Nursing Case Study for Pneumonia
Watch More! Unlock the full videos with a FREE trial

Included In This Lesson
Study tools.
Access More! View the full outline and transcript with a FREE trial
Charles is a 72-year-old male patient admitted via the emergency department to the medical surgical floor at 2220 with a diagnosis of community acquired pneumonia (CAP). He arrives in the room via stretcher with oxygen (O2) via nasal cannula (NC) and is able to transfer to the bed with minimal assistance. He does get short of breath (SOB) with exertion.
What assessment findings does the nurse expect for this patient? Should there be a particular focus to the assessment?
- The great majority of patients with CAP present with fever. Other systemic symptoms such as chills, fatigue, malaise, chest pain (which may be pleuritic, nurse should ask questions about onset/radiation/provoking factors), and anorexia are also common. Tachycardia, leukocytosis with a leftward shift, or leukopenia are also findings that are mediated by the systemic inflammatory response. Focus should be respiratory in nature (auscultation, adventitious lung sounds like crackles & rhonchi) along with checking labs, CXR. Level of consciousness (LOC) on admission is important to monitor for changes.
Are there any ER results the nurse should ask about during the bedside report?
- Since the patient has a cough and fever, the nurse should check to see if a COVID test was done. It would also be beneficial to ask about chest x-rays (CXR), if blood and/or sputum cultures were taken, AND if antibiotics were already started. Most healthcare systems treat pneumonia as a core measure and must meet very strict metric guidelines (following a protocol, doing certain things within a narrow time frame window, etc)
What orders does the nurse expect the admitting provider to give?
- After admission, it is common for providers to give continuous pulse oximetry, O2 titration orders (i.e. titrate O2 to keep O2 saturation above 92%), and IV fluids. If cultures are not done already, those should be ordered. There may be a daily CXR to monitor changes. The nurse should check the med administration record for antibiotics and there may be medications for the cough/sputum (tesslon perles, guaifenesin, etc.) and fever control (acetaminophen 1000 mg q 6 hrs PRN fever greater than 101 F for example)
After screening and assessing the patient, the nurse has the following data:
Patient AA&Ox4. SOB noted with speaking and after he moves around. IV 20g noted in left arm. Productive cough with moderate sputum production occasionally. Lung sounds in all fields indicate crackles; no barrel chest noted. Skin is warm and dry. He voids per urinal no assistance needed. Verbalizes understanding of call light use.
BP 120/60 SpO2 93% on NC 2L HR 100 bpm and regular Ht 172 cm RR 18 bpm Wt 60 kg Temp 38.3°C
CXR – posteroanterior and lateral chest radiographs obtained (two view). Radiographic findings consistent with the diagnosis of CAP including minor lobar consolidations, moderate interstitial infiltrates
CBC (abnormal/significant only listed, if NOT listed then the value falls within expected limits or is not significant for this patient), for reference see nursing.com Lab Value cheat sheet: WBC 15,000 cells/mcL Bands 10% Neutrophils 60% Eosinophils 1% Basophils 1% Lymphocytes 20%
Prioritize the top nursing interventions.
- Frequent respiratory reassessments are vital for this patient along with continued LOC monitoring. The patient may need assistance with managing secretions so suction should be readily available. Positioning in the bed may alleviate symptoms and provide comfort – patient should not lie flat if there are airway concerns. The nurse should also ensure core measures are being followed. Blood cultures are needed as well as sputum so CORRECT collection and time of collection are necessary for proper monitoring. Timely administration of antibiotics helps improve outcomes.
What should the nurse be on the lookout for as the shift progresses? What warrants a call to the provider?
- Watch for airway compromise or O2 sat decline. Ensure LOC does not decline inappropriately as this may indicate worsening of condition (respiratory failure). If the provider has given parameters to call, the nurse must either hesitate nor apologize for reporting these to the provider. If there is a sepsis algorithm, this should be followed since the patient is at risk for this condition. Fever uncontrolled with antipyretics needs to be reported. Worsening chest pain or sense of impending doom may indicate a pulmonary embolism or other complication and should be reported.
Are there other orders the nurse might anticipate and/or suggest?
- A baseline lactic acid level (blood test) helps screen for sepsis. Strict I&O collection should begin since patients may have decreased appetite and/or thirst. Decreased urine output could be a sign of inadequate perfusion, so monitoring output is important. Respiratory therapy should be consulted for O2 titration, breathing treatments, O2 equipment/humidification and incentive spirometry (IS). Placing another IV may be helpful in case of patient deterioration (one in each upper extremity). Consider asking for Urinary antigen testing for S. pneumoniae
Are there past medical history concerns specific to this patient and his background that may aid in the plan of care?
- Checking pneumococcal vaccine history is important – the patient may need education if he did not receive this vaccine. If he is homeless there is a greater risk he has tuberculosis or possibly non-compliant at discharge (due to lack of resources) so should be screened. His travel history may be relevant as treatment progresses and for Infectious diseases to consider. If he has a tobacco use history, this must be documented (i.e. 20 pack history) because that puts him at higher risk of chronic lung disease. If he is unable to care adequately for himself then case management may need to be involved for short-term acute care post-hospitalization.
ABG values:
pH 7.30 PaCO2 50 mmHg HCO3- 23 mEq/L PaO2 88 mmHg
What does this ABG indicate? How do you know? What may have caused this value? What can you do?
- This is respiratory acidosis (pH < 7.35; PaCO2 > 45). It can be from hypoventilation -CNS depression -Pulmonary edema -Respiratory arrest -Airway obstruction. He may have an airway obstruction (thick sputum in throat) or his respiratory status could be worsening overall. Obtain VS, increase RR by arousing/waking him, reposition patient, maintain patent airway
The nurse gets the CNA to assist and repositions Charles in his hospital bed and he now sits straight but comfortably up in bed with pillows to bolster him. A yankauer at the bedside that he can use for a productive cough allows him to clear his airway after a brief teaching session. He had been frequently removing his NC due to ear discomfort, so RT brought padding for the tubing and Charles reports improved comfort. RT and the nurse teach him about “turn, cough, deep breath” aka TCDB.
After sleeping on and off through the shift, Charles is able to consume approximately 75% of his breakfast. He can properly demonstrate use of his IS and TCDB techniques. His NC remains in place with the padding on ears and his O2 sat is 95% on 2 L. He has two functioning IVs, one in each arm. Physician rounds and advises to continue plan of care including medication regimen based on test results after he and nurse discuss patient during rounds with the clinical pharmacist.
Describe examples of interdisciplinary team collaboration that may be useful in this patient’s care.
- The nurse should maintain open communication and good rapport with respiratory therapy and work as a team for the best outcomes. Pharmacy may be consulted for an appropriate antibiotic regimen and/or if core measures are being used. Nursing assistants can assist with repositioning and I&O adherence. A team of physicians may be on this patient’s case (i.e. Pulmonology, Infectious Diseases, etc), so being able to give appropriate updates to a variety of professionals is vital (i.e. SBAR).
View the FULL Outline
When you start a FREE trial you gain access to the full outline as well as:
- SIMCLEX (NCLEX Simulator)
- 6,500+ Practice NCLEX Questions
- 2,000+ HD Videos
- 300+ Nursing Cheatsheets
“Would suggest to all nursing students . . . Guaranteed to ease the stress!”
References:
View the full transcript, nursing case studies.

This nursing case study course is designed to help nursing students build critical thinking. Each case study was written by experienced nurses with first hand knowledge of the “real-world” disease process. To help you increase your nursing clinical judgement (critical thinking), each unfolding nursing case study includes answers laid out by Blooms Taxonomy to help you see that you are progressing to clinical analysis.We encourage you to read the case study and really through the “critical thinking checks” as this is where the real learning occurs. If you get tripped up by a specific question, no worries, just dig into an associated lesson on the topic and reinforce your understanding. In the end, that is what nursing case studies are all about – growing in your clinical judgement.
Nursing Case Studies Introduction
Cardiac nursing case studies.
- 6 Questions
- 7 Questions
- 5 Questions
- 4 Questions
GI/GU Nursing Case Studies
- 2 Questions
- 8 Questions
Obstetrics Nursing Case Studies
Respiratory nursing case studies.
- 10 Questions
Pediatrics Nursing Case Studies
- 3 Questions
- 12 Questions
Neuro Nursing Case Studies
Mental health nursing case studies.
- 9 Questions
Metabolic/Endocrine Nursing Case Studies
Other nursing case studies.
Community-acquired pneumonia (non Covid-19)
- Overview
- Theory
- Diagnosis
- Management
- Follow up
- Resources
Case history
A 54-year-old smoker with multiple comorbidities (diabetes, hypertension, coronary artery disease) presents with a 2-day history of a productive cough with yellow sputum, chest tightness, and fever. Physical exam reveals a temperature of 101°F (38.3°C), BP of 150/95 mmHg, heart rate of 85 bpm, and a respiratory rate of 20 breaths per minute. His oxygen saturation is 95% at rest; lung sounds are distant but clear, with crackles at the left base. Chest x-ray reveals a left lower lobe infiltrate.
Other presentations
Pneumonia can occur at any age, but the incidence increases significantly in old age, and pneumonia is a leading cause of illness and death in older patients. The clinical manifestations of pneumonia in elderly persons are often less intense than those in younger patients. [1] Simonetti AF, Viasus D, Garcia-Vidal C, et al. Management of community-acquired pneumonia in older adults. Ther Adv Infect Dis. 2014;2:3-16. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4072047 http://www.ncbi.nlm.nih.gov/pubmed/25165554?tool=bestpractice.com Atypical pathogens such as Mycoplasma pneumoniae , Chlamydophila pneumophila , and respiratory viruses can present in a subacute fashion with gradual onset of fever, nonproductive cough, constitutional symptoms, relatively normal white blood cell count, and absent or diffuse findings on lung exam. [2] Masiá M, Gutiérrez F, Padilla S, et al. Clinical characterisation of pneumonia caused by atypical pathogens combining classic and novel predictors. Clin Microbiol Infect. 2007;13:53-61. http://www.clinicalmicrobiologyandinfection.com/article/S1198-743X%2814%2961580-9/fulltext http://www.ncbi.nlm.nih.gov/pubmed/17328727?tool=bestpractice.com Patients with severe pneumococcal or Legionella pneumophila pneumonia often progress rapidly to respiratory failure.
Use of this content is subject to our disclaimer
Log in or subscribe to access all of BMJ Best Practice
Log in to access all of bmj best practice, help us improve bmj best practice.
Please complete all fields.
I have some feedback on:
We will respond to all feedback.
For any urgent enquiries please contact our customer services team who are ready to help with any problems.
Phone: +44 (0) 207 111 1105
Email: [email protected]
Your feedback has been submitted successfully.
- Study Protocol
- Open access
- Published: 20 August 2024
Multicentre case–control study of pneumococcal infections among children with pneumonia in Peninsular Malaysia (MY-Pneumo): a study protocol
- Nurul Hanis Ramzi 1 na1 ,
- Andrew Tan Chun Hoong 1 na1 ,
- Nur Alia Johari 1 ,
- Anna Marie Nathan 2 ,
- Cindy Shuan Ju Teh 3 ,
- Norhayati Aida Sulaiman 2 ,
- Mohamad Ikram Ilias 4 ,
- Zakuan Zainy Deris 5 ,
- Siti Nur Haidar Hazlan 5 ,
- Nur Syafiqah Mohamad Nasir 5 ,
- Asrar Abu Bakar 6 ,
- Muhd Alwi Muhd Helmi 6 ,
- Wan Khairunnisa Wan Juhari 6 ,
- Norhidayah Kamarudin 7 ,
- Chun Wie Chong 1 , 8 ,
- David W. Cleary 9 , 10 ,
- Stuart C. Clarke 1 , 10 , 11 &
- Lokman Hakim Sulaiman 1 , 12
BMC Public Health volume 24 , Article number: 2255 ( 2024 ) Cite this article
Metrics details
S. pneumoniae (SPN) is the most common cause of pneumonia. The disease can be effectively prevented through immunisation. Since December 2020, the Malaysian Government has included the 10-valent pneumococcal conjugate vaccine (PCV10) for all infants born on or after 1 January 2020 as part of the National Immunisation Programme (NIP). However, the epidemiology of pneumonia remains poorly understood. To fill the knowledge gap, we established a multicentre surveillance study to understand the burden of pneumococcal pneumonia among young children in Peninsular Malaysia.
MY-Pneumo is a multicentre prospective case–control study conducted in three sentinel sites located in three different states of Peninsular Malaysia – Kuala Lumpur, Pahang, and Kelantan. A cohort of at least 500 incident cases and 500 controls is enrolled beginning in October 2021 and matched for age. Cases are hospitalised children < 5 years with radiologically confirmed pneumonia, and the controls are children without any features suggestive of pneumonia. Clinical samples, including nasopharyngeal swabs (NPS) and urine, are collected according to the study protocol. Biological fluids such as blood, cerebrospinal fluid (CSF) and pleural fluid are obtained from invasive pneumonia disease (IPD) patients, if available. All children are tested for SPN using polymerase chain reaction (PCR) and pneumococcal urine antigen test (PUAT) using BinaxNow.
Surveillance data, including carriage rate, serotype variations and the phylogeny data structure of SPN among young children in Malaysia during PCV implementation, will be generated from this study. Trends and patterns of pneumococcal serotypes by different regions are important for targeted public health strategies. Our data will provide baseline information for estimating the impact of PCV10 implementation and will influence policymakers' decisions regarding the upgrade from PCV10 to a higher-valency conjugate vaccine in Malaysia.
Trial registration
This project was registered at ClinicalTrials.gov (NCT04923035) on 2021, June 11. The study protocol was approved by the International Medical University Joint-Committee on Research & Ethics (4.15/JCM-216/2021) and the Institutional Review Board at sentinel sites (USM/JEPeM/21020190, IREC 2021–114, MREC ID No: 2021128–9769) and University of Southampton's Ethics and Research Governance (ERGo II 64844).
Peer Review reports
According to the World Health Organization (WHO), pneumonia accounts for a substantial portion of deaths in children under five [ 1 ]. The burden of pneumonia is high in developing countries with limited access to healthcare resources, overcrowding and vaccines. Preventive measures, such as routine vaccinations, exclusive breastfeeding, good nutrition, and reducing exposure to indoor air pollution, can reduce the risk of pneumonia in children [ 2 , 3 , 4 ]. Additionally, timely diagnosis and appropriate treatment, including the use of antibiotics when necessary, are crucial in managing pneumonia and preventing severe outcomes [ 5 , 6 ].
The most common cause of pneumonia among children under five is infection with Streptococcus pneumoniae (SPN), also known as pneumococcus. Immunisation with a pneumococcal vaccine is an effective way to prevent pneumonia. In Malaysia, pneumococcal vaccination under the NIP for children has commenced for infants born from January 2020, comprising three doses at 4, 6 and 15 months. The routine use of the 10-valent pneumococcal conjugate vaccine (PCV10) in children is expected to reduce the burden of pneumococcal infections in the country, especially severe infections. The impact of the coronavirus disease 2019 (COVID-19) pandemic may also have implications on the pneumococcal serotype and clinical presentation of infections in the community. There was a 30% to 80% decline in IPD incidence rate observed for all pneumococcal serotype groups in England and the Netherlands populations, respectively [ 7 , 8 ]. In Malaysia, children with severe pneumonia due to COVID-19 exhibited a less severe clinical trajectory when compared with cases caused by other respiratory viruses [ 9 ]. The children manifested early in the disease progression, exhibiting no atypical biomarkers, such as lymphopenia and elevated C-reactive protein (CRP) levels. There were no invasive pneumococcal coinfections despite the low pneumococcal vaccination rates among the study population [ 9 ]. Therefore, we conducted a prospective case–control study to understand the burden of pneumococcal pneumonia in young children and to provide a baseline assessment to monitor changes in SPN carriage post-PCV implementation in Malaysia.
Methods/design
Study objectives.
The study’s primary objectives are to provide baseline surveillance of pneumococcal pneumonia in young children in Malaysia by determining the prevalence of SPN nasopharyngeal carriage among children aged 5 years and below with pneumonia and IPD. Secondary study objectives are: 1) to determine SPN serotypes by polymerase chain reaction (PCR) and whole-genome sequencing (WGS), 2) to evaluate the correlation of SPN detection between nasopharyngeal carriage and urine samples, and 3) to establish sensitivity and specificity cutoffs of BinaxNOW for the detection of SPN serotypes in children with pneumonia and IPD.
Study size power calculation
This is a prospective case–control study in which all children aged 5 years and below with clinically diagnosed pneumonia and healthy controls will be recruited at three study sites. As per assumptions of 95% confidence interval (CI), 80% power and detectable odds ratio (OR) of 1.5, we estimate 164 cases and 164 healthy controls per sentinel hospital site. Thus, we aim to recruit a total of 500 confirmed pneumonia/IPD cases and 500 healthy controls for this study.
Study sites and design
This prospective, hospital-based, multicentre case–control study is being conducted at three university hospitals in different states within Peninsular Malaysia – Kuala Lumpur, Pahang, and Kelantan (Fig. 1 ). Kuala Lumpur serves as the capital city of Malaysia and is centrally located in the western part of Peninsular Malaysia. Pahang and Kelantan are located on the east coast of Peninsular Malaysia, along the South China Sea, providing them with access to the coastline. Kelantan is situated to the north of Kuantan and shares its eastern border with Thailand. Study enrolment is at 1) University Malaya Medical Centre (UMMC), Kuala Lumpur; 2) Hospital Universiti Sains Malaysia (HUSM), Kota Bharu, Kelantan; and 3) Sultan Ahmad Shah Medical Centre International Islamic University Malaysia (SASMEC IIUM), Kuantan, Pahang. Table 1 summarises the demographics and burden of pneumonia in each state of the participating sentinel site. Cases and controls are age-matched within the range of 6 months. Cases are age-matched children clinically diagnosed with pneumonia and attending the outpatient department or admitted as a hospital inpatient, Invasive Pneumococcal Disease (IPD) (without pneumonia), bacteraemic pneumococcal pneumonia, and chest radiograph (CXR) confirmed pneumonia (by WHO guideline) [ 10 ]. Controls are healthy age-matched children without any intercurrent respiratory illness. Subject enrollment is over 24 months for each participating site, and a total sample of 400 subjects (200 cases and 200 controls) is targeted for UMMC and HUSM, respectively, and 200 subjects (100 cases and 100 controls) for IIUM. Male and female patients from the three major ethnic groups (Malay, Chinese, and Indian) are being recruited from each sentinel site. The study protocol workflow is as outlined in Fig. 2 .
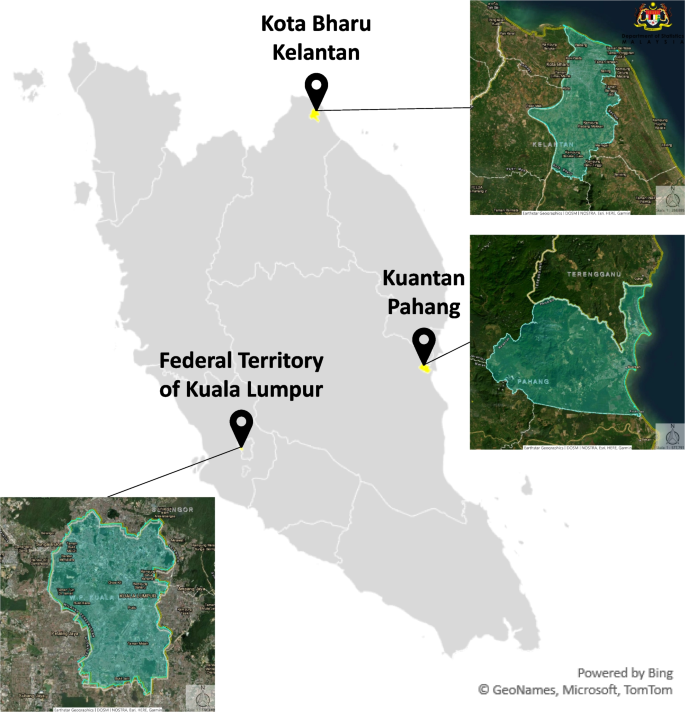
Geographical locations of participating university hospitals in Peninsular Malaysia: Kuala Lumpur, Pahang, and Kelantan. Source: Adapted from Department of Statistics, Malaysia. (2023, August 16). https://statsgeo.mycensus.gov.my/geostats/report.php

Summary of the study protocol workflow. The specimen collection, processing, and storage of nasopharyngeal swabs (NPS) were adapted from CDC Pneumococcal Carriage Protocols. Clinical samples were taken according to local policy, including NPS and urine samples. Different methods were used to collect the urine depending on the age and tolerability of the participant i.e. clean catch/void, urine collection bag, and diaper. Additional blood, cerebrospinal fluid (CSF) and pleural fluid were taken for invasive pneumococcal disease (IPD) patients, if available. NPS was inoculated into a medium containing skim milk, tryptone, glucose, and glycerin (STGG) and stored at -80 °C before shipment to IMU-Advanced Microbiology Collaborative Research Laboratory (AMCRL). General questionnaires/case report form (CRF) were administered to the parents/caregivers of the patients to obtain socio-demographic, vaccination history and medical history of the child. The gene targets for pneumococcal identification, including the main pneumococcal capsular biosynthesis gene A (cpsA), were analysed through PCR. SPN isolates will be transferred to the University of Southampton (UoS), United Kingdom (UK), for whole-genome sequencing (WGS) analysis
Study participants
The study population is comprised of children under 5 years of age who comply with protocol definitions and inclusion criteria. Eligible participants are identified by study paediatricians and research assistants at each participating site. The following criteria define cases: 1) hospitalised patients aged between 2 weeks and 59 months, 2) clinical features of pneumonia, as described below, 3) radiological confirmation of pneumonia based on CXR findings as per WHO guidelines [ 10 ], and 4) an informed consent statement signed by the children’s parents or legal guardian. The exclusion criteria for cases are the following: children who 1) do not meet the case definition, and 2) whose parents or legal guardian declined to sign the informed consent statement. Controls are defined by children aged 5 years and below, who are in good health, as determined by a brief medical history and/or clinical judgement of the investigator, and whose parent or legal guardian is willing and able to give informed consent. Exclusion criteria for the controls are: 1) any symptom suggestive of respiratory illness, 2) has nasal surgery, 3) has significant diseases or symptoms, such as febrile illness or a temperature ≥ 38 °C on the day of the visit or in the preceding 72 h that can place the patient at an increased risk of the disease, 4) has a history of antibiotic administration in the month prior to sampling, or 5) minors whose parents or legal guardian decline to sign the informed consent statement. Cases and controls are matched for study site and age (± 6 months). General questionnaires are administered to the parents or legal guardians of the participants to obtain demographic and socio-economic data and their medical history. Subjects are identified based on an anonymised identifier. The master list is kept in a password-protected spreadsheet.
Definition of pneumonia
Pneumonia cases are defined as patients with a history of cough and/or difficulty/rapid breathing and/or intercostal recession, with or without fever, and radiological confirmation of pneumonia as per WHO guidelines [ 10 ].
Biological samples
Samples are collected in the first 24 h of patient hospitalisation (Table 2 ). Nasopharyngeal swabs (NPS) and urine samples are collected from all pneumonia cases and controls following Centers for Disease Control and Prevention (CDC) Pneumococcal Carriage Protocols [ 11 ]. Each sample is aliquoted as per protocols outlined in this study. Each NPS is inoculated into a medium containing skim milk, tryptone, glucose, and glycerol (STGG) and stored at -80 °C before shipment to the International Medical University Advanced Microbiology Collaborative Research Laboratory (IMU-AMCRL) in Kuala Lumpur, Malaysia, every 4 months by a licensed/registered courier. One NPS and one 15 mL urine sample are collected from each subject at the time of enrolment. The collection procedure is performed by trained clinical staff, nurses, and the research assistant at the sentinel site. The NPS collection procedure involves inserting a nylon-tipped FLOQswab (COPAN Diagnostics Inc., USA) through the nostril into the cavity between the nose and mouth for 5 s and rotating it several times. The swab is then inserted into a cryovial with 1 mL of STGG media (2% (w/v) skim milk powder, 3% (w/v) tryptone soy broth powder, 0.5% (w/v) glucose and 10% (v/v) glycerol in water), and immediately vortexed briefly and frozen at -80 °C within 4 h. Different methods of urine collection are used depending on the age and tolerability of the participant, such as clean catch or void, urine collection bag, and diaper. Briefly, for children using diapers, we used the “urine ball method”, which involves placing sterile cotton balls on the subject’s diaper. The urine is subsequently collected by placing the urine-soaked cotton balls into a sterile 20 mL syringe, and the fluid is extracted with a plunger. The collected urine is mixed with PIPES buffer and aliquoted into three tubes of 5 ml each. All urine sampling supplies, including tubes, urine bags, buffer and BinaxNOW test kits, are provided to sentinel sites by Merck Sharp & Dohme (MSD) via Pharmaceutical Product Development (PPD). Urine samples are tested with BinaxNOW at sentinel sites, and the remaining aliquots are shipped to the MSD Central Lab on dry ice. The BinaxNOW® test kit includes a test device (strip or card), a specimen swab, and a buffer solution. The test device is placed on a clean, flat surface before a buffer solution is added from a dropper bottle. A specimen swab is dipped into the urine specimen, removed, and then inserted into the test card. The card is then closed, bringing the specimen into contact with the test strip. Pneumococcal antigen present in the specimen reacts to bind anti-S. pneumoniae-conjugated antibody. The resulting antigen-conjugate complexes are captured by immobilised anti-S. pneumoniae antibody, forming the Sample Line. Immobilised control antibody captures anti-species conjugate, forming the Control Line. Test results are interpreted by the presence or absence of visually detectable pink-to-purple coloured lines. A positive test result, read in 15 min, will include the detection of both a Sample and a Control Line. A negative test result, read in 15 min, will produce only a Control Line, indicating that S. pneumoniae antigen was not detected in the specimen. Failure of the Control Line to appear, whether the Sample Line is present or not, indicates an invalid assay. Additional blood, cerebrospinal fluid (CSF) and pleural fluid will be taken for IPD patients, if available, at each sentinel hospital site.
Laboratory analysis
Laboratory isolation (including genomic deoxyribonucleic acid (DNA) extraction), identification and confirmation of SPN in each sample are carried out at the IMU-AMCRL. Aliquots of NPS in STGG media include volumes of 400 µl, 350 µl and 250 µl, are stored in -80 °C freezers. The 250 µl NPS-STGG aliquot is the working sample used for blood agar culture, optochin-sensitivity, and DNA extraction for each participant. A 10 µl loopful of sample is taken from the 250 µl aliquot, plated onto Columbia agar with 5% sheep blood (CBA) (Oxoid), and incubated in 5% CO 2 at 37 °C for 24 h. The plate culture is observed after 24 h of incubation, and colonies exhibiting SPN morphology are picked for replating onto fresh CBA plates with 5 mcg optochin disc (HIMEDIA), followed by incubation as in the previous step. SPN isolates are identified as small, greyish, alpha-hemolytic culture growths showing Draughtsman morphology, and are optochin sensitive. Genomic DNA from the remaining 240 µl NPS-STGG aliquot is extracted using the New England Biolabs (NEB) Monarch® Genomic DNA Purification Kit (USA). The extracted genomic DNA is then subjected to multiplex conventional PCR analysis according to the CDC protocol (US scheme protocol) to detect SPN serotypes by amplifying the capsular polysaccharide biosynthesis gene A (cpsA) targets. SPN isolates will be transferred to the University of Southampton (UoS), United Kingdom (UK), for WGS analysis. Isolates will be sequenced using a MiSeq (Illumina, UK) to generate 2 × 300 paired-end data. Assembly will be done using SPAdes with assembly improvement and QC as described previously [ 12 ].
Data sources and quality control
Clinical site monitoring for research conduct and management is conducted yearly by the Principal Investigator team from the International Medical University (IMU). The main purpose of clinical site monitoring is primarily to ensure protocol adherence, source data verification, investigator training, site performance, data quality assurance, and maintaining data integrity at each participating site. Tasks and responsibilities are based on standard research guidelines, including standard operating procedures. Data sources are monitored and evaluated for case and control definition conformity, errors, and missing data at each sentinel site. Vaccination records, underlying diseases, medical history, radiological findings, and demographic characteristics are recorded prospectively for each patient on a case report form (CRF) (Table 3 ). Data quality reporting is redacted for each site to ensure the confidentiality and conformity of all study data variables. This process will be applied to data analysis of each enrolled case and control subject. Data accuracy will be assessed by comparing the recorded values with source documents. The principal investigator at each site is contacted for queries regarding this quality assessment and is involved in resolution.
Data analysis
An anonymous database will be built, and clinical data will be linked to laboratory data. Quantitative variables will be described and categorised according to their distribution in the study population. Descriptive analysis will address each covariate for the entire population and will be stratified by site. Patients’ characteristics and laboratory data for cases and controls will be compared. The associations between risk factors and carriage will also be examined by estimating the relative risk in the study population. Data analysis will be conducted using software such as R and SPSS. The absence/presence of SPN will be modelled using a mixed effects logistic regression model and random forest. The validity of the model will be tested using cross-validation. Sensitivity analysis will also be carried out to evaluate the impact of selected clinical and demographic parameters on the BinaxNOW test outcome.
MY-Pneumo study collects data on potential risk factors that may influence trends in respiratory disease, as well as pneumococcal carriage among healthy controls. This study incorporates different study designs which will help us to interpret the changes over time in younger children with pneumonia following PCV10 introduction. The results obtained from this study will be reported in due course, with the hope that the information gained will contribute to a better understanding of pneumococcal disease in the Malaysian context. Regional site analysis, focusing on specific interests, will also be described and published at a later date. Study analysis will generally focus on the prevalence of pneumonia for the entire population and by the sentinel site. Insufficient data regarding pneumonia aetiology in developing countries is evident from the geographical distribution of study sites worldwide [ 13 , 14 , 15 ]. It has been suggested that further carriage and disease studies are required in middle-income countries, especially in Malaysia, to assess the effectiveness of pneumococcal vaccination to monitor serotype changes in the population [ 16 , 17 , 18 ]. The Pneumonia Etiology Research for Child Health (PERCH) study was the largest, most comprehensive pneumonia aetiology study conducted in seven countries in Africa and Asia: Gambia, Mali, Kenya, Zambia, South Africa, Bangladesh, and Thailand from 2011 to 2014 [ 19 ]. The study setting involved severe childhood pneumonia cases (4,232 children between 1 month and 5 years), and each country had different characteristics that may have influenced the causes of pneumonia. Yet, the research study was pivotal in advancing our understanding of the causes and contributors to childhood pneumonia in developing countries. By investigating a diverse range of variables and risk factors, the PERCH study contributed to driving transformative changes in child health outcomes, reducing the burden of pneumonia-related morbidity and mortality. A more comprehensive understanding of the pathogens responsible for childhood pneumonia holds the potential to significantly enhance both preventive measures, including the implementation of effective vaccine policies, and therapeutic interventions. This collective effort towards a better understanding of pneumonia causality has the power to drive improved management strategies, ultimately resulting in a remarkable reduction in the burden of morbidity and mortality associated with childhood pneumonia.
The present study’s main strength is the prospective multicentre case–control study design that will permit the description of paediatric pneumococcal pneumonia in study-related locations, especially in urban and rural areas. The sampling and laboratory methods used are consistent with other research studies that have described nasopharyngeal carriage in young children [ 19 , 20 ]. Gold-standard molecular methods have been utilised to detect pneumococcus in the nasopharynx [ 21 ]. The use of the PUAT assay, which detects pneumococcal polysaccharides in the urine of young children, will enable rapid detection of pneumococcal antigens, allowing for timely intervention and reducing the risk of complications.
Whilst our study includes three states in both urban and rural community areas of Peninsular Malaysia, we did not include other states in East Malaysia. Therefore, our findings may not be applicable to represent the diversified population and demographics of Malaysia. The COVID-19 pandemic and co-infection status for pneumonia cases may impact study outcomes as we do not have administrative data available for both. However, we plan to incorporate this information whenever available into the descriptive interpretation of study results. Moreover, we do not have pneumococcal carriage data for the retrospective period and have therefore chosen clinical endpoints as our primary study objective.
This study will contribute to the incomplete evidence available on the burden of pneumococcal pneumonia in children below the age of 5 years in low-resourced countries, particularly in the Asia–Pacific region. Data on the burden of pneumococcal pneumonia and the impact of PCV can guide decisions related to vaccine prioritisation, resource allocation, and healthcare strategies. As PCV is being introduced in various low-resource settings to combat pneumococcal diseases, understanding its effectiveness and potential benefits is critical for public health strategies. The study is one of the few active population-based pneumonia surveillance programs evaluating the indirect impact of PCV in a resource-limited setting. With the increasing introduction of PCV in low-resourced settings, the methods, experiences, and lessons learned from our study may guide the development of such systems in other countries.
Availability of data and materials
Not applicable – manuscript does not contain any data.
Data availability
No datasets were generated or analysed during the current study.
Abbreviations
Columbia agar with 5% sheep blood
Centers for Disease Control and Prevention
Confidence interval
Coronavirus disease 2019
The capsular polysaccharide biosynthesis gene A
Case report form
C-reactive protein
Cerebrospinal fluid
Chest radiograph
Deoxyribonucleic acid
Hospital Universiti Sains Malaysia
International Medical University Advanced Microbiology Collaborative Research Laboratory
Invasive pneumococcal disease
National Immunisation Programme
Nasopharyngeal swab
Polymerase chain reaction
- Pneumococcal conjugate vaccine
10-Valent pneumococcal conjugate vaccine
Pneumonia Etiology Research for Child Health
Pneumococcal urine antigen test
Sultan Ahmad Shah Medical Centre International Islamic University Malaysia
- Streptococcus pneumoniae
Skim milk, tryptone, glucose, and glycerol
University Malaya Medical Centre
Whole-genome sequencing
World Health Organization
WHO. Pneumonia in children. 2022. Available from: https://www.who.int/en/news-room/fact-sheets/detail/pneumonia Cited 2023 Aug 17.
Google Scholar
UNICEF DATA. neumonia in Children Statistics. 2022. Available from: https://data.unicef.org/topic/child-health/pneumonia/ Cited 2023 Aug 17.
Sutriana VN, Sitaresmi MN, Wahab A. Risk factors for childhood pneumonia: a case-control study in a high prevalence area in Indonesia. Clin Exp Pediatr. 2021;64(11):588–95.
Article PubMed PubMed Central Google Scholar
Beletew B, Bimerew M, Mengesha A, Wudu M, Azmeraw M. Prevalence of pneumonia and its associated factors among under-five children in East Africa: A systematic review and meta-analysis. BMC Pediatr. 2020;20(1):254.
Bartlett JG, Dowell SF, Mandell LA, File TM, Musher DM, Fine MJ. Practice guidelines for the management of community-acquired pneumonia in adults. Clin Infect Dis. 2000;31(2):347–82.
Article PubMed CAS Google Scholar
Chee E, Huang K, Haggie S, Britton PN. Systematic review of clinical practice guidelines on the management of community acquired pneumonia in children. Paediatr Respir Rev. 2022;42:59–68.
PubMed Google Scholar
Amin-Chowdhury Z, Aiano F, Mensah A, Sheppard CL, Litt D, Fry NK, et al. Impact of the Coronavirus Disease 2019 (COVID-19) Pandemic on Invasive Pneumococcal Disease and Risk of Pneumococcal Coinfection with Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2): Prospective National Cohort Study. England Clin Infect Dis. 2021;72(5):e65–75.
RIVM. The National Immunisation Programme in the Netherlands Surveillance and developments in 2019–2020. Netherlands; 2020.
Ng DCE, Tan KK, Ting GSS, Ling C, Fadzilah NFB, Tan SF, et al. Comparison of severe viral pneumonia caused by SARS-CoV-2 and other respiratory viruses among Malaysian children during the COVID-19 pandemic. Front Pediatr. 2022;10:865099.
Cherian T, Mulholland EK, Carlin JB, Ostensen H, Amin R, De Campo M, et al. Standardized interpretation of paediatric chest radiographs for the diagnosis of pneumonia in epidemiological studies. Bull World Health Organ. 2005;83(5):353–9.
PubMed PubMed Central Google Scholar
CDC Streptococcus Laboratory. NCIRD/DBD/RDB-Centers for Disease Control and Prevention. 2010. Streptococcus pneumoniae carriage study protocol ‐ nasopharyngeal (NP) swab processing. Available from: https://www.cdc.gov/streplab/pneumococcus/resources.html#carriage-protocols Cited 2023 Aug 17.
Bankevich A, Nurk S, Antipov D, Gurevich AA, Dvorkin M, Kulikov AS, et al. SPAdes: A new genome assembly algorithm and its applications to single-cell sequencing. J Comput Biol. 2012;19(5):455–77.
Article PubMed PubMed Central CAS Google Scholar
Ali H, Aziz S. Rising Pediatric Morbidity and Mortality in the Developing World. Cureus; 2021.
Book Google Scholar
Nathan AM, Teh CSJ, Jabar KA, Teoh BT, Tangaperumal A, Westerhout C, et al. Bacterial pneumonia and its associated factors in children from a developing country: A prospective cohort study. PLoS ONE. 2020;15(2):e0228056.
Rudan I, Boschi-Pinto C, Biloglav Z, Mulholland K, Campbell H. Epidemiology and etiology of childhood pneumonia. Bull World Health Organ. 2008;86(5):408–16.
Tricarico S, McNeil HC, Head MG, Cleary DW, Clarke SC. Informing pneumococcal conjugate vaccine policy in middle-income countries: The case of Malaysia. Vaccine. 2017;35(18):2288–90.
Article PubMed Google Scholar
Tricarico S, McNeil HC, Cleary DW, Head MG, Lim V, Yap IKS, et al. Pneumococcal conjugate vaccine implementation in middle-income countries. Pneumonia. 2017;9(1):6.
Lister AJJ, Dombay E, Cleary DW, Sulaiman LH, Clarke SC. A brief history of and future prospects for pneumococcal vaccination in Malaysia. Pneumonia. 2023;15(1):12.
O’Brien KL, Baggett HC, Brooks WA, Feikin DR, Hammitt LL, Higdon MM, et al. Causes of severe pneumonia requiring hospital admission in children without HIV infection from Africa and Asia: the PERCH multi-country case-control study. Lancet. 2019;394(10200):757–79.
Article Google Scholar
Picot VS, Bénet T, Messaoudi M, Telles JN, Chou M, Eap T, et al. Multicenter case-control study protocol of pneumonia etiology in children: Global Approach to Biological Research, Infectious diseases and Epidemics in Low-income countries (GABRIEL network). BMC Infect Dis. 2014;14(1):635.
Satzke C, Dunne EM, Porter BD, Klugman KP, Mulholland EK, Vidal JE, et al. The PneuCarriage Project: A Multi-Centre Comparative Study to Identify the Best Serotyping Methods for Examining Pneumococcal Carriage in Vaccine Evaluation Studies. PLoS Med. 2015;12(11):e1001903.
Download references
Acknowledgements
The authors thank all staff nurses and medical officers from the sentinel sites for their valuable contributions to this study. The authors also would like to thank all the parents/legal guardians and children who participated in the study.
This work is funded in part by a research grant from the Investigator Initiated Studies Program of Merck Sharp & Dohme Corp (MSIP #60200). The funding body did not play any role in data collection, decision to publish, or drafting of the manuscript. The opinions expressed in this paper are those of the authors and do not necessarily represent those of Merck Sharp & Dohme Corp.
Author information
Nurul Hanis Ramzi and Andrew Tan Chun Hoong contributed equally to this work.
Authors and Affiliations
Institute for Research, Development and Innovation, IMU University (formerly known as International Medical University), Kuala Lumpur, 57000, Malaysia
Nurul Hanis Ramzi, Andrew Tan Chun Hoong, Nur Alia Johari, Chun Wie Chong, Stuart C. Clarke & Lokman Hakim Sulaiman
Department of Paediatrics, Faculty of Medicine, University of Malaya, Kuala Lumpur, 50603, Malaysia
Anna Marie Nathan & Norhayati Aida Sulaiman
Department of Medical Microbiology, Faculty of Medicine, University of Malaya, Kuala Lumpur, 50603, Malaysia
Cindy Shuan Ju Teh
Department of Paediatrics, School of Medical Sciences, Universiti Sains Malaysia, Kota Bharu, Kelantan, 16150, Malaysia
Mohamad Ikram Ilias
Department of Medical Microbiology & Parasitology, School of Medical Sciences, Universiti Sains Malaysia Health Campus, Kota Bharu, 16150, Malaysia
Zakuan Zainy Deris, Siti Nur Haidar Hazlan & Nur Syafiqah Mohamad Nasir
Department of Paediatric, Kulliyyah of Medicine, International Islamic University Malaysia, Kuantan, Pahang, 25200, Malaysia
Asrar Abu Bakar, Muhd Alwi Muhd Helmi & Wan Khairunnisa Wan Juhari
Department of Pathology and Laboratory Medicine, Kulliyyah of Medicine, International Islamic University Malaysia, Kuantan, Pahang, 25200, Malaysia
Norhidayah Kamarudin
School of Pharmacy, Monash University Malaysia, Subang Jaya, Selangor, 47500, Malaysia
Chun Wie Chong
Institute of Microbiology and Infection, College of Medical and Dental Sciences, University of Birmingham, Birmingham, UK
David W. Cleary
Faculty of Medicine & Institute for Life Sciences, University of Southampton, Southampton, UK
David W. Cleary & Stuart C. Clarke
Southampton Biomedical Research Centre, National Institute for Health and Care Research (NIHR), University Hospital Southampton Foundation NHS Trust, Southampton, UK
Stuart C. Clarke
Department of Community Medicine, School of Medicine, IMU University (formerly known as International Medical University), Kuala Lumpur, 57000, Malaysia
Lokman Hakim Sulaiman
You can also search for this author in PubMed Google Scholar
Contributions
All authors designed and co-authored the protocol. NHR and ATCH were responsible for preparing the manuscript. LHS and SCC conceived the idea. LHS, SCC, CCW, NHR, and NAJ drafted the original proposal. CSJT, SNHH, ZZD, and NK supported microbiological aspects-based protocols. AMN, NAS, MII, ZZD, NSMN, AAB, MAMH, and WKWJ coordinated study implementation at sentinel sites. DWC supported the WGS analysis. All authors read, commented on, and approved the final manuscript version.
Corresponding author
Correspondence to Nurul Hanis Ramzi .
Ethics declarations
Ethics approval and consent to participate.
The study protocol, informed consent statement, case report form, any amendments and all other study documents have been submitted to and approved by the institutional ethics committee of each site:
The International Medical University Joint-Committee on Research & Ethics (4.15/JCM-216/2021),
The Human Research Ethics Committee, Universiti Sains Malaysia (USM/JEPeM/21020190),
The International Islamic University Malaysia Research Ethics Committee (IREC 2021–114), and
The Medical Research Ethics Committee, University Malaya Medical Centre (MREC ID No: 2021128–9769)
University of Southampton's Ethics and Research Governance (ERGo II 64844)
Consent for publication
Not required because no individual identifiers have been included in the manuscript.

Competing interests
DWC was a post-doctoral researcher on GSK funded projects in 2014/15 and has received grant support from Pfizer and the National Institute for Health via the NIHR Southampton Biomedical Research Centre. LHS and SCC act as principal investigators for clinical trials and other studies conducted on behalf of IMU University, and University Hospital Southampton NHS Foundation Trust/University of Southampton, respectively, that are sponsored by vaccine manufacturers. No personal payments are received from them. SCC has participated in advisory boards for vaccine manufacturers but receives no personal payments for this work. NHR and SCC have received financial assistance from vaccine manufacturers to attend conferences. All grants and honoraria are paid into accounts within the respective IMU University and NHS Trusts or Universities, or to independent charities. All other authors have no conflicts of interest.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/ .
Reprints and permissions
About this article
Cite this article.
Ramzi, N.H., Hoong, A.T.C., Johari, N.A. et al. Multicentre case–control study of pneumococcal infections among children with pneumonia in Peninsular Malaysia (MY-Pneumo): a study protocol. BMC Public Health 24 , 2255 (2024). https://doi.org/10.1186/s12889-024-19789-9
Download citation
Received : 04 March 2024
Accepted : 13 August 2024
Published : 20 August 2024
DOI : https://doi.org/10.1186/s12889-024-19789-9
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Pneumococcal Pneumonia
- Pneumonia Childhood
- Invasive Pneumonia Disease
- Surveillance
BMC Public Health
ISSN: 1471-2458
- General enquiries: [email protected]
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- My Bibliography
- Collections
- Citation manager
Save citation to file
Email citation, add to collections.
- Create a new collection
- Add to an existing collection
Add to My Bibliography
Your saved search, create a file for external citation management software, your rss feed.
- Search in PubMed
- Search in NLM Catalog
- Add to Search
Community-acquired pneumonia: a case study
Affiliation.
- 1 Long Island Jewish Medical Center, New Hyde Park, New York, USA. [email protected]
- PMID: 11858290
Community-acquired pneumonia (CAP) is an infectious disease commonly seen in the primary care environment. CAP is ranked as the sixth leading cause of death in the United States. It affects more than 10 million individuals per year and accounts for 500,000-1,000,000 hospital admissions. Precise diagnosis of CAP continues to be complex. Despite enormous advances in serologic analysis and antimicrobial development, at least 50% of causative pathogens are not identified. This article presents a case report of a white female in her seventies diagnosed with CAP and emphasizes the need for early detection, immunization, and prompt interventions to reduce morbidity and mortality rates. This case brings to light the dilemma practitioners can face when treating high-risk populations on an outpatient basis.
PubMed Disclaimer
Similar articles
- Severe community-acquired pneumonia. Restrepo MI, Anzueto A. Restrepo MI, et al. Infect Dis Clin North Am. 2009 Sep;23(3):503-20. doi: 10.1016/j.idc.2009.04.003. Infect Dis Clin North Am. 2009. PMID: 19665080 Review.
- Community-acquired pneumonia. The 'captain of death' can be controlled. Fitzgerald MA. Fitzgerald MA. Adv Nurse Pract. 2000 Jan;8(1):59-61. Adv Nurse Pract. 2000. PMID: 11011597 No abstract available.
- Treatment of community-acquired pneumonia in an ambulatory setting. Butt S, Swiatlo E. Butt S, et al. Am J Med. 2011 Apr;124(4):297-300. doi: 10.1016/j.amjmed.2010.06.027. Am J Med. 2011. PMID: 21435417 Review.
- Community-acquired pneumonia in adolescents. Gordon RC. Gordon RC. Adolesc Med. 2000 Oct;11(3):681-95. Adolesc Med. 2000. PMID: 11060562 Review.
- Community-acquired pneumonia. Spoto S, De Galasso L, Costantino S. Spoto S, et al. Clin Ter. 2002 May-Jun;153(3):225-7. Clin Ter. 2002. PMID: 12161986 No abstract available.
Publication types
- Search in MeSH
Related information
Linkout - more resources, miscellaneous.
- NCI CPTAC Assay Portal
- Citation Manager
NCBI Literature Resources
MeSH PMC Bookshelf Disclaimer
The PubMed wordmark and PubMed logo are registered trademarks of the U.S. Department of Health and Human Services (HHS). Unauthorized use of these marks is strictly prohibited.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Acad Pathol
- v.6; Jan-Dec 2019
Educational Case: Aspiration Pneumonia
Candice c. black.
1 Department of Pathology and Laboratory Medicine, Dartmouth-Hitchcock Medical Center, Lebanon, NH, USA
Ryland Richards
Julianna m. czum.
2 Department of Radiology, Dartmouth-Hitchcock Medical Center, Lebanon, NH, USA
The following fictional case is intended as a learning tool within the Pathology Competencies for Medical Education (PCME), a set of national standards for teaching pathology. These are divided into three basic competencies: Disease Mechanisms and Processes, Organ System Pathology, and Diagnostic Medicine and Therapeutic Pathology. For additional information, and a full list of learning objectives for all three competencies, see http://journals.sagepub.com/doi/10.1177/2374289517715040 . 1
Primary Objective
Objective RS2.8: Aspiration Pneumonia. Name risk factors for aspiration pneumonia and describe the pathology, prognosis, and potential complications.
Competency 2: Organ System Pathology; Topic RS: Respiratory System; Learning Goal 2: Pulmonary Infection.
Patient Presentation
A 79-year-old female presented to her primary care doctor with the complaint of persistent cough and fatigue. This persisted for approximately 3 months and was accompanied by shortness of breath with exertional activities such as brisk walking and stair climbing. She was given a prescription for antibiotics for presumed infection 4 weeks prior at an urgent care center while on vacation, with only slight improvement. Her husband, who accompanies her, states that she coughs more while eating meals. Her past medical history is remarkable for a stroke 2 years earlier. She also had 20 pack-years of cigarette smoking but quit over 25 years ago. On physical examination, she has a low-grade fever with decreased lung sounds bilaterally to auscultation (right side slightly more than left side).
Diagnostic Findings, Part 1
A chest radiograph (CXR) is ordered. It is shown in Figure 1A . A follow-up computed tomography (CT) scan is ordered to better define the CXR findings, and a coronal view of the lung tissue is shown in Figure 1B .

A, Chest radiograph, showing arrows pointing to bilateral bronchocentric opacification of basal lower lobes. B, Coronal view of computed tomography scan shows thickening of bilateral basal lower lobes. Arrows are pointing to low-density tubular opacities consistent with aspirated material in bronchi.
Questions/Discussion Points, Part 1
Please interpret the radiographs and discuss a differential for your findings.
The CXR shows multiple areas of peribronchial shadowing with thickening of airways in the basal lower lobes bilaterally ( Figure 1A ). This finding is not specific. The differential diagnosis includes infectious pneumonia, especially given her symptoms of fatigue, dyspnea, cough, and fever. Because the antibiotics did not clear her symptoms, it is possible that this is not infection; however, it is also possible that the antibiotic prescribed was ineffective for the causative infectious agent. Given her history of smoking, the differential also includes lung cancer. Lung cancer can present with fatigue, cough, and dyspnea. Some lung cancers, especially small-cell neuroendocrine carcinoma, are classically located in the hilar/peribronchial location of the lung. A CT scan would help to define the character and location of the infiltrate better than a CXR. Because this CXR does not show a single mass lesion, the consideration of a cancer from a non-lung primary that is metastatic to the lungs is also in the differential. A CT scan can better clarify if smaller lung masses are present, if lymph nodes are enlarged, and if any pleural cancer deposits are present. Given her history of stroke, and her husband’s comment that the cough seems to worsen with eating, aspiration of particles such as food is also within the differential.
A CT scan was ordered, and the coronal CT scan shows low-density tubular opacities associated with the airways ( Figure 1B ). A tissue biopsy directed at the airway-associated opacity was ordered to confirm the diagnosis.
Diagnostic Findings, Part 2
The histologic findings of the lung biopsy tissue are shown in Figures 2 , ,3, 3 , and and4 4 .

A, Lung photomicrograph showing the inflammatory process centered on an airway (arrow). Note the normal lung tissue on the left side (H&E stain, ×4 magnification). B, A higher magnification with residual bronchial epithelium on the right center (single thin arrow). The airway is filled with luminal foreign debris and cuffing inflammation (short thick arrows). The debris is pink colored and acellular (H&E stain, ×10 magnification).

A, This airway shows foreign material embedded into the lung tissue (arrow; H&E stain, ×10 magnification). B, A higher magnification with the foreign particle surrounded by multinucleated giant cells (arrow; H&E stain, ×20 magnification).

The foreign material is somewhat amorphous and pink, similar to the material in Figure 2 (long arrow); however, there is an acute neutrophil infiltrate mixed with the material (short arrow) in addition to the chronic inflammation and giant cells (H&E stain, ×10 magnification).
Questions/Discussion Points, Part 2
Please interpret the histologic findings ( figure 2 ).
On lower magnification in Figure 2A , normal lung tissue and alveolar spaces are seen on the left side of the image, while the right side appears to be consolidated lung tissue. Central in the image is a bronchus that appears disrupted and full of pink material (arrow). This area is enlarged in Figure 2B , showing a strip of residual normal bronchial airway epithelium (long thin arrow). There is an inflammatory infiltrate composed of chronic-type inflammatory cells, lymphocytes, and plasma cells, surrounding the airway. Acellular pink luminal content ( Figure 2B , short arrows) is seen, which likely represents aspirated material.
A Different Airway Is Shown in Figure 3 . What Is the Arrow Pointing to in These Photos?
In Figure 3A , foreign material is seen embedded in lung tissue. The pleural surface can be seen on the right edge of the photo. On higher magnification of this material ( Figure 3B ), the foreign material is seen surrounded by multinucleated giant cells. The foreign material in this photo is likely food and shows fine cellular detail suggestive of a more recent aspiration event. The multinucleated giant cells will degrade the foreign material by phagocytosis over time. 2
The Airway in Figure 4 Shows Luminal Content. What Inflammatory Cells Are Seen in Figure 4 ?
In Figure 4 , the long arrow is pointing to the luminal content. The short arrow is pointing to a strip of the residual normal airway epithelial lining. This helps us to recognize the location of the material in an airway. The cellular infiltrate in this airway is composed mainly of the acute inflammatory cell, the neutrophil. A collection of neutrophils is called an abscess. Giant cells and lymphocytes are also found in lesser numbers. The foreign material in this airway is more degraded, similar in appearance to the luminal content in Figure 2 , and may represent material that has been in the lung for a longer time than the material in Figure 3 . 2
What Is the Diagnosis?
The patient is suffering from chronic aspiration pneumonia or a chronic inhalation of foreign particles into her lungs. The inhalations of foreign particles is ongoing, meaning that she is likely aspirating or inhaling small food particles while she is eating. Her clinical history is positive for coughing, especially while eating, which is a common finding in patients who aspirate small particles of food, but is sometimes noticed by others, and not by the patient themselves. She has also suffered a stroke 2 years prior, which is a risk factor for aspiration, as it could impair her swallow ability and put her at risk for aspiration events.
Which Patient Populations Are at Risk for Aspiration Pneumonia?
Although aspiration is most common in children, aspiration affects adults, especially the elderly population. Often the aspiration event is clinically “silent,” meaning that the patient does not realize that a small amount of food was inhaled into the lung, rather than swallowed. Because coughing becomes chronic, a patient may not be able to realize the connection of aspiration to coughing. Difficulty swallowing (dysphasia) and impaired neurological status (causing secondary dysphasia) are two of the most important clinical conditions that predispose patients to aspiration. 3 Dysphagia is a symptom that is shared by many neurological diseases. In patients with stroke, it may improve over time, while in patients with dementia, it tends to progress with the disease. Clinically, patients with dysphagia do not always complain of difficulty swallowing, but advanced testing such as videofluoroscopic swallow evaluation demonstrates aspiration. 4 Mechanical devices that interfere with swallowing, such as nasogastric tubes or tracheostomies, also increase risk. In the community setting, impairment of consciousness by alcohol or drug use is most commonly associated with aspiration pneumonia, followed by dysphagia. 3 In addition, poor oral hygiene has been reported as a risk factor. Aggressive oral care in elderly patients has been associated with a lower incidence of aspiration pneumonia. 5 Gastroesophageal reflux disease has also been implicated in aspiration, although it is present in a variety of pulmonary diseases; therefore, its role as a causative agent of aspiration pneumonia likely depends on other factors as well. 6
Describe the Etiology and Natural History of Aspiration Pneumonia
The lung’s reaction to the aspiration event depends on the composition and size of the aspirated content. Solid materials and fluids can both be aspirated. They can cause obstruction, infection, or tissue injury. Fluids are not apparent in tissue biopsies, but the reaction of the lung tissue to the fluid (inflammation, injury) may be present. In children, aspiration commonly involves larger particles and can lead to airway obstruction or ball-valve type obstructions. In debilitated patients, small particulate matter aspiration is more common. When toxic material such as gastric acid is aspirated, it can hurt the delicate lung tissue. This is called chemical aspiration. The lung tissue reacts to the damage with varying degrees of necrosis, edema, and inflammation. This reaction is called chemical pneumonitis. Pneumonitis results from an inflammatory reaction to the aspirated material, whereas pneumonia is an infection of the lung by microbiota within the aspirate. 7 In an acute inflammatory reaction, the main inflammatory cell present is the neutrophil. This is the common and predominant reaction to bacterial infection. With infection, oral bacteria are aspirated along with the foreign material, causing the infection. Common oral flora include anaerobic organisms such as Bacteroides, Prevotella, Fusobacterium, Peptostreptococcus, and aerobic flora including Streptococcus pneumonia , Staphylococcus aureus , Haemophilus influenzae , and Pseudomonas aeruginosa . 8 Many patients with aspiration events have components of chemical and infectious pneumonia. Infections can yield multiple organisms on microbiology culture.
What Are the Clinical Presentations of Aspiration Pneumonia?
Presenting symptoms include cough, dyspnea, and hypoxemia. Infectious aspiration pneumonia is more likely to present with a productive cough and persistent fever, whereas in pure chemical pneumonitis, the cough is generally nonproductive and fever is either transient or may not be present at all. Again, many aspirations have features of both.
What Are the Typical Radiographic Findings for Aspiration?
Aspiration commonly involves the posterior segment of the upper lobes and the superior segment of the lower lobes. Because of the more obtuse angle of the right-sided bronchi, the right lower lobe is frequently involved with aspiration, but the position of the patient during the episode of aspiration leads to bilateral involvement in half of cases. Foreign body aspiration typically manifests as obstructive lobar or segmental over inflation or atelectasis. An extensive, patchy bronchopneumonic pattern may be observed in patients following massive aspiration of gastric acid or liquid. Aspiration of infectious material manifests as necrotizing consolidation and abscess formation. The low specificity of diagnostic CXR in aspiration diseases can be improved with CT and by being familiar with the clinical settings in which aspiration is likely to occur. 9 , 10 The radiographic differential depends on the pattern of lung involvement but includes acute infection, chronic infection such as fungal infection, nodular fibrosing lung disease, and cancer metastasis, especially if the patient had a history of a prior cancer.
What Are the Potential Complications of Aspiration Pneumonia?
In addition to an infectious pneumonia involving a lobe of lung, or a segment of lung, lobar or segmental pneumonia, tissue abscess, empyema, and necrosis can occur. In a tissue abscess, a collection of purulent neutrophils and cellular debris aggregates and is difficult to treat with antibiotics due to the poor vascularization from the microscopic tissue destruction. The abscess often needs surgical intervention in the form of drainage or surgical excision. The drained fluid is rich in neutrophils and cellular debris and appears pus-like or purulent. If infection extends to the pleural surface of the lung, the space between the lung and inner chest wall can become infected. Involvement of the pleura and pleural space is called empyema. The purulent material may collect in this “potential space” and impede lung inflation or cause adhesions between the lung and the chest wall, which can make breathing difficult. This also requires surgical intervention in the form of drainage and debridement. In complex cases, it may lead to sepsis and death.
Teaching Points
- Aspiration pneumonia causes a bronchocentric pattern involvement, mainly in the posterior segment of the upper lobes and the superior segment of the lower lobes.
- Aspiration pneumonia is common in elderly patients and patients who are debilitated, such as those with neurologic or swallowing deficiencies.
- Aspiration pneumonia can lead to chemical pneumonitis, infectious pneumonia, or a combination of both.
- Degrading foreign material can be visualized microscopically in many cases of particular aspiration.
- Infections in aspiration pneumonia are caused mainly by oral contaminant.
- The most common infectious organisms in aspiration pneumonia are oral flora.
- Aspiration of a material that damages the lung tissue and causes a tissue reaction, but not infection, is called chemical aspiration.
- Complications of aspiration include pneumonia, abscess, tissue necrosis, and death.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.

Citation, DOI, disclosures and case data
At the time the case was submitted for publication Frank Gaillard had no recorded disclosures.
Presentation
Acutely unwell.
Patient Data
Extensive consolidation and air bronchograms with loss of the right hemidiaphragm in keeping with right lower lobe consolidation. In this setting most likely community-acquired pneumonia. Whether or not there is an associated small pleural effusion is uncertain. Minor patchy airspace opacity is also in the left midzone.
Case Discussion
Chest x-ray demonstrates extensive consolidation and air bronchograms. Patient treated in ICU for numerous days.
Streptococcus pneumoniae isolated.
1 article features images from this case
- Lobar pneumonia
101 public playlists include this case
- Favourites by Andreas S Fazekas
- PA Matrix cases by Denise Foulkes
- FRCR 2B AMR SAADAWY (part 2) (part 1) by Amr Saadawy
- infectious CXR by Christopher Zamani
- Chest Rad 3rd Year by Stephanie Vojvodin
- Important chest xray for emergency board exam by Maryam Saif AlAli
- CHEST VIVA by Juliana Tsuruta
- FFICM OSCE Radiology Head and Chest by Lisa Shannon ◉
- Xrays by Sarah Hodgson
- Chest - breathlessness 1 by Radiology Registrar PULSE Teaching
- Chest x-ray basic search strategies and pathology (part 1) by Andrew Murphy ◉
- IMAG5042 Module 3 by Sally Ayesa ◉
- Group 11 Tutorial by Sam Maxwell
- BPT Chest by Wayland Wang ◉ ◈
- A quiz sfu by Eva Fischer ◉
- Yaz Q8 ex3 by Joshua Evans
- Torax by Agustin Marotta
- Lung Infections JK by Jan Kaczmarek
- Cviko by Andrea Úriová
- Micro by Shalitha Bandara Samarakoon
- Chest cases by Muhammad Qasim Khan
- FA - week 1 by Elena Dama
- Thorax by Tobias Boppel
- Chest by Gajan Surendra
- Chest imaging (focal lung lesions) by Mohamed Shedeed
- pneumonia by Matiullah Hamdard
- Careers Day Radiology by Osama Al-Jibury
- Chest cases by N Seth
- 一FY Adult Chest by Jeremy Jones ◉
- Chest by Piyathida
- BOARDS by Rachel Martin
- STUDENTS ! by Hysni Dida
- Chest Xray PG by Hamid Hassan
- MSSP Week 30 by Simon MacGowan
- ED chest cases by Ana Brusic ◉
- Propofology by David Lyness
- CHEST101 by Sherif Maccar ◉
- Medical Student CXR 1 by Lisa Shannon ◉
- Macormiston lung infection by Mark
- Imanchest by Iman Fani
- RS by Marko Atanasković
- Lobar pneumonia by Vincent Nguyen
- Basic chest by Steve Thomas
- RACGP cases by Henry Knipe ◉
- 1.RESPIRATORY-Pneumonia by Dinesh Madhavan Nair
- ćwiczenia 5 rok by Katarzyna Gwoździewicz
- Mod 11 Chest by Candace Higney
- AkutsjvNU1 by Daniel Vestberg
- Mk by Iryna Drevych Romanivna
- Lp AMG An 2 by Vlad-Octavian Bolocan
- GK - Chest - CXR Basic by GLK
- Thoracic Spine/Chest by Sean Norkus
- Chest Lungs by Oleksii Burian
- MSSP Week 24 by Simon MacGowan
- Chest by Kayla Beck
- Trabalho 6p by Fernando Machado Maia
- Revision - Chest by Aman Sandhu
- Derby FY2 Teaching Emergency Radiology by Kushal Joshi
- ICU chest cases by Paul Heyworth
- DH Chest by David Hocking
- av frcr 2 by Avni K P Skandhan
- 一MBChB 5th year CXR by Jeremy Jones ◉
- Medical Student Course by Lewis Donovan
- Examen by Samantha Angeles
- Polmonite by Tommaso Lo Castro
- ED CXR Hao by Hao Xiang
- Prova Elise by ferdinand duenas cabrera filho
- Lung by Maria Mirabela Fratila
- Intern Education - Chest by Wayland Wang ◉ ◈
- exam1 by Behdin Abed
- Core Conditions 08.2 - Lungs and pleura pre-reading by RMH Core Conditions ◈
- RAD6705 Exam 1 by Chris Borgerding
- Tórax 2 by Laura Bellis Nitoli
- CXR 101: A Primer by Aaron Wong
- Chest by Albs Pols
- chest by Emil Michalski
- Chest Reads by Matthew Blais
- Respiratory by Shaurya Singh Baghel
- Tutorial by HOUDA ISMAIL AGHIL
- Thoracic FRCR 2B by Dr Feras Salhi
- Ed SHO teaching Cxr by Henry Dillon
- DI 3302 Mod 11 by Talia LaForest
- Chest x ray by Emil Michalski
- Pulmonology by Muhammad Umair Shafique Sheikh
- b7 by Tse Yan Becky Chan
- THORACIC FRCR 2B by Nazahat Pasha
- pneumo by Indira E.J Poulina
- Chest X-Ray by Salman Jehanzeb Tanauli
- Chest case review - Adv Imaging by Whitney Graff
- pneumonia by Simone Afonso Dini
- Lung Pathologies by Sean Norkus
- pneumonia by jenny Barrett
- Polmoniti Batteriche by Marco Raffaele Ciuffreda
- Clinical Diagnostics Test 2 by William Tanner Slay
- exam 2 by Jessica Patak
- Radio 2 exam by edioardo bonamano
- On-Call Simulation (g) by James Coey
- Pneumonia by Do Van Hien
- CHESTRad - Infection by Tito Alfredo Atencia Rincón
Related Radiopaedia articles
- Air bronchogram
Promoted articles (advertising)
How to use cases.
You can use Radiopaedia cases in a variety of ways to help you learn and teach.
- Add cases to playlists
- Share cases with the diagnosis hidden
- Use images in presentations
- Use them in multiple choice question
Creating your own cases is easy.
- Case creation learning pathway
ADVERTISEMENT: Supporters see fewer/no ads
By Section:
- Artificial Intelligence
- Classifications
- Imaging Technology
- Interventional Radiology
- Radiography
- Central Nervous System
- Gastrointestinal
- Gynaecology
- Haematology
- Head & Neck
- Hepatobiliary
- Interventional
- Musculoskeletal
- Paediatrics
- Not Applicable
Radiopaedia.org
- Feature Sponsor
- Expert advisers

More From Forbes
Why vertical integration is the path to strategic advantage.
- Share to Facebook
- Share to Twitter
- Share to Linkedin
Marc Emmer is president of Optimize Inc. and an author, speaker and consultant specializing in strategy and strategic planning.
Tesla's ascent in the automotive world is a story of innovation, not only because of technology and engineering but also because of a shrewd business strategy. Spearheaded by Elon Musk, Tesla has not just revolutionized the automotive industry but also provided a masterclass in vertical integration. In a world where supply chains have gone from being long and slow to short and agile, Tesla controls almost every facet of production.
Tesla's Strategic Mastery: A Case Study in Vertical Integration
Tesla's approach to vertical integration —owning as many aspects of production as possible, from raw materials to final assembly—is a stark contrast to the traditional automotive industry model of outsourcing key components and relying heavily on global supply chains. For example, Nissan recently announced plans to produce batteries through a partner in Great Britain.
This strategy not only allows Tesla to maintain quality control but also to innovate rapidly. By owning the supply chain, Tesla can bypass traditional barriers, accelerate its production cycles and maintain flexibility, which allows it to adapt quickly to new technologies or market demands.
The benefits of this approach became particularly evident during the global semiconductor shortage. While most automotive giants struggled with production halts, Tesla redesigned its software to support alternative chips, which showcases agility in its operations.
Impacts Beyond Risk Reduction
The shift to shorter supply chains has broader implications than mere risk reduction. It marks a significant change in how companies approach production, impacting everything from innovation to consumer relations.
1. Enhanced quality control: With more control over their supply chains, companies can improve quality standards, as this direct oversight can allow for immediate rectification of issues and help ensure the end product consistently meets consumer expectations.
2. Local economic benefits: Shorter supply chains often mean more localized and regional production, which can have positive effects on local economies. By sourcing and manufacturing closer to home, companies can contribute to job creation and economic growth in their regions.
3. Accelerated innovation: Shorter supply chains facilitate quicker feedback loops, which can allow companies to innovate at a faster pace. This rapid iteration is crucial in today's fast-evolving marketplaces, where staying ahead often means being the first to harness new technologies or trends.
4. Sustainability and ethical practices: With greater control over their supply chains, businesses can more effectively implement sustainable and ethical practices. This aspect is increasingly important to consumers, who are more likely to support brands that demonstrate environmental responsibility and ethical sourcing.
The Road Ahead: Challenges And Opportunities
While the move toward shorter supply chains is promising, it is not without its challenges . Establishing a controlled supply chain requires significant investment and expertise.
Companies must be willing to invest in infrastructure, technology and talent to manage this transition successfully.
As industries increasingly adopt this model, the competitive landscape could shift. Companies that are slow to adapt could find themselves at a disadvantage, struggling to keep pace with more agile competitors.
The New Era Of Supply Chains
The Covid-19 pandemic was as a significant disruptor across industries, underlining the fragility and complexities of extended global supply chains. It’s particularly crucial in an era marked by frequent and unpredictable global disruptions.
Alongside the primary objective of risk mitigation, the adoption of shorter supply chains presents a myriad of supplementary benefits. These include an enhanced ability to swiftly adapt to evolving market trends and consumer preferences, leading to more dynamic and responsive business operations.
• Logistics: Companies may observe a reduction in transportation and logistical costs, as shorter supply chains typically involve less complex and more direct routes.
• Carbon footprint: From an environmental perspective, this shift may also lead to a reduction in the carbon footprint, as shorter supply chains could mean less extensive transportation requirements.
• Inventory management: A critical element in this transition is the evolution of inventory management strategies. I've observed many companies that are actively rethinking their approach to inventory management, aiming to revise strategies that include redefining decoupling points and adjusting buffer sizes.
As companies adapt to this evolving landscape, the insights from Tesla's model are invaluable. The future of business success increasingly hinges on adept supply chain management, a domain where Tesla has already set a precedent.
Forbes Business Council is the foremost growth and networking organization for business owners and leaders. Do I qualify?
- Editorial Standards
- Reprints & Permissions

COMMENTS
A 44-year-old woman presented with cough, dyspnea, and chest pain. On examination, she had tachycardia and hypotension. Evaluation revealed SARS-CoV-2 RNA in a nasopharyngeal swab, as well as eleva...
We're going to go through a case study for pneumonia together. Let's get started in this scenario. We have a 72-year-old patient who is male. He was admitted via the emergency department to the med-surg floor with a diagnosis of community-acquired pneumonia. He arrives in the room by a stretcher with oxygen flowing through a nasal cannula.
Pneumonia (from the Greek pneuma, "breath") is a potentially fatal infection and inflammation of the lower. respiratory tract (i.e., bronchioles and alveoli) usually caused by inhaled bacteria ...
To focus on clinical trial design issues pertinent to the population of patients with mild pneumonia, a typical clinical-trial candidate patient is described below. Case Presentation. Present illness. A 35-year-old male resident of Boston, Massachusetts, presents with fever and cough.
This case report describes common historical and physical examination findings in CABP and the use of traditional and more modern diagnostic tools, as well as treatment dilemmas currently facing clinicians. Streptococcus pneumoniae remains the leading bacterial cause of pneumonia in the United States and globally.
A 57-year-old man was admitted to the intensive care unit in the winter because of severe pneumonia and acute hypoxemic respiratory failure. ... Case 32 -2015 — A 57 ... For example, one study ...
This case study of severe Covid-19 pneumonia and CRS illustrates some of the diagnostic and therapeutic challenges and controversies regarding the management of this novel and complex infection. Meticulous monitoring for and early treatment of the hyperinflammatory phase of the disease may be crucial in preventing progression to severe ARDS ...
lung, pneumonia, pneumonia, recurrent, pleural effusion, atelectasis A previously healthy 15-year-old girl presents with a history of back pain, chills, and shortness of breath of 1 day's duration. On examination she is afebrile and well appearing despite mild tachypnea (respiratory rate of 24 breaths/min).
This case study aimed to represent the actual scenario of severe childhood pneumonia case management at community clinic. Considering that circumstances, International Centre for Diarrheal Disease Research, Bangladesh (icddr,b) developed an innovative day care management approach as safe, effective and less expensive alternative to hospital ...
Case history. A 54-year-old smoker with multiple comorbidities (diabetes, hypertension, coronary artery disease) presents with a 2-day history of a productive cough with yellow sputum, chest tightness, and fever. Physical exam reveals a temperature of 101°F (38.3°C), BP of 150/95 mmHg, heart rate of 85 bpm, and a respiratory rate of 20 ...
Abstract. Pneumonia is a potentially fatal infection and inflammation of the lower respiratory tract, namely the bronchioles and alveoli, caused by bacteria and viruses inhaled into the lungs. In older individuals all around the world, community-acquired pneumonia (CAP) is a common cause of hospitalisation and death.
Sample Case Study Of Pneumonia Richard G. Bachur,Kathy N. Shaw Case Studies in Adult Intensive Care Medicine Daniele Bryden,Andrew Temple,2017-04-20 This case-based approach to the intensive care medicine curriculum provides 48 case studies linking core knowledge to clinical context. Topics chosen
This is a prospective case-control study in which all children aged 5 years and below with clinically diagnosed pneumonia and healthy controls will be recruited at three study sites. As per assumptions of 95% confidence interval (CI), 80% power and detectable odds ratio (OR) of 1.5, we estimate 164 cases and 164 healthy controls per sentinel ...
Community-acquired pneumonia (CAP) is an infectious disease commonly seen in the primary care environment. CAP is ranked as the sixth leading cause of death in the United States. It affects more than 10 million individuals per year and accounts for 500,000-1,000,000 hospital admissions. Precise diagnosis of CAP continues to be complex.
current issue. current issue; browse recently published; browse full issue index; learning/cme
Case Study RESPIRATORY SYSTEM CHAPTER 23, MANAGEMENT OF PATIENTS WITH CHEST AND LOWER RESPIRATORY TRACT DISORDERS Harry Smith, 70 years of age, is a male patient who is admitted to the medical-surgical unit with acute community-acquired pneumonia. He was diagnosed with parastatal emphysema years ago.
Abstract. The following fictional case is intended as a learning tool within the Pathology Competencies for Medical Education (PCME), a set of national standards for teaching pathology. These are divided into three basic competencies: Disease Mechanisms and Processes, Organ System Pathology, and Diagnostic Medicine and Therapeutic Pathology.
Pneumonia Case Study. HS is 70 years of age and a male patient who is admitted to the medical-surgical unit with acute Community Acquired Pneumonia. He was diagnosed with paraseptal emphysema three years ago. The patient smoked cigarettes 1 pack per day for 55 years and quit three years ago.
Case Study - Pneumonia - Free download as Word Doc (.doc), PDF File (.pdf), Text File (.txt) or read online for free. Community-acquired pneumonia (CAP) is the most common type of pneumonia and is caused by a variety of pathogens including bacteria and viruses. CAP is the fourth leading cause of death in the UK and sixth in the US. The document discusses CAP, including causes, symptoms, and ...
Patient Data. Extensive consolidation and air bronchograms with loss of the right hemidiaphragm in keeping with right lower lobe consolidation. In this setting most likely community-acquired pneumonia. Whether or not there is an associated small pleural effusion is uncertain. Minor patchy airspace opacity is also in the left midzone.
This case study presents a 94-year-old Filipino woman, Rachel, who was admitted to the hospital for community-acquired pneumonia. She reported a one-week history of difficulty breathing, productive cough, and undocumented fever before seeking initial medical care. Upon admission, her vital signs and oxygen saturation were abnormal. As an elderly patient, details of her past medical history ...
Tesla's Strategic Mastery: A Case Study in Vertical Integration. ... For example, Nissan recently announced plans to produce batteries through a partner in Great Britain.