
The Research Gap (Literature Gap)
Everything you need to know to find a quality research gap
By: Ethar Al-Saraf (PhD) | Expert Reviewed By: Eunice Rautenbach (DTech) | November 2022
If you’re just starting out in research, chances are you’ve heard about the elusive research gap (also called a literature gap). In this post, we’ll explore the tricky topic of research gaps. We’ll explain what a research gap is, look at the four most common types of research gaps, and unpack how you can go about finding a suitable research gap for your dissertation, thesis or research project.
Overview: Research Gap 101
- What is a research gap
- Four common types of research gaps
- Practical examples
- How to find research gaps
- Recap & key takeaways
What (exactly) is a research gap?
Well, at the simplest level, a research gap is essentially an unanswered question or unresolved problem in a field, which reflects a lack of existing research in that space. Alternatively, a research gap can also exist when there’s already a fair deal of existing research, but where the findings of the studies pull in different directions , making it difficult to draw firm conclusions.
For example, let’s say your research aims to identify the cause (or causes) of a particular disease. Upon reviewing the literature, you may find that there’s a body of research that points toward cigarette smoking as a key factor – but at the same time, a large body of research that finds no link between smoking and the disease. In that case, you may have something of a research gap that warrants further investigation.
Now that we’ve defined what a research gap is – an unanswered question or unresolved problem – let’s look at a few different types of research gaps.
Types of research gaps
While there are many different types of research gaps, the four most common ones we encounter when helping students at Grad Coach are as follows:
- The classic literature gap
- The disagreement gap
- The contextual gap, and
- The methodological gap
Need a helping hand?
1. The Classic Literature Gap
First up is the classic literature gap. This type of research gap emerges when there’s a new concept or phenomenon that hasn’t been studied much, or at all. For example, when a social media platform is launched, there’s an opportunity to explore its impacts on users, how it could be leveraged for marketing, its impact on society, and so on. The same applies for new technologies, new modes of communication, transportation, etc.
Classic literature gaps can present exciting research opportunities , but a drawback you need to be aware of is that with this type of research gap, you’ll be exploring completely new territory . This means you’ll have to draw on adjacent literature (that is, research in adjacent fields) to build your literature review, as there naturally won’t be very many existing studies that directly relate to the topic. While this is manageable, it can be challenging for first-time researchers, so be careful not to bite off more than you can chew.
2. The Disagreement Gap
As the name suggests, the disagreement gap emerges when there are contrasting or contradictory findings in the existing research regarding a specific research question (or set of questions). The hypothetical example we looked at earlier regarding the causes of a disease reflects a disagreement gap.
Importantly, for this type of research gap, there needs to be a relatively balanced set of opposing findings . In other words, a situation where 95% of studies find one result and 5% find the opposite result wouldn’t quite constitute a disagreement in the literature. Of course, it’s hard to quantify exactly how much weight to give to each study, but you’ll need to at least show that the opposing findings aren’t simply a corner-case anomaly .

3. The Contextual Gap
The third type of research gap is the contextual gap. Simply put, a contextual gap exists when there’s already a decent body of existing research on a particular topic, but an absence of research in specific contexts .
For example, there could be a lack of research on:
- A specific population – perhaps a certain age group, gender or ethnicity
- A geographic area – for example, a city, country or region
- A certain time period – perhaps the bulk of the studies took place many years or even decades ago and the landscape has changed.
The contextual gap is a popular option for dissertations and theses, especially for first-time researchers, as it allows you to develop your research on a solid foundation of existing literature and potentially even use existing survey measures.
Importantly, if you’re gonna go this route, you need to ensure that there’s a plausible reason why you’d expect potential differences in the specific context you choose. If there’s no reason to expect different results between existing and new contexts, the research gap wouldn’t be well justified. So, make sure that you can clearly articulate why your chosen context is “different” from existing studies and why that might reasonably result in different findings.

4. The Methodological Gap
Last but not least, we have the methodological gap. As the name suggests, this type of research gap emerges as a result of the research methodology or design of existing studies. With this approach, you’d argue that the methodology of existing studies is lacking in some way , or that they’re missing a certain perspective.
For example, you might argue that the bulk of the existing research has taken a quantitative approach, and therefore there is a lack of rich insight and texture that a qualitative study could provide. Similarly, you might argue that existing studies have primarily taken a cross-sectional approach , and as a result, have only provided a snapshot view of the situation – whereas a longitudinal approach could help uncover how constructs or variables have evolved over time.

Practical Examples
Let’s take a look at some practical examples so that you can see how research gaps are typically expressed in written form. Keep in mind that these are just examples – not actual current gaps (we’ll show you how to find these a little later!).
Context: Healthcare
Despite extensive research on diabetes management, there’s a research gap in terms of understanding the effectiveness of digital health interventions in rural populations (compared to urban ones) within Eastern Europe.
Context: Environmental Science
While a wealth of research exists regarding plastic pollution in oceans, there is significantly less understanding of microplastic accumulation in freshwater ecosystems like rivers and lakes, particularly within Southern Africa.
Context: Education
While empirical research surrounding online learning has grown over the past five years, there remains a lack of comprehensive studies regarding the effectiveness of online learning for students with special educational needs.
As you can see in each of these examples, the author begins by clearly acknowledging the existing research and then proceeds to explain where the current area of lack (i.e., the research gap) exists.
How To Find A Research Gap
Now that you’ve got a clearer picture of the different types of research gaps, the next question is of course, “how do you find these research gaps?” .
Well, we cover the process of how to find original, high-value research gaps in a separate post . But, for now, I’ll share a basic two-step strategy here to help you find potential research gaps.
As a starting point, you should find as many literature reviews, systematic reviews and meta-analyses as you can, covering your area of interest. Additionally, you should dig into the most recent journal articles to wrap your head around the current state of knowledge. It’s also a good idea to look at recent dissertations and theses (especially doctoral-level ones). Dissertation databases such as ProQuest, EBSCO and Open Access are a goldmine for this sort of thing. Importantly, make sure that you’re looking at recent resources (ideally those published in the last year or two), or the gaps you find might have already been plugged by other researchers.
Once you’ve gathered a meaty collection of resources, the section that you really want to focus on is the one titled “ further research opportunities ” or “further research is needed”. In this section, the researchers will explicitly state where more studies are required – in other words, where potential research gaps may exist. You can also look at the “ limitations ” section of the studies, as this will often spur ideas for methodology-based research gaps.
By following this process, you’ll orient yourself with the current state of research , which will lay the foundation for you to identify potential research gaps. You can then start drawing up a shortlist of ideas and evaluating them as candidate topics . But remember, make sure you’re looking at recent articles – there’s no use going down a rabbit hole only to find that someone’s already filled the gap 🙂
Let’s Recap
We’ve covered a lot of ground in this post. Here are the key takeaways:
- A research gap is an unanswered question or unresolved problem in a field, which reflects a lack of existing research in that space.
- The four most common types of research gaps are the classic literature gap, the disagreement gap, the contextual gap and the methodological gap.
- To find potential research gaps, start by reviewing recent journal articles in your area of interest, paying particular attention to the FRIN section .
If you’re keen to learn more about research gaps and research topic ideation in general, be sure to check out the rest of the Grad Coach Blog . Alternatively, if you’re looking for 1-on-1 support with your dissertation, thesis or research project, be sure to check out our private coaching service .

Psst... there’s more!
This post was based on one of our popular Research Bootcamps . If you're working on a research project, you'll definitely want to check this out ...
You Might Also Like:

32 Comments
This post is REALLY more than useful, Thank you very very much
Very helpful specialy, for those who are new for writing a research! So thank you very much!!
I found it very helpful article. Thank you.
Just at the time when I needed it, really helpful.
Very helpful and well-explained. Thank you
VERY HELPFUL
We’re very grateful for your guidance, indeed we have been learning a lot from you , so thank you abundantly once again.
hello brother could you explain to me this question explain the gaps that researchers are coming up with ?
Am just starting to write my research paper. your publication is very helpful. Thanks so much
How to cite the author of this?
your explanation very help me for research paper. thank you
Very important presentation. Thanks.
Best Ideas. Thank you.
I found it’s an excellent blog to get more insights about the Research Gap. I appreciate it!
Kindly explain to me how to generate good research objectives.
This is very helpful, thank you
How to tabulate research gap
Very helpful, thank you.
Thanks a lot for this great insight!
This is really helpful indeed!
This article is really helpfull in discussing how will we be able to define better a research problem of our interest. Thanks so much.
Reading this just in good time as i prepare the proposal for my PhD topic defense.
Very helpful Thanks a lot.
Thank you very much
This was very timely. Kudos
Great one! Thank you all.
Thank you very much.
This is so enlightening. Disagreement gap. Thanks for the insight.
How do I Cite this document please?
Research gap about career choice given me Example bro?
I found this information so relevant as I am embarking on a Masters Degree. Thank you for this eye opener. It make me feel I can work diligently and smart on my research proposal.
Submit a Comment Cancel reply
Your email address will not be published. Required fields are marked *
Save my name, email, and website in this browser for the next time I comment.
- Print Friendly
- Privacy Policy

Home » Research Gap – Types, Examples and How to Identify
Research Gap – Types, Examples and How to Identify
Table of Contents

Research Gap
Definition:
Research gap refers to an area or topic within a field of study that has not yet been extensively researched or is yet to be explored. It is a question, problem or issue that has not been addressed or resolved by previous research.
How to Identify Research Gap
Identifying a research gap is an essential step in conducting research that adds value and contributes to the existing body of knowledge. Research gap requires critical thinking, creativity, and a thorough understanding of the existing literature . It is an iterative process that may require revisiting and refining your research questions and ideas multiple times.
Here are some steps that can help you identify a research gap:
- Review existing literature: Conduct a thorough review of the existing literature in your research area. This will help you identify what has already been studied and what gaps still exist.
- Identify a research problem: Identify a specific research problem or question that you want to address.
- Analyze existing research: Analyze the existing research related to your research problem. This will help you identify areas that have not been studied, inconsistencies in the findings, or limitations of the previous research.
- Brainstorm potential research ideas : Based on your analysis, brainstorm potential research ideas that address the identified gaps.
- Consult with experts: Consult with experts in your research area to get their opinions on potential research ideas and to identify any additional gaps that you may have missed.
- Refine research questions: Refine your research questions and hypotheses based on the identified gaps and potential research ideas.
- Develop a research proposal: Develop a research proposal that outlines your research questions, objectives, and methods to address the identified research gap.
Types of Research Gap
There are different types of research gaps that can be identified, and each type is associated with a specific situation or problem. Here are the main types of research gaps and their explanations:
Theoretical Gap
This type of research gap refers to a lack of theoretical understanding or knowledge in a particular area. It can occur when there is a discrepancy between existing theories and empirical evidence or when there is no theory that can explain a particular phenomenon. Identifying theoretical gaps can lead to the development of new theories or the refinement of existing ones.
Empirical Gap
An empirical gap occurs when there is a lack of empirical evidence or data in a particular area. It can happen when there is a lack of research on a specific topic or when existing research is inadequate or inconclusive. Identifying empirical gaps can lead to the development of new research studies to collect data or the refinement of existing research methods to improve the quality of data collected.
Methodological Gap
This type of research gap refers to a lack of appropriate research methods or techniques to answer a research question. It can occur when existing methods are inadequate, outdated, or inappropriate for the research question. Identifying methodological gaps can lead to the development of new research methods or the modification of existing ones to better address the research question.
Practical Gap
A practical gap occurs when there is a lack of practical applications or implementation of research findings. It can occur when research findings are not implemented due to financial, political, or social constraints. Identifying practical gaps can lead to the development of strategies for the effective implementation of research findings in practice.
Knowledge Gap
This type of research gap occurs when there is a lack of knowledge or information on a particular topic. It can happen when a new area of research is emerging, or when research is conducted in a different context or population. Identifying knowledge gaps can lead to the development of new research studies or the extension of existing research to fill the gap.
Examples of Research Gap
Here are some examples of research gaps that researchers might identify:
- Theoretical Gap Example : In the field of psychology, there might be a theoretical gap related to the lack of understanding of the relationship between social media use and mental health. Although there is existing research on the topic, there might be a lack of consensus on the mechanisms that link social media use to mental health outcomes.
- Empirical Gap Example : In the field of environmental science, there might be an empirical gap related to the lack of data on the long-term effects of climate change on biodiversity in specific regions. Although there might be some studies on the topic, there might be a lack of data on the long-term effects of climate change on specific species or ecosystems.
- Methodological Gap Example : In the field of education, there might be a methodological gap related to the lack of appropriate research methods to assess the impact of online learning on student outcomes. Although there might be some studies on the topic, existing research methods might not be appropriate to assess the complex relationships between online learning and student outcomes.
- Practical Gap Example: In the field of healthcare, there might be a practical gap related to the lack of effective strategies to implement evidence-based practices in clinical settings. Although there might be existing research on the effectiveness of certain practices, they might not be implemented in practice due to various barriers, such as financial constraints or lack of resources.
- Knowledge Gap Example: In the field of anthropology, there might be a knowledge gap related to the lack of understanding of the cultural practices of indigenous communities in certain regions. Although there might be some research on the topic, there might be a lack of knowledge about specific cultural practices or beliefs that are unique to those communities.
Examples of Research Gap In Literature Review, Thesis, and Research Paper might be:
- Literature review : A literature review on the topic of machine learning and healthcare might identify a research gap in the lack of studies that investigate the use of machine learning for early detection of rare diseases.
- Thesis : A thesis on the topic of cybersecurity might identify a research gap in the lack of studies that investigate the effectiveness of artificial intelligence in detecting and preventing cyber attacks.
- Research paper : A research paper on the topic of natural language processing might identify a research gap in the lack of studies that investigate the use of natural language processing techniques for sentiment analysis in non-English languages.
How to Write Research Gap
By following these steps, you can effectively write about research gaps in your paper and clearly articulate the contribution that your study will make to the existing body of knowledge.
Here are some steps to follow when writing about research gaps in your paper:
- Identify the research question : Before writing about research gaps, you need to identify your research question or problem. This will help you to understand the scope of your research and identify areas where additional research is needed.
- Review the literature: Conduct a thorough review of the literature related to your research question. This will help you to identify the current state of knowledge in the field and the gaps that exist.
- Identify the research gap: Based on your review of the literature, identify the specific research gap that your study will address. This could be a theoretical, empirical, methodological, practical, or knowledge gap.
- Provide evidence: Provide evidence to support your claim that the research gap exists. This could include a summary of the existing literature, a discussion of the limitations of previous studies, or an analysis of the current state of knowledge in the field.
- Explain the importance: Explain why it is important to fill the research gap. This could include a discussion of the potential implications of filling the gap, the significance of the research for the field, or the potential benefits to society.
- State your research objectives: State your research objectives, which should be aligned with the research gap you have identified. This will help you to clearly articulate the purpose of your study and how it will address the research gap.
Importance of Research Gap
The importance of research gaps can be summarized as follows:
- Advancing knowledge: Identifying research gaps is crucial for advancing knowledge in a particular field. By identifying areas where additional research is needed, researchers can fill gaps in the existing body of knowledge and contribute to the development of new theories and practices.
- Guiding research: Research gaps can guide researchers in designing studies that fill those gaps. By identifying research gaps, researchers can develop research questions and objectives that are aligned with the needs of the field and contribute to the development of new knowledge.
- Enhancing research quality: By identifying research gaps, researchers can avoid duplicating previous research and instead focus on developing innovative research that fills gaps in the existing body of knowledge. This can lead to more impactful research and higher-quality research outputs.
- Informing policy and practice: Research gaps can inform policy and practice by highlighting areas where additional research is needed to inform decision-making. By filling research gaps, researchers can provide evidence-based recommendations that have the potential to improve policy and practice in a particular field.
Applications of Research Gap
Here are some potential applications of research gap:
- Informing research priorities: Research gaps can help guide research funding agencies and researchers to prioritize research areas that require more attention and resources.
- Identifying practical implications: Identifying gaps in knowledge can help identify practical applications of research that are still unexplored or underdeveloped.
- Stimulating innovation: Research gaps can encourage innovation and the development of new approaches or methodologies to address unexplored areas.
- Improving policy-making: Research gaps can inform policy-making decisions by highlighting areas where more research is needed to make informed policy decisions.
- Enhancing academic discourse: Research gaps can lead to new and constructive debates and discussions within academic communities, leading to more robust and comprehensive research.
Advantages of Research Gap
Here are some of the advantages of research gap:
- Identifies new research opportunities: Identifying research gaps can help researchers identify areas that require further exploration, which can lead to new research opportunities.
- Improves the quality of research: By identifying gaps in current research, researchers can focus their efforts on addressing unanswered questions, which can improve the overall quality of research.
- Enhances the relevance of research: Research that addresses existing gaps can have significant implications for the development of theories, policies, and practices, and can therefore increase the relevance and impact of research.
- Helps avoid duplication of effort: Identifying existing research can help researchers avoid duplicating efforts, saving time and resources.
- Helps to refine research questions: Research gaps can help researchers refine their research questions, making them more focused and relevant to the needs of the field.
- Promotes collaboration: By identifying areas of research that require further investigation, researchers can collaborate with others to conduct research that addresses these gaps, which can lead to more comprehensive and impactful research outcomes.
Disadvantages of Research Gap
While research gaps can be advantageous, there are also some potential disadvantages that should be considered:
- Difficulty in identifying gaps: Identifying gaps in existing research can be challenging, particularly in fields where there is a large volume of research or where research findings are scattered across different disciplines.
- Lack of funding: Addressing research gaps may require significant resources, and researchers may struggle to secure funding for their work if it is perceived as too risky or uncertain.
- Time-consuming: Conducting research to address gaps can be time-consuming, particularly if the research involves collecting new data or developing new methods.
- Risk of oversimplification: Addressing research gaps may require researchers to simplify complex problems, which can lead to oversimplification and a failure to capture the complexity of the issues.
- Bias : Identifying research gaps can be influenced by researchers’ personal biases or perspectives, which can lead to a skewed understanding of the field.
- Potential for disagreement: Identifying research gaps can be subjective, and different researchers may have different views on what constitutes a gap in the field, leading to disagreements and debate.
About the author
Muhammad Hassan
Researcher, Academic Writer, Web developer
You may also like

Data Collection – Methods Types and Examples

Delimitations in Research – Types, Examples and...

Research Process – Steps, Examples and Tips

Research Design – Types, Methods and Examples

Institutional Review Board – Application Sample...

Evaluating Research – Process, Examples and...

Identifying Research Gaps to Pursue Innovative Research
This article is an excerpt from a lecture given by my Ph.D. guide, a researcher in public health. She advised us on how to identify research gaps to pursue innovative research in our fields.
What is a Research Gap?
Today we are talking about the research gap: what is it, how to identify it, and how to make use of it so that you can pursue innovative research. Now, how many of you have ever felt you had discovered a new and exciting research question , only to find that it had already been written about? I have experienced this more times than I can count. Graduate studies come with pressure to add new knowledge to the field. We can contribute to the progress and knowledge of humanity. To do this, we need to first learn to identify research gaps in the existing literature.
A research gap is, simply, a topic or area for which missing or insufficient information limits the ability to reach a conclusion for a question. It should not be confused with a research question, however. For example, if we ask the research question of what the healthiest diet for humans is, we would find many studies and possible answers to this question. On the other hand, if we were to ask the research question of what are the effects of antidepressants on pregnant women, we would not find much-existing data. This is a research gap. When we identify a research gap, we identify a direction for potentially new and exciting research.
How to Identify Research Gap?
Considering the volume of existing research, identifying research gaps can seem overwhelming or even impossible. I don’t have time to read every paper published on public health. Similarly, you guys don’t have time to read every paper. So how can you identify a research gap?
There are different techniques in various disciplines, but we can reduce most of them down to a few steps, which are:
- Identify your key motivating issue/question
- Identify key terms associated with this issue
- Review the literature, searching for these key terms and identifying relevant publications
- Review the literature cited by the key publications which you located in the above step
- Identify issues not addressed by the literature relating to your critical motivating issue
It is the last step which we all find the most challenging. It can be difficult to figure out what an article is not saying. I like to keep a list of notes of biased or inconsistent information. You could also track what authors write as “directions for future research,” which often can point us towards the existing gaps.
Different Types of Research Gaps
Identifying research gaps is an essential step in conducting research, as it helps researchers to refine their research questions and to focus their research efforts on areas where there is a need for more knowledge or understanding.
1. Knowledge gaps
These are gaps in knowledge or understanding of a subject, where more research is needed to fill the gaps. For example, there may be a lack of understanding of the mechanisms behind a particular disease or how a specific technology works.
2. Conceptual gaps
These are gaps in the conceptual framework or theoretical understanding of a subject. For example, there may be a need for more research to understand the relationship between two concepts or to refine a theoretical framework.
3. Methodological gaps
These are gaps in the methods used to study a particular subject. For example, there may be a need for more research to develop new research methods or to refine existing methods to address specific research questions.
4. Data gaps
These are gaps in the data available on a particular subject. For example, there may be a need for more research to collect data on a specific population or to develop new measures to collect data on a particular construct.
5. Practical gaps
These are gaps in the application of research findings to practical situations. For example, there may be a need for more research to understand how to implement evidence-based practices in real-world settings or to identify barriers to implementing such practices.
Examples of Research Gap
Limited understanding of the underlying mechanisms of a disease:.
Despite significant research on a particular disease, there may be a lack of understanding of the underlying mechanisms of the disease. For example, although much research has been done on Alzheimer’s disease, the exact mechanisms that lead to the disease are not yet fully understood.
Inconsistencies in the findings of previous research:
When previous research on a particular topic has inconsistent findings, there may be a need for further research to clarify or resolve these inconsistencies. For example, previous research on the effectiveness of a particular treatment for a medical condition may have produced inconsistent findings, indicating a need for further research to determine the true effectiveness of the treatment.
Limited research on emerging technologies:
As new technologies emerge, there may be limited research on their applications, benefits, and potential drawbacks. For example, with the increasing use of artificial intelligence in various industries, there is a need for further research on the ethical, legal, and social implications of AI.
How to Deal with Literature Gap?
Once you have identified the literature gaps, it is critical to prioritize. You may find many questions which remain to be answered in the literature. Often one question must be answered before the next can be addressed. In prioritizing the gaps, you have identified, you should consider your funding agency or stakeholders, the needs of the field, and the relevance of your questions to what is currently being studied. Also, consider your own resources and ability to conduct the research you’re considering. Once you have done this, you can narrow your search down to an appropriate question.
Tools to Help Your Search
There are thousands of new articles published every day, and staying up to date on the literature can be overwhelming. You should take advantage of the technology that is available. Some services include PubCrawler , Feedly , Google Scholar , and PubMed updates. Stay up to date on social media forums where scholars share new discoveries, such as Twitter. Reference managers such as Mendeley can help you keep your references well-organized. I personally have had success using Google Scholar and PubMed to stay current on new developments and track which gaps remain in my personal areas of interest.
The most important thing I want to impress upon you today is that you will struggle to choose a research topic that is innovative and exciting if you don’t know the existing literature well. This is why identifying research gaps starts with an extensive and thorough literature review . But give yourself some boundaries. You don’t need to read every paper that has ever been written on a topic. You may find yourself thinking you’re on the right track and then suddenly coming across a paper that you had intended to write! It happens to everyone- it happens to me quite often. Don’t give up- keep reading and you’ll find what you’re looking for.
Class dismissed!
How do you identify research gaps? Share your thoughts in the comments section below.
Frequently Asked Questions
A research gap can be identified by looking for a topic or area with missing or insufficient information that limits the ability to reach a conclusion for a question.
Identifying a research gap is important as it provides a direction for potentially new research or helps bridge the gap in existing literature.
Gap in research is a topic or area with missing or insufficient information. A research gap limits the ability to reach a conclusion for a question.
Thank u for your suggestion.
Very useful tips specially for a beginner
Thank you. This is helpful. I find that I’m overwhelmed with literatures. As I read on a particular topic, and in a particular direction I find that other conflicting issues, topic a and ideas keep popping up, making me more confused.
I am very grateful for your advice. It’s just on point.
The clearest, exhaustive, and brief explanation I have ever read.
Thanks for sharing
Thank you very much.The work is brief and understandable
Thank you it is very informative
Thanks for sharing this educative article
Thank you for such informative explanation.
Great job smart guy! Really outdid yourself!
Nice one! I thank you for this as it is just what I was looking for!😃🤟
Thank you so much for this. Much appreciated
Thank you so much.
Thankyou for ur briefing…its so helpful
Thank you so much .I’ved learn a lot from this.❤️
Rate this article Cancel Reply
Your email address will not be published.

Enago Academy's Most Popular Articles

- Reporting Research
Choosing the Right Analytical Approach: Thematic analysis vs. content analysis for data interpretation
In research, choosing the right approach to understand data is crucial for deriving meaningful insights.…

Comparing Cross Sectional and Longitudinal Studies: 5 steps for choosing the right approach
The process of choosing the right research design can put ourselves at the crossroads of…

- Career Corner
Unlocking the Power of Networking in Academic Conferences
Embarking on your first academic conference experience? Fear not, we got you covered! Academic conferences…

Research Recommendations – Guiding policy-makers for evidence-based decision making
Research recommendations play a crucial role in guiding scholars and researchers toward fruitful avenues of…

- AI in Academia
Disclosing the Use of Generative AI: Best practices for authors in manuscript preparation
The rapid proliferation of generative and other AI-based tools in research writing has ignited an…
Intersectionality in Academia: Dealing with diverse perspectives
Meritocracy and Diversity in Science: Increasing inclusivity in STEM education
Avoiding the AI Trap: Pitfalls of relying on ChatGPT for PhD applications

Sign-up to read more
Subscribe for free to get unrestricted access to all our resources on research writing and academic publishing including:
- 2000+ blog articles
- 50+ Webinars
- 10+ Expert podcasts
- 50+ Infographics
- 10+ Checklists
- Research Guides
We hate spam too. We promise to protect your privacy and never spam you.
I am looking for Editing/ Proofreading services for my manuscript Tentative date of next journal submission:

As a researcher, what do you consider most when choosing an image manipulation detector?

- [email protected]
- Shapiro Library
- SNHU Library Frequently Asked Questions
FAQ: What is a research gap and how do I find one?
- 7 Academic Integrity & Plagiarism
- 64 Academic Support, Writing Help, & Presentation Help
- 29 Access/Remote Access
- 7 Accessibility
- 9 Building/Facilities
- 7 Career/Job Information
- 26 Catalog/Print Books
- 26 Circulation
- 129 Citing Sources
- 14 Copyright
- 311 Databases
- 24 Directions/Location
- 18 Faculty Resources/Needs
- 7 Hours/Contacts
- 2 Innovation Lab & Makerspace/3D Printing
- 25 Interlibrary Loan
- 43 IT/Computer/Printing Support
- 3 Library Instruction
- 39 Library Technology Help
- 6 Multimedia
- 17 Online Programs
- 19 Periodicals
- 25 Policies
- 8 RefWorks/Citation Managers
- 4 Research Guides (LibGuides)
- 216 Research Help
- 23 University Services
Last Updated: Jun 27, 2023 Views: 475194
What is a research gap.
A research gap is a question or a problem that has not been answered by any of the existing studies or research within your field. Sometimes, a research gap exists when there is a concept or new idea that hasn't been studied at all. Sometimes you'll find a research gap if all the existing research is outdated and in need of new/updated research (studies on Internet use in 2001, for example). Or, perhaps a specific population has not been well studied (perhaps there are plenty of studies on teenagers and video games, but not enough studies on toddlers and video games, for example). These are just a few examples, but any research gap you find is an area where more studies and more research need to be conducted. Please view this video clip from our Sage Research Methods database for more helpful information: How Do You Identify Gaps in Literature?
How do I find one?
It will take a lot of research and reading. You'll need to be very familiar with all the studies that have already been done, and what those studies contributed to the overall body of knowledge about that topic. Make a list of any questions you have about your topic and then do some research to see if those questions have already been answered satisfactorily. If they haven't, perhaps you've discovered a gap! Here are some strategies you can use to make the most of your time:
- One useful trick is to look at the “suggestions for future research” or conclusion section of existing studies on your topic. Many times, the authors will identify areas where they think a research gap exists, and what studies they think need to be done in the future.
- As you are researching, you will most likely come across citations for seminal works in your research field. These are the research studies that you see mentioned again and again in the literature. In addition to finding those and reading them, you can use a database like Web of Science to follow the research trail and discover all the other articles that have cited these. See the FAQ: I found the perfect article for my paper. How do I find other articles and books that have cited it? on how to do this. One way to quickly track down these seminal works is to use a database like SAGE Navigator, a social sciences literature review tool. It is one of the products available via our SAGE Knowledge database.
- In the PsycINFO and PsycARTICLES databases, you can select literature review, systematic review, and meta analysis under the Methodology section in the advanced search to quickly locate these. See the FAQ: Where can I find a qualitative or quantitative study? for more information on how to find the Methodology section in these two databases.
- In CINAHL , you can select Systematic review under the Publication Type field in the advanced search.
- In Web of Science , check the box beside Review under the Document Type heading in the “Refine Results” sidebar to the right of the list of search hits.
- If the database you are searching does not offer a way to filter your results by document type, publication type, or methodology in the advanced search, you can include these phrases (“literature reviews,” meta-analyses, or “systematic reviews”) in your search string. For example, “video games” AND “literature reviews” could be a possible search that you could try.
Please give these suggestions a try and contact a librarian for additional assistance.
Content authored by: GS
- Share on Facebook
Was this helpful? Yes 381 No 152
Frequently Asked Questions (FAQs) are a self-serve option for users to search and find answers to their questions.
Use the search box above to type your question to search for an answer or browse existing FAQs by group, topic, etc.
Tell Me More
Link to Question Form
More assistance.
Submit a Question
Related FAQs

- Research Process
What is a Research Gap
- 3 minute read
- 286.1K views
Table of Contents
If you are a young researcher, or even still finishing your studies, you’ll probably notice that your academic environment revolves around certain research topics, probably linked to your department or to the interest of your mentor and direct colleagues. For example, if your department is currently doing research in nanotechnology applied to medicine, it is only natural that you feel compelled to follow this line of research. Hopefully, it’s something you feel familiar with and interested in – although you might take your own twists and turns along your career.
Many scientists end up continuing their academic legacy during their professional careers, writing about their own practical experiences in the field and adapting classic methodologies to a present context. However, each and every researcher dreams about being a pioneer in a subject one day, by discovering a topic that hasn’t been approached before by any other scientist. This is a research gap.
Research gaps are particularly useful for the advance of science, in general. Finding a research gap and having the means to develop a complete and sustained study on it can be very rewarding for the scientist (or team of scientists), not to mention how its new findings can positively impact our whole society.
How to Find a Gap in Research
How many times have you felt that you have finally formulated THAT new and exciting question, only to find out later that it had been addressed before? Probably more times than you can count.
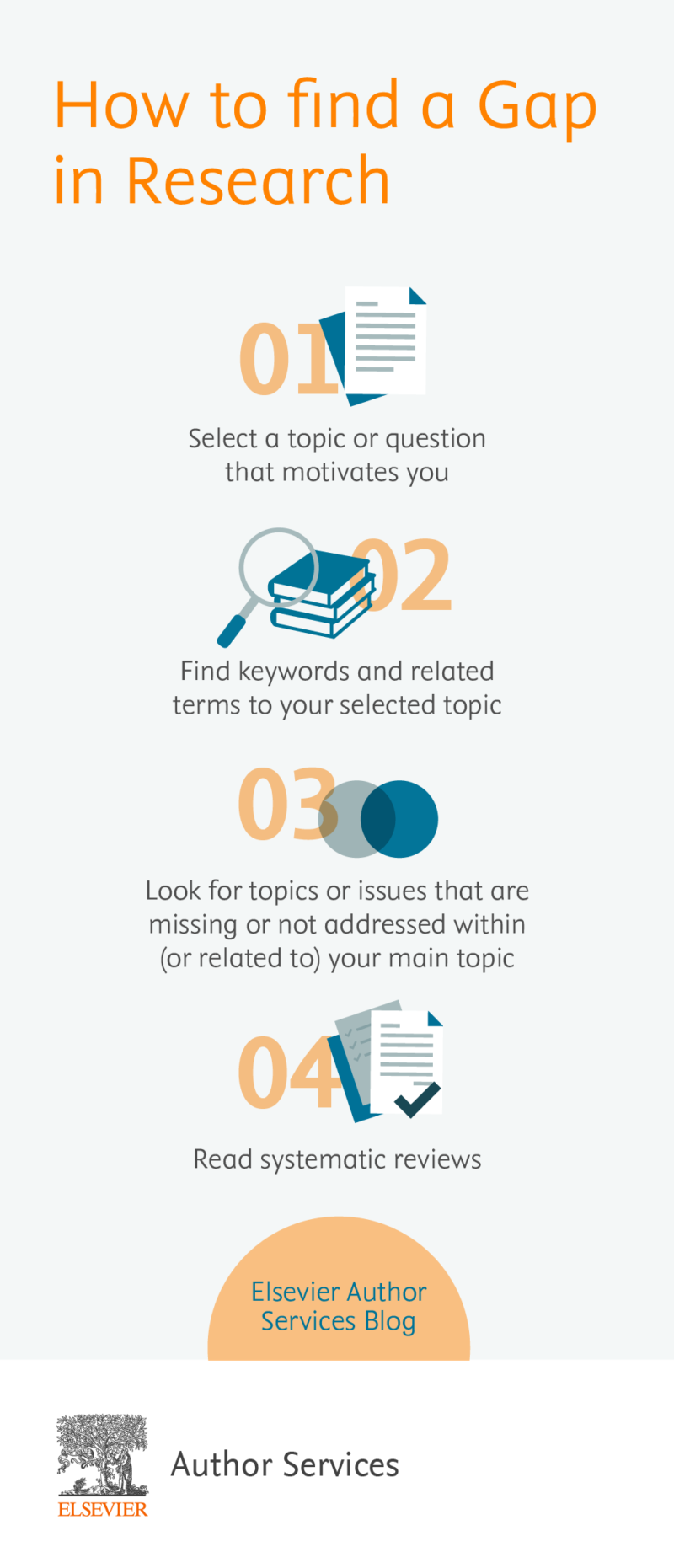
There are some steps you can take to help identify research gaps, since it is impossible to go through all the information and research available nowadays:
- Select a topic or question that motivates you: Research can take a long time and surely a large amount of physical, intellectual and emotional effort, therefore choose a topic that can keep you motivated throughout the process.
- Find keywords and related terms to your selected topic: Besides synthesizing the topic to its essential core, this will help you in the next step.
- Use the identified keywords to search literature: From your findings in the above step, identify relevant publications and cited literature in those publications.
- Look for topics or issues that are missing or not addressed within (or related to) your main topic.
- Read systematic reviews: These documents plunge deeply into scholarly literature and identify trends and paradigm shifts in fields of study. Sometimes they reveal areas or topics that need more attention from researchers and scientists.
Keeping track of all the new literature being published every day is an impossible mission. Remember that there is technology to make your daily tasks easier, and reviewing literature can be one of them. Some online databases offer up-to-date publication lists with quite effective search features:
- Elsevier’s Scope
- Google Scholar
Of course, these tools may be more or less effective depending on knowledge fields. There might be even better ones for your specific topic of research; you can learn about them from more experienced colleagues or mentors.
Find out how FINER research framework can help you formulate your research question.
Literature Gap
The expression “literature gap” is used with the same intention as “research gap.” When there is a gap in the research itself, there will also naturally be a gap in the literature. Nevertheless, it is important to stress out the importance of language or text formulations that can help identify a research/literature gap or, on the other hand, making clear that a research gap is being addressed.
When looking for research gaps across publications you may have noticed sentences like:
…has/have not been… (studied/reported/elucidated) …is required/needed… …the key question is/remains… …it is important to address…
These expressions often indicate gaps; issues or topics related to the main question that still hasn’t been subject to a scientific study. Therefore, it is important to take notice of them: who knows if one of these sentences is hiding your way to fame.
Language Editing Services by Elsevier Author Services:

- Manuscript Review
Systematic Review VS Meta-Analysis

Literature Review in Research Writing
You may also like.

Descriptive Research Design and Its Myriad Uses

Five Common Mistakes to Avoid When Writing a Biomedical Research Paper

Making Technical Writing in Environmental Engineering Accessible

To Err is Not Human: The Dangers of AI-assisted Academic Writing

When Data Speak, Listen: Importance of Data Collection and Analysis Methods

Choosing the Right Research Methodology: A Guide for Researchers

Why is data validation important in research?

Writing a good review article
Input your search keywords and press Enter.
Advertisement
Methods for Identifying Health Research Gaps, Needs, and Priorities: a Scoping Review
- Systematic Review
- Published: 08 November 2021
- Volume 37 , pages 198–205, ( 2022 )
Cite this article

- Eunice C. Wong PhD ORCID: orcid.org/0000-0001-8640-4548 1 ,
- Alicia R. Maher MD 1 ,
- Aneesa Motala BA 1 , 2 ,
- Rachel Ross MPH 1 ,
- Olamigoke Akinniranye MA 1 ,
- Jody Larkin MS 1 &
- Susanne Hempel PhD 1 , 2
3363 Accesses
9 Citations
5 Altmetric
Explore all metrics
Well-defined, systematic, and transparent processes to identify health research gaps, needs, and priorities are vital to ensuring that available funds target areas with the greatest potential for impact.
The purpose of this review is to characterize methods conducted or supported by research funding organizations to identify health research gaps, needs, or priorities.
We searched MEDLINE, PsycINFO, and the Web of Science up to September 2019. Eligible studies reported on methods to identify health research gaps, needs, and priorities that had been conducted or supported by research funding organizations. Using a published protocol, we extracted data on the method, criteria, involvement of stakeholders, evaluations, and whether the method had been replicated (i.e., used in other studies).
Among 10,832 citations, 167 studies were eligible for full data extraction. More than half of the studies employed methods to identify both needs and priorities, whereas about a quarter of studies focused singularly on identifying gaps (7%), needs (6%), or priorities (14%) only. The most frequently used methods were the convening of workshops or meetings (37%), quantitative methods (32%), and the James Lind Alliance approach, a multi-stakeholder research needs and priority setting process (28%). The most widely applied criteria were importance to stakeholders (72%), potential value (29%), and feasibility (18%). Stakeholder involvement was most prominent among clinicians (69%), researchers (66%), and patients and the public (59%). Stakeholders were identified through stakeholder organizations (51%) and purposive (26%) and convenience sampling (11%). Only 4% of studies evaluated the effectiveness of the methods and 37% employed methods that were reproducible and used in other studies.
To ensure optimal targeting of funds to meet the greatest areas of need and maximize outcomes, a much more robust evidence base is needed to ascertain the effectiveness of methods used to identify research gaps, needs, and priorities.
Similar content being viewed by others

A protocol for ongoing systematic scoping reviews of World Trade Center Health research

What do we know about evidence-informed priority setting processes to set population-level health-research agendas: an overview of reviews
Lack of systematicity in research prioritisation processes — a scoping review of evidence syntheses
Avoid common mistakes on your manuscript.
Well-defined, systematic, and transparent methods to identify health research gaps, needs, and priorities are vital to ensuring that available funds target areas with the greatest potential for impact. 1 , 2 As defined in the literature, 3 , 4 research gaps are defined as areas or topics in which the ability to draw a conclusion for a given question is prevented by insufficient evidence. Research gaps are not necessarily synonymous with research needs , which are those knowledge gaps that significantly inhibit the decision-making ability of key stakeholders, who are end users of research, such as patients, clinicians, and policy makers. The selection of research priorities is often necessary when all identified research gaps or needs cannot be pursued because of resource constraints. Methods to identify health research gaps, needs, and priorities (from herein referred to as gaps, needs, priorities) can be multi-varied and there does not appear to be general consensus on best practices. 3 , 5
Several published reviews highlight the diverse methods that have been used to identify gaps and priorities. In a review of methods used to identify gaps from systematic reviews, Robinson et al. noted the wide range of organizing principles that were employed in published literature between 2001 and 2009 (e.g., care pathway, decision tree, and patient, intervention, comparison, outcome framework,). 6 In a more recent review spanning 2007 to 2017, Nyanchoka et al. found that the vast majority of studies with a primary focus on the identification of gaps (83%) relied solely on knowledge synthesis methods (e.g., systematic review, scoping review, evidence mapping, literature review). A much smaller proportion (9%) relied exclusively on primary research methods (i.e., quantitative survey, qualitative study). 7
With respect to research priorities, in a review limited to a PubMed database search covering the period from 2001 to 2014, Yoshida documented a wide range of methods to identify priorities including the use of not only knowledge synthesis (i.e., literature reviews) and primary research methods (i.e., surveys) but also multi-stage, structured methods such as Delphi, Child Health and Nutrition Research Initiative (CHNRI), James Lind Alliance Priority Setting Partnership (JLA PSP), and Essential National Health Research (ENHR). 2 The CHNRI method, originally developed for the purpose of setting global child health research priorities, typically employs researchers and experts to specify a long list of research questions, the criteria that will be used to prioritize research questions, and the technical scoring of research questions using the defined criteria. 8 During the latter stages, non-expert stakeholders’ input are incorporated by using their ratings of the importance of selected criteria to weight the technical scores. The ENHR method, initially designed for health research priority setting at the national level, involves researchers, decision-makers, health service providers, and communities throughout the entire process of identifying and prioritizing research topics. 9 The JLA PSP method convenes patients, carers, and clinicians to equally and jointly identify questions about healthcare that cannot be answered by existing evidence that are important to all groups (i.e., research needs). 10 The identified research needs are then prioritized by the groups resulting in a final list (often a top 10) of research priorities. Non-clinical researchers are excluded from voting on research needs or priorities but can be involved in other processes (e.g., knowledge synthesis). CHNRI, ENHR, and JLA PSP usually employ a mix of knowledge synthesis and primary research methods to first identify a set of gaps or needs that are then prioritized. Thus, even though CHNRI, ENHR, and JLA PSP have been referred to as priority setting methods, they actually consist of a gaps or needs identification stage that feeds into a research prioritization stage.
Nyanchoka et al.’s review found that the majority of studies focused on the identification of gaps alone (65%), whereas the remaining studies focused either on research priorities alone (17%) or on both gaps and priorities (19%). 7 In an update to Robinson et al.’s review, 6 Carey et al. reviewed the literature between 2010 and 2011 and observed that the studies conducted during this latter period of time focused more on research priorities than gaps and had increased stakeholder involvement, and that none had evaluated the reproducibility of the methods. 11
The increasing development and diversity of formal processes and methods to identify gaps and priorities are indicative of a developing field. 2 , 12 To facilitate more standardized and systematic processes, other important areas warrant further investigation. Prior reviews did not distinguish between the identification of gaps versus research needs. The Agency for Healthcare Research and Quality Evidence-based Practice Center (AHRQ EPC) Program issued a series of method papers related to establishing research needs as part of comparative effectiveness research. 13 , 14 , 15 The AHRQ EPC Program defined research needs as “evidence gaps” identified within systematic reviews that are prioritized by stakeholders according to their potential impact on practice or care. 16 Furthermore, Nyanchoka et al. relied on author designations to classify studies as focusing on gaps versus research priorities and noted that definitions of gaps varied across studies, highlighting the need to apply consistent taxonomy when categorizing studies in reviews. 7 Given the rise in the use of stakeholders in both gaps and prioritization exercises, a greater understanding of the range of practices involving stakeholders is also needed. This includes the roles and responsibilities of stakeholders (e.g., consultants versus final decision-makers), the composition of stakeholders (e.g., non-research clinicians, patients, caregivers, policymakers), and the methods used to recruit stakeholders. The lack of consensus of best practices also highlights the importance of learning the extent to which evaluations to determine the effectiveness of gaps, needs, and prioritization exercises have been conducted, and if so, what were the resultant outcomes.
To better inform efforts and organizations that fund health research, we conducted a scoping review of methods used to identify gaps, needs, and priorities that were linked to potential or actual health research funding decision-making. Hence, this scoping review was limited to studies in which the identification of health research gaps, needs, or priorities was supported or conducted by funding organizations to address the following questions 1 : What are the characteristics of methods to identify health research gaps, needs, and priorities? and 2 To what extent have evaluations of the impact of these methods been conducted? Given that scoping reviews may be executed to characterize the ways an area of research has been conducted, 17 , 18 this approach is appropriate for the broad nature of this study’s aims.
Protocol and Registration
We employed methods that conform to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses extension for Scoping Reviews. 19 See Appendix A in the Supplementary Information. The scoping review protocol is registered with the Open Science Framework ( https://osf.io/5zjqx/ ).
Eligibility Criteria
Studies published in English that described methods to identify health research gaps, needs, or priorities that were supported or conducted by funding organizations were eligible for inclusion. We excluded studies that reported only the results of the exercise (e.g., list of priorities) absent of information on the methods used. We also excluded studies involving evidence synthesis (e.g., literature or systematic reviews) that were solely descriptive and did not employ an explicit method to identify research gaps, needs, or priorities.
Information Sources and Search Strategy
We searched the following electronic databases: MEDLINE, PsycINFO, and Web of Science. Our database search also included an update of the Nyanchoka et al. scoping review, which entailed executing their database searches for the time period following 2017 (the study’s search end date). 7 Nyanchoka et al. did not include database searches for research needs. The electronic database search and scoping review update were completed in August and September 2019, respectively . The search strategy employed for each of the databases is presented in Appendix B in the Supplementary Information.
Selection of Sources of Evidence and Data Charting Process
Two reviewers screened titles and abstracts and full-text publications. Citations that one or both reviewers considered potentially eligible were retrieved for full-text review. Relevant background articles and scoping and systematic reviews were reference mined to screen for eligible studies. Full-text publications were screened against detailed inclusion and exclusion criteria. Data was extracted by one reviewer and checked by a second reviewer. Discrepancies were resolved through discussion by the review team.
Information on study characteristics were extracted from each article including the aims of the exercise (i.e., gaps, needs, priorities, or a combination) and health condition (i.e., physical or psychological). Based on definitions in the literature, 3 , 4 , 5 the aims of the exercise were coded according to the activities that were conducted, which may not have always corresponded with the study authors’ labeling of the exercises. For instance, the JLA PSP method is often described as a priority exercise but we categorized it as a needs and priority exercise. Priority exercises can be preceded by exercises to identify gaps or needs, which then feed into the priority exercise such as in JLA PSP; however, standalone priority exercises can also be conducted (e.g., stakeholders prioritize an existing list of emerging diseases).
For each type of exercise, information on the methods were recorded. An initial list of methods was created based on previous reviews. 9 , 12 , 20 During the data extraction process, any methods not included in the initial list were subsequently added. If more than one exercise was reported within an article (e.g., gaps and priorities), information was extracted for each exercise separately. Reviewers extracted the following information: methods employed (e.g., qualitative, quantitative), criteria used (e.g., disease burden, importance to stakeholders), stakeholder involvement (e.g., stakeholder composition, method for identifying stakeholders), and whether an evaluation was conducted on the effectiveness of the exercise (see Appendix C in the Supplementary Information for full data extraction form).
Synthesis of results entailed quantitative descriptives of study characteristics (e.g., proportion of studies by aims of exercise) and characteristics of methods employed across all studies and by each type of study (e.g., gaps, needs, priorities).
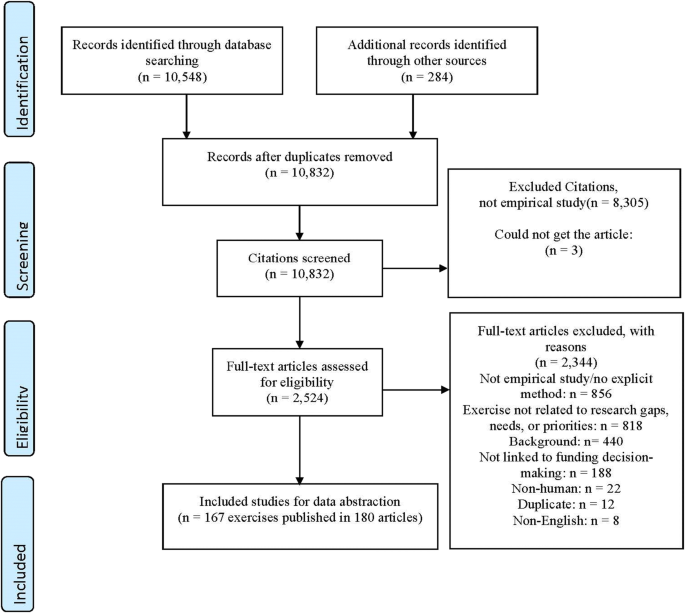
The electronic database search yielded a total of 10,548 titles. Another 284 articles were identified after searching the reference lists of full-text publications, including three systematic reviews 21 , 22 , 23 and one scoping review 24 that had met eligibility criteria. Moreover, a total of 99 publications designated as relevant background articles were also reference mined to screen for eligible studies. We conducted full-text screening for 2524 articles, which resulted in 2344 exclusions (440 studies were designated as background articles). A total of 167 exercises related to the identification of gaps, needs, or priorities that were supported or conducted by a research funding organization were described across 180 publications and underwent full data extraction. See Figure 1 for the flow diagram of our search strategy and reasons for exclusion.
Literature flow
Characteristics of Sources of Evidence
Among the published exercises, the majority of studies (152/167) conducted gaps, need, or prioritization exercises related to physical health, whereas only a small fraction of studies focused on psychological health (12/167) (see Appendix D in the Supplementary Information).
Methods for Identifying Gaps, Needs, and Priorities
As seen in Table 1 , only about a quarter of studies involved a singular type of exercise with 7% focused on the identification of gaps only (i.e., areas with insufficient information to draw a conclusion for a given question), 6% on needs only (i.e., knowledge gaps that inhibit the decision-making of key stakeholders), and 14% priorities only (i.e., ranked gaps or needs often because of resource constraints). Studies more commonly conducted a combination of multiple types of exercises with more than half focused on the identification of both research needs and priorities, 14% on gaps and priorities, 3% gaps, needs, and priorities, and 3% gaps and needs.
Across the 167 studies, the three most frequently used methods were the convening of workshops/meetings/conferences (37%), quantitative methods (32%), and the JLA PSP approach (28%). This was followed by methods involving literature reviews (17%), qualitative methods (17%), consensus methods (13%), and reviews of source materials (15%). Other methods included the CHNRI process (7%), reviews of in-progress data (7%), consultation with (non-researcher) stakeholders (4%), applying a framework tool (4%), ENHR (1%), systematic reviews (1%), and evidence mapping (1%).
The criterion most widely applied across the 167 studies was the importance to stakeholders (72%) (see Table 2 ). Almost one-third (29%) considered the potential value and 18% feasibility as criteria. Burden of disease (9%), addressing inequities (8%), costs (6%), alignment with organization’s mission (3%), and patient centeredness (2%) were adopted as criteria to a lesser extent.
About two-thirds of the studies included researchers (66%) and clinicians (69%) as stakeholders (see Appendix E in the Supplementary Information). Patients and the public were involved in 59% of the studies. A smaller proportion included policy makers (20%), funders (13%), product makers (8%), payers (5%), and purchasers (2%) as stakeholders. Nearly half of the studies (51%) relied on stakeholder organizations to identify stakeholders (see Appendix F in the Supplementary Information). A quarter of studies (26%) used purposive sampling and some convenience sampling (11%). Few (9%) used snowball sampling to identify stakeholders. Only a minor fraction of studies, seven of the 167 (4%), reported some type of effectiveness evaluation. 25 , 26 , 27 , 28 , 29 , 30 , 31
Our scoping review revealed that approaches to identifying gaps, needs, and priorities are less likely to occur as discrete processes and more often involve a combination of exercises. Approaches encompassing multiple exercises (e.g., gaps and needs) were far more prevalent than singular standalone exercises (e.g., gaps only) (73% vs. 27%). Findings underscore the varying importance placed on gaps, needs, and priorities, which reflect key principles of the Value of Information approach (i.e., not all gaps are important, addressing gaps do not necessarily address needs nor does addressing needs necessarily address priorities). 32
Findings differ from Nyanchoka et al.’s review in which studies involving the identification of gaps only outnumbered studies involving both gaps and priorities. 7 However, Nyanchoka et al. relied on author definitions to categorize exercises, whereas our study made designations based on our review of the activities described in the article and applied definitions drawn from the literature. 3 , 4 Lack of consensus on definitions of gaps and priority setting has been noted in the literature. 33 , 34 To the authors’ knowledge, no prior scoping review has focused on methods related to the identification of “research needs.” Findings underscore the need to develop and apply more consistent taxonomy to this growing field of research.
More than 40% of studies employed methods with a structured protocol including JLA PSP, ENHR, CHRNI, World Café, and the Dialogue model. 10 , 35 , 36 , 37 , 38 , 39 , 40 The World Café and Dialogue models particularly value the experiential perspectives of stakeholders. The World Café centers on creating a special environment, often modeled after a café, in which rounds of multi-stakeholder, small group, conversations are facilitated and prefaced with questions designed for the specific purpose of the session. Insights and results are reported and shared back to the entire group with no expectation to achieve consensus, but rather diverse perspectives are encouraged. 36 The Dialogue model is a multi-stakeholder, participatory, priority setting method involving the following phases: exploratory (informal discussions), consultation (separate stakeholder consultations), prioritization (stakeholder ratings), and integration (dialog between stakeholders). 39 Findings may indicate a trend away from non-replicable methods to approaches that afford greater transparency and reproducibility. 41 For instance, of the 17 studies published between 2000 and 2009, none had employed CHNRI and 6% used JLA PSP compared to the 141 studies between 2010 and 2019 in which 8% applied CHNRI and 32% JLA PSP. However, notable variations in implementing CHNRI and JLA PSP have been observed. 41 , 42 , 43 Though these protocols help to ensure a more standardized process, which is essential when testing the effectiveness of methods, such evaluations are infrequent but necessary to establish the usefulness of replicable methods.
Convening workshops, meetings, or conferences was the method used by the greatest proportion of studies (37%). The operationalization of even this singular method varied widely in duration (e.g., single vs. multi-day conferences), format (e.g., expert panel presentations, breakout discussion groups), processes (e.g., use of formal/informal consensus methods), and composition of stakeholders. The operationalization of other methods (e.g., quantitative, qualitative) also exhibited great diversity.
The use of explicit criteria to determine gaps, needs, or priorities is a key component of certain structured protocols 40 , 44 and frameworks. 9 , 45 In our scoping review, the criterion applied most frequently across studies (71%) was “importance to stakeholders” followed by potential value (31%) and feasibility (18%). Stakeholder values are being incorporated into the identification of gaps, needs, and exercises across a significant proportion of studies, but how this is operationalized varies widely across studies. For instance, the CHNRI typically employs multiple criteria that are scored by technical experts and these scores are then weighted based on stakeholder ratings of their relative importance. Other studies totaled scores across multiple criteria, whereas JLA PSP asks multiple stakeholders to rank the top ten priorities. The importance of involving stakeholders, especially patients and the public, in priority setting is increasingly viewed as vital to ensuring the needs of end users are met, 46 , 47 particularly in light of evidence demonstrating mismatches between the research interests of patients and researchers and clinicians. 48 , 49 , 50 In our review, clinicians (69%) and researchers (66%) were the most widely represented stakeholder groups across studies. Patients and the public (e.g., caregivers) were included as stakeholders in 59% of the studies. Only a small fraction of studies involved exercises in which stakeholders were limited to researchers only. Patients and the public were involved as stakeholders in 12% of studies published between 2000 and 2009 compared to 60% of studies between 2010 and 2019. Findings may reflect a trend away from researchers traditionally serving as one of the sole drivers of determining which research topics should be pursued.
More than half of the studies reported relying on stakeholder organizations to identify participants. Partnering with stakeholder organizations has been noted as one of the primary methods for identifying stakeholders for priority setting exercises. 34 Purposive sampling was the next most frequently used stakeholder identification method. In contrast, convenience sampling (e.g., recommendations by study team) and snowball sampling (e.g., identified stakeholders refer other stakeholders who then refer additional stakeholders) were not as frequently employed, but were documented as common methods in a prior review conducted almost a decade ago. 14 The greater use of stakeholder organizations than convenience or snowball sampling may be partly due to the more recent proliferation of published studies using structured protocols like JLA PSP, which rely heavily on partnerships with stakeholder organizations. Though methods such as snowball sampling may introduce more bias than random sampling, 14 there are no established best practices for stakeholder identification methods. 51 Nearly a quarter of studies provided either unclear or no information on stakeholder identification methods, which has been documented as a barrier to comparing across studies and assessing the validity of research priorities. 34
Determining the effectiveness of gaps, needs, and priority exercises is challenging given that outcome evaluations are rarely conducted. Only seven studies reported conducting an evaluation. 25 , 26 , 27 , 28 , 29 , 30 , 31 Evaluations varied with respect to their focus on process- (e.g., balanced stakeholder representation, stakeholder satisfaction) versus outcome-related impact (e.g., prioritized topics funded, knowledge production, benefits to health). There is no consensus on what constitutes optimal outcomes, which has been found to vary by discipline. 52
More than 90% of studies involved exercises related to physical health in contrast to a minor portfolio of work being dedicated to psychological health, which may be an indication of the low priority placed on psychological health policy research. Understanding whether funding decisions for physical versus psychological health research are similarly or differentially governed by more systematic, formal processes may be important to the extent that this affects the effective targeting of funds.
Limitations
By limiting studies to those supported or conducted by funding organizations, we may have excluded global, national, or local priority setting exercises. In addition, our scoping review categorized approaches according to the actual exercises conducted and definitions provided in the scientific literature rather than relying on the terminology employed by studies. This resulted in instances in which the category assigned to an exercise within our scoping review could diverge from the category employed by the study authors. Lastly, this study’s findings are subject to limitations often characteristic of scoping reviews such as publication bias, language bias, lack of quality assessment, and search, inclusion, and extraction biases. 53
Conclusions
The diversity and growing establishment of formal processes and methods to identify health research gaps, needs, and priorities are characteristic of a developing field. Even with the emergence of more structured and systematic approaches, the inconsistent categorization and definition of gaps, needs, and priorities inhibit efforts to evaluate the effectiveness of varied methods and processes, such efforts are rare and sorely needed to build an evidence base to guide best practices. The immense variation occurring within structured protocols, across different combinations of disparate methods, and even within singular methods, further emphasizes the importance of using clearly defined approaches, which are essential to conducting investigations of the effectiveness of these varied approaches. The recent development of reporting guidelines for priority setting for health research may facilitate more consistent and clear documentation of processes and methods, which includes the many facets of involving stakeholders. 34 To ensure optimal targeting of funds to meet the greatest areas of need and maximize outcomes, a much more robust evidence base is needed to ascertain the effectiveness of methods used to identify research gaps, needs, and priorities.
Chalkidou K, Whicher D, Kary W, Tunis SR . Comparative Effectiveness Research Priorities: Identifying Critical Gaps in Evidence for Clinical and Health Policy Decision Making. International journal of technology assessment in health care . 2009;25(3):241-8. doi: https://doi.org/10.1017/S0266462309990225
Article PubMed Google Scholar
Yoshida S . Approaches, Tools and Methods Used for Setting Priorities in Health Research in the 21(st) Century. Journal of global health . 2016;6(1):010507-010507. doi: https://doi.org/10.7189/jogh.06.010507
Robinson KA, Saldanha IJ, McKoy NA . Development of a Framework to Identify Research Gaps from Systematic Reviews. Journal of clinical epidemiology . 2011;64(12):1325-30. [Comment in: J Clin Epidemiol. 2013 May;66(5):522-3; [ https://www.ncbi.nlm.nih.gov/pubmed/23265604 ]]. doi: https://doi.org/10.1016/j.jclinepi.2011.06.009
Saldanha IJ, Wilson LM, Bennett WL, Nicholson WK, Robinson KA . Development and Pilot Test of a Process to Identify Research Needs from a Systematic Review. J Clin Epidemiol . May 2013;66(5):538-45. doi: https://doi.org/10.1016/j.jclinepi.2012.07.009
Viergever RF, Terry R, Matsoso M . Health research prioritization at WHO: an overview of methodology and high level analysis of WHO led health research priority setting exercises. Geneva: World Health Organization . 2010;
Google Scholar
Robinson KA, Akinyede O, Dutta T, et al. Framework for Determining Research Gaps During Systematic Review: Evaluation . 2013. AHRQ Methods for Effective Health Care .
Nyanchoka L, Tudur-Smith C, Thu VN, Iversen V, Tricco AC, Porcher R . A Scoping Review describes Methods Used to Identify, Prioritize and Display Gaps in Health Research. J Clin Epidemiol . Jan 30 2019;doi: https://doi.org/10.1016/j.jclinepi.2019.01.005
Rudan I, Gibson JL, Ameratunga S, et al. Setting priorities in global child health research investments: guidelines for implementation of CHNRI method. Croatian medical journal . 2008;49(6):720-33.
Article PubMed PubMed Central Google Scholar
Viergever RF, Olifson S, Ghaffar A, Terry RF . A Checklist for Health Research Priority Setting: Nine Common Themes of Good Practice. Health Res Policy Syst . Dec 15 2010;8:36. doi: https://doi.org/10.1186/1478-4505-8-36
James Lind Alliance. The James Lind Alliance Guidebook . March 2020. http://www.jla.nihr.ac.uk/jla-guidebook/downloads/JLA-Guidebook-V9-download-March-2020.pdf
Carey TY, A.; Beadles, C.; Wines, R . Prioritizing Future Research through Examination of Research Gaps in Systematic Reviews . 2012.
Carey T, Yon A, Beadles C, Wines R . Prioritizing future research through examination of research gaps in systematic reviews. Prepared for the Patient-Centered Outcomes Research Institute . 2012;
Carey TS, Sanders GD, Viswanathan M, Trikalinos TA, Kato E, Chang S . Framework for Considering Study Designs for Future Research Needs. Methods Future Research Needs Paper No. 8 (Prepared by the RTI–UNC Evidence-based Practice Center under Contract No. 290-2007- 10056-I.) AHRQ Publication No. 12-EHC048-EF. Rockville, MD: Agency for Healthcare Research and Quality . March 2012. Framework for Considering Study Designs for Future Research Needs . https://www.ncbi.nlm.nih.gov/pubmed/22624168
O’Haire C, McPheeters M, Nakamoto E, et al. Methods for Engaging Stakeholders To Identify and Prioritize Future Research Needs. Methods Future Research Needs Report No. 4. (Prepared by the Oregon Evidence-based Practice Center and the Vanderbilt Evidence-based Practice Center under Contract No. 290-2007-10057-I.) AHRQ Publication No. 11-EHC044-EF. Rockville, MD: Agency for Healthcare Research and Quality . Vol. Methods Future Research Needs Reports. 2011. June 2011. https://www.ncbi.nlm.nih.gov/books/NBK62571/
Trikalinos T, Dahabreh I, Lee J, Moorthy D . Methods Research on Future Research Needs: Defining an Optimal Format for Presenting Research Needs. Methods Future Research Needs Report No. 3. (Prepared by the Tufts Evidence-based Practice Center under Contract No. 290-2007-10057-I.) AHRQ Publication No. 11-EHC027-EF. Rockville, MD: Agency for Healthcare Research and Quality . June 2011. www.effectivehealthcare.ahrq.gov/reports/final.cfm .
Kane RL, Guise JM, Hartman K, Rothenberg B, Trikalinos T, Wilt T . Presentation of Future Research Needs . 2012. AHRQ Methods for Effective Health Care .
Munn Z, Peters MDJ, Stern C, Tufanaru C, McArthur A, Aromataris E . Systematic Review or Scoping Review? Guidance for Authors When Choosing Between a Systematic or Scoping Review Approach. journal article. BMC Medical Research Methodology . November 19 2018;18(1):143. doi: https://doi.org/10.1186/s12874-018-0611-x
Peters MD, Godfrey CM, Khalil H, McInerney P, Parker D, Soares CB . Guidance for Conducting Systematic Scoping Reviews. Int J Evid Based Healthc . Sep 2015;13(3):141-6. doi: https://doi.org/10.1097/xeb.0000000000000050
Tricco AC, Lillie E, Zarin W, et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. The PRISMA-ScR Statement. Annals of Internal Medicine . 2018;169(7):467-473. doi: https://doi.org/10.7326/m18-0850
Tomlinson M, Chopra M, Hoosain N, Rudan I . A review of selected research priority setting processes at national level in low and middle income countries: towards fair and legitimate priority setting. Health Research Policy and Systems . 2011;9(1):19.
Rylance J, Pai M, Lienhardt C, Garner P . Priorities for tuberculosis research: a systematic review. Lancet Infect Dis . 2010;10(12):886-892.
Tong A, Chando S, Crowe S, et al. Research priority setting in kidney disease: a systematic review. American journal of kidney diseases: the official journal of the National Kidney Foundation . 2015;65(5):674-83. [Comment in: Am J Kidney Dis. 2015 May;65(5):641-3; [ https://www.ncbi.nlm.nih.gov/pubmed/25919496 ]]. doi: https://doi.org/10.1053/j.ajkd.2014.11.011
Article Google Scholar
Tong A, Sautenet B, Chapman JR, et al. Research priority setting in organ transplantation: a systematic review. Transplant international: official journal of the European Society for Organ Transplantation . 2017;30(4):327-343. doi: https://doi.org/10.1111/tri.12924
Bourne AM, Johnston RV, Cyril S, et al. Scoping Review of Priority Setting of Research Topics for Musculoskeletal Conditions Review. BMJ Open . 2018;8(12):9 e023962. doi: https://doi.org/10.1136/bmjopen-2018-023962
Bennett WL, Nicholson WK, Saldanha IJ, Wilson LM, McKoy NA, Robinson KA . Future Research Needs for the Management of Gestational Diabetes. 2010. AHRQ Future Research Needs Papers .
Buckley BS, Grant AM, Glazener CMA . Case study: a patient-clinician collaboration that identified and prioritized evidence gaps and stimulated research development. Journal of clinical epidemiology . 2013;66(5):483-9. doi: https://doi.org/10.1016/j.jclinepi.2011.03.016
Elberse JE, Pittens CACM, de Cock Buning T, Broerse JEW . Patient Involvement in a Scientific Advisory Process: Setting the Research Agenda for Medical Products. Health policy (Amsterdam, Netherlands) . 2012;107(2-3):231-42. doi: https://doi.org/10.1016/j.healthpol.2012.05.014
Fun WH, Sararaks S, Tan EH, et al. Research funding impact and priority setting - advancing universal access and quality healthcare research in Malaysia. BMC Health Services Research . Apr 24 2019;19(1):248.
Husereau D, Boucher M, Noorani H . Priority Setting for Health Technology Assessment at CADTH. Article. International Journal of Technology Assessment in Health Care . 2010;26(3):341-347. doi: https://doi.org/10.1017/s0266462310000383
Mador RL, Kornas K, Simard A, Haroun V . Using the Nine Common Themes of Good Practice Checklist as a Tool for Evaluating the Research Priority Setting Process of a Provincial Research and Program Evaluation Program. Health research policy and systems . 2016;14:22. doi: https://doi.org/10.1186/s12961-016-0092-5
Sanders GD, Powers B, Crowley M, et al. Future Research Needs for Angiotensin Converting Enzyme Inhibitors or Angiotensin II Receptor Blockers Added to Standard Medical Therapy for Treating Stable Ischemic Heart Disease: Identification of Future Research Needs from Comparative Effectiveness Review No. 18. Future Research Needs for Angiotensin Converting Enzyme Inhibitors or Angiotensin II Receptor Blockers Added to Standard Medical Therapy for Treating Stable Ischemic Heart Disease: Identification of Future Research Needs from Comparative Effectiveness Review No 18 . 2010. AHRQ Future Research Needs Papers .
Minelli C, Baio G . Value of Information: a Tool to Improve Research Prioritization and Reduce Waste. PLos Med . 2015;12(9):e1001882-e1001882. doi: https://doi.org/10.1371/journal.pmed.1001882
Bryant J, Sanson-Fisher R, Walsh J, Stewart J . Health Research Priority Setting in Selected High Income Countries: a Narrative Review of Methods Used and Recommendations for Future Practice. Cost Eff Resour Alloc . 2014;12:23. doi: https://doi.org/10.1186/1478-7547-12-23
Tong A, Synnot A, Crowe S, et al. Reporting Guideline for Priority Setting of Health Research (REPRISE). BMC Med Res Methodol . Dec 28 2019;19(1):243. doi: https://doi.org/10.1186/s12874-019-0889-3
Article CAS PubMed PubMed Central Google Scholar
Uneke CJ, Ezeoha AE, Ndukwe CD, Oyibo PG, Onwe F, Aulakh BK . Research Priority Setting for Health Policy and Health Systems Strengthening in Nigeria: the Policymakers and Stakeholders Perspective and Involvement. The Pan African medical journal . 2013;16:10. doi: https://doi.org/10.11604/pamj.2013.16.10.2318
MacFarlane A, Galvin R, O’Sullivan M, et al. Participatory Methods for Research Prioritization in Primary Care: an Analysis of the World Cafe Approach in Ireland and the USA. Family practice . 2017;34(3):278-284. doi: https://doi.org/10.1093/fampra/cmw104
Nelson ML, McKellar KA, Munce S, et al. Addressing the Evidence Gap in Stroke Rehabilitation for Complex Patients: a Preliminary Research Agenda. Archives of physical medicine and rehabilitation . 2018;99(6):1232-1241. doi: https://doi.org/10.1016/j.apmr.2017.08.488
Restall GJ, Carnochan TN, Roger KS, Sullivan TM, Etcheverry EJ, Roddy P . Collaborative Priority Setting for Human Immunodeficiency Virus Rehabilitation Research: a Case Report. Canadian journal of occupational therapy Revue canadienne d’ergotherapie . 2016;83(1):7-13. doi: https://doi.org/10.1177/0008417415577423
Abma TA, Broerse JEW . Patient Participation as Dialogue: Setting Research Agendas. Health expectations: an international journal of public participation in health care and health policy . 2010;13(2):160-73. doi: https://doi.org/10.1111/j.1369-7625.2009.00549.x
Rudan I . Setting Health Research Priorities Using the CHNRI Method: IV. Key conceptual advances. J Glob Health . 2016;6(1):010501. doi: https://doi.org/10.7189/jogh-06-010501
Yoshida S, Wazny K, Cousens S, Chan KY . Setting Health Research Priorities Using the CHNRI Method: III Involving Stakeholders. J Glob Health. Jun 2016;6(1):010303. doi: https://doi.org/10.7189/jogh.06.010303
Rudan I, Yoshida S, Chan KY, et al. Setting Health Research Priorities Using the CHNRI Method: VII. A Review of the First 50 Applications of the CHNRI Method. J Glob Health . 2017;7(1):011004. doi: https://doi.org/10.7189/jogh.07.011004
Nygaard A, Halvorsrud L, Linnerud S, Grov EK, Bergland A . The James Lind Alliance Process Approach: Scoping Review. BMJ Open . 2019;9(8):e027473. doi: https://doi.org/10.1136/bmjopen-2018-027473
Okello D, Chongtrakul P , The COHRED Working Group on Priority Setting. A Manual for Research Priority Setting using the ENHR Strategy. Reference mining. Accessed July 24, 2019. http://www.cohred.org/downloads/578.pdf
Fadlallah R, El-Harakeh A, Bou-Karroum L, et al. A Common Framework of Steps and Criteria for Prioritizing Topics for Evidence Syntheses: a Systematic Review. J Clin Epidemiol . 2020;120:67-85. doi: https://doi.org/10.1016/j.jclinepi.2019.12.009
Natale CV, Gross D . The ROI of engaged patients. Healthc Financ Manage . 2013;67(8):90-7.
PubMed Google Scholar
Clavisi O, Bragge P, Tavender E, Turner T, Gruen RL . Effective Stakeholder Participation in Setting Research Priorities Using a Global Evidence Mapping Approach. Journal of clinical epidemiology . 2013;66(5):496-502.e2. doi: https://doi.org/10.1016/j.jclinepi.2012.04.002
Tallon D, Chard J, Dieppe P . Relation Between Agendas of the Research Community and the Research Consumer. Lancet . 2000;355(9220):2037-40. doi: https://doi.org/10.1016/S0140-6736(00)02351-5
Article CAS PubMed Google Scholar
Crowe S, Fenton M, Hall M, Cowan K, Chalmers I . Patients’, Clinicians’ and the Research Communities’ Priorities for Treatment Research: There is an Important Mismatch. Res Involv Engagem . 2015;1:2. doi: https://doi.org/10.1186/s40900-015-0003-x
Kapiriri L, Tomlinson M, Gibson J, et al. Setting priorities in global child health research investments: addressing values of stakeholders. Croatian medical journal . 2007;48(5):618-627.
PubMed PubMed Central Google Scholar
Guise J-M, O’Haire C, McPheeters M, et al. A Practice-Based Tool for Engaging Stakeholders in Future Research: a Synthesis of Current Practices. Journal of clinical epidemiology . 2013;66(6):666-74. doi: https://doi.org/10.1016/j.jclinepi.2012.12.010
Sibbald SL, Singer PA, Upshur R, Martin DK . Priority Setting: What Constitutes Success? A Conceptual Framework for Successful Priority Setting. Article. Bmc Health Services Research . 2009;9:12. 43. doi: https://doi.org/10.1186/1472-6963-9-43
Pham MT, Rajić A, Greig JD, Sargeant JM, Papadopoulos A, McEwen SA . A Scoping Review of Scoping Reviews: Advancing the Approach and Enhancing the Consistency. Research synthesis methods . 2014;5(4):371-385. doi: https://doi.org/10.1002/jrsm.1123
Download references
Acknowledgements
This scoping review is part of research that was sponsored by Defense Centers of Excellence for Psychological Health and Traumatic Brain Injury (now Psychological Health Center of Excellence).
Author information
Authors and affiliations.
RAND Corporation, Santa Monica, CA, USA
Eunice C. Wong PhD, Alicia R. Maher MD, Aneesa Motala BA, Rachel Ross MPH, Olamigoke Akinniranye MA, Jody Larkin MS & Susanne Hempel PhD
Department of Population and Public Health Sciences, University of Southern California Gehr Family Center for Health Systems Science & Innovation, Los Angeles, USA
Aneesa Motala BA & Susanne Hempel PhD
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Eunice C. Wong PhD .
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
(PDF 1205 kb)
Rights and permissions
Reprints and permissions
About this article
Wong, E.C., Maher, A.R., Motala, A. et al. Methods for Identifying Health Research Gaps, Needs, and Priorities: a Scoping Review. J GEN INTERN MED 37 , 198–205 (2022). https://doi.org/10.1007/s11606-021-07064-1
Download citation
Received : 01 March 2021
Accepted : 21 July 2021
Published : 08 November 2021
Issue Date : January 2022
DOI : https://doi.org/10.1007/s11606-021-07064-1
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- research gaps
- research needs
- research priorities
- priority setting
- Find a journal
- Publish with us
- Track your research
From research discovery to gap finding
ResGap is an application that helps you identify research gaps quickly and easily, specifically it:
- Provides a quick and comprehensive overview of your research topic.
- Finds the most cited publications, authors, journals and refereed outlets in your research area.
- Visualises how topics in your area have evolved over time, showing topics that have increased or decreased in appearance.
- Identifies research gaps by comparing different sets of literature (i.e. academic vs practitioner publications).
ResGap showcases research where the application was used:
ResGap showcases research conducted in a variety of research areas with diverse collaborators across the globe. This research applies the ResGap tool and associated methodologies, e.g. entity-linking, machine learning, text mining, natural language processing, etc.
Browse examples below:
- environmental accounting
- interdisciplinary research maps
- digital disruption and digital transformation
- trending topics in the top Information System journals from 1996 to 2017
Follow the ResGap blog for current updates.

Researchers
Whether you are a senior researcher or are just embarking on an academic career, ResGap can speed up your data analysis for literature reviews.
ResGap can help you to identify, for example:
- which are the most important topics within an area of study
- how research trends evolve over time
- which topics are being explored extensively, and which are possibly being overlooked
- which are the “hot” topics for top journals
Institutions
ResGap helps organisations determine where new research should be focused. The tool helps identify gaps and helps build a case for the development or expansion of research centres or departments.
Curricula are continuously evolving and must reflect the most up to date research. ResGap can highlight trends in the relevant literature, helping to identify learning objectives which may be overlooked or inadequately covered in course materials. As a ResGap user, you will have access to a bank of data covering 6,000+ published articles (from 1999 to 2017), enabling you to track the progression & popularity of published topics, which should inform curriculum development.
Empower your academic work and research with an automated, intelligent and efficient assistant which can help you identify relevant research gaps.
With ResGap you can simply, efficiently and reliably identify research trends, finding which topics in your area of interest are salient, emergent or waning. Efficiently comparing literature at scale while drawing reliable conclusions which assist you in your academic research, ResGap can help you uncover unmet research needs and more.
Our portal shows research trends of topics appearing in Information Systems journals (basket of 8). ResGap consolidates and groups data on over 6,000 actual publications (from 1996 until 2017). This data is then be used to generate a range of accessible graphics and models, allowing you to track the most important topics within your area of study over time.
Once signed into ResGap, you will also have access to a literature-comparison tool which was developed to identify gaps in different sets of literature and offers a wide variety of applications and features.
Dr. Mauricio Marrone – Founder
An Associate Professor at Macquarie University (Sydney, Australia) with interests in Information Systems, Research Methods, Innovation Diffusion and Text Analytics, Mauricio originally developed ResGap as a means to identify gaps in the research in his field. It soon became apparent that the portal had broader applications.
Tim Chard – Developer
Assoc. prof. mark dras – advisor, yvonne black – outreach manager.
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Published: 08 May 2024
A meta-analysis on global change drivers and the risk of infectious disease
- Michael B. Mahon ORCID: orcid.org/0000-0002-9436-2998 1 , 2 na1 ,
- Alexandra Sack 1 , 3 na1 ,
- O. Alejandro Aleuy 1 ,
- Carly Barbera 1 ,
- Ethan Brown ORCID: orcid.org/0000-0003-0827-4906 1 ,
- Heather Buelow ORCID: orcid.org/0000-0003-3535-4151 1 ,
- David J. Civitello 4 ,
- Jeremy M. Cohen ORCID: orcid.org/0000-0001-9611-9150 5 ,
- Luz A. de Wit ORCID: orcid.org/0000-0002-3045-4017 1 ,
- Meghan Forstchen 1 , 3 ,
- Fletcher W. Halliday 6 ,
- Patrick Heffernan 1 ,
- Sarah A. Knutie 7 ,
- Alexis Korotasz 1 ,
- Joanna G. Larson ORCID: orcid.org/0000-0002-1401-7837 1 ,
- Samantha L. Rumschlag ORCID: orcid.org/0000-0003-3125-8402 1 , 2 ,
- Emily Selland ORCID: orcid.org/0000-0002-4527-297X 1 , 3 ,
- Alexander Shepack 1 ,
- Nitin Vincent ORCID: orcid.org/0000-0002-8593-1116 1 &
- Jason R. Rohr ORCID: orcid.org/0000-0001-8285-4912 1 , 2 , 3 na1
Nature ( 2024 ) Cite this article
6264 Accesses
600 Altmetric
Metrics details
- Infectious diseases
Anthropogenic change is contributing to the rise in emerging infectious diseases, which are significantly correlated with socioeconomic, environmental and ecological factors 1 . Studies have shown that infectious disease risk is modified by changes to biodiversity 2 , 3 , 4 , 5 , 6 , climate change 7 , 8 , 9 , 10 , 11 , chemical pollution 12 , 13 , 14 , landscape transformations 15 , 16 , 17 , 18 , 19 , 20 and species introductions 21 . However, it remains unclear which global change drivers most increase disease and under what contexts. Here we amassed a dataset from the literature that contains 2,938 observations of infectious disease responses to global change drivers across 1,497 host–parasite combinations, including plant, animal and human hosts. We found that biodiversity loss, chemical pollution, climate change and introduced species are associated with increases in disease-related end points or harm, whereas urbanization is associated with decreases in disease end points. Natural biodiversity gradients, deforestation and forest fragmentation are comparatively unimportant or idiosyncratic as drivers of disease. Overall, these results are consistent across human and non-human diseases. Nevertheless, context-dependent effects of the global change drivers on disease were found to be common. The findings uncovered by this meta-analysis should help target disease management and surveillance efforts towards global change drivers that increase disease. Specifically, reducing greenhouse gas emissions, managing ecosystem health, and preventing biological invasions and biodiversity loss could help to reduce the burden of plant, animal and human diseases, especially when coupled with improvements to social and economic determinants of health.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
24,99 € / 30 days
cancel any time
Subscribe to this journal
Receive 51 print issues and online access
185,98 € per year
only 3,65 € per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
Towards common ground in the biodiversity–disease debate

Biological invasions facilitate zoonotic disease emergences

Measuring the shape of the biodiversity-disease relationship across systems reveals new findings and key gaps
Data availability.
All the data for this Article have been deposited at Zenodo ( https://doi.org/10.5281/zenodo.8169979 ) 52 and GitHub ( https://github.com/mahonmb/GCDofDisease ) 53 .
Code availability
All the code for this Article has been deposited at Zenodo ( https://doi.org/10.5281/zenodo.8169979 ) 52 and GitHub ( https://github.com/mahonmb/GCDofDisease ) 53 . R markdown is provided in Supplementary Data 1 .
Jones, K. E. et al. Global trends in emerging infectious diseases. Nature 451 , 990–994 (2008).
Article ADS CAS PubMed PubMed Central Google Scholar
Civitello, D. J. et al. Biodiversity inhibits parasites: broad evidence for the dilution effect. Proc. Natl Acad. Sci USA 112 , 8667–8671 (2015).
Halliday, F. W., Rohr, J. R. & Laine, A.-L. Biodiversity loss underlies the dilution effect of biodiversity. Ecol. Lett. 23 , 1611–1622 (2020).
Article PubMed PubMed Central Google Scholar
Rohr, J. R. et al. Towards common ground in the biodiversity–disease debate. Nat. Ecol. Evol. 4 , 24–33 (2020).
Article PubMed Google Scholar
Johnson, P. T. J., Ostfeld, R. S. & Keesing, F. Frontiers in research on biodiversity and disease. Ecol. Lett. 18 , 1119–1133 (2015).
Keesing, F. et al. Impacts of biodiversity on the emergence and transmission of infectious diseases. Nature 468 , 647–652 (2010).
Cohen, J. M., Sauer, E. L., Santiago, O., Spencer, S. & Rohr, J. R. Divergent impacts of warming weather on wildlife disease risk across climates. Science 370 , eabb1702 (2020).
Article CAS PubMed PubMed Central Google Scholar
Rohr, J. R. et al. Frontiers in climate change-disease research. Trends Ecol. Evol. 26 , 270–277 (2011).
Altizer, S., Ostfeld, R. S., Johnson, P. T. J., Kutz, S. & Harvell, C. D. Climate change and infectious diseases: from evidence to a predictive framework. Science 341 , 514–519 (2013).
Article ADS CAS PubMed Google Scholar
Rohr, J. R. & Cohen, J. M. Understanding how temperature shifts could impact infectious disease. PLoS Biol. 18 , e3000938 (2020).
Carlson, C. J. et al. Climate change increases cross-species viral transmission risk. Nature 607 , 555–562 (2022).
Halstead, N. T. et al. Agrochemicals increase risk of human schistosomiasis by supporting higher densities of intermediate hosts. Nat. Commun. 9 , 837 (2018).
Article ADS PubMed PubMed Central Google Scholar
Martin, L. B., Hopkins, W. A., Mydlarz, L. D. & Rohr, J. R. The effects of anthropogenic global changes on immune functions and disease resistance. Ann. N. Y. Acad. Sci. 1195 , 129–148 (2010).
Rumschlag, S. L. et al. Effects of pesticides on exposure and susceptibility to parasites can be generalised to pesticide class and type in aquatic communities. Ecol. Lett. 22 , 962–972 (2019).
Allan, B. F., Keesing, F. & Ostfeld, R. S. Effect of forest fragmentation on Lyme disease risk. Conserv. Biol. 17 , 267–272 (2003).
Article Google Scholar
Brearley, G. et al. Wildlife disease prevalence in human‐modified landscapes. Biol. Rev. 88 , 427–442 (2013).
Rohr, J. R. et al. Emerging human infectious diseases and the links to global food production. Nat. Sustain. 2 , 445–456 (2019).
Bradley, C. A. & Altizer, S. Urbanization and the ecology of wildlife diseases. Trends Ecol. Evol. 22 , 95–102 (2007).
Allen, T. et al. Global hotspots and correlates of emerging zoonotic diseases. Nat. Commun. 8 , 1124 (2017).
Sokolow, S. H. et al. Ecological and socioeconomic factors associated with the human burden of environmentally mediated pathogens: a global analysis. Lancet Planet. Health 6 , e870–e879 (2022).
Young, H. S., Parker, I. M., Gilbert, G. S., Guerra, A. S. & Nunn, C. L. Introduced species, disease ecology, and biodiversity–disease relationships. Trends Ecol. Evol. 32 , 41–54 (2017).
Barouki, R. et al. The COVID-19 pandemic and global environmental change: emerging research needs. Environ. Int. 146 , 106272 (2021).
Article CAS PubMed Google Scholar
Nova, N., Athni, T. S., Childs, M. L., Mandle, L. & Mordecai, E. A. Global change and emerging infectious diseases. Ann. Rev. Resour. Econ. 14 , 333–354 (2021).
Zhang, L. et al. Biological invasions facilitate zoonotic disease emergences. Nat. Commun. 13 , 1762 (2022).
Olival, K. J. et al. Host and viral traits predict zoonotic spillover from mammals. Nature 546 , 646–650 (2017).
Guth, S. et al. Bats host the most virulent—but not the most dangerous—zoonotic viruses. Proc. Natl Acad. Sci. USA 119 , e2113628119 (2022).
Nelson, G. C. et al. in Ecosystems and Human Well-Being (Millennium Ecosystem Assessment) Vol. 2 (eds Rola, A. et al) Ch. 7, 172–222 (Island Press, 2005).
Read, A. F., Graham, A. L. & Raberg, L. Animal defenses against infectious agents: is damage control more important than pathogen control? PLoS Biol. 6 , 2638–2641 (2008).
Article CAS Google Scholar
Medzhitov, R., Schneider, D. S. & Soares, M. P. Disease tolerance as a defense strategy. Science 335 , 936–941 (2012).
Torchin, M. E. & Mitchell, C. E. Parasites, pathogens, and invasions by plants and animals. Front. Ecol. Environ. 2 , 183–190 (2004).
Bellay, S., de Oliveira, E. F., Almeida-Neto, M. & Takemoto, R. M. Ectoparasites are more vulnerable to host extinction than co-occurring endoparasites: evidence from metazoan parasites of freshwater and marine fishes. Hydrobiologia 847 , 2873–2882 (2020).
Scheffer, M. Critical Transitions in Nature and Society Vol. 16 (Princeton Univ. Press, 2020).
Rohr, J. R. et al. A planetary health innovation for disease, food and water challenges in Africa. Nature 619 , 782–787 (2023).
Reaser, J. K., Witt, A., Tabor, G. M., Hudson, P. J. & Plowright, R. K. Ecological countermeasures for preventing zoonotic disease outbreaks: when ecological restoration is a human health imperative. Restor. Ecol. 29 , e13357 (2021).
Hopkins, S. R. et al. Evidence gaps and diversity among potential win–win solutions for conservation and human infectious disease control. Lancet Planet. Health 6 , e694–e705 (2022).
Mitchell, C. E. & Power, A. G. Release of invasive plants from fungal and viral pathogens. Nature 421 , 625–627 (2003).
Chamberlain, S. A. & Szöcs, E. taxize: taxonomic search and retrieval in R. F1000Research 2 , 191 (2013).
Newman, M. Fundamentals of Ecotoxicology (CRC Press/Taylor & Francis Group, 2010).
Rohatgi, A. WebPlotDigitizer v.4.5 (2021); automeris.io/WebPlotDigitizer .
Lüdecke, D. esc: effect size computation for meta analysis (version 0.5.1). Zenodo https://doi.org/10.5281/zenodo.1249218 (2019).
Lipsey, M. W. & Wilson, D. B. Practical Meta-Analysis (SAGE, 2001).
R Core Team. R: A Language and Environment for Statistical Computing Vol. 2022 (R Foundation for Statistical Computing, 2020); www.R-project.org/ .
Viechtbauer, W. Conducting meta-analyses in R with the metafor package. J. Stat. Softw. 36 , 1–48 (2010).
Pustejovsky, J. E. & Tipton, E. Meta-analysis with robust variance estimation: Expanding the range of working models. Prev. Sci. 23 , 425–438 (2022).
Lenth, R. emmeans: estimated marginal means, aka least-squares means. R package v.1.5.1 (2020).
Bartoń, K. MuMIn: multi-modal inference. Model selection and model averaging based on information criteria (AICc and alike) (2019).
Burnham, K. P. & Anderson, D. R. Multimodel inference: understanding AIC and BIC in model selection. Sociol. Methods Res. 33 , 261–304 (2004).
Article MathSciNet Google Scholar
Marks‐Anglin, A. & Chen, Y. A historical review of publication bias. Res. Synth. Methods 11 , 725–742 (2020).
Nakagawa, S. et al. Methods for testing publication bias in ecological and evolutionary meta‐analyses. Methods Ecol. Evol. 13 , 4–21 (2022).
Gurevitch, J., Koricheva, J., Nakagawa, S. & Stewart, G. Meta-analysis and the science of research synthesis. Nature 555 , 175–182 (2018).
Bates, D., Mächler, M., Bolker, B. & Walker, S. Fitting linear mixed-effects models using lme4. J. Stat. Softw. 67 , 1–48 (2015).
Mahon, M. B. et al. Data and code for ‘A meta-analysis on global change drivers and the risk of infectious disease’. Zenodo https://doi.org/10.5281/zenodo.8169979 (2024).
Mahon, M. B. et al. Data and code for ‘A meta-analysis on global change drivers and the risk of infectious disease’. GitHub github.com/mahonmb/GCDofDisease (2024).
Download references
Acknowledgements
We thank C. Mitchell for contributing data on enemy release; L. Albert and B. Shayhorn for assisting with data collection; J. Gurevitch, M. Lajeunesse and G. Stewart for providing comments on an earlier version of this manuscript; and C. Carlson and two anonymous reviewers for improving this paper. This research was supported by grants from the National Science Foundation (DEB-2109293, DEB-2017785, DEB-1518681, IOS-1754868), National Institutes of Health (R01TW010286) and US Department of Agriculture (2021-38420-34065) to J.R.R.; a US Geological Survey Powell grant to J.R.R. and S.L.R.; University of Connecticut Start-up funds to S.A.K.; grants from the National Science Foundation (IOS-1755002) and National Institutes of Health (R01 AI150774) to D.J.C.; and an Ambizione grant (PZ00P3_202027) from the Swiss National Science Foundation to F.W.H. The funders had no role in study design, data collection and analysis, decision to publish or preparation of the manuscript.
Author information
These authors contributed equally: Michael B. Mahon, Alexandra Sack, Jason R. Rohr
Authors and Affiliations
Department of Biological Sciences, University of Notre Dame, Notre Dame, IN, USA
Michael B. Mahon, Alexandra Sack, O. Alejandro Aleuy, Carly Barbera, Ethan Brown, Heather Buelow, Luz A. de Wit, Meghan Forstchen, Patrick Heffernan, Alexis Korotasz, Joanna G. Larson, Samantha L. Rumschlag, Emily Selland, Alexander Shepack, Nitin Vincent & Jason R. Rohr
Environmental Change Initiative, University of Notre Dame, Notre Dame, IN, USA
Michael B. Mahon, Samantha L. Rumschlag & Jason R. Rohr
Eck Institute of Global Health, University of Notre Dame, Notre Dame, IN, USA
Alexandra Sack, Meghan Forstchen, Emily Selland & Jason R. Rohr
Department of Biology, Emory University, Atlanta, GA, USA
David J. Civitello
Department of Ecology and Evolutionary Biology, Yale University, New Haven, CT, USA
Jeremy M. Cohen
Department of Botany and Plant Pathology, Oregon State University, Corvallis, OR, USA
Fletcher W. Halliday
Department of Ecology and Evolutionary Biology, Institute for Systems Genomics, University of Connecticut, Storrs, CT, USA
Sarah A. Knutie
You can also search for this author in PubMed Google Scholar
Contributions
J.R.R. conceptualized the study. All of the authors contributed to the methodology. All of the authors contributed to investigation. Visualization was performed by M.B.M. The initial study list and related information were compiled by D.J.C., J.M.C., F.W.H., S.A.K., S.L.R. and J.R.R. Data extraction was performed by M.B.M., A.S., O.A.A., C.B., E.B., H.B., L.A.d.W., M.F., P.H., A.K., J.G.L., E.S., A.S. and N.V. Data were checked for accuracy by M.B.M. and A.S. Analyses were performed by M.B.M. and J.R.R. Funding was acquired by D.J.C., J.R.R., S.A.K. and S.L.R. Project administration was done by J.R.R. J.R.R. supervised the study. J.R.R. and M.B.M. wrote the original draft. All of the authors reviewed and edited the manuscript. J.R.R. and M.B.M. responded to reviewers.
Corresponding author
Correspondence to Jason R. Rohr .
Ethics declarations
Competing interests.
The authors declare no competing interests.
Peer review
Peer review information.
Nature thanks Colin Carlson and the other, anonymous, reviewer(s) for their contribution to the peer review of this work. Peer reviewer reports are available.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Extended data figures and tables
Extended data fig. 1 prisma flowchart..
The PRISMA flow diagram of the search and selection of studies included in this meta-analysis. Note that 77 studies came from the Halliday et al. 3 database on biodiversity change.
Extended Data Fig. 2 Summary of the number of studies (A-F) and parasite taxa (G-L) in the infectious disease database across ecological contexts.
The contexts are global change driver ( A , G ), parasite taxa ( B , H ), host taxa ( C , I ), experimental venue ( D , J ), study habitat ( E , K ), and human parasite status ( F , L ).
Extended Data Fig. 3 Summary of the number of effect sizes (A-I), studies (J-R), and parasite taxa (S-a) in the infectious disease database for various parasite and host contexts.
Shown are parasite type ( A , J , S ), host thermy ( B , K , T ), vector status ( C , L , U ), vector-borne status ( D , M , V ), parasite transmission ( E , N , W ), free living stages ( F , O , X ), host (e.g. disease, host growth, host survival) or parasite (e.g. parasite abundance, prevalence, fecundity) endpoint ( G , P , Y ), micro- vs macroparasite ( H , Q , Z ), and zoonotic status ( I , R , a ).
Extended Data Fig. 4 The effects of global change drivers and subsequent subcategories on disease responses with Log Response Ratio instead of Hedge’s g.
Here, Log Response Ratio shows similar trends to that of Hedge’s g presented in the main text. The displayed points represent the mean predicted values (with 95% confidence intervals) from a meta-analytical model with separate random intercepts for study. Points that do not share letters are significantly different from one another (p < 0.05) based on a two-sided Tukey’s posthoc multiple comparison test with adjustment for multiple comparisons. See Table S 3 for pairwise comparison results. Effects of the five common global change drivers ( A ) have the same directionality, similar magnitude, and significance as those presented in Fig. 2 . Global change driver effects are significant when confidence intervals do not overlap with zero and explicitly tested with two-tailed t-test (indicated by asterisks; t 80.62 = 2.16, p = 0.034 for CP; t 71.42 = 2.10, p = 0.039 for CC; t 131.79 = −3.52, p < 0.001 for HLC; t 61.9 = 2.10, p = 0.040 for IS). The subcategories ( B ) also show similar patterns as those presented in Fig. 3 . Subcategories are significant when confidence intervals do not overlap with zero and were explicitly tested with two-tailed one sample t-test (t 30.52 = 2.17, p = 0.038 for CO 2 ; t 40.03 = 4.64, p < 0.001 for Enemy Release; t 47.45 = 2.18, p = 0.034 for Mean Temperature; t 110.81 = −4.05, p < 0.001 for Urbanization); all other subcategories have p > 0.20. Note that effect size and study numbers are lower here than in Figs. 3 and 4 , because log response ratios cannot be calculated for studies that provide coefficients (e.g., odds ratio) rather than raw data; as such, all observations within BC did not have associated RR values. Despite strong differences in sample size, patterns are consistent across effect sizes, and therefore, we can be confident that the results presented in the main text are not biased because of effect size selection.
Extended Data Fig. 5 Average standard errors of the effect sizes (A) and sample sizes per effect size (B) for each of the five global change drivers.
The displayed points represent the mean predicted values (with 95% confidence intervals) from the generalized linear mixed effects models with separate random intercepts for study (Gaussian distribution for standard error model, A ; Poisson distribution for sample size model, B ). Points that do not share letters are significantly different from one another (p < 0.05) based on a two-sided Tukey’s posthoc multiple comparison test with adjustment for multiple comparisons. Sample sizes (number of studies, n, and effect sizes, k) for each driver are as follows: n = 77, k = 392 for BC; n = 124, k = 364 for CP; n = 202, k = 380 for CC; n = 517, k = 1449 for HLC; n = 96, k = 355 for IS.
Extended Data Fig. 6 Forest plots of effect sizes, associated variances, and relative weights (A), Funnel plots (B), and Egger’s Test plots (C) for each of the five global change drivers and leave-one-out publication bias analyses (D).
In panel A , points are the individual effect sizes (Hedge’s G), error bars are standard errors of the effect size, and size of the points is the relative weight of the observation in the model, with larger points representing observations with higher weight in the model. Sample sizes are provided for each effect size in the meta-analytic database. Effect sizes were plotted in a random order. Egger’s tests indicated significant asymmetries (p < 0.05) in Biodiversity Change (worst asymmetry – likely not bias, just real effect of positive relationship between diversity and disease), Climate Change – (weak asymmetry, again likely not bias, climate change generally increases disease), and Introduced Species (relatively weak asymmetry – unclear whether this is a bias, may be driven by some outliers). No significant asymmetries (p > 0.05) were found in Chemical Pollution and Habitat Loss/Change, suggesting negligible publication bias in reported disease responses across these global change drivers ( B , C ). Egger’s test included publication year as moderator but found no significant relationship between Hedge’s g and publication year (p > 0.05) implying no temporal bias in effect size magnitude or direction. In panel D , the horizontal red lines denote the grand mean and SE of Hedge’s g and (g = 0.1009, SE = 0.0338). Grey points and error bars indicate the Hedge’s g and SEs, respectively, using the leave-one-out method (grand mean is recalculated after a given study is removed from dataset). While the removal of certain studies resulted in values that differed from the grand mean, all estimated Hedge’s g values fell well within the standard error of the grand mean. This sensitivity analysis indicates that our results were robust to the iterative exclusion of individual studies.
Extended Data Fig. 7 The effects of habitat loss/change on disease depend on parasite taxa and land use conversion contexts.
A) Enemy type influences the magnitude of the effect of urbanization on disease: helminths, protists, and arthropods were all negatively associated with urbanization, whereas viruses were non-significantly positively associated with urbanization. B) Reference (control) land use type influences the magnitude of the effect of urbanization on disease: disease was reduced in urban settings compared to rural and peri-urban settings, whereas there were no differences in disease along urbanization gradients or between urban and natural settings. C) The effect of forest fragmentation depends on whether a large/continuous habitat patch is compared to a small patch or whether disease it is measured along an increasing fragmentation gradient (Z = −2.828, p = 0.005). Conversely, the effect of deforestation on disease does not depend on whether the habitat has been destroyed and allowed to regrow (e.g., clearcutting, second growth forests, etc.) or whether it has been replaced with agriculture (e.g., row crop, agroforestry, livestock grazing; Z = 1.809, p = 0.0705). The displayed points represent the mean predicted values (with 95% confidence intervals) from a metafor model where the response variable was a Hedge’s g (representing the effect on an infectious disease endpoint relative to control), study was treated as a random effect, and the independent variables included enemy type (A), reference land use type (B), or land use conversion type (C). Data for (A) and (B) were only those studies that were within the “urbanization” subcategory; data for (C) were only those studies that were within the “deforestation” and “forest fragmentation” subcategories. Sample sizes (number of studies, n, and effect sizes, k) in (A) for each enemy are n = 48, k = 98 for Virus; n = 193, k = 343 for Protist; n = 159, k = 490 for Helminth; n = 10, k = 24 for Fungi; n = 103, k = 223 for Bacteria; and n = 30, k = 73 for Arthropod. Sample sizes in (B) for each reference land use type are n = 391, k = 1073 for Rural; n = 29, k = 74 for Peri-urban; n = 33, k = 83 for Natural; and n = 24, k = 58 for Urban Gradient. Sample sizes in (C) for each land use conversion type are n = 7, k = 47 for Continuous Gradient; n = 16, k = 44 for High/Low Fragmentation; n = 11, k = 27 for Clearcut/Regrowth; and n = 21, k = 43 for Agriculture.
Extended Data Fig. 8 The effects of common global change drivers on mean infectious disease responses in the literature depends on whether the endpoint is the host or parasite; whether the parasite is a vector, is vector-borne, has a complex or direct life cycle, or is a macroparasite; whether the host is an ectotherm or endotherm; or the venue and habitat in which the study was conducted.
A ) Parasite endpoints. B ) Vector-borne status. C ) Parasite transmission route. D ) Parasite size. E ) Venue. F ) Habitat. G ) Host thermy. H ) Parasite type (ecto- or endoparasite). See Table S 2 for number of studies and effect sizes across ecological contexts and global change drivers. See Table S 3 for pairwise comparison results. The displayed points represent the mean predicted values (with 95% confidence intervals) from a metafor model where the response variable was a Hedge’s g (representing the effect on an infectious disease endpoint relative to control), study was treated as a random effect, and the independent variables included the main effects and an interaction between global change driver and the focal independent variable (whether the endpoint measured was a host or parasite, whether the parasite is vector-borne, has a complex or direct life cycle, is a macroparasite, whether the study was conducted in the field or lab, habitat, the host is ectothermic, or the parasite is an ectoparasite).
Extended Data Fig. 9 The effects of five common global change drivers on mean infectious disease responses in the literature only occasionally depend on location, host taxon, and parasite taxon.
A ) Continent in which the field study occurred. Lack of replication in chemical pollution precluded us from including South America, Australia, and Africa in this analysis. B ) Host taxa. C ) Enemy taxa. See Table S 2 for number of studies and effect sizes across ecological contexts and global change drivers. See Table S 3 for pairwise comparison results. The displayed points represent the mean predicted values (with 95% confidence intervals) from a metafor model where the response variable was a Hedge’s g (representing the effect on an infectious disease endpoint relative to control), study was treated as a random effect, and the independent variables included the main effects and an interaction between global change driver and continent, host taxon, and enemy taxon.
Extended Data Fig. 10 The effects of human vs. non-human endpoints for the zoonotic disease subset of database and wild vs. domesticated animal endpoints for the non-human animal subset of database are consistent across global change drivers.
(A) Zoonotic disease responses measured on human hosts responded less positively (closer to zero when positive, further from zero when negative) than those measured on non-human (animal) hosts (Z = 2.306, p = 0.021). Note, IS studies were removed because of missing cells. (B) Disease responses measured on domestic animal hosts responded less positively (closer to zero when positive, further from zero when negative) than those measured on wild animal hosts (Z = 2.636, p = 0.008). These results were consistent across global change drivers (i.e., no significant interaction between endpoint and global change driver). As many of the global change drivers increase zoonotic parasites in non-human animals and all parasites in wild animals, this may suggest that anthropogenic change might increase the occurrence of parasite spillover from animals to humans and thus also pandemic risk. The displayed points represent the mean predicted values (with 95% confidence intervals) from a metafor model where the response variable was a Hedge’s g (representing the effect on an infectious disease endpoint relative to control), study was treated as a random effect, and the independent variable of global change driver and human/non-human hosts. Data for (A) were only those diseases that are considered “zoonotic”; data for (B) were only those endpoints that were measured on non-human animals. Sample sizes in (A) for zoonotic disease measured on human endpoints across global change drivers are n = 3, k = 17 for BC; n = 2, k = 6 for CP; n = 25, k = 39 for CC; and n = 175, k = 331 for HLC. Sample sizes in (A) for zoonotic disease measured on non-human endpoints across global change drivers are n = 25, k = 52 for BC; n = 2, k = 3 for CP; n = 18, k = 29 for CC; n = 126, k = 289 for HLC. Sample sizes in (B) for wild animal endpoints across global change drivers are n = 28, k = 69 for BC; n = 21, k = 44 for CP; n = 50, k = 89 for CC; n = 121, k = 360 for HLC; and n = 29, k = 45 for IS. Sample sizes in (B) for domesticated animal endpoints across global change drivers are n = 2, k = 4 for BC; n = 4, k = 11 for CP; n = 7, k = 20 for CC; n = 78, k = 197 for HLC; and n = 1, k = 2 for IS.
Supplementary information
Supplementary information.
Supplementary Discussion, Supplementary References and Supplementary Tables 1–3.
Reporting Summary
Peer review file, supplementary data 1.
R markdown code and output associated with this paper.
Supplementary Table 4
EcoEvo PRISMA checklist.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
Reprints and permissions
About this article
Cite this article.
Mahon, M.B., Sack, A., Aleuy, O.A. et al. A meta-analysis on global change drivers and the risk of infectious disease. Nature (2024). https://doi.org/10.1038/s41586-024-07380-6
Download citation
Received : 02 August 2022
Accepted : 03 April 2024
Published : 08 May 2024
DOI : https://doi.org/10.1038/s41586-024-07380-6
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
By submitting a comment you agree to abide by our Terms and Community Guidelines . If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing: Anthropocene newsletter — what matters in anthropocene research, free to your inbox weekly.
- Future Students
- Current Students
- Faculty/Staff

News and Media
- News & Media Home
- Research Stories
- School's In
- In the Media
You are here
70 years after brown v. board of education, new research shows rise in school segregation.

As the nation prepares to mark the 70th anniversary of the landmark U.S. Supreme Court ruling in Brown v. Board of Education , a new report from researchers at Stanford and USC shows that racial and economic segregation among schools has grown steadily in large school districts over the past three decades — an increase that appears to be driven in part by policies favoring school choice over integration.
Analyzing data from U.S. public schools going back to 1967, the researchers found that segregation between white and Black students has increased by 64 percent since 1988 in the 100 largest districts, and segregation by economic status has increased by about 50 percent since 1991.
The report also provides new evidence about the forces driving recent trends in school segregation, showing that the expansion of charter schools has played a major role.
The findings were released on May 6 with the launch of the Segregation Explorer , a new interactive website from the Educational Opportunity Project at Stanford University. The website provides searchable data on racial and economic school segregation in U.S. states, counties, metropolitan areas, and school districts from 1991 to 2022.
“School segregation levels are not at pre- Brown levels, but they are high and have been rising steadily since the late 1980s,” said Sean Reardon , the Professor of Poverty and Inequality in Education at Stanford Graduate School of Education and faculty director of the Educational Opportunity Project. “In most large districts, school segregation has increased while residential segregation and racial economic inequality have declined, and our findings indicate that policy choices – not demographic changes – are driving the increase.”
“There’s a tendency to attribute segregation in schools to segregation in neighborhoods,” said Ann Owens , a professor of sociology and public policy at USC. “But we’re finding that the story is more complicated than that.”
Assessing the rise
In the Brown v. Board decision issued on May 17, 1954, the U.S. Supreme Court ruled that racially segregated public schools violated the Equal Protection Clause of the Fourteenth Amendment and established that “separate but equal” schools were not only inherently unequal but unconstitutional. The ruling paved the way for future decisions that led to rapid school desegregation in many school districts in the late 1960s and early 1970s.
Though segregation in most school districts is much lower than it was 60 years ago, the researchers found that over the past three decades, both racial and economic segregation in large districts increased. Much of the increase in economic segregation since 1991, measured by segregation between students eligible and ineligible for free lunch, occurred in the last 15 years.
White-Hispanic and white-Asian segregation, while lower on average than white-Black segregation, have both more than doubled in large school districts since the 1980s.
Racial-economic segregation – specifically the difference in the proportion of free-lunch-eligible students between the average white and Black or Hispanic student’s schools – has increased by 70 percent since 1991.
School segregation is strongly associated with achievement gaps between racial and ethnic groups, especially the rate at which achievement gaps widen during school, the researchers said.
“Segregation appears to shape educational outcomes because it concentrates Black and Hispanic students in higher-poverty schools, which results in unequal learning opportunities,” said Reardon, who is also a senior fellow at the Stanford Institute for Economic Policy Research and a faculty affiliate of the Stanford Accelerator for Learning .
Policies shaping recent trends
The recent rise in school segregation appears to be the direct result of educational policy and legal decisions, the researchers said.
Both residential segregation and racial disparities in income declined between 1990 and 2020 in most large school districts. “Had nothing else changed, that trend would have led to lower school segregation,” said Owens.
But since 1991, roughly two-thirds of districts that were under court-ordered desegregation have been released from court oversight. Meanwhile, since 1998, the charter sector – a form of expanded school choice – has grown.
Expanding school choice could influence segregation levels in different ways: If families sought schools that were more diverse than the ones available in their neighborhood, it could reduce segregation. But the researchers found that in districts where the charter sector expanded most rapidly in the 2000s and 2010s, segregation grew the most.
The researchers’ analysis also quantified the extent to which the release from court orders accounted for the rise in school segregation. They found that, together, the release from court oversight and the expansion of choice accounted entirely for the rise in school segregation from 2000 to 2019.
The researchers noted enrollment policies that school districts can implement to mitigate segregation, such as voluntary integration programs, socioeconomic-based student assignment policies, and school choice policies that affirmatively promote integration.
“School segregation levels are high, troubling, and rising in large districts,” said Reardon. “These findings should sound an alarm for educators and policymakers.”
Additional collaborators on the project include Demetra Kalogrides, Thalia Tom, and Heewon Jang. This research, including the development of the Segregation Explorer data and website, was supported by the Russell Sage Foundation, the Robert Wood Johnson Foundation, and the Bill and Melinda Gates Foundation.
More Stories

⟵ Go to all Research Stories
Get the Educator
Subscribe to our monthly newsletter.
Stanford Graduate School of Education
482 Galvez Mall Stanford, CA 94305-3096 Tel: (650) 723-2109
- Contact Admissions
- GSE Leadership
- Site Feedback
- Web Accessibility
- Career Resources
- Faculty Open Positions
- Explore Courses
- Academic Calendar
- Office of the Registrar
- Cubberley Library
- StanfordWho
- StanfordYou
Improving lives through learning

- Stanford Home
- Maps & Directions
- Search Stanford
- Emergency Info
- Terms of Use
- Non-Discrimination
- Accessibility
© Stanford University , Stanford , California 94305 .
- Open access
- Published: 16 May 2024
Competency gap among graduating nursing students: what they have achieved and what is expected of them
- Majid Purabdollah 1 , 2 ,
- Vahid Zamanzadeh 2 , 3 ,
- Akram Ghahramanian 2 , 4 ,
- Leila Valizadeh 2 , 5 ,
- Saeid Mousavi 2 , 6 &
- Mostafa Ghasempour 2 , 4
BMC Medical Education volume 24 , Article number: 546 ( 2024 ) Cite this article
116 Accesses
Metrics details
Nurses’ professional competencies play a significant role in providing safe care to patients. Identifying the acquired and expected competencies in nursing education and the gaps between them can be a good guide for nursing education institutions to improve their educational practices.
In a descriptive-comparative study, students’ perception of acquired competencies and expected competencies from the perspective of the Iranian nursing faculties were collected with two equivalent questionnaires consisting of 85 items covering 17 competencies across 5 domains. A cluster sampling technique was employed on 721 final-year nursing students and 365 Iranian nursing faculties. The data were analyzed using descriptive statistics and independent t-tests.
The results of the study showed that the highest scores for students’ acquired competencies and nursing faculties’ expected competencies were work readiness and professional development, with mean of 3.54 (SD = 0.39) and 4.30 (SD = 0.45), respectively. Also, the lowest score for both groups was evidence-based nursing care with mean of 2.74 (SD = 0.55) and 3.74 (SD = 0.57), respectively. The comparison of competencies, as viewed by both groups of the students and the faculties, showed that the difference between the two groups’ mean scores was significant in all 5 core-competencies and 17 sub-core competencies ( P < .001). Evidence-based nursing care was the highest mean difference (mean diff = 1) and the professional nursing process with the lowest mean difference (mean diff = 0.70).
The results of the study highlight concerns about the gap between expected and achieved competencies in Iran. Further research is recommended to identify the reasons for the gap between the two and to plan how to reduce it. This will require greater collaboration between healthcare institutions and nursing schools.
Peer Review reports
Introduction| Background
Nursing competence refers to a set of knowledge, skills, and behaviors that are necessary to successfully perform roles or responsibilities [ 1 ]. It is crucial for ensuring the safe and high-quality care of patients [ 2 , 3 , 4 , 5 ]. However, evaluating nursing competence is challenging due to the complex, dynamic, and multi factorial nature of the clinical environment [ 3 ]. The introduction of nursing competencies and their assessment as a standard measure of clinical performance at the professional level has been highlighted by the Association of American Colleges of Nursing [ 6 , 7 ]. As a result, AACN (2020) introduces competence assessment as an emerging concept in nursing education [ 7 ].
On the other hand, the main responsibility of nursing education is to prepare graduates who have the necessary competencies to provide safe and quality care [ 3 ]. Although it is believed that it is impossible to teach everything to students, acquiring some competencies requires entering a real clinical setting and gaining work experience [ 8 ]. However, nursing students are expected to be competent to ensure patient safety and quality of care after graduation [ 9 ]. To the extent that the World Health Organization (WHO), while expressing concern about the low quality of nursing education worldwide, has recommended investing in nursing education and considers that the future to require nurses who are theoretically and clinically competent [ 5 ]. Despite efforts, the inadequate preparation of newly graduated nursing students and doubts about the competencies acquired in line with expectations to provide safe care for entering the nursing setting have become a global concern [ 10 , 11 , 12 , 13 ]. The results of studies in this field are different. The results of Amsalu et al. showed that the competence of newly graduated nursing students to provide quality and safe care was not satisfactory [ 14 ]. Some studies have also highlighted shortcomings in students’ “soft” skills, such as technical competency, critical thinking, communication, teamwork, helping roles, and professionalism [ 15 ]. Additionally, prior research has indicated that several nursing students have an unrealistic perception of their acquired competencies before entering the clinical setting and they report a high level of competence [ 2 ]. In other study, Hickerson et al. showed that the lack of preparation of nursing students is associated with an increase in patient errors and poor patient outcomes [ 16 ]. Some studies also discussed nursing competencies separately; Such as patient safety [ 17 ], clinical reasoning [ 18 ], interpersonal communication [ 19 ], and evidence-based care competence [ 20 ].
On the other hand, the growing need for safe nursing care and the advent of new educational technologies, the emergence of infectious diseases has increased the necessity of nursing competence. As a result, the nursing profession must be educated to excellence more than ever before [ 5 , 21 , 22 ]. Therefore, the self-assessment of students’ competence levels as well as the evaluation of nursing managers about the competencies expected from them is an essential criterion for all healthcare stakeholders, educators, and nursing policymakers to ensure the delivery of safe, and effective nursing care [ 9 , 23 , 24 ].
However, studies of nurse managers’ perceptions of the competence of newly graduated nursing students are limited and mostly conducted at the national level. Hence, further investigation is needed in this field [ 25 , 26 ]. Some other studies have been carried out according to the context and the needs of societies [ 3 , 26 , 27 , 28 ]. The results of some other studies in the field of students’ self-assessment of perceived competencies and managers’ and academic staff’s assessment of expected competency levels are different and sometimes contradictory, and there is the “academic-clinical gap” between expected and achieved competencies [ 25 , 29 , 30 ]. A review of the literature showed that this gap has existed for four decades, and the current literature shows that it has not changed much over time. The academe and practice settings have also been criticized for training nurses who are not sufficiently prepared to fully engage in patient care [ 1 ]. Hence, nursing managers must understand the expected competencies of newly graduated students, because they have a more complete insight into the healthcare system and the challenges facing the nursing profession. Exploration of these gaps can reveal necessities regarding the work readiness of nursing graduates and help them develop their competencies to enter the clinical setting [ 1 , 25 ].
Although research has been carried out on this topic in other countries, the educational system in those countries varies from that of Iran’s nursing education [ 31 , 32 ]. Iran’s nursing curriculum has tried to prepare nurses who have the necessary competencies to meet the care needs of society. Despite the importance of proficiency in nursing education, many nursing graduates often report feeling unprepared to fulfill expected competencies and they have deficiencies in applying their knowledge and experience in practice [ 33 ]. Firstly, the failure to define and identify the expected competencies in the nursing curriculum of Iran led to the absence of precise and efficient educational objectives. Therefore, it is acknowledged that the traditional nursing curriculum of Iran focuses more on lessons organization than competencies [ 34 ]. Secondly, insufficient attention has been given to the scheduling, location, and level of competencies in the nursing curriculum across different semesters [ 35 ]. Thirdly, the large volume of content instead of focusing on expected competencies caused nursing graduates challenged to manage complex situations [ 36 ]. Therefore, we should not expect competencies such as critical thinking, clinical judgment, problem-solving, decision-making, management, and leadership from nursing students and graduates in Iran [ 37 ]. Limited research has been conducted in this field in Iran. Studies have explored the cultural competence of nursing students [ 38 ] and psychiatric nurses [ 39 ]. Additionally, the competence priorities of nurses in acute care have been investigated [ 40 ], as well as the competency dimensions of nurses [ 41 ].
In Iran, after receiving the diploma, the students participate in a national exam called Konkur. Based on the results of this exam, they enter the field of nursing without conducting an aptitude test interview and evaluating individual and social characteristics. The 4-year nursing curriculum in Iran has 130 units including 22 general, 54 specific, 15 basic sciences, and 39 internship units. In each semester, several workshops are held according to the syllabus [ 42 ]. Instead of the expected competencies, a list of general competencies is specified as learning outcomes in the program. Accepted students based on their rank in the exam and their choice in public and Islamic Azad Universities (non-profit), are trained with a common curriculum. Islamic Azad Universities are not supported by government funding and are managed autonomously, this problem limits the access to specialized human resources and sufficient educational fields, and the lower salaries of faculty members in Azad Universities compared to the government system, students face serious challenges. Islamic Azad Universities must pay exorbitant fees to medical universities for training students in clinical departments and medical training centers, doubling these Universities’ financial problems. In some smaller cities, these financial constraints cause students to train in more limited fields of clinical training and not experience much of what they have learned in the classroom in practice and the real world of nursing. The evaluation of learners in the courses according to the curriculum is based on formative and summative evaluation with teacher-made tests, checklists, clinical assignments, conferences, and logbooks. The accreditation process of nursing schools includes two stages internal evaluation, which is done by surveying students, professors and managers of educational groups, and external accreditation is done by the nursing board. After completing all their courses, to graduate, students must participate in an exam called “Final”, which is held by each faculty without the supervision of an accreditation institution, the country’s assessment organization or the Ministry of Health, and obtain at least a score of 10 out of 20 to graduate.
Therefore, we conducted this comprehensive study as the first study in Iran to investigate the difference between the expected and perceived competence levels of final year nursing students. The study’s theoretical framework is based on Patricia Benner’s “From Novice to Expert” model [ 43 ].
Materials and methods
The present study had the following three objectives:
Determining self-perceived competency levels from the perspective of final year nursing students in Iran.
Determining expected levels of competency from the perspective of nursing faculties in Iran.
To determine the difference between the expected competencies from the perspective of nursing faculties and the achieved competencies from the perspective of final-year nursing students.
This study is a descriptive-comparative study.
First, we obtained a list of all nursing schools in the provinces of Iran from the Ministry of Health ( n = 31). From 208 Universities, 72 nursing schools were randomly selected using two-stage cluster sampling. Among the selected faculties, we chose 721 final-year nursing students and 365 nursing faculties who met the eligibility criteria for the study. Final-year nursing students who consented to participate in the study were selected. Full-time faculty members with at least 2 years of clinical experience and nurse managers with at least 5 years of clinical education experience were also included. In this study, nursing managers, in addition to their educational roles in colleges, also have managerial roles in the field of nursing. Some of these roles include nursing faculty management, nursing board member, curriculum development and review, planning and supervision of nursing education, evaluation, and continuous improvement of nursing education. The selection criteria were based on the significant role that managers play in nursing education and curriculum development [ 44 ]. Non-full-time faculty members and managers without clinical education experience were excluded from the study.
The instrument used in this study is a questionnaire developed and psychometrically tested in a doctoral nursing dissertation [ 45 ]. To design the tool, the competencies expected of undergraduate nursing students in Iran and worldwide were first identified through a scoping review using the methodology recommended by the Joanna Briggs Institute (JBI) and supported by the PAGER framework. Summative content analysis by Hsieh and Shannon (2005) was used for analysis, which included: counting and comparing keywords and content, followed by interpretation of textual meaning. In the second step, the results of the first step were used to create tool statements. Then the validity of the instrument was checked by face validity, content validity (determination of the ratio and index of content validity), and validity of known groups. Its reliability was also checked by internal consistency using Cronbach’s alpha method and stability using the test-retest method. The competency questionnaire comprises 85 items covering 17 competencies across 5 domains: “individualized care” (4 competencies with 21 items), “evidence-based nursing care” (2 competencies with 10 items), “professional nursing process” (3 competencies with 13 items), “nursing management” (2 competencies with 16 items), and “work readiness and professional development” (6 competencies with 25 items) [ 45 ]. “The Bondy Rating Scale was utilized to assess the competency items, with ratings ranging from 1 (Dependent) to 5 (Independent) on a 5-point Likert scale [ 46 ]. The first group (nursing students) was asked to indicate the extent to which they had acquired each competency. The second group (nursing faculties) was asked to specify the level to which they expected nursing students to achieve each competency.
Data collection
First, the researcher contacted the deans and managers of the selected nursing schools by email to obtain permission. After explaining the aims of the study and the sampling method, we obtained the telephone number of the representative of the group of final year nursing students and also the email of the faculty members. The representative of the student group was then asked to forward the link to the questionnaire to 10 students who were willing to participate in the research. Informed consent for students to participate in the online research was provided through the questionnaires, while nursing faculty members who met the eligibility criteria for the study received an informed consent form attached to the email questionnaire. The informed consent process clarified the study objectives and ensured anonymity of respondent participation in the research, voluntary agreement to participate and the right to revoke consent at any time. An electronic questionnaire was then sent to 900 final year nursing students and 664 nursing faculties (from 4 March 2023 to 11 July 2023). Reminder emails were sent to nursing faculty members three times at two-week intervals. The attrition rate in the student group was reported to be 0 (no incomplete questionnaires). However, four questionnaires from nursing faculty members were discarded because of incomplete responses. Of the 900 questionnaires sent to students and 664 sent to nursing faculties, 721 students and 365 nursing faculty members completed the questionnaire. The response rates were 79% and 66% respectively.
Data were analyzed using SPSS version 22. Frequencies and percentages were used to report categorical variables and mean and standard deviations were used for quantitative variables. The normality of the quantitative data was confirmed using the Shapiro-Wilk and Skewness tests. An independent t-test was used for differences between the two groups.
Data analysis revealed that out of 721 students, 441 (61.20%) was female. The mean and deviation of the students’ age was 22.50 (SD = 1.21). Most of the students 577 (80%) were in their final semester. Also, of the total 365 faculties, the majority were female 253 (69.31%) with a mean of age 44.06 (SD = 7.46) and an age range of 22–65. The academic rank of most nursing faculty members 156 (21.60%) was assistant professor (Table 1 ).
The results of the study showed that in both groups the highest scores achieved by the students and expected by the nursing faculty members were work readiness and professional development with a mean and standard deviation of 3.54 (0.39) and 4.30 (0.45) respectively. The lowest score for both groups was also evidence-based nursing care with a mean and standard deviation of 2.74 (0.55) for students and 3.74 (0.57) for nursing faculty members (Table 2 ).
Also, the result of the study showed that the highest expected competency score from the nursing faculty members’ point of view was the safety subscale. In other words, faculty members expected nursing students to acquire safety competencies at the highest level and to be able to provide safe care independently according to the rating scale (Mean = 4.51, SD = 0.45). The mean score of the competencies achieved by the students was not above 3.77 in any of the subscales and the highest level of competency achievement according to self-report of students was related to safety competencies (mean = 3.77, SD = 0.51), preventive health services (mean = 3.69, SD = 0.79), values and ethical codes (mean = 3.67, SD = 0.77), and procedural/clinical skills (mean = 3.67, SD = 0.71). The other competency subscales from the perspective of the two groups are presented in Table 3 , from highest to lowest score.
The analysis of core competencies achieved and expected from both students’ and nursing faculty members’ perspectives revealed that, firstly, there was a significant difference between the mean scores of the two groups in all five core competencies ( P < .001) and that the highest mean difference was related to evidence-based care with mean diff = 1 and the lowest mean difference was related to professional care process with mean diff = 0.70 (Table 4 ).
Table 5 indicates that there was a significant difference between the mean scores achieved by students and nursing faculty members in all 5 core competencies and 17 sub-core Competencies ( p < .001).
The study aimed to determine the difference between nursing students’ self-perceived level of competence and the level of competence expected of them by their nursing faculty members. The study results indicate that students scored highest in work readiness and professional development. However, they were not independent in this competency and required support. The National League for Nursing (NLN) recognizes nursing professional development as the goal of nursing education programs [ 47 ] However, Aguayo-Gonzalez [ 48 ] believes that the appropriate time for professional development is after entering a clinical setting. This theme includes personal characteristics, legality, clinical/ procedural skills, patient safety, preventive health services, and mentoring competence. Personality traits of nursing students are strong predictors of coping with nursing stress, as suggested by Imus [ 49 ]. These outcomes reflect changes in students’ individual characteristics during their nursing education. Personality changes, such as the need for patience and persistence in nursing care and understanding the nurse identity prepare students for the nursing profession, which is consistent with the studies of Neishabouri et al. [ 50 ]. Although the students demonstrated a higher level of competence in this theme, an examination of the items indicates that they can still not adapt to the challenges of bedside nursing and to use coping techniques. This presents a concerning issue that requires attention and resolution. Previous studies have shown that nursing education can be a very stressful experience [ 51 , 52 , 53 ].
Of course, there is no consensus on the definition of professionalism and the results of studies in this field are different. For example, Akhtar et al. (2013) identified common viewpoints about professionalism held by nursing faculty and students, and four viewpoints emerged humanists, portrayers, facilitators, and regulators [ 54 ]. The findings of another study showed that nursing students perceived vulnerability, symbolic representation, role modeling, discontent, and professional development are elements that show their professionalism [ 55 ]. The differences indicate that there may be numerous contextual variables that affect individuals’ perceptions of professionalism.
The legal aspects of nursing were the next item in this theme that students needed help with. The findings of studies regarding the legal competence of newly graduated nursing students are contradictory reported that only one-third of nurse managers were satisfied with the legal competence of newly graduated nursing students [ 56 , 57 ]. Whereas the other studies showed that legality was the highest acquired competence for newly graduated nursing students [ 58 , 59 ]. However, the results of this study indicated that legality may be a challenge for newly graduated nursing students. Benner [ 43 ] highlighted the significant change for new graduates in that they now have full legal and professional responsibility for the patient. Tong and Epeneter [ 60 ] also reported that facing an ethical dilemma is one of the most stressful factors for new graduates. Therefore, the inexperience of new graduates cannot reduce the standard of care that patients expect from them [ 60 ]. Legal disputes regarding the duties and responsibilities of nurses have increased with the expansion of their roles. This is also the case in Iran. Nurses are now held accountable by law for their actions and must be aware of their legal obligations. To provide safe healthcare services, it is essential to know of professional, ethical, and criminal laws related to nursing practice. The nursing profession is accountable for the quality of services delivered to patients from both professional and legal perspectives. Therefore, it is a valuable finding that nurse managers should support new graduates to better deal with ethical dilemmas. Strengthening ethical education in nursing schools necessitates integrating real cases and ethical dilemmas into the curriculum. Especially, Nursing laws are missing from Iran’s undergraduate nursing curriculum. By incorporating authentic case studies drawn from clinical practice, nursing schools provide students with opportunities to engage in critical reflection, ethical analysis, and moral deliberation. These real cases challenge students to apply ethical principles to complex and ambiguous situations, fostering the development of ethical competence and moral sensitivity. Furthermore, ethical reflection and debriefing sessions during clinical experiences enable students to discuss and process ethical challenges encountered in practice, promoting self-awareness, empathy, and professional growth. Overall, by combining theoretical instruction with practical application and the use of real cases, nursing schools can effectively prepare future nurses to navigate ethical dilemmas with integrity and compassion.
However, the theme of evidence-based nursing care was the lowest scoring, indicating that students need help with this theme. The findings from studies conducted in this field are varied. A limited number of studies reported that nursing students were competent to implement evidence-based care [ 61 ], while other researchers reported that nursing students’ attitudes toward evidence-based care to guide clinical decisions were largely negative [ 20 , 62 ]. The principal barriers to implementing evidence-based care are lack of authority to change patient care policy, slow dissemination of evidence and lack of time at the bedside to implement evidence [ 10 ], and lack of knowledge and awareness of the process of searching databases and evaluating research [ 63 ]. While the European Higher Education Area (EHEA) framework and the International Council of Nurses Code of Ethics introduce the ability to identify, critically appraise, and apply scientific information as expected learning outcomes for nursing students [ 64 , 65 ], the variation in findings highlights the complexity of the concept of competence and its assessment [ 23 ]. Evidence-Based Nursing (EBN) education for nursing students is most beneficial when it incorporates a multifaceted approach. Interactive workshops play a crucial role, providing students with opportunities to critically appraise research articles, identify evidence-based practices, and apply them to clinical scenarios. Simulation-based learning further enhances students’ skills by offering realistic clinical experiences in a safe environment. Additionally, clinical rotations offer invaluable opportunities for students to observe and participate in evidence-based practices under the guidance of experienced preceptors. Journal clubs foster a culture of critical thinking and ongoing learning, where students regularly review and discuss current research articles. Access to online resources such as databases and evidence-based practice guidelines allows students to stay updated on the latest evidence and best practices. To bridge the gap between clinical practice and academic theory, collaboration between nursing schools and healthcare institutions is essential. This collaboration can involve partnerships to create clinical learning environments that prioritize evidence-based practice, inter professional education activities to promote collaboration across disciplines, training and support for clinical preceptors, and continuing education opportunities for practicing nurses to strengthen their understanding and application of EBN [ 66 ]. By implementing these strategies, nursing education programs can effectively prepare students to become competent practitioners who integrate evidence-based principles into their clinical practice, ultimately improving patient outcomes.
The study’s findings regarding the second objective showed that nursing faculty members expected students to achieve the highest level of competence in work readiness and professional development, and the lowest in evidence-based nursing care competence. The results of the studies in this area revealed that there is a lack of clarity about the level of competence of newly graduated nursing students and that confusion about the competencies expected of them has become a major challenge [ 13 , 67 ]. Evidence of nurse managers’ perceptions of newly graduated nursing student’s competence is limited and rather fragmented. There is a clear need for rigorous empirical studies with comprehensive views of managers, highlighting the key role of managers in the evaluation of nurse competence [ 1 , 9 ]. Some findings also reported that nursing students lacked competence in primary and specialized care after entering a real clinical setting [ 68 ] and that nursing managers were dissatisfied with the competence of students [ 30 ].
The results of the present study on the third objective confirmed the gap between expected and achieved competence requirements. The highest average difference was related to evidence-based nursing care, and the lowest mean difference was related to the professional nursing process. The findings from studies in this field vary. For instance, Brown and Crookes [ 13 ] reported that newly graduated nursing students were not independent in at least 26 out of 30 competency domains. Similar studies have also indicated that nursing students need a structured program after graduation to be ready to enter clinical work [ 30 ]. It can be stated that the nursing profession does not have clear expectations of the competencies of newly graduated nursing students, and preparing them for entry into clinical practice is a major challenge for administrators [ 13 ]. These findings can be explained by the Duchscher transition shock [ 69 ]. It is necessary to support newly graduated nursing students to develop their competence and increase their self-confidence.
The interesting but worrying finding was the low expectations of faculty members and the low scores of students in the theme of evidence-based care. However, nursing students need to keep their competencies up to date to provide safe and high-quality care. The WHO also considers the core competencies of nurse educators to be the preparation of effective, efficient, and skilled nurses who can teach the evidence-based learning process and help students apply it clinically [ 44 ]. The teaching of evidence-based nursing care appears to vary across universities, and some clinical Faculties do not have sufficient knowledge to support students. In general, it can be stated that the results of the present study are in line with the context of Iran. Some of the problems identified include a lack of attention to students’ academic talent, a lack of a competency-based curriculum, a gap between theory and clinical practice, and challenges in teaching and evaluating the achieved competencies [ 42 ].
Strengths and limitations
The study was conducted on a national level with a sizable sample. It is one of the first studies in Iran to address the gap between students’ self-perceived competence levels and nursing faculty members’ expected competency levels. Nevertheless, one of the limitations of the study is the self-report nature of the questionnaire, which may lead to social desirability bias. In addition, the COVID-19 pandemic coinciding with the student’s first and second years could potentially impact their educational quality and competencies. The limitations established during the outbreak negatively affected the nursing education of students worldwide.
Acquiring nursing competencies is the final product of nursing education. The current study’s findings suggest the existence of an academic-practice gap, highlighting the need for educators, faculty members, and nursing managers to collaborate in bridging the potential gap between theory and practice. While nursing students were able to meet some expectations, such as value and ethical codes, there is still a distance between expectations and reality. Especially, evidence-based care was identified as one of the weaknesses of nursing students. It is recommended that future research investigates the best teaching strategies and more objective assessments of competencies. The findings of this study can be used as a guide for the revision of undergraduate nursing education curricula, as well as a guide for curriculum development based on the development of competencies expected of nursing students. Nursing managers can identify existing gaps and plan to fill them and use them for the professionalization of students. This requires the design of educational content and objective assessment tools to address these competencies at different levels throughout the academic semester. This significant issue necessitates enhanced cooperation between healthcare institutions and nursing schools. Enhancing nursing education requires the implementation of concrete pedagogical strategies to bridge the gap between theoretical knowledge and practical skills. Simulation-based learning emerges as a pivotal approach, offering students immersive experiences in realistic clinical scenarios using high-fidelity simulators [ 70 ]. Interprofessional education (IPE) is also instrumental, in fostering collaboration among healthcare professionals and promoting holistic patient care. Strengthening clinical preceptorship programs is essential, with a focus on providing preceptors with formal training and ongoing support to facilitate students’ clinical experiences and transition to professional practice [ 71 ]. Integrating evidence-based practice (EBP) principles throughout the curriculum cultivates critical thinking and inquiry skills among students, while technology-enhanced learning platforms offer innovative ways to engage students and support self-directed learning [ 72 ]. Diverse and comprehensive clinical experiences across various healthcare settings ensure students are prepared for the complexities of modern healthcare delivery. By implementing these practical suggestions, nursing education programs can effectively prepare students to become competent and compassionate healthcare professionals.
Data availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Huston C, et al. The academic-practice gap: strategies for an enduring problem . In nursing forum . Wiley Online Library; 2018.
Meretoja R, Isoaho H, Leino-Kilpi H. Nurse competence scale: development and psychometric testing. J Adv Nurs. 2004;47(2):124–33.
Article Google Scholar
Järvinen T, et al. Nurse educators’ perceptions of factors related to the competence of graduating nursing students. Nurse Educ Today. 2021;101:104884.
Satu KU, et al. Competence areas of nursing students in Europe. Nurse Educ Today. 2013;33(6):625–32.
World Health Organization. State of the world’s nursing 2020: investing in education, jobs and leadership. 2020 [cited 12 June 2023; https://www.who.int/publications-detail-redirect/9789240003279 .
Lee W-H, Kim S, An J. Development and evaluation of korean nurses’ core competency scale (KNCCS) 2017.
American Association of Colleges of Nursing. The essentials: core competencies for professional nursing education… 2020 [cited 2023; https://www.aacnnursing.org/Portals/0/PDFs/Publications/Essentials-2021.pdf .
Gardulf A, et al. The Nurse Professional competence (NPC) scale: self-reported competence among nursing students on the point of graduation. Nurse Educ Today. 2016;36:165–71.
Kajander-Unkuri S, et al. The level of competence of graduating nursing students in 10 European countries-comparison between countries. Nurs Open. 2021;8(3):1048–62.
Labrague LJ et al. A Multicountry Study on Nursing Students’ Self-Perceived Competence and Barriers to Evidence‐Based Practice 2019. 16(3): pp. 236–246.
Visiers-Jiménez L, et al. Clinical learning environment and graduating nursing students’ competence: a multi-country cross-sectional study. Nurs Health Sci. 2021;23(2):398–410.
Herron EK. New graduate nurses’ preparation for recognition and prevention of failure to rescue: a qualitative study. J Clin Nurs. 2018;27(1–2):e390–401.
Google Scholar
Brown RA, Crookes PA. What are the ‘necessary’ skills for a newly graduating RN? Results of an Australian survey. BMC Nurs. 2016;15:23.
Amsalu B, et al. Clinical practice competence of Mettu University nursing students: a cross-sectional study. Adv Med Educ Pract. 2020;11:791–8.
Song Y, McCreary LL. New graduate nurses’ self-assessed competencies: an integrative review. Nurse Educ Pract. 2020;45:102801.
Hickerson KA, Taylor LA, Terhaar MF. The Preparation-Practice gap: an Integrative Literature Review. J Contin Educ Nurs. 2016;47(1):17–23.
Huang FF, et al. Self-reported confidence in patient safety competencies among Chinese nursing students: a multi-site cross-sectional survey. BMC Med Educ. 2020;20(1):32.
Hong S et al. A Cross-Sectional Study: What Contributes to Nursing Students’ Clinical Reasoning Competence? Int J Environ Res Public Health, 2021. 18(13).
Mcquitty DJPE, Counseling. Teaching interpersonal communication concepts to increase awareness and reduce health disparities: Presenter (s): DaKysha Moore, NCAT, United States 2023. 109: pp. 25–26.
Lam CK, Schubert CF, Herron EK. Evidence-based practice competence in nursing students preparing to transition to practice. Worldviews Evid Based Nurs. 2020;17(6):418–26.
Lake MA. What we know so far: COVID-19 current clinical knowledge and research. Clin Med (Lond). 2020;20(2):124–7.
Shustack L. Integrating Google Earth in Community Health nursing courses: preparing globally aware nurses. Nurse Educ. 2020;45(2):E11–2.
Zeleníková R, et al. Self-assessed competence of final-year nursing students. Nurs Open. 2023;10(7):4607–18.
Hyun A, Tower M, Turner C. Exploration of the expected and achieved competency levels of new graduate nurses. J Nurs Manag. 2020;28(6):1418–31.
Kukkonen P, et al. Nurse managers’ perceptions of the competence of newly graduated nurses: a scoping review. J Nurs Manag. 2020;28(1):4–16.
Nilsson J et al. Nurse professional competence (NPC) assessed among newly graduated nurses in higher educational institutions in Europe. 2019. 39(3): p. 159–67.
Kajander-Unkuri S et al. Students’ Self-assessed Competence Levels during Nursing Education Continuum - A Cross-sectional Survey. Int J Nurs Educ Scholarsh, 2020. 17(1).
Salminen L, et al. The competence of nurse educators and graduating nurse students. Nurse Educ Today. 2021;98:104769.
Numminen O, et al. Newly graduated nurses’ competence and individual and organizational factors: a multivariate analysis. J Nurs Scholarsh. 2015;47(5):446–57.
Södersved Källestedt ML, et al. Perceptions of managers regarding prerequisites for the development of professional competence of newly graduated nurses: a qualitative study. J Clin Nurs. 2020;29(23–24):4784–94.
Ezzati E, et al. Exploring the social accountability challenges of nursing education system in Iran. BMC Nurs. 2023;22(1):7.
Farsi Z, et al. Comparison of Iran’s nursing education with developed and developing countries: a review on descriptive-comparative studies. BMC Nurs. 2022;21(1):105.
Salem OA et al. Competency based nursing curriculum: establishing the standards for nursing competencies in higher education. 2018. 5(11): p. 1–8.
Noohi E, Ghorbani-Gharani L. and A.J.S.i.D.o.M.E. Abbaszadeh, A comparative study of the curriculum of undergraduate nursing education in Iran and selected renowned universities in the world 2015. 12(3): pp. 450–471.
Rassouli M, Zagheri Tafreshi M. J.J.o.c.e. Esmaeil. Challenges Clin Nurs Educ Iran Strategies. 2014;2(1):11–22.
Riazi S, et al. Understanding gaps and needs in the undergratue nursing curriculum in Iran: a prelude to design a competency-based curriculum model %J payesh (Health Monitor). Journal. 2020;19(2):145–58.
ADIB HM, Mazhariazad F. Nursing Bachelor’s Education program in Iran and UCLA: A comparative study 2019.
Farokhzadian J, et al. Using a model to design, implement, and evaluate a training program for improving cultural competence among undergraduate nursing students: a mixed methods study. BMC Nurs. 2022;21(1):85.
Sargazi O, et al. Improving the professional competency of psychiatric nurses: results of a stress inoculation training program. Psychiatry Res. 2018;270:682–7.
Faraji A, et al. Evaluation of clinical competence and its related factors among ICU nurses in Kermanshah-Iran: a cross-sectional study. Int J Nurs Sci. 2019;6(4):421–5.
Atashzadeh-Shoorideh F, et al. Essential dimensions of professional competency examination in Iran from academic and clinical nurses’ perspective: a mixed-method study. J Educ Health Promot. 2021;10:414.
Purabdollah M, et al. Comparison of the Iranian and scandinavian bachelor of nursing curriculum (Sweden): a scoping review. J Educ Health Promotion. 2023;12(1):389.
Benner P. J.B.o.s., technology and society, using the Dreyfus model of skill acquisition to describe and interpret skill acquisition and clinical judgment in nursing practice and education . 2004. 24(3): p. 188–99.
World Health Organization. Nurse educator core competencies. Geneva, Switzerland: World Health Organization. 2016 [cited 23 June 2023; https://www.who.int/hrh/nursing_midwifery/nurse_educator050416.pdf .
Purabdollah M, et al. Competencies expected of undergraduate nursing students: a scoping review. Nurs Open. 2023;10(12):7487–508.
Bondy KN. Clinical evaluation of student performance: the effects of criteria on accuracy and reliability. Res Nurs Health. 1984;7(1):25–33.
NLf N. Outcomes for graduates of practical/vocational, diploma, associate degree, baccalaureate, master’s, practice doctorate, and research doctorate programs in nursing . New York 2010; 201]. https:api.semanticscholar.org/corpus ID: 68620057.
Aguayo-González M, Castelló-Badía M, Monereo-Font C. Critical incidents in nursing academics: discovering a new identity. Rev Bras Enferm. 2015;68(2):195–202. 219 – 27.
Scott Imus FJJNEP. Nurse anesthesia student’s personality characteristics and academic performance: A big five personality model perspective 2019. 9: pp. 47–55.
Neishabouri M, Ahmadi F, Kazemnejad A. Iranian nursing students’ perspectives on transition to professional identity: a qualitative study. Int Nurs Rev. 2017;64(3):428–36.
Zheng S, et al. New nurses’ experience during a two year transition period to clinical practice: a phenomenological study. Nurse Educ Today. 2023;121:105682.
Aryuwat P, et al. An integrative review of resilience among nursing students in the context of nursing education. Nurs Open. 2023;10(5):2793–818.
Ayaz-Alkaya S, Simones J. Nursing education stress and coping behaviors in Turkish and the United States nursing students: a descriptive study. Nurse Educ Pract. 2022;59:103292.
Akhtar-Danesh N, et al. Perceptions of professionalism among nursing faculty and nursing students. West J Nurs Res. 2013;35(2):248–71.
Keeling J, Templeman J. An exploratory study: student nurses’ perceptions of professionalism. Nurse Educ Pract. 2013;13(1):18–22.
Nilsson J, et al. Development and validation of a new tool measuring nurses self-reported professional competence–the nurse professional competence (NPC) scale. Nurse Educ Today. 2014;34(4):574–80.
Berkow S, et al. Assessing new graduate nurse performance. J Nurs Adm. 2008;38(11):468–74.
Lofmark A, Smide B, Wikblad K. Competence of newly-graduated nurses–a comparison of the perceptions of qualified nurses and students. J Adv Nurs. 2006;53(6):721–8.
Park E, Choi J. Attributes associated with person-centered care competence among undergraduate nursing students. Res Nurs Health. 2020;43(5):511–9.
Tong V, Epeneter BJ. A comparative study of newly licensed registered nurses’ stressors: 2003 and 2015. J Contin Educ Nurs. 2018;49(3):132–40.
Florin J, et al. Educational support for research utilization and capability beliefs regarding evidence-based practice skills: a national survey of senior nursing students. J Adv Nurs. 2012;68(4):888–97.
Reid J, et al. Enhancing utility and understanding of evidence based practice through undergraduate nurse education. BMC Nurs. 2017;16:58.
Phillips JM, Cullen D. Improving the adoption of evidence-based practice through RN-to-BSN education. J Contin Educ Nurs. 2014;45(10):467–72.
Stievano A, Tschudin V. The ICN code of ethics for nurses: a time for revision. Int Nurs Rev. 2019;66(2):154–6.
Ministry of Education and Research. Norwegian qualifications framework: levels and learning outcome descriptors… 2011 [cited 23 June 2023; https://www.regjeringen.no/contentassets/e579f913fa1d45c2bf2219afc726670b/nkr.pdf .
Chen Q, et al. Differences in evidence-based nursing practice competencies of clinical and academic nurses in China and opportunities for complementary collaborations: a cross‐sectional study. J Clin Nurs. 2023;32(13–14):3695–706.
Missen K, McKenna L, Beauchamp A. Registered nurses’ perceptions of new nursing graduates’ clinical competence: a systematic integrative review. Nurs Health Sci. 2016;18(2):143–53.
Leonardsen AL, et al. Nurses’ perspectives on technical skill requirements in primary and tertiary healthcare services. Nurs Open. 2020;7(5):1424–30.
Duchscher JE. B.J.J.o.a.n. Transition Shock: Initial Stage role Adaptation New Graduated Registered Nurses. 2009;65(5):1103–13.
Ajemba MN, Ikwe C, Iroanya JC. Effectiveness of simulation-based training in medical education: assessing the impact of simulation-based training on clinical skills acquisition and retention: a systematic review. World J Adv Res Reviews. 2024;21(1):1833–43.
Krystallidou D et al. Interprofessional education for healthcare professionals. A BEME realist review of what works, why, for whom and in what circumstances in undergraduate health sciences education: BEME Guide No. 83 Medical Teacher, 2024: pp. 1–18.
Sun Y, et al. Critical thinking abilities among newly graduated nurses: a cross-sectional survey study in China. Nurs Open. 2023;10(3):1383–92.
Download references
Acknowledgements
The authors extend their gratitude to all the nursing students and faculties who took part in this study.
This article is part of research approved with the financial support of the deputy of research and technology of Tabriz University of Medical Sciences.
Author information
Authors and affiliations.
Department of Nursing, Khoy University of Medical Sciences, Khoy, Iran
Majid Purabdollah
Medical Education Research Center, Health Management and Safety Promotion Research Institute, Tabriz University of Medical Sciences, Tabriz, Iran
Majid Purabdollah, Vahid Zamanzadeh, Akram Ghahramanian, Leila Valizadeh, Saeid Mousavi & Mostafa Ghasempour
Department of Medical-Surgical Nursing, School of Nursing and Midwifery, Shahid Beheshti University of Medical Sciences, Tehran, Iran
Vahid Zamanzadeh
Department of Medical Surgical Nursing, Faculty of Nursing and Midwifery, Tabriz University of Medical Sciences, Tabriz, Iran
Akram Ghahramanian & Mostafa Ghasempour
Department of Pediatric Nursing, School of Nursing and Midwifery, Shahid Beheshti University of Medical Sciences, Tehran, Iran
Leila Valizadeh
Department of Epidemiology and Biostatistics, Assistant Professor of Biostatistics, School of Health, Tabriz University of Medical Sciences, Tabriz, Iran
Saeid Mousavi
You can also search for this author in PubMed Google Scholar
Contributions
M P: conceptualized the study, data collection, analysis and interpretation, drafting of manuscript; V Z: conceptualized the study, analysis and interpretation, drafting of manuscript; LV: conceptualized the study, data collection and analysis, manuscript revision; A Gh: conceptualized the study, data collection, analysis, and drafting of manuscript; S M: conceptualized the study, analysis, and drafting of manuscript; M Gh: data collection, analysis, and interpretation, drafting of manuscript; All authors read and approved the final manuscript.
Ethics declarations
Ethics approval and consent to participate.
All the participants voluntarily participated in this study and provided written informed consent. The study was approved by the ethics committee of the Tabriz University of Medical Sciences (Ethical Code: IR.TBZMED.REC.1400.791) and all methods were performed in accordance with relevant guidelines and regulations.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Purabdollah, M., Zamanzadeh, V., Ghahramanian, A. et al. Competency gap among graduating nursing students: what they have achieved and what is expected of them. BMC Med Educ 24 , 546 (2024). https://doi.org/10.1186/s12909-024-05532-w
Download citation
Received : 23 November 2023
Accepted : 07 May 2024
Published : 16 May 2024
DOI : https://doi.org/10.1186/s12909-024-05532-w
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Nursing education
- Self-Assessment
- Nursing students
- Professional Competency Professional
BMC Medical Education
ISSN: 1472-6920
- Submission enquiries: [email protected]
- General enquiries: [email protected]

Mentorship in Health Research Institutions in Africa: A Systematic Review of Approaches, Benefits, Successes, Gaps and Challenges
- Find this author on Google Scholar
- Find this author on PubMed
- Search for this author on this site
- ORCID record for Maurine Ng'oda
- For correspondence: [email protected]
- ORCID record for Peter Muriuki Gatheru
- Info/History
- Preview PDF
In Africa, where the burden of diseases is disproportionately high, significant challenges arise from a shortage of skilled researchers, lack of research funding, and limited mentorship opportunities. The continent faces a substantial gap in research output largely attributed to the dearth of mentorship opportunities for early career researchers. We conducted this systematic review to explore existing mentorship approaches, identify challenges, gaps, successes, and benefits, and provide insights for strengthening mentorship programs in African health research institutions. We registered the review protocol on the International Prospective Register of Systematic Reviews [CRD42021285018] and searched six electronic databases – EMBASE, AJOL, Web of Science, PubMed, DOAJ and JSTOR from inception to 10 November 2023, for studies published in English reporting on approaches of mentorship in health research in African countries. We also searched grey literature repositories, institutional websites, and reference lists of included studies for additional literature. Two independent reviewers conducted screening of titles and abstracts of identified studies, full-text screening, assessment of methodological quality, and data extraction. We assessed study quality against the Mixed Methods Appraisal Tool (MMAT). We resolved any disagreements through discussion and consensus. We employed a narrative approach to synthesize the findings. We retrieved 1799 articles and after screening, included 21 studies in the review. The reviewers identified 20 mentorship programs for health researchers (N=1198) in 12 African countries mostly focusing on early career researchers and junior faculty members. A few included mid-career and senior researchers. We categorized the programs under three key mentoring approaches: international collaborative programs, regional and in-country collaborations, and specialized capacity-building initiatives. Our review highlighted the following successes and benefits of health research mentorship programs: the establishment of collaborations and partnerships, development of research programs and capacities, improvement of individual skills and confidence, increased publications, and successful grant applications. The gaps identified were limited funding, lack of a mentorship culture, negative attitudes towards research careers, and lack of prioritization of research mentorship. Our review highlights a diverse landscape of health research mentorship aspects predominantly targeting early career researchers and heavily driven by the North. There is a need for locally driven mentorship initiatives in Africa to strengthen mentorship in order to advance health research in the region.
Competing Interest Statement
The authors have declared no competing interest.
Funding Statement
This work received funding from the African Research Excellent Fund (AREF) through the Research and Related Capacity Strengthening (RRCS) unit at the African Population and Health Research Center. The funder had no role in the design, execution, synthesis, interpretation or decision to publish this manuscript.
Author Declarations
I confirm all relevant ethical guidelines have been followed, and any necessary IRB and/or ethics committee approvals have been obtained.
The details of the IRB/oversight body that provided approval or exemption for the research described are given below:
The article is a systematic review that synthesized secondary data. No ethical approval was required.
I confirm that all necessary patient/participant consent has been obtained and the appropriate institutional forms have been archived, and that any patient/participant/sample identifiers included were not known to anyone (e.g., hospital staff, patients or participants themselves) outside the research group so cannot be used to identify individuals.
I understand that all clinical trials and any other prospective interventional studies must be registered with an ICMJE-approved registry, such as ClinicalTrials.gov. I confirm that any such study reported in the manuscript has been registered and the trial registration ID is provided (note: if posting a prospective study registered retrospectively, please provide a statement in the trial ID field explaining why the study was not registered in advance).
I have followed all appropriate research reporting guidelines, such as any relevant EQUATOR Network research reporting checklist(s) and other pertinent material, if applicable.
Data Availability
Data underlying the findings for this review has been provided as part of the submitted article in the supplementary information.
View the discussion thread.
Thank you for your interest in spreading the word about medRxiv.
NOTE: Your email address is requested solely to identify you as the sender of this article.

Citation Manager Formats
- EndNote (tagged)
- EndNote 8 (xml)
- RefWorks Tagged
- Ref Manager
- Tweet Widget
- Facebook Like
- Google Plus One
- Addiction Medicine (324)
- Allergy and Immunology (628)
- Anesthesia (165)
- Cardiovascular Medicine (2379)
- Dentistry and Oral Medicine (289)
- Dermatology (207)
- Emergency Medicine (379)
- Endocrinology (including Diabetes Mellitus and Metabolic Disease) (837)
- Epidemiology (11775)
- Forensic Medicine (10)
- Gastroenterology (703)
- Genetic and Genomic Medicine (3747)
- Geriatric Medicine (350)
- Health Economics (634)
- Health Informatics (2399)
- Health Policy (933)
- Health Systems and Quality Improvement (898)
- Hematology (341)
- HIV/AIDS (782)
- Infectious Diseases (except HIV/AIDS) (13318)
- Intensive Care and Critical Care Medicine (768)
- Medical Education (365)
- Medical Ethics (105)
- Nephrology (398)
- Neurology (3508)
- Nursing (198)
- Nutrition (526)
- Obstetrics and Gynecology (675)
- Occupational and Environmental Health (664)
- Oncology (1825)
- Ophthalmology (538)
- Orthopedics (219)
- Otolaryngology (287)
- Pain Medicine (233)
- Palliative Medicine (66)
- Pathology (446)
- Pediatrics (1035)
- Pharmacology and Therapeutics (426)
- Primary Care Research (420)
- Psychiatry and Clinical Psychology (3178)
- Public and Global Health (6145)
- Radiology and Imaging (1280)
- Rehabilitation Medicine and Physical Therapy (747)
- Respiratory Medicine (828)
- Rheumatology (379)
- Sexual and Reproductive Health (372)
- Sports Medicine (323)
- Surgery (402)
- Toxicology (50)
- Transplantation (172)
- Urology (146)
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Lippincott Open Access
Identifying Research Gaps and Prioritizing Psychological Health Evidence Synthesis Needs
Susanne hempel.
* RAND Corporation, Evidence-based Practice Center (EPC), Santa Monica
† University of Southern California, Keck School of Medicine, Los Angeles, CA
Kristie Gore
‡ RAND, National Security Research Division, Arlington
Bradley Belsher
§ Defense Health Agency, Psychological Health Center of Excellence (PHCoE), Falls Church, VA
Associated Data
Supplemental Digital Content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal's website, www.lww-medicalcare.com .
Supplemental Digital Content is available in the text.
Background:
Evidence synthesis is key in promoting evidence-based health care, but it is resource-intense. Methods are needed to identify and prioritize evidence synthesis needs within health care systems. We describe a collaboration between an agency charged with facilitating the implementation of evidence-based research and practices across the Military Health System and a research center specializing in evidence synthesis.
Scoping searches targeted 15 sources, including the Veterans Affairs/Department of Defense Guidelines and National Defense Authorization Acts. We screened for evidence gaps in psychological health management approaches relevant to the target population. We translated gaps into potential topics for evidence maps and/or systematic reviews. Gaps amenable to evidence synthesis format provided the basis for stakeholder input. Stakeholders rated topics for their potential to inform psychological health care in the military health system. Feasibility scans determined whether topics were ready to be pursued, that is, sufficient literature exists, and duplicative efforts are avoided.
We identified 58 intervention, 9 diagnostics, 12 outcome, 19 population, and 24 health services evidence synthesis gaps. Areas included: posttraumatic stress disorder (PTSD) (19), suicide prevention (14), depression (9), bipolar disorder (9), substance use (24), traumatic brain injury (20), anxiety (1), and cross-cutting (14) synthesis topics. Stakeholder input helped prioritize 19 potential PTSD topics and 22 other psychological health topics. To date, 46 topics have undergone feasibility scans. We document lessons learned across clinical topics and research methods.
Conclusion:
We describe a transparent and structured approach to evidence synthesis topic selection for a health care system using scoping searches, translation into evidence synthesis format, stakeholder input, and feasibility scans.
Evidence synthesis is an essential step in promoting evidence-based medicine across health systems; it facilitates the translation of research to practice. A systematic review of the research literature on focused review questions is a key evidence synthesis approach that can inform practice and policy decisions. 1 However, systematic reviews are resource-intense undertakings. In a resource-constrained environment, before an evidence review is commissioned, the need and the feasibility of the review must be established.
Establishing the need for the review can be achieved through a research gap analysis or needs assessment. Identification of a gap serves as the first step in developing a new research question. 2 Research gaps in health care do not necessarily align directly with research needs. Research gaps are only critical where knowledge gaps substantially inhibit the decision-making ability of stakeholders such as patients, health care providers, and policymakers, thus creating a need to fill the knowledge gap. Evidence synthesis enables the assessment of whether a research gap continues to exist or whether there is adequate evidence to close the knowledge gap.
Furthermore, a gap analysis often identifies multiple, competing gaps that are worthwhile to be pursued. Given the resource requirements of formal evidence reviews, topic prioritization is needed to best allocate resources to those areas deemed the most relevant for the health system. Regardless of the topic, the prioritization process is likely to be stakeholder-dependent. Priorities for evidence synthesis will vary depending on the mission of the health care system and the local needs of the health care stakeholders. A process of stakeholder input is an important mechanism to ensure that the evidence review will meet local needs as well to identify a receptive audience of the review findings.
In addition to establishing the need for an evidence review, the feasibility of conducting the review must also be established. In conducting primary research, feasibility is often mainly a question of available resources. For evidence reviews, the resources, the availability of primary research, and the presence of existing evidence reviews on the topic need to be explored. Not all topics are amenable for a systematic review which focus on a specific range of research questions and rely heavily on published literature. Furthermore, evidence review synthesizes the existing evidence; hence, if there is insufficient evidence in the primary research literature, an evidence review is not useful. Establishing a lack of evidence is a worthwhile exercise since it identifies the need for further research. However, most health care delivery organizations will be keen to prioritize areas that can be synthesized, that is, investing in synthesizing a body of research sizable enough to derive meaningful results. For evidence reviews, the presence of existing evidence syntheses is also an important consideration, in particular, to determine the incremental validity of a new review. Although primary research benefits profoundly by replication, secondary literature, in particular in the context of existing high-quality reviews and/or limited evidence, may not add anything to our knowledge base. 3
This work describes a structured and transparent approach to identify and prioritize areas of psychological health that are important and that can be feasibly addressed by a synthesis of the research literature. It describes a collaboration between an agency charged with facilitating the implementation of evidence-based research and practices across the Military Health System (MHS) and a research center specializing in evidence synthesis.
This project is anchored in the relationship between the Defense Health Agency Psychological Health Center of Excellence (PHCoE) and the RAND Corporation’s National Defense Research Institute (NDRI), one of the Federally Funded Research and Development Centers (FFRDC) dedicated to providing long-term analytic support to the Defense Health Agency. PHCoE, an agency charged with facilitating the implementation of evidence-based research and practices across the Military Health System funded a series of systematic reviews and evidence maps synthesizing psychological research. The project draws on the expertise of the Southern California Evidence-based Practice Center (EPC) located at RAND, a center specializing in evidence synthesis. The project included scoping searches, stakeholder input, and feasibility scans. The project is ongoing; this manuscript describes methods and results from June 2016 to September 2018. The project was assessed by our Human Subject Protection staff and determined to be exempt (date July 7, 2016, ID ND3621; August 6, 2017, ID ND3714).
The following describes the process, Figure Figure1 1 provides a visual overview.

Process of identifying research gaps and prioritizing psychological health evidence synthesis needs.
Scoping Searches to Identify Evidence Synthesis Gaps
Scoping searches targeted pertinent sources for evidence gaps. The searches focused on clinical conditions and interventions relevant to psychological health, including biological psychiatry, health care services research, and mental health comorbidity. Proposed topics and study populations were not limited by deployment status or deployment eligibility, but the topic section considered the prevalence of clinical conditions among Department of Defense active duty military personnel managed by the MHS. The scoping searches excluded evidence gaps addressing children and adolescents and clinical conditions exclusively relevant to veterans managed by the Department of Veterans Affairs.
Scoping Search Sources
We screened 15 sources in total for evidence synthesis gaps.
Veterans Affairs/Department of Defense clinical practice guidelines were a key source for documented evidence gaps. 4 – 9 Recently updated guidelines were screened only for evidence gaps that indicated a lack of synthesis of existing research or content areas that were outside the scope of that guideline (guidelines rely primarily on published systematic reviews and can only review a limited number of topic areas).
We consulted the current report of the committee on armed services of the House of Representatives regarding the proposed National Defense Authorization Act (NDAA) and the report for the upcoming fiscal year. 10 , 11 We specifically screened the report for research priorities identified for psychological health. We also screened the published National Research Action Plan designed to improve access to mental health services for veterans, service members, and military families. 12
We conducted a literature search for publications dedicated to identifying evidence gaps and research needs for psychological health and traumatic brain injury. We searched for publications published since 2000–2016 in the most relevant databases, PubMed and PsycINFO, that had the words research gap, knowledge gap, or research priority in the title and addressed psychological health (Supplemental Digital Content, http://links.lww.com/MLR/B836 ). The search retrieved 203 citations. Six publications were considered potentially relevant and obtained as full text, 1 source was subsequently excluded because the authors conducted a literature search <3 years ago and it was deemed unlikely that a new review would identify substantially more eligible studies. 13 – 19
We also used an analysis of the utilization of complementary and alternative medicine in the MHS 20 to identify interventions that were popular with patients but for which potentially little evidence-based guidance exists. We focused our scoping efforts on complementary approaches such as stress management, hypnotherapy, massage, biofeedback, chiropractic, and music therapy to align with the funding scope. In the next step, we reviewed the existing clinical practice guidelines to determine whether clinicians have guidance regarding these approaches. The Department of Defense Health Related Behaviors Survey of Active Duty Military Personnel 21 is an anonymous survey conducted every 3 years on service members with the aim of identifying interventions or health behaviors patients currently use. To address evidence gaps most relevant to patients, we screened the survey results, and then matched the more prevalent needs identified with guidance provided in relevant clinical practice guidelines.
We consulted the priority review list assembled by the Cochrane group to identify research needs for systematic reviews. We screened the 2015–2017 lists for mental health topics that are open to new authors, that is, those that do not have an author team currently dedicated to the topic. None of the currently available topics appeared relevant to psychological health and no topics were added to the table. We also consulted with ongoing federally funded projects to identify evidence gaps that were beyond the scope of the other projects. In addition, we screened a list of psychological health research priorities developed at PHCoE for knowledge gaps that could be addressed in systematic reviews or evidence maps. Finally, we screened resources available on MHS web sites for evidence gaps.
Gap Analysis Procedure and Approach to Translating Gaps into Evidence Review Format
We first screened these sources for knowledge gaps, regardless of considerations of whether the gap is amenable to evidence review. However, we did not include research gaps where the source explicitly indicated that the knowledge gap is due to the lack of primary research. We distinguished 5 evidence gap domains and abstracted gaps across pertinent areas: interventions or diagnostic questions, treatment outcomes or specific populations, and health services research and health care delivery models.
We then translated the evidence gaps into potential topics for evidence maps and/or systematic reviews. Evidence maps provide a broad overview of large research areas using data visualizations to document the presence and absence of evidence. 22 Similar to scoping reviews, evidence maps do not necessarily address the effects of interventions but can be broader in scope. Systematic reviews are a standardized research methodology designed to answer clinical and policy questions with published research using meta-analysis to estimate effect sizes and formal grading of the quality of evidence. We considered systematic reviews for effectiveness and comparative effectiveness questions regarding specific intervention and diagnostic approaches.
Stakeholder Input
Evidence synthesis gaps that were determined to be amenable to systematic review or evidence map methods provided the basis for stakeholder input. Although all topics were reviewed by project personnel, we also identified psychological health service leads for Army, Navy, Air Force, and Marines within the Defense Health Agency as key stakeholders to be included in the topic selection process. To date, 2 rounds of formal ratings by stakeholders have been undertaken.
The first round focused on the need for systematic review covering issues related to posttraumatic stress disorder (PTSD). The second round focused on other potential psychological health topics determined to be compatible with the MHS mission. Represented clinical areas were suicide prevention and aftercare, depressive disorders, anxiety disorders, traumatic brain injury, substance use disorder including alcohol and opioid use disorder, and chronic pain. All of the potential topics addressed either the effects of clinical interventions or health service research questions.
Stakeholders rated the topics based on their potential to inform psychological health care in the military health system. The raters used a scale 5-point rating scale ranging from “No impact” to “Very high impact.” In addition, stakeholders were able to add additional suggestions for evidence review. We analyzed the mean, the mode, and individual stakeholder rating indicating “high impact” for individual topics.
Feasibility Scans
Feasibility scans provided an estimate of the volume and the type of existing research literature which is informative for 3 reasons. First, this process determined whether sufficient research was available to inform a systematic review or an evidence map. Second, feasibility scans can provide an estimate of the required resources for an evidence review by establishing whether only a small literature base or a large number of research studies exists. Finally, feasibility scans identify existing high-profile evidence synthesis reports that could make a new synthesis obsolete.
Feasibility scans for potential evidence maps concentrated on the size of the body of research that would need to be screened and the relevant synthesis questions that can inform how this research should be organized in the evidence map. Feasibility scans for systematic reviews aimed to determine the number of relevant studies, existing high-quality reviews, and the number of studies not covered in existing reviews. Randomized controlled trials (RCTs) are the focus of most of the systematic review topics, that is, strong research evidence that could inform clinical practice guideline committees to recommend either for or against interventions. An experienced systematic reviewer used PubMed, a very well-maintained and user-friendly database for biomedical literature, developed preliminary search strategies, and applied database search filters (eg, for RCTs or systematic reviews) in preliminary literature searches to estimate the research volume for each topic.
Scans also identified any existing high-quality evidence review published by agencies specializing in unbiased evidence syntheses such as the Agency for Healthcare Research and Quality (AHRQ)’s Evidence-based Practice Center program, the Cochrane Collaboration, the Campbell Collaboration, the Evidence Synthesis Program of the Department of Veterans Affairs, and the Federal Health Technology Assessment program. We used the databases PubMed and PubMed Health to identify reports. We appraised the scope, relevance and publication year of the existing high-profile evidence reviews. The research base for psychological health develops rapidly and evidence syntheses need to ensure that current clinical policies reflect the best available evidence. When determining the feasibility and appropriateness of a new systematic review, we took the results of the original review and any new studies that had been published subsequent to the systematic review on the same topic into account.
The following results are described: the results of the scoping searches and gap analysis, the translation of gaps into evidence synthesis format, the stakeholder input ratings, and the feasibility scans.
Scoping Searches and Gap Analysis Results
The scoping search and gap analysis identified a large number of evidence gaps as documented in the gap analysis table in the Appendix (Supplemental Digital Content, http://links.lww.com/MLR/B836 ). Across sources, we identified 58 intervention, 9 diagnostics, 12 outcome, 19 population, and 24 health services evidence synthesis gaps. The evidence gaps varied considerably with regard to scope and specificity, for example, highlighting knowledge gaps in recommendations for medications for specific clinical indications or treatment combinations 4 to pointing out to gaps in supporting caregivers. 11 The largest group of evidence gaps were documented for interventions. This included open questions for individual interventions (eg, ketamine) 12 as well as the best format and modality within an intervention domain (eg, use of telehealth). 6 Diagnostic evidence gaps included open questions regarding predictive risk factors that could be used in suicide prevention 8 and the need for personalized treatments. 12 Outcome evidence gaps often pointed to the lack of measured outcomes to include cost-effectiveness as well as the lack of knowledge on hypothesized effects, such as increased access or decreased stigma associated with technology-based modalities. 23 Population evidence gaps addressed specific patient populations such as complex patients 5 and family members of service members. 11 The health services evidence gaps addressed care support through technology (eg, videoconferencing 23 ) as well as treatment coordination within health care organizations such as how treatment for substance use disorder should be coordinated with treatment for co-occurring conditions. 4
Potential Evidence Synthesis Topics
The gaps were translated into potential evidence map or systematic review topics. This translation process took into account that some topics cannot easily be operationalized as an evidence review. For example, knowledge gaps regarding prevalence or utilization estimates were hindered by the lack of publicly available data. In addition, we noted that some review questions may require an exhaustive search and a full-text review of the literature because the information cannot be searched for directly, and hence were outside the budget restraints.
The clinical areas and number of topics were: PTSD (n=19), suicide prevention (n=14), depression (n=9), bipolar disorder (n=9), substance use (n=24), traumatic brain injury (n=20), anxiety (n=1), and cross-cutting (n=14) evidence synthesis topics. All topic areas are documented in the Appendix (Supplemental Digital Content, http://links.lww.com/MLR/B836 ).
Stakeholder Input Results
Stakeholders rated 19 PTSD-related research gaps and suggested an additional 5 topics for evidence review, addressing both preventions as well as treatment topics. Mean ratings for topics ranged from 1.75 to 3.5 on a scale from 0 (no impact potential) to 4 (high potential for impact). Thus, although identified as research gaps, the potential of an evidence review to have an important impact on the MHS varied across the topics. Only 2 topics received a mean score of ≥3 (high potential), including predictors of PTSD treatment retention and response and PTSD treatment dosing, duration, and sequencing . In addition, raters’ opinions varied considerably across some topics with SDs ranging from 0.5 to 1.5 across all topics.
The stakeholders rated 22 other psychological health topics, suggested 2 additional topics for evidence review, and revised 2 original topics indicating which aspect of the research gap would be most important to address. Mean scores for the rated topics ranged from 0.25 to 3.75, with the SDs for each item ranging from 0 to 1.4. Six topics received an average score of ≥3, primarily focused on the topics of suicide prevention, substance use disorders, and telehealth interventions. Opinions on other topics varied widely across service leads.
Feasibility Scan Results
Evidence review topics that were rated by stakeholders as having some potential for impact (using a rating cutoff score>1) within the MHS were selected for formal feasibility scans. To date, 46 topics have been subjected to feasibility scans. Of these, 11 were evaluated as potential evidence map, 17 as a systematic review, and 18 as either at the time of the topic suggestion. The results of the feasibility scans are documented in the table in the Appendix (Supplemental Digital Content, http://links.lww.com/MLR/B836 ).
The feasibility scan result table shows the topic, topic modification suggestions based on literature reviews, and the mean stakeholder impact rating. The table shows the employed search strategy to determine the feasibility; the estimated number of RCTs in the database PubMed; the number and citation of Cochrane, Evidence Synthesis Program, and Health Technology Assessment reviews, that is, high-quality syntheses; and the estimated number of RCTs published after the latest existing systematic review that had been published on the topic.
Each potential evidence review topic was discussed in a narrative review report that documented the reason for determining the topic to be feasible or not feasible. Reasons for determining the topic to be not feasible included the lack of primary research for an evidence map or systematic review, the presence of an ongoing research project that may influence the evidence review scope, and the presence of an existing high-quality evidence review. Some topics were shown to be feasible upon further modification; this included topics that were partially addressed in existing reviews or topics where the review scope would need to be substantially changed to result in a high-impact evidence review. Topics to be judged feasible met all outlined criteria, that is, the topic could be addressed in a systematic review or evidence map, there were sufficient studies to justify a review, and the review would not merely replicate an existing review but make a novel contribution to the evidence base.
The project describes a transparent and structured approach to identify and prioritize evidence synthesis topics using scoping reviews, stakeholder input, and feasibility scans.
The work demonstrates an approach to establishing and evaluating evidence synthesis gaps. It has been repeatedly noted that research gap analyses often lack transparency with little information on analytic criteria and selection processes. 24 , 25 In addition, research need identification may not be informed by systematic literature searches documenting gaps but primarily rely on often unstructured content expert input. 26 , 27 Evidence synthesis needs assessment is a new field that to date has received very little attention. However, as health care delivery organizations move towards providing evidence-based treatments and the existing research continue to grow, both evidence reviews and evidence review gap identification and prioritization will become more prominent.
One of the lessons learned is that the topic selection process added to the timeline and required additional resources. The scoping searches, translation into evidence synthesis topics, stakeholder input, and feasibility scans each added time and the project required a longer period of performance compared to previous evidence synthesis projects. The project components were undertaken sequentially and had to be divided into topic areas. For example, it was deemed too much to ask for stakeholder input for all 122 topics identified as potential evidence review topics. Furthermore, we needed to be flexible to be able to respond to unanticipated congressional requests for evidence reviews. However, our process of identifying synthesis gaps, checking whether topics can be translated into syntheses, obtaining stakeholder input to ensure that the gaps are meaningful and need filling, and estimating the feasibility and avoiding duplicative efforts, has merit considering the alternative. More targeted funding of evidence syntheses ensures relevance and while resources need to be spent on the steps we are describing, these are small investments compared to the resources required for a full systematic review or evidence map.
The documented stakeholder engagement approach was useful for many reasons, not just for ensuring that the selection of evidence synthesis topics was transparent and structured. The stakeholders were alerted to the evidence synthesis project and provided input for further topic refinement. This process also supported the identification of a ‘customer’ after the review was completed, that is, a stakeholder who is keen on using the evidence review is likely to take action on its results and ready to translate the findings into clinical practice. The research to practice gap is substantial and the challenges of translating research to practice are widely documented. 28 – 30 Inefficient research translation delays delivery of proven clinical practices and can lead to wasteful research and practice investments.
The project had several strengths and limitations. The project describes a successful, transparent, and structured process to engage stakeholders and identifies important and feasible evidence review topics. However, the approach was developed to address the specific military psychological health care system needs, and therefore the process may not be generalizable to all other health care delivery organizations. Source selection was tailored to psychological health synthesis needs and process modifications (ie, sources to identify gaps) are needed for organizations aiming to establish a similar procedure. To keep the approach manageable, feasibility scans used only 1 database and we developed only preliminary, not comprehensive searches. Hence, some uncertainty about the true evidence base for the different topics remained; feasibility scans can only estimate the available research. Furthermore, the selected stakeholders were limited to a small number of service leads. A broader panel of stakeholders would have likely provided additional input. In addition, all evaluations of the literature relied on the expertise of experienced systematic reviewers; any replication of the process will require some staff with expertise in the evidence review. Finally, as outlined, all described processes added to the project timeline compounding the challenges of providing timely systematic reviews for practitioners and policymakers. 31 , 32
We have described a transparent and structured approach to identify and prioritize areas of evidence synthesis for a health care system. Scoping searches and feasibility scans identified gaps in the literature that would benefit from evidence review. Stakeholder input helped ensure the relevance of review topics and created a receptive audience for targeted evidence synthesis. The approach aims to advance the field of evidence synthesis needs assessment.
Supplementary Material
Acknowledgments.
The authors thank Laura Raaen, Margaret Maglione, Gulrez Azhar, Margie Danz, and Thomas Concannon for content input and Aneesa Motala and Naemma Golshan for administrative assistance.
Supported by the Office of the Secretary of Defense, Psychological Health Center of Excellence. The findings and conclusions in this manuscript are those of the authors and do not necessarily represent the views of the Psychological Health Center of Excellence, the Office of the Secretary of Defense, or the United States government.
The authors declare no conflict of interest.

- Previous Article
- Next Article
Performance of Medication Tasks: Relationship Among Patient-Reported Outcomes, Performance-Based Assessments, and Objective Assessments
- Article contents
- Figures & tables
- Supplementary Data
- Peer Review
- Get Permissions
- Cite Icon Cite
- Search Site
Jaclyn K. Schwartz , Katherine Aylmer , Samara Green , Sami Tayeb , Timothy J. Wolf , Elizabeth Unni , Emily Somerville; Performance of Medication Tasks: Relationship Among Patient-Reported Outcomes, Performance-Based Assessments, and Objective Assessments. Am J Occup Ther May/June 2024, Vol. 78(3), 7803205060. doi: https://doi.org/10.5014/ajot.2024.050500
Download citation file:
- Ris (Zotero)
- Reference Manager
Importance: Occupational therapy practitioners use standardized assessments to guide their clinical decision-making, but it is unclear how well performance on standardized assessments translates to performance at home.
Objective: To understand the concurrent and predictive validity of patient-reported outcomes and performance-based assessments for monitoring performance at home within the context of medication management and adherence.
Design: Exploratory study.
Setting: Participants completed standardized assessments in a lab or at home, which were followed by home-based electronic monitoring of medication adherence.
Participants: Sixty community-dwelling adults with hypertension or stroke who independently took antihypertensive medications.
Outcomes and Measures: Participants completed the Hill-Bone Medication Adherence Scale, the Hill-Bone Medication Adherence Reasons Scale, the Performance Assessment of Self-Care Skills Medication Management subtask, and the Executive Function Performance Test–Enhanced Medication Management subtest. Then, they used an electronic pill cap to monitor medication adherence at home for 1 month.
Results: Patient-reported outcomes and performance-based assessments in the context of medication management and adherence demonstrated poor concurrent and predictive validity to medication adherence at home.
Conclusions and Relevance: There is a gap between what people think they will do, what they can do on a standardized assessment, and what they actually do at home. Future research is needed to strengthen concurrent and predictive validity to clinically meaningful outcomes.
Plain-Language Summary: Occupational therapy practitioners should use caution when using standardized assessments to try to predict client performance at home. They should also continue to use a battery of assessments, clinical reasoning, and client preferences to guide their decision-making for monitoring performance at home within the context of medication management and adherence.

Citing articles via
Email alerts.

- Special Collections
- Conference Abstracts
- Browse AOTA Taxonomy
- AJOT Authors & Issues Series
- Online ISSN 1943-7676
- Print ISSN 0272-9490
- Author Guidelines
- Permissions
- Privacy Policy
- Cookie Policy
- Accessibility
- Terms of Use
- Copyright © American Occupational Therapy Association, Inc.
This Feature Is Available To Subscribers Only
Sign In or Create an Account
- Correspondence
- Open access
- Published: 20 May 2024
Generation of sarconoids from angiosarcoma patients as a systematic-based rational approach to treatment
- Da Jung Jung 1 ,
- Jae Hee Byeon 1 ,
- Young Chul Kim 3 ,
- Woo Shik Jeong 3 ,
- Jong-Woo Choi 3 , 4 &
- Gi Seok Jeong 1 , 2 , 5
Journal of Hematology & Oncology volume 17 , Article number: 35 ( 2024 ) Cite this article
Metrics details
Angiosarcoma is a rare subtype of malignant neoplasm originating from vascular or lymphatic endothelial cells; its low incidence has posed significant challenges for comprehensive investigations into its pathogenic mechanisms and the development of innovative treatment modalities through in vitro and in vivo models. Recent endeavors spearheaded by patient-partnered research initiatives have aimed to elucidate the intricacies of angiosarcomas by leveraging biological omics approaches, with the overarching objective of enhancing prognostic indicators and therapeutic options for this uncommon pathology. To bridge the gap between preclinical research and translational applications, we engineered angiosarcoma-derived organoids from surgically resected primary tumors, hereafter referred to as “sarconoids,” as a proof-of-concept model. A novel protocol for the establishment of these sarconoids has been developed and validated. To ensure that the sarconoids faithfully recapitulate the heterogeneity and complexities of the patients’ original tumors, including transcriptomic signatures, cell-type specificity, and morphological traits, exhaustive histological and transcriptomic analyses were conducted. Subsequently, we expanded the scope of our study to include an evaluation of a sarconoid-based drug screening platform; for this purpose, a drug library (AOD IX), supplied by the National Cancer Institute’s Developmental Therapeutics Program, was screened using 96-well plates. Our findings suggest that sarconoids can be reliably generated from angiosarcoma patient-derived tissues and can serve as accurate models for evaluating therapeutic responses, thereby holding far-reaching implications for translational research and clinical applications aimed at advancing our understanding and treatment of angiosarcoma.
To the editor
Patient-derived cancer organoids have become increasingly pivotal in pre-clinical and translational cancer research, having been generated from a diverse array of human cancer tissues [ 1 , 2 ]. Notably, most extant human cancer organoid models are derived from ectodermal or endodermal epithelial progenitors, and, to our knowledge, none have originated from mesenchymal or endothelial tissues [ 3 , 4 ].
Angiosarcoma is a rare yet aggressive mesenchymal tumor of endothelial origin [ 5 ]. There are several specific challenges associated with the clinical development of therapeutics for this disease, such as absence of prior clinical studies, and a lack of information on disease mechanisms and progression [ 6 , 7 ].
In this study, we propose a methodology to develop personalized angiosarcoma organoid models, termed “sarconoids,” for biological characterization and high-throughput drug screenings. To identify FDA-approved drugs amenable to repurposing for individualized treatment of rare diseases, we generated sarconoids using surgically resected angiosarcoma specimens (Fig. 1 a, Fig. S1 a). Immunohistochemical analyses and quantitative real-time PCR (qPCR) analyses revealed elevated expression levels of various vascular and mesenchymal markers in both primary tumors and tumor-derived sarconoids, as compared to normal tissues (Fig. 1 b, Fig. S1 c, Fig S2 a-c). To evaluate the angiogenic potential of our sarconoids, we conducted Matrigel-based sprouting assays. The results indicated that they exhibited more extensive matrix sprouting compared to HUVEC spheroids (Fig. S1 b, Fig. S2 d, e).
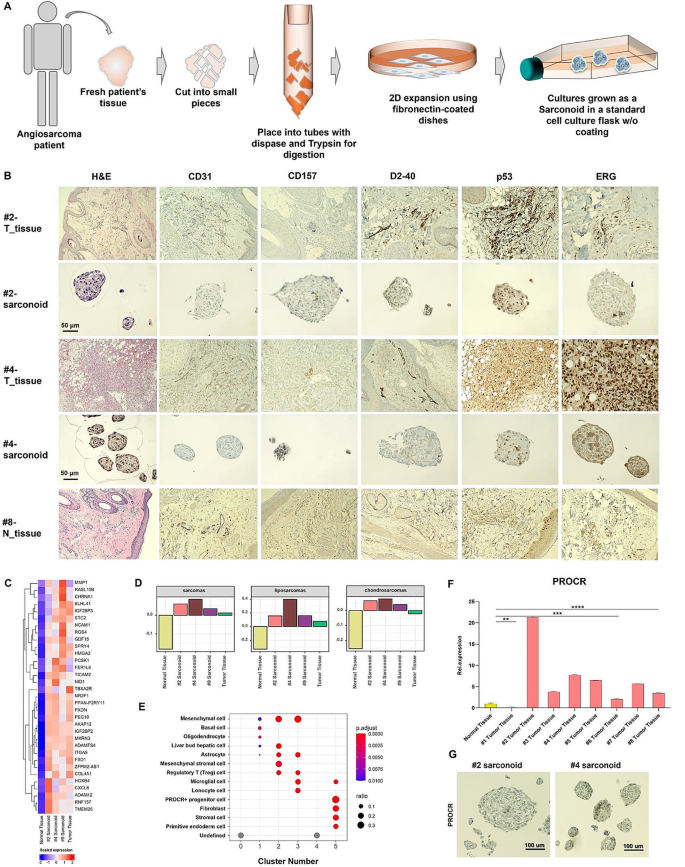
Establishment and characterization of sarconoids derived from angiosarcoma patients. ( a ) Schematic illustration of the workflow for the generation of sarconoids. ( b ) Histopathological staining of vascular neoplasm markers (CD31, CD157, ERG, and p53) and a lymphatic marker (D2-40) in primary resected angiosarcoma tumors and their corresponding sarconoids; scale bars, 50 μm. ( c ) Heat map of the scaled FPKM values of representative gene sets significantly upregulated in the patient-derived sarconoids and tumor tissue. ( d ) Gene set variation analysis (GSVA)-based subtyping of normal tissue, patient #2 tumor tissue, and patient #2-, #4 and #9-sarconoids against published gene sets (GeneRIF Biological Term Annotations), among the sarcoma subtypes. ( e ) Dot plot of the mean expression of canonical marker genes using the CellMarker database for 14 major lineages from each patient #2-sarconoid cluster, as indicated. ( f ) Quantification of PROCR expression by qRT-PCR in normal and cancer tissues ( n = 3). An unpaired t-test was used; * p < 0.05, ** p < 0.01,*** p < 0.001,**** p < 0.0001. ( g ) IHC assays of serial sections from patient #2- and patient #4-sarconoids for PROCR expression. Scale bars, 100 μm
To further elucidate the gene expression signature of sarconoids in comparison to their tissues of origin, angiosarcoma tissues and patient-derived sarconoids, collected from consenting patients, were analyzed using RNA-seq (Fig. S3 a). A heatmap depicting 33 genes that are upregulated across all four samples is presented in Fig. 1 c and Fig. S3 e (fold change > 4 and Bonferroni-corrected p < 0.001). Furthermore, gene set enrichment analysis techniques, such as gene set variation analysis, were employed to stratify sarcoma into distinct subgroups based on previously reported data [ 8 ]. Patient-derived sarconoids were classified into sarcoma, liposarcoma, and chondrosarcoma categories (Fig. 1 d). Hierarchical clustering results revealed an enrichment of angiogenesis-associated genes in both tissue and sarconoids derived from angiosarcomas (Fig. S3 f). Gene Ontology (GO) term enrichment analysis of the upregulated differentially expressed genes (DEGs) indicated that a variety of DEGs were enriched in biological processes pertinent to angiogenesis, muscle cell differentiation, and extracellular matrix (ECM) organization (Fig. S3 b-d). Conversely, GO terms associated with skin development were overrepresented in the downregulated genes (Fig. S3 g).
Utilizing UMAP to embed and cluster our single-cell expression data, we identified six distinct cell populations, labeled C0-C5 (Fig. S4 a). Each cluster was mapped to compare its most representative expressed genes with known markers (Fig. S4 b-d). Utilizing the CellMarker Database, we were able to assign multiple cell type labels to each cluster (Fig. 1 e). Notably, Cluster 5, which partially consists of PROCR-expressing progenitor cells, has been associated with vascular endothelial stem cells [ 9 , 10 ]. PROCR expression in tissue samples was analyzed using both qRT-PCR and immunohistochemistry, revealing high levels in 8 of the 9 angiosarcoma cases as compared to normal tissue (Fig. 1 f and Fig. S5b). Additionally, we performed qRT-PCR analyses to assess PROCR expression in patient-derived sarconoids, finding it to be significantly higher in sarconoids from patients #2 and #4 compared to normal cells (Fig. 1 g and Fig. S5 a).
To confirm the suitability of our sarconoid model for drug screening and response prediction, we conducted single-dose trials between 2.5 nM and 20 µM using anti-angiogenic agents on sarconoids derived from patient #4 (Fig. 2 a). Using a high-throughput in vitro drug screen, we assessed the cytotoxic activities of 147 FDA-approved compounds on patient-derived sarconoids, observing differing sensitivities between the three sarconoid strains (Fig. 2 b). Image-based phenotypic analyses helped categorize individual sarconoids as either insensitive or sensitive to specific treatments (Fig. S6a, b). Overall, 10 compounds demonstrated activity against at least one sarconoid strain. To validate these findings, we performed more comprehensive dose-response assays on 7 active compounds (Fig. 2 d, e). Intriguingly, EGFR-TKIs like afatinib and dacomitinib did not significantly impact the viability of sarconoids from patient #2 in our image-based assays, suggesting specific molecular targets and pathways are at play (Fig. 2 c). Moreover, sarconoids from patient #2 showed greater sensitivity to histone deacetylase (HDAC) inhibitors like romidepsin and panobinostat (Fig. S6c), suggesting up-regulation of the HDAC pathway in this case (Fig. 2 f). Each sarconoid line exhibited unique phenotypic and genomic features, resulting in varied drug sensitivities.
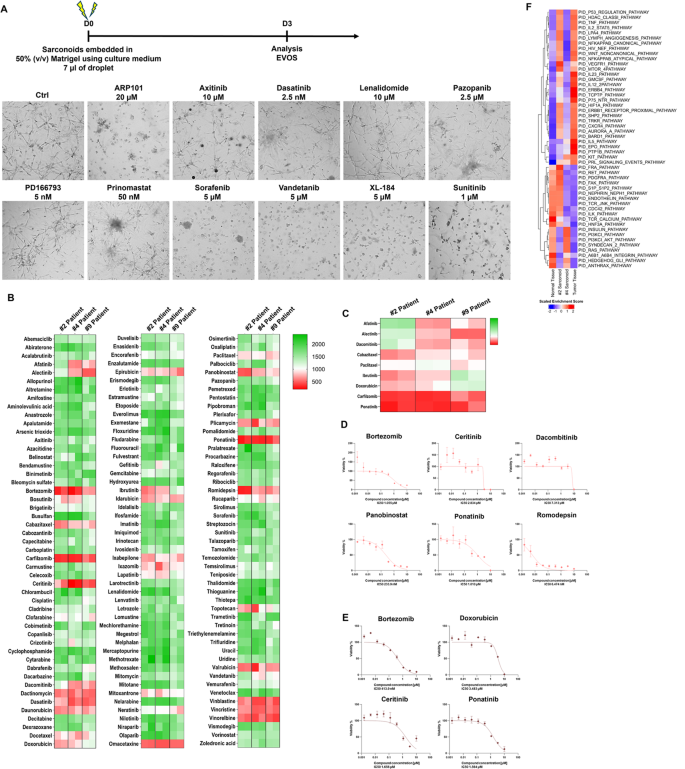
Visualization of high-throughput screening results for 147 FDA-approved compounds against patient-derived sarconoids. ( a ) Experimental design. Representative bright field images show the morphology of the patient #4-sarconoids after three days of treatment with the indicated compounds at different concentrations. ( b ) The 147 FDA-approved compounds were tested in patient #2-, #4- and #9-sarconoids. The percentiles for the obtained anti-proliferative values are depicted using a heat map. Low values (indicating resistance) are depicted in green, and high values (indicating sensitivity) in red. Compounds are ordered alphabetically. ( c ) Heat map of drug effects demonstrating heterogeneous drug responses between the patient #2-, #4-and #9-sarconoids. The columns indicate samples, and the rows indicate the tested drugs and nominal targets. ( d ) Representative drug response curves for bortezomib, ceritinib, dacombitinib, panobinostat, ponatinib, and romidepsin in patient #2-sarconoid. ( e ) Representative drug response curves for bortezomib, doxorubicin, ceritinib, and ponatinib in the patient #4-sarconoids. Normalized mean ± SEM ( n = 3) viability data from triplicate wells for each drug concentration are presented. ( f ) Sibling cultures from patients #2 and #4 display heterogeneous pathway activity. The HDAC pathway was specifically activated in only the patient #2-sarconoid tissue, which resulted in a better response to HDAC inhibitor compared to patient #4-sarconoids. Only patient #4-sarconoids showed an upregulation of the PI3K/Akt and RAS pathway, which underpinned their better response to the TKIs. The indicated color code represents scaled mRNA expression across the samples
Each sarconoid line exhibited unique phenotypic and genomic features, resulting in varied drug sensitivities. This underscores the importance of tailoring treatments to individual patients, which may help narrow down therapeutic options and optimize the treatment regimen for angiosarcoma.
Data availability
Any additional information required to reanalyze the data reported in this paper is available from the corresponding authors on reasonable request, [email protected].
Abbreviations
Food and drug administration
Quantitative real-time PCR
Human umbilical vein endothelial cells
RNA Sequencing
Gene ontology
Differentially expressed genes
Extracellular matrix
Uniform manifold approximation and projection
Protein C receptor
Epidermal growth factor receptor
Tyrosine kinase inhibitors
Histone deacetylases
High-throughput screening
Vlachogiannis G, Hedayat S, Vatsiou A, Jamin Y, Fernandez-Mateos J, Khan K, Lampis A, Eason K, Huntingford I, Burke R, et al. Patient-derived organoids model treatment response of metastatic gastrointestinal cancers. Science. 2018;359(6378):920–6.
Article CAS PubMed PubMed Central Google Scholar
Broutier L, Mastrogiovanni G, Verstegen MM, Francies HE, Gavarro LM, Bradshaw CR, Allen GE, Arnes-Benito R, Sidorova O, Gaspersz MP, et al. Human primary liver cancer-derived organoid cultures for disease modeling and drug screening. Nat Med. 2017;23(12):1424–35.
Eiraku M, Takata N, Ishibashi H, Kawada M, Sakakura E, Okuda S, Sekiguchi K, Adachi T, Sasai Y. Self-organizing optic-cup morphogenesis in three-dimensional culture. Nature. 2011;472(7341):51–6.
Article CAS PubMed Google Scholar
Takebe T, Wells JM. Organoids by design. Science. 2019;364(6444):956–9.
Zhang J, Gong H, Wang Y, Zhang G, Hou P. Angiosarcoma of the visceral organs: a morphological, immunohistochemical, and C-MYC status analysis. Pathol Res Pract. 2022;238:154118.
Painter CA, Jain E, Tomson BN, Dunphy M, Stoddard RE, Thomas BS, Damon AL, Shah S, Kim D, Gomez Tejeda Zanudo J, et al. The Angiosarcoma Project: enabling genomic and clinical discoveries in a rare cancer through patient-partnered research. Nat Med. 2020;26(2):181–7.
Weidema ME, Versleijen-Jonkers YMH, Flucke UE, Desar IME, van der Graaf WTA. Targeting angiosarcomas of the soft tissues: a challenging effort in a heterogeneous and rare disease. Crit Rev Oncol Hematol. 2019;138:120–31.
Burns J, Wilding CP, Krasny L, Zhu X, Chadha M, Tam YB, Ps H, Mahalingam AH, Lee ATJ, Arthur A, et al. The proteomic landscape of soft tissue sarcomas. Nat Commun. 2023;14(1):3834.
Yu QC, Song W, Wang D, Zeng YA. Identification of blood vascular endothelial stem cells by the expression of protein C receptor. Cell Res. 2016;26(10):1079–98.
Gur-Cohen S, Lapidot T. Vascular procr(+) stem cells: finding new branches while looking for the roots. Cell Res. 2016;26(10):1071–2.
Download references
Acknowledgements
We thank the study patients for agreeing to participate, as well as the study teams at Asan Medical Center, the High Throughput Screening (HTS) Core Lab, for their support with the drug screening analyses. We further thank the NCI Development Therapeutics Program (DTP) for providing the agents used in this study.
This work was supported by a National Research Foundation of Korea (NRF) (NRF-2022R1F1A1069608), and by the Ministry of Health & Welfare (HR21C0198), and by the Asan Institute for Life Sciences, Asan Medical Center (2021IP0026).
Author information
Authors and affiliations.
Biomedical Engineering Research Center, Asan Institute for Life Sciences, Seoul, South Korea
Da Jung Jung, Jae Hee Byeon & Gi Seok Jeong
Department of Covergence Medicine, College of Medicine, University of Ulsan, Seoul, South Korea
Gi Seok Jeong
Department of Plastic and Reconstructive Surgery, Asan Medical Center, Seoul, South Korea
Young Chul Kim, Woo Shik Jeong & Jong-Woo Choi
Department of Plastic and Reconstructive Surgery, College of Medicine, University of Ulsan, Seoul, South Korea
Jong-Woo Choi
Department of Biomedical Engineering, College of Medicine, University of Ulsan, Seoul, South Korea
You can also search for this author in PubMed Google Scholar
Contributions
D.J.J., G.S.J., and J.W.C. designed the study. D.J.J., J.H.B., Y.C.K., and W.S.J. contributed to data gathering and data analysis. D.J.J., J.H.B., Y.C.K., W.S.J., G.S.J., and J.W.C. interpreted the data. D.J.J., J.H.B., Y.C.K., and G.S.J. drafted the manuscript. All authors critically reviewed the manuscript and agreed to its submission for publication.
Corresponding authors
Correspondence to Jong-Woo Choi or Gi Seok Jeong .
Ethics declarations
Ethical approval.
for the study was granted by the Institutional Review Board of Asan Medical Center. Written informed consent was secured from all participating patients.
Conflict of interest
The authors declare no competing financial or other interests in relation to this study.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1
Supplementary material 2, supplementary material 3, supplementary material 4, rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Jung, D.J., Byeon, J.H., Kim, Y.C. et al. Generation of sarconoids from angiosarcoma patients as a systematic-based rational approach to treatment. J Hematol Oncol 17 , 35 (2024). https://doi.org/10.1186/s13045-024-01556-3
Download citation
Received : 15 February 2024
Accepted : 07 May 2024
Published : 20 May 2024
DOI : https://doi.org/10.1186/s13045-024-01556-3
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Angiosarcoma
- Translational research
- Drug screening platform
Journal of Hematology & Oncology
ISSN: 1756-8722
- General enquiries: [email protected]

COMMENTS
2. The Disagreement Gap. As the name suggests, the disagreement gap emerges when there are contrasting or contradictory findings in the existing research regarding a specific research question (or set of questions). The hypothetical example we looked at earlier regarding the causes of a disease reflects a disagreement gap.
Identifying practical gaps can lead to the development of strategies for the effective implementation of research findings in practice. Knowledge Gap. This type of research gap occurs when there is a lack of knowledge or information on a particular topic. It can happen when a new area of research is emerging, or when research is conducted in a ...
BACKGROUND. Well-defined, systematic, and transparent methods to identify health research gaps, needs, and priorities are vital to ensuring that available funds target areas with the greatest potential for impact. 1, 2 As defined in the literature, 3, 4 research gaps are defined as areas or topics in which the ability to draw a conclusion for a given question is prevented by insufficient evidence.
These are gaps in the data available on a particular subject. For example, there may be a need for more research to collect data on a specific population or to develop new measures to collect data on a particular construct. 5. Practical gaps. These are gaps in the application of research findings to practical situations.
The identification of gaps from systematic reviews is essential to the practice of "evidence-based research." Health care research should begin and end with a systematic review.1-3 A comprehensive and explicit consideration of the existing evidence is necessary for the identification and development of an unanswered and answerable question, for the design of a study most likely to answer ...
Research gaps prevent systematic reviewers from making conclusions and, ultimately, limit our ability to make informed health care decisions. While there are well-defined methods for conducting a systematic review, there has been no explicit process for the identification of research gaps from systematic reviews. In a prior project we developed a framework to facilitate the systematic ...
A research gap is a question or a problem that has not been answered by any of the existing studies or research within your field. Sometimes, a research gap exists when there is a concept or new idea that hasn't been studied at all. Sometimes you'll find a research gap if all the existing research is outdated and in need of new/updated research ...
The findings of this study highlight the critical importance of addressing research gaps in advancing knowledge and improving evidence-based practice, which can lead to significant advancements ...
An empirical gap is the type of gap that deals with gaps in the prior research. This conflict deals with the research findings or propositions need to be evaluated or empirically verified.
A research gap is identified by combining results and findings across several interrelated studies. 6 5. Consult: Seeking expert feedback will help you understand if the research gaps identified are adequate and feasible or if improvements are required.
This is a research gap. Research gaps are particularly useful for the advance of science, in general. Finding a research gap and having the means to develop a complete and sustained study on it can be very rewarding for the scientist (or team of scientists), not to mention how its new findings can positively impact our whole society. How to ...
A research gap or a literature gap refers to such unexplored or underexplored areas that have scope for further research. Why is it important to identify a unique research gap? Assume that you have completed your research work and published the findings only to find out that another researcher has already published something similar.
An essential aspect of reviewing the literature is to identify research gaps (Webster and Watson 2002). While reviews oug ht to be conducted rigorously (e.g., Fink 2010), there has been a lack of ...
Background Well-defined, systematic, and transparent processes to identify health research gaps, needs, and priorities are vital to ensuring that available funds target areas with the greatest potential for impact. Objective The purpose of this review is to characterize methods conducted or supported by research funding organizations to identify health research gaps, needs, or priorities ...
Identification of Research Gaps. "Topic or area for which missing or inadequate information limits the ability of reviewers to reach a conclusion for a given question.". Utility of an analytic framework illustrating the relationship of gaps to the key questions and analytic framework of the review. Stakeholders may identify gaps not ...
Key findings • We identified 12 different definitions of the term research gaps. We found seven specific methods for identifying research gaps involving secondary and primary research: quantitative survey, academic crowd-sourcing, needs assessment, knowledge synthesis, bibliometric study, priority setting, and global evidence-mapping methods.
Despite decades of research into why this gap remains, there is still a continuing and heated debate as to why it exists and how it could be resolved. ... allowing for the analysis of the various drivers and solutions for addressing the gap. The findings show that to resolve this gap is necessary to change our perspective of the gap and ...
For nearly two decades, the dominant model for evidence-based education (EBE) has focused on improving schools by researching "what works." Yet anyone familiar with EBE recognizes its relentless adversary: the gap between research and practice (Coburn & Stein, 2010; Farley-Ripple, May, Karpyn, Tilley, & McDonough, 2018; McIntyre, 2005; Nelson & Campbell, 2017; Tseng & Nutley, 2014).
Generalizable knowledge about how research findings should be applied in clinical practice, resulting from translational research, provides a jumpstart for local quality improvement efforts. The 21st Century Cures Act, proposed by Congress, is a more controversial approach to resolving the research to practice gap. 9 ...
ResGap. ResGap is an application that helps you identify research gaps quickly and easily, specifically it: Provides a quick and comprehensive overview of your research topic. Finds the most cited publications, authors, journals and refereed outlets in your research area. Visualises how topics in your area have evolved over time, showing topics ...
Publication bias is the selective publishing of certain research findings, such as significant or favourable results. ... S. R. et al. Evidence gaps and diversity among potential win-win ...
The findings were released on May 6 with the launch of the Segregation ... School segregation is strongly associated with achievement gaps between racial and ethnic groups, especially the rate at which achievement gaps widen during school, the researchers said. ... This research, including the development of the Segregation Explorer data and ...
Exploration of these gaps can reveal necessities regarding the work readiness of nursing graduates and help them develop their competencies to enter the clinical setting [1, 25]. Although research has been carried out on this topic in other countries, the educational system in those countries varies from that of Iran's nursing education [31 ...
In Africa, where the burden of diseases is disproportionately high, significant challenges arise from a shortage of skilled researchers, lack of research funding, and limited mentorship opportunities. The continent faces a substantial gap in research output largely attributed to the dearth of mentorship opportunities for early career researchers. We conducted this systematic review to explore ...
This process also supported the identification of a 'customer' after the review was completed, that is, a stakeholder who is keen on using the evidence review is likely to take action on its results and ready to translate the findings into clinical practice. The research to practice gap is substantial and the challenges of translating ...
Deloitte US | Audit, Consulting, Advisory, and Tax Services
The study findings reveal a gap between patient-reported outcomes and performance-based assessments in the context of medication management at home. ... There is a gap between what people think they will do, what they can do on a standardized assessment, and what they actually do at home. Future research is needed to strengthen concurrent and ...
Physical activity is known to be good for one's health.1 2 On the other hand, physical inactivity and sedentary behaviour are known to be harmful to health.2 3 Agreement exists about these general statements; however, emerging research points to a need to be more domain-specific as physical activity conducted during work may be harmful to health. Most physical activity research is based on ...
To bridge the gap between preclinical research and translational applications, we engineered angiosarcoma-derived organoids from surgically resected primary tumors, hereafter referred to as "sarconoids," as a proof-of-concept model. ... Our findings suggest that sarconoids can be reliably generated from angiosarcoma patient-derived tissues ...