Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- My Account Login
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Systematic Review
- Open access
- Published: 20 July 2022

The serotonin theory of depression: a systematic umbrella review of the evidence
- Joanna Moncrieff 1 , 2 ,
- Ruth E. Cooper 3 ,
- Tom Stockmann 4 ,
- Simone Amendola 5 ,
- Michael P. Hengartner 6 &
- Mark A. Horowitz 1 , 2
Molecular Psychiatry volume 28 , pages 3243–3256 ( 2023 ) Cite this article
1.26m Accesses
230 Citations
9424 Altmetric
Metrics details
- Diagnostic markers
The serotonin hypothesis of depression is still influential. We aimed to synthesise and evaluate evidence on whether depression is associated with lowered serotonin concentration or activity in a systematic umbrella review of the principal relevant areas of research. PubMed, EMBASE and PsycINFO were searched using terms appropriate to each area of research, from their inception until December 2020. Systematic reviews, meta-analyses and large data-set analyses in the following areas were identified: serotonin and serotonin metabolite, 5-HIAA, concentrations in body fluids; serotonin 5-HT 1A receptor binding; serotonin transporter (SERT) levels measured by imaging or at post-mortem; tryptophan depletion studies; SERT gene associations and SERT gene-environment interactions. Studies of depression associated with physical conditions and specific subtypes of depression (e.g. bipolar depression) were excluded. Two independent reviewers extracted the data and assessed the quality of included studies using the AMSTAR-2, an adapted AMSTAR-2, or the STREGA for a large genetic study. The certainty of study results was assessed using a modified version of the GRADE. We did not synthesise results of individual meta-analyses because they included overlapping studies. The review was registered with PROSPERO (CRD42020207203). 17 studies were included: 12 systematic reviews and meta-analyses, 1 collaborative meta-analysis, 1 meta-analysis of large cohort studies, 1 systematic review and narrative synthesis, 1 genetic association study and 1 umbrella review. Quality of reviews was variable with some genetic studies of high quality. Two meta-analyses of overlapping studies examining the serotonin metabolite, 5-HIAA, showed no association with depression (largest n = 1002). One meta-analysis of cohort studies of plasma serotonin showed no relationship with depression, and evidence that lowered serotonin concentration was associated with antidepressant use ( n = 1869). Two meta-analyses of overlapping studies examining the 5-HT 1A receptor (largest n = 561), and three meta-analyses of overlapping studies examining SERT binding (largest n = 1845) showed weak and inconsistent evidence of reduced binding in some areas, which would be consistent with increased synaptic availability of serotonin in people with depression, if this was the original, causal abnormaly. However, effects of prior antidepressant use were not reliably excluded. One meta-analysis of tryptophan depletion studies found no effect in most healthy volunteers ( n = 566), but weak evidence of an effect in those with a family history of depression ( n = 75). Another systematic review ( n = 342) and a sample of ten subsequent studies ( n = 407) found no effect in volunteers. No systematic review of tryptophan depletion studies has been performed since 2007. The two largest and highest quality studies of the SERT gene, one genetic association study ( n = 115,257) and one collaborative meta-analysis ( n = 43,165), revealed no evidence of an association with depression, or of an interaction between genotype, stress and depression. The main areas of serotonin research provide no consistent evidence of there being an association between serotonin and depression, and no support for the hypothesis that depression is caused by lowered serotonin activity or concentrations. Some evidence was consistent with the possibility that long-term antidepressant use reduces serotonin concentration.
Similar content being viewed by others

Genetic contributions to brain serotonin transporter levels in healthy adults
Silvia Elisabetta Portis Bruzzone, Arafat Nasser, … Patrick MacDonald Fisher
The kynurenine pathway in major depressive disorder, bipolar disorder, and schizophrenia: a meta-analysis of 101 studies
Wolfgang Marx, Amelia J. McGuinness, … Brisa S. Fernandes

The complex clinical response to selective serotonin reuptake inhibitors in depression: a network perspective
Lynn Boschloo, Fredrik Hieronymus, … Elias Eriksson
Introduction
The idea that depression is the result of abnormalities in brain chemicals, particularly serotonin (5-hydroxytryptamine or 5-HT), has been influential for decades, and provides an important justification for the use of antidepressants. A link between lowered serotonin and depression was first suggested in the 1960s [ 1 ], and widely publicised from the 1990s with the advent of the Selective Serotonin Reuptake Inhibitor (SSRI) antidepressants [ 2 , 3 , 4 ]. Although it has been questioned more recently [ 5 , 6 ], the serotonin theory of depression remains influential, with principal English language textbooks still giving it qualified support [ 7 , 8 ], leading researchers endorsing it [ 9 , 10 , 11 ], and much empirical research based on it [ 11 , 12 , 13 , 14 ]. Surveys suggest that 80% or more of the general public now believe it is established that depression is caused by a ‘chemical imbalance’ [ 15 , 16 ]. Many general practitioners also subscribe to this view [ 17 ] and popular websites commonly cite the theory [ 18 ].
It is often assumed that the effects of antidepressants demonstrate that depression must be at least partially caused by a brain-based chemical abnormality, and that the apparent efficacy of SSRIs shows that serotonin is implicated. Other explanations for the effects of antidepressants have been put forward, however, including the idea that they work via an amplified placebo effect or through their ability to restrict or blunt emotions in general [ 19 , 20 ].
Despite the fact that the serotonin theory of depression has been so influential, no comprehensive review has yet synthesised the relevant evidence. We conducted an ‘umbrella’ review of the principal areas of relevant research, following the model of a similar review examining prospective biomarkers of major depressive disorder [ 21 ]. We sought to establish whether the current evidence supports a role for serotonin in the aetiology of depression, and specifically whether depression is associated with indications of lowered serotonin concentrations or activity.
Search strategy and selection criteria
The present umbrella review was reported in accordance with the 2009 PRISMA statement [ 22 ]. The protocol was registered with PROSPERO in December 2020 (registration number CRD42020207203) ( https://www.crd.york.ac.uk/prospero/display_record.php?RecordID=207203 ). This was subsequently updated to reflect our decision to modify the quality rating system for some studies to more appropriately appraise their quality, and to include a modified GRADE to assess the overall certainty of the findings in each category of the umbrella review.
In order to cover the different areas and to manage the large volume of research that has been conducted on the serotonin system, we conducted an ‘umbrella’ review. Umbrella reviews survey existing systematic reviews and meta-analyses relevant to a research question and represent one of the highest levels of evidence synthesis available [ 23 ]. Although they are traditionally restricted to systematic reviews and meta-analyses, we aimed to identify the best evidence available. Therefore, we also included some large studies that combined data from individual studies but did not employ conventional systematic review methods, and one large genetic study. The latter used nationwide databases to capture more individuals than entire meta-analyses, so is likely to provide even more reliable evidence than syntheses of individual studies.
We first conducted a scoping review to identify areas of research consistently held to provide support for the serotonin hypothesis of depression. Six areas were identified, addressing the following questions: (1) Serotonin and the serotonin metabolite 5-HIAA–whether there are lower levels of serotonin and 5-HIAA in body fluids in depression; (2) Receptors - whether serotonin receptor levels are altered in people with depression; (3) The serotonin transporter (SERT) - whether there are higher levels of the serotonin transporter in people with depression (which would lower synaptic levels of serotonin); (4) Depletion studies - whether tryptophan depletion (which lowers available serotonin) can induce depression; (5) SERT gene – whether there are higher levels of the serotonin transporter gene in people with depression; (6) Whether there is an interaction between the SERT gene and stress in depression.
We searched for systematic reviews, meta-analyses, and large database studies in these six areas in PubMed, EMBASE and PsycINFO using the Healthcare Databases Advanced Search tool provided by Health Education England and NICE (National Institute for Health and Care Excellence). Searches were conducted until December 2020.
We used the following terms in all searches: (depress* OR affective OR mood) AND (systematic OR meta-analysis), and limited searches to title and abstract, since not doing so produced numerous irrelevant hits. In addition, we used terms specific to each area of research (full details are provided in Table S1 , Supplement). We also searched citations and consulted with experts.
Inclusion criteria were designed to identify the best available evidence in each research area and consisted of:
Research synthesis including systematic reviews, meta-analysis, umbrella reviews, individual patient meta-analysis and large dataset analysis.
Studies that involve people with depressive disorders or, for experimental studies (tryptophan depletion), those in which mood symptoms are measured as an outcome.
Studies of experimental procedures (tryptophan depletion) involving a sham or control condition.
Studies published in full in peer reviewed literature.
Where more than five systematic reviews or large analyses exist, the most recent five are included.
Exclusion criteria consisted of:
Animal studies.
Studies exclusively concerned with depression in physical conditions (e.g. post stroke or Parkinson’s disease) or exclusively focusing on specific subtypes of depression such as postpartum depression, depression in children, or depression in bipolar disorder.
No language or date restrictions were applied. In areas in which no systematic review or meta-analysis had been done within the last 10 years, we also selected the ten most recent studies at the time of searching (December 2020) for illustration of more recent findings. We performed this search using the same search string for this domain, without restricting it to systematic reviews and meta-analyses.
Data analysis
Each member of the team was allocated one to three domains of serotonin research to search and screen for eligible studies using abstract and full text review. In case of uncertainty, the entire team discussed eligibility to reach consensus.
For included studies, data were extracted by two reviewers working independently, and disagreement was resolved by consensus. Authors of papers were contacted for clarification when data was missing or unclear.
We extracted summary effects, confidence intervals and measures of statistical significance where these were reported, and, where relevant, we extracted data on heterogeneity. For summary effects in the non-genetic studies, preference was given to the extraction and reporting of effect sizes. Mean differences were converted to effect sizes where appropriate data were available.
We did not perform a meta-analysis of the individual meta-analyses in each area because they included overlapping studies [ 24 ]. All extracted data is presented in Table 1 . Sensitivity analyses were reported where they had substantial bearing on interpretation of findings.
The quality rating of systematic reviews and meta-analyses was assessed using AMSTAR-2 (A MeaSurement Tool to Assess systematic Reviews) [ 25 ]. For two studies that did not employ conventional systematic review methods [ 26 , 27 ] we used a modified version of the AMSTAR-2 (see Table S3 ). For the genetic association study based on a large database analysis we used the STREGA assessment (STrengthening the REporting of Genetic Association Studies) (Table S4 ) [ 28 ]. Each study was rated independently by at least two authors. We report ratings of individual items on the relevant measure, and the percentage of items that were adequately addressed by each study (Table 1 , with further detail in Tables S3 and S4 ).
Alongside quality ratings, two team members (JM, MAH) rated the certainty of the results of each study using a modified version of the GRADE guidelines [ 29 ]. Following the approach of Kennis et al. [ 21 ], we devised six criteria relevant to the included studies: whether a unified analysis was conducted on original data; whether confounding by antidepressant use was adequately addressed; whether outcomes were pre-specified; whether results were consistent or heterogeneity was adequately addressed if present; whether there was a likelihood of publication bias; and sample size. The importance of confounding by effects of current or past antidepressant use has been highlighted in several studies [ 30 , 31 ]. The results of each study were scored 1 or 0 according to whether they fulfilled each criteria, and based on these ratings an overall judgement was made about the certainty of evidence across studies in each of the six areas of research examined. The certainty of each study was based on an algorithm that prioritised sample size and uniform analysis using original data (explained more fully in the supplementary material), following suggestions that these are the key aspects of reliability [ 27 , 32 ]. An assessment of the overall certainty of each domain of research examining the role of serotonin was determined by consensus of at least two authors and a direction of effect indicated.
Search results and quality rating
Searching identified 361 publications across the 6 different areas of research, among which seventeen studies fulfilled inclusion criteria (see Fig. 1 and Table S1 for details of the selection process). Included studies, their characteristics and results are shown in Table 1 . As no systematic review or meta-analysis had been performed within the last 10 years on serotonin depletion, we also identified the 10 latest studies for illustration of more recent research findings (Table 2 ).
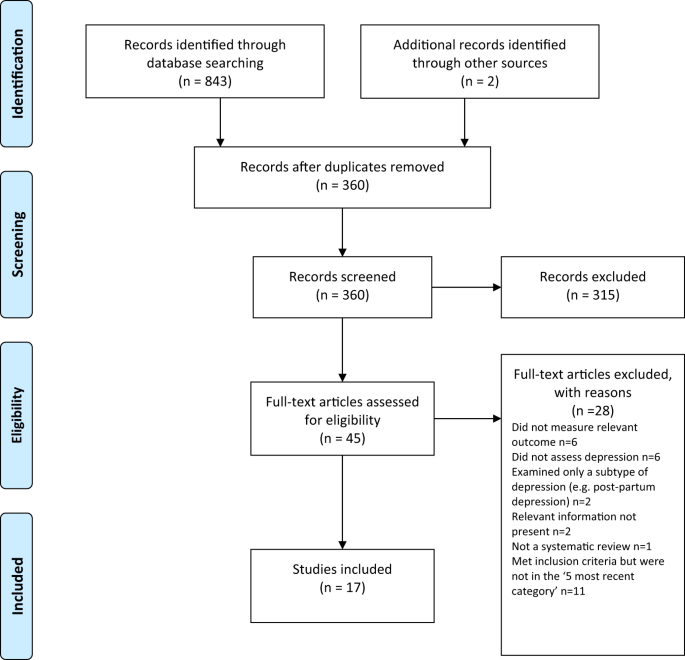
Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) flow diagramme.
Quality ratings are summarised in Table 1 and reported in detail in Tables S2 – S3 . The majority (11/17) of systematic reviews and meta-analyses satisfied less than 50% of criteria. Only 31% adequately assessed risk of bias in individual studies (a further 44% partially assessed this), and only 50% adequately accounted for risk of bias when interpreting the results of the review. One collaborative meta-analysis of genetic studies was considered to be of high quality due to the inclusion of several measures to ensure consistency and reliability [ 27 ]. The large genetic analysis of the effect of SERT polymorphisms on depression, satisfied 88% of the STREGA quality criteria [ 32 ].
Serotonin and 5-HIAA
Serotonin can be measured in blood, plasma, urine and CSF, but it is rapidly metabolised to 5-hydroxyindoleacetic acid (5-HIAA). CSF is thought to be the ideal resource for the study of biomarkers of putative brain diseases, since it is in contact with brain interstitial fluid [ 33 ]. However, collecting CSF samples is invasive and carries some risk, hence large-scale studies are scarce.
Three studies fulfilled inclusion criteria (Table 1 ). One meta-analysis of three large observational cohort studies of post-menopausal women, revealed lower levels of plasma 5-HT in women with depression, which did not, however, reach statistical significance of p < 0.05 after adjusting for multiple comparisons. Sensitivity analyses revealed that antidepressants were strongly associated with lower serotonin levels independently of depression.
Two meta-analyses of a total of 19 studies of 5-HIAA in CSF (seven studies were included in both) found no evidence of an association between 5-HIAA concentrations and depression.
Fourteen different serotonin receptors have been identified, with most research on depression focusing on the 5-HT 1A receptor [ 11 , 34 ]. Since the functions of other 5-HT receptors and their relationship to depression have not been well characterised, we restricted our analysis to data on 5-HT 1A receptors [ 11 , 34 ]. 5-HT 1A receptors, known as auto-receptors, inhibit the release of serotonin pre-synaptically [ 35 ], therefore, if depression is the result of reduced serotonin activity caused by abnormalities in the 5-HT 1A receptor, people with depression would be expected to show increased activity of 5-HT 1A receptors compared to those without [ 36 ].
Two meta-analyses satisfied inclusion criteria, involving five of the same studies [ 37 , 38 ] (see Table 1 ). The majority of results across the two analyses suggested either no difference in 5-HT 1A receptors between people with depression and controls, or a lower level of these inhibitory receptors, which would imply higher concentrations or activity of serotonin in people with depression. Both meta-analyses were based on studies that predominantly involved patients who were taking or had recently taken (within 1–3 weeks of scanning) antidepressants or other types of psychiatric medication, and both sets of authors commented on the possible influence of prior or current medication on findings. In addition, one analysis was of very low quality [ 37 ], including not reporting on the numbers involved in each analysis and using one-sided p-values, and one was strongly influenced by three studies and publication bias was present [ 38 ].
The serotonin transporter (SERT)
The serotonin transporter protein (SERT) transports serotonin out of the synapse, thereby lowering the availability of serotonin in the synapse [ 39 , 40 ]. Animals with an inactivated gene for SERT have higher levels of extra-cellular serotonin in the brain than normal [ 41 , 42 , 43 ] and SSRIs are thought to work by inhibiting the action of SERT, and thus increasing levels of serotonin in the synaptic cleft [ 44 ]. Although changes in SERT may be a marker for other abnormalities, if depression is caused by low serotonin availability or activity, and if SERT is the origin of that deficit, then the amount or activity of SERT would be expected to be higher in people with depression compared to those without [ 40 ]. SERT binding potential is an index of the concentration of the serotonin transporter protein and SERT concentrations can also be measured post-mortem.
Three overlapping meta-analyses based on a total of 40 individual studies fulfilled inclusion criteria (See Table 1 ) [ 37 , 39 , 45 ]. Overall, the data indicated possible reductions in SERT binding in some brain areas, although areas in which effects were detected were not consistent across the reviews. In addition, effects of antidepressants and other medication cannot be ruled out, since most included studies mainly or exclusively involved people who had a history of taking antidepressants or other psychiatric medications. Only one meta-analysis tested effects of antidepressants, and although results were not influenced by the percentage of drug-naïve patients in each study, numbers were small so it is unlikely that medication-related effects would have been reliably detected [ 45 ]. All three reviews cited evidence from animal studies that antidepressant treatment reduces SERT [ 46 , 47 , 48 ]. None of the analyses corrected for multiple testing, and one review was of very low quality [ 37 ]. If the results do represent a positive finding that is independent of medication, they would suggest that depression is associated with higher concentrations or activity of serotonin.
Depletion studies
Tryptophan depletion using dietary means or chemicals, such as parachlorophenylalanine (PCPA), is thought to reduce serotonin levels. Since PCPA is potentially toxic, reversible tryptophan depletion using an amino acid drink that lacks tryptophan is the most commonly used method and is thought to affect serotonin within 5–7 h of ingestion. Questions remain, however, about whether either method reliably reduces brain serotonin, and about other effects including changes in brain nitrous oxide, cerebrovascular changes, reduced BDNF and amino acid imbalances that may be produced by the manipulations and might explain observed effects independent of possible changes in serotonin activity [ 49 ].
One meta-analysis and one systematic review fulfilled inclusion criteria (see Table 1 ). Data from studies involving volunteers mostly showed no effect, including a meta-analysis of parallel group studies [ 50 ]. In a small meta-analysis of within-subject studies involving 75 people with a positive family history, a minor effect was found, with people given the active depletion showing a larger decrease in mood than those who had a sham procedure [ 50 ]. Across both reviews, studies involving people diagnosed with depression showed slightly greater mood reduction following tryptophan depletion than sham treatment overall, but most participants had taken or were taking antidepressants and participant numbers were small [ 50 , 51 ].
Since these research syntheses were conducted more than 10 years ago, we searched for a systematic sample of ten recently published studies (Table 2 ). Eight studies conducted with healthy volunteers showed no effects of tryptophan depletion on mood, including the only two parallel group studies. One study presented effects in people with and without a family history of depression, and no differences were apparent in either group [ 52 ]. Two cross-over studies involving people with depression and current or recent use of antidepressants showed no convincing effects of a depletion drink [ 53 , 54 ], although one study is reported as positive mainly due to finding an improvement in mood in the group given the sham drink [ 54 ].
SERT gene and gene-stress interactions
A possible link between depression and the repeat length polymorphism in the promoter region of the SERT gene (5-HTTLPR), specifically the presence of the short repeats version, which causes lower SERT mRNA expression, has been proposed [ 55 ]. Interestingly, lower levels of SERT would produce higher levels of synaptic serotonin. However, more recently, this hypothesis has been superseded by a focus on the interaction effect between this polymorphism, depression and stress, with the idea that the short version of the polymorphism may only give rise to depression in the presence of stressful life events [ 55 , 56 ]. Unlike other areas of serotonin research, numerous systematic reviews and meta-analyses of genetic studies have been conducted, and most recently a very large analysis based on a sample from two genetic databanks. Details of the five most recent studies that have addressed the association between the SERT gene and depression, and the interaction effect are detailed in Table 1 .
Although some earlier meta-analyses of case-control studies showed a statistically significant association between the 5-HTTLPR and depression in some ethnic groups [ 57 , 58 ], two recent large, high quality studies did not find an association between the SERT gene polymorphism and depression [ 27 , 32 ]. These two studies consist of by far the largest and most comprehensive study to date [ 32 ] and a high-quality meta-analysis that involved a consistent re-analysis of primary data across all conducted studies, including previously unpublished data, and other comprehensive quality checks [ 27 , 59 ] (see Table 1 ).
Similarly, early studies based on tens of thousands of participants suggested a statistically significant interaction between the SERT gene, forms of stress or maltreatment and depression [ 60 , 61 , 62 ], with a small odds ratio in the only study that reported this (1.18, 95% CI 1.09 to 1.28) [ 62 ]. However, the two recent large, high-quality studies did not find an interaction between the SERT gene and stress in depression (Border et al [ 32 ] and Culverhouse et al.) [ 27 ] (see Table 1 ).
Overall results
Table 3 presents the modified GRADE ratings for each study and the overall rating of the strength of evidence in each area. Areas of research that provided moderate or high certainty of evidence such as the studies of plasma serotonin and metabolites and the genetic and gene-stress interaction studies all showed no association between markers of serotonin activity and depression. Some other areas suggested findings consistent with increased serotonin activity, but evidence was of very low certainty, mainly due to small sample sizes and possible residual confounding by current or past antidepressant use. One area - the tryptophan depletion studies - showed very low certainty evidence of lowered serotonin activity or availability in a subgroup of volunteers with a family history of depression. This evidence was considered very low certainty as it derived from a subgroup of within-subject studies, numbers were small, and there was no information on medication use, which may have influenced results. Subsequent research has not confirmed an effect with numerous negative studies in volunteers.
Our comprehensive review of the major strands of research on serotonin shows there is no convincing evidence that depression is associated with, or caused by, lower serotonin concentrations or activity. Most studies found no evidence of reduced serotonin activity in people with depression compared to people without, and methods to reduce serotonin availability using tryptophan depletion do not consistently lower mood in volunteers. High quality, well-powered genetic studies effectively exclude an association between genotypes related to the serotonin system and depression, including a proposed interaction with stress. Weak evidence from some studies of serotonin 5-HT 1A receptors and levels of SERT points towards a possible association between increased serotonin activity and depression. However, these results are likely to be influenced by prior use of antidepressants and its effects on the serotonin system [ 30 , 31 ]. The effects of tryptophan depletion in some cross-over studies involving people with depression may also be mediated by antidepressants, although these are not consistently found [ 63 ].
The chemical imbalance theory of depression is still put forward by professionals [ 17 ], and the serotonin theory, in particular, has formed the basis of a considerable research effort over the last few decades [ 14 ]. The general public widely believes that depression has been convincingly demonstrated to be the result of serotonin or other chemical abnormalities [ 15 , 16 ], and this belief shapes how people understand their moods, leading to a pessimistic outlook on the outcome of depression and negative expectancies about the possibility of self-regulation of mood [ 64 , 65 , 66 ]. The idea that depression is the result of a chemical imbalance also influences decisions about whether to take or continue antidepressant medication and may discourage people from discontinuing treatment, potentially leading to lifelong dependence on these drugs [ 67 , 68 ].
As with all research synthesis, the findings of this umbrella review are dependent on the quality of the included studies, and susceptible to their limitations. Most of the included studies were rated as low quality on the AMSTAR-2, but the GRADE approach suggested some findings were reasonably robust. Most of the non-genetic studies did not reliably exclude the potential effects of previous antidepressant use and were based on relatively small numbers of participants. The genetic studies, in particular, illustrate the importance of methodological rigour and sample size. Whereas some earlier, lower quality, mostly smaller studies produced marginally positive findings, these were not confirmed in better-conducted, larger and more recent studies [ 27 , 32 ]. The identification of depression and assessment of confounders and interaction effects were limited by the data available in the original studies on which the included reviews and meta-analyses were based. Common methods such as the categorisation of continuous measures and application of linear models to non-linear data may have led to over-estimation or under-estimation of effects [ 69 , 70 ], including the interaction between stress and the SERT gene. The latest systematic review of tryptophan depletion studies was conducted in 2007, and there has been considerable research produced since then. Hence, we provided a snapshot of the most recent evidence at the time of writing, but this area requires an up to date, comprehensive data synthesis. However, the recent studies were consistent with the earlier meta-analysis with little evidence for an effect of tryptophan depletion on mood.
Although umbrella reviews typically restrict themselves to systematic reviews and meta-analyses, we aimed to provide the most comprehensive possible overview. Therefore, we chose to include meta-analyses that did not involve a systematic review and a large genetic association study on the premise that these studies contribute important data on the question of whether the serotonin hypothesis of depression is supported. As a result, the AMSTAR-2 quality rating scale, designed to evaluate the quality of conventional systematic reviews, was not easily applicable to all studies and had to be modified or replaced in some cases.
One study in this review found that antidepressant use was associated with a reduction of plasma serotonin [ 26 ], and it is possible that the evidence for reductions in SERT density and 5-HT 1A receptors in some of the included imaging study reviews may reflect compensatory adaptations to serotonin-lowering effects of prior antidepressant use. Authors of one meta-analysis also highlighted evidence of 5-HIAA levels being reduced after long-term antidepressant treatment [ 71 ]. These findings suggest that in the long-term antidepressants might produce compensatory changes [ 72 ] that are opposite to their acute effects [ 73 , 74 ]. Lowered serotonin availability has also been demonstrated in animal studies following prolonged antidepressant administration [ 75 ]. Further research is required to clarify the effects of different drugs on neurochemical systems, including the serotonin system, especially during and after long-term use, as well as the physical and psychological consequences of such effects.
This review suggests that the huge research effort based on the serotonin hypothesis has not produced convincing evidence of a biochemical basis to depression. This is consistent with research on many other biological markers [ 21 ]. We suggest it is time to acknowledge that the serotonin theory of depression is not empirically substantiated.
Data availability
All extracted data is available in the paper and supplementary materials. Further information about the decision-making for each rating for categories of the AMSTAR-2 and STREGA are available on request.
Coppen A. The biochemistry of affective disorders. Br J Psychiatry. 1967;113:1237–64.
CAS PubMed Google Scholar
American Psychiatric Association. What Is Psychiatry? 2021. https://www.psychiatry.org/patients-families/what-is-psychiatry-menu .
GlaxoSmithKline. Paxil XR. 2009. www.Paxilcr.com (site no longer available). Last accessed 27th Jan 2009.
Eli Lilly. Prozac - How it works. 2006. www.prozac.com/how_prozac/how_it_works.jsp?reqNavId=2.2 . (site no longer available). Last accessed 10th Feb 2006.
Healy D. Serotonin and depression. BMJ: Br Med J. 2015;350:h1771.
Google Scholar
Pies R. Psychiatry’s New Brain-Mind and the Legend of the “Chemical Imbalance.” 2011. https://www.psychiatrictimes.com/view/psychiatrys-new-brain-mind-and-legend-chemical-imbalance . Accessed March 2, 2021.
Geddes JR, Andreasen NC, Goodwin GM. New Oxford Textbook of Psychiatry. Oxford, UK: Oxford University Press; 2020.
Sadock BJ, Sadock VA, Ruiz P. Kaplan & Sadock’s Comprehensive Textbook of Psychiatry. 10th Editi. Lippincott Williams & Wilkins (LWW); 2017.
Cowen PJ, Browning M. What has serotonin to do with depression? World Psychiatry. 2015;14:158–60.
PubMed PubMed Central Google Scholar
Harmer CJ, Duman RS, Cowen PJ. How do antidepressants work? New perspectives for refining future treatment approaches. Lancet Psychiatry. 2017;4:409–18.
Yohn CN, Gergues MM, Samuels BA. The role of 5-HT receptors in depression. Mol Brain. 2017;10:28.
Hahn A, Haeusler D, Kraus C, Höflich AS, Kranz GS, Baldinger P, et al. Attenuated serotonin transporter association between dorsal raphe and ventral striatum in major depression. Hum Brain Mapp. 2014;35:3857–66.
Amidfar M, Colic L, Kim MWAY-K. Biomarkers of major depression related to serotonin receptors. Curr Psychiatry Rev. 2018;14:239–44.
CAS Google Scholar
Albert PR, Benkelfat C, Descarries L. The neurobiology of depression—revisiting the serotonin hypothesis. I. Cellular and molecular mechanisms. Philos Trans R Soc Lond B Biol Sci. 2012;367:2378–81.
CAS PubMed PubMed Central Google Scholar
Pilkington PD, Reavley NJ, Jorm AF. The Australian public’s beliefs about the causes of depression: associated factors and changes over 16 years. J Affect Disord. 2013;150:356–62.
PubMed Google Scholar
Pescosolido BA, Martin JK, Long JS, Medina TR, Phelan JC, Link BG. A disease like any other? A decade of change in public reactions to schizophrenia, depression, and alcohol dependence. Am J Psychiatry. 2010;167:1321–30.
Read J, Renton J, Harrop C, Geekie J, Dowrick C. A survey of UK general practitioners about depression, antidepressants and withdrawal: implementing the 2019 Public Health England report. Therapeutic Advances in. Psychopharmacology. 2020;10:204512532095012.
Demasi M, Gøtzsche PC. Presentation of benefits and harms of antidepressants on websites: A cross-sectional study. Int J Risk Saf Med. 2020;31:53–65.
Jakobsen JC, Gluud C, Kirsch I. Should antidepressants be used for major depressive disorder? BMJ Evidence-Based. Medicine. 2020;25:130–130.
Moncrieff J, Cohen D. Do antidepressants cure or create abnormal brain states? PLoS Med. 2006;3:e240.
Kennis M, Gerritsen L, van Dalen M, Williams A, Cuijpers P, Bockting C. Prospective biomarkers of major depressive disorder: a systematic review and meta-analysis. Mol Psychiatry. 2020;25:321–38.
Moher D, Liberati A, Tetzlaff J, Altman DG, Group P. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6:e1000097.
Fusar-Poli P, Radua J. Ten simple rules for conducting umbrella reviews. Evid Based Ment Health. 2018;21:95–100.
Pollock M, Fernandes RM, Becker LA, Pieper D, Hartling L. Chapter V: Overviews of Reviews. In: Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, et al., editors. Cochrane Handbook for Systematic Reviews of Interventions version 6.2,. version 6.Cochrane; 2021.
Shea BJ, Reeves BC, Wells G, Thuku M, Hamel C, Moran J, et al. AMSTAR 2: a critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. BMJ. 2017;358:j4008.
Huang T, Balasubramanian R, Yao Y, Clish CB, Shadyab AH, Liu B, et al. Associations of depression status with plasma levels of candidate lipid and amino acid metabolites: a meta-analysis of individual data from three independent samples of US postmenopausal women. Mol Psychiatry. 2020;2020. https://doi.org/10.1038/s41380-020-00870-9 .
Culverhouse RC, Saccone NL, Horton AC, Ma Y, Anstey KJ, Banaschewski T, et al. Collaborative meta-analysis finds no evidence of a strong interaction between stress and 5-HTTLPR genotype contributing to the development of depression. Mol Psychiatry. 2018;23:133–42.
Little J, Higgins JPT, Ioannidis JPA, Moher D, Gagnon F, von Elm E, et al. STrengthening the REporting of Genetic Association Studies (STREGA)— An Extension of the STROBE Statement. PLoS Med. 2009;6:e1000022.
Guyatt GH, Oxman AD, Kunz R, Vist GE, Falck-Ytter Y, Schünemann HJ. What is quality of evidence and why is it important to clinicians? BMJ. 2008;336:995–8.
Yoon HS, Hattori K, Ogawa S, Sasayama D, Ota M, Teraishi T, et al. Relationships of cerebrospinal fluid monoamine metabolite levels with clinical variables in major depressive disorder. J Clin Psychiatry. 2017;78:e947–56.
Kugaya A, Seneca NM, Snyder PJ, Williams SA, Malison RT, Baldwin RM, et al. Changes in human in vivo serotonin and dopamine transporter availabilities during chronic antidepressant administration. Neuropsychopharmacology. 2003;28:413–20.
Border R, Johnson EC, Evans LM, Smolen A, Berley N, Sullivan PF, et al. No support for historical candidate gene or candidate gene-by-interaction hypotheses for major depression across multiple large samples. Am J Psychiatry. 2019;176:376–87.
Ogawa S, Tsuchimine S, Kunugi H. Cerebrospinal fluid monoamine metabolite concentrations in depressive disorder: A meta-analysis of historic evidence. J Psychiatr Res. 2018;105:137–46.
Nautiyal KM, Hen R. Serotonin receptors in depression: from A to B. F1000Res. 2017;6:123.
Rojas PS, Neira D, Muñoz M, Lavandero S, Fiedler JL. Serotonin (5‐HT) regulates neurite outgrowth through 5‐HT1A and 5‐HT7 receptors in cultured hippocampal neurons. J Neurosci Res. 2014;92:1000–9.
Kaufman J, DeLorenzo C, Choudhury S, Parsey RV. The 5-HT1A receptor in Major Depressive Disorder. Eur Neuropsychopharmacol. 2016;26:397–410.
Nikolaus S, Müller H-W, Hautzel H. Different patterns of 5-HT receptor and transporter dysfunction in neuropsychiatric disorders – a comparative analysis of in vivo imaging findings. Rev Neurosci. 2016;27:27–59.
Wang L, Zhou C, Zhu D, Wang X, Fang L, Zhong J, et al. Serotonin-1A receptor alterations in depression: A meta-analysis of molecular imaging studies. BMC Psychiatry. 2016;16:1–9.
Kambeitz JP, Howes OD. The serotonin transporter in depression: Meta-analysis of in vivo and post mortem findings and implications for understanding and treating depression. J Affect Disord. 2015;186:358–66.
Meyer JH. Imaging the serotonin transporter during major depressive disorder and antidepressant treatment. J Psychiatry Neurosci. 2007;32:86–102.
Mathews TA, Fedele DE, Coppelli FM, Avila AM, Murphy DL, Andrews AM. Gene dose-dependent alterations in extraneuronal serotonin but not dopamine in mice with reduced serotonin transporter expression. J Neurosci Methods. 2004;140:169–81.
Shen H-W, Hagino Y, Kobayashi H, Shinohara-Tanaka K, Ikeda K, Yamamoto H, et al. Regional differences in extracellular dopamine and serotonin assessed by in vivo microdialysis in mice lacking dopamine and/or serotonin transporters. Neuropsychopharmacology. 2004;29:1790–9.
Hagino Y, Takamatsu Y, Yamamoto H, Iwamura T, Murphy DL, Uhl GR, et al. Effects of MDMA on extracellular dopamine and serotonin levels in mice lacking dopamine and/or serotonin transporters. Curr Neuropharmacol. 2011;9:91–5.
Zhou Z, Zhen J, Karpowich NK, Law CJ, Reith MEA, Wang D-N. Antidepressant specificity of serotonin transporter suggested by three LeuT-SSRI structures. Nat Struct Mol Biol. 2009;16:652–7.
Gryglewski G, Lanzenberger R, Kranz GS, Cumming P. Meta-analysis of molecular imaging of serotonin transporters in major depression. J Cereb Blood Flow Metab. 2014;34:1096–103.
Benmansour S, Owens WA, Cecchi M, Morilak DA, Frazer A. Serotonin clearance in vivo is altered to a greater extent by antidepressant-induced downregulation of the serotonin transporter than by acute blockade of this transporter. J Neurosci. 2002;22:6766–72.
Benmansour S, Cecchi M, Morilak DA, Gerhardt GA, Javors MA, Gould GG, et al. Effects of chronic antidepressant treatments on serotonin transporter function, density, and mRNA level. J Neurosci. 1999;19:10494–501.
Horschitz S, Hummerich R, Schloss P. Down-regulation of the rat serotonin transporter upon exposure to a selective serotonin reuptake inhibitor. Neuroreport. 2001;12:2181–4.
Young SN. Acute tryptophan depletion in humans: a review of theoretical, practical and ethical aspects. J Psychiatry Neurosci. 2013;38:294–305.
Ruhe HG, Mason NS, Schene AH. Mood is indirectly related to serotonin, norepinephrine and dopamine levels in humans: a meta-analysis of monoamine depletion studies. Mol Psychiatry. 2007;12:331–59.
Fusar-Poli P, Allen P, McGuire P, Placentino A, Cortesi M, Perez J. Neuroimaging and electrophysiological studies of the effects of acute tryptophan depletion: A systematic review of the literature. Psychopharmacology. 2006;188:131–43.
Hogenelst K, Schoevers RA, Kema IP, Sweep FCGJ, aan het Rot M. Empathic accuracy and oxytocin after tryptophan depletion in adults at risk for depression. Psychopharmacology. 2016;233:111–20.
Weinstein JJ, Rogers BP, Taylor WD, Boyd BD, Cowan RL, Shelton KM, et al. Effects of acute tryptophan depletion on raphé functional connectivity in depression. Psychiatry Res. 2015;234:164–71.
Moreno FA, Erickson RP, Garriock HA, Gelernter J, Mintz J, Oas-Terpstra J, et al. Association study of genotype by depressive response during tryptophan depletion in subjects recovered from major depression. Mol. Neuropsychiatry. 2015;1:165–74.
Munafò MR. The serotonin transporter gene and depression. Depress Anxiety. 2012;29:915–7.
Caspi A, Sugden K, Moffitt TE, Taylor A, Craig IW, Harrington H, et al. Influence of life stress on depression: moderation by a polymorphism in the 5-HTT gene. Science 2003;301:386–9.
ADS CAS PubMed Google Scholar
Kiyohara C, Yoshimasu K. Association between major depressive disorder and a functional polymorphism of the 5-hydroxytryptamine (serotonin) transporter gene: A meta-analysis. Psychiatr Genet. 2010;20:49–58.
Oo KZ, Aung YK, Jenkins MA, Win AK. Associations of 5HTTLPR polymorphism with major depressive disorder and alcohol dependence: A systematic review and meta-analysis. Aust N. Z J Psychiatry. 2016;50:842–57.
Culverhouse RC, Bowes L, Breslau N, Nurnberger JI, Burmeister M, Fergusson DM, et al. Protocol for a collaborative meta-analysis of 5-HTTLPR, stress, and depression. BMC Psychiatry. 2013;13:1–12.
Karg K, Burmeister M, Shedden K, Sen S. The serotonin transporter promoter variant (5-HTTLPR), stress, and depression meta-analysis revisited. Arch Gen Psychiatry. 2011;68:444.
Sharpley CF, Palanisamy SKA, Glyde NS, Dillingham PW, Agnew LL. An update on the interaction between the serotonin transporter promoter variant (5-HTTLPR), stress and depression, plus an exploration of non-confirming findings. Behav Brain Res. 2014;273:89–105.
Bleys D, Luyten P, Soenens B, Claes S. Gene-environment interactions between stress and 5-HTTLPR in depression: A meta-analytic update. J Affect Disord. 2018;226:339–45.
Delgado PL. Monoamine depletion studies: implications for antidepressant discontinuation syndrome. J Clin Psychiatry. 2006;67:22–26.
Kemp JJ, Lickel JJ, Deacon BJ. Effects of a chemical imbalance causal explanation on individuals’ perceptions of their depressive symptoms. Behav Res Ther. 2014;56:47–52.
Lebowitz MS, Ahn W-K, Nolen-Hoeksema S. Fixable or fate? Perceptions of the biology of depression. J Consult Clin Psychol. 2013;81:518.
Zimmermann M, Papa A. Causal explanations of depression and treatment credibility in adults with untreated depression: Examining attribution theory. Psychol Psychother. 2020;93:537–54.
Maund E, Dewar-Haggart R, Williams S, Bowers H, Geraghty AWA, Leydon G, et al. Barriers and facilitators to discontinuing antidepressant use: A systematic review and thematic synthesis. J Affect Disord. 2019;245:38–62.
Eveleigh R, Speckens A, van Weel C, Oude Voshaar R, Lucassen P. Patients’ attitudes to discontinuing not-indicated long-term antidepressant use: barriers and facilitators. Therapeutic Advances in. Psychopharmacology. 2019;9:204512531987234.
Harrell FE Jr. Regression Modeling Strategies: With Applications to Linear Models, Logistic and Ordinal Regression, and Survival Analysis. Springer, Cham; 2015.
Schafer JL, Kang J. Average causal effects from nonrandomized studies: a practical guide and simulated example. Psychol Methods. 2008;13:279–313.
Pech J, Forman J, Kessing LV, Knorr U. Poor evidence for putative abnormalities in cerebrospinal fluid neurotransmitters in patients with depression versus healthy non-psychiatric individuals: A systematic review and meta-analyses of 23 studies. J Affect Disord. 2018;240:6–16.
Fava GA. May antidepressant drugs worsen the conditions they are supposed to treat? The clinical foundations of the oppositional model of tolerance. Therapeutic Adv Psychopharmacol. 2020;10:2045125320970325.
Kitaichi Y, Inoue T, Nakagawa S, Boku S, Kakuta A, Izumi T, et al. Sertraline increases extracellular levels not only of serotonin, but also of dopamine in the nucleus accumbens and striatum of rats. Eur J Pharm. 2010;647:90–6.
Gartside SE, Umbers V, Hajós M, Sharp T. Interaction between a selective 5‐HT1Areceptor antagonist and an SSRI in vivo: effects on 5‐HT cell firing and extracellular 5‐HT. Br J Pharmacol. 1995;115:1064–70.
Bosker FJ, Tanke MAC, Jongsma ME, Cremers TIFH, Jagtman E, Pietersen CY, et al. Biochemical and behavioral effects of long-term citalopram administration and discontinuation in rats: role of serotonin synthesis. Neurochem Int. 2010;57:948–57.
Download references
There was no specific funding for this review. MAH is supported by a Clinical Research Fellowship from North East London NHS Foundation Trust (NELFT). This funder had no role in study design, data collection, data analysis, data interpretation, or writing of the report.
Author information
Authors and affiliations.
Division of Psychiatry, University College London, London, UK
Joanna Moncrieff & Mark A. Horowitz
Research and Development Department, Goodmayes Hospital, North East London NHS Foundation Trust, Essex, UK
Faculty of Education, Health and Human Sciences, University of Greenwich, London, UK
- Ruth E. Cooper
Psychiatry-UK, Cornwall, UK
Tom Stockmann
Department of Dynamic and Clinical Psychology, and Health Studies, Faculty of Medicine and Psychology, Sapienza University of Rome, Rome, Italy
Simone Amendola
Department of Applied Psychology, Zurich University of Applied Sciences, Zurich, Switzerland
Michael P. Hengartner
You can also search for this author in PubMed Google Scholar
Contributions
JM conceived the idea for the study. JM, MAH, MPH, TS and SA designed the study. JM, MAH, MPH, TS, and SA screened articles and abstracted data. JM drafted the first version of the manuscript. JM, MAH, MPH, TS, SA, and REC contributed to the manuscript’s revision and interpretation of findings. All authors had full access to all the data in the study and had final responsibility for the decision to submit for publication.
Corresponding author
Correspondence to Joanna Moncrieff .
Ethics declarations
Competing interests.
All authors have completed the Unified Competing Interest form at http://www.icmje.org/coi_disclosure.pdf (available on request from the corresponding author). SA declares no conflicts of interest. MAH reports being co-founder of a company in April 2022, aiming to help people safely stop antidepressants in Canada. MPH reports royalties from Palgrave Macmillan, London, UK for his book published in December, 2021, called “Evidence-biased Antidepressant Prescription.” JM receives royalties for books about psychiatric drugs, reports grants from the National Institute of Health Research outside the submitted work, that she is co-chairperson of the Critical Psychiatry Network (an informal group of psychiatrists) and a board member of the unfunded organisation, the Council for Evidence-based Psychiatry. Both are unpaid positions. TS is co-chairperson of the Critical Psychiatry Network. RC is an unpaid board member of the International Institute for Psychiatric Drug Withdrawal.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Supplementary tables, rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Moncrieff, J., Cooper, R.E., Stockmann, T. et al. The serotonin theory of depression: a systematic umbrella review of the evidence. Mol Psychiatry 28 , 3243–3256 (2023). https://doi.org/10.1038/s41380-022-01661-0
Download citation
Received : 21 June 2021
Revised : 31 May 2022
Accepted : 07 June 2022
Published : 20 July 2022
Issue Date : August 2023
DOI : https://doi.org/10.1038/s41380-022-01661-0
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
This article is cited by
The involvement of serotonin in major depression: nescience in disguise.
- Danilo Arnone
- Catherine J. Harmer
Molecular Psychiatry (2024)
Serotonin effects on human iPSC-derived neural cell functions: from mitochondria to depression
- Iseline Cardon
- Sonja Grobecker
- Christian H. Wetzel
Neither serotonin disorder is at the core of depression nor dopamine at the core of schizophrenia; still these are biologically based mental disorders
- Konstantinos N. Fountoulakis
- Eva Maria Tsapakis
The impact of adult neurogenesis on affective functions: of mice and men
- Mariana Alonso
- Anne-Cécile Petit
- Pierre-Marie Lledo
Difficult lives explain depression better than broken brains
- Joanna Moncrieff
- Mark A. Horowitz
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Change Password
Your password must have 8 characters or more and contain 3 of the following:.
- a lower case character,
- an upper case character,
- a special character
Password Changed Successfully
Your password has been changed
- Sign in / Register
Request Username
Can't sign in? Forgot your username?
Enter your email address below and we will send you your username
If the address matches an existing account you will receive an email with instructions to retrieve your username
An Exploratory Study of Students with Depression in Undergraduate Research Experiences
- Katelyn M. Cooper
- Logan E. Gin
- M. Elizabeth Barnes
- Sara E. Brownell
*Address correspondence to: Katelyn M. Cooper ( E-mail Address: [email protected] ).
Department of Biology, University of Central Florida, Orlando, FL, 32816
Search for more papers by this author
Biology Education Research Lab, Research for Inclusive STEM Education Center, School of Life Sciences, Arizona State University, Tempe, AZ 85281
Depression is a top mental health concern among undergraduates and has been shown to disproportionately affect individuals who are underserved and underrepresented in science. As we aim to create a more inclusive scientific community, we argue that we need to examine the relationship between depression and scientific research. While studies have identified aspects of research that affect graduate student depression, we know of no studies that have explored the relationship between depression and undergraduate research. In this study, we sought to understand how undergraduates’ symptoms of depression affect their research experiences and how research affects undergraduates’ feelings of depression. We interviewed 35 undergraduate researchers majoring in the life sciences from 12 research-intensive public universities across the United States who identify with having depression. Using inductive and deductive coding, we identified that students’ depression affected their motivation and productivity, creativity and risk-taking, engagement and concentration, and self-perception and socializing in undergraduate research experiences. We found that students’ social connections, experiencing failure in research, getting help, receiving feedback, and the demands of research affected students’ depression. Based on this work, we articulate an initial set of evidence-based recommendations for research mentors to consider in promoting an inclusive research experience for students with depression.
INTRODUCTION
Depression is described as a common and serious mood disorder that results in persistent feelings of sadness and hopelessness, as well as a loss of interest in activities that one once enjoyed ( American Psychiatric Association [APA], 2013 ). Additional symptoms of depression include weight changes, difficulty sleeping, loss of energy, difficulty thinking or concentrating, feelings of worthlessness or excessive guilt, and suicidality ( APA, 2013 ). While depression results from a complex interaction of psychological, social, and biological factors ( World Health Organization, 2018 ), studies have shown that increased stress caused by college can be a significant contributor to student depression ( Dyson and Renk, 2006 ).
Depression is one of the top undergraduate mental health concerns, and the rate of depression among undergraduates continues to rise ( Center for Collegiate Mental Health, 2017 ). While we cannot discern whether these increasing rates of depression are due to increased awareness or increased incidence, it is clear that is a serious problem on college campuses. The percent of U.S. college students who self-reported a diagnosis with depression was recently estimated to be about 25% ( American College Health Association, 2019 ). However, higher rates have been reported, with one study estimating that up to 84% of undergraduates experience some level of depression ( Garlow et al. , 2008 ). Depression rates are typically higher among university students compared with the general population, despite being a more socially privileged group ( Ibrahim et al. , 2013 ). Prior studies have found that depression is negatively correlated with overall undergraduate academic performance ( Hysenbegasi et al. , 2005 ; Deroma et al. , 2009 ; American College Health Association, 2019 ). Specifically, diagnosed depression is associated with half a letter grade decrease in students’ grade point average ( Hysenbegasi et al. , 2005 ), and 21.6% of undergraduates reported that depression negatively affected their academic performance within the last year ( American College Health Association, 2019 ). Provided with a list of academic factors that may be affected by depression, students reported that depression contributed to lower exam grades, lower course grades, and not completing or dropping a course.
Students in the natural sciences may be particularly at risk for depression, given that such majors are noted to be particularly stressful due to their competitive nature and course work that is often perceived to “weed students out”( Everson et al. , 1993 ; Strenta et al. , 1994 ; American College Health Association, 2019 ; Seymour and Hunter, 2019 ). Science course instruction has also been described to be boring, repetitive, difficult, and math-intensive; these factors can create an environment that can trigger depression ( Seymour and Hewitt, 1997 ; Osborne and Collins, 2001 ; Armbruster et al ., 2009 ; Ceci and Williams, 2010 ). What also distinguishes science degree programs from other degree programs is that, increasingly, undergraduate research experiences are being proposed as an essential element of a science degree ( American Association for the Advancement of Science, 2011 ; President’s Council of Advisors on Science and Technology, 2012 ; National Academies of Sciences, Engineering, and Medicine [NASEM], 2017 ). However, there is some evidence that undergraduate research experiences can add to the stress of college for some students ( Cooper et al. , 2019c ). Students can garner multiple benefits from undergraduate research, including enhanced abilities to think critically ( Ishiyama, 2002 ; Bauer and Bennett, 2003 ; Brownell et al. , 2015 ), improved student learning ( Rauckhorst et al. , 2001 ; Brownell et al. , 2015 ), and increased student persistence in undergraduate science degree programs ( Jones et al. , 2010 ; Hernandez et al. , 2018 ). Notably, undergraduate research experiences are increasingly becoming a prerequisite for entry into medical and graduate programs in science, particularly elite programs ( Cooper et al. , 2019d ). Although some research experiences are embedded into formal lab courses as course-based undergraduate research experiences (CUREs; Auchincloss et al. , 2014 ; Brownell and Kloser, 2015 ), the majority likely entail working with faculty in their research labs. These undergraduate research experiences in faculty labs are often added on top of a student’s normal course work, so they essentially become an extracurricular activity that they have to juggle with course work, working, and/or personal obligations ( Cooper et al. , 2019c ). While the majority of the literature surrounding undergraduate research highlights undergraduate research as a positive experience ( NASEM, 2017 ), studies have demonstrated that undergraduate research experiences can be academically and emotionally challenging for students ( Mabrouk and Peters, 2000 ; Seymour et al. , 2004 ; Cooper et al. , 2019c ; Limeri et al. , 2019 ). In fact, 50% of students sampled nationally from public R1 institutions consider leaving their undergraduate research experience prematurely, and about half of those students, or 25% of all students, ultimately leave their undergraduate research experience ( Cooper et al. , 2019c ). Notably, 33.8% of these individuals cited a negative lab environment and 33.3% cited negative relationships with their mentors as factors that influenced their decision about whether to leave ( Cooper et al. , 2019c ). Therefore, students’ depression may be exacerbated in challenging undergraduate research experiences, because studies have shown that depression is positively correlated with student stress ( Hish et al. , 2019 ).
While depression has not been explored in the context of undergraduate research experiences, depression has become a prominent concern surrounding graduate students conducting scientific research. A recent study that examined the “graduate student mental health crisis” ( Flaherty, 2018 ) found that work–life balance and graduate students’ relationships with their research advisors may be contributing to their depression ( Evans et al. , 2018 ). Specifically, this survey of 2279 PhD and master’s students from diverse fields of study, including the biological/physical sciences, showed that 39% of graduate students have experienced moderate to severe depression. Fifty-five percent of the graduate students with depression who were surveyed disagreed with the statement “I have good work life balance,” compared to only 21% of students with depression who agreed. Additionally, the study highlighted that more students with depression disagreed than agreed with the following statements: their advisors provided “real” mentorship, their advisors provided ample support, their advisors positively impacted their emotional or mental well-being, their advisors were assets to their careers, and they felt valued by their mentors. Another recent study identified that depression severity in biomedical doctoral students was significantly associated with graduate program climate, a perceived lack of employment opportunities, and the quality of students’ research training environment ( Nagy et al. , 2019 ). Environmental stress, academic stress, and family and monetary stress have also been shown to be predictive of depression severity in biomedical doctoral students ( Hish et al. , 2019 ). Further, one study found that self-esteem is negatively correlated and stress is positively correlated with graduate student depression; presumably research environments that challenge students’ self-esteem and induce stress are likely contributing to depressive symptoms among graduate students ( Kreger, 1995 ). While these studies have focused on graduate students, and there are certainly notable distinctions between graduate and undergraduate research, the research-related factors that affect graduate student depression, including work–life balance, relationships with mentors, research environment, stress, and self-esteem, may also be relevant to depression among undergraduates conducting research. Importantly, undergraduates in the United States have reported identical levels of depression as graduate students but are often less likely to seek mental health care services ( Wyatt and Oswalt, 2013 ), which is concerning if undergraduate research experiences exacerbate depression.
Based on the literature on the stressors of undergraduate research experiences and the literature identifying some potential causes of graduate student depression, we identified three aspects of undergraduate research that may exacerbate undergraduates’ depression. Mentoring: Mentors can be an integral part of a students’ research experience, bolstering their connections with others in the science community, scholarly productivity, and science identity, as well as providing many other benefits ( Thiry and Laursen, 2011 ; Prunuske et al. , 2013 ; Byars-Winston et al. , 2015 ; Aikens et al. , 2016 , 2017 ; Thompson et al. , 2016 ; Estrada et al. , 2018 ). However, recent literature has highlighted that poor mentoring can negatively affect undergraduate researchers ( Cooper et al. , 2019c ; Limeri et al. , 2019 ). Specifically, one study of 33 undergraduate researchers who had conducted research at 10 institutions identified seven major ways that they experienced negative mentoring, which included absenteeism, abuse of power, interpersonal mismatch, lack of career support, lack of psychosocial support, misaligned expectations, and unequal treatment ( Limeri et al. , 2019 ). We hypothesize negative mentoring experiences may be particularly harmful for students with depression, because support, particularly social support, has been shown to be important for helping individuals with depression cope with difficult circumstances ( Aneshensel and Stone, 1982 ; Grav et al. , 2012 ). Failure: Experiencing failure has been hypothesized to be an important aspect of undergraduate research experiences that may help students develop some the most distinguishing abilities of outstanding scientists, such as coping with failure, navigating challenges, and persevering ( Laursen et al. , 2010 ; Gin et al. , 2018 ; Henry et al. , 2019 ). However, experiencing failure and the stress and fatigue that often accompany it may be particularly tough for students with depression ( Aldwin and Greenberger, 1987 ; Mongrain and Blackburn, 2005 ). Lab environment: Fairness, inclusion/exclusion, and social support within one’s organizational environment have been shown to be key factors that cause people to either want to remain in the work place and be productive or to want to leave ( Barak et al. , 2006 ; Cooper et al. , 2019c ). We hypothesize that dealing with exclusion or a lack of social support may exacerbate depression for some students; patients with clinical depression react to social exclusion with more pronounced negative emotions than do individuals without clinical depression ( Jobst et al. , 2015 ). While there are likely other aspects of undergraduate research that affect student depression, we hypothesize that these factors have the potential to exacerbate negative research experiences for students with depression.
Depression has been shown to disproportionately affect many populations that are underrepresented or underserved within the scientific community, including females ( American College Health Association, 2018 ; Evans et al. , 2018 ), first-generation college students ( Jenkins et al. , 2013 ), individuals from low socioeconomic backgrounds ( Eisenberg et al. , 2007 ), members of the LGBTQ+ community ( Eisenberg et al. , 2007 ; Evans et al. , 2018 ), and people with disabilities ( Turner and Noh, 1988 ). Therefore, as the science community strives to be more diverse and inclusive ( Intemann, 2009 ), it is important that we understand more about the relationship between depression and scientific research, because negative experiences with depression in scientific research may be contributing to the underrepresentation of these groups. Specifically, more information is needed about how the research process and environment of research experiences may affect depression.
Given the high rate of depression among undergraduates, the links between depression and graduate research, the potentially challenging environment of undergraduate research, and how depression could disproportionately impact students from underserved communities, it is imperative to begin to explore the relationship between scientific research and depression among undergraduates to create research experiences that could maximize student success. In this exploratory interview study, we aimed to 1) describe how undergraduates’ symptoms of depression affect their research experiences, 2) understand how undergraduate research affects students’ feelings of depression, and 3) identify recommendations based on the literature and undergraduates’ reported experiences to promote a positive research experience for students with depression.
This study was done with an approved Arizona State University Institutional Review Board protocol #7247.
In Fall 2018, we surveyed undergraduate researchers majoring in the life sciences across 25 research-intensive (R1) public institutions across the United States (specific details about the recruitment of the students who completed the survey can be found in Cooper et al. (2019c) ). The survey asked students for their opinions about their undergraduate research experiences and their demographic information and whether they would be interested in participating in a follow-up interview related to their research experiences. For the purpose of this study, we exclusively interviewed students about their undergraduate research experiences in faculty member labs; we did not consider students’ experiences in CUREs. Of the 768 undergraduate researchers who completed the survey, 65% ( n = 496) indicated that they would be interested in participating in a follow-up interview. In Spring 2019, we emailed the 496 students, explaining that we were interested in interviewing students with depression about their experiences in undergraduate research. Our specific prompt was: “If you identify as having depression, we would be interested in hearing about your experience in undergraduate research in a 30–60 minute online interview.” We did not define depression in our email recruitment because we conducted think-aloud interviews with four undergraduates who all correctly interpreted what we meant by depression ( APA, 2013 ). We had 35 students agree to participate in the interview study. The interview participants represented 12 of the 25 R1 public institutions that were represented in the initial survey.
Student Interviews
We developed an interview script to explore our research questions. Specifically, we were interested in how students’ symptoms of depression affect their research experiences, how undergraduate research negatively affects student depression, and how undergraduate research positively affects student depression.
We recognized that mental health, and specifically depression, can be a sensitive topic to discuss with undergraduates, and therefore we tried to minimize any discomfort that the interviewees might experience during the interview. Specifically, we conducted think-aloud interviews with three graduate students who self-identified with having depression at the time of the interview. We asked them to note whether any interview questions made them uncomfortable. We also sought their feedback on questions given their experiences as persons with depression who had once engaged in undergraduate research. We revised the interview protocol after each think-aloud interview. Next, we conducted four additional think-aloud interviews with undergraduates conducting basic science or biology education research who identified with having depression to establish cognitive validity of the questions and to elicit additional feedback about any questions that might make someone uncomfortable. The questions were revised after each think-aloud interview until no question was unclear or misinterpreted by the students and we were confident that the questions minimized students’ potential discomfort ( Trenor et al. , 2011 ). A copy of the final interview script can be found in the Supplemental Material.
All interviews were individually conducted by one of two researchers (K.M.C. and L.E.G.) who conducted the think-aloud interviews together to ensure that their interviewing practices were as similar as possible. The interviews were approximately an hour long, and students received a $15 gift card for their participation.
Personal, Research, and Depression Demographics
All student demographics and information about students’ research experiences were collected using the survey distributed to students in Fall 2018. We collected personal demographics, including the participants’ gender, race/ethnicity, college generation status, transfer status, financial stability, year in college, major, and age. We also collected information about the students’ research experiences, including the length of their first research experiences, the average number of hours they spend in research per week, how they were compensated for research, who their primary mentors were, and the focus areas of their research.
In the United States, mental healthcare is disproportionately unavailable to Black and Latinx individuals, as well as those who come from low socioeconomic backgrounds ( Kataoka et al. , 2002 ; Howell and McFeeters, 2008 ; Santiago et al. , 2013 ). Therefore, to minimize a biased sample, we invited anyone who identified with having depression to participate in our study; we did not require students to be diagnosed with depression or to be treated for depression in order to participate. However, we did collect information about whether students had been formally diagnosed with depression and whether they had been treated for depression. After the interview, all participants were sent a link to a short survey that asked them if they had ever been diagnosed with depression and how, if at all, they had ever been treated for depression. A copy of these survey questions can be found in the Supplemental Material. The combined demographic information of the participants is in Table 1 . The demographics for each individual student can be found in the Supplemental Material.
a Students reported the time they had spent in research 6 months before being interviewed and only reported on the length of time of their first research experiences.
b Students were invited to report multiple ways in which they were treated for their depression; other treatments included lifestyle changes and meditation.
c Students were invited to report multiple means of compensation for their research if they had been compensated for their time in different ways.
d Students were asked whether they felt financially stable, particularly during the undergraduate research experience.
e Students reported who they work/worked with most closely during their research experiences.
f Staff members included lab coordinators or lab managers.
g Other focus areas of research included sociology, linguistics, psychology, and public health.
Interview Analysis
The initial interview analysis aimed to explore each idea that a participant expressed ( Charmaz, 2006 ) and to identify reoccurring ideas throughout the interviews. First, three authors (K.M.C., L.E.G., and S.E.B.) individually reviewed a different set of 10 interviews and took detailed analytic notes ( Birks and Mills, 2015 ). Afterward, the authors compared their notes and identified reoccurring themes throughout the interviews using open coding methods ( Saldaña, 2015 ).
Once an initial set of themes was established, two researchers (K.M.C. and L.E.G.) individually reviewed the same set of 15 randomly selected interviews to validate the themes identified in the initial analysis and to screen for any additional themes that the initial analysis may have missed. Each researcher took detailed analytic notes throughout the review of an interview, which they discussed after reviewing each interview. The researchers compared what quotes from each interview they categorized into each theme. Using constant comparison methods, they assigned quotes to each theme and constantly compared the quotes to ensure that each quote fit within the description of the theme ( Glesne and Peshkin, 1992 ). In cases in which quotes were too different from other quotes, a new theme was created. This approach allowed for multiple revisions of the themes and allowed the authors to define a final set of codes; the researchers created a final codebook with refined definitions of emergent themes (the final coding rubric can be found in the Supplemental Material). Once the final codebook was established, the researchers (K.M.C. and L.E.G.) individually coded seven additional interviews (20% of all interviews) using the coding rubric. The researchers compared their codes, and their Cohen’s κ interrater score for these seven interviews was at an acceptable level (κ = 0.88; Landis and Koch, 1977 ). One researcher (L.E.G.) coded the remaining 28 out of 35 interviews. The researchers determined that data saturation had been reached with the current sample and no further recruitment was needed ( Guest et al. , 2006 ). We report on themes that were mentioned by at least 20% of students in the interview study. In the Supplemental Material, we provide the final coding rubric with the number of participants whose interview reflected each theme ( Hannah and Lautsch, 2011 ). Reporting the number of individuals who reported themes within qualitative data can lead to inaccurate conclusions about the generalizability of the results to a broader population. These qualitative data are meant to characterize a landscape of experiences that students with depression have in undergraduate research rather than to make claims about the prevalence of these experiences ( Glesne and Peshkin, 1992 ). Because inferences about the importance of these themes cannot be drawn from these counts, they are not included in the results of the paper ( Maxwell, 2010 ). Further, the limited number of interviewees made it not possible to examine whether there were trends based on students’ demographics or characteristics of their research experiences (e.g., their specific area of study). Quotes were lightly edited for clarity by inserting clarification brackets and using ellipses to indicate excluded text. Pseudonyms were given to all students to protect their privacy.
The Effect of Depressive Symptoms on Undergraduate Research
We asked students to describe the symptoms associated with their depression. Students described experiencing anxiety that is associated with their depression; this could be anxiety that precedes their depression or anxiety that results from a depressive episode or a period of time when an individual has depression symptoms. Further, students described difficulty getting out of bed or leaving the house, feeling tired, a lack of motivation, being overly self-critical, feeling apathetic, and having difficulty concentrating. We were particularly interested in how students’ symptoms of depression affected their experiences in undergraduate research. During the think-aloud interviews that were conducted before the interview study, graduate and undergraduate students consistently described that their depression affected their motivation in research, their creativity in research, and their productivity in research. Therefore, we explicitly asked undergraduate researchers how, if at all, their depression affected these three factors. We also asked students to describe any additional ways in which their depression affected their research experiences. Undergraduate researchers commonly described five additional ways in which their depression affected their research; for a detailed description of each way students’ research was affected and for example quotes, see Table 2 . Students described that their depression negatively affected their productivity in the lab. Commonly, students described that their productivity was directly affected by a lack of motivation or because they felt less creative, which hindered the research process. Additionally, students highlighted that they were sometimes less productive because their depression sometimes caused them to struggle to engage intellectually with their research or caused them to have difficulty remembering or concentrating; students described that they could do mundane or routine tasks when they felt depressed, but that they had difficulty with more complex and intellectually demanding tasks. However, students sometimes described that even mundane tasks could be difficult when they were required to remember specific steps; for example, some students struggled recalling a protocol from memory when their depression was particularly severe. Additionally, students noted that their depression made them more self-conscious, which sometimes held them back from sharing research ideas with their mentors or from taking risks such as applying to competitive programs. In addition to being self-conscious, students highlighted that their depression caused them to be overly self-critical, and some described experiencing imposter phenomenon ( Clance and Imes, 1978 ) or feeling like they were not talented enough to be in research and were accepted into a lab by a fluke or through luck. Finally, students described that depression often made them feel less social, and they struggled to socially engage with other members of the lab when they were feeling down.
The Effect of Undergraduate Research Experiences on Student Depression
We also wanted to explore how research impacted students’ feelings of depression. Undergraduates described how research both positively and negatively affected their depression. In the following sections, we present aspects of undergraduate research and examine how each positively and/or negatively affected students’ depression using embedded student quotes to highlight the relationships between related ideas.
Lab Environment: Relationships with Others in the Lab.
Some aspects of the lab environment, which we define as students’ physical, social, or psychological research space, could be particularly beneficial for students with depression.
Specifically, undergraduate researchers perceived that comfortable and positive social interactions with others in the lab helped their depression. Students acknowledged how beneficial their relationships with graduate students and postdocs could be.
Marta: “I think always checking in on undergrads is important. It’s really easy [for us] to go a whole day without talking to anybody in the lab. But our grad students are like ‘Hey, what’s up? How’s school? What’s going on?’ (…) What helps me the most is having that strong support system. Sometimes just talking makes you feel better, but also having people that believe in you can really help you get out of that negative spiral. I think that can really help with depression.”
Kelley: “I know that anytime I need to talk to [my postdoc mentors] about something they’re always there for me. Over time we’ve developed a relationship where I know that outside of work and outside of the lab if I did want to talk to them about something I could talk to them. Even just talking to someone about hobbies and having that relationship alone is really helpful [for depression].”
In addition to highlighting the importance of developing relationships with graduate students or postdocs in the lab, students described that forming relationships with other undergraduates in the lab also helped their depression. Particularly, students described that other undergraduate researchers often validated their feelings about research, which in turn helped them realize that what they are thinking or feeling is normal, which tended to alleviate their negative thoughts. Interestingly, other undergraduates experiencing the same issues could sometimes help buffer them from perceiving that a mentor did not like them or that they were uniquely bad at research. In this article, we use the term “mentor” to refer to anyone who students referred to in the interviews as being their mentors or managing their research experiences; this includes graduate students, postdoctoral scholars, lab managers, and primary investigators (PIs).
Abby: “One of my best friends is in the lab with me. A lot of that friendship just comes from complaining about our stress with the lab and our annoyance with people in the lab. Like when we both agree like, ‘Yeah, the grad students were really off today, it wasn’t us,’ that helps. ‘It wasn’t me, it wasn’t my fault that we were having a rough day in lab; it was the grad students.’ Just being able to realize, ‘Hey, this isn’t all caused by us,’ you know? (…) We understand the stresses in the lab. We understand the details of what each other are doing in the lab, so when something doesn’t work out, we understand that it took them like eight hours to do that and it didn’t work. We provide empathy on a different level.”
Meleana: “It’s great to have solidarity in being confused about something, and it’s just that is a form of validation for me too. When we leave a lab meeting and I look at [another undergrad] I’m like, ‘Did you understand anything that they were just saying?’ And they’re like, ‘Oh, no.’ (…) It’s just really validating to hear from the other undergrads that we all seem to be struggling with the same things.”
Developing positive relationships with faculty mentors or PIs also helped alleviate some students’ depressive feelings, particularly when PIs shared their own struggles with students. This also seemed to normalize students’ concerns about their own experiences.
Alexandra: “[Talking with my PI] is helpful because he would talk about his struggles, and what he faced. A lot of it was very similar to my struggles. For example, he would say, ‘Oh, yeah, I failed this exam that I studied so hard for. I failed the GRE and I paid so much money to prepare for it.’ It just makes [my depression] better, like okay, this is normal for students to go through this. It’s not an out of this world thing where if you fail, you’re a failure and you can’t move on from it.”
Students’ relationships with others in the lab did not always positively impact their depression. Students described instances when the negative moods of the graduate students and PIs would often set the tone of the lab, which in turn worsened the mood of the undergraduate researchers.
Abby: “Sometimes [the grad students] are not in a good mood. The entire vibe of the lab is just off, and if you make a joke and it hits somebody wrong, they get all mad. It really depends on the grad students and the leadership and the mood that they’re in.”
Interviewer: “How does it affect your depression when the grad students are in a bad mood?”
Abby: “It definitely makes me feel worse. It feels like, again, that I really shouldn’t go ask them for help because they’re just not in the mood to help out. It makes me have more pressure on myself, and I have deadlines I need to meet, but I have a question for them, but they’re in a bad mood so I can’t ask. That’s another day wasted for me and it just puts more stress, which just adds to the depression.”
Additionally, some students described even more concerning behavior from research mentors, which negatively affected their depression.
Julie: “I had a primary investigator who is notorious in the department for screaming at people, being emotionally abusive, unreasonable, et cetera. (…) [He was] kind of harassing people, demeaning them, lying to them, et cetera, et cetera. (…) Being yelled at and constantly demeaned and harassed at all hours of the day and night, that was probably pretty bad for me.”
While the relationships between undergraduates and graduate, postdoc, and faculty mentors seemed to either alleviate or worsen students’ depressive symptoms, depending on the quality of the relationship, students in this study exclusively described their relationships with other undergraduates as positive for their depression. However, students did note that undergraduate research puts some of the best and brightest undergraduates in the same environment, which can result in students comparing themselves with their peers. Students described that this comparison would often lead them to feel badly about themselves, even though they would describe their personal relationship with a person to be good.
Meleana: “In just the research field in general, just feeling like I don’t really measure up to the people around me [can affect my depression]. A lot of the times it’s the beginning of a little spiral, mental spiral. There are some past undergrads that are talked about as they’re on this pedestal of being the ideal undergrads and that they were just so smart and contributed so much to the lab. I can never stop myself from wondering like, ‘Oh, I wonder if I’m having a contribution to the lab that’s similar or if I’m just another one of the undergrads that does the bare minimum and passes through and is just there.’”
Natasha: “But, on the other hand, [having another undergrad in the lab] also reminded me constantly that some people are invested in this and meant to do this and it’s not me. And that some people know a lot more than I do and will go further in this than I will.”
While students primarily expressed that their relationships with others in the lab affected their depression, some students explained that they struggled most with depression when the lab was empty; they described that they did not like being alone in the lab, because a lack of stimulation allowed their minds to be filled with negative thoughts.
Mia: “Those late nights definitely didn’t help [my depression]. I am alone, in the entire building. I’m left alone to think about my thoughts more, so not distracted by talking to people or interacting with people. I think more about how I’m feeling and the lack of progress I’m making, and the hopelessness I’m feeling. That kind of dragged things on, and I guess deepened my depression.”
Freddy: “Often times when I go to my office in the evening, that is when I would [ sic ] be prone to be more depressed. It’s being alone. I think about myself or mistakes or trying to correct mistakes or whatever’s going on in my life at the time. I become very introspective. I think I’m way too self-evaluating, way too self-deprecating and it’s when I’m alone when those things are really, really triggered. When I’m talking with somebody else, I forget about those things.”
In sum, students with depression highlighted that a lab environment full of positive and encouraging individuals was helpful for their depression, whereas isolating or competitive environments and negative interactions with others often resulted in more depressive feelings.
Doing Science: Experiencing Failure in Research, Getting Help, Receiving Feedback, Time Demands, and Important Contributions.
In addition to the lab environment, students also described that the process of doing science could affect their depression. Specifically, students explained that a large contributor to their depression was experiencing failure in research.
Interviewer: “Considering your experience in undergraduate research, what tends to trigger your feelings of depression?”
Heather: “Probably just not getting things right. Having to do an experiment over and over again. You don’t get the results you want. (…) The work is pretty meticulous and it’s frustrating when I do all this work, I do a whole experiment, and then I don’t get any results that I can use. That can be really frustrating. It adds to the stress. (…) It’s hard because you did all this other stuff before so you can plan for the research, and then something happens and all the stuff you did was worthless basically.”
Julie: “I felt very negatively about myself [when a project failed] and pretty panicked whenever something didn’t work because I felt like it was a direct reflection on my effort and/or intelligence, and then it was a big glaring personal failure.”
Students explained that their depression related to failing in research was exacerbated if they felt as though they could not seek help from their research mentors. Perceived insufficient mentor guidance has been shown to be a factor influencing student intention to leave undergraduate research ( Cooper et al. , 2019c ). Sometimes students talked about their research mentors being unavailable or unapproachable.
Michelle: “It just feels like [the graduate students] are not approachable. I feel like I can’t approach them to ask for their understanding in a certain situation. It makes [my depression] worse because I feel like I’m stuck, and that I’m being limited, and like there’s nothing I can do. So then I kind of feel like it’s my fault that I can’t do anything.”
Other times, students described that they did not seek help in fear that they would be negatively evaluated in research, which is a fear of being judged by others ( Watson and Friend, 1969 ; Weeks et al. , 2005 ; Cooper et al. , 2018 ). That is, students fear that their mentor would think negatively about them or judge them if they were to ask questions that their mentor thought they should know the answer to.
Meleana: “I would say [my depression] tends to come out more in being more reserved in asking questions because I think that comes more like a fear-based thing where I’m like, ‘Oh, I don’t feel like I’m good enough and so I don’t want to ask these questions because then my mentors will, I don’t know, think that I’m dumb or something.’”
Conversely, students described that mentors who were willing to help them alleviated their depressive feelings.
Crystal: “Yeah [my grad student] is always like, ‘Hey, I can check in on things in the lab because you’re allowed to ask me for that, you’re not totally alone in this,’ because he knows that I tend to take on all this responsibility and I don’t always know how to ask for help. He’s like, ‘You know, this is my lab too and I am here to help you as well,’ and just reminds me that I’m not shouldering this burden by myself.”
Ashlyn: “The graduate student who I work with is very kind and has a lot of patience and he really understands a lot of things and provides simple explanations. He does remind me about things and he will keep on me about certain tasks that I need to do in an understanding way, and it’s just because he’s patient and he listens.”
In addition to experiencing failure in science, students described that making mistakes when doing science also negatively affected their depression.
Abby: “I guess not making mistakes on experiments [is important in avoiding my depression]. Not necessarily that your experiment didn’t turn out to produce the data that you wanted, but just adding the wrong enzyme or messing something up like that. It’s like, ‘Oh, man,’ you know? You can get really down on yourself about that because it can be embarrassing.”
Commonly, students described that the potential for making mistakes increased their stress and anxiety regarding research; however, they explained that how other people responded to a potential mistake was what ultimately affected their depression.
Briana: “Sometimes if I made a mistake in correctly identifying an eye color [of a fly], [my PI] would just ridicule me in front of the other students. He corrected me but his method of correcting was very discouraging because it was a ridicule. It made the others laugh and I didn’t like that.”
Julie: “[My PI] explicitly [asked] if I had the dedication for science. A lot of times he said I had terrible judgment. A lot of times he said I couldn’t be trusted. Once I went to a conference with him, and, unfortunately, in front of another professor, he called me a klutz several times and there was another comment about how I never learn from my mistakes.”
When students did do things correctly, they described how important it could be for them to receive praise from their mentors. They explained that hearing praise and validation can be particularly helpful for students with depression, because their thoughts are often very negative and/or because they have low self-esteem.
Crystal: “[Something that helps my depression is] I have text messages from [my graduate student mentor] thanking me [and another undergraduate researcher] for all of the work that we’ve put in, that he would not be able to be as on track to finish as he is if he didn’t have our help.”
Interviewer: “Why is hearing praise from your mentor helpful?”
Crystal: “Because a lot of my depression focuses on everybody secretly hates you, nobody likes you, you’re going to die alone. So having that validation [from my graduate mentor] is important, because it flies in the face of what my depression tells me.”
Brian: “It reminds you that you exist outside of this negative world that you’ve created for yourself, and people don’t see you how you see yourself sometimes.”
Students also highlighted how research could be overwhelming, which negatively affected their depression. Particularly, students described that research demanded a lot of their time and that their mentors did not always seem to be aware that they were juggling school and other commitments in addition to their research. This stress exacerbated their depression.
Rose: “I feel like sometimes [my grad mentors] are not very understanding because grad students don’t take as many classes as [undergrads] do. I think sometimes they don’t understand when I say I can’t come in at all this week because I have finals and they’re like, ‘Why though?’”
Abby: “I just think being more understanding of student life would be great. We have classes as well as the lab, and classes are the priority. They forget what it’s like to be a student. You feel like they don’t understand and they could never understand when you say like, ‘I have three exams this week,’ and they’re like, ‘I don’t care. You need to finish this.’”
Conversely, some students reported that their research labs were very understanding of students’ schedules. Interestingly, these students talked most about how helpful it was to be able to take a mental health day and not do research on days when they felt down or depressed.
Marta: “My lab tech is very open, so she’ll tell us, ‘I can’t come in today. I have to take a mental health day.’ So she’s a really big advocate for that. And I think I won’t personally tell her that I’m taking a mental health day, but I’ll say, ‘I can’t come in today, but I’ll come in Friday and do those extra hours.’ And she’s like, ‘OK great, I’ll see you then.’ And it makes me feel good, because it helps me take care of myself first and then I can take care of everything else I need to do, which is amazing.”
Meleana: “Knowing that [my mentors] would be flexible if I told them that I’m crazy busy and can’t come into work nearly as much this week [helps my depression]. There is flexibility in allowing me to then care for myself.”
Interviewer: “Why is the flexibility helpful given the depression?”
Meleana: “Because sometimes for me things just take a little bit longer when I’m feeling down. I’m just less efficient to be honest, and so it’s helpful if I feel like I can only go into work for 10 hours in a week. It declutters my brain a little bit to not have to worry about all the things I have to do in work in addition the things that I need to do for school or clubs, or family or whatever.”
Despite the demanding nature of research, a subset of students highlighted that their research and research lab provided a sense of stability or familiarity that distracted them from their depression.
Freddy: “I’ll [do research] to run away from those [depressive] feelings or whatever. (…) I find sadly, I hate to admit it, but I do kind of run to [my lab]. I throw myself into work to distract myself from the feelings of depression and sadness.”
Rose: “When you’re sad or when you’re stressed you want to go to things you’re familiar with. So because lab has always been in my life, it’s this thing where it’s going to be there for me I guess. It’s like a good book that you always go back to and it’s familiar and it makes you feel good. So that’s how lab is. It’s not like the greatest thing in the world but it’s something that I’m used to, which is what I feel like a lot of people need when they’re sad and life is not going well.”
Many students also explained that research positively affects their depression because they perceive their research contribution to be important.
Ashlyn: “I feel like I’m dedicating myself to something that’s worthy and something that I believe in. It’s really important because it contextualizes those times when I am feeling depressed. It’s like, no, I do have these better things that I’m working on. Even when I don’t like myself and I don’t like who I am, which is again, depression brain, I can at least say, ‘Well, I have all these other people relying on me in research and in this area and that’s super important.’”
Jessica: “I mean, it just felt like the work that I was doing had meaning and when I feel like what I’m doing is actually going to contribute to the world, that usually really helps with [depression] because it’s like not every day you can feel like you’re doing something impactful.”
In sum, students highlighted that experiencing failure in research and making mistakes negatively contributed to depression, especially when help was unavailable or research mentors had a negative reaction. Additionally, students acknowledged that the research could be time-consuming, but that research mentors who were flexible helped assuage depressive feelings that were associated with feeling overwhelmed. Finally, research helped some students’ depression, because it felt familiar, provided a distraction from depression, and reminded students that they were contributing to a greater cause.
We believe that creating more inclusive research environments for students with depression is an important step toward broadening participation in science, not only to ensure that we are not discouraging students with depression from persisting in science, but also because depression has been shown to disproportionately affect underserved and underrepresented groups in science ( Turner and Noh, 1988 ; Eisenberg et al. , 2007 ; Jenkins et al. , 2013 ; American College Health Association, 2018 ). We initially hypothesized that three features of undergraduate research—research mentors, the lab environment, and failure—may have the potential to exacerbate student depression. We found this to be true; students highlighted that their relationships with their mentors as well as the overall lab environment could negatively affect their depression, but could also positively affect their research experiences. Students also noted that they struggled with failure, which is likely true of most students, but is known to be particularly difficult for students with depression ( Elliott et al. , 1997 ). We expand upon our findings by integrating literature on depression with the information that students provided in the interviews about how research mentors can best support students. We provide a set of evidence-based recommendations focused on mentoring, the lab environment, and failure for research mentors wanting to create more inclusive research environments for students with depression. Notably, only the first recommendation is specific to students with depression; the others reflect recommendations that have previously been described as “best practices” for research mentors ( NASEM, 2017 , 2019 ; Sorkness et al. , 2017 ) and likely would benefit most students. However, we examine how these recommendations may be particularly important for students with depression. As we hypothesized, these recommendations directly address three aspects of research: mentors, lab environment, and failure. A caveat of these recommendations is that more research needs to be done to explore the experiences of students with depression and how these practices actually impact students with depression, but our national sample of undergraduate researchers with depression can provide an initial starting point for a discussion about how to improve research experiences for these students.
Recommendations to Make Undergraduate Research Experiences More Inclusive for Students with Depression
Recognize student depression as a valid illness..
Allow students with depression to take time off of research by simply saying that they are sick and provide appropriate time for students to recover from depressive episodes. Also, make an effort to destigmatize mental health issues.
Undergraduate researchers described both psychological and physical symptoms that manifested as a result of their depression and highlighted how such symptoms prevented them from performing to their full potential in undergraduate research. For example, students described how their depression would cause them to feel unmotivated, which would often negatively affect their research productivity. In cases in which students were motivated enough to come in and do their research, they described having difficulty concentrating or engaging in the work. Further, when doing research, students felt less creative and less willing to take risks, which may alter the quality of their work. Students also sometimes struggled to socialize in the lab. They described feeling less social and feeling overly self-critical. In sum, students described that, when they experienced a depressive episode, they were not able to perform to the best of their ability, and it sometimes took a toll on them to try to act like nothing was wrong, when they were internally struggling with depression. We recommend that research mentors treat depression like any other physical illness; allowing students the chance to recover when they are experiencing a depressive episode can be extremely important to students and can allow them to maximize their productivity upon returning to research ( Judd et al. , 2000 ). Students explained that if they are not able to take the time to focus on recovering during a depressive episode, then they typically continue to struggle with depression, which negatively affects their research. This sentiment is echoed by researchers in psychiatry who have found that patients who do not fully recover from a depressive episode are more likely to relapse and to experience chronic depression ( Judd et al. , 2000 ). Students described not doing tasks or not showing up to research because of their depression but struggling with how to share that information with their research mentors. Often, students would not say anything, which caused them anxiety because they were worried about what others in the lab would say to them when they returned. Admittedly, many students understood why this behavior would cause their research mentors to be angry or frustrated, but they weighed the consequences of their research mentors’ displeasure against the consequences of revealing their depression and decided it was not worth admitting to being depressed. This aligns with literature that suggests that when individuals have concealable stigmatized identities, or identities that can be hidden and that carry negative stereotypes, such as depression, they will often keep them concealed to avoid negative judgment or criticism ( Link and Phelan, 2001 ; Quinn and Earnshaw, 2011 ; Jones and King, 2014 ; Cooper and Brownell, 2016 ; Cooper et al. , 2019b ; Cooper et al ., unpublished data ). Therefore, it is important for research mentors to be explicit with students that 1) they recognize mental illness as a valid sickness and 2) that students with mental illness can simply explain that they are sick if they need to take time off. This may be useful to overtly state on a research website or in a research syllabus, contract, or agreement if mentors use such documents when mentoring undergraduates in their lab. Further, research mentors can purposefully work to destigmatize mental health issues by explicitly stating that struggling with mental health issues, such as depression and anxiety, is common. While we do not recommend that mentors ask students directly about depression, because this can force students to share when they are not comfortable sharing, we do recommend providing opportunities for students to reveal their depression ( Chaudoir and Fisher, 2010 ). Mentors can regularly check in with students about how they’re doing, and talk openly about the importance of mental health, which may increase the chance that students may feel comfortable revealing their depression ( Chaudoir and Quinn, 2010 ; Cooper et al ., unpublished data ).
Foster a Positive Lab Environment.
Encourage positivity in the research lab, promote working in shared spaces to enhance social support among lab members, and alleviate competition among undergraduates.
Students in this study highlighted that the “leadership” of the lab, meaning graduate students, postdocs, lab managers, and PIs, were often responsible for establishing the tone of the lab; that is, if they were in a bad mood it would trickle down and negatively affect the moods of the undergraduates. Explicitly reminding lab leadership that their moods can both positively and negatively affect undergraduates may be important in establishing a positive lab environment. Further, students highlighted how they were most likely to experience negative thoughts when they were alone in the lab. Therefore, it may be helpful to encourage all lab members to work in a shared space to enhance social interactions among students and to maximize the likelihood that undergraduates have access to help when needed. A review of 51 studies in psychiatry supported our undergraduate researchers’ perceptions that social relationships positively impacted their depression; the study found that perceived emotional support (e.g., someone available to listen or give advice), perceived instrumental support (e.g., someone available to help with tasks), and large diverse social networks (e.g., being socially connected to a large number of people) were significantly protective against depression ( Santini et al. , 2015 ). Additionally, despite forming positive relationships with other undergraduates in the lab, many undergraduate researchers admitted to constantly comparing themselves with other undergraduates, which led them to feel inferior, negatively affecting their depression. Some students talked about mentors favoring current undergraduates or talking positively about past undergraduates, which further exacerbated their feelings of inferiority. A recent study of students in undergraduate research experiences highlighted that inequitable distribution of praise to undergraduates can create negative perceptions of lab environments for students (Cooper et al. , 2019). Further, the psychology literature has demonstrated that when people feel insecure in their social environments, it can cause them to focus on a hierarchical view of themselves and others, which can foster feelings of inferiority and increase their vulnerability to depression ( Gilbert et al. , 2009 ). Thus, we recommend that mentors be conscious of their behaviors so that they do not unintentionally promote competition among undergraduates or express favoritism toward current or past undergraduates. Praise is likely best used without comparison with others and not done in a public way, although more research on the impact of praise on undergraduate researchers needs to be done. While significant research has been done on mentoring and mentoring relationships in the context of undergraduate research ( Byars-Winston et al. , 2015 ; Aikens et al. , 2017 ; Estrada et al. , 2018 ; Limeri et al. , 2019 ; NASEM, 2019 ), much less has been done on the influence of the lab environment broadly and how people in nonmentoring roles can influence one another. Yet, this study indicates the potential influence of many different members of the lab, not only their mentors, on students with depression.

Develop More Personal Relationships with Undergraduate Researchers and Provide Sufficient Guidance.
Make an effort to establish more personal relationships with undergraduates and ensure that they perceive that they have access to sufficient help and guidance with regard to their research.
When we asked students explicitly how research mentors could help create more inclusive environments for undergraduate researchers with depression, students overwhelmingly said that building mentor–student relationships would be extremely helpful. Students suggested that mentors could get to know students on a more personal level by asking about their career interests or interests outside of academia. Students also remarked that establishing a more personal relationship could help build the trust needed in order for undergraduates to confide in their research mentors about their depression, which they perceived would strengthen their relationships further because they could be honest about when they were not feeling well or their mentors might even “check in” with them in times where they were acting differently than normal. This aligns with studies showing that undergraduates are most likely to reveal a stigmatized identity, such as depression, when they form a close relationship with someone ( Chaudoir and Quinn, 2010 ). Many were intimidated to ask for research-related help from their mentors and expressed that they wished they had established a better relationship so that they would feel more comfortable. Therefore, we recommend that research mentors try to establish relationships with their undergraduates and explicitly invite them to ask questions or seek help when needed. These recommendations are supported by national recommendations for mentoring ( NASEM, 2019 ) and by literature that demonstrates that both social support (listening and talking with students) and instrumental support (providing students with help) have been shown to be protective against depression ( Santini et al. , 2015 ).
Treat Undergraduates with Respect and Remember to Praise Them.
Avoid providing harsh criticism and remember to praise undergraduates. Students with depression often have low self-esteem and are especially self-critical. Therefore, praise can help calibrate their overly negative self-perceptions.
Students in this study described that receiving criticism from others, especially harsh criticism, was particularly difficult for them given their depression. Multiple studies have demonstrated that people with depression can have an abnormal or maladaptive response to negative feedback; scientists hypothesize that perceived failure on a particular task can trigger failure-related thoughts that interfere with subsequent performance ( Eshel and Roiser, 2010 ). Thus, it is important for research mentors to remember to make sure to avoid unnecessarily harsh criticisms that make students feel like they have failed (more about failure is described in the next recommendation). Further, students with depression often have low self-esteem or low “personal judgment of the worthiness that is expressed in the attitudes the individual holds towards oneself” ( Heatherton et al. , 2003 , p. 220; Sowislo and Orth, 2013 ). Specifically, a meta-analysis of longitudinal studies found that low self-esteem is predictive of depression ( Sowislo and Orth, 2013 ), and depression has also been shown to be highly related to self-criticism ( Luyten et al. , 2007 ). Indeed, nearly all of the students in our study described thinking that they are “not good enough,” “worthless,” or “inadequate,” which is consistent with literature showing that people with depression are self-critical ( Blatt et al. , 1982 ; Gilbert et al. , 2006 ) and can be less optimistic of their performance on future tasks and rate their overall performance on tasks less favorably than their peers without depression ( Cane and Gotlib, 1985 ). When we asked students what aspects of undergraduate research helped their depression, students described that praise from their mentors was especially impactful, because they thought so poorly of themselves and they needed to hear something positive from someone else in order to believe it could be true. Praise has been highlighted as an important aspect of mentoring in research for many years ( Ashford, 1996 ; Gelso and Lent, 2000 ; Brown et al. , 2009 ) and may be particularly important for students with depression. In fact, praise has been shown to enhance individuals’ motivation and subsequent productivity ( Hancock, 2002 ; Henderlong and Lepper, 2002 ), factors highlighted by students as negatively affecting their depression. However, something to keep in mind is that a student with depression and a student without depression may process praise differently. For a student with depression, a small comment that praises the student’s work may not be sufficient for the student to process that comment as praise. People with depression are hyposensitive to reward or have reward-processing deficits ( Eshel and Roiser, 2010 ); therefore, praise may affect students without depression more positively than it would affect students with depression. Research mentors should be mindful that students with depression often have a negative view of themselves, and while students report that praise is extremely important, they may have trouble processing such positive feedback.
Normalize Failure and Be Explicit about the Importance of Research Contributions.
Explicitly remind students that experiencing failure is expected in research. Also explain to students how their individual work relates to the overall project so that they can understand how their contributions are important. It can also be helpful to explain to students why the research project as a whole is important in the context of the greater scientific community.
Experiencing failure has been thought to be a potentially important aspect of undergraduate research, because it may provide students with the potential to develop integral scientific skills such as the ability to navigate challenges and persevere ( Laursen et al. , 2010 ; Gin et al. , 2018 ; Henry et al. , 2019 ). However, in the interviews, students described that when their science experiments failed, it was particularly tough for their depression. Students’ negative reaction to experiencing failure in research is unsurprising, given recent literature that has predicted that students may be inadequately prepared to approach failure in science ( Henry et al. , 2019 ). However, the literature suggests that students with depression may find experiencing failure in research to be especially difficult ( Elliott et al. , 1997 ; Mongrain and Blackburn, 2005 ; Jones et al. , 2009 ). One potential hypothesis is that students with depression may be more likely to have fixed mindsets or more likely to believe that their intelligence and capacity for specific abilities are unchangeable traits ( Schleider and Weisz, 2018 ); students with a fixed mindset have been hypothesized to have particularly negative responses to experiencing failure in research, because they are prone to quitting easily in the face of challenges and becoming defensive when criticized ( Forsythe and Johnson, 2017 ; Dweck, 2008 ). A study of life sciences undergraduates enrolled in CUREs identified three strategies of students who adopted adaptive coping mechanisms, or mechanisms that help an individual maintain well-being and/or move beyond the stressor when faced with failure in undergraduate research: 1) problem solving or engaging in strategic planning and decision making, 2) support seeking or finding comfort and help with research, and 3) cognitive restructuring or reframing a problem from negative to positive and engaging in self encouragement ( Gin et al. , 2018 ). We recommend that, when undergraduates experience failure in science, their mentors be proactive in helping them problem solve, providing help and support, and encouraging them. Students also explained that mentors sharing their own struggles as undergraduate and graduate students was helpful, because it normalized failure. Sharing personal failures in research has been recommended as an important way to provide students with psychosocial support during research ( NASEM, 2019 ). We also suggest that research mentors take time to explain to students why their tasks in the lab, no matter how small, contribute to the greater research project ( Cooper et al. , 2019a ). Additionally, it is important to make sure that students can explain how the research project as a whole is contributing to the scientific community ( Gin et al. , 2018 ). Students highlighted that contributing to something important was really helpful for their depression, which is unsurprising, given that studies have shown that meaning in life or people’s comprehension of their life experiences along with a sense of overarching purpose one is working toward has been shown to be inversely related to depression ( Steger, 2013 ).
Limitations and Future Directions
This work was a qualitative interview study intended to document a previously unstudied phenomenon: depression in the context of undergraduate research experiences. We chose to conduct semistructured interviews rather than a survey because of the need for initial exploration of this area, given the paucity of prior research. A strength of this study is the sampling approach. We recruited a national sample of 35 undergraduates engaged in undergraduate research at 12 different public R1 institutions. Despite our representative sample from R1 institutions, these findings may not be generalizable to students at other types of institutions; lab environments, mentoring structures, and interactions between faculty and undergraduate researchers may be different at other institution types (e.g., private R1 institutions, R2 institutions, master’s-granting institutions, primarily undergraduate institutions, and community colleges), so we caution against making generalizations about this work to all undergraduate research experiences. Future work could assess whether students with depression at other types of institutions have similar experiences to students at research-intensive institutions. Additionally, we intentionally did not explore the experiences of students with specific identities owing to our sample size and the small number of students in any particular group (e.g., students of a particular race, students with a graduate mentor as the primary mentor). We intend to conduct future quantitative studies to further explore how students’ identities and aspects of their research affect their experiences with depression in undergraduate research.
The students who participated in the study volunteered to be interviewed about their depression; therefore, it is possible that depression is a more salient part of these students’ identities and/or that they are more comfortable talking about their depression than the average population of students with depression. It is also important to acknowledge the personal nature of the topic and that some students may not have fully shared their experiences ( Krumpal, 2013 ), particularly those experiences that may be emotional or traumatizing ( Kahn and Garrison, 2009 ). Additionally, our sample was skewed toward females (77%). While females do make up approximately 60% of students in biology programs on average ( Eddy et al. , 2014 ), they are also more likely to report experiencing depression ( American College Health Association, 2018 ; Evans et al. , 2018 ). However, this could be because women have higher rates of depression or because males are less likely to report having depression; clinical bias, or practitioners’ subconscious tendencies to overlook male distress, may underestimate depression rates in men ( Smith et al. , 2018 ). Further, females are also more likely to volunteer to participate in studies ( Porter and Whitcomb, 2005 ); therefore, many interview studies have disproportionately more females in the data set (e.g., Cooper et al. , 2017 ). If we had been able to interview more male students, we might have identified different findings. Additionally, we limited our sample to life sciences students engaged in undergraduate research at public R1 institutions. It is possible that students in other majors may have different challenges and opportunities for students with depression, as well as different disciplinary stigmas associated with mental health.
In this exploratory interview study, we identified a variety of ways in which depression in undergraduates negatively affected their undergraduate research experiences. Specifically, we found that depression interfered with students’ motivation and productivity, creativity and risk-taking, engagement and concentration, and self-perception and socializing. We also identified that research can negatively affect depression in undergraduates. Experiencing failure in research can exacerbate student depression, especially when students do not have access to adequate guidance. Additionally, being alone or having negative interactions with others in the lab worsened students’ depression. However, we also found that undergraduate research can positively affect students’ depression. Research can provide a familiar space where students can feel as though they are contributing to something meaningful. Additionally, students reported that having access to adequate guidance and a social support network within the research lab also positively affected their depression. We hope that this work can spark conversations about how to make undergraduate research experiences more inclusive of students with depression and that it can stimulate additional research that more broadly explores the experiences of undergraduate researchers with depression.
Important note
If you or a student experience symptoms of depression and want help, there are resources available to you. Many campuses provide counseling centers equipped to provide students, staff, and faculty with treatment for depression, as well as university-dedicated crisis hotlines. Additionally, there are free 24/7 services such as Crisis Text Line, which allows you to text a trained live crisis counselor (Text “CONNECT” to 741741; Text Depression Hotline , 2019 ), and phone hotlines such as the National Suicide Prevention Lifeline at 1-800-273-8255 (TALK). You can also learn more about depression and where to find help near you through the Anxiety and Depression Association of American website: https://adaa.org ( Anxiety and Depression Association of America, 2019 ) and the Depression and Biopolar Support Alliance: http://dbsalliance.org ( Depression and Biopolar Support Alliance, 2019 ).
ACKNOWLEDGMENTS
We are extremely grateful to the undergraduate researchers who shared their thoughts and experiences about depression with us. We acknowledge the ASU LEAP Scholars for helping us create the original survey and Rachel Scott for her helpful feedback on earlier drafts of this article. L.E.G. was supported by a National Science Foundation (NSF) Graduate Fellowship (DGE-1311230) and K.M.C. was partially supported by a Howard Hughes Medical Institute (HHMI) Inclusive Excellence grant (no. 11046) and an NSF grant (no. 1644236). Any opinions, findings, conclusions, or recommendations expressed in this material are those of the authors and do not necessarily reflect the views of the NSF or HHMI.
- Aikens, M. L., Robertson, M. M., Sadselia, S., Watkins, K., Evans, M., Runyon, C. R. , … & Dolan, E. L. ( 2017 ). Race and gender differences in undergraduate research mentoring structures and research outcomes . CBE—Life Sciences Education , 16 (2), ar34. Link , Google Scholar
- Aikens, M. L., Sadselia, S., Watkins, K., Evans, M., Eby, L. T., & Dolan, E. L. ( 2016 ). A social capital perspective on the mentoring of undergraduate life science researchers: An empirical study of undergraduate–postgraduate–faculty triads . CBE—Life Sciences Education , 15 (2), ar16. Link , Google Scholar
- Aldwin, C., & Greenberger, E. ( 1987 ). Cultural differences in the predictors of depression . American Journal of Community Psychology , 15 (6), 789–813. Medline , Google Scholar
- American Association for the Advancement of Science . ( 2011 ). Vision and change in undergraduate biology education: A call to action . Retrieved November 29, 2019, from http://visionandchange.org/files/2013/11/aaas-VISchange-web1113.pdf Google Scholar
- American College Health Association . ( 2018 ). Undergraduate reference group executive summary, Fall 2018 . Retrieved November 29, 2019, from www.acha.org/documents/ncha/NCHA-II_Fall_2018_Reference_Group_Executive_Summary.pdf Google Scholar
- American College Health Association . ( 2019 ). Retrieved November 29, 2019, from NCHA-II_SPRING_2019_UNDERGRADUATE_REFERENCE_GROUP_DATA_REPORT.pdf www.acha.org/documents/ncha/NCHA-II_SPRING_2019_UNDERGRADUATE_REFERENCE_GROUP_DATA_REPORT.pdf Google Scholar
- American Psychiatric Association . ( 2013 ). Diagnostic and statistical manual of mental disorders (5th ed.). Washington, DC: American Psychiatric Publishing. Google Scholar
- Aneshensel, C. S., & Stone, J. D. ( 1982 ). Stress and depression: A test of the buffering model of social support . Archives of General Psychiatry , 39 (12), 1392–1396. Medline , Google Scholar
- Anxiety and Depression Association of America . ( 2019 ). Home page . Retrieved November 29, 2019, from https://adaa.org Google Scholar
- Armbruster, P., Patel, M., Johnson, E., & Weiss, M. ( 2009 ). Active learning and student-centered pedagogy improve student attitudes and performance in introductory biology . CBE—Life Sciences Education , 8 (3), 203–213. Link , Google Scholar
- Ashford, S. J. ( 1996 ). Working with doctoral students: Rhythms of Academic Life: Personal Accounts of Careers in Academia . In Front, P. J.Taylor, M. S. (Eds.), Rhythms of Academic Life: Personal Accounts of Careers in Academia (pp. 153–158). Thousand Oaks, CA: Sage. Google Scholar
- Auchincloss, L. C., Laursen, S. L., Branchaw, J. L., Eagan, K., Graham, M., Hanauer, D. I. , … & Rowland, S. ( 2014 ). Assessment of course-based undergraduate research experiences: A meeting report . CBE—Life Sciences Education , 13 (1), 29–40. Link , Google Scholar
- Barak, M. E. M., Levin, A., Nissly, J. A., & Lane, C. J. ( 2006 ). Why do they leave? Modeling child welfare workers’ turnover intentions . Children and Youth Services Review , 28 (5), 548–577. Google Scholar
- Bauer, K. W., & Bennett, J. S. ( 2003 ). Alumni perceptions used to assess undergraduate research experience . Journal of Higher Education , 74 (2), 210–230. Google Scholar
- Birks, M., & Mills, J. ( 2015 ). Grounded theory: A practical guide . Thousand Oaks, CA: Sage. Google Scholar
- Blatt, S. J., Quinlan, D. M., Chevron, E. S., McDonald, C., & Zuroff, D. ( 1982 ). Dependency and self-criticism: Psychological dimensions of depression . Journal of Consulting and Clinical Psychology , 50 (1), 113. Medline , Google Scholar
- Brown, R. T., Daly, B. P., & Leong, F. T. ( 2009 ). Mentoring in research: A developmental approach . Professional Psychology: Research and Practice , 40 (3), 306. Google Scholar
- Brownell, S. E., Hekmat-Scafe, D. S., Singla, V., Seawell, P. C., Imam, J. F. C., Eddy, S. L. , … & Cyert, M. S. ( 2015 ). A high-enrollment course-based undergraduate research experience improves student conceptions of scientific thinking and ability to interpret data . CBE—Life Sciences Education , 14 (2), ar21. Link , Google Scholar
- Brownell, S. E., & Kloser, M. J. ( 2015 ). Toward a conceptual framework for measuring the effectiveness of course-based undergraduate research experiences in undergraduate biology . Studies in Higher Education , 40 (3), 525–544. Google Scholar
- Byars-Winston, A. M., Branchaw, J., Pfund, C., Leverett, P., & Newton, J. ( 2015 ). Culturally diverse undergraduate researchers’ academic outcomes and perceptions of their research mentoring relationships . International Journal of Science Education , 37 (15), 2533–2554. Medline , Google Scholar
- Cane, D. B., & Gotlib, I. H. ( 1985 ). Depression and the effects of positive and negative feedback on expectations, evaluations, and performance . Cognitive Therapy and Research , 9 (2), 145–160. Google Scholar
- Ceci, S. J., & Williams, W. M. ( 2010 ). Sex differences in math-intensive fields . Current Directions in Psychological Science , 19 (5), 275–279. Medline , Google Scholar
- Center for Collegiate Mental Health . ( 2017 ). Center for Collegiate Mental Health 2017 Annual Report . State College, PA: Penn State Universit. Google Scholar
- Charmaz, K. ( 2006 ). Constructing grounded theory: A practical guide through qualitative research . Thousand Oaks, CA: Sage. Google Scholar
- Chaudoir, S. R., & Fisher, J. D. ( 2010 ). The disclosure processes model: Understanding disclosure decision making and postdisclosure outcomes among people living with a concealable stigmatized identity . Psychological Bulletin , 136 (2), 236. Medline , Google Scholar
- Chaudoir, S. R., & Quinn, D. M. ( 2010 ). Revealing concealable stigmatized identities: The impact of disclosure motivations and positive first-disclosure experiences on fear of disclosure and well-being . Journal of Social Issues , 66 (3), 570–584. Medline , Google Scholar
- Clance, P. R., & Imes, S. A. ( 1978 ). The imposter phenomenon in high achieving women: Dynamics and therapeutic intervention . Psychotherapy: Theory, Research & Practice , 15 (3), 241. Google Scholar
- Cooper, K. M., Ashley, M., & Brownell, S. E. ( 2017 ). A bridge to active learning: A summer bridge program helps students maximize their active-learning experiences and the active-learning experiences of others . CBE—Life Sciences Education , 16 (1), ar17. Link , Google Scholar
- Cooper, K. M., Blattman, J. N., Hendrix, T., & Brownell, S. E. ( 2019a ). The impact of broadly relevant novel discoveries on student project ownership in a traditional lab course turned CURE . CBE—Life Sciences Education , 18 (4), ar57. Link , Google Scholar
- Cooper, K. M., & Brownell, S. E. ( 2016 ). Coming out in class: Challenges and benefits of active learning in a biology classroom for LGBTQIA students . CBE—Life Sciences Education , 15 (3), ar37. https://doi.org/10.1187/cbe.16-01-0074 Link , Google Scholar
- Cooper, K. M., Brownell, S. E., & Gormally, C. C. ( 2019b ). Coming out to the class: Identifying factors that influence college biology instructor decisions about whether to reveal their LGBQ identity in class . Journal of Women and Minorities in Science and Engineering , 25 (3). Google Scholar
- Cooper, K. M., Downing, V. R., & Brownell, S. E. ( 2018 ). The influence of active learning practices on student anxiety in large-enrollment college science classrooms . International Journal of STEM Education , 5 (1), 23. Medline , Google Scholar
- Cooper, K. M., Gin, L. E., Akeeh, B., Clark, C. E., Hunter, J. S., Roderick, T. B. , … & Brownell, S. E. ( 2019c ). Factors that predict life sciences student persistence in undergraduate research experiences . PLoS ONE , 14 (8). https://doi.org/10.1371/journal.pone.0220186 Google Scholar
- Cooper, K. M., Gin, L. E., & Brownell, S. E. ( 2019d ). Diagnosing differences in what introductory biology students in a fully online and an in-person biology degree program know and do regarding medical school admission . Advances in Physiology Education , 43 (2), 221–232. Medline , Google Scholar
- Cooper, K. M., Gin, L. E., & Brownell, S. E. ( In press ). Depression as a concealable stigmatized identity: What influences whether students conceal or reveal their depression in undergraduate research experiences? International Journal of STEM Education , ( in press ). Google Scholar
- Depression and Biopolar Support Alliance . ( 2019 ). Home page . Retrieved November 28, 2019, from www.dbsalliance.org Google Scholar
- Deroma, V. M., Leach, J. B., & Leverett, J. P. ( 2009 ). The relationship between depression and college academic performance . College Student Journal , 43 (2), 325–335. Google Scholar
- Dweck, C. S. ( 2008 ). Mindset: The new psychology of success . New York, NY: Random House Digital. Google Scholar
- Dyson, R., & Renk, K. ( 2006 ). Freshmen adaptation to university life: Depressive symptoms, stress, and coping . Journal of Clinical Psychology , 62 (10), 1231–1244. Medline , Google Scholar
- Eddy, S. L., Brownell, S. E., & Wenderoth, M. P. ( 2014 ). Gender gaps in achievement and participation in multiple introductory biology classrooms . CBE—Life Sciences Education , 13 (3), 478–492. https://doi.org/10.1187/cbe.13-10-0204 Link , Google Scholar
- Eisenberg, D., Gollust, S. E., Golberstein, E., & Hefner, J. L. ( 2007 ). Prevalence and correlates of depression, anxiety, and suicidality among university students . American Journal of Orthopsychiatry , 77 (4), 534–542. Medline , Google Scholar
- Elliott, R., Sahakian, B. J., Herrod, J. J., Robbins, T. W., & Paykel, E. S. ( 1997 ). Abnormal response to negative feedback in unipolar depression: Evidence for a diagnosis specific impairment . Journal of Neurology, Neurosurgery & Psychiatry , 63 (1), 74–82. Medline , Google Scholar
- Eshel, N., & Roiser, J. P. ( 2010 ). Reward and punishment processing in depression . Biological Psychiatry , 68 (2), 118–124. Medline , Google Scholar
- Estrada, M., Hernandez, P. R., & Schultz, P. W. ( 2018 ). A longitudinal study of how quality mentorship and research experience integrate underrepresented minorities into STEM careers . CBE—Life Sciences Education , 17 (1), ar9. Link , Google Scholar
- Evans, T. M., Bira, L., Gastelum, J. B., Weiss, L. T., & Vanderford, N. L. ( 2018 ). Evidence for a mental health crisis in graduate education . Nature Biotechnology , 36 (3), 282. Medline , Google Scholar
- Everson, H. T., Tobias, S., Hartman, H., & Gourgey, A. ( 1993 ). Test anxiety and the curriculum: The subject matters . Anxiety, Stress, and Coping , 6 (1), 1–8. Google Scholar
- Flaherty, C. ( 2018 ). New study says graduate students’ mental health is a “crisis.” Retrieved November 29, 2019, from www.insidehighered.com/news/2018/03/06/new-study-says-graduate-students-mental-health-crisis Google Scholar
- Forsythe, A., & Johnson, S. ( 2017 ). Thanks, but no-thanks for the feedback . Assessment & Evaluation in Higher Education , 42 (6), 850–859. Google Scholar
- Garlow, S. J., Rosenberg, J., Moore, J. D., Haas, A. P., Koestner, B., Hendin, H., & Nemeroff, C. B. ( 2008 ). Depression, desperation, and suicidal ideation in college students: Results from the American Foundation for Suicide Prevention College Screening Project at Emory University . Depression and Anxiety , 25 (6), 482–488. Medline , Google Scholar
- Gelso, C. J., & Lent, R. W. ( 2000 ). Scientific training and scholarly productivity: The person, the training environment, and their interaction . In Brown, S. D.Lent, R. W. (Eds.), Handbook of counseling psychology (pp. 109–139). Hoboken, NJ: John Wiley & Sons Inc. Google Scholar
- Gilbert, P., Baldwin, M. W., Irons, C., Baccus, J. R., & Palmer, M. ( 2006 ). Self-criticism and self-warmth: An imagery study exploring their relation to depression . Journal of Cognitive Psychotherapy , 20 (2), 183. Google Scholar
- Gilbert, P., McEwan, K., Bellew, R., Mills, A., & Gale, C. ( 2009 ). The dark side of competition: How competitive behaviour and striving to avoid inferiority are linked to depression, anxiety, stress and self-harm . Psychology and Psychotherapy: Theory, Research and Practice , 82 (2), 123–136. Medline , Google Scholar
- Gin, L. E., Rowland, A. A., Steinwand, B., Bruno, J., & Corwin, L. A. ( 2018 ). Students who fail to achieve predefined research goals may still experience many positive outcomes as a result of CURE participation . CBE—Life Sciences Education , 17 (4), ar57. Link , Google Scholar
- Glesne, C., & Peshkin, A. ( 1992 ). Becoming qualitative researchers: An introduction . London, England, UK: Longman. Google Scholar
- Grav, S., Hellzèn, O., Romild, U., & Stordal, E. ( 2012 ). Association between social support and depression in the general population: The HUNT study, a cross-sectional survey . Journal of Clinical Nursing , 21 (1–2), 111–120. Medline , Google Scholar
- Guest, G., Bunce, A., & Johnson, L. ( 2006 ). How many interviews are enough? An experiment with data saturation and variability . Field Methods , 18 (1), 59–82. Google Scholar
- Hancock, D. R. ( 2002 ). Influencing graduate students’ classroom achievement, homework habits and motivation to learn with verbal praise . Educational Research , 44 (1), 83–95. Google Scholar
- Hannah, D. R., & Lautsch, B. A. ( 2011 ). Counting in qualitative research: Why to conduct it, when to avoid it, and when to closet it . Journal of Management Inquiry , 20 (1), 14–22. Google Scholar
- Heatherton, T. F., & Wyland, C. L. ( 2003 ). Assessing self-esteem . In Lopez, S. J.Snyder, C. R. (Eds.), Positive psychological assessment: A handbook of models and measures (pp. 219–233). Washington, DC: American Psychological Association. https://doi.org/10.1037/10612-014 . Google Scholar
- Henderlong, J., & Lepper, M. R. ( 2002 ). The effects of praise on children’s intrinsic motivation: A review and synthesis . Psychological Bulletin , 128 (5), 774. Medline , Google Scholar
- Henry, M. A., Shorter, S., Charkoudian, L., Heemstra, J. M., & Corwin, L. A. ( 2019 ). FAIL is not a four-letter word: A theoretical framework for exploring undergraduate students’ approaches to academic challenge and responses to failure in STEM learning environments . CBE—Life Sciences Education , 18 (1), ar11. Link , Google Scholar
- Hernandez, P. R., Woodcock, A., Estrada, M., & Schultz, P. W. ( 2018 ). Undergraduate research experiences broaden diversity in the scientific workforce . BioScience , 68 (3), 204–211. Google Scholar
- Hish, A. J., Nagy, G. A., Fang, C. M., Kelley, L., Nicchitta, C. V., Dzirasa, K., & Rosenthal, M. Z. ( 2019 ). Applying the stress process model to stress–burnout and stress–depression relationships in biomedical doctoral students: A cross-sectional pilot study . CBE—Life Sciences Education , 18 (4), ar51. Link , Google Scholar
- Howell, E., & McFeeters, J. ( 2008 ). Children’s mental health care: Differences by race/ethnicity in urban/rural areas . Journal of Health Care for the Poor and Underserved , 19 (1), 237–247. Medline , Google Scholar
- Hysenbegasi, A., Hass, S. L., & Rowland, C. R. ( 2005 ). The impact of depression on the academic productivity of university students . Journal of Mental Health Policy and Economics , 8 (3), 145. Medline , Google Scholar
- Ibrahim, A. K., Kelly, S. J., Adams, C. E., & Glazebrook, C. ( 2013 ). A systematic review of studies of depression prevalence in university students . Journal of Psychiatric Research , 47 (3), 391–400. Medline , Google Scholar
- Intemann, K. ( 2009 ). Why diversity matters: Understanding and applying the diversity component of the National Science Foundation’s broader impacts criterion . Social Epistemology , 23 (3–4), 249–266. Google Scholar
- Ishiyama, J. ( 2002 ). Does early participation in undergraduate research benefit social science and humanities students? College Student Journal , 36 (3), 381–387. Google Scholar
- Jenkins, S. R., Belanger, A., Connally, M. L., Boals, A., & Durón, K. M. ( 2013 ). First-generation undergraduate students’ social support, depression, and life satisfaction . Journal of College Counseling , 16 (2), 129–142. Google Scholar
- Jobst, A., Sabass, L., Palagyi, A., Bauriedl-Schmidt, C., Mauer, M. C., Sarubin, N. , … & Zill, P. ( 2015 ). Effects of social exclusion on emotions and oxytocin and cortisol levels in patients with chronic depression . Journal of Psychiatric Research , 60 , 170–177. Medline , Google Scholar
- Jones, K. P., & King, E. B. ( 2014 ). Managing concealable stigmas at work: A review and multilevel model . Journal of Management , 40 (5), 1466–1494. Google Scholar
- Jones, M. T., Barlow, A. E., & Villarejo, M. ( 2010 ). Importance of undergraduate research for minority persistence and achievement in biology . Journal of Higher Education , 81 (1), 82–115. Google Scholar
- Jones, N. P., Papadakis, A. A., Hogan, C. M., & Strauman, T. J. ( 2009 ). Over and over again: Rumination, reflection, and promotion goal failure and their interactive effects on depressive symptoms . Behaviour Research and Therapy , 47 (3), 254–259. Medline , Google Scholar
- Judd, L. L., Paulus, M. J., Schettler, P. J., Akiskal, H. S., Endicott, J., Leon, A. C. , … & Keller, M. B. ( 2000 ). Does incomplete recovery from first lifetime major depressive episode herald a chronic course of illness? American Journal of Psychiatry , 157 (9), 1501–1504. Medline , Google Scholar
- Kahn, J. H., & Garrison, A. M. ( 2009 ). Emotional self-disclosure and emotional avoidance: Relations with symptoms of depression and anxiety . Journal of Counseling Psychology , 56 (4), 573. Google Scholar
- Kataoka, S. H., Zhang, L., & Wells, K. B. ( 2002 ). Unmet need for mental health care among US children: Variation by ethnicity and insurance status . American Journal of Psychiatry , 159 (9), 1548–1555. Medline , Google Scholar
- Kreger, D. W. ( 1995 ). Self-esteem, stress, and depression among graduate students . Psychological Reports , 76 (1), 345–346. Medline , Google Scholar
- Krumpal, I. ( 2013 ). Determinants of social desirability bias in sensitive surveys: A literature review . Quality & Quantity , 47 (4), 2025–2047. Google Scholar
- Landis, J. R., & Koch, G. G. ( 1977 ). An application of hierarchical kappa-type statistics in the assessment of majority agreement among multiple observers . Biometrics , 33 (2), 363–374. Medline , Google Scholar
- Laursen, S., Hunter, A.-B., Seymour, E., Thiry, H., & Melton, G. ( 2010 ). Undergraduate research in the sciences: Engaging students in real science . Hoboken, NJ: Wiley. Google Scholar
- Limeri, L. B., Asif, M. Z., Bridges, B. H., Esparza, D., Tuma, T. T., Sanders, D. , … & Maltese, A. V. ( 2019 ). “Where’s my mentor?” Characterizing negative mentoring experiences in undergraduate life science research . CBE—Life Sciences Education , 18 (4), ar61. Link , Google Scholar
- Link, B. G., & Phelan, J. C. ( 2001 ). Conceptualizing stigma . Annual Review of Sociology , 27 (1), 363–385. Google Scholar
- Luyten, P., Sabbe, B., Blatt, S. J., Meganck, S., Jansen, B., De Grave, C. , … & Corveleyn, J. ( 2007 ). Dependency and self-criticism: Relationship with major depressive disorder, severity of depression, and clinical presentation . Depression and Anxiety , 24 (8), 586–596. Medline , Google Scholar
- Mabrouk, P. A., & Peters, K. ( 2000 ). Student perspectives on undergraduate research (UR) experiences in chemistry and biology . CUR Quarterly , 21 (1), 25–33. Google Scholar
- Maxwell, J. A. ( 2010 ). Using numbers in qualitative research . Qualitative Inquiry , 16 (6), 475–482. Google Scholar
- Mongrain, M., & Blackburn, S. ( 2005 ). Cognitive vulnerability, lifetime risk, and the recurrence of major depression in graduate students . Cognitive Therapy and Research , 29 (6), 747–768. Google Scholar
- Nagy, G. A., Fang, C. M., Hish, A. J., Kelly, L., Nicchitta, C. V., Dzirasa, K., & Rosenthal, M. Z. ( 2019 ). Burnout and mental health problems in biomedical doctoral students . CBE—Life Sciences Education , 18 (2), ar27. Link , Google Scholar
- National Academies of Sciences, Engineering, and Medicine (NASEM) . ( 2017 ). Undergraduate research experiences for STEM students: Successes, challenges, and opportunities . Washington, DC: National Academies Press. https://doi.org/10.17226/24622 Google Scholar
- NASEM . ( 2019 ). The science of effective mentorship in STEMM . Washington, DC: National Academies Press. Retrieved November 29, 2019, from www.nap.edu/download/25568 Google Scholar
- Osborne, J., & Collins, S. ( 2001 ). Pupils’ views of the role and value of the science curriculum: A focus-group study . International Journal of Science Education , 23 (5), 441–467. https://doi.org/10.1080/09500690010006518 Google Scholar
- Porter, S. R., & Whitcomb, M. E. ( 2005 ). Non-response in student surveys: The role of demographics, engagement and personality . Research in Higher Education , 46 (2), 127–152. Google Scholar
- President’s Council of Advisors on Science and Technology . ( 2012 ). Engage to excel: Producing one million additional college graduates with degrees in science, Technology, Engineering, and mathematics . Washington, DC: U.S. Government Office of Science and Technology. Google Scholar
- Prunuske, A. J., Wilson, J., Walls, M., & Clarke, B. ( 2013 ). Experiences of mentors training underrepresented undergraduates in the research laboratory . CBE—Life Sciences Education , 12 (3), 403–409. Link , Google Scholar
- Quinn, D. M., & Earnshaw, V. A. ( 2011 ). Understanding concealable stigmatized identities: The role of identity in psychological, physical, and behavioral outcomes . Social Issues and Policy Review , 5 (1), 160–190. Google Scholar
- Rauckhorst, W. H., Czaja, J. A., & Baxter Magolda, M. ( 2001 ). Measuring the impact of the undergraduate research experience on student intellectual development . Snowbird, UT: Project Kaleidoscope Summer Institute. Google Scholar
- Saldaña, J. ( 2015 ). The coding manual for qualitative researchers . Thousand Oaks, CA: Sage. Google Scholar
- Santiago, C. D., Kaltman, S., & Miranda, J. ( 2013 ). Poverty and mental health: How do low-income adults and children fare in psychotherapy? Journal of Clinical Psychology , 69 (2), 115–126. Medline , Google Scholar
- Santini, Z. I., Koyanagi, A., Tyrovolas, S., Mason, C., & Haro, J. M. ( 2015 ). The association between social relationships and depression: A systematic review . Journal of Affective Disorders , 175 , 53–65. Medline , Google Scholar
- Schleider, J., & Weisz, J. ( 2018 ). A single-session growth mindset intervention for adolescent anxiety and depression: 9-month outcomes of a randomized trial . Journal of Child Psychology and Psychiatry , 59 (2), 160–170. Medline , Google Scholar
- Seymour, E., & Hewitt, N. M. ( 1997 ). Talking about leaving: Why undergraduates leave the sciences . Westview Press. Google Scholar
- Seymour, E., & Hunter, A.-B. ( 2019 ). Talking about leaving revisited . New York, NY: Springer. Google Scholar
- Seymour, E., Hunter, A.-B., Laursen, S. L., & DeAntoni, T. ( 2004 ). Establishing the benefits of research experiences for undergraduates in the sciences: First findings from a three-year study . Science Education , 88 (4), 493–534. Google Scholar
- Smith, D. T., Mouzon, D. M., & Elliott, M. ( 2018 ). Reviewing the assumptions about men’s mental health: An exploration of the gender binary . American Journal of Men’s Health , 12 (1), 78–89. Medline , Google Scholar
- Sorkness, C. A., Pfund, C., Ofili, E. O., Okuyemi, K. S., Vishwanatha, J. K., Zavala, M. E. , … & Deveci, A. ( 2017 ). A new approach to mentoring for research careers: The National Research Mentoring Network . BMC Proceedings , 11 , 22. Medline , Google Scholar
- Sowislo, J. F., & Orth, U. ( 2013 ). Does low self-esteem predict depression and anxiety? A meta-analysis of longitudinal studies . Psychological Bulletin , 139 (1), 213. Medline , Google Scholar
- Steger, M. F. ( 2013 ). Experiencing meaning in life: Optimal functioning at the nexus of well-being, psychopathology, and spirituality . In Wong, P. T. P. (Ed.), The human quest for meaning (pp. 211–230). England, UK: Routledge. Google Scholar
- Strenta, A. C., Elliott, R., Adair, R., Matier, M., & Scott, J. ( 1994 ). Choosing and leaving science in highly selective institutions . Research in Higher Education , 35 (5), 513–547. Google Scholar
- Text Depression Hotline . ( 2019 ). Crisis text line . Retrieved November 29, 2019, from www.crisistextline.org/depression Google Scholar
- Thiry, H., & Laursen, S. L. ( 2011 ). The role of student–advisor interactions in apprenticing undergraduate researchers into a scientific community of practice . Journal of Science Education and Technology , 20 (6), 771–784. Google Scholar
- Thompson, J. J., Conaway, E., & Dolan, E. L. ( 2016 ). Undergraduate students’ development of social, cultural, and human capital in a networked research experience . Cultural Studies of Science Education , 11 (4), 959–990. Google Scholar
- Trenor, J. M., Miller, M. K., & Gipson, K. G. ( 2011 ). Utilization of a think-aloud protocol to cognitively validate a survey instrument identifying social capital resources of engineering undergraduates . 118th American Society for Engineering Education Annual Conference and Exposition, Vancouver, BC, Canada . Google Scholar
- Turner, R. J., & Noh, S. ( 1988 ). Physical disability and depression: A longitudinal analysis . Journal of Health and Social Behavior , 29 (1), 23–37. Medline , Google Scholar
- Watson, D., & Friend, R. ( 1969 ). Measurement of social-evaluative anxiety . Journal of Consulting and Clinical Psychology , 33 (4), 448. Medline , Google Scholar
- Weeks, J. W., Heimberg, R. G., Fresco, D. M., Hart, T. A., Turk, C. L., Schneier, F. R., & Liebowitz, M. R. ( 2005 ). Empirical validation and psychometric evaluation of the Brief Fear of Negative Evaluation Scale in patients with social anxiety disorder . Psychological Assessment , 17 (2), 179. Medline , Google Scholar
- World Health Organization . ( 2018 ). Depression . Retrieved November 29, 2019, from www.who.int/news-room/fact-sheets/detail/depression Google Scholar
- Wyatt, T., & Oswalt, S. B. ( 2013 ). Comparing mental health issues among undergraduate and graduate students . American Journal of Health Education , 44 (2), 96–107. Google Scholar
- Carly A. Busch ,
- Tala Araghi ,
- Jingyi He ,
- Katelyn M. Cooper , and
- Colin Harrison, Monitoring Editor
- Emma C. Goodwin ,
- Danielle Pais ,
- Logan E. Gin , and
- Derek Braun, Monitoring Editor
- Baylee A. Edwards ,
- Chloe Bowen ,
- M. Elizabeth Barnes , and
- Tati Russo-Tait, Monitoring Editor
- Sara E. Grineski ,
- Danielle X. Morales , and
- Timothy W. Collins
- Carly A. Busch , and
- Tasneem F. Mohammed ,
- Erika M. Nadile ,
- Madison L. Witt ,
- Cindy Vargas ,
- Missy Tran ,
- Joseph Gazing Wolf ,
- Danielle Brister , and
- Sehoya Cotner, Monitoring Editor
- Katelyn M. Cooper ,
- Sarah L. Eddy , and
- Coping behavior versus coping style: characterizing a measure of coping in undergraduate STEM contexts 14 February 2022 | International Journal of STEM Education, Vol. 9, No. 1
- Lisa A. Corwin ,
- Michael E. Ramsey ,
- Eric A. Vance ,
- Elizabeth Woolner ,
- Stevie Maiden ,
- Nina Gustafson and
- Joseph A. Harsh
- Erin Shortlidge, Monitoring Editor
- K. Supriya ,
- Brian Sato, Monitoring Editor
- Logan E. Gin ,
- Clark Coffman, Monitoring Editor
- Nicholas J. Wiesenthal , and
- Maryrose Weatherton and
- Elisabeth E. Schussler
- Erika Offerdahl, Monitoring Editor
- Eight Recommendations to Promote Effective Study Habits for Biology Students Enrolled in Online Courses Journal of Microbiology & Biology Education, Vol. 23, No. 1
- Fostering professional development through undergraduate research: supporting faculty mentors and student researchers 30 March 2022 | Mentoring & Tutoring: Partnership in Learning, Vol. 30, No. 2
- Jeffrey Maloy ,
- Monika B. Kwapisz , and
- Bryce E. Hughes
- Terrell Morton, Monitoring Editor
- Anxiety and depression among US college students engaging in undergraduate research during the COVID-19 pandemic 14 December 2021 | Journal of American College Health, Vol. 9
- Danielle Brister ,
- Sara E. Brownell ,
- Chade T. Claiborne ,
- Curtis Lunt ,
- Kobe M. Walker ,
- Tamiru D. Warkina ,
- Yi Zheng , and
- Rebecca Price, Monitoring Editor
- Dominant Learning Styles of Interior Design Students in Generation Z 26 July 2021 | Journal of Interior Design, Vol. 46, No. 4
- Linking Emotional Intelligence, Physical Activity and Aggression among Undergraduates 26 November 2021 | International Journal of Environmental Research and Public Health, Vol. 18, No. 23
- Advancing undergraduate synthetic biology education: insights from a Canadian iGEM student perspective Canadian Journal of Microbiology, Vol. 67, No. 10
- Frank A. Guerrero ,
- Sara E. Brownell , and
- Jennifer Momsen, Monitoring Editor
- Nicholas J. Wiesenthal ,
- Isabella Ferreira , and
- Grant Ean Gardner, Monitoring Editor
- Carolyn E. Clark ,
- Deanna B. Elliott ,
- Travis B. Roderick ,
- Rachel A. Scott ,
- Denisse Arellano ,
- Diana Ramirez ,
- Kimberly Velarde ,
- Allyson Aeschliman ,
- Sarah T. Avalle ,
- Jessica Berkheimer ,
- Rachel Campos ,
- Michael Gerbasi ,
- Sophia Hughes ,
- Julie A. Roberts ,
- Quinn M. White ,
- Ehren Wittekind ,
- Rachelle Spell, Monitoring Editor
- Christine Pfund ,
- Janet L. Branchaw ,
- Melissa McDaniels ,
- Angela Byars-Winston ,
- Steven P. Lee ,, and
- Bruce Birren
- Vladimir Anokhin ,
- MacKenzie J. Gray ,
- Daniel E. Zajic ,
- Jason E. Podrabsky , and
- Erin E. Shortlidge
- Depression as a concealable stigmatized identity: what influences whether students conceal or reveal their depression in undergraduate research experiences? 4 June 2020 | International Journal of STEM Education, Vol. 7, No. 1
Submitted: 4 November 2019 Revised: 24 February 2020 Accepted: 6 March 2020
© 2020 K. M. Cooper, L. E. Gin, et al. CBE—Life Sciences Education © 2020 The American Society for Cell Biology. This article is distributed by The American Society for Cell Biology under license from the author(s). It is available to the public under an Attribution–Noncommercial–Share Alike 3.0 Unported Creative Commons License (http://creativecommons.org/licenses/by-nc-sa/3.0).
Have a language expert improve your writing
Run a free plagiarism check in 10 minutes, generate accurate citations for free.
- Knowledge Base
- Research paper
Writing a Research Paper Introduction | Step-by-Step Guide
Published on September 24, 2022 by Jack Caulfield . Revised on March 27, 2023.
The introduction to a research paper is where you set up your topic and approach for the reader. It has several key goals:
- Present your topic and get the reader interested
- Provide background or summarize existing research
- Position your own approach
- Detail your specific research problem and problem statement
- Give an overview of the paper’s structure
The introduction looks slightly different depending on whether your paper presents the results of original empirical research or constructs an argument by engaging with a variety of sources.
Instantly correct all language mistakes in your text
Upload your document to correct all your mistakes in minutes
Table of contents
Step 1: introduce your topic, step 2: describe the background, step 3: establish your research problem, step 4: specify your objective(s), step 5: map out your paper, research paper introduction examples, frequently asked questions about the research paper introduction.
The first job of the introduction is to tell the reader what your topic is and why it’s interesting or important. This is generally accomplished with a strong opening hook.
The hook is a striking opening sentence that clearly conveys the relevance of your topic. Think of an interesting fact or statistic, a strong statement, a question, or a brief anecdote that will get the reader wondering about your topic.
For example, the following could be an effective hook for an argumentative paper about the environmental impact of cattle farming:
A more empirical paper investigating the relationship of Instagram use with body image issues in adolescent girls might use the following hook:
Don’t feel that your hook necessarily has to be deeply impressive or creative. Clarity and relevance are still more important than catchiness. The key thing is to guide the reader into your topic and situate your ideas.
The only proofreading tool specialized in correcting academic writing - try for free!
The academic proofreading tool has been trained on 1000s of academic texts and by native English editors. Making it the most accurate and reliable proofreading tool for students.
Try for free
This part of the introduction differs depending on what approach your paper is taking.
In a more argumentative paper, you’ll explore some general background here. In a more empirical paper, this is the place to review previous research and establish how yours fits in.
Argumentative paper: Background information
After you’ve caught your reader’s attention, specify a bit more, providing context and narrowing down your topic.
Provide only the most relevant background information. The introduction isn’t the place to get too in-depth; if more background is essential to your paper, it can appear in the body .
Empirical paper: Describing previous research
For a paper describing original research, you’ll instead provide an overview of the most relevant research that has already been conducted. This is a sort of miniature literature review —a sketch of the current state of research into your topic, boiled down to a few sentences.
This should be informed by genuine engagement with the literature. Your search can be less extensive than in a full literature review, but a clear sense of the relevant research is crucial to inform your own work.
Begin by establishing the kinds of research that have been done, and end with limitations or gaps in the research that you intend to respond to.
The next step is to clarify how your own research fits in and what problem it addresses.
Argumentative paper: Emphasize importance
In an argumentative research paper, you can simply state the problem you intend to discuss, and what is original or important about your argument.
Empirical paper: Relate to the literature
In an empirical research paper, try to lead into the problem on the basis of your discussion of the literature. Think in terms of these questions:
- What research gap is your work intended to fill?
- What limitations in previous work does it address?
- What contribution to knowledge does it make?
You can make the connection between your problem and the existing research using phrases like the following.
Now you’ll get into the specifics of what you intend to find out or express in your research paper.
The way you frame your research objectives varies. An argumentative paper presents a thesis statement, while an empirical paper generally poses a research question (sometimes with a hypothesis as to the answer).
Argumentative paper: Thesis statement
The thesis statement expresses the position that the rest of the paper will present evidence and arguments for. It can be presented in one or two sentences, and should state your position clearly and directly, without providing specific arguments for it at this point.
Empirical paper: Research question and hypothesis
The research question is the question you want to answer in an empirical research paper.
Present your research question clearly and directly, with a minimum of discussion at this point. The rest of the paper will be taken up with discussing and investigating this question; here you just need to express it.
A research question can be framed either directly or indirectly.
- This study set out to answer the following question: What effects does daily use of Instagram have on the prevalence of body image issues among adolescent girls?
- We investigated the effects of daily Instagram use on the prevalence of body image issues among adolescent girls.
If your research involved testing hypotheses , these should be stated along with your research question. They are usually presented in the past tense, since the hypothesis will already have been tested by the time you are writing up your paper.
For example, the following hypothesis might respond to the research question above:
Here's why students love Scribbr's proofreading services
Discover proofreading & editing
The final part of the introduction is often dedicated to a brief overview of the rest of the paper.
In a paper structured using the standard scientific “introduction, methods, results, discussion” format, this isn’t always necessary. But if your paper is structured in a less predictable way, it’s important to describe the shape of it for the reader.
If included, the overview should be concise, direct, and written in the present tense.
- This paper will first discuss several examples of survey-based research into adolescent social media use, then will go on to …
- This paper first discusses several examples of survey-based research into adolescent social media use, then goes on to …
Full examples of research paper introductions are shown in the tabs below: one for an argumentative paper, the other for an empirical paper.
- Argumentative paper
- Empirical paper
Are cows responsible for climate change? A recent study (RIVM, 2019) shows that cattle farmers account for two thirds of agricultural nitrogen emissions in the Netherlands. These emissions result from nitrogen in manure, which can degrade into ammonia and enter the atmosphere. The study’s calculations show that agriculture is the main source of nitrogen pollution, accounting for 46% of the country’s total emissions. By comparison, road traffic and households are responsible for 6.1% each, the industrial sector for 1%. While efforts are being made to mitigate these emissions, policymakers are reluctant to reckon with the scale of the problem. The approach presented here is a radical one, but commensurate with the issue. This paper argues that the Dutch government must stimulate and subsidize livestock farmers, especially cattle farmers, to transition to sustainable vegetable farming. It first establishes the inadequacy of current mitigation measures, then discusses the various advantages of the results proposed, and finally addresses potential objections to the plan on economic grounds.
The rise of social media has been accompanied by a sharp increase in the prevalence of body image issues among women and girls. This correlation has received significant academic attention: Various empirical studies have been conducted into Facebook usage among adolescent girls (Tiggermann & Slater, 2013; Meier & Gray, 2014). These studies have consistently found that the visual and interactive aspects of the platform have the greatest influence on body image issues. Despite this, highly visual social media (HVSM) such as Instagram have yet to be robustly researched. This paper sets out to address this research gap. We investigated the effects of daily Instagram use on the prevalence of body image issues among adolescent girls. It was hypothesized that daily Instagram use would be associated with an increase in body image concerns and a decrease in self-esteem ratings.
The introduction of a research paper includes several key elements:
- A hook to catch the reader’s interest
- Relevant background on the topic
- Details of your research problem
and your problem statement
- A thesis statement or research question
- Sometimes an overview of the paper
Don’t feel that you have to write the introduction first. The introduction is often one of the last parts of the research paper you’ll write, along with the conclusion.
This is because it can be easier to introduce your paper once you’ve already written the body ; you may not have the clearest idea of your arguments until you’ve written them, and things can change during the writing process .
The way you present your research problem in your introduction varies depending on the nature of your research paper . A research paper that presents a sustained argument will usually encapsulate this argument in a thesis statement .
A research paper designed to present the results of empirical research tends to present a research question that it seeks to answer. It may also include a hypothesis —a prediction that will be confirmed or disproved by your research.
Cite this Scribbr article
If you want to cite this source, you can copy and paste the citation or click the “Cite this Scribbr article” button to automatically add the citation to our free Citation Generator.
Caulfield, J. (2023, March 27). Writing a Research Paper Introduction | Step-by-Step Guide. Scribbr. Retrieved April 17, 2024, from https://www.scribbr.com/research-paper/research-paper-introduction/
Is this article helpful?

Jack Caulfield
Other students also liked, writing strong research questions | criteria & examples, writing a research paper conclusion | step-by-step guide, research paper format | apa, mla, & chicago templates, "i thought ai proofreading was useless but..".
I've been using Scribbr for years now and I know it's a service that won't disappoint. It does a good job spotting mistakes”
Depression Research Paper

This sample depression research paper features: 5700 words (approx. 19 pages), an outline, and a bibliography with 7 sources. Browse other research paper examples for more inspiration. If you need a thorough research paper written according to all the academic standards, you can always turn to our experienced writers for help. This is how your paper can get an A! Feel free to contact our writing service for professional assistance. We offer high-quality assignments for reasonable rates.

Academic Writing, Editing, Proofreading, And Problem Solving Services
Get 10% off with 24start discount code.
Even for professionals the use of the term depression can vary. In 1987, Kendall and colleagues noted that “The professional use of the term depression has several levels of reference: symptom, syndrome, nosologic disorder . . . . Depression itself can be a symptom – for example, being sad. As a syndrome, depression is a constellation of signs and symptoms that cluster together . . . . The syndrome of depression is itself a psychological dysfunction but can also be present, in secondary ways, in other diagnosed disorders. Finally, for depression to be a nosologic category careful diagnostic procedures are required during which other potential diagnostic categories are excluded. The presumption, of course, is that a discrete nosologic entity will ultimately prove to be etiologically distinct from other discrete entities, with associated differences likely in course, prognosis, and treatment response.” It is this likely nosologic disorder of depression that we will discuss.
I. Definition of Depression
A. symptoms of depression, b. comorbidity: the relationship between depression and anxiety, ii. diagnostic classification, a. major depressive disorder, b. dysthymic disorder, c. bipolar i disorder, d. bipolar ii disorder, e. cyclothymic disorder, iii. exploratory categories of depressive disorders, a. premenstrual dysphoric disorder, b. minor depressive disorder, c. recurrent brief depressive disorder, d. mixed anxiety-depressive disorder, iv. epidemiology, a. prevalence, 1. national prevalence, 2. international prevalence, b. age differences, c. sex and ethnic differences, d. environmental correlates, v. etiological theories of depression, a. psychological theories, 1. psychoanalytic approaches, 2. interpersonal approaches, 3. cognitive approaches, b. biological theories, 1. genetic approaches, 2. neurotransmitter approaches, vi. protective factors, a. social support, b. coping styles.
Any definition of depression must begin with the fourth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV). The DSM-IV represents the official diagnostic classification system of the American Psychiatric Association and provides the criteria that are used to diagnosis depression. These criteria consist of the symptoms of depression. In order to make a diagnosis of depression, at least five out of nine possible symptoms must be present. These include (1) depressed mood; (2) diminished pleasure or interest in activities; (3) significant weight loss or weight gain; (4) insomnia or hypersomnia; (5) agitation; (6) fatigue or loss of energy; (7) thoughts of worthlessness or inappropriate guilt; (8) diminished concentration ability; and (9) thoughts of death or suicide.
Symptoms of depression may vary according to an individual’s age and culture. Children who are depressed, for instance, may express symptoms of irritability rather than sadness. They may also fail to make expected weight gains rather than lose weight. On the other end of the age continuum, older adults are more likely than younger adults to experience symptoms such as loss of appetite, loss of interest, and thoughts of death. Cultural differences also exist in report of depressive symptoms. One study, for example, found that depressed Jewish patients reported more somatic symptoms, and less guilt, than did non-Jewish patients. Another study that examined depressive symptomatology in American, Korean, Philippine, and Taiwanese college students found that Taiwanese students reported the lowest numbers of somatic symptoms and the highest numbers of affective symptoms. The other ethnic groups reporting similar levels of these symptoms. One’s age and culture thus seems to affect how depression is expressed.
Comorbidity refers to the occurrence of more than one disorder at the same time. Although researchers and clinicians generally acknowledge depression as a distinct disorder, it does overlap with a variety of other difficulties. Much current research on this overlap has focused on the relationship between anxiety and depression. This is not surprising, given the high rates of comorbidity found in studies of the two disorder types. For example, one study found that 63% of a group of patients with panic disorder also experienced major depression. One possible explanation provided for such overlap lies in the concept of “negative affectivity.” In 1984, Watson and Clark described individuals with high levels of negative affectivity as having a tendency “to be distressed and upset and have a negative view of self, whereas those low on the dimension are relatively content and secure and satisfied with themselves.” Other characteristics of high negative affectivity include nervousness, tension, worry, anger, scorn, revulsion, guilt, self-dissatisfaction, rejectedness, and sadness.
Both anxiety and depression seem to consist of high negative affectivity. There are however, important differences between depression and anxiety. While both depression and anxiety are characterized by high levels of negative affect, only depression is related to lowered levels of positive affect. Thus, depressed individuals tend to display both high negative affect and low positive affect, whereas anxious individuals display high negative affect and may or may not have lowered positive affect–the level of positive affect is unrelated to one’s anxiety state. Research on negative affect as a link between anxiety and depression is continuing at a rapid pace.
Earlier we noted the DSM-IV. The DSM-IV is the most widely used classification scheme for psychiatric disorders in North America. According to this manual, there are five types of mood disorders that include depression as a significant component. These are (1) Major Depressive Disorder; (2) Dysthymic Disorder; (3) Bipolar I Disorder; (4) Bipolar II Disorder; and (5) Cyclothymic Disorder. Each of these classifications differs in terms of etiology, course, and symptomatology.
For a diagnosis of Major Depressive Disorder (MDD), DSM-IV specifies that at least five symptoms must occur for a period of at least 2 weeks. Chief among these symptoms is depressed mood that occurs most of the day, nearly every day for at least 2 weeks, or significantly diminished interest or pleasure in virtually all activities most of the day, nearly every day for the 2-week period.
MDD can be further classified according to severity (i.e., mild, moderate, severe without psychotic features, severe with psychotic features), course (e.g., single episode versus recurrent episodes), and presentation (e.g., with catatonic features, with melancholic features). Psychotic features of depression include such experiences as delusions (i.e., false beliefs) and hallucinations (i.e., sensory experiences that have no basis in reality). A delusion, for example, would be a person who believes that she is dead. Catatonic features of depression involve psychomotor disturbances such as excessive movement or stupor. Melancholic features include the inability to experience pleasure even when good things happen and a lack of interest in previously pleasurable activities. No matter what the specific characteristics of a given individual’s disturbance, MDD is, by definition, extremely distressing to the sufferer and is associated with significant impairment in important areas of the person’s life (e.g., at work, home or school).
Dysthymic Disorder is characterized by a chronic depressed mood that lasts at least 2 years in adults and at least 1 year in children and adolescents. This depressed mood is accompanied by at least two of the following six depressive symptoms: (1) poor appetite or overeating; (2) insomnia or hypersomnia; (3) low energy or fatigue; (4) low self-esteem; (5) poor concentration or difficulty making decisions; and (6) feelings of hopelessness. As fewer depressive symptoms are required to make a diagnosis, Dysthymic Disorder is often considered a milder form of depression than MDD. However, it can be just as upsetting to the sufferer and can cause just as much impairment. In addition, Dysthymic Disorder may occur in combination with episodes of major depression. When Dysthymic Disorder occurs along with major depression, the individual is considered to be suffering from a “double depression.” The co-occurrence of MDD and dysthymia is not uncommon.
The hallmark characteristic of Bipolar I Disorder is mania. According to DSM-IV, a manic episode is characterized by elevated, expansive, or irritable mood that is persistent and distinctly different from normal elevated or irritable moods. This period is accompanied by at least three of seven possible symptoms. These symptoms include (1) inflated self-esteem; (2) a decreased need for sleep; (3) unusual talkativeness; (4) the feeling that one’s thoughts are racing; (5) increased distractibility; (6) increased activity; (7) involvement in pleasurable but potentially harmful activities (e.g., sexual indiscretions).
Bipolar I Disorder is typically recurrent; according to DSM-IV, additional episodes occur in more than 90% of individuals who have had a single manic episode. The manic episodes of those with Bipolar I Disorder are often intermixed with periods of depression. Like those with MDD, people with Bipolar I Disorder may exhibit psychotic, catatonic, and melancholic features as part of either their mania or their depression.
Bipolar II Disorder is characterized by periods of hypomania intermixed with periods of depression. Hypomanic episodes are characterized by the same symptoms as manic episodes. However, hypomanic episodes are shorter (e.g., 4 days in duration) and are associated with less impairment. While manic episodes may include psychotic features, interrupt daily functioning, and require hospitalization, hypomanic episodes typically do not. The depression experienced as part of Bipolar II Disorder, however, can be just as severe as that experienced in MDD and Bipolar I Disorder.
Cyclothymic disorder is characterized by hypomanic periods intermixed with depressive periods that are not as severe as those experienced in MDD, Bipolar I Disorder, and Bipolar II Disorder. In Cyclothymia, the periods of mood disturbance may alternate rapidly, with little respite from affective difficulties. For a diagnosis of Cyclothymia these periods of shifting moods must be problematic for at least 2 years in adults and at least i year in children and adolescents.
In addition to the five official diagnoses, DSM-IV has denoted four classifications for further study that include depression as a significant component. Such classifications are not yet considered to be disorders and more information is needed on factors such as symptom presentation, etiology, and degree of impairment to sufferers before these might be considered disorders in their own right. Nevertheless, these may represent serious problems and even though they are currently exploratory, we describe them here. They are: (1) Premenstrual Dysphoric Disorder; (2) Minor Depressive Disorder; (3) Recurrent Brief Depressive Disorder; and (4) Mixed Anxiety-Depressive Disorder.
Premenstrual Dysphoric Disorder is characterized by several hallmark symptoms of depression (e.g., decreased interest in usual activities, depressed mood, difficulty sleeping or sleeping too much) in addition to symptoms such as affective lability, feelings of being overwhelmed or out of control, and food cravings. In order to meet the criteria that have been proposed for this diagnosis, such symptoms must have occurred during the late luteal phase of most of a woman’s menstrual cycles in the past year. As a number of authors have pointed out, such a classification has potentially serious social, political, and legal ramifications for women. For example, some have argued that if this classification is adopted as an orificial diagnosis then women might be stigmatized as more unstable than or inferior to men. Arguments such as this keep the classification of Premenstrual Dysphoric Disorder a topic of considerable debate.
Minor Depressive Disorder is characterized by fewer depressive symptoms than are seen in MDD. The level of impairment is also less than that associated with MDD. To meet the proposed criteria for Minor Depressive Disorder, a person must demonstrate either a depressed mood or loss of interest and two additional symptoms of a Major Depressive Episode. If this classification were included in future DSM editions as a disorder, it would constitute a residual category to be used only after the other mood disorders have been ruled out.
The principle difference between Recurrent Brief Depressive Disorder and MDD is one of duration. Recurrent Brief Depressive Disorder is characterized by periods of depression that meet all of the criteria for a Major Depressive Episode except for the duration requirement. While in major depressive episodes, symptoms must last at least 2 weeks, in recurrent brief depressive episodes, symptoms must last at least 2 but less than 14 days. In addition, these brief episodes must occur at least once a month for 12 months to meet criteria for the classification of Recurrent Brief Depressive Disorder. Recurrent Brief Depressive Disorder is quite similar to MDD in its age of onset and family incidence rates, thus raising questions as to whether this should be considered a distinct disorder.
The impetus behind a mixed anxious-depressed category lies in the finding that there are many people suffering from symptoms of anxiety and depression who do not meet criteria for any DSM anxiety or mood disorder, but who are nonetheless significantly impaired by their difficulties. The classification of Mixed Anxiety-Depressive Disorder is characterized by a dysphoric mood for at least 1 month in addition to at least four additional symptoms that primarily reflect anxiety (e.g., mind going blank, worry, hypervigilance). The primary argument in favor of adopting this proposed disorder is that it would cover the large number of people who have significant impairment linked to depression and anxiety but who do not fall into any currently existing diagnostic category. The primary argument against this classification is that people suffering from both depression and anxiety could in fact be categorized into already existing disorders with the use of more precise assessment methods.
Epidemiology refers to information about the incidence and prevalence of disorders in a population. A prevalence rate refers to the number of people who have a given disorder during a particular time period (e.g., the percentage of people in given location diagnosed with MDD within a 1-year period of time). An incidence rate refers to the number of new cases of a disorder which occur during a given time period (e.g., the number of people diagnosed with Dysthymic Disorder during April 1996). Because the distribution of a disorder can be examined to determine whether it correlates with other factors, epidemiological information can be important for understanding some of the possible causes and correlates of depression.
Two recent large-scale surveys of psychopathology in the United States have provided differing prevalence data on depression. Using diagnostic criteria from the revised 3rd Edition of the DSM (DSM-III-R), the Epidemiologic Catchment Area (ECA) study examined the rates of depression in five sites: New Haven, Baltimore, St. Louis, Los Angeles, and Durham. The ECA study found the lifetime prevalence of major depression (i.e., the number of people experiencing major depression during any point in life) to be 4.9% and the lifetime prevalence of dysthymia to be 3.2%. Alternatively, the National Comorbidity Survey (NCS) reported much higher prevalence rates: 14.9% for lifetime major depression and 6.4% for dysthymia. The discrepancies between these two studies may be accounted for by the different assessment instruments used, slightly different diagnostic criteria employed, and different age ranges studied (i.e., the ECA sample was 18 years of age or older, whereas the NCS sample ranged in age from 15 to 54 years). According to the ECA study, prevalence rates for bipolar disorders were much lower; lifetime prevalence of these disorders was .8% for Bipolar I and .5% for Bipolar II. The NCS lifetime prevalence for manic episode was somewhat higher: 1.6 %. Even though these epidemiological studies reported somewhat discrepant rates, they are in agreement that mood disorders are relatively common in the United States.
A number of studies have examined the community prevalence of major depression in countries besides the United States. International lifetime prevalence rates vary widely, from a low of 3.3% in Seoul to a high of 15.1% among New Zealand residents aged 25 to 46. While such differences may indeed reflect true international differences in the occurrence of depression, other factors such as cultural differences in the sensitivity of the instruments used to assess disorder and different sample ages may also account for this range. In prevalence studies focusing on bipolar illness, ranges from .07% in Sweden to 7% in Ireland have been reported. Most studies, however, place prevalence at about 1% for bipolar illnesses, consistent with data from the ECA and NCS studies.
The ECA study also reported incidence rates of depression for various age groups. For men, major depression was highest among those aged 18 to 29. A large decline in incidence was noted for men aged 45 and older. For women, the incidence of major depression was highest in the group aged 30 to 44 and did not decline until age 65.
According to the ECA study, lifetime prevalence rates of major depression, dysthymia, and all mood disorders are approximately twice as high for women as for men. Women’s lifetime rates were 7.0%, 4.1%, and 10.2%, respectively, while rates for men were 2.6%, 2.2 %, and 5.2 %, respectively. These differences occur across a variety of ethnic groups (e.g., African American, Hispanic, Caucasian) even when differences in education, income, and occupations are controlled. Sex differences are also found in countries besides the United States. While sex differences in depression are among the most stable of findings across studies, no sex differences in the rates of bipolar disorder are reliably found.
Although sex difference in the incidence of depression occur across different ethnic groups, there are some differences among these groups overall. For instance, the ECA study found higher rates of Major Depression and Dysthymia among Caucasians and Hispanics than among African Americans. However, few difference in the rates of bipolar disorders among the three groups were found.
The ECA study also examined a number of environmental correlates of depression and bipolar disorders. This study found that people who were separated or divorced had higher 1-year prevalence rates of major depression (6.3%) than those who were never married (2.8%), currently married (2.1%), or widowed (2.1%). This was also true of those with bipolar disorders, although the rates for those separated or divorced versus never married were nearly identical (1.7% versus 1.6%). The 1-year prevalence rate of major depression was also higher among the unemployed than the employed (3.4% versus 2.2%), but the rate was nearly identical for those with bipolar disorders (1.1% versus 1.0%). In addition, the ECA study found higher rates of major depression among white-collar workers and those with at least 12 years of education, but lower rates of depression among those with annual incomes of $15,000 or more. Consistent with the major depression findings, bipolar disorders were also less prevalent among those with annual incomes of $15,000 or more. Bipolar disorders were also found to be the most prevalent among none-white-collar workers with less than 12 years of education. Overall, these socioeconomic status differences were quite small.
A variety of different psychological theories of the causes of depression have been proposed. These can be grouped in psychoanalytic, interpersonal, and cognitive.
The first psychoanalytic writers to theorize about the etiology of depression were Sigmund Freud and his student, Karl Abraham. As would be expected, there are a number of similarities in the theories proposed by Freud and Abraham. First, both Freud and Abraham believed that some people are predisposed to experience depression. For Abraham, this predisposition consisted of anatomical anomalies that allowed a person to experience a great deal of oral eroticism. For Freud, this predisposition consisted of narcissistic object choices (e.g., object choices which are so similar to the self that love of the object is truly love of self). Second, both believed that a predisposition to experience depression was not, in and of itself, enough to cause depression. In order to experience a depression, a predisposed individual must also experience the loss of a loved object (e.g., through death or rejection).
Despite these basic similarities, the two theorists diverge somewhat on how depression occurs once a loss has been experienced. For Abraham, the loss of a loved object in a person predisposed to depression triggers a regression to the oral stage of psychosexual development. Such a regression is meant to achieve three purposes: (1) to increase pleasure; (2) to hold on to the object through oral incorporation; and (3) to discharge one’s aggressive impulses on to the object. Such a regression manifests itself most saliently in the depressive symptoms of eating too much or too little. For Freud, the loss of a loved object possesses different implications. Since the lost object was a narcissistic choice and thus represented the self, loss of the object means loss of the self. This loss of self triggers feelings of anger and depression. The energy associated with these negative feelings is withdrawn from the lost object and brought inward, in a process called introjection. Thus, depression as conceptualized by Freud is often summarized as “anger turned inward.” For Freud, the difference between sadness and “true” depression was the difference between “this is awful” and “I am awful.” Freud further extended his theory to account for the mania characteristic of bipolar depressive disorders. He hypothesized that, once the feelings of anger and depression over loss of the object are resolved, the energy associated with these negative feelings is freed for other purposes. In a person with bipolar disorder, this freed energy is used to zealousy search for new objects, thus accounting for the symptoms of mania.
More recent psychoanalytic theorists have focused on the superego’s role in depression. Some theorists, for example, have suggested that depression is distinguished from other states such as shame, apathy, or resentment by the presence of guilt. As guilt results only from an intrapsychic conflict of the superego, the superego is necessarily implicated in depression. One result of these differences in etiological focus has been the proposition of two forms of depression: anaclitic and introjective. Anaclitic depression is characterized by feelings of helplessness, inferiority, and being unloved. Anaclitic depression is proposed to be associated with the earlier stages of development and is most closely associated with the theorizing of Abraham and Freud. Alternatively, introjective depression focuses on feelings of unworthiness and failure to measure up to expectations and standards. It is associated with later stages of development, and more closely aligned with the works of later psychoanalytic theorists. Although much of psychoanalytic theory has been criticized on grounds that it has not been empirically tested, the distinction between anaclitic and introjectire depressions has been empirically examined and found to be valid. Psychoanalytic theorists have accounted for the development of bipolar disorders as well. Most notable amongst these theorists is Melanie Klein, who expanded upon the work of Freud.
Interpersonal approaches to the etiology and maintenance of depression focus on the interplay between a depressed person and his or her relations with others. Empirical research in this area has taken several directions. For example, some researchers focus on the role of social skills in depression, asking such questions as whether depressed people have poor social skills and whether the lack of such skills results in decreased reinforcement from others and consequent depression. Other research has evaluated the types of communications depressed people emit (e.g., sadness, hopelessness) and the effects these communications have on others. If others find the communications of depressed persons aversive, they will likely avoid such persons, which may then exacerbate depressive symptoms such as isolation and loneliness. Still others address the interplay between stress, social support, and depression. All of these lines of research have found some support; interpersonal research highlights the fact that depression is caused by a multitude of factors in interplay with one another.
Much of the research converges on the theoretical idea that depression is maintained by a vicious cycle that is caused by disruptions in interpersonal interactions. For instance, many depressed individuals quite understandably seek out social support from others. If this support does not alleviate the negative feelings, further support is sought. This intensified support seeking, however, has the paradoxical effect of pushing away those who have been supportive. That is, as individuals begin to feel that their support capacity has been exhausted they pull back from the depressed person, leading to an even further intensification of social support seeking, and the further distancing of potentially supportive people.
Interpersonal factors in the etiology of bipolar depressive disorders have not received as much research attention as such factors in unipolar depressive disorders. Nonetheless, persons with both types of depressive disorders seem to have difficulties in retaining social support. Indeed, in one recent study, people with bipolar disorder perceived their social supports as less available to them and as less adequate in the amount of support received than people in a community sample. Furthermore, perceptions of social support availability seemed to decrease as the duration of illness increased. Thus, it seems likely that social support plays a role in bipolar as well as unipolar depressive disorders.
Currently, cognitive approaches are among the most widely studied theories in the etiology of depression. One of the most influential of these theories was proposed by Aaron Beck in 1967. Beck argued that all individuals possess cognitive structures called schemas that guide the ways information in the environment is attended to and interpreted. Such schemas are determined from childhood by our interactions with the external world. For example, a child who is constantly criticized may begin to believe she is worthless. She might then begin to interpret every failure experience as further evidence of her worthlessness. If this negative processing of information is not changed, it will become an enduring part of her cognitive organization, that is, a schema. When this schema is activated (e.g., by a poor grade on a test or any other failure experience), it will predispose her to depressive feelings (e.g., I’m no good). Beck stated that, as a result of this faulty information processing, depressed persons demonstrate a cognitive triad of negative thoughts about themselves, the world, and the future. He further extended his argument to include the manic phases of bipolar depressive disorders. Beck stated that such phases are characterized by a manic triad of irrationally positive thoughts about oneself, the world, and the future. Like the depressive triad in unipolar depressive disorders, the manic triad in bipolar depressive disorders was hypothesized to lead to the symptoms of mania, such as inflated selfesteem and extremely elevated mood.
There is widespread agreement that depression can be caused by different factors. Some theorists have argued that dysfunctional cognitions cause only a subset of depressions. Termed the “negative cognition” subtype, this type of depression is brought about by either the kinds of schemas discussed by Aaron Beck or by dysfunctional attributional patterns that lead depressed people to take responsibility for the occurrence of negative events, and to avoid taking responsibility for positive events. This dysfunctional attributional pattern can lead to a sense of hopelessness that results in a “hopelessness depression,” a component of negative cognition depression.
Although there are a variety of biologically based theories of depression, they can be broken down into two general approaches: genetic and neurotransmitter.
Genetic approaches suggest that depression is the result of inheriting genes that predispose to occurrence of depression. Three types of studies that are used to investigate genetic inheritance of depression illustrate this approach. These studies consist of family studies, twin studies, and adoption studies. In a typical family study, families with a depressed member are interviewed to determine how many other family members have or had an affective disorder. In twin studies, the concordance rate of affective disorder between monozygotic and dizygotic twin pairs is compared. Because monozygotic twins have identical genes, if genetic theories are correct then concordance rates of depression should be higher than for dizygotic twins (who have similar but not identical genes). In adoption studies, two strategies are most often used. In the first, the rate of depressive disorder in the biological parents of adopted persons with and without affective disorders is compared. In the second, the rate of depressive disorders is compared between adopted children with and without affectively disordered biological parents. Adoption studies have an advantage over family and twin studies, as the effects of environment on affective disorder are reduced in this design. However, adoption studies constitute the least-used approach to investigating genetic factors in depression; the difficulty of obtaining complete records on adoptees and their biological parents makes this design quite prohibitive.
Despite design differences, all three genetic approaches to the etiology of depression have yielded similar results: depression is heritable to at least some degree. A recent review of the research literature, for example, found rates of affective disorders among first-degree relatives of unipolar-disordered individuals ranging from 11.8% to 32.2%. Rates of affective disorders among first-degree relatives of bipolardisordered individuals ranged from 10.6% to 33.1%. Rates of affective disorder among first-degree relatives of normal individuals ranged from 4.8% to 6.3. In twin studies of unipolar and bipolar depression, concordance rates ranged from .04 to 1.0 for monozygotic twins, and from 0.0 to .43 to dizygotic twins, with the majority of studies reviewed reporting no concordance for dizygotic twins. The results of genetic investigations clearly suggest that there is a genetic component to depression, although the exact nature and functioning of this component is thus far still unknown.
Research on brain chemistry as an etiological factor in unipolar depression has focused on two monoamine neurotransmitters: norepinephrine (NE) and serotonin (5-HT). Initially, researchers believed that depression was due to a lack of NE in the brain, and later, to a lack of both NE and 5-HT. However, several difficulties with these hypotheses arose: (1) While the effects of antidepressants on monoamine levels start within hours of taking the medication, decreased depression levels do not become apparent until weeks later. (2) Some drugs that do not affect monoamine levels alleviate depression. (3) Some drugs that increase monoamine levels do not alleviate depression. Thus, researchers have directed their efforts to investigating more complicated relations between these neurotransmitters and depression. Recent efforts have included the study of receptor site hyposensitivity, relationships between NE and 5-HT, and relationships between. 5-HT and the neurotransmitter dopamine (DA).
Research on brain chemistry as in etiological factor in bipolar depression has followed much the same course as such research on unipolar depression. Initially, researchers believed that the mania characteristic of bipolar disorders was due to excesses of the neurotransmitters NE and 5-HT, exactly opposite the belief for depression. However, difficulties arose with this hypothesis, including findings that (1) lithium, the medical treatment of choice for bipolar disorder which seems to affect both NE and 5-HT, was effective at controlling both depression and mania, and (2) both depression and mania may be characterized by lower levels of 5-HT. Thus, as with unipolar depression, researchers of bipolar depression have begun investigating more complicated relationships between bipolar depression and neurotransmitters. Similar to the recent efforts concerning unipolar depression, researchers have investigated interactions between 5-HT and DA, interactions between NE and DA, and receptor site hypersensitivity. These types of investigations represent promising areas of research in elucidating the multifaceted etiology of depression. Certainly, biology and psychology are implicated in the causes of depression, both unipolar and bipolar forms.
Given the potentially devastating effects of depression, many researchers have devoted their efforts to studying factors that decrease the likelihood of becoming depressed or decrease the amount of time spent in depressive episodes. Among the most widely studied of such protective factors are social support and coping styles.
There are numerous facets to the concept of social support. For example, social support can be conceived as the number of persons one can rely on for support. Social support can also be conceived as the amount of support received, regardless of the number of persons one receives support from. In addition, socially supportive relationships can be conceptualized on a continuum of quality from very poor to very good. Examination of all these facets has proven important in understanding relationships between depression and social support.
Overall, people in contact with numerous socially supportive persons are less likely to have mental health difficulties, including depression. In addition, those who perceive a great deal of support from others are less likely to be negatively affected by stressors that might lead to depression. For people who have become depressed, having a confidant such as a spouse or best friend and a supportive family is related to greater success in treatment. The quality of such relationships is also important to treatment. In one study, for example, depressed persons with good-quality confidant relationships needed shorter periods of treatment than those with poor-quality confidant relationships.
The effects of social support for people with bipolar depressive disorders have not been as well studied as the effects for people with unipolar depressive disorders. Nonetheless, research suggests that social support is indeed beneficial for people with bipolar disorders. In one study, for example, a great deal of available social support was related to fewer psychological symptoms, better social adjustment, and better overall functioning.
Ways of coping with stressors can be roughly divided into two categories: approach strategies and avoidance strategies. Approach strategies are characterized by identifying the problematic situation, devising reasonable solutions to it, an implementing those solutions. Avoidance strategies include trying not to think about the problem, wishing the problem did not exist, and fantasizing about life without the problem. Overall, approach strategies seem to help people cope with stressors that might otherwise lead to depression. In addition, use of approach strategies is associated with better treatment outcome for those who become depressed. Conversely, people who use avoidance strategies to cope with stress seem more likely to become depressed and to have poorer treatment outcomes.
As with the effects of social support, research on coping styles among people with bipolar depressive disorders is scarce. Nonetheless, one recent study that examined differences in coping between high- and low-functioning people with bipolar disorders suggested that avoidant coping styles are associated with poorer functioning. Thus, relationships between coping styles and bipolar depressive disorders and coping and unipolar depressive disorders may be similar.
Bibliography:
- Beck, A. T. (1967). Depression: Causes and treatment. Philadelphia: University of Pennsylvania Press.
- Beckham, E. E., & Leber W. R. (1995). (Eds.). Handbook of depression (2nd ed. ). New York: Guilford Press.
- Cicchetti, D., & Toth, S. L. (1992). (Eds.). Developmental perspectives on depression. Rochester, NY: University of Rochester Press.
- Craig, K. D., & Dobson, K. S. (1995). (Eds.). Anxiety and depression in children and adults. Thousand Oaks, CA: Sage.
- Kendall, P. C., Hollon, S. D., Beck, A. T., Hammen, C. L., & Ingram, R. E. (1987). Issues and recommendations regarding use of the Beck Depression Inventory. Cognitive Therapy and Research, 11,289-299.
- Ingrain, R. E., Miranda, J., & Segal, Z. V. (in press). Cognitive vulnerability to depression. New York: Guilford Press.
- Robins, L. N., & Regier, D. A. (1991). (Eds.). Psychiatric disorders in America. New York: The Free Press.
ORDER HIGH QUALITY CUSTOM PAPER

An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Indian J Psychiatry
- v.52(Suppl1); 2010 Jan
An overview of Indian research in depression
Sandeep grover.
Department of Psychiatry, Postgraduate Institute of Medical Education and Research, Chandigarh, India
Alakananda Dutt
Ajit avasthi.
Depression as a disorder has always been a focus of attention of researchers in India. Over the last 50-60 years, large number of studies has been published from India addressing various aspects of this commonly prevalent disorder. The various aspects studied included epidemiology, demographic and psychosocial risk factor, neurobiology, symptomatology, comorbidity, assessment and diagnosis, impact of depression, treatment related issues and prevention of depression in addition to the efficacy and tolerability of various antidepressants. Here, we review data on various aspects of depression, originating from India.
INTRODUCTION
Depression is a disorder of major public health importance, in terms of its prevalence and the suffering, dysfunction, morbidity, and economic burden. Depression is more common in women than men. The report on Global Burden of Disease estimates the point prevalence of unipolar depressive episodes to be 1.9% for men and 3.2% for women, and the one-year prevalence has been estimated to be 5.8% for men and 9.5% for women. It is estimated that by the year 2020 if current trends for demographic and epidemiological transition continue, the burden of depression will increase to 5.7% of the total burden of disease and it would be the second leading cause of disability-adjusted life years (DALYs), second only to ischemic heart disease.[ 1 ] In view of the morbidity, depression as a disorder has always been a focus of attention of researchers in India. Various authors have tried to study its prevalence, nosological issues, psychosocial risk factors including life events, sympto matology in the cultural context, comorbidity, psychoneurobiology, treatment, outcome, prevention, disability and burden. Some of the studies have also tried to address various issues in children and elderly.
This review focuses on research done on various depressive disorders in India. For this, a thorough internet search was done using key words like depression, life events, prevalence, classification, cultural issues, outcome, prevention, disability and burden etc in various combinations. The various search engines like Pubmed, Google Scholar, Sciencedirect, Search Medica, Scopus, And Medknow etc were used. In addition thorough search of all the issues of Indian Journal of Psychiatry available online was done. Hand search of some of the missing issues was also attempted and this yielded a few more articles. Review articles which were felt to be not reflecting the Indian scenario to a large extent or not covering the available Indian data were excluded. Treatment issues (antidepressants) are reviewed separately by us in this compilation of annotations to be published. Data from animal studies and originating in the form of case reports and small case series, until felt necessary haven’t been included. The available data has been organized under the headings of epidemiology, demographic and psychosocial risk factors, neurobiology, symptomatology, comorbidity, assessment and diagnosis, impact of depression, treatment related issues and prevention of depression.
Epidemiology
Many studies have estimated the prevalence of depression in community samples and the prevalence rates have varied from 1.7 to 74 per thousand population.[ 2 , 3 ] Reddy and Chandrasekhar[ 2 ] carried out a metanalysis, which included 13 studies on epidemiology of psychiatric disorders which include 33572 subjects from the community and reported prevalence of depression to be 7.9 to 8.9 per thousand population and the prevalence rates were nearly twice in the urban areas.[ 2 ] The findings with regard to prevalence in urban population are in line with the findings of a survey done on the entire adult population of an industrial township, which showed that the prevalence rate for depression to be 19.4 per thousand.[ 4 ]
A recent large population-based study from South India, which screened more than 24,000 subjects in Chennai using Patient Health Questionnaire (PHQ)-12 reported overall prevalence of depression to be 15.1% after adjusting for age using the 2001 census data.[ 5 ] In another recent study, Nandi et al .[ 3 ] compared the prevalence of depression in the same catchment area after a period of 20 years (first in 1972 and then in 1992) and reported that the prevalence of depression increased from 49.93 cases per 1000 population to 73.97 cases per 1000 population.[ 3 ] Studies done in primary care clinics/center have estimated a prevalence rate of 21-40.45%.[ 6 – 9 ] Studies done in hospitals have shown that 5 to 26.7% of cases attending the psychiatric outpatient clinics have depression.[ 10 – 13 ]
Studies on the elderly population, either in the community, inpatient, outpatient and old age homes have shown that depression is the commonest mental illness in elderly subjects.[ 14 – 19 ] Nandi et al .[ 14 ] studied psychiatric morbidity of the elderly population of a rural community in West Bengal. In a sample of 183 subjects (male 85, female 98) they found 60% of the population to be mentally ill with higher morbidity in women compared to men (77.6% and 42.4% respectively). There was significantly more morbidity in population in the age group 70-74 and 80+ as compared to normal population. The total mental morbidity rate was as high as 612/1000 population. Depression was the commonest illness of old age in this sample, the rate being 522/1000 population (101 cases out of 112 were diagnosed as cases of depression). Women had a higher rate of depression-704/1000 population. Another significant finding was the high rate of morbidity amongst the widowed persons.
An epidemiological study from rural Uttar Pradesh showed that psychiatric morbidity in the geriatric group (43.32%) was higher than in the nongeriatric group (4.66%) and most common psychiatric morbidity was neurotic depression, followed by manic-depressive psychosis depression, and anxiety state. Psychiatric morbidity was more prevalent in those who were socially, economically, and educationally disadvantaged.[ 15 ] Recent community-based studies have reported a prevalence rate of 21.7% to 45.9%.[ 20 , 21 ]
Chhabra and Kar[ 16 ] studied the profile of psychiatric disorders in elderly psychiatric inpatients and reported that mood disorders were the most common diagnosis (46.5%). Older studies from Gero-psychiatric clinics reported a prevalence of depression ranging from 13 to 22.2%.[ 22 , 23 ] A recent outpatient study, which evaluated psychiatric morbidity in 100 randomly selected elderly subjects attending geriatric clinic, found that 29% patients suffered from psychiatric illness of which depressive disorders were the most common.[ 17 ] Another study also reported depression to be the most common psychiatric diagnosis among the 1586 elderly subjects (age ≥60 years), who attended the Geriatric Clinic of the All India Institute of Medical Sciences, New Delhi.[ 24 ] In a study of old age home population, Guha and Valdiya[ 18 ] reported that major depressive disorder (13.4%) was the most common psychiatric diagnosis in this population.
With regard to epidemiology of depression in children and adolescents in a community sample from south India, Srinath et al .[ 25 ] reported a prevalence of 0.1% in the 4-16 year age group and no child in the age group 0-3 was diagnosed to have depression. Another study from north India reported an annual incidence rate of 1.61/1000 children in a community based study on school children.[ 26 ] Clinic-based studies have reported a prevalence rate of 1.2 to 9.2% for the affective dis orders, amongst which unipolar depression was the commonest category in most of the studies.[ 27 – 32 ] However, in a recent study evaluating the trend of various diagnoses in clinic population, Malhotra et al .[ 33 ] reported increase in prevalence of affective disorders from 2% to 13.49% in children (0-14 years) attending the psychiatric outpatient clinics. Studies done in women during and after pregnancy have reported incidence of post-natal depression to be 11%.[ 34 ]
Demographic and psychosocial risk factors for depression
In terms of sociodemographic variables studies have shown that depression is more common in women,[ 4 , 5 , 35 – 37 ] younger subjects,[ 13 ] in subjects from poor economic background[ 5 , 36 , 38 ] and subjects with poor nutritional status,[ 38 ] Muslims,[ 35 ] those who are divorced or widowed,[ 5 ] those residing in nuclear families[ 39 ] and urban areas.[ 2 ] Studies which have evaluated the subjects with late onset or old age depression (first episode of depression at or after the age of 50) have also shown that depression is more common in low social class, widowed state,[ 14 , 37 , 40 ] unemployed condition, low educational level, in subjects living in nuclear family or in those living alone.[ 15 , 21 , 37 , 40 ] With regard to gender most of the studies have reported that it is more common in elderly females,[ 14 , 37 , 40 ] however, some clinic-based studies suggest that it is more common in elderly males.[ 41 ] It is also seen that prevalence of depression increases with increasing age in elderly.[ 20 ]
Studies have shown that compared to healthy controls and subjects with schizophrenia, depressed patients have significantly greater number of life events prior (6-12 months) to the onset of their illness.[ 42 – 46 ] In terms of type of life events, it is seen that depressed patients experience significantly higher proportion of life events related to death of a family member, personal health related events, bereavement, interpersonal and social events[ 34 , 42 , 44 , 47 ] and lower number of life events in the form of illness of family members compared to patients with schizophrenia.[ 44 ]
It is also seen that compared to patients with mild depression patients with moderate and severe depression tend to use avoidance as a coping strategies more frequently for the stressful life events, suggesting that it may be a maladaptive way to cope with the situation, which is responsible for development of depression.[ 43 ] Studies have also reported that parental loss before the age of 18 years, parental disharmony and eldest birth order tend to be more common in subjects with depression.[ 48 ]
Studies in elderly also suggest that life events, especially financial problems and death in the family are as important a precipitating event for depression as they are in young adult.[ 20 , 40 , 49 ] It is also seen that stressful life events were specifically more in the elderly females and those with lower per capita income.[ 50 ]
With respect to life events in children and adolescents, Patel et al . found that depressed adolescent girls report life events in the form of death of a family member, change in residence, failure in examination, end of a relationship and serious illness.[ 51 ] Other risk factors identified to be associated with depression in children include stress at school and family as well as family history of mental illness.[ 52 ] However, one of the older studies failed to find a link between childhood bereavement and depression.[ 53 ]
Women as a group have also received considerable attention with regard to risk factors for development of depressive disorders. In an incidence study of common mental disorders, Patel et al .[ 54 ] reported that poverty (low income and having difficulty in making ends meet), being married as compared with being single, use of tobacco, experiencing abnormal vaginal discharge and reporting a chronic physical illness were associated with risk of developing a common mental disorder.[ 54 ] Studies have also reported that economic and interpersonal relationship difficulties, partner violence, sexual coercion by the partner as the common causal factors related to development of depression in general and depression during antenatal and postnatal period.[ 34 , 55 – 58 ] It has been shown that gender of the newborn child is an important determinant of postnatal depression.[ 34 , 56 , 57 ]
Among the psychological factors, attribution style was proposed to predispose individuals to depression and maintain depressive symptoms once they develop. A study using the Attribution Style Questionnaire[ 59 ] showed that depressed patients have a specific attribution style for their failures and successes in comparison to patients with schizophrenia and medical disorders. According to this study, patients with depression made more internal, stable and global attributions for bad events when compared to other disorders.[ 60 ] A study evaluating the cognitive model of depression as given by Beck failed to find support for the causal role of cognitive errors in relapse of depressed subjects as a significant proportion of patients were free from cognitive distortions following remission. However, it was also observed that those who had persistent cognitive distortions during remission ran the risk of early relapse.[ 61 ] It has also been seen that patients with neurosis, including depression, have poor social interactions and reports of more interactions of unpleasant type and less of pleasant type of social interactions as compared with healthy controls.[ 62 ]
With regard to personality factors, a study showed that higher scores on the hardiness, a personality trait, correlates with lower scores on the depression scale suggesting that presence of hardiness doesn’t allow depressive feelings to become more severe.[ 63 ]
Studies on Neurobiology
Compared to schizophrenia, there is relatively less research on the neurobiology of depression from India.
Neurochemicals
Studies have evaluated the levels of catecholamine metabolites in cerebrospinal fluid, urine and blood. Studies have showed that urinary 5-hydroxyindoleacetic acid (5HIAA), a metabolic end product of serotonin was significantly higher in depressed patients as compared to controls and these values decreased following successful treatment.[ 64 , 65 ] However, one study didn’t find any difference in the CSF 5HIAA levels between subjects with depression and healthy controls.[ 66 ] Studies have also shown significant positive correlation between the severity of depression and the patient’s urinary 5HIAA values[ 64 , 65 ] and negative correlation between the suicidal ideations and the patient’s urinary and cerebrospinal fluid (CSF) 5HIAA and homovanillic acid (HVA) values.[ 65 ] It has also been found that compared to controls, platelet serotonin (5HT) uptake is significantly lower in patients with depression, which improves temporarily with Electroconvulsive Therapy (ECT).[ 67 ] Another study by the same authors showed that treatment with Imipramine resulted in significant decrease in platelet 5HT uptake while ECT led to a significant increase in uptake.[ 68 ] With regard to dopamine metabolites, it has been seen that HVA levels are low in depressed subjects compared to controls and this correlates with platelet monoamine oxidase (MAO) activity, erythrocyte adenosine deaminase activity and 5-HIAA levels.
Further it was seen that compared to healthy controls HVA/5-HIAA ratio was also lower in subjects with depression.[ 66 ] Studies have also shown that both ECT and imipramine cause significant reduction in platelet MAO activity which normalizes during the post-treatment phase.[ 69 ] It has been demonstrated that there is significantly low serum dopamine-β-hydroxylase activity in patients with psychotic major depressive disorder compared to healthy controls. However, dopamine-β-hydroxylase activity did not differ between healthy controls, acute schizophrenia patients, subjects with non-psychotic depression and mania.[ 70 ] Srinivasan et al .[ 71 ] also showed that during the acute phase of depression there is low urinary 5-vinyl mandelic acid (VMA), which decrease further during treatment with imipramine. The authors also observed similar finding with respect to effect of imipramine in normal subjects. The levels also normalize in post treatment phase in depressed subjects and after stoppage of treatment in normal subjects.
Electrophysiology
Many studies have evaluated the pretreatment P300 amplitude and latency in depressed subjects and compared the same with healthy controls. All studies have consistently shown that P300 amplitude is smaller in depressed subjects and this normalizes with recovery[ 72 – 74 ] suggesting that it may be a state marker of depression. However, the findings with regard to pretreatment P300 latency are inconsistent.[ 72 – 74 ] Studies have also shown that P300 latency has a significant positive correlation with age of the patient and severity of depression while P300 amplitude have a significant negative correlation with age[ 73 ] and severity of depression.[ 72 ] A study showed that P300 amplitude is lower in depressed subjects, but there is no difference between subjects with depression and dysthymia,[ 74 ] however, the pretreatment P300 amplitude does not predict the treatment response.[ 75 ]
Studies have also shown that there is no difference between subjects of melancholic depression and control group in the latency of the middle components of evoked potential.[ 76 ] Studies done using Bereitschafts potential (BP) a measure of frontal lobe functions have also shown that the amplitude and frequency are lower in subjects with melancholic depression compared to the healthy controls.[ 76 ]
Endocrinology
As a marker for melancholia, studies have shown that dexamethasone suppression test (DST) has low sensitivity but high specificity.[ 77 – 79 ] Studies have also shown that, compared to DST suppressors, DST non-suppressors are significantly more depressed, attempt suicide more frequently, have higher rates of past and family history of depression, more frequently require electroconvulsive therapy and show better response to treatment.[ 79 ] A similar finding with respect to response to treatment has also been reported in another study.[ 80 ] Another study on subjects with post-stroke depression showed that DST response parallels the clinical course and response to treatment.[ 81 ]
A study of absolute eosinophil counts as an indirect measure of adrenocortical function showed that initial pretreatment level of eosinophils was higher than normal in depressed subjects, which showed a variable response to treatment indicating towards a varying degree of diminished activity of adrenal cortex.[ 82 ] Studies have also shown that plasma cortisol levels are higher in depressed subjects compared to healthy subjects and the increase in levels do not correlate with severity of depression.[ 83 ] Studies have also demonstrated that abnormal plasma cortisol level can differentiate patients with depression from patients with schizophrenia and healthy controls with a confidence level of 60%-93.3%. Urinary free cortisol after dexamethasone suppression test was considered as the best indicator of differentiating depressed patients from healthy subjects and patients with schizophrenia.[ 84 ]
Adrenocorticotrophic Hormone (ACTH) measurements, both at baseline and post-DST in patients of major depression, have been found to be significantly high at baseline and post DST as compared to healthy controls.[ 85 ] A study evaluated the role of dexamethasone in treatment based on the hypothesis that dexamethasone would hasten recovery, but did not find any advantage in favor of dexamethasone compared to placebo.[ 86 ]
Two studies have found that significantly higher number of patients with unipolar depression have subnormal T3 and T4 levels and a corresponding increase in thyroid stimulating hormone (TSH) levels compared with healthy controls.[ 87 , 88 ] In the second study, mildly depressed patients had significantly lower and severely depressed patients had significantly higher levels of TSH suggesting the direct relationship of severity of depression and TSH levels.[ 88 ] Another study found that 20.5% subjects of major depressive disorders have hypothyroidism.[ 89 ] When drug naive first episode depression patients were evaluated, they showed significantly higher T4 levels, but there was no significant difference in the level of T3 and TSH between depressed and healthy control subjects. However, when depressed subjects with and without psychotic features were compared, it was seen that subjects with psychotic symptoms had significantly higher levels of TSH.[ 90 ]
It has been shown that there is significant increase in total CSF protein levels in depressed subjects compared to subjects with neurological and surgical illnesses. It was seen that levels of immunoglobulin (Ig) M, IgG and IgA are higher in depressed and neurologically ill subjects compared to subjects with surgical illnesses. Further, when the levels of immunoglobulins were compared between depressed and normal subjects, IgG and IgA were significantly higher in depressed subjects. However, the study did not find evidence of viral markers for rubella and cytomegalovirus in CSF of depressed subjects.[ 91 ]
Extracellular fluid
Verma and Wig[ 92 ] showed that the extracellular fluid (ECF) volume of patients with depression tends to be lower than normal controls and normalization of the same correlates with clinical improvement.
Studies have shown that urinary melatonin levels can help in distinguishing subjects of endogenous depression from those with neurotic depression. Nocturnal as well as 24 hours urinary melatonin levels are low in subjects with endogenous depression whereas subjects with neurotic depression have higher than normal levels. It was also seen that melatonin levels were related to suicide attempts, diurnal variation and psychomotor retardation.[ 93 ]
Neurocognitive functioning
Studies from India suggest that definite cognitive impairments are present in the domains of intelligence and memory (Bhatia’s Battery test or the Weschler Adult Performance Intelligence Scale and PGI memory scale) in the depressed state but these don’t persist following recovery.[ 94 – 96 ] It is also reported that subjects with depression perform poorly on the Wisconsin Card Sorting Test (WCST) as compared to controls suggesting cognitive inflexibility and prefrontal dysfunction. Further, more severe illness is associated with greater impairment in the executive functioning on WCST.[ 97 ] Other studies which have evaluated various cognitive domains have shown that when patients with depression are asked to discriminate the emotional tone in terms of intensity of facial expression while presented in pairs, it is seen that they are highly evaluative of sadness and less evaluative of happiness, in comparison to the normal.[ 98 ]
A recent study, showed the importance of genetic factors in treatment response. Significantly better response to escitalopram was seen in patients homozygous for long allele of the serotonin transporter gene compared to the patients who were homozygous for short allele or heterozygous for short and long allele.[ 99 ] Another study showed that short variants of D7S1875 marker in LEP gene may be a risk factor for depression.[ 100 ]
A recent study evaluated the serum total cholesterol level in depressed subjects and showed that there is significant elevation of serum total cholesterol in depressed patients compared with normal controls and this persists even after controlling for the confounders.[ 101 ] Another study suggested that measurement of serum cholesterol levels may actually indicate towards hypothyroidism in depressed subjects.[ 89 ]
Symptomatology
Many studies have reported the symptom profile of subjects with depressive disorders.[ 5 , 13 , 36 , 39 , 52 , 102 – 118 ] The findings of symptomatology in general can be understood with respect to somatic symptoms, guilt and other depressive ideations, suicidal behavior, phenomenology of delusions and sleep architecture. Studies have also compared the symptomatology across different regions of the country. Studies have also attempted to distinguish the phenomenology in depression from negative symptoms of schizophrenia and the phenomenology in dysthymia.
One common theme with regard to symptomatology of depression, which has been reported by most of the researchers is high prevalence of somatic symptoms and some studies report that somatic symptoms are the most common manifestation of depression in India.[ 5 , 36 , 104 – 106 , 110 , 111 , 119 , 113 , 114 , 122 ] Erna Hoch[ 120 ] also reported that many Indian subjects with depression have hypochondriacal ideas considering body and its functioning. Studies have also shown pain as a depressive equivalent symptom.[ 42 , 1 ] Studies which have compared Indian subjects with depressed subjects from the West have also reported that somatic symptoms are more common in Indian subjects.[ 104 ] On the other hand studies on prevalence of functional somatic complaints in patients attending the psychiatric outpatient have also reported that most of these cases are diagnosed as depression.[ 122 , 124 ] It has also been shown that depressed subjects have greater difficulty in identifying bodily sensations and feelings as well as in expressing feelings.[ 125 ]
However, some of the studies evaluating depressive symptoms using the standardized instrument have reported that other symptoms are also present quite frequently in depressed subjects. One study which assessed 100 subjects with depression on HDRS reported that depressed mood and difficulties in work are present in all cases. Other symptoms reported in more than 50% of subjects included late insomnia, somatic anxiety, initial insomnia, psychic anxiety, suicidal ideations, retardation, loss of insight, middle insomnia, genital symptoms, hypochondriasis, gastrointestinal symptoms, agitation somatic symptoms in general and diurnal variation. Depersonalization, paranoid and obsessional symptoms were reported very infrequently. Guilt was present in about half of the subjects.[ 106 ] Gutpa et al .[ 103 ] also studied the symptomatology of depression from north India and compared it with findings from south India. Significantly higher number of subjects from north India reported joylessness, disruption in social functioning, lack of self confidence, early morning awakening, lack of appetite, feeling of pressure, other psychological symptoms, psychomotor restlessness, mood worsening in the morning, subjective experience of memory loss, retardation and guilt feeling; significantly higher number of subjects from south India reported hypochondriasis. There was no difference in other symptoms.
Another study from north India evaluated the symptomatology of depression and reported sadness, lack of interest, disturbed sleep, hypochondriasis, poor concentration, agitation, suicidal thoughts, and appetite change as the commonly occurring symptoms. Guilt was reported in about 40% of cases. The authors also compared their findings with studies from other parts of the country and the West and reported that lack of interest was more common in subjects from north India while reduced self-confidence, delusions and suicidal thoughts were seen more often in the south Indian sample.[ 47 ] Studies from Mumbai less frequently reported hypochondriasis, guilt, weight change, reduced interest and more frequently reported constipation.[ 47 ]
Earlier a few dynamically oriented psychiatrists envisaged guilt as the core symptom of depression. It is also suggested that guilt is less commonly seen in eastern population compared to the west. Studies done in India suggest that it is present in 5.3-67.5% of subjects.[ 36 , 47 , 106 , 126 – 129 ] Bhattacharyya and Vyas[ 130 ] also reported lesser frequency of guilt feeling in Indian subjects compared to Australian subjects. Venkoba Rao[ 127 ] on the basis of karma theory hypothesized that guilt may not be integral part of depression in Indian subjects and is actually a consequence of depression.[ 127 ] Sethi et al .[ 131 ] also reported that there is no relationship of guilt with severity of depression[ 131 ] and Trivedi et al .[ 132 ] reported higher level of guilt in depressed subjects as compared to neurotic subjects.[ 132 ]
Studies have also evaluated suicidal thinking in depressed subjects. Venkoba Rao and Nammalvar[ 107 ] reported that about two-third of depressed subjects have suicidal behavior and on the basis of the content they classified suicidal ideation into four broad categories, viz., ideas to kill oneself, a mere wish to die, a wish to be killed and a fourth unclassifiable category. In a recent study on the relationship between anger and suicidality, depressed patients with anger attacks exhibited more suicide-related phenomena in comparison to depressed patients without anger attacks.[ 133 ] Studies which have evaluated depressed subjects with suicidal ideation have shown that 16.6% of these subjects make suicidal attempt and a higher risk of suicidal attempt is found in individuals less than 30 years of age, single men, married women and students and higher education.
Attempters scored significantly higher in severity of suicidal ideation, agitation and paranoid symptoms whereas among non-attempters, hypochondriasis and general somatic symptoms were more common.[ 111 ] Studies have also shown that depressed subjects who attempt suicide are at higher risk of indulging in further suicidal behavior, compared to those who do not attempt.[ 134 ] However, it has also been shown that presence of suicidal behavior does not predict overall poor clinical outcome.[ 135 ]
Studies have reported that amongst the delusions in subjects with depression, delusions of persecution occurs most frequently (67.5%) (with persecution involving either the patients themselves or people close to them) followed by delusions of reference. Hypochondriacal, guilt and nihilistic delusions, which are considered classical in depression, are relatively uncommon in Indian subjects.[ 109 ]
In terms of sleep architecture, it is reported that subjects with depression have lesser total sleep time, longer sleep latency, frequent awakenings, greater wake-after-sleep onset and offset times, lesser sleep efficiency and tendency to wake up earlier than controls. Subjects with severe depression differ from patients with mild and moderate depression with regards to total sleep time, night-time sleep and sleep efficiency.[ 136 ]
Studies which have tried to distinguish depression from negative symptoms have shown that depressed patients score significantly higher on subjective complaints, total score, global ratings on Scale for the Assessment of Negative Symptoms (SANS), while schizophrenia is associated with significantly higher scores on global rating of alogia, poor eye contact, inappropriate affect, and blocking.[ 115 ] Another study showed that anhedonia-asociality are seen commonly in both patients with depression and schizophrenia while the global ratings on affective flattening, alogia, avolition and inattention are significantly higher in subjects with schizophrenia.[ 114 ]
A study which tried to distinguish the symptomatology of chronic major depression and dysthymia showed that symptomatically dysthymia and chronic major depression are indistinguishable.[ 137 ]
Studies have evaluated the symptomatology of depression in elderly depressed subjects too and have reported that the common symptoms in order of frequency were sadness, depressed mood, somatic symptoms and signs, suicidal ideas, lack of energy, anxiety or tension, inability to fall asleep, early awakening, hopelessness, irritability and inability to enjoy.[ 41 ] Another study from community sample reported that disturbed sleep pattern is the most common symptom in depressed elderly subjects.[ 21 ]
One study which evaluated the symptomatology of depression in children and adolescents reported multiple somatic complaints as the most common presenting complaint in children with depression.[ 117 ] Another study, which compared the symptomatology of children and adults, showed that more children than the adults presented with the somatic symptoms and the predominant mood symptom in children was irritability in contrast to sadness in adults.[ 118 ] Other commonly reported symptoms of depression across studies include low mood, diminished interest in play and activities, excessive tiredness, low self-esteem, problems with concentration, behavior symptoms like anger and aggression, decreased interest in school and recent deterioration in school performance, death wish and suicidal behavior.[ 52 , 117 ]
In terms of symptomatology in postpartum depression, infanticidal ideas have been reported in depressed mothers.[ 34 ] Studies evaluating subjects with seasonal affective disorder found that atypical vegetative features are not prominent part of the symptomatology in India.[ 138 , 139 ]
Comorbidity
Many studies done in subjects with depression have shown high level of comorbidity of both psychiatric and physical illnesses, especially in elderly individuals with depression.[ 140 , 141 ] On the other hand studies on the prevalence of psychiatric morbidity in physical disorders have shown that depression is quite prevalent in these conditions.
The commonly reported physical illnesses in subjects with depression include those involving the musculoskeletal, cardiovascular and ophthalmological systems and the commonly reported diagnosis in order of frequency were osteoarthritis, hypertension and cataract in one study.[ 141 ] The commonly and consistently reported comorbid conditions in children with depression include anxiety and conversion/dissociative disorder.[ 51 , 116 , 117 ] Other comorbid conditions include, dysthymia, adjustment disorder, conduct disorder and attention deficit hyperactivity disorder.[ 52 , 117 , 118 ]
Studies done in subjects with intentional self harm,[ 142 ] subjects with serious suicide attempts,[ 143 ] divorce seeking couples,[ 144 ] earth quake victims,[ 145 ] women after childbirth,[ 56 ] obsessive compulsive disorder,[ 146 ] alcohol dependent subjects,[ 147 ] dementia,[ 148 ] Dhat syndrome,[ 149 , 150 ] medical in-patients,[ 151 – 153 ] epilepsy,[ 154 ] neurological disorders,[ 155 ] end stage renal disease,[ 156 , 157 ] cancer,[ 158 ] chronic and disfiguring skin disorders,[ 159 ] age related macular degeneration,[ 160 ] HIV-infected heterosexuals,[ 161 ] industrial population[ 162 ] have shown that depression is the most common or one of the most common psychiatric diagnosis in such patient groups and prevalence rate as high as 86.7% has been reported.
Assessment and Diagnostic issues
In clinical and research work, apart from uniform diagnostic criteria, some means to objectively quantify the presence of particular symptoms and level of their severity is required. For this purpose, a number of rating scales have been devised worldwide, of which clinician rated Hamilton Depression Rating Scale (HDRS),[ 163 ] self reporting Beck Depressive Inventory,[ 164 ] Montgomery-Asberg Depression rating scale (MADRS) are the most popular ones. Indian researchers have adapted/modified these scales for the Indian population.[ 165 – 167 ] Additionally scales like Amritsar Depressive Inventory (ADI) a self reporting scale has been developed on the basis of symptoms and signs of depression as manifested by Indian patients.[ 168 ] Avasthi et al .[ 169 ] translated the PRIME-MD questionnaire in Hindi and showed that it is useful for screening various psychiatric disorders. Brief Patient Health Questionnaire (PHQ) has also been translated in 11 languages and validated for Indian population.[ 170 ] Many studies have also evaluated the psychometric properties of various scales in India.[ 171 – 173 ]
Impact of Depression
Studies have shown that depressive disorders lead to significant dysfunction,[ 174 ] disability[ 175 ] and poor quality of life in sufferers[ 176 ] and pose a significant burden on the caregivers.[ 177 ] The pattern of burden experienced by relatives of patients with affective disorders and schizophrenia have been shown to be similar, being principally felt in the areas of family routine, leisure, interaction and finances. However, the caregivers of subjects with depression experience lesser degree of burden compared to caregivers of schizophrenia and bipolar disorders.[ 177 , 178 ] Another study showed that the burden of dysthymia is similar to neurotic disorders like obsessive compulsive disorder and generalized anxiety disorder.[ 179 ] It has also been seen that patients with dysthymia have significant impairment on measures of quality of life, disability, social support and marital adjustment compared to normal/medically ill controls. The study also showed that duration of illness and severity of depression are the most important correlates of impaired quality of life and disability.[ 180 ] A study assessing the relationship of stigma to both depression and somatization in psychiatric patients of south India showed that although both depressive and somatic symptoms were distressing, perceived stigma was more for depressive symptoms. Depressive symptoms were perceived as socially disadvantageous as compared to somatization symptoms.[ 167 ]
Course and Outcome
There are very few studies which have evaluated the course and outcome of depression. Venkoba Rao and Nammalvar[ 181 ] followed up 109 out of 122 cases of endogenous depression 3-13 years after their index diagnosis. No recurrence occurred in 28 cases. Forty-two cases turned out to be bipolar and 21 remained unipolar. Manic episodes outnumbered the depressive ones. The change of polarity from depression to mania occurred within three years after the initial depression, though in others the shift occurred between 3 to 12 years. The number of episodes of depression before the onset of mania varied from one to three. While the onset of depression before the age of 40 years predisposed to recurrences, there was risk of chronicity in those patients who developed the illness after 40 years. Gada[ 182 ] studied 92 out of 100 cases of major depressive disorder five to 10 years after the index diagnosis and showed that 36.6% cases had no recurrence of episodes and 63.4% had recurrence. Of the total subjects, 37.8% were diagnosed as bipolar disorders and 25.6% were diagnosed as recurrent depressive disorder.
The change of diagnosis from major depressive disorder to bipolar disorder occurred within three years after the initial depression in 77% of cases. In another study Brown et al .[ 183 ] reported that in their cohort all subjects experienced full recovery within the one-year period. At one-year follow-up, 71% of depressive patients demonstrated no symptoms or social impairment.[ 183 ] The mean duration of depressive episode was 14.2 weeks and the rate of relapse was 18%. The authors concluded that overall outcome was considerably more favorable than in comparable studies of affective disorders in developed settings. All these findings suggest that depressive disorders have high chance of recurrence and many of the subjects initially diagnosed as cases of unipolar depression are later diagnosed as bipolar disorder. In another prospective study of subjects with seasonal affective disorder (SAD), Avasthi et al .[ 184 ] reported that after the initial diagnosis of SAD the subjects did not display any variation in mood, behavior, sleep pattern and weight fluctuation over a period of five to seven years.
Study done in elderly patients with depression have reported that complete recovery occurs in 58% of cases and 24% of cases have partial recovery with 18% registering relapses.[ 41 ] Sachdev et al .[ 185 ] studied various factors related to prognosis of depression and found that sleep-disturbances, agitation, depth of depression, age at the time of present onset, age at first onset, history over one year with no symptom-free period, sudden onset of illness, adequate premorbid personality and adequate psychogenesis are of prognostic significance.
Treatment related issues
One of the important patient characteristic which has been reported to influence treatment adherence is their attitudes and beliefs towards medication. In a recent study, Chakraborty et al .[ 186 ] reported that most of the patients value the doctor-patient relationship and their partners are also supportive regarding diagnosis and treatment of depression. However, most patients have erroneous beliefs regarding antidepressants per se which in turn influence the drug compliance.
Sethi et al .[ 187 ] proposed a prevention model for depression focusing on improving social network and educational programs, designed to educate the public with regard to the risks inherent to change of jobs, residence, pattern of living as well as how to protect against them and removal of malnutrition and infections. A recent review suggests that religiosity can be protective against depression.[ 188 ]
Conclusion and future directions
Depression is the most common psychiatric disorder reported in most of the community based studies. It is also reported as one of the most common psychiatric disorder in outpatient clinic population and in subjects seen in various medical and surgical setting. It is also reported to be the most common psychiatric disorder in elderly subjects across various settings. Studies from India have also shown that life events during the period preceding the onset of depression play a major role in depression. Studies on women have also shown the importance of identifying risk factors like interpersonal conflicts, marital disharmony and sexual coercion.
There is need for further study of factors like cost, attitude towards treatment, adherence, compliance and neurobiological correlates. There is also a need to study the course of depressive disorders in India so as to determine the need and duration of continuation treatment. Studies should also evaluate the cost-effective models of treatment which can be easily used in the primary care setting to effectively treat depression.
Source of Support: Nil
Conflict of Interest: None declared.

IMAGES
VIDEO
COMMENTS
Introduction. Depression is one of the most common mental health issues, ... This review may be used as an evidence base by those in public health, clinical practice, and research. This paper discusses key areas in depression research; however, an exhaustive discussion of all the risk factors and determinants linked to depression and their ...
Abstract. Major depression is a mood disorder characterized by a sense of inadequacy, despondency, decreased activity, pessimism, anhedonia and sadness where these symptoms severely disrupt and ...
Depression is a mood disorder that causes a persistent feeling of sadness and loss of interest. The American Psychiatric Association's Diagnostic Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) classifies the depressive disorders into Disruptive mood dysregulation disorder; Major depressive disorder; Persistent depressive ...
In line with the Research Domain Criteria Project launched by the National Institute of Mental Health (Insel, 2014; Insel et al., 2010), a distinguished aim in developing an integrated neuroscientific model of depression therefore has to be the separation of distinct aetiological and pathophysiological trajectories which, although eventually ...
INTRODUCTION. Depression is a common psychiatric disorder and a major contributor to the global burden of diseases. According to the World Health Organization, depression is the second-leading cause of disability in the world and is projected to rank first by 2030[].Depression is also associated with high rates of suicidal behavior and mortality[].
1. Introduction. About 280 million people worldwide suffer from a depressive disorder (WHO, 2022).These disorders are associated with considerable suffering by patients and their families, increased mortality and morbidity (Cuijpers et al., 2014a), and enormous economic costs (König et al., 2020).In addition, they are the second leading cause of years lived with disability on the population ...
The idea that depression is the result of abnormalities in brain chemicals, particularly serotonin (5-hydroxytryptamine or 5-HT), has been influential for decades, and provides an important ...
The current paper has the purpose of reviewing the meaning of depression from a ... Introduction. Type 2 Diabetes Mellitus is a chronic metabolic disease, which causes a concomitant alteration ...
To improve our understanding, some research has been undertaken in which YP themselves are asked about their experience of depression. In a questionnaire study involving adolescents with depression in New Zealand, the researchers identified the aforementioned irritability as the most common characteristic alongside interpersonal problems and thought-processing symptoms (Crowe, Ward, Dunnachie ...
INTRODUCTION. Depression is described as a common and serious mood disorder that results in persistent feelings of sadness and hopelessness, as well as a loss of interest in activities that one once enjoyed (American Psychiatric Association [APA], 2013).Additional symptoms of depression include weight changes, difficulty sleeping, loss of energy, difficulty thinking or concentrating, feelings ...
university students, found the rate of depression among Nigerian students was only 2.7%. This is much lower compared to the rate of depression among Nigerian outpatients visiting. general clinics ...
At the same time, studies of trait anxiety suggest that moderate (vs. low) ELS is associated with greater self-reported anxiety. This study tested the hypothesis that stress inoculation effects are evident for implicit (nonconscious) but not explicit (conscious) aspects of anxiety. Methods: Ninety-seven healthy women were assessed for ELS and ...
1. Introduction. The World Health Organization [] estimates that 264 million people worldwide were suffering from an anxiety disorder and 322 million from a depressive disorder in 2015, corresponding to prevalence rates of 3.6% and 4.4%.While their prevalence varies slightly by age and gender [], they are among the most common mental disorders in the general population [2,3,4,5,6].
After applying the inclusion and exclusion criteria, 470 papers were included in this review (Supplementary Table S1). We focused on aspects related to biological, psychological, and social determinants of depression (examples of determinants and related outcomes are provided under each of the following sections. 3.1.
Abstract. Epidemiologic data from around the world demonstrate that major depression is approximately twice as common in women than men and that its first onset peaks during the childbearing years. Progress has been made in understanding the epidemiology of depression and in developing effective treatments. Much remains to be learned about the ...
Introduction: Anxiety and Depression Linda Gask1 and Carolyn Chew-Graham2 1University of Manchester, Manchester, UK 2 Research Institute, Primary Care and Health Sciences and National School for Primary Care Research, Keele University, Keele, UK Box 1.1 Broad Street The O'Sullivans live in a three-storey Victorian house in need of repair,
The research is done on both gender, male and female. 29 students are female and. male students are 112. This portion of research is to check whether female students can have more chances. of ...
More relevant to the current paper is the possibility that the exhaustive medicalization of the term; the wealth of non-behavior-analytic research data on biology and genetics, personality, and cognitive factors; and the emphasis on private events in depression—on how depression feels and on changing that feeling—may function to evoke ...
Table of contents. Step 1: Introduce your topic. Step 2: Describe the background. Step 3: Establish your research problem. Step 4: Specify your objective (s) Step 5: Map out your paper. Research paper introduction examples. Frequently asked questions about the research paper introduction.
This sample depression research paper features: 5700 words (approx. 19 pages), an outline, and a bibliography with 7 sources. Browse other research paper examples for more inspiration. If you need a thorough research paper written according to all the academic standards, you can always turn to our experienced writers for help.
Introduction. Health issues are becoming more and more important to people due to the continuous development of health care. ... Peoples R China, as the only developing country, ranks 3rd in the top 10 countries with high production of research papers in the field of depression, and Peoples R China's research in the field of depression has ...
Introduction. • Depression is a mood disorder that causes a. persist ent f eeling of sadness and loss of. inter est (Sawchuk, 2022). • It is a common and serious medical illness. that is also ...
1-) Start with a Catchy Hook. Your first sentence is one of the factors that most influence a reader's decision to read your paper. This sentence determines the tone of your paper and attracts the reader's attention. For this reason, we recommend that you start your introduction paragraph with a strong and catchy hook sentence.
population aged 16-85 years, 14.4% have an anxiety. disorder. The pre valence of depression is 6.2%, with the. prevalence of unipolar depressive episodes being 4.1%, dysthymia, 1.3%, and bipolar ...
Epidemiology. Many studies have estimated the prevalence of depression in community samples and the prevalence rates have varied from 1.7 to 74 per thousand population.[2,3] Reddy and Chandrasekhar[] carried out a metanalysis, which included 13 studies on epidemiology of psychiatric disorders which include 33572 subjects from the community and reported prevalence of depression to be 7.9 to 8.9 ...