

Key Takeaways
- Alcohol is among the most used drugs, plays a large role in many societies and cultures around the world, 1 and greatly impacts public health. 2,3 More people over age 12 in the United States have used alcohol in the past year than any other drug or tobacco product, and alcohol use disorder is the most common type of substance use disorder in the United States. 4
- NIDA works closely with the National Institute on Alcohol Abuse and Alcoholism (NIAAA) , the lead NIH institute supporting and conducting research on the impact of alcohol use on human health and well-being. For information on alcohol and alcohol use disorder , please visit the NIAAA website .
- Because many people use alcohol while using other drugs, 4 NIDA supports and conducts research on both the biological and social dynamics between alcohol use and the use of other substances.
Looking for Treatment?
Use the SAMHSA Treatment Locator or call 1-800-662-HELP (4357) .
NIH Resources

- Find treatment for alcohol use disorder and alcohol addiction (previously called alcoholism) using the NIAAA Alcohol Treatment Navigator .
- Read more about the latest advances in alcohol addiction research on the NIAAA Director’s Blog .
- Learn more about how NIH Institutes and Centers work together to better understand, treat and prevent addiction through the Collaborative Research on Addiction at NIH (CRAN) initiative.
- Learn more about the scientific meeting “ Opioid Use in the Context of Polysubstance Use: Research Opportunities for Prevention, Treatment, and Sustained Recovery .”
NIDA Resources
- See the latest statistics on alcohol use among young students from NIDA’s Monitoring the Future Survey.
Addiction often goes hand-in-hand with other mental illnesses. both must be addressed., reported drug use among adolescents continued to hold below pre-pandemic levels in 2023, heart medication shows potential as treatment for alcohol use disorder, marijuana and hallucinogen use among young adults reached all time-high in 2021, additional resources.
- Find basic health information on alcohol use disorder from MEDLINEplus , a service of NIH’s National Library of Medicine (NIH).
- Read Alcohol Misuse information from the Substance Abuse and Mental Health Services Administration (SAMHSA).
- Learn more about medical approaches to treating alcohol use disorder from the Substance Abuse and Mental Health Services Administration (SAMHSA) in Medication for the Treatment of Alcohol Use Disorder: A Brief Guide .
- Read Alcohol Misuse Prevention: A Conversation for Everyone from the Substance Abuse and Mental Health Services Administration (SAMHSA).
- Sudhinaraset M, Wigglesworth C, Takeuchi DT. Social and Cultural Contexts of Alcohol Use: Influences in a Social-Ecological Framework. Alcohol Res. 2016;38(1):35-45.
- Witkiewitz K, Litten RZ, Leggio L. Advances in the science and treatment of alcohol use disorder. Sci Adv. 2019;5(9):eaax4043. Published 2019 Sep 25. doi:10.1126/sciadv.aax4043
- GBD 2016 Alcohol Collaborators. Alcohol use and burden for 195 countries and territories, 1990-2016: a systematic analysis for the Global Burden of Disease Study 2016 [published correction appears in Lancet. 2018 Sep 29;392(10153):1116] [published correction appears in Lancet. 2019 Jun 22;393(10190):e44]. Lancet. 2018;392(10152):1015-1035. doi:10.1016/S0140-6736(18)31310-2
- Substance Abuse Center for Behavioral Health Statistics and Quality. Results from the 2021 National Survey on Drug Use and Health: Detailed Tables, SAMHSA . Accessed January 2023.
Deaths from Excessive Alcohol Use — United States, 2016–2021
Weekly / February 29, 2024 / 73(8);154–161
Marissa B. Esser, PhD 1 ; Adam Sherk, PhD 2 ; Yong Liu, MD 1 ; Timothy S. Naimi, MD 2 ( View author affiliations )
What is already known about this topic?
U.S. deaths from causes fully due to excessive alcohol use increased during the past 2 decades.
What is added by this report?
Average annual number of deaths from excessive alcohol use, including partially and fully alcohol-attributable conditions, increased approximately 29% from 137,927 during 2016–2017 to 178,307 during 2020–2021, and age-standardized death rates increased from approximately 38 to 48 per 100,000 population. During this time, deaths from excessive drinking among males increased approximately 27%, from 94,362 per year to 119,606, and among females increased approximately 35%, from 43,565 per year to 58,701.
What are the implications for public health practice?
Evidence-based alcohol policies (e.g., reducing the number and concentration of places selling alcohol and increasing alcohol taxes) could help reverse increasing alcohol-attributable death rates.
- Article PDF
- Full Issue PDF
Deaths from causes fully attributable to alcohol use have increased during the past 2 decades in the United States, particularly from 2019 to 2020, concurrent with the onset of the COVID-19 pandemic. However, previous studies of trends have not assessed underlying causes of deaths that are partially attributable to alcohol use, such as injuries or certain types of cancer. CDC’s Alcohol-Related Disease Impact application was used to estimate the average annual number and age-standardized rate of deaths from excessive alcohol use in the United States based on 58 alcohol-related causes of death during three periods (2016–2017, 2018–2019, and 2020–2021). Average annual number of deaths from excessive alcohol use increased 29.3%, from 137,927 during 2016–2017 to 178,307 during 2020–2021; age-standardized alcohol-related death rates increased from 38.1 to 47.6 per 100,000 population. During this time, deaths from excessive alcohol use among males increased 26.8%, from 94,362 per year to 119,606, and among females increased 34.7%, from 43,565 per year to 58,701. Implementation of evidence-based policies that reduce the availability and accessibility of alcohol and increase its price (e.g., policies that reduce the number and concentration of places selling alcohol and increase alcohol taxes) could reduce excessive alcohol use and alcohol-related deaths.
Introduction
Deaths from causes fully attributable to alcohol use (i.e., 100% alcohol-attributable causes, such as alcoholic liver disease and alcohol use disorder) have increased during the past 2 decades in the United States ( 1 ); rates were particularly elevated from 2019 to 2020,* concurrent with the onset of the COVID-19 pandemic. In addition, emergency department visit rates associated with acute alcohol use ( 2 ) and per capita alcohol sales † also increased during this time. Previous studies of trends have not included underlying causes of death that are partially attributable to alcohol ( 1 , 3 ), such as injuries or certain types of cancer, for which drinking is a substantial risk factor ( 4 , 5 ). A comprehensive assessment of changes in deaths from excessive alcohol use that includes conditions that are fully and partially attributable to alcohol can guide the rationale for and implementation of effective prevention strategies.
Data Sources and Measures
Total U.S. deaths from alcohol-related conditions during 2016–2021 identified from the National Vital Statistics System were grouped into three periods (2016–2017, 2018–2019, and 2020–2021). Deaths were defined using the underlying cause of death for the 58 alcohol-related conditions § in CDC’s Alcohol-Related Disease Impact (ARDI) application and estimated using ARDI methods. ¶ For each cause of death, alcohol-attributable fractions were used, reflecting the cause-specific proportion that is due to excessive alcohol use. For the 15 fully alcohol-attributable conditions,** the alcohol-attributable fraction is 1.0. Fully alcohol-attributable conditions include the 100% alcohol-attributable chronic causes as well as the 100% alcohol-attributable acute causes (i.e., alcohol poisonings that are a subset of deaths in the alcohol-related poisonings category and deaths from suicide by exposure to alcohol that are a subset of the suicide category). Partially alcohol-attributable conditions are those that are caused by alcohol use or other factors, and alcohol-attributable fractions are applied to calculate the deaths from alcohol use. For most of the partially alcohol-related chronic conditions, population-attributable fractions were estimated using relative risks from published meta-analyses and adjusted prevalence estimates of low, medium, and high average daily alcohol use among U.S. adults. Prevalence estimates were obtained from the Behavioral Risk Factor Surveillance System †† and adjusted using alcohol per capita sales information to account for underreporting of self-reported drinking ( 6 ).
Alcohol-attributable fractions for acute causes (e.g., injuries) were determined mostly from a recent meta-analysis that generally measured the proportion of decedents who had a blood alcohol concentration (BAC) ≥0.10% ( 7 ). Alcohol-attributable fractions for motor vehicle crashes and other road vehicle crash deaths were obtained from the Fatality Analysis Reporting System, based on the proportion of crash deaths that involved a decedent with BAC ≥0.08%. §§
Deaths from excessive alcohol use (as opposed to deaths from any level of drinking) includes all decedents whose deaths were attributed to conditions that are fully caused by alcohol use, alcohol-related acute causes of death that involved binge drinking, and alcohol-related chronic conditions that involved medium or high average daily levels of alcohol use. For the chronic causes of death estimated using cause-specific population-attributable fractions by sex, the relative risks for death at medium daily average drinking levels (females: >1 to ≤2 drinks, males: >2 to ≤4 drinks) and high daily average drinking levels (females: >2 drinks, males: >4 drinks) were relative to the risks at low daily average drinking levels (females: >0 to ≤1 drink, males: >0 to ≤2 drinks).
Data Analyses
The average annual number of deaths resulting from excessive alcohol use during three 2-year periods, percentage change in numbers of deaths, ¶¶ and death rates were calculated overall and by sex and cause of death category. The number of sex-stratified deaths from excessive drinking was also assessed by age group. In general, deaths from chronic conditions were calculated among decedents aged ≥20 years, and deaths from acute causes were calculated among decedents aged ≥15 years. Younger children whose deaths resulted from someone else’s drinking (e.g., as passengers in motor vehicle crashes) were also included for several causes of death. Death rates (deaths per 100,000 population) were calculated based on midyear postcensal population estimates and age-standardized to the 2000 U.S. Census Bureau standard population. Nonoverlapping 95% CIs were considered significantly different. Analyses were conducted using SAS software (version 9.4; SAS Institute). This activity was reviewed by CDC, deemed not research, and was conducted consistent with applicable federal law and CDC policy.***
Average annual deaths from excessive alcohol use in the United States increased 5.3%, from 137,927 during 2016–2017 to 145,253 during 2018–2019; these deaths then increased more sharply (22.8%) from 2018–2019 to 178,307 during 2020–2021, for an overall 29.3% increase from 2016–2017 to 2020–2021 ( Table 1 ). Age-standardized death rates increased from 38.1 per 100,000 population during 2016–2017 to 39.1 during 2018–2019 to 47.6 during 2020–2021. Approximately two thirds of these deaths resulted from chronic causes during each period: alcohol-attributable death rates from chronic causes increased from 23.2 per 100,000 population to 24.3 to 29.4 during the respective analysis periods. During 2020–2021, fully alcohol-attributable causes ††† accounted for 51,665 deaths (29.0% of all alcohol-attributable deaths), a 46.2% increase compared with the 35,344 deaths that occurred during 2016–2017. During 2020–2021, partially alcohol-attributable causes accounted for 126,642 deaths (71.0% of all alcohol-attributable deaths), a 23.5% increase compared with the 102,583 partially alcohol-attributable deaths that occurred during 2016–2017.
Increases Among Males and Females
The average annual number of deaths from excessive alcohol use among males increased by 25,244 (26.8%), from 94,362 deaths during 2016–2017 to 119,606 during 2020–2021 ( Table 2 ). Age-standardized death rates among males increased from 54.8 per 100,000 population during 2016–2017 to 55.9 during 2018–2019, and to 66.9 during 2020–2021. During each period, among all excessive alcohol use cause of death categories, death rates among males were highest from 100% alcohol-attributable chronic conditions.
Among females, the average annual number of deaths from excessive alcohol use increased by 15,136 (34.7%), from 43,565 during 2016–2017, to 58,701 during 2020–2021. Age-standardized alcohol-attributable death rates among females increased from 22.7 per 100,000 population during 2016–2017 to 23.6 during 2018–2019, and to 29.4 during 2020–2021. Death rates among females were highest from heart disease and stroke during each period. Among both males and females, alcohol-attributable death rates increased for most cause of death categories. The average number of sex-specific alcohol-attributable deaths increased among all age groups from 2016–2017 to 2020–2021( Figure ).
From 2016–2017 to 2020–2021, the average annual number of U.S. deaths from excessive alcohol use increased by more than 40,000 (29%), from approximately 138,000 per year (2016–2017) to 178,000 per year (2020–2021). This increase translates to an average of approximately 488 deaths each day from excessive drinking during 2020–2021. From 2016–2017 to 2020–2021, the average annual number of deaths from excessive alcohol use increased by more than 25,000 among males and more than 15,000 among females; however, the percentage increase in the number of deaths during this time was larger for females (approximately 35% increase) than for males (approximately 27%). These findings are consistent with another recent study that found a larger increase in fully alcohol-attributable death rates among females compared with males ( 8 ).
Increases in deaths from excessive alcohol use during the study period occurred among all age groups. A recent study found that one in eight total deaths among U.S. adults aged 20–64 years during 2015–2019 resulted from excessive alcohol use ( 9 ). Because of the increases in these deaths during 2020–2021, including among adults in the same age group, excessive alcohol use could account for an even higher proportion of total deaths during that 2-year period. In addition, data from Monitoring the Future, an ongoing study of the behaviors, attitudes, and values of U.S. residents from adolescence through adulthood, showed that the prevalence of binge drinking among adults aged 35–50 years was higher in 2022 than in any other year during the past decade §§§ ; this increase could contribute to future increases in alcohol-attributable deaths. In this study, fewer than one third of deaths from excessive alcohol use were from fully alcohol-attributable causes, highlighting the importance of also assessing partially alcohol-attributable causes to better understand the harms from excessive drinking, including binge drinking.
The nearly 23% increase in the deaths from excessive alcohol use that occurred from 2018–2019 to 2020–2021 was approximately four times as high as the previous 5% increase that occurred from 2016–2017 to 2018–2019. Increases in the availability of alcohol in many states might have contributed to this disproportionate increase ( 10 ). During the peak of the COVID-19 pandemic in 2020–2021, policies were widely implemented to expand alcohol carryout and delivery to homes, and places that sold alcohol for off-premise consumption (e.g., liquor stores) were deemed as essential businesses in many states (and remained open during lockdowns). ¶¶¶ General delays in seeking medical attention, including avoidance of emergency departments**** for alcohol-related conditions †††† ; stress, loneliness, and social isolation; and mental health conditions might also have contributed to the increase in deaths from excessive alcohol use during the COVID-19 pandemic.
Limitations
The findings in this report are subject to at least two limitations. First, population-attributable fractions were calculated based on data including only persons who currently drank alcohol. Because some persons who formerly drank alcohol might also die from alcohol-related causes, population-attributable fractions might underestimate alcohol-attributable deaths. Second, several conditions (e.g., HIV/AIDS and tuberculosis) for which excessive alcohol use is a substantial risk factor were not included because relative risk estimates relevant to the U.S. population were not available for calculating the portion of these deaths attributable to drinking alcohol, further contributing to conservative death estimates in this report.
Implications for Public Health Practice
States and communities can discourage excessive alcohol use and reverse recent increases in alcohol-attributable deaths by implementing comprehensive strategies, including evidence-based alcohol policies that reduce the availability and accessibility of alcohol and increase its price (e.g., policies that reduce the number and concentration of places selling alcohol and increase alcohol taxes). §§§§ Also, CDC’s electronic screening and brief intervention ¶¶¶¶ can be used in primary and acute care, or nonclinical, settings to allow adults to check their alcohol use, receive personalized feedback, and create a plan for drinking less alcohol. Integration of screening and brief intervention into routine clinical services***** for adults and mass media communications campaigns ††††† to support people in drinking less can also help. Increased use of these strategies, particularly effective alcohol policies, could help reduce excessive alcohol use and related deaths among persons who drink and also reduce harms to persons who are affected by others’ alcohol use (e.g., child and adult relatives, friends, and strangers).
Corresponding author: Marissa B. Esser, [email protected] .
1 Division of Population Health, National Center for Chronic Disease Prevention and Health Promotion, CDC; 2 Canadian Institute for Substance Use Research, Victoria, British Columbia, Canada.
All authors have completed and submitted the International Committee of Medical Journal Editors form for disclosure of potential conflicts of interest. Adam Sherk reports institutional support from the Canadian Cancer Society and Canadian Institutes for Health Research. No other potential conflicts of interest were disclosed.
* https://www.cdc.gov/nchs/products/databriefs/db448.htm
† https://www.niaaa.nih.gov/publications/surveillance-reports/surveillance120
§ https://www.cdc.gov/alcohol/ardi/alcohol-related-icd-codes.html
¶ https://www.cdc.gov/alcohol/ardi/methods.html
** Deaths from causes fully attributable to alcohol use (i.e., 100% alcohol-attributable causes) include alcohol abuse, alcohol cardiomyopathy, alcohol dependence syndrome, alcohol poisoning, alcohol polyneuropathy, alcohol-induced acute pancreatitis, alcohol-induced chronic pancreatitis, alcoholic gastritis, alcoholic liver disease, alcoholic myopathy, alcoholic psychosis, degeneration of the nervous system due to alcohol use, fetal alcohol syndrome, fetus and newborn issues caused by maternal alcohol use, and suicide by exposure to alcohol.
†† Daily average alcohol use prevalence estimates were from the Behavioral Risk Factor Surveillance System ( https://www.cdc.gov/brfss/data_documentation/index.htm ), aligning with the respective years of the death data for the three periods in this study, and used in population attributable fraction calculations. Prevalence estimates of daily average alcohol use were calculated for three levels, including low (females: >0 to ≤1 drink, males: >0 to ≤2 drinks), medium (females: >1 to ≤2 drinks, males: >2 to ≤4 drinks), and high (females: >2 drinks, males: >4 drinks), unless the source of the relative risk estimates specified otherwise. For the three periods in this study, the categorical relative risks were calculated to correspond with the median of the alcohol use distribution for each drinking level.
§§ https://www.nhtsa.gov/research-data/fatality-analysis-reporting-system-fars
¶¶ The percentage represents the equation {[(estimated average annual number of deaths from excessive alcohol use in more recent period − estimated average annual number of deaths from excessive alcohol use in earlier period) / estimated average annual number of deaths from excessive alcohol use in earlier period] x 100}.
*** 45 C.F.R. part 46.102(l)(2), 21 C.F.R. part 56; 42 U.S.C. Sect. 241(d); 5 U.S.C. Sect. 552a; 44 U.S.C. Sect. 3501 et seq.
††† Fully alcohol-attributable conditions include the 100% alcohol-attributable chronic causes as well as the 100% alcohol-attributable acute causes (i.e., alcohol poisonings that are a subset of deaths in the alcohol-related poisonings category and suicide by exposure to alcohol that are a subset of deaths in the suicide category).
§§§ https://monitoringthefuture.org/wp-content/uploads/2023/07/mtfpanel2023.pdf
¶¶¶ https://alcoholpolicy.niaaa.nih.gov/sites/default/files/file-page/digest_state_alcohol_policies_in_response_to_covid-19_220101.pdf
**** https://www.cdc.gov/mmwr/volumes/70/wr/mm7015a3.htm
†††† https://onlinelibrary.wiley.com/doi/10.1111/joim.13545
§§§§ https://www.cdc.gov/alcohol/fact-sheets/prevention.htm
¶¶¶¶ https://www.cdc.gov/alcohol/checkyourdrinking/index.html
***** https://www.uspreventiveservicestaskforce.org/uspstf/recommendation/unhealthy-alcohol-use-in-adolescents-and-adults-screening-and-behavioral-counseling-interventions
††††† https://www.thecommunityguide.org/findings/health-communication-and-social-marketing-campaigns-include-mass-media-and-health-related.html
- Maleki N, Yunusa I, Karaye IM. Alcohol-induced mortality in the USA: trends from 1999 to 2020. Int J Ment Health Addict 2023;6:1–13. https://doi.org/10.1007/s11469-023-01083-1 PMID:37363762
- Esser MB, Idaikkadar N, Kite-Powell A, Thomas C, Greenlund KJ. Trends in emergency department visits related to acute alcohol consumption before and during the COVID-19 pandemic in the United States, 2018–2020. Drug Alcohol Depend Rep 2022;3:100049. https://doi.org/10.1016/j.dadr.2022.100049 PMID:35368619
- White AM, Castle IP, Powell PA, Hingson RW, Koob GF. Alcohol-related deaths during the COVID-19 pandemic. JAMA 2022;327:1704–6. https://doi.org/10.1001/jama.2022.4308 PMID:35302593
- Naimi TS, Sherk A, Esser MB, Zhao J. Estimating alcohol-attributable injury deaths: a comparison of epidemiological methods. Addiction 2023;118:2466–76. https://doi.org/10.1111/add.16299 PMID:37466014
- Islami F, Goding Sauer A, Miller KD, et al. Proportion and number of cancer cases and deaths attributable to potentially modifiable risk factors in the United States. CA Cancer J Clin 2018;68:31–54. https://doi.org/10.3322/caac.21440 PMID:29160902
- Esser MB, Sherk A, Subbaraman MS, et al. Improving estimates of alcohol-attributable deaths in the United States: impact of adjusting for the underreporting of alcohol consumption. J Stud Alcohol Drugs 2022;83:134–44. https://doi.org/10.15288/jsad.2022.83.134 PMID:35040769
- Alpert HR, Slater ME, Yoon YH, Chen CM, Winstanley N, Esser MB. Alcohol consumption and 15 causes of fatal injuries: a systematic review and meta-analysis. Am J Prev Med 2022;63:286–300. https://doi.org/10.1016/j.amepre.2022.03.025 PMID:35581102
- Karaye IM, Maleki N, Hassan N, Yunusa I. Trends in alcohol-related deaths by sex in the US, 1999–2020. JAMA Netw Open 2023;6:e2326346. https://doi.org/10.1001/jamanetworkopen.2023.26346 PMID:37505494
- Esser MB, Leung G, Sherk A, et al. Estimated deaths attributable to excessive alcohol use among US adults aged 20 to 64 years, 2015 to 2019. JAMA Netw Open 2022;5:e2239485. https://doi.org/10.1001/jamanetworkopen.2022.39485 PMID:36318209
- Trangenstein PJ, Greenfield TK, Karriker-Jaffe KJ, Kerr WC. Beverage-and context-specific alcohol consumption during COVID-19 in the United States: the role of alcohol to-go and delivery purchases. J Stud Alcohol Drugs 2023;84:842–51. https://doi.org/10.15288/jsad.22-00408 PMID:37449953
* Includes 58 causes of death related to alcohol use. Deaths from excessive alcohol use includes all decedents whose deaths were attributed to conditions that were fully caused by alcohol use, alcohol-related acute causes of death that involved binge drinking, and alcohol-related chronic conditions that involved medium (females: >1 to ≤2 drinks, males: >2 to ≤4 drinks) or high (females: >2 drinks, males: >4 drinks) daily average drinking levels. † Nonoverlapping 95% CIs of age-standardized death rates compared with 2016–2017. § Nonoverlapping 95% CIs of age-standardized death rates compared with 2018–2019. ¶ The 100% alcohol-attributable chronic causes of death included alcohol abuse, alcohol cardiomyopathy, alcohol dependence syndrome, alcohol polyneuropathy, alcohol-induced acute pancreatitis, alcohol-induced chronic pancreatitis, alcoholic gastritis, alcoholic liver disease, alcoholic myopathy, and alcoholic psychosis. ** Cancer deaths from excessive alcohol use were estimated for deaths from breast cancer (females only), colorectal cancer, esophageal cancer (for the proportion due to squamous cell carcinoma only, based on the Surveillance, Epidemiology, and End Results Program data in 17 states), laryngeal cancer, liver cancer, oral cavity and pharyngeal cancer, pancreatic cancer, prostate cancer (males only), and stomach cancer. Deaths from pancreatic and stomach cancers were calculated among people consuming high daily average levels of alcohol only (females: >2 drinks, males: >4 drinks). †† Deaths from excessive alcohol use from heart disease and stroke were estimated for deaths from atrial fibrillation, coronary heart disease, hemorrhagic stroke, hypertension, and ischemic stroke. §§ Deaths from excessive alcohol use were estimated for deaths from conditions of the gallbladder, liver, and pancreas, including those from acute pancreatitis, chronic pancreatitis, esophageal varices, gallbladder disease, gastroesophageal hemorrhage, portal hypertension, and unspecified liver cirrhosis. ¶¶ Deaths from excessive alcohol use were estimated for deaths from other chronic conditions including chronic hepatitis; infant deaths due to low birthweight, preterm birth, and small for gestational age; pneumonia; and seizure disorder, seizures, and unprovoked epilepsy. *** Deaths from alcohol-related poisonings included those from alcohol poisoning (100% attributable to alcohol) and the portion of deaths from poisonings that involved another substance (e.g., drug overdoses) in addition to a high blood alcohol concentration (≥0.10%). ††† Deaths from excessive alcohol use from suicide included those from suicide by exposure to alcohol (100% attributable to alcohol) and a portion of deaths from suicide based on the alcohol-attributable fraction of 0.21. §§§ Deaths from excessive alcohol use from other acute conditions included the cause-specific portion of deaths for air-space transport, aspiration, child maltreatment, drowning, fall injuries, fire injuries, firearm injuries, homicide, hypothermia, motor vehicle nontraffic crashes, occupational and machine injuries, other road vehicle crashes, and water transport.
* Includes 58 causes of death related to alcohol use. Deaths from excessive alcohol use includes all decedents whose deaths were attributed to conditions that were fully caused by alcohol use, alcohol-related acute causes of death that involved binge drinking, and alcohol-related chronic conditions that involved medium (females: >1 to ≤2 drinks, males: >2 to ≤4 drinks) or high (females: >2 drinks, males: >4 drinks) daily average drinking levels. † Nonoverlapping 95% CIs of age-standardized death rates compared with 2016–2017. § Nonoverlapping 95% CIs of age-standardized death rates compared with 2018–2019. ¶ The 100% alcohol-attributable chronic causes of death included alcohol abuse, alcohol cardiomyopathy, alcohol dependence syndrome, alcohol polyneuropathy, alcohol-induced acute pancreatitis, and alcohol-induced chronic pancreatitis, alcoholic gastritis, alcoholic liver disease, alcoholic myopathy, and alcoholic psychosis. ** Cancer deaths from excessive alcohol use were estimated for deaths from breast cancer (females only), colorectal cancer, esophageal cancer (for the proportion due to squamous cell carcinoma only, based on the Surveillance, Epidemiology, and End Results Program data in 17 states), laryngeal cancer, liver cancer, oral cavity and pharyngeal cancer, pancreatic cancer, prostate cancer (males only), and stomach cancer. Deaths from pancreatic and stomach cancers were calculated among people consuming high daily average levels of alcohol only (females: >2 drinks, males: >4 drinks). †† Deaths from excessive alcohol use from heart disease and stroke were estimated for deaths from atrial fibrillation, coronary heart disease, hemorrhagic stroke, hypertension, and ischemic stroke. §§ Deaths from excessive alcohol use were estimated for deaths from conditions of the gallbladder, liver, and pancreas including those from acute pancreatitis, chronic pancreatitis, esophageal varices, gallbladder disease, gastroesophageal hemorrhage, portal hypertension, and unspecified liver cirrhosis. ¶¶ Deaths from excessive alcohol use were estimated for deaths from other chronic conditions including chronic hepatitis; infant deaths due to low birth weight, preterm birth, and small for gestational age; pneumonia; and seizure disorder, seizures, and unprovoked epilepsy. *** Deaths from alcohol-related poisonings included those from alcohol poisoning (100% attributable to alcohol) and the portion of deaths from poisonings that involved another substance (e.g., drug overdoses) in addition to a high blood alcohol concentration (≥0.10%). ††† Deaths from excessive alcohol use from suicide included those from suicide by exposure to alcohol (100% attributable to alcohol) and a portion of deaths from suicide based on the alcohol-attributable fraction of 0.21. §§§ No change in percentage of average annual deaths. ¶¶¶ Deaths from excessive alcohol use from other acute conditions included the cause-specific portion of deaths for air-space transport, aspiration, child maltreatment, drowning, fall injuries, fire injuries, firearm injuries, homicide, hypothermia, motor vehicle nontraffic crashes, occupational and machine injuries, other road vehicle crashes, and water transport.
FIGURE . Average annual number of deaths from excessive alcohol use,* by age group and period among males (A) and females (B) — United States, 2016–2021
* Deaths from excessive alcohol use includes all decedents whose deaths were attributed to conditions that were fully caused by alcohol use, alcohol-related acute causes of death that involved binge drinking, and alcohol-related chronic conditions that involved medium (females: >1 to ≤2 drinks, males: >2 to ≤4 drinks) or high (females: >2 drinks, males: >4 drinks) daily average drinking levels.
Suggested citation for this article: Esser MB, Sherk A, Liu Y, Naimi TS. Deaths from Excessive Alcohol Use — United States, 2016–2021. MMWR Morb Mortal Wkly Rep 2024;73:154–161. DOI: http://dx.doi.org/10.15585/mmwr.mm7308a1 .
MMWR and Morbidity and Mortality Weekly Report are service marks of the U.S. Department of Health and Human Services. Use of trade names and commercial sources is for identification only and does not imply endorsement by the U.S. Department of Health and Human Services. References to non-CDC sites on the Internet are provided as a service to MMWR readers and do not constitute or imply endorsement of these organizations or their programs by CDC or the U.S. Department of Health and Human Services. CDC is not responsible for the content of pages found at these sites. URL addresses listed in MMWR were current as of the date of publication.
All HTML versions of MMWR articles are generated from final proofs through an automated process. This conversion might result in character translation or format errors in the HTML version. Users are referred to the electronic PDF version ( https://www.cdc.gov/mmwr ) and/or the original MMWR paper copy for printable versions of official text, figures, and tables.
Exit Notification / Disclaimer Policy
- The Centers for Disease Control and Prevention (CDC) cannot attest to the accuracy of a non-federal website.
- Linking to a non-federal website does not constitute an endorsement by CDC or any of its employees of the sponsors or the information and products presented on the website.
- You will be subject to the destination website's privacy policy when you follow the link.
- CDC is not responsible for Section 508 compliance (accessibility) on other federal or private website.
- U.S. Department of Health & Human Services

- Virtual Tour
- Staff Directory
- En Español
You are here
The nih almanac, national institute on alcohol abuse and alcoholism (niaaa).
- Important Events
Legislative Chronology
The mission of the National Institute on Alcohol Abuse and Alcoholism (NIAAA) is to generate and disseminate fundamental knowledge about the adverse effects of alcohol on health and well-being, and apply that knowledge to improve diagnosis, prevention, and treatment of alcohol-related problems, including alcohol use disorder (AUD), across the lifespan.
NIAAA provides leadership in the national effort to reduce alcohol-related problems by:
- Conducting and supporting alcohol-related research in a wide range of scientific areas including neuroscience and behavior, epidemiology and prevention, treatment and recovery, and metabolism and health effects.
- Coordinating and collaborating with other research institutes and federal programs on alcohol-related issues.
- Collaborating with international, national, state, and local institutions, organizations, agencies, and programs engaged in alcohol-related work.
- Translating and disseminating research findings to health care providers, researchers, policymakers, and the public.
Important Events in NIAAA History
1970 —The Comprehensive Alcohol Abuse and Alcoholism Prevention, Treatment, and Rehabilitation Act was passed, establishing NIAAA as part of the National Institute of Mental Health (NIMH). Senator Harold E. Hughes of Iowa played a pivotal role in sponsoring the legislation, which recognized “alcohol abuse” and “alcoholism” as major public health problems.
1971 —The First Special Report to the U.S. Congress on Alcohol and Health was issued in December, part of a series of triennial reports established to chart the progress made by alcohol research toward understanding, preventing, and treating alcohol abuse and alcoholism.
1974 —NIAAA became an independent Institute within the Alcohol, Drug Abuse, and Mental Health Administration (ADAMHA), which also housed NIMH and the National Institute on Drug Abuse (NIDA).
1977 —NIAAA organized the first national research workshop on fetal alcohol syndrome (FAS), which reviewed the state of the research on FAS.
1980 —NIAAA science and staff were instrumental to the development of the Report to the President and the Congress on Health Hazards Associated with Alcohol and Methods to Inform the General Public of these Hazards ; this report influenced the following year’s publication of the U.S. Surgeon General’s Advisory on Alcohol and Pregnancy of 1981 .
1989 —NIAAA launched the Collaborative Studies on Genetics of Alcoholism with the goal of identifying the specific genes underlying vulnerability to alcoholism as well as collecting clinical, neuropsychological, electrophysiological, and biochemical data, and establishing a repository of immortalized cell lines.
1991 —NIAAA began the National Longitudinal Alcohol Epidemiologic Survey, designed to study drinking practices, behaviors, and related problems.
1994 —The medical success of disulfiram, a drug approved in 1951 by the U.S. Food and Drug Administration (FDA), spotlighted the effectiveness of pharmacological approaches for treating AUD. In 1994 and 2004, respectively, scientific evidence from NIAAA-supported studies helped achieve FDA approval of two new medications: naltrexone and acamprosate. NIAAA-supported studies also provided the foundation for the FDA’s more recent change in AUD clinical trial endpoints, opening the door for regulatory approval of a larger number of candidate AUD medications. In 2007, NIAAA established the NIAAA Clinical Investigations Group, a network of sites established to accelerate phase 2 clinical trials of promising compounds, and later expanded NCIG to include early human laboratory studies.
1995 —NIAAA celebrated its 25th anniversary.
1996 —NIAAA established the Mark Keller Honorary Lecture Series. The series pays tribute to Mark Keller, a pioneer in the field of alcohol research, and features a lecture each year by an outstanding alcohol researcher who has made significant and long-term contributions to our understanding of alcohol's effects on the body and mind.
1999 —NIAAA organized the first National Alcohol Screening Day, created to provide public education, screening, and referral for treatment when indicated. The program was held at 1,717 sites across the United States, including 499 college sites.
NIAAA co-sponsored the launch of The Leadership to Keep Children Alcohol Free, a unique coalition of state governors' spouses, federal agencies, and public and private organizations that targets prevention of drinking in young people ages 9–15.
2001 —NIAAA launched the 2001-2002 National Epidemiologic Survey on Alcohol and Related Conditions, a representative sample of the U.S. population with data on alcohol and drug use; alcohol and drug abuse and dependence; and associated psychiatric and other co-occurring disorders.
2002 —NIAAA published A Call to Action: Changing the Culture of Drinking at U.S. Colleges , which was developed by the Task Force of the National Advisory Council on Alcohol Abuse and Alcoholism as a comprehensive review of research on college drinking and the effectiveness of prevention programs.
2004 —NIAAA established the Underage Drinking Research Initiative by convening a steering committee of experts in adolescent development, child health, brain imaging, genetics, neuroscience, prevention research, and other research fields, with the goal of working towards a more complete and integrated scientific understanding of the environmental, biobehavioral, and genetic factors that promote initiation, maintenance, and acceleration of alcohol use among youth, framed within the context of human development.
2005 —NIAAA published Helping Patients Who Drink Too Much: A Clinician's Guide to help primary care and mental health clinicians incorporate alcohol screening and intervention into their practices. The 2005 edition introduced a simple one-question screening tool that streamlined recommendations published in earlier NIAAA guides.
The Surgeon General released the Surgeon General's Advisory on Alcohol Use in Pregnancy , updated from the original advisory released in 1981. As with the 1981 report, NIAAA science contributed significantly to the development of this document, and NIAAA staff were instrumental in its crafting.
2007 —NIAAA partnered with NIDA, the Robert Wood Johnson Foundation, and HBO to produce Addiction, an Emmy-award winning documentary exploring alcohol and drug addiction, treatment, and recovery, and featuring interviews with medical researchers working to better understand and treat addictive disorders.
2008 —The Acting Surgeon General of the United States issued The Surgeon General's Call to Action to Prevent and Reduce Underage Drinking . NIAAA’s Underage Drinking Research Initiative provided much of the scientific foundation for that document.
NIAAA published a special supplemental issue of the journal Pediatrics , presenting a developmental framework for understanding and addressing underage drinking as a guide to future research, prevention, and treatment efforts. The research reflected in these articles contributed to the development of The Surgeon General’s Call to Action To Prevent and Reduce Underage Drinking .
2009 —NIAAA established the Jack Mendelson, M.D., Honorary Lecture Series. The series pays tribute to Dr. Mendelson’s contributions to the field of clinical alcohol research, and features a lecture each year by an outstanding alcohol researcher whose clinical research has made significant and long-term contributions to our understanding of susceptibility to alcohol use disorder (AUD), alcohol's effects on the brain and other organs, and the prevention and treatment of AUD.
NIAAA launched Rethinking Drinking , a website and booklet, following extensive audience usability testing. These resources offer valuable, research-based information enabling people to take a look at their drinking patterns and how these patterns may be affecting their health.
2010 —To celebrate NIAAA’s 40th anniversary, the Institute published a special double issue of its peer-reviewed journal, Alcohol Research & Health that describes the Institute’s public health impact and multidisciplinary contributions to alcohol research. Additionally, on October 4, 2010, the Institute hosted a special symposium recognizing the 40th anniversary, where, leaders in the field discussed the ways in which alcohol research has evolved over the past 40 years, as well as NIAAA's role in this progress.
2011 —NIAAA released Alcohol Screening and Brief Intervention for Youth: A Practitioner's Guide , Developed in collaboration with the American Academy of Pediatrics, clinical researchers, and health practitioners, the guide introduced a two-question screening tool and an innovative youth alcohol risk estimator to help clinicians overcome time constraints and other common barriers to youth alcohol screening.
2012 —NIH announced the Trans-NIH Substance Use, Abuse, and Addiction Functional Integration to enhance the NIH Institute and Center (IC) collaborations around this important scientific and public health topic. The Functional Integration is a collaborative framework that draws on the collaboration among the NIH ICs on substance use, abuse, and addiction-related research. NIAAA and NIDA have made significant progress toward integrating their intramural research programs in substance use, abuse, and addiction, including the appointment of a single Clinical Director for both Institutes and the establishment of a joint genetics intramural research program and a common optogenetics lab. By pooling resources and expertise, the Functional Integration will identify cross-cutting areas of research and confront challenges faced by multiple Institutes and Centers.
2013 —NIAAA helped establish and participated in the NIH partnership, Collaborative Research on Addiction at NIH (CRAN). CRAN’s mission is to provide a strong collaborative framework to enable NIAAA, NIDA, and the National Cancer Institute (NCI), to integrate resources and expertise to advance substance use, abuse, and addiction research and public health outcomes. NIAAA helped launch a website to share funding opportunities and research resources readily with the public.
In addition, NIAAA developed and launched an online course for health care professionals to learn more about screening youth for alcohol problems. Doctors, nurses, psychologists, and others can take the online training to earn continuing medical education credits. The course, produced jointly with Medscape, shows providers how to conduct fast, evidence-based alcohol screening and brief intervention for patients ages 9–18. Since its launch in August, more than 5,000 health care professionals have earned credit for the course.
2015 —NIAAA launched CollegeAIM — the College Alcohol Intervention Matrix , a new resource to help schools address harmful and underage student drinking. In 2020, NIAAA published significant updates to the CollegeAIM website, updating resources and scientific evidence. NIAAA also added a clinician’s portal to the Alcohol Treatment Navigator website, helping clinicians to feel more confident making patient referrals for AUD.
2016 —NIAAA science and staff were instrumental to the development of Facing Addiction in America: The Surgeon General’s Report on Alcohol, Drugs, and Health . HBO Documentary Films premiered Risky Drinking, which follows the stories of four people whose drinking dramatically affects their relationships and their lives. This 85-minute film features commentary by experts including NIAAA Director George F. Koob, Ph.D., and NIAAA Medical Project Officer Deidra Roach, M.D.
2017 —NIAAA issued the NIAAA Strategic Plan, 2017-2021.
NIAAA also launched the Alcohol Treatment Navigator website to help adults find alcohol treatment for themselves or an adult loved one.
2018 —CRAN, based on the need to understand how substance use and other experiences during adolescence influence development, established the Adolescent Behavioral and Cognitive (ABCD) Study , a large scale, long-term, longitudinal study. In 2018, the ABCD study successfully completed its baseline enrollment of 11,874 participants ages 9 to 10 and began follow-up assessments which will continue into adulthood.
2020 —NIAAA celebrated its 50th anniversary with a range of events and promotional activities. These efforts culminated with a virtual 50th anniversary science symposium on November 30 and December 1, “Alcohol Across the Lifespan: 50 Years of Evidence-Based Diagnosis, Prevention, and Treatment Research.” Presentations spotlighted scientific milestones, the current state of the science, and future opportunities for alcohol research.
During the COVID-19 pandemic, NIAAA developed a list of web-based resources for the research community, healthcare professionals, and the general public regarding the potential for alcohol misuse, including information about telehealth for alcohol treatment. NIAAA also supported research on trends in alcohol use during the pandemic, and served as the lead institute for the NIH RADx-rad request for applications on “Automatic Detection and Tracing of SARs-CoV-2” to support proof-of-concept research on automatic, real-time detection and tracing of SARS-COV-2.
2022 —NIAAA released The Healthcare Professional's Core Resource on Alcohol help healthcare professionals provide evidence-based care for people who drink alcohol. Created with busy clinicians in mind, the HPCR provides concise, thorough information designed to help them integrate alcohol care into their practice.
2023 —As part of its efforts to raise awareness of and combat underage drinking, NIAAA launched the web resources NIAAA for Middle School and NIAAA for Teens , as well as a virtual reality and video experience, Alcohol and Your Brain .
December 31, 1970 —NIAAA was established under authority of the Comprehensive Alcohol Abuse and Alcoholism Prevention, Treatment, and Rehabilitation Act of 1970 (Public Law 91-616) with authority to develop and conduct comprehensive health, education, training, research, and planning programs for the prevention and treatment of alcohol abuse and alcoholism.
May 14, 1974 —P.L. 93-282 was passed, establishing NIAAA, NIMH, and NIDA as coequal institutes within the Alcohol, Drug Abuse, and Mental Health Administration (ADAMHA).
July 26, 1976 —NIAAA's research authority was expanded to include behavioral and biomedical etiology of the social and economic consequences of alcohol abuse and alcoholism under authority of the Comprehensive Alcohol Abuse and Alcoholism Prevention, Treatment, and Rehabilitation Act amendments of 1976 (P.L. 94-371).
August 1981 —The Omnibus Budget Reconciliation Act of 1981 (P.L. 97-35) was passed, transferring responsibility and funding for alcoholism treatment services to the states through the creation of an Alcohol, Drug Abuse, and Mental Health Services block grant administered by ADAMHA and strengthening NIAAA's research mission.
October 27, 1986 —A new Office for Substance Abuse Prevention in ADAMHA was created through the Anti-Drug Abuse Act of 1986 (P.L. 99-570), which consolidated the remainder of NIAAA's non-research prevention activities with those of NIDA and permitted NIAAA's total commitment to provide national stewardship to alcohol research.
July 10, 1992 —NIAAA became a new NIH research institute under the ADAMHA Reorganization Act of 1992 (P.L. 102-321).
December 20, 2006 —The Sober Truth on Preventing Underage Drinking Act (P.L. 109-422) was passed, requiring the Secretary of Health and Human Services to formally establish and enhance the efforts of the Interagency Coordinating Committee on the Prevention of Underage Drinking that began operating in 2004.
December 13, 2016 —The 21 st Century Cures Act (P.L. 114-255) was passed, requiring the Directors of NIAAA, the National Institute of Mental Health (NIMH), and the National Institute on Drug Abuse (NIDA) to serve as ex officio members of the Substance Abuse and Mental Health Services Administration (SAMHSA) Advisory Councils. It also called for increased collaboration between SAMHSA and NIAAA, NIDA, and the States to promote the study of substance abuse prevention and the dissemination and implementation of research findings that will improve the delivery and effectiveness of substance abuse prevention activities. Finally, it reauthorized the Sober Truth on Preventing Underage Drinking Act from 2018 through 2022.
Biographical Sketch of NIAAA Director George F. Koob, Ph.D.
George F. Koob, Ph.D. , is an internationally recognized expert on alcohol and stress, and the neurobiology of alcohol and drug addiction. As the Director of the NIAAA, he provides leadership in the national effort to reduce the public health burden associated with alcohol misuse. He oversees a broad portfolio of alcohol research ranging from basic science to epidemiology, diagnostics, prevention, and treatment.
Dr. Koob earned his doctorate in Behavioral Physiology from Johns Hopkins University in 1972. Prior to taking the helm at NIAAA, he served as Professor and Chair of the Scripps’ Committee on the Neurobiology of Addictive Disorders and Director of the Alcohol Research Center at the Scripps Research Institute. Early in his career, Dr. Koob conducted research in the Department of Neurophysiology at the Walter Reed Army Institute of Research and in the Arthur Vining Davis Center for Behavioral Neurobiology at the Salk Institute for Biological Studies. He was a post-doctoral fellow in the Department of Experimental Psychology and the MRC Neuropharmacology Unit at the University of Cambridge.
Dr. Koob began his career investigating the neurobiology of emotion, particularly how the brain processes reward and stress. He subsequently applied basic research on emotions, including on the anatomical and neurochemical underpinnings of emotional function, to alcohol and drug addiction, significantly broadening knowledge of the adaptations within reward and stress neurocircuits that lead to addiction. This work has advanced our understanding of the physiological effects of alcohol and other substance use and why some people transition from use to misuse to addiction, while others do not. Dr. Koob has authored more than 650 peer-reviewed scientific papers and is a co-author of The Neurobiology of Addiction , a comprehensive textbook reviewing the most critical neurobiology of addiction research conducted over the past 50 years.
Dr. Koob is the recipient of many prestigious honors and awards for his research, mentorship, and international scientific collaboration. In 2018, Dr. Koob received the E.M. Jellinek Memorial Award for his outstanding contributions to understanding the behavioral course of addiction, In 2017, Dr. Koob was elected to the National Academy of Medicine (NAM). In 2016, the government of France awarded Dr. Koob with the insignia of Chevalier de la Légion d’honneur (Knight of the Legion of Honor) for developing scientific collaborations between France and the United States. [View the video: World-class scientist Dr Koob receives the Legion of Honor .]
In addition, Dr. Koob previously received the Research Society on Alcoholism (RSA) Seixas Award for extraordinary service in advancing alcohol research; the RSA Distinguished Investigator Award; the RSA Marlatt Mentorship Award; the Daniel Efron Award for excellence in basic research and the Axelrod Mentorship Award, both from the American College of Neuropsychopharmacology; the NIAAA Mark Keller Award for his lifetime contributions to our understanding of the neurobiology of alcohol use disorder; and an international prize in the field of neuronal plasticity awarded by La Fondation Ipsen.
NIAAA Directors
NIAAA’s organizational chart is available here .
NIAAA Offices manage administrative, policy and communications activities across the institute.
Office of the Director, Director: Dr. George F. Koob The Office of the Director leads the Institute by setting research and programmatic priorities and coordinating cross-cutting initiatives. The Office includes:
Office of Extramural Activities, Director: Dr. Philippe Marmillot (Acting) The Office of Extramural Activities is responsible for extramural grant and contract review, the management of chartered initial review groups and special emphasis panels, and all grants management activities. OEA also manages the Committee Management Office—responsible for advisory council activities and nominations to advisory and review panels—and provides advice to the Institute's senior leadership on matters that concern FACA (Federal Advisory Committee Act) and non-FACA meetings.
Office of Science Policy and Communications , Director: Dr. Bridget Williams-Simmons The goal of the Office of Science Policy and Communications (OSPC) is to give visibility to NIAAA-supported research and initiatives and to establish NIAAA as an authoritative source of evidence-based information on alcohol and health in support of the NIAAA mission. OSPC serves a broad range of stakeholders including NIH and NIAAA leadership, the Department of Health and Human Services, the Office of National Drug Control Policy, Congress, the research community, health professionals, advocacy organizations, the media, and patients and the public at large.
Office of Resource Management, Director: Ms. Vicki Buckley The Office of Resource Management provides administrative management support to the Institute in the areas of financial management, grants and contracts management, administrative services, and personnel operations; (2) develops administrative management policies, procedures, guidelines, and operations; (3) maintains liaison with the management staff of the Office of the Director and implements within the Institute general management policies prescribed by NIH and higher authorities.
NIAAA’s Divisions manage the Institute’s intramural and extramural basic, translational, and clinical research.
Division of Intramural Clinical and Biological Research , Scientific Director: Dr. David Lovinger; Clinical Director: Dr. David Goldman The Division of Intramural Clinical and Biological Research seeks to understand the mechanisms by which alcohol produces intoxication, dependence, and damage to vital body organs, and to develop tools to prevent and treat those biochemical and behavioral processes.
Division of Epidemiology and Prevention Research , Director: Dr. Ralph Hingson The Division of Epidemiology and Prevention Research promotes and supports applied, translational, and methodological research on the epidemiology and prevention of hazardous alcohol consumption and related behaviors, alcohol use disorder, alcohol-related mortality and morbidity, and other alcohol-related problems and consequences.
Division of Metabolism and Health Effects , Director: Dr. Kathy Jung The Division of Metabolism and Health Effects develops scientific initiatives and supports basic and translational research on the health consequences of alcohol consumption and metabolism.
Division of Neuroscience and Behavior , Director: Dr. Antonio Noronha The Division of Neuroscience and Behavior promotes research on ways in which neuronal and behavioral systems are influenced by genetic, developmental, and environmental factors in conjunction with alcohol exposure to engender alcohol use disorder.
Division of Treatment and Recovery , Director: Dr. Raye Z. Litten The Division of Treatment and Recovery stimulates and supports research to identify and improve pharmacological and behavioral treatment for alcohol use disorder, enhance methods for sustaining recovery, and increase the use of evidence-based treatments in real-world practice.
For more information about NIAAA research programs, visit the NIAAA Research webpage .
Communications and Outreach Activities
NIAAA has several major web resources to disseminate unbiased science and health information to a range of audiences and stakeholders, which include:
- NIAAA primary website
- Rethinking Drinking
- Alcohol Treatment Navigator
- NIAAA for Middle School
- NIAAA for Teens
- College Drinking Prevention
- College Alcohol Intervention Matrix (CollegeAIM )
- The Healthcare Professional's Core Resource on Alcohol
- Alcohol Research: Current Reviews
- Collaborative Research on Addiction at NIH
NIAAA also uses social media outlets to share health information, the latest science discoveries, funding and training opportunities, events, and initiatives with broader, more diverse audiences.
- Twitter: @NIAAAnews
- Facebook: @NIAAAgov
- Instagram: @NIAAAnews
- YouTube: @NIAAANIH
NIAAA also plans events and other activities with a network of liaison organizations. These organizations include research and professional societies, advocacy groups, and other interested stakeholders.
This page last reviewed on March 28, 2024
Connect with Us
- More Social Media from NIH
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.

Trusted Health Information from the National Institutes of Health
Why alcohol-use research is more important than ever
Nih's george koob talks about how addiction changes the brain and the rise in alcohol-related deaths.

Alcohol use disorder is a common but serious condition that affects how the brain functions.

George Koob, Ph.D.
Alcohol use disorder (AUD) affects roughly 15 million people in the U.S. People with the condition may drink in ways that are compulsive and uncontrollable, leading to serious health issues.
"It's the addiction that everyone knows about, but no one wants to talk about," says George Koob, Ph.D., the director of the National Institute on Alcohol Abuse and Alcoholism (NIAAA).
As NIAAA celebrates an important milestone this year—its 50th anniversary—the institute's research is more important than ever. Like NIAAA reported earlier this year, alcohol-related health complications and deaths as a result of short-term and long-term alcohol misuse are rising in the U.S.
"Alcohol-related harms are increasing at multiple levels—from emergency department visits and hospitalizations to deaths," Dr. Koob says. He spoke about NIAAA efforts that are working to address this and how people can get help.
What has your own research focused on?
I started my career researching the science of emotion: how the brain processes things like reward and stress. Later, I translated this to alcohol and drug addiction and investigating why some people go from use to misuse to addiction, while others do not.
What are some major breakthroughs NIAAA has made in this area?
We now understand how alcohol affects the brain and why it causes symptoms of AUD . This has far-reaching implications for everything from prevention to treatment. We also understand today that AUD physically changes the brain. This has been critical in treating it as a mental disorder, like you would treat major depressive disorder.
Other breakthroughs have been made in screening and intervention, and in the medications available for treatment. All of this has led to a better understanding of how the body changes when one misuses alcohol and the proactive actions we can take to prevent alcohol misuse.
What is a misconception that people have about AUD?
Many people don't realize how common AUD is. There are seven times more people affected by AUD than opioid use disorder, for example. It doesn't discriminate against who it affects. People also don't realize that AUD is a brain disorder that actually changes how the brain functions. Severe AUD is associated with widespread injury to the brain, though some of the effects might be partially reversible.
What's next for NIAAA?
For five decades, the institute has studied how alcohol affects our health, bringing greater awareness to alcohol-related health issues and providing better options for diagnosis and treatment. Recent research has focused on areas such as the genetics of addiction, links between excessive alcohol use and mental health and other disorders, harm to long-term brain health that can be caused by adolescent alcohol use, and the effects of prenatal alcohol exposure, among others.
"We want everyone from pharmacists and nurses to addiction medicine specialists to know more about alcohol and addiction." - George Koob, Ph.D.
Currently, we are working on a number of initiatives. One is education. We want everyone from pharmacists and nurses to addiction medicine specialists to know more about alcohol and addiction. We're also working on prevention resources for middle school-aged adolescents. Other goals include understanding recovery and what treatments work best for people and why. We're also learning more about alcohol's effects on sleep and pain, and we have ongoing efforts in medication development.
Finally, we're learning more about the impact of alcohol on women and older adults. Women have begun to catch up to men in alcohol consumption and alcohol-related harms. Women are more susceptible to some of the negative effects that alcohol has on the body, from liver disease to certain cancers. Further, more older adults are binge drinking and this places them at greater risk of alcohol-medication interactions, falls, and health problems related to alcohol misuse.
How can someone get help?
If alcohol is negatively affecting you or someone you know, seek help from someone you respect. For example, a primary care doctor or clergy member. There are a number of online resources from NIAAA, like the NIAAA Alcohol Treatment Navigator® , an online resource to help people understand AUD treatment options and search for professionally led, evidence-based alcohol treatment nearby. There's also Rethinking Drinking SM , an interactive website to help individuals assess and change their drinking habits. Also, know that there is hope. Many people recover from AUD and lead vibrant lives.
July 16, 2020
You May Also Like

Eric Paslay doesn’t miss a note living with type 1 diabetes
Singer and songwriter Eric Paslay may have chosen a different career path than his original dream of pediatrics, but he’s...

ADHD support toolkit
If someone in your life has attention-deficit/hyperactivity disorder (ADHD), here are some ways you can offer your support. ...

ADHD across the lifespan: What it looks like in children and teens
Attention-deficit/hyperactivity disorder (ADHD) affects the brain's ability to focus and control impulses and is one of the most...
Trusted health information delivered to your inbox
Enter your email below

An official website of the United States government
Here's how you know
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.

Volume 38 Issue 1 January 1, 2016
Drinking Across the Lifespan: Focus on Older Adults
Part of the Topic Series: Alcohol Use Among Special Populations
Kristen L. Barry, Ph.D., and Frederic C. Blow, Ph.D.
Kristen L. Barry, Ph.D., is a research professor and Frederic C. Blow is a professor, both in the Department of Psychiatry at the University of Michigan, Ann Arbor, Michigan.
A substantial and growing number of older adults misuse alcohol. The emerging literature on the “Baby Boom” cohort, which is now reaching older adulthood, indicates that they are continuing to use alcohol at a higher rate than previous older generations. The development and refinement of techniques to address these problems and provide early intervention services will be crucial to meeting the needs of this growing population. This review provides background on the extent of alcohol misuse among older adults, including the Baby Boom cohort that has reached age 65, the consequences of misuse, physiological changes related to alcohol use, guidelines for alcohol use, methods for screening and early interventions, and treatment outcomes.
In 2010, when the leading edge of the post–World War II “Baby Boom” reached age 65, the United States began a period of increased growth in its older adult population. By 2030, it is expected that there will be 72.1 million adults age 65 or older living in the United States, almost double the 2008 population. Those older adults will represent 19.3 percent of the U.S. population, compared with 12.9 percent of the population in 2009 (Administration on Aging 2011; U.S. Census Bureau 2013). The United States is facing a “silver tsunami” that will greatly influence many segments of society, including the economy, large-scale societal programs, and the health care system. Aging research focused on “older adulthood” defines this cohort in a variety of ways, most commonly as age 50 or older, 60 or older, and 65 or older (Substance Abuse and Mental Health Service Administration [SAMHSA] 2012 a ). In this article, “older adulthood” refers to individuals who are age 65 or older, unless otherwise indicated in the text (Bartels and Naslund 2013).
The aging of the Baby Boom population will severely tax the current health care system (Bartels and Naslund 2013). There is a paucity of clinicians specializing in geriatric medicine and geriatric psychiatry. In addition, there is no single agency in the United States in charge of the mental and physical health care of this vulnerable and growing population of older adults who are more likely than previous older generations to experience problems related to mental health and alcohol use. In fact, as the Baby Boom cohort moves into older adulthood, they are likely to use more alcohol than previous generations of older adults. Misuse and abuse of alcohol, and the combination of alcohol with the use of some medications (including benzodiazepines, sedatives, and opioid analgesics), can lead to negative health outcomes. With the size of the emerging older population and their comparatively higher acceptance of alcohol and drugs, there is a growing concern that there will be a substantial increase in the number of older adults at risk for alcohol misuse and abuse (Agency for Healthcare Research and Quality 2010; Korper and Council 2002).
Increased at-risk use and abuse of alcohol in older adults will present unique challenges in terms of recognition, interventions, and determining the most appropriate treatment options, when needed. Alcohol problems in this age group often are not recognized and, if recognized, generally are undertreated. However, older adults are more likely than younger adults to seek services from their primary and specialty care providers, which opens the door to greater recognition and assistance for those who drink above guidelines. Health care providers who work with older adults have a unique opportunity to observe and treat the repercussions of alcohol misuse, abuse, and dependence.
This review focuses on the prevalence of alcohol misuse, abuse, and dependence in older adults; guidelines for use; physiological changes in sensitivity and tolerance; and the efficacy and effectiveness of screening, interventions, and treatments in this age group.
Prevalence of Alcohol Misuse Among Older Adults
At-risk alcohol and drug use.
Over the last three decades, studies have estimated that the prevalence of at-risk and problem drinking among older adults ranges from 1 percent to 16 percent (Menninger 2002; Moore et al. 1999; SAMHSA 2004, 2007). These rates vary widely, depending on the definitions of older adults, at-risk and problem drinking, alcohol abuse/dependence, and the methodology used in obtaining samples. The 2013 National Survey on Drug Use and Health (NSDUH), for example, found heavy drinking (defined as drinking 5 or more drinks on the same occasion on each of 5 or more days in the past 30 days) among 5.6 percent of 50- to 54-year-olds, 3.9 percent of 55- to 59-year-olds, 4.7 percent of 60- to 64-year-olds, and 2.1 percent of those over age 65 (SAMHSA 2014). It found even higher rates of binge drinking (defined as drinking 5 or more drinks on the same occasion on at least 1 day in the past 30 days) among these age groups; 23.0 percent of 50- to 54-year-olds, 15.9 percent of 55- to 59-year-olds, 14.1 percent of 60- to 64-year-olds, and 9.1 percent of those over 65 (SAMHSA 2014).
In addition, studies find higher rates of at-risk use and abuse among people seeking health care, because people with alcohol dependence who have at-risk use and/or are beginning to experience consequences related to that use are more likely to seek medical care (Oslin 2004). Early studies in primary care settings found that 10 to 15 percent of older patients met criteria for at-risk or problem drinking (Barry 1999), defined by the National Institute on Alcohol Abuse and Alcoholism (NIAAA) as more than one-half to 1 drink per day or 7 drinks per week for women and more than 2 drinks per day or 14 drinks per week for men (Gunzerath et al. 2004; NIAAA 1995, 2007; Willenbring et al. 2009). Because patients with a previous history of problems with alcohol or other drugs are at risk for relapse, establishing a history of use can provide important clues for future problems.
Alcohol Misuse/Dependence
The rates of alcohol misuse/dependence in older adults are by far smaller than the rates of at-risk use. In 2002, over 616,000 adults age 55 and older reported meeting the criteria for alcohol dependence in the past year, as defined by the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM–IV) . They represented 1.8 percent of those age 55–59, 1.5 percent of those age 60–64, and 0.5 percent of those age 65 or older (SAMHSA 2002). Later data from NSDUH showed that 780,000 older adults had alcohol abuse/dependence (SAMHSA 2012 a ). The NSDUH also has shown that illicit drug use increased from 1 percent in 2003 and 2004 to 3.9 percent in 2013 (SAMHSA 2014), suggesting that both alcohol and drug use have increased slightly in older adulthood.
Although substance dependence is less common in older adults when compared with younger adults, the mental and physical health consequences in this age group are serious (Barry and Blow 2010). Indeed, although the majority of older adults who are experiencing drinking-related problems do not meet criteria from the DSM–IV for alcohol abuse or dependence (SAMHSA 2012 b ), the diagnostic criteria that relate to the physical and emotional consequences of alcohol use may be especially important in identifying alcohol use disorders in older adults.
Impact of Physiological Changes on Alcohol Consumption
Older adults are more vulnerable to the physiological effects of alcohol than younger adults (Gargiulo et al. 2013). Alcohol consumption in amounts considered light or moderate for younger adults may have untoward health effects in older people because it is processed differently (Ferreira and Weems 2008; Gargiulo et al. 2013). In particular, as people age, liver enzymes that metabolize alcohol and other drugs are less efficient, and the central nervous system becomes more sensitive to drugs. In addition, age-related decreases in lean body mass result in a decrease in the aqueous volume of cells, which in turn increases the effective concentration of alcohol and other mood-altering chemicals in the body. Because drinking comparable amounts of alcohol produces higher and longer-lasting blood alcohol levels in older adults than in younger people, many problems common among older people, such as chronic illness and poor nutrition may be exacerbated by even small amounts of alcohol. Likewise, because older adults who drink are more likely to take alcohol-interactive medications than younger drinkers (Breslow et al. 2015), they may be at increased risk for adverse alcohol-medication interactions. Clinicians who treat older patients can assess the number of drinks per day, the number of drinking days, and any binge drinking to begin to address the health implications of an individual’s pattern of use.
Risks of Heavier Drinking in Older Adulthood
Studies analyzing data from the National Health and Retirement Study (Bobo et al. 2013) found that, although overall alcohol consumption declined with age, for a minority of individuals, consumption increased. Those who increased their consumption over time were more likely to be affluent, highly educated, male, Caucasian, unmarried, less religious, and perceive themselves to be in excellent health.
Heavy drinking or binge drinking is of particular concern in all age groups. But, as people age, binge drinking is thought to pose even higher risks for morbidity, including accidents, and mortality. To evaluate the relationship between drinking patterns and health in older adults, Holahan and colleagues (2012) studied 446 people with a mean age of 62 at the beginning of the study. Study participants were “moderate drinkers” based on NIAAA’s guidelines of drinking at least half a drink per day but no more than half a drink per day for women and two drinks per day for men (NIAAA 2007). Some also were moderate drinkers who had periods of episodic heavy drinking or binge drinking defined as drinking four or more drinks for women and five or more drinks for men on the occasion of the largest amount of drinking. Overall, the study found that moderate drinkers who engaged in episodic heavy drinking were more than twice as likely to die within 20 years compared with regular moderate drinkers.
Older adults also are at greater risk for harmful drug interactions, injury, depression, memory problems, liver disease, cognitive changes, sleep problems, cancer, and diabetes that can be related to heavier alcohol consumption (Blow and Barry 2012; Holahan et al. 2012; Moore et al. 2007; Mukamal et al. 2010; Wu and Blazer 2011). In addition, heavier drinking in this age group can significantly affect a number of other conditions in older adults (Fleming and Barry 1992), including mood disorders, sleep, and pain, as well as general health functioning (American Medical Association [AMA] 2008; Blow et al. 2002).
Not all research finds negative consequences of alcohol for older adults. In particular, one study suggests alcohol may decrease the risk of coronary heart disease. The Coro nary Heart Disease Study looked at factors, including alcohol consumption, related to the risk of coronary heart disease in older adults. In the older adult sample of more than 4,400 subjects who were free of known coronary heart disease at baseline, consumption of 14 or more drinks per week was associated with the lowest risk of coronary heart disease in the long term (Mukamal et al. 2010). Because of the risks of other disorders related to heavy alcohol use, these findings need to be placed in the context of known adverse effects of heavy drinking and the established recommended guidelines for alcohol use in older adults.
In addition to concerns regarding the misuse of alcohol alone, up to 19 percent of older Americans combine alcohol and medications in a way that can be considered misuse (NIAAA 1998 a , b ). Mixing alcohol and psychoactive medications such as benzodiazepines, sedatives, and opioid analgesics has the potential for very serious negative outcomes that prescribing physicians should discuss with older adult patients. And although the use and misuse of illicit drugs is less common in the current cohort of older adults—1.8 percent among people age 50 and over in 2002–2003 (SAMHSA 2007)—research suggests that that number is likely to increase as a result of the aging of the Baby Boom generation (Bartels and Naslund 2013).
Screening and Brief Interventions
Alcohol screening and brief interventions offer opportunities for early detection, focused motivational enhancement, and targeted encouragement to seek needed substance abuse treatment, where appropriate. The majority of older adults who misuse alcohol do not need formal specialized substance abuse treatment. Rather, many can benefit from screening and brief interventions regarding their drinking (Kuerbis et al. 2015; Pilowsky and Wu 2012).
Screening, including rapid prescreening, for alcohol use and potential deleterious consequences of alcohol use is a critical first step in identifying individuals who may need additional in-depth assessment and those who may benefit from brief interventions and/or treatment. Screening generally identifies at-risk and harmful substance use. In contrast, more extensive assessments measure the severity of the substance use; problems and consequences associated with use; factors that may be contributing to substance abuse; and other characteristics of the problem. The screening and assessment process should help clinicians determine if the level of alcohol use is appropriate for a brief intervention or if it warrants a different approach. Clinicians can administer simple questions about alcohol use via a paper-and-pencil or computerized questionnaire or as part of a clinical interview and can follow up with additional questions as needed (adapted from Helping Patients Who Drink Too Much: A Clinician’s Guide , NIAAA 2007).
The Alcohol Use Disorders Identification Test (AUDIT) is a useful validated brief screening instrument for excessive drinking developed by the World Health Organization (WHO) (Barry and Fleming 1993; Fiellin et al. 2000; Schmidt et al. 1995). A 10-item questionnaire that collects alcohol-related information about the previous year only, AUDIT often is used without a clinical examination. And although the recommended cut-off score for the AUDIT typically is 8, early research suggests that, for older adults, a score of 5 should trigger additional clarifying questions (Barry et al. 2001).
Researchers at the University of Michigan have developed the Michigan Alcoholism Screening Test—Geriatric Version (MAST-G) and the shorter version, the Short Michigan Alcoholism Screening Test—Geriatric Version SMAST-G (Blow et al. 1992) as a screening instrument specifically for use with older adults in a variety of settings. The MAST-G includes items unique to older problem drinkers and relies on a 24-item scale with good sensitivity and specificity in older adults. The SMAST-G, with 10 items, is a validated shortened form of the MAST-G.
Brief Interventions
There is a large body of evidence showing that brief interventions delivered in a variety of health care and social service settings can effectively reduce drinking, particularly for at-risk and problem users under age 60. Indeed, researchers have conducted over 100 studies of brief intervention techniques over the past 25 years. The general format of brief alcohol interventions has been relatively consistent over time (Barry 1999). Typically, interventions include personalized feedback based on a person’s responses to screening questions and generic messages to cut down on or stop drinking. In primary care, brief interventions for a patient with at-risk or problem drinking might include a few simple, straightforward comments about concerns regarding the patient’s pattern of alcohol use and recommendations that the patient reduce or stop drinking or might include several short counseling sessions followed by telephone followup (NIAAA 2007). Brief interventions use motivational interviewing principles and nonjudgmenta l language, eliciting the potential to change and/or consider change.
Early studies in Europe and other countries demonstrated 10 to 20 percent reductions in drinking for people receiving a brief intervention compared with people in control groups (e.g., Saunders et al. 1993). In addition, meta-analyses of randomized controlled studies examining the effectiveness of brief interventions find that these techniques generally reduce drinking in the intervention group. For example, Whitlock and colleagues (2004) examined 39 studies. Among the 12 that met their criteria for inclusion, participants reduced their average number of drinks per week by 13 to 34 more than did control subjects. The majority of brief intervention trials have been conducted in primary care settings (e.g., Fleming et al. 1997; Whitlock et al. 2004). However, a number of successful brief alcohol intervention trials have been conducted in emergency settings with individuals of varying ages and levels of alcohol use (see Havard et al. 2008 and Carey et al. 2012 for meta-analyses).
The few studies of brief interventions with older adults have found them to be effective in reducing at-risk alcohol use (e.g., Fleming et al. 1997; Moore et al. 2011). Specifically, screening and brief interventions in a variety of health care and social service settings have reduced alcohol consumption among older adults, with these reductions sustained for 2 to 18 months (Fleming et al. 1997; Moore et al. 2011; Schonfeld et al. 2010).
Alcohol Treatment
Although alcohol abuse/dependence is a significant and growing health problem for the increasing population of older adults in the United States (AMA 1996; Bartels and Naslund 2013), there have been very few systematic studies of alcohol treatment outcomes for older adults (Bobo et al. 2013; Oslin et al. 2005; Satre et al. 2012). Because traditional substance use treatment programs have provided services to few older adults, sample size issues have been a barrier to studying treatment outcomes for older adults who meet criteria for abuse/dependence.
The few studies in this area generally have focused on the completion of prescribed treatment activities and adherence to drinking goals—generally abstinence. Of note is that older adults with alcohol use disorder were significantly more likely to complete treatment than younger adults. More recently, Lemke and Moos (2003) found that older adults in residential treatment had better long-term outcomes than matched groups of young and middle-aged patients. Longer duration of care and more use of self-help groups positively influenced outcomes. They also found that older adults were more likely to complete treatment and had more days of sobriety than younger adults. Satre and colleagues (2012) compared 5-year treatment outcomes for adults age 55 or older, age 18–39, and age 40–54. They found that the 55-and-over group were less likely to be alcohol/drug dependent at treatment entry and stayed longer in treatment. They also were less likely, at 5 years posttreatment, to have family and friends that encouraged alcohol use. Older females were more likely than any other group to be abstinent at followup.
Age of onset of alcohol problems has been posited as a consideration in treatment outcomes. Specifically, some researchers have hypothesized that people who experience alcohol problems later in life are more likely to have better outcomes than those whose alcohol problems start earlier. A small study by Schonfeld and Dupree (1991) used a matched-pairs, post hoc design to determine rates of completion of a 6-month day-treatment program. They compared alcohol-dependent male and female patients, age 55 or older, whose alcohol problems began before age 50 (early onset) with those who began problem drinking after age 50 (late onset). The late-onset group was significantly more likely to complete treatment.
There remain major limitations in the treatment literature for older adults, including insufficient drinking outcome data, failure to report on treatment dropouts, and variations in definitions of treatment completion. However, with the aging of the Baby Boom cohort and the potential for treatment needs in a larger population of older drinkers, there is beginning to be a greater emphasis on determining treatment outcomes for this population.
Conclusions
The health care delivery system remains one of the most efficient and effective venues in which to detect at-risk drinking, combined use of alcohol and psychoactive prescription medications, and comorbid mental and physical health conditions in older adults. It also is a key setting for interventions to improve the quality of life for many older adults. And there is a growing body of knowledge about useful screening tools, easy-to-use intervention methods, and brief and long-term treatments for use in the health care setting with this age group.
However, clinicians may need brief skills training to be able to assess effectively and more rapidly the quantity and frequency of alcohol use as well as any comorbid physical and mental health issues (e.g., depression and suicide risk) in this age group. Health care delivery occurs in an increasingly fast-paced environment, with many competing demands being placed on providers. Therefore, targeted training that focuses on screening and nonjudgmental intervention techniques with older adults could improve both skills and efficiency. Changes in the health care environment in the United States underscore the importance of using these brief cost-effective techniques with older adults with substance-related problems. Because many older adults confront multiple challenges, including social isolation, loss and grief, economic difficulties, and physical illnesses, health care professionals may assume that all symptoms are an inevitable result of these difficulties and may not recognize characteristics of at-risk drinking or alcohol abuse. The use of screening and intervention techniques that take into account issues specific to older adults moves the field toward providing best practice care to a potentially vulnerable population.

Disclosures
The authors declare that they have no competing financial interests.
Administration on Aging. A Profile of Older Americans: 2011 . Washington, DC: U.S. Department of Health and Human Services, 2011.
Agency for Healthcare Research and Quality (AHRQ). Hospitalizations for Medication and Illicit Drug-Related Conditions on the Rise among Americans Ages 45 and Older, 2010. Rockville, MD: AHRQ, 2010. Available at: http://archive.ahrq.gov/news/newsroom/press-releases/2010/hospmed.html . Accessed July 9, 2015.
American Medical Association, Council on Scientific Affairs. Alcoholism in the elderly. JAMA 275(10):797–801, 1996. PMID: 8598598
American Medical Association (AMA). Opinion 2.02—Physicians’ Obligations in Preventing, Identifying, and Treating Violence and Abuse. Chicago: AMA, 2008. Available at: http://www.ama-assn.org/ama/pub/physician-resources/medical-ethics/code-medical-ethics/opinion202.page? . Accessed July 9, 2015.
Barry, K. Brief Interventions and Brief Therapies for Substance Abuse . Rockville, MD: Substance Abuse and Mental Health Services Administration, Center for Substance Abuse Treatment, 1999.
Barry, K.L., and Blow, F.C. Screening, assessing and intervening for alcohol and medication misuse in older adults. In: Lichtenberg, P., Ed. Handbook of Assessment in Clinical Gerontology, 2nd Edition. New York: Wiley, 2010, pp. 307−330.
Barry, K.L., and Fleming, M.F. The Alcohol Use Disorders Identification Test (AUDIT) and the SMAST-13: Predictive validity in a rural primary care sample. Alcohol and Alcoholism 28(1):33–42, 1993. PMID: 8471085
Barry, K.L.; Oslin, D.W.; and Blow, F.C. Alcohol Problems in Older Adults: Prevention and Management . New York: Springer, 2001.
Bartels, S.J., and Naslund, J.A. The underside of the silver tsunami: Older adults and mental health care. New England Journal of Medicine 368(6):493–496, 2013. PMID: 23343039
Blow, F.C., and Barry, K.L. Alcohol and substance misuse in older adults. Current Psychiatry Reports 14(4):310–319, 2012. PMID: 22660897
Blow, F.C.; Barry, K.L.; Fuller, B.; and Booth, B.M. Analysis of the National Health and Nutrition Examination Survey (NHANES): Longitudinal analysis of drinking over the lifespan. In: Korper, S.P., and Council, C.L., Eds. Substance Use by Older Adults: Estimates of Future Impact on the Treatment System . Rockville, MD: Substance Abuse and Mental Health Services Administration, Office of Applied Studies, 2002, pp. 125–141.
Blow, F.C.; Brower, K.J.; Schulenberg, J.E.; et al. The Michigan Alcoholism Screening Test–Geriatric Version (MAST-G): A new elderly-specific screening instrument [abstract]. Alcoholism: Clinical and Experimental Research 16:372, 1992.
Bobo, J.K.; Greek, A.A.; Klepinger, D.H.; and Herting, J.R. Predicting 10-year alcohol use trajectories among men age 50 years and older. American Journal of Geriatric Psychiatry 21(2):204–213, 2013. PMID: 23343494
Breslow, R.A.; Dong, C.; and White, A. Prevalence of Alcohol-Interactive Prescription Medication Use Among Current Drinkers: United States, 1999 to 2010. Alcoholism: Clinical and Experimental Research 39(2):371–379, 2015.
Carey, K.B.; Scott-Sheldon, L.A.; Elliott, J.C.; et al. Face-to-face versus computer-delivered alcohol interventions for college drinkers: A meta-analytic review, 1998 to 2010. Clinical Psychology Review 32(8):690–703, 2012. PMID: 23022767
Ferreira, M.P., and Weems, M.K. Alcohol consumption by aging adults in the United States: Health benefits and detriments. Journal of the American Dietetic Association 108(10):1668–1676, 2008. PMID: 18926132
Fiellin, D.A.; Reid, M.C.; and O’Connor, P.G. Outpatient management of patients with alcohol problems. Annals of Internal Medicine 133(10):815–827, 2000. PMID: 11085845
Fleming, M.F., and Barry, K.L. Eds. Addictive Disorders . St. Louis, MO: Mosby Yearbook Medical Publishers, 1992.
Fleming, M.F.; Barry, K.L.; Manwell, L.B.; et al. Brief physician advice for problem alcohol drinkers: A randomized controlled trial in community-based primary care practices. JAMA 277(13):1039–1045, 1997. PMID: 9091691
Gargiulo, G.; Testa, G.; Cacciatore, F.; et al. Moderate alcohol consumption predicts long-term mortality in elderly subjects with chronic heart failure. Journal of Nutrition, Health, & Aging 17(5):480–485, 2013. PMID: 23636551
Gunzerath, L.; Faden, V.; Zakhari, S.; and Warren, K. National Institute on Alcohol Abuse and Alcoholism report on moderate drinking. Alcoholism: Clinical and Experimental Research 28(6):829–847, 2004. PMID: 15201626
Havard, A.; Shakeshaft, A.; and Sanson-Fisher, R. Systematic review and meta-analyses of strategies targeting alcohol problems in emergency departments: Interventions reduce alcohol-related injuries. Addiction 103(3)368–376; discussion 377–378, 2008. PMID: 18190671
Holahan, C.J.; Schutte, K.K.; Brennan, P.L.; et al. Wine consumption and 20-year mortality among late-life moderate drinkers. Journal of Studies on Alcohol and Drugs 73(1):80–88, 2012. PMID: 22152665
Korper, S.P., and Council, C.L., Eds. Substance Use by Older Adults: Estimates of Future I mpact on the Treatment System . Rockville, MD: SAMHSA, Office of Applied Studies, 2002 .
Kuerbis, A.N.; Yuan, S.E.; Borok, J.; et al. Testing the initial efficacy of a mailed screening and brief feedback intervention to reduce at-risk drinking in middle-aged and older adults: The Comorbidity Alcohol Risk Evaluation Study. Journal of the American Geriatrics Society 63(2):321–326, 2015. PMID: 25643851
Lemke, S., and Moos, R.H. Outcomes at 1 and 5 years for older patients with alcohol use disorders. Journal of Substance Abuse Treatment 24(1):43–50, 2003. PMID: 12646329
Menninger, J.A. Assessment and treatment of alcoholism and substance-related disorders in the elderly. Bulletin of the Menninger Clinic 66(2):166–183, 2002. PMID: 12141383
Moore, A.A.; Blow, F.C.; Hoffing, M.; et al. Primary care-based intervention to reduce at-risk drinking in older adults: A randomized controlled trial. Addiction 106(1):111–120, 2011. PMID: 21143686
Moore, A.A.; Morton, S.C.; Beck, J.C.; et al. A new paradigm for alcohol use in older persons. Medical Care 37(2):165–179, 1999. PMID: 10024121
Moore, A.A.; Whiteman, E.J.; and Ward, K.T. Risks of combined alcohol/medication use in older adults. American Journal of Geriatric Pharmacotherapy 5(1):64–74, 2007. PMID: 17608249
Mukamal, K.J.; Chen, C.M.; Rao, S.R.; and Breslow, R.A. Alcohol consumption and cardiovascular mortality among U.S. adults, 1987 to 2002. Journal of the American College of Cardiology 55(13):1328–1335, 2010. PMID: 20338493
National Institute on Alcohol Abuse and Alcoholism (NIAAA). The Physician’s Guide to Helping Patients With Alcohol Problems . Rockville, MD: NIAAA, 1995.
National Institute on Alcohol Abuse and Alcoholism (NIAAA). Alcohol Alert, No. 40: “Alcohol and Aging.” Rockville, MD: NIAAA, 1998 a .
National Institute on Alcohol Abuse and Alcoholism (NIAAA). Drinking in the United States: Main Findings from the 1992 National Longitudinal Alcohol Epidemiologic Survey (NLAES) . Rockville, MD: NIAAA, 1998 b .
National Institute on Alcohol Abuse and Alcoholism (NIAAA). Helping Patients Who Drink Too Much: A Clinician’s Guide (Updated) . NIH Publications No. 07–3769. Rockville, MD: NIAAA, 2007. Available at: https://pubs.niaaa.nih.gov/publications/Practitioner/CliniciansGuide2005/guide.pdf .
Oslin, D.W. Late-life alcoholism: Issues relevant to the geriatric psychiatrist. American Journal of Geriatric Psychiatry 12(6):571–583, 2004. PMID: 15545325
Oslin, D.W.; Slaymaker, V.J.; Blow, F.C.; et al. Treatment outcomes for alcohol dependence among middle-aged and older adults. Addictive Behaviors 30(7):1431–1436, 2005. PMID: 16022937
Pilowsky, D.J., and Wu, L.T. Screening for alcohol and drug use disorders among adults in primary care: A review. Substance Abuse and Rehabilitation 3(1):25–34, 2012. PMID: 22553426
Satre, D.D.; Chi, F.W.; Mertens, J.R.; and Weisner, C.M. Effects of age and life transitions on alcohol and drug treatment outcome over nine years. Journal of Studies on Alcohol and Drugs 73(3):459–468, 2012. PMID: 22456251
Saunders, J.B.; Aasland, O.G.; Babor, T.F.; et al. Development of the Alcohol Use Disorders Identification Test (AUDIT): WHO collaborative project on early detection of persons with harmful alcohol consumption—II. Addiction 88(6):791–804, 1993. PMID: 8329970
Schmidt, A.; Barry, K.L.; and Fleming, M.F. Detection of problem drinkers: The Alcohol Use Disorders Identification Test (AUDIT). Southern Medical Journal 88(1):52–59, 1995. PMID: 7817228
Schonfeld, L.; King-Kallimanis, B.L.; Duchene, D.M. et al. Screening and brief intervention for substance misuse among older adults: The Florida BRITE project. American Journal of Public Health 100(1):108–114, 2010. PMID: 19443821
Schonfeld, L., and Dupree, L.W. Antecedents of drinking for early- and late-onset elderly alcohol abusers. Journal of Studies of Alcohol 52(6):587–592, 1991. PMID: 1661802
Substance Abuse and Mental Health Services Administration (SAMHSA). Summary of Findings from the 2002 National Survey on Drug Use and Health . Rockville, MD: SAMHSA, Office of Applied Studies, 2002.
Substance Abuse and Mental Health Services Administration (SAMHSA). Results From the 2003 National Survey on Drug Use and Health: National Findings, in NSDUH Series H-25 . Rockville, MD: SAMHSA, Office of Applied Studies, 2004.
Substance Abuse and Mental Health Services Administration (SAMHSA). The DASIS Report: Older Adults in Substance Abuse Treatment: Update, 2007. Rockville, MD: SAMHSA, Office of Applied Studies, 2007.
Substance Abuse and Mental Health Services Administration ( SAMHSA). Results from the 2011 National Survey on Drug Use and Health: Summary of National Findings , NSDUH Series H-44, HHS Publication No. (SMA) 12-4713. Rockville, MD: SAMHSA, Center for Behavioral Health Statistics and Quality, 2012 a .
Substance Abuse and Mental Health Services Administration (SAMHSA). Older Americans Behavioral Health Issue Brief 2: Alcohol Misuse and Abuse Prevention . Rockville, MD: SAMHSA, Administration on Aging, 2012 b .
Substance Abuse and Mental Health Services Administration (SAMHSA). Results from the 2013 National Survey on Drug Use and Health: Detailed Tables . Rockville, MD: SAMHSA, 2014.
U.S. Census Bureau. 2010 Census of Population and Housing, Summary Population and Housing Characteristics, CPH-1-1 , 2013 . Washington, DC: U.S. Government Printing Office, 2013.
Whitlock, E.P.; Polen, M.R.; Green, C.A.; et al. Behavioral counseling interventions in primary care to reduce risky/harmful alcohol use by adults: A summary of the evidence for the U.S. Preventive Services Task Force. Annals of Internal Medicine 140(7):557–568, 2004. PMID: 15068985
Willenbring, M.L.; Massey, S.H.; and Gardner, M.B. Helping patients who drink too much: An evidence-based guide for primary care clinicians. American Family Physician 80(1):44–50, 2009. PMID: 19621845
Wu, L.-T., and Blazer, D.G. Illicit and nonmedical drug use among older adults: A review. Journal of Aging and Health 23(3):481–504, 2011. PMID: 21084724

An official website of the United States government
Here’s how you know
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock Locked padlock icon ) or https:// means you’ve safely connected to the .gov website. Share sensitive information only on official, secure websites.

Alcohol's Effects on Health
Research-based information on drinking and its impact.
National Institute on Alcohol Abuse and Alcoholism (NIAAA)
Find science-based information on the effects of alcohol on health., alcohol topics a to z.

Facts and Stats

Drinking Levels Defined
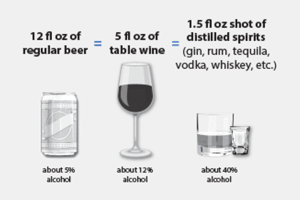
Alcohol's Effects on the Body
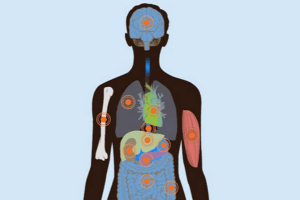
Underage And Young Adults

Getting Help

Order Publications
Short takes, translations.
niaaa.nih.gov
An official website of the National Institutes of Health and the National Institute on Alcohol Abuse and Alcoholism
- Patient Care & Health Information
- Diseases & Conditions
- Alcohol use disorder
Alcohol use disorder is a pattern of alcohol use that involves problems controlling your drinking, being preoccupied with alcohol or continuing to use alcohol even when it causes problems. This disorder also involves having to drink more to get the same effect or having withdrawal symptoms when you rapidly decrease or stop drinking. Alcohol use disorder includes a level of drinking that's sometimes called alcoholism.
Unhealthy alcohol use includes any alcohol use that puts your health or safety at risk or causes other alcohol-related problems. It also includes binge drinking — a pattern of drinking where a male has five or more drinks within two hours or a female has at least four drinks within two hours. Binge drinking causes significant health and safety risks.
If your pattern of drinking results in repeated significant distress and problems functioning in your daily life, you likely have alcohol use disorder. It can range from mild to severe. However, even a mild disorder can escalate and lead to serious problems, so early treatment is important.
Products & Services
- A Book: Mayo Clinic Family Health Book, 5th Edition
- Newsletter: Mayo Clinic Health Letter — Digital Edition
Alcohol use disorder can be mild, moderate or severe, based on the number of symptoms you experience. Signs and symptoms may include:
- Being unable to limit the amount of alcohol you drink
- Wanting to cut down on how much you drink or making unsuccessful attempts to do so
- Spending a lot of time drinking, getting alcohol or recovering from alcohol use
- Feeling a strong craving or urge to drink alcohol
- Failing to fulfill major obligations at work, school or home due to repeated alcohol use
- Continuing to drink alcohol even though you know it's causing physical, social, work or relationship problems
- Giving up or reducing social and work activities and hobbies to use alcohol
- Using alcohol in situations where it's not safe, such as when driving or swimming
- Developing a tolerance to alcohol so you need more to feel its effect or you have a reduced effect from the same amount
- Experiencing withdrawal symptoms — such as nausea, sweating and shaking — when you don't drink, or drinking to avoid these symptoms
Alcohol use disorder can include periods of being drunk (alcohol intoxication) and symptoms of withdrawal.
- Alcohol intoxication results as the amount of alcohol in your bloodstream increases. The higher the blood alcohol concentration is, the more likely you are to have bad effects. Alcohol intoxication causes behavior problems and mental changes. These may include inappropriate behavior, unstable moods, poor judgment, slurred speech, problems with attention or memory, and poor coordination. You can also have periods called "blackouts," where you don't remember events. Very high blood alcohol levels can lead to coma, permanent brain damage or even death.
- Alcohol withdrawal can occur when alcohol use has been heavy and prolonged and is then stopped or greatly reduced. It can occur within several hours to 4 to 5 days later. Signs and symptoms include sweating, rapid heartbeat, hand tremors, problems sleeping, nausea and vomiting, hallucinations, restlessness and agitation, anxiety, and occasionally seizures. Symptoms can be severe enough to impair your ability to function at work or in social situations.
What is considered 1 drink?
The National Institute on Alcohol Abuse and Alcoholism defines one standard drink as any one of these:
- 12 ounces (355 milliliters) of regular beer (about 5% alcohol)
- 8 to 9 ounces (237 to 266 milliliters) of malt liquor (about 7% alcohol)
- 5 ounces (148 milliliters) of wine (about 12% alcohol)
- 1.5 ounces (44 milliliters) of hard liquor or distilled spirits (about 40% alcohol)
When to see a doctor
If you feel that you sometimes drink too much alcohol, or your drinking is causing problems, or if your family is concerned about your drinking, talk with your health care provider. Other ways to get help include talking with a mental health professional or seeking help from a support group such as Alcoholics Anonymous or a similar type of self-help group.
Because denial is common, you may feel like you don't have a problem with drinking. You might not recognize how much you drink or how many problems in your life are related to alcohol use. Listen to relatives, friends or co-workers when they ask you to examine your drinking habits or to seek help. Consider talking with someone who has had a problem with drinking but has stopped.
If your loved one needs help
Many people with alcohol use disorder hesitate to get treatment because they don't recognize that they have a problem. An intervention from loved ones can help some people recognize and accept that they need professional help. If you're concerned about someone who drinks too much, ask a professional experienced in alcohol treatment for advice on how to approach that person.
There is a problem with information submitted for this request. Review/update the information highlighted below and resubmit the form.
From Mayo Clinic to your inbox
Sign up for free and stay up to date on research advancements, health tips, current health topics, and expertise on managing health. Click here for an email preview.
Error Email field is required
Error Include a valid email address
To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
Thank you for subscribing!
You'll soon start receiving the latest Mayo Clinic health information you requested in your inbox.
Sorry something went wrong with your subscription
Please, try again in a couple of minutes
Genetic, psychological, social and environmental factors can impact how drinking alcohol affects your body and behavior. Theories suggest that for certain people drinking has a different and stronger impact that can lead to alcohol use disorder.
Over time, drinking too much alcohol may change the normal function of the areas of your brain associated with the experience of pleasure, judgment and the ability to exercise control over your behavior. This may result in craving alcohol to try to restore good feelings or reduce negative ones.
Risk factors
Alcohol use may begin in the teens, but alcohol use disorder occurs more frequently in the 20s and 30s, though it can start at any age.
Risk factors for alcohol use disorder include:
- Steady drinking over time. Drinking too much on a regular basis for an extended period or binge drinking on a regular basis can lead to alcohol-related problems or alcohol use disorder.
- Starting at an early age. People who begin drinking — especially binge drinking — at an early age are at a higher risk of alcohol use disorder.
- Family history. The risk of alcohol use disorder is higher for people who have a parent or other close relative who has problems with alcohol. This may be influenced by genetic factors.
- Depression and other mental health problems. It's common for people with a mental health disorder such as anxiety, depression, schizophrenia or bipolar disorder to have problems with alcohol or other substances.
- History of trauma. People with a history of emotional trauma or other trauma are at increased risk of alcohol use disorder.
- Having bariatric surgery. Some research studies indicate that having bariatric surgery may increase the risk of developing alcohol use disorder or of relapsing after recovering from alcohol use disorder.
- Social and cultural factors. Having friends or a close partner who drinks regularly could increase your risk of alcohol use disorder. The glamorous way that drinking is sometimes portrayed in the media also may send the message that it's OK to drink too much. For young people, the influence of parents, peers and other role models can impact risk.
Complications
Alcohol depresses your central nervous system. In some people, the initial reaction may feel like an increase in energy. But as you continue to drink, you become drowsy and have less control over your actions.
Too much alcohol affects your speech, muscle coordination and vital centers of your brain. A heavy drinking binge may even cause a life-threatening coma or death. This is of particular concern when you're taking certain medications that also depress the brain's function.
Impact on your safety
Excessive drinking can reduce your judgment skills and lower inhibitions, leading to poor choices and dangerous situations or behaviors, including:
- Motor vehicle accidents and other types of accidental injury, such as drowning
- Relationship problems
- Poor performance at work or school
- Increased likelihood of committing violent crimes or being the victim of a crime
- Legal problems or problems with employment or finances
- Problems with other substance use
- Engaging in risky, unprotected sex, or experiencing sexual abuse or date rape
- Increased risk of attempted or completed suicide
Impact on your health
Drinking too much alcohol on a single occasion or over time can cause health problems, including:
- Liver disease. Heavy drinking can cause increased fat in the liver (hepatic steatosis) and inflammation of the liver (alcoholic hepatitis). Over time, heavy drinking can cause irreversible destruction and scarring of liver tissue (cirrhosis).
- Digestive problems. Heavy drinking can result in inflammation of the stomach lining (gastritis), as well as stomach and esophageal ulcers. It can also interfere with your body's ability to get enough B vitamins and other nutrients. Heavy drinking can damage your pancreas or lead to inflammation of the pancreas (pancreatitis).
- Heart problems. Excessive drinking can lead to high blood pressure and increases your risk of an enlarged heart, heart failure or stroke. Even a single binge can cause serious irregular heartbeats (arrhythmia) called atrial fibrillation.
- Diabetes complications. Alcohol interferes with the release of glucose from your liver and can increase the risk of low blood sugar (hypoglycemia). This is dangerous if you have diabetes and are already taking insulin or some other diabetes medications to lower your blood sugar level.
- Issues with sexual function and periods. Heavy drinking can cause men to have difficulty maintaining an erection (erectile dysfunction). In women, heavy drinking can interrupt menstrual periods.
- Eye problems. Over time, heavy drinking can cause involuntary rapid eye movement (nystagmus) as well as weakness and paralysis of your eye muscles due to a deficiency of vitamin B-1 (thiamin). A thiamin deficiency can result in other brain changes, such as irreversible dementia, if not promptly treated.
- Birth defects. Alcohol use during pregnancy may cause miscarriage. It may also cause fetal alcohol spectrum disorders (FASDs). FASDs can cause a child to be born with physical and developmental problems that last a lifetime.
- Bone damage. Alcohol may interfere with making new bone. Bone loss can lead to thinning bones (osteoporosis) and an increased risk of fractures. Alcohol can also damage bone marrow, which makes blood cells. This can cause a low platelet count, which may result in bruising and bleeding.
- Neurological complications. Excessive drinking can affect your nervous system, causing numbness and pain in your hands and feet, disordered thinking, dementia, and short-term memory loss.
- Weakened immune system. Excessive alcohol use can make it harder for your body to resist disease, increasing your risk of various illnesses, especially pneumonia.
- Increased risk of cancer. Long-term, excessive alcohol use has been linked to a higher risk of many cancers, including mouth, throat, liver, esophagus, colon and breast cancers. Even moderate drinking can increase the risk of breast cancer.
- Medication and alcohol interactions. Some medications interact with alcohol, increasing its toxic effects. Drinking while taking these medications can either increase or decrease their effectiveness, or make them dangerous.
Early intervention can prevent alcohol-related problems in teens. If you have a teenager, be alert to signs and symptoms that may indicate a problem with alcohol:
- Loss of interest in activities and hobbies and in personal appearance
- Red eyes, slurred speech, problems with coordination and memory lapses
- Difficulties or changes in relationships with friends, such as joining a new crowd
- Declining grades and problems in school
- Frequent mood changes and defensive behavior
You can help prevent teenage alcohol use:
- Set a good example with your own alcohol use.
- Talk openly with your child, spend quality time together and become actively involved in your child's life.
- Let your child know what behavior you expect — and what the consequences will be for not following the rules.
Alcohol use disorder care at Mayo Clinic
- Nguyen HT. Allscripts EPSi. Mayo Clinic. May 5, 2022.
- What is A.A.? Alcoholics Anonymous. https://www.aa.org/what-is-aa. Accessed April 1, 2022.
- Mission statement. Women for Sobriety. https://womenforsobriety.org/about/#. Accessed April 1, 2022.
- Al-Anon meetings. Al-Anon Family Groups. https://al-anon.org/al-anon-meetings/. Accessed April 1, 2022.
- Substance-related and addictive disorders. In: Diagnostic and Statistical Manual of Mental Disorders DSM-5. 5th ed. American Psychiatric Association; 2013. https://dsm.psychiatryonline.org. Accessed April 26, 2018.
- Rethinking drinking: Alcohol and your health. National Institute on Alcohol Abuse and Alcoholism. https://www.rethinkingdrinking.niaaa.nih.gov/. Accessed April 1, 2022.
- Treatment for alcohol problems: Finding and getting help. National Institute on Alcohol Abuse and Alcoholism. https://www.niaaa.nih.gov/publications/brochures-and-fact-sheets/treatment-alcohol-problems-finding-and-getting-help. Accessed April 1, 2022.
- Alcohol's effect on the body. National Institute on Alcohol Abuse and Alcoholism. https://www.niaaa.nih.gov/alcohols-effects-health/alcohols-effects-body. Accessed April 1, 2022.
- Understanding the dangers of alcohol overdose. National Institute on Alcohol Abuse and Alcoholism. https://www.niaaa.nih.gov/publications/brochures-and-fact-sheets/understanding-dangers-of-alcohol-overdose. Accessed April 1, 2022.
- Frequently asked questions: About alcohol. Centers for Disease Control and Prevention. https://www.cdc.gov/alcohol/faqs.htm. Accessed April 1, 2022.
- Harmful interactions: Mixing alcohol with medicines. National Institute on Alcohol Abuse and Alcoholism. https://www.niaaa.nih.gov/publications/brochures-and-fact-sheets/harmful-interactions-mixing-alcohol-with-medicines. Accessed April 1, 2022.
- Parenting to prevent childhood alcohol use. National Institute on Alcohol Abuse and Alcoholism. https://www.niaaa.nih.gov/publications/brochures-and-fact-sheets/parenting-prevent-childhood-alcohol-use. Accessed April 1, 2022.
- Tetrault JM, et al. Risky drinking and alcohol use disorder: Epidemiology, pathogenesis, clinical manifestations, course, assessment, and diagnosis. https://www.uptodate.com/contents/search. Accessed April 1, 2022.
- Holt SR. Alcohol use disorder: Pharmacologic management. https://www.uptodate.com/contents/search. Accessed April 1, 2022.
- Saxon AJ. Alcohol use disorder: Psychosocial treatment. https://www.uptodate.com/contents/search. Accessed April 1, 2022.
- Charness ME. Overview of the chronic neurologic complications of alcohol. https://www.uptodate.com/contents/search. Accessed April 1, 2022.
- Chen P, et al. Acupuncture for alcohol use disorder. International Journal of Physiology, Pathophysiology and Pharmacotherapy. 2018;10:60.
- Ng S-M, et al. Nurse-led body-mind-spirit based relapse prevention intervention for people with diagnosis of alcohol use disorder at a mental health care setting, India: A pilot study. Journal of Addictions Nursing. 2020; doi:10.1097/JAN.0000000000000368.
- Lardier DT, et al. Exercise as a useful intervention to reduce alcohol consumption and improve physical fitness in individuals with alcohol use disorder: A systematic review and meta-analysis. Frontiers in Psychology. 2021; doi:10.3389/fpsyg.2021.675285.
- Sliedrecht W, et al. Alcohol use disorder relapse factors: A systematic review. Psychiatry Research. 2019; doi:10.1016/j.psychres.2019.05.038.
- Thiamin deficiency. Merck Manual Professional Version. https://www.merckmanuals.com/professional/nutritional-disorders/vitamin-deficiency,-dependency,-and-toxicity/thiamin-deficiency. Accessed April 2, 2022.
- Alcohol & diabetes. American Diabetes Association. https://www.diabetes.org/healthy-living/medication-treatments/alcohol-diabetes. Accessed April 2, 2022.
- Marcus GM, et al. Acute consumption of alcohol and discrete atrial fibrillation events. Annals of Internal Medicine. 2021; doi:10.7326/M21-0228.
- Means RT. Hematologic complications of alcohol use. https://www.uptodate.com/contents/search. Accessed April 1, 2022.
- What people recovering from alcoholism need to know about osteoporosis. NIH Osteoporosis and Related Bone Diseases National Resource Center. https://www.bones.nih.gov/health-info/bone/osteoporosis/conditions-behaviors/alcoholism. Accessed April 2, 2022.
- How to tell if your child is drinking alcohol. Substance Abuse and Mental Health Services Administration. https://www.samhsa.gov/talk-they-hear-you/parent-resources/how-tell-if-your-child-drinking-alcohol. Accessed April 2, 2022.
- Smith KE, et al. Problematic alcohol use and associated characteristics following bariatric surgery. Obesity Surgery. 2018; doi:10.1007/s11695-017-3008-8.
- Fairbanks J, et al. Evidence-based pharmacotherapies for alcohol use disorder: Clinical pearls. Mayo Clinic Proceedings. 2020; doi:10.1016/j.mayocp.2020.01.030.
- U.S. Preventive Services Task Force. Screening and behavioral counseling interventions to reduce unhealthy alcohol use in adolescents and adults: U.S. Preventive Services Task Force Recommendation Statement. JAMA. 2018; doi:10.1001/jama.2018.16789.
- Hall-Flavin DK (expert opinion). Mayo Clinic. April 25, 2022.
- Celebrate Recovery. https://www.celebraterecovery.com/. Accessed April 26, 2022.
- SMART Recovery. https://www.smartrecovery.org/. Accessed April 26, 2022.
- Symptoms & causes
- Diagnosis & treatment
- Doctors & departments
- Care at Mayo Clinic
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
Make twice the impact
Your gift can go twice as far to advance cancer research and care!
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Front Psychol
Alcohol, Aggression, and Violence: From Public Health to Neuroscience
Kajol v. sontate.
1 National Forensic Sciences University, Gandhinagar, India
Mohammad Rahim Kamaluddin
2 Centre for Research in Psychology and Human Well-Being, Faculty of Social Sciences and Humanities, Universiti Kebangsaan Malaysia, Bangi, Malaysia
Isa Naina Mohamed
3 Department of Pharmacology, Faculty of Medicine, Universiti Kebangsaan Malaysia Medical Centre, Kuala Lumpur, Malaysia
Rashidi Mohamed Pakri Mohamed
4 Department of Family Medicine, Faculty of Medicine, Universiti Kebangsaan Malaysia Medical Centre, Kuala Lumpur, Malaysia
Mohd. Farooq Shaikh
5 Neuropharmacology Research Laboratory, Jeffrey Cheah School of Medicine and Health Sciences, Monash University Malaysia, Subang Jaya, Malaysia
Haziq Kamal
6 Department of Physiology, Faculty of Medicine, Universiti Kebangsaan Malaysia Medical Centre, Kuala Lumpur, Malaysia
Alcohol has been associated with violent crimes and domestic violence across many nations. Various etiological factors were linked to chronic alcohol use and violence including psychiatric comorbidities of perpetrators such as personality disorders, mood disorders, and intermittent explosive disorders. Aggression is the precursor of violence and individuals prone to aggressive behaviors are more likely to commit impulsive violent crimes, especially under the influence of alcohol. Findings from brain studies indicate long-term alcohol consumption induced morphological changes in brain regions involved in self-control, decision-making, and emotional processing. In line with this, the inherent dopaminergic and serotonergic anomalies seen in aggressive individuals increase their susceptibility to commit violent crimes when alcohol present in their system. In relation to this, this article intends to investigate the influence of alcohol on aggression with sociopsychological and neuroscientific perspectives by looking into comorbidity of personality or mood disorders, state of the mind during alcohol consumption, types of beverages, environmental trigger, neurochemical changes, and gender differences that influence individual responses to alcohol intake and susceptibility to intoxicated aggression.
Introduction
Alcohol use disorder (AUD) is one of the leading causes of the global burden of disease and injury (WHO), despite the continuous discovery of novel pharmacotherapeutic agents (Pakri Mohamed et al., 2018 ). Various factors such as environmental, social, situational, and cultural context have distinctive consequences toward substance use and its effects on individuals (Latkin et al., 2017 ). Alcohol alters the mental state of individuals, including emotional processing and rational thinking, making the users unpredictable and dangerous, especially young people (Australian Government, 2017 ) or those with pre-existing psychological or psychiatric comorbidities (Brem et al., 2018 ; Puhalla et al., 2020 ). Violence related to substance use has been widely reported and studied, particularly the potential for violent outcomes between the different substances of use (Duke et al., 2018 ). Studies from various countries have reported crimes and domestic violence owing to alcohol (Hagelstam and Häkkänen, 2006 ; Mayshak et al., 2020 ), especially during the recent state of global coronavirus disease 2019 (COVID-19) pandemic (Finlay and Gilmore, 2020 ).
Alcohol and Domestic Abuse/Violence
There is a strong evidence linking alcohol with domestic abuse or domestic violence (Gadd et al., 2019 ). A study conducted within the metropolitan area of Melbourne, Australia found that alcohol outlet density was significantly associated with domestic violence rates over time (Livingston, 2011 ). In Australia, alcohol-related domestic violence is twice more likely to involve physical violence including life-threatening injuries (Mayshak et al., 2020 ). In the UK police report audit, approximately two-thirds of domestic incidents reported to police involve “under the influence of alcohol” (Alcohol Research UK). The same study also noted more aggression if alcohol was involved and persons involved considered alcohol to have a direct effect on their behavior. International evidence reveals a similar pattern with men tend to cause worse assaults after drinking and women are more likely to suffer from abuse with living partners who are heavy drinkers (Reno et al., 2010 ; Graham et al., 2011 ). These behavioral patterns cannot be inferred from women. Studies have demonstrated that women who are heavy alcohol drinkers tend to suffer from abuse themselves and also suffer from higher aggression from their partners (Hutchison, 1999 ; Iverson et al., 2013 ). In India, those who had a heavy drinker in their lives (family, relative, neighbor, etc.) reported having been harmed by them through physical, sexual, psychological, financial, and social. In Kerala, India, a cross-sectional study involving spouses of alcohol-dependent males undergoing a deaddiction program reported a high correlation between domestic violence and years of marriage and the number of stressful events in the past year (Indu et al., 2018 ). In the USA, 40% of the reported domestic violence has the alcohol factor present during the time of the offense (Galbicsek, 2020 ). It is also found that the intensity of violence is greater when the offender is intoxicated compared to when he/she is not. Based on existing literature, alcohol consumption is more related to the severity of domestic violence rather than its occurrence (Graham et al., 2011 ) and exacerbated by an increase in consumption (Ferrari et al., 2016 ). Although there is a clear correlation between alcohol and domestic abuse, these correlations are limited to men and, therefore, form a complex relationship, hence establishing a unidirectional relationship between domestic violence and alcohol is not possible at present (De Paula Gebara et al., 2015 ). As per UN Women of the United Nations, the global prevalence of domestic violence against women was 1 in 3 prior to COVID-19 pandemic, mainly perpetrated by their intimate partners. Emerging data from a number of countries show an increase in calls to domestic violence helplines since the beginning of COVID-19 pandemic. The United Nations Secretary-General has referred to this surge in domestic violence amid COVID-19 pandemic as a “shadow pandemic” (Women UN, 2020 ). Several countries showed a shockingly increasing pattern of domestic violence cases globally, up to 50% in Brazil, 20% rise in helpline calls in Spain, 30% in Cyprus (The Guardian, 2020 ), 25% increase in helpline calls and about 150% rise in Refuge website in the UK (Bradbury-Jones and Isham, 2020 ), and almost doubled cases of domestic violence in the Hubei, China (Anju, 2019 ). COVID-19 pandemic-induced increase in global domestic violence was irrespective of the economic status of the countries (Finlay and Gilmore, 2020 ). In line with this, the alcohol sales in March 2020 were increased by 67% in the UK during lockdown (Finlay and Gilmore, 2020 ). Contrary to this, a recent systematic review revealed that there is insufficient evidence to suggest that COVID-19 pandemic has led to increased substance use and domestic violence (Abdo et al., 2020 ) ( Table 1 ).
Alcohol and domestic violence.
Alcohol, Aggression, and Violence: Psychiatric Comorbidities
There were various publications related to the etiological factors associating alcohol use and violence. Study has shown that alcohol was most commonly abused among adolescents and school children (Bland et al., 2018 ). Factors such as developmental milestones when a child is growing up can predict violence and substance abuse in adults (Hentges et al., 2018 ; Malti, 2020 ). Retrospectively, heavy drinking in later life can be predicted by early childhood aggression (Gottfried and Christopher, 2017 ). A combination of substance use and psychiatric disorders is associated with an above-average risk of adult violent behavior (Wiener et al., 2018 ). Mental disorders such as anxiety and mood disorders have also been commonly associated with AUD (Gimeno et al., 2017 ). AUD and depressive symptoms are commonly reported with other mood disorders and have greater severity and worse prognosis compared when it is concomitant with AUD (Higley and Linnoila, 2002 ). There are possibilities of the symptoms exhibited by the patients during withdrawal or acute intoxication that are pre-existing effective disorders or in a combination (Serafini et al., 2017 ). The most common symptoms of substance withdrawal include agitation. Other symptoms such as disinhibition and despair are commonly associated with substance abuse disorder that would be amplified into self-destructive acts and impulsivity (Goldstein et al., 2017 ; Duica et al., 2020 ). In addition, men with antisocial traits are at greater risk of binge alcohol consumption and commit intimate partner violence (Brem et al., 2018 ). In US, the prevalence of antisocial personality disorder and adulthood antisocial behavioral syndrome was 4.3 and 20%, respectively, and both the syndromes were significantly associated with 12-month and lifetime substance use (Goldstein et al., 2017 ). Based on a study conducted in Italy that had a population of 717 make subjects−404 alcoholics and 282 having a personality disorder, alcohol consumption was higher among those who suffer from psychiatric conditions, especially personality disorder (39%; antisocial personality disorder at the most) and 14.2% have a dual diagnosis (personality disorder and alcohol dependence). The antisocial personality population (more than any other personality disorder) had an early onset of alcohol abuse and its association with physical dependence and legal problems (Poldrugo, 1998 ). Similar studies were conducted in the prisons of North Italy, which also suggested that there is a positive correlation between AUD and personality disorders and the risk of engaging in criminal acts is higher within the individuals with dual diagnosis (alcoholics and sociopaths). Intermittent explosive disorder (IED), characterized by repeated, sudden explosive outbursts of anger or violence, has been associated with a history of childhood abuse and AUD is at a greater risk for intoxicated aggression (Puhalla et al., 2020 ) and also to develop substance use disorder compared to those without IED (Coccaro et al., 2017 ).
Alcohol, Aggression, and Crime
Aggression is the basic ingredient of acts of violence (Eisner and Malti, 2015 ). Violence as aggression has the goal of extreme harm including death. In this context, violent and criminal behavior is often associated with substance abuse (Anderson and Bushman, 2002 ). Alcohol is one of the major ingredients of violent incidents (i.e., murder) due to its disinhibiting effects along with loss of emotional control that increases the susceptibility to physical assaults and eventually murder (Karlsson, 1998 ). According to Mokdad et al. ( 2004 ) and Pinel and Barnes ( 2018 ), alcohol is involved in more than 2 million deaths (deaths due to ill health, accidents, and violence) each year across the world. A moderate dose of alcohol in the blood tends to cause cognitive, perceptual, verbal, and motor impairments as well as a loss of control, which eventually lead to unacceptable social behavior including violence (Pinel and Barnes, 2018 ). From a criminological perspective, alcohol is an important factor in violent interactions that culminate in murder (Wahlsten et al., 2007 ). Substance abuse, especially alcohol, is widely acknowledged as an important risk marker for criminal behavior and violent crimes including those with mental disorders (Brennan et al., 2000 ; Wallace et al., 2004 ; Erkiran et al., 2006 ). The strong link between alcohol use and violence is well-demonstrated (Mann et al., 2006 ), as alcohol consumption is an important factor for the prevalence of violence (Room and Rossow, 2001 ).
Alcohol facilitates conflicts with others and increases the potential for violent behavior among the drinkers and others (Wieczorek et al., 1990 ; Mann et al., 2006 ; Wahlsten et al., 2007 ). Expressive murders are most often preceded by arguments and altercations and the level of intoxication increases the viciousness of the attack (Karlsson, 1998 ). Block and Block ( 1992 ) defined expressive murders as a result of the expression, emotions, and psychological states. Emotional states such as anger, frustration, and hostility are said to lead an individual to perform expressive murders. In this context, alcohol is said to be the credible factor leading to emotional loss and instability and eventually leading to expressive-based murders. A national study of 16,698 inmates found that alcohol had a stronger role in violent offending such as homicide, physical assaults, and sexual assaults compared to offenses such as burglary and robbery. In this study, the majority of the respondents claimed to have been under the influence/intoxication of substance(s) such as alcohol during the commission of murder (Felson and Staff, 2010 ).
In 2011, 73 and 57% of the homicides recorded in the United States and Russia were alcohol related (Landberg and Norström, 2011 ), whereas, in countries including Finland, Netherlands, and Sweden, alcohol consumption led to lethal violent crimes reported from 2003 to 2006. In Finland alone, 491 persons were killed within 4 years period and ~82% of the perpetrators were intoxicated with alcohol, where 39% of them were alcoholics and 45% of the reported murders were committed with knives (Liem et al., 2013 ). In Singapore, out of 253 homicide offenders, 141 individuals (56%) were suffering from AUD and 121 offenders (48%) drank alcohol within 24 h preceding their criminal offense (Yeo et al., 2019 ). In the Brazilian city of Diadem, limiting the hours of alcoholic sales in bars to 11 p.m. significantly declined the crime rate to 9 homicides per month (Duailibi et al., 2007 ). Chervyakov et al. ( 2002 ) reported that 4 in every 5 Russians convicted of murder were intoxicated with alcohol during the murderous act. In a British prison sample, over a third of male homicide offenders had consumed alcohol and were considered drunk at the time of the offense and 14.0% had been using drugs (Dobash and Dobash, 2011 ).
Even though many findings from various countries strongly concluded that alcohol is a risk factor for murderous acts, however, most of these studies correlated level of alcohol consumption rather than the pattern of hazardous intake or types of beverages consumed, which is more likely to cause severe disinhibition, hence more damages. In line with this, using a sample of 85 countries, Weiss et al. ( 2018 ) reported no association between alcohol consumption level and homicide rates; however, they found a positive association between hazardous drinking pattern and homicide rates. Contrary to this, a cross-sectional analysis of data from 83 countries that controlled for several possible covariates reported that countries with riskier drinking patterns did not have higher homicide rates compared to countries with less risky drinking patterns. However, the same investigators also reported that the association between homicide rates and alcohol was beverage specific, with beer and spirit consumption were positively correlated with homicide rates and wine negatively correlated with the rate of homicides (Hockin et al., 2018 ) ( Table 2 ).
Alcohol and homicide rates.
Alcohol and Aggression: A Neuroscience Perspective
Alcohol accentuates or promotes the mental state of the drinkers at the time of consumption, fueling negative emotions such as aggressive behavior or positive emotional outcomes such as gregariousness and warmth. Aggression is classified as impulsive, premeditated, and medically driven (Gollan et al., 2005 ). Even cognitively intact alcohol-dependent individuals showed higher psychopathological symptoms with trait impulsivity (Kovács et al., 2020 ) and other psychiatric comorbidities such as antisocial and borderline personalities (Helle et al., 2019 ) triggering medically driven aggression. Unlike impulse-driven aggression, which is reflective of an agitated state of mind, premeditated aggression is a planned aggressive act (Martin et al., 2019 ).
The aggressive acts at some points could be goal oriented, whereas in some instances could be impulse driven. Impulsivity is defined as fast actions taken without adequate or with little thought and conscious judgment of the consequences (Bakhshani, 2014 ). Assessment of various brain regions of 1,200 men and women of 18–35 years old along with their tendency to make rapid decisions seek for novel and intense experiences and risk-taking traits revealed a significant decrease in the cortical thickness of brain regions related to self-control and decision-making processes, particularly anterior cingulate and middle frontal gyrus (Holmes et al., 2016 ). Alcohol itself directly interrupts the executive cognitive functions by disrupting the functions of the prefrontal cortex (PFC), which has been associated with disinhibition and aggression (Heinrichs, 1989 ). The PFC, which regulates aggressive and social behavior (Davidson et al., 2000 ; Seo et al., 2008 ), was shown to be reduced in its volume in individuals with antisocial personality disorder (Raine et al., 2000 ). In addition, neuroimaging of individuals with IED revealed lower white matter integrity in long-range connections between the frontal and temporoparietal regions (Lee et al., 2016 ), reduced gray matter volume in the frontolimbic structures (Coccaro et al., 2016 ), and gray matter deficit and dysfunction of the left insula (Seok and Cheong, 2020 ). The orbitomedial region within the PFC regulates anger and impulsive aggression (Lapierre et al., 1995 ; Davidson et al., 2000 ) and assigns appropriate emotion to the consequences of actions (Bechara et al., 2000 ). During aggressive behaviors, reduced activity was reported within the orbitofrontal PFC (Goyer et al., 1994 ; Pietrini et al., 2000 ), where the impaired PFC is unable to inhibit the subcortical structures such as the amygdala, hippocampus, and nucleus accumbens from activating emotional output (Raine et al., 1998 ; Davidson et al., 2000 ). In line with this, an increase in amygdala limbic connectivity and a significant decrease in amygdala-medial PFC connectivity were reported among violent offenders (Siep et al., 2019 ). Hyperactivation of the amygdala is also reported in individuals with IED in response to angry faces compared to controls (McCloskey et al., 2016 ). Moreover, alcohol-dependent patients with a history of aggressive behavior also recorded elevated glutamate/creatine ratio in the bilateral amygdala (Liu et al., 2020 ) corroborating various other behavioral changes associated with glutamatergic hyperexcitability state in the amygdala reported in past studies (Kumar et al., 2013 , 2016 , 2018 ; Pakri Mohamed et al., 2018 ; Kamal et al., 2020 ).
Serotonin in AUD and Aggression
Aggression is a complex behavior involving interactions between the gene, environment, personality, and physiology (Armstrong et al., 2017 ; Zhang et al., 2017 ; Kanen et al., 2021 ). Dysregulation of serotonin is associated with many psychiatric disorders (Rappek et al., 2018 ; Conio et al., 2020 ; Fanning et al., 2020 ) due to the widespread distribution of serotonergic fibers originating from midbrain raphe nuclei to various other regions (Sharp and Barnes, 2020 ). Based on a systematic review, the association between serotonin and aggression is rather mixed, where reduced 5-hydroxytryptamine (5-HT) concentration in central nervous system (CNS) was associated with reactive aggression (impulsivity; response to provocation), whereas increased 5-HT (small number of findings) may be related to callous-unemotional traits, which is another possible pathway to aggressive behavior (Runions et al., 2019 ). In line with this, SLC6A4 * HTTLPR or 5-HTTLPR (serotonin transporter) was associated with aggression within the population of Pakistan (Qadeer et al., 2021 ), China (Zhang et al., 2017 ), and the United States of America (Armstrong et al., 2017 ), whereas, in a study conducted among Russian inmates, such correlation was not found (Toshchakova et al., 2017 ). Furthermore, other genes of serotonin such as 5-hydroxytryptamine receptor 2A (5HTR2A), 5-hydroxytryptamine receptor 2B (5HTR2B), and 5-hydroxytryptamine receptor 2C (5HTR2C) also showed no association with aggressive behavior (Toshchakova et al., 2017 ; Qadeer et al., 2021 ), suggesting a stronger link between brain serotonin level and aggression rather than the receptors, which was also proven by studies using selective serotonin reuptake inhibitors (SSRIs) (Nord et al., 2013 ; Lagerberg et al., 2020 ). Likewise, a lower cerebrospinal level of 5-hydroxyindoleacetic acid (5-HIAA), the main metabolite of serotonin, was reported in the impulsive offenders than the premeditated murderers (Linnoila et al., 1983 ). Regions such as the cingulate cortex, ventromedial, and the orbitofrontal PFC were shown to have reduced serotonergic activity during impulsive aggression (Siever et al., 1999 ). Similar findings also reproduced in non-human animal models (Harrison et al., 1997 ; Kästner et al., 2019 ; Gorlova et al., 2020 ).
Some researchers have reported high serotonin transporter (SERT) bindings in the brains of deceased alcoholics (Underwood et al., 2018 ), whereas others have reported low binding (Mantere et al., 2002 ) and some reported no differences (Brown et al., 2007 ; Martinez et al., 2009 ). Similarly, mixed findings were also reported for 5-HT1A and 5-HT2A receptor bindings (Underwood et al., 2008 , 2018 ; Storvik et al., 2009 ). Chronic alcohol intake increases the metabolites of serotonin in the raphe nuclei area, however reduces 5-HT2A protein levels in the mice cortex, indicating reduced serotonergic activity (Popova et al., 2020 ). Acute alcohol intake reduces tryptophan availability to the brain (non-aggressive), which leads to a decrease in serotonin synthesis and turnover, about 25% of the concentration of tryptophan following an oral intake of alcohol (Badawy et al., 1995 ). Hence, it is probable that in the aggressive brain, the drop in brain serotonin synthesis might even be greater (40–60%) during moderate intake of alcohol (Badawy, 2003 ). However, the inconsistent findings of serotonin markers in brain imaging studies of alcoholics suggest that comorbidity of AUD with other psychiatric disorders may complicate the serotonin hypothesis in real life. In addition, even individual differences in personality traits determine the types of emotion affected by the depletion of serotonin (Kanen et al., 2021 ).
Dopamine in AUD And Aggression
Serotonin and dopamine levels are significant predictors of aggression and suicide risk (Prepelita et al., 2019 ). A systematic review of pre-clinical findings suggests that adolescence chronic stress may lead to a hyperdopaminergic state of the PFC, which eventually blunts the adulthood prefrontal dopaminergic neurotransmission, increasing the vulnerability to maladaptive aggression in adulthood (Tielbeek et al., 2018 ). In relation to this, polymorphisms of catecholamine-converting enzymes such as monoamine oxidase and catechol-o-methyltransferase along with traumatic childhood significantly increase appetitive and Facilitative Aggression Scale (Fritz et al., 2021 ). Furthermore, a study conducted on convicted Pakistani murderers revealed a high prevalence of the 9R allele of DAT-1VNTR, which influences the intrasynaptic dopamine levels (Qadeer et al., 2017 ). Pharmacological modulation of dopamine D2 receptor via its antagonist, sulpiride, impaired the ability to discern angry facial expressions in humans (Lawrence et al., 2002 ). However, some researchers have reported the opposite, where polymorphism in DRD2 genotypes causes reduced dopamine functioning that is directly associated with increased aggression (Zai et al., 2012 ) which may occur through sensation seeking (Chester et al., 2016 ). Nevertheless, it was hypothesized that impaired serotonin neuromodulatory effects may lead to dopamine hyperactivity in subcortical structures and aggressive behaviors (Seo et al., 2008 ). Studies investigating the interaction between genetic polymorphism of dopamine system (dopamine receptors; DRD2, DRD4, transporter; DAT1), and environmental factors (financial stressor and adolescent social experiences) on intimate partner violence revealed a strong influence of negative environmental changes on increased odds of violence perpetration regardless of the alleles (Schwab-Reese et al., 2020 ).
In addition to aggression, alcohol alone modulates dopaminergic neurotransmission, where even the cues of alcohol could increase the dopamine release in the nucleus accumbens (Melendez et al., 2002 ). Dysregulation of dopaminergic neurotransmission in AUD has been demonstrated in several brain imaging studies (Leurquin-Sterk et al., 2018 ; Chukwueke et al., 2021 ). Factors such as personality traits and comorbidities with other psychiatric disorders along with environmental stressors influence how one could engage in violent behaviors. Hence, even though alcohol might be the precursor to violence for some, it certainly takes more than the beverage to increase the likelihood of someone shooting from the hip.
Alcohol, Aggression, and Violence: A Conundrum
Individual reports from multiple countries have associated alcohol with violent crimes and domestic abuse. Consumption of alcoholic beverages with higher alcohol content at a dose of 0.75 g/kg and higher was correlated with increased aggression (Hockin et al., 2018 ; Kuypers et al., 2020 ), whereas a comprehensive review found no association between homicide rates and alcohol consumption level (Weiss et al., 2018 ). Even countries with a riskier drinking pattern did not show a higher crime rate compared to countries with less risky drinking patterns (Hockin et al., 2018 ). This led us to the question, does alcohol alone is sufficient to trigger violent or aggressive behavior? Based on the pieces of literature gathered in this article and past findings, it is evident that several individual and environmental factors determine the likelihood of an intoxicated person engaging in an aggressive or violent act. Emotional dysregulation and impulsivity in combination with pre-existing psychiatric comorbidities such as personality disorders, intermittent explosive disorder along with genetic pre-disposition and environmental stressors, such as the most commonly associated childhood adversity, are one of the triggers of intoxicated aggression. Genetic polymorphism findings indicate that environmental stressors play a more significant role in perpetration violence compared to high-risk genotypes (Schwab-Reese et al., 2020 ). However, some have reported that epigenetic mechanisms mediate the interaction between genetic and environmental factors by altering genes of many systems including the nervous, immune, and neuroendocrine (Chistiakov and Chekhonin, 2017 ).
Stress during early life, also known as childhood adversity or childhood maltreatment, is associated with the development of personality disorders (Lemgruber and Juruena, 2013 ; Porter et al., 2020 ), affective disorders (Hoppen and Chalder, 2018 ), and alcohol use disorder (Evans et al., 2017 ). Among these, physical, emotional abuse, and maternal rejection are associated with the shaping of personality (Schouw et al., 2020 ) and maladaptive schemes in adulthood (Pilkington et al., 2021 ). For an instance, physical abuse and neglect lead to antisocial traits (Schorr et al., 2020 ). Factors such as family dysfunction, as violence in the family, show a strong correlation with adulthood aggression (Khodabandeh et al., 2018 ; Labella and Masten, 2018 ) through emotion-related impulsivity and behavioral response inhibition (Madole et al., 2020 ). In line with this, it has been reported that a high level of childhood adversity increases one's likelihood to substance use through reduced functioning of the anterior cingulate cortex in inhibitory control, indicating a higher impulsive response (Fava et al., 2019 ). The very nature of adversity (threat vs. deprivation) has a distinctive effect on emotional circuits. For an instance, childhood threat was reported to reduce the volume of the medial PFC, amygdala, and hippocampus along with increased activation of the amygdala in response to a threat, whereas childhood deprivation alters the function and volume of the frontoparietal regions, which are associated with goal oriented and executive functions (McLaughlin et al., 2019 ). In addition to the type of adversities, individual differences in threat and executive control-related brain regions also determine how one with childhood adversity would express adult trait anger. Individuals with the low amygdala and high dorsolateral PFC activity do not express high trait anger, despite having experienced stress in early life (Kim et al., 2018 ). Suppression of adult trait anger was owing to the higher microstructural integrity of white matter pathways, including the uncinate fasciculus, which anatomically links the PFC and amygdala in the regulation of negative emotion (Kim et al., 2019 ). However, the findings by Kim et al. ( 2019 ) were based on subjects free of borderline and personality disorders, which are the most commonly associated psychiatric comorbidities with intoxicated aggression and also known to have reduced white matter integrity in regions associated with risky behavior and impulsivity (Jiang et al., 2017 ; Ninomiya et al., 2018 ). Hence, more longitudinal studies are needed in the future to understand the effects of early life stress on the development of aggression-related psychiatric comorbidities from neurological perspectives. Furthermore, the role of white matter integrity in one's expression of anger despite the chronic stress in early life should be further explored to understand the cause behind such discrepancy and the consistent neurological changes noticed in conjunction with high-risk behaviors could be investigated as potential biomarkers to predict one's risk factor along with social experiences ( Figure 1 ).

Childhood adversity affects the shaping of personality, which eventually leads to development of personality disorder, alcohol use disorder, substance use disorder, intermittent explosive disorder (IED), and aggressive behaviors such as domestic abuse or expressive murders in adulthood. Factors such as genetics and environment also interact with alcohol intake and causing neuroplasticity in brain regions associated with emotional and cognitive regulation. Childhood stress such as deprivation alters the function and reduces the volume of frontoparietal regions that associated with goal-oriented and executive functions. Childhood adversity including threat reduces the volume of the medial prefrontal cortex (MPFC), amygdala (AMG), and hippocampus (HPC). Chronic early life stress also blunts the dopaminergic activity in the PFC. Alcohol disrupts the serotonergic activity in the PFC. Altered functions of the orbitofrontal cortex (OFC) unable to inhibit the increased emotional output from subcortical structures such as the hyperactivation of AMG in IED. Reduced connectivity between MPFC and AMG was reported in violent offenders. Adults having experienced childhood adversity and do not express high adult trait anger were due to higher white matter integrity in pathways connecting the PFC and AMG.
Gender Differences in Binge Drinking, Alcohol-Induced Aggression, and Violence
It was initially reported that women are less likely to engage in binge drinking patterns than men (Bobrova et al., 2010 ). However, in the recent years, data from the United States indicate that the binge-drinking rate in adult women (age 21–49 years) has been rising (Hasin et al., 2019 ; Sarah and Keyes, 2020 ). Evidence suggests that there is a little convergence in the pattern of binge drinking in men and women. It was found that the prevalence was higher for females than males from 2000 to 2010 for any binge drinking in the preceding month. On the contrary, the reason for the convergence of frequency in the male and female binge drinking habits is estimated to occur due to the large decline in the binge drinking frequency within men than the women. Furthermore, evidence also shows that the convergence of men and women has usually been stronger in the age group of young adults in comparison to any other age group (Wilsnack et al., 2018 ). Data from 2006 to 2018 indicate that both the men and women increasingly binge drink; in women, the largest increase was found in the age group 30–44 years without children (Sarah and Keyes, 2019 ).
Several studies have investigated the risk factors pertaining to intimate partner violence (IPV)/domestic violence (DV) and found that gender-specific differences exist in DV. The likelihood of females being victimized is greater than the male victimization, whereas evidence for the males being the perpetrators is higher than that of the females. The risk factors that are found to be common in both the men and women reporting perpetration involved being exposed to parental violence and physical abuse during childhood and alcohol abuse. Risk factors that are thought to be associated with male perpetration include unemployment, lower income, cohabitation, mood disorders, and no or lower level of education (Gass et al., 2011 ; Lee et al., 2014 ). Lack of education is thought to play a role in both the perpetration and victimization of women (Capaldi et al., 2012 ). Moreover, factors such as pregnancy, young age, higher income than the partner, and previous relationships increase the risk of victimization for women (Capaldi et al., 2012 ).
Prior reports have established alcohol-induced aggression among males (Lipsey et al., 1997 ), which appears to vary across the ethnic groups and geographical regions (Caetano et al., 2001 ). Systematic comparison between males and females in relation to alcohol-induced aggression revealed greater effects of alcohol on males than females (Ito et al., 1996 ; Bushman, 2002 ); however, the analysis was limited by insufficient power to detect significant effects due to limited female data. In agreement with this, a separate study reported a small-to-moderate effect size for the association between alcohol use and male-to-female partner violence, whereas a small effect size for the association between alcohol intake and female-to-male partner violence (Foran and O'Leary, 2008 ). More recently, a significant, small effect size was reported for the association between alcohol intake and aggression in female subjects who consumed alcohol compared to those who did not drink, in response to a subsequent aggression paradigm (Crane et al., 2017 ).
Males are more likely to express aggression in a physical and/or direct form, whereas females are more likely to express it in an indirect form. It has also been reported that both the males and females are equally aggressive when verbal aggression is at play (Archer, 2004 ; Björkqvist, 2017 ). In an experiment conducted by Giancola and Zeichner ( 1995 ), 128 participants (64 males and 64 females) performed a task where they gave an electric shock to the fictional opponents, which included both the genders. The participants were assigned to either alcohol, a placebo, or a sober group. The researchers found that the intensity and duration of shock were higher in the men from the alcohol group, while only shock duration was increased in women. They also noted that men were highly aggressive toward the same gender, while women were aggressive regardless of gender. This indicated that alcohol-induced aggression affects both the genders in different ways, suggesting that men are likely to respond in a direct and indirect manner, whereas women exhibit aggression in an indirect manner. A slightly different finding to the previous study was seen in an investigation conducted by Hoaken and Pihl ( 2000 ). The researchers assigned the participants (54 males and 60 females) to compete in a competitive aggression paradigm in an intoxicated or sober state. The result was that the intoxicated men were more aggressive than the sober men; however, in the circumstances where the women were highly provoked, both the intoxicated and sober women displayed higher levels of aggression, which could resemble the men. This suggested that both the women and men can be equally aggressive and alcohol does not seem to play a prominent role in the gender biases in aggression.
Several brain imaging studies have examined the neurological changes in men and women during aggression either by including an equal number (almost) of male and female subjects or a single gender (against a control group) (Chester and DeWall, 2016 ; Emmerling et al., 2016 ; Denson et al., 2018 ). To date, very few studies have tested the gender difference hypothesis using both the male and female subjects. Generally, men have recorded higher activation of the amygdala (McRae et al., 2008 ) and the PFCs (Rahko et al., 2010 ) during emotional reactions. Investigation of sex differences in neural correlates of aggression using 22 male and 20 female subjects revealed differential brain activation patterns between both the genders in response to provocation. Aggressive men recorded higher activation of the left amygdala than aggressive women and a positive correlation with orbitofrontal cortex (OFC), rectal gyrus, and ACC activity, which was negatively correlated in women. The findings indicate that aggressive men are more inclined to automatic emotion regulation (attributed to OFC and rectal gyrus) in response to provocation compared to aggressive women (Repple et al., 2018 ). In a separate study involving 24 men and 11 women, alcohol alone had no effect on the amygdala and ventral striatum; however, their activities were positively correlated with aggression in response to provocation. Alcohol decreased their bold responses in the right PFC, thalamus, hippocampus, caudate, and putamen. Neither gender had any significant impact on the results (Gan et al., 2015 ). Contrary to this, a single administration of 0.5 per thousand alcohol was shown to reduce frontal interhemispheric connectivity in female participants, but not in male participants (Hoppenbrouwers et al., 2010 ). Intergender neurological and behavioral responses to alcohol are also influenced by ethanol metabolism (Arthur et al., 1984 ) and influences of hormones such as testosterone, cortisol, estradiol, progesterone, and oxytocin (Denson et al., 2018 ).
Alcohol intoxication-induced aggression is an interplay between gender, genetic, psychiatric comorbidities, blood alcohol level, and environmental factors. Risk factors associated with intoxicated aggression or aggression should be packaged into a scientific explanation to educate the public. Alcohol is a weak drug, which needs to be consumed in large amounts in order to cause intoxication. Hence, high-risk individuals should practice moderate drinking. Parental roles in shaping the personalities of children should be incorporated into the marriage course as one of the preventive measures. Future studies and policymakers should include more behavioral interventions in the high-risk adolescent groups.
Author Contributions
KS and JK contributed to the conceptual framework, design, and drafted the manuscript. MR, IN, RM, and MS searched references and critically revised the manuscript. HK prepared the figure and legend. All the authors critically reviewed content and approved the final version for publication of manuscript.
This study was funded by the Ministry of Higher Education Malaysia, FRGS/1/2020/SKK0/UKM/02/3.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
The authors would like to thank the Ministry of Higher Education, Malaysia, and Faculty of Medicine, UKM.
- Abdo C., Miranda E. P., Santos C. S., de Bessa Júnior J., Bernardo W. M. (2020). Domestic violence and substance abuse during COVID19: a systematic review . Indian J. Psychiatry 62 :S337. 10.4103/psychiatry.IndianJPsychiatry_1049_20 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Adjah E. O., Agbemafle I. (2016). Determinants of domestic violence against women in Ghana . BMC Public Health 16 :368. 10.1186/s12889-016-3041-x [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Ali A. A., Yassin K., Omer R. (2014). Domestic violence against women in Eastern Sudan . BMC Public Health 14 :1136. 10.1186/1471-2458-14-1136 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Anderson C. A., Bushman B. J. (2002). Human aggression . Ann. Rev. Psychol. 53 , 27–51. 10.1146/annurev.psych.53.100901.135231 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Anju S. R.. (2019). A true experimental study to evaluate the effectiveness of structured teaching programme on knowledge regarding III–effects of alcohol consumption among adolescents in selected senior secondary school at panipat haryana . Amarjeet Kaur Sandhu 11 :424. 10.5958/0974-9357.2019.00081.3 [ CrossRef ] [ Google Scholar ]
- Archer J.. (2004). Sex differences in aggression in real-world settings: a meta-analytic review . Rev Gen Psychol . 8 :291. 10.1037/1089-2680.8.4.291 [ CrossRef ] [ Google Scholar ]
- Armstrong T. A., Boisvert D., Flores S., Symonds M., Gangitano D. (2017). Heart rate, serotonin transporter linked polymorphic region (5-HTTLPR) genotype, and violence in an incarcerated sample . J. Crim. Just. 51 , 1–8. 10.1016/j.jcrimjus.2017.05.012 [ CrossRef ] [ Google Scholar ]
- Arthur M. J. P., Lee A., Wright R. (1984). Sex differences in the metabolism of ethanol and acetaldehyde in normal subjects . Clin. Sci. 67 , 397–401. 10.1042/cs0670397 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Australian Government (2017). What are drugs? Department of Health . Available online at: https://www.health.gov.au/health-topics/drugs/about-drugs/what-are-drugs
- Badawy A. A. B.. (2003). Alcohol and violence and the possible role of serotonin . Crim. Behav. Mental Health 13 , 31–44. 10.1002/cbm.529 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Badawy A. B., Morgan C. J., Lovett J. W. T., Bradley D. M., Thomas R. (1995). Decrease in circulating tryptophan availability to the brain after acute ethanol consumption by normal volunteers: implications for alcohol-induced aggressive behaviour and depression . Pharmacopsychiatry 28 , 93–97. 10.1055/s-2007-979626 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Bakhshani N. M.. (2014). Impulsivity: a predisposition toward risky behaviors . Int. J. High Risk Behav. Addic. 3 :20428. 10.5812/ijhrba.20428 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Bechara A., Damasio H., Damasio A. R. (2000). Emotion, decision making and the orbitofrontal cortex . Cerebral Cortex 10 , 295–307. 10.1093/cercor/10.3.295 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Begum S., Donta B., Nair S., Prakasam C. P. (2015). Socio-demographic factors associated with domestic violence in urban slums, Mumbai, Maharashtra, India . Indian J. Med. Res. 141 , 783–788. 10.4103/0971-5916.160701 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Björkqvist K.. (2017). Gender differences in aggression . Curr. Opin. Psychol . 19 , 39–42. 10.1016/j.copsyc.2017.03.030 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Bland V. J., Lambie I., Best C. (2018). Does childhood neglect contribute to violent behavior in adulthood? A review of possible links . Clin. Psychol. Rev. 60 , 126–135. 10.1016/j.cpr.2018.02.001 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Block R., Block C. (1992). Homicide syndromes and vulnerability: violence in Chicago's community areas over 25 years . Stud. Crime Crime Prevent. 1 , 61–87. [ Google Scholar ]
- Bobrova N., West R., Malyutina D., Malyutina S., Bobak M. (2010). Gender differences in drinking practices in middle aged and older russians . Alcohol Alcohol. (Oxford, Oxfordshire) 45 , 573–580. 10.1093/alcalc/agq069 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Bradbury-Jones C., Isham L. (2020). The pandemic paradox: the consequences of COVID-19 on domestic violence . J. Clin. Nurs . 29 , 2047–2049. 10.1111/jocn.15296 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Branas C. C., Han S., Wiebe D. J. (2016). Alcohol use and firearm violence . Epidemiol. Rev. 38 , 32–45. 10.1093/epirev/mxv010 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Brem M. J., Florimbio A. R., Elmquist J., Shorey R. C., Stuart G. L. (2018). Antisocial traits, distress tolerance, and alcohol problems as predictors of intimate partner violence in men arrested for domestic violence . Psychol. Viol. 8 :132. 10.1037/vio0000088 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Brennan P., Mednick S. A., Hodgins S. (2000). Major mental disorders and criminal violence in a Danish birth cohort . Arch. Gen. Psychiatry 57 , 494–500. 10.1001/archpsyc.57.5.494 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Brown A. K., George D. T., Fujita M., Liow J. S., Ichise M., Hibbeln J., et al.. (2007). PET [11C] DASB imaging of serotonin transporters in patients with alcoholism . Alcohol. Clin. Exp. Res . 31 , 28–32. 10.1111/j.1530-0277.2006.00261.x [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Bushman B. J.. (2002). Effects of alcohol on human aggression . Recent Dev. Alcohol . 13 , 227–243. 10.1007/0-306-47141-8_13 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Bye E. K.. (2008). Alcohol and homicide in eastern europe: a time series analysis of six countries . Homicide Stud. 12/ 1 , 7–27. 10.1177/1088767907310851 [ CrossRef ] [ Google Scholar ]
- Caetano R., John S., Cunradi C. B. (2001). Alcohol-related intimate partner violence among white, black, and Hispanic couples in the United States . Alcohol Res Health 25 :158. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Capaldi D. M., Knoble N. B., Shortt J. W., Kim H. K. (2012). A systematic review of risk factors for intimate partner violence . Partner Abuse 3 , 231–280. 10.1891/1946-6560.3.2.231 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Chervyakov V. V., Shkdnikov V. M., Pridemore W. A., McKee M. (2002). The changing nature of murder in Russia . Soc. Sci. Med. 55 :17131724. 10.1016/S0277-9536(01)00299-4 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Chester D. S., DeWall C. N. (2016). Sound the alarm: the effect of narcissism on retaliatory aggression is moderated by dACC reactivity to rejection . J. Pers . 84 , 361–368. 10.1111/jopy.12164 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Chester D. S., DeWall C. N., Derefinko K. J., Estus S., Lynam D. R., Peters J. R., Jiang Y. (2016). Looking for reward in all the wrong places: dopamine receptor gene polymorphisms indirectly affect aggression through sensation-seeking . Soc. Neurosci. 11 , 487–494. 10.1080/17470919.2015.1119191 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Chistiakov D. A., Chekhonin V. P. (2017). Early-life adversity-induced long-term epigenetic programming associated with early onset of chronic physical aggression: studies in humans and animals . World J. Biol. Psychiatry . 20 , 258–277. 10.1080/15622975.2017.1322714 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Chukwueke C. C., Nona C. N., McPhee M. D., Mansouri E., Rubin-Kahana D. S., Martinez D., et al.. (2021). Exploring regulation and function of dopamine D3 receptors in alcohol use disorder. A PET [11C]-(+)-PHNO study . Neuropsychopharmacology 46 , 2112–2120. 10.1038/s41386-021-01095-2 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Coccaro E. F., Fanning J. R., Lee R. (2017). Intermittent explosive disorder and substance use disorder: analysis of the national comorbidity survey replication sample . J. Clin. Psychiatry 78 , 697–702. 10.4088/JCP.15m10306 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Coccaro E. F., Fitzgerald D. A., Lee R., McCloskey M., Phan K. L. (2016). Frontolimbic morphometric abnormalities in intermittent explosive disorder and aggression . Biol. Psychiatry Cogn. Neurosci. Neuroimag. 1 , 32–38. 10.1016/j.bpsc.2015.09.006 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Conio B., Martino M., Magioncalda P., Escelsior A., Inglese M., Amore M., Northoff G. (2020). Opposite effects of dopamine and serotonin on resting-state networks: review and implications for psychiatric disorders . Mol. Psychiatry 25 , 82–93. 10.1038/s41380-019-0406-4 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Crane C. A., MacKenzie L., Schlauch R. C., Testa M., Easton C. J. (2017). The proximal effects of acute alcohol use on female aggression: a meta-analytic review of the experimental literature . Psychol. Addict. Behav. 31 :21. 10.1037/adb0000244 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Curtis A., Vandenberg B., Mayshak R., Coomber K., Hyder S., Walker A., et al.. (2019). Alcohol use in family, domestic and other violence: findings from a cross-sectional survey of the Australian population . Drug Alcohol Rev . 38 , 349–358. 10.1111/dar.12925 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Davidson R. J., Putnam K. M., Larson C. L. (2000). Dysfunction in the neural circuitry of emotion regulation – a possible prelude to violence . Science 289 , 591–594. 10.1126/science.289.5479.591 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- De Paula Gebara C. F., Ferri C. P., Lourenço L. M., de Toledo Vieira M., de Castro Bhona F. M., Noto A. R. (2015). Patterns of domestic violence and alcohol consumption among women and the effectiveness of a brief intervention in a household setting: a protocol study . BMC Womens Health 15 , 1–8. 10.1186/s12905-015-0236-8 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Denson T. F., O'Dean S. M., Blake K. T., Beames J. R. (2018). Aggression in women: behavior, brain and hormones . Front. Behav. Neurosci. 12 :81. 10.3389/fnbeh.2018.00081 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Devries K. M., Child J. C., Bacchus L. J., Mak J., Falder G., Graham K., et al.. (2014). Intimate partner violence victimization and alcohol consumption in women: a systematic review and meta-analysis . Addiction (Abingdon, England) 109 , 379–391. 10.1111/add.12393 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Dobash R. E., Dobash R. P. (2011). What were they thinking? Men who murder an intimate partner . Viol. Against Women 17 , 111–134. 10.1177/1077801210391219 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Drake S.. (2010). The toxicology of homicide offenders and victims: a review . Drug Alcohol Rev. 29 , 202–215 10.1111/j.1465-3362.2009.00099.x [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Duailibi S., Ponicki W., Grube J., Pinsky I., Laranjeira R., Raw M. (2007). The effect of restricting opening hours on alcohol-related violence . Am. J. Public Health. 97 , 2276–2280. 10.2105/AJPH.2006.092684 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Duica L., Dragulescu V., Pîrlog M. (2020). Neurobiological elements of hopelessness and impulsivity in suicidal behavior . Int. J. Med. Rev. Case Rep. 4 , 1–4. 10.5455/IJMRCR.suicidal-behaviour-neuro [ CrossRef ] [ Google Scholar ]
- Duke A. A., Smith K. M., Oberleitner L., Westphal A., McKee S. A. (2018). Alcohol, drugs, and violence: a meta-meta-analysis . Psychol. Viol. 8 :238. 10.1037/vio0000106 [ CrossRef ] [ Google Scholar ]
- Eisner M. P., Malti T. (2015). Aggressive and violent behavior . Handbook Child Psychol. Dev. Sci . 794–841. 10.1002/9781118963418.childpsy319 [ CrossRef ] [ Google Scholar ]
- Emmerling F., Schuhmann T., Lobbestael J., Arntz A., Brugman S., Sack A. T. (2016). The role of the insular cortex in retaliation . PLoS ONE 11 :e0152000. 10.1371/journal.pone.0152000 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Eriksson L., Bryant S., McPhedran S., Mazerolle P., Wortley R. (2020). Alcohol and drug problems among Australian homicide offenders . Addiction . 116 , 618–631. 10.1111/add.15169 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Erkiran M., Özünalan H., Evren C., Aytaçlar S., Kirisci L., Tarter R. (2006). Substance abuse amplifies the risk for violence in schizophrenia spectrum disorder . Addict. Behav. 31 , 1797–1805. 10.1016/j.addbeh.2005.12.024 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Evans E. A., Grella C. E., Upchurch D. M. (2017). Gender differences in the effects of childhood adversity on alcohol, drug, and polysubstance-related disorders . Soc. Psychiatry Psychiatr. Epidemiol. 52 , 901–912. 10.1007/s00127-017-1355-3 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Fanning J. R., Lee R., Coccaro E. F. (2020). Chapter 10: Neurotransmitter function in impulsive aggression and intermittent explosive disorder, in The Wiley International Handbook on Psychopathic Disorders and the Law, 2nd Edn . p. 249–269. 10.1002/9781119159322.ch10 [ CrossRef ] [ Google Scholar ]
- Fava N. M., Trucco E. M., Martz M. E., Cope L. M., Jester J. M., Zucker R. A., et al.. (2019). Childhood adversity, externalizing behavior, and substance use in adolescence: Mediating effects of anterior cingulate cortex activation during inhibitory errors . Dev. Psychopathol. 31 , 1439–1450. 10.1017/S0954579418001025 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Felson R. B., Staff J. (2010). The effects of alcohol intoxication on violent versus other offending . Crim. Just. Behav. 37 :13431360. 10.1177/0093854810382003 [ CrossRef ] [ Google Scholar ]
- Ferrari G., Agnew-Davies R., Bailey J., Howard L., Howarth E., Peters T. J., et al.. (2016). Domestic violence and mental health: a cross-sectional survey of women seeking help from domestic violence support services . Global Health Act. 9 :29890. 10.3402/gha.v9.29890 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Finlay I., Gilmore I. (2020). Covid-19 and alcohol—a dangerous cocktail . BMJ 369 :m1987 10.1136/bmj.m1987 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Foran H. M., O'Leary K. D. (2008). Alcohol and intimate partner violence: a meta-analytic review . Clin. Psychol. Rev. 28 , 1222–1234. 10.1016/j.cpr.2008.05.001 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Forsman J., Sturup J., Masterman T. (2018). Pre-offense alcohol intake in homicide offenders and victims: a forensic-toxicological case-control study . J. Foren. Legal Med . 56 , 55–58. 10.1016/j.jflm.2018.03.004 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Fritz M., Rösel F., Dobler H., Streb J., Dudeck M. (2021). Childhood trauma, the combination of MAO-A and COMT genetic polymorphisms and the joy of being aggressive in forensic psychiatric patients . Brain Sci. 11 :1008. 10.3390/brainsci11081008 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Gadd D., Henderson J., Radcliffe P., Stephens-Lewis D., Johnson A., Gilchrist G. (2019). The dynamics of domestic abuse and drug and alcohol dependency . Br. J. Criminol. 59 , 1035–1053. 10.1093/bjc/azz011 [ CrossRef ] [ Google Scholar ]
- Galbicsek C. (2020). Alcohol-Related Crimes . Available online at: https://www.alcoholrehabguide.org/alcohol/crimes/ (accessed October 15, 2021).
- Gan G., Sterzer P., Marxen M., Zimmermann U. S., Smolka M. N. (2015). Neural and behavioral correlates of alcohol-induced aggression under provocation . Neuropsychopharmacology 40 , 2886–2896. 10.1038/npp.2015.141 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Gass J. D., Stein D. J., Williams D. R., Seedat S. (2011). Gender differences in risk for intimate partner violence among South African adults . J. Interpers. Violence 26 , 2764–2789. 10.1177/0886260510390960 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Giancola P. R., Zeichner A. (1995). An investigation of gender differences in alcohol-related aggression . J. Stud Alcohol 56 , 573–579. 10.15288/jsa.1995.56.573 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Gimeno C., Dorado M. L., Roncero C., Szerman N., Vega P., Balanzá-Martínez V., et al.. (2017). Treatment of comorbid alcohol dependence and anxiety disorder: review of the scientific evidence and recommendations for treatment . Front. Psychiatry 8 :173. 10.3389/fpsyt.2017.00173 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Goldstein R. B., Chou S. P., Saha T. D., Smith S. M., Jung J., Zhang H., et al.. (2017). The epidemiology of antisocial behavioral syndromes in adulthood: results from the national epidemiologic survey on alcohol and related conditions-III . J. Clin. Psychiatry 78 , 90–98. 10.4088/JCP.15m10358 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Gollan J. K., Lee R., Coccaro E. F. (2005). Developmental psychopathology and neurobiology of aggression . Dev. Psychopathol. 17 , 1151–1171. 10.1017/S0954579405050546 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Gonçalves R. E. M., Ponce J. C., Leyton V. (2020). Alcohol consumption and violent deaths in the city of São Paulo in 2015 . Subst. Use Misuse . 55 , 1875–1880. 10.1080/10826084.2020.1771596 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Gorlova A., Ortega G., Waider J., Bazhenova N., Veniaminova E., Proshin A., et al.. (2020). Stress-induced aggression in heterozygous TPH2 mutant mice is associated with alterations in serotonin turnover and expression of 5-HT6 and AMPA subunit 2A receptors . J. Affect. Disord . 272 , 440–451. 10.1016/j.jad.2020.04.014 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Gottfried E. D., Christopher S. C. (2017). Mental disorders among criminal offenders: a review of the literature . J. Correct. Health Care 23 , 336–346. 10.1177/1078345817716180 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Goyer P. F., Andreason P. J., Semple W. E., Clayton A. H., King A. C., Compton-Toth B. A., et al.. (1994). Positron-emission tomography and personality disorders . Neuropsychopharmacology 10 :21. 10.1038/npp.1994.3 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Graham K., Bernards S., Wilsnack S., Gmel G. (2011). Alcohol may not cause partner violence but it seems to make it worse . J. Interpers. Violence 26 , 1503–1523. 10.1177/0886260510370596 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Guclu Y. A., Can H. (2018). Ethnic background and alcohol use of the spouse emerge as major risk factors for domestic violence: an observational study from Turkey . JPMA. J. Pak. Med. Assoc. 68 , 1782–1786. [ PubMed ] [ Google Scholar ]
- Hagelstam C., Häkkänen H. (2006). Homicidal adolescents: offense and offender characteristics . Foren. Sci. Int. 164 , 110–115. 10.1016/j.forsciint.2005.12.006 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Harrison A. A., Everitt B. J., Robbins T. W. (1997). Central 5-HT depletion enhances impulsive responding without affecting the accuracy of attentional performance: interactions with dopaminergic mechanisms . Psychopharmacology (Berl) 133 , 329–342. 10.1007/s002130050410 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Hasin D. S., Dvora S., Katherine K.. (2019). Alcohol use and binge drinking among US men, pregnant and non-pregnant women ages 18–44: 2002–2017 . Drug Alcohol Depend. 205 :107590. 10.1016/j.drugalcdep.2019.107590 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Heinrichs R.. (1989). Frontal cerebral lesions and violent incidents in chronic neuropsychiatric patients . Biol. Psychiatry 25 , 174–178. 10.1016/0006-3223(89)90161-3 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Helle A. C., Watts A. L., Trull T. J., Sher K. J. (2019). Alcohol use disorder and antisocial and borderline personality disorders . Alcohol Res. Health. 40. 10.35946/arcr.v40.1.05 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Hentges R. F., Shaw D. S., Wang M. T. (2018). Early childhood parenting and child impulsivity as precursors to aggression, substance use, and risky sexual behavior in adolescence and early adulthood . Dev. Psychopathol. 30 , 1305–1319. 10.1017/S0954579417001596 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Higley J. D., Linnoila M. (2002). A nonhuman primate model of excessive alcohol intake . Recent Dev. Alcohol. 13 , 191–219. 10.1007/0-306-47141-8_11 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Hoaken P. N. S., Pihl R. O. (2000). The effects of alcohol intoxication on aggressive responses in men and women . Alcohol Alcohol . 35 , 471–477. 10.1093/alcalc/35.5.471 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Hockin S., Rogers M. L., Pridemore W. A. (2018). Population-level alcohol consumption and national homicide rates . Eur. J. Criminol. 15 , 235–252. 10.1177/1477370817731042 [ CrossRef ] [ Google Scholar ]
- Holmes A. J., Hollinshead M. O., Roffman J. L., Smoller J. W., Buckner R. L. (2016). Individual differences in cognitive control circuit anatomy link sensation seeking, impulsivity, and substance use . J.Neurosci. 36 , 4038–4049. 10.1523/JNEUROSCI.3206-15.2016 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Hoppen T. H., Chalder T. (2018). Childhood adversity as a transdiagnostic risk factor for affective disorders in adulthood: a systematic review focusing on biopsychosocial moderating and mediating variables . Clin. Psychol. Rev. 65 , 81–151. 10.1016/j.cpr.2018.08.002 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Hoppenbrouwers S. S., Hofman D., Schutter D. J. (2010). Alcohol breaks down interhemispheric inhibition in females but not in males . Psychopharmacology 208 , 469–474. 10.1007/s00213-009-1747-5 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Hutchison I. W.. (1999). Alcohol, fear and woman abuse . Sex Roles . 40 , 893–920. 10.1023/A:1018877106056 [ CrossRef ] [ Google Scholar ]
- Indu P. V., Jinu C. R., Pallikkal N. R., Sampathkumar R., Joy J. (2018). Experience of domestic violence and psychological morbidity in spouses of alcohol-dependent males . Indian J. Psychol. Med. 40 , 322–327. 10.4103/IJPSYM.IJPSYM_38_18 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Ito T. A., Miller N., Pollock V. E. (1996). Alcohol and aggression: a meta-analysis on the moderating effects of inhibitory cues, triggering events, and self-focused attention . Psychol. Bull. 120 :60. 10.1037/0033-2909.120.1.60 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Iverson K. M., Litwack S. D., Pineles S. L., Suvak M. K., Vaughn R. A., Resick P. A. (2013), Predictors of intimate partner violence revictimization . J. Traumatic Stress 26 , 102–110. 10.1002/jts.21781 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Jiang W., Shi F., Liu H., Li G., Ding Z., Shen H., et al.. (2017). Reduced white matter integrity in antisocial personality disorder: a diffusion tensor imaging study . Sci. Rep. 7 , 1–11. 10.1038/srep43002 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Kamal H., Tan G. C., Ibrahim S. F., Shaikh M. F., Mohamed I. N., Mohamed R. M. P., et al.. (2020). Alcohol use disorder, neurodegeneration, Alzheimer's and Parkinson's disease: interplay between oxidative stress, neuroimmune response and excitotoxicity . Front. Cell. Neurosci. 14 :282. 10.3389/fncel.2020.00282 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Kanen J. W., Arntz F. E., Yellowlees R., Cardinal R. N., Price A., Christmas D. M., et al.. (2021). Serotonin depletion amplifies distinct human social emotions as a function of individual differences in personality . Transl. Psychiatry 11 , 1–12. 10.1038/s41398-020-00880-9 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Karlsson T.. (1998). Sharp force homicides in the Stockholm area, 1983-1992 . Foren. Sci. Int. 94 , 129–139. 10.1016/S0379-0738(98)00067-X [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Kästner N., Richter S. H., Urbanik S., Kunert J., Waider J., Lesch K. P., et al.. (2019). Brain serotonin deficiency affects female aggression . Sci. Rep. 9 :1366. 10.1038/s41598-018-37613-4 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Kaufmann V. G., O'Farrell T. J., Murphy C. M., Murphy M. M., Muchowski P. (2014). Alcohol consumption and partner violence among women entering substance use disorder treatment . Psychol. Addict. Behav. 28 , 313–321. 10.1037/a0034971 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Kazzaz Y. M., AlAmeer K. M., AlAhmari R. A., Househ M., El-Metwally A. (2019). The epidemiology of domestic violence in Saudi Arabia: a systematic review . Int. J. Public Health 64 , 1223–1232. 10.1007/s00038-019-01303-3 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Khodabandeh F., Khalilzadeh M., Hemati Z. (2018). The impact of adverse childhood experiences on adulthood aggression and self-esteem-a study on male forensic clients . Novelty Biomed. 6 , 85–91. [ Google Scholar ]
- Kim M. J., Elliott M. L., d'Arbeloff T. C., Knodt A. R., Radtke S. R., Brigidi B. D., et al.. (2019). Microstructural integrity of white matter moderates an association between childhood adversity and adult trait anger . Aggressive Behav. 45 , 310–318. 10.1002/ab.21820 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Kim M. J., Scult M. A., Knodt A. R., Radtke S. R., d'Arbeloff T. C., Brigidi B. D., et al.. (2018). A link between childhood adversity and trait anger reflects relative activity of the amygdala and dorsolateral prefrontal cortex . Biol. Psychiatry Cogn. Neurosci. Neuroimag. 3 , 644–649. 10.1016/j.bpsc.2018.03.006 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Kovács I., Demeter I., Janka Z., Demetrovics Z., Maraz A., Andó B. (2020). Different aspects of impulsivity in chronic alcohol use disorder with and without comorbid problem gambling . PLoS ONE 15 :e0227645. 10.1371/journal.pone.0227645 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Kuhns J. B., Exum M. L., Clodfelter T. A., Bottia M. C. (2014). The prevalence of alcohol-involved homicide offending: a meta-analytic review . Homicide Stud. 18 , 251–270. 10.1177/1088767913493629 [ CrossRef ] [ Google Scholar ]
- Kumar J., Hapidin H., Bee Y. T. G., Ismail Z. (2013). Effects of the mGluR5 antagonist MPEP on ethanol withdrawal induced anxiety-like syndrome in rats . Behav. Brain Funct. 9 , 1–13. 10.1186/1744-9081-9-43 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Kumar J., Hapidin H., Bee Y. T. G., Ismail Z. (2016). The effects of acute ethanol administration on ethanol withdrawal-induced anxiety-like syndrome in rats: a biochemical study . Alcohol 50 , 9–17. 10.1016/j.alcohol.2015.10.001 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Kumar J., Ismail Z., Hatta N. H., Baharuddin N., Hapidin H., Get Bee Y. T., et al.. (2018). Alcohol addiction-metabotropic glutamate receptor subtype 5 and its ligands: How they all come together? Curr. Drug Targets 19 , 907–915. 10.2174/1389450118666170511144302 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Kuypers K. P. C., Verkes R. J., Van den Brink W., Van Amsterdam J. G. C., Ramaekers J. G. (2020). Intoxicated aggression: do alcohol and stimulants cause dose-related aggression? A review . Eur. Neuropsychopharmacol. 30 , 114–147. 10.1016/j.euroneuro.2018.06.001 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Kwagala B., Wandera S. O., Ndugga P., Kabagenyi A. (2013). Empowerment, partner's behaviours and intimate partner physical violence among married women in Uganda . BMC Public Health 13 :1112. 10.1186/1471-2458-13-1112 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Labella M. H., Masten A. S. (2018). Family influences on the development of aggression and violence . Curr. Opin. Psychol. 19 , 11–16. 10.1016/j.copsyc.2017.03.028 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Lagerberg T., Fazel S., Molero Y., Franko M. A., Chen Q., Hellner C., et al.. (2020). Associations between selective serotonin reuptake inhibitors and violent crime in adolescents, young, and older adults–a Swedish register-based study . Eur. Neuropsychopharmacol. 36 , 1–9. 10.1016/j.euroneuro.2020.03.024 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Landberg J., Norström T. (2011). Alcohol and homicide in Russia and the United States: a comparative analysis . J. Stud. Alcohol Drugs 72 , 723–730. 10.15288/jsad.2011.72.723 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Lapierre D., Braun C. M. J., Hodgings S. (1995). Ventral frontal deficits in psychopathy: neuropsychological test findings . Neuropsychologia 33 , 139–151. 10.1016/0028-3932(94)00110-B [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Latkin C. A., Edwards C., Davey-Rothwell M. A., Tobin K. E. (2017). The relationship between social desirability bias and self-reports of health, substance use, and social network factors among urban substance users in Baltimore, Maryland . Addict. Behav. 73 , 133–136. 10.1016/j.addbeh.2017.05.005 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Lawrence A. D., Calder A. J., McGowan S. W., Grasby P. M. (2002). Selective disruption of the recognition of facial expressions of anger . Neuroreport 13 , 881–884. 10.1097/00001756-200205070-00029 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Lee M., Stefani K. M., Park E. C. (2014). Gender-specific differences in risk for intimate partner violence in South Korea . BMC Public Health 14 :415. 10.1186/1471-2458-14-415 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Lee R., Arfanakis K., Evia A. M., Fanning J., Keedy S., Coccaro E. F. (2016). White matter integrity reductions in intermittent explosive disorder . Neuropsychopharmacology 41 , 2697–2703. 10.1038/npp.2016.74 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Leite F., Luis M. A., Amorim M., Maciel E., Gigante D. P. (2019). Violence against women and its association with the intimate partner's profile: a study with primary care users . Brazilian J. Epidemiol . 22 :e190056. [ PubMed ] [ Google Scholar ]
- Lemgruber V. B., Juruena M. F. (2013). The role of early life stress in adult psychiatric disorders . J. Nerv. Ment. Dis. 201 :1007Y1020. 10.1097/NMD.0000000000000049 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Leurquin-Sterk G., Ceccarini J., Crunelle C. L., Weerasekera A., de Laat B., Himmelreich U., et al.. (2018). Cerebral dopaminergic and glutamatergic transmission relate to different subjective responses of acute alcohol intake: an in vivo multimodal imaging study . Addict. Biol. 23 , 931–944. 10.1111/adb.12542 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Lewis R. J., Padilla M. A., Milletich R. J., Kelley M. L., Winstead B. A., Lau-Barraco C., et al.. (2015). Emotional distress, alcohol use, and bidirectional partner violence among lesbian women . Violence Against Women 21 , 917–938. 10.1177/1077801215589375 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Liem M., Soenita G., Sven G., Johanna H., Janne K., Martti L., et al.. (2013). Homicide in Finland, the Netherlands, and Sweden: first findings from the European homicide monitor . Homicide Stud . 17 , 75–95. 10.1177/1088767912452130 [ CrossRef ] [ Google Scholar ]
- Linnoila M., Virkkunen M., Scheinin M., Nuutila A., Rimon R., Goodwin F. K. (1983). Low cerebrospinal fluid 5-hydroxyindoleacetic acid concentration differentiates impulsive from nonimpulsive violent behavior . Life Sci. 33 , 2609–2614. 10.1016/0024-3205(83)90344-2 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Lipsey M. W., Wilson B. M., Cohen M. A., Derzon J. H. (1997). Is there a causal relationship between alcohol use and violence?, in: Recent Developments in Alcoholism and Violence , eds. Galanter M. (New York, NY: Plenum Press; ), 245–282. [ PubMed ] [ Google Scholar ]
- Lira M. C., Xuan Z., Coleman S. M., Swahn M. H., Heeren T. C., Naimi T. S. (2019). Alcohol policies and alcohol involvement in intimate partner homicide in the U.S . Am. J. Prevent. Med. 57 , 172–179. 10.1016/j.amepre.2019.02.027 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Liu C., Tian X., Ling Y., Xu J., Zhou X. (2020). Alterations of metabolites in the frontal cortex and amygdala are associated with cognitive impairment in alcohol dependent patients with aggressive behavior . Front. Psychiatry 11 :684. 10.3389/fpsyt.2020.00694 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Livingston M.. (2011). A longitudinal analysis of alcohol outlet density and domestic violence . Addiction (Abingdon, England) 106 , 919–925. 10.1111/j.1360-0443.2010.03333.x [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Madole J. W., Johnson S. L., Carver C. S. (2020). A model of aggressive behavior: early adversity, impulsivity, and response inhibition . J. Aggr. Maltreat. Trauma 29 , 594–610. 10.1080/10926771.2019.1591561 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Maffli E., Zumbrunn A. (2003). Alcohol and domestic violence in a sample of incidents reported to the police of Zurich City . Subst. Use Misuse 38 , 881–893. 10.1081/JA-120017615 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Malti T.. (2020). Children and violence: nurturing social-emotional development to promote mental health . Soc. Policy Rep . 33 , 1–27. 10.1002/sop2.8 [ CrossRef ] [ Google Scholar ]
- Mann R. E., Zalcman R. F., Smart R. G., Rush B. R., Suurvali H. (2006). Alcohol consumption, alcoholics anonymous membership, and homicide mortality rates in Ontario 1968 to 1991 . Alcohol. Clin. Exp. Res. 30 , 1743–1751. 10.1111/j.1530-0277.2006.00216.x [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Mantere T., Tupala E., Hall H., Särkioja T., Räsänen P., Bergström K., et al.. (2002). Serotonin transporter distribution and density in the cerebral cortex of alcoholic and nonalcoholic comparison subjects: a whole-hemisphere autoradiography study . Am. J. Psychiatry. 159 , 599–606. 10.1176/appi.ajp.159.4.599 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Martin S., Zabala C., Del-Monte J., Graziani P., Aizpurua E., Barry T. J., et al.. (2019). Examining the relationships between impulsivity, aggression, and recidivism for prisoners with antisocial personality disorder . Aggr. Violent Behav. 49 :101314. 10.1016/j.avb.2019.07.009 [ CrossRef ] [ Google Scholar ]
- Martinez D., Slifstein M., Gil R., Hwang D. R., Huang Y., Perez A., et al.. (2009). Positron emission tomography imaging of the serotonin transporter and 5-HT1A receptor in alcohol dependence . Biol. Psychiatry. 65 , 175–180. 10.1016/j.biopsych.2008.08.034 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Mayshak R., Curtis A., Coomber K., Tonner L., Walker A., Hyder S., et al.. (2020). Alcohol-involved family and domestic violence reported to police in Australia . J. Interpers. Violence 886260520928633. 10.1177/0886260520928633 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- McCloskey M. S., Phan K. L., Angstadt M., Fettich K. C., Keedy S., Coccaro E. F. (2016). Amygdala hyperactivation to angry faces in intermittent explosive disorder . J. Psychiatr. Res. 79 , 34–41. 10.1016/j.jpsychires.2016.04.006 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- McLaughlin K. A., Weissman D., Bitrán D. (2019). Childhood adversity and neural development: a systematic review . Ann. Rev. Dev. Psychol. 1 , 277–312. 10.1146/annurev-devpsych-121318-084950 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- McRae K., Ochsner K. N., Mauss I. B., Gabrieli J. J. D., Gross J. J. (2008). Gender differences in emotion regulation: an fMRI study of cognitive reappraisal . Gr. Process Intergr. Relat. 11 , 143–162. 10.1177/1368430207088035 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Melendez R. I., Rodd-Henricks Z. A., Engleman E. A., Li T. K., McBride W. J., Murphy J. M. (2002). Microdialysis of dopamine in the nucleus accumbens of alcohol-preferring (P) rats during anticipation and operant self-administration of ethanol . Alcohol Clin. Exp. Res. 26 , 318–325. 10.1111/j.1530-0277.2002.tb02540.x [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Mokdad A. H., Marks J. S., Stroup D. F., Geberding J. L. (2004). Actual causes of death in the United States, 2000 . J. Am. Med. Assoc. 291 , 1238–1245. 10.1001/jama.291.10.1238 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Naimi T. S., Xuan Z., Coleman S. M., Lira M. C., Hadland S. E., Cooper S. E., et al.. (2017). Alcohol policies and alcohol-involved homicide victimization in the United States . J. Stud. Alcohol Drugs 78 , 781–788. 10.15288/jsad.2017.78.781 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Ninomiya T., Oshita H., Kawano Y., Goto C., Matsuhashi M., Masuda K., et al.. (2018). Reduced white matter integrity in borderline personality disorder: a diffusion tensor imaging study . J. Affect. Disord. 225 , 723–732. 10.1016/j.jad.2017.09.007 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Nord M., Finnema S. J., Halldin C., Farde L. (2013). Effect of a single dose of escitalopram on serotonin concentration in the non-human and human primate brain . Int. J. Neuropsychopharmacol. 16 , 1577–1586. 10.1017/S1461145712001617 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Pakri Mohamed R. M., Kumar J., Ahmad S. U., Mohamed I. N. (2018). Novel pharmacotherapeutic approaches in treatment of alcohol addiction . Curr. Drug Targets 19 , 1378–1390. 10.2174/1389450119666180523092534 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Pewa P., Thomas S., Dagli R., Solanki J., Arora G., Garla B. (2015). Occurrence of domestic violence among women and its impact on oral health in Jodhpur City . J. Contemp. Dental Pract. 16 , 227–233. 10.5005/jp-journals-10024-1666 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Pietrini P., Guazzelli M., Basso G., Jaffe K., Grafman J. (2000). Neural correlates of imaginal aggressive behavior assessed by positron emission tomography in healthy subjects . Am. J. Psychiatry 157 , 1772–1781. 10.1176/appi.ajp.157.11.1772 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Pilkington P. D., Bishop A., Younan R. (2021). Adverse childhood experiences and early maladaptive schemas in adulthood: a systematic review and meta-analysis . Clin. Psychol. Psychother. 28 , 569–565 10.1002/cpp.2533 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Pinel J. P. J., Barnes S. J. (2018). Biopsychology, 10th Edn . England: Pearson Education Limited. [ Google Scholar ]
- Poldrugo F.. (1998). General clinical, ethical and medico-legal aspects - alcohol and criminal behaviour . Alcohol Alcohol . 33 , 12–15. 10.1093/oxfordjournals.alcalc.a008340 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Popova N. K., Ilchibaeva T. V., Antonov E. V., Pershina A. V., Bazovkina D. V., Naumenko V. S. (2020). On the interaction between BDNF and serotonin systems: the effects of long-term ethanol consumption in mice . Alcohol . 87 , 1–15. 10.1016/j.alcohol.2020.04.002 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Porter C., Palmier-Claus J., Branitsky A., Mansell W., Warwick H., Varese F. (2020). Childhood adversity and borderline personality disorder: a meta-analysis . Acta Psychiatr. Scand. 141 , 6–20. 10.1111/acps.13118 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Prepelita R., Cristofor A. C., Dobrin R., Trus C., Ciobica A., Chirita R. (2019). The serotonin-dopamine relationship on the aggression-suicidal risk axis in patients with major depression disorder: describing some social implications . Rev. Cercetare Interv. Soc. 65 , 111–130. 10.33788/rcis.65.8 [ CrossRef ] [ Google Scholar ]
- Puhalla A. A., Berman M. E., Coccaro E. F., Fahlgren M. K., McCloskey M. S. (2020). History of childhood abuse and alcohol use disorder: relationship with intermittent explosive disorder and intoxicated aggression frequency . J. Psychiatr. Res. 125 , 38–44. 10.1016/j.jpsychires.2020.02.025 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Qadeer M. I., Amar A., Huang Y. Y., Min E., Galfalvy H., Hasnain S., et al.. (2021). Association of serotonin system-related genes with homicidal behavior and criminal aggression in a prison population of Pakistani Origin . Sci. Rep. 11 , 1–12. 10.1038/s41598-021-81198-4 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Qadeer M. I., Amar A., Mann J. J., Hasnain S. (2017). Polymorphisms in dopaminergic system genes; association with criminal behavior and self-reported aggression in violent prison inmates from Pakistan . PLoS ONE 12 :e0173571. 10.1371/journal.pone.0173571 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Rahko J., Paakki J. J., Starck T., Nikkinen J., Remes J., Hurtig T., et al.. (2010). Functional mapping of dynamic happy and fearful facial expression processing in adolescents . Brain Imaging Behav. 4 , 164–176. 10.1007/s11682-010-9096-x [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Raine A., Lencz T., Bihrle S., LaCasse L., Colletti P. (2000). Reduced prefrontal gray matter volume and reduced autonomic activity in antisocial personality disorder . Arch. Gen. Psychiatry 57 , 119–127. 10.1001/archpsyc.57.2.119 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Raine A., Meloy J. R., Bihrle S., Stoddard J., LaCasse L., Buchsbaum M. S. (1998). Reduced prefrontal and increased subcortical brain functioning assessed using positron emission tomography in predatory and affective murderers . Behav. Sci. Law 16 , 319–332. 10.1002/(sici)1099-0798(199822)16:3<319::aid-bsl311>3.0.co;2-g [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Rappek N. A. M., Sidi H., Kumar J., Kamarazaman S., Das S., Masiran R., et al.. (2018). Serotonin selective reuptake inhibitors (SSRIs) and female sexual dysfunction (FSD): hypothesis on its association and options of treatment . Curr. Drug Targets 19 , 1352–1358. 10.2174/1389450117666161227142947 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Reno J., Marcus D., Leary M.-L., Samuels J. E. (2010). Full Report of the Prevalence, Incidence, and Consequences of Violence Against Women. Department of Justice . Available online at: https://www.ncjrs.gov/pdffiles1/nij/183781.pdf
- Renzetti C. M., Lynch K. R., DeWall C. N. (2018). Ambivalent sexism, alcohol use, and intimate partner violence perpetration . J. Interp. Violence 33 , 183–210. 10.1177/0886260515604412 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Repple J., Ute H., Lisa W., Christina M. P., Schneider F., Kohn N. (2018). "Sex differences in the neural correlates of aggression . Brain Struct. Funct. 223 , 4115–4124. 10.1007/s00429-018-1739-5 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Room R., Rossow I. (2001). Share of violence attributable to drinking . J. Subst. Use 6 , 218–228. 10.1080/146598901753325048 [ CrossRef ] [ Google Scholar ]
- Rossow I.. (2001). Alcohol and homicide: a cross-cultural comparison of the relationship in 14 European countries . Addiction 96 ( Suppl. 1 ), S77–92. 10.1080/09652140020021198 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Rossow I.. (2004). Alcohol consumption and homicides in Canada, 1950–1999 . Contemp. Drug Prob. 31 , 541–559. 10.1177/009145090403100305 [ CrossRef ] [ Google Scholar ]
- Runions K. C., Morandini H. A., Rao P., Wong J. W., Kolla N. J., Pace G., et al.. (2019). Serotonin and aggressive behaviour in children and adolescents: a systematic review . Acta Psychiatr. Scand. 139 , 117–144. 10.1111/acps.12986 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Sarah M., Keyes K. M. (2019). Heavy and binge alcohol drinking and parenting status in the United States from 2006 to 2018: an analysis of nationally representative cross-sectional surveys . PLoS Med. 16 :e1002954. 10.1371/journal.pmed.1002954 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Sarah M., Keyes K. M. (2020). Trends in US women's binge drinking in middle adulthood by socioeconomic status, 2006–2018 . Drug Alcohol Depend. 212 :108026. 10.1016/j.drugalcdep.2020.108026 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Schorr M. T., Tietbohl-Santos B., de Oliveira L. M., Terra L., de Borba Telles L. E., Hauck S. (2020). Association between different types of childhood trauma and parental bonding with antisocial traits in adulthood: a systematic review . Child Abuse Neglect 107 :104621. 10.1016/j.chiabu.2020.104621 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Schouw J. E., Verkes R. J., Schene A. H., Schellekens A. F. (2020). The relationship between childhood adversity and adult personality revealed by network analysis . Child Abuse Neglect 99 :104254. 10.1016/j.chiabu.2019.104254 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Schwab-Reese L. M., Parker E. A., Peek-Asa C. (2020). Interactions of adolescent social experiences and dopamine genes to predict physical intimate partner violence perpetration . PLoS ONE 12 :e0172840. 10.1371/journal.pone.0172840 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Semahegn A., Belachew T., Abdulahi M. (2013). Domestic violence and its predictors among married women in reproductive age in Fagitalekoma Woreda, Awi zone, Amhara regional state, North Western Ethiopia . Reprod. Health 10 :63. 10.1186/1742-4755-10-63 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Seo D., Patrick C. J., Kennealy P. J. (2008). Role of serotonin and dopamine system interactions in the neurobiology of impulsive aggression and its comorbidity with other clinical disorders . Aggres. Violent Behav. 13 , 383–395. 10.1016/j.avb.2008.06.003 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Seok J. W., Cheong C. (2020). Gray matter deficits and dysfunction in the insula among individuals with intermittent explosive disorder . Front. Psychiatry 11 :439. 10.3389/fpsyt.2020.00439 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Serafini G., Gonda X., Canepa G., Pompili M., Rihmer Z., Amore M., et al.. (2017). Extreme sensory processing patterns show a complex association with depression, and impulsivity, alexithymia, and hopelessness . J. Affect. Disord. 210 , 249–257. 10.1016/j.jad.2016.12.019 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Sharp T., Barnes N. M. (2020). Central 5-HT receptors and their function; present and future . Neuropharmacology 177 :108155. 10.1016/j.neuropharm.2020.108155 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Siep N., Tonnaer F., van de Ven V., Arntz A., Raine A., Cima M. (2019). Anger provocation increases limbic and decreases medial prefrontal cortex connectivity with the left amygdala in reactive aggressive violent offenders . Brain Imaging Behav. 13 , 1311–1323. 10.1007/s11682-018-9945-6 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Siever L. J., Buchsbaum M. S., New A. S., Spiegel-Cohen J., Wei T., Hazlett E. A., et al.. (1999). l-fenfluramine response in impulsive personality disorder assessed with [18F] fluorodeoxyglucose positron emission tomography . Neuropsychopharmacology 20 , 413–423. 10.1016/S0893-133X(98)00111-0 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Smith P. H., Homish G. G., Leonard K. E., Cornelius J. R. (2012). Intimate partner violence and specific substance use disorders: findings from the National Epidemiologic Survey on Alcohol and Related Conditions . Psychol. Addict. Behav. 26 , 236–245. 10.1037/a0024855 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Storvik M., Hakkinen M., Tupala E., Tiihonen J. (2009). 5-HT(1A) receptors in the frontal cortical brain areas in Cloninger type 1 and 2 alcoholics measured by whole-hemisphere autoradiography . Alcohol. Alcohol . 44 , 2–7. 10.1093/alcalc/agn090 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Swart L., Seedat M., Nel J. (2015). Alcohol consumption in adolescent homicide victims in the city of Johannesburg, South Africa . Addiction . 110 , 595–501. 10.1111/add.12825 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- The Guardian (2020). Lockdowns Around the World Bring Rise in Domestic Violence . Available online at: https://www.theguardian.com/society/2020/mar/28/lockdowns-world-rise-domestic-violence?CMP=Share_iOSApp_Other
- Tielbeek J. J., Al-Itejawi Z., Zijlmans J., Polderman T. J., Buckholtz J. W., Popma A. (2018). The impact of chronic stress during adolescence on the development of aggressive behavior: a systematic review on the role of the dopaminergic system in rodents . Neurosci. Biobehav. Rev. 91 , 187–197. 10.1016/j.neubiorev.2016.10.009 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Toshchakova V. A., Bakhtiari Y., Kulikov A. V., Gusev S. I., Trofimova M. V., Fedorenko O. Y., et al.. (2017). Association of polymorphisms of serotonin transporter (5HTTLPR) and 5-HT2C receptor genes with criminal behavior in Russian criminal offenders . Neuropsychobiology 75 , 200–210. 10.1159/000487484 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Trangenstein P. J., Greene N., Eck R. H., Milam A. J., Furr-Holden C. D., Jernigan D. H. (2020). Alcohol advertising and violence . Am. J. Prevent. Med. 58 , 343–351. 10.1016/j.amepre.2019.10.024 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Underwood M. D., Kassir S. A., Bakalian M. J., Galfalvy H., Dwork A. J., Mann J. J., et al.. (2018). Serotonin receptors and suicide, major depression, alcohol use disorder and reported early life adversity . Transl. Psychiatry 8 , 1–15. 10.1038/s41398-018-0309-1 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Underwood M. D., Mann J. J., Huang Y. Y., Arango V. (2008). Family history of alcoholism is associated with lower, 5-H T2A receptor binding in the prefrontal cortex . Alcohol. Clin. Exp. Res . 32 , 593–599. 10.1111/j.1530-0277.2007.00610.x [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Wahlsten P., Koiranen V., Saukko P. (2007). Survey of medico-legal investigation of homicides in the city of Turku, Finland . J. Clin. Foren. Med. 14 , 243–252. 10.1016/j.jcfm.2006.07.007 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Wallace C., Mullen P. E., Burgess P. (2004). Criminal offending in schizophrenia over a 25-year period marked by deinstitutionalization and increasing prevalence of comorbid substance use disorders . Am. J. Psychiatry 161 , 716–727. 10.1176/appi.ajp.161.4.716 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Weiss D. B., Testa A., Rennó Santos M. (2018). Hazardous alcohol drinking and cross-national homicide rates: the role of demographic, political, and cultural context . J. Drug Issues 48 , 246–268. 10.1177/0022042617750579 [ CrossRef ] [ Google Scholar ]
- Wieczorek W. F., Welte J. W., Abel E. L. (1990). Alcohol, drugs, and murder: a study of convicted homicide offenders . J. Crim. Justice 18 , 217–227. 10.1016/0047-2352(90)90002-S [ CrossRef ] [ Google Scholar ]
- Wiener C. D., Moreira F. P., Zago A., Souza L. M., Branco J. C., Oliveira J. F. D., et al.. (2018). Mood disorder, anxiety, and suicide risk among subjects with alcohol abuse and/or dependence: a population-based study . Braz. J. Psychiatry 40 , 1–5. 10.1590/1516-4446-2016-2170 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Wilsnack R. W., Wilsnack S. C., Gmel G., Kantor L. W. (2018). Gender differences in binge drinking . Alcohol Res. Curr. Rev. 39 , 57–76. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Women UN. (2020). The Shadow Pandemic: Violence Against Women During COVID-19 . Available online at: unwomen. org: https://www.unwomen.org/en/news/in-focus/in-focus-gender-equality-in-covid-19-response/violence-against-women-during-covid-19
- Yeo D. C. K., Singham T., Poremski D. (2019). The presence of alcohol consumption prior to homicide in Singapore . Asian J. Psychiatry 44 , 80–85. 10.1016/j.ajp.2019.07.019 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Zai C. C., Ehtesham S., Choi E., Nowrouzi B., De Luca V., Stankovich L., et al.. (2012). Dopaminergic system genes in childhood aggression: possible role for DRD2 . World J. Biol. Psychiatry 13 , 65–74. 10.3109/15622975.2010.543431 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Zhang Y., Ming Q. S., Yi J. Y., Wang X., Chai Q. L., Yao S. Q. (2017). Gene-gene-environment interactions of serotonin transporter, monoamine oxidase A and childhood maltreatment predict aggressive behavior in Chinese adolescents . Front. Behav. Neurosci. 11 :17. 10.3389/fnbeh.2017.00017 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]

IMAGES
COMMENTS
Alcohol Research Resource (R24 and R28) Awards. Resources include biological specimens, animals, data, materials, tools, or services made available to any qualified investigato r to accelerate alcohol-related research in a cost-effective manner. Current and potential alcohol research investigators and trainees are encouraged to subscribe to our ...
Abstract. Alcohol is a major contributor to global disease and a leading cause of preventable death, causing approximately 88,000 deaths annually in the United States alone. Alcohol use disorder is one of the most common psychiatric disorders, with nearly one-third of U.S. adults experiencing alcohol use disorder at some point during their lives.
Learn up-to-date facts and statistics on alcohol consumption and its impact in the United States and globally. Explore topics related to alcohol misuse and treatment, underage drinking, the effects of alcohol on the human body, and more. Find up-to-date statistics on lifetime drinking, past-year drinking, past-month drinking, binge drinking ...
Only a small percent of individuals with alcohol use disorder contribute to the greatest societal and economic costs ().For example, in the 2015 National Survey on Drug Use and Health survey (total n = 43,561), a household survey conducted across the United States, 11.8% met criteria for an alcohol use disorder (n = 5124) ().Of these 5124 individuals, 67.4% (n = 3455) met criteria for a mild ...
NIDA works closely with the National Institute on Alcohol Abuse and Alcoholism (NIAAA), the lead NIH institute supporting and conducting research on the impact of alcohol use on human health and well-being. For information on alcohol and alcohol use disorder, please visit the NIAAA website. Because many people use alcohol while using other ...
Alcohol consumption is a causal factor in more than 200 diseases, injuries and other health conditions. Drinking alcohol is associated with a risk of developing health problems such as mental and behavioural disorders, including alcohol dependence, and major noncommunicable diseases such as liver cirrhosis, some cancers and cardiovascular ...
Various research studies conducted over many years clearly show the association of prolonged alcohol intake in the causation, aggravation, worsening, and deterioration of the health of its consumers. ... Alcohol abuse along with other associated factors is one of the leading causes of secondary cardiomyopathy . Cardiac arrhythmias get ...
The average annual number of deaths from excessive alcohol use among males increased by 25,244 (26.8%), from 94,362 deaths during 2016-2017 to 119,606 during 2020-2021 ( Table 2 ). Age-standardized death rates among males increased from 54.8 per 100,000 population during 2016-2017 to 55.9 during 2018-2019, and to 66.9 during 2020-2021.
Introduction. There has been a global increase in alcohol misuse and rates of alcohol use disorder (AUD) over the last two decades. 1 Recent substantial increases in the United States come from dramatic rises in the prevalence of alcohol misuse and AUD in women relative to men (women, 84% increase; men, 35% increase). 2 This dramatic rise stems from increases in hazardous and binge drinking in ...
Recent estimates for the United States indicate that 5.6% of cancer cases and 4.0% of cancer deaths are attributable to alcohol consumption. 6; Research has shown that people who misuse alcohol have a greater risk of liver disease, heart disease, depression, stroke, and stomach bleeding, as well as cancers of the oral cavity, esophagus, larynx ...
Alcohol use disorder (AUD) is a prevalent psychiatric condition in the United States, characterized by problematic and unhealthy patterns of alcohol consumption. It is a well-recognized disorder that encompasses a broad spectrum of symptoms and behaviors associated with alcohol misuse. AUD affects a significant portion of the population, making it one of the most widespread psychiatric ...
December 31, 1970—NIAAA was established under authority of the Comprehensive Alcohol Abuse and Alcoholism Prevention, Treatment, and Rehabilitation Act of 1970 (Public Law 91-616) with authority to develop and conduct comprehensive health, education, training, research, and planning programs for the prevention and treatment of alcohol abuse ...
Recent research has focused on areas such as the genetics of addiction, links between excessive alcohol use and mental health and other disorders, harm to long-term brain health that can be caused by adolescent alcohol use, and the effects of prenatal alcohol exposure, among others. "We want everyone from pharmacists and nurses to addiction ...
NIAAA supports and conducts research on the impact of alcohol use on human health and well-being. ... Raising Awareness about Alcohol Misuse Among Teens The Healthcare Professional's Core Resource on Alcohol from NIAAA A Virtual Reality Experience from NIAAA Alcohol Facts & Statistics Latest News & Events More News & Events . Image.
Introduction. Excessive alcohol use amongst college students is associated with low grades, poor mental health, and risks to physical safety. Neuroticism, characterized by emotional instability and anxiety, and self-reported stress have both been shown to be strong predictors of alcohol use and misuse, however, previous studies have shown that measures of stress and Neuroticism are frequently ...
Alcohol Misuse/Dependence. The rates of alcohol misuse/dependence in older adults are by far smaller than the rates of at-risk use. In 2002, over 616,000 adults age 55 and older reported meeting the criteria for alcohol dependence in the past year, as defined by the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV ...
Science-based information on alcohol from NIAAA, including alcohol's effects on the brain and body, drinking levels, ... National Institute on Alcohol Abuse and Alcoholism (NIAAA) ... PDF materials for patient education and free, research-focused print materials. Short Takes These brief, informative videos from NIAAA offers researched based ...
Literature on the onset of substance use among youth and young adults has indicated that internalizing symptoms (e.g., depression and anxiety) generally protect against the onset of alcohol misuse in adolescents.23 However, the association between internalizing symptoms and risk for alcohol use and misuse is influenced by key moderating factors ...
The National Institute on Alcohol Abuse and Alcoholism defines one standard drink as any one of these: 12 ounces (355 milliliters) of regular beer (about 5% alcohol) ... Some research studies indicate that having bariatric surgery may increase the risk of developing alcohol use disorder or of relapsing after recovering from alcohol use disorder.
Alcohol-related harms. To identify what the most harmful drug is in the world, British researchers recently conducted multi-criteria decision analysis to rank medications in this respect.9 They found that in the United Kingdom (UK), the reputation of being the most dangerous substance in terms of overall harm to users and others belonged to alcohol. In another study on substance abuse, a scale ...
Alcohol and Domestic Abuse/Violence. There is a strong evidence linking alcohol with domestic abuse or domestic violence (Gadd et al., 2019).A study conducted within the metropolitan area of Melbourne, Australia found that alcohol outlet density was significantly associated with domestic violence rates over time (Livingston, 2011).In Australia, alcohol-related domestic violence is twice more ...