Obstetrics and gynaecology
Showing results 1 - 10 of 100
Sorted by most recent
14 May 2024
22 April 2024
16 April 2024
8 April 2024
2 April 2024
27 March 2024

Masks Strongly Recommended but Not Required in Maryland, Starting Immediately
Due to the downward trend in respiratory viruses in Maryland, masking is no longer required but remains strongly recommended in Johns Hopkins Medicine clinical locations in Maryland. Read more .
- Vaccines
- Masking Guidelines
- Visitor Guidelines
Center for Bloodless Medicine and Surgery
Case study: obstetrics and gynecology, embolization to treat uterine fibroids with bleeding and severe anemia.
A 45-year old female Jehovah’s Witness patient with a history of uterine fibroids and severe menorrhagia presented with shortness of breath, fatigue and weakness. She also had a history of deep venous thrombosis (DVT) and pulmonary emboli (PE). She was admitted with iron-deficient anemia for workup and treatment.
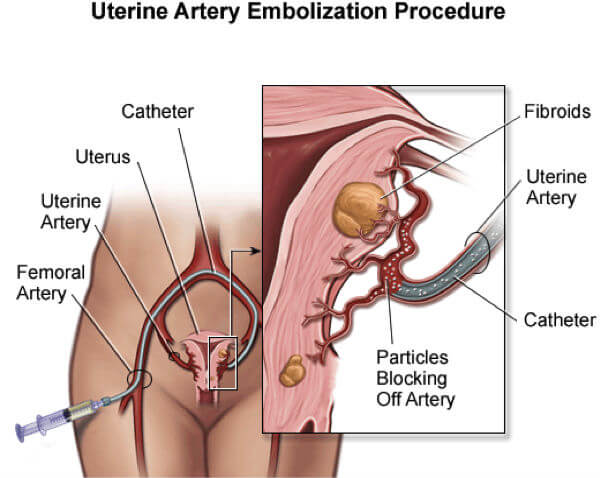
After a Hematology consult, the Coumadin she had been taking for her DVT/PE history was discontinued. Gynecology was consulted and she was diagnosed with multiple large fibroids after a transvaginal ultrasound examination. It was determined that a hysterectomy may be needed, but her 3.8 g/dL hemoglobin level upon admission was too low for surgery. She was started on Lupron (Leuprolide acetate), a long acting (depot) injection medication that suppresses secretion of the gonadotropins luteinizing hormone (LH) and follicle-stimulating hormone (FSH), and is thereby helpful in cessation of hemorrhage from uterine fibroids. She was also started on daily, intravenous 200 mg iron sucrose, and was given darbepoetin alpha 25 mcg intravenously weekly. After 3 weeks her hemoglobin level was 5.5 g/dL and she was sent home on monthly Lupron injections and oral iron supplements. She was also followed in our Hematology clinic.
Four months later she was admitted again with shortness of breath, fatigue and weakness, this time with a hemoglobin level of 3.8 g/dL. She had missed one treatment in her Lupron regimen, and had started to bleed again. Her ferritin level was 9 ng/mL (normal level for women being 18-160). On her third hospital day she was taken to interventional radiology for a uterine artery fibroid embolization. Two days later she was discharged with a hemoglobin level of 4.9 on oral iron sulfate, 325 mg twice a day. One month later on a follow up visit in the Hematology Clinic her hemoglobin level was 8.0 and she is now off of Lupron and continuing her oral iron supplements.

Case Reviews, Study Guides, and Step Exams: Obstetrics & Gynecology
- Cases and Self-Assessment
- Anatomy, Histology, and Physiology
- Emergency Medicine
- Family Medicine
- Internal Medicine
- Microbiology & Biochemistry
- Neurology/Neuroscience
- Obstetrics & Gynecology
- Pharmacology
Reviews at a Glance
- LWW Medical Education Exam Review Texts
- LWW Clerkship/Clinical Rotations Exam Review Texts
- AccessMedicine Self-Assessment
Ob/Gyn Review Titles
Helpful Review Links
- Obstetrics & Gynecology Subject Guide Created and curated by the Maguire Medical Library
- LWW Health Library Ob/Gyn Exam Prep
- Williams Obstetrics Study Guide
- << Previous: Neurology/Neuroscience
- Next: Pathology >>
- Last Updated: May 14, 2024 3:57 PM
- URL: https://med-fsu.libguides.com/cases
Maguire Medical Library Florida State University College of Medicine 1115 W. Call St., Tallahassee, FL 32306 Call 850-644-3883 (voicemail) or Text 850-724-4987 Questions? Ask us .
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- J Intensive Care Soc
- v.18(3); 2017 Aug
A complex obstetric case
A 33-year-old primigravida presented with severe sepsis, severe pre-eclampsia, peripartum cardiomyopathy and the haemolysis, elevated liver enzymes and low platelets syndrome manifesting over the course of 24 h causing a diagnostic conundrum and a difficult sequence of physiological problems to overcome. We describe a previously unreported sequence of events involving a pre-eclamptic, septic parturient to improve anaesthetic and intensive care physician awareness of confounding factors that complicate assessment and management of these patients.
Pre-eclampsia is a common and potentially fatal condition associated with the later stages of pregnancy. The pathophysiology is believed to relate to imperfect trophoblastic implantation of the placenta to the uterus. This results in endothelial dysfunction, not localised to the uteroplacental unit, causing maternal hypertension and proteinuria. A spectrum of illness is described ranging from mild through severe, qualified by diagnostic parameters or the presence of other organ involvement: namely eclamptic seizures; acute kidney injury; or haemolysis, elevated liver enzymes and low platelets (HELLP) syndrome. Again, the pathophysiology of these complications is well studied yet poorly defined with multiple theories – many of which centre on endothelial dysfunction and vasoconstriction. A summary of pre-eclampsia is available in multiple review articles. This report describes a near-fatal combination of complications of pregnancy.
Peripartum cardiomyopathy is an uncommon complication of pregnancy historically occurring in around 1:4000 deliveries. 1 The incidence is believed to have been rising over the past decade due to increasing maternal age with rates approaching 1:2000 – such that the average delivery unit will be encountering several cases each year. 2 , 3 The diagnosis is based on exclusion of other causes of cardiomyopathy in the setting of late pregnancy. There is an increased risk of peripartum cardiomyopathy in pre-eclampsia and some papers describe it as a direct consequence thereof. The illness mandates a left ventricular ejection fraction (LVEF) of less than 45% developing in the last month of pregnancy or the first 5 weeks post-partum in the absence of other causes. The pathophysiology is unknown with multiple theories including it being the cardiac manifestation of pre-eclampsia or the consequence of an autoimmune myocarditis. 4 , 5 An increasing focus is the role of abnormal cleavage of prolactin in the near-term parturient. Genetically modified mice producing an atypical 16 kDa prolactin fragment show altered vascular endothelium leading to myocardial dysfunction, remodelling and symptomatic peripartum cardiomyopathy. 6 The same raised prolactin derivative has been found in women with peripartum cardiomyopathy and has opened up a therapeutic target through the use of bromocriptine (a dopamine agonist that reduces prolactin production). 7 Managing one of these conditions can be challenging but a patient with a combination of these conflicting physiological changes causes difficult diagnostic and therapeutic dilemmas.
Case report
A 33-year-old primigravida with an in vitro fertilisation pregnancy using a donor egg presented at Term + 7 with a 2-week history of coryzal symptoms and pyrexia. Her past medical history consisted of a previous deep vein thrombosis whilst taking the oral contraceptive pill for which she had been prophylactically anticoagulated during pregnancy.
On initial presentation, our patient had evidence of moderate pre-eclampsia (blood pressure (BP) 150/80 mmHg; urinary protein-creatinine ratio (PCR) 216) with a pyrexia (temperature 38.7℃) and raised inflammatory markers (C-reactive protein (CRP) 109 mg/dl; white cell count 12.9 × 10 9 /L). She was admitted to the labour ward for observation, antibiotics (IV Cefuroxime (1.5 g), Metronidazole (500 mg) 8-hourly as per obstetric guidelines), and induction of labour (Propess 10 mg). Throughout her induction, she was tachycardic and tachypnoeic with a productive cough and pyrexia, whilst her systolic BP remained roughly between 140 and 150 mmHg.
Pre-eclampsia protocols mandate strict fluid monitoring (with fluid restriction in the case of severe pre-eclampsia – whose criteria our patient did not fulfil), whilst sepsis protocols advocate targeted fluid challenges. Following the departmental sepsis algorithm, our patient received 11 L of IV crystalloid over 96 h and IV antibiotics for 4 days. She failed induction of labour and underwent a Category 3 lower segment caesarean section (LSCS) under combined spinal-epidural delivering a healthy baby boy on the fifth day.
Following delivery, she was transferred to obstetric recovery where she deteriorated significantly over the ensuing 24 h, becoming increasingly tachypnoeic (RR 30–40 breaths per minute) and tachycardic (HR 130–150 beats per minute (bpm)) with an increasing oxygen requirement. BP remained around 150/95 mmHg. She was reviewed multiple times by both medical, obstetric and anaesthetic teams. Diagnoses considered at the time included possible pulmonary embolus (PE) and worsening of her chest sepsis. A computed tomography pulmonary angiogram (CTPA) showed bilateral consolidation and significant interstitial oedema with no PE. Following this, she was admitted to the intensive care unit (ICU) due to severe hypoxaemia.
On admission to ICU, she was in pulmonary oedema, requiring 15 L/min O 2 therapy via non-rebreather mask to maintain SpO 2 > 94% with a respiratory rate of 40 breaths per minute. Her heart rate was 140 bpm and BP 192/114 mmHg – a diagnosis of severe pre-eclampsia was made. Her Glasgow Coma Scale score was 15 throughout. Considering our patient did not have a PE but had hypertension with consolidation; pre-eclampsia and sepsis alone did not adequately account for the clinical severity of her pulmonary oedema as manifested by severe hypoxia and copious pink frothy sputum. On this basis, an echocardiogram was requested. However, due to her rapid deterioration it could not be performed immediately.
Knowing a diagnosis of severe pre-eclampsia at this time, management should involve BP control and MgSO 4 therapy. However, given the possible need for intubation and the potential cardiovascular changes anticipated at induction, these were withheld and she was trialled on continuous positive airway pressure ventilation (CPAP + 10 cm H 2 O, FiO 2 1.0).
Unfortunately, she deteriorated with a HR of 180 bpm (sinus rhythm), BP of 190/130 mmHg and falling peripheral oxygen saturations to 70–80% despite the aforementioned CPAP settings. She underwent peri-arrest (secondary to hypoxaemia) intubation (Propofol 50 mg, Fentanyl 150 mcg, Rocuronium 70 mg, Propofol 50 mg) with a brief (pulseless electrical activity) cardiac arrest on induction. Return of spontaneous circulation was quickly obtained (<40 s) through advanced life support protocols with 1 mg adrenaline given. Persistent hypotension followed, resistant to noradrenaline (0.3 mcg/kg/min) and intravascular volume resuscitation.
A transthoracic echocardiogram (TTE) was performed to assess ventricular function, which showed an equally dilated LV/RV with global severe systolic impairment and LVEF < 12%, implicating cardiomyopathy as a significant contributor to her deterioration.
Oesophageal Doppler monitoring was used to titrate further inotropic support sequentially: adrenaline (0.1 mcg/kg/min), dobutamine (15 mcg/kg/min) and enoximone (5 mcg/kg/min), the emphasis on inotropy. Optimised treatment achieved stroke volume 27 ml, corrected flow time 300 ms and a cardiac output of 3.7 L/min. Early liaison with a tertiary cardiothoracic centre prompted intra-aortic balloon pump insertion and transfer to regional heart transplant centre for further management.
During the above 12-h period, the patient’s platelet count fell from 172 to 48 × 10 9 /L, whilst hepatic transaminases rose from 89 to 470 IU/L with development of coagulopathy (International Normalised Ratio 1.6) and resistant hypoglycaemia. There was a mild anaemia (haemoglobin concentration of 11.2 g/dl) and a partial HELLP syndrome was diagnosed. 8 Supportive management was initiated with emphasis placed on the optimisation of cardiac output. Once her haemodynamic status had stabilised, she was commenced on an MgSO 4 infusion in an attempt to mitigate her pre-eclampsia (4 g IV bolus followed by 1 g/h infusion for 24 h).
Following arrival at the cardiac centre, she was commenced on bromocriptine. Other cardiovascular support was slowly weaned. Her liver function deteriorated for the first 36 h with transaminases peaking > 1000 IU/L before slowly improving. Inotropes were weaned and LVEF recovered to 20% by the end of 2 weeks. She was then extubated and discharged to the medical ward and subsequently home approximately 5 weeks after her initial hospital presentation. Two months after discharge, follow-up TTE showed a LVEF of 68% with normal sized chambers.
The septic, pre-eclamptic patient
Sepsis and pre-eclampsia are both common enough pathologies that the two co-present. The pre-eclamptic exists in a state of hypertensive vasoconstriction with endothelial dysfunction predisposing to renal proteinuria and peripheral oedema. As a consequence of this, patients tend to be intravascularly fluid deplete. The septic patient also experiences endothelial aberrance but develops hypotension due to fluid deficit and cytokine-mediated vasodilatation. The common theme of these two syndromes is an intravascularly hypovolaemic patient. Cardiovascular collapse can be seen on induction of anaesthesia both due to further vasodilatation secondary to the centrally mediated actions of anaesthetic drugs combined with the abrupt reduction in venous return seen in the transition to positive pressure ventilation. In this combination of contrasting physiologies, how does one interpret a reasonably normotensive patient – are either both, or neither, pathologies at work?
Sepsis remains a significant cause of maternal mortality in the CEMACH/MBRACE reports. It is possible that the hypertension of pre-eclampsia can compensate for what would otherwise be sepsis-induced hypotension. In mild cases, adverse consequences of this may not be seen but at the severe end of both spectra, there is potential for significant organ dysfunction, albeit with a seemingly normal blood pressure.
Whilst early management of sepsis should continue as per the Surviving Sepsis Guidelines, the liberal administration of fluid may be poorly tolerated in pre-eclampsia. Lack of experience and confidence in the management of these combined conditions can lead to suboptimal management of both and patient deterioration as a consequence. There is a good argument to be made for early ICU input for invasive monitoring to optimise cardiac output.
Peripartum cardiomyopathy
The presence of a dilated, cardiomyopathic heart in a previously healthy obstetric patient is, thankfully, uncommon. Differentials for this form of acute heart failure include septic and peripartum cardiomyopathies.
- Septic cardiomyopathy is not uncommon but characteristically forms a part of multi-organ dysfunction seen in advanced sepsis in a patient who is usually on multiple vasopressors/inotropes, more associated with Gram negative sepsis. Management often follows a sequence of preload optimisation, inotropic improvement of contractility and as a later line, inodilation. Source control should be achieved.
- Peripartum cardiomyopathy is a rare complication of pregnancy and is thought to be slightly more common in pre-eclampsia (although may simply be more symptomatic). Presentation is that of heart failure with symptoms including low BP and a tendency to both peripheral and pulmonary oedema. Management aims to optimise contractility whilst minimising further myocardial damage.
Hypotension may be poorly tolerated by the uteroplacental unit and augmentation of left ventricular function should be the primary goal.
Cardiomyopathy in the pre-eclamptic patient
A number of case reports describe the antepartum diagnosis of peripartum cardiomyopathy and the management through late pregnancy and labour. There is no significant treatment difference between this and any acute heart failure other than the avoidance of teratogenic drugs pre-delivery. The role for bromocriptine is increasing to ameliorate prolactin-related pathology and should be discussed promptly with local cardiac centres. Mechanical left ventricular support should be employed early as recovery may be slow and can be comorbidity-dependent. As a consequence of the vasoconstriction associated with pre-eclampsia, this subgroup of patients typically presents with the extremes of low ejection fractions resulting from the increased workload placed on an already failing ventricle. However, providing the patient survives the initial period, there is subsequently a rapid improvement in function following delivery once pre-eclampsia starts to resolve as subsidence of the vasoconstriction augments LV recovery making a strong case for pre-emptive delivery.
As large studies are lacking, figures defining overall prognosis are variable and based on small case-series. Approximately half of patients will make a functional recovery back to baseline although show inducible cardiac dysfunction; a quarter of patients will go on to live in a state of pharmacologically managed heart failure but be reasonably asymptomatic; whilst the final quarter develop long-term symptomatic heart failure and may require cardiac transplantation if they survive the initial illness. 9 – 11 It is likely that a lot of milder cases go undiagnosed.
Diagnosing cardiomyopathy in the presence of pre-eclampsia
Pre-eclampsia is associated with poor tolerance of fluid overload and pulmonary oedema is well described. In our patient’s case, the combination of chest sepsis and pre-eclampsia explained her symptoms through the early stages and a hunt for further diagnoses was, not inappropriately, delayed. With retrospect, her deteriorations both occurred following periods of supination, specifically her LSCS and CTPA.
The role of B-natriuretic peptide (BNP) has been suggested as a screening technique and its levels in normal pregnancy should not be significantly elevated (up to twice normal). 12 In the absence of pre-eclampsia, a BNP level of < 100 pg/ml has a negative predictive value of 100%. 13 However, BNP levels rise significantly in pre-eclampsia making its interpretation in the investigation of cardiomyopathy less useful and warrants discussion with cardiologists. 14
The definitive investigation is echocardiography although this may be difficult in this group of patients: the gravid uterus renders transthoracic imaging significantly more uncomfortable for the parturient whilst impairing image quality; a transoesophageal echo is not a low-risk intervention in late pregnancy with high regurgitation and aspiration risk, not to mention difficulties with positioning.
(H)ELLP syndrome
In the critically ill patient, multi-organ failure can involve both the liver and bone marrow. Severe sepsis is a common cause of this. A complication of pre-eclampsia includes HELLP syndrome but this diagnosis needs to be made with consideration to other causes of the involved triad. A review article of HELLP syndrome and its imitators provides a fascinating summary of the similarities and differences between these. 8 Preservation of renal function in our patient counts against sepsis being the cause of the liver dysfunction together with a normal central venous pressure refuting a cardiac component to this. Minimal anaemia may occur in up to a third of HELLP patients (as in our case). The antecedence of the transaminitis in relation to cardiovascular deterioration implies it worsened concomitantly with the pre-eclampsia rather than being a consequence of multi-organ failure.
Combined pathologies
The interaction between the vasoconstriction of pre-eclampsia, the vasodilatation of sepsis and peripartum cardiomyopathy will be unpredictable and dependent on the severity of each component. Ultimately, it will make clinical measurement less reliable in the assessment of each one – leading to a dependence on biochemical and radiological investigations. In our patient, the presence of chest sepsis with pre-eclampsia was considered sufficient explanation for her symptoms until she failed to respond to vasopressors/fluids. BP maintenance through her early illness led to an assumption that her sepsis was mild despite a CRP stubbornly between 100 and 150 mg/dL on antibiotics. Postoperatively, this rose to > 300 mg/dL, but it is not possible to say whether this was related purely to sepsis or to what degree there was post-surgical change involved.
The profound hypertension that she developed in extremis is another confounder that could lead one to discount cardiac failure and sepsis as co-existent pathologies. This may represent the desperate catecholaminergic response to her severe hypoxaemia compounding the decompensation of her impaired LV and further exacerbating her pulmonary oedema. We recognise that reconciling the severe hypertension in the face of a poor LV is subject to conjecture but the final spiral of symptoms occurred over a short space of time and may have represented the last reserves of her physiological capabilities (the documented LVEF of 12% was not until after her cardiac arrest and intubation – by which time, there may have been some superadded myocardial stunning).
With advances in fertility treatment and congenital heart disease survival rates, it is likely that an ever more complex maternal population will present with cardiomyopathy or pre-eclampsia, with or without sepsis. This case emphasises the importance of close liaison between obstetrics and ICU services, as advocated by recent Royal College meetings, and hopefully reminds others of the difficulties encountered when managing patients with opposing pathological processes.
In our case, the hypertension of pre-eclampsia reduced during the induction of labour. Whether this was an improvement of her pre-eclampsia, progression of sepsis or myocardial depression secondary to cardiomyopathy is an irreconcilable academic query. That said, its distinction could have impacted management in so far as improving early care.
Consensus amongst experts is that this patient had a peripartum cardiomyopathy whose LV failure will have been exacerbated by the increased afterload seen in pre-eclampsia. The balance struck between these two pathologies, together with her ongoing sepsis meant that the clinical manifestation was an isolated tachycardia and tachypnoea, without gross haemodynamic compromise until her complete cardiovascular collapse.
The physiological combination of pre-eclampsia and sepsis offset each other clinically leading to a delay in diagnosis. The fallout from these both compounded and was compounded by the presence of undiagnosed peripartum cardiomyopathy.
This patient reflects the most severe of interactions between opposing pathologies. Whilst sequential management of organ failure in all conditions remains supportive, the discrimination between deteriorating pre-eclampsia and worsening sepsis, with or without cardiomyopathy, is an important one to make to guide further management.
- The potential for continuing deterioration of cardiomyopathy in the progressing pregnancy requires consideration of delivery of the foetus and early use of mechanical LV support given the high morbidity and mortality found in severe cardiomyopaths. Where possible, this should be done at a specialist centre.
- Bromocriptine is an emerging potential treatment for peripartum cardiomyopathy.
- Pre-eclampsia exacerbates a failing ventricle but its resolution accelerates symptomatic recovery in peripartum cardiomyopathy.
- The hypotension of severe sepsis may be masked by pre-eclampsia, whereas the hypertension of severe pre-eclampsia may be suppressed in septic shock. This may be compounded by cardiomyopathy.
- Collapsed inferior vena cava (IVC), kissing ventricle in preload depletion;
- Dilated right ventricle (RV); collapsed left ventricle (LV) in pulmonary artery obstruction (either mechanical or physiological);
- Dilated RV and LV with reduced contractility in cardiomyopathy.
- Multidisciplinary management by cardiology, obstetricians and intensive care should be assumed mandatory in the care of these patients outside of tertiary cardiac units and early interhospital liaison should be considered.
Published with generous written consent of the patient.
Declaration of conflicting interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
The author(s) received no financial support for the research, authorship, and/or publication of this article.
- Not an Guest! Login
- Forgot Password

- CASE REPORTS
Wilson’s Disease Diagnosed Postnatally Due to Neurological Manifestation
Pregnancy and its outcome in a rare case of combined protein c and protein s deficiency with severe adenomyosis case, spontaneous ohss in a young adolescent: a diagnostic dilemma, laparoscopic approach for recurrent huge vulval mass, pregnancy in a persistent vegetative state: a management dilemma. case report, literature review and ethical concerns.
Sujata Siwatch 1 • Minakshi Rohilla 1 • Apinderpreet Singh 2 • Chirag Ahuja 3 • Kajal Jain 4 • Vanita Jain 1
A woman who developed a persistent vegetative state in the late first trimester after an arterio-venous fistula (AVF) bleed in the brain presented at 12 weeks period of gestation. The difficult clinical and ethical management issues faced include whether to continue pregnancy, antenatal care and planning for delivery. Multidisciplinary team management along with a family centred approach helped in planning and continuing the pregnancy that resulted in a successful fetal outcome.
Keywords: Pregnancy • Persistent vegetative state • Coma • Ethical issues
Abbreviations:
AV arterio-venous ICH intracranial hemorrhage ECA external carotid artery ICA internal carotid artery MCA middle cerebral artery DSA digital subtraction angiography PVS persistent vegetative state
Inflammatory Myofibroblastic Tumour at Episiotomy Site: A Rare Case Report with Review of Literature
Meenal Bhati 1 • Meenakshi Gothwal 2 • Pratibha Singh 3 • Garima Yadav 2
An inflammatory myofibroblastic tumour (IMT) is a rare mesenchymal neoplasm which was earlier considered under the broad category of inflammatory pseudotumor. It can arise from various anatomic location, out of all lung is the most common site. In our case a 27 years old female presented in our OPD with a mass arising from the episiotomy scar site in the vagina. The histopathological examination showed spindle-shaped cells in fascicles with inflamed granulation tissue with dense mixed inflammation. Immunohistochemistry test showed immunoreactivity for Smooth muscle actin (SMA) and are focally immunoreactive for Bcl2 and Desmin, negative for CK, CD34 and S100 protein. We framed our diagnosis of an inflammatory myofibroblastic tumour of the episiotomy site. However, female genital tract IMT's are rare; to the best of our knowledge, there are no reported cases of IMT involving episiotomy site.
Pancreatitis in Pregnancy: Case Series for 5 Years
Chandrakala Magudapathi 1 • Sudha Shanthi 2 • R. Palanisamy 3
Background To study the course of pancreatitis in pregnant women and demonstrate that early diagnosis and conservative management leads to good maternal and perinatal outcome.
Methods: This article is a retrospective case series study. Six patients with acute pancreatitis during pregnancy were seen in a tertiary referral based obstetric practice at our department in the last 5 years. One of them had gallstones, one hyperlipidemia, one Diabetes and one miliary tuberculosis on ATT . Conservative treatment was instituted for pancreatitis. All of them were followed at least six weeks post-partum.
Results: There was no maternal mortality and perinatal mortality. Acute pancreatitis occurred in both primipara and multipara patients. Preterm labor was a complication in most of our cases complicated by acute pancreatitis. Most patients experienced relief from the pancreatitis soon after delivery. One patient underwent cesarean section due to fetal distress all the other 5 patients had vaginal delivery. One patient had Pseudopancreatic cyst and had a morbid postpartum period.
Conclusion: Pancreatitis is a rare event in pregnancy, approximately 3 in 10,000 pregnancies. It is most often acute and related to gallstones but nonbiliary causes should be sought because they are associated with worse outcomes. Although acute pancreatitis is a rare complication of pregnancy with 50% maternal and 70 % perinatal mortality early and appropriate treatment is of utmost importance to improve the outcome.
Ovarian Follicle: Twirling Microfilaria’s New Abode
Sachin Khanduri 1 · Namrata Nigam 2 · Mazhar Khan 1 · Anvisha Shukla 1 · Ekta Tyagi 1 · Tariq Ahmad Imam 1 · Shobha Khanduri 3
Filariasis is parasitic disease with significant morbidity and socio-economic implications. Its uncommon presentation in female genital organs and rarer presentation in ovarian follicles pose a major diagnostic problem even in endemic regions.As in recent times, there is increase in travel and immigration ,physicians need to be familiar with cases not only endemic to their region but to non endemic diseases as well.Herein ,we report a case of a 26 year old female patient who presented with chronic pelvic pain and polymenorrhoea. Transvaginal ultrasonography revealed microfilariae in ovarian follicular fluid which led to correct diagnosis. This case report sheds light on uncommon presentation of filariasis which needs to be considered for correct diagnosis in endemic as well as non-endemic regions.
Effective Management of Early Cervical Pregnancy with Bilateral Uterine Artery Embolization Followed by Immediate Evacuation and Curettage: A Case Report
Pregnancy in a rare case of intracranial rosai dorfman disease (rdd).
Shashikala Ksheerasagar 1,2 · N. Venkatesh 1 · Niti Raizada 1 · K. M. Prathima 1 · Ravindra B. Kamble 1 · K. Srinivas 1 · M. A. Suzi Jacklin 1 · B. A. Chandramouli 1
We report an extremely rare case of spontaneous pregnancy in a 38 year women following chemotherapy for Rosai-Dorfman Disease (Rosai-dorfman Disease). What made the case more interesting was the challenges that obstetric team faced managing the patient in the presence of co-morbidities like Gestational Diabetes Mellitus , anemia , sub clinical hypothyroidism , allergic bronchitis , progressive symptoms of Rosai-Dorfman Disease like diplopia and cerebellar ataxia
Granulosa Cell Tumor of the Ovary Accompanying with Ollier’s Disease: First Case of Contralateral Presentations
Amirmohsen Jalaeefar 1 · Mohammad Shirkhoda 1 · Amirsina Sharifi 2 · Mohsen Sfandbod 3
Objective: Granulosa cell tumor (GCT) is a rare entity of ovarian malignancies. Juvenile GCT is considered a malignant tumor with an indolent course and tendency toward late recurrence. However, the association of this tumor and multiple enchondromas has been reported.
Case Presentation: A 17-year-old female with abnormal uterine bleeding was referred to our center. Ultrasonographic evaluation revealed a mass with origin in right ovary. Patient was worked up to undergo salpingo-oophorectomy, she felt a dull pain in her left lower limb. X-ray imaging was indicative for Ollier’s disease at the distal part of femur and proximal part of tibia. Postoperative pathological review was compatible with juvenile granulosa tumor of the right ovary.
Conclusion: This case was the first of its kind that ovarian tumor was contralateral to the side involved by enchondromatosis.
Ogilvie Syndrome with Caecal Perforation After Caesarean Section
Osseous metaplasia of the vaginal vault: a case report, heterotopic quadruplet pregnancy after icsi conception.
Background : Heterotopic pregnancy (HP) is a condition characterized by the coexistence of multiple fetuses at two or more implantation sites. It occurs in 1% of pregnancies after assisted reproductive techniques (ART). Presence of triplet intrauterine pregnancy with ectopic gestational sac is one of the rarest forms of HP. Ectopic pregnancy is implanted in the ampullary segment of the fallopian tube in 80% of cases. Most of the patients present with acute abdominal symptoms due to rupture of the tube. Case Presentation This article reports a case of quadruplet heterotopic pregnancy after intracytoplasmic sperm injection (ICSI) with an ampullary ectopic pregnancy and intrauterine triplet pregnancies. The ruptured ampullary pregnancy was emergently managed by right salpingectomy. This was followed by embryo reduction at 12 ? 6 weeks and successful outcome of intrauterine twin pregnancy.
A Rare Case of Adenoma Malignum: Preparing for the Unforeseen
Gayathri Dinesh Kamath 1 • Aditi Bhatt 1 • Veena Ramaswamy 1
Gonadal Vein Graft for Maintaining Renal Circulation After a Complication During Para-Aortic Nodal Dissection: A Case Report
Pesona Grace Lucksom 1 • Jaydip Bhaumik 1 • Gautam Biswas 2 • Sujoy Gupta 3 • Basumita Chakraborti 1
A 39 year old female underwent staging laparotomy for carcinoma endometrium. During para aortic node dissection the left renal vein (LRV) was accidentally injured. The patency of the LRV after rent repair was not adequate for functioning of the left kidney. Nepherectomy was considered but plans for saving the kidney was discussed by the joint team of surgeons. The venous blood of the left kidney was diverted through an anastomosis of the left gonadal vein with the venacava. Patency of the anastomosis was checked and was found to be adequate for keeping the left kidney functional. Doppler of the renal veins done on post-operative day three was normal and she was fit for discharge on day four.

Benign Ovarian Edema Masquerading as Malignancy: A Case Report
Shalini Singh 1 • Kameswari Surampudi 1 • Meenakshi Swain 2
Solid ovarian masses in young age can pose significant diagnostic and therapeutic challenges to the clinician. A young 16 year old girl presented with irregular cycles, pain abdomen and reportedly bulky ovaries with calcifications. Examination was unremarkable. Ultrasound scan revealed bilateral complex ovarian masses suggestive of neoplasm. MRI confirmed a solid right ovarian mass with normal left ovary. Tumour markers were normal. Option of frozen section followed by complete surgery if malignant or two stage procedure including staging laparotomy and if necessary a second surgery were discussed. Parents opted for the latter. At midline laparotomy, free fluid from abdomen was sent for cytology. Right ovary was irregular and enlarged measuring 10 x 8 cm with unruptured white capsule and no torsion. Left ovary was normal. Right salpingo-oophorectomy with omental and peritoneal biopsies were performed. Cytology was benign and histopathology showed massive ovarian edema which was a surprise and relief. Massive ovarian edema is a unique condition with tumour like enlargement of the ovary mimicking neoplasm on imaging leading to overtreatment of patients. Knowledge of this condition allows for fertility sparing procedures.
Maternal Near-Miss: A Perimortem Caesarean Section Resulting in a Remarkable Foetomaternal Recovery in a Rural Tertiary Care Centre in Eastern India
Leiomyoma of urinary bladder in middle-aged female.
Bhushan Dodia 1 • Abhay Mahajan 1 • Dhruti Amlani 1 • Sandeep Bathe 1
Member Login
Your attention is required, important notice.

The case-control study: a primer for the obstetrician-gynecologist
Affiliation.
- 1 Department of Obstetrics and Gynecology, Women & Infants' Hospital, Brown University School of Medicine, Providence, Rhode Island.
- PMID: 8008310
Case-control studies begin at the end. Two groups of patients, those with disease (cases) and those without (controls), are compared to determine the degree of exposure to a presumed risk factor. This research method is commonly used to study rare diseases or diseases that take years to develop. If a higher proportion of cases than controls has the exposure of interest, the exposure may be associated with illness. The strength of this association is measured by an "odds ratio," which is a good proxy for a relative risk when the illness in question is infrequent. Although some case-control studies are easy to do, all are easy to do poorly, especially because of selection bias in the choice of controls. A greater familiarity with the case-control study should enable obstetrician-gynecologists to evaluate critically published studies using this research method.
Publication types
- Case-Control Studies*
- Cohort Studies
- Confounding Factors, Epidemiologic
- Data Interpretation, Statistical
- Gynecology / education*
- Obstetrics / education*
- Reproducibility of Results
- Research / education
- Research Design* / standards
- Risk Factors
- Selection Bias
- Time Factors
- Introduction
- Article Information
A, The increase in VBAC rate by race and ethnicity was largest among Hispanic individuals (5.2%; 95% CI, 4.9%-5.5%), followed by Asian or Pacific Islander (4.7%; 95% CI, 4.1%-5.2%), multiracial (4.3%; 95% CI, 3.4%-5.2%), American Indian or Alaska Native (4.1%; 95% CI, 1.7%-6.7%), White (4.0%; 95% CI, 3.5%-4.5%), and Black (3.0%; 95% CI, 2.5%-3.4%) individuals. B, The largest increase in VBAC rate by geographic region was in the West (6.9%; 95% CI, 6.1% to 7.7%), followed by Midwest (3.6%; 95% CI, 3.0% to 4.2%), South (3.6%; 95% CI, 3.0% to 4.1%), and Northeast (2.9%; 95% CI, 2.4% to 3.3%
APC indicates annual percentage change.
a Some states had not adopted the 2003 revised version of the birth certificate by 2011. The trend in these states was examined from the first year they adopted the 2003 revised version, which is as follows: 2012, Virginia; 2013, Alabama, Maine, and Mississippi; 2014, Alabama, Arizona, Arkansas, Hawaii, and West Virginia; 2015, Rhode Island; and 2016, Connecticut and New Jersey. All other states had adopted the revised version by 2011.
eAppendix. Supplemental Methods
eReferences
Data Sharing Statement
See More About
Sign up for emails based on your interests, select your interests.
Customize your JAMA Network experience by selecting one or more topics from the list below.
- Academic Medicine
- Acid Base, Electrolytes, Fluids
- Allergy and Clinical Immunology
- American Indian or Alaska Natives
- Anesthesiology
- Anticoagulation
- Art and Images in Psychiatry
- Artificial Intelligence
- Assisted Reproduction
- Bleeding and Transfusion
- Caring for the Critically Ill Patient
- Challenges in Clinical Electrocardiography
- Climate and Health
- Climate Change
- Clinical Challenge
- Clinical Decision Support
- Clinical Implications of Basic Neuroscience
- Clinical Pharmacy and Pharmacology
- Complementary and Alternative Medicine
- Consensus Statements
- Coronavirus (COVID-19)
- Critical Care Medicine
- Cultural Competency
- Dental Medicine
- Dermatology
- Diabetes and Endocrinology
- Diagnostic Test Interpretation
- Drug Development
- Electronic Health Records
- Emergency Medicine
- End of Life, Hospice, Palliative Care
- Environmental Health
- Equity, Diversity, and Inclusion
- Facial Plastic Surgery
- Gastroenterology and Hepatology
- Genetics and Genomics
- Genomics and Precision Health
- Global Health
- Guide to Statistics and Methods
- Hair Disorders
- Health Care Delivery Models
- Health Care Economics, Insurance, Payment
- Health Care Quality
- Health Care Reform
- Health Care Safety
- Health Care Workforce
- Health Disparities
- Health Inequities
- Health Policy
- Health Systems Science
- History of Medicine
- Hypertension
- Images in Neurology
- Implementation Science
- Infectious Diseases
- Innovations in Health Care Delivery
- JAMA Infographic
- Law and Medicine
- Leading Change
- Less is More
- LGBTQIA Medicine
- Lifestyle Behaviors
- Medical Coding
- Medical Devices and Equipment
- Medical Education
- Medical Education and Training
- Medical Journals and Publishing
- Mobile Health and Telemedicine
- Narrative Medicine
- Neuroscience and Psychiatry
- Notable Notes
- Nutrition, Obesity, Exercise
- Obstetrics and Gynecology
- Occupational Health
- Ophthalmology
- Orthopedics
- Otolaryngology
- Pain Medicine
- Palliative Care
- Pathology and Laboratory Medicine
- Patient Care
- Patient Information
- Performance Improvement
- Performance Measures
- Perioperative Care and Consultation
- Pharmacoeconomics
- Pharmacoepidemiology
- Pharmacogenetics
- Pharmacy and Clinical Pharmacology
- Physical Medicine and Rehabilitation
- Physical Therapy
- Physician Leadership
- Population Health
- Primary Care
- Professional Well-being
- Professionalism
- Psychiatry and Behavioral Health
- Public Health
- Pulmonary Medicine
- Regulatory Agencies
- Reproductive Health
- Research, Methods, Statistics
- Resuscitation
- Rheumatology
- Risk Management
- Scientific Discovery and the Future of Medicine
- Shared Decision Making and Communication
- Sleep Medicine
- Sports Medicine
- Stem Cell Transplantation
- Substance Use and Addiction Medicine
- Surgical Innovation
- Surgical Pearls
- Teachable Moment
- Technology and Finance
- The Art of JAMA
- The Arts and Medicine
- The Rational Clinical Examination
- Tobacco and e-Cigarettes
- Translational Medicine
- Trauma and Injury
- Treatment Adherence
- Ultrasonography
- Users' Guide to the Medical Literature
- Vaccination
- Venous Thromboembolism
- Veterans Health
- Women's Health
- Workflow and Process
- Wound Care, Infection, Healing
Get the latest research based on your areas of interest.
Others also liked.
- Download PDF
- X Facebook More LinkedIn
Chehab RF , Ferrara A , Grobman WA, et al. Racial, Ethnic, and Geographic Differences in Vaginal Birth After Cesarean Delivery in the US, 2011-2021. JAMA Netw Open. 2024;7(5):e2412100. doi:10.1001/jamanetworkopen.2024.12100
Manage citations:
© 2024
- Permissions
Racial, Ethnic, and Geographic Differences in Vaginal Birth After Cesarean Delivery in the US, 2011-2021
- 1 Division of Research, Kaiser Permanente Northern California, Oakland
- 2 Division of Maternal-Fetal Medicine, Department of Obstetrics and Gynecology, The Ohio State University College of Medicine, Columbus
- 3 Department of Obstetrics and Gynecology, Kaiser Permanente Northern California, Oakland
- 4 Regional Perinatal Service Center, Kaiser Permanente Northern California, Santa Clara
- 5 Department of Epidemiology and Biostatistics, University of California, San Francisco
Cesarean delivery rates are higher in the US than in other high-income countries. 1 Vaginal birth after cesarean (VBAC) is associated with reduced risk of maternal morbidity and future pregnancy complications vs cesarean delivery. 2 The VBAC rate increased in the US from 10.7% in 2010 to 16.2% in 2020, 3 but it is unknown whether racial, ethnic, and geographic differences exist. We assessed trends in VBAC rate by race, ethnicity, and geographic region in the US from 2011 to 2021.
This was a repeated cross-sectional analysis of data, captured by the National Center for Health Statistics, of singleton deliveries in the US from 2011 to 2021 among individuals aged 15 to 44 years with a history of cesarean delivery. Race and ethnicity, recognized as social constructs, were self-reported by pregnant individuals. We classified states of birth into the 4 US Census Bureau regions.
We estimated age-standardized VBAC rate with 95% CIs and quantified trends from 2011 to 2021 using annual percentage change (APC) by Joinpoint Regression. Kaiser Foundation Research Institute’s institutional review board deemed this study exempt. Technical details are available in the eAppendix in Supplement 1 .
Among 5 841 858 individuals, the mean (SD) age at delivery was 30.7 (5.3) years, with 57 487 (1.0%) American Indian or Alaska Native, 369 544 (6.3%) Asian or Pacific Islander, 926 332 (15.9%) Black, 1 496 958 (25.6%) Hispanic, 2 860 802 (49.0%) White, and 130 735 (2.2%) multiracial individuals. The overall age-standardized VBAC rate increased from 10.0% (95% CI, 9.9%-10.1%) in 2011 to 14.7% (95% CI, 14.6%-14.9%) in 2021 (APC, 3.9%; 95% CI, 3.3%-4.4%).
Trends by race and ethnicity are shown in Figure 1 A. Trends by geographic region are shown in Figure 1 B. Most states had increases in VBAC rate, with the largest increase in California (11.1%; 95% CI, 10.0% to 12.2%), whereas 2 states, Hawaii (−3.6%; 95% CI, −7.1% to 0.1%) and Rhode Island (−2.8%; 95% CI, −8.6% to 3.4%), had decreases, although the results were not statistically significant ( Figure 2 ).
Using US nationally representative data, in this cross-sectional study we report a nearly 50% increase in VBAC rate from 2011 to 2021, with lingering racial, ethnic, and geographic differences in absolute rate and APC. Black individuals had the smallest and Hispanic individuals had the largest increase in VBAC rate from 2011 to 2021, with both groups having lower VBAC rates than the overall population in recent years. It is critical to monitor race- and ethnicity-specific VBAC rates to expose maternal health inequities while acknowledging that race and ethnicity are not risk factors per se but proxies for root causes of health disparities such as structural racism. 4
The South maintained the lowest VBAC rate from 2011 to 2021 despite having an APC similar to the Midwest. The West, on the other hand, had a VBAC rate similar to the South in 2011 but had the largest APC and reached a rate similar to the Midwest and Northeast in 2021. Geographic differences in VBAC rate may be associated with contextual factors, including health care access and availability and training of obstetric care practitioners. 5
Study limitations include that VBAC rate calculations before 2016 might be affected by the exclusion of birth certificates that did not use the 2003 revised version; nevertheless, a sensitivity analysis of deliveries from 2016 to 2021 yielded results similar to the main analysis. Furthermore, misclassification in birth certificate reporting is possible, but mode of delivery in the birth certificates has been previously validated. 6
Our findings reflect lingering racial, ethnic, and geographic differences in VBAC rates, highlighting the need for person-centered clinical counseling and management of pregnant individuals with a history of cesarean delivery and public health efforts to promote health equity. Future research is warranted to better understand the root causes of these differences to inform targeted strategies toward more equitable maternal health care.
Accepted for Publication: March 18, 2024.
Published: May 17, 2024. doi:10.1001/jamanetworkopen.2024.12100
Open Access: This is an open access article distributed under the terms of the CC-BY License . © 2024 Chehab RF et al. JAMA Network Open .
Corresponding Author: Yeyi Zhu, PhD, Division of Research, Kaiser Permanente Northern California, 2000 Broadway, Oakland, CA 94612 ( [email protected] ).
Author Contributions: Drs Chehab and Zhu had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Concept and design: Chehab, Ferrara, Zhu.
Acquisition, analysis, or interpretation of data: Chehab, Grobman, Greenberg, Ngo, Wang, Zhu.
Drafting of the manuscript: Chehab, Greenberg.
Critical review of the manuscript for important intellectual content: All authors.
Statistical analysis: Chehab, Ngo.
Obtained funding: Chehab, Zhu.
Administrative, technical, or material support: Chehab, Wang, Zhu.
Supervision: Chehab, Zhu.
Conflict of Interest Disclosures: None reported.
Funding/Support: This study was supported in part by grants from The Permanente Medical Group Delivery Science Fellowship and the National Heart, Lung, and Blood Institute (R01HL157666).
Role of the Funder/Sponsor: The funders had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Data Sharing Statement: See Supplement 2 .
- Register for email alerts with links to free full-text articles
- Access PDFs of free articles
- Manage your interests
- Save searches and receive search alerts
Occult endometrial cancer in women undergoing hysterectomy for benign indications: a retrospective cohort study in a tertiary hospital in China
- Gynecologic Oncology
- Published: 10 May 2024
Cite this article

- Yang Cao 1 ,
- Honghui Shi ORCID: orcid.org/0000-0003-3908-1322 1 &
- Xiuping Zhuo 1
35 Accesses
Explore all metrics
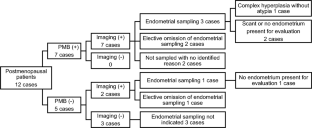
To evaluate the feasibility of further reducing the incidence of occult endometrial cancer in women undergoing hysterectomy for benign gynecological indications.
Patients who underwent hysterectomies for presumed benign gynecologic conditions at Peking Union Medical College Hospital were retrospectively identified. Patients with occult endometrial cancer, which was defined as endometrial cancer diagnosed on postoperative histopathology with no preoperative confirmed malignancy, were selected.
24/7558 (0.32%; 95% CI 0.20–0.47%) patients undergoing hysterectomy for benign indications had occult endometrial cancer. Asymptomatic patients with normal endometrial imaging all tended to have favorable pathology. Heavy menstrual bleeding was the most overlooked AUB pattern in the premenopausal group. In the postmenopausal group, all the patients with serous adenocarcinoma or G3 endometrioid adenocarcinoma histology/stage T1b disease/LVSI space invasion had a history of persistent or recurrent PMB ≥ 6 months and/or an intracavitary lesion > 20 mm in diameter. 3/4 of the samples of the postmenopausal patients did not have adequate endometrium for evaluation.
To further reduce the incidence of occult endometrial cancer, physicians should focus on the patient’s bleeding pattern and actively implement endometrial sampling whenever indicated. Transvaginal ultrasonography is a valuable preoperative evaluation. Hysteroscopy with directed biopsy is the preferred procedure in postmenopausal patients.
This is a preview of subscription content, log in via an institution to check access.
Access this article
Price includes VAT (Russian Federation)
Instant access to the full article PDF.
Rent this article via DeepDyve
Institutional subscriptions
Similar content being viewed by others

Endometrial Cancer

Clinical significance of endometrial abnormalities: an observational study on 1020 women undergoing hysteroscopic surgery
Carcinoma of the Endometrium Surveillance Counterpoint: Japan
Data availability.
All available data are presented in this paper.
American College of, O. and Gynecologists, (2005) ACOG practice bulletin clinical management guidelines for obstetrician gynecologists, number 65, august 2005: management of endometrial cancer. Obstet Gynecol. https://doi.org/10.1097/00006250-200508000-00050
Article Google Scholar
Kimura T et al (2004) Abnormal uterine bleeding and prognosis of endometrial cancer. Int J Gynaecol Obstet 85(2):145–150. https://doi.org/10.1016/j.ijgo.2003.12.001
Article CAS PubMed Google Scholar
Seebacher V et al (2009) The presence of postmenopausal bleeding as prognostic parameter in patients with endometrial cancer: a retrospective multi-center study. BMC Cancer 9:460. https://doi.org/10.1186/1471-2407-9-460
Article PubMed PubMed Central Google Scholar
Tsakiridis I, Giouleka S, Koutsouki G, Kostakis N, Kalogiannidis I, Kourtis A, Athanasiadis A, Goulis DG, Dagklis T (2022) Investigation and management of abnormal uterine bleeding in reproductive-aged women: a descriptive review of national and international recommendations. Eur J Contracept Reprod Health Care 27(6):504–517. https://doi.org/10.1080/13625187.2022.2112169
Article PubMed Google Scholar
Papakonstantinou E, Adonakis G (2022) Management of pre-, peri-, and post-menopausal abnormal uterine bleeding: when to perform endometrial sampling? Int J Gynaecol Obstet 158(2):252–259. https://doi.org/10.1002/ijgo.13988
Vitale SG, Buzzaccarini G, Riemma G, Pacheco LA, Di Spiezio SA, Carugno J, Chiantera V, Török P, Noventa M, Haimovich S, De Franciscis P, Perez-Medina T, Angioni S, Laganà AS (2023) Endometrial biopsy: indications, techniques and recommendations. an evidence-based guideline for clinical practice. J Gynecol Obstet Hum Reprod 52(6):102588. https://doi.org/10.1016/j.jogoh.2023.102588
Brun JL, Plu-Bureau G, Huchon C, Ah-Kit X, Barral M, Chauvet P, Cornelis F, Cortet M, Crochet P, Delporte V, Dubernard G, Giraudet G, Gosset A, Graesslin O, Hugon-Rodin J, Lecointre L, Legendre G, Maitrot-Mantelet L, Marcellin L, Miquel L, Le Mitouard M, Proust C, Roquette A, Rousset P, Sangnier E, Sapoval M, Thubert T, Torre A, Trémollières F, Vernhet-Kovacsik H, Vidal F, Marret H (2023) Management of women with abnormal uterine bleeding: clinical practice guidelines of the French National College of Gynaecologists and Obstetricians (CNGOF). Eur J Obstet Gynecol Reprod Biol 288:90–107. https://doi.org/10.1016/j.ejogrb.2023.07.001
Committee on Practice Bulletins—Gynecology (2012) Practice bulletin no: diagnosis of abnormal uterine bleeding in reproductive-aged women. Obstet Gynecol 120:197–206. https://doi.org/10.1097/AOG.0b013e318262e320
National Collaborating Centre for Women’s and Children’s Health (2007) Heavy Menstrual Bleeding. RCOG Press, London
Google Scholar
Exceptional Surveillance of Heavy Menstrual Bleeding (2021) assessment and management (NICE guideline NG88) [Internet]. National Institute for Health and Care Excellence (NICE), London
Munro MG, Critchley HOD, Fraser IS, Menstrual Disorders Committee FIGO (2018) The two FIGO systems for normal and abnormal uterine bleeding symptoms and classification of causes of abnormal uterine bleeding in the reproductive years: 2018 revisions. Int J Gynaecol Obstet 143(3):393–408. https://doi.org/10.1002/ijgo.12666
Farquhar CM, Lethaby A, Sowter M, Verry J, Baranyai J (1999) An evaluation of risk factors for endometrial hyperplasia in premenopausal women with abnormal menstrual bleeding. Am J Obstet Gynecol 181(3):525–529. https://doi.org/10.1016/s0002-9378(99)70487-4
Ash SJ, Farrell SA, Flowerdew G (1996) Endometrial biopsy in DUB. J Reprod Med 41(12):892–896
CAS PubMed Google Scholar
Farquhar CM (1999) An evidence-based guideline for the management of heavy menstrual bleeding. N Z Med J 112:174–177
MacGregor R, Jain V, Hillman S, Lumsden MA (2022) Investigating abnormal uterine bleeding in reproductive aged women. BMJ 16(378):e070906. https://doi.org/10.1136/bmj-2022-070906
Smith-Bindman R et al (1998) Endovaginal ultrasound to exclude endometrial cancer and other endometrial abnormalities. JAMA 280(17):1510–1517. https://doi.org/10.1001/jama.280.17.1510
Trimble CL et al (2006) Concurrent endometrial carcinoma in women with a biopsy diagnosis of atypical endometrial hyperplasia: a gynecologic oncology group study. Cancer 106(4):812–819. https://doi.org/10.1002/cncr.21650
Theben JU et al (2013) Unexpected malignancies after laparoscopic-assisted supracervical hysterectomies (LASH): an analysis of 1584 LASH cases. Arch Gynecol Obstet 287(3):455–462. https://doi.org/10.1007/s00404-012-2559-0
Mahnert N et al (2015) Unexpected gynecologic malignancy diagnosed after hysterectomy performed for benign indications. Obstet Gynecol 125(2):397–405. https://doi.org/10.1097/AOG.0000000000000642
Takamizawa S et al (1999) Risk of complications and uterine malignancies in women undergoing hysterectomy for presumed benign leiomyomas. Gynecol Obstet Invest 48(3):193–196. https://doi.org/10.1159/000010172
Frick AC et al (2010) Risk of unanticipated abnormal gynecologic pathology at the time of hysterectomy for uterovaginal prolapse. Am J Obstet Gynecol 202:507. https://doi.org/10.1016/j.ajog.2010.01.077
Ramm O et al (2012) Utility of preoperative endometrial assessment in asymptomatic women undergoing hysterectomy for pelvic floor dysfunction. Int Urogynecol J 23(7):913–917. https://doi.org/10.1007/s00192-012-1694-2
Soliman PT, Oh JC, Schmeler KM, Sun CC, Slomovitz BM, Gershenson DM, Burke TW, Lu KH (2005) Risk factors for young premenopausal women with endometrial cancer. Obstet Gynecol 105(3):575–580. https://doi.org/10.1097/01.AOG.0000154151.14516.f7
Pennant ME, Mehta R, Moody P, Hackett G, Prentice A, Sharp SJ, Lakshman R (2017) Premenopausal abnormal uterine bleeding and risk of endometrial cancer. BJOG 124(3):404–411. https://doi.org/10.1111/1471-0528.14385
Parsons LHP, Pedersen R, Richardson DL, Kho KA (2018) The prevalence of occult endometrial cancer in women undergoing hysterectomy for benign indications. Eur J Obstet Gynecol Reprod Biol 223:108–112. https://doi.org/10.1016/j.ejogrb.2018.02.017
Wagner P, Kommoss FKF, Kommoss S, Hartkopf AD, Pasternak I, Oberlechner E, Greif K, Wallwiener M, Neis F, Abele H, Krämer B, Reisenauer C, Staebler A, Wallwiener D, Brucker SY, Taran FA (2019) Unexpected malignant uterine pathology: Incidence, characteristics and outcome in a large single-center series of hysterectomies for presumed benign uterine disease. Gynecol Oncol 153(1):49–54. https://doi.org/10.1016/j.ygyno.2018.12.026
Download references
This work was supported by a grant from National High Level Hospital Clinical Research Funding (2022-PUMCH-C-031).
Author information
Authors and affiliations.
Department of Obstetrics and Gynecology, National Clinical Research Center for Obstetric and Gynecologic Disease, Peking Union Medical College (PUMC) Hospital, Chinese Academy of Medical Sciences and Peking Union Medical College, No.1 Shuaifuyuan Wangfujing, Dongcheng District, Beijing, 100730, People’s Republic of China
Yang Cao, Honghui Shi & Xiuping Zhuo
You can also search for this author in PubMed Google Scholar
Contributions
HHS and YC contributed to the study conception and design. Material preparation, data collection and analysis were performed by YC and XPZ. The first draft of the manuscript was written by YC and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Honghui Shi .
Ethics declarations
Conflict of interest.
The authors have no relevant financial or non-financial interests to disclose.
Ethics approval
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Ethics Committee of Peking Union Medical College Hospital (reference no: I-22PJ848).
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
Reprints and permissions
About this article
Cao, Y., Shi, H. & Zhuo, X. Occult endometrial cancer in women undergoing hysterectomy for benign indications: a retrospective cohort study in a tertiary hospital in China. Arch Gynecol Obstet (2024). https://doi.org/10.1007/s00404-024-07532-z
Download citation
Received : 11 December 2023
Accepted : 24 April 2024
Published : 10 May 2024
DOI : https://doi.org/10.1007/s00404-024-07532-z
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Postmenopausal bleeding
- Abnormal uterine bleeding
- Transvaginal ultrasonography
- Hysteroscopy
- Find a journal
- Publish with us
- Track your research

COMMENTS
Obstetrics and gynaecology. Showing results 1 - 10 of 100. Sorted by most recent. Title Author Date Achalasia in pregnancy. Zafirah Akmal Azahar, Mohd Fadliyazid Ab Rahim, Nasriah Ahmad, Roziana Ramli. 14 May 2024. Placental mesenchymal disease masquerading as molar pregnancy with a favourable maternal and fetal outcome.
Maternal outcomes in pregnancies affected by varicella zoster virus infections: population-based study on 7.7million pregnancy admissions. J Obstet Gynaecol Res 2015;41:62-68. Crossref
Case Study: Obstetrics and Gynecology. Embolization to Treat Uterine Fibroids with Bleeding and Severe Anemia. A 45-year old female Jehovah's Witness patient with a history of uterine fibroids and severe menorrhagia presented with shortness of breath, fatigue and weakness. She also had a history of deep venous thrombosis (DVT) and pulmonary ...
1. Obstetrics-Case studies. 2. Gynecology-Case studies. 3. Women-Health and hygiene. L Howat, Pant II. Title. (Series; Clinical cases in emergency medicine). 618 Published in Australia by M~Graw~Hm Australia Pty Ltd Level 2, 82 Waterloo Road, North Ryde NSW 2113 Publishing Manager: Jo Munnelly Acquisitions Editor: Nicole Mech~n
Journal profile. Case Reports in Obstetrics and Gynecology publishes case reports and case series related to obstetrics, maternal-fetal medicine, gynecology, gynecologic oncology, uro-gynecology, reproductive medicine, infertility, and reproductive endocrinology. About this journal.
This study aimed to present a case of first-trimester uterine rupture and perform a systematic review to identify common presentations, risk factors, and management strategies. First-trimester uterine rupture: a case report and systematic review of the literature - American Journal of Obstetrics & Gynecology
American Journal of Obstetrics & Gynecology Vol. 230 Issue 5 p540.e1 Original Research Gynecology Open Access A 52-mg levonorgestrel-releasing intrauterine system vs bipolar radiofrequency nonresectoscopic endometrial ablation in women with heavy menstrual bleeding: long-term follow-up of a multicenter randomized controlled trial
Case Rep Obstet Gynecol; Case Reports in Obstetrics and Gynecology Vols. 2011 to 2024; 2011 to 2024 ... 2017: v.2018 2018: v.2019 2019: v.2020 2020: 2011 to 2015: v.2011 2011: v.2012 2012: v.2013 2013: v.2014 2014: v.2015 2015: Articles from Case Reports in Obstetrics and Gynecology are provided here courtesy of Hindawi Limited. Follow NCBI ...
Obstetrics & Gynecology is the official publication of the American College of Obstetricians and Gynecologists (ACOG). Popularly known as "The Green Journal," Obstetrics & Gynecology has been published since 1953. Then as is now, the goal of the journal is to promote excellence in the clinical practice of obstetrics and gynecology and closely related fields.
Ultrasound in Obstetrics & Gynecology (UOG), the official journal of the International Society of Ultrasound in Obstetrics and Gynecology (ISUOG), is the leading international peer-reviewed journal in the field.UOG features the latest, most clinically relevant research, including guidelines, consensus statements, expert commentaries, original articles and systematic reviews.
Sharing Clinical Knowledge on Women's Health First IF expected June 2024 ! An official Journal of the European Menopause and Andropause Society (EMAS). Case Reports in Women's Health publishes open access case reports covering all aspects of women's health. The scope reflects the comprehensive nature of women's health and includes not only the core areas of reproductive and postreproductive ...
Professor, Department of Obstetrics and Gynecology, Division of Maternal-Fetal Medicine, Wayne State University/Hutzel Women's Hospital, Detroit, MI, USA Robert H. Ball MD Associate Professor, Department of Obstetrics, Gynecology, and Reproductive Sciences and Radiology, UCSF Fetal Treatment Center, San Francisco, CA, USA Frederick C ...
The October 2023 issue of Obstetrics & Gynecology will be dedicated exclusively to issues of racism and reproductive health and tangible steps that we can take to pave the path to health equity. The call for papers is available at https://bit.ly/3wKXvHg . On October 25, we hosted a webinar to engage potential authors and reviewers, and to ...
Case Files Obstetrics and Gynecology, 6e by Eugene C. Toy; Patti Jayne Ross; Benton Baker; ... Williams Obstetrics Study Guide, 25e by Shivani Patel. Publication Date: 2019. Helpful Review Links. Obstetrics & Gynecology Subject Guide. Created and curated by the Maguire Medical Library.
is uncertain and the vast majority are benign. In this specific case all the differential diag-noses are effectively excluded by the history and examination. 100 Cases in Obstetrics and Gynaecology 2 • Cervical malignancy • Cervical ectropion • Endocervical polyp • Atrophic vaginitis • Pregnancy • Irregular bleeding related to the ...
Uterine torsion is rare in pregnancy and the cause in most cases is unknown. It is associated with fetal compromise, with perinatal mortality reported to be around 12%. Our case describes an acute torsion, presenting in pregnancy with severe abdominal pain and vomiting with a viable 32-week gestation. Emergency caesarean section was performed ...
As large studies are lacking, figures defining overall prognosis are variable and based on small case-series. ... cardiomyopathy or pre-eclampsia, with or without sepsis. This case emphasises the importance of close liaison between obstetrics and ICU services, as advocated by recent Royal College meetings, and hopefully reminds others of the ...
Abstract . BackgroundTo study the course of pancreatitis in pregnant women and demonstrate that early diagnosis and conservative management leads to good maternal and perinatal outcome.. Methods:This article is a retrospective case series study.Six patients with acute pancreatitis during pregnancy were seen in a tertiary referral based obstetric practice at our department in the last 5 years.
Ultrasound in Obstetrics & Gynecology. The UOG 30th anniversary Special Issue in January 2021 is completely free to access and features Opinions and high-impact research papers from leaders in the field of obstetrics and gynecology, which highlight the breadth of topics in which ultrasound plays an instrumental or supporting role. The series of ...
Obstetrics & Gynecology: June 9, 2022 - Volume - Issue - 10.1097/AOG.0000000000004839. doi: 10.1097/AOG.0000000000004839. Open. PAP. Metrics. Abstract. In Brief. As restrictions on abortion increase nationwide, it is critical to ensure ongoing access to abortion care throughout pregnancy. People may seek abortions later in pregnancy as a result ...
There are more than 79 existing FIGO (International Federation of Gynecology and Obstetrics) ethics and professionalism guidelines in a volume which is updated every few years by the committee. The committee also has a bioethical curriculum suitable for practicing gynecologists as well as students and teachers.
current issue. current issue; browse recently published; browse full issue index; learning/cme
Case-control studies begin at the end. Two groups of patients, those with disease (cases) and those without (controls), are compared to determine the degree of exposure to a presumed risk factor. ... 1 Department of Obstetrics and Gynecology, Women & Infants' Hospital, Brown University School of Medicine, Providence, Rhode Island. PMID: 8008310
This cross-sectional study examines racial, ethnic, and geographic differences in vaginal birth after cesarean delivery in the US, from 2011 to 2021. ... Department of Obstetrics and Gynecology, The Ohio State University College of Medicine, Columbus. 3 Department of Obstetrics and Gynecology, ...
MG patients experience fluctuating muscle weakness, mainly in the muscles of the eyes, limbs, face, and breathing. 1 Although this disease is rare, with a reported prevalence in the general population of 0.3-7.7 per 100,000 people, its prevalence is increasing in women aged between 20 and 30, which may have implications for pregnancy. 2 The ...
Background The aim of this study is to investigate whether planned caesarean delivery compared to planned induction of labour in women with severe pre-eclampsia at gestational age of more than 37 weeks of pregnancy will reduce maternal morbidity and/or perinatal morbidity. Method This randomized controlled study was conducted from April 2021 to March 2022 at Department of Obstetrics and ...
Popularly known as "The Green Journal," Obstetrics & Gynecology has been published since 1953. ... A Qualitative Study of Transgender and Nonbinary Perspectives Regarding the Desired Properties of a Peer Support Intervention for the Initiation of Gender-Affirming Hormone Therapy [ID 2683451] ... Case Series: Medical Versus Surgical Management ...
Department of Obstetrics and Gynecology, School of Medicine, University of Occupational and Environmental Health, Japan, Fukuoka, Japan. ... Using a Japanese administrative database, our study shows that hospital case volume was not significantly associated with the severity of maternal illness among patients with PA.
(a) Study Design A randomized controlled trial was used in this study. (b) Study Duration The study duration was 18 months. (c) Sampling technique Simple random sample was used in this study. (d) Study site Department of obstetrics and gynaecology, JSS HOSPITAL, Mysuru. (e) Sample size In the study done by Topsoee M F et al. [], the percentage of study subjects who had total blood loss of more ...
In a study enrolled 708 women undergoing hysterectomy for POP and/or urinary incontinence, five cases of endometrial cancer (0.6%) were detected; four of these women had normal preoperative screening, including endometrial biopsy (2 cases), TVUS (1case), or both tests (1 case) . Considering the low prevalence, the low efficiency of screening ...