- Open access
- Published: 01 December 2022

Building connections between biomedical sciences and ethics for medical students
- Oluwaseun Olaiya 1 ,
- Travis Hyatt 2 ,
- Alwyn Mathew 2 ,
- Shawn Staudaher 2 ,
- Zachary Bachman 3 &
- Yuan Zhao 4
BMC Medical Education volume 22 , Article number: 829 ( 2022 ) Cite this article
2432 Accesses
1 Citations
4 Altmetric
Metrics details
Medical ethics education is crucial for preparing medical students to face ethical situations that can arise in patient care. Instances of ethics being integrated into biomedical science education to build the connection between human science and ethics is limited. The specific aim of this study was to measure student attitudes towards an innovative curriculum design that integrates ethics education directly into a biomedical science course in pre-clinical medical curriculum.
In this cross-sectional study, three ethics learning modules were designed and built in a biomedical science course in the pre-clinical curriculum. All students of Class of 2024 who were enrolled in the course in 2021 were included in the study. Each module integrated ethics with basic science topics and was delivered with different teaching modalities. The first module used a documentary about a well-known patient with severe combined immunodeficiency disease. The second module was delivered through a clinical scenario on HIV infection. The third module used small group discussion and debate on the topic of blood transfusion. For evaluation, students were asked to self-identify the ethical challenges associated with each module and complete reflective writing to assess their knowledge and attitude. Quantitative and qualitative analyses were conducted on student perceptions of each module.
Likert scale ratings on the usefulness of each module revealed significantly higher ratings for the small group discussion/debate module, seconded by the documentary and lastly the case scenario only modules. Narrative analysis on student feedback revealed three themes: General favorable impression , Perceived learning outcomes , and Critiques and suggestion . Common and unique codes were identified to measure the strengths and weaknesses of each module. Overall, students’ perception of the curriculum design was extremely positive.
Conclusions
This curriculum design enabled us to highlight foundational biomedical sciences and clinical conditions with ethical dilemmas that physicians are likely to face in practice. Students found value in the modules, with a preference for the most active learning method. This study provides insight on a novel approach for integrating medical ethics into biomedical science courses that can be tailored to any institution. Strategies learned include utilizing active learning modalities and discussion.
Peer Review reports
Medical ethics is the study of the moral issues inherent in the practice of medicine, including, among many other topics, the moral choices physicians face in their day-to-day interactions with patients, colleagues, and the broader society in which they practice [ 1 , 2 , 3 , 4 ]. Knowledge of medical ethics is crucial for training morally competent healthcare professionals to manage ethical considerations that arise in patient care [ 5 ]. Evolving health care systems, expanding involvement of allied health professionals, and advances in technologies and treatment regimens have given rise to increasingly complex moral dilemmas faced by medical professionals in everyday practice. There is thus a compelling argument to continuously improve the incorporation of medical ethics into both pre-clinical and clinical medical education.
In the Association of American Medical Colleges published curriculum report, 143 out of 145 allopathic medical schools covered medical ethics in either a required or an elective course in 2016-2017 academic year [ 6 ]. The curriculum topics reported by the American Association of College of Osteopathic Medicine shows all osteopathic medical schools checked off medical ethics in a required course or rotation and 21 out of 38 schools had it covered in a selective/elective course or rotation in academic year of 2017-2018 [ 7 ]. Not surprisingly, reports on medical student perspectives of ethics education have revealed strong recognition of the importance of ethics as part of their medical training and a perceived need and desire for more formal bioethical education [ 8 , 9 ]. Although there is consensus from both faculty and students that medical ethics is an important part of medical training, literature suggests notable heterogeneity across medical schools regarding the best practice of teaching medical ethics [ 10 , 11 , 12 ].
Various pedagogical approaches have been employed to teach this subject, including the content, method, and timing of ethics education [ 10 , 13 , 14 ]. In the aspect of curriculum design, ethics inclusion in pre-clinical medical education has been done through various strategies. In addition to the most common traditional stand-alone ethics course, other approaches have also been explored, such as elective courses, students’ medical ethics rounds, a scholarly concentration program, etc [ 15 , 16 , 17 , 18 ]. Various formats of delivery have been reported as well, including small group session, case-based teaching, narrative approach, peer-based teaching, team-based learning, etc [ 15 , 19 , 20 , 21 ]. A commonality among these various pedagogical approaches is that the ethics content is delivered in a way that tends to treat ethics as a distinct subject matter that students are required to learn.
A core component of medical education is, of course, also learning the sciences related to understanding the human body. Many of the ethical challenges that doctors face – such as recruiting patients for clinical trials or securing informed consent for an invasive procedure – are directly related to the science that students learn in pre-clinical biomedical education. When an ethics education is cleaved off from the underlying context that gives rise to the ethical issues being studied, it is natural to treat ethics and the sciences core to medicine as inhabiting separate realms: after all, ethics studies how the world ought to be while science studies how the world is . Ethical norms often become viewed as a set of norms externally imposed on scientists and doctors, rather than norms internal to their practice [ 22 ]. But since medicine is fundamentally about using science to treat disease and illness in the context of a doctor-patient relationship, it stands to reason that the aim of the practice of medicine is to use science in a way consistent with the moral norms that govern the doctor-patient relationship. A good doctor, in other words, is one who uses science in an ethical manner to promote healing. Given the way in which ethics and science are interwoven in medical practice, we asked the question whether ethics could be integrated in biomedical science curriculum of pre-clinical medical training. While a review of literature has revealed recent efforts to implement ethics education into science education [ 23 , 24 , 25 , 26 ], we couldn’t find any discussion of efforts to embed ethics curriculum within the biomedical science curriculum in particular, except for anatomy [ 27 ].
Given the rationale above, we initiated a project to develop strategies for medical educators to integrate ethics modules into biomedical science courses, with the aim of promoting student awareness of how scientific practice and ethics are interrelated. Our first step in this project, which this paper analyzes, was to assess student attitudes towards the inclusion of ethics modules in pre-clinical biomedical science courses - how will students respond to this new course design? Future objectives, not undertaken here, will be to measure student learning as a result of our interventions, assess the effectiveness of different inclusion strategies, and create a framework that other medical educators can use in their courses.
Our study concerns a curriculum design we implemented that incorporates ethics threads in a pre-clinical biomedical science course using various teaching modalities. Our model enabled us to highlight the pathophysiology and clinical presentations of the disorders, along with ethical dilemmas that physicians are likely to face in clinical practice. By learning biomedical science side-by-side with medical ethics, students could make meaningful connections between the two domains. We believe this pedagogical approach of teaching medical ethics can help students better understand the relationship between science and ethics in medical practice as well as build richer “organizational structures” of knowledge that will aid in the retention and application of information [ 28 , 29 ]. This curriculum design can also shed light on how to incorporate ethics education creatively and effectively in the pre-clinical medical curriculum.
This study was conducted at Sam Houston State University College of Osteopathic Medicine in 2021. Three ethics learning modules were designed and built in a six-week system course “Immune System and HEENT” (HEENT: Head, Eyes, Ears, Nose, Throat) which was offered in the spring semester of the first year of pre-clinical curriculum. In this course, students were introduced to the principles of trauma, inflammatory disorders, infections and cancers associated with HEENT as it relates to the immune system. Students learned to apply the basic concepts of immunology in normal and disease states and to diagnose, prevent, and treat infections, cancers and immunological diseases. All students from our institute who were enrolled in this course in 2021 were included in the study. These students were in their first year of a four-year Doctor of Osteopathic Medicine program. A total of 74 first-year medical students in the Class of 2024 were enrolled in the course and completed all three modules and assessments. Forty were males and thirty-four were females. The average age of the cohort was 26 years ranging from 23 to 45 years.
The learning objectives of the ethics modules were identified and standardized based on the Romanell Report [ 28 ] which reviewed medical ethics education in the United States and offers suggestions for objectives, teaching methods, and assessment strategies.
The design of the three modules is presented in Table 1 .
The first module used a documentary about David Vetter, a well-known pediatric patient with severe combined immunodeficiency disease. After students completed the session “Introduction of the Immune System”, they were provided an asynchronous ethics module in a learning management software and assigned a one-hour long documentary named The Boy in the Bubble released in 2006 by PBS [ 29 ], and then completed the assessments at their own time. The second module used a clinical case on human immunodeficiency virus (HIV) that was introduced in team-based learning (TBL), a form of peer collaboration. This case concerned a patient diagnosed with HIV and the dual roles of physician as mandatory reporter of communicable disease and protector of patient confidentiality. Immediately following the two-hour TBL, the students were provided assessments to be completed on their own. The third module was a one-hour mandatory live session offered 4 days after students completed the session “Blood Transfusion”. The students were given an ethics case about a young Jehovah’s Witness in need of a blood transfusion and asked to complete the assessments in class. They were then sorted into small groups for discussion and subsequently assigned a position to debate on whether the patient should receive the blood transfusion. For all three module assessments, students were provided a list of twenty ethical challenges cited from the Romanell report and were asked to select the challenges that they recognized in the learning module and provide supporting explanations (Additional file 1 : Appendix 1). Reflective writing prompts were included for students to complete on their own for thinking critically about the ethical challenges associated with the module. Module #1 reflective questions were tied to surrogate decision making and informed consent. An example of the reflective writing prompt from Module #1 includes “Would the case have been handled any differently were David a competent adult? At what point should David be considered autonomous and capable of making healthcare decisions? Explain your reasoning.” Module #2 reflective questions were tied to patient confidentiality and the reporting of communicable diseases. Module #3 reflective questions were tied to the impact of religion on clinical decisions. Students were also asked to voluntarily respond to the perception question “How useful did you consider this module in ethics training?” to rate the usefulness of the module on a 1 to 5 Likert scale (1-not useful at all, 5-very useful) and provide feedback. We expected students took 30 min to 1 h to complete all assessments. General feedback were provided by YZ and OO in person or in writing for each module.
Analytical procedure
The analytical procedure was aligned with the study’s aim to measure student attitudes about the ethics modules. The first analysis measured differences between perceived usefulness of the modules to determine if students found one teaching modality more useful than the others. The second was a qualitative study on written student feedback.
The statistical analysis of perceived usefulness was performed with the python programming language using the pandas, statsmodels, scipy, and scikit_posthocs packages. Descriptive statistics were calculated for each analysis with reported averages following the format of the mean ± one standard deviation. Group differences between the Likert-based usefulness ratings were initially analyzed with an ANOVA and normalcy of the standardized residuals were computed with a Shapiro-Wilk test. The final analysis used a Kruskal-Wallis test and post-hoc Dunn test with a Bonferroni correction to determine differences between groups (corrected- α for all tests was set to 0.05).
Student feedback was analyzed using two different qualitative approaches: constant comparison analysis [ 30 ] and classical content analysis [ 31 ]. Using more than one approach in qualitative data analysis, as recommended by Leech and Onwuegbuzie [ 32 ], can increase interpretive validity, or the degree to which the perspectives of students are accurately rendered by the researcher [ 33 ]. Two of the investigators (YZ and KO) double coded the de-identified student feedback with Dedoose 8.3.47b to independently assign codes to the text for each module. The investigators then reviewed the accuracy and relevance of these codes according to their interpretation of the students’ meaning and used the software to merge similar codes and remove other codes that were no longer pertinent. Next, the investigators used printouts from the software to complete axial coding, which involves comparing text segments and codes to create categories made up of similar codes, and to combine categories into broad themes. Last, the investigators used printouts from the software to conduct classical content analysis, calculating percentages of codes associated with each theme to determine their relative significance to the participants. The premise underlying classical content analysis is that the frequency of occurrence is connected to the meaning of the content [ 31 ]. This analysis allowed the investigators to discover the relative importance that each theme held for students (i.e., based upon the frequency of the codes associated with each theme), which gave more insight into students’ responses. The data were entered into Microsoft Excel for data management.
Ethical considerations
Exempt status for the research project was granted by the IRB committee of SHSU.
The majority of students (73/74) completed the Likert-based usefulness ratings. In general, students found each module useful, with an average across all modules of 4.37 ± 0.99. Descriptive statistics for each module are reported in Table 2 and the distribution of answers are shown in Fig. 1 .
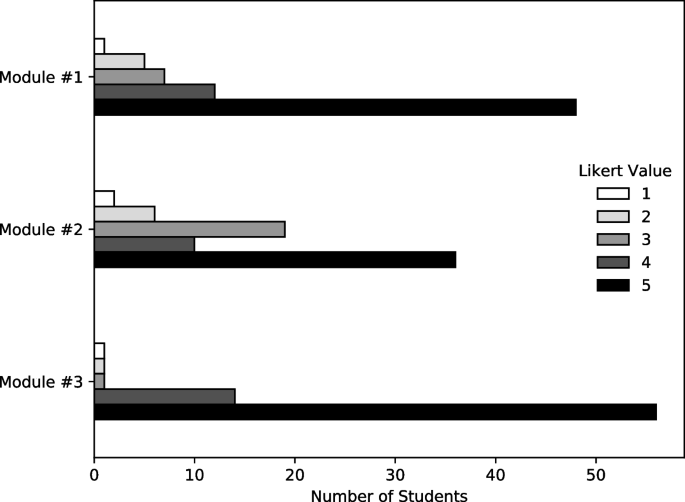
Usefulness ratings for each ethics learning module
To test differences between the Likert-based usefulness ratings between modules, a one-way ANOVA was performed with modules as groups and Likert-results as the dependent variable. However, it was found that the standardized residuals of the ANOVA did not follow a normal distribution after testing with a Shapiro-Wilk test ( W = 0.84, p < 0.001). Due to non-normal standardized residuals, a Kruskal-Wallis test was employed and found a statistically significant difference in rank-order between treatments ( H = 16.2, p < 0.001). A post-hoc Dunn test with a Bonferroni correction found that the only treatment pair with a statistically significant difference (corrected- α < 0.05) was between Module #3 and Module #2 (corrected p < 0.001). Complete results from the post-hoc Dunn test are reported in Table 3 .
The number of narrative responses to the perception question was consistently high, but not complete, with 82% of students who completed Module #1 providing feedback, with 85% for Module #2 and 80% for Module #3. Constant comparison analysis of student perception of the learning modules reveals three themes. These include general favorable impression for the learning modules , perceived learning outcomes for the learning module , and suggestions and critiques from students (Table 4 ).
General favorable impression of students for the learning modules
Students’ overall impression of the ethics learning modules integrated in a biomedical science course was positive. Based on classical content analysis (Table 4 ), the student’s general impression theme contains the highest percentage of codes, suggesting it is the most relevant theme from students’ perceptive responses. A detailed breakdown of common and unique codes for this theme is presented in Table 5 .
Engaging and enjoyable is the most dominant code in this theme with more comments from Module #1 (documentary) and Module #3 (SGD/Debate). In addition, several students described participating in Module #3 as “ fun ”.
“It was very interesting to learn about ethics this way and certainly something that I will not forget for a very long time.” (Module #1)
“Everyone in my group was excited to participate and contribute thought. I loved this.” (Module #3)
According to students, all the modules were considered effective and useful, thought provoking, and provided opportunities for them to examine ethical challenges and different perspectives which promoted their critical thinking. Most of the relevant comments associated with these codes were from Module #3, seconded by Module #2 and then Module #1.
“If I had watched the documentary on my own, I probably would not have thought about it as deeply as I did for this activity” (Module #1)
“ … the questions challenge me to think from different perspectives and consider multiples factors.” (Module #2)
“The debate made me think of the case on a deeper level and truly analyze each argument.” (Module #3)
Unique codes were also identified for Modules #1 and #3. For Module #1, students commented that watching the documentary helped them to see different viewpoints and it is more effective than traditional teaching styles such as reading text. For Module #3, the students described the debate as stress free but challenging and highlighted that it provided the opportunity to present and view different perspectives which ultimately allowed them to learn from each other. It was well perceived by students as a favorable format of teaching ethics.
“Thus, having these discussions are still very important, and sharing unique perspectives is great for that in two regards. One, these discussions teach us who others are and what others think about the world around them, and we must try our best to respect and understand these perspectives of others. Two, these discussions could reveal more about ourselves and even help us understand ourselves better, which allows us to develop our sense of uniqueness.” (Module #3)
Perceived learning outcome
Our analysis also revealed students’ perceived learning outcomes for each module. Several common and overlapping codes were identified as well as unique codes. (Table 6 ).
Many students felt that all the modules provided real world preparation and increased awareness of their roles as future physician. This code was the most dominant one compared to the other common codes. They felt that the modules helped them recognize the impact of ethical issues in clinical situations and made them think ahead as to how they might and should proceed in real-life circumstances.
“ … this is a very ethically engaging case and an issue that we will likely come across in our careers.” (Module #1)
“Really challenging situations like this do happen in real life and we need to have the skills to navigate through these situations and do what is best for the patient and their life.” (Module #3)
Students also described that the modules helped them raise awareness of the complexity of ethics by seeing the difficulty of ethics and how sometimes there is not a clear-cut answer as to what to do in a situation . In addition, the integration of ethics learning in biomedical science course helped them build connection of ethics with science. The classroom activities encouraged the application of biomedical knowledge learned in the course.
“I found this module to be useful in terms of utilizing all that we have learned so far to understand HIV from a different lens than previously thought.” (Module #2)
“I really like seeing the ethical side of the science that we are learning. It is easy to get so focused in the science and technology that it is nice to take a step back and think of the human perspective of it.” (Module #3)
The unique codes for the perceived learning outcomes were consistent with the distinct ethical challenges that were highlighted in each module. In Module #1, several students felt it improved awareness of the connection of ethics and research as well as recognizing the importance of a research compliance body oversight. Students felt this module helped them understand the role of ethics within the larger health care system. One student commented:
“My value of the scientific community and of institutional review boards has now increased as I believe that they could have helped improve the situation David and his family were facing if they intervened appropriately. ” (Module #1)
In Module #2, many students felt it raised awareness of the interplay between ethics and law, made them consider the legal rights versus the patients’ rights when it comes down to certain situations as physician.In Module #3, students identified increased awareness of the complexity of patient care as well and of the role of religion in health care. They also felt this highlighted the importance of patient-centered care.
“ … physicians must not just deal with symptoms but also the social aspects and ethical principles when addressing a patient’s care. Education, personal experience, stress, and religious beliefs are a few of the variables that differ amongst individuals and increase the complexity of a patient case. ” (Module #3)
Student critiques and suggestions
Some students commented on the fact that addition of group discussion would have been preferred and more effective in both Module #1 and #2. In Module #1, some wished for more structured instruction along with concrete objectives and didactic information . In Module #2, some students felt that the case was hypothetical and lacked background information. As one student commented “ It would be more useful knowing more about the state laws and regulations surrounding this kind of diagnosis.” Adding more context to the case and providing relevant learning materials would allow for more insightful discussion to the suggested way to approach difficult scenarios for us as future physicians . In Module #3, one student felt they needed more time to consider the ethical challenges as it was a harder ethics choice .
Although the goal is for students to explore and identify ethical challenges on their own, one student commented the Module #1 is not instructional in pointing out ethical issues/errors in the video as they happen. A detailed breakdown of common and unique codes for this theme is presented in Table 7 .
Given the importance of ethics in medical education, we created an innovative curriculum design for ethics learning made up of three unique modules that were integrated into a biomedical science course in the first-year pre-clinical curriculum. We started this project with the overall aim to increase student awareness and understanding of the ethical dimensions of the biomedical sciences. The literature on interleaving would suggest that students who learn medical ethics within a biomedical science context will improve their learning of both the foundational science content and the medical ethics content [ 34 ], for by exercising different forms of reasoning – scientific reasoning and ethical reasoning – within the same course, students may increase their ability to retain and apply the content learned, at least as compared to massed learning [ 35 ]. Literature is limited regarding strategies to integrate ethics in biomedical science courses [ 35 ]. Ultimately, we believe that a curricular design like the one that we developed can help medical students build connections between science, human disease and ethics, but our first step for this project was to see how students would react to this novel course design by evaluating their attitudes.
The design of our ethics modules was heavily influenced by the mounting evidence suggesting that students learn better and retain information longer when they learn through multiple modalities [ 35 ]. Several educational modalities have been shown to be effective in the teaching and learning of ethics in medical education. Examples include the use of ethical dilemmas in integrated small group sessions, standardized patients, team-based approaches, case-based discussion, problem-based methods, student-driven curriculum, peer-based teaching and ethics guest lectures [ 4 , 10 , 13 , 20 , 36 , 37 ]. These teaching modalities additionally provide opportunities for active learning which can increase student engagement and retention of information [ 35 ].
With this in mind, our modules were created utilizing different modalities to allow for maximal engagement and connection with the content. The particular choice of active learning strategy for each module was made by considering the content and the availability of course schedule along with the instructors’ content expertise. All three modules generated a consensus regarding the effectiveness and benefits of this curriculum design of ethics education in improving understanding and future preparation for encountering real dilemmas in medical practice. While all modules were considered to be engaging and thought-provoking, student responses highlighted various perceived strengths and weaknesses of each unique module and pedagogical modality. Module #1 was delivered through an asynchronous module using a commercially available documentary without formalized discussion. While the design of the documentary module did not allow for collaboration between the students or didactic instruction, choosing media with an existing reputation for engaging audiences made it more likely that the students would have at least a base-level interest in the module. Interactive learning strategies such as using the documentary as a basis for an interrupted case study could be utilized in the future to enhance the engagement. Module #2 was presented in a case-based fashion and without group discussion. A perceived weakness of this module was the lack of detailed background information in comparison to Module #1 which is a well-publicized case with robust details. Since the module was embedded in a TBL case that was focused on the scientific foundations of HIV, students felt it helped them strengthen their understanding of the ethical dimensions of the science they learned. Module #3 allowed for both small and large group discussion while incorporating a debate format which prompted rich discussion.
Although all modules were considered useful, student responses indicated a strong preference for Module #3, with a statistical significance when compared to Module #2, but not Module #1. There were more unique codes and comments generated related to its complexity and challenging format. This could be because the debate allowed students the uninterrupted opportunity to voice an opinion regarding the many ethical dilemmas central to the case being examined. Further, students enjoyed learning about their classmates and hearing new viewpoints from colleagues. Students were assigned a side to defend which compelled some students to make arguments different from their own perspective. Our finding resonates with existing literature which has suggested that the use of debates can be an effective tool for teaching medical ethics because it increases students’ critical thinking expression and tolerance toward ambiguity [ 38 ]. In addition, the reflective writing time was integrated into the session module which encouraged more valuable, thorough, and accurate feedback. Another reason students may have reported a preference for Module #3 could be that it was the last module of the course and close to the completion of the course. Overall, these elements highlighted the benefit of a debate format to encourage discussion of difficult topics emphasized in ethics courses, which contributed to the preference of Module #3. Interestingly, only one participant mentioned the link between ethics and science for Module #3, this might be due to the timing and method of the science session delivery. The session “Blood Transfusion” was offered asynchronously at the beginning of the week, while Module #3 was delivered at the end of the week due to scheduling conflict. This suggests the importance of purposeful design, delivery, and sequencing of both science and ethics sessions to help students better recognize the connection between the two subjects.
Our study has several limitations that affect the reliability and validity of the study. Although students were provided opportunities to practice ethical reasoning and decision making through providing explanation for self-identified ethical challenges and reflective writing, the direct learning outcome was not assessed. The lack of baseline data has hindered the analysis on the gain of students’ knowledge and attitude, although as a whole they perceived the modules as valuable and beneficial. Future studies should include pre- and post-assessment and longitudinal evaluation of the growth of the knowledge and moral attitudes of students. We also do not know whether students’ usefulness ratings were based on their preference for learning modalities or their specific interest in the topic of the module. For future studies the usefulness question should be revised to remove this ambiguity and improve content validity. The students were also not asked to directly compare the modules. Instead, they gave their responses at the time they completed each module, which was weeks apart from one another. Their general opinion may have changed over time and the order in which the modules were delivered may have influenced their responses. The modules could also be expanded to include multiple classes and to incorporate the modules in multiple courses. Furthermore, backward design strategy could be incorporated to ensure achievement of ethics learning objectives. The long-term impact of the modules may be evaluated by using preceptors survey in clerkship.
Expanding the study, and ethics education in general, faces several obstacles. Perhaps the most challenging obstacles are mundane: the lack of time within curriculum, lack of time in faculty schedules, and the lack of teachers qualified to teach ethics in the context of medical education [ 10 ]. Our study shows that ethics may be integrated in non-traditional places in curriculum and that student-directed learning can be used to alleviate the burden of curriculum load, although more student interaction should be encouraged. We plan to develop pre- and post-testing along with additional modules in order to measure longitudinal learning and to further integrate ethics into our biomedical science curriculum. To address the lack of standardized ethics training or certification for the instructors some institutions may face, collaborating with ethicists through interdepartmental or interinstitutional effort may be helpful. Together, the team can develop the modules as well as provide narrative feedback to students, which may enhance the delivery and assessment of the ethics modules.
Our study demonstrates that ethics education can be integrated with biomedical sciences. As is universal in education, the pedagogical design of the curriculum and relevant activities is the key to gaining students’ interest in learning. Strategies for ethics learning that we noted include the importance of purposeful design and sequence as well as the use of active learning modalities that involve discussion such as debate. Our model can shed light on an innovative way of integrating ethics education into medical education.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Veatch RM. Medical Ethics: Jones and Bartlett Publishers; 1997. (Jones and Bartlett series in philosophy). Available from: https://books.google.com/books?id=UCOT4sj-DwUC
Google Scholar
Beauchamp TL, Childress JF. Principles of biomedical ethics. 7th ed: Oxford University Press; 2013.
Vaugh L. Bioethics: principles, issues, and cases. 4th ed. New York, NY: Oxford University Press; 2020.
Miles SH, Lane LW, Bickel J, Walker RM, Cassel CK. Medical ethics education: coming of age. Acad Med. 1989;64(12):705–14.
Article Google Scholar
Savulescu J, Crisp R, Fulford KWM, Hope T. Evaluating ethics competence in medical education. J Med Ethics. 1999;25(5):367–74.
Curriculum Topics in Required and Elective Courses at Medical School Programs. AAMC. https://www.aamc.org/data-reports/curriculum-reports/interactive-data/curriculum-topics-required-and-elective-courses-medical-school-programs . Accessed 29 Nov 2022.
2017-18 Osteopathic Medical College Curriculum Topics. AACOM. https://www.aacom.org/reports-programs-initiatives/aacom-reports/curriculum . Accessed 29 Nov 2022.
DeFoor MT, Chung Y, Zadinsky JK, Dowling J, Sams RW. An interprofessional cohort analysis of student interest in medical ethics education: a survey-based quantitative study. BMC Med Ethics. 2020;21:26.
AlMahmoud T, Hashim MJ, Elzubeir MA, Branicki F. Ethics teaching in a medical education environment: preferences for diversity of learning and assessment methods. Med Educ Online. 2017;22(1):1328257.
Soleymani Lehmann L, Kasoff WS, Koch P, Federman DD. A survey of medical ethics education at U.S. and Canadian medical schools. Acad Med. 2004;79(7):682–9.
DuBois JM, Burkemper J. Ethics education in U.S. medical schools: a study of syllabi. Acad Med. 2002;77(5):432–7.
Shamim M, Baig L, Zubairi N, Torda A. Review of ethics teaching in undergraduate medical education. J Pak Med Assoc. 2019;70(6):1056–62.
de la Garza S, Phuoc V, Throneberry S, Blumenthal-Barby J, McCullough L, Coverdale J. Teaching medical ethics in graduate and undergraduate medical education: a systematic review of effectiveness. Acad Psychiatry. 2017;41(4):520–5.
Giubilini A, Milnes S, Savulescu J. The medical ethics curriculum in medical schools: present and future. J Clin Ethics. 2016;27(2):129–45.
Goldie J. Review of ethics curricula in undergraduate medical education. Med Educ. 2000;34:108–19.
Aguilera ML, Martínez Siekavizza S, Barchi F. A practical approach to clinical ethics education for undergraduate medical students: a case study from Guatemala. J Med Educ Curric Dev. 2019;6:238212051986920.
Beigy M, Pishgahi G, Moghaddas F, Maghbouli N, Shirbache K, Asghari F, et al. Students’ medical ethics rounds: a combinatorial program for medical ethics education. J Med Ethics Hist Med. 2016;9:3.
Liu EY, Batten JN, Merrell SB, Shafer A. The long-term impact of a comprehensive scholarly concentration program in biomedical ethics and medical humanities. BMC Med Educ. 2018;18(1):204.
Chung EK, Rhee JA, Baik YH, A OS. The effect of team-based learning in medical ethics education. Med Teach. 2009;31(11):1013–7.
Hindmarch T, Allikmets S, Knights F. A narrative review of undergraduate peer-based healthcare ethics teaching. Int J Med Educ. 2015;6:184–90.
Donaldson TM, Fistein E, Dunn M. Case-based seminars in medical ethics education: how medical students define and discuss moral problems. J Med Ethics. 2010;36(12):816–20.
Wolpe PR. Reasons scientists avoid thinking about ethics. Cell. 2006;125(6):1023–5.
Mcgowan A. Teaching science and ethics to undergraduates: a multidisciplinary approach. Sci Eng Ethics. 2013;19(2):535–43.
Reese AJ. An undergraduate elective course that introduces topics of diversity, equity, and inclusion into discussions of science. J Microbiol Biol Educ. 2020;21(1):21.1.10.
Mann MK. The right place and the right time: incorporating ethics into the undergraduate biochemistry curriculum. In: Kloepper KD, Crawford GL, editors. ACS symposium series. Washington, DC: American Chemical Society; 2017. p. 45–70. Available from: https://pubs.acs.org/doi/abs/10.1021/bk-2017-1266.ch004 . [Cited 2022 Jul 19].
Smith K, Wueste D, Frugoli J. Using “ethics labs” to set a framework for ethical discussion in an undergraduate science course. Biochem Mol Biol Educ. 2007;35(5):332–6.
Cornwall J, Hildebrandt S. Anatomy, education, and ethics in a changing world. Anat Sci Educ. 2019;12(4):329–31.
Carrese JA, Malek J, Watson K, Lehmann LS, Green MJ, McCullough LB, et al. The essential role of medical ethics education in achieving professionalism: the Romanell report. Acad Med. 2015;90(6):744–52.
The boy in the bubble. Public Broadcasting Service (PBS); 2006.
Glaser B. The constant comparative method of qualitative analysis. Soc Probl. 1965;12(4):436–45.
Berelson B. Content analysis in communication research. Ann Am Acad Pol Soc Sci. 1952;283(1):197–8.
Leech NL, Onwuegbuzie AJ. An array of qualitative data analysis tools: a call for data analysis triangulation. Sch Psychol Q. 2007;22(4):557–84.
Maxwell JA. Understanding and validity in qualitative research. In: The qualitative Researcher’s companion. Thousand Oaks: SAGE Publications, Inc.; 2022. Available from: https://methods.sagepub.com/book/the-qualitative-researchers-companion .
Safuan S, Ali S, Kuan G, Long I, Nik N. The challenges of bioethics teaching to mixed-ability classes of health sciences students. Educ Med J. 2017;9:41–9.
Brown PC. Make it stick : the science of successful learning. Cambridge: The Belknap Press of Harvard University Press, [2014]; 2014. Available from: https://search.library.wisc.edu/catalog/9910195454802121
Book Google Scholar
Mattick K. Teaching and assessing medical ethics: where are we now? J Med Ethics. 2006;32(3):181–5.
Sullivan BT, DeFoor MT, Hwang B, Flowers WJ, Strong W. A novel peer-directed curriculum to enhance medical ethics training for medical students: a single-institution experience. J Med Educ Curric Dev. 2020;7:2382120519899148.
Amar-Gavrilman N, Bentwich ME. To debate or not to debate? Examining the contribution of debating when studying medical ethics in small groups. BMC Med Educ. 2022;22(1):114.
Download references
Acknowledgements
The authors thank Dr. Amber Sechelski for her recommendations on the qualitative analysis.
Not applicable.
Author information
Authors and affiliations.
Department of Primary Care and Clinical Medicine, College of Osteopathic Medicine, Sam Houston State University, Conroe, USA
Oluwaseun Olaiya
College of Osteopathic Medicine, Sam Houston State University, Conroe, USA
Travis Hyatt, Alwyn Mathew & Shawn Staudaher
Department of Psychology and Philosophy, College of Humanities and Social Sciences, Sam Houston State University, Huntsville, USA
Zachary Bachman
Department of Molecular and Cellular Biology, College of Osteopathic Medicine, Sam Houston State University, Conroe, USA
You can also search for this author in PubMed Google Scholar
Contributions
YZ and OO designed the study and delivered all learning modules. They collected the data and conducted the qualitative data analysis and were major contributors in writing the manuscript. TH and AM conducted the literature review and contributed to the writing of the manuscript. SS conducted the quantitative data analysis and contributed to the editing of the manuscript. ZB contributed to the editing of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Yuan Zhao .
Ethics declarations
Ethics approval and consent to participate.
Decision of exempt status for this research project was granted by the IRB committee of Sam Houston State University. Informed consent was exempted by the IRB committee of Sam Houston State University due to retrospective nature of the study. All methods were carried out in accordance with the principles, guidelines and regulations of Declaration of Helsinki.
Consent for publication
Competing interests.
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1..
Appendix 1. List of Ethical Challenges Cited from the Romanell Report.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Olaiya, O., Hyatt, T., Mathew, A. et al. Building connections between biomedical sciences and ethics for medical students. BMC Med Educ 22 , 829 (2022). https://doi.org/10.1186/s12909-022-03865-y
Download citation
Received : 27 July 2022
Accepted : 04 November 2022
Published : 01 December 2022
DOI : https://doi.org/10.1186/s12909-022-03865-y
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Medical ethics
- Medical education
- Curriculum development
- Biomedical science
BMC Medical Education
ISSN: 1472-6920
- General enquiries: [email protected]
To Determine the Effectiveness of Current Ethical Teachings in Medical Students and Ways to Reform this Aspect
- Published: 20 August 2024
Cite this article

- Rida Saleem ORCID: orcid.org/0000-0002-1126-2773 1 ,
- Syeda Zainab Fatima ORCID: orcid.org/0000-0002-8606-5854 1 ,
- Roha Shafaut ORCID: orcid.org/0000-0001-6857-2943 1 ,
- Asifa Maqbool 1 ,
- Faiza Zakaria ORCID: orcid.org/0000-0002-1067-264X 1 ,
- Saba Zaheer ORCID: orcid.org/0000-0002-5911-581X 1 ,
- Musfirah Danyal Barry ORCID: orcid.org/0000-0002-4236-3462 1 ,
- Haris Jawaid ORCID: orcid.org/0000-0003-1879-4139 1 &
- Dr. Fauzia Imtiaz 1
1 Altmetric
Explore all metrics
To determine the effectiveness of current ethical teaching and to suggest ways to reform the current ethical curriculum in light of students’ perspectives and experiences. Students of Dow Medical College were selected for this cross-sectional study conducted between the year 2020 till 2023. The sample size was 387, calculated by OpenEpi. A questionnaire consisting of 17 close-ended questions was used to collect data from participants selected via stratified random sampling. The questionnaire consisted of two parts. The first part included the demographics. While the second contained 15 questions designed to assess the participants’ current teaching of ethics and effective ways to further improve it. The data obtained were analyzed using IBM SPSS statistics 26. Out of the 376 students who gave consent, the majority of the respondents (64.6%) encountered situations where they felt that their current teaching of ethics was insufficient and (54%) believed that the current teaching of ethics could be improved and made further effective. Practical sessions, PBLs (problem-based learning), case analysis, and ward visits were some of the ways the participants believed could help improve the teaching of medical ethics. Most students (92.8%) agreed that external factors like burnout and excessive workload have an impact on medical professionals’ ethical practices. In light of our study, a refined curriculum with a focus on ethical teaching must be established, with input from students to ensure that the medical students have the necessary expertise to manage an ethical dilemma.
This is a preview of subscription content, log in via an institution to check access.
Access this article
Subscribe and save.
- Get 10 units per month
- Download Article/Chapter or eBook
- 1 Unit = 1 Article or 1 Chapter
- Cancel anytime
Price includes VAT (Russian Federation)
Instant access to the full article PDF.
Rent this article via DeepDyve
Institutional subscriptions

Similar content being viewed by others

What Do Students Perceive as Ethical Problems? A Comparative Study of Dutch and Indonesian Medical Students in Clinical Training
Must we remain blind to undergraduate medical ethics education in africa a cross-sectional study of nigerian medical students.
The state of ethics education at medical schools in Turkey: taking stock and looking forward
Explore related subjects.
- Medical Ethics
- Artificial Intelligence
Data Availability
The authors confirm that the data supporting the findings of this study are available within the article and its supplementary materials.
Aleem, I., Zaidi, TafazzulHyder, Usman, G., Siddiq, H., Usman, T., Baloch, Z. H., & Abbas, K. (2021). Practice of medical ethics among house officers at tertiary care hospital in karachi. Pakistan Journal of Neurological Sciences (PJNS), 16 (3), 3.
Google Scholar
Althobaiti, M. H., Alkhaldi, L. H., Alotaibi, W. D., Alshreef, M. N., Alkhaldi, A. H., Alshreef, N. F., Alzahrani, N. N., & Atalla, A. A. (2021). Knowledge, attitude, and practice of medical ethics among health practitioners in Taif government, KSA. Journal of Family Medicine and Primary Care, 10 (4), 1759–1765. https://doi.org/10.4103/jfmpc.jfmpc_2212_20
Article Google Scholar
Chen, D., Lew, R., Hershman, W., & Orlander, J. (2007). A cross-sectional measurement of medical student empathy. Journal of General Internal Medicine, 22 (10), 1434–1438. https://doi.org/10.1007/s11606-007-0298-x
Chen, D. C., Kirshenbaum, D. S., Yan, J., Kirshenbaum, E., & Aseltine, R. H. (2012). Characterizing changes in student empathy throughout medical school. Medical Teacher, 34 (4), 305–311. https://doi.org/10.3109/0142159X.2012.644600
Cho, D., Cosimini, M., & Espinoza, J. (2017). Podcasting in medical education: A review of the literature. Korean Journal of Medical Education, 29 (4), 229–239. https://doi.org/10.3946/kjme.2017.69
Gabel, S. (2011). Ethics and values in clinical practice: whom do they help? Mayo Clinic proceedings, 86 (5), 421–424. https://doi.org/10.4065/mcp.2010.0781
Jafarey, A. M. (2003). Bioethics and medical education. Journal of Pakistan Medical Association, 53 (6), 210–214.
Kelly, J. M., Perseghin, A., Dow, A. W., Trivedi, S. P., Rodman, A., & Berk, J. (2022). Learning through listening: a scoping review of podcast use in medical education. Academic Medicine : Journal of the Association of American Medical Colleges, 97 (7), 1079–1085. https://doi.org/10.1097/ACM.0000000000004565
Martins, V., Santos, C., Bataglia, P., & Duarte, I. (2021). The teaching of ethics and the moral competence of medical and nursing students. Health Care Analysis: HCA: Journal of Health Philosophy and Policy, 29 (2), 113–126. https://doi.org/10.1007/s10728-020-00401-1
Nandi, P. L. (2000). Ethical aspects of clinical practice. Archives of surgery (Chicago, Ill. : 1960), 135 (1), 22–25. https://doi.org/10.1001/archsurg.135.1.22
Ozgonul, L., & Alimoglu, M. K. (2019). Comparison of lecture and team-based learning in medical ethics education. Nursing Ethics, 26 (3), 903–913. https://doi.org/10.1177/0969733017731916
Ridd, M., Shaw, A., Lewis, G., & Salisbury, C. (2009). The patient-doctor relationship: A synthesis of the qualitative literature on patients’ perspectives. The British Journal of General Practice: THe Journal of the Royal College of General Practitioners, 59 (561), e116–e133. https://doi.org/10.3399/bjgp09X420248
Roberts, L. W., Warner, T. D., Hammond, K. A., Geppert, C. M., & Heinrich, T. (2005). Becoming a good doctor: Perceived need for ethics training focused on practical and professional development topics. Academic Psychiatry : THe Journal of the American Association of Directors of Psychiatric Residency Training and the Association for Academic Psychiatry, 29 (3), 301–309. https://doi.org/10.1176/appi.ap.29.3.301
Ruberton, P. M., Huynh, H. P., Miller, T. A., Kruse, E., Chancellor, J., & Lyubomirsky, S. (2016). The relationship between physician humility, physician-patient communication, and patient health. Patient Education and Counseling, 99 (7), 1138–1145. https://doi.org/10.1016/j.pec.2016.01.012
Silverman, H. J., Dagenais, J., Gordon-Lipkin, E., Caputo, L., Christian, M. W., Maidment, B. W., 3rd., Binstock, A., Oyalowo, A., & Moni, M. (2013). Perceived comfort level of medical students and residents in handling clinical ethics issues. Journal of Medical Ethics, 39 (1), 55–58.
Stratta, E. C., Riding, D. M., & Baker, P. (2016). Ethical erosion in newly qualified doctors: Perceptions of empathy decline. International Journal of Medical Education, 7 , 286–292. https://doi.org/10.5116/ijme.57b8.48e4
Syed, S. S., John, A., & Hussain, S. (1996). Attitudes and perceptions of current ethical practices . PakIstan Journal of Medical Ethics, 1 , 5–6.
Download references
No funding was received to assist with the preparation of this manuscript.
Author information
Authors and affiliations.
Dow University of Health Sciences, Baba-E-Urdu Road, Karachi 74200, Pakistan
Rida Saleem, Syeda Zainab Fatima, Roha Shafaut, Asifa Maqbool, Faiza Zakaria, Saba Zaheer, Musfirah Danyal Barry, Haris Jawaid & Dr. Fauzia Imtiaz
You can also search for this author in PubMed Google Scholar
Contributions
All the authors took an equal part in performing the literature search, drafting the questionnaire, and the data collection of this study. Rida Saleem, Syeda Zainab Fatima, Roha Shafaut, Asfa Maqbool, and Faiza Zakaria drafted the initial manuscript and approved the final version of the manuscript. Saba Zaheer and Musfirah Danyal Barry contributed to the editing and revisions of the initial and subsequent drafts for incorporating important intellectual content and approved the final version of the manuscript. Haris Jawaid played an essential role in the data analysis and formulation of the results of this study. This study was completed under the supervision and guidance of Dr. Fauzia Imtiaz. She contributed to getting the IRB approval from DUHS- Research Committee. All authors agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Corresponding author
Correspondence to Syeda Zainab Fatima .
Ethics declarations
Ethical approval.
Approval to conduct this study was obtained from Ethics Committee of the institutional review board (IRB), (Authors will indicate the name of the granting institution after the acceptance of the manuscript).
Competing Interest
All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest or non-financial interest in the subject matter or materials discussed in this manuscript.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
Reprints and permissions
About this article
Saleem, R., Fatima, S.Z., Shafaut, R. et al. To Determine the Effectiveness of Current Ethical Teachings in Medical Students and Ways to Reform this Aspect. J Acad Ethics (2024). https://doi.org/10.1007/s10805-024-09550-7
Download citation
Accepted : 11 July 2024
Published : 20 August 2024
DOI : https://doi.org/10.1007/s10805-024-09550-7
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Medical Education
- Malpractices
- Medical Students
- Government Sector
- Find a journal
- Publish with us
- Track your research
- Subscribe to journal Subscribe
- Get new issue alerts Get alerts
Secondary Logo
Journal logo.
Colleague's E-mail is Invalid
Your message has been successfully sent to your colleague.
Save my selection
The Essential Role of Medical Ethics Education in Achieving Professionalism
The romanell report.
Carrese, Joseph A. MD, MPH; Malek, Janet PhD; Watson, Katie JD; Lehmann, Lisa Soleymani MD, PhD; Green, Michael J. MD, MS; McCullough, Laurence B. PhD; Geller, Gail ScD, MHS; Braddock, Clarence H. III MD, MPH; Doukas, David J. MD
J.A. Carrese is professor, Division of General Internal Medicine, Department of Medicine, Johns Hopkins University School of Medicine, and core faculty, Johns Hopkins Berman Institute of Bioethics, Johns Hopkins University, Baltimore, Maryland.
J. Malek is associate professor, Department of Bioethics and Interdisciplinary Studies, Brody School of Medicine, East Carolina University, Greenville, North Carolina.
K. Watson is assistant professor, Medical Humanities and Bioethics Program, Feinberg School of Medicine, Northwestern University, Chicago, Illinois.
L.S. Lehmann is associate professor, Center for Bioethics, Brigham and Women’s Hospital, and Division of Medical Ethics, Harvard Medical School, Boston, Massachusetts.
M.J. Green is professor, Department of Humanities and Department of Medicine, Penn State College of Medicine, Hershey, Pennsylvania.
L.B. McCullough is professor and Dalton Tomlin Chair in Medical Ethics and Health Policy, Center for Medical Ethics and Health Policy, Baylor College of Medicine, Houston, Texas.
G. Geller is professor, Division of General Internal Medicine, Department of Medicine, Johns Hopkins University School of Medicine, and core faculty, Johns Hopkins Berman Institute of Bioethics, Johns Hopkins University, Baltimore, Maryland.
C.H. Braddock III is professor and vice dean for education, David Geffen School of Medicine at UCLA, Los Angeles, California.
D.J. Doukas is William Ray Moore Endowed Chair of Family Medicine and Medical Humanism and director, Division of Medical Humanism and Ethics, Department of Family and Geriatric Medicine, University of Louisville School of Medicine, Louisville, Kentucky.
Funding/Support: The Project to Rebalance and Integrate Medical Education was supported by the Patrick and Edna Romanell Fund for Bioethics Pedagogy of the University of Buffalo.
Other disclosures: J.A. Carrese, D.J. Doukas, M.J. Green, and J. Malek hold leadership roles in the Academy for Professionalism in Health Care (APHC). At the time of writing, C.H. Braddock and L.S. Lehmann also held APHC leadership roles.
Ethical approval: Reported as not applicable.
Disclaimers: The views expressed by the authors reflect their personal perspectives and do not necessarily reflect those of the APHC.
Correspondence should be addressed to Joseph A. Carrese, Division of General Internal Medicine, Johns Hopkins Bayview Medical Center, 5200 Eastern Ave., Mason F. Lord Building, Center Tower, Suite 2300, Baltimore, MD 21224; telephone: (410) 550-2247; e-mail: [email protected] .
This article—the Romanell Report—offers an analysis of the current state of medical ethics education in the United States, focusing in particular on its essential role in cultivating professionalism among medical learners. Education in ethics has become an integral part of medical education and training over the past three decades and has received particular attention in recent years because of the increasing emphasis placed on professional formation by accrediting bodies such as the Liaison Committee on Medical Education and the Accreditation Council for Graduate Medical Education. Yet, despite the development of standards, milestones, and competencies related to professionalism, there is no consensus about the specific goals of medical ethics education, the essential knowledge and skills expected of learners, the best pedagogical methods and processes for implementation, and optimal strategies for assessment. Moreover, the quality, extent, and focus of medical ethics instruction vary, particularly at the graduate medical education level. Although variation in methods of instruction and assessment may be appropriate, ultimately medical ethics education must address the overarching articulated expectations of the major accrediting organizations. With the aim of aiding medical ethics educators in meeting these expectations, the Romanell Report describes current practices in ethics education and offers guidance in several areas: educational goals and objectives, teaching methods, assessment strategies, and other challenges and opportunities (including course structure and faculty development). The report concludes by proposing an agenda for future research.
In 1985, the landmark article “Basic Curricular Goals in Medical Ethics,” known as the DeCamp Report, argued that basic instruction in medical ethics should be a requirement in all U.S. medical schools. 1 That same year, the Liaison Committee on Medical Education (LCME) introduced standards stipulating that in U.S. medical schools “ethical, behavioral, and socioeconomic subjects pertinent to medicine must be included in the curriculum and that material on medical ethics and human values should be presented.” 2 More recently, medical educators and accrediting organizations have expanded the scope of ethics education guidelines, manifested in part by requirements that learners at all levels receive instruction addressing professional formation to prepare them for a lifelong commitment to professionalism in patient care, education, and research. 3 A physician’s ability and willingness to act in accordance with accepted moral norms and values is one key component of professional behavior; as a result, educational objectives relating to ethics are now often incorporated into broader goals for professionalism education.
Despite broad consensus on the importance of teaching medical ethics and professionalism, there is no consensus about the specific goals of medical ethics education for future physicians, the essential knowledge and skills learners should acquire, the best methodologies and processes for instruction, and the optimal strategies for assessment. 4–8 Moreover, the quality and extent of instruction, particularly at the graduate medical education (GME) level, varies within and across institutions and residency training programs. 9–11 Although such variation may be appropriate in light of differences in educational contexts, medical ethics education efforts must ultimately address the overarching expectations articulated by accrediting organizations. Variation raises concerns about whether all approaches succeed in meeting basic educational objectives, which leads to the question, “Which approaches to medical ethics education are most effective?”
This article, the Romanell Report, is a product of the Project to Rebalance and Integrate Medical Education (PRIME), funded by the Patrick and Edna Romanell Fund for Bioethics Pedagogy. PRIME was a national working group that focused on medical ethics and humanities education as they relate to professionalism education in medical school and residency training. 12 , 13 PRIME led to the founding of the Academy for Professionalism in Health Care as an organization devoted to professionalism education. 14
As members of PRIME with a particular interest in medical ethics education, we address in this report the essential role of such education in cultivating professionalism among medical learners. We previously described medical professionalism as (1) becoming scientifically and clinically competent; (2) using clinical knowledge and skills primarily for the protection and promotion of the patient’s health-related interests, keeping self-interest systematically secondary; and (3) sustaining medicine as a public trust, rather than as a guild primarily concerned with protecting the economic, political, and social power of its members. 13
We take our working definition of “medical ethics” from a prominent textbook on clinical ethics: “Clinical ethics concerns both the ethical features that are present in every clinical encounter and the ethical problems that occasionally occur in those encounters.” 15 In addition, we consider medical ethics to include attention to determining what ought to be done when problems or values conflicts are present: that is, determining the right course of action or a morally acceptable choice from among the available options.
We consider it self-evident that there is a close relationship between medical ethics and professionalism and that the extensive body of scholarship on medical ethics informs how we think about professionalism. However, a thorough analysis of this relationship is beyond the scope of this article. We do not address the important role of humanities education in the pursuit of professional formation in this report; we plan to focus on that in future work. Additionally, although our focus in this article is on medical ethics education during medical school and residency training, we acknowledge that the educational continuum extends on either side of this focus. We believe that medical ethics and professionalism should also be made a priority during premedical studies and reinforced post residency through continuing medical education (CME).
In this report, with the aim of aiding medical ethics educators in meeting the articulated expectations of accrediting organizations, we address the following aspects of medical ethics education in medical schools and residency programs: goals and objectives, teaching methods, assessment strategies, and additional challenges and opportunities. We conclude by recommending next steps and areas for future study.
Goals and Objectives
Although most educators agree that the central goal of medical ethics education is to promote excellence in patient care, there are diverse views about how best to achieve this aim. 4 Whereas some educators emphasize the importance of developing future physicians’ character, others hold that shaping their behavior is a more appropriate focus. Still others believe that ethics and professionalism cannot be taught; rather, virtuous individuals must be selected through the medical school admission process. The debate among proponents of these schools of thought is unlikely to be resolved in the near future.
Although medical schools should seek to select students with the “right” character and attitudes, those qualities are difficult to assess accurately. Further, effecting character change in the limited time available for medical ethics and professionalism education seems challenging at best. The practical challenges of shaping and evaluating character traits logically lead to the alternative: cultivating behavior that exemplifies ethical and professional virtues. The foundation of this approach is to provide trainees with conceptual tools for seeing, preventing, analyzing, and resolving the ethical dilemmas encountered in clinical medicine. Although an argument can be made that this pragmatic approach is not ideal, it is a workable compromise that may be the best available option given existing constraints.
This focus on behavioral goals is supported by the major accrediting bodies for U.S. medical schools and residency programs, which have established behavior-based standards and competencies that learners must achieve during training. For example, LCME standard ED-23 states: “A medical education program must include instruction in medical ethics and human values and require its medical students to exhibit scrupulous ethical principles in caring for patients and in relating to patients’ families and to others involved in patient care.” 16 The LCME specifies that students’ behavior must be observed and assessed to ensure that it is in line with accepted ethical guidelines.
Similarly, the Accreditation Council for Graduate Medical Education (ACGME) has defined six core competencies 17 and has called for the development of milestones that establish benchmarks for the behaviors that physicians completing U.S. residency programs must demonstrate for each competency. One of the six core competencies specifically focuses on professionalism, stating, “Residents must demonstrate a commitment to carrying out professional responsibilities and an adherence to ethical principles.” Residents are expected to show compassion and respect for others, put patients’ needs above their own, respect patients’ autonomy, act accountably, and demonstrate sensitivity to patients from diverse backgrounds. The ACGME has left it to individual specialties to define the milestones that compose this core competency. As an example, the professionalism milestones identified by the American Board of Internal Medicine are presented in Table 1 . It should be noted that all six of the ACGME core competencies involve various aspects of professionalism, explicitly or implicitly.

With respect to the continuum of medical learning, there is interest in extending the focus on competencies and milestones beyond GME. Some educators suggest integrating them into undergraduate medical education (UME) as well as addressing them as part of CME and maintenance of certification. 18
In addition, attention has been directed at linking milestones to instances of actual clinical practice by defining entrustable professional activities (EPAs) and using them as a basis for assessing learner performance. 19 To successfully and independently perform one of these core clinical activities, learners must not only demonstrate the requisite knowledge, attitudes, and skills but also seamlessly integrate competencies, subcompetencies, and milestones. Some educators 18 have argued for tailoring EPAs to the learner’s developmental level, which could serve to further integrate the learning continuum.
EPAs, milestones, and competencies define where learners are expected to be by the end of their training, but they do not specify the detailed objectives that educators should use to lead them there. Among ethics educators, there is no consensus on a set of specific objectives for medical ethics education, although several lists of key skills and topics have been put forward. 20–22 Our attempt to synthesize current thought on a minimum set of objectives for medical ethics education is presented in List 1 . These objectives apply to both medical students and residents, with greater proficiency expected of higher-level trainees. This list was developed collaboratively by our group of experienced educators and draws on relevant empirical studies and other published literature. 4 , 6 , 9 , 20 , 21 , 23 It is important to emphasize that this list represents what we consider to be the basic requirements for medical ethics education. We acknowledge that other objectives to promote professionalism in learners (i.e., objectives incorporating other specific skills and topics) could be added to this list.
List 1 Proposed Objectives for Medical Ethics Education Cited Here
Upon completion of medical school or a residency training program, learners will, with an appropriate level of proficiency:
- Demonstrate an understanding of the concept of the physician as fiduciary and the historical development of medicine as a profession
- Recognize ethical issues that may arise in the course of patient care
- Utilize relevant ethics statements from professional associations to guide clinical ethical judgment and decision making
- Think critically and systematically through ethical problems using bioethical principles and other tools of ethical analysis
- Provide a reasoned account of professionally responsible management of ethical problems and act in accordance with those judgments
- Articulate ethical reasoning to others coherently and respectfully
Upon completion of medical school or a residency training program, learners will, with an appropriate level of proficiency, manage ethical challenges in a professional manner in the following areas:
- Protection of patient privacy and confidentiality
- Disclosure of information to patients, including medical errors and the delivery of bad news
- Assessment of patient decision-making capacity and issues related to surrogate decision making
- Shared decision making, including informed consent and informed refusal of medical interventions by patients
- Care at the end of life, including patient advance directives, withholding and withdrawing life-sustaining interventions, care for the dying, and determination of death
- Maternal–fetal medicine, including reproductive technologies and termination of pregnancy
- Pediatric and neonatal medicine
- Access to health care, including health care disparities, the health care system, and the allocation of scarce resources
- Cross-cultural communication, including cultural competency and humility
- Role of the health care professional’s personal values in the clinical encounter, including the extent and limits of the right of conscience
- Conflicts of interest and of obligation in education, clinical practice, and research
- Research with human subjects, including institutional review boards
- Work within the medical team, including interprofessional interactions
- Concerns about colleagues, including impairment, incompetence, and mistakes
- Medical trainee issues, including disclosure of student status, the tension between education and best care for patients, the hidden curriculum, and moral distress
- Self-awareness, including professional identity and self-care
- Management of challenging patients/family members, including recognition of what the clinician may be contributing to the difficulty
- Social media
- Religion and spirituality
- Acceptance of gifts from patients, including grateful patient philanthropy
For comparison, we have summarized the objectives for medical ethics education presented in the 1985 DeCamp Report 1 in List 2 . The objectives proposed in this report ( List 1 ) differ from the earlier objectives in several ways. First, our objectives are more comprehensive, which may reflect an increased emphasis on ethics and professionalism in medical training and therefore an expectation that more curricular time will be devoted to these topics. It may also reflect the broadening scope of the still-developing field of bioethics. A second difference between the objectives offered in the DeCamp and Romanell Reports is our inclusion of items that take into account the context in which medicine is practiced, particularly issues of access to health care and cultural competence. The inclusion of these items mirrors recent social trends—expanding awareness of socioeconomic inequalities, emphasizing the social determinants of health, and increasingly respecting and valuing diversity. Third, our expansion of ethical considerations beyond the patient–physician dyad to interprofessional interaction and self-care should be noted. An improved understanding of the important role of effective teams in preventing medical errors and in offering patients excellent care can explain our addition of an item on working within the medical team. The attention to self-care reflects a developing awareness that experiencing a loss of meaning in clinical practice and inadequate work–life balance can lead to waning commitment, dissatisfaction, and burnout, 24 and these in turn can be associated with lapses in professionalism. 25 , 26 Fourth, the DeCamp Report objectives emphasize moral reasoning and knowledge to be acquired in specific content areas, but devote less attention to specific skills to be developed. Our inclusion of more skills-based items in the Romanell Report objectives reflects accrediting agencies’ move toward evaluation of learners’ actual performance in clinical encounters and their achievement of corresponding milestones.
List 2 The DeCamp Report’s Proposed Objectives of Medical Ethics Education a Cited Here
- The ability to identify the moral aspects of medical practice
- The ability to obtain a valid consent or a valid refusal of treatment
- Knowledge of how to proceed if a patient is only partially competent or incompetent to consent or to refuse treatment
- Knowledge of how to proceed if a patient refuses treatment
- The ability to decide when it is morally justified to withhold information from a patient
- The ability to decide when it is morally justified to breach confidentiality
- Knowledge of the moral aspects of the care of patients with a poor prognosis, including patients who are terminally ill
- Additional areas considered for inclusion:
- Distribution of health care
a Objectives articulated in Culver et al, 1985. 1
In addition to these differences in learning objectives, the Romanell Report devotes attention to several areas not addressed by the DeCamp Report: methods of teaching, assessment strategies, and additional challenges and opportunities. We now turn our attention to these issues.
Teaching Methods
There is no single, best pedagogical approach for teaching medical ethics and professionalism. Learning styles and institutional resources vary, so teaching methods need to be flexible and varied to reflect this diversity. For example, to address the ACGME professionalism subcompetency “sensitivity and responsiveness to a diverse patient population,” 17 an educator could deliver a conventional didactic lecture, present clinical cases, or show a “trigger tape” intended to inspire discussion and debate. 27 Similarly, articles that illuminate issues of diversity by presenting patient perspectives 28 , 29 or that address the evolution of different “worldviews” on health and healing could be assigned and discussed. 30 Another pedagogical technique is to invite learners to write reflective narratives about cases they have been involved in that have raised ethics issues. 31 , 32 Whenever possible, medical ethics and professionalism instruction should involve collaboration among faculty from different disciplines to reinforce the team approach required in clinical practice. In recent years, multidisciplinary contributions to professionalism teaching have expanded beyond the traditional fields of philosophy, history, literature, law, and social sciences to include applied methods from the arts such as improvisational theater exercises, 33 comics drawing, 34 creative writing practices, 35 and fine art study. 36–38
Educational theory suggests that spacing and repetition of content improve learning. 39 A medical ethics and professionalism curriculum is therefore most likely to result in sustained changes in reasoning and behavior when it is longitudinal, such that early educational interventions are reinforced or advanced by subsequent exposures. For example, a method for ethics case analysis introduced in the first year of medical school could be reinforced in clinical clerkships by asking students to apply that method to analyze ethical issues they are encountering in clinical settings. In addition, learner-driven teaching strategies should be considered. For example, learners could identify clinical cases with ethics issues for discussion and take an active role in facilitating case discussions.
Ethics and professionalism education must strive to move learners from knowledge acquisition and skills development to behavior change in which excellent patient care is the goal (by way of achieving the ACGME core competencies). This is challenging, but—to borrow from the language of theater—script does not become performance without rehearsal. After students gain medical knowledge in the classroom, educators commonly employ role-play scenarios (often with simulated patients or in an “ethics OSCE” [objective structured clinical examination] 40 ) to help students practice translating their medical knowledge into skills (and as a means for demonstrating that knowledge) before they encounter the complexity of actual patients. 41–43 This approach is highly effective for teaching ethics and professionalism. 44 , 45
Technological advances have increased the variety of options for teaching ethics and professionalism. Some materials are now available online, such as recorded lectures 46 or formal ethics courses. 47 Educators are also creating online content for their own classes, and the “flipped classroom” approach (where students watch lectures online, on their own, saving class time for discussion and application of the material) may complement (or replace) the traditional approach of in-person lectures. 48 Educators should be open to these innovations and carefully evaluate which content is best delivered by new technologies. Advantages of moving lectures online include increasing both time for group discussions and the focus on students’ critical thinking and behavioral skills during class. However, the use of innovative educational technologies may not be suited to situations in which learners do not consistently engage in outside preparation (e.g., busy residency programs with limited protected learning time). The wide range of available teaching methods gives educators opportunities to choose the pedagogical tools that are best suited to the jobs they are asked to do, but this variety also raises questions about which methods are most effective (an important area for future research).
Although it is not feasible in this report to offer a full account of how medical ethics education efforts should vary between GME and UME levels, it is worth noting some key differences. First, educational materials offered to residents can typically be more complex and contextual than those intended for medical students, and ethical issues can be more nuanced and discussed in greater depth. As a general point, educators must recognize that any teaching session may involve learners at different levels of sophistication; accordingly, educators should tailor cases and teaching points to offer material appropriate to the range of learners with whom they are working. Second, differences in schedules and responsibilities require educators to adopt different approaches for teaching ethics and professionalism to medical students and residents. Whereas a variety of formats, including longitudinal courses, can generally be included in a medical school curriculum, finding opportunities for formal ethics and professionalism instruction can be more challenging in residency training programs where face-to-face educational sessions tend to take the form of sporadic, irregularly attended one-hour conferences. Although this conference format can be conducive to case-based discussions, educators need to be creative in turning these opportunities into a coherent curriculum.
Assessment Strategies
Faculty teaching ethics and professionalism cannot just assume that their pedagogical techniques achieve the intended goals. Rather, consistent with a broader trend in medical education, they are expected to demonstrate that what they are doing is working. Increasingly, they must justify the amount of curricular time allotted for medical ethics and professionalism education as well as any financial support they receive for such efforts.
Toward these ends, there is evidence that medical ethics education improves certain outcomes. Specifically, studies have shown an improvement in learner awareness, 49 attitudes, 50 knowledge, 51 confidence, 52 decision making, 53 and moral reasoning. 54 However, a more robust evidence base is required to examine the relationships between medical ethics education, physician performance, and—ideally—patient outcomes. Accrediting bodies, medical school deans, and residency program directors seek assessment tools to evaluate whether educational programs are effective in producing prepared clinicians. Further, it is in patients’ interests to have (justified) confidence that their physicians have been trained adequately in ethics and professionalism.
A starting point for assessment is linking evaluation to learning objectives when doing so is possible and sensible. This requires careful consideration of the nature of individual objectives, whether individual objectives can be evaluated, and the complexity of the material being taught. If assessment is viewed as feasible, one model for linking learning objectives to assessment is the SMART approach 55 —creating objectives that are specific, measurable, action oriented, reasonable, and time bound. For example, “At the end of this session participants will describe the 5 components of the R.E.S.P.E.C.T. model for cross-cultural communication.” 56 Objectives of this type reflect a focus on behavior-based educational goals, as discussed earlier, rather than an emphasis on character development.
Varied assessment strategies may be needed to determine whether ethics and professionalism learning objectives have been met. Possible strategies include, but are not limited to, learner self-assessment; learner reflection; evaluation of changes in learner empathy, cynicism, and attitudes; performance portfolios; traditional, knowledge-based exams; use of clinical evaluation exercises; use of OSCEs and other exercises with simulated patients; written feedback from faculty after small-discussion-group modules; and 360-degree feedback from peers, faculty, nurses, staff, patients, and families in the patient care context. 57–62 As noted above, an emerging assessment strategy is using defined EPAs to evaluate learner performance in the context of actual clinical activities. A recent article presents one institution’s efforts related to medical ethics education to integrate goals, methodology, curriculum, and assessment. 23
Although an expectation of performance-oriented assessment is challenging for many areas of the medical curriculum, it is especially challenging for ethics and professionalism: Some aspects of ethics and professionalism are not performance related, and even those aspects that are “behavorial” may be difficult to measure. 63 For example, some authors have pointed out that certain qualities of character desirable in any health care professional (e.g., humility, compassion, integrity, altruism) are not measureable in any conventional, quantitative sense. 64 , 65
Further, evaluators of educational programs tend to focus on formal course work rather than the hidden curriculum, 66 and to look for improvement rather than lack of erosion . Yet, there is substantial evidence that manifestations of professional behaviors decrease throughout the medical socialization process. 64 , 67 Arguably, evaluation should also include assessing the learning environment of educational institutions 68 and measuring the ability of interventions to inoculate learners against diminishment of professional behaviors. 69
Additionally, if the primary goal of medical ethics and professionalism education is improved patient care, we need to develop methods of connecting educational interventions to patient outcomes. One recent study provides an example of this by documenting a relationship between physician empathy and improved glucose control. 70
If assessment is limited to what is formally taught and to what can be quantitatively assessed, or there is a requirement of positive change, we risk evaluating some of the most important qualities of professionalism in ways that fail to capture their nuances. Given this, some authors have argued for alternative strategies to assess the presence of such qualities and the corresponding success of educators’ efforts to cultivate them in learners. 71 , 72 Clearly, there needs to be a good fit between what is being assessed and the strategies used to assess it. Quantitative ratings should not be the sole means to evaluate excellence in professionalism; rather, they should be complemented by qualitative assessments. This combined approach will enable richer, contextualized evaluations, but it also presents the challenge of identifying evaluators with the observational, perceptual, and analytical capabilities to conduct these assessments.
The phenomenon of latency also must be considered in the assessment of ethics and professionalism instruction: Outcomes of interest may not manifest themselves for years. One goal of medical ethics education is to prepare learners to address difficult ethical issues when they arise, yet learners may not encounter a particular ethics problem until years after they were taught about it in the classroom. However, their later performance may be profoundly affected by recollecting a distant reading or in-class discussion. This scenario creates challenges for evaluation. Accordingly, professionalism and ethics educators should develop long-term evaluation and/or research strategies to supplement the assessment of more immediate outcomes. In List 3 , we propose items to assess and a “to-do” list (i.e., work to be done) with respect to assessment in medical ethics education.
List 3 Assessment in Medical Ethics Education: Items to Assess in Medical Learners and a “To-Do” List Cited Here
Items to assess
- Mastery of a basic body of medical ethics content
- Mastery of the intellectual skills for ethical analysis and reasoning/argument
- Performance in core bioethics behavioral skills: obtaining meaningful informed consent or informed refusal, assessing decision-making capacity, breaking bad news, analyzing a case with ethics issues, and using a shared decision-making approach with patients
Assessment “to-do” list
- Work with clinical colleagues to develop medical ethics components of passports and other learner self-assessment tools, as well as tools for faculty to use in assessing medical students’ and residents’ learning on clinical rotations
- Work with clinical colleagues on medical ethics components of tools for summative assessment of medical students and residents
- Work with colleagues who are specialists in medical education to ensure that medical ethics curricular design and assessment take into account variation in learning styles of adult learners
- Develop assessment strategies that address the relationships between medical ethics education and physician performance and patient outcomes
- Utilize a range of assessment strategies, both quantitative and qualitative, to ensure a “goodness of fit” between what is being assessed and the strategies used to assess it
- Develop long-term evaluation/research strategies to supplement assessment of more immediate outcomes (to address the phenomenon of latency)
Additional Challenges and Opportunities
Beyond the challenges we have already noted related to goals and objectives, teaching methods, and assessment strategies, additional challenges—as well as opportunities—exist in medical ethics education. First, training in ethics and professionalism exists within the larger context of the health care system and medical practice. Numerous external factors affecting doctor–patient encounters have negative influences on the learning environment and, thus, have the potential to undermine the foundation of medical education. When learners do not see what is taught in the classroom being honored in the clinical setting, they have difficult choices to make. 73 , 74 An institution’s learning environment can either exacerbate moral erosion, burnout, and impairment among learners, or it can support learners by creating a culture that prioritizes learner well-being. 3 In response to this challenge, medical ethics and professionalism educators need to (1) provide learners with tools that can help them reconcile the mixed messages they may be receiving, and (2) measure, monitor, and improve their learning environments. 68
Second, where and how to locate medical ethics and professionalism education in the overall curriculum of a medical school or residency training program is an important—and contested—issue. Careful consideration should be given to the timing and structure of this instruction and the level of expertise needed to deliver it.
Some medical schools have recently undertaken curricular revisions that reflect a philosophical change in approach to ethics education. 75 Instead of offering medical ethics and professionalism as a discrete course, instruction is woven throughout the entire curriculum in a developmentally appropriate way. The justification for this integrated approach is that ethics is germane to all of medicine—from clinical decision making at the bedside and clinical investigations to policy considerations at the health care delivery system level—and should be incorporated into the curriculum wherever and whenever it is relevant.
There is considerable debate about the benefits and disadvantages of integrated approaches. It is important that ethics and professionalism education not be integrated into the curriculum to the point of being invisible, because students need to be able to identify the discipline of medical ethics and be familiar with its literature. In our view, the best practice may be to seek a healthy balance between emphasizing ethics and professionalism instruction and seamlessly integrating it into clinical education. However, appropriate incorporation of this content requires coordination with other course directors who may not be committed to its inclusion. Mechanisms must be put in place to ensure the inclusion of ethics material on other courses’ exams and to enable formative and summative determinations of students’ mastery of ethics and professionalism on an annual basis. Further, when ethics and professionalism teaching is woven into courses and clerkships directed by non-ethics faculty, there are questions about who will be responsible for teaching this material, what level of expertise is needed, and how much time should be set aside for this teaching (in the context of busy schedules).
Third, faculty considerations factor significantly into the teaching and evaluation of medical learners. Successful medical ethics and professionalism education efforts require a sufficient number of faculty with appropriate training who are committed to establishing meaningful, ongoing relationships with learners to act as role models, share their own experiences, and teach, observe, give feedback to, and ultimately evaluate learners. Achieving success requires financial support, recognition, and reward for faculty educators. This is particularly challenging in an era of fiscal constraint because nonphysician faculty educators (i.e., those with PhDs and JDs) do not generate clinical revenue, whereas clinician educators tend to generate revenue by seeing patients, not by teaching. In some medical school settings, participation in medical education is implicitly devalued by the fact that teaching is a voluntary, nonremunerated activity—a discouraging message for all but the most committed educators. Until the issue of how to pay educators and reward them academically for their efforts is resolved, the quality of medical ethics and professionalism education efforts is likely to suffer.
Finally, faculty considerations are relevant when addressing expectations for assessment. If institutions strive for defensible quantitative evaluations of learner behavior, they need to ensure that there are enough qualified faculty observers to make a sufficient number of observations to achieve reliability. 60 Similarly, if assessment of some desired outcomes and qualities requires a qualitative approach, then faculty evaluators must be skilled at listening, observing, and “reading” learners to truly understand and “see” them. 76
Moving Forward: Key Next Steps and Considerations
We believe that this report on the state of medical ethics education offers cause for optimism. In the three decades since publication of the DeCamp Report, 1 medical ethics has become a core component of the medical school curriculum. Further, the emphasis on ethics in the ACGME’s core competencies—especially the professionalism competency—indicates that medical ethics education is a valued component of residency training as well.
However, our report also identifies many challenges facing medical ethics educators. First, there is no consensus about specific educational objectives for medical ethics and professionalism. Second, several pedagogical methods have been shown to offer some benefit to learners, but the supporting data are rarely robust, and educational approaches vary greatly between programs and institutions. Third, increasing pressure to demonstrate effectiveness raises particular challenges for faculty teaching medical ethics and professionalism because these educational efforts do not always produce short-term, quantitatively measurable improvements. Finally, the “hidden curriculum” 66 can undermine learners’ professional development, creating a need for attention to the learning environment and for widespread faculty development that would require significant resources and expertise.
Addressing these challenges requires a rigorous, systematic, and interdisciplinary approach. Although this is a daunting task, we propose the following research questions as first steps toward a comprehensive agenda for scholarship, both empirical (including qualitative and quantitative methods) and conceptual:
- What specific role does medical ethics education play in supporting professional formation? Research that answers this question would help focus medical ethics education efforts as they relate to professionalism and potentially provide a rationale for financial support.
- What constitutes a consensus list of specific educational objectives for medical ethics education? Research that establishes and leads to the dissemination of such a list would help ensure that all learners receive an agreed-upon basic level of medical ethics education.
- What are the strengths and weaknesses of pedagogical approaches used in medical ethics education, and which are associated with better learner outcomes? Research that addresses this issue would help educators make informed choices from a long list of possible teaching strategies.
- How are medical ethics and professionalism education associated with learner performance and patient outcomes? Research that answers this question would help establish a much-needed evidence base linking education to outcomes. Such an evidence base could, in turn, provide additional rationale for financial support of these efforts.
- What constitutes an evidence-based portfolio of effective medical ethics educational interventions for medical students, residents, physician faculty, and practicing physicians? Work on this issue could lead to the creation of a helpful resource for educators who do not have time to develop a portfolio themselves.
- Which assessment tools are most effective at measuring outcomes of interest in medical ethics education? Which assessment strategies should be paired with which learner and patient outcomes? Research that responds to these questions would help educators select assessment strategies that are appropriate for the outcome of interest and proven to be effective. Work in this area should address the latency challenge noted above and recognize the limitations of quantitative measurement with respect to certain aspects of ethics and professionalism.
Another challenge is that few interinstitutional opportunities exist for medical educators to explore these problems and seek answers to these questions. One goal of the Academy for Professionalism in Health Care is to provide a forum for all stakeholders—including medical ethics, humanities, and professionalism educators—to come together to work on these challenging issues. 14
In conclusion, we believe that the medical ethics curriculum can be improved by focusing it on professional formation as preparation for a lifelong commitment to professionalism in patient care, education, and research. It will require the hard work of many to ensure that medicine preserves its status as a caring profession that situates the needs of patients as its top priority.
Reference cited in Table 1 only
- + Favorites
- View in Gallery
Readers Of this Article Also Read
Boyer's expanded definitions of scholarship, the standards for assessing..., redesigning the mcat exam: balancing multiple perspectives, the development of professionalism: curriculum matters, beyond curriculum reform: confronting medicine's hidden curriculum, introduction: the humanities and medical education</strong>', 'charon rita md; williams, peter jd phd', 'academic medicine', 'september 1995', '70', '9' , 'p 758-760');" onmouseout="javascript:tooltip_mouseout()" class="ejp-uc__article-title-link"> introduction: the humanities and medical education.
- - Google Chrome
Intended for healthcare professionals
- My email alerts
- BMA member login
- Username * Password * Forgot your log in details? Need to activate BMA Member Log In Log in via OpenAthens Log in via your institution

Search form
- Advanced search
- Search responses
- Search blogs
- The ethics of medical...
The ethics of medical education
- Related content
- Peer review
- Reshma Jagsi , resident in radiation oncology 1 ,
- Lisa Soleymani Lehmann ( llehmann1{at}partners.org ) , instructor in medicine and medical ethics 2
- 1 Department of Radiation Oncology, Massachusetts General Hospital, Harvard Medical School, Boston, MA, USA
- 2 Division of General Medicine and Primary Care, Brigham and Women's Hospital, Harvard Medical School, 1620 Tremont Street, Boston, MA 02120-1613, USA
- Correspondence to: L S Lehmann
- Accepted 23 March 2004
Medical students and doctors in training need to hone their clinical skills on patients to make themselves better doctors, but patients may not benefit directly from such attention. Jagsi and Lehmann consider this ethical dilemma and suggest ways to minimise the potential harm to patients
Participation of trainees in patient care is an integral part of medical education. Although educating doctors is critical to society, an ethical dilemma results from the fact that patients may not benefit from doctors in training and medical students participating in their care, and may even be harmed by it. 1 2 However, this dilemma has received little attention—political, 3 institutional, 4 or academic. 5 6 Professional societies advise only generally, noting that participation should be voluntary without providing specific procedural requirements. As a result, patients may be misinformed about the qualifications and experience of their care givers. 7 This situation is objectionable in its own right, but it also provides a problematic example at a critical point during trainees' moral development.
In contrast, the ethics of medical research on human subjects have been the subject of much analysis and policy development. 8 A compelling analogy exists between such research and medical education. 9 10 In both cases doctors ask patients to participate in an endeavour whose primary aim is to benefit society as a whole, not the individual. In both cases doctors must also balance the good to society and potential benefit to individual participants against potential harm to those participants, avoid the unfair distribution of risks and benefits, and maintain respect for patient autonomy. Although education and research have different goals, their similarities are sufficient to allow for fruitful discussion based on this analogy.
Credit: FELDMAN/SPL STEPHEN
In this article we apply three principles of research ethics—respect for individuals, beneficence, and distributive justice—to medical education in order to review current practice and guide further research and policy.
Respect for individuals
Western philosophers have long argued that human beings have an inherent personal dignity that merits respect for its own sake. To use people only as a means to an end—as is the case when patients are the objects of medical education or research without meaningful consent—violates that fundamental principle.
Evidence suggests that the current practice of medical education does not always accord adequate respect to patients. In one US survey, only 38% of responding teaching hospitals claimed that they informed patients that students would be involved in their care. 11 Other studies show that students and their supervisors sometimes misrepresent or inadequately explain students' status. 12 Moreover, student conscientiousness about disclosing their status seems to decay over the course of training. 13 Patient surveys confirm that they receive inadequate information about trainees' roles. 14
Procedures to ensure meaningful consent from patients to participation in medical education are therefore necessary. Patients must be fully informed of the training status and experience of all staff caring for them and must comprehend the risks, benefits, and alternatives. The proximity of consent to individual procedures is crucial, and a “blanket” consent at admission is insufficient.
Beneficence
The principle of beneficence consists of a spectrum of obligations to promote welfare, ranging from the negative duty not to inflict harm to the positive duty to do good. Beneficence requires that, even before patients are asked to participate in research or education, doctors must first decide whether the overall balance of risks and benefits justifies requesting that participation. It also requires that doctors minimise risks. Understanding the nature and probability of risks and benefits is thus essential.
Both medical education and research are primarily directed at providing benefits to society as a whole. With research, society benefits from contributions to medical knowledge; with education, it benefits from the production of well trained doctors. Both medical education and research may also benefit participating individuals. Patients may benefit from participating in research by gaining access to experimental treatments and from closer follow up. Similarly, patients may benefit from closer attention when trainees participate in their care.
Studies have shown that patient satisfaction does not decrease when students participate in their medical care. Many patients are willing to allow students to participate in invasive procedures and pelvic examinations, 15 indicating that they may believe the balance of potential benefits to themselves and society outweigh the risks. Altruism, rather than perceived benefit to self, seems to be the primary motivation for participation in medical education. 16 Self interest may play a larger role in patients' motivations for participating in research than in the case of education, and this difference has important implications. While researchers may reasonably be bound by non-maleficence alone, educators bear a stricter positive duty to do good.
Few empirical data exist regarding potential hazards of participation in medical education. Research relating provider inexperience to patient outcomes, including the idea of a “July phenomenon” (increased patient morbidity and mortality linked with the influx of new medical trainees), has been inconclusive. 17 Because the goals and nature of education and research differ, it seems appropriate to require a higher threshold by which benefits should exceed risks in the case of education. Further research into outcomes of trainee participation is necessary to allow doctors to provide comprehensive information to patients regarding the risks and benefits they face. Such research could also be used to develop guidelines about the appropriate level of supervision for given classes of activity and levels of experience. Educators should also identify ways to minimise the risk of participation by inexperienced providers, such as increased reliance on advanced technological simulations. 18
Distributive justice
The burdens of medical education are not currently distributed fairly. In one US study, students saw disproportionately high numbers of non-white patients and patients with Medicaid (public insurance for the indigent). 19 Another study found that children of doctor parents were less likely to be seen by trainees than were other children. 20
Such disparities may exist because disadvantaged patients may not feel empowered to withhold consent. They may also exist because consultants assume that certain patients are likely to refuse and therefore do not ask them to participate. The lack of participation of trainees in the care of doctors' children is particularly troubling, for it indicates that those most informed about the true risks and benefits of the system of medical education are more likely to withhold consent. There is a tension between the three principles, as it is difficult to secure the societal benefit of medical education and maintain respect for patients who withhold consent without placing an unfair burden on disempowered groups.
Summary points
The current system of medical education, in which doctors in training and medical students participate in patient care, may expose patients to physical, psychological, and economic risks, often without their full consent
Few analyses of the ethics of trainee participation in patient care have been made, and policies are not well developed
The ethics of medical education can be informed by the ethics of research on human subjects
We provide a theoretical framework for ethical medical education by extending three key concepts from the literature of research ethics—respect for individuals, beneficence, and distributive justice
Within the framework provided by these concepts, we assess the current practice and effects of trainee participation in patient care and provide suggestions for policy development and further research
When socioeconomic constraints lead certain groups to participate in medical education because it is their only opportunity to obtain care, the principle of distributive justice is clearly violated. System-wide changes, including broadening the location of medical training to settings outside the wards of inner city hospitals and improving the access of disempowered groups to health care more generally, particularly in the United States, are necessary if the distribution of the benefits and burdens of medical education is to be truly just.
Medical educators have much to gain from research ethics. As in clinical research, patient participation should be guided by the principles of respect for individuals, beneficence, and justice. Systematic procedures are necessary to apply these principles to the practice of medical education. Professional organisations should give detailed guidelines, and teaching institutions must develop, in consultation with community members, effective mechanisms to ensure the ethical practice of medical education.
Some readers may cringe at the spectre of a new bureaucracy being created to implement these recommendations. The rapidly evolving nature of medical research and the wide variety of research proposals necessitate standing independent boards to conduct frequent reviews. Since the field of medical education has a well developed infrastructure, the application of these ethical principles should not entail substantial extra administrative burdens.
Just as there is a continuum between innovative practice and research, there is a continuum between practice and education, for medicine is a career of life-long learning. The principles discussed in this paper are applicable not only to medical trainees but may prove useful to junior doctors and even senior doctors attempting new procedures or practices.
The history of research ethics suggests that the medical profession should be proactive rather than reactive in approaching the ethics of medical education. The time has come for the profession to turn its attention to this important issue.
Contributors and sources: LSL had the initial idea for this article. The concepts were refined by dialogue between LSL and RJ. RJ did a Medline search from 1966 to the present, and both authors examined references cited in commonly used textbooks of medical ethics and clinical research ethics. Both authors reviewed the published literature. RJ wrote the first draft of the article, which was revised by LSL. LSL is guarantor for the article.
Funding This study was funded by the Harvard Medical School Division of Medical Ethics.
Competing interests None declared.
- Robertson DW ,
- Robinson DL ,
- Coldicott Y ,
- Basson MD ,
- Dworkin G ,
- Marracino RK ,
- McCullough LB ,
- Kessel RWI ,
- Apostolides AY ,
- Heiderich KJ ,
- Vinicky JK ,
- Connors RB Jr . ,
- Heiderich KJ
- Beatty ME ,
- Silver-Isenstadt A ,
- Benbow SJ ,
- Elizabeth J ,
- Williams CT ,
- Magrane D ,
- Gifford G ,
- Luxenberg M ,
- Butters JM ,
- Stange KC ,
- Diekema DS ,
- Cummings P ,
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Indian J Psychiatry
- v.55(1); Jan-Mar 2013
Ethics in medical research: General principles with special reference to psychiatry research
Ajit avasthi.
Department of Psychiatry, Postgraduate Institute of Medical Education and Research, Chandigarh, India
Abhishek Ghosh
Sidharth sarkar, sandeep grover.
Ethics is an understanding of the nature of conflicts arising from moral imperatives and how best we may deal with them. Ethics in medical research deals with the conflicts of interest across various levels. Guidelines have been proposed for standardized ethical practice throughout the globe. The four fundamental principles of ethics which are being underscored are autonomy, non-maleficence, beneficence, and justice. Some special ethical issues have particular relevance to psychiatric research arising primarily from the specific vulnerabilities of those with mental illness and the risks posed by some research methodologies. Accordingly, sensitivity is required in the design of psychiatric research. It is suggested that though the value of published guidelines and the help that may be available from research ethics committees is quite great, the primary responsibility for maintaining high standards of practice in research rests with research workers themselves.
INTRODUCTION
The word “ethics” is derived from the Greek word, ethos, which means custom or character. Ethics is an understanding of the nature of conflicts arising from moral imperatives and how best we may deal with them.[ 1 ] It deals with the choices we make and our actions in relation to those choices. It deals with the choices made by both clinicians and patients and the duties and obligations of clinicians to their patients. Medical ethics also deals with the choices made by society, the distribution of resources, and access to health care, and the dilemmas arising from them.[ 2 ] An issue, mainly for the developing countries, has been the extent to which ethical principles are considered universal or as culturally relative – the universalist versus the pluralist view. The challenge to international research ethics is to apply universal ethical principles to biomedical research in a multicultural world with a multiplicity of health-care systems and considerable variation in standards of health care.[ 3 ]
History is unfortunately peppered with stories of abuse carried out in the name of medical research. The most dreadful of all atrocities was possibly conducted by Nazi doctors who used convicts for human experimentation. The discovery of these experiments stunned the whole world which led to the formulation of Nuremberg code[ 4 ] to prevent recurrence of such episodes. It was the first international code for ethics in clinical research laying down the guidelines for research on human subjects. It laid down 10 clear principles to be followed by researchers and made voluntary consent essential, allowed subjects to withdraw from the experimentation at any time, banned experiments that could result in major injury or death of the subjects, and made mandatory to have preclinical data before experimenting on humans. Even Nuremberg code failed to terminate unethical research practices. Eventually a set of guidelines was adopted by the 18 th World Medical Association (WMA)[ 5 ] General Assembly, which was called the Declaration of Helsinki. It contained 32 principles, which stress on informed consent, confidentiality of data, vulnerable population, and requirement of a protocol, including the scientific reasons of the study, to be reviewed by the ethics committee. Though Declaration of Helsinki had created a stir in the medical community, medical atrocities continued. The malpractice in the Tuskegee Syphilis Study in the US was possibly the next eye opener which ushered the Belmont Report[ 6 ] in 1979 and laid the foundation for regulations regarding ethics and human subjects’ research in the US. With the increasing interest of pharmaceutical industries in carrying out research experiments in the developing and the underdeveloped countries, the Council for International Organizations of Medical Sciences (CIOMS)[ 3 ] in association with World Health Organization (WHO) developed “International Ethical Guidelines for Biomedical Research Involving Human Subjects” in 1982.

CARDINAL PRINCIPLES OF ETHICS IN RESEARCH
The four principles of Beauchamp and Childress – autonomy, non-maleficence, beneficence, and justice – have been extremely influential in the field of medical ethics, and are fundamental for understanding the current approach to ethical assessment in health care. Respect for autonomy stands for acting intentionally after being given sufficient information and time to understand the information. Beneficence is directed to promote the well-being of patients and society. On the other hand, non-maleficence implies first do no harm which can be achieved by careful decision making and having adequate training. Justice deals with the equitable distribution of social benefits.[ 7 , 8 ]
MEDICAL RESEARCH – DEFINITION, TYPES, AND ISSUES
The term “research” refers to a class of activity designed to develop or contribute to generalizable knowledge. Generalizable knowledge consists of theories, principles, or relationships, or the accumulation of information on which they are based, that can be corroborated by accepted scientific methods of observation and inference. In the present context, “research” includes both medical and behavioral studies pertaining to human health. Usually “research” is modified by the adjective “biomedical” to indicate its relation to health. Those who support the need for research argue that no new treatment should be offered outside the context of a controlled trial, so that treatments’ effectiveness and efficacy can be measured ab initio , not only for the sake of the patients currently receiving it but also for all future patients. Research involving human subjects includes:[ 1 , 9 ]
- Studies of a physiological, biochemical, or pathological process, or of the response to a specific intervention – whether physical, chemical, or psychological – in healthy subjects or patients;
- Controlled trials of diagnostic, preventive, or therapeutic measures in larger groups of persons, designed to demonstrate a specific generalizable response to these measures against a background of individual biological variation;
- Studies designed to determine the consequences for individuals and communities of specific preventive or therapeutic measures; and
- Studies concerning human health-related behavior in a variety of circumstances and environments.
Conflicts of interest are inherent to the majority of relationships among individuals and of those with companies and institutions and, certainly, research involving human beings is no exception. In relation to clinical research, conflicts of interest occur at different levels and usually permeate through various lines (e.g., in the pharmaceutical industry, about their decisions to invest and develop new products, especially vaccines and drugs, and also in relation to marketing of these products). Among the investigators, the conflicts may be related to the financial gains to participate in pharmacy sponsored trials, or to the expected academic career boost attained with the publication of the results of the trials and also to personal interests such as the financial support for trips to international conferences.[ 10 ]
Therefore, medical research which is absolutely necessary and fundamental for acquiring and propagating worthwhile novel knowledge is equally controversial because of the conflicts of interest of the researchers or the sponsors. Both universal and regional guidelines have been proposed to strike a balance between these two opposing interests and to ensure standardized ethical research.
PRINCIPLES OF ETHICS IN MEDICAL RESEARCH
Principles of essentiality.
Refers to whether the research is considered to be absolutely essential after a due consideration of the existing scientific knowledge in the proposed area of research. This should be scrutinized by an independent and responsible body of persons who, after careful consideration, come to the conclusion that the research is likely to benefit the humanity or environment.[ 11 ]
Principles of voluntariness, informed consent, and community agreement
Research participants should be fully apprised of the research and the associated risks and benefits. The participants should be informed of the right to abstain from the research or withdraw consent at any time. Where research entails treating any community, the principles of voluntariness and informed consent apply to the community as a whole and to each individual member. In case a person is incapable of giving consent, a legally acceptable guardian should give the informed consent.
Principles of non-exploitation
The participants should be fully apprised of all the possible dangers that may arise during the research so that they can appreciate all the physical and psychological risks. Each research should include an in-built mechanism for compensation for the human participants either through insurance cover or by any other appropriate means to cover foreseeable and unforeseeable risks, and provide remedial action and comprehensive aftercare.
Principles of privacy and confidentiality
The identity and records of the participants are as far as possible kept confidential (except when required for legal reasons). This is to avoid any form of hardship, discrimination or stigmatization as a consequence of having participated in the research.
Principles of precaution and risk minimization
Due care and caution should be taken at all stages of the research and experiment to ensure that the research participant and those affected by it including the community are put to the minimum risk, suffer from no known irreversible adverse effects, and generally, benefit from the research or experiment. There should be a plan for interim reviews to detect whether any intervention arm (active or control) is associated with increased risks, so that undue harms are avoided by stopping the research.
Principles of professional competence
Research should be conducted by competent and qualified persons who act with total integrity and impartiality and who have been made aware of the ethical considerations to be borne in mind in respect of such research or experiment.
Principles of accountability and transparency
The research or experiment should be conducted in a fair, honest, impartial, and transparent manner after full disclosure is made by those associated with the research or experiment of each aspect of their interest in the research, and any conflict of interest that may exist. Full and complete records of the research should be retained for such reasonable period as may be prescribed or considered necessary for the purposes of post-research monitoring, evaluation of the research, conducting further research, and scrutiny by the appropriate legal and administrative authority, if necessary.
Principles of the maximization of the public interest and of distributive justice
The research or experiment and its subsequent application should be conducted and used to benefit all human kind (and not just those who are socially better off), in particular, the research participants themselves and or the community from which they are drawn.
Principles of public domain
The research findings should be brought into the public domain so that its results are generally made known through scientific and other publications. This would help in consolidating the scientific knowledge base of the field being studied and would prevent the undue replication of studies which pose risks to some subjects.
Principles of totality of responsibility
Professional and moral responsibility should be observed, for the due observance of all the principles, guidelines, or prescriptions of those directly or indirectly connected with the medical research. This extends to the institutes where this research is carried out, as well as the sponsors of the research. The research should be duly monitored and constantly subject to review and remedial action at all stages.[ 11 ]
SPECIAL REFERENCE TO PSYCHIATRY RESEARCH
Neuropsychiatric disorders are highly prevalent conditions with significant morbidity, yet only modestly effective treatments are available. The suffering and loss caused by these diseases call for the development of truly innovative interventions. Testing such innovative approaches can carry risks of significant harm[ 12 ] even while raising hopes for future benefits.[ 13 ] Furthermore, the very nature of many neuropsychiatric disorders creates ethical complexity because many persons with such disorders have impaired cognition or emotion. If a patient's impairment is severe enough, he or she will be incompetent to give informed consent for research.[ 14 ] In our society, surrogate or proxy consent-based research remains an area of unsettled policy. Finally, at a more speculative level, interventions that alter behavior, or even knowledge that can predict or explain behaviors, can challenge traditional norms of social regulation and interaction.[ 15 ]
Methods for solving these dilemmas have included the development of more objective rules to guide the practitioner, such as utilitarianism and deontology. Deontological approaches possibly cannot resolve moral conflicts, and so the psychiatrist is “denied an available remedy.” Utilitarianism is seen by the authors as too difficult to calculate benefits and risks, and demands an impartiality that clinicians would find difficult to achieve. Both deontology and utilitarianism, a respect for patient autonomy, and utility, a measurement of consequences, are seen as theories that do not help clinicians in practice. This is particularly the case in conflict situations as in psychiatric research.[ 16 ] Therefore, research in psychiatry demands a special attention.
Issues in relation to competence and consent
Participation in research usually involves some degree of risk, discomfort, or sacrifice of the personal care that patients enjoy when they receive ordinary treatment.[ 17 ] Ordinarily, we allow research subjects to incur these discomforts or sacrifice personal care because we believe that people have the right to run certain risks for rewards that seem to them worthwhile. These rewards may include the pride that comes from altruistic behavior, the hope that they themselves might benefit from the results of the study at some point in the future, and the more immediate possibility that they may have access through the study to assessment techniques or therapeutic approaches that would not otherwise be available to them. But when subjects’ capacities to make decisions are impaired, they may materially misconstrue the situation into which they are entering.[ 18 ]
To resolve these conflicts, proposals have been made that range from banning certain types of research with psychiatric patients to requiring independent evaluation of the capacities of potential subjects, to appointing representatives to remove subjects from studies when the risk–benefit ratio appears to be swinging against them.[ 19 , 20 ]
As per WMA guidelines for ethical research, “In research involving subjects who are mentally incapable of giving consent, the physician should seek informed consent from the legally authorized representative. If no such representative is available and if the research cannot be delayed, the study may proceed without informed consent provided that the specific reasons for their inability to give informed consent have been stated in the research protocol and the study has been approved by a research ethics committee. Consent to remain in the research should be obtained as soon as possible from the subject or a legally authorized representative” (WMA 2008; clause 29). An additional caveat in clause 28 reads, “When a potential research subject who is deemed incompetent is able to give assent to decisions about participation in research, the physician must seek that assent in addition to the consent of the legally authorized representative. The potential subject's dissent should be respected.”[ 21 ] It should always be remembered that impairments exist on a spectrum, and some degree of dysfunction is not incompatible with competent decision making. Thus, although the presence of cognitive and related impairments in schizophrenia, for example, warrants concern about subjects’ abilities to decide whether to enter a research project, by no means does it call for the exclusion of all persons with schizophrenia from investigational studies. Individuals who have severe mental disorder and lack adequate decision-making capacity may improve significantly with educational remediation.[ 22 , 23 ] Patients can be given information through conversation, lectures, pamphlets, articles, medication groups, instruction sheets, books and videotapes, consent forms, and interactive videodiscs. Repeated disclosure of information is another technique which can be followed.[ 24 ]
However, systematic evaluation, even in non-psychiatric populations and in high-income countries, has shown that participants in randomized trials recall information poorly, are not often aware that placebos form one arm of treatment, demonstrate inadequate comprehension of the process of chance in treatment allocation, understand and use only a proportion of what is presented in consent forms, do not really understand the issue of equipoise, and participate not for altruistic reasons but because they expect some improvement by participation.[ 25 ] Cognitive dysfunction and the symptoms shown to be associated with impaired decisional capacity are not unique to schizophrenia and may occur with many other forms of illness.[ 26 ] Furthermore, studies have also shown that many people with schizophrenia are able to give informed consent and retain related information across time. So, diagnosis of mental illness itself does not disqualify a person to enter into a research as competence of decision making is case specific and variable across the time.
Issues in relation to confidentiality
Patients, health-care providers, and patient advocacy organizations have expressed increasing concern about the confidentiality of clinical information stored in large computerized databases.[ 27 – 30 ] The accumulation of ever-larger stockpiles of sensitive information raises reasonable concerns about inappropriate access and unauthorized disclosure. Given the stigma often attached to psychiatric disorders and psychiatric treatment, confidentiality of information on mental health and substance abuse treatment is especially critical. A few occurrences of inappropriate use or disclosure of clinical information have been well publicized.[ 28 , 30 ]
Firstly, continued research access to population-based records data is essential to protecting the rights and interests of people with psychiatric illness. Investigators conducting any such research should take all possible steps to limit access to confidential information, minimize risks of disclosure, and (when possible) obtain informed consent for research use of clinical data. The most effective strategy for preventing disclosure of confidential information is to remove all identifying information from medical records data before any research use.[ 31 ] Secondly, when potential research uses are anticipated at the time of data collection, those collecting clinical information should be obligated to advise patients regarding possible research use. However, obtaining individual informed consent for each specific research use is impossible or extremely impractical.[ 32 ] Lastly, research intended to increase public domain medical knowledge should be clearly differentiated from proprietary activities. If legitimate public domain research activities were clearly distinguished from other uses of large clinical databases, efforts to regulate storage and disclosure of clinical data could concentrate on the activities that are now largely unregulated.[ 33 ]
However, advances in mental health science promise great benefits for those who suffer, or will come to suffer, from mental illness and, in some cases, for research subjects themselves. While persons with mental illness may be vulnerable in several ways, research regulations that focus primarily on their vulnerabilities and deficits could encourage and possibly exacerbate the stigmatization already felt by this population.[ 34 , 35 ] Further, it may be unjust to exclude, by overly restrictive regulation, those people with mental illness who could benefit from research participation. An ethically appropriate framework for psychiatric research ethics balances rigorous protections for human subjects with recognition of the enormous social and individual benefits arising from well-designed and ethically conducted scientific research.[ 36 – 38 ] How this balance is struck has important implications for research ethics generally, particularly for research involving vulnerable persons.
Though a number of ethical guidelines have been formulated for clinical research, malpractice is still widely acknowledged. It could be understood by the fact that ethical guidelines in many countries like India are just the recommendations and not a law. For proper enforcement, guidelines should be made a part of the law as has been done in the US and some other countries of the world.[ 39 ] We need better research, and research done for the right reasons. The second intriguing issue is the cross-cultural applicability of ethical guidelines.[ 40 ] In this era of advanced globalization, the problems of medical ethics can no longer be viewed only from the perspective of wealthy countries. Global bioethics seeks to identify key ethical problems faced by the world's 6 billion inhabitants and envisages solutions that transcend national borders and cultures. The relevance of global bioethics is obvious with respect to international research ethics (as evidenced by the controversy over changes to the Declaration of Helsinki), global vaccine initiatives, or global health equity.[ 41 ] Last but not the least; doctors are specially trained to be good clinicians but are seldom taught even the fundamentals of ethical clinical research. The post-graduate dissertation or the PhD thesis is a precious opportunity to train tomorrow's investigators in the elements of ethical clinical research.[ 42 ] The attributes of a clinical researcher like truthfulness and accountability toward integrity are expected to propagate standardized ethical practice.
Source of Support: Nil
Conflict of Interest: None declared
- Open access
- Published: 19 March 2022
Ethics education to support ethical competence learning in healthcare: an integrative systematic review
- Henrik Andersson 1 , 2 , 3 ,
- Anders Svensson 1 , 2 , 4 ,
- Catharina Frank 1 , 2 ,
- Andreas Rantala 2 , 5 , 6 ,
- Mats Holmberg 1 , 2 , 7 , 8 &
- Anders Bremer 1 , 2 , 9
BMC Medical Ethics volume 23 , Article number: 29 ( 2022 ) Cite this article
22k Accesses
50 Citations
2 Altmetric
Metrics details
Ethical problems in everyday healthcare work emerge for many reasons and constitute threats to ethical values. If these threats are not managed appropriately, there is a risk that the patient may be inflicted with moral harm or injury, while healthcare professionals are at risk of feeling moral distress. Therefore, it is essential to support the learning and development of ethical competencies among healthcare professionals and students. The aim of this study was to explore the available literature regarding ethics education that promotes ethical competence learning for healthcare professionals and students undergoing training in healthcare professions.
In this integrative systematic review, literature was searched within the PubMed, CINAHL, and PsycInfo databases using the search terms ‘health personnel’, ‘students’, ‘ethics’, ‘moral’, ‘simulation’, and ‘teaching’. In total, 40 articles were selected for review. These articles included professionals from various healthcare professions and students who trained in these professions as subjects. The articles described participation in various forms of ethics education. Data were extracted and synthesised using thematic analysis.
The review identified the need for support to make ethical competence learning possible, which in the long run was considered to promote the ability to manage ethical problems. Ethical competence learning was found to be helpful to healthcare professionals and students in drawing attention to ethical problems that they were not previously aware of. Dealing with ethical problems is primarily about reasoning about what is right and in the patient’s best interests, along with making decisions about what needs to be done in a specific situation.
Conclusions
The review identified different designs and course content for ethics education to support ethical competence learning. The findings could be used to develop healthcare professionals’ and students’ readiness and capabilities to recognise as well as to respond appropriately to ethically problematic work situations.
Peer Review reports
Introduction
Healthcare professionals and students undergoing training in healthcare professions are confronted with a variety of ethical problems in their clinical practice. These ethical problems appear as ethical challenges, conflicts, or dilemmas that influence the daily provision of care and treatment for patients [ 1 , 2 ]. Addressing these problems requires ethical competencies that involve the ethical dimensions of sensitivity, knowledge, reflection, decision making, action, and behaviour [ 3 ]. As the future workforce, students need training to effectively deal with ethically problematic situations [ 4 ], and experienced professionals need to develop ways to manage ethical problems [ 5 ]. Therefore, it is essential for ethics education to support the learning and development of ethical competencies among healthcare professionals and students undergoing training to work in healthcare. In this study, ethics education is referred to educational components with a content of support and learning activities that promote understanding and management of ethical problems. The focus is on ethics education that is carried out at universities and in clinical practice. In conclusion, it would be valuable to first compile the existing knowledge about designs and course content that support ethical competence learning.
The provision of care is based on patients’ care needs and the complexity of their health conditions; this process is further complicated by the nature of the care environment, which is frequently chaotic and/or unpredictable, with care often being provided under stressful working conditions [ 6 , 7 , 8 , 9 , 10 ]. Healthcare professionals and students in clinical practice are confronted daily with difficult choices and must cope with questions of ‘rightness’ or ‘wrongness’ that influence their decision-making and the quality of the care provided [ 11 , 12 ]. The underlying reasons for the emergence of ethical problems in everyday healthcare work are multifaceted, unfold over time, and are caused by factors such as a lack of resources, insufficient leadership, hierarchical organisational structures, chaotic work environments, or a lack of competencies [ 13 ]. Ethical problems and value conflicts are inherent in clinical practice and do not necessarily mean that healthcare professionals or students have done anything inappropriate or that structures are inadequate. Whatever the cause, ethical problems can lead to conflicts between principles, values, and ways of acting [ 14 ]. This, in turn, might lead to compromised moral integrity and generate moral distress [ 11 , 15 , 16 ], as these reactions result from acting or not acting on the basis of one's own sense of right and wrong [ 17 ]. At worst, moral distress can lead to moral injury, which occurs as a result of witnessing human suffering or failing to prevent outcomes that transgress deeply held beliefs [ 18 ]. Therefore, healthcare professionals and students in clinical practice need to develop their ethical competencies to be prepared for their responsibility and commitment to caring for patients.
The concept of competence is multifaceted and include many things. In this study, competence is viewed as entailing knowledge, skills, and attitudes that are essential when healthcare professionals and students are carrying out their work in clinical practice [ 19 ]. Ethical competence contain components such as the capability to identify ethical problems, knowledge about the ethical and moral aspects of care, reflection on one’s own knowledge and actions, and the ability to make wise choices and carefully manage ethically challenging work situations [ 3 ]. Ethical competence is essential for the ability to respect the patient’s rights and the quality of care [ 20 , 21 ]. This means that ethical competence includes not only knowledge of the ethical and moral aspects of care, but it also includes moral aspects of thinking and decision-making. Furthermore, ethical competence is important since it may prevent or reduce moral distress [ 22 ].
Healthcare professionals and students in clinical practice need a solid foundation that supports when they are confronted with ethically problematic situations. Care and treatment depend not only on knowledge and skills or acting according to guidelines; they also depend on personal values, beliefs, and ethical orientations [ 23 ]. There are various strategies to support and develop the capability to identify and solve ethical problems. [ 24 ]. Ethics education is one such way to develop ethical competencies [ 20 ]. Simultaneously, ethics education raises questions about the content and teaching methods relevant for clinical practice [ 25 ]. While theoretical education via small-group discussions, lectures, and seminars in which ethical principles are applied is quite common [ 26 ], an alternative educational method is simulation-based learning [ 27 ]. However, there is no evidence to support the determination of the most effective strategy to promote the application of ethics in care. There are also challenges to teaching and assessing ethics education. For example, ethics education does not always occur contextually or in a realistic situation, and theoretical knowledge of ethics does not necessarily lead to improved ethical practice [ 28 ]. Teaching ethical principles and maintaining codes of ethics without contextualising them risks forcing healthcare professionals and students in clinical practice to adapt to ethical practice without questioning their own beliefs. Thus, ethical competence risks being hampered by limited reflection and moral reasoning about the situation as a whole [ 29 ].
In summary, ethical problems in everyday healthcare work arise for many reasons, and sometimes themselves constitute threats to ethical values. Hence, healthcare professionals and students in clinical practice require readiness and the capability to recognise and respond appropriately to ethically problematic work situations. Therefore, the aim of this integrative review was to explore the available literature on ethics education that promotes ethical competency learning for healthcare professionals and students undergoing training in healthcare professions.
This integrative review followed the method described by Whittemore and Knafl and was used to summarise and synthesise the current state of research on a particular area of interest [ 30 ], which in this study was the area of ethics education in healthcare.
According to Whittemore and Knafl [ 30 ], the review process is composed of the following stages, which were applied in this study:
Stage 1: problem identification
Two questions were addressed in this review to explore the available literature regarding ethics education: (1) How can ethics education support the understanding and management of ethical problems in clinical practice? (2) What kind of design and course content can support ethical competence learning?
Stage 2: literature search
Prior to the literature search, a study protocol was submitted to the PROSPERO database with the ID number CRD42019123055. In collaboration with three experienced information specialists at a university library, guidance and support were provided in the creation of a search strategy. A systematic and comprehensive data search was conducted using the standards of the PRISMA guidelines [ 31 ]. To enhance the breadth and depth of the database searches, the main search strategy was based on three themes; study population, exposure/intervention and outcomes. The following search and/or Medical Subject Heading’s (MeSH) terms were used: ‘health personnel’, ‘students’, ‘ethics’, ‘moral’, ‘simulation’ and ‘teaching’. The search strategy was different between the databases as the construction of search and MeSH terms differs between the selected databases, see Table 1 . The main search was carried out between 22 and 23 June 2020 in three scientific publication databases and indexing services: PubMed, CINAHL, and PsycINFO. A supplementary search was carried out 10 January 2022.The searches was limited to (a) articles in English, (b) peer-reviewed articles, (c) theoretical articles as well as qualitative and quantitative empirical research articles, and d) articles published in the last 12 years (January 1, 2010–December 31, 2021). Articles were included if published after 2010, and they (a) described the design and content of ethics education for healthcare professionals or students in, or preparing for, clinical practice, and/or (b) described ethics education supportive of understanding and/or managing ethical problems in clinical practice. Articles were excluded if they focused on research ethics, ethical problems in a military context and ethical consultation with the primary and main goal of supporting ethical decision-making for an individual patient and the healthcare team. In the literature search, the search for “grey literature” such as dissertations, conference papers, reports, etc. was excluded since this was too resource and time consuming. The article searches resulted in 5953 articles, including 1559 in PubMed, 529 in CINAHL, and 3865 in PsycINFO. For a detailed description of the search results, see Fig. 1 . After the search process was completed, all the articles were uploaded onto Endnote X9 (Clarivate Analytics, Philadelphia, PA), and duplicates were then excluded (n = 860). A total of 5093 articles were then imported into the Rayyan QCRI, a web-based sorting tool for systematic literature reviews [ 32 ].
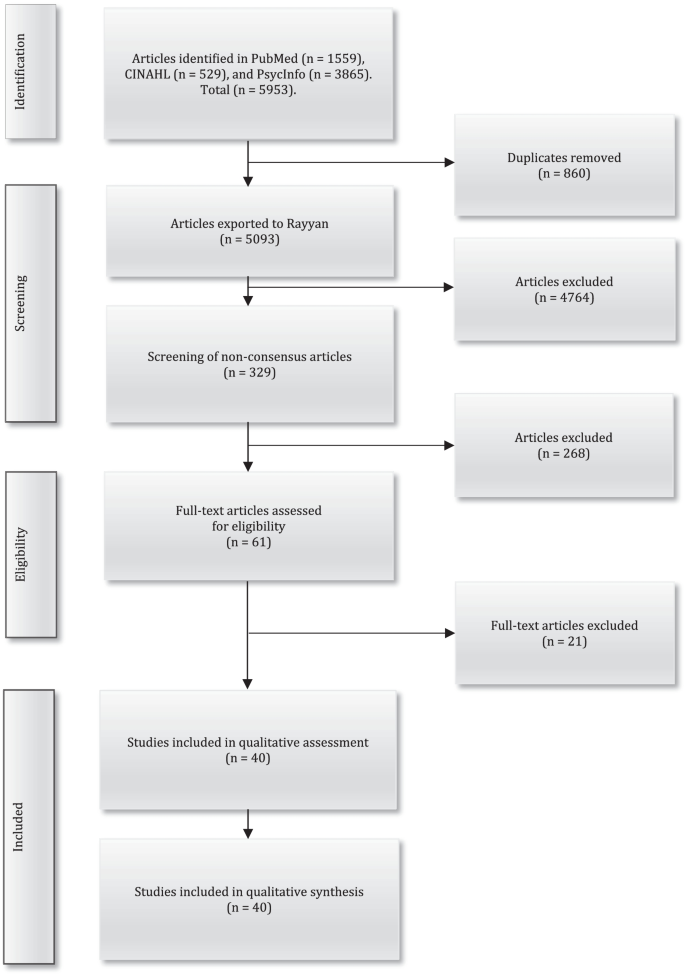
Flow diagram of the data selection and quality assessment process based on the PRISMA statement
Four of the authors (HA, AB, AS, and MH) independently screened all titles and abstracts, with the support of Rayyan QCRI, against the inclusion/exclusion criteria. The screening process consisted of two steps: (1) screening of articles identified in the main search and (2) screening of articles identified in the supplementary search. In the screening of articles identified in the main search, the blinded article selection in Rayyan QCRI indicated a 93% consensus between the authors with respect to the articles to exclude (n = 3811). After this, those articles for which there was no consensus regarding their inclusion (n = 287) were screened. Through discussions between the authors (HA, AB, AS, and MH), consensus was reached on which articles should then be excluded (n = 235). In the screening of articles identified in the supplementary search, the blinded article selection in Rayyan QCRI indicated a 95% consensus between the authors with respect to the articles to exclude (n = 953). After this, those articles for which there was no consensus regarding their inclusion (n = 42) were screened. Through discussions between the authors (HA, AB, AS, and MH), consensus was reached on which articles should then be excluded (n = 33). In total, 61 articles were selected for an additional full-text review. The articles were independently read in full by five of the authors (HA, AB, AS, MH, and AR) and then discussed, leading to an agreement to exclude 21 articles that did not meet the inclusion criteria. This led to 40 articles remaining for the quality assessment (see Fig. 1 ).
Stage 3: data evaluation
The quality assessment of the 40 articles was independently performed by two of the authors (HA and AB). A critical appraisal tool was used to score the articles on a four-graded scale (i.e., good, fair, poor, and very poor) [ 33 ]. The quality assessment consisted of two steps: (1) quality assessment of articles identified in the main search and (2) quality assessment of articles identified in the supplementary search. In the quality assessment of articles identified in the main search, there was consensus on the quality of 17 of the reviewed articles. However, there were different views on the quality assessment of 14 articles. Any discrepancies regarding authenticity, methodological quality, information value, and representativeness were considered, discussed, and resolved in the data evaluation process [ 34 ], leading to consensus between the authors regarding 11 articles pending between two adjacent grades: good–fair (n = 6), fair–poor (n = 3), and poor–very poor (n = 2). The authors’ quality assessment differed by more than one grade regarding three articles. However, even in these cases, the disagreement could be resolved through discussions between the two authors, after which a consensus was reached. In the quality assessment of articles identified in the supplementary search, there was consensus on the quality of 7 of the reviewed articles. However, there were different views on the quality assessment of 2 articles. Any discrepancies regarding authenticity, methodological quality, information value, and representativeness were considered, discussed, and resolved in the data evaluation process [ 34 ], leading to consensus between the authors regarding 2 articles pending between two adjacent grades good–fair. No articles were excluded due to a low-quality score. The characteristics of the included articles, as well as the quality scores, are presented in Table 2 .
Stage 4: data analysis
The data analysis was conducted by the first author. The findings were summarised and synthesised using a thematic analysis method [ 35 ] to identify the key themes that describe ethics education for healthcare professionals and students in clinical practice. This inductive approach also allowed us to answer the question regarding the design and content of ethics education and how ethics education could support the understanding and/or management of ethical problems in clinical practice, based on the available literature.
The analysis was conducted in the following six phases [ 35 ]: (1) reading and re-reading the included articles closely to become familiar with the data, (2) generating initial codes (228 codes in the present study) based on the information obtained from the included articles, (3) searching for themes, (4) reviewing themes, (5) defining and naming themes, and (6) producing a report where the findings are presented in terms of broad themes. The interpretation of the themes was discussed, and disagreement was resolved through discussion between the authors (HA, CF, AB, and AR) until a common understanding was reached.
Forty articles were included for review to explore the available literature regarding ethics education for healthcare professionals and students in clinical practice. The results showed a widespread international distribution of studies. Most of the studies were conducted in the United States (n = 5) and Taiwan (n = 5). When dividing the articles into continents, 17 were from Asia, 14 from Europe, six from North America, and three from Australia. Table 3 shows the key themes and sub-themes identified through the thematic analysis.
Making ethical competence learning possible
Making ethical competence learning possible for managing ethical problems in clinical practice requires support. However, this support entails those certain conditions be met for learning in the organisation in which ethics education is conducted, including opportunities to plan the education. The design and content of education are governed by external structures and the way in which the learning objectives have been specified. To support learning, it is also important that education is designed to facilitate opportunities to receive and create meaning with respect to the information received, change one’s own values and attitudes, and determine the consequences of one’s own actions. Interaction with others is important since it can constitute a valuable source of knowledge, especially with respect to determining whether the individual healthcare professional or student has understood or done something correctly. Simultaneously, ethics education is influenced by both the healthcare professionals and the students who have different qualifications, expectations, and strategies for their learning.
The factors influencing the planning and organization of ethical education were discussed in 32 articles. Three sub-themes were identified: (1) creating conditions for learning, (2) designing strategies for learning, and (3) interacting with others.
Creating conditions for learning
A starting point for making ethical competence learning possible is to identify and shed light on the kinds of ethical problems that healthcare professionals and students in clinical practice are expected to be able to manage and to create conditions for this learning. Therefore, it is important that ethics education reflect the relevant conditions for ethical competence learning by using real work situations [ 36 ]. One way to create such conditions is to construct appropriate learning objectives that clearly describe what should be achieved in terms of knowledge, skills, approaches, and values to effectively manage ethical problems [ 37 , 38 ]. However, the perception of what is relevant is influenced by healthcare professionals’ and students’ previous experiences of ethical problems in their everyday healthcare work. Limited experience entails a risk that the education will not be perceived as relevant, and that the educational content may be difficult to absorb [ 39 ].
Another condition that influences ethics education is the time available. Developing an ethical identity and creating meaning in discussions about ethical problems in everyday healthcare work takes time [ 37 , 40 ]. Simultaneously, it might be difficult to predict how long, for example, group discussions may take to shed light on the various aspects of ethical problems [ 39 ]. There is thus a risk that the time will be too short and insufficient to finish the discussion, or that there may be too much time, thus causing the discussions to be perceived as less engaged [ 37 ]. Therefore, it is important that the time aspect be considered in the design of education.
Finally, it is essential to create conditions for psychological safety and confidence in ethics education, or, in other words, to enable opportunities to express opinions or make blunders without this leading to consequences for the participants [ 41 ]. Instead, trust between the participants should be emphasised and acknowledged in discussions about ethical problems in clinical practice [ 40 , 42 , 43 ]. Simultaneously, there is a risk that high staff turnover and frequent changes in management may limit opportunities for building trust through conversation [ 44 ]. Passive or absent healthcare professionals and students might also limit opportunities for establishing such trust, for example, in group discussions [ 45 ].
Design strategies for learning
Different design strategies make ethical competence learning possible, through which the healthcare professionals and students can be brought to ask questions, make comments, and talk about their previous knowledge or own experiences. Knowledge of, for example, ethical values can be gained through theoretical lectures and the reading of appropriate literature [ 46 , 47 , 48 ]. Simultaneously, it is valuable to design ethics education so that theoretical learning activities are integrated with practical ones and thereby provide an experience of real-life situations [ 46 ]. Skills can be practiced through workshops [ 49 ], case studies and problem-solving sessions [ 37 , 43 , 47 , 48 , 50 , 51 , 52 , 53 ]. Understanding one’s own values and attitudes can be facilitated through, for example, role-play or simulation activities [ 54 , 55 , 56 ], narratives [ 40 , 57 , 58 ], storytelling [ 42 ] and discussions in small groups [ 38 , 43 , 44 , 45 , 47 , 59 , 60 , 61 , 62 ]. Small group discussions are appropriate when healthcare professionals or students are unwilling to stand out by asking questions or giving individual opinions in learning situations in which many people participate [ 63 ].
There are also different educational technologies to consider in the design of strategies for ethical competence learning. For example, the internet makes it easier to deliver lectures and carry out exercises [ 64 ], as well as to discuss issues in groups with digital aids [ 59 ]. This means that ethics education can take place in the form of internet-based education where video conferencing technique is used. This technique is valuable when using external educators in a rural setting for example in rural-based hospitals [ 59 ]. This technique is also useful to stimulate discussions with other healthcare professionals or students who are outside their regular workplaces [ 59 ]. However, a prerequisite for internet-based education is that the workplace has the required learning resources such as reliable internet connection and video equipment [ 64 ].
Ethics education needs to be built on strategies that optimise the ability to achieve the desired learning objectives [ 48 ]. To achieve these objectives, it may be necessary to choose different design strategies [ 36 ]. However, the strategy that best supports the development of a “professional self” is difficult to determine, for example, in terms of its ability to influence healthcare professionals’ and students’ capabilities for moral sensitivity [ 47 , 65 , 66 ] and critical thinking [ 47 ]. Nevertheless, support and learning activities do not necessarily promote ethical competence learning. Instead, these activities can also lead to stagnation in the development of ethical competence [ 67 , 68 ].
Interacting with others
An open atmosphere and interaction between participants are important in ethics education when sensitive issues are discussed [ 69 ]. Sometimes, it is difficult to express one’s critical thoughts about ethical problems in everyday healthcare work, since relationships with others and cohesion between individuals can be affected and compromised [ 45 , 57 ]. Simultaneously, there is a need for healthcare professionals and students to formulate their thoughts, feelings, and intentions about the ethical problems that they have observed themselves or heard about through colleagues [ 37 , 38 , 41 , 43 , 45 ]. Making ethical competence learning possible based on problem solving, interaction, and discussion of ethical problems in clinical practice can therefore be a support mechanism for healthcare professionals and students [ 37 ]. Learning together about issues that are perceived as ethically problematic can strengthen both the individual and their relationships with their colleagues [ 44 , 52 ].
Simulation is a way of highlighting ethical problems that exist in interactions with other individuals, such as patients or family members [ 54 ]. Narrative groupwork is another way of highlighting and processing ethical problems [ 57 ]. Through a narrative, different perspectives can be made visible and lead to in-depth learning about ethically challenging work situations [ 58 ]. With group discussions, ethical problems can be viewed in different ways [ 59 ], which in turn can lead to improvements in dealing with such problems [ 44 ]. However, if group discussions are to lead to improvements, it is necessary that there be a willingness to discuss what is perceived as ethically problematic in everyday healthcare work [ 38 , 45 ], as well as an interest in learning new approaches [ 37 ]. There is also a need for a welcoming climate in which the contradictions between different perceptions and attitudes can be balanced in a constructive way [ 43 , 51 ].
Having awareness of one’s own thoughts and perceptions
Ethical competence learning can help healthcare professionals and students in clinical practice direct their attention to ethical problems that they were not previously aware of. Such learning can involve unconscious attitudes, approaches, or emotions. These aspects influence how healthcare professionals and students react to ethical problems in everyday healthcare work.
The aspects that influence awareness of one’s own thoughts and perceptions were discussed in 22 articles in terms of both educational design and the content of ethics education. Two sub-themes were identified: (1) visualising attitudes and approaches, and (2) experiencing emotional conditions.
Visualising attitudes and approaches
Being aware of one’s own thoughts and perceptions in one’s attitudes and approaches to circumstances such as a certain illness, patient, or event influence what is perceived as an ethical problem in clinical practice [ 41 , 70 ]. One way of designing ethics education that facilitates the visualisation of ethical problems is to use a narrative approach [ 40 , 57 , 58 ]. Using narrative writing, one’s own or others’ attitudes and approaches to everyday healthcare work situations where ethical problems occur can be made visible [ 57 ]. Examples of such ethical problems are when honesty and respect for the patient are not demonstrated, or when the establishment of trust in the care encounter is lacking [ 57 ].
Another way to visualise one’s own or others’ attitudes and approaches when designing ethics education is to use learning activities based on problems or scenarios [ 48 , 51 , 52 , 54 , 55 , 56 , 64 ]. This ethical competence learning focuses on challenging and realistic situations, such as conflicts regarding informed consent or cases where tensions arise between the patient’s wishes and needs in relation to professional norms [ 36 ]. Problem- or scenario-based learning stimulates healthcare professionals and students to learn and develop new understandings that allow them to manage ethical problems in their clinical practice [ 36 ]. Such learning could also create a means of engagement to discuss how ethical problems should be managed [ 64 ]. The visibility can also emerge by reserving time for ethical reflection and, in systematic forms, discussing ethical problems in everyday healthcare work [ 38 , 43 , 44 , 45 , 59 , 70 ]. Attitudes towards a particular illness or patient, for example, govern our way of justifying the approaches used [ 70 ]. By highlighting how healthcare professionals and students think about and analyse their attitudes and approaches when designing ethics education, previous habits can be made visible and critically examined [ 44 ]. The visibility of attitudes and approaches promotes a process of change in one’s own thoughts and perceptions [ 43 , 45 ]. However, it is essential to consider that attitudes and approaches are complex, developed over time, and strongly influenced by the perceptions of individuals who are close to the healthcare professionals and students undergoing training in healthcare professions [ 36 , 48 ]. Accordingly, ethics education to support ethical competence learning does not always lead to a change in how ethical problems are managed in everyday clinical practice [ 71 ].
Experiencing emotional conditions
Awareness of one’s own or others’ emotions influences what is perceived as an ethical problem in everyday healthcare work. Healthcare professionals and students in clinical practice encounter a variety of ethical problems in which they are either actors or observers. Depending on the prevailing circumstances on site and at a given time, ethical problems, and their significance, as well as their relevance, can be experienced differently. When designing ethics education, real experiences, such as incidents that are ethically challenging and witnessed by healthcare professionals or students, can be used in ethical competence learning [ 58 ]. Group discussions make it possible for all participants to hear different interpretations and reflections on the same situation [ 38 , 45 ]. Furthermore, such discussions can draw attention to situations where care and treatment have been experienced as unethical, such as when the patients’ concerns are not heard, or their needs are not met [ 61 ].
By imitating a realistic situation through simulation, healthcare professionals and students are given the opportunity to learn about real-life situations, apply ethical content in the situation, and experience different emotional states [ 56 ]. Educational content that highlights emotions, such as feelings of dependence, vulnerability, fear of abandonment, and a lack of control, gives healthcare professionals and students an opportunity to change their perspectives on factors such as caregiving and care-recipients [ 55 ]. Simulation can also be a way to raise awareness of other people’s ways of feeling and experiencing specific work situations, regardless of whether they play the role of professional, patient, or family member [ 56 ].
Doing right by the patient’s best interests
Healthcare professionals and students in clinical practice are constantly faced with ethical problems related to patients, their significant others, colleagues, and the work organization. Dealing with such problems primarily involves reasoning about what is right and good to make decisions about what needs to be done in a specific situation. However, doing right based on the patient’s best interests can sometimes jeopardize the management of ethical problems since it could conflict with other patients’ interest, which may not be ethically acceptable or legally permitted.
Those aspects influencing healthcare professionals’ and students’ capabilities to do right by the patient’s best interests were discussed in 19 articles. Two sub-themes were identified: (1) managing emotions and tensions, and (2) managing different perspectives in the situation.
Managing emotions and tensions
Ethical problems can provoke strong emotions, such as anger, disapproval, and frustration [ 40 ]. These emotions, in turn, generate tensions, such as those between ethical values and legal principles in relation to how healthcare professionals and students in clinical practice perceive a particular situation [ 40 , 51 ]. Therefore, it is essential that ethics education be designed to provide time and space for reflection. By reflecting together with others, thoughts and perceptions about these emotions and tensions can be verbalised [ 43 , 72 ]. Ethics education should provide the opportunity to learn how to deal with emotions [ 40 ] and foster understanding of what is ethically ‘right’ or ‘wrong’ for the patient [ 45 ], which in turn influences the decisions made by healthcare professionals and students in clinical practice [ 51 , 70 ]. Group discussion, for example in ethics seminar, is a way to reduce unethical behaviour [ 73 ]. There is, however, a difference between learning how to manage ethical problems in everyday healthcare work and how these problems are actually managed, since one’s own inabilities or limitations may influence the outcome [ 62 ].
Managing different perspectives on the situation
In everyday healthcare work, healthcare professionals and students face several challenges in determining how to ‘do the right thing’ in situations that arise in their contact with patients and their significant others. Ethical problems can arise when two perspectives, such as an ethical and a legal perspective, collide, as would be the case when there is conflict between what is perceived to be best for the patient and the patient’s right to self-determination [ 37 ]. There may also be a feeling of inadequacy in managing ethical problems in care situations [ 38 ] since there is rarely only one way to cope with the situation [ 51 ]. Therefore, ethics education needs to be designed in such a way that the content includes both medical and ethical reasoning when the care situation is to be resolved [ 70 , 74 ].
The design of such training could consist of lectures that are combined with watching movies, playing games, and performing case analyses and group discussions [ 37 , 47 , 60 , 65 ]. Through such training, an increased understanding of ethical problems can be gained [ 54 , 72 ], for example, regarding the ways in which certain patients, events, and situations are to be viewed [ 37 , 57 , 65 ]. Ethical competence learning with a focus on ‘thinking ethics’ and problematising one’s own capabilities to judge and act can be an eye-opener for healthcare professionals and students [ 72 , 75 ]. This can strengthen the capability to identify certain situations and provide examples of instances where ethical values and norms have been violated [ 66 ].
Even if the design and content of ethics education focus on thinking about critical ethics, this does not necessarily mean that the degree of critical ethics thinking is influenced [ 47 ]. Prerequisites for ethical competence learning of how to manage different perspectives and do right by the patient’s best interests are, among other things, that there is time for discussion, and that the educational content is perceived as useful [ 37 ]. It is also crucial that such learning be based on consideration and respect for different beliefs, so that ethical problems can be managed effectively in everyday healthcare work [ 43 , 44 , 45 , 54 ].
Making ethical competence learning possible, having awareness of one’s own thoughts and perceptions, and doing right by the patient’s best interests are important aspects when seeking to increase the understanding and management of ethical problems in everyday healthcare work.
An important aspect emphasised in the present study is the need to create a psychosocial climate that allows healthcare professionals and students to feel safe. Previous knowledge reveals that feeling psychologically safe is important for engagement in educational activities, regardless of the context in which they are implemented [ 76 ]. Hence, it is important that educators use an approach that clarifies what psychological security in feedback conversations can look like [ 77 ]. To promote effective learning conditions in which healthcare professionals and students feel safe, educators need to encourage an open dialogue aimed at enhancing the implementation of the intended learning activity [ 76 , 77 ].
The results present different designs and educational strategies for making ethical competence learning possible. In general, it is essential that educators develop course content that supports healthcare professionals and students in developing ethical competence in terms of their ethical decision-making ability and the moral courage to confront ethical dilemmas [ 78 ]. However, although ethical education might increase ethical sensitivity and the ability to detect an ethical problem, it is not obvious that education influences the development of ethical behaviour [ 79 ].
The results show how interaction with others is important since it constitutes a valuable source of knowledge; it also allows for the determination of whether the individual healthcare professional or student has understood or done something in an ethically defensible manner. Relationships between people constitute the foundation of ethics, and ethics is essential to the maintenance of relationships between two or more people [ 80 ].
Another critical aspect is the value of clinical experience. According to the results, limited experience poses a potential risk of not enabling healthcare professionals and students to absorb and contextually relate to the content of ethical education. However, previous research indicates that those with less clinical experience are more perceptive of ethical issues than more experienced colleagues, possibly counteracting the potential lack of experience [ 11 ].
The results underline the significance of attending to ethical problems that individual participants in ethics education may not already be aware of. This might be related to the fact that the patients, healthcare professionals, and students each have different and unique perspectives in caring encounters. To provide care based on the preferences of a specific patient, one needs insight into the patient’s lifeworld [ 81 ]. This might pose some challenges in designing and developing course content for ethics education.
Further, based on the present results, narrative approaches and realistic simulation are considered components that could influence ethical competence learning. Such learning should be based on the patient’s perspective to transform healthcare professionals’ and students’ tacit knowledge into explicit knowledge with support from reflective practice [ 82 ]. According to this, reflection with some theoretical depth grounded in caring science can contribute to a deeper understanding beyond that which is common in the clinical practice [ 83 ]. However, being aware of ethical problems—earlier not being aware of—raises new moral concerns among healthcare professionals and students. Thus, ethical education needs to be dynamically designed to capture different aspects of ethical problems.
The result highlights the importance of doing right by the patient’s best interests. Besides clinical competence, decisions regarding care and treatment also require ethical competence [ 3 ]. To do the right and good thing, an educational design that emphasises the healthcare professionals’ and students’ personal experiences, understanding, and views is required; such a skill can be cultivated, for example, through reflection [ 84 ]. Approaches such as moral case deliberation, ethics rounds, or discussion groups can be advantageously used to support ethical reflection [ 85 ]. At the same time, there are challenges regarding how ethical problems can be handled in clinical practice. Each problem and situation is unique, complex, and uncertain, since it can never be completely predicted. Therefore, doing right by the patient’s best interests may not necessarily only be about what to do in a specific situation; it can also be about scrutinising, interpreting, and processing other healthcare professionals’ and students’ knowledge, skills, and attitudes to ethical problems in clinical practice.
Doing right by the patient’s best interests also requires an educational design that provides space and time for reflection. Research indicates that the opportunity to share thoughts and obtain support from others, as well as from the organization, when ethical problems occur is considered helpful [ 86 ]. However, there are other factors that are essential for reflection. Space for reflection, for example, to create psychological safety is crucial for healthcare professionals and students to express themselves or make blunders without this leading to consequences. A hierarchical organizational climate influences sensitivity to ethical concerns, and a conformist work attitude could lead to an unwillingness to challenge routines in everyday clinical practice [ 86 ]. Time is also required to ensure that there is an opportunity for reflection. Without time, there is a risk that decision-making regarding ethical problems may become inconsistent [ 87 ].
Methodological strengths and limitations
This study followed the recommendations for conducting and reporting the results of an integrative systematic review, and the researchers have strived to make the research process as transparent as possible, which is considered to have strengthened its reliability.
In this study, a broad literature search strategy was used to find as many articles as possible to answer the study aim and research questions. However, some issues may be encountered when conducting broad literature searches. One is that such a literature search likely leads to a greater number of irrelevant articles that match the search criteria. Another weakness is that it is time consuming to review a great number of articles. Accordingly, there is a risk that relevant articles may have been accidentally deleted, thereby weakening the validity of the study. However, this risk was partly managed by involving four of the authors in the screening process against the inclusion/exclusion criteria. The decision not to include “grey literature” can be considered a limitation as this may have affected the validity of the results.
Three available databases at a university in western Sweden were used. Since universities have different levels of licenses to access the contents of the databases, there is a risk that the search terms and search strings used in this study have failed to identify all articles on ethics education due to limited license agreements. Thus, there is a risk that some articles that are available in more extensive license agreements are not included in this literature review, which should be considered a limitation.
The decision not to include the perspective of those who supervise, and mediate ethics education could be seen as a weakness. However, it was a deliberate choice not to include the search term ‘educators’ based on the study aim and research questions. The requirements for educators can be different depending on whether the participants are students at a university or if they are healthcare professionals and are taught at their workplace. However, continued research on what competencies these educators should have in relation to supporting the learning and development of ethical competencies is important, and possibly points to a need for a systematic literature review that describes the educators’ competencies.
This study is limited to and focused on providing answers to questions regarding ethics education in various healthcare contexts in different countries. This is considered, on the one hand, to strengthen the validity and transferability of the results and, on the other hand, to limit the transferability of the results to contexts with similar cultural, economic, and social conditions, which are reflected in the included articles.
This integrative systematic review provides insights into ethics education for healthcare professionals, students, and educators. The results show that ethical competence learning is essential when seeking to draw attention to and deal effectively with ethical problems. Healthcare professionals and students in clinical practice need a supportive learning environment in which they can experience a permissive climate for reflection on ethical challenges, conflicts, or dilemmas that influence everyday healthcare work. The design and course content of ethics education meant to increase the understanding and management of ethical problems in clinical practice may vary. However, regardless of the design or course content, educators need supportive conditions both on campus and in clinical practice to maximise opportunities to generate a high level of learning in ethics education.
Further studies on ethics education should be carried out. Comparative research, through which different educational designs can illuminate what provides the best possible learning process for managing ethical problems, would be valuable. Intervention studies aiming to maintain and protect the autonomy of patients with impaired decision-making capabilities may also be warranted. Another interesting area for further studies is about the educators’ and their competencies in ethics education with a special focus on the requirements if the participants are students at a university or if they are healthcare personnel and are taught at their workplace. Further studies could be used to develop healthcare professionals’ and students’ readiness and capabilities to recognise and respond appropriately when they encounter ethically problematic situations. This would, in turn, give healthcare professionals and students a sense of self-confidence and faith in their everyday clinical practice.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author upon reasonable request.
Langeland K, Sørlie V. Ethical challenges in nursing emergency practice. J Clin Nurs. 2011;20:2064–70.
Google Scholar
Zafar W. Moral experience and ethical challenges in an emergency department in Pakistan: emergency physicians’ perspectives. Emerg Med J. 2015;32:263–8.
Lechasseur K, Caux C, Dollé S, Legault A. Ethical competence: an integrative review. Nurs Ethics. 2018;25(6):694–706.
Bremer A, Holmberg M. Ethical conflicts in patient relationships: experiences of ambulance nursing students. Nurs Ethics. 2020;27(4):946–59.
Svensson A, Bremer A, Rantala A, Andersson H, Williams J, Devenish S, et al. Ambulance clinicians’ attitudes to older patients’ self-determination when the patient has impaired decision-making ability: a Delphi study. Int J Older People Nurs. 2021. https://doi.org/10.1111/opn.12423 .
Article Google Scholar
Holmberg M, Forslund K, Wahlberg AC, Fagerberg I. To surrender in dependence of another: the relationship with the ambulance clinicians experienced by patients. Scand J Caring Sci. 2014;28:544–51.
McConnell D, McCance T, Melby V. Exploring person-centredness in emergency departments: a literature review. Int Emerg Nurs. 2016;26:38–46.
Wireklint Sundström B, Dahlberg K. Caring assessment in the Swedish ambulance services re-lieves suffering and enables safe decisions. Int Emerg Nurs. 2011;19:113–9.
Andersson H, Jakobsson E, Furåker C, Nilsson K. The everyday work at a Swedish emergency department: the practitioners’ perspective. Int Emerg Nurs. 2012;20:58–68.
Svensson C, Bremer A, Holmberg M. Ambulance nurses’ experiences of patient relationships in urgent and emergency situations: a qualitative exploration. Clin Ethics. 2019;14(2):70–9.
Ulrich CM, Taylor C, Soeken K, O’Donnell P, Farrar A, Danis M, et al. Everyday ethics: ethical issues and stress in nursing practice. J Adv Nurs. 2010;66(11):2510–9.
Torabi M, Borhani F, Abbaszadeh A, Atashzadeh-Shoorideh F. Barriers to ethical decision-makingfor pre-hospital care professionals. Nurs Ethics. 2020;27(2):407–18.
The Swedish Society of Nursing. Values for nursing. Stockholm: The Swedish Society of Nursing; 2016.
Beauchamp T, Childress J. Principles of biomedical ethics. 8th ed. New York: Oxford University Press; 2019.
Torabi M, Borhani F, Abbaszadeh A, Atashzadeh-Shoorideh F. Experiences of pre-hospital emergency medical personnel in ethical decision-making: a qualitative study. BMC Med Ethics. 2018;19:95. https://doi.org/10.1186/s12910-018-0334-x .
Fernandez-Parsons R, Rodriguez L, Goyal D. Moral distress in emergency nurses. J Emerg Nurs. 2013;39(6):547–52.
Wilkinson JM. Moral distress in nursing practice. Nurs Forum. 1987/1988;23(1):16–29.
Murray E, Krahé C, Goodsman D. Are medical students in prehospital care at risk of moral injury? Emerg Med J. 2018;35:590–4.
Ellström P-E. The many meanings of occupational competence and qualification. J Eur Ind Training. 1997;21:266–73.
Poikkeus T, Numminen O, Suhonen R, Leino-Kilpi H. A mixed-method systematic review: support for ethical competence of nurses. J Adv Nurs. 2014;70(2):256–71.
Poikkeus T, Suhonen R, Katajisto J, Leino-Kilpi H. Organisational and individual support for nurses’ ethical competence: a cross-sectional survey. Nurs Ethics. 2018;25(3):376–92.
Kälvemark-Sporrong S, Arnetz B, Hansson M, Westerholm P, Höglund A. Developing ethical competence in health care organizations. Nurs Ethics. 2007;14:825–37.
Trobec I, Starcic A. Developing nursing ethical competences online versus in traditional classroom. Nurs Ethics. 2015;22(3):352–66.
Vanlaere L, Gastmans C. Ethics in nursing education: learning to reflect on care practices. Nurs Ethics. 2007;14(6):758–66.
Kalaitzidis E, Schmitz K. A study of an ethics education topics for undergraduate nursing students. Nurse Educ Today. 2012;32:111–5.
Numminen O, Leino-Kilpi H, van der Arend A, Katajisto J. Comparison of nurse educators’ and nursing students’ descriptions of teaching codes of ethics. Nurs Ethics. 2011;18(5):710–24.
Gisondi MA, Smith-Coggins R, Harter PM, Soltysik RC, Yarnold PR. Assessment of resident professionalism using high-fidelity simulation of ethical dilemmas. Acad Emerg Med. 2004;11(9):931–7.
Godbold R, Lees A. Ethics educations for health professionals: a values based approach. Nurse Edu Pract. 2013;13:553–60.
Mpeli M. Analysis of self-evaluated ethical competence of midwifery students at a selected nursing college in the Free State. Curationis. 2018;41(1):e1–9. https://doi.org/10.4102/curationis.v41i1.1925 .
Whittemore R, Knafl K. The integrative review: updated methodology. J Adv Nurs. 2005;52(5):546–53.
Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interven-tions: explanation and elaboration. BMJ. 2009;339:b2700. https://doi.org/10.1136/bmj.b2700 .
Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A. Rayyan—a web and mobile app for systematic reviews. Syst Rev. 2016;5:210. https://doi.org/10.1186/s13643-016-0384-4 .
Hawker S, Payne S, Kerr C, Hardey M, Powell J. Appraising the evidence: reviewing disparate data systematically. Qual Health Res. 2002;12(9):1284–99.
Kirkevold M. Integrative nursing research: an important strategy to further the development of nursing science and nursing practice. J Adv Nurs. 1997;25:977–84.
Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3(2):77–101.
Sherer R, Dong H, Cong Y, Wan J, Chen H, Wang Y, et al. Medical ethics education in China: lessons from three schools. Edu Health. 2017;30:35–43.
Schonfeld T, Johnson K, Seville E, Suratt C, Goedken J. Differences between two methods of ethics education: focus group results. Ethics Soc Welf. 2015;9(3):240–54.
Parker L, Watts L, Scicluna H. Clinical ethics ward rounds: building on the core curriculum. J Med Ethics. 2012;38:501–5.
Grace AJ, Kirkpatrick HA. Teaching ethics that honor the patient’s and the provider’s voice: the role of clinical integrity. Int J Psychiatry Med. 2018;53(5–6):445–54.
Gillam L, Delany C, Guillemin M, Warmington S. The role of emotions in health professional ethics teaching. J Med Ethics. 2014;40:331–5.
Honkavuo L. Ethics simulation in nursing education: nursing students’ experiences. Nurs Ethics. 2021;28(7–8):1269–81. https://doi.org/10.1177/0969733021994188 .
Paton A, Kotzee B. The fundamental role of storytelling and practical wisdom in facilitating the ethics education of junior doctors. Health. 2021;25(4):417–33. https://doi.org/10.1177/1363459319889102 .
Hem MH, Molewijk B, Gjerberg E, Lillemoen L, Pedersen R. The significance of ethics reflection groups in mental health care: a focus group study among health care professionals. BMC Med Ethics. 2018;19:54. https://doi.org/10.1186/s12910-018-0297-y .
Lillemoen L, Pedersen R. Ethics reflection groups in community health services: an evaluation study. BMC Med Ethics. 2015;16:25. https://doi.org/10.1186/s12910-015-0017-9 .
Blomberg K, Bisholt B. Clinical group supervision for integrating ethical reasoning: views from students and supervisors. Nurs Ethics. 2015;23(7):761–9.
Shamim M, Torda A, Baig L, Zubairi N, Balasooriya C. Systematic development and refinement of a contextually relevant strategy for undergraduate medical ethics education: a qualitative study. BMC Med Educ. 2021;21(1):9. https://doi.org/10.1186/s12909-020-02425-6 .
Yeom H-A, Ahn S-H, Kim S-J. Effects of ethics education on moral sensitivity of nursing students. Nurs Ethics. 2017;24(6):644–52.
Harasym PH, Tsai T-C, Munshi FM. Is problem-based learning an ideal format for developing ethical decision skills? Kaohsiung J Med Sci. 2013;29:523–9.
Mohammadi M, Sheikhasadi M, Mahani S, Taheri A, Sheikhbardsiri H, Abdi K. The effect of bio ethical principles education on ethical attitude of prehospital paramedic personnel. J Educ Health Promot. 2021;31(10):289. https://doi.org/10.4103/jehp.jehp_708_20 .
Monteverde S. Undergraduate healthcare ethics education, moral resilience, and the role of ethical theories. Nurs Ethics. 2013;21(4):385–401.
Lin Y-C, Chan T-F, Lai C-S, Chin C-C, Chou F-H, Lin H-J. The impact of an interprofessional problem-based learning curriculum of clinical ethics on medical and nursing students’ attitudes and ability of interprofessional collaboration: a pilot study. Kaohsiung J Med Sci. 2013;29:505–11.
Chou FC, Kwan C-Y, Hsin D. Examining the effects of interprofessional problem-based clinical ethics: findings from a mixed methods study. J Interprof Care. 2016;30(3):362–9.
McCormick AJ, Stowell-Weiss P, Carson J, Tebo G, Hanson I, Quesada B. Continuing education in ethical decision making using case studies from medical social work. Soc Work Health Care. 2014;53(4):344–63.
Buxton M, Phillippi JC, Collins MR. Simulation: a new approach to teaching ethics. J Midwifery Womens Health. 2015;60:70–4.
Gallagher A, Peacock M, Zasada M, Janssens N, Coucke T, Cox A. Care-givers’ reflections on an ethics education immersive simulation care experience: a series of epiphanous events. Nurs Inq. 2017;24:e12174.
Smith K, Klaassen J, Zimmerman C, Cheng A-L. The evolution of a high-fidelity patient simulation learning experience to teach legal and ethical issues. J Prof Nurs. 2013;29(3):168–73.
Tsuruwaka M, Asahara K. Narrative writing as a strategy for nursing ethics education in Japan. Int J Med Educ. 2018;9:198–205.
Pandya R, Shukla R, Gor AP, Ganguly B. Personal experience narratives by students: a teaching–learning tool in bioethics. Indian J Med Ethics. 2016;1(3):144–7.
Watts L, Parker L, Scicluna H. Rural ethics ward rounds: enhancing medical students’ ethical awareness in rural medicine. Aust J Rural Health. 2013;21:128–9.
Silén M, Haglund K, Hansson MG, Ramklint M. Ethics rounds do not improve the handling of ethical issues by psychiatric staff. Nord J Psychiatry. 2015;69(6):1700–7.
Langlois S, Lymer E. Learning professional ethics: student experiences in a health mentor program. Educ Health. 2016;29:10–5.
Kong WM, Knight S. Bridging the education–action gap: a near-peer case-based undergraduate ethics teaching programme. J Med Ethics. 2017;43:692–6.
Lee W, Choi S, Kim S, Min A. A case-centered approach to nursing ethics education: a qualitative study. Int J Environ Res Public Health. 2020;17(21):7748. https://doi.org/10.3390/ijerph17217748 .
Hsu L-L. Blended learning in ethics education: a survey of nursing students. Nurs Ethics. 2011;18(3):418–30.
Maddineshat M, Yousefzadeh MR, Mohseni M, Maghsoudi Z, Ghaffari ME. Teaching ethics using games: impact on Iranian nursing students’ moral sensitivity. Indian J Med Ethics. 2019;4(1):14–20.
Baykara ZG, Demir SG, Yaman S. The effect of ethics training on students recognizing ethical violations and developing moral sensitivity. Nurs Ethics. 2015;22(6):661–75.
Martins V, Santoss C, Duarte I. Bioethics education and the development of nursing students’ moral competence. Nurse Educ Today. 2020;95: 104601. https://doi.org/10.1016/j.nedt.2020.104601 .
Martins V, Santos C, Bataglia P, Duarte I. The teaching of ethics and the moral competence of medical and nursing students. Health Care Anal. 2021;29(2):113–26. https://doi.org/10.1007/s10728-020-00401-1 .
Kuhn E, Lunden L, Moysich P, Rogge K, Roscher M, Caning L, et al. Ethik First: extracurricular support for medical students and young physicians facing moral dilemmas in hospital routine. GMS J Med Educ. 2021. https://doi.org/10.3205/zma001470 .
Tsai T-C, Harasym PH. A medical ethical reasoning model and its contributions to medical education. Med Educ. 2010;44:864–73.
Bowsher G, Parry-Billings L, Georgeson A, Baraitser P. Ethical learning on international medical electives: a case-based analysis of medical student learning experiences. BMC Med Educ. 2018;18:78. https://doi.org/10.1186/s12909-018-1181-7 .
Savitha D, Vaz M, Vaz M. “Thinking ethics”: a novel, pilot, proof-of-concept program of integrating ethics into the physiology curriculum in South India. Adv Physiol Educ. 2017;41:306–11.
Lee C, Kim S, Choe K, Kim S. Effect of ethics seminar on moral sensitivity and ethical behavior of clinical nurses. Int J Environ Res Public Health. 2021;18(1):241. https://doi.org/10.3390/ijerph18010241 .
Torabizadeh C, Homayuni L, Moattari M. Impacts of Socratic questioning on moral reasoning of nursing students. Nurs Ethics. 2016;25(2):174–85.
Sánchez- Izquierdo M, Santacreu M, Olmos R, Fernández-Ballesteros R. A training intervention to reduce paternalistic care and promote autonomy: a preliminary study. Clin Interv Aging. 2019;14:1515–25.
Lyman B, Mendon C. Pre-licensure nursing students’ experiences of psychological safety: a qualitative descriptive study. Nurs Educ Today. 2021;105: 105026. https://doi.org/10.1016/j.nedt.2021.105026 .
Johnson C, Keating J, Molloy E. Psychological safety in feedback: what does it look like and how can educators work with learners to foster it? Med Educ. 2020;54(6):559–70.
Albert J, Younas A, Sana S. Nursing students’ ethical dilemmas regarding patient care: an integrative review. Nurse Educ Today. 2020;88:104389. https://doi.org/10.1016/j.nedt.2020.104389 .
Cannaerts N, Gastmans C, Dierckx de Casterlé B. Contribution of ethics education to the ethical competence of nursing students: educators’ and students’ perceptions. Nurs Ethics. 2014;21(8):861–78.
Ulrich C. Nursing ethics in everyday practice. Indianapolis: Sigma Theta Tau International; 2012.
Dahlberg K, Segesten K. Health and caring in theory and praxis. Stockholm: Natur & Kultur; 2010. ( (in Swedish) ).
Schön DA. The reflective practitioner. How professionals think in action. Farnhamn: Ashgate Publishing; 1991.
Lindberg E. Lecturers’ lived experiences of guiding reflective seminars during nursing education. Nurse Educ Pract. 2018;31:165–70.
Ekeberg M. A learning model for nursing students during clinical studies. Nurse Educ Prac. 2011;11:384–9.
Haan MM, van Gurp J, Naber S, Groenewoud AS. Impact of moral case deliberation in healthcare settings: a literature review. BMC Med Ethics. 2018;19:85. https://doi.org/10.1186/s12910-018-0325-y .
Huang FF, Yang Q, Zhang J, Khoshnood K, Zhang JP. Chinese nurses’ perceived barriers and facilitators of ethical sensitivity. Nurs Ethics. 2016;23:507–22.
Rogne L, McCune S. Advanced care planning. Communicating about mattes of life and death. New York: Springer; 2013.
Download references
Acknowledgements
We would like to thank the librarians Anna Wolke, Ida Henriksson, and Lynn Rudholm at Linnaeus University for their valuable assistance with the systematic literature search process.
Open access funding provided by University of Boras. The authors received the following financial support for the research, authorship, and/or publication of this article: This work was funded by the Kamprad Family Foundation for Entrepreneurship, Research & Charity (Ref. No. 20180157).
Author information
Authors and affiliations.
Faculty of Health and Life Sciences, Linnaeus University, Växjö, Sweden
Henrik Andersson, Anders Svensson, Catharina Frank, Mats Holmberg & Anders Bremer
Centre of Interprofessional Collaboration within Emergency Care (CICE), Linnaeus University, Växjö, Sweden
Henrik Andersson, Anders Svensson, Catharina Frank, Andreas Rantala, Mats Holmberg & Anders Bremer
Faculty of Caring Science, Work Life, and Social Welfare, University of Borås, 50190, Borås, Sweden
Henrik Andersson
Department of Ambulance Service, Region Kronoberg, Växjö, Sweden
Anders Svensson
Department of Health Sciences, Lund University, Lund, Sweden
Andreas Rantala
Emergency Department, Helsingborg General Hospital, Helsingborg, Sweden
Centre for Clinical Research Sörmland, Uppsala University, Eskilstuna, Sweden
Mats Holmberg
Department of Ambulance Service, Region Sörmland, Katrineholm, Sweden
Department of Ambulance Service, Region Kalmar County, Kalmar, Sweden
Anders Bremer
You can also search for this author in PubMed Google Scholar
Contributions
All the authors contributed to the study design. The review design and literature search were performed by HA and AB. Data extraction was done by HA, AB, AS, MH, and AR. The data analysis was conducted by HA, CF, AB, and AR. All authors made substantial contributions to the study and have read and approved the final version of the submitted manuscript. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Henrik Andersson .
Ethics declarations
Ethics approval and consent to participate.
Not applicable.
Consent for publication
Competing interests.
The authors declare that they have no competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Andersson, H., Svensson, A., Frank, C. et al. Ethics education to support ethical competence learning in healthcare: an integrative systematic review. BMC Med Ethics 23 , 29 (2022). https://doi.org/10.1186/s12910-022-00766-z
Download citation
Received : 16 December 2021
Accepted : 07 March 2022
Published : 19 March 2022
DOI : https://doi.org/10.1186/s12910-022-00766-z
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Ethical competencies
- Ethical problems
- Ethics education
- Healthcare professionals
- Integrative systematic review
BMC Medical Ethics
ISSN: 1472-6939
- General enquiries: [email protected]
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- My Bibliography
- Collections
- Citation manager
Save citation to file
Email citation, add to collections.
- Create a new collection
- Add to an existing collection
Add to My Bibliography
Your saved search, create a file for external citation management software, your rss feed.
- Search in PubMed
- Search in NLM Catalog
- Add to Search
[Ethics in medical education]
Affiliation.
- 1 Institut für Geschichte, Ethik und Philosophie der Medizin, Medizinische Hochschule Hannover, Hannover, BRD. [email protected]
- PMID: 18787865
- DOI: 10.1007/s00103-008-0608-4
Ethics education is a topic of growing importance in the medical curriculum. Medical ethics can be defined as the skilled professional discourse on moral issues in patient care, medical research and the health-care system. Ethical competence comprises conscientiousness and the ability to give reasons for intuitive moral convictions. In the curriculum, course content and didactic approaches should be aimed at all levels (cognitive, affective, practical), as discussed in this paper. Case based seminars are the gold standard of ethics education. The teacher's responsibility is rooted in their character as role models during case discussions. Ethics education should continue throughout the curriculum. In Germany the compulsory subject "history, theory, ethics of medicine" is predominant in the curriculum, but courses vary greatly between different universities. Further research is needed in the fields of adequate assessment formats and evaluation of final outcomes of ethics education. Interprofessional ethics education (undergraduate and postgraduate) is a major challenge for the future, especially since services for clinical ethics consultation and moral case deliberation are becoming more established in German hospitals.
PubMed Disclaimer
Similar articles
- Ethics education in research involving human beings in undergraduate medicine curriculum in Brazil. Novaes MR, Guilhem D, Barragan E, Mennin S. Novaes MR, et al. Dev World Bioeth. 2013 Dec;13(3):163-8. doi: 10.1111/j.1471-8847.2012.00336.x. Epub 2012 Sep 20. Dev World Bioeth. 2013. PMID: 22994866
- The Medical Ethics Curriculum in Medical Schools: Present and Future. Giubilini A, Milnes S, Savulescu J. Giubilini A, et al. J Clin Ethics. 2016 summer;27(2):129-45. J Clin Ethics. 2016. PMID: 27333063
- Education in medical ethics. Sidorov JJ. Sidorov JJ. Gastroenterol Jpn. 1993 Jul;28 Suppl 6:3-7; discussion 8-10. Gastroenterol Jpn. 1993. PMID: 8359632
- Ethics education: curricular considerations for the allied health disciplines. Layman E. Layman E. J Allied Health. 1996 Spring;25(2):149-60. J Allied Health. 1996. PMID: 8827428 Review.
- Medical ethics education: past, present, and future. Fox E, Arnold RM, Brody B. Fox E, et al. Acad Med. 1995 Sep;70(9):761-9. Acad Med. 1995. PMID: 7669152 Review.
- Analyzing the Evolution of Medical Ethics Education: A Bibliometric Analysis of the Top 100 Cited Articles. Roy S, Shah MH, Ahluwalia A, Harky A. Roy S, et al. Cureus. 2023 Jul 5;15(7):e41411. doi: 10.7759/cureus.41411. eCollection 2023 Jul. Cureus. 2023. PMID: 37416085 Free PMC article. Review.
- Ethics education in pediatrics: Implementation and evaluation of an interactive online course for medical students. Kidszun A, Forth FA, Matheisl D, Busch F, Kaltbeitzel L, Kurz S. Kidszun A, et al. GMS J Med Educ. 2022 Nov 15;39(5):Doc55. doi: 10.3205/zma001576. eCollection 2022. GMS J Med Educ. 2022. PMID: 36540566 Free PMC article.
- [Moral distress in medical students and young professionals: research desiderata in the context of the COVID-19 pandemic]. Kühlmeyer K, Kuhn E, Knochel K, Hildesheim H, Witt VD, Friedrich O, Rogge A. Kühlmeyer K, et al. Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz. 2020 Dec;63(12):1483-1490. doi: 10.1007/s00103-020-03244-2. Epub 2020 Nov 12. Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz. 2020. PMID: 33180160 Free PMC article. Review. German.
- Medical ethics: knowledge, attitude and practice among doctors in three teaching hospitals in Sri Lanka. Ranasinghe AWIP, Fernando B, Sumathipala A, Gunathunga W. Ranasinghe AWIP, et al. BMC Med Ethics. 2020 Aug 5;21(1):69. doi: 10.1186/s12910-020-00511-4. BMC Med Ethics. 2020. PMID: 32758219 Free PMC article.
Publication types
- Search in MeSH
Related information
Linkout - more resources, full text sources.
- MedlinePlus Health Information
- Citation Manager
NCBI Literature Resources
MeSH PMC Bookshelf Disclaimer
The PubMed wordmark and PubMed logo are registered trademarks of the U.S. Department of Health and Human Services (HHS). Unauthorized use of these marks is strictly prohibited.
Department of Medical Ethics

The Department of Medical Ethics (DME) strives to assist the CHOP community – patients, parents and staff – to respond to the ethical challenges we face, seeking understanding, and promoting the best interest of children. To achieve this goal, the DME:
- supports the Ethics Consultation Service
- oversees the CHOP Ethics Committee
- offers extensive ethics education to all CHOP staff members (clinical and non-clinical)
Ethics Consult Service
As a parent or guardian, you may have questions or concerns about your child’s care that involve your values or beliefs. These kinds of concerns are called “ethical” concerns. If you have an ethical concern or experience a conflict, we encourage you to use our Ethics Consultation Service . Free to use 24/7, this service offers help to patients, families and the healthcare team to resolve any ethical issues that may arise.
Ethics Committee
The Ethics Committee is a standing committee of the CHOP Medical Staff. Its members include at least six members of the Medical Staff, including the physician co-chair, who is appointed for a 2-year term by Medical Staff leadership.
The Committee membership represents multiple disciplines and backgrounds and includes, but is not limited to, representation from the medical staff, nursing, social work, chaplaincy, child life and school programs, behavioral health, and CHOP’s family partners.
The Committee's duties include:
- Promoting education about ethical issues
- Providing guidance to CHOP regarding ethics issues
- Reviewing pertinent policies associated with institutional ethics and patient rights

Meet our team
Our Medical Ethics team is available to help families (and the clinical team) navigate any ethical concerns they may have about the best care for our patients.

Medical ethic resources for families
We have created resources in partnership with families to help provide guidance around ethical interactions and frequently asked questions many families have about interacting with their care teams.

Medical ethics education for professionals
Healthcare professionals can access free online educational modules that focus on important concepts in pediatric medical ethics. Modules can be accessed 24/7 through CHOP’s Online Pediatric Education Network (OPEN). Search by “ethics” to find relevant courses.
Medical ethics education for CHOP staff
The Department of Medical Ethics provides educational opportunities to CHOP staff (clinical and non-clinical), such as Ethics Brown Bags, Ethics Case Discussions, Ethics Grand Rounds and other sessions as requested. These educational opportunities allow CHOP staff members to expand their understanding of medical ethics and their ability to apply that knowledge to their daily work.
Some frequent medical ethics education topics include:
- Decision making for children
- Ethical dilemmas related to social media
- Professional boundaries in therapeutic relationships
In addition, a series of pediatric ethics online education sessions – focused on concepts in pediatric medical ethics – can be accessed 24/7 through CHOP’s Department of Medical Ethics SharePoint site . NOTE: This site is only accessible to CHOP staff.

IMAGES
COMMENTS
As research participants, medical trainees may face several risks and in many ways constitute a vulnerable group. In this commentary, the author examines several of the ethical challenges involved in medical education research, including confidentiality and the risk of stigma; the need for equity, diversity, and inclusion; genetic testing of ...
The 4 main ethical principles, that is beneficence, nonmaleficence, autonomy, and justice, are defined and explained. Informed consent, truth-telling, and confidentiality spring from the principle of autonomy, and each of them is discussed. In patient care situations, not infrequently, there are conflicts between ethical principles (especially ...
In this commentary, the author examines several of the ethical challenges involved in medical education research, including confidentiality and the risk of stigma; the need for equity, diversity, and inclusion; genetic testing of students; clustered randomized trials of training programs; and questions about quality improvement activities.
The Accreditation Council for Graduation Medical Education (ACGME) has adopted requirements for competency in, among other areas, professionalism, practice-based learning and improvement, and systems based practices. Learning outcomes for these competencies require residents to demonstrate a commitment to ethical principles of health care ...
The ethics of medical education can be informed by the ethics of research on human subjects. We provide a theoretical framework for ethical medical education by extending three key concepts from the literature of research ethics—respect for individuals, beneficence, and distributive justice. Within the framework provided by these concepts, we ...
In contrast, the ethics of medical research on human subjects have been the subject of much analysis and policy development.8 A compelling analogy exists between such research and medical education.910In both cases doctors ask patients to participate in an endeavour whose primary aim is to benefit society as a whole, not the individual.
We emulated the Scoping Review method articulated by Levac [] to evaluate and collate information found on virtue and care ethics in medical education, then analyze relevant themes, and make note of significant metaphors that then lend themselves to our research question [26, 28, 43].We first identified our research question, identified relevant citations, extracted data from the literature ...
The ethics of research in health professions education has developed quite extensively in the past few decades, following advances in biomedical and other research domains, and are now grounded in several useful and authoritative guidelines. At the end of the day, however, ethical research conduct is a matter of internalized rules and ...
Medical ethics education is crucial for preparing medical students to face ethical situations that can arise in patient care. Instances of ethics being integrated into biomedical science education to build the connection between human science and ethics is limited. The specific aim of this study was to measure student attitudes towards an innovative curriculum design that integrates ethics ...
Our study was limited to medical students' perspective only, if the audience of this research was expanded to practicing doctors, the study would have been more well-rounded. ... Ozgonul, L., & Alimoglu, M. K. (2019). Comparison of lecture and team-based learning in medical ethics education. Nursing Ethics, 26(3), 903-913. https://doi.org ...
There is a lack of consistency in curriculum planning for bioethics education in Portuguese medical schools. Bioethics may be taught in different curricular years at each school (Conselho de Escolas Médicas Portuguesas, 2021).In the medical school where this study was developed, bioethics is taught in the fourth academic year with 30 hours of workload dedicated to it.
Medical research involving human subjects must be conducted only by individuals with the appropriate ethics and scientific education, training and qualifications. Research on patients or healthy volunteers requires the supervision of a competent and appropriately qualified physician or other health care professional.
In 1985, the landmark article "Basic Curricular Goals in Medical Ethics," known as the DeCamp Report, argued that basic instruction in medical ethics should be a requirement in all U.S. medical schools. 1 That same year, the Liaison Committee on Medical Education (LCME) introduced standards stipulating that in U.S. medical schools "ethical, behavioral, and socioeconomic subjects ...
Our hope is that the Fundamentals of Medical Ethics series will suggest broad lessons to keep in mind as physicians, patients, research participants, families, and communities struggle with new ...
The ethics of medical education can be informed by the ethics of research on human subjects. We provide a theoretical framework for ethical medical education by extending three key concepts from the literature of research ethics—respect for individuals, beneficence, and distributive justice. Within the framework provided by these concepts, we ...
The Accreditation Council for Graduation Medical Education (ACGME) has adopted requirements for competency in, among other areas, professionalism, practice-based learning and improvement, and systems based practices. Learning outcomes for these competencies require residents to demonstrate a commitment to ethical principles of health care ...
Research ethics topics also show a considerable variance within the regional medical schools. Approaches to teaching research ethics vary, even within the same country. The proposed model for education in this area is based on the United Nations Educational, Scientific and Cultural Organization Bioethics Core Curriculum.
Introduction. Whereas knowledge and competencies are the primary goals of formal medical training, an understanding of professional values and ethical conduct is essential for fostering the development of a good doctor [Citation 1 - Citation 3].In recent years, medical ethics has become a universal component of undergraduate and graduate education and clinical training [Citation 4].
Enhancing medical ethics education for medical students in clinical research - Jia Li, Zirui Zhou, Xiaohui Zhang 32. Alfaar AS, Hassan WM, Bakry MS, et al. Clinical Research Recession: Training N ...
Ethics in medical research deals with the conflicts of interest across various levels. Guidelines have been proposed for standardized ethical practice throughout the globe. The four fundamental principles of ethics which are being underscored are autonomy, non-maleficence, beneficence, and justice. Some special ethical issues have particular ...
A combination of moral principles and values that. are applied to take judgements in medical education, practice, and research are termed as medical ethics. History enlightens us that guidelines ...
Articles were excluded if they focused on research ethics, ethical problems in a military context and ethical consultation with the primary and main goal of supporting ethical decision-making for an individual patient and the healthcare team. ... Sherer R, Dong H, Cong Y, Wan J, Chen H, Wang Y, et al. Medical ethics education in China: lessons ...
This paper addresses current issues regarding the place and role of ethics in educational research. Academic researchers and professional associations have argued current ethical procedures in the form of ethics review committees are often lacking in knowledge and expertise of particular ethical contexts, including education (Sikes and Piper, 2010).
Ethics education is a topic of growing importance in the medical curriculum. Medical ethics can be defined as the skilled professional discourse on moral issues in patient care, medical research and the health-care system. Ethical competence comprises conscientiousness and the ability to give reasons for intuitive moral convictions.
The Department of Medical Ethics (DME) strives to assist the CHOP community - patients, parents and staff - to respond to the ethical challenges we face, seeking understanding, and promoting the best interest of children. To achieve this goal, the DME: supports the Ethics Consultation Service; oversees the CHOP Ethics Committee; offers extensive ethics education to all CHOP staff members ...