999.
African Union. Stolen futures: the impact of corruption on children in Africa. Addis Ababa; 2021.
Griffore KA, Bowra A, Guilcher SJT, Kohler J. Corruption risks in health procurement during the COVID-19 pandemic and anti-corruption, transparency and accountability (ACTA) mechanisms to reduce these risks: a rapid review. Global Health. 2023;19:91.
Kohler JC, Martinez MG, Petrov M, Sale J. Corruption in the pharmaceutical sector: diagnosing the challenges. London: Transparency International UK; 2016. https://www.transparency.org.uk/sites/default/files/pdf/publications/29-06-2016-Corruption_In_The_Pharmaceutical_Sector_Web-2.pdf
Sié KJF. Industrial policy and labour productivity growth in Africa: does the technology choice matter? J Econ Struct. 2023;12:10.
Article Google Scholar
De Rosa D, Gooroochurn N, Görg H. Corruption and productivity: firm-level evidence. Jahrb Natl Okon Stat. 2015;235:115–38.
The Africa Report. AU: member states complain of unfair hiring practices, internal corruption. Paris; 2023.
World Trade Organization. Ministerial decision on the TRIPS agreement. Geneva; 2022.
Andrade MV, Noronha K, Diniz BPC, Guedes G, Carvalho LR, Silva VA, et al. The economic burden of malaria: a systematic review. Malar J. 2022;21:283.
Cirera L, Sacoor C, Meremikwu M, Ranaivo L, Manun’Ebo M, Arikpo D, et al. The economic costs of malaria in pregnancy: evidence from four sub-Saharan countries. Gates Open Res. 2023;7:47.
African Union. Assembly of the African Union eighth ordinary session: decisions and declarations. Addis Ababa; 2007.
Caelers D, Okoth D. Research funding in Africa: navigating sustainability and shifting perspectives. Nat Africa. 2023. https://doi.org/10.1038/d44148-023-00360-4 .
Adepoju P. Africa’s future depends on government-funded R&D: investing in research is key pathway to development on the continent. Nat Africa. 2022. https://doi.org/10.1038/d44148-022-00134-4 .
Kurowski C, Kumar A, Mieses Ramirez JC, Schmidt M, Silfverberg DV. Health financing in a time of global shocks: strong advance, early retreat. Washington: The International Bank for Reconstruction and Development/The World Bank; 2023.
Ngcamu BS, Mantzaris E. Anatomy and the detection of corruption in ‘previously disadvantaged’ South African universities. J Contemp Manage. 2023;20:323–49.
Varghese N. Governance reforms in higher education: a study of selected countries in Africa. Paris: United Nations Educational, Scientific and Cultural Organization (UNESCO) - International Institute for Educational Planning (IIEP); 2016.
Hedt-Gauthier BL, Jeufack HM, Neufeld NH, Alem A, Sauer S, Odhiambo J, et al. Stuck in the middle: a systematic review of authorship in collaborative health research in Africa, 2014–2016. BMJ Glob Health. 2019;4:e001853.
Africa Centers for Disease Control and Prevention (Africa CDC) – African Union Development Agency-New Partnership for Africa’s Development (AUDA-NEPAD). Optimizing efficiency and impact in the African clinical trials ecosystem. Addis Ababa: Africa Centers for Disease Control and Prevention (Africa CDC) – African Union Development Agency-New Partnership for Africa’s Development (AUDA-NEPAD); 2023.
Ganley M, Holz LE, Minnell JJ, de Menezes MN, Burn OK, Yew Poa KC, et al. mRNA vaccine against malaria tailored for liver-resident memory T cells. Nat Immunol. 2023;24:1487–98.
Article CAS PubMed Google Scholar
Saied AA. Building Africa’s first mRNA vaccine facility. Lancet. 2023;402:287–8.
Article PubMed Google Scholar
WHO. mRNA Technology Transfer Programme moves to the next phase of its development. Geneva: World Health Organization; 2023.
Bill & Melinda Gates Foundation. Gates Foundation to accelerate mRNA vaccine innovation and manufacturing in Africa and globally. Seattle: Bill & Melinda Gates Foundation; 2023.
Dahm R. Discovering DNA: Friedrich Miescher and the early years of nucleic acid research. Hum Genet. 2008;122:565–81.
Watson JD, Crick FH. Molecular structure of nucleic acids: a structure for deoxyribose nucleic acid. Nature. 1953;171:737–8.
The Nobel Assembly at The Karolinska Institutet. Scientific background 2023 – Discoveries concerning nucleoside base modifications that enabled the development of effective mRNA vaccines against COVID-19. Stockholm; 2023.
The Economist. A growing number of governments hope to clone America’s DARPA. London; 2021.
World Health Organization. WHO issues its first emergency use validation for a COVID-19 vaccine and emphasizes need for equitable global access. Geneva: World Health Organization; 2020.
WHO. Recommendation for an emergency use listing of COVID-19 mRNA vaccine (nucleoside modified) submitted by Moderna Biotech (Spain). Geneva: World Health Organization; 2021.
El-Moamly AA, El-Sweify MA. Malaria vaccines: the 60-year journey of hope and final success—lessons learned and future prospects. Trop Med Health. 2023;51:29.
Nussenzweig RS, Vanderberg J, Most H, Orton C. Protective immunity produced by the injection of x-irradiated sporozoites of Plasmodium berghei . Nature. 1967;216:160–2.
Anton L, Cobb DW, Ho CM. Structural parasitology of the malaria parasite Plasmodium falciparum . Trends Biochem Sci. 2022;47:149–59.
Oyedeji SI, Bassi PU, Oyedeji SA, Ojurongbr O, Oluwatoyin H. Genetic diversity and complexity of Plasmodium falciparum infections in the microenvironment among siblings of the same household in North-Central Nigeria. Malar J. 2020;19:338.
Download references
Acknowledgements
Author information, authors and affiliations.
Faculty of Medicine, Eduardo Mondlane University, Maputo, Mozambique
Floriano Amimo
You can also search for this author in PubMed Google Scholar
Contributions
FA contributed to conceptualization, methodology, software, validation, formal analysis, investigation, resources, data curation, writing—original draft, writing—review and editing, visualization, project administration, and funding acquisition. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Floriano Amimo .
Ethics declarations
Ethics approval and consent to participate.
Ethics approval and consent to participate are not necessary because this research did not collect identifiable human material and data.
Consent for publication
Not applicable.
Competing interests
FA reports consultancy fees from the WHO.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Amimo, F. Leveraging malaria vaccines and mRNA technology to tackle the global inequity in pharmaceutical research and production towards disease elimination. Malar J 23 , 136 (2024). https://doi.org/10.1186/s12936-024-04972-5
Download citation
Received : 12 October 2023
Accepted : 01 May 2024
Published : 06 May 2024
DOI : https://doi.org/10.1186/s12936-024-04972-5
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Drug development
- Plasmodium falciparum
Malaria Journal
ISSN: 1475-2875
- Submission enquiries: [email protected]
- Tata Steel share price
- 164.20 -2.03%
- ITC share price
- 440.40 1.33%
- Power Grid Corporation Of India share price
- 295.25 -3.80%
- HDFC Bank share price
- 1,506.40 -1.08%
- Kotak Mahindra Bank share price
- 1,644.30 1.20%
World Malaria Day 2024: 7 things you don't know about the disease
World malaria day 2024: world malaria day is celebrated every year across the world to spread the word about the disease, its symptoms, and precautions.

World Malaria Day 2024: A vector borne disease, malaria, is highly prevalent in tropical countries due to rainy and humid weather. The disease is caused by mosquito bites. One of the most common symptoms of malaria is fever with shaking chills. Even though the disease is very common, proper hygiene and sanitation can prevent the spread of the disease.
World Malaria Day 2024: Theme for the year
This year's theme for World Malaria Day 2024 is “Accelarate the fight against malaria for a more equitable world". The day is celebrated across the world th
The theme for this year is “Accelerate the fight against malaria for a more equitable world." The day is celebrated across the world to signify the efforts to end the disease from the root and spread awareness among people.
World Malaria Day 2024 theme extension of previous year's theme
This theme, which is in sync with this year's World Health Day theme -- "My Health, My Right" -- underscores the urgent need to address the stark inequities that persist in access to malaria prevention, detection and treatment services.
Most nations reporting death due to malaria
According to UNICEF data, four out of five malaria deaths are reported in African nations. The 15 countries with most number of deaths due to malraria are Nigeria, the Democratic Republic of the Congo, India, Mozambique, Ghana, Angola, Uganda, etc.
How to prevent malaria infection?
One of the most effective measures to prevent malaria infection is sleeping under an insecticide-treated bed net (ITN). According to UNICEF data 2016, nearly 54% of people at risk of malaria in sub-Saharan Africa used an insecticide-treated bed net to prevent malaria infection.
Malaria is the third largest killer of children
Malaria is the third largest communicable disease which is killing children between the ages of one month and five years, after pneumonia and diarrhea. Nearly 300,000 children under the age of five die of malaria died in 2016 equivalent to nearly 800 young lives lost each day.
Global immunisation efforts
The global immunisation efforts by the World Health Organisation (WHO) have saved nearly 154 million lieves in last five decades. Infants have emerged as the largest beneficiary of the immunisation effots.
In a study published in the Lancet, WHO gave a comprehensive analysis of the impact of 14 vaccines used under the Expanded Programme on Immunisation (EPI), which celebrates its 50th anniversary next month.
Thanks to these vaccines, "a child born today is 40 percent more likely to see their fifth birthday than a child born 50 years ago", WHO chief Tedros Adhanom Ghebreyesus told reporters.
Malaria a significant risk to refugees, migrants
Malaria is a bigger risk to refugees, migrants, internally displaced people and indigenous people, according to Saima Wazed, WHO Regional Director for South-East Asia
"Malaria remains a significant public health challenge in our region, affecting nine out of eleven countries and accounting for a third of the global burden outside Africa," the WHO regional director for South-East Asia said.
Milestone Alert! Livemint tops charts as the fastest growing news website in the world 🌏 Click here to know more.
Amazon Summer Sale is here! Splurge and save now! Click Here!
Wait for it…
Log in to our website to save your bookmarks. It'll just take a moment.
You are just one step away from creating your watchlist!
Oops! Looks like you have exceeded the limit to bookmark the image. Remove some to bookmark this image.
Your session has expired, please login again.
Congratulations!
You are now subscribed to our newsletters. In case you can’t find any email from our side, please check the spam folder.

Subscribe to continue
This is a subscriber only feature Subscribe Now to get daily updates on WhatsApp

Sign up for the Health News Florida newsletter
The invisible lives — and deaths — of the children of sex workers.

Havilah Uloma doesn't have any pictures of her son, Kamsi.
"I had to destroy the pictures," she says.
Uloma – who lives in Rivers State, Nigeria, and works in a brothel – says it's too painful to remember her son, who died in November. He was 1 year old.
"I didn't go to the hospital. There was no money," says Uloma, who is 40 and doesn't have any other children. "I was buying roadside [medications] to give him. That was when he gave up. He left. He died."
She doesn't know exactly what killed her son; she thinks it might have been an infection or maybe the roadside medications were counterfeit. What Uloma does know is that as painful as her experience is, it is "common," she says. Many of her fellow sex workers have lost children.
While countries routinely collect child mortality data, very little is known about the lives — and premature deaths — of sex workers' children. Sometimes there are no records of these kids' births or deaths.
"They could be born in a brothel and their birth is not registered. So for many of these children, on paper, they may not exist," says Dr. Wendy Macias-Konstantopoulos , an associate professor at Harvard Medical School and a specialist in health equity.
Researchers have also ignored this population. "Although there are studies on HIV among female sex workers, these children are not making the radar," she says.
Now there are efforts to shed light: A study published in March provides some of the first figures on the possible causes of death for these youngsters. In addition, a program for pregnant sex workers and their children at a small Nigerian hospital has revealed dire health problems. This push is spearheaded by the nonprofit Global Health Promise , which is based in Oregon and works in nine countries, focusing on the health of mothers who are sex workers and their children.
"The issues are overwhelming. I think I'd actually call it a state of emergency," says Dr. Patrick Ezie , medical director of Silver Cross Hospital in Abuja, Nigeria, which houses the new program for pregnant sex workers and their children. "It is shocking — and we don't get shocked easily."
'These babies are born struggling'
Ezie has been a doctor in Nigeria for 15 years. In that time, he's seen a lot of suffering, he says. But still, he was taken aback by the severity of the health problems he saw when his hospital began the program for pregnant sex workers in November 2023.
For starters, he says, many of the sex workers he's met have received no prenatal care. He cites both financial constraints and logistical constraints, since many work at night and sleep during the day. The lack of prenatal care is a particular problem for the mothers who learn at the time of delivery that they are HIV positive or have syphilis, he says. Without preventive medication during pregnancy, it is hard to avoid transmission to the baby.
For those women who are brought into the program early enough for prenatal care, Ezie's clinical staff have noticed a number of issues. He says the women often don't have enough food during pregnancy and many face harsh situations. "They have to work even though they're pregnant and the male partner that they meet every night may not be gentle," he explains.
Ezie's found that when sex workers deliver their babies, the newborns are more likely to be born small, weak or in need of resuscitation.
"These babies are born struggling," he says, adding that their struggle often continues into childhood. Many infants are weaned off breast milk and given solid foods far too young, sometimes at just one month old, because their mothers have to work. Not only do those kids lose the protective benefits of breast milk but they could be at risk of choking. A too-early diet of solids is also associated with long-term health complications such as obesity and diabetes.
And Ezie sees children with stunted growth. For example, many of the 5-year-olds who come to his hospital's program are the size of an average 3-year-old because they're malnourished.
Ezie's program currently serves about 40 sex workers and their families. Global Health Promise also supports maternal and child health programs for sex workers in five other Nigerian cities as well as in Uganda and Kenya.
"What we're doing is very insignificant compared to the volume of the women who are out there who are doing sex work and need help," Ezie says.
'Let me give this child this drug'
Brian Willis – who is the founder and director of Global Health Promise – argues that there's not more help because the population is often invisible. The lack of information, he says, means there are "no policies, no funding, no awareness." He's trying to change that.
In 2019, the researchers for the study interviewed sex workers in Angola, Brazil, the Democratic Republic of the Congo, India, Indonesia, Kenya, Nigeria and South Africa. They gathered detailed information on the deaths of nearly 600 children of sex workers. The findings were published in March in The Journal of Global Health, a peer-reviewed journal.
The study used an approach called "community knowledge" – interviewing sex workers about the children of fellow sex workers who had died.
In research circles, t his methodology is employed in hard to reach populations and when it is challenging to get information directly from the source. Willis says his team found that mothers are sometimes reluctant to talk about their own child's death, likely because it's emotionally hard and shameful or because parents fear consequences if neglect is involved.
"Most of us would know if the child of a friend died or a neighbor died. And they do too. It is no different than that," says Willis, who explains that the researchers combed the data to ensure duplicate deaths were removed.
"What we found was that there are a large number of deaths among the children of female sex workers across these countries," says Macias-Konstantopoulos, of Harvard Medical School, who is the lead author of the study and an adviser to Global Health Promise.
The researchers got as many details as they could about why each child might have died and found that malnutrition was common as were accidents – like house fires – and communicable diseases – like malaria and HIV. Another cause of death frequently cited by the mothers was a reaction to medication.
This doesn't surprise Uloma, the sex worker from Nigeria whose 1-year-old son died.
She says one of her fellow sex workers, who had to work at night and didn't have anyone to watch her 2-year-old daughter, gave her child Tramadol, a strong pain killer known to make people drowsy. The goal was for the toddler to sleep through the night.
"She was like: 'Let me give this child this drug. She will sleep. Nobody will know I am not around,' " recounts Uloma. "But unfortunately to her, before she came back, the child died."
Outside experts have praised the research for beginning to fill a major gap in information. "It's commendable that they were able to engage in this work and collect this data so that we even have a starting point," says Jennifer Seager , an associate professor in the department of global health at George Washington University.
However, people in the field say there are many unanswered questions about the study. Seager wondered why the study was not able to draw conclusions about how much more or less likely it is for sex workers' children to die compared to children in a similar economic setting. The researchers say they looked at just a small subset of the population of sex workers and nobody knows the total numbers.
Seager also wonders whether there are different rates and causes of child mortality among sex workers who work on the street compared to those in a brothel or those who do sex work as a second job.
For her part, Uloma is eager to see action to improve the situation. And she has an idea of what might help: "The community, the society need more awareness," she says. "Most times people don't really know that sex workers, they even have children."
One thing she does is try to let people in her community know that sex workers have children – and those children "have their own lives to live."
Copyright 2024 NPR

IMAGES
COMMENTS
The Center for the Study of Complex Malaria in India. The Center for the Study of Complex Malaria in India (CSCMi) is a partnership between Indian and U.S.-based investigators to develop the knowledge, tools and evidence-based strategies needed to support the intervention and control programs of Indian government organizations, and to build ...
The three inter-related objectives of this study were: (1) identification of the trends of malaria cases in India over the period 1990 to 2022 using time series analysis in order to forecast future malaria case burden for 2023 and 2030; (2) perform segmented regression on interrupted time series data to assess the impact of major interventions ...
The WHO's World Malaria Report 2020 highlighted India's gains in the path to elimination. India recorded impressive 60% reduction in reported cases compared with 2017, and a 46% reduction in cases compared with 2018, which built momentum to reach the goal of zero indigenous malaria cases by 2027. India's National Strategic Plan for ...
Summary of World Malaria Report 2021. In 2020, 29 of the 85 countries that were malaria-endemic accounted for 96% of malaria cases. India contributed 1.7% of malaria cases and 1.2% deaths globally. Between 2019 and 2020, all high burden to high impact (HBHI) countries except India reported increases in cases and deaths (and in India, the rate ...
Malaria and risk in clinic studies. In our clinic studies (passive case detection), ... Malaria in India: the Center for the Study of Complex Malaria in India. Acta Trop 121, 267-273 (2012).
India is slated for malaria elimination by 2030.4 It contributed 83% of the estimated malaria cases and 82% of malaria deaths in South-East Asia Region (SEAR) in 2020, according to the 2021 WMR. Plasmodium falciparum and P. vivax are the major prevalent parasites in India. The country contributed 51% of the global P. vivax cases in 2016, when the country launched the National Framework for ...
India's goal of eliminating malaria by 2030 may appear at first glance to be easily attainable. Reported cases of the disease dropped by around half between 2001 and 2016 and, in nearly three-quarters of India's more than 650 districts, the number of people falling ill from malaria is very low.
Purulia is a malaria-prone district in West Bengal, India, with approximately half of the blocks defined as malaria endemic. We analyzed the malaria case in each block of the Purulia district from ...
The World Malaria Report (WMR) 2020 released by WHO, which gives the estimated cases for malaria across the world, based on mathematical projections, indicates that India has made considerable progress in reducing its malaria burden. India is the only high endemic country which has reported a decline of 17.6% in 2019 as compared to 2018.
The malaria situation in India is complex as a result of diverse socio-environmental conditions. India contributes a substantial burden of malaria outside sub-Saharan Africa, with the third highest Plasmodium vivax prevalence in the world. Successful malaria control in India is likely to enhance malaria elimination efforts in the region. Despite modest gains, there are many challenges for ...
Background India has launched the malaria elimination initiative in February 2016. Studies suggest that estimates of malaria are useful to rationalize interventions and track their impact. Hence, a national study was launched to estimate burden of malaria in India in 2015. Methods For sampling, all 624 districts of India were grouped in three Annual Parasite Incidence (cases per thousand ...
The variability and heterogeneity in malaria parameters in a vast country like India requires a highly granular approach for analyzing malaria incidence and planning appropriate interventional tools. Understanding the malaria-metric data of a particular region is a prerequisite for effectively designing any operational study.
Malaria continues to have devastating effect on people's lives especially in developing countries. India is slated for malaria elimination by 2030. Though India has sustained a decline in malaria burden at the national level the epidemiological picture remains heterogenous. India's road to malaria elimination plan is riddled with many roadblocks. Major challenges include insufficient ...
In India, approximately 44% of cases have been reported to be disproportionately contributed by approximately 27 districts. 1 A comparative analysis of reported malaria cases between January 2017 and December 2022 was performed in Mandla district, which is the site of a model malaria elimination demonstration project (MEDP) in Madhya Pradesh ...
Odisha has recorded a 24% decline in malaria cases and 60% decline in reported deaths in 2011 compared to 2010. The total number of reported malaria deaths declined from 247 to 100 between 2010 ...
More than 90% of India's 161,516 reported malaria cases in 2021 were concentrated in just 8 states, all of which have significant tribal populations. The tribal districts that report malaria ...
This study relies on an extensive surveillance dataset of Plasmodium falciparum cases for Surat, India, to investigate the variation and drivers of malaria risk in a heterogeneous urban environment. A statistical model for the spatiotemporal variation of cases was developed, which includes both climatic and socioeconomic drivers, with the ...
Study site. The observations took place in the Suaq Balimbing research area (N 3° 02.873′, E97° 25.013′), a part of the Gunung Leuser National Park in South Aceh, Indonesia.
The good news is that the World Malaria Report has also documented the remarkable decline in malaria incidence in India, the estimated malaria cases were reduced by 24% in 2017 compared to 2016 and 28% in 2018 compared to 2017. In May 2015, the World Health Assembly endorsed the Global Technical Strategy (GTS) for Malaria Elimination 2016-2030 ...
Reliance on imported medicines has traditionally been a major weakness of malaria control efforts in Africa. About 96-95.4% and 75.7-74.5% of global malaria deaths in 2021-2022 occurred in the WHO African Region (AFR) and among children younger than 5 years (U5) in the region, respectively [7, 12, 13].Yet the continent has to import medicines to protect itself against the disease.
Most nations reporting death due to malaria. According to UNICEF data, four out of five malaria deaths are reported in African nations. The 15 countries with most number of deaths due to malraria ...
In 2019, the researchers for the study interviewed sex workers in Angola, Brazil, the Democratic Republic of the Congo, India, Indonesia, Kenya, Nigeria and South Africa. They gathered detailed information on the deaths of nearly 600 children of sex workers. The findings were published in March in The Journal of Global Health, a peer-reviewed ...
What I saw was that things like diarrhea, pneumonia, malaria, that each were killing over a million children were getting almost no attention because the poorest in the world who were suffering from these things didn't have a voice in the marketplace. It seemed like these poverty-related diseases deserved philanthropic attention.