An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Front Psychiatry

Mental Health Prevention and Promotion—A Narrative Review
Associated data.
Extant literature has established the effectiveness of various mental health promotion and prevention strategies, including novel interventions. However, comprehensive literature encompassing all these aspects and challenges and opportunities in implementing such interventions in different settings is still lacking. Therefore, in the current review, we aimed to synthesize existing literature on various mental health promotion and prevention interventions and their effectiveness. Additionally, we intend to highlight various novel approaches to mental health care and their implications across different resource settings and provide future directions. The review highlights the (1) concept of preventive psychiatry, including various mental health promotions and prevention approaches, (2) current level of evidence of various mental health preventive interventions, including the novel interventions, and (3) challenges and opportunities in implementing concepts of preventive psychiatry and related interventions across the settings. Although preventive psychiatry is a well-known concept, it is a poorly utilized public health strategy to address the population's mental health needs. It has wide-ranging implications for the wellbeing of society and individuals, including those suffering from chronic medical problems. The researchers and policymakers are increasingly realizing the potential of preventive psychiatry; however, its implementation is poor in low-resource settings. Utilizing novel interventions, such as mobile-and-internet-based interventions and blended and stepped-care models of care can address the vast mental health need of the population. Additionally, it provides mental health services in a less-stigmatizing and easily accessible, and flexible manner. Furthermore, employing decision support systems/algorithms for patient management and personalized care and utilizing the digital platform for the non-specialists' training in mental health care are valuable additions to the existing mental health support system. However, more research concerning this is required worldwide, especially in the low-and-middle-income countries.
Introduction
Mental disorder has been recognized as a significant public health concern and one of the leading causes of disability worldwide, particularly with the loss of productive years of the sufferer's life ( 1 ). The Global Burden of Disease report (2019) highlights an increase, from around 80 million to over 125 million, in the worldwide number of Disability-Adjusted Life Years (DALYs) attributable to mental disorders. With this surge, mental disorders have moved into the top 10 significant causes of DALYs worldwide over the last three decades ( 2 ). Furthermore, this data does not include substance use disorders (SUDs), which, if included, would increase the estimated burden manifolds. Moreover, if the caregiver-related burden is accounted for, this figure would be much higher. Individual, social, cultural, political, and economic issues are critical mental wellbeing determinants. An increasing burden of mental diseases can, in turn, contribute to deterioration in physical health and poorer social and economic growth of a country ( 3 ). Mental health expenditure is roughly 3–4% of their Gross Domestic Products (GDPs) in developed regions of the world; however, the figure is abysmally low in low-and-middle-income countries (LMICs) ( 4 ). Untreated mental health and behavioral problems in childhood and adolescents, in particular, have profound long-term social and economic adverse consequences, including increased contact with the criminal justice system, lower employment rate and lesser wages among those employed, and interpersonal difficulties ( 5 – 8 ).
Need for Mental Health (MH) Prevention
Longitudinal studies suggest that individuals with a lower level of positive wellbeing are more likely to acquire mental illness ( 9 ). Conversely, factors that promote positive wellbeing and resilience among individuals are critical in preventing mental illnesses and better outcomes among those with mental illness ( 10 , 11 ). For example, in patients with depressive disorders, higher premorbid resilience is associated with earlier responses ( 12 ). On the contrary, patients with bipolar affective- and recurrent depressive disorders who have a lower premorbid quality of life are at higher risk of relapses ( 13 ).
Recently there has been an increased emphasis on the need to promote wellbeing and positive mental health in preventing the development of mental disorders, for poor mental health has significant social and economic implications ( 14 – 16 ). Research also suggests that mental health promotion and preventative measures are cost-effective in preventing or reducing mental illness-related morbidity, both at the society and individual level ( 17 ).
Although the World Health Organization (WHO) defines health as “a state of complete physical, mental, and social wellbeing and not merely an absence of disease or infirmity,” there has been little effort at the global level or stagnation in implementing effective mental health services ( 18 ). Moreover, when it comes to the research on mental health (vis-a-viz physical health), promotive and preventive mental health aspects have received less attention vis-a-viz physical health. Instead, greater emphasis has been given to the illness aspect, such as research on psychopathology, mental disorders, and treatment ( 19 , 20 ). Often, physicians and psychiatrists are unfamiliar with various concepts, approaches, and interventions directed toward mental health promotion and prevention ( 11 , 21 ).
Prevention and promotion of mental health are essential, notably in reducing the growing magnitude of mental illnesses. However, while health promotion and disease prevention are universally regarded concepts in public health, their strategic application for mental health promotion and prevention are often elusive. Furthermore, given the evidence of substantial links between psychological and physical health, the non-incorporation of preventive mental health services is deplorable and has serious ramifications. Therefore, policymakers and health practitioners must be sensitized about linkages between mental- and physical health to effectively implement various mental health promotive and preventive interventions, including in individuals with chronic physical illnesses ( 18 ).
The magnitude of the mental health problems can be gauged by the fact that about 10–20% of young individuals worldwide experience depression ( 22 ). As described above, poor mental health during childhood is associated with adverse health (e.g., substance use and abuse), social (e.g., delinquency), academic (e.g., school failure), and economic (high risk of poverty) adverse outcomes in adulthood ( 23 ). Childhood and adolescence are critical periods for setting the ground for physical growth and mental wellbeing ( 22 ). Therefore, interventions promoting positive psychology empower youth with the life skills and opportunities to reach their full potential and cope with life's challenges. Comprehensive mental health interventions involving families, schools, and communities have resulted in positive physical and psychological health outcomes. However, the data is limited to high-income countries (HICs) ( 24 – 28 ).
In contrast, in low and middle-income countries (LMICs) that bear the greatest brunt of mental health problems, including massive, coupled with a high treatment gap, such interventions remained neglected in public health ( 29 , 30 ). This issue warrants prompt attention, particularly when global development strategies such as Millennium Development Goals (MDGs) realize the importance of mental health ( 31 ). Furthermore, studies have consistently reported that people with socioeconomic disadvantages are at a higher risk of mental illness and associated adverse outcomes; partly, it is attributed to the inequitable distribution of mental health services ( 32 – 35 ).
Scope of Mental Health Promotion and Prevention in the Current Situation
Literature provides considerable evidence on the effectiveness of various preventive mental health interventions targeting risk and protective factors for various mental illnesses ( 18 , 36 – 42 ). There is also modest evidence of the effectiveness of programs focusing on early identification and intervention for severe mental diseases (e.g., schizophrenia and psychotic illness, and bipolar affective disorders) as well as common mental disorders (e.g., anxiety, depression, stress-related disorders) ( 43 – 46 ). These preventive measures have also been evaluated for their cost-effectiveness with promising findings. In addition, novel interventions such as digital-based interventions and novel therapies (e.g., adventure therapy, community pharmacy program, and Home-based Nurse family partnership program) to address the mental health problems have yielded positive results. Likewise, data is emerging from LMICs, showing at least moderate evidence of mental health promotion intervention effectiveness. However, most of the available literature and intervention is restricted mainly to the HICs ( 47 ). Therefore, their replicability in LMICs needs to be established and, also, there is a need to develop locally suited interventions.
Fortunately, there has been considerable progress in preventive psychiatry over recent decades, including research on it. In the light of these advances, there is an accelerated interest among researchers, clinicians, governments, and policymakers to harness the potentialities of the preventive strategies to improve the availability, accessibility, and utility of such services for the community.
The Concept of Preventive Psychiatry
Origins of preventive psychiatry.
The history of preventive psychiatry can be traced back to the early 1900's with the foundation of the national mental health association (erstwhile mental health association), the committee on mental hygiene in New York, and the mental health hygiene movement ( 48 ). The latter emphasized the need for physicians to develop empathy and recognize and treat mental illness early, leading to greater awareness about mental health prevention ( 49 ). Despite that, preventive psychiatry remained an alien concept for many, including mental health professionals, particularly when the etiology of most psychiatric disorders was either unknown or poorly understood. However, recent advances in our understanding of the phenomena underlying psychiatric disorders and availability of the neuroimaging and electrophysiological techniques concerning mental illness and its prognosis has again brought the preventive psychiatry in the forefront ( 1 ).
Levels of Prevention
The literal meaning of “prevention” is “the act of preventing something from happening” ( 50 ); the entity being prevented can range from the risk factors of the development of the illness, the onset of illness, or the recurrence of the illness or associated disability. The concept of prevention emerged primarily from infectious diseases; measures like mass vaccination and sanitation promotion have helped prevent the development of the diseases and subsequent fatalities. The original preventive model proposed by the Commission on Chronic Illness in 1957 included primary, secondary, and tertiary preventions ( 48 ).
The Concept of Primary, Secondary, and Tertiary Prevention
The stages of prevention target distinct aspects of the illness's natural course; the primary prevention acts at the stage of pre-pathogenesis, that is, when the disease is yet to occur, whereas the secondary and tertiary prevention target the phase after the onset of the disease ( 51 ). Primary prevention includes health promotion and specific protection, while secondary and tertairy preventions include early diagnosis and treatment and measures to decrease disability and rehabilitation, respectively ( 51 ) ( Figure 1 ).

The concept of primary and secondary prevention [adopted from prevention: Primary, Secondary, Tertiary by Bauman et al. ( 51 )].
The primary prevention targets those individuals vulnerable to developing mental disorders and their consequences because of their bio-psycho-social attributes. Therefore, it can be viewed as an intervention to prevent an illness, thereby preventing mental health morbidity and potential social and economic adversities. The preventive strategies under it usually target the general population or individuals at risk. Secondary and tertiary prevention targets those who have already developed the illness, aiming to reduce impairment and morbidity as soon as possible. However, these measures usually occur in a person who has already developed an illness, therefore facing related suffering, hence may not always be successful in curing or managing the illness. Thus, secondary and tertiary prevention measures target the already exposed or diagnosed individuals.
The Concept of Universal, Selective, and Indicated Prevention
The classification of health prevention based on primary/secondary/tertiary prevention is limited in being highly centered on the etiology of the illness; it does not consider the interaction between underlying etiology and risk factors of an illness. Gordon proposed another model of prevention that focuses on the degree of risk an individual is at, and accordingly, the intensity of intervention is determined. He has classified it into universal, selective, and indicated prevention. A universal preventive strategy targets the whole population irrespective of individual risk (e.g., maintaining healthy, psychoactive substance-free lifestyles); selective prevention is targeted to those at a higher risk than the general population (socio-economically disadvantaged population, e.g., migrants, a victim of a disaster, destitute, etc.). The indicated prevention aims at those who have established risk factors and are at a high risk of getting the disease (e.g., family history of psychiatric illness, history of substance use, certain personality types, etc.). Nevertheless, on the other hand, these two classifications (the primary, secondary, and tertiary prevention; and universal, selective, and indicated prevention) have been intended for and are more appropriate for physical illnesses with a clear etiology or risk factors ( 48 ).
In 1994, the Institute of Medicine (IOM) Committee on Prevention of Mental Disorders proposed a new paradigm that classified primary preventive measures for mental illnesses into three categories. These are indicated, selected, and universal preventive interventions (refer Figure 2 ). According to this paradigm, primary prevention was limited to interventions done before the onset of the mental illness ( 48 ). In contrast, secondary and tertiary prevention encompasses treatment and maintenance measures ( Figure 2 ).

The interventions for mental illness as classified by the Institute of Medicine (IOM) Committee on Prevention of Mental Disorders [adopted from Mrazek and Haggerty ( 48 )].
Although the boundaries between prevention and treatment are often more overlapping than being exclusive, the new paradigm can be used to avoid confusion stemming from the common belief that prevention can take place at all parts of mental health management ( 48 ). The onset of mental illnesses can be prevented by risk reduction interventions, which can involve reducing risk factors in an individual and strengthening protective elements in them. It aims to target modifiable factors, both risk, and protective factors, associated with the development of the illness through various general and specific interventions. These interventions can work across the lifespan. The benefits are not restricted to reduction or delay in the onset of illness but also in terms of severity or duration of illness ( 48 ).On the spectrum of mental health interventions, universal preventive interventions are directed at the whole population without identifiable risk factors. The interventions are beneficial for the general population or sub-groups. Prenatal care and childhood vaccination are examples of preventative measures that have benefited both physical and mental health. Selective preventive mental health interventions are directed at people or a subgroup with a significantly higher risk of developing mental disorders than the general population. Risk groups are those who, because of their vulnerabilities, are at higher risk of developing mental illnesses, e.g., infants with low-birth-weight (LBW), vulnerable children with learning difficulties or victims of maltreatment, elderlies, etc. Specific interventions are home visits and new-born day care facilities for LBW infants, preschool programs for all children living in resource-deprived areas, support groups for vulnerable elderlies, etc. Indicated preventive interventions focus on high-risk individuals who have developed minor but observable signs or symptoms of mental disorder or genetic risk factors for mental illness. However, they have not fulfilled the criteria of a diagnosable mental disorder. For instance, the parent-child interaction training program is an indicated prevention strategy that offers support to children whose parents have recognized them as having behavioral difficulties.
The overall objective of mental health promotion and prevention is to reduce the incidence of new cases, additionally delaying the emergence of mental illness. However, promotion and prevention in mental health complement each other rather than being mutually exclusive. Moreover, combining these two within the overall public health framework reduces stigma, increases cost-effectiveness, and provides multiple positive outcomes ( 18 ).
How Prevention in Psychiatry Differs From Other Medical Disorders
Compared to physical illnesses, diagnosing a mental illness is more challenging, particularly when there is still a lack of objective assessment methods, including diagnostic tools and biomarkers. Therefore, the diagnosis of mental disorders is heavily influenced by the assessors' theoretical perspectives and subjectivity. Moreover, mental illnesses can still be considered despite an individual not fulfilling the proper diagnostic criteria led down in classificatory systems, but there is detectable dysfunction. Furthermore, the precise timing of disorder initiation or transition from subclinical to clinical condition is often uncertain and inconclusive ( 48 ). Therefore, prevention strategies are well-delineated and clear in the case of physical disorders while it's still less prevalent in mental health parlance.
Terms, Definitions, and Concepts
The terms mental health, health promotion, and prevention have been differently defined and interpreted. It is further complicated by overlapping boundaries of the concept of promotion and prevention. Some commonly used terms in mental health prevention have been tabulated ( Table 1 ) ( 18 ).
Commonly used terms in mental health prevention.
Mental Health Promotion and Protection
The term “mental health promotion” also has definitional challenges as it signifies different things to different individuals. For some, it means the treatment of mental illness; for others, it means preventing the occurrence of mental illness; while for others, it means increasing the ability to manage frustration, stress, and difficulties by strengthening one's resilience and coping abilities ( 54 ). It involves promoting the value of mental health and improving the coping capacities of individuals rather than amelioration of symptoms and deficits.
Mental health promotion is a broad concept that encompasses the entire population, and it advocates for a strengths-based approach and tries to address the broader determinants of mental health. The objective is to eliminate health inequalities via empowerment, collaboration, and participation. There is mounting evidence that mental health promotion interventions improve mental health, lower the risk of developing mental disorders ( 48 , 55 , 56 ) and have socioeconomic benefits ( 24 ). In addition, it strives to increase an individual's capacity for psychosocial wellbeing and adversity adaptation ( 11 ).
However, the concepts of mental health promotion, protection, and prevention are intrinsically linked and intertwined. Furthermore, most mental diseases result from complex interaction risk and protective factors instead of a definite etiology. Facilitating the development and timely attainment of developmental milestones across an individual's lifespan is critical for positive mental health ( 57 ). Although mental health promotion and prevention are essential aspects of public health with wide-ranging benefits, their feasibility and implementation are marred by financial and resource constraints. The lack of cost-effectiveness studies, particularly from the LMICs, further restricts its full realization ( 47 , 58 , 59 ).
Despite the significance of the topic and a considerable amount of literature on it, a comprehensive review is still lacking that would cover the concept of mental health promotion and prevention and simultaneously discusses various interventions, including the novel techniques delivered across the lifespan, in different settings, and level of prevention. Therefore, this review aims to analyze the existing literature on various mental health promotion and prevention-based interventions and their effectiveness. Furthermore, its attempts to highlight the implications of such intervention in low-resource settings and provides future directions. Such literature would add to the existing literature on mental health promotion and prevention research and provide key insights into the effectiveness of such interventions and their feasibility and replicability in various settings.
Methodology
For the current review, key terms like “mental health promotion,” OR “protection,” OR “prevention,” OR “mitigation” were used to search relevant literature on Google Scholar, PubMed, and Cochrane library databases, considering a time period between 2000 to 2019 ( Supplementary Material 1 ). However, we have restricted our search till 2019 for non-original articles (reviews, commentaries, viewpoints, etc.), assuming that it would also cover most of the original articles published until then. Additionally, we included original papers from the last 5 years (2016–2021) so that they do not get missed out if not covered under any published review. The time restriction of 2019 for non-original articles was applied to exclude papers published during the Coronavirus disease (COVID-19) pandemic as the latter was a significant event, bringing about substantial change and hence, it warranted a different approach to cater to the MH needs of the population, including MH prevention measures. Moreover, the COVID-19 pandemic resulted in the flooding of novel interventions for mental health prevention and promotion, specifically targeting the pandemic and its consequences, which, if included, could have biased the findings of the current review on various MH promotion and prevention interventions.
A time frame of about 20 years was taken to see the effectiveness of various MH promotion and protection interventions as it would take substantial time to be appreciated in real-world situations. Therefore, the current paper has put greater reliance on the review articles published during the last two decades, assuming that it would cover most of the original articles published until then.
The above search yielded 320 records: 225 articles from Google scholar, 59 articles from PubMed, and 36 articles from the Cochrane database flow-diagram of records screening. All the records were title/abstract screened by all the authors to establish the suitability of those records for the current review; a bibliographic- and gray literature search was also performed. In case of any doubts or differences in opinion, it was resolved by mutual discussion. Only those articles directly related to mental health promotion, primary prevention, and related interventions were included in the current review. In contrast, records that discussed any specific conditions/disorders (post-traumatic stress disorders, suicide, depression, etc.), specific intervention (e.g., specific suicide prevention intervention) that too for a particular population (e.g., disaster victims) lack generalizability in terms of mental health promotion or prevention, those not available in the English language, and whose full text was unavailable were excluded. The findings of the review were described narratively.
Interventions for Mental Health Promotion and Prevention and Their Evidence
Various interventions have been designed for mental health promotion and prevention. They are delivered and evaluated across the regions (high-income countries to low-resource settings, including disaster-affiliated regions of the world), settings (community-based, school-based, family-based, or individualized); utilized different psychological constructs and therapies (cognitive behavioral therapy, behavioral interventions, coping skills training, interpersonal therapies, general health education, etc.); and delivered by different professionals/facilitators (school-teachers, mental health professionals or paraprofessionals, peers, etc.). The details of the studies, interventions used, and outcomes have been provided in Supplementary Table 1 . Below we provide the synthesized findings of the available research.
The majority of the available studies were quantitative and experimental. Randomized controlled trials comprised a sizeable proportion of the studies; others were quasi-experimental studies and, a few, qualitative studies. The studies primarily focussed on school students or the younger population, while others were explicitly concerned with the mental health of young females ( 60 ). Newer data is emerging on mental health promotion and prevention interventions for elderlies (e.g., dementia) ( 61 ). The majority of the research had taken a broad approach to mental health promotion ( 62 ). However, some studies have focused on universal prevention ( 63 , 64 ) or selective prevention ( 65 – 68 ). For instance, the Resourceful Adolescent Program (RAPA) was implemented across the schools and has utilized cognitive-behavioral and interpersonal therapies and reported a significant improvement in depressive symptoms. Some of the interventions were directed at enhancing an individual's characteristics like resilience, behavior regulation, and coping skills (ZIPPY's Friends) ( 69 ), while others have focused on the promotion of social and emotional competencies among the school children and attempted to reduce the gap in such competencies across the socio-economic classes (“Up” program) ( 70 ) or utilized expressive abilities of the war-affected children (Writing for Recover (WfR) intervention) ( 71 ) to bring about an improvement in their psychological problems (a type of selective prevention) ( 62 ) or harnessing the potential of Art, in the community-based intervention, to improve self-efficacy, thus preventing mental disorders (MAD about Art program) ( 72 ). Yet, others have focused on strengthening family ( 60 , 73 ), community relationships ( 62 ), and targeting modifiable risk factors across the life course to prevent dementia among the elderlies and also to support the carers of such patients ( 61 ).
Furthermore, more of the studies were conducted and evaluated in the developed parts of the world, while emerging economies, as anticipated, far lagged in such interventions or related research. The interventions that are specifically adapted for local resources, such as school-based programs involving paraprofessionals and teachers in the delivery of mental health interventions, were shown to be more effective ( 62 , 74 ). Likewise, tailored approaches for low-resource settings such as LMICs may also be more effective ( 63 ). Some of these studies also highlight the beneficial role of a multi-dimensional approach ( 68 , 75 ) and interventions targeting early lifespan ( 76 , 77 ).
Newer Insights: How to Harness Digital Technology and Novel Methods of MH Promotion and Protection
With the advent of digital technology and simultaneous traction on mental health promotion and prevention interventions, preventive psychiatrists and public health experts have developed novel techniques to deliver mental health promotive and preventive interventions. These encompass different settings (e.g., school, home, workplace, the community at large, etc.) and levels of prevention (universal, selective, indicated) ( 78 – 80 ).
The advanced technologies and novel interventions have broadened the scope of MH promotion and prevention, such as addressing the mental health issues of individuals with chronic medical illness ( 81 , 82 ), severe mental disorders ( 83 ), children and adolescents with mental health problems, and geriatric population ( 78 ). Further, it has increased the accessibility and acceptability of such interventions in a non-stigmatizing and tailored manner. Moreover, they can be integrated into the routine life of the individuals.
For instance, Internet-and Mobile-based interventions (IMIs) have been utilized to monitor health behavior as a form of MH prevention and a stand-alone self-help intervention. Moreover, the blended approach has expanded the scope of MH promotive and preventive interventions such as face-to-face interventions coupled with remote therapies. Simultaneously, it has given way to the stepped-care (step down or step-up care) approach of treatment and its continuation ( 79 ). Also, being more interactive and engaging is particularly useful for the youth.
The blended model of care has utilized IMIs to a varying degree and at various stages of the psychological interventions. This includes IMIs as a supplementary approach to the face-to-face-interventions (FTFI), FTFI augmented by behavior intervention technologies (BITs), BITs augmented by remote human support, and fully automated BITs ( 84 ).
The stepped care model of mental health promotion and prevention strategies includes a stepped-up approach, wherein BITs are utilized to manage the prodromal symptoms, thereby preventing the onset of the full-blown episode. In the Stepped-down approach, the more intensive treatments (in-patient or out-patient based interventions) are followed and supplemented with the BITs to prevent relapse of the mental illness, such as for previously admitted patients with depression or substance use disorders ( 85 , 86 ).
Similarly, the latest research has developed newer interventions for strengthening the psychological resilience of the public or at-risk individuals, which can be delivered at the level of the home, such as, e.g., nurse family partnership program (to provide support to the young and vulnerable mothers and prevent childhood maltreatment) ( 87 ); family healing together program aimed at improving the mental health of the family members living with persons with mental illness (PwMI) ( 88 ). In addition, various novel interventions for MH promotion and prevention have been highlighted in the Table 2 .
Depiction of various novel mental health promotion and prevention strategies.
a/w, associated with; A-V, audio-visual; b/w, between; CBT, Cognitive Behavioral Therapy; CES-Dep., Center for Epidemiologic Studies-Depression scale; CG, control group; FU, follow-up; GAD, generalized anxiety disorders-7; IA, intervention arm; HCWs, Health Care Workers; LMIC, low and middle-income countries; MDD, major depressive disorders; mgt, management; MH, mental health; MHP, mental health professional; MINI, mini neuropsychiatric interview; NNT, number needed to treat; PHQ-9, patient health questionnaire; TAU, treatment as usual .
Furthermore, school/educational institutes-based interventions such as school-Mental Health Magazines to increase mental health literacy among the teachers and students have been developed ( 80 ). In addition, workplace mental health promotional activities have targeted the administrators, e.g., guided “e-learning” for the managers that have shown to decrease the mental health problems of the employees ( 102 ).
Likewise, digital technologies have also been harnessed in strengthening community mental health promotive/preventive services, such as the mental health first aid (MHFA) Books on Prescription initiative in New Zealand provided information and self-help tools through library networks and trained book “prescribers,” particularly in rural and remote areas ( 103 ).
Apart from the common mental disorders such as depression, anxiety, and behavioral disorders in the childhood/adolescents, novel interventions have been utilized to prevent the development of or management of medical, including preventing premature mortality and psychological issues among the individuals with severe mental illnesses (SMIs), e.g., Lets' talk about tobacco-web based intervention and motivational interviewing to prevent tobacco use, weight reduction measures, and promotion of healthy lifestyles (exercise, sleep, and balanced diets) through individualized devices, thereby reducing the risk of cardiovascular disorders ( 83 ). Similarly, efforts have been made to improve such individuals' coping skills and employment chances through the WorkingWell mobile application in the US ( 104 ).
Apart from the digital-based interventions, newer, non-digital-based interventions have also been utilized to promote mental health and prevent mental disorders among individuals with chronic medical conditions. One such approach in adventure therapy aims to support and strengthen the multi-dimensional aspects of self. It includes the physical, emotional or cognitive, social, spiritual, psychological, or developmental rehabilitation of the children and adolescents with cancer. Moreover, it is delivered in the natural environment outside the hospital premises, shifting the focus from the illness model to the wellness model ( 81 ). Another strength of this intervention is it can be delivered by the nurses and facilitate peer support and teamwork.
Another novel approach to MH prevention is gut-microbiota and dietary interventions. Such interventions have been explored with promising results for the early developmental disorders (Attention deficit hyperactive disorder, Autism spectrum disorders, etc.) ( 105 ). It works under the framework of the shared vulnerability model for common mental disorders and other non-communicable diseases and harnesses the neuroplasticity potential of the developing brain. Dietary and lifestyle modifications have been recommended for major depressive disorders by the Clinical Practice Guidelines in Australia ( 106 ). As most childhood mental and physical disorders are determined at the level of the in-utero and early after the birth period, targeting maternal nutrition is another vital strategy. The utility has been expanded from maternal nutrition to women of childbearing age. The various novel mental health promotion and prevention strategies are shown in Table 2 .
Newer research is emerging that has utilized the digital platform for training non-specialists in diagnosis and managing individuals with mental health problems, such as Atmiyata Intervention and The SMART MH Project in India, and The Allillanchu Project in Peru, to name a few ( 99 ). Such frameworks facilitate task-sharing by the non-specialist and help in reducing the treatment gap in these countries. Likewise, digital algorithms or decision support systems have been developed to make mental health services more transparent, personalized, outcome-driven, collaborative, and integrative; one such example is DocuMental, a clinical decision support system (DSS). Similarly, frameworks like i-PROACH, a cloud-based intelligent platform for research outcome assessment and care in mental health, have expanded the scope of the mental health support system, including promoting research in mental health ( 100 ). In addition, COVID-19 pandemic has resulted in wider dissemination of the applications based on the evidence-based psycho-social interventions such as National Health Service's (NHS's) Mind app and Headspace (teaching meditation via a website or a phone application) that have utilized mindfulness-based practices to address the psychological problems of the population ( 101 ).
Challenges in Implementing Novel MH Promotion and Prevention Strategies
Although novel interventions, particularly internet and mobile-based interventions (IMIs), are effective models for MH promotion and prevention, their cost-effectiveness requires further exploration. Moreover, their feasibility and acceptability in LMICs could be challenging. Some of these could be attributed to poor digital literacy, digital/network-related limitations, privacy issues, and society's preparedness to implement these interventions.
These interventions need to be customized and adapted according to local needs and context, for which implementation and evaluative research are warranted. In addition, the infusion of more human and financial resources for such activities is required. Some reports highlight that many of these interventions do not align with the preferences and use the pattern of the service utilizers. For instance, one explorative research on mental health app-based interventions targeting youth found that despite the burgeoning applications, they are not aligned with the youth's media preferences and learning patterns. They are less interactive, have fewer audio-visual displays, are not youth-specific, are less dynamic, and are a single touch app ( 107 ).
Furthermore, such novel interventions usually come with high costs. In low-resource settings where service utilizers have limited finances, their willingness to use such services may be doubtful. Moreover, insurance companies, including those in high-income countries (HICs), may not be willing to fund such novel interventions, which restricts the accessibility and availability of interventions.
Research points to the feasibility and effectiveness of incorporating such novel interventions in routine services such as school, community, primary care, or settings, e.g., in low-resource settings, the resource persons like teachers, community health workers, and primary care physicians are already overburdened. Therefore, their willingness to take up additional tasks may raise skepticism. Moreover, the attitudinal barrier to moving from the traditional service delivery model to the novel methods may also impede.
Considering the low MH budget and less priority on the MH prevention and promotion activities in most low-resource settings, the uptake of such interventions in the public health framework may be lesser despite the latter's proven high cost-effectiveness. In contrast, policymakers may be more inclined to invest in the therapeutic aspects of MH.
Such interventions open avenues for personalized and precision medicine/health care vs. the traditional model of MH promotion and preventive interventions ( 108 , 109 ). For instance, multivariate prediction algorithms with methods of machine learning and incorporating biological research, such as genetics, may help in devising tailored, particularly for selected and indicated prevention, interventions for depression, suicide, relapse prevention, etc. ( 79 ). Therefore, more research in this area is warranted.
To be more clinically relevant, greater biological research in MH prevention is required to identify those at higher risk of developing given mental disorders due to the existing risk factors/prominent stress ( 110 ). For instance, researchers have utilized the transcriptional approach to identify a biological fingerprint for susceptibility (denoting abnormal early stress response) to develop post-traumatic stress disorders among the psychological trauma survivors by analyzing the expression of the Peripheral blood mononuclear cell gene expression profiles ( 111 ). Identifying such biological markers would help target at-risk individuals through tailored and intensive interventions as a form of selected prevention.
Similarly, such novel interventions can help in targeting the underlying risk such as substance use, poor stress management, family history, personality traits, etc. and protective factors, e.g., positive coping techniques, social support, resilience, etc., that influences the given MH outcome ( 79 ). Therefore, again, it opens the scope of tailored interventions rather than a one-size-fits-all model of selective and indicated prevention for various MH conditions.
Furthermore, such interventions can be more accessible for the hard-to-reach populations and those with significant mental health stigma. Finally, they play a huge role in ensuring the continuity of care, particularly when community-based MH services are either limited or not available. For instance, IMIs can maintain the improvement of symptoms among individuals previously managed in-patient, such as for suicide, SUDs, etc., or receive intensive treatment like cognitive behavior therapy (CBT) for depression or anxiety, thereby helping relapse prevention ( 86 , 112 ). Hence, such modules need to be developed and tested in low-resource settings.
IMIs (and other novel interventions) being less stigmatizing and easily accessible, provide a platform to engage individuals with chronic medical problems, e.g., epilepsy, cancer, cardiovascular diseases, etc., and non-mental health professionals, thereby making it more relevant and appealing for them.
Lastly, research on prevention-interventions needs to be more robust to adjust for the pre-intervention matching, high attrition rate, studying the characteristics of treatment completers vs. dropouts, and utilizing the intention-to-treat analysis to gauge the effect of such novel interventions ( 78 ).
Recommendations for Low-and-Middle-Income Countries
Although there is growing research on the effectiveness and utility of mental health promotion/prevention interventions across the lifespan and settings, low-resource settings suffer from specific limitations that restrict the full realization of such public health strategies, including implementing the novel intervention. To overcome these challenges, some of the potential solutions/recommendations are as follows:
- The mental health literacy of the population should be enhanced through information, education, and communication (IEC) activities. In addition, these activities should reduce stigma related to mental problems, early identification, and help-seeking for mental health-related issues.
- Involving teachers, workplace managers, community leaders, non-mental health professionals, and allied health staff in mental health promotion and prevention is crucial.
- Mental health concepts and related promotion and prevention should be incorporated into the education curriculum, particularly at the medical undergraduate level.
- Training non-specialists such as community health workers on mental health-related issues across an individual's life course and intervening would be an effective strategy.
- Collaborating with specialists from other disciplines, including complementary and alternative medicines, would be crucial. A provision of an integrated health system would help in increasing awareness, early identification, and prompt intervention for at-risk individuals.
- Low-resource settings need to develop mental health promotion interventions such as community-and school-based interventions, as these would be more culturally relevant, acceptable, and scalable.
- Utilizing a digital platform for scaling mental health services (e.g., telepsychiatry services to at-risk populations) and training the key individuals in the community would be a cost-effective framework that must be explored.
- Infusion of higher financial and human resources in this area would be a critical step, as, without adequate resources, research, service development, and implementation would be challenging.
- It would also be helpful to identify vulnerable populations and intervene in them to prevent the development of clinical psychiatric disorders.
- Lastly, involving individuals with lived experiences at the level of mental health planning, intervention development, and delivery would be cost-effective.
Clinicians, researchers, public health experts, and policymakers have increasingly realized mental health promotion and prevention. Investment in Preventive psychiatry appears to be essential considering the substantial burden of mental and neurological disorders and the significant treatment gap. Literature suggests that MH promotive and preventive interventions are feasible and effective across the lifespan and settings. Moreover, various novel interventions (e.g., internet-and mobile-based interventions, new therapies) have been developed worldwide and proven effective for mental health promotion and prevention; such interventions are limited mainly to HICs.
Despite the significance of preventive psychiatry in the current world and having a wide-ranging implication for the wellbeing of society and individuals, including those suffering from chronic medical problems, it is a poorly utilized public health field to address the population's mental health needs. Lately, researchers and policymakers have realized the untapped potentialities of preventive psychiatry. However, its implementation in low-resource settings is still in infancy and marred by several challenges. The utilization of novel interventions, such as digital-based interventions, and blended and stepped-care models of care, can address the enormous mental health need of the population. Additionally, it provides mental health services in a less-stigmatizing and easily accessible, and flexible manner. More research concerning this is required from the LMICs.
Author Contributions
VS, AK, and SG: methodology, literature search, manuscript preparation, and manuscript review. All authors contributed to the article and approved the submitted version.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2022.898009/full#supplementary-material
- Open access
- Published: 28 January 2021
Evidence for implementation of interventions to promote mental health in the workplace: a systematic scoping review protocol
- Charlotte Paterson ORCID: orcid.org/0000-0001-6796-227X 1 ,
- Caleb Leduc 2 , 3 ,
- Margaret Maxwell 1 ,
- Birgit Aust 4 ,
- Benedikt L. Amann 5 ,
- Arlinda Cerga-Pashoja 6 ,
- Evelien Coppens 7 ,
- Chrisje Couwenbergh 8 ,
- Cliodhna O’Connor 2 , 3 ,
- Ella Arensman 2 , 3 , 9 , 10 &
- Birgit A. Greiner 2
Systematic Reviews volume 10 , Article number: 41 ( 2021 ) Cite this article
12k Accesses
15 Citations
14 Altmetric
Metrics details
Mental health problems are common in the working population and represent a growing concern internationally, with potential impacts on workers, organisations, workplace health and compensation authorities, labour markets and social policies. Workplace interventions that create workplaces supportive of mental health, promote mental health awareness, destigmatise mental illness and support those with mental disorders are likely to improve health and economical outcomes for employees and organisations. Identifying factors associated with successful implementation of these interventions can improve intervention quality and evaluation, and facilitate the uptake and expansion. Therefore, we aim to review research reporting on the implementation of mental health promotion interventions delivered in workplace settings, in order to increase understanding of factors influencing successful delivery.
Methods and analysis
A scoping review will be conducted incorporating a stepwise methodology to identify relevant literature reviews, primary research and grey literature. This review is registered with Research Registry (reviewregistry897). One reviewer will conduct the search to identify English language studies in the following electronic databases from 2008 through to July 1, 2020: Scopus, PROSPERO, Health Technology Assessments, PubMed, Campbell Collaboration, Joanna Briggs Library, PsycINFO, Web of Science Core Collection, CINAHL and Institute of Occupational Safety and Health (IOSH). Reference searching, Google Scholar, Grey Matters, IOSH and expert contacts will be used to identify grey literature. Two reviewers will screen title and abstracts, aiming for 95% agreement, and then independently screen full texts for inclusion. Two reviewers will assess methodological quality of included studies using the Mixed Methods Appraisal Tool and extract and synthesize data in line with the RE-AIM framework, Nielson and Randall’s model of organisational-level interventions and Moore’s sustainability criteria, if the data allows. We will recruit and consult with international experts in the field to ensure engagement, reach and relevance of the main findings.
This will be the first systematic scoping review to identify and synthesise evidence of barriers and facilitators to implementing mental health promotion interventions in workplace settings. Our results will inform future evaluation studies and randomised controlled trials and highlight gaps in the evidence base.
Systematic review registration
Research Registry ( reviewregistry897 )
Peer Review reports
Mental health problems are common in the working population and represent a growing concern, with potential impacts on workers’ wellbeing, health and discrimination; organisations through lost productivity; workplace health and compensation authorities due to growing job stress-related claims; and social welfare systems owing to increased working age disability pensions for mental disorders [ 1 ]. Mental health refers to ‘a state of wellbeing in which the individual realizes his or her own abilities, can cope with normal stresses of life, can work productively and fruitfully, and is able to make a contribution to his or her community’ [ 2 ]. Mental health problems therefore include daily worries, stress, burnout and poor wellbeing, as well as mental health conditions such as depression or anxiety [ 3 ]. Psychosocial stresses in the workplace, such as job uncertainty, low job control, poor management, harassment and bullying, poor communication and long hours, have been shown to undermine mental wellbeing [ 4 ]. A negative working environment may lead to physical and mental health problems, harmful use of substances or alcohol, absenteeism, presenteeism and lost productivity [ 5 ]. Although it is acknowledged that mental health problems exist in the workplace, stigma and the social exclusion of people with mental health problems may be leading to under-recognition of such problems and the subsequent low treatment rate of mental health problems [ 6 , 7 , 8 ]. Under-treatment has been shown to increase the indirect cost of mental disorders, physical morbidity and mortality [ 9 , 10 ].
Several studies have evaluated workplace interventions targeting mental wellbeing [ 11 ]. Workplace interventions that support mental health and wellbeing have been shown to help reduce sickness absence [ 12 ]. In addition, workplaces that promote mental health awareness, destigmatise mental illness and support people with mental disorders are more likely to reduce levels of depression and absenteeism while increasing productivity as well as benefiting from associated economic gains [ 13 ]. Improving access to evidence-based interventions for minor stress-related depressive symptoms in occupational sectors associated with high suicide rates, e.g. construction, healthcare and information communication and technology (ICT), is likely to prevent the development of severe depressive disorders and comorbidities, and subsequent suicidal behaviour [ 13 ].
Although high-quality evaluations underpin evidence-based interventions (EBI), implementation research can improve the quality of such evaluations and facilitate the uptake and reach of EBIs and other research findings into practice [ 14 ]. One effective way to do this is to identify factors that influence the delivery and uptake of interventions during development, feasibility, evaluation and implementation stages [ 15 ].
So far, research into specific mechanisms and process factors associated with the successful delivery of mental health promotion interventions in the workplace is limited [ 16 , 17 ]. This review aims to identify and analyse research on the implementation of workplace mental health promotion interventions; specifically, to understand the barriers and facilitators that influence their delivery in order to provide insights and inform future intervention, evaluation and implementation efforts. This work represents a direct response to recent calls within intervention research to examine the mechanisms through which interventions bring about change and the documentation of contextual and procedural considerations that either facilitate or limit implementation [ 16 , 17 ].
Aims and objectives
This review is part of a wider project intending to develop, evaluate and implement a multi-level intervention (Mental Health Promotion and Intervention in Occupational Settings, MENTUPP) [ 18 ], which aims to improve mental health and wellbeing in the workplace involving 15 European and Australian partners, with a particular focus on small to medium sized enterprises (SMEs) in three sectors with high prevalence rates of mental health problems and suicidal behaviour, namely ICT, healthcare and construction sectors. More broadly, the purpose of this review is to collate and critically appraise workplace mental health intervention implementation literature to understand how and why certain interventions are more effectively implemented than others and inform MENTUPP and future programmes. The objectives of the review are to:
1. Systematically identify and document research explicitly reporting on the quality of delivery and implementation of mental health promotion interventions in workplaces (e.g. reporting the quality of implementation, a process evaluation or realist evaluation) and, if the evidence allows, specifically in ICT, construction and healthcare settings and SMEs.
2. Identify the barriers and facilitators associated with the quality of implementation of mental health promotion interventions in workplace settings and, if the evidence allows, specifically in ICT, construction or healthcare settings and within SMEs, as it relates to the MENTUPP programme of work.
Based on these objectives, our research questions are:
What is the scope of research with explicit analysis of implementation aspects of mental health promotion interventions in the workplace?
What are the barriers and facilitators to implementing mental health promotion interventions in the workplace?
What are the barriers and facilitators to implementing mental health promotion interventions in SMEs and in the ICT, construction and healthcare sectors?
Methods/design
Study design.
We will conduct a systematic scoping review using the 6-stage scoping review framework [ 19 , 20 ] to systematically identify the implementation evidence and factors associated with successful implementation of mental health promotion in workplace settings. Scoping reviews aim to map a broad field of literature and to summarise and disseminate research findings [ 19 , 21 ], rather than address very focussed questions. This approach is in line with the aims of this review, given the wide range of potential successful and failed interventions, contexts and implementation factors. We will comprehensively explore the relevant research, using iterative methods to develop a rigorous and systematic search of the existing literature [ 20 ]. We will recruit and consult with international experts in the field according to both applied organisational and research experience at key stages of the review process and subsequently to ensure engagement, reach and relevance of the process and main findings. The active involvement of people affected by a research topic has been argued to be beneficial to the quality, relevance and impact of research [ 22 , 23 ], and it enhances the perceived usefulness of systematic review evidence and addresses barriers to the uptake of synthesised research evidence [ 24 , 25 ].
Our protocol was developed using the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) Protocol checklist (PRISMA-P) [ 26 ] (see Additional file 1 ). The present protocol has been registered within the Research Registry (reviewregistry897). The results of our scoping review will be reported in accordance with PRISMA-ScR [ 27 ].
Operationally, the current review will systematically conduct the searches based on the following definition of key terms :
● Implementation : The results of this review will inform the design of a feasibility and definitive trial of mental health promotion in the workplace. As such, implementation refers to interventions being delivered at feasibility and piloting, evaluation and implementation stages of the Medical Research Council (MRC) framework (15).
● Mental health promotion refers to interventions or programmes that aim to treat (intervene to improve mental health), prevent (inhibit the escalation of subclinical symptoms to clinical severity or prevent the onset of mental health problems) and promote (improve mental health by targeting positive components of mental health) mental health and wellbeing [ 28 ].
● Barriers are defined as any variable or condition that impedes the implementation or delivery of mental health promotion interventions.
● Facilitators are defined as any variable or condition that facilitates or improves the implementation or delivery of mental health promotion interventions.
● Workplace settings include any organisation operating with paid employees. Therefore, mental health promotion interventions must be delivered through, or be associated with, the workplace. Sector-specific definitions from the European Commission were used [ 29 ]. The ICT sector will include telecommunications activities, information technology activities and other information service activities (divisions 61–63); the healthcare sector will include healthcare provided by medical professionals in hospitals or other facilities and residential activities, but not social work activities (divisions 86–87); and the construction sector will include construction of buildings, civil engineering and specialised construction activities (divisions 41–43). Small- to medium-sized enterprises include those employing < 250 employees [ 30 ].
Information sources and search strategy
We will use iterative methods to develop and apply a rigorous and comprehensive search strategy, combining a series of free text terms and Medical Subject Headings (MeSH) terms for key concepts: (a) workplace AND (b) mental health, AND (c) interventions, AND (d) implementation. A preliminary search strategy (see Additional file 2 ) has been developed for PsycINFO, using established search terms (from Cochrane and other previous search strategies [ 31 , 32 , 33 ], peer-reviewed in accordance with PRESS guidelines [ 34 ]. Boolean operators will be used to maximise the penetration of terms searched, and appropriate “wild cards” will be employed to account for plurals, variations in databases, and spelling.
We will use a stepwise methodology [ 35 ] to identify the highest quality evidence in a systematic way and capture grey literature. Grey literature will be included because it is likely that due to publication bias some unsuccessful interventions have not been published in peer-reviewed journals. A number of contingency plans have been built into the methods to allow an iterative approach to the search and selection of evidence for the review (Additional file 3 ). We will use established search terms and adapt searches for each of the following major electronic databases outlined below.
In step 1, we will search the following electronic databases for systematic reviews:
● Health Technology Assessments
● Campbell Collaboration
● Joanna Briggs Library
● Web of Science Core Collection
In step 2, we will look for primary studies reporting implementation of mental health promotion interventions in the following electronic databases:
● PsychINFO
● Institute of Occupational Safety and Health (IOSH) research database.
Step 3 will involve supplementary searches involving a thorough review of relevant study references, grey literature and personal contacts using a systematic approach (Additional file 3 ). This will include searching:
● Reference searching : relevant studies included in published guidelines, relevant systematic reviews and listed in the included studies’ reference lists and bibliographies.
● Grey literature : Google Scholar (25 pages relevant), Grey Matters and the Institute of Occupational Safety and Health (IOSH) research database.
● Personal contacts : we will contact international experts and authors of papers reporting trials (from 2008) on workplace interventions to address mental health promotion.
Criteria for considering studies for inclusion
The scoping review will address factors associated with successful implementation and therefore focus primarily on feasibility and process studies or realist evaluations. Although we will look at the relation between implementation and effects, the main aim of the review is to identify factors associated with implementation, specifically barriers and facilitators. The focus of this review will be cognisant of outcomes indicating successful implementation, including programme uptake, retention and impact.
Study designs
We will include any paper, regardless of study design, using either quantitative, qualitative or mixed-methods, which explicitly investigates, reports or discusses, in the title or abstract, any aspect of implementation of specific mental health promotion interventions (i.e. quality of implementation, a process evaluation including rich data or a realist evaluation) delivered in the workplace. This includes literature reviews (systematic reviews, scoping reviews, meta-analyses) and primary research studies published either in the peer-reviewed scientific literature or in the grey literature. We will exclude opinion pieces, commentaries, website discussions, blogs and magazine and newspaper articles.
We will include studies with adult participants (aged 16–65) who are in formal employment, including those on sickness absence leave and are expected to return to work.
Interventions
Interventions, whose implementation is of interest, are purposefully applied strategies delivered in the workplace, targeting either workers, supervisors, managers, occupational health professionals, owners/executives or entire organisations. Included interventions will aim to (i) help protect mental health by reducing work-related risk factors (e.g. job strain, poor working conditions and job stressors such as job insecurity, psychological harassment (e.g. due to stigma), low social support at work, organisational injustice, and effort-reward imbalance); (ii) promote workplace mental health wellbeing by creating positive aspects of work, and develop employees’ strengths (e.g. satisfaction, wellbeing, psychological capital, positive mental health, resilience and positive organisational attributes such as authentic leadership, supportive workplace culture and workplace social capital); and (iii) respond to mental health problems when they occur (e.g. interventions targeting burnout, stress, anxiety, depression or return to work) [ 36 ]. We will exclude studies that evaluate the implementation of general mental health interventions that are not specifically associated with workplace factors or delivered in work contexts (e.g. healthy eating or exercise at home), mental health interventions that are not formally implemented in the workplace (e.g. online work-related mental health interventions freely available online without association to an organisation) and one-off events (e.g. distribution of mental health educational material or one-off information sessions through guest lecturers). Interventions not directly targeting psychological wellbeing or mental health will be included if the primary outcome is related to psychological wellbeing or mental health (e.g. a physical activity programmes delivered in the workplace with a primary outcome for improving mental health). Interventions that target a wide range of health and wellbeing outcomes, e.g. physical activity, obesity, smoking cessation and stress, will be excluded.
Outcomes of interest
We will only include studies reporting rich data on any implementation outcomes and will categorise outcomes within our data charting. We anticipate that identified outcomes may include fidelity, reach, dose delivered, dose received, adoption, penetration, feasibility, acceptability, context factors, process factors, sustainability factors, programme theories, theories of change and failure theories. We will exclude studies focusing on only the impact of interventions on disease end points, i.e. which do not evaluate implementation quality.
Types of settings
We will include studies conducted in any geographical location, and we will categorise the location based on relevance to Europe and Australia during data charting. The intervention must be delivered in, or in association with, a workplace setting and be implemented in the work schedule, work systems or administrative structures.
Studies published in English will be included in steps 1 and 2. Studies published in English, French and German will be included in step 3.
Publication date
Studies published in the last 13 years will be included. The World Health Organization’s (WHO) Global Plan of Action on Work’s Health (2008–2017) [ 37 ] and the Mental Health Action Plan (2013–2020) [ 38 ] highlight the importance of promoting good mental health in the workplace. Furthermore, the field of implementation science is fairly new; therefore, literature published after 2008 is deemed to be most relevant to this review.
Study selection
Rayyan will be used for the study selection process [ 39 ]. Two reviewers will be utilised for a provisional screening of all titles (CP, CL), removing any clearly irrelevant papers. To ensure reliability between reviewers, 15% of the study titles will be reviewed blindly by both reviewers independently, aiming for 95% agreement. Where 95% agreement is not reached, a further 15% will be reviewed by both reviewers independently. Any discrepancy between reviewers will be discussed and, if necessary, will involve a third reviewer to resolve. The remaining study titles will be screened for abstract review by a single reviewer. Two reviewers will then be involved in screening the remaining potential abstracts (CP, CL) and rate them as relevant, irrelevant or unsure. To ensure consistency between reviewers, 15% will be checked independently, and where agreement does not reach 95%, a further 15% will be reviewed by both reviewers. Studies that are ranked as irrelevant will be excluded. We will obtain the full papers for the remaining studies. Two reviewers (CP, CL) will then independently assess each of these against the selection criteria. We will resolve any disagreement through discussion and will involve a third independent reviewer if needed.
Charting the data
Data extraction.
We will pilot a data extraction template on the first four included studies and amend as required. We will extract key study details (e.g. study design, country, sample size, sector, intervention characteristics, impact on primary outcome, etc.) and implementation data (e.g. direct quotes, page numbers) will be structured using an adapted version of the RE-AIM framework [ 40 ] which has been complemented using selected categories from Nielson and Randall’s model of organisational-level interventions [ 16 ] and Moore’s sustainability criteria [ 41 ]. To ensure reliability, data from 15% of included papers will be coded by two reviewers (CP and CL) independently. Any ambiguity identified will be resolved through discussion with other members of the review team. Study authors will be contacted via email where data are missing or unclearly reported.
Data coding
Data will be coded as follows:
● Stage of intervention development/evaluation will be coded according to the MRC framework (i.e. feasibility, evaluation or implementation) [ 15 ].
● Countries will be coded using the World Bank classification [ 42 ] to identify countries of relevance to future research, e.g. Europe and Australia.
● Implementation evidence will be mapped using a modified version of the RE-AIM framework [ 40 ], which is organised into five categories: reach, effectiveness, adoption, implementation and maintenance. This framework also allows evaluation of implementation at an individual and organisational level.
● Nielson and Randall’s model of organisational-level interventions [ 16 ] will supplement the RE-AIM framework for this review allowing for extraction based on the intervention itself, the context in which it was delivered and participants’ mental models.
● Intervention sustainability will be coded using Moore’s definitions of sustainability [ 41 ], e.g. continued delivery, behaviour change, evolution/adaptation and continued benefits.
Quality appraisal
In line with previous systematic and scoping reviews that include mixed methods literature [ 32 , 43 ], the methodological quality of included studies will be assessed using the Mixed Methods Appraisal Tool (MMAT) [ 44 ] for quantitative, qualitative and mixed methods research designs. Each study will receive a methodological rating between 0 and 100 (with 100 being the highest quality), based on the evaluation of study selection bias, study design, data collection methods, sample size, intervention integrity and analysis. Where studies integrate the process evaluation into the study design, the quality of the entire study will be assessed. Methodological quality will be rated by two reviewers (CL and CP). To ensure consistency between reviewers, 15% will be rated independently, and if agreement is reached, one reviewer will rate the remaining papers. Any ambiguity identified will be resolved through discussion with other members of the review team.
Collating, summarising and reporting
Descriptive characteristics of included studies will be tabulated and brought together using a narrative synthesis. To answer question one, we will summarise the type of evidence relating to the implementation of the interventions in workplace settings. To answer questions two and three, barriers and facilitators will be categorised according to the RE-AIM framework [ 40 ], modified using Nielson & Randall’s (2013) model for evaluation organisational-level interventions [ 16 ] and Moore’s sustainability criteria [ 45 ]. We will present tabulated data by sector and then occupational level (i.e. organisational, managerial, etc.) and intervention type. If the evidence allows, to further answer research question three, we will present tabulated data from included studies focusing specifically on SMEs using the same format. Key findings will be brought together within a narrative synthesis [ 46 , 47 ].
The aim of this systematic scoping review is to identify research that reports on the feasibility and implementation of mental health promotion interventions that are delivered in workplace settings, and to specifically understand the factors (barriers and facilitators) that influence the successful delivery of mental health promotion interventions in the workplace. This review is part of the MENTUPP project [ 18 ] which aims to develop, evaluate and implement mental health promotion interventions for the workplace, particularly in SMEs in the construction, healthcare and ICT sectors. As such, our review will aim to focus on intervention implementation barriers and facilitators in SMEs and in the construction, healthcare and ICT sectors. This work addresses recent calls within intervention research to examine the mechanisms through which interventions bring about change and the documentation of contextual and procedural considerations that either facilitate or limit implementation [ 16 , 17 ]. Additionally, this timely review responds to international policy regarding mental health in the workplace [ 8 ]. In an effort to maintain quality and identify all relevant information, we have presented a rigorous and systematic approach to this scoping review. We have maintained a broad search strategy in order to capture the variety of implementation research that may be available, and we will consult with stakeholders to ensure the main findings are useful and relevant. The results of this review will identify barriers and facilitators to implementation of mental health promotion interventions in the workplace and inform future pilot and definitive RCTs within the MENTUPP project [ 18 ]. This will help inform future interventions, and the evaluation and implementation efforts of such interventions, which will subsequently improve outcomes for employees and organisations through improved mental wellbeing; reduced symptoms of depression, anxiety and stress; and reduced presenteeism and absenteeism. In addition, this review will contribute to implementation science related to workplace mental health promotion.
Availability of data and materials
All data generated or analysed during this study will be included in the published scoping review article and will be available by request to the corresponding author.
Abbreviations
Information and communication technology
Institution of occupational safety and health
Medical research council
Medical subject heading
Mixed methods appraisal tool
Preferred reporting items for systematic reviews and meta-analyses
Preferred reporting items for systematic reviews and meta-analyses extension for scoping reviews
Randomized controlled trial
Reach, effectiveness, adoption, implementation and maintenance
Small-to-medium sized enterprises
World health Organization
Publications Office of the European Union. 5th European Working Conditions Survey [Internet]. Quality Assurance Report, 2010 http://www.eurofound.europa.eu/surveys/ewcs/2010/documents/qualassurance.pdf .[cited 2020 May 7]. Available from: www.eurofound.europa.eu .
WHO. Mental health: strengthening our response [Internet]. Fact sheet N°220. 2010 [cited 2020 Jul 27]. Available from: https://www.who.int/news-room/fact-sheets/detail/mental-health-strengthening-our-response .
MentalHealthFoundation.org [Internet]. United Kingdom: Mental Health Foundation; [cited 2020 Jul 27]. Available from: https://www.mentalhealth.org.uk/your-mental-health/about-mental-health/what-are-mental-health-problems .
Virtanen M. Psychosocial job stressors and suicidality: can stress at work lead to suicide? Occup Environ Med. [Internet] 2018;75(4):243–4. Available from: https://doi.org/10.1136/oemed-2017-104689 . [cited 2020 July 27].
World Health Organisation. Addressing comorbidity between mental disorders and major noncommunicable diseases [Internet]. 2017 [cited 2020 May 7]. Available from: http://www.euro.who.int/pubrequest .
Brohan E, Thornicroft G. Stigma and discrimination of mental health problems workplace implications. Occup Med. [Internet] 2010;60(6):414–5. Available from: https://doi.org/10.1093/occmed/kqq048 . [cited 2020 July 27].
Mental Health Foundation Scotland. Mental Health in the Workplace Seminar Report. 2018.
WHO. Mental health in the workplace [Internet]. WHO. World Health Organization; 2019 [cited 2020 Jul 27]. Available from: http://www.who.int/mental_health/in_the_workplace/en/ .
Rugulies R, Aust B, Madsen IEH. Effort–reward imbalance at work and risk of depressive disorders. A systematic review and meta-analysis of prospective cohort studies. Scand J Work Environ Health. 2017;43:294–306.
Theorell T, Hammarström A, Aronsson G, Träskman Bendz L, Grape T, Hogstedt C, et al. A systematic review including meta-analysis of work environment and depressive symptoms [Internet]. Vol. 15, BMC Public Health; 2015. p. 738. [cited 2020 May 7] Available from: http://bmcpublichealth.biomedcentral.com/articles/ https://doi.org/10.1186/s12889-015-1954-4 .
Graveling R, Crawford J, Cowrie H, Amati C, Vohra S. A review of workplace interventions that promote mental wellbeing in the workplace [Internet]. 2008. Available from: https://www.researchgate.net/publication/239615077_A_Review_of_Workplace_Interventions_that_Promote_Mental_Wellbeing_in_the_Workplace .
Milner A, Hjelmeland H, Arensman E, De LD. Social-environmental factors and suicide mortality: a narrative review of over 200 articles. Sociol Mind. 2013;03(02):137–48 [cited 2020 May 7] Available from: http://www.scirp.org/journal/sm .
Article Google Scholar
Milner A, Maheen H, Currier D, LaMontagne AD. Male suicide among construction workers in Australia: a qualitative analysis of the major stressors precipitating death. BMC Public Health. 2017;17(1):584 [cited 2020 May 7] Available from: http://bmcpublichealth.biomedcentral.com/articles/10.1186/s12889-017-4500-8 .
Wensing M. Implementation science in healthcare: introduction and perspective. Z Evid Fortbild Qual Gesundhwes. 2015;109(2):97–102. [cited 2017 Aug 2] Available from: http://dx.doi.org/ https://doi.org/10.1016/j.zefq.2015.02.014 .
Craig P, Dieppe P, Macintyre S, Michie S, Nazareth I, Petticrew M, et al. Developing and evaluating complex interventions: the new Medical Research Council guidance. Br Med J (Clin Res Ed). 2008;337(7262):a1655 [cited 2017 May 12] Available from: http://www.bmj.com/content/bmj/337/bmj.a1655.full.pdf .
Google Scholar
Nielsen K, Randall R. Opening the black box: presenting a model for evaluating organizational-level interventions. Eur J Work Organ Psychol. 2013;22(5):601–17.
Nielsen K, Abildgaard JS. Organizational interventions: a research-based framework for the evaluation of both process and effects. Work Stress. 2013;27(3):278–297. [cited 2020 Jul 3] Available from: http://dx.doi.org/ https://doi.org/10.1080/02678373.2013.812358 .
MENTUPPproject.eu [Internet]. Ireland; [updated 2020 January; cited 2020 May 7]. Available from: https://www.mentuppproject.eu/ .
Arksey H, Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005;8:19–32 [cited 2020 Feb 13] Available from: http://journalsonline.tandf.co.uk/OpenURLlinktothearticle:http://www.journalsonline.tandf.co.uk/openurl.asp?genre=article&eissn=1464-5300&volume=8&issue=1&spage=19.
Levac D, Colquhoun H, O’Brien KK. Scoping studies: advancing the methodology. Implement Sci. 2010;5(1) [cited 2020 Feb 13] Available from: http://www.cihr-irsc.ca .
Munn Z, Peters MDJ, Stern C, Tufanaru C, McArthur A, Aromataris E. Systematic review or scoping review? Guidance for authors when choosing between a systematic or scoping review approach. BMC Med Res Methodol. 2018;18(1):1–7.
Kreis J, Puhan MA, Schünemann HJ, Dickersin K. Consumer involvement in systematic reviews of comparative effectiveness research. Heal Expect. 2013;16(4):323–337. [cited 2020 May 7] Available from: https://onlinelibrary.wiley.com/doi/abs/ https://doi.org/10.1111/j.1369-7625.2011.00722.x .
INVOLVE. Public involvement in systematic reviews: Supplement to the briefing notes for researchers [Internet]. 2012 [cited 2020 May 7]. Available from: www.invo.org.uk/resource-centre/ .
Wallace J, Nwosu B, Clarke M. Barriers to the uptake of evidence from systematic reviews and meta-analyses: a systematic review of decision makers’ perceptions. BMJ Open. 2012;2(5):e001220.
Pollock A, Campbell P, Baer G, Choo PL, Morris J, Forster A. User involvement in a Cochrane systematic review: using structured methods to enhance the clinical relevance, usefulness and usability of a systematic review update. Syst Rev. 2015;4(1):1–11.
Moher D, Shamseer L, Clarke M, Ghersi D, Liberatî A, Petticrew M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement [Internet]. 2015 [cited 2020 May 7]. Available from: http://www.crd.york.ac.uk/prospero .
Tricco AC, Lillie E, Zarin W, O’Brien KK, Colquhoun H, Levac D, et al. PRISMA extension for scoping reviews (PRISMA-ScR): Checklist and explanation. Ann Intern Med. 2018;169:467–73.
WHO. Prevention and promotion in mental health. [Internet] Geneva; 2002. [2020 July 27]. Available from: https://www.who.int/mental_health/media/en/545.pdf .
European Commission. NACE Rev. 2 – Statistical classification of economic activites in the European Community. 2nd ed. [Internet]. 2008. [cited 2020 July 27]. Available from: https://ec.europa.eu/eurostat/documents/3859598/5902521/KS-RA-07-015-EN.PDF .
European Commission. User guide to the SME definition [Internet]. 2015. Available from: http://ec.europa.eu/growth/index_en.htm%5Cnhttp://scholar.google.com/scholar?hl=en&btnG=Search&q=intitle:BOOKLET+OF+STANDARDIZED+SMALL+AND+MEDIUM+ENTERPRISES+BOOKLET+OF+DEFINITION-2007#0.
Garne-Dalgaard A, Mann S, Bredahl TVG, Stochkendahl MJ. Implementation strategies, and barriers and facilitators for implementation of physical activity at work: a scoping review [Internet]. Vol. 27, Chiropr Man Ther. 2019 [cited 2020 Apr 2]. Available from: https://doi.org/10.1186/s12998-019-0268-5 .
Scott SD, Rotter T, Flynn R, Brooks HM, Plesuk T, Bannar-Martin KH, et al. Systematic review of the use of process evaluations in knowledge translation research. Syst Rev. 2019;8(1):1–10.
Uphoff E, Purgato M, Churchill R, Barbui C. An overview of systematic reviews on mental health promotion, prevention, and treatment of common mental disorders for refugees, asylum seekers, and internally displaced persons. Cochrane Database Syst Rev. [Internet] 2019. [cited 2020 July 27]. Available from: https://doi.org/10.1002/14651858.CD013458.pub2 .
Mcgowan J, Sampson M, Salzwedel DM, Cogo E, Foerster V, Lefebvre C. PRESS peer review of electronic search strategies: 2015 guideline strategies: 2015 guideline statement. JClin Epidemool. 2016;75:40–6.
Jepson R, Macgillivray S, Platt S. A review of the effectiveness of interventions, approaches and models at individual, community and population level that are aimed at changing health outcomes through changing knowledge attitudes and behaviour [Internet]. 2007 [cited 2020 May 7]. Available from: https://www.nice.org.uk/guidance/ph6/evidence/behaviour-change-review-1-effectiveness-review2 .
AD LM, Martin A, Page KM, Reavley NJ, Noblet AJ, Milner AJ, et al. Workplace mental health: developing an integrated intervention approach. BMC Psychiatry. 2014;14(1) [cited 2020 Feb 13] Available from: http://www.biomedcentral.com/1471-244X/14/131 .
World Health Organization. Workers’ health: global plan of action (2008-2017) [Internet]. 2008 [cited 2020 May 7]. Available from: https://www.who.int/occupational_health/who_workers_health_web.pdf .
World Health Organisation. Mental Health Action Plan 2013-2020 [Internet]. 2013 [cited 2020 May 7]. Available from: https://apps.who.int/iris/bitstream/handle/10665/89966/9789241506021_eng.pdf?sequence = 1.
Ouzzani M, Hammady H, Fedorowicz Z, Elamagarmid A. Rayyan - a web and mobile app for systematic reviews. Syst Rev. 2016;5:210.
Glasgow RE, Harden SM, Gaglio B, Rabin B, Smith ML, Porter GC, et al. RE-AIM planning and evaluation framework: Adapting to new science and practice with a 20-year review. Front Public Heal. [Internet] 2019;7(64). Available from: https://doi.org/10.3389/fpubh.2019.00064 . [cited 2020 July 27].
Moore JE, Mascarenhas A, Bain J, Straus SE. Developing a comprehensive definition of sustainability. Implement Sci. 2017;12(1).
World Bank. How does the World Bank classify countries? – World Bank Data Help Desk [Internet]. 2016 [cited 2020 May 7]. Available from: https://datahelpdesk.worldbank.org/knowledgebase/articles/378834-how-does-the-world-bank-classify-countries .
Mulqueeny DM, Nkabini SM, Mashamba-Thompson TP. School-going transgender youths’ experiences at health care facilities: a systematic scoping review protocol. Syst Rev. 2020;9(1). [cited 2020 Jun 30] Available from: https://doi.org/ https://doi.org/10.1186/s13643-020-01347-0 .
Pace R, Pluye P, Bartlett G, Macaulay AC, Salsberg J, Jagosh J, et al. Testing the reliability and efficiency of the pilot Mixed Methods Appraisal Tool (MMAT) for systematic mixed studies review. Int J Nurs Stud 2012;49(1):47–53. Available from: http://dx.doi.org/ https://doi.org/10.1016/j.ijnurstu.2011.07.002 .
Moore GF, Audrey S, Barker M, Bond L, Bonell C, Hardeman W, et al. Process evaluation of complex interventions: medical research council guidance. BMJ. 2015;350(6):h1258 Available from: http://www.bmj.com/content/bmj/350/bmj.h1258.full.pdf . [cited 2020 July 27].
Snilstveit B, Oliver S, Vojtkova M. Narrative approaches to systematic review and synthesis of evidence for international development policy and practice. J Dev Eff. 2012;4(3):409–29.
Popay J, Arai L, Britten N. Guidance on the conduct of narrative synthesis in systematic reviews: a product from the ESRC Methods Programme Child “DNAs” and Safeguarding View project A pragmatic evaluation of a family-based intervention for childhood overweight and obesity View project. 2006 [cited 2020 Jul 27]; Available from: https://www.researchgate.net/publication/233866356 .
Download references
Acknowledgements
The authors express their gratitude to Pauline Campbell, Glasgow Caledonian University, for her guidance and support with the search strategy, and to Donna O’Doibhlin, University College Cork, for her agreement to review the final search strategy. The authors would also like to express appreciation to all other MENTUPP partners [ 18 ].
This study is funded by the European Union’s Horizon 2020 research and innovation programme under grant agreement No 848137. The material presented and views expressed here are the responsibility of the author(s) only. The EU Commission takes no responsibility for any use made of the information set out.
Author information
Authors and affiliations.
NMAHP-RU, University of Stirling https://www.nmahp-ru.ac.uk/
Charlotte Paterson & Margaret Maxwell
School of Public Health, University College Cork, Cork, Ireland
Caleb Leduc, Cliodhna O’Connor, Ella Arensman & Birgit A. Greiner
National Suicide Research Foundation, Cork, Ireland
Caleb Leduc, Cliodhna O’Connor & Ella Arensman
National Research Centre for the Working Environment, Copenhagen, Denmark
Birgit Aust
Centro Forum Research Unit, Institut de Neuropsiquiatria i Addicions (INAD), Parc de Salut Mar, Hospital del Mar Medical Research Institute (IMIM), Autonomous University Barcelona, CIBERSAM, Barcelona, Spain
Benedikt L. Amann
London School of Hygiene and Tropical Medicine, London, UK
Arlinda Cerga-Pashoja
Centre for Health Research and Consultancy, Katholieke Universiteit Leuven, Leuven, Belgium
Evelien Coppens
Kenniscentrum Phrenos, Utrecht, Netherlands
Chrisje Couwenbergh
Australian Institute for Research, Griffith University, Mount Gravatt, Australia
Ella Arensman
International Association for Suicide Prevention (IASP), Washington, DC, USA
You can also search for this author in PubMed Google Scholar
Contributions
The protocol was conceptualised, designed, reviewed and approved by all authors. MM and CP contributed to the writing of the protocol. The subsequent study, review of abstracts, full studies and synthesis will be conducted by CP and CL and supported by MM, BG and BA.
Corresponding author
Correspondence to Charlotte Paterson .
Ethics declarations
Ethics approval and consent to participate.
Not applicable.
Consent for publication
Competing interests.
The authors have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1..
PRISMA-P checklist.
Additional file 2.
Draft Search Strategy.
Additional file 3.
Outline of the step-wise review methodology.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Paterson, C., Leduc, C., Maxwell, M. et al. Evidence for implementation of interventions to promote mental health in the workplace: a systematic scoping review protocol. Syst Rev 10 , 41 (2021). https://doi.org/10.1186/s13643-020-01570-9
Download citation
Received : 05 August 2020
Accepted : 21 December 2020
Published : 28 January 2021
DOI : https://doi.org/10.1186/s13643-020-01570-9
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Barriers and facilitators
- Mental health promotion
- Implementation science
- Scoping review
- Organisational interventions
- Workplace interventions
- Process evaluation
- Wellbeing promotion
Systematic Reviews
ISSN: 2046-4053
- Submission enquiries: Access here and click Contact Us
- General enquiries: [email protected]
Change Password
Your password must have 6 characters or more:.
- a lower case character,
- an upper case character,
- a special character
Password Changed Successfully
Your password has been changed
Create your account
Forget yout password.
Enter your email address below and we will send you the reset instructions
If the address matches an existing account you will receive an email with instructions to reset your password
Forgot your Username?
Enter your email address below and we will send you your username
If the address matches an existing account you will receive an email with instructions to retrieve your username

- April 01, 2024 | VOL. 75, NO. 4 CURRENT ISSUE pp.307-398
- March 01, 2024 | VOL. 75, NO. 3 pp.203-304
- February 01, 2024 | VOL. 75, NO. 2 pp.107-201
- January 01, 2024 | VOL. 75, NO. 1 pp.1-71
The American Psychiatric Association (APA) has updated its Privacy Policy and Terms of Use , including with new information specifically addressed to individuals in the European Economic Area. As described in the Privacy Policy and Terms of Use, this website utilizes cookies, including for the purpose of offering an optimal online experience and services tailored to your preferences.
Please read the entire Privacy Policy and Terms of Use. By closing this message, browsing this website, continuing the navigation, or otherwise continuing to use the APA's websites, you confirm that you understand and accept the terms of the Privacy Policy and Terms of Use, including the utilization of cookies.
Mental Illness Prevention and Mental Health Promotion: When, Who, and How
- Michael T. Compton , M.D., M.P.H. , and
- Ruth S. Shim , M.D., M.P.H.
Search for more papers by this author
Classification as primary, secondary, or tertiary prevention is based on when during the course of disease the intervention is provided. Another approach to classification—as universal, selective, or indicated preventive interventions—relates to who receives the intervention. The social determinants of health framework also provides a guide to prevention, which requires changing both public policies and social norms. It also addresses the weaknesses of the first two approaches, such as persistent health inequities regarding who has access to preventive services. The social determinants framework is a guide to providing timely and targeted preventive interventions in a way that ensures equal access.
Many health professionals are familiar with two approaches to classification of disease prevention: classification as primary, secondary, or tertiary prevention and as universal, selective, or indicated preventive interventions.
Alternatively, the social determinants of health framework suggests that prevention requires changing public policies and social norms while focusing on eliminating health inequities.
According to our conceptualization ( 1 – 6 ), the social determinants of mental health are societal problems affecting large segments of the population (individuals, families, communities, and, indirectly, the entire population) that interfere with optimal mental health. These factors increase risk for mental illnesses and substance use disorders, worsen outcomes among those with existing mental illnesses or substance use disorders, and account for the mental health disparities and inequities that exist across population groups. Such determinants include adverse early life experiences; discrimination and the resultant social exclusion; exposure to violence, war, forced migration, and related issues; involvement in the criminal justice system; educational, employment, and financial inequalities; area-level and concentrated neighborhood poverty; poor access to stable housing, high-quality diet, transportation, health care, or health insurance; adverse features of the built environment (e.g., building design, city planning); neighborhood disorder; and exposure to pollution or the effects of climate change.
All of these problems, which are manifestations of social injustice, interfere with health and increase the risk of diseases, medical and psychiatric alike. At the individual level, they adversely affect health and cause disease through at least three mechanisms. First, these problems often result in reduced options for individuals. For example, lack of access to or lack of resources to purchase healthy food often results in reliance on an inexpensive, high-calorie, micronutrient-poor diet replete with processed food, junk food, and fast food. In turn, these poor options from which individuals must choose are behavioral risk factors for diseases and conditions such as obesity, diabetes, hypertension, and depression. Second, they create substantial and persistent stress, thereby triggering psychological and physiological stress responses that increase the risk for disease. Third, they can interact with genetic constitution through such mechanisms as gene-by-environment interactions and epigenetics.
Although the social determinants are relevant to the tertiary prevention work of clinical care, they are also central to health disparities and inequities, and they provide insights into how best to prevent mental illnesses and substance use disorders and promote mental health. Two frameworks are widely known to guide the medical and public health communities in thinking about how to approach prevention. The first provides a how-to guide by focusing on when to provide an intervention; the second focuses on who receives the intervention. A third framework—and our main focus here—provides a pair of upstream, population-based how-to approaches and crucially informs and improves the how-to guides for the first two frameworks.
When: Primary, Secondary, and Tertiary Prevention
The first framework centers on when in the course of a disease the preventive intervention is provided. Primary prevention occurs before any evidence of disease and aims to reduce or eliminate causal risk factors, prevent onset, and thus reduce incidence of the disease. Well-known examples include vaccinations to prevent infectious diseases and encouraging healthy eating and physical activity to prevent obesity, diabetes, hypertension, and other chronic diseases and conditions. Secondary prevention occurs at a latent stage of disease—after a disease has begun but before the person has become symptomatic. The goals, which ultimately reduce the prevalence of the disease, are early identification through screening as well as providing interventions to prevent the disease from becoming manifest. Screening tools and tests (e.g., checking body mass index, mammography, HIV testing) are examples of secondary prevention. Finally, tertiary prevention is an intervention implemented after a disease is established, with the goal of preventing disability, further morbidity, and mortality. Medical treatments delivered during the course of diseases can be considered tertiary prevention. This is the bulk of the work carried out by today’s medical field, including psychiatry. Relapse prevention is another form of tertiary prevention. In psychiatry, primary, secondary, and tertiary prevention are exemplified, respectively, by eliminating certain forms of dementia that stem from vitamin deficiencies, screening for problematic drinking that precedes alcohol use disorder, and providing psychosocial treatments to reduce disability among individuals with serious mental illnesses. One caveat of the when (primary, secondary, tertiary) framework is that it does not inherently address health inequities (e.g., unjust health disparities based on race inequities, socioeconomic status, or geographic location) that occur with regard to not only treatment but also access to primary and secondary prevention.
Who: Universal, Selective, and Indicated Preventive Interventions
The second approach for thinking through prevention largely focuses on who receives an intervention. This framework, popularized by Institute of Medicine reports in recent decades ( 7 , 8 ), also has three levels of prevention (universal, selective, and indicated), divided in terms of who should be given a preventive intervention. Universal preventive interventions are given to the entire group (e.g., a school, an entire community, or the whole population), regardless of individuals’ level of risk for the disease. Examples include fortification or enrichment of foods, school-based curricula about substance abuse, and informational campaigns, such as public service announcements about wearing seat belts or not texting while driving. Selective preventive interventions are those delivered to a subgroup at increased risk for a disease outcome. This category is exemplified by statin use among those with hyperlipidemia (to prevent later cardiovascular disease) and pneumococcal vaccination in older adults. Indicated preventive interventions are those given to an even more select group that is at particularly high risk or is already exhibiting subclinical symptoms. Examples include lifestyle modifications for prediabetes or prehypertension. In psychiatry, universal, selective, and indicated preventive interventions are exemplified, respectively, by social and emotional development curricula provided in elementary schools, group-based psychotherapy for children of parents with depressive disorders, and efforts to identify and treat adolescents and young adults who appear to be at clinical high risk (often termed “ultra-high risk,” although the rate of false positives remains high) for schizophrenia. Similar to the when framework, a weakness of the who framework is that inequities exist in access to these preventive interventions; this framework at times provides a pound of prevention for some groups and only an ounce for others.
How: Pursuing Prevention While Promoting Health Equity
Psychiatry has long been interested in how, as a field, we mental health professionals might pursue the prevention of mental illnesses. Several disciplines (e.g., the field of community psychology), academic and training programs (e.g., the Division of Public Behavioral Health and Justice Policy at the University of Washington), and esteemed researchers (including Sheppard Kellam, a child psychiatrist by training) have established and advanced the field of mental illness prevention. However, despite advances, the prevalence of and disability stemming from mental illnesses indicate that major strides are still needed. In addition to the very useful when (primary, secondary, and tertiary prevention) and who (universal, selective, and indicated preventive interventions) frameworks, the social determinants of health framework guides us on how to go about prevention in at least two ways.
First, reducing the population burden of any of the social determinants (which tend to be highly interconnected) will improve the physical and mental health of the population and will reduce the risk for disease. Given their societal roots (often built into the very structure of society), changing the social determinants of health is no easy task. It requires, in our conceptualization, changing both public policies (e.g., organizational policies, legislation, court decisions) and social norms (i.e., culturally sanctioned ways of interacting with one another on the basis of innate characteristics or social position). Reducing the burden of these social risks on individuals (e.g., in the clinical setting) will have a similar effect, albeit with just one patient at a time. Addressing the social determinants also has an effect on the disease course—in part, by making it easier to be adherent to treatment (and thus having a better response to therapeutic interventions) and by improving one’s ability for disease self-management—which is highly relevant to the tertiary prevention work in which nearly all health care providers engage. Therefore, addressing the social determinants themselves is a means of prevention.
Second, the social determinants of health framework guides practitioners on how to go about prevention because it reminds us that we must work to eliminate inequities (including inequities in access to preventive services and interventions). For the when and the who frameworks to be effective in preventing mental illnesses and substance use disorders, they need to be available to all. Changing public policies and social norms will move us toward realizing the promise of prevention, because those activities are preventive themselves but also because they will help us level the playing field (i.e., eliminate unjust health inequities) so that prevention is a right for everyone. We must ensure that measures are in place to monitor equity in access to all illness prevention and health promotion services. Given the social injustice that leads to the social determinants themselves, we must be wary of inequities not only with regard to treatment but also in all arenas of prevention.
The authors report no financial relationships with commercial interests.
1 Compton MT, Shim RS : The Social Determinants of Mental Health . Washington, DC, American Psychiatric Publishing, 2015 Google Scholar
2 Compton MT, Shim RS : The social determinants of mental health . Focus 2015 ; 13:419–425 Crossref , Google Scholar
3 Shim RS, Compton MT : Addressing the social determinants of mental health: if not now, when? If not us, who? Psychiatr Serv 2018 ; 69:844–846 Link , Google Scholar
4 Shim RS, Compton MT : The social determinants of mental health ; in The American Psychiatric Association Publishing Textbook of Psychiatry , 7th ed. Edited by Weiss Roberts L . Washington, DC, American Psychiatric Association Publishing, 2019 Google Scholar
5 Compton MT, Shim RS : Why employers must focus on the social determinants of mental health . Am J Health Promot 2020 ; 34:215–219 Crossref , Medline , Google Scholar
6 Shim RS, Compton MT : The social determinants of mental health: psychiatrists’ roles in addressing discrimination and food insecurity . Focus 2020 ; 18:25–30 Crossref , Medline , Google Scholar
7 Institute of Medicine: Reducing Risks for Mental Disorders: Frontiers for Preventive Intervention Research . Washington, DC, National Academy Press, 1994 Google Scholar
8 National Research Council and Institute of Medicine: Preventing Mental, Emotional, and Behavioral Disorders Among Young People: Progress and Possibilities. Washington, DC, National Academies Press, 2009 Google Scholar
- Robyn M. Powell , Ph.D., J.D. , and
- Joanne Nicholson , Ph.D.
- Health equity
- Mental health promotion
- Mental illness prevention
- Social determinants
- Sociopolitical Issues
To read this content please select one of the options below:
Please note you do not have access to teaching notes, mental health promotion theory and practice: insights from a literature review.
Journal of Public Mental Health
ISSN : 1746-5729
Article publication date: 1 January 1999
This article reports on a literature review of interventions specifically identified as emanating from a mental health promotion (as opposed to prevention) paradigm. A number of recurring debates in the field were identified, including language and terminology, defining ‘mental health’, models of mental health promotion, the use of overgeneralised concepts, values, beliefs and assumptions implicit in mental health promotion interventions, and diversity in what gets called mental health promotion and who does mental health promotion. The paper concludes by highlighting key issues critical to the future development of mental health promotion: the implications of mental health promotion being at an embryonic stage of development, the need for greater reflexivity, the need for integration, and issues concerning professional identity and practice in the mental health promotion field.
Mauthner, N. , Killoran‐Ross, M. and Brown, J. (1999), "Mental Health Promotion Theory and Practice: Insights from a Literature Review", Journal of Public Mental Health , Vol. 1 No. 1, pp. 37-42. https://doi.org/10.1108/17465729199900008
Copyright © 1999, MCB UP Limited
Related articles
We’re listening — tell us what you think, something didn’t work….
Report bugs here
All feedback is valuable
Please share your general feedback
Join us on our journey
Platform update page.
Visit emeraldpublishing.com/platformupdate to discover the latest news and updates
Questions & More Information
Answers to the most commonly asked questions here
Advertisement
Review of mental health promotion interventions in schools
- Invited Review
- Open access
- Published: 11 May 2018
- Volume 53 , pages 647–662, ( 2018 )
Cite this article
You have full access to this open access article

- Michelle O’Reilly 1 ,
- Nadzeya Svirydzenka 2 ,
- Sarah Adams 3 &
- Nisha Dogra 1
57k Accesses
143 Citations
59 Altmetric
Explore all metrics
The prevalence of mental disorders amongst children and adolescents is an increasing global problem. Schools have been positioned at the forefront of promoting positive mental health and well-being through implementing evidence-based interventions. The aim of this paper is to review current evidence-based research of mental health promotion interventions in schools and examine the reported effectiveness to identify those interventions that can support current policy and ensure that limited resources are appropriately used.
The authors reviewed the current state of knowledge on school mental health promotion interventions globally. Two major databases, SCOPUS and ERIC were utilised to capture the social science, health, arts and humanities, and education literature.
Initial searches identified 25 articles reporting on mental health promotion interventions in schools. When mapped against the inclusion and exclusion criteria, 10 studies were included and explored. Three of these were qualitative and seven were quantitative.
Conclusions
A range of interventions have been tested for mental health promotion in schools in the last decade with variable degrees of success. Our review demonstrates that there is still a need for a stronger and broader evidence base in the field of mental health promotion, which should focus on both universal work and targeted approaches to fully address mental health in our young populations.
Similar content being viewed by others

The Role of School in Adolescents’ Identity Development. A Literature Review

Community Interventions to Promote Mental Health and Social Equity

Factors that influence mental health of university and college students in the UK: a systematic review
Avoid common mistakes on your manuscript.
Introduction
Globally 10–20% of children and young people experience a mental disorder [ 28 ]; and this is increasing [ 26 ]. Additionally, it is estimated that 50% of adults with disorders experienced them prior to age 15 [ 25 ]. To address this, it is important to pay attention to promotion and prevention practice, with schools being well-placed to deliver. This is because of the amount of time young people spend in this environment [ 49 ]. The focus of this review is therefore, on universal mental health promotion interventions in schools rather than those that target high-risk individuals or where health education is part of the treatment of a mental health disorder.
Mental health promotion and prevention: operational definitions
The World Health Organisation [ 58 ] defines mental health promotion as actions to create living conditions and environments that support mental health and allow people to adopt and maintain healthy lifestyles. These include actions to optimise people’s chances of experiencing better mental health. The WHO noted that fundamental to mental health promotion are actions that facilitate an environment that respects and protects basic civil, political, socio-economic and cultural rights. Without the security and freedom provided by these rights, arguably it is difficult to maintain high levels of mental health. The WHO argued that mental health policies should include mental health promotion and not be limited to the health sector, but also involve education, labour, justice, transport, environment, housing, and welfare.
The WHO defines mental illness prevention as encompassing the reduction of incidence, prevalence, and recurrence of illness. Prevention strategies tend to be useful in targeting groups ‘at-risk’ to prevent them from developing disorders. However, although differentiated, it is important to note that the distinction is less rigid for young populations, because children develop skills as they mature [ 3 ] and skill development aimed at promoting well-being can have preventative effects [ 46 ].
Mental health promotion in schools
Schools are pervasive environments in young peoples’ lives and can positively impact on their mental health, mitigating some negative impacts of other social factors. However, for some, schools can present as considerable sources of stress, worry, and unhappiness [ 12 ], which can hinder academic attainment. In focusing on promotion, therefore, it is important to consider the educational context as a natural environment in which it is possible to build rights of agency, security, and personal freedom in young people, whilst recognising any limitations this may have.
Schools are positioned at the forefront of promoting positive mental health. This is an important way of tackling the growing prevalence of mental disorders worldwide. This has prompted the publication of numerous guidelines and policies in how this could be achieved in the UK and internationally. Recently, in England the government pledged that all secondary (high) schools will receive mental health training by 2020 and each school should have a mental health champion [ 38 ]. Similarly, governments in Wales and Scotland have produced policies and statements to advocate the promotion of positive mental health in school-aged children [ 43 , 57 ]. Furthermore, such thinking is reflected internationally as several countries have been exploring ways of integrating health and education [ 2 ].
Evidently, mental health promotion in schools needs to be achieved through the provision of a continuum of intervention programmes. Weist and Murray [ 55 ] argued that these should focus on social and emotional learning, competence for all students, and actively involve young people, schools and communities. The authors further argued that quality is central, and many factors need to be accounted for:
Inclusive approach.
Build programmes responsive to student, school and community needs, building connections between resources.
Focus on reducing barriers to student learning through programmes, based on evidence.
Emphasise and provide support for systematic quality assessment and improvement.
Ensure staff are engaged and supported.
Ensure efforts are sensitive to developmental and diversity factors of students.
Build interdisciplinary relationships in schools, strong teams and coordinating mechanisms.
Weist and Murray [ 55 ] observed that for change to happen, training and involvement from a range of people is needed to create a cultural shift in the educational context. This is mirrored in other western countries, where involvement of several people is considered necessary for successful mental health promotion programmes in schools (e.g. [ 32 , 42 ]). Furthermore, developing partnerships between the health and educational sectors can support meaningful engagement and lasting change [ 50 ].
Whole-school approaches
A ‘whole school approach’ for promoting positive mental health, recognises the importance of working collaboratively with all parts of the school community; students, families and staff, whilst acknowledging the impact of local and government policies [ 18 ]. Adopting this approach advocates that schools should tackle mental health and well-being through their behaviour policy, curriculum design, care and support for young people, as well as staff, and engagement of parents. Internationally, this has been implemented through schools adopting social and emotional programmes; for example, in the USA, the Collaborative for Academic, Social, Emotional Learning [ 8 ], in Australia, KidsMatter [ 10 ] and the UK, Social and Emotional Aspects of Learning (SEAL, DCSF, [ 9 ]). Where implemented, it has been found to not only support positive mental health, but also raise academic attainment [ 37 ].
Despite the outlined benefits of this approach, it is not without challenges. The whole-school approach advocated by many authors (e.g. [ 42 , 48 , 55 ]), may be undermined by:
lack of adequate support (in terms of staff willingness and/or funding)
clarity operationalisation, and consistency in terminology used (this would also need to consider how mental health and illness are conceptualised)
having appropriately trained staff to provide support and supervision, and
engaging young people in the development of the promotion of positive mental health.
Furthermore, recognition of the need to have sustainable multi-sector partnership in mental health promotion offers little guidance about who the partnerships should involve or specific roles of stakeholders. However, it would seem appropriate to engage the wider community and include families, as well as young people and their teachers.
Focus and aims of the review
Research has indicated that many young people worldwide are not well informed about mental health [ 13 , 39 , 40 , 44 , 47 ], and there is a clear need to raise awareness, educate, and provide interventions that facilitate the maintenance of mental well-being in young populations. Mental health promotions are potentially central to the solution, and therefore, it is unsurprising that many interventions that take this approach have been developed.
The focus of our review is on universal interventions of mental health promotion in schools, recognising that universal and target types require different approaches as the aim of the interventions are different. This review aims to examine advancements in mental health promotion in contemporary education, in the context of global austerity in the last 10 years. In presenting this review, it is necessary to be aware that terminology across the educational and health sectors differs [ 42 ] and sometimes mental health promotion is described as positive psychology (e.g. Terjesen et al. [ 51 ]) or emotional health (e.g. Kidger et al. [ 27 ]). This lack of universal terminology makes reviews complex and comparisons challenging. Therefore, for clarity our searches focused on studies that described interventions as promoting mental health and/or well-being.
As noted, the challenge in reviewing mental health promotion is the lack of universality in language and operational definitions of key terms. It is not always clear whether when the term mental health promotion is used, it is consistent with the WHO definition. Additionally, in education, several programmes go under a different title. For example, social and emotional learning (SEAL) is often used and interventions designed to promote effective mastery of social–emotional competencies aim to achieve greater well-being and better school performance by reducing risk factors and promoting protective mechanisms for positive adjustments [ 20 ]. For our review, we focused on searching for positive mental health promotion interventions as defined by the WHO, including social and emotional well-being, to capture an inclusive overview of the work that has been done.
Inclusion and exclusion criteria
To ensure included studies focused on mental health promotion interventions in schools we utilised the literature to facilitate our identification of appropriate inclusion and exclusion criteria. Studies eligible were:
Written in English.
Published between 1 January 2007 and 30 November 2017 for three reasons; (1) because there were reviews conducted in the early millennium that captured earlier work (e.g. Wells et al. [ 56 ]); (2) a decade is a sufficient time-frame to examine impact and change; and (3) captures recent policy changes that may impact on design and delivery of interventions.
Universal mental health promotion (or equivalent) (these should be different from targeted approaches as the interventions for universal and targeted interventions have different aims, objectives, intervention type and audience).
Whole-school interventions, programmes, frameworks, models, and tools, involving many levels of school personnel.
Target population was school age (that is, children of any age who are attending school. This spectrum varies internationally, but is generally from 3 to 18 years), and included any type of school (e.g. public, private, special, residential).
Original research.
We also provided parameters by identifying exclusion criteria:
Not published in English.
Not book chapters, editorials or guidance documents.
Not focused on risk factors or related to these.
Not reporting planning and development, and not pilots of interventions (as these would only present feasibility and would not be conclusive).
Not those interventions targeting children with pre-existing mental health problems.
Search strategy
Two large database systems were utilised for the search which captured the multidisciplinary nature of mental health promotion. First, was SCOPUS, a database that captures science, medicine, social science, arts and humanities research. Second, was ERIC, a database of the literature in the field of education. A range of search terms were utilised by two of the authors to ensure the searches were consistent. There were three independent searches across the two databases and these were:
Mental health AND promotion AND schools
Positive AND mental AND health AND promotion AND schools AND NOT illness
Mental health promotion AND well-being AND intervention AND schools
The top 100 results for each key-word combination based on relevance were searched as relevance dropped significantly after this point. This produced 25 articles that appeared to be appropriate. These were mapped against criteria and narrowed to 10 intervention studies.
When matched against the inclusion and exclusion criteria, a total of ten papers were returned. Three of these utilised a qualitative design and seven quantitative design. The literature was well spread globally (e.g. UK, Australia, USA, Sweden, Denmark, Germany, Ireland) and included different interventions, all of which were targeted at the general population of young people in schools. We organised our findings around four main issues: (1) the theoretical framework underpinning the intervention; (2) support, training and supervision for staff implementing the intervention; (3) outcomes of the interventions and (4) long-term impact. The findings were subsequently summarised and an overview of the articles is presented in Table 1 .

Theoretical frameworks
Most interventions were reported to be underpinned by a theoretical framework, but these were variable. Six studies reported a clear theory underpinning the intervention, and two described the theoretical position of the methodology; two of the studies made no explicit reference to theory. Mostly, studies were underpinned by the framework of a whole-school approach and/or a child-centred approach to mental health promotion [ 1 , 11 , 16 , 21 , 32 ], although the underpinning theoretical framework was not always clear in the way it was described. Neilsen et al. [ 32 ] integrated this whole–school approach framework in the intervention evaluation with an Action Competence focus, linking democracy, participation and empowerment [ 7 ]. Franz and Paulus [ 17 ] utilised the theoretical position of a resource-based conceptual theory, which balances internal and external needs and resources (see Becker, [ 4 ] [non-English publication] in Franze and Paulus, [ 17 ]) and did not make explicit reference to the whole-school framework, but did include school personnel in the implementation.
Support, training, and supervision of staff
A challenge for any intervention is, in part, dependent upon those who deliver it. Notably, seven of the interventions were delivered by teachers, although in one case this was implied rather than stated. Two of the interventions were delivered by specialists including physiotherapists [ 22 ] and educational psychologists [ 21 ]. For one intervention, the authors did not provide clear details [ 11 ]. The support, training, and supervision of teachers during the intervention was described in five of the seven papers that reported staff involvement. For some, training was provided via a workshop [ 32 ] and for others, through training sessions. Some staff had continued support and supervision [ 29 ], but many did not. Interventions delivered by school staff were also reported to be supported by instruction manuals. Most of these interventions were described as structured [ 1 , 16 , 17 ].
Mental health outcomes
In reviewing the interventions, all but two clearly reported a positive impact. Eight of the ten interventions highlighted some degree of impact and argued that the intervention was a successful mental health promotion tool. Notably, two interventions did not produce such positive results. Lendrum et al. [ 31 ] reported that the national SEAL programme had no significant impact, and this was the case in all schools. They noted that there were several barriers to success, including, challenges and confusion regarding implementation, staff skills and training needs, lack of awareness, reluctance of staff, poor communication and limited coordination of the whole-school approach. Similarly, Fitzpatrick et al. [ 16 ] found few differences following the comparison of a standard versus an enhanced intervention programme for mental health promotion. They argued that the difference between the enhanced and the standard programme may be too small to have a statistically significant effect on outcomes.
Long-term impact
Although most of the interventions demonstrated degrees of success in promoting mental health and well-being, the papers were less clear about the sustainability and maintenance of this success. The eight interventions reporting a positive impact highlighted variability in the long-term outcomes, mostly projecting the potential of the intervention and arguing that long-term evaluations are necessary [ 1 , 17 , 32 ]. Two of the interventions were tested over longer periods of 3- and 2-years [ 11 , 29 ] respectively, which suggested some sustainability. However, some caution must be exercised as most of the long-term outcomes in terms of mental health promotion were not known and authors argued that commitment from the schools and further evaluations are required in future. Indeed, interventions that showed no change demonstrated that flexibility of the intervention can cause confusion for implementation suggesting the need to balance prescriptive guidelines and flexible adaptations with school culture and ethos [ 31 ].
Overall results
This review has contextualised the broader literature on mental health promotion and specifically explored advancements of universal interventions in the last decade. The results demonstrated that there has been limited advancement of this field. Specifically, we have shown that terminology remains variable, there is still limited evaluation of long-term impacts, and there remains inconsistency regarding the people chosen to run the interventions, with their qualifications and training being varied. Like previous reviews in this area, we demonstrated that methods used were of variable quality, some authors were vague in their descriptions of the intervention, and there was not always clarity regarding sources of funding. Somewhat surprisingly, there was a lack of digital interventions, using AI, informatics, robotics, social media, or internet-based approaches.
Globally, there is continued development and implementation of various interventions in schools designed to promote positive mental health, and yet the effectiveness of most of these is not well evaluated [ 1 ]. If we are to move forward and make advances in mental health promotion and help young people cope with daily stresses, we need a better understanding of the outcomes and possible ways of sustaining them. Over the last decade, several mental health promotion interventions have been evaluated and were included in this review.
Universal school-based interventions have great potential to target large populations of young people to promote well-being at a general level. Indeed, this is a common approach taken by schools. Over time, several interventions has emerged based on different theoretical frameworks ([ 11 , 17 , 21 , 29 , 32 ], to name a few). A unifying factor that often underpins or is central to these universal approaches is the whole-school approach, or at least an approach that requires the cooperation of different levels of school personnel, wider communities, and other agencies. Previous reviews over the last couple of decades on the beneficial effects of mental health, social, emotional and educational outcomes have shown that a whole-school approach sustained for more than a year is positive for health promotion and prevention. These conclusions were supported by Weare and Murray [ 53 ] who found that a multi-dimensional and integrated whole-school approach is needed for mental health promotion to be effective and to create positive change in the well-being of young people. A more recent review highlighted that for positive outcomes to be achieved, any intervention must be sequenced in the sense that the activities need to be coordinated, incorporating an active form of learning, focused on personal or social skills and explicitly targeting specific skills rather than positive development [ 15 ].
However, these interventions also showcase variability in outcomes, challenges of concepts and ideas, difficulties in implementation and attitudes, and issues of sustainability. Early reviews by Wells and colleagues [ 56 ] showed a large variation in type and quality of publications and our review demonstrates that the situation has barely changed since. The quality of evidence has been appraised as generally low-to-moderate, with many studies relying on students’ accounts of their own behaviour, with some studies suffering from high attrition rates [ 30 ]. Therefore, while popularity of the universal whole-school approach is undeniable, shortcomings of these interventions need to be addressed. Green et al. [ 19 ] stated that “while the limited information from the reviews makes it difficult to comment on universal approaches to mental health promotion, whole-school approaches to the promotion of social and emotional health implemented over years appear to be more effective than brief class-based programmes aimed at preventing mental health problems”. However, like previous reviews, our findings demonstrated that considerable methodological issues remain.
Challenges of using interventions
The core challenge for successful mental health promotion is that most of the school-based interventions reported tended to be short-term with little long-term follow-up. Furthermore, they were also often evaluated immediately or shortly after the intervention. However, there is increasing evidence that some long-term effects are emerging and that although effects gradually decrease over time they can remain substantial [ 54 ].
Although some whole-school approaches related to mental health promotion have found fewer advantages than others, sometimes this is attributed to a lack of consistent, rigorous and faithful implementation of the overall programme and/or lack of support for teachers administering it [ 29 ]. For example, in a survey of 599 primary and 137 secondary schools in the UK, two-thirds of schools adopted universal approaches, but gaps in teacher training and support were identified as problematic [ 52 ]. For schools with limited resources or those that place high demands on teachers’ time, it may be more beneficial that the universal whole-school approach in the mental health promotion is set aside in favour of a smaller scale targeted intervention that is more manageable and sustainable. The crucial challenge of either model of intervention would be to effectively and consistently engage the learners (that is the young people themselves) in development and delivery.
In attempts to bolster schools’ responsibilities for catering for young peoples’ mental health, funding for schools in England has been provided to ensure all schools have a trained ‘mental health champion’ by 2020 [ 38 ]. By having an identified and trained responsible member of staff, this may alleviate some of the challenges faced in implementing a whole-school approach. The ‘mental health champion’ will be able to act as a strategic lead in implementing interventions designed to promote positive mental health, whilst also monitoring the impact and cost effectiveness. However, this raises issues for schools, as training will be central to successful implementation, but training for teachers cannot tackle mental health promotion in isolation from the practical difficulties of supporting children who have diagnosed conditions [ 41 ]. Additionally, while training teachers is a positive move to address the large-scale issues, in isolation it will not form the solution as it needs to be part of a continued process supported by greater funding for child mental health [ 24 ] otherwise it risks being a “sticking plaster solution” to the challenge [ 45 , n.p]. Currently, the Welsh government is piloting specialist CAHMS workers to act as a link between schools and CAHMS whereby school staff are supported to cater for the mental health of their pupils whilst also having support in place when more specialist interventions are needed [ 57 ].
Achieving the goals of mental health promotion, and implementing interventions, relies heavily on good quality evidence, and yet much work in this area is not sufficiently evidence-based [ 52 ]. Vostanis et al. argued that there is a clear need to improve this situation. These improvements could include more effective evaluation methodologies (e.g. rationalisation and operationalisation of selected theoretical frameworks and models, methods and instruments used), explicit application procedure of interventions, and details of teacher training and support packages [ 36 ]. Evidently, the popularity of a ‘one approach fits all’ needs to be matched with rigorous systematic development, recognising contributing/challenging factors as well as application and measurement across different populations, school systems, and wider cultural contexts. Additionally, more work needs to include the ‘child’s voice’, to be child-centred and respect children’s rights, and therefore, there is a need for more qualitative work in this area.
Strengths and limitations
This review is not without its limitations. First, to provide a targeted and focused message about mental health promotion in schools, we have been prescriptive in the search terms used to identify the scope of the literature. Given a broader search, we might have included papers that have not utilised specific terminology in their interventions. Additionally, research conducted prior to 2007 was not included, and this work may not have been replicated or evaluated since. These studies were excluded from the review as arguably they may not account for contemporary policy and older reviews may exist which evaluate that work. Second, we have only included results published in English, and therefore, rely on research that has been promoted through English publication streams. While included papers did offer an international perspective in terms of interventions across different educational systems in different countries, the sample remained focused on the developed world. No papers looked at mental health promotion efforts in schools in developing countries, which is an area of great significance in terms of mental health outcomes for young people. This is probably missing from the review due to publishing language barriers and/or research not being undertaken in this area as resources are often even more limited in the developing world. Therefore, the current review and discussion is limited in its applicability to countries with similar development profiles to the ones included. However, arguably, factors of effective and sustainable mental health promotion interventions outlined here could be applicable across variety of cultural contexts, albeit untested.
Directions for future research
In their review, Weare and Nind [ 53 ] identified that the characteristics of high-quality programmes that were successfully implemented include:
A sound theoretical base with specific, well-defined goals that were communicated effectively.
Focus on the desired outcomes.
Explicit guidelines and through training, which is quality assured.
Complete and accurate implementation.
This list of recommendations is consistent with the need for high-quality training interventions in any field [ 14 ]. Weare and Nind [ 54 ] argued that much of the evidence related to mental health work in schools would support that these characteristics will be beneficial in implementation, although the benefits may be small and not sustained, as supported by our review findings. The authors, however, argued that even change that is small in statistical terms may translate into a significant impact on well-being and this is something that should be explored.
Nonetheless, it is evident from our review, that there is still a need for a stronger and broader evidence base in the field of mental health promotion, which should focus on both universal work and targeted approaches to fully address mental health in our young populations. In terms of intervention development, research has demonstrated that it is essential to include young peoples’ views when developing interventions to ensure a child-centred approach and support at a whole-school level [ 21 , 35 ] and thus the co-development of programmes could be helpful. Further to this is the need to develop teachers’ understanding, competence and confidence in delivering and sustaining mental health promotion with their pupils [ 31 ], as research shows that teachers are resistant to holding too much responsibility in terms of mental health and lack confidence [ 34 ]. Methodologically, interventions need to be able to adapt to school culture and available resources while still offering measurable set of outcomes. More attention needs to be paid to the culture of schools as part of any intervention, as there may be little value in implementing programmes when it is already known that the factors needed for their success are not in place at the time or are not sustainable in long-term (e.g. if funding/support expires with termination of the research project). Furthermore, rigour and quality in the evaluation of interventions also needs attention. Programme effectiveness, safety, and cost is not always as rigorous and robust as it could be [ 30 , 33 ] and therefore, attention to the quality of studies is essential for future examinations of interventions. Validation tools can go some way to addressing these issues [ 5 ].
Our review has demonstrated that there is some success for interventions, many of which were underpinned by the whole-school approach or similar frameworks. This was also the case for other intervention types that were not so broad in scope. However, training teachers in delivery was important and long-term outcomes unclear. Thus, building on previous work, we have demonstrated that there remain gaps in knowledge, that there are issues with sustainability of universal approaches, and that success, to some extent, relies on cooperation, training and involvement of the schools and the young people themselves. Furthermore, modes of delivery and the nature of the interventions are important and need to appeal to young people. This could be facilitated by more scoping work in terms of digital health promotion. In a digital age, with digital tools, mobile apps, robotics, social media and the internet all forming a central part in daily life, there is potential to integrate a whole-school approach with digital interventions, and there is room to be creative with universal mental health promotion.
Anthony H, McLean L (2015) Promoting mental health at school: short-term effectiveness of a popular school-based resiliency programme. Adv Sch Ment Health Promot 8(4):199–215
Article Google Scholar
Atkins MS, Hoagwood KK, Seidman E (2010) Toward the integration of education and mental health in schools. Adm Policy Ment Health Ment Health Serv Res 37:40–47
Barnes J (1998) Mental health promotion: a developmental perspective. Psychol Health Med 3:55–69
Becker P (1997) Psychologie der seelischen Gesundheit. Band 1: Theorien, Modelle, Diagnostik. Hogrefe, Göttingen
Google Scholar
Bjørnsen H, Eilertsen ME, Ringdal R, Espnes G, Mosnes U (2017) Positive mental health literacy: development and validation of a measure among Norwegian adolescents. BMC Public Health 17:717–727
Article PubMed PubMed Central Google Scholar
Butzer B, LoRusso A, Windsor R, Riley F, Frame K, Khalsa S, Conboy L (2017) A qualitative examination of yoga for middle school adolescents. Adv Sch Ment Health Prom 10(3):195–219
Clift S, Jensen B (2005) The health promoting school: international advances in theory, evaluation and practice. Danish University of Education Press, Copenhagen
Collaborative for academic, social, and emotional learning. https://casel.org/ . Accessed 12 Feb 2018
DCSF (2010). Social and emotional aspects of learning (SEAL) programme in secondary schools: national evaluation. Department for Children, Schools and Families, Nottingham
Department of Health KidsMatter. https://www.kidsmatter.edu.au/ . Accessed 9 Feb 2018
Dix K, Slee P, Lawson M (2012) Implementation quality of whole-school mental health promotion and students’ academic performance. Child Adolesc Ment Health 17:45–51
Dogra N (2010) Social factors that influence child mental health. In: Bhugra D, Morgan C (eds) Principles of social psychiatry, 2nd edn. Wiley-Blackwell, Oxford, pp 295–304
Dogra N, Omigbodun O, Adedokun T, Bella T, Ronzoni P, Adesokan A (2012) Nigerian secondary school children’s knowledge of and attitudes to mental health and illness. Clin Child Psychol Psychiatry. https://doi.org/10.1177/1359104511410804
Article PubMed Google Scholar
Dogra N, Parkin A, Gale F, Frake C (2017) A multidisciplinary handbook of child and adolescent mental health for front-line professionals, 2nd edn. Jessica Kingsley Publishers, London
Durlak J, Weissberg R, Dymnicki A, Taylor R, Schellinger K (2011) The impact of enhancing students’ social and emotional learning: a meta-analysis of school-based universal interventions. Child Dev 82(1):405–432
Fitzpatrick C, Conlon A, Cleary A, Power M, King F, Guerin S (2013) Enhancing the mental health promotion component of health and personal development programme in Irish schools. Adv Sch Ment Health Promot 6(2):122–138
Franze M, Paulus P (2009) MindMatters—a programme for the promotion of mental health in primary and secondary schools: results of an evaluation of the German Language Adaptation. Health Educ 109(4):369–379
Graetz B, Littlefield L, Trinder M, Dobia B, Souter M, Champion C, Boucher S, Killick-Moran C, Cummins R (2008) KidsMatter: a population health model to support student mental health and well-being in primary schools. Int J Ment Health Promot 10(4):13–20
Green J, Howes F, Waters E, Maher E, Oberklaid F (2005) Promoting the social and emotional health of primary school-aged children, reviewing the evidence base for school-based interventions. Int J Ment Health Promot 7(3):30–36
Guerra NG, Bradshaw CP (2008) Re-thinking the prevention of problem behaviors and positive youth development: core competencies for positive youth development and risk prevention. New Dir Child Adolesc Dev 122:1–17
Hall S (2010) Supporting mental health and well-being at a whole-school level: listening to and acting upon children’s views. Emot Behav Diffic 15(4):323–339
Haraldsson K, Lindgen EC, Fridlund B, Baigi A, Lydell M, Marklund B (2008) Evaluation of a school-based health promotion programme for adolescents aged 12–15 years with focus on well-being related to stress. Public Health 122:25–33
Humphrey N, Lendrum A, Wigelsworth M (2010) Social and emotional aspects of learning (SEAL) programme in secondary schools: national evaluation. DFE
Karim K, O’Reilly M (2017) Comment on Public Health England’s investment in mental health training for schools. https://www2.le.ac.uk/offices/press/think-leicester/health-and-medicine/2017/comment-on-public-health-england-investment-in-mental-health-training-for-schools . Accessed 12 Feb 2018
Kessler R, Berglund O, Demler R, Jin R, Walters E (2005) Life-time prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey replication. Arch Gen Psychiatry 62:593–602
(The) Key (2017) State of Education Survey Report 2017. Rising to the challenge: examining the pressures of schools and how they are responding. https://view.joomag.com/state-of-education-report-2017/0676372001494577623 . Accessed 12 Feb 2018
Kidger J, Donovan J, Biddle L, Campbell R, Gunnell D (2009) Supporting adolescent emotional health in schools: a mixed methods study of student and staff views in England. BMC Public Health 9:403–421
Kieling C, Baker-Henningham H, Belfer M, Conti G, Ertem I, Omigbodun O, Rohde LA, Srinath S, Ulkuer N, Rahman A (2011) Child and adolescent mental health worldwide: evidence for action. Lancet. https://doi.org/10.1016/S0140-6736(11)60827-1
Kimber B, Sandell S, Bremberg S (2008) Social and emotional training in Swedish schools for the promotion of mental health: an effectiveness study of 5 years of intervention. Health Educ Res 23(6):931–940
Langford R, Bonell CP, Jones HE, Pouliou T, Murphy SM, Waters E, Komro KA, Gibbs LF, Magnus D, Campbell R (2014) The WHO Health Promoting School framework for improving the health and well-being of students and their academic achievement. Cochrane Database Syst Rev. https://doi.org/10.1002/14651858.CD008958.pub2
Lendrum A, Humphrey N, Wigelsworth M (2013) Social and emotional aspects of learning (SEAL) for secondary schools: implementation difficulties and their implications for school-based mental health promotion. Child Adolesc MentHealth 18(3):158–164
Nielsen L, Meilstrup C, Nelausen M, Koushede V, Holstein B (2015) Promotion of social and emotional competence: experiences from a mental health intervention applying a whole school approach. Health Educ 115:339–356
O’Mara L, Lind C (2013) What do we know about school mental health promotion programmes for children and youth? Adv Sch Ment Health Promot 6(2):203–224
O’Reilly M, Adams S, Whiteman N, Hughes J, Reilly P, Dogra N (2018) Whose responsibility is adolescent’s mental health in the UK? Perspectives of key stakeholders. Sch Ment Health. https://doi.org/10.1007/s12310-018-9263-6
O’Reilly M, Dogra N, Hughes J, Reilly P, Whiteman N (2017) Written evidence for parliament: mental health in schools. http://data.parliament.uk/writtenevidence/committeeevidence.svc/evidencedocument/health-committee/children-and-young-peoples-mental-healththe-role-of-education/written/45583.pdf . Accessed 12 Feb 2018
Power M, Cleary D, Fitzpatrick C (2008) Mental health promotion in Irish schools: a selective review. Adv Sch Ment Health Promot Vol 1(1):5–15
Public Health England (2015) Promoting children and young people’s emotional health and well-being: a whole school and college approach. Public Health England, London. https://www.gov.uk/government/publications/promoting-children-and-young-peoples-emotional-health-and-well-being . Accessed 12 Feb 2018
Public Health England (2017) Secondary school staff get mental health ‘first aid’ training. https://www.gov.uk/government/news/secondary-school-staff-get-mental-health-first-aid-training . Accessed 12 Feb 2018
Ronzoni P, Dogra N, Omigbodun O, Bella T, Atitola O (2010) Stigmatization of mental illness among Nigerian schoolchildren. Int J Soc Psychiatry. https://doi.org/10.1177/0020764009341230
Rose D, Thornicroft G, Pinfold V, Kassam A (2007) 250 labels used to stigmatise people with mental illness. BioMedCentral Health Serv Res. https://doi.org/10.1186/1472-6963-7-97
Rothi D, Leavey G, Best R (2008) On the front-line: teachers as active observers of pupils’ mental health. Teach Teach Educ 24(5):1217–1231
Rowling L (2009) Strengthening ‘school’ in school mental health promotion. Health Educ 109(4):357–368
Scottish Government (2017) Mental health strategy 2017–2027 http://www.gov.scot/Publications/2017/03/1750/5 Accessed 10 Apr 2018
Sessa B (2005) I’ll have to lie about where I’ve been. Young Minds Mag 76:34–5
Sims-Schouten W (2017) Mental health first aid training in schools is a sticking-plaster solution. https://theconversation.com/mental-health-first-aid-training-in-schools-is-a-sticking-plaster-solution-80166 Accessed 12 Feb 2018
Sroufe A, Rutter M (1984) The domain of developmental psychopathology. J Child Dev 55:705–711
Stengård E, Appelqvist-Schmidlechner K (2010) Mental health promotion in young people: an investment for the future. World Health Organisation, Geneva
Stewart-Brown S. What is the evidence on school health promotion in improving or preventing disease and, specifically, what is the effectiveness of the health promoting schools approach? Copenhagen: WHO Regional Office for Europe (Health Evidence Network Report). http://www.euro.who.int/__data/assets/pdf_file/0007/74653/E88185.pdf . Accessed 8 Feb 2017
Sturgeon S (2007) Promoting mental health as an essential aspect of health promotion. Health Promot Int 21(S1):36–41
Svirydzenka N, Bone C, Dogra N (2014) Schoolchildren’s perspectives on the meaning of mental health. J Public Ment Health. https://doi.org/10.1108/JPMH-09-2012-0003
Terjesen M, Jacofsky M, Froh J, DiGiuseppe R (2004) Integrating positive psychology into schools: implications for practice. Psychol Sch. https://doi.org/10.1002/pits.10148/full
Vostanis P, Humphrey N, Fitzgerald-Yau N, Wolpert M (2013) How do schools promote emotional well-being among their pupils? Findings from a national scoping survey of mental health provision in English schools. Child Adolesc Ment Health 18(3):151–157
Weare K, Murrary M (2004) Building a sustainable approach to mental health work in schools. Int J Health Promot 6(2):53–59
Weare K, Nind M (2011) Mental health promotion and problem prevention in schools: what does the evidence say? Health Promot Int 26:i29–i69
Weist MD, Murray M (2007) Advancing school mental health promotion globally. J Adv Sch Ment Health Promot. https://doi.org/10.1080/1754730X.2008.9715740
Wells J, Barlow J, Stewart-Brown S (2003) A systematic review of universal approaches to mental health promotion in schools. Health Educ 103(4):197–220
Welsh Government (2017) Written statement—providing for the emotional and mental health needs of young people in school. http://gov.wales/about/cabinet/cabinetstatements/2017/mentalhealthneeds/?lang=en Accessed 10 Apr 2018
(The) World Health Organisation (WHO) (2016) Mental health: strengthening our response. http://www.who.int/mediacentre/factsheets/fs220/en/ . Accessed 23 Mar 2017
Download references
Author information
Authors and affiliations.
The Greenwood Institute, University of Leicester, Westcotes Drive, Leicester, LE3 0QU, UK
Michelle O’Reilly & Nisha Dogra
Faculty of Health and Life Sciences, De Montfort University, The Gateway, Leicester, LE1 9BG, UK
Nadzeya Svirydzenka
School of Education, University of Leicester, University Road, Leicester, LE1 7RH, UK
Sarah Adams
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Michelle O’Reilly .
Ethics declarations
Conflict of interest.
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License ( http://creativecommons.org/licenses/by/4.0/ ), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
Reprints and permissions
About this article
O’Reilly, M., Svirydzenka, N., Adams, S. et al. Review of mental health promotion interventions in schools. Soc Psychiatry Psychiatr Epidemiol 53 , 647–662 (2018). https://doi.org/10.1007/s00127-018-1530-1
Download citation
Received : 14 February 2018
Accepted : 30 April 2018
Published : 11 May 2018
Issue Date : July 2018
DOI : https://doi.org/10.1007/s00127-018-1530-1
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Mental health promotion
- Interventions
- Find a journal
- Publish with us
- Track your research
SYSTEMATIC REVIEW article
Promoting university students' mental health: a systematic literature review introducing the 4m-model of individual-level interventions.

- 1 Guidance & Counseling Office, Student Services & Registration, Mohammed Bin Rashid University of Medicine and Health Sciences (MBRU), Dubai, United Arab Emirates
- 2 Strategy & Institutional Excellence, Mohammed Bin Rashid University of Medicine and Health Sciences (MBRU), Dubai, United Arab Emirates
Objective: The purpose of this study is to systematically review recently published individual student-level interventions aimed at alleviating the burden of mental health challenges faced by the students and/ or at equipping them with coping mechanism that will foster their resilience.
Methods: This study relied on a systematic literature review. PubMed dataset was used; the search was confined to the following period: July 2016-December 2020.
Results: A total of 1,399 records were identified by the electronic search, out of which 40 studies were included in this study. The authors inductively identified four overlapping categories of interventions across all included articles, and coded them as follows: Mindfulness, Movement, Meaning, and Moderator. Accordingly, each study was linked to at least one of four overlapping categories based on the nature of the intervention(s) under investigation, leading to differing assortments of categories.
Conclusions: The 4M-Model generated by this study encourages focusing on devising holistic, university-based interventions that embrace the individuality of students to improve their mental health through elements of mindfulness, movement, meaning, and moderator. Through this focused approach, university counselors are enabled to design interventions that address students' physical, psychological, emotional, and social needs.
Introduction
There has been a positive paradigm shift in the way our world and its citizens are perceiving the concept of mental health. Mental health is a state of well-being that allows individuals to enjoy and maintain relationships as well as handle stress in a healthy manner without compromising on productivity ( 1 ).
A large body of literature on tertiary education students highlights the importance of maintaining mental health with evidence relating it to educational attainment and productivity ( 2 ), social relationships, engagement on campus, and quality of life ( 3 ), and placement performance ( 4 ). Poor mental health has also been linked with lower retention within a programme, grade point averages, and graduation rates among university students ( 5 ). Counseling, psychoeducation, and mental health services on campuses are no longer deemed as merely supportive but rather an integral component necessary to empower students. These services are integral to help students develop skills such as psychological flexibility ( 6 ) which in turn influences mental health ( 1 ).
The current generation of university students is vastly different from previous generations, especially in their attitudes and beliefs toward their mental health needs. Well-being is a dynamic concept of interlinked physical, social, and psychological dimensions which is constantly changing depending on intrinsic and extrinsic environments and motivations ( 7 ). It is not only the demographics of the current generation of university students that has changed considerably from the past ( 8 ), but so have their attitudes and beliefs toward their needs, including mental health ( 3 ). This population is considered high risk because most mental health problems are triggered before the age of 24 ( 9 ). There is enough evidence to link personal and academic stressors to mental health ( 10 – 12 ). Contemporary tertiary education is striving to attain and maintain cultures of excellence, similar to traditional universities in the past ( 13 ). However, there has been a shift to turn modern day campuses into high stakes competitive testing environments with well-intended emphasis on preparing students to become part of the global economy. This change has influenced the context in which modern universities function. There are a set of challenges that contemporary universities face that extend beyond the earlier tertiary educational institutions and there is an assumption that students are coming to college “overwhelmed and more damaged than those of previous years” ( 14 ).
Although good citizenship has always been an important foundation of all educational institutions, with the dynamic social landscape that the universities are set within, there seems to be a tendency to lead students to fixate on extrinsic factors such as: results and Grade Point Averages, over intrinsic interest such as innovative learning, and expansion of lateral thinking ( 13 ). When the priority is grades, it manifests itself in excessive hours of focused studying, and in negative coping behaviors, such as: inadequate sleep and addictive behaviors, which could potentially affect the well-being of the student. Often, in this pursuit of academic excellence, there is the danger of ignoring the social, emotional, and psychological problems that modern students are now increasingly facing.
There is enough research that indicates that students are experiencing more mental health disorders in contemporary times and are less resilient than students in the past ( 8 ), with lower levels of frustration tolerance ( 15 ). Anxiety and depression are most prevalent among tertiary students ( 16 ). There is a rise in the number of college students with a diagnosable psychological disorder ( 17 ) with some students at greater risk than others of experiencing stress and mental health problems ( 18 ). There has been also a shift in the severity of the problems by students seeking counseling services over the past decade. It is no longer just presenting challenges of adjustment and individuation ( 19 ), or benign hormonal developmental problems associated with the age that prompts students to seek counseling. Students are presenting with severe psychological problems ( 20 ) with a sizeable number of them on psychiatric medication to help them function better on campus ( 15 ).
A common narrative through an exhaustive body of literature highlights the barriers to seeking help for mental health problems by students on campus due to stigma ( 21 ), scepticism about treatment efficacy ( 22 ), and a belief that their emotional problems will not be completely understood. This leads to a sense of social isolation as the students restrain from reaching out for help ( 21 ). Two contributing factors to inadequate help-seeking are the stigma of having a mental health problem and the personal characteristics of the individual student ( 20 ). A fear of negative consequences on academic records ( 23 ) is another common barrier among university students. Interestingly, students resist seeking help because they do not perceive their condition to require intervention or do not perceive it as a priority among their other commitments. They also have the tendency to normalize stress as part of university life, expecting it “will go away with time,” and prefer to handle their problems on their own ( 24 ).
More recent research indicates that students also rely on informal sources of help-seeking from non-professionals, particularly peer groups ( 25 ). Students report having no inhibitions about having open discussions about their mental health problems via social-networking websites ( 26 ). This resonates with the network episode model of help-seeking that emphasizes the social network as an integral, contemporary support in enhancing knowledge and attitudes toward seeking help ( 27 ). However, there is also a significant increase in the number of students with major psychological problems seeking counseling services on campus ( 3 ) challenging the stigma connected with help-seeking. The newer generation's familiarity with psychosocial support services and openness toward seeking them are putting mental health at the core of self-care, much like diet and exercise ( 26 ).
Along with rapid social changes and expectations, the dilution of traditional family anchors (that is the changes to family systems which include busy yet isolated lifestyles, social media pressures, a living free from parental influence which is very common to this age group, and forced separation from families in the pursuit of dream destinations for education) all compounding to the considerable degree of stress that students report upon ( 18 ). Considering all these transitions, focusing on the support that is available to young people on campus is increasingly becoming a necessity. This is not only a personal benefit for students but a national and international investment that could also result in considerable economic benefit ( 28 ) as these students stand to become contributors to the global economy.
A wealth of research exists which highlights the effectiveness of changing organizational factors that influence mental health ( 29 , 30 ). However, there is limited research on person-centric mental health strategies used in university settings ( 31 ). A Systematic Literature Review that was conducted by Fernandez et al. focused on evaluating the effect of setting-based interventions that stimulated and improved the mental health and well-being of university students and employees ( 32 ). That review constitutes an asset for universities seeking to adopt setting-based strategies that were proven efficacious. Yet, given the highspeed in which the higher education ecosystem has been evolving, there is an evident need for a more up-to-date review. Also, despite the importance of modifying the environment for it to become more nurturing for university students' mental health, this needs to be in conjunction with embracing the individuality of each student. Accordingly, the purpose of this study is to bridge this gap through providing a review of the literature on recently published individual student-level interventions that aim to alleviate the burden of mental health challenges faced by the students and/or help them with coping mechanisms that will foster their resilience.
We conducted a systematic review following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines ( 33 ). The protocol of the systematic review was published in PROSPERO, a database of prospectively registered systematic reviews in health and social care (CRD42021227862).
Search Strategy
To complement the work of Fernandez et al., focusing on the recent literature, the search period was confined to July 2016 through December 2020 ( 32 ). PubMed database was used. The search strategy used, with its key words and Boolean logic, is available as an online resource. It was structured as follows:
• Subjects: student or resident.
• Location: higher education, university, college, or tertiary education.
• State-of-being : mental health.
• Challenges faced by subjects : psychosocial, anxiety, depression, burnout, stress, peer-pressure, social media pressure, bullying, eating disorder, perfectionism, or learning difficulties.
• Intervention to address the challenges : psychotherapy, mindfulness, Counseling, support group, yoga, breathing, art therapy, awareness, resilience, gratitude, affirmations, or peer-Counseling.
Pure qualitative studies were excluded. We included all quantitative studies, so long as they contained information on the impact of the intervention. These included those using experimental (i.e., randomized controlled trials) or observational (i.e., controlled trials without randomization, and pre-post and time series) approaches. Duplicated papers were excluded. Studies were screened for inclusion in three phases:
1. BN and FO went over all the abstracts, together, to remove the articles that certainly did not meet the inclusion criteria.
2. The full text of all the remaining abstracts were reviewed independently by BN and FO. The results were discussed. Any discrepancies were investigated and reflected upon until reaching consensus.
3. Finally, all remaining articles were thoroughly reviewed for summarizing purposes based on a preset template: research study objective, context, design, method, sample, intervention, and main conclusion.
Articles were included if:
a) Empirical/applied (i.e., theoretical studies or systematic reviews, and studies using secondary data were excluded),
b) Conducted in one or more university,
c) Aimed at evaluating, the immediate or long-term effect of an intervention on the mental health status of students,
d) Included global measures of mental health and well-being,
e) Had the university counselor involved in the intervention,
f) Involved full-time students, and
g) Was written in English.
Quality Assessment
The quality of each of the included articles was evaluated considering the internal and external validity. For the internal validity (risk of bias), each study's methodological quality was assessed using the criteria introduced by Jadad et al. ( 34 ). As for the external/ ecological validity of the included studies, it was assessed using the criteria developed by Green and Glasgow ( 35 ). This quality assessment was not used to exclude articles. Yet, the results of the assessment were thoroughly reflected upon as an evaluative measure of the review output.
Data Analysis
The interventions referred to in the included studies were analyzed by the researchers using the framework of Braun and Clarke ( 36 ). The intention was to inductively build a general interpretation of all included studies, in alignment with the paradigm of constructivism ( 37 , 38 ). The assumption was that reality is socially-constructed. This required thoroughly reflecting upon the interventions investigated in the included studies. The process of exploratory reflection adapted was spiral, where the researchers' observations kept getting revisited which culminated into the development of an evidence-driven model. Since the constructivism paradigm gives precedence to thoroughness and insightfulness over extensiveness and generalizability ( 39 ), the decision was made upfront, as abovementioned, for this search to be limited to a single database ( 40 ). As for the purpose of the qualitative meta-synthesis, it was to create a dynamic individual-level intervention framework that is holistic and context-specific ( 41 ). All articles were categorized based on the nature of the intervention(s) under investigation. It is all narratively presented in the results section.
A total of 1,399 records were identified by the electronic search. Two researchers (BN and FO) reviewed all the abstracts of the resulting papers to identify ones that fitted the inclusion criteria. Based on that, a total of 1,178 articles were excluded. The full text of all remaining 220 articles were extracted and thoroughly reviewed by the two researchers (110 by each). Accordingly, 133 articles were excluded. The remaining 87 articles underwent another round of assessment by both researchers together. Out of these 87 articles, 47 papers were excluded: four studies did not meet the eligibility criteria of having an intervention in them, 31 studies did not include assessing the effectiveness of an intervention,10 studies were not exclusively on university students, and 1 was not on full-time students. Also, one study was excluded because it was not counselor-led but outsourced. Out of the initially identified 1399 articles, 40 articles were finally included in the study ( Figure 1 ).
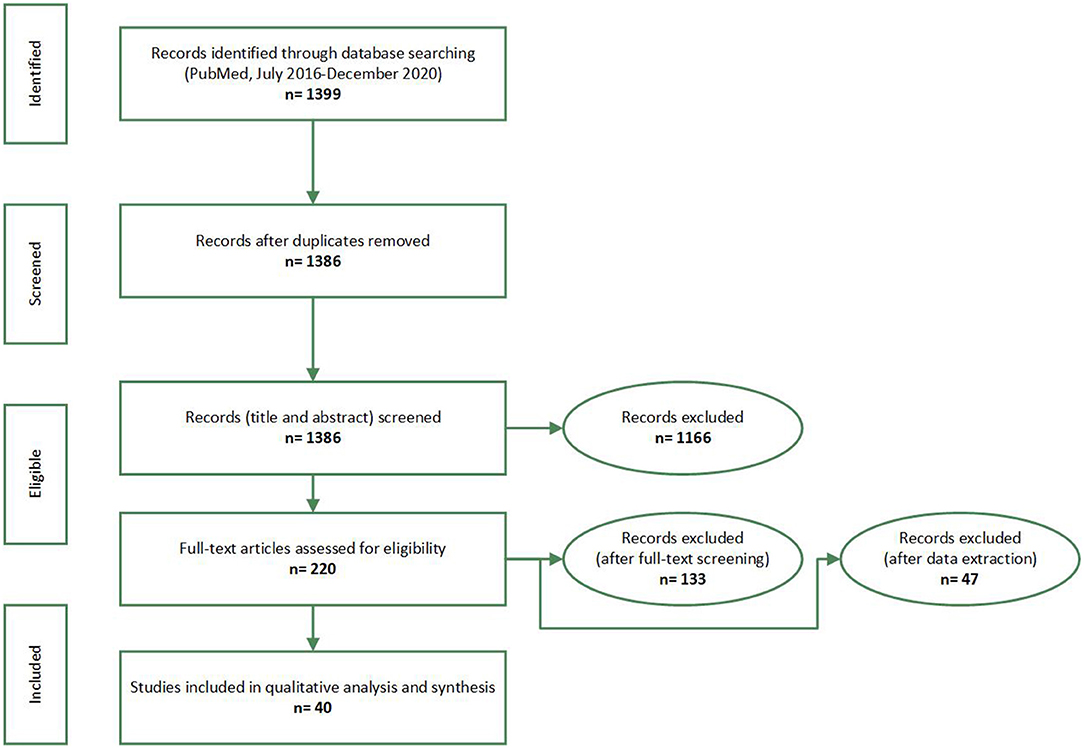
Figure 1 . PRISMA flow-diagram. Promoting university students' mental health: a systematic literature review introducing the 4M-Model of individual-level interventions, Dubai, United Arab Emirates, 2020.
Of the 40 studies, nine studies were conducted in USA, eight in United Kingdom, four in Canada, three in Australia, five in Germany, four in China, and one in each of Turkey, Hungary, Israel, Ireland, Japan, South Korea and Netherlands. The quality of evidence is very high in terms of internal validity because most of the studies ( 25 ) employed RCT, five studies used a quasi-experimental method, two had a cross sectional design, and eight studies utilized a pre-post design without a control group.
The external validity of the papers could be considered low/ moderate. Since most of the studies indicated the experience of only one institution; generalization of the findings is limited. The only exceptions were one study that was conducted in Israel which included three institutions and one conducted in UK which included eight universities. After thoroughly reflecting upon the interventions under investigation across all 40 resulting studies, the authors qualitatively synthesized a holistic framework. This involved inductively identifying four overlapping categories of interventions. Each category was in turn coded with a label that appeared to be most fit to the encapsulated interventions and that is in harmony with the codes of the rest of the categories (i.e., alliteration).
Accordingly, each study was linked to at least one of four overlapping categories based on the nature of the intervention(s) under investigation ( Table 1 ). The first category, coded as Mindfulness, included individual-level interventions that used mindfulness as a strategy to promote mental health. Mindfulness, in this context, refers to any intervention that aims to promote living in the moment or “now” and adopting acceptance and a non-judgmental attitude to guide action. The popular Mindfulness Based Stress Reduction (MBSR) curriculum was used in four studies ( 8 , 42 – 45 ). Mindfulness Based Cognitive Therapy (MBCT) which focuses on reframing thoughts along with becoming aware of the nature and quality of them was found to also be effective in two studies ( 46 , 47 ). In three studies, the intervention(s) made use of imagery and self-guidance ( 48 – 51 ), whereas two other studies explored the effectiveness of Acceptance and Commitment Therapy (ACT) ( 6 ) to improve the psychological flexibility, school engagement, and mental health among University students.
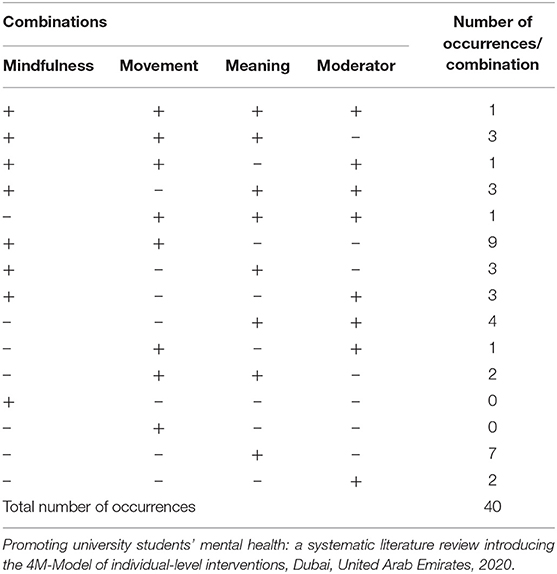
Table 1 . Distribution of the output of the systematic literature review depending on the nature of the intervention(s) under investigation.
The second category of studies was coded as Movement and included individual-level interventions which have a predominant physical element and solicit change in bodily sensations including but not limited to yoga, fitness, dance, kickboxing, and aerobics and breathing exercises. While Tong et al. ( 52 ) exclusively looked at the effect of Yoga and Fitness on mental health, five sets of researchers ( 8 , 42 , 43 , 45 , 46 ) looked at breathing and simple yoga as part of their mindfulness course. Sleep was studied in connection to mental health in two studies ( 53 , 54 ) as it has been found to be a precursor to many mental health problems with insomnia and the quality of sleep put on top of the list affecting sleep hygiene. Behavioral activation, a personalized therapeutic tool mainly used in the treatment of depression targeting behaviors that feed into the condition, was found to be effective in three studies that were reviewed ( 55 – 57 ) involving students with mild depression. The goal of Behavioral Activation is engaging in enjoyable activities with a part of the process focusing on getting past obstacles that may impede that enjoyment. One study included peer-led support ( 56 ) and online delivery of the course ( 57 ), where both appeared to be efficacious. Only one study by Chalo et al. ( 58 ) used Biofeedback intervention, that involved measuring students' quantifiable bodily functions to convey information to them in real-time as a solution to help students manage their physiological response to anxiety and stress.
The third category was coded as Meaning and included studies that investigate individual-level interventions that focus on the counselor addressing connections and associations between variables and enabling the student to reframe cognitions. Psychoeducation was widely utilized with cognitive training as the most common ( 54 , 59 – 63 ). Eustis et al. ( 49 ) focused their study on the student's self-awareness, while Demir and Ercan ( 64 ) explored communication techniques among students. In addition, three studies explored the feasibility of having courses embedded within the curriculum ( 38 , 48 , 50 ) to improve the mental health of students, while nine studies explored the effect of elective courses that aimed at stress reduction ( 18 , 43 , 50 , 56 , 58 , 65 – 69 ).
The last category of studies was coded as Moderator which referred to any element of support that was deployed in conjunction with the counselor, in an individual-level intervention, that acts as a moderator between the student and the counselor. Pet therapy was explored in three studies ( 70 – 72 ) to assess well-being, and an extensive use of the computer to deliver courses such as ACT, Psychoeducation, and Cognitive Behavior Therapy (CBT) which are all traditionally effective in psychotherapy, were found to be efficacious online in 10 studies ( 44 , 50 , 57 , 61 , 73 – 78 ) highlighting the significance of the potential of web-based interventions to impart psychotherapy to a wider audience.
This literature review showed that elements of Mindfulness were a major part of the 23 studies, Meaning was predominant in 24 studies, while Movement was an important feature in 17 studies. An element of support complementary to the therapist, either in the form of a pet (canine) or a web/phone application (i.e., Moderator), was part of 16 interventions. Commonly used approaches were Mindfulness based therapies, ACT, Cognitive Behavior Therapy, and Psychoeducation. The duration of the interventions investigated in the included studies ranged between 1 and 12 weeks, with most of the studies spanning between 6 and 8 weeks. Nine studies had just one element, and only one study ( 49 ) had all the four elements included ( Figure 2 ), which the authors perceived as a “lucky find.”
Figure 2 . The 4M-Model generated from this study's qualitative synthesis, visually illustrated as a four-leaf clover which is a symbol of luck. Promoting university students' mental health: a systematic literature review introducing the 4M-Model of individual-level interventions, Dubai, United Arab Emirates, 2020.
Thirty-one studies had overlapping elements indicating that these elements are not mutually exclusive and rather interlinked and are blended with the intention of enhancing the effectiveness of a program.
The output of this Systematic Literature Review revealed diverse interventions. Most of these interventions were hybrid versions of existing evidence-based interventions. A few of the identified articles reflected upon contextualized home-grown interventions. There appeared to be a lack of consensus on a common model/ approach to effectively improve the mental health and wellness of university students ( 61 ) who are known to have their own set of challenges. Hence, this paper provides an outline of practices that have been deployed in this direction, illustrating them from a holistic perspective. Elements of mindfulness, meaning, movement, and use of a moderator were seen to overlap in the studies. The blending of these elements was proven to be effective in improving metacognitive awareness, emotional regulation ( 79 ), concentration, and mental clarity ( 80 ), and decreasing emotional reactivity ( 81 ) and rumination (through disengagement with persistent negative thoughts) ( 82 ) and in turn reducing depression, stress, and anxiety ( 83 ). It has also shown to foster social connectedness and the ability to express oneself in various social situations ( 84 ) thereby reducing stress and anxiety and increasing patience, gratitude, and body awareness ( 85 ). With so many elements that need to be taken into consideration, the researchers have attempted to comprehend the output of this review from the field theory point-of-view where the “organism and environment are perceived as part of an interacting field” ( 86 ).
Moreover, Counseling strategies and interventions are meant to emphasize on the growth of an individual. The human potential for self-actualization, a concept understood by Abraham Maslow as a change process that aims at making a person “aware of what is going on inside himself” [Maslow, as cited in Seaman ( 87 ), p. 3] is core to Counseling interventions, which is where the four elements blend to become crucial to the process of self-awareness and eventually self-growth.
The results of the study indicate that self-awareness through mindfulness is an important foundation upon which all other elements build up to improve mental health of students. This was not a surprising find because this is in alignment with the results of many previously conducted studies ( 88 , 89 ). Mindfulness seems to be the new mantra and has been intensively researched ( 90 ). However, despite a substantial amount of theoretical work conducted to merge Buddhist and Western conceptual viewpoints to psychotherapy ( 91 ), there is minimal literature on how it can translate to practice making this review an important addition to the limited knowledge around the topic of psychological interventions that have been found to be effective among university students. MBSR has proven to reduce stress and anxiety among university students by fostering insight and concentration along with physiologic relaxation ( 92 ). Teaching students to live in the present moment by reframing thoughts (i.e., MBCT) has been found to be effective in reducing depression ( 93 ). It also lessens the risk of relapse with comparable efficacy to antidepressant medication ( 94 ) which, in itself, is a breakthrough for psychotherapy. ACT which focuses on acceptance has been found to improve coping, self-regulation, psychological flexibility, and school engagement ( 6 ). Counseling young adults, in particular students at the university level, would benefit by basing it on Engel's biopsychosocial viewpoint which includes taking into consideration the hormonal changes (biological), identity crisis, and the challenges arising from intimacy and isolation (psychological) which have been hypothesized in Eric Erickson's psychosocial stages of development for this age group. The new age technological challenges of peer-pressure over social media sites and the demands of fitting in and changing family dynamics (sociological) also need to be taken into consideration when conceptualizing a Counseling program for this target group.
Moreover, this transition stage between adolescence and adulthood, also referred to as “emerging adulthood” ( 95 ), is considered to be a period of accepting responsibility for one's actions and livelihood, developing belief systems and values independent of parental and external influences, and establishing relationships with parents on equal grounds. Young university students who are still financially dependent and living with parents during this period are arbitrarily considered to be adolescents if adult responsibilities are not yet accessed. These intangible markers gradually develop. The entailed process could last many years until the corresponding responsibilities are effectively adopted. As such, the range between adolescence and adulthood becomes wider than typically defined, stretching from the beginning of puberty to the early twenties ( 96 ).
Counseling has been traditionally associated as a profession that requires the physical presence of a minimum of two people in a professional relationship to talk through and process experiences to gain insight and understanding. However, in this review, it is evident that web-based interventions seem to produce an equally effective result ( 97 ) as observed in 16 studies of the literature review which could be utilized as a complementary medium widening the scope of practice of counselors and psychotherapists. This could also help in minimizing the stigma associated with getting undesirably labeled and help in reducing psychological self-restraint which has been termed as ‘online disinhibition effect' ( 98 ). Web-based mental health interventions also are becoming a preferred medium for students to gain services and information ( 99 ) as they accommodate their busy schedules ( 100 ).
Another observation was that even though most of the interventions were conducted only for a short period of time, the effectiveness of the interventions was established. Embedding interventions within the curriculum has been suggested ( 101 ) which makes this review even more pertinent for innovations in curriculum planning. This may also help in alleviating the stigma that is attached to Counseling services which is often a barrier that prevents students from reaching out for help ( 102 ). This aligns with Vygotsky's notion of Zone of Proximal Development ( 103 ) which refers to pedagogical support being beneficial for activities, in this context, psychoeducation of positive behaviors that facilitate help seeking behaviors before they can start using them independently.
The above observations prompted the researchers to recognize that the four identified elements when combined would result in a holistic approach of addressing the individual from a biopsychosocial point-of-view. This was depicted in the form of the 4M-Model to guide counselors to develop and implement university-level interventions that could help to reduce stress, anxiety, and depression as well as improve emotion regulation and self-awareness to address the mental health needs of young adults. It would be worthwhile for future research studies to validate the suggested 4M-Model through a similar systematic review of the literature relying on a combination of databases ( 104 ). The analysis in this case would be deductive where the model conceived from this study can be used as a preset template. Also, for validation purposes, it is recommended to conduct follow-up studies aimed at evaluating the efficaciousness of a tailor-made assortment of interventions that can be linked to all elements of the 4M-Model. For that purpose, it would be useful to adapt a mixed methods approach to research, where quantitative and qualitative findings will be integrated to obtain a holistic perspective of the output, outcome, and impact of such university-based, individual-student level mental health initiatives.
Findings of this review reveal the 4M-Model that happen to address all aspects of holistic well-being: physical, psychological, emotional, and social. Effectiveness of the varied interventions that have been reviewed in this study indicate that if a comprehensive approach toward intervention including mindfulness, movement, moderator, and meaning is adapted, then it would not only help students to be supported in a holistic manner but would help counselors plan and execute their programs in a focused approach to address the needs of any university student population who are increasingly overwhelmed and burned out with the stressors from their outside worlds as well as from within. The findings from the review add to the growing evidence for the urgent need of an intervention model that can serve as a directive for counselors and students.
Data Availability Statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author/s.
Author Contributions
BN and FO conceptualized the study, conducted the review, performed the qualitative meta-synthesis, and prepared and approved the manuscript. Both authors contributed to the article and approved the submitted version.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
The authors would like to extensd their gratitude to three of their colleagues: Dr. Lisa Jackson, Dr. Leigh Powell, and Ms. Mersiha Kovacevic, for their active role, and valuable reflections and feedback in reviewing the complete manuscript.
1. WHO. Gender and Women's Health . World Health Organization (2009). Available from: http://www.who.int/mental_health/prevention/genderwomen/en/ (accessed May 11, 2021).
2. Breslau J, Lane M, Sampson N, Kessler RC. Mental disorders and subsequent educational attainment in a US national sample. J Psychiatr Res. (2008) 42:708–16. doi: 10.1016/j.jpsychires.2008.01.016
PubMed Abstract | CrossRef Full Text | Google Scholar
3. Kitzrow MA. The mental health needs of today's college students: challenges and recommendations. NASPA J . (2003) 41:167–81. doi: 10.2202/1949-6605.1310
CrossRef Full Text | Google Scholar
4. Thomas MR, Dyrbye LN, Huntington JL, Lawson KL, Novotny PJ, Sloan JA, et al. How do distress and well-being relate to medical student empathy? A multicenter study. J Gen Intern Med. (2007) 22:177–83. doi: 10.1007/s11606-006-0039-6
5. Byrd DR, McKinney KJ. Individual, interpersonal, and institutional level factors associated with the mental health of college students. J Am Coll Health. (2012) 60:185–93. doi: 10.1080/07448481.2011.584334
6. Gregoire S, Lachance L, Bouffard T, Dionne F. The use of acceptance and commitment therapy to promote mental health and school engagement in university students: a multisite randomized controlled trial. Behav Ther. (2018) 49:360–72. doi: 10.1016/j.beth.2017.10.003
7. Seligman MEP, Ernst RM, Gillham J, Reivich K, Linkins M. Positive education: positive psychology and classroom interventions. Oxford Rev Educ. (2009) 35:293–311. doi: 10.1080/03054980902934563
8. Galante J, Dufour G, Vainre M, Wagner AP, Stochl J, Benton A, et al. A mindfulness-based intervention to increase resilience to stress in university students (the Mindful Student Study): a pragmatic randomised controlled trial. Lancet Public Health. (2018) 3:e72–81. doi: 10.1016/S2468-2667(17)30231-1
9. Reavley NJ, Jorm AF. Recognition of mental disorders and beliefs about treatment and outcome: findings from an Australian national survey of mental health literacy and stigma. Aust N Z J Psychiatry. (2011) 45:947–56. doi: 10.3109/00048674.2011.621060
10. Cvetkovski S, Reavley NJ, Jorm AF. The prevalence and correlates of psychological distress in Australian tertiary students compared to their community peers. Aust N Z J Psychiatry. (2012) 46:457–67. doi: 10.1177/0004867411435290
11. Hamaideh SH. Stressors and reactions to stressors among university students. Int J Soc Psychiatry. (2011) 57:69–80. doi: 10.1177/0020764009348442
12. Tupler LA, Hong JY, Gibori R, Blitchington TF, Krishnan KR. Suicidal ideation and sex differences in relation to 18 major psychiatric disorders in college and university students: anonymous web-based assessment. J Nerv Ment Dis. (2015) 203:269–78. doi: 10.1097/NMD.0000000000000277
13. Oades LG, Robinson P, Green S, Spence GB. Towards a positive university. In: Positive Psychology in Higher Education . Routledge (2014). p. 15–22. doi: 10.4324/9781315829692-7
14. Levine A, Cureton JS. What we know: about today's college students. Education. (1998) 3:4–9. doi: 10.1177/108648229800300103
15. Gallagher RP, Gill A, Sysko H. National Survey of Counseling Centre Directors (2000).
Google Scholar
16. Center for Collegiate Mental Health. 2017 Annual Report . (Publication No. STA 18-166) (2018).
17. Blanco C, Okuda M, Wright C, Hasin DS, Grant BF, Liu SM, et al. Mental health of college students and their non-college-attending peers: results from the National Epidemiologic Study on Alcohol and Related Conditions. Arch Gen Psychiatry. (2008) 65:1429–37. doi: 10.1001/archpsyc.65.12.1429
18. Nguyen-Feng VN, Greer CS, Frazier P. Using online interventions to deliver college student mental health resources: evidence from randomized clinical trials. Psychol Serv. (2017) 14:481–9. doi: 10.1037/ser0000154
19. Pledge DS, Lapan RT, Heppner PP, Kivlighan D, Roehlke HJ. Stability and severity of presenting problems at a university counseling center: a 6-year analysis. Prof Psychol Res Pract. (1998) 29:386–9. doi: 10.1037/0735-7028.29.4.386
20. Storrie K, Ahern K, Tuckett A. A systematic review: students with mental health problems–a growing problem. Int J Nurs Pract. (2010) 16:1–6. doi: 10.1111/j.1440-172X.2009.01813.x
21. Megivern D, Pellerito S, Mowbray C. Barriers to higher education for individuals with psychiatric disabilities. Psychiatr Rehabil J. (2003) 26:217–31. doi: 10.2975/26.2003.217.231
22. Eisenberg D, Downs MF, Golberstein E, Zivin K. Stigma and help seeking for mental health among college students. Med Care Res Rev. (2009) 66:522–41. doi: 10.1177/1077558709335173
23. Tjia J, Givens JL, Shea JA. Factors associated with undertreatment of medical student depression. J Am Coll Health. (2005) 53:219–24. doi: 10.3200/JACH.53.5.219-224
24. Eisenberg D, Hunt J, Speer N, Zivin K. Mental health service utilization among college students in the United States. J Nerv Ment Dis. (2011) 199:301–8. doi: 10.1097/NMD.0b013e3182175123
25. Repper J, Carter T. A review of the literature on peer support in mental health services. J Mental Health. (2011) 20:392–411. doi: 10.3109/09638237.2011.583947
26. Eisenberg D, Speer N, Hunt JB. Attitudes and beliefs about treatment among college students with untreated mental health problems. Psychiatr Serv. (2012) 63:711–3. doi: 10.1176/appi.ps.201100250
27. Pescosolido BA, Boyer CA. Understanding the context and dynamic social processes of mental health treatment. In: A Handbook for the Study of Mental Health: Social Contexts, Theories, and Systems , Vol. 2 (2010). p. 420–38. doi: 10.1017/CBO9780511984945.026
28. Patton GC, Sawyer SM, Santelli JS, Ross DA, Afifi R, Allen NB, et al. Our future: a lancet commission on adolescent health and wellbeing. Lancet. (2016) 387:2423–78. doi: 10.1016/S0140-6736(16)00579-1
29. Conley CS, Durlak JA, Kirsch AC. A meta-analysis of universal mental health prevention programs for higher education students. Prev Sci. (2015) 16:487–507. doi: 10.1007/s11121-015-0543-1
30. Davies EB, Morriss R, Glazebrook C. Computer-delivered and web-based interventions to improve depression, anxiety, and psychological well-being of university students: a systematic review and meta-analysis. J Med Internet Res. (2014) 16:e130. doi: 10.2196/jmir.3142
31. Dooris M. Holistic and sustainable health improvement: the contribution of the settings-based approach to health promotion. Perspect Public Health. (2009) 129:29–36. doi: 10.1177/1757913908098881
32. Fernandez A, Howse E, Rubio-Valera M, Thorncraft K, Noone J, Luu X, et al. Setting-based interventions to promote mental health at the university: a systematic review. Int J Public Health. (2016) 61:797–807. doi: 10.1007/s00038-016-0846-4
33. Moher D, Liberati A, Tetzlaff J, Altman DG, Group P. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. (2009) 6:e1000097. doi: 10.1371/journal.pmed.1000097
34. Jadad AR, Moore RA, Carroll D, Jenkinson C, Reynolds DJ, Gavaghan DJ, et al. Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials. (1996) 17:1–12. doi: 10.1016/0197-2456(95)00134-4
35. Green LW, Glasgow RE. Evaluating the relevance, generalization, and applicability of research: issues in external validation and translation methodology. Eval Health Prof. (2006) 29:126–53. doi: 10.1177/0163278705284445
36. Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. (2006) 3:2:77–101. doi: 10.1191/1478088706qp063oa
37. Theoret C, Ming X. Our education, our concerns: the impact on medical student education of COVID-19. Med Educ. (2020) 54:591–2. doi: 10.1111/medu.14181
38. Gordon M. Are we talking the same paradigm? Considering methodological choices in health education systematic review. Med Teach. (2016) 38:746–50. doi: 10.3109/0142159X.2016.1147536
39. Gheondea-Eladi A. Is qualitative research generalizable? Jurnalul Practicilor Comunitare Pozitive. (2014) 14:114–24.
40. Seaman J, Dettweiler U, Humberstone B, Martin B, Prince H, Quay J. Joint recommendations on reporting empirical research in outdoor, experiential, environmental, and adventure education journals. J Exp Educ. (2020) 43:348–64. doi: 10.1177/1053825920969443
41. Yilmaz K. Comparison of Quantitative and Qualitative Research Traditions: epistemological, theoretical, and methodological differences. Eur J Educ. (2013) 48:311–25.
42. Falsafi N. A randomized controlled trial of mindfulness versus yoga: effects on depression and/or anxiety in college students. J Am Psychiatr Nurses Assoc. (2016) 22:483–97. doi: 10.1177/1078390316663307
43. van Dijk I, Lucassen PL, Akkermans RP, van Engelen BG, van Weel C, Speckens AE. Effects of mindfulness-based stress reduction on the mental health of clinical clerkship students: a cluster-randomized controlled trial. AEMAcad Med. (2017) 92:1012–21. doi: 10.1097/ACM.0000000000001546
44. Malpass A, Binnie K, Robson L. Medical students' experience of mindfulness training in the UK: well-being, coping reserve, and professional development. Educ Res Int. (2019) 2019. doi: 10.1155/2019/4021729
45. Alkoby A, Pliskin R, Halperin E, Levit-Binnun N. An eight-week mindfulness-based stress reduction (MBSR) workshop increases regulatory choice flexibility. Emotion. (2019) 19:593–604. doi: 10.1037/emo0000461
46. O'Driscoll M, Sahm LJ, Byrne H, Lambert S, Byrne S. Impact of a mindfulness-based intervention on undergraduate pharmacy students' stress and distress: quantitative results of a mixed-methods study. Curr Pharm Teach Learn. (2019) 11:876–87. doi: 10.1016/j.cptl.2019.05.014
47. Gu Y, Xu G, Zhu Y. A randomized controlled trial of mindfulness-based cognitive therapy for college students with ADHD. J Atten Disord. (2018) 22:388–99. doi: 10.1177/1087054716686183
48. Hall BJ, Xiong P, Guo X, Sou EKL, Chou UI, Shen Z. An evaluation of a low intensity mHealth enhanced mindfulness intervention for Chinese university students: a randomized controlled trial. Psychiatry Res. (2018) 270:394–403. doi: 10.1016/j.psychres.2018.09.060
49. Eustis EH, Hayes-Skelton SA, Orsillo SM, Roemer L. Surviving and thriving during stress: a randomized clinical trial comparing a brief web-based therapist-assisted acceptance-based behavioral intervention versus waitlist control for college students. Behav Ther. (2018) 49:889–903. doi: 10.1016/j.beth.2018.05.009
50. Cavanagh K, Churchard A, O'Hanlon P, Mundy T, Votolato P, Jones F, et al. A randomised controlled trial of a brief online mindfulness-based intervention in a non-clinical population: replication and extension. Mindfulness. (2018) 9:1191–205. doi: 10.1007/s12671-017-0856-1
51. Dvorakova K, Kishida M, Li J, Elavsky S, Broderick PC, Agrusti MR, et al. Promoting healthy transition to college through mindfulness training with first-year college students: pilot randomized controlled trial. J Am Coll Health. (2017) 65:259–67. doi: 10.1080/07448481.2017.1278605
52. Tong J, Qi X, He Z, Chen S, Pedersen SJ, Cooley PD, et al. The immediate and durable effects of yoga and physical fitness exercises on stress. J Am Coll Health. (2020) 11:1–9. doi: 10.1080/07448481.2019.1705840
53. Friedrich A, Classen M, Schlarb AA. Sleep better, feel better? Effects of a CBT-I and HT-I sleep training on mental health, quality of life and stress coping in university students: a randomized pilot controlled trial. BMC Psychiatry. (2018) 18:268. doi: 10.1186/s12888-018-1860-2
54. Morris J, Firkins A, Millings A, Mohr C, Redford P, Rowe A. Internet-delivered cognitive behavior therapy for anxiety and insomnia in a higher education context. Anxiety Stress Coping. (2016) 29:415–31. doi: 10.1080/10615806.2015.1058924
55. Takagaki K, Okamoto Y, Jinnin R, Mori A, Nishiyama Y, Yamamura T, et al. Behavioral activation for late adolescents with subthreshold depression: a randomized controlled trial. Eur Child Adolesc Psychiatry. (2016) 25:1171–82. doi: 10.1007/s00787-016-0842-5
56. Byrom N. An evaluation of a peer support intervention for student mental health. J Ment Health. (2018) 27:240–6. doi: 10.1080/09638237.2018.1437605
57. Puspitasari AJ, Kanter JW, Busch AM, Leonard R, Dunsiger S, Cahill S, et al. A randomized controlled trial of an online, modular, active learning training program for behavioral activation for depression. J Consult Clin Psychol. (2017) 85:814–25. doi: 10.1037/ccp0000223
58. Chalo P, Pereira A, Batista P, Sancho L. Brief biofeedback intervention on anxious freshman university students. Appl Psychophysiol Biofeedback. (2017) 42:163–8. doi: 10.1007/s10484-017-9361-5
59. Bettis AH, Coiro MJ, England J, Murphy LK, Zelkowitz RL, Dejardins L, et al. Comparison of two approaches to prevention of mental health problems in college students: enhancing coping and executive function skills. J Am Coll Health. (2017) 65:313–22. doi: 10.1080/07448481.2017.1312411
60. Biro E, Veres-Balajti I, Adany R, Kosa K. Social cognitive intervention reduces stress in Hungarian university students. Health Promot Int. (2017) 32:73–8. doi: 10.1093/heapro/dau006
61. Farrer LM, Gulliver A, Katruss N, Fassnacht DB, Kyrios M, Batterham PJ. A novel multi-component online intervention to improve the mental health of university students: randomised controlled trial of the Uni Virtual Clinic. Internet Interv. (2019) 18:100276. doi: 10.1016/j.invent.2019.100276
62. Kotter T, Niebuhr F. Resource-oriented coaching for reduction of examination-related stress in medical students: an exploratory randomized controlled trial. Adv Med Educ Pract. (2016) 7:497–504. doi: 10.2147/AMEP.S110424
63. Kuhlmann SM, Huss M, Burger A, Hammerle F. Coping with stress in medical students: results of a randomized controlled trial using a mindfulness-based stress prevention training (MediMind) in Germany. BMC Med Educ. (2016) 16:316. doi: 10.1186/s12909-016-0833-8
64. Demir S, Ercan F. The effect of a self-awareness and communication techniques course on the communication skills and ways of coping with stress of nursing students: An interventional study in Ankara, Turkey. J Pak Med Assoc. (2019) 69:659–65.
PubMed Abstract
65. Shannon S, Hanna D, Haughey T, Leavey G, McGeown C, Breslin G. Effects of a mental health intervention in athletes: applying self-determination theory. Front Psychol. (2019) 10:1875. doi: 10.3389/fpsyg.2019.01875
66. Tolgou T, Rohrmann S, Stockhausen C, Krampen D, Warnecke I, Reiss N. Physiological and psychological effects of imagery techniques on health anxiety. Psychophysiology. (2018) 55:e12984. doi: 10.1111/psyp.12984
67. Scholz M, Neumann C, Wild K, Garreis F, Hammer CM, Ropohl A, et al. Teaching to relax: development of a program to potentiate stress-results of a feasibility study with medical undergraduate students. Appl Psychophysiol Biofeedback. (2016) 41:275–81. doi: 10.1007/s10484-015-9327-4
68. Guo YF, Zhang X, Plummer V, Lam L, Cross W, Zhang JP. Positive psychotherapy for depression and self-efficacy in undergraduate nursing students: a randomized, controlled trial. Int J Ment Health Nurs. (2017) 26:375–83. doi: 10.1111/inm.12255
69. Kim S KH, Lee H, Lee H, Noh D. Effectiveness of a brief stress management intervention in male college students. Perspect Psychiatr Care. (2018) 54:88–94. doi: 10.1111/ppc.12212
70. Grajfoner D, Harte E, Potter LM, McGuigan N. The effect of dog-assisted intervention on student well-being, mood, and anxiety. Int J Environ Res Public Health. (2017) 14:483. doi: 10.3390/ijerph14050483
71. Wood E, Ohlsen S, Thompson J, Hulin J, Knowles L. The feasibility of brief dog-assisted therapy on university students stress levels: the PAwS study. J Ment Health. (2018) 27:263–8. doi: 10.1080/09638237.2017.1385737
72. Binfet JT PH, Cebry A, Struik K, McKay C. Reducing university students' stress through a drop-in canine-therapy program. J Mental Health. (2018) 27:197–204. doi: 10.1080/09638237.2017.1417551
73. Viskovich S, Pakenham KI. Pilot evaluation of a web-based acceptance and commitment therapy program to promote mental health skills in university students. J Clin Psychol. (2018) 74:2047–69. doi: 10.1002/jclp.22656
74. McCall HC, Richardson CG, Helgadottir FD, Chen FS. Evaluating a web-based social anxiety intervention among university students: randomized controlled trial. J Med Int Res. (2018) 20:e91. doi: 10.2196/jmir.8630
75. Lee RA, Jung ME. Evaluation of an mHealth App (DeStressify) on university students' mental health: pilot trial. JMIR Ment Health. (2018) 5:e2. doi: 10.2196/mental.8324
76. Viskovich S, Pakenham KI. Randomized controlled trial of a web-based Acceptance and Commitment Therapy (ACT) program to promote mental health in university students. J Clin Psychol. (2020) 76:929–51. doi: 10.1002/jclp.22848
77. Fulmer R, Joerin A, Gentile B, Lakerink L, Rauws M. Using psychological artificial intelligence (tess) to relieve symptoms of depression and anxiety: randomized controlled trial. JMIR Ment Health. (2018) 5:e64. doi: 10.2196/mental.9782
78. Juncos DG, Heinrichs GA, Towle P, Duffy K, Grand SM, Morgan MC, et al. Acceptance and commitment therapy for the treatment of music performance anxiety: a pilot study with student vocalists. Front Psychol. (2017) 8:986. doi: 10.3389/fpsyg.2017.00986
79. Farb NA, Anderson AK, Mayberg H, Bean J, McKeon D, Segal ZV. Minding one's emotions: mindfulness training alters the neural expression of sadness. Emotion. (2010) 10:25–33. doi: 10.1037/a0017151
80. Moore A, Malinowski P. Meditation, mindfulness and cognitive flexibility. Conscious Cogn. (2009) 18:176–86. doi: 10.1016/j.concog.2008.12.008
81. Ortner CNM, Kilner SJ, Zelazo PD. Mindfulness meditation and reduced emotional interference on a cognitive task. Motiv Emot. (2007) 31:271–83. doi: 10.1007/s11031-007-9076-7
82. Chambers R, Lo BC, Allen NB. The impact of intensive mindfulness training on attentional control, cognitive style, and affect. Cogn Ther Res. (2008) 32:303–22. doi: 10.1007/s10608-007-9119-0
83. Cohen JS, Miller L. Interpersonal mindfulness training for well-being: a pilot study with psychology graduate students. Teach Coll Rec. (2009) 111:2760–74.
84. Dekeyser M, Raes F, Leijssen M, Leyson S, Dewulf D. Mindfulness skills and interpersonal behavior. Person Ind Differ. (2008) 44:1235–45. doi: 10.1016/j.paid.2007.11.018
85. Rothaupt JW, Morgan MM. Counselors' and counselor educators' practice of mindfulness: a qualitative inquiry. Counsel Values. (2007) 52:40–54. doi: 10.1002/j.2161-007X.2007.tb00086.x
86. Bourgault du Coudray C. Theory and praxis in experiential education: some insights from gestalt therapy. J Exp Educ. (2020) 43:156–70. doi: 10.1177/1053825920904387
87. Seaman J. Is group therapy democratic? enduring consequences of outward Bound's alignment with the human potential movement. A response to “how to be nice and get what you want: structural referents of ‘Self' and ‘Other' in experiential education as (Un) democratic practice. Democr. Educ. (2016) 24:13. Available online at: https://democracyeducationjournal.org/home/vol24/iss2/13
88. Groves P. Mindfulness in psychiatry - where are we now? BJPsych Bull. (2016) 40:289–92. doi: 10.1192/pb.bp.115.052993
89. Walsh R, Shapiro SL. The meeting of meditative disciplines and Western psychology: a mutually enriching dialogue. Am Psychol. (2006) 61:227–39. doi: 10.1037/0003-066X.61.3.227
90. Powell A. When Science Meets Mindfulness: The Harvard Gazette (2018. Available from: https://news.harvard.edu/gazette/story/2018/04/harvard-researchers-study-how-mindfulness-may-change-the-brain-in-depressed-patients/ (accessed May 11, 2021).
91. Epstein M. Psychotherapy Without the Self: A Buddhist Perspective . Yale University Press (2008).
92. Rosenzweig S, Reibel DK, Greeson JM, Brainard GC, Hojat M. Mindfulness-based stress reduction lowers psychological distress in medical students. Teach Learn Med. (2003) 15:88–92. doi: 10.1207/S15328015TLM1502_03
93. Tickell A, Ball S, Bernard P, Kuyken W, Marx R, Pack S, et al. The effectiveness of mindfulness-based cognitive therapy (MBCT) in real-world healthcare services. Mindfulness. (2020) 11:279–90. doi: 10.1007/s12671-018-1087-9
94. Kuyken W, Warren FC, Taylor RS, Whalley B, Crane C, Bondolfi G, et al. Efficacy of mindfulness-based cognitive therapy in prevention of depressive relapse: an individual patient data meta-analysis from randomized trials. JAMA Psychiatry. (2016) 73:565–74. doi: 10.1001/jamapsychiatry.2016.0076
95. Arnett JJ. Are college students adults? Their conceptions of the transition to adulthood. J Adult Dev. (1994) 1:213–24. doi: 10.1007/BF02277582
96. Arnett J. Reckless behavior in adolescence: a developmental perspective. Dev Rev. (1992) 12:339–73. doi: 10.1016/0273-2297(92)90013-R
97. Astramovich R, Jones W, Coker K. Technology-Enhanced Consultation in Counselling: A Comparative Study. Guid Counsel. (2004) 19:72–80.
98. Suler J. The online disinhibition effect. Cyberpsychol Behav. (2004) 7:321–6. doi: 10.1089/1094931041291295
99. Ryan ML, Shochet IM, Stallman HM. Universal online interventions might engage psychologically distresseduniversity students who are unlikely to seek formal help. Adv Mental Health. (2010) 9:73–83. doi: 10.5172/jamh.9.1.73
100. Amstadter AB, Broman-Fulks J, Zinzow H, Ruggiero KJ, Cercone J. Internet-based interventions for traumatic stress-related mental health problems: a review and suggestion for future research. Clin Psychol Rev. (2009) 29:410–20. doi: 10.1016/j.cpr.2009.04.001
101. Chodkiewicz ARB. Positive psychology school-based interventions: a reflection on current success and future directions. Rev Educ. (2017) 5:60–86. doi: 10.1002/rev3.3080
102. Sullivan C, Mancillas A. Stigma toward seeking mental health services among graduate counseling students. VISTAS. (2015) 83.
103. Vygotsky LS. Mind in Society: The Development of Higher Psychological Processes . Harvard University Press (1980). doi: 10.2307/j.ctvjf9vz4.5
104. Bramer WM, Rethlefsen ML, Kleijnen J, Franco OH. Optimal database combinations for literature searches in systematic reviews: a prospective exploratory study. Syst Rev. (2017) 6:245. doi: 10.1186/s13643-017-0644-y
PubMed Abstract | CrossRef Full Text
Keywords: mental health, health and well-being, holism, university students, mindfulness, higher education, student support
Citation: Nair B and Otaki F (2021) Promoting University Students' Mental Health: A Systematic Literature Review Introducing the 4M-Model of Individual-Level Interventions. Front. Public Health 9:699030. doi: 10.3389/fpubh.2021.699030
Received: 22 April 2021; Accepted: 31 May 2021; Published: 25 June 2021.
Reviewed by:
Copyright © 2021 Nair and Otaki. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY) . The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Bhavana Nair, bhavana.nair@mbru.ac.ae
† ORCID: Bhavana Nair orcid.org/0000-0002-3381-8293 Farah Otaki orcid.org/0000-0002-8944-4948
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
- Research article
- Open access
- Published: 24 October 2019
A scoping review of the literature on the current mental health status of physicians and physicians-in-training in North America
- Mara Mihailescu ORCID: orcid.org/0000-0001-6878-1024 1 &
- Elena Neiterman 2
BMC Public Health volume 19 , Article number: 1363 ( 2019 ) Cite this article
26k Accesses
57 Citations
11 Altmetric
Metrics details
This scoping review summarizes the existing literature regarding the mental health of physicians and physicians-in-training and explores what types of mental health concerns are discussed in the literature, what is their prevalence among physicians, what are the causes of mental health concerns in physicians, what effects mental health concerns have on physicians and their patients, what interventions can be used to address them, and what are the barriers to seeking and providing care for physicians. This review aims to improve the understanding of physicians’ mental health, identify gaps in research, and propose evidence-based solutions.
A scoping review of the literature was conducted using Arksey and O’Malley’s framework, which examined peer-reviewed articles published in English during 2008–2018 with a focus on North America. Data were summarized quantitatively and thematically.
A total of 91 articles meeting eligibility criteria were reviewed. Most of the literature was specific to burnout ( n = 69), followed by depression and suicidal ideation ( n = 28), psychological harm and distress ( n = 9), wellbeing and wellness ( n = 8), and general mental health ( n = 3). The literature had a strong focus on interventions, but had less to say about barriers for seeking help and the effects of mental health concerns among physicians on patient care.
Conclusions
More research is needed to examine a broader variety of mental health concerns in physicians and to explore barriers to seeking care. The implication of poor physician mental health on patients should also be examined more closely. Finally, the reviewed literature lacks intersectional and longitudinal studies, as well as evaluations of interventions offered to improve mental wellbeing of physicians.
Peer Review reports
The World Health Organization (WHO) defines mental health as “a state of well-being in which the individual realizes his or her own abilities, can cope with the normal stresses of life, can work productively and fruitfully, and is able to make a contribution to his or her community.” [ 41 ] One in four people worldwide are affected by mental health concerns [ 40 ]. Physicians are particularly vulnerable to experiencing mental illness due to the nature of their work, which is often stressful and characterized by shift work, irregular work hours, and a high pressure environment [ 1 , 21 , 31 ]. In North America, many physicians work in private practices with no access to formal institutional supports, which can result in higher instances of social isolation [ 13 , 27 ]. The literature on physicians’ mental health is growing, partly due to general concerns about mental wellbeing of health care workers and partly due to recognition that health care workers globally are dissatisfied with their work, which results in burnout and attrition from the workforce [ 31 , 34 ]. As a consequence, more efforts have been made globally to improve physicians’ mental health and wellness, which is known as “The Quadruple Aim.” [ 34 ] While the literature on mental health is flourishing, however, it has not been systematically summarized. This makes it challenging to identify what is being done to improve physicians’ wellbeing and which solutions are particularly promising [ 7 , 31 , 33 , 37 , 38 ]. The goal of our paper is to address this gap.
This paper explores what is known from the existing peer-reviewed literature about the mental health status of physicians and physicians-in-training in North America. Specifically, we examine (1) what types of mental health concerns among physicians are commonly discussed in the literature; (2) what are the reported causes of mental health concerns in physicians; (3) what are the effects that mental health concerns may have on physicians and their patients; (4) what solutions are proposed to improve mental health of physicians; and (5) what are the barriers to seeking and providing care to physicians with mental health concerns. Conducting this scoping review, our goal is to summarize the existing research, identifying the need for a subsequent systematic review of the literature in one or more areas under the study. We also hope to identify evidence-based interventions that can be utilized to improve physicians’ mental wellbeing and to suggest directions for future research [ 2 ]. Evidence-based interventions might have a positive impact on physicians and improve the quality of patient care they provide.
A scoping review of the academic literature on the mental health of physicians and physicians-in-training in North America was conducted using Arksey and O’Malley’s [ 2 ] methodological framework. Our review objectives and broad focus, including the general questions posed to conduct the review, lend themselves to a scoping review approach, which is suitable for the analysis of a broader range of study designs and methodologies [ 2 ]. Our goal was to map the existing research on this topic and identify knowledge gaps, without making any prior assumptions about the literature’s scope, range, and key findings [ 29 ].
Stage 1: identify the research question
Following the guidelines for scoping reviews [ 2 ], we developed a broad research question for our literature search, asking what does the academic literature tell about mental health issues among physicians, residents, and medical students in North America ? Burnout and other mental health concerns often begin in medical training and continue to worsen throughout the years of practice [ 31 ]. Recognizing that the study and practice of medicine plays a role in the emergence of mental health concerns, we focus on practicing physicians – general practitioners, specialists, and surgeons – and those who are still in training – residents and medical students. We narrowed down the focus of inquiry by asking the following sub-questions:
What types of mental health concerns among physicians are commonly discussed in the literature?
What are the reported causes of mental health problems in physicians and what solutions are available to improve the mental wellbeing of physicians?
What are the barriers to seeking and providing care to physicians suffering from mental health problems?
Stage 2: identify the relevant studies
We included in our review empirical papers published during January 2008–January 2018 in peer-reviewed journals. Our exclusive focus on peer-reviewed and empirical literature reflected our goal to develop an evidence-based platform for understanding mental health concerns in physicians. Since our focus was on prevalence of mental health concerns and promising practices available to physicians in North America, we excluded articles that were more than 10 years old, suspecting that they might be too outdated for our research interest. We also excluded papers that were not in English or outside the region of interest. Using combinations of keywords developed in consultation with a professional librarian (See Table 1 ), we searched databases PUBMed, SCOPUS, CINAHL, and PsychNET. We also screened reference lists of the papers that came up in our original search to ensure that we did not miss any relevant literature.
Stage 3: literature selection
Publications were imported into a reference manager and screened for eligibility. During initial abstract screening, 146 records were excluded for being out of scope, 75 records were excluded for being outside the region of interest, and 4 papers were excluded because they could not be retrieved. The remaining 91 papers were included into the review. Figure 1 summarizes the literature search and selection.
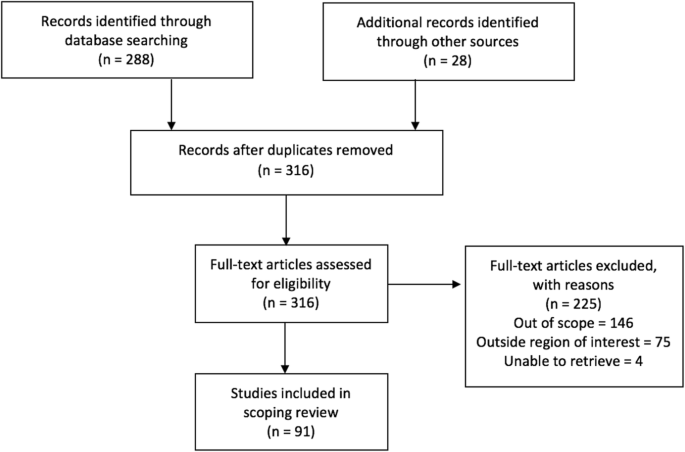
PRISMA Flow Diagram
Stage 4: charting the data
A literature extraction tool was created in Microsoft Excel to record the author, date of publication, location, level of training, type of article (empirical, report, commentary), and topic. Both authors coded the data inductively, first independently reading five articles and generating themes from the data, then discussing our coding and developing a coding scheme that was subsequently applied to ten more papers. We then refined and finalized the coding scheme and used it to code the rest of the data. When faced with disagreements on narrowing down the themes, we discussed our reasoning and reached consensus.
Stage 5: collating, summarizing, and reporting the results
The data was summarized by frequency and type of publication, mental health topics, and level of training. The themes inductively derived from the data included (1) description of mental health concerns affecting physicians and physicians-in-training; (2) prevalence of mental health concerns among this population; (3) possible causes that can explain the emergence of mental health concerns; (4) solutions or interventions proposed to address mental health concerns; (5) effects of mental health concerns on physicians and on patient outcomes; and (6) barriers for seeking and providing help to physicians afflicted with mental health concerns. Each paper was coded based on its relevance to major theme(s) and, if warranted, secondary focus. Therefore, one paper could have been coded in more than one category. Upon analysis, we identified the gaps in the literature.
Characteristics of included literature
The initial search yielded 316 records of which 91 publications underwent full-text review and were included in our scoping review. Our analysis revealed that the publications appear to follow a trend of increase over the course of the last decade reflecting the growing interest in physicians’ mental health. More than half of the literature was published in the last 4 years included in the review, from 2014 to 2018 ( n = 55), with most publications in 2016 ( n = 18) (Fig. 2 ). The majority of papers ( n = 36) focused on practicing physicians, followed by papers on residents ( n = 22), medical students ( n = 21), and those discussing medical professionals with different level of training ( n = 12). The types of publications were mostly empirical ( n = 71), of which 46 papers were quantitative. Furthermore, the vast majority of papers focused on the United States of America (USA) ( n = 83), with less than 9% focusing on Canada ( n = 8). The frequency of identified themes in the literature is broken down into prevalence of mental health concerns ( n = 15), causes of mental health concerns ( n = 18), effects of mental health concerns on physicians and patients ( n = 12), solutions and interventions for mental health concerns ( n = 46), and barriers to seeking and providing care for mental health concerns ( n = 4) (Fig. 3 ).
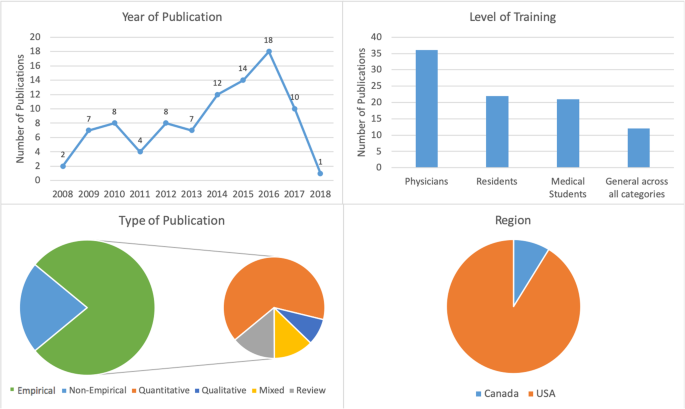
Number of sources by characteristics of included literature
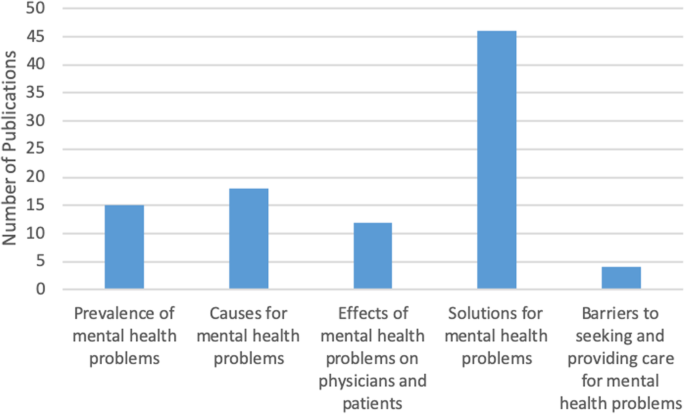
Frequency of themes in literature ( n = 91)
Mental health concerns and their prevalence in the literature
In this thematic category ( n = 15), we coded the papers discussing the prevalence of specific mental health concerns among physicians and those comparing physicians’ mental health to that of the general population. Most papers focused on burnout and stress ( n = 69), which was followed by depression and suicidal ideation ( n = 28), psychological harm and distress ( n = 9), wellbeing and wellness ( n = 8), and general mental health ( n = 3) (Fig. 4 ). The literature also identified that, on average, burnout and mental health concerns affect 30–60% of all physicians and residents [ 4 , 5 , 8 , 9 , 15 , 25 , 26 ].
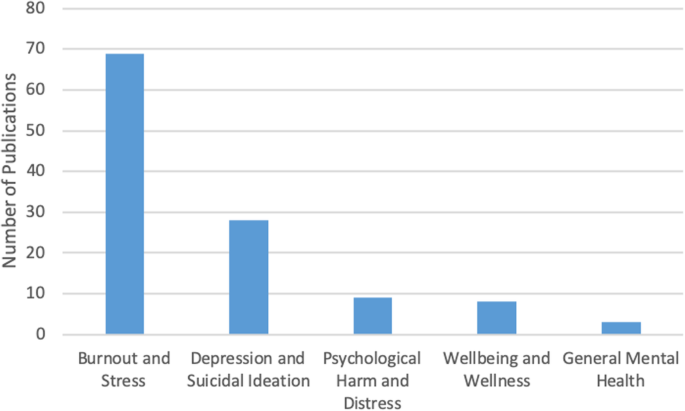
Number of sources by mental health topic discussed ( n = 91)
There was some overlap between the papers discussing burnout, depression, and suicidal ideation, suggesting that work-related stress may lead to the emergence of more serious mental health problems [ 3 , 12 , 21 ], as well as addiction and substance abuse [ 22 , 27 ]. Residency training was shown to produce the highest rates of burnout [ 4 , 8 , 19 ].
Causes of mental health concerns
Papers discussing the causes of mental health concerns in physicians formed the second largest thematic category ( n = 18). Unbalanced schedules and increasing administrative work were defined as key factors in producing poor mental health among physicians [ 4 , 5 , 6 , 13 , 15 , 27 ]. Some papers also suggested that the nature of the medical profession itself – competitive culture and prioritizing others – can lead to the emergence of mental health concerns [ 23 , 27 ]. Indeed, focus on qualities such as rigidity, perfectionism, and excessive devotion to work during the admission into medical programs fosters the selection of students who may be particularly vulnerable to mental illness in the future [ 21 , 24 ]. The third cluster of factors affecting mental health stemmed from structural issues, such as pressure from the government and insurance, fragmentation of care, and budget cuts [ 13 , 15 , 18 ]. Work overload, lack of control over work environment, lack of balance between effort and reward, poor sense of community among staff, lack of fairness and transparency by decision makers, and dissonance between one’s personal values and work tasks are the key causes for mental health concerns among physicians [ 20 ]. Govardhan et al. conceptualized causes for mental illness as having a cyclical nature - depression leads to burnout and depersonalization, which leads to patient dissatisfaction, causing job dissatisfaction and more depression [ 19 ].
Effects of mental health concerns on physicians and patients
A relatively small proportion of papers (13%) discussed the effects of mental health concerns on physicians and patients. The literature prioritized the direct effect of mental health on physicians ( n = 11) with only one paper focusing solely on the indirect effects physicians’ mental health may have on patients. Poor mental health in physicians was linked to decreased mental and physical health [ 3 , 14 , 15 ]. In addition, mental health concerns in physicians were associated with reduction in work hours and the number of patients seen, decrease in job satisfaction, early retirement, and problems in personal life [ 3 , 5 , 15 ]. Lu et al. found that poor mental health in physicians may result in increased medical errors and the provision of suboptimal care [ 25 ]. Thus physicians’ mental wellbeing is linked to the quality of care provided to patients [ 3 , 4 , 5 , 10 , 17 ].
Solutions and interventions
In this largest thematic category ( n = 46) we coded the literature that offered solutions for improving mental health among physicians. We identified four major levels of interventions suggested in the literature. A sizeable proportion of literature discussed the interventions that can be broadly categorized as primary prevention of mental illness. These papers proposed to increase awareness of physicians’ mental health and to develop strategies that can help to prevent burnout from occurring in the first place [ 4 , 12 ]. Some literature also suggested programs that can help to increase resilience among physicians to withstand stress and burnout [ 9 , 20 , 27 ]. We considered the papers referring to the strategies targeting physicians currently suffering from poor mental health as tertiary prevention . This literature offered insights about mindfulness-based training and similar wellness programs that can increase self-awareness [ 16 , 18 , 27 ], as well as programs aiming to improve mental wellbeing by focusing on physical health [ 17 ].
While the aforementioned interventions target individual physicians, some literature proposed workplace/institutional interventions with primary focus on changing workplace policies and organizational culture [ 4 , 13 , 23 , 25 ]. Reducing hours spent at work and paperwork demands or developing guidelines for how long each patient is seen have been identified by some researchers as useful strategies for improving mental health [ 6 , 11 , 17 ]. Offering access to mental health services outside of one’s place of employment or training could reduce the fear of stigmatization at the workplace [ 5 , 12 ]. The proposals for cultural shift in medicine were mainly focused on promoting a less competitive culture, changing power dynamics between physicians and physicians-in-training, and improving wellbeing among medical students and residents. The literature also proposed that the medical profession needs to put more emphasis on supporting trainees, eliminating harassment, and building strong leadership [ 23 ]. Changing curriculum for medical students was considered a necessary step for the cultural shift [ 20 ]. Finally, while we only reviewed one paper that directly dealt with the governmental level of prevention, we felt that it necessitated its own sub-thematic category because it identified the link between government policy, such as health care reforms and budget cuts, and the services and care physicians can provide to their patients [ 13 ].
Barriers to seeking and providing care
Only four papers were summarized in this thematic category that explored what the literature says about barriers for seeking and providing care for physicians suffering from mental health concerns. Based on our analysis, we identified two levels of factors that can impact access to mental health care among physicians and physicians-in-training.
Individual level barriers stem from intrinsic barriers that individual physicians may experience, such as minimizing the illness [ 21 ], refusing to seek help or take part in wellness programs [ 14 ], and promoting the culture of stoicism [ 27 ] among physicians. Another barrier is stigma associated with having a mental illness. Although stigma might be experienced personally, literature suggests that acknowledging the existence of mental health concerns may have negative consequences for physicians, including loss of medical license, hospital privileges, or professional advancement [ 10 , 21 , 27 ].
Structural barriers refer to the lack of formal support for mental wellbeing [ 3 ], poor access to counselling [ 6 ], lack of promotion of available wellness programs [ 10 ], and cost of treatment. Lack of research that tests the efficacy of programs and interventions aiming to improve mental health of physicians makes it challenging to develop evidence-based programs that can be implemented at a wider scale [ 5 , 11 , 12 , 18 , 20 ].
Our analysis of the existing literature on mental health concerns in physicians and physicians-in-training in North America generated five thematic categories. Over half of the reviewed papers focused on proposing solutions, but only a few described programs that were empirically tested and proven to work. Less common were papers discussing causes for deterioration of mental health in physicians (20%) and prevalence of mental illness (16%). The literature on the effects of mental health concerns on physicians and patients (13%) focused predominantly on physicians with only a few linking physicians’ poor mental health to medical errors and decreased patient satisfaction [ 3 , 4 , 16 , 24 ]. We found that the focus on barriers for seeking and receiving help for mental health concerns (4%) was least prevalent. The topic of burnout dominated the literature (76%). It seems that the nature of physicians’ work fosters the environment that causes poor mental health [ 1 , 21 , 31 ].
While emphasis on burnout is certainly warranted, it might take away the attention paid to other mental health concerns that carry more stigma, such as depression or anxiety. Establishing a more explicit focus on other mental health concerns might promote awareness of these problems in physicians and reduce the fear such diagnosis may have for doctors’ job security [ 10 ]. On the other hand, utilizing the popularity and non-stigmatizing image of “burnout” might be instrumental in developing interventions promoting mental wellbeing among a broad range of physicians and physicians-in-training.
Table 2 summarizes the key findings from the reviewed literature that are important for our understanding of physician mental health. In order to explicitly summarize the gaps in the literature, we mapped them alongside the areas that have been relatively well studied. We found that although non-empirical papers discussed physicians’ mental wellbeing broadly, most empirical papers focused on medical specialty (e.g. neurosurgeons, family medicine, etc.) [ 4 , 8 , 15 , 19 , 25 , 28 , 35 , 36 ]. Exclusive focus on professional specialty is justified if it features a unique context for generation of mental health concerns, but it limits the ability to generalize the findings to a broader population of physicians. Also, while some papers examined the impact of gender on mental health [ 7 , 32 , 39 ], only one paper considered ethnicity as a potential factor for mental health concerns and found no association [ 4 ]. Given that mental health in the general population varies by gender, ethnicity, age, and sexual orientation, it would be prudent to examine mental health among physicians using an intersectional analysis [ 30 , 32 , 39 ]. Finally, of the empirical studies we reviewed, all but one had a cross-sectional design. Longitudinal design might offer a better understanding of the emergence and development of mental health concerns in physicians and tailor interventions to different stages of professional career. Additionally, it could provide an opportunity to evaluate programs’ and policies’ effectiveness in improving physicians’ mental health. This would also help to address the gap that we identified in the literature – an overarching focus on proposing solutions with little demonstrated evidence they actually work.
This review has several limitations. First, our focus on academic literature may have resulted in overlooking the papers that are not peer-reviewed but may provide interesting solutions to physician mental health concerns. It is possible that grey literature – reports and analyses published by government and professional organizations – offers possible solutions that we did not include in our analysis or offers a different view on physicians’ mental health. Additionally, older papers and papers not published in English may have information or interesting solutions that we did not include in our review. Second, although our findings suggest that the theme of burnout dominated the literature, this may be the result of the search criteria we employed. Third, following the scoping review methodology [ 2 ], we did not assess the quality of the papers, focusing instead on the overview of the literature. Finally, our research was restricted to North America, specifically Canada and the USA. We excluded Mexico because we believed that compared to the context of medical practice in Canada and the USA, which have some similarities, the work experiences of Mexican physicians might be different and the proposed solutions might not be readily applicable to the context of practice in Canada and the USA. However, it is important to note that differences in organization of medical practice in Canada and the USA do exist, as do differences across and within provinces in Canada and the USA. A comparative analysis can shed light on how the structure and organization of medical practice shapes the emergence of mental health concerns.
The scoping review we conducted contributes to the existing research on mental wellbeing of American and Canadian physicians by summarizing key knowledge areas and identifying key gaps and directions for future research. While the papers reviewed in our analysis focused on North America, we believe that they might be applicable to the global medical workforce. Identifying key gaps in our knowledge, we are calling for further research on these topics, including examination of medical training curricula and its impact on mental wellbeing of medical students and residents, research on common mental health concerns such as depression or anxiety, studies utilizing intersectional and longitudinal approaches, and program evaluations assessing the effectiveness of interventions aiming to improve mental wellbeing of physicians. Focus on the effect physicians’ mental health may have on the quality of care provided to patients might facilitate support from government and policy makers. We believe that large-scale interventions that are proven to work effectively can utilize an upstream approach for improving the mental health of physicians and physicians-in-training.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
United States of America
World Health Organization
Ahmed N, Devitt KS, Keshet I, Spicer J, Imrie K, Feldman L, et al. A systematic review of the effects of resident duty hour restrictions in surgery: impact on resident wellness, training, and patient outcomes. Ann Surg. 2014;259(6):1041–53.
Article Google Scholar
Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005;8(1):19–32.
Atallah F, McCalla S, Karakash S, Minkoff H. Please put on your own oxygen mask before assisting others: a call to arms to battle burnout. Am J Obstet Gynecol. 2016;215(6):731.e1.
Baer TE, Feraco AM, Tuysuzoglu Sagalowsky S, Williams D, Litman HJ, Vinci RJ. Pediatric resident burnout and attitudes toward patients. Pediatrics. 2017;139(3):e20162163. https://doi.org/10.1542/peds.2016-2163 .
Article PubMed Google Scholar
Blais R, Safianyk C, Magnan A, Lapierre A. Physician, heal thyself: survey of users of the Quebec physicians health program. Can Fam Physician. 2010;56(10):e383–9.
PubMed PubMed Central Google Scholar
Brennan J, McGrady A. Designing and implementing a resiliency program for family medicine residents. Int J Psychiatry Med. 2015;50(1):104–14.
Cass I, Duska LR, Blank SV, Cheng G, NC dP, Frederick PJ, et al. Stress and burnout among gynecologic oncologists: a Society of Gynecologic Oncology Evidence-based Review and Recommendations. Gynecol Oncol. 2016;143(2):421–7.
Chan AM, Cuevas ST, Jenkins J 2nd. Burnout among osteopathic residents: a cross-sectional analysis. J Am Osteopath Assoc. 2016;116(2):100–5.
Chaukos D, Chad-Friedman E, Mehta DH, Byerly L, Celik A, McCoy TH Jr, et al. Risk and resilience factors associated with resident burnout. Acad Psychiatry. 2017;41(2):189–94.
Compton MT, Frank E. Mental health concerns among Canadian physicians: results from the 2007-2008 Canadian physician health study. Compr Psychiatry. 2011;52(5):542–7.
Cunningham C, Preventing MD. Burnout. Trustee. 2016;69(2):6–7 1.
PubMed Google Scholar
Daskivich TJ, Jardine DA, Tseng J, Correa R, Stagg BC, Jacob KM, et al. Promotion of wellness and mental health awareness among physicians in training: perspective of a national, multispecialty panel of residents and fellows. J Grad Med Educ. 2015;7(1):143–7.
Dyrbye LN, Shanafelt TD. Physician burnout: a potential threat to successful health care reform. JAMA. 2011;305(19):2009–10.
Article CAS Google Scholar
Epstein RM, Krasner MS. Physician resilience: what it means, why it matters, and how to promote it. Acad Med. 2013;88(3):301–3.
Evans RW, Ghosh K. A survey of headache medicine specialists on career satisfaction and burnout. Headache. 2015;55(10):1448–57.
Fahrenkopf AM, Sectish TC, Barger LK, Sharek PJ, Lewin D, Chiang VW, et al. Rates of medication errors among depressed and burnt out residents: prospective cohort study. BMJ. 2008;336(7642):488–91.
Fargen KM, Spiotta AM, Turner RD, Patel S. The importance of exercise in the well-rounded physician: dialogue for the inclusion of a physical fitness program in neurosurgery resident training. World Neurosurg. 2016;90:380–4.
Gabel S. Demoralization in Health Professional Practice: Development, Amelioration, and Implications for Continuing Education. J Contin Educ Health Prof 2013 Spring. 2013;33(2):118–26.
Google Scholar
Govardhan LM, Pinelli V, Schnatz PF. Burnout, depression and job satisfaction in obstetrics and gynecology residents. Conn Med. 2012;76(7):389–95.
Jennings ML, Slavin SJ. Resident wellness matters: optimizing resident education and wellness through the learning environment. Acad Med. 2015;90(9):1246–50.
Keller EJ. Philosophy in medical education: a means of protecting mental health. Acad Psychiatry. 2014;38(4):409–13.
Krall EJ, Niazi SK, Miller MM. The status of physician health programs in Wisconsin and north central states: a look at statewide and health systems programs. WMJ. 2012;111(5):220–7.
Lemaire JB, Wallace JE. Burnout among doctors. BMJ. 2017;358:j3360.
Linzer M, Bitton A, Tu SP, Plews-Ogan M, Horowitz KR, Schwartz MD, et al. The end of the 15-20 minute primary care visit. J Gen Intern Med. 2015;30(11):1584–6.
Lu DW, Dresden S, McCloskey C, Branzetti J, Gisondi MA. Impact of burnout on self-reported patient care among emergency physicians. West J Emerg Med. 2015;16(7):996–1001.
Maslach C, Schaufeli WB, Leiter MP. Job burnout. Annu Rev Psychol. 2001;52:397–422.
McClafferty H, Brown OW. Section on integrative medicine, committee on practice and ambulatory medicine, section on integrative medicine. Physician health and wellness. Pediatrics. 2014;134(4):830–5.
Miyasaki JM, Rheaume C, Gulya L, Ellenstein A, Schwarz HB, Vidic TR, et al. Qualitative study of burnout, career satisfaction, and well-being among US neurologists in 2016. Neurology. 2017;89(16):1730–8.
Peterson J, Pearce P, Ferguson LA, Langford C. Understanding scoping reviews: definition, purpose, and process. JAANP. 2016;29:12–6.
Przedworski JM, Dovidio JF, Hardeman RR, Phelan SM, Burke SE, Ruben MA, et al. A comparison of the mental health and well-being of sexual minority and heterosexual first-year medical students: a report from the medical student CHANGE study. Acad Med. 2015;90(5):652–9.
Ripp JA, Privitera MR, West CP, Leiter R, Logio L, Shapiro J, et al. Well-being in graduate medical education: a call for action. Acad Med. 2017;92(7):914–7.
Salles A, Mueller CM, Cohen GL. Exploring the relationship between stereotype perception and Residents’ well-being. J Am Coll Surg. 2016;222(1):52–8.
Shiralkar MT, Harris TB, Eddins-Folensbee FF, Coverdale JH. A systematic review of stress-management programs for medical students. Acad Psychiatry. 2013;37(3):158–64.
Sikka R, Morath J, Leape L. The quadruple aim: care, health, cost and meaning in work. BMJ Qual Saf. 2015;24(10):608–10. https://doi.org/10.1136/bmjqs-2015-004160 .
Tawfik DS, Phibbs CS, Sexton JB, Kan P, Sharek PJ, Nisbet CC, et al. Factors Associated With Provider Burnout in the NICU. Pediatrics. 2017;139(5):608. https://doi.org/10.1542/peds.2016-4134 Epub 2017 Apr 18.
Turner TB, Dilley SE, Smith HJ, Huh WK, Modesitt SC, Rose SL, et al. The impact of physician burnout on clinical and academic productivity of gynecologic oncologists: a decision analysis. Gynecol Oncol. 2017;146(3):642–6.
West CP, Dyrbye LN, Erwin PJ, Shanafelt TD. Interventions to prevent and reduce physician burnout: a systematic review and meta-analysis. Lancet. 2016;388(10057):2272.
Williams D, Tricomi G, Gupta J, Janise A. Efficacy of burnout interventions in the medical education pipeline. Acad Psychiatry. 2015;39(1):47–54.
Woodside JR, Miller MN, Floyd MR, McGowen KR, Pfortmiller DT. Observations on burnout in family medicine and psychiatry residents. Acad Psychiatry. 2008;32(1):13–9.
World Health Organization. (2001). Mental disorders affect one in four people.
World Health Organization. Promoting mental health: concepts, emerging evidence, practice (Summary Report). Geneva: World Health Organization; 2004.
Download references
Acknowledgements
Not Applicable.
Not Applicable
Author information
Authors and affiliations.
Telfer School of Management, University of Ottawa, 55 Laurier Ave E, Ottawa, ON, K1N 6N5, Canada
Mara Mihailescu
School of Public Health and Health Systems, University of Waterloo, 200 University Avenue West, Waterloo, ON, N2L 3G1, Canada
Elena Neiterman
You can also search for this author in PubMed Google Scholar
Contributions
M.M. and E.N. were involved in identifying the relevant research question and developing the combinations of keywords used in consultation with a professional librarian. M.M. performed the literature selection and screening of references for eligibility. Both authors were involved in the creation of the literature extraction tool in Excel. Both authors coded the data inductively, first independently reading five articles and generating themes from the data, then discussing their coding and developing a coding scheme that was subsequently applied to ten more papers. Both authors then refined and finalized the coding scheme and M.M. used it to code the rest of the data. M.M. conceptualized and wrote the first copy of the manuscript, followed by extensive drafting by both authors. E.N. was a contributor to writing the final manuscript. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Mara Mihailescu .
Ethics declarations
Ethics approval and consent to participate, consent for publication, competing interests.
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License ( http://creativecommons.org/licenses/by/4.0/ ), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated.
Reprints and permissions
About this article
Cite this article.
Mihailescu, M., Neiterman, E. A scoping review of the literature on the current mental health status of physicians and physicians-in-training in North America. BMC Public Health 19 , 1363 (2019). https://doi.org/10.1186/s12889-019-7661-9
Download citation
Received : 29 April 2019
Accepted : 20 September 2019
Published : 24 October 2019
DOI : https://doi.org/10.1186/s12889-019-7661-9
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Mental health
- Mental illness
- Medical students
- Scoping review
- Interventions
- North America
BMC Public Health
ISSN: 1471-2458
- Submission enquiries: [email protected]
- General enquiries: [email protected]
- Research article
- Open access
- Published: 05 July 2018
Systematic review of resilience-enhancing, universal, primary school-based mental health promotion programs
- Amanda Fenwick-Smith 1 ,
- Emma E. Dahlberg 1 &
- Sandra C. Thompson ORCID: orcid.org/0000-0003-0327-7155 1
BMC Psychology volume 6 , Article number: 30 ( 2018 ) Cite this article
42k Accesses
136 Citations
252 Altmetric
Metrics details
Wellbeing and resilience are essential in preventing and reducing the severity of mental health problems. Equipping children with coping skills and protective behavior can help them react positively to change and obstacles in life, allowing greater mental, social and academic success. This systematic review studies the implementation and evaluation of universal, resilience-focused mental health promotion programs based in primary schools.
A systematic review of literature used five primary databases: PsycINFO; Web of Science; PubMed; Medline; Embase and The Cochrane Library; and keywords related to (a) health education, health promotion, mental health, mental health promotion, social and emotional wellbeing; (b) school health service, student, schools, whole-school; (c) adolescent, child, school child, pre-adolescent; (d) emotional intelligence, coping behavior, emotional adjustment, resilienc*, problem solving, to identify relevant articles. Articles included featured programs that were universally implemented in a primary school setting and focused on teaching of skills, including coping skills, help-seeking behaviors, stress management, and mindfulness, and were aimed at the overall goal of increasing resilience among students.
Of 3087 peer-reviewed articles initially identified, 475 articles were further evaluated with 11 reports on evaluations of 7 school-based mental health promotion programs meeting the inclusion criteria. Evaluation tools used in program evaluation are also reviewed, with successful trends in evaluations discussed. Encouraging results were seen when the program was delivered by teachers within the schools. Length of programing did not seem important to outcomes. Across all 7 programs, few long-term sustained effects were recorded following program completion.
Conclusions
This review provides evidence that mental health promotion programs that focus on resilience and coping skills have positive impacts on the students’ ability to manage daily stressors.
Peer Review reports
This review looks at resilience-boosting mental health promotion programs implemented universally at schools for primary school-aged children (5–12 years). Wellbeing and resilience are important in preventing and reducing the severity of mental health problems. The skills of problem solving, building and maintaining interpersonal relationships, and realistic goal-setting are well-established as enhancing an individual’s ability to contribute meaningfully in daily life. There is substantial literature on resilience [ 1 ] which is defined as a capacity or set of skills that allows a person to “prevent, minimize or overcome the damaging effects of adversity” [ 2 ] and includes factors that are internal and external to the person - emotions, behavior, biology, development, and context affect mental health [ 3 ]. Potential risks for poor self-esteem and mental health can be overcome by protective factors, including one’s coping skills, healthy family and social relationships, help-seeking behaviors, and meaningful activities in interactions [ 4 ].
Resilience theory states that all children, regardless of risk or current mental health status, can benefit from help and support in the development of effective, mentally-healthy strategies and resilience skills [ 5 ]. Support for and a focus on the development of children’s resilience skills does not lead to a risk-free life, but can increase a child’s ability to seek support while building their self-worth and self-efficacy. By providing children with skills with which to cope with negative life stressors through the promotion of resilience and protective factors, children can thrive despite obstacles [ 6 ]. An argument for a population approach for mental health strengthening can be extrapolated from Geoffrey Rose’s argument that the largest number of cases of ill health happen not in those at high risk, but in those who have just some risk, simply because in a normal population distribution more people (and hence adverse events) will occur to them [ 7 ]. Since all people experience adversity at some point in their life, teaching strategies for resilient thinking would be better applied in advance to the potential “at risk” population. The positive outcomes and possibilities associated with strengthening children’s resilience universally applied can act as a mitigating approach, allowing for early support and strengthening of mental health, rather than requiring interventions for acute situations in the future [ 8 ]. The approach of boosting resilience can enhance children’s abilities to self-protect, as well as being an effective counter to offset the effects of maltreatment and potential traumatic life events [ 9 , 10 , 11 ]. As such, universal application of programs to enhance resilience stands as not only useful for those recognized as being at risk and who require additional mental health support currently, but also as a protective shield for all children moving through life.
Universal, school-based programing
School-based mental health promotion programs delivered to all students within a class, grade, or the entire school are categorized as universal programs. In developed countries, all children are required to attend school, making it an ideal setting for programs providing key interventions for children, particularly children from challenged families, homes and communities that may not have easy access to community or home-based intervention programs [ 12 ]. Mental health promotion programs have been developed and implemented in schools using a variety of different approaches. Many mental illness prevention or intervention programs use a targeted approach, focusing on children deemed at risk due to their background, history or signs of mental health problems, usually based upon defined socio-demographic factors or certain behavioral characteristics.
Universal programs vary in their approach and implementation. Some universal programs are class-based, with weekly sessions delivered by classroom teachers or program staff to the entire classroom. Another universal approach is to change the entire school environment to be friendlier and more supportive of positive mental health messages, and this is often implemented in combination with class-based approaches [ 13 ]. Class-based, universal mental health promotion programs vary in their aims, focusing on different elements of cognitive or affective skills and behaviors, environmental or cultural factors, while increasing knowledge of mental health and resources.
Mental health promotion programs specifically targeting resilience may be referred to as social and emotional learning programs, mindfulness programs, stress management programs, or emotional wellbeing programs and vary in terms of curriculum, length and implementation, and use of different tools and activities to convey key themes and topics. Methods of delivery vary as well, including the use of clinical tools, educational resources, training of teachers and parents, changes to school systems and resources, and use of narrative tools. As such, the curricula used in these programs vary, although all utilize a pre-established definition of resilience and the desired outcomes to be achieved from a social and emotional learning program. The most effective social and emotional learning curricula are highly interactive and use a variety of educational tools, addressing both specific and general skills, and are delivered in supportive environments [ 14 ]. Mental health promotion programs promoting resilience focus on the development of coping skills, mindfulness, emotion recognition and management, empathic relationships, self-awareness and efficacy, and help-seeking behavior. Secondary outcomes often include decreased symptoms of anxiety, depression, and increased academic outcomes.
Relevant research reviews
Given the importance and reach of school settings, many reports describe universal, school-based mental health promotion programs. Prior reviews have explored school-based mental health promotion programs in different contexts, countries, applications, and within specific demographic parameters. There are many reviews addressing targeted programs aimed at suicide prevention, sexual health, substance abuse and misuse, physical activity and nutrition improvement and these often measure as secondary outcomes changes in self-efficacy, coping and resilience skills [ 5 , 15 , 16 , 17 ]. A number of reviews analyzing mental health promotion programs that focus on resilience across a range of age groups have established that school-based interventions can have significant impacts on achievement, social and emotional skills, behavior, and symptoms of anxiety and depressive disorders [ 12 , 16 , 18 ]. In their 2017 review, Dray and colleagues looked at control-based trial evaluations of programs of universal resilience-programing in schools spanning all ages, reporting on those that yielded significant results in resilience factor changes. Durlak and colleagues compared 213 programs, also targeting all age groups, assessing the outcomes on attitudes, behaviors and academic performance and analyzing effect size and factors that moderate program outcomes. Waere and Mind assessed the key features that make school-based curricula successful as an approach, highlighting the importance of social and emotional competence as part of the curriculum within schools [ 12 ]. Another review considered studies on mental health promotion programs solely conducted with control and comparison groups [ 19 ].
The current review
This review aims to inform policy, programing and evaluation of universal, resilience-focused mental health interventions for primary school-aged children as it focuses on the specific tools and key elements for the population that will benefit the most from increased resilience in an easy-to-reach setting, aspects which have not been highlighted in previous reviews. The multitude of existing mental health promotion programs highlights the need to establish what specific elements and evaluations contribute to successful programing. Unlike previous reviews, this review focuses on programs delivered solely to primary school students (aged 5–12 years), as there is evidence that the younger the implementation of mental health promotion and resilience programing, the greater the positive effect [ 3 , 20 , 21 ]. Rather than focusing on the program curriculum, it considers the criteria for implementation and key elements of programing for a comprehensive intervention, highlighting the elements of that allow for best program fidelity and student engagement. It also describes the criteria and outcome measures (tools and methods) used in implementing and evaluating resilience-focused, universal school-based mental health promotion programs.
Studies eligible for inclusion were published from 2002 to 2017, describe mental health promotion programs focusing on resilience and protective factors, and were delivered universally at schools for primary school children aged 5–12 years. A universal program is defined as being a program offered for a specific all-inclusive group, whether it be the entire school, grade or classroom. All students within the group participate in at least one component of the program, regardless of their mental health status and risk factors. Resilience is defined as a capacity or set of skills that allows a person to “prevent, minimize or overcome the damaging effects of adversity” [ 2 ], through the promotion of protective factors including coping skills, peer socialization and empathy building, self-efficacy, help-seeking behaviors, mindfulness and emotion literacy.
Search procedures
A preliminary review of literature revealed key terms related to resilience-focused, school-based, universal mental health promotion programs. A broad search strategy was then developed to identify relevant peer-reviewed articles in five primary databases: PsycINFO; Web of Science; PubMed; Medline; Embase and The Cochrane Library. The search strategy was modified as necessary for advanced searches of each database, using keyword search criteria: (a) health education, health promotion, mental health, mental health promotion, social and emotional wellbeing; (b) school health service, student, schools, whole-school; (c) adolescen*, child, school child, pre-adolescent; (d) emotional intelligence, coping behavior, emotional adjustment, resilienc*, problem solving. Searches were conducted in September 2016 and updated in May 2018. Articles were initially screened by abstract by the lead author. All full-text articles were reviewed by two reviewers, with additional checks and consultations with other authors, to ensure consensus around those articles where eligibility was less clear. Snowball citation was used to identify other relevant articles.
Inclusion criteria
To be included in the review, each study had to meet the following criteria: (a) adhere to the above definition of a universal program; (b) be based in a primary school; (c) be delivered to children aged between 5 and 12 years of age; (d) focus on resilience and protective factors (meeting the above definition); (e) contain a qualitative, quantitative or mixed-methods evaluation of the program; (f) be published in English since 2002 in a peer-reviewed journal.
Exclusion criteria
Programs targeting specific behaviors where resilience is a secondary outcome, or programs primarily focusing on post-traumatic stress among students affected by natural disasters or war were not included . Programs with the ultimate goal and outcome measurements relating to a specific behavior, emotional condition or mental illness were not included, even if the tools taught in the intervention could be classified as resilience promoting. Universal programs that sought to change school atmosphere through teacher resilience training, or increasing school health services were not included. After-school or recess resilience programing was not included, even if it took place at a school. Programs that were available but not implemented universally were not included, as the self-selecting nature of optional programing is unlikely to reach the most at-risk children, and such programs do not insure a comprehensive program for all students regardless of risk. Studies where many students were outside of the age group and during a transition period between different schools were not included. Resilience programing that fits our inclusion criteria but is solely delivered to a population that has been exposed to high stress situations and is at risk or may develop PTSD are not included. Unpublished dissertations, grey literature and reports were not included.
Excluded studies
It is worth commenting upon how exclusion criteria were applied in practice. A number of programs were not included in this review despite having a resilience focus, being universally-delivered and school-based because they have not been reported upon within the preceding 15 years (since 2002). Other excluded programs had an ultimate goal that was not general mental health promotion program, but rather aimed at addressing a specific condition or behavior through the promotion of certain resilience skills and protective factors. Notable programs include the Penn Resilience Program, which has been shown to reduce depressive symptoms through the cognitive-behavioral therapy programing, including the promotion of coping skills [ 22 ]. The Good Behavior Games specifically target behavior control through the promotion of resilience, but fall outside of the age range of this review [ 23 ]. REACH for RESILIENCE promotes resilience skills to prevent anxiety problems, and targets very young children [ 24 ]. The nation-wide Australian program, beyondblue, focuses on social and resilience skills to prevent depression, targeting adolescents [ 25 ]. Evaluations of the FRIENDS program were not included as it targets childhood anxiety through the promotion of social-emotional skills [ 26 ]. Another exclusion was the Aussie Optimism: Positive Thinking Skills Program (AOP-PTS) which promotes social and coping skills to prevent and address depression symptoms [ 27 ].
Article quality assessment
The Mixed Methods Appraisal Tool (MMAT) was used to assess the quality of included studies and provides a validated method of assessing qualitative, quantitative, and mixed methods studies. After the initial screening, articles were scored based on the criteria for each respective study [ 28 ]. Two researchers independently assessed each article [ 29 ]. Of note, the tool does not address the quality of the reporting, but only the quality of the reported methods of the study.
The initial search strategy shows that of an initial 3087 publications identified using the search terms and following abstract assessment of 475 references, 34 articles were selected for full-text assessment. An additional 7 articles were identified through citation snowballing and after reading of the full-text so that 41 articles were fully assessed for eligibility. A total of 11 studies reporting on 7 programs met all the inclusion criteria (Fig. 1 ), with key characteristics including MMAT scores recorded (Table 1 ). The most common reasons for exclusion were: focus on trauma, incorrect age group or target population; not meeting our definition of universal programs; and lack of focus on resilience and protective factors. Included articles. Key elements of each program’s curriculum and implementation are shown (Table 2 ).
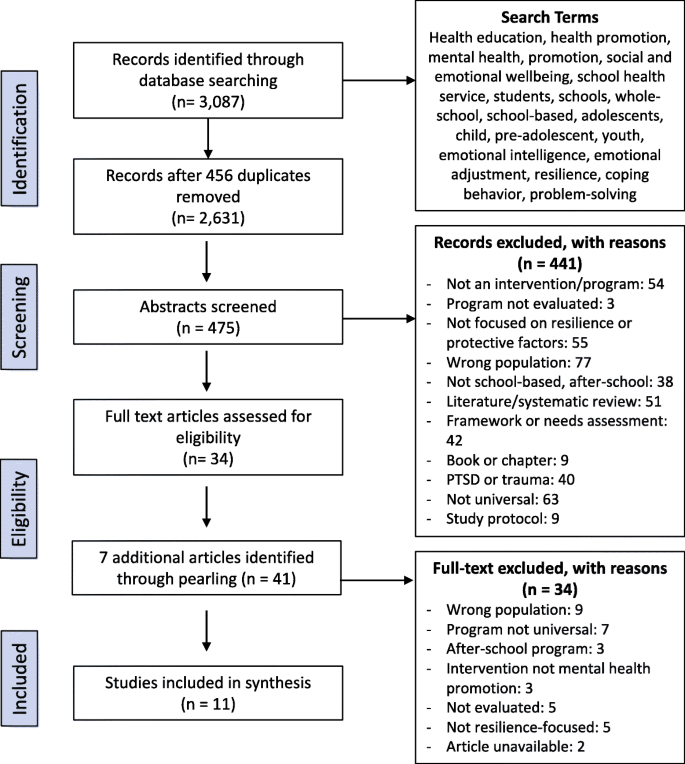
Flow diagram of selection process for relevant literature
Aim of the program
The aims of the seven programs (reported on in eleven articles) included varied in their approach to resilience and the protective factors they sought to address. All six programs sought to increase social and emotional competencies with the ultimate aim of increasing mental wellbeing and future protection from risks. Six articles, addressing 2 different programs, Mindfulness-Based Stress Reduction and Zippy’s Friends, specifically sought to improve psychological functioning with the goal of ameliorating the negative effects of stress and increasing coping skills [ 30 , 31 , 32 , 33 , 34 , 35 ]. The RALLY program aimed at increasing the prevalence of resilience protective factors in students, with a particular focus on academic outcomes and learning potential [ 36 ] while the Up program, a social and emotional competencies program, aimed at enhancing existing competencies and decreasing inequity in social and emotional competencies across socioeconomic lines [ 37 ]. The You Can Do It! (YCDI!) Education program sought to ameliorate children’s ability to positively control their emotions in daily life [ 38 ]. All programs sought to improve the outcomes of one or more protective factors, hypothesizing increased resilience as a result. A strong emphasis on increased coping skills and strategies as well as improved relationships was evident in all the programs.
Target population
Universal programs demand the application of the program to an entire cohort of students, but how that was done varied from delivering the program to an entire class, across an entire grade or across multiple schools. As such, sample size varied significantly between studies. Details of sample populations (Table 1 ) show all but two studies were implemented and evaluated across multiple schools, with ten of eleven conducted across multiple classrooms [ 30 , 31 , 32 , 33 , 34 , 35 , 37 , 38 , 39 ]. Age groups varied across the programs, with 4 studies addressing populations 10 years and above [ 30 , 36 , 38 , 39 ], and 6 studies addressing populations younger than 10 years of age [ 31 , 32 , 33 , 34 , 35 , 40 ]. Socio-demographic profiles of students varied across studies. Four studies described programs delivered at socio-economically disadvantaged schools [ 30 , 31 , 33 , 36 ] whereas four programs took place in middle or upper class neighborhoods [ 32 , 37 , 39 , 40 ]. Dufour et al . (2011) did not report on socio-demographic data of students who received the program [ 34 ] whereas the students involved in the report by Holen et al (2012) were from homes where parents had educational attainment levels higher than the national average [ 35 ]. Yamamoto et al. (2017) delivered the program to students in the Tokyo Metropolitan Area, making no demographic distinctions, other than to address the specific contextual implications of Japanese emotion- and stress-culture as impactful in their student population [ 38 ].
Key elements of programs
Key elements of the programs (Table 2 ) show that Malti et al (2008) was the only study in which the program comprised more than one student-focused component [ 36 ]. Although only a few components were delivered universally, all students were exposed to at least one component of the program [ 36 ]. The Up program included parent and teacher training, and school environment programing [ 37 ] and program fidelity and adaptability were identified as key contributing factors to successful implementation with four studies reporting high levels of program fidelity and program support [ 32 , 33 , 39 , 40 ]. The five studies that implemented and evaluated the Zippy’s Friends program described no changes in curriculum or delivery, but allowed for activity adaptability during sessions [ 31 , 32 , 33 , 34 , 35 ]. Teachers delivering it felt equipped to adapt the program as they saw necessary to their class while still maintaining high program fidelity [ 34 ]. Adaptability was also highlighted as being an important program factor for the You Can Do It! Education program in Japan, where program staff translated and altered the internationally-implemented program with Japan-specific illustrations, examples and exercises to optimize the connection with students [ 38 ]. Three studies identified problems with implementation of programming due to teacher perceptions, time constraints, participation rates and class literacy levels [ 32 , 33 , 38 , 40 ].
Evaluation frameworks, tools and indicators
Study evaluation frameworks and indicators (summarised in Table 3 ) are reported with more detail on evaluation tools and methods used for evaluating elements of programing reported in Appendix . Studies varied greatly on the timing and purpose of their evaluation although all applied a combination of pre-assessment, post-assessment, process evaluation, implementation evaluation and follow up assessments. Within specific programs, different evaluations were used for different implementations and contexts. The five articles reporting on the Zippy’s Friends program utilized different evaluation methods [ 31 , 32 , 33 , 34 , 35 ]. Mishara and Ystgaard (2006) evaluated the implementation of Zippy’s Friends in two countries with similar socio-demographic characteristics, Lithuania and Denmark, and found similar results in outcomes of students in the intervention groups in both countries. Yamamoto et al. used a semi-experimental design with intervention and control groups and utilized three self-report scales to evaluate students [ 38 ]. Clarke evaluated a randomized-controlled trial implementation of Zippy’s Friends in Ireland using both standard measures [ 33 ] and a participatory workshop with a subsample of students. The workshop was semi-structured around three key themes: lived experiences and coping reactions; emotion recognition and regulation; and program evaluation [ 31 ]. In all articles meeting out inclusion criteria, multiple standardized, validated tools were used for evaluation measures, most commonly the Children’s Depression Inventory (CDI, Short or Complete Form) [ 30 , 39 ], the Strengths and Difficulties Questionnaire [ 33 , 35 ], the Schoolagers’ Coping Strategies Inventory [ 32 , 34 ], and a Program Fidelity Checklist [ 33 , 40 ]. Evaluation methods commonly included in-class observations [ 33 , 34 , 36 , 40 ], researcher-developed questionnaires [ 34 , 36 ] and session reports [ 32 , 34 , 35 ].
Each article identified outcomes associated with their research question and hypothesis with outcomes following program implementation to assess the impact of the program. Table 4 presents a summary of whether major outcomes were considered by the article to have changed as a result of programing. In eight studies, researchers identified at baseline an overarching need for resilience programing among students, including low levels of trust and empathy; problems with emotion control, relationships and help-seeking; or reported symptoms [ 30 , 31 , 33 , 36 , 37 , 38 , 39 , 40 ]. Ten out of eleven studies reported positive outcomes with improvements in student resilience and protective factors, including frequency of use of coping skills, internalizing behaviors, and self-efficacy at post-assessment [ 30 , 31 , 32 , 33 , 34 , 36 , 37 , 38 , 39 , 40 ]. Three studies identified shortcomings in outcomes despite positive results from the overall program implementation and outcomes. Kraag et al. (2009) identified a lack of follow up and social reinforcement for components taught in programing, with negative implications on long-term follow-up outcomes [ 39 ]. Clarke and colleagues (2014) showed limited effects on resilience itself, but highlighted a marked increase in self-awareness among students [ 33 ]. Variations in outcomes between informants was highlighted in Holen et al (2012) who did not determine that resilience itself was an outcome of the program [ 35 ].
This review examined the program criteria and outcome measures used in the implementation and evaluation of resilience-focused, universal, school-based mental health promotion programs. Eleven published studies based on seven different programs were identified and included.
Characteristics of effective programs
Several characteristics of effective programing stood out. The involvement of teachers in the delivery of programs emerged as key. Numerous studies used teachers to deliver the program, a feature presented positively as providing the opportunity for adaptability of programing and more seamless implementation, if provided with programmatic support and training. For example, the Zippy’s Friends program uses teachers to deliver the content materials [ 33 ] and teachers reported receiving substantial, helpful program support by research and program staff.
In their review of factors of success for implementation, adaptation of programing was identified as a key component of implementation [ 38 , 41 ]. Teachers of the Zippy’s Friends Program reported the ability to adapt, add and remove activities relating to thematic content based on student literacy, mood and timing, as one of the most important parts of program delivery [ 33 ]. This allowed the maintenance of high program fidelity while also involving students in the most effective way possible. Teachers are an important resource in the development of children’s resilience, as they already have rapport and an understanding of the students and are more likely to know their students lived experiences and current coping and help-seeking strategies. Yamamoto et al. credit their successful implementation of the YCDI! Program with the extensive edits to the curriculum to adapt it to Japanese culture and relationships [ 38 ].
The length of programing did not appear to impact on the number of outcomes achievable. The RALLY program ran for an entire school year and provided consistent resilience outcomes [ 36 ], while the Mindfulness-Based Stress Reduction program ran for only 12 weeks and showed positive resilience outcomes as well [ 30 ]. The YCDI! Program ran for a shorter period of time than most implementations of the program but still demonstrated significant results [ 38 ]. Importance was placed on the intensity of sessions and the content delivered, as opposed to the regularity. However, importantly, if follow up evaluations were conducted, they did not reveal that outcomes were maintained in the longer term after most programs. This suggests that program length may not alter the ongoing resiliency of students once the program ends.
Emergent themes across studies
Although all eleven articles presented programs that aimed at fostering the resilience skills and protective factors of students, the specific skills and outcomes taught in each program differed. This is consistent with research highlighting the difficulty that exists in defining resilience and creating programs around the topic [ 1 ]. Not only is the definition difficult and variable between studies, but the criteria and skills that come with developing resilience differ as well. In the RALLY study, researchers targeted resilience, and the outcomes evaluated were empathy, trust of others, and emotional regulation skills [ 36 ]. On the other hand, the UP study targeted resilience through social and emotional competencies that allow students to engage and navigate daily life, social interactions and society [ 37 ]. Both programs aimed to foster social and emotional development by increasing resilience skills and protective factors, but were based on differences in terminology and theory. Evaluations of both programs determined they had a positive outcome on resilience in students despite these differences.
An effect noted by a number of studies included in this review was the “ceiling effect” since many of the students enrolled in universal-based programs have high baseline mental health and social and emotional competence [ 33 ]. Although individuals within the group might suffer from higher risk factors or mental illness, across the board students present with generally normal levels. As such, when the program is implemented, outcomes may be generated but will not be large as there is little room for change. This is not the case when providing targeted programs with students who all generally have much more room for change, given that they begin the program with lower scores at baseline. Despite the ceiling effect, research has shown that resilience-boosting programing benefits at-risk but are not specific for at-risk children. Additionally, properly identifying and screening target groups for targeted programing is often unsuccessful due to the complexities of mental health, and preventive approaches, such as universal resilience-boosting programing, are considered the most all-encompassing method [ 42 ]. As such, a program promoting resilience will support positive changes and growth in both groups of kids, although with more significant differences in the at-risk group.
Characteristics and methodologies of evaluations
An element of the evaluations that emerged in many articles is the removed nature of evaluation when collecting data on children’s capacities. Many of the programs seek to foster resilience through the development of coping skills, and use scales or observations in order to measure outcomes. The Learn Young, Learn Fair program evaluated a positive effect on emotion-focused, adaptive coping skills using validated questionnaires and scales [ 39 ]. This approach is used in all the program evaluations, but does not leave room for lived experiences to be factored into the interpretation of outcomes. These traditional evaluation methodologies can be seen as researching on a topic, rather than researching for a cause or population, as they do not leave room for ambiguity or other factors.
Additionally, a couple of studies in this review used evaluation tools that did not take into account the views of children themselves. The researchers chose to interview and evaluate both teachers’ and the program deliverers’ perceptions and ratings, rather than interviewing or evaluating the children themselves. For example, Caldarella, Christensen et al. (2009) evaluate children’s outcomes through pre- and post-assessments of the teacher’s perceptions of her students, using validated assessment tools [ 40 ]. However, evaluations like this introduce an additional limitation to the outcome analysis, as they gather data through secondary sources with the program delivered to children for their benefit, but outcomes not gathered directly from the children. However, observational data is a key component of a program evaluation with many studies successfully using observations to ensure program fidelity and as part of process evaluations.
More insight around outcomes occurs when multiple evaluation tools and methods are used [ 43 ]. Clarke and colleagues (2015) evaluated the use of a participatory workshop determining children’s coping skills which used draw and write techniques that allowed children to share their feelings using their own words rather than those of researchers [ 44 ], as well as vignettes to eliminate interview processes [ 45 ]. Students from the intervention group were found to use more adaptive coping skills in their daily life, both in and out of the classroom than children in the control group [ 31 ]. These results were supported by the quantitative data collected on the larger student sample from which the participatory workshop subsample was drawn [ 33 ]. A clearer picture of children’s coping skills and experiences with the Zippy’s Friends program was gathered through the use of both qualitative and quantitative evaluation methodology. Additionally, children’s lived experiences and direct insights were gathered through the participatory workshop model, allowing for a greater breadth of understanding on the program’s efficiency.
Limitations of articles and evidence
Consideration must be given to the ethics and feasibility of implementing and evaluating programs for mental health promotion. Ethical concerns arise from providing a program that might be highly beneficial for a group of children, and not for another, essentially disadvantaging them. The ethics are further confounded by the lack of complete or stringent randomization described in the studies that include a control group. To avoid the dilemma of disadvantaging students, studies on success factors have highlighted that in many studies the control groups do not receive ‘no intervention’ [ 41 ]. For example, Sibinga et al. (2016) included an active control group. While the intervention group received the Mindfulness-Based Stress Reduction program being studied, the control group received Healthy Topics, a general health program to match the MBSR structure. Thus, while the control group students are not receiving a resilience-focused, mental health promotion program, they still receive a health promotion program but one which allows a distinction between control and intervention groups around resilience outcomes and mental health [ 30 ]. Yamamoto and colleagues, however, did not provide programing to the control group following the intervention [ 38 ].
The evidence provided by certain articles must be weighed with differing criteria. Seven articles evaluated a program against a control group, allowing for comparison of outcomes. These articles present more substantial outcome evidence than those that do not include a control group for comparison. For example, Nielsen and colleagues (2015) and Caldarella and colleagues (2009) did not have a control group, decreasing the strength of their evaluation. Nielsen et al. (2015) implemented the UP program in kindergarten through grade 9, but only evaluated grades 5–9. Such selective evaluation introduces potential bias and paired with the absence of a control group makes it difficult to identify if the increase in social and emotional competencies is due to the UP intervention, or simply a natural developmental progression [ 37 ].
A limitation of the evaluations in many programs is the involvement of the person delivering the program as the evaluator. This can be seen in many studies on the Zippy’s Friends program, where the classroom teacher delivers the program and conducts the process and implementation evaluation themselves. Third-party observations are sometimes conducted in addition to verify program fidelity and implementation outcomes. Of note is that observational evaluation and the use of independent evaluators have been more extensively documented as reliable than using tools based on self-report [ 41 ].
We also note that despite gender differences in the prevalence of mental health problems and the type of resilience protective factors that children and adolescents use, the studies did not generally report results by gender [ 46 , 47 ]. This limitation could be overcome by encouraging that future studies provide a gender breakdown or highlight gender-specific results.
This review complements previous reviews on mental health promotion programing for students. Our focus on universally delivered programs in primary schools reveals key components and strengths of programing that make for the most successful delivery and evaluation and enables important conclusions to be drawn.
The review confirms that adaptability and teacher involvement are key elements of program delivery, with student engagement and use of multiple methods strengthening program evaluation. The use of participatory methods to engage children allows for greater assessment of lived experiences and use of coping skills compared to self-reporting tools or observations. Adaptability of curriculum to different contexts, seen in the Zippy’s Friends program, was considered successful by multiple authors, illustrating that broad program application across multiple contexts is possible and effective.
This review demonstrates the importance of establishing key criteria to be measured during delivery and evaluation of youth mental health promotion programs, particularly in terms of defining resilience and its associated indicators. The successes of the programs detailed by the studies included in this review highlight the need for and benefits of such programs. Further research on primary-school, universally delivered mental health promotion programs could be conducted in specific contexts, particularly more difficult settings such as developing countries or conflict zones.
Abbreviations
Aussie optimism: positive thinking skills program
Children’s depression index
Mindfulness-Based stress reduction
Mixed methods appraisal tool
Western Australia
Kaufman J, Cook A, Arny L, Jones B, Pittinsky T. Problems defining resiliency: illustrations from the study of maltreated children. Dev Psychopathol. 1994;6(1):215–29.
Article Google Scholar
Grotberg EH: The international resilience project findings from the research and the effectiveness of interventions [microform] / Edith H. Grotberg. [Washington D.C.]: distributed by ERIC clearinghouse; 1996.
Greenberg M, Domitrovich C, Bumbarger B. The prevention of mental disorders in school-aged children: current state of the field. Prev Treat. 2001;4(1):1–62 https://www.researchgate.net/profile/Brian_Bumbarger/publication/216458565_The_Prevention_of_Mental_Disorders_in_School-Aged_Children_Current_State_of_the_Field/links/0fcfd50d20aaf66cf7000000/The-Prevention-of-Mental-Disorders-in-School-Aged-Children-Current-State-of-the-Field.pdf
Hodgson R, Abbasi T, Clarkson J. Effective mental health promotion: a literature review. Health Educ J. 1996;55(1):55–74.
Catalano RF, Berglund ML, Ryan JAM, Lonczak HS, Hawkins JD. Positive youth development in the United States: research findings on evaluations of positive youth development programs. ANNALS Am Acad Polit Soc Sci. 2004;591(1):98–124.
Benson PL, Saito RN. The Scientific Foundations of Youth Development. In: Benson PL, Pittman KJ, editors. Trends in Youth Development: Visions, Realities and Challenges. Boston, MA: Springer US; 2001. p. 135–54.
Chapter Google Scholar
Rose G. Sick individuals and sick populations. Int J Epidemiol. 2001;30(3):427–32.
Article PubMed Google Scholar
Catherine PB, LJ F. Editorial commentary: resilience in child development – interconnected pathways to wellbeing. J Child Psychol Psychiatry. 2013;54(4):333–6.
Karatsoreos IN, McEwen BS. Annual research review: the neurobiology and physiology of resilience and adaptation across the life course. J Child Psychol Psychiatry. 2013;54(4):337–47.
Bonanno GA, Diminich ED. Annual research review: positive adjustment to adversity – trajectories of minimal–impact resilience and emergent resilience. J Child Psychol Psychiatry. 2013;54(4):378–401.
Dante C. Annual research review: resilient functioning in maltreated children – past, present, and future perspectives. J Child Psychol Psychiatry. 2013;54(4):402–22.
Weare K, Nind M. Mental health promotion and problem prevention in schools: what does the evidence say? Health Promot Int. 2011;26(suppl 1):i29–69.
Adi Y, Killoran A, Janmohamed K, Stewart-Brown S. Systematic Review of the Effectiveness of Interventions to Promote Mental Wellbeing in Primary Schools: Universal Approaches Which Do not Focus on Violence or Bullying. London: National Institute for Clinical Excellence; 2007.
Google Scholar
Diekstra R. Effectiveness of school-based social and emotional education programmes worlwide - part one, a review of meta-analytic literature. In: Social and motional education: an international analysis edn.: Fundacion Marcelino Botin; 2008. p. 255–84.
Browne G, Gafni A, Roberts J, Byrne C, Majumdar B. Effective/efficient mental health programs for school-age children: a synthesis of reviews. Soc Sci Med. 2004;58(7):1367–84.
Durlak JA, Weissberg RP, Dymnicki AB, Taylor RD, Schellinger KB. The impact of enhancing students' social and emotional learning: a meta-analysis of school-based universal interventions. Child Dev. 2011;82(1):405–32.
Murphy JM, Abel MR, Hoover S, Jellinek M, Fazel M. Scope, scale, and dose of the world's largest school-based mental health programs. Harv Rev Psychiatry. 2017;25(5):218–28.
Dray J, Bowman J, Campbell E, Freund M, Wolfenden L, Hodder RK, McElwaine K, Tremain D, Bartlem K, Bailey J, et al. Systematic review of universal resilience-focused interventions targeting child and adolescent mental health in the school setting. J Am Acad Child Adolesc Psychiatry. 2017;56(10):813–24.
Wells J, Barlow J, Stewart-Brown S. A systematic review of universal approaches to mental health promotion in schools. Health Educ. 2003;103(4):197–220.
Durlak JA, Wells AM. Primary prevention mental health programs for children and adolescents: a meta-analytic review. Am J Community Psychol. 1997;25(2):115–52.
Zoritch B, Roberts I, Oakley A. The health and welfare effects of day-care: a systematic review of randomised controlled trials. Soc Sci Med (1982). 1998;47(3):317–27.
Gillham JE, Reivich KJ, Freres DR, Chaplin TM, Shatté AJ, Samuels B, Elkon AGL, Litzinger S, Lascher M, Gallop R, et al. School-based prevention of depressive symptoms: a randomized controlled study of the effectiveness and specificity of the Penn resiliency program. J Consult Clin Psychol. 2007;75(1):9–19.
Article PubMed PubMed Central Google Scholar
Vuijk P, van Lier PA, Crijnen AA, Huizink AC. Testing sex-specific pathways from peer victimization to anxiety and depression in early adolescents through a randomized intervention trial. J Affect Disord. 2007;100(1–3):221–6.
Dadds MR, Roth JH. Prevention of anxiety disorders: results of a universal trial with young children. J Child Fam Stud. 2008;17(3):320–35.
Sawyer MG, Pfeiffer S, Spence SH, Bond L, Graetz B, Kay D, Patton G, Sheffield J. School-based prevention of depression: a randomised controlled study of the beyondblue schools research initiative. J Child Psychol Psychiatry. 2010;51(2):199–209.
Iizuka CA, Barrett PM, Gillies R, Cook CR, Marinovic W. A combined intervention targeting both Teachers' and Students' social-emotional skills: preliminary evaluation of Students' outcomes. Aust J Guid Couns. 2014;24(2):152–66.
Rooney R, Hassan S, Kane R, Roberts CM, Nesa M. Reducing depression in 9-10 year old children in low SES schools: a longitudinal universal randomized controlled trial. Behav Res Ther. 2013;51(12):845–54.
Pluye P, Robert E, Cargo M, Bartlett G, O'Cathain A, Griffiths F, Boardman F, Gagnon MP, Rousseau MC. Proposal: A mixed methods appraisal tool for systematic mixed studies reviews. Montreal, Canada: McGill University; 2011.
National Collaborating Center for Methods and Tools. Appraising Qualitative, Quantitative, and Mixed Methods Studies included in Mixed Studies Reviews: The MMAT. Hamilton, ON: McMaster University; 2015.
Sibinga EMS, Webb L, Ghazarian SR, Ellen JM: School-based mindfulness instruction: an RCT. Pediatrics 2016, 137 (1) (no pagination)(e20152532).
Clarke AM, Sixsmith J, Barry MM. Evaluating the implementation of an emotional wellbeing programme for primary school children using participatory approaches. Health Educ J. 2015;74(5):578–93.
Mishara BL, Ystgaard M. Effectiveness of a mental health promotion program to improve coping skills in young children: Zippy's friends. Early Child Res Q. 2006;21(1):110–23.
Clarke AM, Bunting B, Barry MM. Evaluating the implementation of a school-based emotional well-being programme: a cluster randomized controlled trial of Zippy’s friends for children in disadvantaged primary schools. Health Educ Res. 2014;29(5):786–98.
Dufour S, Denoncourt J, Mishara BL. Improving Children's adaptation: new evidence regarding the effectiveness of Zippy's friends, a school mental health promotion program. Adv School Ment Health Promot. 2011;4(3):18–28.
Holen S, Waaktaar T, Lervåg A, Ystgaard M. The effectiveness of a universal school-based programme on coping and mental health: a randomised, controlled study of Zippy’s friends. Educ Psychol. 2012;32(5):657–77.
Malti T, Schwartz SE, Liu CH, Noam GG. Program evaluation: relationships as key to student development. New Dir Youth Dev. 2008;2008(120):151–77. Table of Contents
Nielsen L, Meilstrup C, Nelausen MK, Koushede V, Holstein BE. Promotion of social and emotional competence. Health Educ. 2015;115(3/4):339–56.
Yamamoto T, Matsumoto Y, Bernard ME. Effects of the cognitive-behavioral you can do it! Education program on the resilience of Japanese elementary school students: a preliminary investigation. Int J Educ Res. 2017;86:50–8.
Kraag G, Van Breukelen GJP, Kok G, Hosman C. Learn young, learn fair', a stress management program for fifth and sixth graders: longitudinal results from an experimental study. J Child Psychol Psychiatry. 2009;50(9):1185–95.
Caldarella P, Christensen L, Kramer TJ, Kronmiller K. Promoting social and emotional learning in second grade students: a study of the strong start curriculum. Early Childhood Educ J. 2009;37(1):51–6.
Durlak JA, DuPre EP. Implementation matters: a review of research on the influence of implementation on program outcomes and the factors affecting implementation. Am J Community Psychol. 2008;41(3–4):327–50.
Moore, TG. Rethinking universal and targeted services. CCCH Working Paper 2. August 2008. Parkville, Victoria: Centre for Community Child Health.
Darbyshire P, MacDougall C, Schiller W. Multiple methods in qualitative research with children: more insight or just more? Qual Res. 2005;5(4):417–36.
Pridmore P, Bendelow G. Images of health: exploring beliefs of children using the 'draw-and-write' technique. Health Educ J. 1995;54(4):473–88.
Barter C, Renold E. 'I wanna tell you a story': exploring the application of vignettes in qualitative research with children and young people. Int J Soc Res Methodol. 2000;3(4):307–23.
Lengua LJ, Stormshak EA. Gender, Gender Roles, and Personality: gender differences in the prediction of coping and psychological symptoms. Sex Roles. 2000;43(11):787–820.
Wasonga T, Christman DE, Kilmer L. Ethnicity, Gender and Age: predicting resilience and academic achievement among urban high school students. Am Second Educ. 2003;32(1):62–74.
Download references
Acknowledgements
We thank Georgetown University, Dr. Helen Fairnie-Jones and staff at the WA Centre for Rural Health for assistance that enabled this work to be undertaken. We particularly thank May Doncon for her valuable help in early discussions and highlighting the importance of the topic.
Availability of data and materials
Data sharing is not applicable to this article as no datasets were generated or analyzed during the current study.
Author information
Authors and affiliations.
Western Australian Centre for Rural Health, University of Western Australia, 167 Fitzgerald St, Geraldton, WA, 6531, Australia
Amanda Fenwick-Smith, Emma E. Dahlberg & Sandra C. Thompson
You can also search for this author in PubMed Google Scholar
Contributions
AF determined the search strategy, conducted the systematic review of the databases, and wrote all parts of the review. AF, ED and ST read all full text articles and agreed upon inclusion and exclusion of articles. AF and ED conducted independent applications of MMAT to the articles, and came to a consensus on article strength. ED assisted in writing the results and discussion section as well. AF and ST edited the article for content and errors. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Sandra C. Thompson .
Ethics declarations
Ethics approval and consent to participate.
Not applicable as all literature is published.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License ( http://creativecommons.org/licenses/by/4.0/ ), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated.
Reprints and permissions
About this article
Cite this article.
Fenwick-Smith, A., Dahlberg, E.E. & Thompson, S.C. Systematic review of resilience-enhancing, universal, primary school-based mental health promotion programs. BMC Psychol 6 , 30 (2018). https://doi.org/10.1186/s40359-018-0242-3
Download citation
Received : 27 April 2018
Accepted : 14 June 2018
Published : 05 July 2018
DOI : https://doi.org/10.1186/s40359-018-0242-3
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Mental health
- Health promotion
- Primary school
- Universal intervention
BMC Psychology
ISSN: 2050-7283
- General enquiries: [email protected]

IMAGES
VIDEO
COMMENTS
Scope of Mental Health Promotion and Prevention in the Current Situation. Literature provides considerable evidence on the effectiveness of various preventive mental health interventions targeting risk and protective factors for various mental illnesses (18, 36-42).There is also modest evidence of the effectiveness of programs focusing on early identification and intervention for severe ...
For the current review, key terms like "mental health promotion," OR "protection," OR "prevention," OR "mitigation" were used to search relevant literature on Google Scholar, PubMed, and Cochrane library databases, considering a time period between 2000 to 2019 (Supplementary Material 1). However, we have restricted our search ...
Study design. We will conduct a systematic scoping review using the 6-stage scoping review framework [19, 20] to systematically identify the implementation evidence and factors associated with successful implementation of mental health promotion in workplace settings.Scoping reviews aim to map a broad field of literature and to summarise and disseminate research findings [19, 21], rather than ...
Background This systematic review provides a narrative synthesis of the evidence on the effectiveness of mental health promotion interventions for young people in low and middle-income countries (LMICs). Commissioned by the WHO, a review of the evidence for mental health promotion interventions across the lifespan from early years to adulthood was conducted. This paper reports on the findings ...
Effective mental health promotion: a literature review. Ray Hodgson, Tina Abbasi, and Johanna Clarkson View all authors and affiliations. Volume 55, Issue 1. ... Mental Health Promotion Theory and Practice: Insights from a Literatur... Go to citation Crossref Google Scholar.
Classification as primary, secondary, or tertiary prevention is based on when during the course of disease the intervention is provided. Another approach to classification—as universal, selective, or indicated preventive interventions—relates to who receives the intervention. The social determinants of health framework also provides a guide to prevention, which requires changing both ...
Mental Health Promotion Theory and Practice: Insights from a Literature Review - Author: Natasha Mauthner, Michael Killoran‐Ross, Jane Brown. This article reports on a literature review of interventions specifically identified as emanating from a mental health promotion (as opposed to prevention) paradigm. A number of recurring debates in the ...
The authors reviewed the current state of knowledge on school mental health promotion interventions globally. Two major databases, SCOPUS and ERIC were utilised to capture the social science, health, arts and humanities, and education literature. Initial searches identified 25 articles reporting on mental health promotion interventions in schools.
TLDR. The current review aimed to synthesize existing literature on various mental health promotion and prevention interventions and their effectiveness and highlight various novel approaches to mental health care and their implications across different resource settings and provide future directions. Expand. 12. PDF.
Promotion—A Narrative Review. Vijender Singh, Akash Kumar and Snehil Gupta *. Department of Psychiatry, All India Institute of Medical Sciences Bhopal, Bhopal, India. Extant literature has ...
With an increased political interest in school-based mental health education, the dominant understanding and measurement of mental health literacy (MHL) in adolescent research should be critically appraised. This systematic literature review aimed to investigate the conceptualisation and measurement of MHL in adolescent research and the extent of methodological homogeneity in the field for ...
Promoting University Students' Mental Health: A Systematic Literature Review Introducing the 4M-Model of Individual-Level Interventions. ... Dooris M. Holistic and sustainable health improvement: the contribution of the settings-based approach to health promotion. Perspect Public Health. (2009) 129:29-36. doi: 10.1177/1757913908098881.
A scoping review of the academic literature on the mental health of physicians and physicians-in-training in North America was conducted using Arksey and O'Malley's [] methodological framework.Our review objectives and broad focus, including the general questions posed to conduct the review, lend themselves to a scoping review approach, which is suitable for the analysis of a broader range ...
Key issues critical to the future development of mental health promotion are highlighted, including the implications ofmental health promotion being at an embryonic stage of development, the need for greater reflexivity, theneed for integration, and issues concerning professional identity and practice in the mental health Promotion field. This article reports on a literature review of ...
Wellbeing and resilience are essential in preventing and reducing the severity of mental health problems. Equipping children with coping skills and protective behavior can help them react positively to change and obstacles in life, allowing greater mental, social and academic success. This systematic review studies the implementation and evaluation of universal, resilience-focused mental ...
promotion of mental health and wellbeing. The VicHealth Mental Health Promotion Framework identified three determinants of mental health: 'social connectedness', 'freedom from discrimination and violence', and 'economic participation'. In 2003 the Sydney Health Projects Group was commissioned to undertake a review of the
Health Promotion: A Literature Review. January 2012; Publisher: (HaPAN) Health Promotion Advocacy Network: Rajarata University of Sri Lanka ... "Health is a state of complete physical, mental ...
International Journal of Mental Health Nursing is a mental health journal examining trends and developments in mental health practice and research. Abstract This review examines factors associated with quality of life (QoL) in persons with young-onset dementia (YOD).