Learn how UpToDate can help you.
Select the option that best describes you
- Medical Professional
- Resident, Fellow, or Student
- Hospital or Institution
- Group Practice
- Patient or Caregiver
- Find in topic

RELATED TOPICS
INTRODUCTION
This topic will provide an overview of major issues related to breech presentation, including choosing the best route for delivery. Techniques for breech delivery, with a focus on the technique for vaginal breech delivery, are discussed separately. (See "Delivery of the singleton fetus in breech presentation" .)
TYPES OF BREECH PRESENTATION
● Frank breech – Both hips are flexed and both knees are extended so that the feet are adjacent to the head ( figure 1 ); accounts for 50 to 70 percent of breech fetuses at term.
● Complete breech – Both hips and both knees are flexed ( figure 2 ); accounts for 5 to 10 percent of breech fetuses at term.

- Pregnancy Classes

Breech Births
In the last weeks of pregnancy, a baby usually moves so his or her head is positioned to come out of the vagina first during birth. This is called a vertex presentation. A breech presentation occurs when the baby’s buttocks, feet, or both are positioned to come out first during birth. This happens in 3–4% of full-term births.
What are the different types of breech birth presentations?
- Complete breech: Here, the buttocks are pointing downward with the legs folded at the knees and feet near the buttocks.
- Frank breech: In this position, the baby’s buttocks are aimed at the birth canal with its legs sticking straight up in front of his or her body and the feet near the head.
- Footling breech: In this position, one or both of the baby’s feet point downward and will deliver before the rest of the body.
What causes a breech presentation?
The causes of breech presentations are not fully understood. However, the data show that breech birth is more common when:
- You have been pregnant before
- In pregnancies of multiples
- When there is a history of premature delivery
- When the uterus has too much or too little amniotic fluid
- When there is an abnormally shaped uterus or a uterus with abnormal growths, such as fibroids
- The placenta covers all or part of the opening of the uterus placenta previa
How is a breech presentation diagnosed?
A few weeks prior to the due date, the health care provider will place her hands on the mother’s lower abdomen to locate the baby’s head, back, and buttocks. If it appears that the baby might be in a breech position, they can use ultrasound or pelvic exam to confirm the position. Special x-rays can also be used to determine the baby’s position and the size of the pelvis to determine if a vaginal delivery of a breech baby can be safely attempted.
Can a breech presentation mean something is wrong?
Even though most breech babies are born healthy, there is a slightly elevated risk for certain problems. Birth defects are slightly more common in breech babies and the defect might be the reason that the baby failed to move into the right position prior to delivery.
Can a breech presentation be changed?
It is preferable to try to turn a breech baby between the 32nd and 37th weeks of pregnancy . The methods of turning a baby will vary and the success rate for each method can also vary. It is best to discuss the options with the health care provider to see which method she recommends.
Medical Techniques
External Cephalic Version (EVC) is a non-surgical technique to move the baby in the uterus. In this procedure, a medication is given to help relax the uterus. There might also be the use of an ultrasound to determine the position of the baby, the location of the placenta and the amount of amniotic fluid in the uterus.
Gentle pushing on the lower abdomen can turn the baby into the head-down position. Throughout the external version the baby’s heartbeat will be closely monitored so that if a problem develops, the health care provider will immediately stop the procedure. ECV usually is done near a delivery room so if a problem occurs, a cesarean delivery can be performed quickly. The external version has a high success rate and can be considered if you have had a previous cesarean delivery.
ECV will not be tried if:
- You are carrying more than one fetus
- There are concerns about the health of the fetus
- You have certain abnormalities of the reproductive system
- The placenta is in the wrong place
- The placenta has come away from the wall of the uterus ( placental abruption )
Complications of EVC include:
- Prelabor rupture of membranes
- Changes in the fetus’s heart rate
- Placental abruption
- Preterm labor
Vaginal delivery versus cesarean for breech birth?
Most health care providers do not believe in attempting a vaginal delivery for a breech position. However, some will delay making a final decision until the woman is in labor. The following conditions are considered necessary in order to attempt a vaginal birth:
- The baby is full-term and in the frank breech presentation
- The baby does not show signs of distress while its heart rate is closely monitored.
- The process of labor is smooth and steady with the cervix widening as the baby descends.
- The health care provider estimates that the baby is not too big or the mother’s pelvis too narrow for the baby to pass safely through the birth canal.
- Anesthesia is available and a cesarean delivery possible on short notice
What are the risks and complications of a vaginal delivery?
In a breech birth, the baby’s head is the last part of its body to emerge making it more difficult to ease it through the birth canal. Sometimes forceps are used to guide the baby’s head out of the birth canal. Another potential problem is cord prolapse . In this situation the umbilical cord is squeezed as the baby moves toward the birth canal, thus slowing the baby’s supply of oxygen and blood. In a vaginal breech delivery, electronic fetal monitoring will be used to monitor the baby’s heartbeat throughout the course of labor. Cesarean delivery may be an option if signs develop that the baby may be in distress.
When is a cesarean delivery used with a breech presentation?
Most health care providers recommend a cesarean delivery for all babies in a breech position, especially babies that are premature. Since premature babies are small and more fragile, and because the head of a premature baby is relatively larger in proportion to its body, the baby is unlikely to stretch the cervix as much as a full-term baby. This means that there might be less room for the head to emerge.
Want to Know More?
- Creating Your Birth Plan
- Labor & Birth Terms to Know
- Cesarean Birth After Care
Compiled using information from the following sources:
- ACOG: If Your Baby is Breech
- William’s Obstetrics Twenty-Second Ed. Cunningham, F. Gary, et al, Ch. 24.
- Danforth’s Obstetrics and Gynecology Ninth Ed. Scott, James R., et al, Ch. 21.
BLOG CATEGORIES
- Can I get pregnant if… ? 3
- Child Adoption 19
- Fertility 54
- Pregnancy Loss 11
- Breastfeeding 29
- Changes In Your Body 5
- Cord Blood 4
- Genetic Disorders & Birth Defects 17
- Health & Nutrition 2
- Is it Safe While Pregnant 54
- Labor and Birth 65
- Multiple Births 10
- Planning and Preparing 24
- Pregnancy Complications 68
- Pregnancy Concerns 62
- Pregnancy Health and Wellness 149
- Pregnancy Products & Tests 8
- Pregnancy Supplements & Medications 14
- The First Year 41
- Week by Week Newsletter 40
- Your Developing Baby 16
- Options for Unplanned Pregnancy 18
- Paternity Tests 2
- Pregnancy Symptoms 5
- Prenatal Testing 16
- The Bumpy Truth Blog 7
- Uncategorized 4
- Abstinence 3
- Birth Control Pills, Patches & Devices 21
- Women's Health 34
- Thank You for Your Donation
- Unplanned Pregnancy
- Getting Pregnant
- Healthy Pregnancy
- Privacy Policy
Share this post:
Similar post.


Episiotomy: Advantages & Complications

Retained Placenta

What is Dilation in Pregnancy?
Track your baby’s development, subscribe to our week-by-week pregnancy newsletter.
- The Bumpy Truth Blog
- Fertility Products Resource Guide
Pregnancy Tools
- Ovulation Calendar
- Baby Names Directory
- Pregnancy Due Date Calculator
- Pregnancy Quiz
Pregnancy Journeys
- Partner With Us
- Corporate Sponsors
Planned caesarean section for term breech delivery
What is the issue?
Babies are usually born head first. If the baby is in another position the birth may be complicated. In a ‘breech presentation’ the unborn baby is bottom-down instead of head-down. Babies born bottom-first are more likely to be harmed during a normal (vaginal) birth than those born head-first. For instance, the baby might not get enough oxygen during the birth. Having a planned caesarean may reduce these problems. We looked at evidence comparing planned caesarean sections and vaginal births at the normal time of birth.
Why is this important?
Although having a caesarean might reduce some risks to babies who are lying bottom-first, the operation itself has other risks for the mother and the baby.
What evidence did we find?
We found 3 studies involving 2396 women. (We included studies up to March 2015.) The quality of the studies and therefore the strength of the evidence was mainly low. In the short term, births with a planned caesarean were safer for babies than vaginal births. Fewer babies died or were seriously hurt when they were born by caesarean. However, children who were born by caesarean had more health problems at age two, though the numbers were too small to be certain. Caesareans caused some short-term problems for mothers such as more abdominal pain. They also had some benefits, such as less urinary incontinence and less perineal pain in one study. The studies did not look at effects on future pregnancies, when having had a previous caesarean may cause complications. The studies only looked at single births (not twins or triplets) and did not study premature babies.
What does this mean? If your baby is in the breech position, it may be safer to have a planned caesarean section. However, caesareans may not be so good for the mother and may make future births less safe. We also do not yet know the effects of caesarean birth on babies’ health when they are older.
Planned caesarean section compared with planned vaginal birth reduced perinatal or neonatal death as well as the composite outcome death or serious neonatal morbidity, at the expense of somewhat increased maternal morbidity. In a subset with 2-year follow up, infant medical problems were increased following planned caesarean section and no difference in long-term neurodevelopmental delay or the outcome "death or neurodevelopmental delay" was found, though the numbers were too small to exclude the possibility of an important difference in either direction.
The benefits need to be weighed against factors such as the mother's preference for vaginal birth and risks such as future pregnancy complications in the woman's specific healthcare setting. The option of external cephalic version is dealt with in separate reviews. The data from this review cannot be generalised to settings where caesarean section is not readily available, or to methods of breech delivery that differ materially from the clinical delivery protocols used in the trials reviewed. The review will help to inform individualised decision-making regarding breech delivery. Research on strategies to improve the safety of breech delivery and to further investigate the possible association of caesarean section with infant medical problems is needed.
Poor outcomes after breech birth might be the result of underlying conditions causing breech presentation or due to factors associated with the delivery.
To assess the effects of planned caesarean section for singleton breech presentation at term on measures of pregnancy outcome.
We searched the Cochrane Pregnancy and Childbirth Group's Trials Register (31 March 2015).
Randomised trials comparing planned caesarean section for singleton breech presentation at term with planned vaginal birth.
Two review authors independently assessed trials for inclusion and risk of bias, extracted data and checked them for accuracy.
Three trials (2396 participants) were included in the review. Caesarean delivery occurred in 550/1227 (45%) of those women allocated to a vaginal delivery protocol and 1060/1169 (91%) of those women allocated to planned caesarean section (average risk ratio (RR) random-effects, 1.88, 95% confidence interval (CI) 1.60 to 2.20; three studies, 2396 women, evidence graded low quality ). Perinatal or neonatal death (excluding fatal anomalies) or severe neonatal morbidity was reduced with a policy of planned caesarean section in settings with a low national perinatal mortality rate (RR 0.07, 95% CI 0.02 to 0.29, one study, 1025 women, evidence graded moderate quality ), but not in settings with a high national perinatal mortality rate (RR 0.66, 95% CI 0.35 to 1.24, one study, 1053 women, evidence graded low quality ). The difference between subgroups was significant (Test for subgroup differences: Chi² = 8.01, df = 1 (P = 0.005), I² = 87.5%). Due to this significant heterogeneity, a random-effects analysis was performed. The average overall effect was not statistically significant (RR 0.23, 95% CI 0.02 to 2.44, one study, 2078 infants). Perinatal or neonatal death (excluding fatal anomalies) was reduced with planned caesarean section (RR 0.29, 95% CI 0.10 to 0.86, three studies, 2388 women). The proportional reductions were similar for countries with low and high national perinatal mortality rates.
The numbers studied were too small to satisfactorily address reductions in birth trauma and brachial plexus injury with planned caesarean section. Neither of these outcomes reached statistical significance (birth trauma: RR 0.42, 95% CI 0.16 to 1.10, one study, 2062 infants (20 events), evidence graded low quality ; brachial plexus injury: RR 0.35, 95% CI 0.08 to 1.47, three studies, 2375 infants (nine events)).
Planned caesarean section was associated with modestly increased short-term maternal morbidity (RR 1.29, 95% CI 1.03 to 1.61, three studies, 2396 women, low quality evidence ). At three months after delivery, women allocated to the planned caesarean section group reported less urinary incontinence (RR 0.62, 95% CI 0.41 to 0.93, one study, 1595 women); no difference in 'any pain' (RR 1.09, 95% CI 0.93 to 1.29, one study, 1593 women, low quality evidence ); more abdominal pain (RR 1.89, 95% CI 1.29 to 2.79, one study, 1593 women); and less perineal pain (RR 0.32, 95% CI 0.18 to 0.58, one study, 1593 women).
At two years, there were no differences in the combined outcome 'death or neurodevelopmental delay' (RR 1.09, 95% CI 0.52 to 2.30, one study, 920 children, evidence graded low quality ); more infants who had been allocated to planned caesarean delivery had medical problems at two years (RR 1.41, 95% CI 1.05 to 1.89, one study, 843 children). Maternal outcomes at two years were also similar. In countries with low perinatal mortality rates, the protocol of planned caesarean section was associated with lower healthcare costs, expressed in 2002 Canadian dollars (mean difference -$877.00, 95% CI -894.89 to -859.11, one study, 1027 women).
All of the trials included in this review had design limitations, and the GRADE level of evidence was mostly low. No studies attempted to blind the intervention, and the process of random allocation was suboptimal in two studies. Two of the three trials had serious design limitations, however these studies contributed to fewer outcomes than the large multi-centre trial with lower risk of bias.
Indications for caesarean section in breech presentation
Affiliation.
- 1 Department of Obstetrics and Gynecology, University of Limburg, Academic Hospital Maastricht, The Netherlands.
- PMID: 9720829
- DOI: 10.1016/s0301-2115(98)00065-7
Objective: The study was conducted because of the still considerable controversies about the variation in obstetric management in breech presentation, in combination with the still increasing caesarean section rate for this type of presentation, as well as doubt concerning the assumed improvement in neonatal and maternal morbidity and mortality obtained by increasing section rate in breeches.
Study design: Two hundred and sixty eight consecutive breech presentations in two university hospitals were studied longitudinally and prospectively. In principle, vaginal delivery was attempted in all cases, under expert supervision and electronic monitoring, except in the presence of clear-cut contraindications. X-ray pelvimetry was not used.
Results: The incidence of caesarean section was 34%. The trial of vaginal delivery succeeded in 64% of the nulliparas and in 60% of the non-frank breeches, without statistically significant differences in outcome measures compared with the multiparous women and the frank group, respectively. Hyperextension of the foetal head rarely occurred.
Conclusion: Several classic obstetric factors have a lower discriminating value for the route of delivery than is currently assumed. Progress of labour was an important factor in determining the route of delivery.
- Birth Weight
- Breech Presentation*
- Cesarean Section*
- Infant, Newborn
- Longitudinal Studies
- Prospective Studies
- MSD careers
Birth Injuries in Newborns
- Head Injuries During Birth |
- Injuries to the Skin and Soft Tissues |
- Bleeding In and Around the Brain |
- Nerve Injuries |
- Bone Injuries |
Birth injury is harm that can happen to a baby during the birthing process, usually in the process of passing through the birth canal.
Many newborns have swelling or minor bruising as a result of the birthing process.
Most injuries resolve without treatment.
Infrequently, more serious injuries occur, such as damage to nerves or a broken bone.
Birth injuries are most commonly due to the natural forces of labor and delivery.
Injuries are more likely to occur during a difficult delivery, which may occur because of fetal size, fetal position, forceps or vacuum-assisted delivery, or other factors.
A very large baby is at increased risk of birth injury. Doctors recommend cesarean delivery (C-section) when they estimate the baby weighs more than 11 pounds (more than 10 pounds when the mother has diabetes).
Injury is also more likely when the fetus is lying in an unusual position in the uterus before birth (see figure Position and Presentation of the Fetus ).
In some deliveries, doctors use forceps (a surgical instrument with rounded edges that fit around the fetus's head) or a vacuum extractor device. When used appropriately, there is a low risk of injury with these delivery methods.
Overall, the rate of birth injuries is much lower now than in previous decades because of improved prenatal assessment with ultrasonography , the limited use of forceps, and because doctors often do a C-section if they foresee an increased risk of birth injury.
(See also Overview of General Problems in Newborns .)
Position and Presentation of the Fetus
Head injuries during birth.
Head molding is not an injury, but parents may be concerned about it. Molding refers to the normal change in shape of the baby's head that results from pressure on the head during delivery. In most births, the head is the first part to enter the birth canal. Because a fetus's skull bones are not rigidly fixed in position, the head elongates as it is pushed through the birth canal, which allows the fetus to pass through more easily. Molding does not affect the brain and does not cause problems or require treatment. The head shape gradually becomes more rounded over several days.
Minor head injury is the most common birth-related injury. Swelling and bruising of the scalp is common but not serious and generally resolves within a few days. Scalp scratches can occur when instruments (such as fetal monitors that attach to the scalp, forceps, or vacuum extractors ) are used during a vaginal delivery.
Bleeding between the scalp and skull bones can lead to an accumulation of blood either above or below the thick fibrous layer (periosteum) that covers the skull bones.
A cephalohematoma is blood accumulation between the scalp and the periosteum. Cephalohematomas feel soft and can increase in size after birth. They disappear on their own over weeks to months and almost never require any treatment. However, they should be evaluated by a pediatrician if they become red or start to drain liquid. Occasionally some of the blood hardens (calcifies) and leaves a hard lump in the scalp. Rarely, the calcified lump needs to be removed surgically.
A subgaleal hemorrhage is an accumulation of blood between the periosteum and the skull bones. Blood in this area can spread and is not confined to one area like a cephalohematoma. It can cause significant blood loss and shock , which may require a blood transfusion . A subgaleal hemorrhage may result from the use of forceps or a vacuum extractor, or may result from a blood clotting problem .
Fracture of one of the bones of the skull may occur before or during the birth process. Skull fractures are not common. Unless the skull fracture forms an indentation (depressed fracture), it generally heals rapidly without treatment.
Did You Know...
Injuries to the skin and soft tissues.
The newborn’s skin may have minor injuries after delivery, especially to the scalp, but also to other areas that receive pressure during contractions or that first emerge from the birth canal during delivery. Instruments needed for delivery, such as forceps , can injure the skin. Swelling and bruising may occur around the eyes and on the face during face-first deliveries and on the genitals after breech deliveries (see Fetal Presentation, Position, and Lie (Including Breech Presentation) ). No treatment for these injuries is needed.
Use of instruments during delivery and stress on the newborn (such as caused by birth asphyxia ) can injure the fat under the skin (called subcutaneous fat necrosis of the newborn). This skin injury can look like red, firm, raised areas on the trunk, arms, thighs, or buttocks. This type of injury usually resolves on its own over weeks to months.
Bleeding In and Around the Brain
Bleeding in and around the brain (intracranial hemorrhage) is caused by the rupture of blood vessels and may be caused by
Birth injury
Significant illness in the newborn that decreases delivery of blood or oxygen to the brain
A blood clotting problem
Prematurity increases the risk of intracranial hemorrhage.
Sometimes, intracranial hemorrhage occurs after a normal delivery in an otherwise well newborn. The cause of bleeding in these cases is unknown.
Bleeding in the brain is much more common among very preterm infants. Newborns who have bleeding disorders (such as hemophilia ) are also at increased risk of bleeding in the brain.
Most infants with bleeding do not have symptoms. However, some infants may have severe symptoms and be sluggish (lethargic), feed poorly, and/or have seizures.
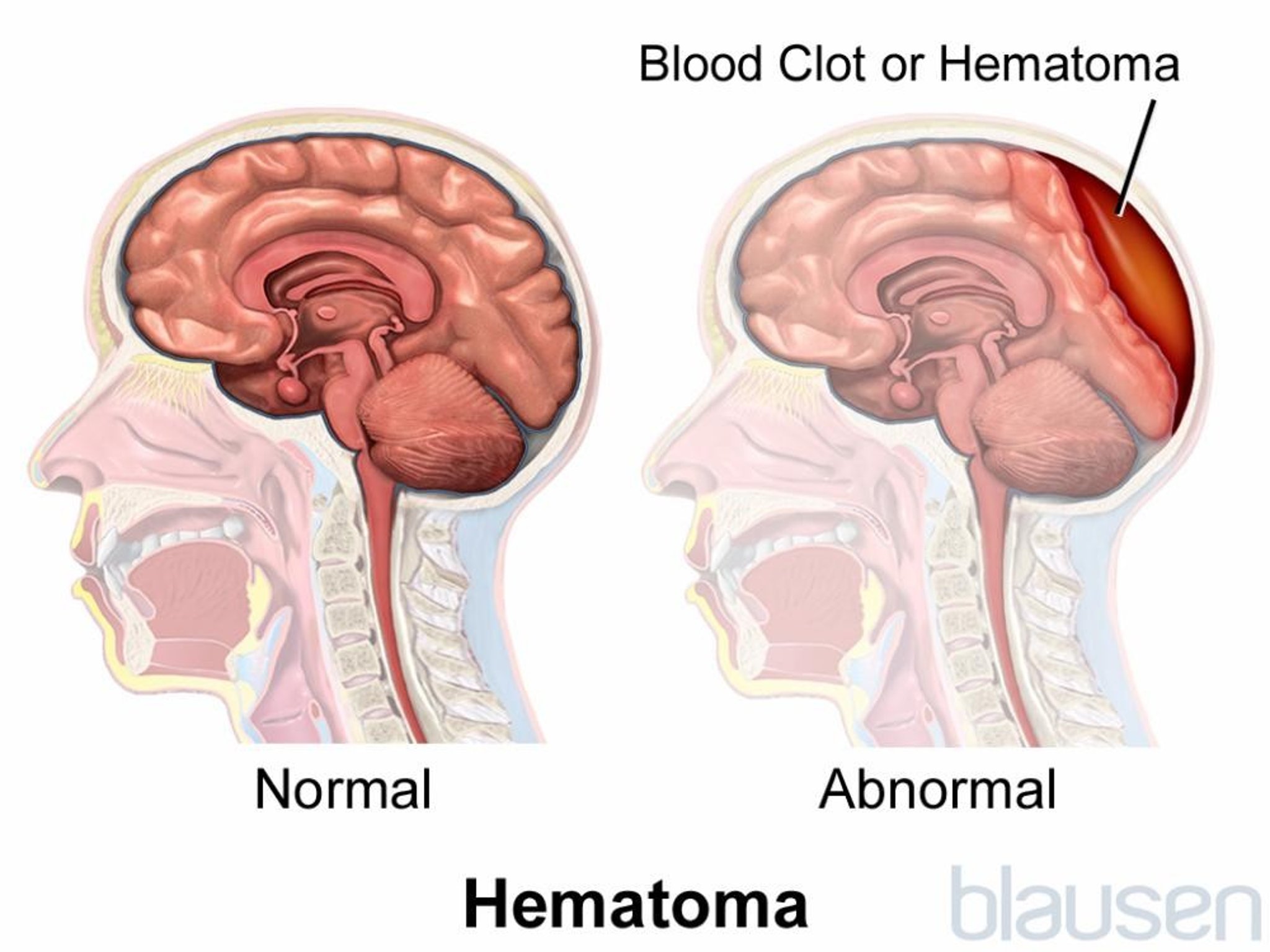
Bleeding can occur in several places in and around the brain:
Subarachnoid hemorrhage is bleeding below the innermost of the two membranes that cover the brain. This is the most common type of intracranial hemorrhage in newborns, usually occurring in full-term newborns. Newborns with a subarachnoid hemorrhage may occasionally have apnea (periods when they stop breathing), seizures , or lethargy during the first 2 to 3 days of life but usually ultimately do well.
Subdural hemorrhage is bleeding between the outer and the inner layers of the brain covering. It is now much less common because of improved childbirth techniques. A subdural hemorrhage can put increased pressure on the surface of the brain. Newborns with a subdural hemorrhage may develop problems such as seizures.
Epidural hematoma is bleeding between the outer layer (dura mater) of tissue covering the brain (meninges) and the skull. An epidural hematoma may be caused by a skull fracture. If the hematoma increases the pressure in the brain, the soft spots between skull bones (fontanelles) may bulge. Newborns with an epidural hematoma may have apnea or seizures.
Intraventricular hemorrhage is bleeding into the normal fluid-filled spaces (ventricles) in the brain.
Intraparenchymal hemorrhage occurs into the brain tissue itself.
Intraventricular hemorrhages and intraparenchymal hemorrhages usually occur in very preterm newborns and occur more typically as a result of an underdeveloped brain rather than a birth injury. Most of these hemorrhages do not cause symptoms, but large ones may cause apnea or a bluish gray discoloration to the skin, or the newborn's entire body may suddenly stop functioning normally. Newborns who have a large hemorrhage, especially one that extends into the parenchyma, have a poor prognosis, but those with small hemorrhages usually survive and do well.
Newborns who have a hemorrhage may be admitted to a neonatal intensive care unit (NICU) for imaging tests (such as a CT scan or MRI) and monitoring, supportive care (such as warmth), fluids given by vein (intravenously), and other treatments to maintain body function.
Nerve Injuries
Nerve injuries may occur before or during delivery. These injuries usually cause weakness of the muscles controlled by the affected nerve. Nerve injuries may involve the
Facial nerve: Lopsided facial expression
Brachial plexus: Arm and/or hand weakness
Phrenic nerve (rare): Difficulty breathing
Spinal cord (rare): Paralysis
Other nerves, such as the radial nerve in the arm, the sciatic nerve in the lower back, or the obturator nerve in the leg, also may be injured during delivery. Most children completely recover from these injuries.
Facial nerve injury
Facial nerve injury is evident when the newborn cries and the face appears lopsided (asymmetric). The facial nerve is the nerve injured most often. This injury is caused by pressure against the nerve due to
The way the fetus was positioned in the uterus before birth
The nerve being pressed against the mother's pelvis during delivery
Forceps used to assist the delivery
No treatment of facial nerve injury is needed, and the muscle weakness usually resolves by 2 to 3 months of age. However, sometimes facial nerve weakness is caused by a congenital disorder rather than an injury and does not resolve.
Brachial plexus injury
The brachial plexus is a group of large nerves located between the neck and shoulder, leading to each arm. During a difficult delivery, one or both of the baby's arms can be stretched and injure the nerves of the brachial plexus (see Plexus Disorders ) and cause weakness or paralysis of part or all of the baby's arm and hand. Weakness of the shoulder and elbow is called Erb palsy, and weakness of the hand and wrist is called Klumpke palsy.
About half of the cases of brachial plexus injuries are related to difficult deliveries, typically involving large babies, and about half occur in babies with no difficulties during delivery. Brachial plexus injury is less frequent in babies delivered by cesarean delivery (C-section).
Extreme movements at the shoulder should be avoided to allow the nerves to heal. Many milder injuries resolve over a few days. If the injury is more severe or lasts for more than 1 or 2 weeks, physical therapy or occupational therapy for proper positioning and gentle movement of the arm are recommended. If there is no improvement over 1 or 2 months, doctors typically recommend the baby be evaluated by a pediatric neurologist and/or orthopedist at a pediatric specialty hospital to see whether surgery may be beneficial.

Phrenic nerve injury
The phrenic nerve, which is the nerve going to the diaphragm (the muscular wall that separates the organs of the chest from those of the abdomen and assists in breathing), is occasionally damaged, resulting in paralysis of the diaphragm on the same side.
In this injury, the newborn may have difficulty breathing and sometimes requires assistance with breathing.
Injury of the phrenic nerve usually resolves completely within a few weeks.
Spinal cord injury
Spinal cord injuries due to overstretching during delivery are extremely rare (see also Spinal Cord Injury in Children ). These injuries can result in paralysis below the site of the injury. Damage to the spinal cord is often permanent.
Some spinal cord injuries that occur high up in the neck are fatal because they prevent the newborn from breathing properly.
Bone Injuries
Bones may be broken (fractured) before or during delivery even when the delivery is normal.
A fracture of the collarbone (clavicle) is relatively common, occurring in 1 to 2% of newborns. Sometimes these fractures are not recognized until several days after birth when a lump of tissue forms around the fracture. Newborns with clavicle fractures are sometimes irritable and may not move the arm on the affected side. These fractures do not require treatment. Healing is complete over a few weeks.
Fractures of the upper arm bone (humerus) or upper leg bone (femur) sometimes occur. Newborns may have pain with movement in the first few days. Doctors usually apply a loose splint to limit movement. These fractures usually heal well.
Fractures of multiple bones can occur in newborns with certain rare genetic conditions in which the bones are very fragile (for example, osteogenesis imperfecta ).

- Cookie Preferences

Copyright © 2024 Merck & Co., Inc., Rahway, NJ, USA and its affiliates. All rights reserved.

IMAGES
VIDEO
COMMENTS
A cesarean section in breech presentation involves more complicated procedures than a cesarean section in cephalic presentation because the former requires additional manipulations for guiding the presenting part of the fetus, liberation of the arms, and the after-coming head delivery. Therefore, a cesarean section in breech presentation is ...
Breech presentation is defined as a fetus in a longitudinal lie with the buttocks or feet closest to the cervix. This occurs in 3-4% of all deliveries. The percentage of breech deliveries decreases with advancing gestational age from 22-25% of births prior to 28 weeks' gestation to 7-15% of births at 32 weeks' gestation to 3-4% of births at term.
Between 1998 and 2002, 35,453 term infants were delivered. The cesarean delivery rate for breech presentation increased from 50% to 80% within 2 months of the trial's publication and remained elevated. The combined neonatal mortality rate decreased from 0.35% to 0.18%, and the incidence of reported birth trauma decreased from 0.29% to 0.08%.
Cesarean is performed for over 90 percent of breech presentations, and this rate has increased worldwide . However, even in institutions with a policy of routine cesarean birth for breech presentation, vaginal breech births occur because of situations such as patient preference, precipitous birth, out-of-hospital birth, and lethal fetal anomaly ...
The main types of breech presentation are: Frank breech - Both hips are flexed and both knees are extended so that the feet are adjacent to the head ( figure 1 ); accounts for 50 to 70 percent of breech fetuses at term. Complete breech - Both hips and both knees are flexed ( figure 2 ); accounts for 5 to 10 percent of breech fetuses at term.
1 INTRODUCTION. Approximately 3% of all infants are born in breech presentation with bottom first, sometimes a foot or knee is leading. 1-3 The risk of breech presentation is sometimes increased, for example, in malformations of the child or the uterus; however, most of the infants and mothers among breech deliveries are totally healthy. 4 Vaginal delivery in breech compared with cephalic ...
Labour with a preterm breech should be managed as with a term breech. C. Where there is head entrapment, incisions in the cervix (vaginal birth) or vertical uterine D incision extension (caesarean section) may be used, with or without tocolysis. Evidence concerning the management of preterm labour with a breech presentation is lacking.
Breech Presentation: A position in which the feet or buttocks of the fetus would appear first during birth. Cervix: The lower, narrow end of the uterus at the top of the vagina. Cesarean Delivery: Delivery of a fetus from the uterus through an incision made in the woman's abdomen. External Cephalic Version (ECV): A technique, ...
Observational, usually retrospective, series have consistently favoured elective caesarean birth over vaginal breech delivery. A meta-analysis of 27 studies examining term breech birth, 5 which included 258 953 births between 1993 and 2014, suggested that elective caesarean section was associated with a two- to five-fold reduction in perinatal mortality when compared with vaginal breech ...
A breech baby (breech birth or breech presentation) is when a baby's feet or buttocks are positioned to come out of your vagina first. This means its head is up toward your chest and its lower body is closest to your vagina. ... Performing a C-section when a baby is breech might be slightly more difficult, but obstetricians are usually familiar ...
Breech Births. In the last weeks of pregnancy, a baby usually moves so his or her head is positioned to come out of the vagina first during birth. This is called a vertex presentation. A breech presentation occurs when the baby's buttocks, feet, or both are positioned to come out first during birth. This happens in 3-4% of full-term births.
Breech presentation is common in about 15% of pregnancies at 29 to 32 weeks. ... Planned c-section for breech birth has been found to lower both perinatal and neonatal death rates, lower short ...
A cesarean section in breech presentation involves more complicated procedures than a cesarean section in ce-phalic presentation because the former requires addi-tional manipulations for guiding the presenting part of the fetus, liberation of the arms, and the after-coming Fig. 1 Selection of the skin incision line. In cases of cesarean section ...
In a 'breech presentation' the unborn baby is bottom-down instead of head-down. Babies born bottom-first are more likely to be harmed during a normal (vaginal) birth than those born head-first. For instance, the baby might not get enough oxygen during the birth. Having a planned caesarean may reduce these problems.
With a policy of routine caesarean section for breech presentation at term, in time, the clinical skills of vaginal breech delivery will be eroded, placing women who deliver vaginally at increased risk. ... Amankwah K, Cheng M, et al. Maternal outcomes at 2 years after planned cesarean section versus planned vaginal birth for breech ...
Cesarean section in breech or transverse presentation involves more complicated procedures than cesarean section in cephalic presentation because the former requires additional manipulations for guiding the presenting part of the fetus, liberation of the arms, and the after-coming head delivery; therefore, those cesarean sections are likely to be more invasive.
Material and methods: The population (P) was pregnant women with a child in breech presentation, from gestational week 34 +0. The intervention (I) was the intention to deliver by cesarean section, the comparison (C) was the intention to deliver vaginally.
Objective: The study was conducted because of the still considerable controversies about the variation in obstetric management in breech presentation, in combination with the still increasing caesarean section rate for this type of presentation, as well as doubt concerning the assumed improvement in neonatal and maternal morbidity and mortality obtained by increasing section rate in breeches.
As for the type of breech presentation, 68% of all frank breeches delivered vaginally and 32% underwent caesarean section. Of the non-frank breeches 60% delivered vaginally and 40% underwent caesarean section ( Table 2 ). In the birth weight category ≥2500 g, 71% of all frank breeches were delivered vaginally, as were 65% of all non-frank ...
Doctors recommend cesarean delivery (C-section) when they estimate the baby weighs more than 11 pounds (more than 10 pounds when the mother has diabetes). Injury is also more likely when the fetus is lying in an unusual position in the uterus before birth (see figure Position and Presentation of the Fetus).
Material and Methods. The population (P) was pregnant women with a child in breech presentation, from gestational week 34 +0.The intervention (I) was the intention to deliver by cesarean section, the comparison (C) was the intention to deliver vaginally.
Breech presentation delivery approach is a controversial issue in obstetrics. How to cope with breech delivery (vaginal or C-section) has been discussed to find the safest in terms of morbidity. The aim of this study was to assess the risks of foetal and maternal mortality and perinatal morbidity associated with vaginal delivery against ...