

PhD Program in Law and Psychology
Application fee waivers.
We are now offering a PhD application fee waiver program. Click here for information or to apply!
Ph.D. Program in Law and Psychology
Select Section
About the Ph.D. Program
Our program is designed to train a new generation of scholars in the field of Law and Psychology by taking a broad interdisciplinary approach that combines rigorous training in the Law and Psychology field along with advanced training in psychological science, research methodology, statistics, criminological theory, and legal theory. Our goal is for our students to use this training to tackle the many important but understudied areas where legal policy is in desperate need of empirical, psychological research. We have created this program for individuals looking for a career in academic research, trial consulting, and/or applied legal policy research. Note that this is not a clinical training program and our graduates are not license-eligible.
Graduate students in this degree program have a set of required and recommended courses:
Statistics & Methods Core: Quantitative Analysis I (ANOVA), Quantitative Analysis II (Regression), Quantitative Analysis III (Multivariate Analysis), Experimental Research Methods
Substantive Core: Advanced Legal Psychology, Advanced Forensic Psychology, Advanced Social Psychology
In addition, students will choose electives based on their desired area of specialization, including (but not limited to):
Basic psychology courses (e.g., Developmental Psychology, Psychopathology, Cognitive Science)
Advanced statistical courses (e.g., SEM, Bayesian Analysis, Data Visualization, Big Data)
Psychology & Law courses (e.g., Advanced Correctional Psychology; Children and the Legal System; Mental Health and the Law; Neuroscience of Crime; Law, Litigation, and Science)
Criminology courses (e.g., Seminar in Criminological Theory; Advanced Topics in Corrections; Advanced Topics in Courts and Sentencing; Advanced Topics in Juvenile Justice; Advanced Topics in Crime and Victimization).
In total, students will complete 84 credit hours (54 credits of coursework plus 30 credits of research), a masters thesis, a comprehensive exam, and a dissertation.
Tuition and Financial Aid
Like most similar programs, the PhD in Law and Psychology seeks to fully fund its students. ASU policy does not allow us to “guarantee” funding, but students are only admitted if we expect to have adequate funding to support them for 4-5 years. Funding may come in the form of a Teaching or Research assistantship, which involves 20 hours per week of responsibilities. The average amount of support for a 20-hour TA/RA academic year position at in our program is a $28,000-$30,000 stipend, health insurance, and full tuition remission. Summer funding is available (typically $8,000-$10,000), but is not guaranteed. In addition to TA/RA positions, ASU offers a number of internal fellowships and grants, and we automatically consider each of our admitted students for these funds.
Joint Degrees (e.g., JD/PhD)
At this time we do not offer a formal joint degree option. Students wishing to obtain a JD/PhD would need to independently apply to and be accepted into our PhD program and the JD program at the Sandra Day O'Connor College of Law. Note that TA/RA tuition remission does not cover law school tuition.
For More Information
Still have questions? Read our list of Frequently Asked Questions or contact Jessica Salerno, program director, at [email protected] .
- JD/PhD Psychology
The JD/PhD Program is an in-depth, cross disciplinary path designed to expose lawyers and psychologists to the growing number of issues that involve both fields, such as competence, mental illness, and incapacity, and the field of behavioral law and economics.
- Degree Requirements
- JD/MBA (4 Year)
- JD/MBE Bioethics
- JD/MSSP Social Policy
- JD/MS Nonprofit Leadership
- JD/MSEd Education Policy
- JD/MSEd Higher Education
- JD/MA or MS Criminology
- JD/MD Doctor of Medicine
- JD/MSE Engineering
- JD/MCP City & Regional Planning
- JD/MPH Master of Public Health
- JD/AM Islamic Studies
- JD/PhD Legal Studies and Business Ethics
- JD/MA and JD/PhD Philosophy
- JD/PhD Anthropology
- JD/PhD Communications
- Certificates
- Legal Practice Skills
- Clinics & Externships
- Academic Support Program
- International Affairs
- Future of the Profession Initiative
- Legal Education Programs
- Executive Education
- Academic Calendar
- Learning Outcomes
- Advocacy Competitions
Program Course Overview
Financial aid.
Once admitted to both programs independently, students will be able to seek each school’s relevant financial support. Students can pay for Law School with standard methods like assets, loans, and need-based financial assistance (if qualified). The PhD program may provide tuition, fees, stipends, and health insurance support according to the Department’s requirements.
How to Apply
Students should apply contemporaneously for admission to both the Department of Psychology and the Law School, noting on both that they have applied to the other. There may be a rare case when a student who has been accepted into the PhD program may, in the first year of that course of study, apply for admission to the Law School and to the Dual Degree Program.
For more information, admitted or current JD students should contact Amanda S. Aronoff. Applicants or prospective applicants to the Law School should contact [email protected] .
Interested in other Phd joint degrees?
JD/Phd American Legal History
JD/PhD Philosophy

Health Law and Policy
Over one dollar in six in the US economy is spent on health care, and the need for wise public and organizational policy decisions to control costs, to improve quality, and to increase access has never been greater. In the public health arena, the nation confronts a rising tide of noncommunicable disease, resurgent threats of infectious disease, and other problems that will demand legal and policy interventions. Stanford Law School is second to none as a training ground for tomorrow’s leaders in health law and policy. Four renowned Law School faculty members offer courses in health care law, public health law, and bioethics and advise students interested in careers in the field. Courses in mental health law, food and drug law, mass tort litigation, environmental law, policy analysis skills, and other critical areas help expand students’ intellectual toolkit. Joint degree programs with the Stanford University School of Medicine, the ability to cross-register for health-related courses taught in other Stanford professional schools and departments, and research opportunities through Stanford’s health-focused research institutes round out the experience.
Faculty on Point

Core Health Law Faculty
Henry T. Greely
- Deane F. and Kate Edelman Johnson Professor of Law
- Director, Center for Law and the Biosciences
- Professor, by courtesy, Genetics
- Chair, Steering Committee of the Center for Biomedical Ethics
- Director, Stanford Program in Neuroscience and Society
Daniel P. Kessler
- Professor of Law
- Keith and Jan Hurlbut Senior Fellow, Hoover Institution

Michelle M. Mello
- Professor of Health Policy

David M. Studdert
- Vice Provost and Dean of Research
More Teaching and Advising Faculty

Mariano-Florentino Cuéllar
- Visiting Scholar

John J. Donohue III
- C. Wendell and Edith M. Carlsmith Professor of Law

Nora Freeman Engstrom
- Ernest W. McFarland Professor of Law
- Co-Director, Deborah L. Rhode Center on the Legal Profession

Deborah Hensler
- Judge John W. Ford Professor of Dispute Resolution

Daniel E. Ho
- William Benjamin Scott and Luna M. Scott Professor of Law
- Professor of Political Science
- Professor of Computer Science (by courtesy)
- Senior Fellow, Stanford Institute for Human-Centered Artificial Intelligence (HAI)
- Senior Fellow, Stanford Institute for Economic and Policy Research
- Director of the Regulation, Evaluation, and Governance Lab (RegLab)

Robert J. MacCoun
- James and Patricia Kowal Professor of Law
- Senior Fellow at the Freeman Spogli Institute for International Studies

Lisa Larrimore Ouellette
- Deane F. Johnson Professor of Law
- Senior Fellow, Stanford Institute for Economic Policy Research (SIEPR)
Robert L. Rabin
- A. Calder Mackay Professor of Law
Faculty Research Projects
Hank Greely has been publishing widely on the issues raised by human germline genome editing and He Jiankui’s “CRISPR’d babies.” Hank Greely has worked on various issues around “human brain surrogates,” from human/non-human brain chimeras, to human neural organoids, to partial or whole human brains kept “alive” outside the body. Hank Greely is writing a book called “Playing With Life” about who advances in the biosciences are, in effect, letting humans change living organisms in ways and to extents never before imagined…and exploring what kind of world(s) we may end up with.
Daniel Kessler is investigating how choice of organizational form by physicians (for example, solo versus group practice), and integration between physicians and hospitals, affect competition and the cost and quality of care. Daniel Kessler is studying how different types of prescription drug insurance affect opioid prescribing behavior by physicians.

Michelle Mello is exploring approaches to governing health care artificial intelligence and regulating high-priced prescription drugs, issues in vaccination policy, and lessons learned about emergency health powers laws during COVID-19. Michelle Mello and David Studdert are studying how governance of data transfers between universities and external organizations for research purposes could be improved.

David Studdert is leading a study examining the relationship between firearm ownership and risks of mortality among residents of California. David Studdert is conducting an international study assessing the role of traffic laws and their enforcement in preventing road accidents. David Studdert and Michelle Mello are investigating how the experience of being sued changes the way physicians deliver care.
Research Programs and Centers
Linkages between SLS and health-focused research centers around Stanford University make for rich environment for research on health law and policy. These centers include:
Center for Law and the Biosciences Stanford Program in Neuroscience and Society Stanford Institute for Economic Policy Research Stanford Center for Biomedical Ethics Stanford Center on Longevity School of Medicine Department of Health Policy Clinical Excellence Research Center Stanford Center for Innovation in Global Health Stanford Human-Centered Artificial Intelligence
Publications
Public health law modernization 2.0: rebalancing public health powers and individual liberty in the age of covid-19, health affairs.
Author(s): Michelle M. Mello , Lawrence O. Gostin
Public health emergency powers laws in the US underwent a profound stress test during the COVID-19 pandemic. Designed with bioterrorism in mind, they struggled to meet the challenges of a multiyear pandemic. Public health legal powers in the US are both too limited, in that they don’t clearly permit officials…
Understanding Liability Risk from Using Health Care Artificial Intelligence Tools
New Eng. J. Med.
Author(s): Michelle M. Mello , Neel Guha
Governing Emerging Technologies—Looking Forward with Horizon Scanning and Looking Back with Technology Audits
Global Public Policy and Governance
Author(s): Henry T. Greely
The 14-Day Embryo Rule: A Modest Proposal
The Death of Roe and the Future of Ex Vivo Embryos
Journal of Law and the Biosciences
Frankenstein and Modern Bioscience: Which Story Should We Heed?
Huntington Library Quarterly (forthcoming 2021)
CRISPR People: The Science and Ethics of Editing Humans
Experiential Learning
SLS offers opportunities for students interested in health to pursue structured experiential learning through:

Juelsgaard Intellectual Property and Innovation Clinic
Occasional Law and Policy Labs offering students a practicum experience in partnership with health policy makers. Recent Policy Labs have included
Evaluating Law Schools and Mental Health Disability
Smoke: Wildfire Science and Policy Lab
Moving Forward from Dobbs
Student Organizations
Student journals, joint degree programs.
- JD/MS in Health Policy (focus in Health Services Research or Epidemiology)
- JD/MD in Law and Medicine
- JD/PhD in Law and Psychology
- JD/PhD in Health Policy
- JD/MS in Epidemiology and Clinical Research
- JD/PhD in Epidemiology and Clinical Research
PRISM Meeting
- April 30, 2024 @ 12:45pm
- Location: @ SLS: Room N112
Mental Health First Aid
- May 4, 2024
- Location: Room offsite
The Debrief: Crip Camp Screening!
- May 9, 2024 @ 7:00pm
- Location: PICC
Inside Stanford Lawyer Magazine
Mello awarded md article prize, goldin receives research award.

Professor Hank Greely on NPR: Scientists Create Immature Human Eggs From Stem Cells

Professor Hank Greely on BBC World Service: The Changing Face of Procreation

Professor Rabia Belt on Off-Kilter

Ana-Mita Betancourt: Navigating Risk for the World’s Underserved

Bright Award for Environmental Sustainability
Law and Wellness

Reforming the Civil Justice System? First, Do No Harm

Veterans Treatment Courts Practicum
Health and Law

SLS to Advance “Neurolaw” as Part of $10 Million Grant

Quentin Cook Named Mormon Apostle

- Career Services

- About USC Gould
- Commencement
- Mission Statement
- Message from the Dean
- History of USC Gould
- Board of Councilors
- Jurist-in-Residence Program
- Social Media
- Consumer Information (ABA Required Disclosures)

- Academic Calendar
- LLM Programs
- Legal Master’s Programs
- Certificates
- Undergraduate Programs
- Bar Admissions
- Concentrations
- Corporate & Custom Education
- Course Descriptions
- Experiential Learning and Externships
- Progressive Degree Programs

Faculty & Research
- Faculty and Lecturer Directory
- Research and Scholarship
- Faculty in the News
- Distinctions and Awards
- Centers and Initiatives
- Workshops and Conferences

- Alumni Association
- Alumni Events
- Class Notes
- USC Law Magazine

- Student Affairs Office
- Student Life and Organizations
- Academic Services and Honors Programs
- Student Wellbeing
- Diversity, Equity, Inclusion and Belonging
- Law School Resources
- USC Resources
- Business Law & Economics
- Constitutional Law
- New Building Initiative
- Law Leadership Society
- How to Give to USC Gould
- Gift Planning
- BS Legal Studies
Explore by Interest
- Legal Master’s Programs
Give to USC Gould
- Giving to Gould
- How to Give
Application Information
Quick links.
- Graduate & International Programs

Contact information
Elyn Saks is Orrin B. Evans Distinguished Professor of Law, Professor of Psychology, and Psychiatry and the Behavioral Sciences at the USC Gould School of Law; Director of the Saks Institute for Mental Health Law, Policy, and Ethics ; Adjunct Professor of Psychiatry at the UC San Diego, School of Medicine; and Faculty at the New Center for Psychoanalysis. She served as USC Gould’s associate dean for research from 2005-2010 and also teaches at the Keck School of Medicine. Saks received her JD from Yale Law School, and a PhD in Psychoanalytic Science from the New Center for Psychoanalysis. She was also awarded an Honorary Doctor of Laws degree (LLD, Hon) from Pepperdine University.
Saks writes extensively in the area of law and mental health, having published five books and more than fifty articles and book chapters. Her research has included the ethical dimensions of psychiatric research and forced treatment of people with mental illness. Her memoir, The Center Cannot Hold: My Journey Through Madness , describes her struggles with schizophrenia and her managing to craft a good life for herself in the face of a dire prognosis. She has won numerous honors, including a 2009 John D. and Catherine T. MacArthur Fellowship (the so-called “Genius Grant”).
In fall 2010, she announced she was using funds from the MacArthur Fellowship to create the Saks Institute for Mental Health Law, Policy, and Ethics at USC, a think tank that studies issues at the intersection of law, mental health, and ethics. The Institute spotlights one important mental health issue per academic year and is a collaborative effort that has included faculty and graduate students from several USC departments: law, psychiatry, psychology, social work, philosophy, neuroscience, gerontology, and engineering.
In addition the The Center Cannot Hold: My Journey Through Madness (Hyperion, 2007), other books include Informed Consent to Psychoanalysis: The Law, the Theory, and the Data (Fordham University Press, 2013), Refusing Care: Forced Treatment and the Rights of the Mentally Ill (University of Chicago Press, 2002), Interpreting Interpretation: The Limits of Hermeneutic Psychoanalysis (Yale University Press, 1999), and Jekyll on Trial: Multiple Personality Disorder and Criminal Law (New York University Press, 1997).
Before joining the USC Gould faculty in 1989, Saks was an attorney in Connecticut and instructor at the University of Bridgeport School of Law. She graduated summa cum laude from Vanderbilt University before earning her master of letters from Oxford University and her JD from Yale, where she edited the Yale Law Journal . Saks is a member of Phi Beta Kappa . In 2013, she was appointed by U.S. Secretary of Health and Human Services to a three-year term on the Center for Mental Health Services (CMHS) National Advisory Council. She also serves as a board member of Mental Health Advocacy Services, Bring Change 2 Mind, Bazelon Center for Mental Health Law, and the Burton Blatt Institute. In 2004, she won both the Associate’s Award for Creativity in Research and Scholarship and the Phi Kappa Phi Faculty Recognition Award.
Selected Works
- Works in Progress
Informed Consent to Psychoanalysis: The Law, The Theory, and The Data (with Shahrokh Golshan) (Fordham University Press, 2013).
- Articles and Book Chapters
"A Conversation between Roburt A. Burt and Elyn R. Saks about Saks’ book, The Center Cannot Hold: My Journey Through Madness " (with Roburt A. Burt) (in press at American Imago).
“Improving Classification of Psychoses" (with Stephen M. Lawrie et al). 3 Lancet Psychiatry 367 (2016).
“Towards Diagnostic Markers for the Psychoses" (with Stephen M. Lawrie et al). 3 Lancet Psychiatry 375 (2016).
“Transitioning Into College with a Mental Health Disorder: Beginnings.” 18 Quinnipiac Health Law Journal 325 (2016).
“Ethical, Legal, and Clinical Considerations when Disclosing a High-Risk Syndrome for Psychosis” (with Vijay A. Mittal et al). 29 Bioethics 543 (2015).
“Psychosis, Pain, and Time: A Personal Reflection.” 72 American Imago 321 (2015).
“The Status of Status Offenses: Helping Reverse the Criminalization of Mental Illness.” 23 Southern California Review of Law & Social Justice 367 (Spring 2014).
“Forcible Medication of Civil Committees: The Most Appropriate Standard.” 2 Mental Health Law & Policy Journal 233 (2013).
“Competency to Refuse Medication: Revisiting the Role of Denial of Mental Illness in Capacity Determinations.” 22 Southern California Review of Law & Social Justice 167 (2013).
"The Politics of Mental Illness: A Professor’s Story, Going Public After Tenure." 19 The American Prospect 7 (2008).
"Commentary: The Importance of Accommodations in Higher Education." 59 Psychiatric Services 376 (2008).
"Proxy Consent to Research: The Legal Landscape" (with Laura B. Dunn, Jessica Wimer, Michael Gonzales and Scott Kim). 8 Yale Journal of Health Policy, Law, and Ethics 37 (2008).
"Decisional Capacity to Consent to Research in Psychosis: An Analysis of Errors" [abstract] (with A. R. Kaup, Barton W. Palmer and Laura B. Dunn). 14 Journal of the International Neuropsychological Society 117 (2008).
"Prevalence and Correlates of Adequate Performance on a Measure of Abilities Related to Decisional Capacity: Differences Among Three Standards for the MacCAT-CR in Patients with Schizophrenia" (with Laura B. Dunn, Barton W. Palmer, P. S. Appelbaum, G. A. Aarons, and Dilip V. Jeste), Schizophrenia Research (2007).
“Assessing Decisional Capacity for Clinical Research or Treatment: A Review of Instruments” (with Laura B. Dunn, M. A. Nowrangi, Barton W. Palmer and Dilip V. Jeste). American Journal of Psychiatry (2006).
“Decisional Capacity in Mental Illness and Substance Use Disorders: Empirical Database and Policy Implications” (with Dilip V. Jeste). 24 Behavioral Sciences and the Law 607 (2006).
“A Collaborative Model for Research on Decisional Capacity and Informed Consent in Older Patients with Schizophrenia: Bioethics Unit of a Geriatric Psychiatry Intervention Research Center” (with Dilip V. Jeste, Laura B. Dunn, Barton W. Palmer, M. Halpin, P. Appelbaum and L. Schneiderman). 171 Psychopharmacology 68 (2004).
“Refusing Care: Forced Treatment and the Use of Psychiatric Advance Directives.” 4 Journal of Forensic Psychology Practice 35 (2004).
"Involuntary Outpatient Commitment." 9 Psychology, Public Policy, and Law 94 (2003).

USC Gould School of Law 699 Exposition Boulevard Los Angeles, California 90089-0071 213-740-7331
USC Gould School of Law
699 Exposition Boulevard
Los Angeles, California 90089-0071
- Academic Programs
- Acceptances
- Awards and Honors
- Book Chapters
- Book Reviews
- Business Law and Economics
- Center for Dispute Resolution
- Center for Law and Philosophy
- Center for Law and Social Science
- Center for Law History and Culture
- Center for Transnational Law and Business
- Centers and Institutes
- Continuing Legal Education
- Contribution to Amicus Briefs
- Contributions to Books
- Criminal Justice
- Degree Programs
- Dispute Resolution
- Election Law
- Environmental Law
- Experiential Learning
- Externships
- Graduate & International Programs
- Hidden Articles
- Housing Law and Policy Clinic
- Immigration Clinic
- Immigration Law
- Initiative and Referendum Institute
- Institute for Corporate Counsel
- Institute on Entertainment Law and Business
- Intellectual Property and Technology Law Clinic
- Intellectual Property Institute
- International Human Rights Clinic
- International Law
- Jurist in Residence
- Legal History
- Legal Theory and Jurisprudence
- LLM On Campus
- Media Advisories
- Media, Entertainment and Technology Law
- Mediation Clinic
- MSL On Campus
- Other Publications
- Other Works
- Planned Giving
- Post-Conviction Justice Project
- Practitioner Guides
- Presentations / Lectures / Workshops
- Public Interest Law
- Publications
- Publications and Shorter Works
- Publications in Books
- Publications in Law Reviews
- Publications in Peer-reviewed Journals
- Real Estate Law and Business Forum
- Redefined Blog
- Research & Scholarship
- Saks Institute for Mental Health Law, Policy, and Ethics
- Scholarly Publications
- Short Pieces
- Small Business Clinic
- Tax Institute
- Trust and Estate Conference
- Uncategorized
- Undergraduate Law
- Working Papers
Copyright © 2024 USC Gould. All Rights Reserved
- Media Contacts
- Make a Gift
- Emergency Information

- Privacy Policy
- Notice of Non-Discrimination
- Digital Accessibility
- Contact Webmaster
Centers, Initiatives & Labs
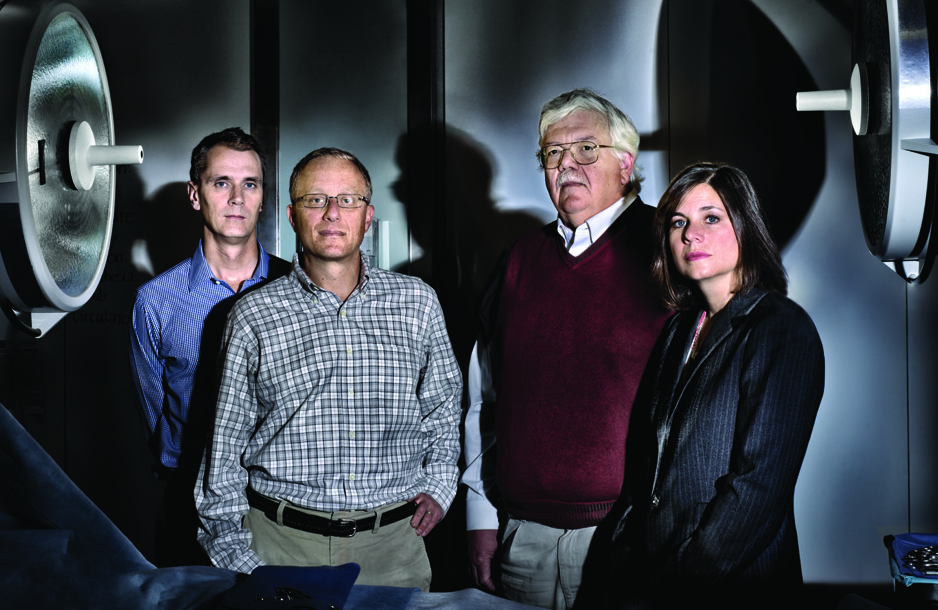
Center for mental health, policy, and the law (cmhpl).
The Center for Mental Health, Policy, and the Law (CMHPL) fosters integrative scholarship to advance empirical knowledge, training, and practice in forensic mental health. The CMHPL’s mission is to address the most urgent issues arising at the interface of mental health and the law, in order to help justice-involved people with mental illness lead full and productive lives.
Jennifer Piel, MD, JD
CMHPL website
Main Challenge
One in two Americans with serious mental illness (SMI) will be arrested in their lifetime. Individuals with SMI are three times more likely to be treated in a jail, state hospital, or other forensic setting than within the broader mental health system. This is one example of the complex association between behavioral health and the legal system.
Our Approach
- Offer empirically-supported assessment and intervention practices for justice-involved individuals with mental illness.
- Enhance law and policy by educating policy makers on mental health, behavioral, and psycholegal issues, and assisting courts in making informed decisions by providing evaluation and consultation services.
- Train and educate the next generation of scholars, practitioners and others in forensic mental health.
Susan E. Reynolds [email protected]
Department Faculty
Sarah kopelovich, phd, katherine michaelsen, md, masc, sarah cusworth walker, phd, ms, sample projects, role of criminal defense attorneys in suicide prevention following defendant arrest, workforce innovation and leadership in forensic mental health.
- Related Training Program
PBSCI 525 – Psychiatry and the Law
Psychology Postdoctoral Fellowship in Psychosis Treatment and Recovery
- UW Medicine
- PsycSource Intranet
- Subscribe to our monthly newsletter to stay up to date on department news.
- Stay Connected:

Best Health Care Law Programs
Ranked in 2024, part of Best Law Schools
Health care law courses often examine medical malpractice
Health care law courses often examine medical malpractice and public health issues, as students are prepared to work with hospitals, physicians, patients and policymakers. These are the top health care law programs. Each school's score reflects its average rating on a scale from 1 (marginal) to 5 (outstanding), based on a survey of academics at peer institutions. Read the methodology »
Here are the Best Health Care Law Programs
Georgia state university, saint louis university, boston university, loyola university chicago, university of maryland (carey), georgetown university, harvard university, northeastern university, university of houston law center.
SEE THE FULL RANKINGS
Try MyLaw Rankings
Create your own custom rankings of the Best Law Schools based on your preferences. Think about your ideal law school experience as you take this five- minute quiz. Don't sweat it — you can continue to customize your list once you receive your school matches.
- Clear Filters

Atlanta , GA
- # 1 in Health Care Law
- # 75 in Best Law Schools (tie)
$17,202 (in-state, full-time) TUITION AND FEES
$36,810 (out-of-state, full-time) TUITION AND FEES
4.5 PEER ASSESSMENT SCORE
160 MEDIAN LSAT (FULL-TIME)
The College of Law at Georgia State University has an application deadline of June 1. The full-time program application... Read More »
TUITION AND FEES
$17,202 (in-state, full-time)
$36,810 (out-of-state, full-time)
PEER ASSESSMENT SCORE
Median lsat (full-time).

St. Louis , MO
- # 2 in Health Care Law
- # 94 in Best Law Schools (tie)
$48,814 (full-time) TUITION AND FEES
$35,530 (part-time) TUITION AND FEES
4.4 PEER ASSESSMENT SCORE
156 MEDIAN LSAT (FULL-TIME)
The full-time program application fee at the School of Law at Saint Louis University is $0. The part-time program... Read More »
$48,814 (full-time)
$35,530 (part-time)

Boston , MA
- # 3 in Health Care Law
- # 24 in Best Law Schools
$65,020 (full-time) TUITION AND FEES
4.3 PEER ASSESSMENT SCORE
170 MEDIAN LSAT (FULL-TIME)
The School of Law at Boston University has an application deadline of April 1. The full-time program application fee at... Read More »
$65,020 (full-time)

Chicago , IL
- # 4 in Health Care Law (tie)
- # 78 in Best Law Schools (tie)
$55,258 (full-time) TUITION AND FEES
$41,090 (part-time) TUITION AND FEES
4.1 PEER ASSESSMENT SCORE
The School of Law at Loyola University Chicago has an application deadline of May 1. The full-time program application... Read More »
$55,258 (full-time)
$41,090 (part-time)

Baltimore , MD
- # 55 in Best Law Schools (tie)
$36,999 (in-state, full-time) TUITION AND FEES
$53,655 (out-of-state, full-time) TUITION AND FEES
163 MEDIAN LSAT (FULL-TIME)
The Francis King Carey School of Law at University of Maryland (Carey) has an application deadline of April 1. The... Read More »
$36,999 (in-state, full-time)
$53,655 (out-of-state, full-time)

Washington , DC
- # 6 in Health Care Law
- # 14 in Best Law Schools (tie)
$75,950 (full-time) TUITION AND FEES
4.0 PEER ASSESSMENT SCORE
171 MEDIAN LSAT (FULL-TIME)
The full-time program application fee at the Law Center at Georgetown University is $85. The part-time program... Read More »
$75,950 (full-time)

Cambridge , MA
- # 7 in Health Care Law (tie)
- # 4 in Best Law Schools (tie)
$75,008 (full-time) TUITION AND FEES
3.8 PEER ASSESSMENT SCORE
174 MEDIAN LSAT (FULL-TIME)
The full-time program application fee at the law school at Harvard University is $85. Its tuition is full-time... Read More »
$75,008 (full-time)

- # 68 in Best Law Schools (tie)
$60,408 (full-time) TUITION AND FEES
$45,300 (part-time) TUITION AND FEES
The School of Law at Northeastern University has an application deadline of March 1. The full-time program application... Read More »
$60,408 (full-time)
$45,300 (part-time)
Houston , TX
$34,942 (in-state, full-time) TUITION AND FEES
$50,132 (out-of-state, full-time) TUITION AND FEES
161 MEDIAN LSAT (FULL-TIME)
The Law Center at University of Houston Law Center has an application deadline of March 15. The full-time program... Read More »
$34,942 (in-state, full-time)
$50,132 (out-of-state, full-time)

Seton Hall University
Newark , NJ
- # 10 in Health Care Law (tie)
- # 61 in Best Law Schools (tie)
$66,780 (full-time) TUITION AND FEES
$50,520 (part-time) TUITION AND FEES
3.7 PEER ASSESSMENT SCORE
The School of Law at Seton Hall University has an application deadline of April 1. The full-time program application... Read More »
$66,780 (full-time)
$50,520 (part-time)
University of South Florida
Department of Mental Health Law & Policy
College of Behavioral & Community Sciences
Main Navigation
Faculty & staff.
Kathleen A. Moore, Ph.D. is a Research Professor in the Department of Mental Health, Law, and Policy of the Louis de la Parte Florida Mental Health Institute (FMHI) at the University of South Florida. She received her B.A. in sociology from the University of Massachusetts, Amherst and both her M.A. and Ph.D. in social/health psychology from Kent State University. She did her post-doctoral fellowship at Duke University Medical Center in which she worked on a NIMH-funded study assessing the effects of exercise vs. medication on clinically depressed older adults. For the past ten years, she has been at FMHI with a primary focus in the area of substance abuse and mental health. Currently, Dr. Moore is working on several community-based research projects with local substance abuse and mental health providers. Her emphasis has been on project evaluation, bridging the gap between research and practice, and social policy issues such as co-occurring disorders, homelessness, and jail diversion. Most recently, she is Co-PI on a National Institute of Drug Abuse (NIDA) grant entitled Center on Co-occurring Disorders, Justice, and Multidisciplinary Research (CJM) along with Dr. Roger Peters, PI and Paul Stiles, Co-PI. The objective of the CJM Center is to enhance the effectiveness of interventions for offenders with CODs within the justice system by: (a) identifying promising intervention strategies, and (b) testing these interventions in theory-informed pilot studies. In coordination with Richard Dembo, Ph.D., she will lead CJM’S Research Team which will coordinate key research activities, including review of pilot projects. The Center will fund three new faculty members in order to conduct significant and innovative research within the area of co-occurring disorders and criminal justice.
Currently, she is Principal Investigator on three grants: (1) Family Dependency Treatment Court,a collaboration involving Hillsborough County Family Dependency Treatment Court (FDTC), a community substance abuse treatment agency, and FMHI. She oversees the coordination of client outcome and process evaluation for an intensive outpatient treatment program utilizing two evidence-based programs (Nurturing Parents and TRIAD) for substance-abusing parents who are involved in the child welfare system; (2) Adult Drug Court Women Empowered and Coping with Addiction to Narcotics (WeCan!), a partnership between Pinellas County Adult Drug Court, two local substance abuse agencies, and FMHI. Dr. Moore coordinates the client outcome and process evaluation for an outpatient treatment program that is providing cognitive-behavioral therapy/motivational enhancement therapy (CBT/MET) to female offenders involved in drug court whose primary drug of choice is prescription drug use; and (3) Medication-Assisted Treatment Drug Treatment Program (MATDTP), a collaboration involving Hillsborough County Adult Drug Court, a behavioral health treatment agency (DACCO), and FMHI. Dr. Moore coordinates the client outcome and process evaluation for this outpatient and residential treatment program that is providing several evidence-based models including Global Assessment of Individualized Needs, medication-assisted treatment for opioid addiction, and the Matrix Model. She also serves as the Co-PI and Evaluator on three other SAMHSA-funded grants: (1) Hillsborough Assertive Community Treatment, a five-year project assessing an Assertive Community Treatment (ACT) approach for homeless individuals diagnosed with severe mental illness; (2) Hillsborough County Jail Diversion, a three-year grant assessing a forensic intensive case management (FICM) approach for adults with co-occurring mental health and substance abuse disorders diverted from jail into treatment; and (3) Charlotte County Home 2 Recovery, a five-year initiative providing integrated services for homeless adults with severe mental illness using an ACT model.
- B.A., University of Massachusetts, Amherst
- M.A., Kent State University
- Ph.D., Kent State University
Research Interests
- Evaluation of community-based agencies
- Co-occurring mental health and substance abuse disorders
- Adolescent drug abuse
- Juvenile and drug treatment court
Research Projects
- ACTS Treatment for Homeless: Evaluation of the Refuge Project
- BayCare Health System Mental Health Crisis Stabilization
- Charlotte County Home 2 Recovery (SAMHSA-CSAT Homeless Treatment)
- Creating a Responsible Thinker (CART) Program
- Driving under the Influence Program
- Evaluation of Pinellas County Adult Drug Court (YouCan!)
- Evaluation of the Northeast Florida Addiction Network (NEFAN)
- Family Dependency Drug Court Program
- Hillsborough Assertive Community Treatment for Homeless People Evaluation
- Hillsborough TCE for Jail Diversion Program ( HTCEJDP) (SAMHSA-CMHS)
- Home-Based Assessments for Diversion-Eligible Youth
- Keystone Project: Treatment for the Homeless (SAMHSA-CSAT)
- Medication Assisted Drug Court Treatment (MADCT) Program
- Pinellas County Adult Treatment Drug Court
- Reclaiming Futures Center for Coaching and Development
- The Women’s Health Project
- USF’s Center on Co-Occurring Disorders, Justice, and Multidisciplinary Research (CJM Center)
Recent Publications
Moore, K.A., Young, M.S., & Snelling, E. (2017). Profile of Alcohol and Drug Indicators for Hillsborough County, Florida. Report prepared for the Hillsborough County Anti-Drug Alliance (HCADA), Tampa, FL.
Moore, K.A., Barongi, M., & Riggs, K. (2016). Reflections of male and female youthful offenders on their experiences in a drug court treatment program. Qualitative Health Research, (July), 1-10.
Young, M. S., & Moore, K. A. (2016). Prevalence and predictors of substance-related emergency psychiatry admissions. Dual Diagnosis: Open Access, 1(1:4), 1-11.
Moore, K. A., Young, M.S., & Rigg, K. (in preparation). WeCan! A 12-month evaluation of preliminary treatment progress of female offenders participating in a drug court treatment program. Criminal Justice Review.
Moore, K.A., Young, M.S., Rigg, K., & Rivera, J. (in preparation). An evaluation of medication-assisted drug court treatment for opiate offenders. Drug and Alcohol Dependence.
Young, M.S., Moore, K.A., & Rigg, K. (in preparation). Substance use reductions among female prescription drug abuse offenders in drug court: Differences between younger and older adults. Drug Court Review.
Young, M.S., Moore, K.A., & Christy, A. (in preparation). Prevalence of and characteristics distinguishing emergency psychiatry admissions with alcohol- or drug-involved presenting problems: Data from three emergency psychiatry departments. Annals of Emergency Medicine.
Barongi, M., Young, M. S., & Moore, K. A. (under review). Baseline characteristics of Hillsborough County family dependency treatment court (FTDC) participants. URC Undergraduate Research Journal.
Givens, E., Barrett, B., Moore, K.A., & Young, M.S. (under review). The impact of age on substance use and arrest among prescription drug offenders in a therapeutic judicial intervention. Evaluation Review: A Journal of Applied Social Research.
Lanza, J., Moore, K.A., & Sharrock, P. (under review). Reflections of male and female youthful offenders on their experiences in a drug court treatment program. International Journal of Offender Therapy and Comparative Criminology.
Snyder, N., Barrett, B., Moore, K.A., & Schonfeld, L. (revise and resubmit). Non-medical prescription drug use in the past year among college students. Journal of Substance Use and Misuse.
Richman, M., Moore, K.A., Barrett, B., & Young, M.S. (2014). Examining baseline mental health symptoms as predictors of drug court graduation for female offenders with prescription drug issues. Undergraduate Research Journal for Human Science, 13, http://www.kon.org/urc/v13/richman.html.
Cohn, A.M., Hagman, B.T., Moore, K.A., Mitchell, J.N., Ehlke, S., and Bramm, S. (2014). Does negative affect mediate the relationship between PTSD symptoms and alcohol involvement in female rape victims? Evidence for the self-medication model using daily interactive voice response methodology. Psychology of Addictive Behaviors, 28(1), 114-126.
Moore, K.A., Barrett, B., Young, M.A., & Ochshorn, E. (in preparation). Family Dependency Treatment Courts: State of the literature, future directions, and implications for behavioral health law and policy. Drug Court Policy Review.
Moore, K.A., Givens, E., & Ochshorn, E. (in preparation). Comparative differences and similarities of drug abuse in China and the United States. International Criminal Justice Review.
Moore, K.A., Broner, N., Frei, A., Ray, J., Parker, T., Foley, G. & Morrisette, D. (under review). Challenges and strategies in implementing jail diversion programs. Journal of Offender Rehabilitation.
Rugs, D., Hills, H.A.., Moore, K.A., & Peters, R.P. (under review). A community planning process for the implementation of evidence-based practice. Evaluation and Program Planning.
Barrett, B., Teague, G.B., Young, M.S., Winarski, J., Moore, K.A., & Ochshorn, E. (in press). Recovery orientation of treatment, consumer empowerment, and satisfaction with services: A mediational model. Psychiatric Rehabilitation Journal.
Lesperance, T., Moore, K.A., Barrett, B., Young, M.S., Clark, C., & Ochshorn, E. (in press). Relationship between trauma and risky behavior in substance-abusing parents involved in a Family Dependency Treatment Court. Journal of Aggression, Maltreatment, and Trauma.
Fogel, S. & Moore, K.A. (2010). Collaborations among diverse organizations: Building evidence to support faith-based partnerships. In M. DeGennaro & S. Fogel (Eds.), Using Evidence to Inform Practice for Community and Organizational Change, (pps. 99-109). Chicago, IL: Lyceum Books, Inc.
Barrett, B., Moore, K.A., Young, M.S., Borum, R., & Ochshorn, E. (2009). Factors predicting arrest for homeless persons receiving integrated residential treatment for co-occurring disorders. Criminal Behaviour and Mental Health.
Hannah, A., Young, M.S., & Moore, K.A. (2009). Relationship between substance use, trauma history, and trauma symptoms among female prescription drug abusing drug court participants. URC Undergraduate Research Journal, http://www.kon.org/urc/v8/hannah.html.
Moore, K.A., Young, M.S., Barrett, B., & Ochshorn, E. (2009). Twelve-month follow-up of integrated treatment for homeless individuals with co-occurring disorders. Journal of Social Service Research, 4(35), 1-14.
University of Virginia School of Law


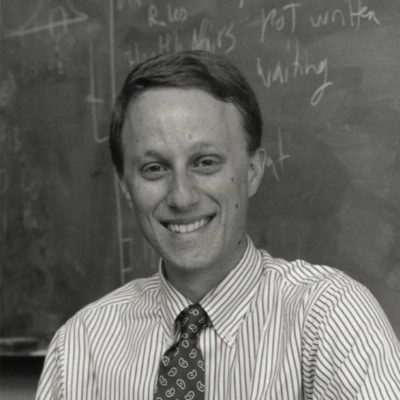
John T. Monahan
- Publications
John Monahan, a psychologist, teaches and writes about how courts use behavioral science evidence, violence risk assessment, criminology and mental health law. He is a member of the National Academy of Medicine and of the American Academy of Arts and Sciences and has served on the National Research Council. Monahan was the founding president of the American Psychological Association’s Division of Psychology and Law and has been a fellow of the John Simon Guggenheim Foundation and the Center for Advanced Study in the Behavioral Sciences. He also has been a visiting fellow at several law schools — including Harvard, Stanford, New York University and the University of California, Berkeley — as well as at the American Academy in Rome, and at All Souls College, Oxford. He twice directed research networks for the John D. and Catherine T. MacArthur Foundation. In 1997, he received an honorary law degree from the City University of New York.
Monahan is the author or editor of 17 books and more than 300 articles and chapters. His work has been cited more than 30,000 times. One of his books, Social Science in Law , co-authored with Laurens Walker , is now in its 10th edition and has been translated into Chinese. Two of his other books won the Manfred Guttmacher Award of the American Psychiatric Association for outstanding research in law and psychiatry. Monahan’s work has been cited frequently by courts, including the California Supreme Court in the landmark case of Tarasoff v. Regents , and the U.S. Supreme Court in Barefoot v. Estelle , in which he was referred to as “the leading thinker on the issue” of violence risk assessment.
Scholarship Profile: Mental Health Law’s “Leading Thinker” ( Virginia Journal 1999)
Coercive Treatment in Psychiatry: Clinical, Legal and Ethical Aspects (edited with Thomas W. Kallert & Juan E. Mezzich), Wiley Blackwell (2011).
An Introduction to Social Science in Law (with W. Laurens Walker), Foundation Press (2006).
Mandated Community Treatment (edited with John Petrila)21 411–521, Behavioral Sciences & the Law (2003).
Adjudicative Competence: The MacArthur Studies (with Richard J. Bonnie et al.), Kluwer Academic/Plenum Publishers (2002).
Rethinking Risk Assessment: The MacArthur Study of Mental Disorder and Violence (with Paul S. Appelbaum et al.), Oxford University Press (2001).
Coercion in Mental Health Services—International Perspectives (edited with Joseph P. Morrissey), JAI Press (1999).
Mental Disorder, Work Disability, and the Law (edited with Richard J. Bonnie), University of Chicago Press (1997).
Coercion and Aggressive Community Treatment: A New Frontier in Mental Health Law (edited with Deborah L. Dennis), Plenum Press (1996).
Violence and Mental Disorder: Developments in Risk Assessment (edited with Henry J. Steadman), University of Chicago Press (1994).
Children, Mental Health, and the Law (edited with Edward P. Mulvey, N. Dickon Reppucci & Lois A. Weithorn), Sage Publications (1984).
Mentally Disordered Offenders: Perspectives from Law and Social Science (edited with Henry J. Steadman), Plenum Press (1983).
Predicting Violent Behavior: An Assessment of Clinical Techniques , Sage Publications (1981).
The Clinical Prediction of Violent Behavior , National Institute of Mental Health (1981).
Prevention in Mental Health: Research, Policy and Practice (edited with Barbara C. Bader, Richard F. Ketterer & Richard H. Price), Sage Publications (1980).
Who Is the Client? The Ethics of Psychological Intervention in the Criminal Justice System , American Psychological Association (1980).
Psychology and Community Change (with Kenneth Heller), Dorsey Press (1977).
Community Mental Health and the Criminal Justice System , Pergamon Press (1976).
Violence and Criminal Justice (edited with Duncan Chappell), Lexington Books (1975).
Social Science in Law: Cases and Materials (with W. Laurens Walker), Foundation Press (10 ed. 2022).
Social Science in Law: Cases and Materials (with W. Laurens Walker), Foundation Press (9 ed. 2018).
Social Science in Law: Cases and Materials (with W. Laurens Walker), Foundation Press (8 ed. 2014).
Social Science in Law: Cases and Materials (with W. Laurens Walker), Foundation Press (7 ed. 2010).
Social Science in Law: Cases and Materials (with W. Laurens Walker), Foundation Press (6 ed. 2006).
Social Science in Law: Cases and Materials (with W. Laurens Walker), Foundation Press (5 ed. 2002).
Social Science in Law: Cases and Materials (with W. Laurens Walker), Foundation Press (4 ed. 1998).
Social Science in Law: Cases and Materials (with W. Laurens Walker), Foundation Press (3 ed. 1994).
Social Science in Law: Cases and Materials (with W. Laurens Walker), Foundation Press (2 ed. 1990).
Social Science in Law: Cases and Materials (with W. Laurens Walker), Foundation Press (1 ed. 1985).
Book Chapters
The Classification of Violence Risk (COVR) , in Handbook of Violence Risk Assessment , Routledge, 93–105 (2 ed. 2021).
Clinical and Actuarial Predictions of Violence (with J. Skeem), in Modern Scientific Evidence: The Law and Science of Expert Testimony , Thomson West, 177–190 (2020).
Predictions of Violence , in The Roots of Modern Psychology and Law: A Narrative History , Oxford University Press, The Roots of Modern Psychology and Law: A Narrative History (2018).
Risk Assessment in Sentencing , in Reforming Criminal Justice , Academy for Justice, 77–94 (2017).
Violence Risk Assessment: The State of the Science (with Jennifer L. Skeem), in Principles and Practice of Forensic Psychiatry , CRC Press, 713–720 (3 ed. 2017).
The Individual Risk Assessment of Terrorism: Recent Developments , in The Handbook of the Criminology of Terrorism , Wiley & Sons, 520–534 (2016).
Legal Process and Social Science: United States , in International Encyclopedia of the Social & Behavioral Sciences , Elsevier, 767–771 (2 ed. 2015).
Afterword , in Violence Risk Assessment and Management: Advances Through Structured Professional Judgement and Sequential Redirections , Wiley Blackwell, 195–199 (2 ed. 2014).
Dangerousness (with Nicola S. Gray et al.), in Forensic Psychiatry: Clinical, Legal, and Ethical Issues , CRC Press, 529–550 (2014).
The Inclusion of Biological Risk Factors in Violence Risk Assessments , in Bioprediction, Biomarkers, and Bad Behavior: Scientific, Legal, and Ethical Challenges , Oxford University Press, 57–76 (2014).
Violence Risk Assessment , in Handbook of Psychology , Wiley, 541–555 (2 ed. 2013).
Extending Violence Reduction Principles to Justice-Involved Persons with Mental Illness (with Henry J. Steadman), in Using Social Science to Reduce Violent Offending , Oxford University Press, 245–261 (2012).
Mandated Psychiatric Treatment in the Community—Forms, Prevalance, Outcomes and Controversies , in Coercive Treatment in Psychiatry: Clinical, Legal and Ethical Aspects , Wiley Blackwell, 33–48 (2011).
Violence and Mandated Community Treatment: The MacArthur Studies , in Violence in Clinical Psychiatry: Proceedings of the 7th European Congress on Violence in Clinical Psychiatry , Kavanah, 34–38 (2011).
The Classification of Violence Risk , in Handbook of Violence Risk Assessment , Routledge, 187–198 (2010).
Standards of Legal Admissibility and Their Implications for Psychological Science (with David L. Faigman), in Psychological Science in the Courtroom: Controversies and Consensus , Guilford Press, 3–25 (2009).
Classification of Violence Risk (COVR) , in Encyclopedia of Psychology and Law , Sage, 92–93 (2008).
Computer-Assisted Violence Risk Assessment among People with Mental Disorder , in Psychology and Law: Bridging the Gap , Ashgate, 211–222 (2008).
MacArthur Violence Risk Assessment Study , in Encyclopedia of Psychology and Law , Sage, 467–470 (2008).
The Scientific Status of Research on Clinical and Actuarial Predictions of Violence , in Modern Scientific Evidence: The Law and Science of Expert Testimony , Thomson/West (2007).
The Future of Violence Risk Management , in The Future of Imprisonment , Oxford University Press, 237–263 (2004).
Mandated Community Treatment: The Potential Role of Violence Risk Assessment , in Involuntary Detention and Therapeutic Jurisprudence: International Perspectives on Civil Commitment , Ashgate, 455–468 (2003).
Violence Risk Assessment in American Law , in Adversarial Versus Inquisitorial Justice : Psychological Perspectives on Criminal Justice Systems , Kluwer Academic/Plenum Publishers, 81–89 (2003).
Violence Risk Assessment , in Handbook of Psychology , Wiley, 527–540 (1 ed. 2003).
Prediction of Crime and Recidivism , in Encyclopedia of Crime and Justice , Macmillan Reference USA, 1125–1131 (2 ed. 2002).
Psychopathy, Treatment Involvement, and Subsequent Violence among Civil Psychiatric Patients , in Modern Scientific Evidence: The Law and Science of Expert Testimony , West, 423–445 (2002).
Legal Process and Social Science: United States , in International Encyclopedia of the Social & Behavioral Sciences , Elsevier, 8660–8663 (1 ed. 2001).
Major Mental Disorder and Violence: Epidemiology and Risk Assessment , in Clinical Assessment of Dangerousness: Empirical Contributions , Cambridge University Press, 89–102 (2001).
Violence Risk Assessment: A Quarter Century of Research (with Henry J. Steadman), in The Evolution of Mental Health Law , American Psychological Association, 195–211 (2001).
'Dangerousness': Violence Risk Assessment , in Encyclopedia of Psychology , Oxford University Press, 169–170 (2000).
Reducing Violence Risk: Diagnostically Based Clues from the MacArthur Violence Risk Assessment Study (with Paul S. Appelbaum), in Effective Prevention of Crime and Violence Among the Mentally Ill , Kluwer, 19–34 (2000).
Sampling Damages (with W. Laurens Walker), in Class Actions and Other Multi-Party Litigation: Cases and Materials , West Group, 822–826 (2000).
Violence and Mental Disorder: Recent Research , in Understanding and Treating Violent Psychiatric Patients , American Psychiatric Press, 167 (2000).
Coercion in the Provision of Mental Health Services: The MacArthur Studies (with et al.), in Research in Community and Mental Health, Vol. 10: Coercion in Mental Health Services - International Perspectives , JAI Press, 13–30 (1999).
Clinical and Actuarial Predictions of Violence , in Modern Scientific Evidence: The Law and Science of Expert Testimony , West, 300–318 (1 ed. 1997).
Epilogue (with Richard J. Bonnie), in Mental Disorder, Work Disability, and the Law , University of Chicago Press, 299–301 (1997).
Major Mental Disorders and Violence to Others , in Handbook of Antisocial Behavior , John Wiley & Sons, 92–100 (1997).
Coercion to Inpatient Treatment: Initial Results and Implications for Assertive Treatment in the Community (with Nancy S. Bennett et al.), in Coercion and Aggressive Community Treatment: A New Frontier in Mental Health Law , Plenum Press, 13–28 (1996).
Designing a New Generation of Risk Assessment Research (with Paul S. Appelbaum et al.), in Violence and Mental Disorder: Developments in Risk Assessment , University of Chicago Press, 297–318 (1994).
Toward a Rejuvenation of Risk Assessment Research (with Henry J. Steadman), in Violence and Mental Disorder: Developments in Risk Assessment , University of Chicago Press, 1–17 (1994).
Causes of Violence , in Drugs & Violence in America: Proceedings of the Inaugural Symposium on Crime and Punishment in the United States , US Government Print Office, 77–85 (1993).
Dangerousness: A View from the United States of America , in Forensic Psychiatry: Clinical, Legal, and Ethical Issues , Betterworth-Heinemann, 640–645 (1993).
Prediction of Criminal Behavior: Recent Developments in Research and Policy in the United States , in Criminal Behavior and the Justice System: Psychological Perspectives , Springer-Verlag, 40–52 (1989).
Foreword , in Clinical Treatment of the Violent Person , Guilford Press, xv-xviii (1987).
Police and the Mentally Disordered , in Police Selection and Training: The Role of Psychology , Martinus Nijhoff, 175–186 (1986).
Evaluating Potentially Violent Persons , in Psychology, Psychiatry, and the Law: A Clinical and Forensic Handbook , Professional Resource Exchange, 9–39 (1985).
Identifying and Treating the Mentally Disordered Prison Inmate (with Eliot Hartstone, Pamela Clark Robbins & Henry J. Steadman), in Mental Health and Criminal Justice , Sage Publications, 279–296 (1984).
Ethical Issues in Prediction of Criminal Violence , in Solutions to Ethical and Legal Problems in Social Research , Academic Press, 83–96 (1983).
Individual-Process Consultation (with Kenneth Heller), in The Mental Health Consultation Field , Human Sciences Press, 57–69 (1983).
Mentally Disordered Sex Offenders (with Sharon Kantorowski Davis), in Mentally Disordered Offenders: Perspectives from Law and Social Science , Plenum Press, 191–204 (1983).
Prediction of Crime and Recidivism , in Encyclopedia of Crime and Justice , Free Press, 1170 (1 ed. 1983).
Prisoners Transferred to Mental Hospitals (with Sharon Kantorowski Davis, Eliot Hartstone & Henry J. Steadman), in Mentally Disordered Offenders: Perspectives from Law and Social Science , Plenum Press, 233–244 (1983).
The Prediction of Violent Behavior: Developments in Psychology and Law , in Psychology and the Law , American Psychological Association, 151–176 (1983).
Childhood Predictors of Adult Criminal Behavior , in Early Childhood Intervention and Juvenile Delinquency , Lexington Books, 11–21 (1982).
Situational Approaches to Understanding and Predicting Individual Violent Behavior (with Dierdre Klassen), in Criminal Violence , Sage Publications, 292–319 (1982).
Three Lingering Issues in Patient Rights , in Psychiatric Patient Rights and Patient Advocacy: Issues and Evidence , Human Sciences Press, 261–277 (1982).
Identifying Chronic Criminals , in Confinement in Maximum Custody: New Last-Resort Prisons in the United States and Western Europe , Lexington Books, 3–14 (1981).
Articles & Reviews
Pretrial risk assessment, risk communication, and racial bias (with S. A. Zottola et al.), 50 Criminal Justice & Behavior 1255–1278 (2023).
Advancing Legal Preparedness through the Global Health Security Agenda (with Ana Ayala et al.), 50 Journal of Law Medicine & Ethics 200–203 (2022).
The Empirical Case for Pretrial Risk Assessment Instruments (with Sarah L. Desmarais & James Austin), 49 Criminal Justice & Behavior 807–816 (2022).
The predictive performance of criminal risk assessment tools used at sentencing: Systematic review of validation studies (with Seena Fazel et al.), 81 Journal of Criminal Justice 101902 (2022).
Impact of Risk Assessment on Judges’ Fairness in Sentencing Relatively Poor Defendants (with Nicholas Scurich & Jennifer Skeem), 44 Law & Human Behavior 51–59 (2020).
Judging Risk (with Brandon L. Garrett), 108 California Law Review 439–493 (2020).
Lost in Translation: “Risks,” “Needs,” and “Evidence” in Implementing the First Step Act (with Jennifer Skeem), 38 Behavioral Sciences & the Law 279–286 (2020).
Risk Assessment in Sentencing and Plea Bargaining: The Roles of Prosecutors and Defense Attorneys (with Brandon L. Garrett, Alexander Jakubow & Anne Metz), Behavioral Sciences & the Law 1–11 (2020).
Valid or Voodoo? A Qualitative Study of Attorney Perceptions of Risk Assessment in Sentencing and Plea Bargaining (with Brandon L. Garrett, Anne Metz & Luke Siebert), 48 Journal of Community Psychology 2053–2068 (2020).
Assessing Risk: The Use of Risk Assessment in Sentencing (with Brandon L. Garrett), 103 Judicature 42–49 (2019).
Judicial Reliance on Risk Assessment in Sentencing Drug and Property Offenders: A Test of the Treatment Resource Hypothesis (with Brandon L. Garrett & Alexander Jakubow), 46 Criminal Justice & Behavior 799–810 (2019).
Lawyers at the Peak of Their Careers: A 30-Year Longitudinal Study of Job and Life Satisfaction (with Jeffrey Swanson), 16 Journal of Empirical Legal Studies 4–25 (2019).
Risk and Resources: A Qualitative Perspective on Low-Level Sentencing in Virginia (with Brandon L. Garrett, Anne L. Metz & Luke Siebert), 47 Journal of Community Psychology 1476–1492 (2019).
Judicial Appraisals of Risk Assessment in Sentencing (with Brandon L. Garrett & Anne L. Metz), 36 Behavioral Sciences & the Law 565–575 (2018).
Predicting Violent Behavior: What Can Neuroscience Add? (with Joshua W. Buckholtz et al.), 22 Trends in Cognitive Sciences 111–123 (2018).
Age, Risk Assessment, and Sanctioning: Overestimating the Old, Underestimating the Young (with Christopher Lowenkamp & Jennifer L. Skeem), 41 Law & Human Behavior 191–201 (2017).
Predicting Sexual Assault Perpetration in the US Army Using Administrative Data (with David M. Benedek et al.), 53 American Journal of Preventative Medicine 661–669 (2017).
Sexual Assault Victimization and Mental Health Treatment, Suicide Attempts, and Career Outcomes Among Women in the US Army (with Paul D. Bliese et al.), 107 American Journal of Public Health 732–739 (2017).
Using Administrative Data to Identify U.S. Army Soldiers at High-Risk of Perpetrating Minor Violent Crimes (with David M. Benedek et al.), 84 Journal of Psychiatric Research 128–136 (2017).
Using Self-Report Surveys at the Beginning of Service to Develop Multi-Outcome Risk Models for New Soldiers in the U.S. Army (with David M. Benedek et al.), 47 Psychological Medicine 2275–2287 (2017).
Violence to Others, Violent Self-Victimization, and Violent Victimization by Others Among Persons with a Mental Illness (with Paul S. Appelbaum, Pamela Clark Robbins & Roumen Vesselinov), 68 Psychiatric Services 516–519 (2017).
Developing a Risk Model to Target High-Risk Preventive Interventions for Sexual Assault Victimization among Female U.S. Army Soldiers (with Paul D. Bliese et al.), 4 Clinical Psychological Science 939–956 (2016).
Evidence Based Sentencing: Public Openness and Opposition to Using Gender, Age, and Race as Risk Factors for Recidivism (with Nicholas Scurich), 40 Law & Human Behavior 36–41 (2016).
Gatekeeping Science: Using the Structure of Scientific Research to Distinguish Between Admissibility and Weight in Expert Testimony (with David L. Faigman & Christopher Slobogin), 110 Northwestern University Law Review 859–904 (2016).
Gender, Risk Assessment, and Sanctioning: The Cost of Treating Women Like Men (with Chistopher Lowenkamp & Jennifer L. Skeem), 40 Law & Human Behavior 580–593 (2016).
Predicting Non-Familial Major Physical Violent Crime Perpetration in the US Army from Administrative Data (with Paul Bliese et al.), 46 Psychological Medicine 303–316 (2016).
Psychosis Uncommonly and Inconsistently Precedes Violence Among High Risk Individuals (with Paul S. Appelbaum et al.), 4 Clinical Psychological Science 40–49 (2016).
Risk Assessment in Criminal Sentencing (with Jennifer L. Skeem), 12 Annual Review of Clinial Psychology 489–513 (2016).
Gun Violence and Victimization of Strangers by Persons with a Mental Illness: Data From the MacArthur Violence Risk Assessment Study (with Debra A. Pinals et al.), 66 Psychiatric Services 1238–1241 (2015).
Group to Individual (G2i) Inference in Scientific Expert Testimony (with David L. Faigman & Christopher Slobogin), 81 University of Chicago Law Review 417–480 (2014).
Risk Redux: The Resurgence of Risk Assessment in Criminal Sanctioning (with Jennifer L. Skeem), 26 Federal Sentencing Reporter 158–166 (2014).
The Evolution of Violence Risk Assessment (with Jennifer L. Skeem), 19 CNS Spectrums 419–424 (2014).
Gangs, Violence, and Psychiatry , 170 American Journal of Psychiatry 942–943 (2013).
The Cost of Assisted Outpatient Treatment: Can It Save States Money? (with Thomas G. McGuire et al.), 170 American Journal of Psychiatry 1423–1432 (2013).
Violent Behavior and Gender of Swedish Psychiatric Patients: A Prospective Clinical Study (with Marianne Kristiansson & Joakim Sturup), 64 Psychiatric Services 688–693 (2013).
Innumeracy and Unpacking: Bridging the Nomothetic/Idiographic Divide in Violence Risk Assessment (with Richard S. John & Nicholas Scurich), 36 Law & Human Behavior 548–554 (2012).
The Individual Risk Assessment of Terrorism , 18 Psychology, Public Policy, & Law 167–195 (2012).
Beyond Context: Social Facts as Case Specific Evidence (with Gregory Mitchell & W. Laurens Walker), 60 Emory Law Journal 1109–1155 (2011).
Case Specific Sociological Inference: Metanorms for Expert Opinions (with Gregory Mitchell & W. Laurens Walker), 40 Social Methods & Research 668–680 (2011).
Current Directions in Violence Risk Assessment (with Jennifer L. Skeem), 20 Current Directions in Psychological Science 38–42 (2011).
Interventions by Virginia’s Colleges to Respond to Student Mental Health Crises (with Richard J. Bonnie, Susan M. Davis & Christopher Flynn), 62 Psychiatric Services 1439–1442 (2011).
The ASA’s Missed Opportunity to Promote Sound Science in Court (with Gregory Mitchell & W. Laurens Walker), 40 Social Methods & Research 605–620 (2011).
Twenty-Five Years of Social Science in Law (with W. Laurens Walker), 35 Law & Human Behavior 72–82 (2011).
Assessing Outcomes for Consumers in New York’s Assisted Outpatient Treatment Program (with Allison R. Gilbert et al.), 61 Psychiatric Services 976–981 (2010).
Cultural Cognition and Public Policy: The Case of Outpatient Commitment Laws (with Donald Braman et al.), 34 Law & Human Behavior 118–140 (2010).
Lawyers at Mid-Career: A 20-Year Longitudinal Study of Job and Life Satisfaction (with Jeffrey W. Swanson), 6 Journal of Empirical Legal Studies 451–483 (2009).
Perceived Coercion to Treatment and Housing Satisfaction in Housing-First and Supportive Housing Programs (with Lisa Callahan & Pamela Clark Robbins), 60 Psychiatric Services 1251–1253 (2009).
Racial Disparities in Involuntary Outpatient Commitment: Are They Real? (with Thomas G. McGuire et al.), 28 Health Affairs 816–826 (2009).
Substance Use, Symptom, and Employment Outcomes of Persons with a Workplace Mandate for Chemical Dependency Treatment (with Paul S. Appelbaum et al.), 60 Psychiatric Services 646–654 (2009).
The Limits of Social Framework Evidence (with Gregory Mitchell & W. Laurens Walker), 8 Law, Probability, & Risk 307–321 (2009).
Understanding and Applying Virginia’s New Statutory Civil Commitment Criteria (with Richard J. Bonnie & Bruce J. Cohen), 28 Developments in Mental Health Law 127–139 (2009).
Alternative Pathways to Violence in Persons with Schizophrenia: The Role of Childhood Antisocial Behavior Problems (with Eric B. Elbogen et al.), 32 Law & Human Behavior 228–240 (2008).
Contextual Evidence of Gender Discrimination: The Ascendance of “Social Frameworks” (with Gregory Mitchell & W. Laurens Walker), 94 Virginia Law Review 1715–1749 (2008).
Mandated Community Treatment: Applying Leverage to Achieve Adherence , 36 Journal of the American Academy of Psychiatry & the Law 282–285 (2008).
A Judges’ Guide to Using Social Science (with W. Laurens Walker), 43 Court Review 156–163 (2007).
Perceived Dangerousness and Support for Coerced Treatment for Children with Mental Health Problems (with Danielle L. Fettes et al.), 58 Psychiatric Services 619–625 (2007).
Sampling Evidence at the Crossroads (with W. Laurens Walker), 80 Southern California Law Review 969–995 (2007).
The Function of Punishment in the “Civil” Commitment of Sexually Violent Predators (with Kevin M. Carlsmith & Alison Evans), 25 Behavioral Sciences & the Law 437–448 (2007).
A Jurisprudence of Risk Assessment: Forecasting Harm among Prisoners, Predators, and Patients , 92 Virginia Law Review 391–435 (2006).
Gender, Threat/Control-Override Delusions and Violence (with Eric Silver & Brent Teasdale), 30 Law & Human Behavior 649–658 (2006).
Patterns of Practice in Mental Health Courts: A National Survey (with John Petrila et al.), 30 Law & Human Behavior 347–362 (2006).
Tarasoff at Thirty: How Developments in Science and Policy Shape the Common Law , 75 University of Cincinnati Law Review 497–521 (2006).
The Classification of Violence Risk (with Paul S. Appelbaum et al.), 24 Behavioral Sciences & the Law 721–730 (2006).
An Actuarial Model of Violence Risk Assessment for Persons with Mental Disorders (with Paul S. Appelbaum et al.), 56 Psychiatric Services 810–815 (2005).
From Coercion to Contract: Reframing the Debate on Mandated Community Treatment for People with Mental Disorders (with Richard J. Bonnie), 29 Law & Human Behavior 485–503 (2005).
From Referral to Disposition: Case Processing in Seven Mental Healthcourts (with Patricia A. Griffin et al.), 23 Behavioral Sciences & the Law 215–226 (2005).
Involuntary Psychiatric Examinations for Danger to Others in Florida after the Attacks of September 11, 2001 (with Ralph A. Catalano, Annette Christy & Eric Kessell), 56 Psychiatric Services 858–862 (2005).
Psychological Evidence at the Dawn of the Law’s Scientific Age (with David L. Faigman), 56 Annual Review of Psychology 631–659 (2005).
The Second Generation of Mental Health Courts (with Patricia A. Griffin et al.), 11 Psychology, Public Policy, & Law 527–538 (2005).
Use of Leverage to Improve Adherence to Psychiatric Treatment in the Community (with Beth Angell et al.), 56 Psychiatric Services 37–44 (2005).
Using a Five Factor Lens to Explore the Relation between Personality Traits and Violence in Psychiatric Patients (with Joshua D. Miller et al.), 73 Journal of Consulting and Clinical Psychology 454–465 (2005).
A Multiple-Models Approach to Violence Risk Assessment among People with Mental Disorder (with Paul S. Appelbaum et al.), 31 Criminal Behavior & Mental Health 324–340 (2004).
License as Leverage: Mandating Treatment for Professionals (with Richard J. Bonnie), 3 International Journal of Forensic Mental Health 131–138 (2004).
S. 1194 Mentally Ill Offender Treatment and Crime Reduction Act of 2003 , 23 Developments in Mental Health Law 19–22 (2004).
Endorsement of Personal Benefit of Outpatient Commitment among Persons with Severe Mental Illness (with Jeffrey W. Swanson & Marvin S. Swartz), 9 Psychology, Public Policy, & Law 70–93 (2003).
Introduction to this Issue: Mandated Community Treatment (with John Petrila), 21 Behavioral Sciences & the Law 411–414 (2003).
Mental Disorder, Violence, and Gender (with Pamela Clark Robbins & Eric Silver), 27 Law & Human Behavior 561–571 (2003).
Perceived Coercion at Hospital Admission and Adherence to Mental Health Treatment after Discharge (with Sarah D. Rain et al.), 54 Psychiatric Services 103–105 (2003).
Communicating Violence Risk: Frequency Formats, Vivid Outcomes, and Forensic Settings (with Jonathan Bone et al.), 1 International Journal of Forensic Mental Health 121–126 (2002).
Psychopathy, Treatment Involvement, and Subsequent Violence Among Civil Psychiatric Patients (with Edward P. Mulvey & Jennifer L. Skeem), 26 Law & Human Behavior 577–603 (2002).
The MacArthur Studies of Violence Risk , 12 Criminal Behavior & Mental Health S67-S72 (2002).
Mandated Community Treatment: Beyond Outpatient Commitment (with Paul S. Appelbaum et al.), 52 Psychiatric Services 1198–1205 (2001).
Special Section on Involuntary Outpatient Commitment: Introduction (with Marvin S. Swartz), 52 Psychiatric Services 323–324 (2001).
A Classification Tree Approach to the Development of Actuarial Violence Risk Assessment Tools (with Paul S. Appelbaum et al.), 24 Law & Human Behavior 83–100 (2000).
Could “Law and Evolution” Be the Next “Law and Economics?” , 8 Virginia Journal of Social Policy & the Law 123–128 (2000).
Developing a Clinically Useful Actuarial Tool for Assessing Violence Risk (with Paul S. Appelbaum et al.), 176 British Journal of Psychiatry 312–319 (2000).
Psychological Science Can Improve Diagnostic Decisions (with Robyn M. Dawes & John A. Swets), 1 Psychological Science in the Public Interest 1–26 (2000).
Scientific Authority: The Breast Implant Litigation and Beyond (with W. Laurens Walker), 86 Virginia Law Review 801–833 (2000).
Sources of Coercive Behaviours in Psychiatric Admissions (with Nancy Bennett et al.), 101 Acta Psychiatrica Scandinavica 73–79 (2000).
Violence and Delusions: Data from the MacArthur Violence Risk Assessment Study (with Paul S. Appelbaum & Pamela Clark Robbins), 157 American Journal of Psychiatry 566–572 (2000).
Violence Risk Assessment and Risk Communication: The Effects of Using Actual Cases, Providing Instruction, and Employing Probability Versus Frequency Formats (with Donald G. MacGregor & Paul Slovic), 24 Law & Human Behavior 271–296 (2000).
Violence Risk Assessment: Scientific Validity and Evidentiary Admissibility , 57 Washington & Lee Law Review 901–918 (2000).
Violent Thoughts and Violent Behavior Following Hospitalization for Mental Disorder (with Paul S. Appelbaum et al.), 68 Journal of Consulting and Clinical Psychology 388–398 (2000).
Assessing Violence Risk among Discharged Psychiatric Patients: Toward an Ecological Approach (with Edward P. Mulvey & Eric Silver), 23 Law & Human Behavior 237–255 (1999).
Coercion in the Provision of Mental Health Services: The MacArthur Studies (with Nancy Bennett et al.), 10 Research in Community & Mental Health 13–30 (1999).
Patients’ Revisions of Their Beliefs about the Need for Hospitalization (with Nancy Bennett et al.), 156 American Journal Psychiatry 1385–1391 (1999).
Real in Their Consequences: A Sociological Approach to Understanding the Association Between Psychotic Symptoms and Violence (with Francis T. Cullen, Bruce G. Link & Ann Stueve), 64 American Sociological Review 316–332 (1999).
Sampling Liability (with W. Laurens Walker), 85 Virginia Law Review 329–351 (1999).
The Public’s View of the Competence, Dangerousness, and Need for Legal Coercion of Persons with Mental Health Problems (with Saeko Kikuzawa et al.), 89 American Journal of Public Health 1339–1345 (1999).
Violence in the Mentally Ill: Questions Remain - In Reply (with Paul S. Appelbaum et al.), 56 Archives of General Psychiatry 193–194 (1999).
Factual Sources of Psychiatric Patients’ Perceptions of Coercion in the Hospital Admission Process (with Marlene M. Eisenberg et al.), 155 American Journal of Psychiatry 1254–1260 (1998).
Factual Sources of Psychiatric Patients’ Perceptions of Coercion in the Hospital Admission Process (with Nancy Bennett et al.), 21 International Journal of Law & Psychiatry 131–146 (1998).
Psychometric Properties of the Macarthur Competence Assessment Tool-Criminal Adjudication (MacCAT-CA) (with Richard J. Bonnie et al.), 10 Psychological Assessment 435–443 (1998).
Sampling Damages (with W. Laurens Walker), 83 Iowa Law Review 545–568 (1998).
The Competence-Related Abilities of Women Criminal Defendants (with Richard J. Bonnie et al.), 26 Journal of the American Academy of Psychiatry and the Law 215–22 (1998).
Violence by People Discharged from Acute Psychiatric Inpatient Facilities and by Others in the Same Neighborhoods (with Paul S. Appelbaum et al.), 55 Archives of General Psychiatry 393–401 (1998).
Actuarial Support for the Clinical Assessment of Violence Risk , 9 International Review of Psychiatry 167–169 (1997).
Law School Performance Predicted by Explanatory Style (with Jason M. Satterfield & Martin E. Seligman), 15 Behavioral Sciences & the Law 95–105 (1997).
Perception of Coercion (with Steven K. Hoge & Charles W. Lidz), 51 Nordic Journal of Psychiatry 214 (1997).
Perceptions of Coercion in the Admission of Voluntary and Involuntary Psychiatric Patients (with Nancy Bennett et al.), 20 International Journal of Law & Psychiatry 167–181 (1997).
The MacArthur Adjudicative Competence Study: A Comparison of Criteria for Assessing the Competence of Criminal Defendants (with Richard J. Bonnie et al.), 25 Journal of the American Academy of Psychiatry and the Law 249–259 (1997).
The MacArthur Adjudicative Competence Study: Development and Validation of a Research Instrument (with Richard J. Bonnie et al.), 21 Law & Human Behavior 141–179 (1997).
The MacArthur Adjudicative Competence Study: Diagnosis, Psychopathology, and Competence-related Abilities (with Richard J. Bonnie et al.), 15 Behavioral Sciences & the Law 329–345 (1997).
The Validity of Mental Patients’ Accounts of Coercion-Related Behaviors in the Hospital Admission Process (with Nancy Bennett et al.), 21 Law & Human Behavior 361–376 (1997).
Commentary: Dangerous Patients or Dangerous Diseases? (with Pamela J. Taylor), 312 British Journal of Medicine 967–969 (1996).
Daubert and the Reference Manual : An Essay on the Future of Science in Law (with W. Laurens Walker), 82 Virginia Law Review 837–857 (1996).
Decision-Making in Criminal Defense: An Empirical Study of Insanity Pleas and the Impact of Doubted Client Competence (with Richard J. Bonnie et al.), 87 Journal of Criminal Law & Criminology 48–62 (1996).
Mentally Ill and Non-Mentally Ill Defendants’ Abilities to Understand Information Relevant to Adjudication: A Preliminary Study (with Richard J. Bonnie et al.), 24 Bulletin of the American Academy of Psychiatry & the Law 187–197 (1996).
Psychotic Symptoms and Disorders and the Risk of Violent Behaviour in the Community (with Randy Borum, Jeffrey W. Swanson & Marvin S. Swartz), 6 Criminal Behavior & Mental Health 309–329 (1996).
Violence by People with Mental Illness: A Consensus Statement by Advocates and Researchers (with Jean Arnold), 19 Psychiatric Rehabilitation 67–70 (1996).
Violence Prediction: The Past Twenty and the next Twenty Years , 23 Criminal Justice & Behavior 107–120 (1996).
Violent Storms and Violent People: How Meteorology Can Inform Risk Communication in Mental Health Law (with Henry J. Steadman), 51 American Psychology 931–938 (1996).
Coercion and Commitment: Understanding Involuntary Mental Hospital Admission (with Nany Bennett et al.), 18 International Journal of Law & Psychiatry 249–263 (1995).
Perceived Coercion in Mental Hospital Admission: Pressures and Process (with Paul Slovic), 19 Law & Human Behavior 49–65 (1995).
Probability, Danger, and Coercion: A Study of Risk Perception and Decision Making in Mental Health Law (with Paul Slovic), 19 Law & Human Behavior 49–65 (1995).
Review of Webster et al., The Violence Prediction Scheme (reviewing Christopher T. Webster, et al., The Violence Prediction Scheme: Assessing Dangerousness in High Risk Men ) 22 Criminal Justice & Behavior 446–447 (1995).
Client Abilities to Assist Counsel and Make Decisions in Criminal Cases: Findings from Three Studies (with Richard J. Bonnie, Steven K. Hoge & Norman Poythress), 18 Law & Human Behavior 427–435 (1994).
Judicial Use of Social Science Research after Daubert (with W. Laurens Walker), 2 Shepard’s Expert & Scientific Evidence Quarterly 327–342 (1994).
Mental Illness as a Factor in Criminality: A Study of Prisoners and Mental Patients (with Carmen Cirincione, Pamela Clark Robbins & Henry J. Steadman), 4 Criminal Behavior & Mental Health 33–47 (1994).
People with Mental Disorder and People Who Offend: Collecting Valid Data , 4 Criminal Behavior & Mental Health 68–83 (1994).
The Causes of Violence , 63 FBI Law Enforcement Bulletin 11–15 (1994).
Ethical and Legal Duties in Conducting Research on Violence: Lessons from the MacArthur Risk Assessment Study (with Paul S. Appelbaum et al.), 8 Violence & Victims 387–396 (1993).
Inclusion, Motivation, and Good Faith: The Morality of Coercion in Mental Hospital Admission (with Nancy S. Bennett et al.), 11 Behavioral Sciences & the Law 295–306 (1993).
Limiting Therapist Exposure to Tarasoff Liability: Guidelines for Risk Containment , 48 American Psychology 242–250 (1993).
Patient, Family, and Staff Perceptions of Coercion in Mental Hospital Admission: An Exploratory Study (with Robert Arnold et al.), 11 Behavioral Sciences & the Law 281–293 (1993).
Review of Blackburn, The Psychology of Criminal Conduct (reviewing Ronald Blackburn, The Psychology of Criminal Coduct: Theory, Research, and Practice ) 3 Criminal Behavior & Mental Health 203–204 (1993).
Two Scales for Measuring Patients’ Perceptions for Coercion During Mental Hospital Admission (with Nancy Bennett et al.), 11 Behavioral Sciences & the Law 307–321 (1993).
“A Terror to Their Neighbors”: Beliefs about Mental Disorder and Violence in Historical and Cultural Perspective , 20 Bulletin of the American Academy of Psychiatry & the Law 191–195 (1992).
Attorney-Client Decision-Making in Criminal Cases: Client Competence and Participation as Perceived by Their Attorneys (with Richard J. Bonnie, Steven K. Hoge & Norman Poythress), 10 Behavioral Sciences & the Law 385–394 (1992).
Mental Disorder and Violent Behavior: Perceptions and Evidence , 47 American Psychology 511–521 (1992).
Risk Assessment: Commentary on Poythress and Otto , 5 Forensic Report 151–154 (1992).
Schizophrenia as a Contingent Risk Factor for Criminal Violence (with Carmen Cirincione, Pamela Clark Robbins & Henry J. Steadman), 15 International Journal of Law & Psychiatry 347–358 (1992).
Empirical Questions without Empirical Answers (with W. Laurens Walker), 1991 Wisconsin Law Review 569–594 (1991).
Judicial Use of Social Science Research (with W. Laurens Walker), 15 Law & Human Behavior 571–584 (1991).
Violence in the Workplace , 32 Journal of Occupational Medicine 1021 (1990).
Dangerousness and Commitment of the Mentally Disordered in the United States , 15 Schizophrenia Bulletin 541–553 (1989).
From the Man Who Brought You Deinstitutionalization (reviewing Thomas Szasz, Insanity: The Idea and Its Consequences ) 33 Journal of Contemporary Psychology 492 (1988).
Risk Assessment of Violence among the Mentally Disordered: Generating Useful Knowledge , 11 International Journal of Law & Psychiatry 249–257 (1988).
Social Facts: Scientific Methodology as Legal Precedent (with W. Laurens Walker), 76 California Law Review 877–896 (1988).
Social Science Research in Law: A New Paradigm (with W. Laurens Walker), 43 American Psychology 465–472 (1988).
Psychologists as Law Professors (with Gary B. Melton & Michael J. Saks), 42 American Psychology 502–598 (1987).
Social Frameworks: A New Use of Social Science in Law (with W. Laurens Walker), 73 Virginia Law Review 559–598 (1987).
Dangerous and Violent Behavior , 1 State of the Art Reviews: Occupational Medicine 559–568 (1986).
Psychiatric Evaluations of Police Referrals in a General Hospital Emergency Room (with Jeraldine Braff, Joseph P. Morrissey & Henry J. Steadman), 8 Journal of International Law & Psychiatry 39–47 (1986).
Slouching toward Crime , 95 Yale Law Journal 1536–1551 (1986).
Social Authority: Obtaining, Evaluating, and Establishing Social Science in Law (with W. Laurens Walker), 134 University of Pennsylvania Law Review 477–517 (1986).
Teaching Social Science in Law: An Alternative to “Law and Society” (with W. Laurens Walker), 35 Journal of Legal Education 478–482 (1985).
The Impact of State Mental Hospital Deinstitutionalization on United States Prison Populations, 1968-1978 (with Barbara Duffee, Eliot Hartstone & Henry J. Steadman), 75 Journal of Criminal Law & Criminology 474–490 (1984).
The Prediction of Violent Behavior: Toward a Second Generation of Theory and Policy , 141 American Journal of Psychiatry 10–15 (1984).
Crime and Mental Disorder: An Epidemiological Approach (with Henry J. Steadman), 4 Crime & Justice 145–189 (1983).
Clinical Prediction of Violent Behavior , 12 Psychiatric Annals 509–513 (1982).
Mentally Disordered Offenders: A National Survey of Patients and Facilities (with Sharon Kantorowski Davis et al.), 6 Law & Human Behavior 31–38 (1982).
Patients’ Perspections of the Family’s Role in Involuntary Commitment (with Herbert D. Friedlander, David Prestholt & Stephanie Splane), 33 Hospital & Community Psychology 569–572 (1982).
Review of Wexler, Mental Health Law (reviewing David B. Wexler, Mental Health Law: Major Issues ) 5 International Journal of Law & Psychiatry 115–116 (1982).
Stone-Roth Model of Civil Commitment and the California Dangerousness Standard: Operational Comparison (with Herbert D. Friedlander & Mary Ruggiero), 39 Archives of General Psychiatry 1267–1271 (1982).
The Case for Prediction in the Modified Desert Model of Criminal Sentencing , 5 International Journal of Law & Psychiatry 103–113 (1982).
The Psychology of Law (with Elizabeth F. Loftus), 33 Annual Review of Psychology 441–475 (1982).
Vitek and Beyond: The Empirical Context of Prison-to-Hospital Transfers (with Eliot Hartstone & Henry J. Steadman), Law & Contemporary Problems 125–136 (1982).
Review of Cohn & Udolf, The Criminal Justice System and Its Psychology (reviewing Alfred Cohn & Roy Udolf, The Criminal Justice System and Its Psychology ) 25 Contemporary Psychology 640–641 (1980).
Empirical Analyses of Civil Commitment: Critique and Context , 11 Law & Society Review 619–628 (1977).
Prediction Research and the Role of Psychologists in Correctional Institutions (with Linda Costa Monahan), 14 San Diego Law Review 1028–1038 (1977).
Psychologically Disordered and Criminal Offenders: Perceptions of Their Volition and Responsibility (with Gloria L. Hood), 3 Criminal Justice & Behavior 123–134 (1976).
Attorneys as Friends out of Court: An Examination of the Santa Clara County Volunteers in Parole Program (with Howard Bidna et al.), 15 Santa Clara Lawyer 817–854 (1975).
New Roles for Psychologists , 1 Criminal Justice & Behavior 190–192 (1974).
Abolish the Insanity Defense?—Not Yet , 26 Rutgers Law Review 719–740 (1973).
Reports & Datasets
Mental Illness and Violent Crime: A Summary of a Presentation , National Institute of Justice (1996).
Crime and Mental Disorder (with Henry J. Steadman), National Institute of Justice (1984).
Statement The Insanity Defense , US Government Print Office 470–479 (1982).
Testimony Insanity Defense in Federal Courts , US Government Print Office 87–94 (1982).
Statement Early Identification and Classification of Juvenile Delinquents , US Government Print Office 2–31 (1981).
Op-Eds, Blogs, Shorter Works
The Challenge of Preventing Violence Is Not Just an American Problem (with Jeffrey W. Swanson), Guardian 2 (April 22, 2007).
Mandated Treatment in the Community for People with Mental Disorders (with Richard J. Bonnie & Marvin S. Swartz), Health Affairs 28–38 (September, 2003).
A Case in Point , 34 Contemporary Psychology 1048 (1989).
The Prediction of Violent Behavior , Virginia Law School Report 9–12 (August, 1982).
Delivering Community Mental Health Services to a County Jail Population: A Research Note (with Leah B. McDonough), 8 American Academy of Psychiatry & the Law Bulletin 28–32 (1980).
Social Science in the Law
- Criminology
- Social science in law
- Forensic psychiatry
- Mental health
- Mental disorders
- Mental hospitals
- Law and psychiatry
Pretrial risk assessment, risk communication, and racial bias
We examined how the presentation of risk assessment results and the race of the person charged affected pretrial court actors’ recommendations to...
The predictive performance of criminal risk assessment tools used at sentencing: Systematic review of validation studies Seena Fazel Matthias Burghart Thomas Fanshawe ... Although risk assessment tools have been widely used to inform sentencing decisions, there is uncertainty about the extent and quality of evidence of... More
Pretrial risk assessment instruments are used in many jurisdictions to inform decisions regarding pretrial release and conditions. Many are concerned...
- Academic Calendar
- J.D. Curriculum
- Current Courses
- Concentrations
- Academic Policies
- Study Abroad
- Graduate Studies (LL.M. and S.J.D.)
- Dual-Degree Programs
- Programs and Centers
- Experiential Learning
- Educating Legal Scholars
- Faculty Scholarship
- The Free Exchange of Ideas at UVA Law
- Admissions Process
- J.D. Application Information
- Virginia Residency
- Online Status Checker
- Make Online Seat Deposit
- Transfer Students
- Brochures and Key Websites
- ABA Required Disclosures
- Diversity, Equity and Belonging
- Admitted Students
- Graduate Studies
- Financial Aid
- Karsh-Dillard Scholarships
- Student Organizations
- Academic Journals
- Student Government
- The Honor System
- Living in Charlottesville
- Awards, Fellowships and Honors
- Moot Court and Trial Advocacy
- Legal Writing Fellows
- Student Affairs
- Student Records
- Career Development
- Law IT/Computing
- Courts & Commerce Bookstore
- Employment Resources for Students
- Office of Private Practice Staff
- Resources for Private Practice Employers
- Public Service Center Staff
- Funding for Public Service
- Program in Law and Public Service
- Resources for Public Service Employers
- Office of Judicial Clerkships Staff
- The Pro Bono Program
- About the School
- Facts & Statistics
- Consumer Information (ABA Required Disclosures)
- Event Calendar
- Video & Audio
- Subscribe and Connect
- University of Virginia

School of Law
Changing regulations in the healthcare industry have sparked demand for professionals who can understand and interpret today's complex legal issues. With a certificate in health law from Northeastern University, you can gain those skills and learn how to effectively work with counsel when a lawyer's involvement is necessary.
If you work in the healthcare industry and are looking to expand your legal knowledge, but are not quite ready to pursue a master’s degree, we offer a 12-credit Graduate Certificate in Health Law. This certificate arises directly from the need for more professionals with legal expertise in the highly regulated field of healthcare. The certificate is designed specifically to provide professionals with the skills necessary to understand, navigate and leverage the legal issues that arise within the healthcare field and to work effectively with counsel when a lawyer’s involvement is necessary. Students can apply their credits from this program to the Master of Legal Studies later on if desired.
Changing regulations in the healthcare industry have sparked demand for professionals who can understand and interpret today’s complex legal issues. With a certificate in health law from Northeastern University, you can gain those skills and learn how to effectively work with counsel when a lawyer’s involvement is necessary.
More Details
Unique features.
- Tailor your education to your schedule. This certificate is offered in a 100-percent-online, asynchronous, flexible format, allowing you to take advantage of the program’s rigorous coursework and experienced faculty regardless of your location.
- Stack your certificate into a master’s degree. The 12 credits from this program can be applied toward a Master of Legal Studies.
- Learn directly from the experts, such as Wendy Parmet, director of Northeastern’s Center on Health Law and Policy, and Patricia Davidson, a former senior staff attorney for the Public Health Advocacy Institute, a nonprofit affiliated with Northeastern’s School of Law.
- Earn a top-ranked education. The School of Law is ranked 15th in healthcare law by U.S. News and World Report.
Program Objectives
Healthcare is a complex legal arena, as it encompasses several key stakeholders from providers, to patients, to insurers. The Graduate Certificate in Health Law can help individuals juggle the varying legal needs in this space. It provides students with an introductory course paired with three electives tailored to the health industry.
The program helps to prepare graduates with the skills and experience to:
- Summarize and apply the appropriate statutes and regulations to concrete situations
- Examine legal regulations governing the provision and financing of healthcare services
- Gain an in-depth overview of health and compliance programs and the code of conduct for particular fields
Looking for something different?
A graduate degree or certificate from Northeastern—a top-ranked university—can accelerate your career through rigorous academic coursework and hands-on professional experience in the area of your interest. Apply now—and take your career to the next level.
Program Costs
Finance Your Education We offer a variety of resources, including scholarships and assistantships.
How to Apply Learn more about the application process and requirements.
Requirements
To apply to the program, you must have:
- Bachelor’s degree from a regionally accredited institution
To complete the application process, you must submit:
- Online application
- Professional resumé
- Transcripts from all previous undergraduate and graduate institutions
- A personal statement
- One letter of recommendation: from individual(s) with either academic or professional knowledge of your capabilities, such as a faculty member, current employer, mentor, or colleague
- Official TOEFL scores (nonnative English speakers only)
- GRE or LSAT scores (optional)
Are You an International Student? Find out what additional documents are required to apply.
Admissions Details Learn more about the School of Law admissions process, policies, and required materials.
Admissions Dates
Industry-aligned courses for in-demand careers..
For 100+ years, we’ve designed our programs with one thing in mind—your success. Explore the current program requirements and course descriptions, all designed to meet today’s industry needs and must-have skills.
View curriculum
Northeastern's signature experience-powered learning model has been at the heart of the university for more than a century. It combines world-class academics with professional practice, allowing you to acquire relevant, real-world skills you can immediately put into action in your current workplace. This makes a Northeastern education a dynamic, transformative experience, giving you countless opportunities to grow as a professional and person.
Our Faculty
Northeastern University faculty represents a broad cross-section of professional practices and fields, including finance, education, biomedical science, management, and the U.S. military. They serve as mentors and advisors and collaborate alongside you to solve the most pressing global challenges facing established and emerging markets.

Patricia Davidson

Joshua Abrams

James Rowan
By enrolling in Northeastern, you’ll gain access to students at 13 campus locations, 300,000+ alumni, and 3,000 employer partners worldwide. Our global university system provides students unique opportunities to think locally and act globally while serving as a platform for scaling ideas, talent, and solutions.
Below is a look at where our Law & Criminology alumni work, the positions they hold, and the skills they bring to their organization.
Where They Work
- Commonwealth of Massachusetts
- City of Boston
- U.S. Department of Justice
What They Do
- Business Development
- Entrepreneurship
- Community and Social Services
What They're Skilled At
- Legal Research
- Legal Writing
- Public Speaking
Learn more about Northeastern Alumni on Linkedin .
Related Articles

5 Tips for Choosing Your DLP Dissertation Topic

How to Get Hands-On Experience in Law & Public Policy

Laws and Regulations Every HR Professional Should Know
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- J Urban Health
- v.94(3); 2017 Jun

Sexual Identity, Stigma, and Depression: the Role of the “Anti-gay Propaganda Law” in Mental Health among Men Who Have Sex with Men in Moscow, Russia
Emily hylton.
1 Center for Public Health and Human Rights, Department of Epidemiology, Johns Hopkins Bloomberg School of Public Health, 615 N. Wolfe St., Room E7141, Baltimore, MD 21205 USA
Andrea L. Wirtz
Carla e. zelaya, carl latkin.
2 Department of Health, Behavior and Society, Johns Hopkins Bloomberg School of Public Health, Baltimore, MD USA
Alena Peryshkina
3 AIDS Infoshare, Moscow, Russian Federation
Vladmir Mogilnyi
Petr dzhigun, irina kostetskaya.
4 Department of Statistics, The University of Haifa, Mt Carmel, Israel
Chris Beyrer
Associated data.
Depression is a major public health problem in the Russian Federation and is particularly of concern for men who have sex with men (MSM). MSM living in Moscow City were recruited via respondent-driven sampling and participated in a cross-sectional survey from October 2010 to April 2013. Multiple logistic regression models compared the relationship between sexual identity, recent stigma, and probable depression, defined as a score of ≥23 on the Center for Epidemiological Studies Depression scale. We investigated the interactive effect of stigma and participation in the study after the passage of multiple “anti-gay propaganda laws” in Russian provinces, municipalities, and in neighboring Ukraine on depression among MSM. Among 1367 MSM, 36.7% ( n = 505) qualified as probably depressed. Fifty-five percent identified as homosexual ( n = 741) and 42.9% identified as bisexual ( n = 578). Bisexual identity had a protective association against probable depression (reference: homosexual identity AOR 0.71; 95%CI 0.52–0.97; p < 0.01). Those who experienced recent stigma (last 12 months) were more likely to report probable depression (reference: no stigma; AOR 1.75; 95%CI 1.20–2.56; p < 0.01). The interaction between stigma and the propaganda laws was significant. Among participants with stigma, probable depression increased 1.67-fold after the passage of the anti-gay laws AOR 1.67; 95%CI 1.04–2.68; p < 0.01). Depressive symptoms are common among MSM in Russia and exacerbated by stigma and laws that deny homosexual identities. Repeal of Russia’s federal anti-gay propaganda law is urgent but other social interventions may address depression and stigma in the current context.
Electronic supplementary material
The online version of this article (doi:10.1007/s11524-017-0133-6) contains supplementary material, which is available to authorized users.
Introduction
Depression and other mental health disorders represent a large proportion of the global burden of disease and are the second leading cause of global disability [ 1 , 2 ]. In the Russian Federation, this trend is consistent, if not magnified, among men. Here, the prevalence of depressive symptoms in men residing in urban areas has been reported as high as 23% in 1999–2000, as defined by a score of ≥16 on the Center for Epidemiological Studies Depression (CES-D) scale [ 3 ]. As of 2011, the suicide rate among Russian men was estimated at 35.1 per 100,000 persons—one of the highest in the world. [ 4 ] Global reports suggest that men who have sex with men (MSM) often have higher prevalence of depression than heterosexual men [ 5 ], and the little research that has been conducted in Russia on the topic suggests that such patterns may persist among MSM [ 6 ]. Analysis of HIV-infected MSM found that over one-third have reported symptomology indicative of probable depression and more than half of MSM in Moscow have reported hazardous or harmful levels of alcohol abuse that may be related to depression [ 7 ].
Across settings, research among MSM has shown that homophobia and social stigma may contribute to depression [ 8 ]. While less is known from the Russian Federation, research from similar epidemiologic settings in Central Asia has provided some insight, demonstrating that even where homosexuality has been decriminalized, stigmatization of homosexuality persists [ 9 ], and MSM who regularly practice the receptive role during anal intercourse experience increased levels of stigma [ 10 ]. Social stigma in Central Asia has been associated with reduced access to health and social services among MSM [ 9 , 11 ], including key HIV prevention and treatment services [ 9 ]. Depressive symptoms among MSM in Central Asia has been explained in part by high prevalence of community-level stigma [ 9 ]. Research from other countries with similar contexts in which homosexuality is decriminalized but where there is no legal protection for MSM against discrimination [ 12 ] have demonstrated the association between increased levels of perceived and experienced stigma and depression among MSM [ 13 , 14 ] and inconsistent use of condoms and depression among MSM [ 15 ]. Social support [ 16 ] and social cohesion [ 13 ] within the MSM community, however, appear to have a protective effect against depression among MSM in these countries.
Recent events within Russia provide context and rationale for understanding the factors associated with poor mental health outcomes among MSM. In June 2013, the Russian government issued the “anti-gay propaganda law,” a national ban on “propaganda for non-traditional sexual relations” that criminalized the sharing of information related to same sex practices. The law effectively legitimized public stigma and violence against lesbian, gay, bisexual, and transgender people (LGBT) in Russia [ 17 , 18 ]. This came on the heels of similar laws in the City of St. Petersburg (March 2012) that would fine individuals up to 500,000 rubles (approximately $17,000 USD) for spreading “homosexual propaganda,” as well as other related legislation in multiple oblasts (administrative divisions) across the Russian Federation, and a widely praised draft law in neighboring Ukraine (October 2012) that would impose up to 5 years imprisonment for spreading “propaganda of homosexuality [ 19 ].” While Russia’s national anti-gay propaganda law was not passed until 2013, the St. Petersburg, other provincial laws, and Ukraine bill (subsequently revoked in 2015 after the conclusion of this study) [ 20 ] received heavy media attention at the time, prompted considerable political and social discussion around the acceptance of homosexuality in Russia, and built substantial support for a possible federal law in Russia. Subsequently, a poll conducted by the Pew Research Center in 2013 found that nearly three in four Russians believed that society should not accept homosexuality [ 21 ]. Political analysts have since suggested that Russian President Vladimir Putin’s stance that homosexuality is a threat to Russian society [ 17 ] is part of a political narrative that deliberately links non-traditional sexualities to an imperialistic West [ 18 ]. Given related literature [ 22 ] and current events in Russia, this research sought to assess the level of depression among MSM in Moscow, Russia, explore the relationship between sexual identity and depressive symptoms among MSM in Russia, and explore the role of environmental changes in acceptance of homosexuality in the Russian Federation as it relates to depression.
The data for this analysis was gathered through a cross-sectional, NIH-funded study conducted in Moscow, Russia, between October 2010 and April 2013. The research was a collaborative effort conducted jointly by Johns Hopkins University and AIDS Infoshare, a local non-governmental organization that provides anonymous HIV testing and counseling and STI screening and treatment in an LGBT-friendly context in Moscow. All sampling, data collection, and biologic testing methods have been previously described [ 7 , 23 ].
Participants
Inclusion criteria required participants to be fluent in Russian, assigned male at birth, aged 18 years or older, currently reside in Moscow, report anal sex with a man in the past 12 months, and provide verbal informed consent. Participants were recruited via respondent-driven sampling (RDS), a chain recruitment method that is used to reach hidden or hard-to-reach populations [ 24 ]. Participants were provided 1000 rubles (approximately $40 USD) as reimbursement for their participation in the study and 500 rubles ($20 USD) for each peer recruited into the study. Thirty-one waves of recruitment produced a sample of 1367 participants for the analysis [ 23 ].
Informed by formative research [ 25 ], cognitive testing [ 26 ], and pilot testing methods, the structured survey was designed to gather information on sociodemographic characteristics, sexual practices and identity, substance use, experienced and perceived stigma, and mental health symptoms. Depression symptoms were the outcome of interest and sexual identity, stigma, and other known correlates [ 13 , 15 , 27 – 30 ] of depression were covariates of interest for this analysis. Measures of sexual identity and practices were adapted from the US CDC’s National Health Behavior Survey [ 31 ] and included questions about sexual identity (“heterosexual,” “homosexual,” “bisexual,” or “other”) and about the sex of the respondent’s sexual partners in the last 12 months (male or female).
The CES-D scale [ 32 ] was used as a screening tool for current (past 7 days) depressive symptomology (Cronbach’s α 0.889). The CES-D score was stratified into three categories: “unlikely to be depressed” (CES-D <16), “possibly depressed” (CES-D 16–22), and “probably depressed” (CES-D ≥23) [ 32 ]. Given that 36.7% endorsed a score of probably depressed ( n = 505) and 11% of the sample scored in the possibly depressed range ( n = 121), coupled with our interest in understanding the factors that were correlated with greater probability of depression [ 33 ], scores were transformed to a binary variable: “unlikely or possibly depressed” (CES-D <23) and probably depressed (CES-D ≥23).
A five-item scale was used to identify recent (last 12 months) experienced stigma (Cronbach’s α 0.713). This was a subscale of a larger stigma scale that had been developed from qualitative research [ 25 ], underwent cognitive testing [ 26 ] among MSM participants for further refinement, and were reviewed by MSM participants to assess face validity. The experienced stigma subscale included experience of public mocking, poor treatment by family members, experience of physical assault, being forced to move accommodation, and experiencing poor treatment within healthcare facilities due to sexual preferences. A positive indication for any one of these five variables was defined as a recent experience of stigma. The alcohol use disorders identification test (AUDIT), a validated scale in Russia, was included in the survey for identification of alcohol use in the last 12 months (Cronbach’s α = 0.80) [ 34 ]. AUDIT scores were stratified into three groups: a score <8 representing abstinence or low use, 8–15 “hazardous use,” and ≥16 “harmful use,” including those with potential alcohol dependency (score of 20 or higher), according to WHO categories [ 35 ].
Statistical Analysis
Survey data were analyzed using the STATA version 14 statistical software (Stata Corporation, College Station, USA). Depression, measured by the CES-D score, was the primary outcome of interest. Descriptive analysis was performed using Pearson’s chi-squared test. Sensitivity analyses were performed first using binary logistic analysis with unlikely to be depressed and a combined “possibly or probably depressed” and then using ordered logistic analysis with all three categories. A final sensitivity analysis was performed to test whether the model results changed with the inclusion of bisexual behavior (reporting both male and female sex partners) in place of bisexual identity.
Data collected via RDS recruitment are often weighted during statistical analysis to provide population prevalence estimates. Population estimates for the population characteristics and depression were calculated using the RDS-II estimator (Volz-Heckathorn) and bootstrapping with 1000 iterations to produce 95% confidence intervals (95%CI) [ 36 ]. Both crude sample proportions and RDS-weighted population prevalence estimates are provided in Appendix .
On exploratory analysis, the linear relationship between CES-D scores and time in which participants were surveyed was evaluated given increasing homophobia and the ultimate passage of the propaganda law. This relationship was significant, thus, we included the date of when participants completed the survey as a covariate in the model. This was transformed to a binary variable with March 7, 2012 as a breakpoint: the date in which the governor of St. Petersburg signed a law banning the sharing of homosexual propaganda [ 37 ]. While our study took place in Moscow City, political and media attention to the St. Petersburg law created an atmosphere of increased violence and discrimination against the LGBT population across Russia. The category for participation in the survey after the passage of the law is also inclusive of other key time periods that signify the deteriorating climate for LGBT populations, including the passage of the draft Ukraine law that received wide support and discussion in Russia (October 2012) and the date when the anti-gay propaganda law was introduced to the Russian Parliament (January 2013) [ 38 ]. Our model tests for an increase in the odds of probable depressive symptoms before and after the St. Petersburg law as a binary variable and as an interaction term with experienced stigma.
Variables known to be associated with depression symptoms (income, sexual identity, experience of stigma, social connectedness, alcohol use) [ 13 , 15 , 27 – 30 ] or with a p value of p < 0.10 in bivariate analysis were included in the multivariable model. The Furnival-Wilson leaps-and-bounds algorithm was used to perform variable selection on a wide array of models with depression as the outcome of interest and socioeconomic, demographic, experiential, and behavioral factors as predictor variables. Akaike’s information criteria were used to select the best model, and multiple logistic regression was used to obtain adjusted odds ratios (AOR) for the variables in the selected model. Collinearity for the model was checked using variance inflation factors (VIFs). While the VIF for the interaction between survey date and experience of stigma was 2.88, all other VIFs were well under 2.0, indicating that collinearity is not of concern. Pearson’s goodness-of-fit test was used to check model fit.
Ethical Review
The study was approved by both the Ethics Committee of the State Medical University, IP Pavlov, St. Petersburg, Russia, and the Johns Hopkins Bloomberg School of Public Health Institutional Review Board, Baltimore, Maryland.
A total of 1376 MSM with a median age of 30 years [IQR 24–36] were enrolled in the study, 85.7% of whom were born within Russia. Over half (55%) identified as homosexual, 42.9% identified as bisexual, and 2.1% identified as other sexual identities, including heterosexual. By contrast, 64.6% reported only male sexual partners, while 35.4% reported both male and female partners in the last 12 months. Thirty-six percent reported experiencing stigma due to their sexual preferences. Over one-third (36.7%) qualified as probably depressed ( n = 505), 11% as possibly depressed ( n = 151), and 52.3% unlikely to be depressed according to the CES-D ( n = 720).
Table Table1 1 presents the participant demographic and behavioral characteristics stratified by depression symptomatology. Appendix Table 1 presents the RDS-weighted estimates stratified by depression symptomatology. Those with symptoms indicating probable depression (CESD ≥23) were more likely to have full-time employment (59.7%) than those with symptoms indicating unlikely or possible depression (CESD <23; 51.4%, p = 0.03). MSM in the probable depression group were more likely to identify as homosexual (64.7% vs. 49.5, p < 0.001) and less likely to report feeling comfortable with their sexual orientation (86.5 vs. 93.2%; p value <0.001) than those in the unlikely/possible depression group. Those with probable depression scores reported higher levels of experienced stigma (62.7 vs. 39.4%; p value <0.001) than those who were possibly/unlikely depressed. A larger proportion of those with probable depression had been detained in jail or prison (8.6%) than those with unlikely/possible depression (4.6%; p value <0.01). A greater proportion of those in the group with probable depression participated in the survey after the “propaganda law” was signed into law in St. Petersburg (61.4%) compared to those in the unlikely/possibly depressed group (48.7%; p value <0.001).
Demographic and behavioral characteristics of MSM in Moscow, Russia, by depression symptomatology from 2010 to 13 ( N = 1376)
Table Table2 2 displays the bivariate and multivariable logistic regression analyses of sexual identity, stigma, passage of the anti-gay propaganda laws, and other correlates with probable depression. After controlling for other confounders, the odds of probable depression was 29% lower among those identifying as bisexual (AOR 0.71 95%CI 0.52–0.97; p = 0.03) as compared to those reporting homosexual identity. The adjusted odds of depression was nearly twice as high for those who reported experiencing stigma in the last 12 months (ref: little/no stigma; AOR 1.75; 95%CI 1.20–2.56; p < 0.01). Those who reported discomfort with their sexual identity had almost sixfold increased odds of depression relative to those who reported feeling comfortable with their sexual identity (AOR 5.85; 95%CI 2.71–12.64; p < 0.001). A history of jail or detention was associated with a nearly twofold increased odds of probable depression (AOR 1.78; 95%CI 1.00–3.17; p = 0.05) compared to those who did not have a history of detention. Probable depression was also 35% lower for those with five or more sexual partners in the last 6 months (ref: ≤1 partner; AOR 0.54; 95%CI 0.37–0.81; p < 0.01).
Crude and adjusted relative odds of depression ( N = 1376)
a Adjusted model includes income, marriage to a woman, sexual identity, comfort with sexual preference, number of sexual partners, experience of stigma, social connectedness to gay space, alcohol use, history of detention in jail or prison, date of taking survey, and time-stigma interaction
Prior to including the interaction between time and experienced stigma in the multivariable model, the adjusted odds of depression for those who were surveyed after the signing of the St. Petersburg propaganda law was 1.5-fold greater than that of participants who were surveyed before the approval of the law (AOR 1.65, 95%CI 1.23–2.22; p = 0.001). After including the interaction between time and experience of stigma in the final model, the adjusted odds of depression associated with the survey date was no longer significant (AOR 1.34, 95%CI 0.95–1.91; p = 0.10). The interaction itself, however, was significant, and computed estimates for the combination with the interaction were highly significant. In this case, among people with experienced stigma, depression increased twofold after the passage of the St. Petersburg law (ref: participation prior to the law; AOR 2.24; 95%CI 1.49–3.39; p < 0.001). Finally, in the period after the law was passed, the odds of probable depression among people with experienced stigma were almost threefold that of those without experienced stigma (AOR 2.92; 95%CI 2.02–4.24; p < 0.001).
A sensitivity analysis was performed with the same multivariable model but including the variable measuring behavioral bisexuality in terms of the gender of reported sex partners in the last 12 months (in lieu of bisexual identity). Here, the association became stronger as the adjusted odds ratio dropped from 0.71 (95%CI 0.52–0.97, p = 0.03) in the previous model to 0.58 (95%CI 0.42–0.81; p < 0.01).
Depression is common in the Russian Federation, and particularly so for MSM. Over a third of MSM in this sample qualified with “probable depression” according to the CES-D scale, and nearly half scored high enough to qualify as at least “possibly depressed.” These estimates for MSM in Russia exceed the general estimates of 23% for possible depression (CES-D cutoff of 16) in men in urban areas of Russia [ 3 ]. While methodological differences and temporal effects may play a role, differences may also be explained, in part, by the high prevalence of experienced stigma and its strong relationship with depressive symptoms.
Evidence has shown that sexual identity may be a correlate of depression and other mental health outcomes. In this study, bisexual identity appears to provide a protective effect against depression among MSM in Russia. Discomfort with sexual identity was also strongly associated with depressive symptoms. The protective relationship between bisexual identity and depression contradicts the general body of research, which predominantly originates from the USA, that has demonstrated increased risk for poor mental health outcomes with bisexual identity and similarly high risk for poor social wellbeing compared to those who identify as homosexual or heterosexual [ 22 ].
One reason for this surprising discrepancy may be the context of increasing and state-sanctioned homophobia in Russia. In a country that has criminalized information related to same sex behaviors, and ultimately criminalized LGBT visibility, the political and social environment has become increasingly hostile towards MSM. The discourse around the anti-gay movement has promoted traditional morals, masculinity, and traditional sexual relations and has been associated with increased violence towards LGBT populations and may decrease individual comfort with one’s sexual identity [ 18 ]. It is possible that endorsing a level of opposite-sex attraction in addition to same-sex attraction allows a degree of psychological refuge from feelings of exclusion, self-stigma, and experiences of violence. Discomfort with sexual identity may further be measuring underlying, internalized homophobia, which has demonstrated significant impact on mental health, including anxiety and depression [ 39 ].
The experience of detention in jail or prison also had a strong relationship with depressive symptoms. While we did not collect information about the reason for imprisonment, it would be interesting to know if sexual identity played either a real or perceived role in the justification for imprisonment.
Several factors limit the inferences of this study. The study was cross-sectional, limiting our ability to determine the temporal relationship between sexual identity and depression and prevents causal association. However, the use of recall periods for experiences of stigma (past 12 months) and depression (past 7 days) allows some interpretation of temporality. We utilized a tool to measure depression symptoms rather than depression diagnosed by a mental health professional, which may potentially misclassify participants; however, the CES-D has been well-established and validated in the Russian context. Enrollment and testing methods, criteria for study inclusion, and financial incentives may have influenced our sample. It is also possible that RDS did not reach particular subgroups within the MSM community. However, this study is unusual in its success of recruiting a large number of MSM (31 waves and over 1300 MSM) in a highly stigmatized setting. Despite potential limitations, RDS seems to have been one of the most productive pathways of recruiting MSM in this context [ 23 ].
Our results show that homosexual identity, experience of stigma, and experience of imprisonment are all associated with depressive symptoms in MSM in Russia. The passing of anti-gay propaganda laws in the region in 2012 and in the Russian Federation in 2013 [ 40 ], which effectively criminalizes information related to homosexual and bisexual identity, further modifies the relationship between stigma and depression among MSM. Because social support has been shown to be protective against depression in MSM in this context [ 41 ], interventions that build social support in the MSM community in Russia and enable access to non-stigmatizing mental health services may help to combat the negative effects of stigma and help protect against depression in this population.
Electronic Supplementary Material
Below is the link to the electronic supplementary material.
(DOCX 35 kb)
Acknowledgements
We wish to thank SANAM clinic and Tatiana Bondarenko for insight, support, and use of the SANAM clinic for conduct of qualitative research and the Be Safe study. We appreciate the efforts put forth by Irina Deobald and Konstantin Dyakonov in the formative phases of this project. We are deeply thankful to the participants who contributed their time and personal experiences to this study.
Authors’ Contributions
CB, ALW, CEZ, NG, VM, AP, and CL collaborated in the design and oversight of the overall study. PD and KI collected data. EH conducted data analysis. ALW reviewed and provided input to the statistical analysis. EH and ALW wrote the initial drafts of this manuscript. All authors had full access to the data, reviewed and edited the manuscript, and all take responsibility for its integrity as well as the accuracy of the analysis.
Compliance with Ethical Standards
Funding for this study came from the National Institute of Mental Health (NIMH R01 MH085574-01A2) “High Risk Men: Identity, Health Risks, HIV and Stigma” funded from 2009 to 2014. Drs. Wirtz, Latkin, Galai, and Beyrer are also supported by the Johns Hopkins University Center for AIDS Research (P30AI094189).
- Program Finder
- Admissions Services
- Course Directory
- Academic Calendar
- Hybrid Campus
- Lecture Series
- Convocation
- Strategy and Development
- Implementation and Impact
- Integrity and Oversight
- In the School
- In the Field
- In Baltimore
- Resources for Practitioners
- Articles & News Releases
- In The News
- Statements & Announcements
- At a Glance
- Student Life
- Strategic Priorities
- Inclusion, Diversity, Anti-Racism, and Equity (IDARE)
- What is Public Health?
Joint ERC/CIRP/POE Seminar: Workplace Mental Health
Department & Center Event
Zhiqing (Albert) Zhou,PhD, studies how employees' work-related experiences can contribute to their health, well-being, and safety.
Sponsored by:
The Johns Hopkins Education and Research Center (ERC) for Occupational Safety and Health Johns Hopkins Center for Injury Research and Policy (CIRP) The Johns Hopkins POE Total Worker Health® Center
Zhiqing (Albert) Zhou, PhD
Associate Professor Department of Mental Health Hopkins Business of Health Initiative The Johns Hopkins P.O.E. Total Worker Health® Center (POE Center) Johns Hopkins Bloomberg School of Public Health
Workplace mental health
Registration
REGISTER HERE to attend via zoom.
Contact Info
Related content.

Research Identifies Characteristics of Cities That Would Support Young People’s Mental Health

How Abortion Trigger Laws Impact Mental Health

Johns Hopkins Bloomberg School of Public Health Wins 8 Anthem Awards

Analysis of U.S. Census Survey Data Reveals Uptick in Anxiety and Depression Among Women in States with Trigger Laws Post-Dobbs Abortion Decision

PTSD: A Legacy of Manipur’s Enduring Conflict
Advertisement
Sexual Identity, Stigma, and Depression: the Role of the “Anti-gay Propaganda Law” in Mental Health among Men Who Have Sex with Men in Moscow, Russia
- Published: 27 February 2017
- Volume 94 , pages 319–329, ( 2017 )
Cite this article

- Emily Hylton 1 ,
- Andrea L. Wirtz 1 ,
- Carla E. Zelaya 1 ,
- Carl Latkin 2 ,
- Alena Peryshkina 3 ,
- Vladmir Mogilnyi 3 ,
- Petr Dzhigun 3 ,
- Irina Kostetskaya 3 ,
- Noya Galai 1 , 4 &
- Chris Beyrer 1
2690 Accesses
44 Citations
10 Altmetric
Explore all metrics
Depression is a major public health problem in the Russian Federation and is particularly of concern for men who have sex with men (MSM). MSM living in Moscow City were recruited via respondent-driven sampling and participated in a cross-sectional survey from October 2010 to April 2013. Multiple logistic regression models compared the relationship between sexual identity, recent stigma, and probable depression, defined as a score of ≥23 on the Center for Epidemiological Studies Depression scale. We investigated the interactive effect of stigma and participation in the study after the passage of multiple “anti-gay propaganda laws” in Russian provinces, municipalities, and in neighboring Ukraine on depression among MSM. Among 1367 MSM, 36.7% ( n = 505) qualified as probably depressed. Fifty-five percent identified as homosexual ( n = 741) and 42.9% identified as bisexual ( n = 578). Bisexual identity had a protective association against probable depression (reference: homosexual identity AOR 0.71; 95%CI 0.52–0.97; p < 0.01). Those who experienced recent stigma (last 12 months) were more likely to report probable depression (reference: no stigma; AOR 1.75; 95%CI 1.20–2.56; p < 0.01). The interaction between stigma and the propaganda laws was significant. Among participants with stigma, probable depression increased 1.67-fold after the passage of the anti-gay laws AOR 1.67; 95%CI 1.04–2.68; p < 0.01). Depressive symptoms are common among MSM in Russia and exacerbated by stigma and laws that deny homosexual identities. Repeal of Russia’s federal anti-gay propaganda law is urgent but other social interventions may address depression and stigma in the current context.
This is a preview of subscription content, log in via an institution to check access.
Access this article
Price includes VAT (Russian Federation)
Instant access to the full article PDF.
Rent this article via DeepDyve
Institutional subscriptions
Similar content being viewed by others

Filipino help-seeking for mental health problems and associated barriers and facilitators: a systematic review
Social Media Addiction and Mental Health Among University Students During the COVID-19 Pandemic in Indonesia

The Stigma of Personality Disorders
Whiteford HA, Degenhardt L, Rehm J, et al. Global burden of disease attributable to mental and substance use disorders: findings from the global burden of disease study. Lancet . 2010; 382(9904): 1575–1586.
Article Google Scholar
Ferrari AJ, Charlson FJ, Norman RE, et al. Burden of depressive disorders by country, sex, age, and year: findings from the global burden of disease study 2010. PLoS Med . 2013. doi: 10.1371/journal.pmed.1001547 .
PubMed PubMed Central Google Scholar
Bobak M, Pikhart H, Pajak AK, et al. Depressive symptoms in urban population samples in Russia, Poland and the Czech Republic. Br J Psychiatry . 2006; 188(4): 359–365. doi: 10.1192/bjp.188.4.359 .
Article PubMed Google Scholar
World Health Organization. Preventing suicide: a global imperative. Geneva, Switzerland: World Health Organization; 2014. http://www.who.int/mental_health/suicide-prevention/world_report_2014/en/ . Accessed 30 August 2016.
King M, Semlyen J, Tai SS, et al. A systematic review of mental disorder, suicide, and deliberate self harm in lesbian, gay and bisexual people. BMC Psychiatry. 2008; 8(70). doi: 10.1186/1471-244X-8-70 .
Wirtz AL, Zelaya CE, Latkin C, et al. The HIV care continuum among men who have sex with men in Moscow, Russia: a cross-sectional study of infection awareness and engagement in care. Sex Transm Infect . 2016; 92: 161–167. doi: 10.1136/sextrans-2015-052076 .
Article CAS PubMed Google Scholar
Wirtz AL, Zelaya CE, Latkin C, et al. Alcohol use and associated sexual and substance use behaviors among men who have sex with men in Moscow, Russia. AIDS Behav . 2016; 20: 523–536.
Article CAS PubMed PubMed Central Google Scholar
Mayer KH, Bekker LG, Stall R, et al. Comprehensive clinical care for men who have sex with men: an integrated approach. Lancet . 2012; 380(9839): 378–387. doi: 10.1016/S0140-6736(12)60835-6 .
Wirtz AL, Kirey A, Peryskina A, et al. Uncovering the epidemic of HIV among men who have sex with men in Central Asia. Drug Alcohol Depend . 2013; 132(1): S17–S24. doi: 10.1016/j.drugalcdep.2013.06.031 .
Latypov A, Rhodes T, Reynolds L. Prohibition, stigma, and violence against men who have sex with men: effects on HIV in Central Asia. Central Asian Survey. 2013; 32(1): 52–65. doi: 10.1080/02634937.2013.768059 .
Republic of Tajikistan. Tajikistan National AIDS spending assessment (2008–09) flow of resources and expenditures for the response to HIV and AIDS . Dushanbe, Tajikistan: National Coordination Committee to Combat HIV/AIDS, TB, and Malaria in the Republic of Tajikistan, MoH of the Republic of Tajikistan; 2011.
Itaborahy LP, Zhu J. State-sponsored homophobia: a world survey of laws criminalizing same-sex sexual acts between consenting adults. In: International Lesbian, Gay, Bisexual, Trans, and Intersex Association. ILGA report. ILGA. http://old.ilga.org/Statehomophobia/ILGA_State_Sponsored_Homophobia_2015.pdf . Accessed 30 Aug 2016.
Stahlman S, Grosso A, Ketende S, et al. Depression and social stigma among MSM in lesotho: implications for HIV and sexually transmitted infection prevention. AIDS Behav . 2015; 19(8): 1460–1469. doi: 10.1007/s10461-015-1094-y .
Article PubMed PubMed Central Google Scholar
Choi KH, Steward WT, Miege P, et al. Sexual stigma, coping styles, and psychological distress: a longitudinal study of men who have sex with men in Beijing, China. Arch Sex Behav . 2016; 45(6): 1483–1491. doi: 10.1007/s10508-015-0640-z .
Deuba K, Ekström AM, Shrestha R, et al. Psychosocial health problems associated with increased HIV risk behavior among men who have sex with men in Nepal: a cross-sectional survey. PLoS One. 2013;8(3). doi: 10.1371/journal.pone.0058099 .
Li J, Mo PK, Wu AM, et al. Roles of self-stigma, social support, and positive and negative effects as determinants of depressive symptoms among HIV infected men who have sex with men in China. AIDS Behav. Published online first. 2016. doi: 10.1007/s10461-016-1321-1 .
Persson E. Banning “homosexual propaganda”: belonging and visibility in contemporary Russian media. Sex Cult . 2015; 19: 256–274. doi: 10.1007/s12119-014-9254-1 .
Bartholomew RE. Beware the medicalisation of deviance in Russia: remembering the lessons of history. J R Soc Med . 2014; 107(5): 176–177. doi: 10.1177/0141076814532393 .
Roberts S. Ukraine gives initial approval to anti-gay law. Pink News. http://www.pinknews.co.uk/2012/10/02/ukraine-gives-initial-approval-to-anti-gay-law/ . Accessed 30 Aug 2016.
Draft law of ex-MP Kolesnichenko banning “gay propaganda” was removed from consideration in Verkhovna Rada. Gay Alliance Ukraine. http://upogau.org/eng/inform/uanews/worldnews_975.html . Accessed 16 Dec 2016.
Reilly K. Russia’s anti-gay laws in line with public’s views on homosexuality . Washington, DC: Pew Research Center; 2013.
Google Scholar
Kertzner RM, Meyer IH, Frost DM, et al. Social and psychological well-being in lesbians, gay men, and bisexuals: the effects of race, gender, age, and sexual identity. Am J Orthopsychiatry . 2009; 79(4): 500–510. doi: 10.1037/a0016848 .
Wirtz AL, Mehta SH, Latkin C, et al. Comparison of respondent-driven sampling estimators to determine HIV prevalence and population characteristics among men who have sex with men in Moscow, Russia. PLoS One. Published online first. 2016. doi: 10.1371/journal.pone.0155519
Magnani R, Sabin K, Saidel T, et al. Review of sampling hard-to-reach and hidden populations for HIV surveillance. AIDS . 2005; 19(Suppl 2): S67–S72.
Wirtz A, Zelaya C, Peryshkina A, et al. Social and structural risks for HIV among migrant and immigrant men who have sex with men in Moscow, Russia: implications for prevention. AIDS Care . 2013; 26: 387–395. doi: 10.1080/09540121.2013.819407 .
Willis G. Cognitive interviewing and questionnaire design: a training manual. Rockville, MD: National Center for Health Statistics. 1994, Working Paper #7.
Ahaneku H, Ross MW, Nyoni JE, et al. Depression and HIV risk among men who have sex with men in Tanzania. AIDS Care . 2016; 1: 140–147. doi: 10.1080/09540121.2016.1146207 .
Secor AM, Wahome E, Micheni M, et al. Depression, substance abuse and stigma among men who have sex with men in coastal Kenya. AIDS . 2015; 29(3): S251–S259. doi: 10.1097/QAD.0000000000000846 .
Tomori C, McFall AM, Srikrishnan AK, et al. Diverse rates of depression among men who have sex with men (MSM) across India: insights from a multi-site mixed method study. AIDS Behav . 2016; 20(2): 304–316. doi: 10.1007/s10461-015-1201-0 .
Safren SA, Thomas BE, Mimiaga MJ, et al. Depressive symptoms and human immunodeficiency virus risk behavior among men who have sex with men in Chennai, India. Psychol Health Med . 2009; 14(6): 705–715. doi: 10.1080/13548500903334754 .
MacKellar DA, Gallagher KM, Finlayson T, et al. Surveillance of HIV risk and prevention behaviors of men who have sex with men—a national application of venue-based, time-space sampling. Public Health Rep . 2007; 122(Suppl 1): 39–47.
Radloff LS. The CES-D scale: a self-report depression scale for research in general population. Appl Psychol Meas . 1977; 1: 385–401.
Stall R, Mills TC, Williamson J, et al. Association of co-occurring psychosocial health problems and increased vulnerability to HIV/AIDs among urban men who have sex with men. Am J Public Health . 2003; 93(6): 939–942.
Saunders JB, Aasland OG, Babor TF, et al. Development of the alcohol-use disorders identification test (AUDIT)—WHO collaborative project on early detection of persons with harmful alcohol-consumption. Addiction . 1993; 88(6): 791–804.
Babor T, Higgins-Biddle J, Saunders JB, Monteiro M. The alcohol use disorders identification test: guidelines for primary care . Geneva, Switzerland: WHO; 2001.
Schonlau M, Liebau E. Respondent-driven sampling. Stata J . 2012; 12(1): 72–93.
Elder M. St. Petersburg bans ‘homosexual propaganda.’ The Guardian. 2012. https://www.theguardian.com/world/2012/mar/12/st-petersburg-bans-homosexual-propaganda . Accessed 30 Aug 2016.
Baczynska G, de Corbonnel A. Russian parliament backs ban on “gay propaganda.” Reuters . http://www.reuters.com/article/us-russia-gay-idUSBRE90O0QT20130125 . Accessed 30 Aug 2016.
Igartua KJ, Gill K, Montoro R. Internalized homophobia: a factor in depression, anxiety, and suicide in the gay and lesbian population. Can J Commun Ment Health . 2003; 22(2): 15–30. doi: 10.7870/cjcmh-2003-0011 .
O Vnesenii Izmenenij v Stat’ju 5 Federal’nogo Zakona “O Zasite Detej ot Informacii, PricinJajusej Vred ih Zdorov’ju i Razvitiju” i Otdel’nye Zakonodatel’nye Akty Rossijskoj Federacii v Celjah Zasity Detej ot Informacii, Propagandirujusej Otricanie Tradicionnyh Semejnyh Cennostej [On Amendments to Article 5 of the Federal Law “On Protection of Children from Information Harmful to Their Health and Development” and to Certain Legislative Acts of the Russian Federation with the Aim of Protecting Children from Information that Promotes the Denial of Traditional Family Values]. Moscow: Sobranie Zakonodatel’stva Rossiiskoi Federatsii [Russian Federation Collection of Legislation]; 2013. No. 26, Item 3208. Russian. http://asozd2.duma.gov.ru/main.nsf/(Spravka)?OpenAgent&RN=44554-6&02 [ http://perma.cc/Y2WQ-EFXH ]. Accessed 30 Aug 2016.
Logie CH, Newman PA, Chakrapani V, et al. Adapting the minority stress model: associations between gender non-conformity stigma, HIV-related stigma and depression among men who have sex with men in South India. Soc Sci Med . 2012; 74(8): 1261–1268. doi: 10.1016/j.socscimed.2012.01.008 .
Download references
Acknowledgements
We wish to thank SANAM clinic and Tatiana Bondarenko for insight, support, and use of the SANAM clinic for conduct of qualitative research and the Be Safe study. We appreciate the efforts put forth by Irina Deobald and Konstantin Dyakonov in the formative phases of this project. We are deeply thankful to the participants who contributed their time and personal experiences to this study.
Authors’ Contributions
CB, ALW, CEZ, NG, VM, AP, and CL collaborated in the design and oversight of the overall study. PD and KI collected data. EH conducted data analysis. ALW reviewed and provided input to the statistical analysis. EH and ALW wrote the initial drafts of this manuscript. All authors had full access to the data, reviewed and edited the manuscript, and all take responsibility for its integrity as well as the accuracy of the analysis.
Author information
Authors and affiliations.
Center for Public Health and Human Rights, Department of Epidemiology, Johns Hopkins Bloomberg School of Public Health, 615 N. Wolfe St., Room E7141, Baltimore, MD, 21205, USA
Emily Hylton, Andrea L. Wirtz, Carla E. Zelaya, Noya Galai & Chris Beyrer
Department of Health, Behavior and Society, Johns Hopkins Bloomberg School of Public Health, Baltimore, MD, USA
Carl Latkin
AIDS Infoshare, Moscow, Russian Federation
Alena Peryshkina, Vladmir Mogilnyi, Petr Dzhigun & Irina Kostetskaya
Department of Statistics, The University of Haifa, Mt Carmel, Israel
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Andrea L. Wirtz .
Ethics declarations
The study was approved by both the Ethics Committee of the State Medical University, IP Pavlov, St. Petersburg, Russia, and the Johns Hopkins Bloomberg School of Public Health Institutional Review Board, Baltimore, Maryland.
Funding for this study came from the National Institute of Mental Health (NIMH R01 MH085574-01A2) “High Risk Men: Identity, Health Risks, HIV and Stigma” funded from 2009 to 2014. Drs. Wirtz, Latkin, Galai, and Beyrer are also supported by the Johns Hopkins University Center for AIDS Research (P30AI094189).
Electronic Supplementary Material
Below is the link to the electronic supplementary material.
(DOCX 35 kb)
Rights and permissions
Reprints and permissions
About this article
Hylton, E., Wirtz, A.L., Zelaya, C.E. et al. Sexual Identity, Stigma, and Depression: the Role of the “Anti-gay Propaganda Law” in Mental Health among Men Who Have Sex with Men in Moscow, Russia. J Urban Health 94 , 319–329 (2017). https://doi.org/10.1007/s11524-017-0133-6
Download citation
Published : 27 February 2017
Issue Date : June 2017
DOI : https://doi.org/10.1007/s11524-017-0133-6
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Men who have sex with men
- Homosexuality
- Bisexuality
- Criminal law
- Russian Federation
- Find a journal
- Publish with us
- Track your research
Sexual Identity, Stigma, and Depression: the Role of the "Anti-gay Propaganda Law" in Mental Health among Men Who Have Sex with Men in Moscow, Russia
Affiliations.
- 1 Center for Public Health and Human Rights, Department of Epidemiology, Johns Hopkins Bloomberg School of Public Health, 615 N. Wolfe St., Room E7141, Baltimore, MD, 21205, USA.
- 2 Center for Public Health and Human Rights, Department of Epidemiology, Johns Hopkins Bloomberg School of Public Health, 615 N. Wolfe St., Room E7141, Baltimore, MD, 21205, USA. [email protected].
- 3 Department of Health, Behavior and Society, Johns Hopkins Bloomberg School of Public Health, Baltimore, MD, USA.
- 4 AIDS Infoshare, Moscow, Russian Federation.
- 5 Department of Statistics, The University of Haifa, Mt Carmel, Israel.
- PMID: 28243868
- PMCID: PMC5481210
- DOI: 10.1007/s11524-017-0133-6
Depression is a major public health problem in the Russian Federation and is particularly of concern for men who have sex with men (MSM). MSM living in Moscow City were recruited via respondent-driven sampling and participated in a cross-sectional survey from October 2010 to April 2013. Multiple logistic regression models compared the relationship between sexual identity, recent stigma, and probable depression, defined as a score of ≥23 on the Center for Epidemiological Studies Depression scale. We investigated the interactive effect of stigma and participation in the study after the passage of multiple "anti-gay propaganda laws" in Russian provinces, municipalities, and in neighboring Ukraine on depression among MSM. Among 1367 MSM, 36.7% (n = 505) qualified as probably depressed. Fifty-five percent identified as homosexual (n = 741) and 42.9% identified as bisexual (n = 578). Bisexual identity had a protective association against probable depression (reference: homosexual identity AOR 0.71; 95%CI 0.52-0.97; p < 0.01). Those who experienced recent stigma (last 12 months) were more likely to report probable depression (reference: no stigma; AOR 1.75; 95%CI 1.20-2.56; p < 0.01). The interaction between stigma and the propaganda laws was significant. Among participants with stigma, probable depression increased 1.67-fold after the passage of the anti-gay laws AOR 1.67; 95%CI 1.04-2.68; p < 0.01). Depressive symptoms are common among MSM in Russia and exacerbated by stigma and laws that deny homosexual identities. Repeal of Russia's federal anti-gay propaganda law is urgent but other social interventions may address depression and stigma in the current context.
Keywords: Bisexuality; Criminal law; Depression; Homosexuality; Men who have sex with men; Russian Federation; Stigma.
Publication types
- Comparative Study
- Bisexuality / psychology*
- Cross-Sectional Studies
- Depressive Disorder / etiology
- HIV Infections / psychology*
- Homosexuality, Male / psychology*
- Homosexuality, Male / statistics & numerical data*
- Logistic Models
- Middle Aged
- Risk-Taking
- Sexual Behavior / psychology*
- Sexual Behavior / statistics & numerical data*
- Sexual and Gender Minorities / legislation & jurisprudence*
- Social Stigma
- Young Adult
Grants and funding
- P30 AI094189/AI/NIAID NIH HHS/United States
- R01 MH085574/MH/NIMH NIH HHS/United States

IMAGES
VIDEO
COMMENTS
Students earn their professional degrees in law and psychology in a total of seven years. The program combines coursework with a year-long internship in a mental health/forensic setting, a master's thesis, a dissertation, a co-op placement in a legal setting and 50 hours of pro bono service in the law.
The JD/PhD Program faculty conduct research and produce scholarship in a variety of psychology-law topic areas, including: mental health law, violence risk assessment, psychopathic personality, diversion and problem-solving courts, forensic mental health assessment, and juvenile justice reform.
Funding may come in the form of a Teaching or Research assistantship, which involves 20 hours per week of responsibilities. The average amount of support for a 20-hour TA/RA academic year position at in our program is a $28,000-$30,000 stipend, health insurance, and full tuition remission. Summer funding is available (typically $8,000-$10,000 ...
The MHS is a nine-month degree program that provides a foundation in the research methods and content-area knowledge essential to public mental health. Doctoral Doctor of Philosophy (PhD) in Mental Health. The PhD program provides advanced training in the application of research methods to understand and enhance public mental health. Combined
JD/PhD Psychology. The JD/PhD Program is an in-depth, cross disciplinary path designed to expose lawyers and psychologists to the growing number of issues that involve both fields, such as competence, mental illness, and incapacity, and the field of behavioral law and economics. Program Course Overview. Financial Aid. How to Apply.
This course will explore some of the major challenges in designing and implementing mental health law and policy in the 21st century. The subjects studied will include emergency mental health interventions and safe and effective responses to persons experiencing mental health crises; reducing access to firearms by people at elevated risk of suicide or violence; criteria for involuntary ...
Stanford Law School is second to none as a training ground for tomorrow's leaders in health law and policy. Four renowned Law School faculty members offer courses in health care law, public health law, and bioethics and advise students interested in careers in the field. Courses in mental health law, food and drug law, mass tort litigation ...
The PhD degree is a research-oriented doctoral degree. In the first two years, students take core courses in the Departments of Mental Health, Biostatistics, and Epidemiology, in research ethics, and attend weekly department seminars. Students must complete a written comprehensive exam (in January of their second year), a preliminary exam, two ...
[email protected]. 602-543-3000. Admission deadlines. Laws are written to maintain order among people in society while psychology studies why people do what they do. This program melds the two fields to help explain how human behavior interacts with and is impacted by the legal system.
International law and the psychological impact of warfare on civilians. Brunel University London Law. Drawing on the emerging field of psychology of international law, the PhD student will examine how international law discusses or should discuss civilian mental harm in warfare from a substantive as well as procedural point of view. Read more.
Saks received her JD from Yale Law School, and a PhD in Psychoanalytic Science from the New Center for Psychoanalysis. She was also awarded an Honorary Doctor of Laws degree (LLD, Hon) from Pepperdine University. Saks writes extensively in the area of law and mental health, having published five books and more than fifty articles and book chapters.
The Center for Mental Health, Policy, and the Law (CMHPL) fosters integrative scholarship to advance empirical knowledge, training, and practice in forensic mental health. The CMHPL's mission is to address the most urgent issues arising at the interface of mental health and the law, in order to help justice-involved people with mental illness ...
Here are the Best Health Care Law Programs. Georgia State University. Saint Louis University. Boston University. Loyola University Chicago. University of Maryland (Carey) Georgetown University ...
an online mental health resource for students, to identify the legal and ethical issues they found most challenging when working with students in distress. Hundreds of IHE administrators and health/mental health professionals took part in the survey, and this document was designed to address some of the key challenges, including: •
The Department of Mental Health Law (MHLP) promotes the health and quality of life of people with mental and substance use disorders by creating, evaluating, disseminating and translating state-of-the-art knowledge to support effective practice across behavioral health and criminal justice systems.
Moore, Kathleen, PhD. Title: Research Professor. Phone: (813) 974-2295. Office: MHC 2712. Send email. Curriculum Vitae. Kathleen A. Moore, Ph.D. is a Research Professor in the Department of Mental Health, Law, and Policy of the Louis de la Parte Florida Mental Health Institute (FMHI) at the University of South Florida.
John Monahan, a psychologist, teaches and writes about how courts use behavioral science evidence, violence risk assessment, criminology and mental health law. He is a member of the National Academy of Medicine and of the American Academy of Arts and Sciences and has served on the National Research Council. Monahan was the founding president of the American Psychological Association's ...
SHPS Doctoral Enquiries. +44 (0) 20 7040 5972. [email protected]. Help us to improve this page. A PhD/MPhil in Mental Health at City, University of London offers you the opportunity to carry out research that will make a real difference to people's lives.
From Our Faculty. "The Graduate Certificate in Health Law is designed for professionals who would like to continue a career in healthcare, but shift their focus to management responsibilities. The certificate can help individuals make this transition by understanding the legal architecture and the role of compliance in the health industry."
It is evident from these and other such findings of research that addressing mental health issues through law and policy is an urgent need for India. The right to a standard of living adequate for health and well-being has been proclaimed as a human right by the Universal Declaration of Human Rights. As a logical corollary, mental health is an ...
On March 18, at 11.00 (Moscow time), the All-Russian online Conference "Law and Mental Health" will be held, which is aimed at raising awareness on legal regulation of mental healthcare provision among students of legal specialties in Russia. Organized by: Law Department of Lomonosov Moscow State University, Department of Psychology of ...
Depression and other mental health disorders represent a large proportion of the global burden of disease and are the second leading cause of global disability [1, 2]. In the Russian Federation, this trend is consistent, if not magnified, among men. ... The law effectively legitimized public stigma and violence against lesbian, gay, bisexual ...
Zhiqing (Albert) Zhou,PhD, studies how employees' work-related experiences can contribute to their health, well-being, and safety. Zhiqing (Albert) Zhou,PhD, studies how employees' work-related experiences can contribute to their health, well-being, and safety. ... How Abortion Trigger Laws Impact Mental Health. February 06, 2024. Johns Hopkins ...
The earmark includes $8.2 million for court-based mental health navigators who build relationships with individuals arraigned in criminal courts, with the goal of reducing recidivism and ...
Depression is a major public health problem in the Russian Federation and is particularly of concern for men who have sex with men (MSM). MSM living in Moscow City were recruited via respondent-driven sampling and participated in a cross-sectional survey from October 2010 to April 2013. Multiple logistic regression models compared the relationship between sexual identity, recent stigma, and ...
Dr. Nev Jones will give a keynote address at the 2024 Psychosis CARE Virtual Conference, which is inviting a broad audience (school staff, PCPs, mental health therapists, SUD professionals, law enforcement, families, individuals with lived experience, etc.) to gather virtually to engage in Community Awareness, Resources, and Education as it relates to Psychosis.
The interaction between stigma and the propaganda laws was significant. Among participants with stigma, probable depression increased 1.67-fold after the passage of the anti-gay laws AOR 1.67; 95%CI 1.04-2.68; p < 0.01). Depressive symptoms are common among MSM in Russia and exacerbated by stigma and laws that deny homosexual identities.