Hot Topics: Health Equity and Health Disparity
- Extending Your Research


Suggested Videos
Other Sites of Interest
- Health Equity: Why It Matters, and How To Take Action - RWJF Robert Wood Johnson Foundation
- Healthy People 2030: Social Determinants of Health Insights into issues that include: Economic Stability, Education Access and Quality, Health Care Access and Quality, Neighborhood and Built Environment, and Social and Community Context
- National Collaborating Centre for Aboriginal Health (NCCAH) Canada
- Office of Health Equity Part of the U.S. Health Resources and Services Administration
- State Health Disparities Legislation and Minority Health Issues Statistics & reports on racial & ethnic health disparities from the National Conference of State Legislatures
What's the Issue?

The goal of health equity is everybody having the same opportunity to improve their health.
A health disparity is a preventable difference between different groups of people in
Populations affected by health disparities contend with social, economic, and environmental disadvantages. For some groups of people, health disparities are also a legacy of discrimination, exclusion, and/or policy.
Image credits: Resized " scales " by Kristen Gee , available from Noun Project , licensed under CC BY . Resized & colored "Health Services" symbol by SEGD available from Healthcare Symbols "for use in your projects." Graphics modified by Nancy R. Curtis.
Some Places to Begin
- Beyond Health Care: The Role of Social Determinants in Promoting Health and Health Equity Kaiser Family Foundation issue brief, 2015
- Health Disparities: MedlinePlus
- Health Equity Boston Public Health Commission
- The Lalonde Report Officially, "A New Perspective on the Health of Canadians." Seminal document (1974) in health promotion. Proposed lifestyle & environment as factors affecting health.
- Let's Talk: Health Equity National Collaborating Centre for Determinants of Health, 2013 [Canada]
- Social Determinants of Health Canadian Medical Association
- Maine Public Health Data Reports - Health Disparities
Maine Health Access Foundation (MeHAF) data briefs & analyses include a statewide view of rural health, rural health profiles of each county, and more:
- Low-Income, Uninsured Mainers Face Substantial Challenges Getting Health Care
- Mental Health Status and Access to Health Care Services for Adults in Maine
Kaiser Family Foundation materials include:
- Disparities in Health and Health Care: Five Key Questions and Answers
- Eliminating Racial/Ethnic Disparities in Health Care: What are the Options?
- Health and Access to Care and Coverage for Lesbian, Gay, Bisexual, and Transgender (LGBT) Individuals in the U.S.
- Health and Health Care for American Indians and Alaska Natives (AIANs)
- Health and Health Care for Asian Americans, Native Hawaiians and other Pacific Islanders (NHOPIs) in the United States
- Health and Health Care for Blacks in the United States
- Health and Health Care for Hispanics in the United States
- Health Coverage of Immigrants
- Living in an Immigrant Family in America: How Fear and Toxic Stress are Affecting Daily Life, Well-Being, & Health
Other resources:
- The Association Between Income and Life Expectancy in the United States, 2001-2014 The Health Inequality Project, 2016
- Health Disparities and People with Disabilities American Association on Health and Disability, 2011
- A New Way to Talk About the Social Determinants of Health Robert Wood Johnson Foundation, 2010. Bridging the gap between academe & communities while minimizing political perspectives and agendas.
- Rural Health Disparities Rural Health Information Hub
- Colour Coded Health Care: The Impact of Race and Racism on Canadians’ Health
- Ensuring Equitable Access to Care: Strategies for Governments, Health System Planners, and the Medical Profession Canadian Medical Association Position Statement [2013?]
- Health Care in Canada: What Makes us Sick? Canadian Medical Association Town Hall Report, July 2013. Summarizes public discussions on social determinants of health. Lists recommendations for further action.
- Thirteen Public Interventions in Canada That Have Contributed to a Reduction in Health Inequalities National Collaborating Centre for Healthy Public Policy, 2010
Visualizing Health Equity: One Size Does Not Fit All Infographic [RWJF]

Visualizing Health Equity: One Size Does Not Fit All Infographic by RWJF on RWJF.org

- Next: Extending Your Research >>
- Last Updated: Dec 22, 2023 12:26 PM
- URL: https://libguides.library.umaine.edu/health-equity-disparity
5729 Fogler Library · University of Maine · Orono, ME 04469-5729 | (207) 581-1673
- U.S. Department of Health & Human Services

- Virtual Tour
- Staff Directory
- En Español
You are here
Ending structural racism, minority health and health disparities research, nih is committed to:.
1. Improving minority health and reducing health disparities.
2. Removing the barriers to advancing health disparities research.

Health disparities are preventable differences in health status and outcomes that adversely affect certain populations. Research on health disparities examines the influence of environment, social determinants, and other underlying mechanisms leading to differences in health outcomes. This multidisciplinary field of science also seeks to identify evidence-based approaches to reduce the unequal burdens of morbidity and mortality among disparity populations defined as racial/ethnic minority, low socio-economic status, rural, and sexual and gender minority populations in the United States.
At NIH, every Institute and Center (IC) supports research into the causes of and potential interventions for health disparities within their mission. However, the National Institute on Minority Health and Health Disparities (NIMHD) is the lead institute on research to improve minority health and reduce health disparities. NIH recognizes the need to increase the proportion of research on minority health and health disparities across the NIH ICs to address public health issues affecting all populations in the United States. Learn more about NIMHD’s efforts .
“Of the many factors that contribute to health disparities, structural racism lies at the center of many by perpetuating established social and health injustices.”
— Eliseo Pérez-Stable, M.D., Director, National Institute on Minority Health and Health Disparities

To address long-standing health disparities and promote health equity, efforts under UNITE will seek to improve transparency, accountability, and sustainability in support for research on minority health and health disparities.
Concrete actions to achieve this goal include:
- Support late-stage translation of multi-level, multi-factor interventions to reduce health disparities.
- Test innovative approaches to address structural racism and eliminate health disparities.
- Marshal adequate and measurable resources across NIH for scientific research that will produce significant reductions in health disparities and improve minority health.
- Develop infrastructure to coordinate/track NIH-wide minority health and health disparities research
- Examine minority health and health disparities research portfolios with NIH-wide stakeholders to aggregate and generate summary recommendations for addressing research and funding gaps.
- Review the scope of NIH intramural and extramural systems, methods, measures, and definitions used to track minority health and health disparity research to identify strengths and limitations of current systems and new models.
- Conduct an analysis of current investments in minority health and health disparity research by intramural and extramural stakeholders.
- Ensure a robust NIH enterprise-wide commitment to support the NIH Strategic Plan on Minority Health and Health Disparities focused on the effects of structural racism and discrimination on minority health and health disparities.
- Support research on behavioral, biological, and social determinants of health and structural racism and discrimination.
This page last reviewed on August 25, 2022
Connect with Us
- More Social Media from NIH

- Mission and Vision
- Scientific Advancement Plan
- Science Visioning
- Research Framework
- Minority Health and Health Disparities Definitions
- Organizational Structure
- Staff Directory
- About the Director
- Director’s Messages
- News Mentions
- Presentations
- Selected Publications
- Director's Laboratory
- Congressional Justification
- Congressional Testimony
- Legislative History
- NIH Minority Health and Health Disparities Strategic Plan 2021-2025
- Minority Health and Health Disparities: Definitions and Parameters
- NIH and HHS Commitment
- Foundation for Planning
- Structure of This Plan
- Strategic Plan Categories
- Summary of Categories and Goals
- Scientific Goals, Research Strategies, and Priority Areas
- Research-Sustaining Activities: Goals, Strategies, and Priority Areas
- Outreach, Collaboration, and Dissemination: Goals and Strategies
- Leap Forward Research Challenge
- Future Plans
- Research Interest Areas
- Research Centers
- Research Endowment
- Community Based Participatory Research Program (CBPR)
- SBIR/STTR: Small Business Innovation/Tech Transfer
- Solicited and Investigator-Initiated Research Project Grants
- Scientific Conferences
- Training and Career Development
- Loan Repayment Program (LRP)
- Data Management and Sharing
- Social and Behavioral Sciences
- Population and Community Health Sciences
- Epidemiology and Genetics
- Medical Research Scholars Program (MRSP)
- Coleman Research Innovation Award
- Health Disparities Interest Group
- Art Challenge
- Breathe Better Network
- Healthy Hearts Network
- DEBUT Challenge
- Healthy Mind Initiative
- Mental Health Essay Contest
- Science Day for Students at NIH
- Fuel Up to Play 60 en Español
- Brother, You're on My Mind
- Celebrating National Minority Health Month
- Reaching People in Multiple Languages
- Funding Strategy
- Active Funding Opportunities
- Expired Funding Opportunities
- Technical Assistance Webinars

- Community Health and Population Sciences
- Clinical and Health Services Research
- Integrative Biological and Behavioral Sciences
- Intramural Research Program
- Training and Diverse Workforce Development
- Inside NIMHD
- ScHARe HDPulse PhenX SDOH Toolkit Understanding Health Disparities For Research Applicants For Research Grantees Research and Training Programs Reports and Data Resources Health Information for the Public Science Education

- Publications
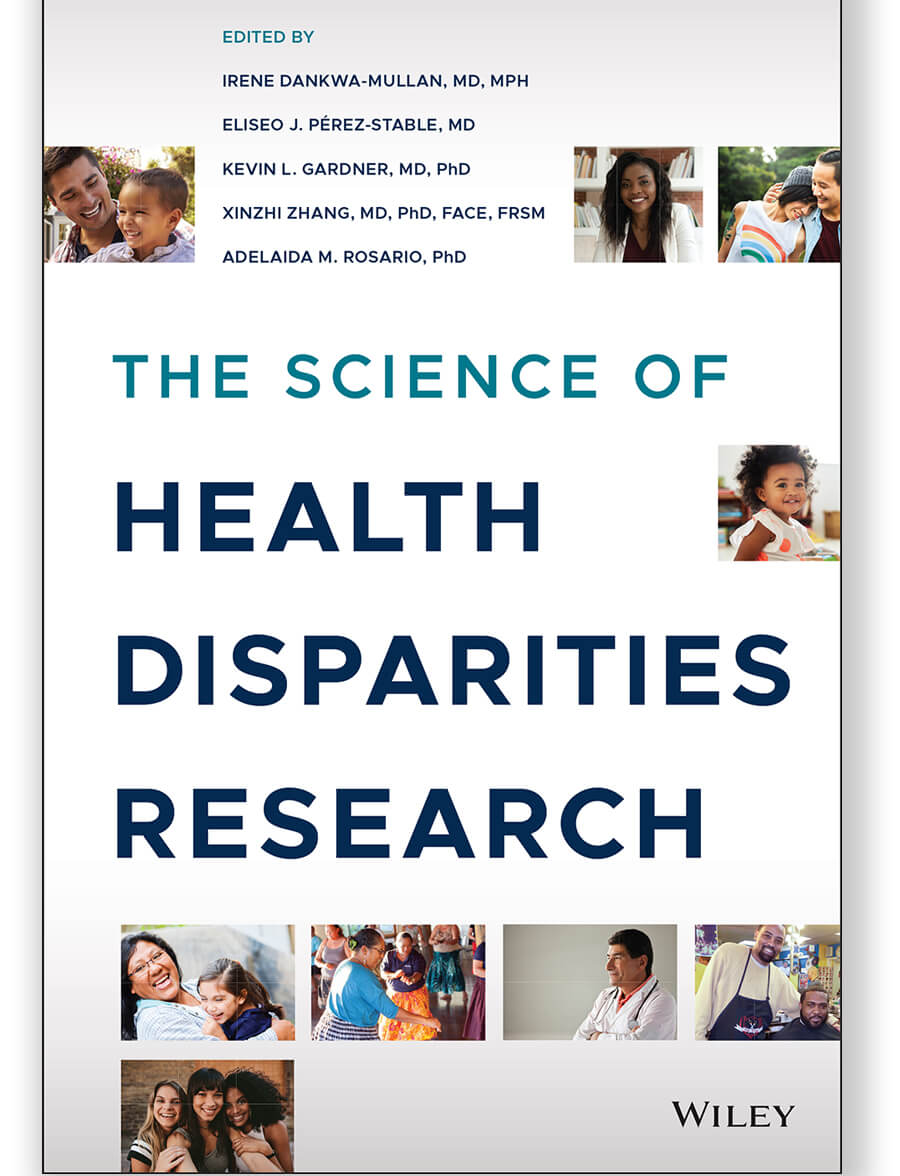
The Science of Health Disparities Research
- Director's Corner
- Legislative Information
- Strategic Plan
- NIMHD Celebrates Its 10 Year Anniversary
- Advisory Council
- Employment Opportunities
Over the years, research in minority health and health disparities has evolved from a descriptive understanding of what health disparities are and who is most affected, to the discovery of the complexity of factors involved in determining health and its outcomes by race/ethnicity and socioeconomic status. Scientific approaches to addressing these factors lead to:
- Improved understanding of mechanisms.
- More options to implement interventions to reduce disparities.
- Greater access to health care.
- A more equitable future.
The Science of Health Disparities Research is an in-depth volume for comprehensive information on conducting clinical and translational health disparities studies.
NIMHD researchers—along with leading experts from around the country—have written this 26-chapter textbook to cover the spectrum of health disparities research. This important new resource:
- Defines the field of health disparities science.
- Explains basic definitions, principles, and concepts for identifying, understanding, and addressing health disparities.
- Suggests new directions in scholarship and research.
- Discusses population health training, capacity building, and the transdisciplinary tools needed to advance health equity.
With contributions from more than 100 recognized scholars and leaders in the field, The Science of Health Disparities Research describes how using an interdisciplinary approach can reduce inequalities in population health studies, the importance of adding community engagement to the research process, and the ways that rigorous research can promote social justice. It also features examples from contemporary research studies, highlights conceptual models, and includes a broad range of scientific perspectives. The lifelong work of the scientists, clinicians, and community-based researchers and their contributions to the scientific literature on minority health and health disparities research provide a strong foundation for this text.
“The chapters contained herein illustrate the importance and feasibility of systematic, rigorous inquiry for understanding the specifics of minority health and health disparities. They also convey the importance of the lessons learned for science in general: for discovery, for generalizability, for advancing theory, for enhancing measurement, for improving investigative methods, for promoting attention to neglected areas of research, and for diversifying the scientific work workforce.”
-Spero M. Manson, Ph.D., Distinguished Professor of Public Health and Psychiatry at the University of Colorado School of Public Health
Intended Audience
This textbook is useful to a variety of audiences. Besides being an essential resource for trainees and clinical researchers in health services, behavioral science, population science, public health and basic science as it intersects with clinical studies, The Science of Health Disparities Research appeals to health care policy makers, epidemiologists, intervention scientists, and clinicians, particularly those working with minority, vulnerable, or underserved populations, health disparity scientists, community-based researchers, and research institutes.
Chapter Topics
- Definitions, Principles, and Concepts for Minority Health and Health Disparities Research
- Racial/Ethnic, Socioeconomic, and Other Social Determinants
- Applying Self‐report Measures in Minority Health and Health Disparities Research
- Applications of Big Data Science and Analytic Techniques for Health Disparities Research
- Healthcare and Public Policy: Challenges and Opportunities for Research
- Addressing Disparities in Access to High-quality Care
- Role of Electronic Health Records and Health Information Technology in Addressing Health Disparities
- Recruitment, Inclusion, and Diversity in Clinical Trials
- Workforce Diversity and Capacity Building to Address Health Disparities
For questions about the textbook, please email [email protected] .
Page updated Oct. 16, 2023

Staying Connected
- Funding Opportunities
- News & Events
- HHS Vulnerability Disclosure
- Privacy/Disclaimer/Accessibility Policy
- Viewers & Players
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
Special 07 April 2021
Highlighting Research on Health Disparities
A collection aimed at highlighting NPP articles and commentaries that address disparities related to gender, race, ethnicity, LGBTQ+ individuals, and early life adversity

Academic ethics of mental health: the national black postdocs framework for the addressment of support for undergraduate and graduate trainees
- Cellas A. Hayes
- Almarely L. Berrios-Negron
- Frankie D. Heyward
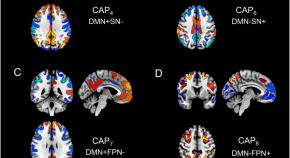
Sex-specific resting state brain network dynamics in patients with major depressive disorder
- Daifeng Dong
- Diego A. Pizzagalli
- Emily L. Belleau

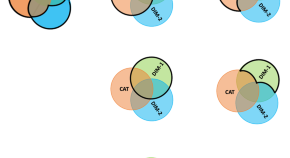
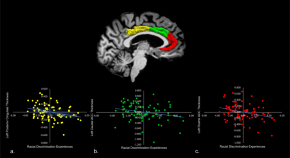
The effects of experience of discrimination and acculturation during pregnancy on the developing offspring brain
- Marisa N. Spann
- Kiarra Alleyne
- Dustin Scheinost

Digital and precision clinical trials: innovations for testing mental health medications, devices, and psychosocial treatments
- John Torous
- Patricia Arean
Associations between childhood ethnoracial minority density, cortical thickness, and social engagement among minority youth at clinical high-risk for psychosis
- Benson S. Ku
- Meghan Collins
- Elaine F. Walker
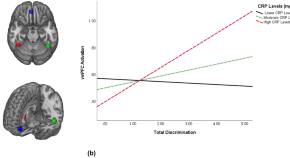
C-reactive protein moderates associations between racial discrimination and ventromedial prefrontal cortex activation during attention to threat in Black American women
- Aziz Elbasheir
- Jennifer C. Felger
Brain health in ethnically minority youth at risk for psychosis
- Rachel A. Rabin
- Lena Palaniyappan
Ensuring psychedelic treatments and research do not leave anyone behind
Psychedelics are a promising approach to caring for persons living with severe mental illness. However, as with all clinical treatments and research in the US, health equity concerns must be considered and addressed. Ensuring health equity and health justice in psychedelic care delivery and research will require strategies to not only reduce disparities and preempt future disparities among minoritized and marginalized populations.
- Melissa A. Simon
The biological embedding of structural inequities: new insight from neuroscience
- E. Kate Webb
- Nathaniel G. Harnett
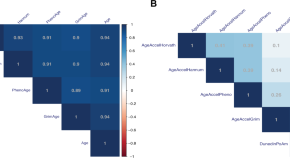
Transdiagnostic evaluation of epigenetic age acceleration and burden of psychiatric disorders
- Natan Yusupov
- Linda Dieckmann
- Elisabeth B. Binder
Ethical considerations in rapid and novel treatments in psychiatry
- Tobias Haeusermann
- Winston Chiong
Perspective on equitable translational studies and clinical support for an unbiased inclusion of the LGBTQIA2S+community
- Teddy G. Goetz
- Krisha Aghi
- Troy A. Roepke
To dismantle structural racism in science, scientists need to learn how it works
- Caleb Weinreb
- Daphne S. Sun
Five recommendations for using large-scale publicly available data to advance health among American Indian peoples: the Adolescent Brain and Cognitive Development (ABCD) Study SM as an illustrative case
- Evan J. White
- Mara J. Demuth
- Robin Aupperle
Deconstructing dissociation: a triple network model of trauma-related dissociation and its subtypes
- Lauren A. M. Lebois
- Poornima Kumar
- Milissa L. Kaufman
Building an intentional and impactful summer research experience to increase diversity in mental health research
- Oluwarotimi O. Folorunso
- Karen Burns White
- Elena H. Chartoff
Sex-dependent risk factors for PTSD: a prospective structural MRI study
- Alyssa R. Roeckner
- Shivangi Sogani
- Jennifer S. Stevens
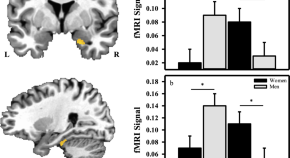
Sex-related differences in violence exposure, neural reactivity to threat, and mental health
- Heather E. Dark
- David C. Knight
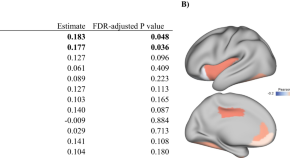
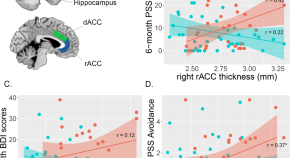
Racial discrimination associates with lower cingulate cortex thickness in trauma-exposed black women
- Leyla Eghbalzad
- Bekh Bradley

The role of racial discrimination in dissociation and interoceptive dysfunction
- Sahib S. Khalsa
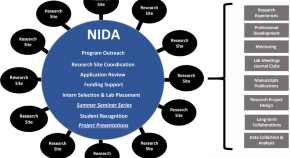
The National Institute on Drug Abuse Summer Research Internship Program: Building a Diverse National Scientific Workforce
- Albert H. Avila
- Jason H. Weixelbaum
- Wilson M. Compton
It’s about racism, not race: a call to purge oppressive practices from neuropsychiatry and scientific discovery
- Sierra E. Carter
- Yara Mekawi
Cross-ancestry genomic research: time to close the gap
- Elizabeth G. Atkinson
- Sevim B. Bianchi
- Sandra Sanchez-Roige
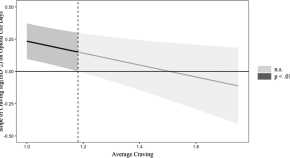
Intra-individual variability and stability of affect and craving among individuals receiving medication treatment for opioid use disorder
- Jennifer D. Ellis
- Chung Jung Mun
- Kenzie L. Preston
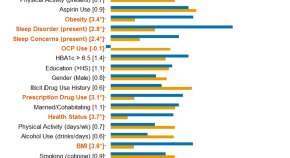
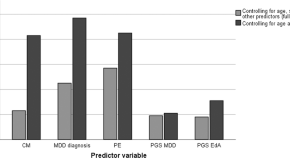
Does the moderator matter? Identification of multiple moderators of the association between peripheral inflammatory markers and depression severity in a large racially diverse community cohort
- Manivel Rengasamy
- Sophia Arruda Da Costa E Silva
- Rebecca B. Price

Altered reward and effort processing in children with maltreatment experience: a potential indicator of mental health vulnerability
- Diana J. N. Armbruster-Genç
- Vincent Valton
- Eamon McCrory
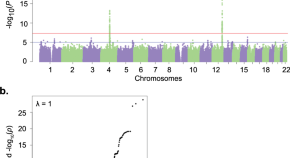
Genome-wide meta-analysis of alcohol use disorder in East Asians
- Rasmon Kalayasiri
- Joel Gelernter
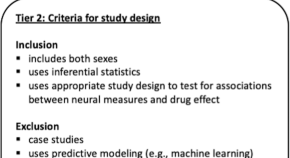
Evaluating the evidence for sex differences: a scoping review of human neuroimaging in psychopharmacology research
- Korrina A. Duffy
- C. Neill Epperson
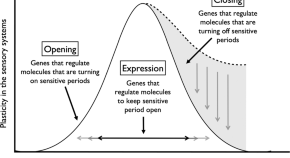
Sensitive period-regulating genetic pathways and exposure to adversity shape risk for depression
- Min-Jung Wang
- Erin C. Dunn
A three-factor model of common early onset psychiatric disorders: temperament, adversity, and dopamine
- Maisha Iqbal
- Sylvia Maria Leonarda Cox
- Marco Leyton
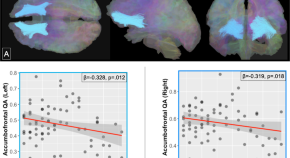
Accumbofrontal tract integrity is related to early life adversity and feedback learning
- Bryan V. Kennedy
- Jamie L. Hanson
- Seth D. Pollak
Brain sex differences: the androgynous brain is advantageous for mental health and well-being
- Barbara J. Sahakian

Transcriptome-wide association study of post-trauma symptom trajectories identified GRIN3B as a potential biomarker for PTSD development
- Adriana Lori
- Katharina Schultebraucks
- Kerry J. Ressler
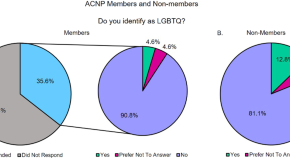
Being counted: LGBTQ+ representation within the American College of Neuropsychopharmacology (ACNP)
- Hayley Fisher
NIH research funding disparities affect diversity, equity and inclusion goals of the ACNP
- Michael A. Taffe
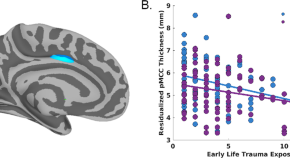
Distinct cortical thickness correlates of early life trauma exposure and posttraumatic stress disorder are shared among adolescent and adult females with interpersonal violence exposure
- Marisa C. Ross
- Anneliis S. Sartin-Tarm
- Josh M. Cisler
Inaction speaks louder than words: tips for increasing black ACNP membership
- Carl L. Hart
- Jean Lud Cadet
Intergenerational trauma is associated with expression alterations in glucocorticoid- and immune-related genes
- Nikolaos P. Daskalakis
- Changxin Xu
- Rachel Yehuda
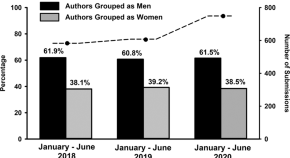
Effects of the COVID-19 pandemic on gender representation among corresponding authors of Neuropsychopharmacology (NPP) manuscripts: submissions during January–June, 2020
- Chloe J. Jordan
- William A. Carlezon Jr.
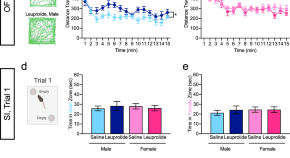
Behavioral and neurobiological effects of GnRH agonist treatment in mice—potential implications for puberty suppression in transgender individuals
- Christoph Anacker
- Ezra Sydnor
- Christine A. Denny
Childhood maltreatment and cognitive functioning: the role of depression, parental education, and polygenic predisposition
- Janik Goltermann
- Ronny Redlich
- Udo Dannlowski
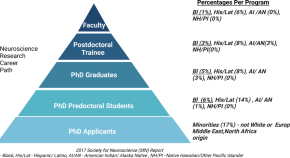
Advancing equity, diversity, and inclusion in the American College of Neuropsychopharmacology (ACNP): advances, challenges, and opportunities to accelerate progress
It is increasingly accepted that higher levels of excellence and innovation in research can be achieved by organizations that promote equity, diversity, and inclusion across several domains including ethnicity and gender. The purpose of this commentary is to provide an overview of the methods used to increase diversity within ACNP, as well as recommendations for accelerating progress. Annual membership surveys confirm increases in female membership and leadership positions, slower but encouraging signals for “Asian” and “Hispanic” members, and less progress for African American and other ethnic populations. Meetings have become visibly more diverse, due in part to ethnic minority travel awards and apparently increasing diversity among guest attendees. Evidence of increasing inclusion includes well-attended networking events and minority-relevant programming, active communications about diversity-related events and resources, and strong statements by ACNP leadership that embrace diversity as a core value and support collaboration among key committees and task forces to identify and implement pro-inclusion and diversity-enhancing efforts. We believe ACNP can accelerate progress with more scientifically valid approaches to assessing diversity and inclusion. The current membership survey includes five outmoded ethnic options and postmeeting surveys that are not designed to assess inclusion efforts and consequences. Measures should be developed that better characterize diversity and assess efforts to reduce the barriers that exist for potential non-White populations (e.g., annual membership and meeting attendance costs). Increased collaboration with NIH and other organizations that are committed to these same goals may also contribute to acceleration of progress by ACNP and other scientific organizations.
- Jack E. Henningfield
- Sherecce Fields
- Carlos A. Zarate
Impact of ADCYAP1R1 genotype on longitudinal fear conditioning in children: interaction with trauma and sex
- Tanja Jovanovic
- Anaïs F. Stenson
NPP statement on racism, discrimination, and abuse of power
- on Behalf of the NPP Team
The ABCD study: understanding the development of risk for mental and physical health outcomes
- Nicole R. Karcher
- Deanna M. Barch
Evaluating the impact of trauma and PTSD on epigenetic prediction of lifespan and neural integrity
- Seyma Katrinli
- Jennifer Stevens
- Alicia K. Smith
Neurobiological consequences of racial disparities and environmental risks: a critical gap in understanding psychiatric disorders
Associations between different dimensions of prenatal distress, neonatal hippocampal connectivity, and infant memory
- Catherine Monk
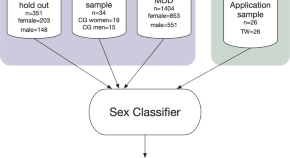
Biological sex classification with structural MRI data shows increased misclassification in transgender women
- Claas Flint
- Katharina Förster
- Dominik Grotegerd
Polygenic scores for psychiatric disorders in a diverse postmortem brain tissue cohort
- Laramie Duncan
- Hanyang Shen
- Stefano Marenco
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- J Womens Health (Larchmt)
Health Equity Among Black Women in the United States
Juanita j. chinn.
1 Population Dynamics Branch, Division of Extramural Research, Eunice Kennedy Shriver National Institute of Child Health and Human Development, Bethesda, Maryland, USA.
Iman K. Martin
2 Blood Epidemiology and Clinical Therapeutics Branch, Division of Blood Diseases and Resources, National Heart, Lung, and Blood Institute, Bethesda, Maryland, USA.
Nicole Redmond
3 Clinical Applications and Prevention Branch, Division of Cardiovascular Sciences, National Heart, Lung, and Blood Institute, Bethesda, Maryland, USA.
Black women in the United States have experienced substantial improvements in health during the last century, yet health disparities persist. These health disparities are in large part a reflection of the inequalities experienced by Black women on a host of social and economic measures. In this paper, we examine the structural contributors to social and economic conditions that create the landscape for persistent health inequities among Black women. Demographic measures related to the health status and health (in)equity of Black women are reviewed. Current rates of specific physical and mental health outcomes are examined in more depth, including maternal mortality and chronic conditions associated with maternal morbidity. We conclude by highlighting the necessity of social and economic equity among Black women for health equity to be achieved.
Black women in the United States experienced substantial improvements in health during the last century, yet health disparities persist. Black women continue to experience excess mortality relative to other U.S. women, including—despite overall improvements among Black women—shorter life expectancies 1 and higher rates of maternal mortality. 2 Moreover, Black women are disproportionately burdened by chronic conditions, such as anemia, cardiovascular disease (CVD), and obesity. Health outcomes do not occur independent of the social conditions in which they exist. The higher burden of these chronic conditions reflects the structural inequities within and outside the health system that Black women experience throughout the life course and contributes to the current crisis of maternal morbidity and mortality. The health inequities experienced by Black women are not merely a cross section of time or the result of a singular incident.
Historical Context for the Current Health Experience of Black Women
Race and ethnicity are sociocultural constructs that reflect common geographic origins, cultures, and social histories of groups that are defined by societies in time-dependent contexts. 3–6 Given the social construction of race and ethnicity, racial groups and identity are fluid; they can, and do, change over time and vary across place. 7
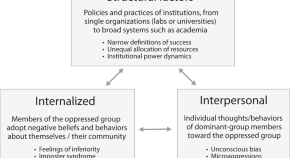
No discussion of health equity among Black women is complete unless it considers the impacts of institutional- and individual-level forms of racism and discrimination against Black people. Nor is a review of health equity among Black women complete without an understanding of the intersectionality of gender and race and the historical contexts that have accumulated to influence Black women's health in the United States.
Research consistently has documented the continued impacts of systematic oppression, bias, and unequal treatment of Black women, 5 , 8 , 9 Substantial evidence exists that racial differences in socioeconomic ( e.g. , education and employment) and housing outcomes among women are the result of segregation, discrimination, and historical laws purposed to oppress Blacks and women in the United States.
Black women earn on average $5,500 less per year and experience higher unemployment and poverty rates than the U.S. average for women ( Table 1 ). 10 Moreover, Black women are more likely to be the head of household than their White counterparts, effectively supporting more dependents with fewer resources. 10 Black women live in neighborhoods that are more racially segregated and have lower property values than their White counterparts. 10 , 11 Mortgage lending discrimination (“redlining”), a legal practice in which lenders deny mortgage loans to communities and individuals based on race, resulted in community disinvestment residential segregation. 11 Residential segregation, as Williams and Collins argued, 12 is a fundamental cause of racial disparities in health, operating through many social institutions (including labor markets and education) to affect health.
Descriptive Demographic Statistics for Black Women in the United States, 2018
Data are collected by sex (female).
Data source: https://blackdemographics.com/population/black-women-statistics 10
The intersectionality of gender and race and its impact on the health of Black women also is important. This intersection of race and gender for Black women is more than the sum of being Black or being a woman: It is the synergy of the two. Black women are subjected to high levels of racism, sexism, and discrimination at levels not experienced by Black men or White women. 13–15
In contrast to Black women, White women in the United States have benefited from living in a politically, culturally, and socioeconomically White-dominated society. 1 These benefits accumulate across generations, creating a cycle of overt and covert privileges 16 , 17 not afforded to Black women, such as wage gap differentials 18 and the invisibility of whiteness ( i.e. , not having to think about one's race). 19 , 20 These privileges do not mean that all White women are similarly advantaged nor are all Black women similarly disadvantaged.
These social conditions create the environment for health disparities to exist and persist. They are the social determinants of health, the “conditions in the environments in which people are born, live, learn, work, play, worship, and age that affect a wide range of health, functioning, and quality-of-life outcomes and risks.” 21 Disparities in Black women's health are particular types of health differences “that are closely linked with social, economic, and/or environmental disadvantage.” 21
The history of Black women's access to health care and treatment by the U.S. medical establishment, particularly in gynecology, contributes to the present-day health disadvantages of Black women. Health inequality among Black women is rooted in slavery. White slave holders viewed enslaved Black women as a means of economic gain, resulting in the abuse of Black women's bodies and a disregard for their reproductive health. Black women were forced to procreate, with little or no self-agency and limited access to medical care. 22 The development of gynecology as a medical specialty in the 1850s 23 ushered in a particularly dark period for the health of Black women. With no regulations for the protection of human subjects in research, Black women were subjected to unethical experimentation without consent. 22–24 Even in more contemporary times, these abuses continue. 25 , 26
As a result of this history and the accumulation of disadvantages across generations, Black women are at the center of a public health emergency. Maternal mortality rates for non-Hispanic Black women are three to four times the maternal mortality rates of non-Hispanic White women. 2 In the next section of this article, we highlight some of the physical and mental health disparities that contribute to the current maternal mortality rates. Although discussed separately, physical health and mental health are inextricably linked.
Physical Health
Demographic characteristics.
Black women are diverse in both nativity and ethnicity. 27 They are not a monolithic group; instead, they comprise multiple cultures and languages. For the purposes of this article, “Black women” refers to the collective identities of Black women, including women of different ethnicities. In the data cited here, “Black women” refers to the women included in the original study population.
Black women currently make up ∼7.0% of the U.S. population and 13.6% of all U.S. women. 10 Although, on average, Black women are younger (36.1 years) than U.S. women overall (39.6 years) ( Table 1 ), 10 they have a higher prevalence of many health conditions, including heart disease, stroke, cancers, diabetes, maternal morbidities, obesity, and stress. Life expectancy at birth is 3 years longer for non-Hispanic White females than for non-Hispanic Black females. Infant mortality rates for children born to non-Hispanic Black women are twice as high as those for children born to non-Hispanic White women 1 ( Table 2 ).
Descriptive Health Statistics for Women
Maternal mortality and pregnancy-related mortality are per 100,000 live births.
Infant mortality rates are per 1,000 live births.
Data sources:
As adults age, their health declines. Aging is affected not only by chronological age but also by biological, behavioral, sociocultural, and environmental factors. 31 Stress, an important factor in aging, is affected strongly by exposure to the built and social environments. Geronimus et al. posit the weathering hypothesis , that is differential exposures to stressful environments are a major factor in widening health disparities as individuals age. They suggest that Black–White disparities in health widen with age because of the accumulation of socioeconomic disadvantages and experiences with racism among Black women throughout the life course. 31–35 Evidence for the weathering hypothesis includes the finding that babies born to Black women in their teens are at lower risk of infant mortality than babies born to older non-Hispanic Black women, the reverse of what is observed for non-Hispanic White women. 31 More recently, Geronimus et al. found that among women aged 49–55 years, telomere length (a biomarker of aging) indicates that Black women are 7.5 years biologically “older” than White women. Perceived stress and poverty account for 27% of this difference. 33
The relatively high levels of morbidity and mortality among Black populations in the United States are, in large part, caused by obesity, which increases the risk of stroke and various CVDs. 36–38 Obesity is a major source of morbidity and mortality for all U.S. populations, but non-Hispanic Blacks have a higher age-adjusted prevalence of obesity than any other racial/ethnic group, with estimates ranging from 34% to 50%. 39 Patterns of obesity vary by many factors across and within races, including location, gender, and educational attainment. 40 Unlike other demographic groups, higher levels of income are not protective against obesity among non-Hispanic Black women. 39 This difference in the prevalence of obesity as reflected in national adiposity data on Black women is the result of the complex multilevel interplay of the measurable and difficult-to-measure social determinants that affect health disparities. Furthermore, Black women lose less weight than other subpopulations do in behavioral weight loss intervention research, 41 and they have a positive body self-image at higher weight levels, which may be psychologically healthy, but also diminishes their motivation to lose weight. 42 These findings support the need for interventions that integrate biological, sociocultural, and environmental factors that influence obesity. 41 The high prevalence of obesity among Black women 36 , 37 impacts the prevalence rates of stroke and various CVDs. 38
Cardiovascular disease
After 50 years of declines in CVD mortality, declines stalled in 2011, with CVD mortality increasing starting in 2015. 43–45 Despite changes in the overall CVD mortality rates, racial and sex disparities persist. Compared with White women, Black women have higher rates of CVD mortality, which have been attributed to poorer cardiovascular (CV) health and a higher burden of modifiable risk factors and clinical comorbidities. 46 , 47 Furthermore, the accumulation of both clinical and behavioral CV risk factors and the manifestation of CVD at younger ages for Black women compared with other racial and ethnic groups—that is, during young adulthood and middle adulthood—have significant implications for maternal and infant health. 48 Understanding the drivers of disparities in CVD among Black women requires examining the intersection of sex as a biological variable 49 and multi-omic influences ( e.g. , genetic ancestry 50 and epigenetic characterization) with multilevel 51 ( e.g. , biological ancestry characterization, individual, interpersonal, community, and society) social constructs ( e.g. , race, ethnicity, and gender).
Although differences in CVD incidence, prevalence, morbidity, and mortality by sex and race/ethnicity are well documented, research on the contributions of genetic factors is limited. People of African ancestry have been underrepresented in genomic research. 52 Furthermore, in genomic studies, analyses of sex chromosomes and the interaction between sex hormones and genetic characteristics are rarely included. 53 Therefore, significant concerns exist about the potential for precision medicine efforts, such as polygenic risk scores, to exacerbate CVD health disparities when using precision medicine research that relies on genetic studies that had inadequate participation from populations with African ancestry. 54
Optimizing such behavioral factors as diet, physical activity, sleep, smoking, alcohol use, emotional health, and stress management is important to maintaining CV health (primordial prevention) and reducing CVD risk (primary and secondary prevention). 55–59 Compared with non-Hispanic White women, non-Hispanic Black women aged 20 years and older have a higher prevalence of several clinical risk factors for CVD, including obesity, high blood pressure, and diabetes. 60
Sleep disparities may contribute to racial/ethnic disparities in CVD. 61 , 62 Blacks have a higher likelihood of short or prolonged sleep durations, obstructive sleep apnea, insomnia, and other measures of poor sleep quality. A study of women of childbearing age showed that, despite Black women having poorer self-reported sleep quality, they were less likely than other women to report their sleep disturbances to a physician. 63 Sleep disturbances may be a manifestation of altered stress reactivity resulting in activation of the chronic stress response and resultant elevations in cardiometabolic disease. 64

Bleeding and blood disorders
Diseases of the blood are as numerous and complex as the fields of hematological physiology and pathophysiology. Benign blood disease include anemia (iron deficiencies), sickle cell anemia (SCD), glucose-6-phosphate dehydrogenase disorders, and hemophilia, among others. Malignant blood diseases (cancers of the blood) include acute myeloid leukemia, acute lymphocytic leukemia, multiple myeloma, non-Hodgkin lymphoma, Hodgkin lymphoma, myeloproliferative neoplasms, and myelodysplastic syndrome. Well-documented differences exist in the prevalence, treatment experiences, and outcomes across races and ethnicities for most benign blood diseases, 65 , 66 and interest in observed disparities in malignancies of the blood is emerging. 67 , 68 Black women are disproportionately impacted by SCD and its complications, as well as by anemia (almost all forms), and they have poor outcomes associated with ancestrally linked disorders, such as G6PD. 69 , 70
Maternal morbidity and mortality
It is estimated that non-Hispanic Black women are three to almost four times more likely to die while pregnant or within 1 year postpartum than their non-Hispanic White and Latina counterparts. 2 The racial disparity in mortality persists at every education level 2 and has persisted or increased over time. 71 As detailed in the sections above, Black women have elevated prevalence rates of chronic conditions associated with higher risk of severe maternal morbidity and mortality. 72 Some of the leading causes of maternal morbidities resulting in pregnancy-associated death occur more in non-Hispanic Black women ( e.g. , hemorrhage, infection [sepsis], thrombotic pulmonary/other embolism, and pregnancy-associated hypertensive disorders). 72 However, changes in the prevalence of these risk factors do not fully account for the increasing trends in severe maternal morbidity 73 and subsequent mortality among non-Hispanic Black women over time. 73
Examination of nonclinical factors, such as hospital quality 74 , 75 (the degree to which health services for individuals and populations increase the likelihood of desired health outcomes) and access to quality care, helps to explain some of the disparities in maternal mortality. Howell et al. 74 , 75 found that women from racial and ethnic minority groups give birth in lower quality hospitals and in hospitals with higher rates of severe maternal morbidity. Using a simulation model, they found that if non-Hispanic Black women gave birth at the same hospitals as non-Hispanic White women, the non-Hispanic Black severe maternal morbidity rate would decrease by 47.7%, from 4.2% to 2.9% (1.3 events per 100 deliveries per year). 74 , 76–79 Qualitative research reveals that many non-Hispanic Black women giving birth in low-performing hospitals experience poor patient–provider communication and difficulties in obtaining appropriate prenatal and postpartum care. 74 , 75
Additionally, homicide is a leading cause of death during pregnancy and postpartum, yet it remains understudied. Typically, homicide is not captured in examinations of pregnancy-related deaths or maternal mortality. Wallace et al. 80 argue that failure to identify and address factors underlying pregnancy-associated homicide will perpetuate racial inequity in mortality during pregnancy and the postpartum period.
Mental Health
National epidemiological surveillance systems that capture information on health risk behaviors and mental health care access—including suicide attempts/occurrence, depression, anxiety, and clinical encounters that record concerns associated with mental health and substance abuse—have notable limitations. Measurement of race and gender across mental health studies varies considerably, creating a dearth of longitudinal research on the nuances of the mental health status of Black women. Even if the experiences of Black women as a racial–gender subgroup are captured with sufficient statistical power to report stratified results of survey findings ( Table 2 ), the results must be interpreted through the lens of the full scope of Black women's experiences in the United States.
Racial discrimination is a toxic “uncontrollable or unpredictable” stressor that is associated not only with poor physical health but also with psychological stress. 76–78 , 81 – 85 Chronic stressors reduce coping resources and increase vulnerability to mental health problems. 76 , 85 Non-Hispanic Blacks with higher levels of multiple stress measures are less likely to achieve intermediate or ideal levels of overall CV health. 86 Research suggests that chronic exposure to environmental stressors, such as racism, across the life span contributes to the weathering of the health of Black women, increasing their allostatic load and, consequently, compromising their reproductive health. 76 , 77 , 81–85 Allostatic load is a measure of the physiological dysregulation that results from cumulative chronic stress on the body. 76 , 87 It is a relevant measure for health disparities research because it can be utilized to assess racial/ethnic differences in biological responses to stressors and their relationship with adverse health outcomes. 83
Maternal mental health
Perceived stress from chronic experiences of discrimination has been found to be a significant predictor of poor birth outcomes. 76 Indeed, non-Hispanic Black women are twice as likely to have a low-birth weight infant than non-Hispanic White women. 76 Non-Hispanic Black women are at a disadvantage regarding the protective factor of the early initiation of prenatal care, with 67% participating in prenatal care in the first trimester compared with 77% of non-Hispanic White women and 81% of Asian women. 76 This is problematic, given that the delivery of perinatal mental health services is critical, particularly for non-Hispanic Black and Latina women because they experience higher rates of depression and anxiety during pregnancy and are at greater risk of poor pregnancy outcomes. 76 , 77 , 81–84 , 88 , 89 Perinatal depression has been linked to risks for adverse maternal and birth outcomes, including preeclampsia, gestational diabetes, preterm birth, and low birth weight. 76 , 90–92 Specifically, it is estimated that up to 28% of non-Hispanic Black women experience perinatal depression. 89
Conclusions
The health of Black women is measured in their disproportionally poor health outcomes, but it is a result of a complex milieu of barriers to quality health care, racism, and stress associated with the distinct social experiences of Black womanhood in U.S. society. Black women are characterized by incredible resilience in the face of adversity and continue to experience improvements in health, even with the socioeconomic contexts that allow disparities to persist. Despite recent mandates by the National Institutes of Health (NIH) to enhance the inclusion of women and racial/ethnic groups that are underrepresented in biomedical research in all NIH-funded research projects, 66 Black women continue to be underrepresented, 93–96 and the resulting interventions may not reflect the unique needs of Black women. Moreover, there is a dearth of current and accessible data on Black women that examines the diversity of Black women (nativity, ethnicity, and country of ancestry). Demographic and health data at the intersection of race and gender are critical to understanding the trends and opportunities for intervention and prevention.
Racism and gender discrimination have profound impacts on the well-being of Black women. Evidence-based care models that are informed by equity and reproductive justice frameworks (reproductive rights as human rights) 76 , 84 need to be explored to address disparities throughout the life course, including the continuum of maternity care, and to ensure favorable outcomes for all women. 79 Interventions to enhance patient–health care provider interactions include raising awareness about the implicit biases that a provider may hold. 97 Black women have continued to make significant inroads in many disciplines yet remain one of few demographic groups that must advocate for themselves to receive consistent and high-quality care. We have outlined disparities in several health conditions and the dire mortality outcomes experienced by Black women. Health does not exist outside its social context. Without equity in social and economic conditions, health equity is unlikely to be achieved, 98 and one cost of health inequality has been the lives of Black women.
Acknowledgment
The authors extend their enormous gratitude to Dr. Beda Jean-Francois for her tireless work and feedback on this article.
The views expressed in this article are those of the authors and do not necessarily represent the views of the Eunice Kennedy Shriver National Institute of Child Health and Human Development; the National Heart, Lung, and Blood Institute; the National Institutes of Health; or the U.S. Department of Health and Human Services.
Author Disclosure Statement
No competing financial interests exist.
Funding Information
No funding was received for this article.
Numbers, Facts and Trends Shaping Your World
Read our research on:
Full Topic List
Regions & Countries
- Publications
- Our Methods
- Short Reads
- Tools & Resources
Read Our Research On:
- Black Americans’ Views of and Engagement With Science
- 3. Black Americans’ views about health disparities, experiences with health care
Table of Contents
- Compared with other professions, fewer Black adults see people of their race at highest levels of success in science, engineering
- A majority of Black high school graduates recall a positive experience in STEM classes, but sizable shares also recall mistreatment
- Half or more Black Americans see mentors as especially influential to how many young people pursue STEM degrees
- Large majorities of Black adults have at least some trust in medical scientists or scientists, generally
- Black Americans generally hold positive views of medical researchers’ competence, skeptical of whether they own up to mistakes
- 75% of Black adults have heard about the Tuskegee study; a majority are skeptical that research procedures today will prevent serious misconduct
- About half of Black Americans say they’ve talked about the coronavirus outbreak multiple times a week
- Black Americans report mix of positive and negative reactions to science news, express frustration over political disagreements
- Acknowledgments
- Methodology
- Appendix: Detailed charts and tables
CORRECTION (Jan. 12, 2024): Chapter 3 of a previous version of this report included an incorrect percentage because one survey question was asked only of women. Among Black adults, 55% say they have ever had at least one of six negative experiences with doctors or other health care providers.
Black Americans offer a mixed assessment of the progress that has been made improving health outcomes for Black people: 47% say health outcomes for Black people have gotten better over the past 20 years, while 31% say they’ve stayed about the same and 20% think they’ve gotten worse.
Less access to quality medical care is the top reason Black Americans see contributing to generally worse health outcomes for Black people in the U.S. Large shares also see other factors as playing a role, including environmental quality problems in Black communities, and hospitals and medical centers giving lower priority to the well-being of Black people.
Asked about their own health care experiences, most Black Americans have positive assessments of the quality of care they’ve received most recently. However, a majority (55%) say they’ve had at least one of six negative experiences, including having to speak up to get the proper care and being treated with less respect than other patients. (A seventh issue asked about applied only to women.)
By and large, Black Americans do not express a widespread preference to see a Black health care provider for routine care: 64% say this makes no difference to them, though 31% say they would prefer to see a Black health care provider for care.
The experiences of younger Black women in the medical system stand out in the survey. A large majority of Black women ages 18 to 49 report having had at least one of seven negative health care experiences included in the survey. They are also more likely than other Black adults to say they would prefer a Black health care provider for routine care and to say a Black doctor or other health care provider would do a better job than medical professionals of other races and ethnicities at providing them with quality medical care.
Beliefs about key factors in health disparities for Black Americans
There are long-standing differences in health outcomes for Black people. Disproportionate mortalities from COVID-19 have heightened disparities between Black and other racial and ethnic populations in the U.S. The most recent estimates from the U.S. Census bureau projects life expectancy at 71.8 years for non-Hispanic Black Americans, the lowest since 2000 and below that estimated for other racial and ethnic groups. The White, non-Hispanic population experienced a smaller decline and, as a result, the gap between expected lifespans for Black and White Americans has widened in the past few years.
Experts have pointed to a number of contributing factors to disparities in health outcomes for Black Americans. The Center survey asked Black Americans for their own views about the reasons behind these disparities and their sense of whether there has been progress over time.
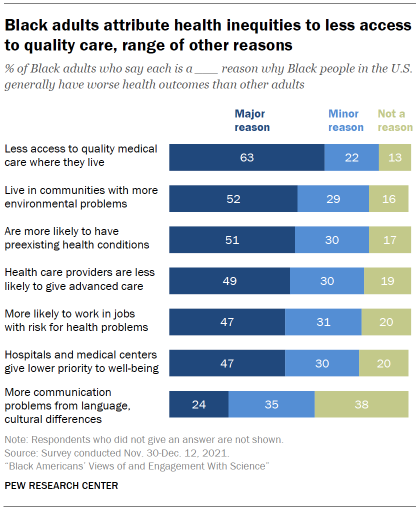
A majority of Black adults say less access to quality medical care where they live is a major reason why Black people in the U.S. generally have worse health outcomes than other adults. About two-in-ten (22%) say this is a minor reason, while just 13% say it is not a reason.
Black adults see a range of other factors – including environmental problems and less-advanced care from health care providers – as contributing to worse health outcomes for Black adults, though somewhat smaller shares cite these as major reasons than point to access issues.
About half (51%) say a major reason why Black people generally have worse health outcomes than others is because they are more likely to have preexisting health conditions. Issues with home and work environments also are seen as playing a role: 52% say a major reason why Black people have worse health outcomes than others is because they live in communities with more environmental problems that cause health issues; 47% say a major reason is that Black people are more likely to work in jobs that put them at risk for health problems.
The health care system is also seen as contributing to the problem: 49% say a major reason why Black people generally have worse health outcomes is because health care providers are less likely to give Black people the most advanced medical care. A roughly equal share (47%) says hospitals and medical centers giving lower priority to their well-being is a major reason for differing health outcomes.
A smaller share (24%) views communication problems from language or cultural differences as a major reason why Black people generally have worse health outcomes than other adults in the U.S.
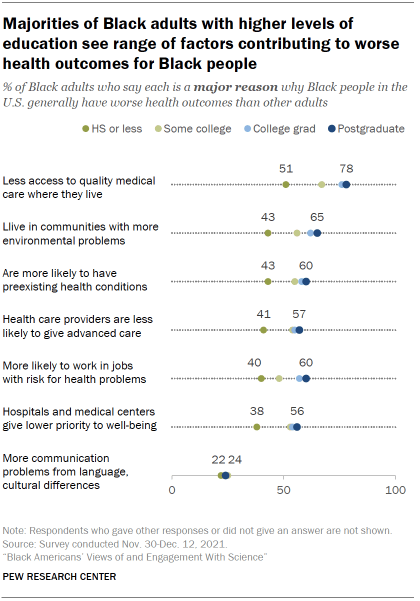
Black adults with higher levels of education are more likely than those with lower levels of education to point to a variety of factors as major reasons for worse health outcomes among Black people.
For instance, large majorities of Black postgraduates (78%) and college graduates (76%) say less access to quality medical care is a major reason Black people have worse health outcomes than other adults in the U.S., compared with 67% of those with some college experience and 51% of Black adults with a high school diploma or less education.
There are also differences in views by age. A majority of Black adults ages 50 and older (58%) say that being more likely to have preexisting health conditions is a major reason why Black people have worse health outcomes than others. Fewer of those under age 50 (46%) see this as a major reason.
Conversely, younger Black adults are more likely than older adults to cite actions from hospitals and medical centers: 50% of those under age 50 say hospitals and medical centers giving lower priority to their well-being is a major reason why Black people have worse health outcomes; 43% of Black adults 50 and older say the same.
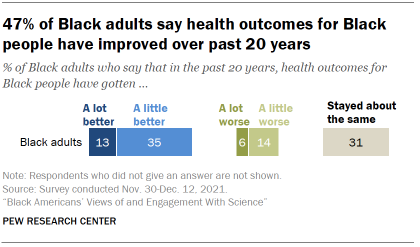
Overall, 47% think health outcomes for Black people have gotten a lot or a little better over the last 20 years. Still, 31% say they have stayed about the same and 20% think they have gotten a lot or a little worse.
For the most part, Black adults’ views on this question are fairly similar across characteristics such as age, gender and levels of educational attainment.
A majority of Black Americans give positive ratings of their recent health care, but can also point to negative experiences in the past
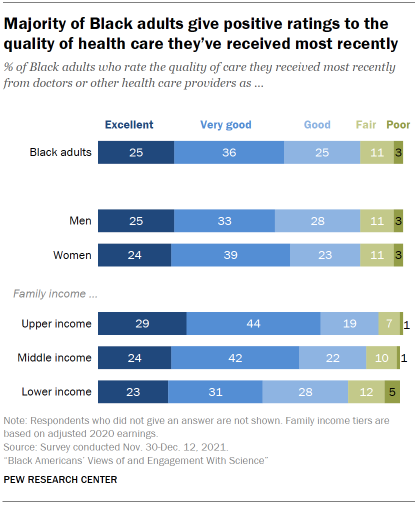
Black adults have generally positive impressions of their most recent experience with health care. A majority (61%) rate the quality of care they’ve received from doctors or other health care providers recently as excellent (25%) or very good (36%). A quarter describe the quality as good, while just 11% say it was fair and only 3% describe the quality of care they’ve received most recently as poor. These ratings are nearly identical to those of all U.S. adults.
Those with higher incomes report more positive recent experiences with doctors and other health care providers than do those with lower incomes.
When it comes to cost, 51% of Black adults describe the out-of-pocket cost of their most recent medical care as ‘about what is fair.’ About a quarter (27%) say they paid more than what’s fair, while 19% say they paid less than what’s fair. For more details, see the Appendix .
A majority of Black adults report at least one negative interaction with doctors and other health care providers at some point in the past
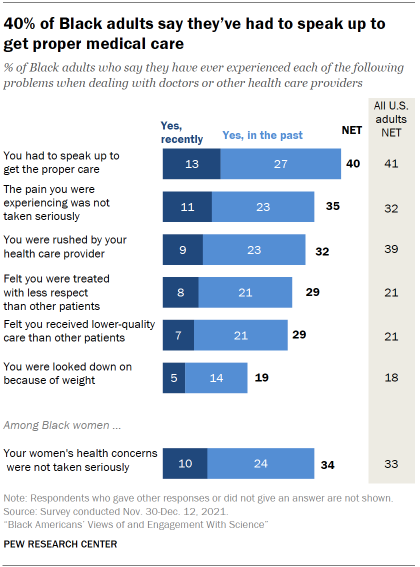
While Black adults generally offer positive ratings of the quality of care they’ve received most recently, a majority (55%) say they’ve had at least one of six negative experiences with doctors or other health care providers at some point in their lives. (A seventh issue asked about applied only to women.)
Overall, 40% of Black adults say they have had to speak up to get the proper care either recently (13%) or in the past (27%). This is the most frequently cited negative experience with medical care across the items included in the survey.
One focus group respondent described their experience this way:
“I had a situation where I had to go through about two different doctors until I was able to get the results that I was requesting, because they did not believe that the issues that I had were valid, or that they were as serious as I made them out to be. It’s kind of been an ongoing thing, so I’m always leery when I’m talking to physicians. I don’t trust them just because they are doctors. I know they have the Hippocratic Oath, but it feels like it’s a little different when they deal with African American patients. And I don’t care if it’s an African American physician or White physicians.” – Black woman, 25-39
When it comes to treatments for pain, 35% of Black adults say they’ve felt the pain they were experiencing was not taken seriously either recently (11%) or in past interactions (23%) with doctors and other health care providers.
About three-in-ten Black adults (32%) say they’ve felt rushed by their health care provider and 29% say they’ve felt they were treated with less respect than other patients, either recently or in past experiences with doctors and other health care providers. Similarly, 29% say they’ve felt they’ve received lower quality medical care at some point; 70% of Black adults say this has not happened to them.
Relatively fewer (19%) say they’ve been looked down on because of their weight or eating habits; 79% say this hasn’t happened to them.
Among Black women, 34% say their women’s health concerns or symptoms were not taken seriously in interactions with doctors and other health care providers.
Black adults at all family income levels are about equally likely to report having at least one of these experiences.
The frequency of negative experiences with the health care system are mostly similar between Black adults and all U.S. adults. However, greater shares of Black adults than all U.S. adults say they’ve felt they’ve received lower-quality care (29% vs. 21% of all U.S. adults) or been treated with less respect than other patients (29% vs. 21%). And fewer Black adults say they were rushed by a health care provider (32% vs. 39% of all U.S. adults).
Black women, especially younger Black women, stand out for the frequency with which they report having had negative health care experiences. Taken together, 63% of Black women say they’ve experienced at least one of the seven negative health care experiences measured in the survey. Among Black men, 46% say they’ve had at least one of six negative experiences with doctors or other health care providers. Black women were asked one more item than men, but the gap between men and women on the six experiences in common is almost identical (62% vs. 46%).
In their own words: Focus group participants on difficulties getting treatment for pain management
There are long-standing concerns about racial biases in pain management. A study in 2020 of emergency room patients experiencing acute appendicitis found wide racial disparities in pain management for both children and adults. The growing use of artificial intelligence algorithms to determine a patient’s need for pain management is raising new questions about how to address systematic bias in pain management treatments.
Here are a few of the comments from focus group participants about getting treatment for pain.
“Well, my husband’s condition (trigeminal neuralgia), it requires a narcotic. And before we got [to current health care provider] for so long, a lot of people just assumed that he was a junkie, like he was just coming in and trying to get pain medication and they wanted to put him on this rotation that just didn’t work, wanted him to take this Tylenol. And it was so frustrating.” – Black woman, age 25-39
“My mom, and I can’t think of it specifically, she has complained to me about being at the hospital and feeling as though they were treating her like she was a drug addict. When they would have to give her pain medication, or she would need something for pain – having her fill out forms, only allotting a certain amount, or cutting it, when her pain is … she goes through pain more times a day, they’ll cut it to less. Less than what she needs to get through the day and not be in pain.” – Black man, age 25-39
“At what point are you going to educate your nurses, your doctors, your ER team that, ‘Hey, this is the protocol when we have sickle cell’? Now, the ironic thing is, when she was going to the children’s hospital, they did have a sickle cell protocol and their treatment of their kids was a little bit different. Most of the time, … 85% of the time … because they were kids, they took their word for it. But when they transitioned over to the adult care, it’s terrible. It’s terrible with the pain, it’s terrible with pain management.” – Black woman, age 40-65
“I was in pain, like in my abdomen. Come to find out I had a fibroid. But I went to the emergency room. ‘Oh, no. You’re fine.’ Something like, ‘Your insurance won’t cover this emergency visit’ or something. ‘Just go to Walgreens and get some Tylenol.’ And I’m like, ’I’m in severe pain. Like I have abdominal pain.’ I ended up going to my doctor, the one I eventually found. He ended up getting me an ultrasound. We did blood work. It was just totally different.” – Black woman, age 25-39
A large majority of younger Black women ages 18 to 49 report negative interactions with health care providers: 71% say they’ve had at least one negative experience in the past. By comparison, a smaller share of Black women ages 50 and older say this (54%).
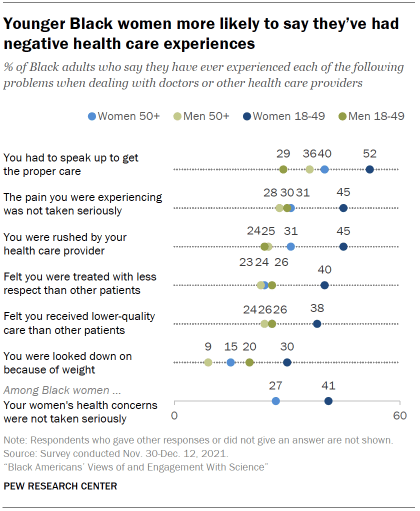
Among Black men, differences by age are more modest than among women, and the pattern runs in the opposite direction: 51% of men ages 50 and older report experiencing at least one of six negative experiences with health care providers, compared with a somewhat smaller share of men ages 18 to 49 (43%).
The experiences of younger Black women stand out across each individual item on health care interactions. For instance, 52% of younger Black women say they’ve had to speak up to get the proper care, compared with 40% of older women, 36% of older men and 29% of younger men.
Among U.S. adults, women ages 18 to 49 are also more likely than older women or than men to say they have had at least one of these negative experiences in a health care visit.
31% of Black adults say they would prefer to see a Black health care provider; a majority have no preference
The share of Black adults working in health-related jobs is roughly equal to their share in the overall workforce, although just 5% of physicians and surgeons are Black. The new survey asked people for their preferences and thoughts about what, if any, difference it makes to have a health care provider who shares their racial background.
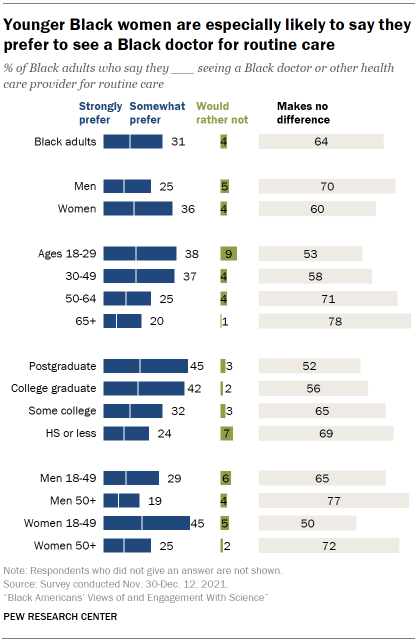
Overall, 31% of Black adults say they would strongly (14%) or somewhat prefer (17%) to see a Black doctor or other health care provider for routine medical care. About two-thirds (64%) say it makes no difference to them, and just 4% say they’d rather not do so for routine care.
Younger Black women stand out from their elders and from Black men in their preferences for seeing a Black health care provider.
Among Black women, a much greater share of those ages 18 to 49 than those 50 and older say they’d prefer to see a Black health care provider for routine care (45% vs. 25%). A majority of older Black women (72%) say it wouldn’t make a difference to them.
There’s a similar pattern in views among Black men, though the gap between younger and older Black men is not as large as among Black women: 29% of Black men ages 18 to 49 would prefer to see a Black health care provider for routine care, compared with 19% of Black men ages 50 and older.
There’s hardly any difference in views on this question between those who have seen a Black doctor or health care provider in the past and those who have not. Among the roughly two-thirds of Black adults who say they’ve seen a Black health care provider for routine care in the past, 32% say they would prefer to see a Black health care provider; among those who have not seen a Black health care provider previously, 30% express this view. See the Appendix for details .
Younger Black women are more likely to see benefits for the quality of medical care from health care treatment with same-race providers
When it comes to key aspects of medical care, majorities of Black adults view a Black doctor and other health care providers as about the same as providers who do not share their race or ethnicity at meeting their needs.
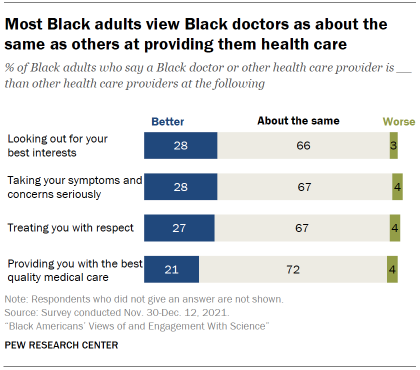
For instance, 72% of Black adults think a Black health care provider is about the same as other health professionals when it comes to the quality of medical care they provide; 21% think a Black health care provider is better than others at this, while just 4% say worse.
Roughly two-thirds view a Black health care provider as about the same as others when it comes to taking their symptoms and concerns seriously, treating them with respect, and looking out for their best interests. Roughly three-in-ten see a Black doctor or health care professional as better than other providers for each of these elements of care.
Among the 31% of Black Americans who say they would prefer to see a Black health care provider for routine matters, majorities think a Black health care provider is better than others at looking out for their best interests (64%), taking their symptoms seriously (64%), treating them with respect (60%) and providing the best quality medical care (53%).
It is unclear whether personal experience lies behind these beliefs. Black adults who have seen a Black health care provider in the past hold similar views on this as those who have not. See Appendix for more details .
Younger Black women are more inclined than older women and men to see an advantage from routine care with a Black health care provider. Still, the majority viewpoint across groups – including among younger Black women – is that a Black health care provider is about the same as others at providing key aspects of care.
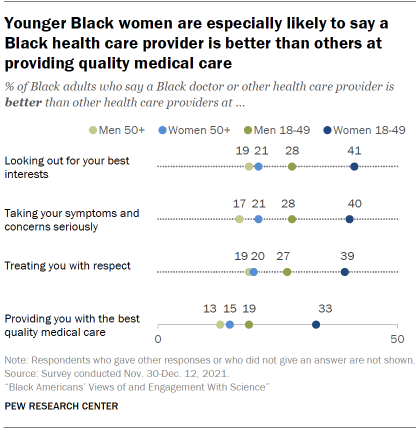
About four-in-ten Black women ages 18 to 49 (41%) say a Black health care provider is better than others at looking out for their best interests, compared with 53% who say they are about the same as other health care providers.
Smaller shares of Black women ages 50 and older (21%), Black men 18 to 49 (28%) and Black men ages 50 and older (19%) view a Black health care provider as better than others at looking out for their best interests. Majorities say they are about the same as others at this.
Age and gender patterns among Black adults are similar across the other aspects of care included in the survey.
When it comes to education, Black adults with higher levels of education tend to be more likely to view a Black doctor or health care provider as better than others when it comes to these key aspects of care. But as with patterns by age and gender, the majority view across levels of educational attainment remains that a Black health care provider is about the same as other healthcare professionals at providing routine health and medical care. See the Appendix for details.
Sign up for our weekly newsletter
Fresh data delivery Saturday mornings
Sign up for The Briefing
Weekly updates on the world of news & information
- Black Americans
- Coronavirus (COVID-19)
- COVID-19 & Science
- COVID-19 in the News
- Medicine & Health
- Racial Bias & Discrimination
- Science News & Information
- STEM Education & Workforce
- Trust in Science
A look at Black-owned businesses in the U.S.
8 facts about black americans and the news, black americans’ views on success in the u.s., among black adults, those with higher incomes are most likely to say they are happy, fewer than half of black americans say the news often covers the issues that are important to them, most popular, report materials.
- American Trends Panel Wave 100
1615 L St. NW, Suite 800 Washington, DC 20036 USA (+1) 202-419-4300 | Main (+1) 202-857-8562 | Fax (+1) 202-419-4372 | Media Inquiries
Research Topics
- Age & Generations
- Economy & Work
- Family & Relationships
- Gender & LGBTQ
- Immigration & Migration
- International Affairs
- Internet & Technology
- Methodological Research
- News Habits & Media
- Non-U.S. Governments
- Other Topics
- Politics & Policy
- Race & Ethnicity
- Email Newsletters
ABOUT PEW RESEARCH CENTER Pew Research Center is a nonpartisan fact tank that informs the public about the issues, attitudes and trends shaping the world. It conducts public opinion polling, demographic research, media content analysis and other empirical social science research. Pew Research Center does not take policy positions. It is a subsidiary of The Pew Charitable Trusts .
Copyright 2024 Pew Research Center
Terms & Conditions
Privacy Policy
Cookie Settings
Reprints, Permissions & Use Policy
- Download PDF
- Share X Facebook Email LinkedIn
- Permissions
Post- Dobbs Challenges in Research and Patient Protections
- 1 Department of Psychiatry, Columbia University Irving Medical Center, New York, New York
- 2 Division on Substance Use Disorders, New York State Psychiatric Institute, New York
- 3 Division of Alcohol, Drugs and Addiction, McLean Hospital, Belmont, Massachusetts
- 4 Division of Women’s Mental Health, McLean Hospital, Belmont, Massachusetts
- 5 Department of Psychiatry, Harvard Medical School, Boston, Massachusetts
The US Supreme Court ruling in Dobbs v Jackson Women’s Health Organization in June 2022 asserted abortion is not a protected right under the US Constitution, overruling 50 years of reproductive autonomy since Roe v Wade . The legality of abortion now falls to individual states, creating an irregular and ambiguous patchwork of regulations and an evolving landscape in which to navigate health care. While the Dobbs decision has far-reaching implications for reproductive health care in the US, it also has significant implications for conducting substance use and other clinical research. There have been other precedents affecting public health decided by a single branch of the federal government, in this case the judicial branch, such as access to firearms and suicide death. 1 The Dobbs decision endangers gains made over the last several decades to increase representation of women, gender-diverse people, and chronically underrepresented racial and ethnic groups in clinical research. Lack of diversity of research participants limits generalizability of medical knowledge and subsequent health benefits for these communities, 2 which can, in turn, exacerbate health disparities. Investigators need to carefully monitor the changing reproductive health legal landscape in the context of state laws to ensure continued participation of women and other people who can become pregnant, while simultaneously maintaining privacy and protection of research participants.
Read More About
Campbell ANC , Greenfield SF. Post- Dobbs Challenges in Research and Patient Protections. JAMA Psychiatry. Published online April 24, 2024. doi:10.1001/jamapsychiatry.2024.0598
Manage citations:
© 2024
Artificial Intelligence Resource Center
Psychiatry in JAMA : Read the Latest
Browse and subscribe to JAMA Network podcasts!
Others Also Liked
Select your interests.
Customize your JAMA Network experience by selecting one or more topics from the list below.
- Academic Medicine
- Acid Base, Electrolytes, Fluids
- Allergy and Clinical Immunology
- American Indian or Alaska Natives
- Anesthesiology
- Anticoagulation
- Art and Images in Psychiatry
- Artificial Intelligence
- Assisted Reproduction
- Bleeding and Transfusion
- Caring for the Critically Ill Patient
- Challenges in Clinical Electrocardiography
- Climate and Health
- Climate Change
- Clinical Challenge
- Clinical Decision Support
- Clinical Implications of Basic Neuroscience
- Clinical Pharmacy and Pharmacology
- Complementary and Alternative Medicine
- Consensus Statements
- Coronavirus (COVID-19)
- Critical Care Medicine
- Cultural Competency
- Dental Medicine
- Dermatology
- Diabetes and Endocrinology
- Diagnostic Test Interpretation
- Drug Development
- Electronic Health Records
- Emergency Medicine
- End of Life, Hospice, Palliative Care
- Environmental Health
- Equity, Diversity, and Inclusion
- Facial Plastic Surgery
- Gastroenterology and Hepatology
- Genetics and Genomics
- Genomics and Precision Health
- Global Health
- Guide to Statistics and Methods
- Hair Disorders
- Health Care Delivery Models
- Health Care Economics, Insurance, Payment
- Health Care Quality
- Health Care Reform
- Health Care Safety
- Health Care Workforce
- Health Disparities
- Health Inequities
- Health Policy
- Health Systems Science
- History of Medicine
- Hypertension
- Images in Neurology
- Implementation Science
- Infectious Diseases
- Innovations in Health Care Delivery
- JAMA Infographic
- Law and Medicine
- Leading Change
- Less is More
- LGBTQIA Medicine
- Lifestyle Behaviors
- Medical Coding
- Medical Devices and Equipment
- Medical Education
- Medical Education and Training
- Medical Journals and Publishing
- Mobile Health and Telemedicine
- Narrative Medicine
- Neuroscience and Psychiatry
- Notable Notes
- Nutrition, Obesity, Exercise
- Obstetrics and Gynecology
- Occupational Health
- Ophthalmology
- Orthopedics
- Otolaryngology
- Pain Medicine
- Palliative Care
- Pathology and Laboratory Medicine
- Patient Care
- Patient Information
- Performance Improvement
- Performance Measures
- Perioperative Care and Consultation
- Pharmacoeconomics
- Pharmacoepidemiology
- Pharmacogenetics
- Pharmacy and Clinical Pharmacology
- Physical Medicine and Rehabilitation
- Physical Therapy
- Physician Leadership
- Population Health
- Primary Care
- Professional Well-being
- Professionalism
- Psychiatry and Behavioral Health
- Public Health
- Pulmonary Medicine
- Regulatory Agencies
- Reproductive Health
- Research, Methods, Statistics
- Resuscitation
- Rheumatology
- Risk Management
- Scientific Discovery and the Future of Medicine
- Shared Decision Making and Communication
- Sleep Medicine
- Sports Medicine
- Stem Cell Transplantation
- Substance Use and Addiction Medicine
- Surgical Innovation
- Surgical Pearls
- Teachable Moment
- Technology and Finance
- The Art of JAMA
- The Arts and Medicine
- The Rational Clinical Examination
- Tobacco and e-Cigarettes
- Translational Medicine
- Trauma and Injury
- Treatment Adherence
- Ultrasonography
- Users' Guide to the Medical Literature
- Vaccination
- Venous Thromboembolism
- Veterans Health
- Women's Health
- Workflow and Process
- Wound Care, Infection, Healing
- Register for email alerts with links to free full-text articles
- Access PDFs of free articles
- Manage your interests
- Save searches and receive search alerts
Change Password
Your password must have 6 characters or more:.
- a lower case character,
- an upper case character,
- a special character
Password Changed Successfully
Your password has been changed
Create your account
Forget yout password.
Enter your email address below and we will send you the reset instructions
If the address matches an existing account you will receive an email with instructions to reset your password
Forgot your Username?
Enter your email address below and we will send you your username
If the address matches an existing account you will receive an email with instructions to retrieve your username

- April 01, 2024 | VOL. 181, NO. 4 CURRENT ISSUE pp.255-346
- March 01, 2024 | VOL. 181, NO. 3 pp.171-254
- February 01, 2024 | VOL. 181, NO. 2 pp.83-170
- January 01, 2024 | VOL. 181, NO. 1 pp.1-82
The American Psychiatric Association (APA) has updated its Privacy Policy and Terms of Use , including with new information specifically addressed to individuals in the European Economic Area. As described in the Privacy Policy and Terms of Use, this website utilizes cookies, including for the purpose of offering an optimal online experience and services tailored to your preferences.
Please read the entire Privacy Policy and Terms of Use. By closing this message, browsing this website, continuing the navigation, or otherwise continuing to use the APA's websites, you confirm that you understand and accept the terms of the Privacy Policy and Terms of Use, including the utilization of cookies.
Mental Health Disparities Research: An Introduction to New Directions
- Crystal L. Barksdale , Ph.D., M.P.H.
Search for more papers by this author
In early 2020, shortly before the United States began to shut down due to the COVID-19 pandemic, leadership at the National Institute of Mental Health (NIMH) recognized the need to address the persistent mental health care disparities that continue to impact millions in this country, despite the significant advances made in mental health with respect to access and quality of care. While the complexities related to disparities reduction and the necessary skills required to conduct culturally and linguistically appropriate care and research have become more widely known and accepted, identifying strategies that create a meaningful reduction in mental health disparities and impact on minority mental health remain elusive. This recognition and the urgent desire to address the issue led NIMH to partner with the National Institute on Minority Health and Health Disparities (NIMHD) to plan and cosponsor a workshop ( 1 ). This virtual workshop held over 2 half days was organized to encourage dialogue about current research and to identify knowledge gaps and innovative strategies to address challenges in mental health disparities research. The workshop featured a diverse panel of researchers who provided their brief perspectives on multidimensional innovative approaches to address a range of mental health and mental health care disparities challenges and served as a think tank that generated novel approaches that the research enterprise and health care system could adopt to support an equity agenda. I served as one of the co-chairs involved in the planning and convening of this workshop, and among the important recommendations that we received from the workshop participants was to distill and broadly disseminate the information and knowledge shared during the workshop to help inform health disparities reduction and equity efforts.
From this interest in disseminating information from the virtual workshop to a wide audience, the idea for this special issue was born. As the special issue concept began to develop, there was a desire to highlight innovative, multidimensional disparities research that could be translated to inform clinical practice that advance health equity. There was also an interest in highlighting information from the workshop that described the historical and contextual issues related to mental health disparities and that articulated the innovative future directions of mental health disparities research and care from multiple perspectives represented at the workshop. After much planning and coordination with the American Journal of Psychiatry Editors, it was determined that some of the NIH Institute leadership and researchers featured during the workshop would expand upon the brief perspectives of their presentations in writing overview papers for the Journal .
As such, the papers included in this special issue represent the perspectives and considerations of NIMH and NIMHD grantees/researchers, program staff, and leadership who were among the numerous participants and attendees that made the virtual workshop a success. These papers range from conceptual and theoretical commentaries to a historically and contextually grounded vision for future disparities research. On behalf of my co-chairs and colleagues that helped plan, convene, and support the virtual workshop and its related activities, I thank all of those that participated and attended, and I am proud to present this special issue as a collection that will continue to inspire and promote important research and clinical work to advance mental health equity.
The author reports no financial relationships with commercial interests.
This work was written as part of the author’s official duties as a government employee. The views expressed in this article are the opinions of the author and do not necessarily represent the views of the NIMHD, NIH, or the United States Government.
1. NIMH Office for Disparities Research and Workforce Diversity and National Institute on Minority Health and Health Disparities : Workshop: Identifying New Directions in Mental Health Disparities Research: Innovations with a Multidimensional Lens . www.nimh.nih.gov/news/events/2020/workshop-identifying-new-directions-in-mental-health-disparities-research-innovations-with-a-multidimensional-lens Google Scholar
- Ned H. Kalin , M.D. ,
- Elisabeth B. Binder , M.D., Ph.D. ,
- Kathleen T. Brady , M.D., Ph.D. ,
- David A. Lewis , M.D. ,
- William M. McDonald , M.D. ,
- Daniel S. Pine , M.D. ,
- Carolyn I. Rodriguez , M.D., Ph.D. ,
- Michael D. Roy , B.S.
Issue Highlights
- Disparities
- Sociopolitical Issues
Health Disparities Research Paper Topics

This page provides a comprehensive exploration of health disparities research paper topics , catering to students in health sciences who are tasked with writing impactful research papers. With a focus on addressing health inequities, the page offers a diverse and extensive list of research paper topics categorized into ten distinct areas. These categories encompass racial and ethnic disparities, socioeconomic disparities, gender disparities, age-related disparities, geographic disparities, access to healthcare disparities, disparities in mental health, disparities in chronic disease management, disparities in maternal and child health, and disparities in health behaviors. By covering these health disparities research paper topics, students can delve into pressing issues within health disparities research and contribute to the body of knowledge surrounding health inequities.
100 Health Disparities Research Paper Topics
The field of health disparities research encompasses a wide range of topics that address the unequal distribution of health outcomes and access to healthcare among diverse populations. As students studying health sciences, you have the opportunity to contribute to this important area of study by exploring and investigating critical health disparities research paper topics. This comprehensive list is designed to provide you with a rich array of research ideas, categorized into ten distinct areas, each highlighting different dimensions of health disparities. By delving into these topics, you can deepen your understanding of the complex factors that contribute to health inequities and generate knowledge that can drive meaningful change in healthcare practices and policies. Whether you are passionate about racial and ethnic disparities, socioeconomic disparities, gender disparities, or other dimensions of health disparities, this list will offer you valuable insights and a foundation for developing your research paper. Explore the categories below to find a topic that aligns with your interests and academic goals, and embark on your journey to make a positive impact in addressing health disparities.
Academic Writing, Editing, Proofreading, And Problem Solving Services
Get 10% off with 24start discount code.
1. Racial and Ethnic Disparities
- Exploring the impact of racial and ethnic disparities on healthcare access and quality
- Understanding the social determinants of health contributing to racial and ethnic health disparities
- Investigating the effects of discrimination and bias on health outcomes among marginalized populations
- Analyzing the role of cultural beliefs and practices in shaping health behaviors and disparities
- Examining racial and ethnic disparities in chronic disease prevalence and management
- Investigating the impact of racism and discrimination on mental health outcomes
- Exploring the relationship between socioeconomic status, race, and health disparities
- Analyzing the role of structural racism in perpetuating health inequities
- Investigating racial and ethnic disparities in maternal and child health outcomes
- Exploring strategies to reduce racial and ethnic health disparities through policy and intervention
2. Socioeconomic Disparities
- Investigating the impact of income inequality on health disparities
- Analyzing the relationship between education and health outcomes among disadvantaged populations
- Exploring the role of social determinants of health in socioeconomic disparities
- Investigating the impact of neighborhood characteristics on health disparities
- Analyzing the effects of food insecurity on health outcomes and disparities
- Exploring the relationship between employment status and health disparities
- Investigating the impact of housing instability on health disparities
- Analyzing the role of social support networks in mitigating socioeconomic health disparities
- Exploring strategies to address healthcare access and affordability among low-income populations
- Investigating the impact of social policies on socioeconomic health disparities
3. Gender Disparities
- Analyzing gender disparities in healthcare utilization and access
- Investigating the impact of gender on mental health outcomes and disparities
- Exploring gender disparities in chronic disease prevalence and management
- Analyzing the role of gender norms and expectations in shaping health behaviors and disparities
- Investigating gender disparities in reproductive health outcomes and access to care
- Exploring the impact of gender-based violence on health disparities
- Investigating the relationship between gender identity and health outcomes among transgender populations
- Analyzing the role of healthcare provider bias in contributing to gender disparities
- Exploring gender disparities in health outcomes among aging populations
- Investigating strategies to address gender disparities in healthcare and improve health equity
4. Age-related Disparities
- Exploring age-related disparities in access to preventive healthcare services
- Investigating the impact of ageism on health outcomes among older adults
- Analyzing age-related disparities in chronic disease prevalence and management
- Exploring the relationship between socioeconomic status and age-related health disparities
- Investigating age-related disparities in mental health outcomes and access to care
- Analyzing the impact of social isolation on health outcomes among older adults
- Exploring age-related disparities in end-of-life care and palliative services
- Investigating the impact of aging on health disparities among minority populations
- Analyzing the role of age-related policy interventions in reducing health disparities
- Exploring strategies to promote healthy aging and reduce age-related health disparities
5. Geographic Disparities
- Investigating rural-urban disparities in healthcare access and outcomes
- Exploring the impact of healthcare provider shortages on geographic health disparities
- Analyzing the role of transportation barriers in contributing to geographic health disparities
- Investigating the impact of environmental factors on geographic health disparities
- Exploring geographic disparities in infectious disease prevalence and control
- Analyzing the relationship between geography and access to specialty care services
- Investigating the impact of telemedicine and technology on reducing geographic health disparities
- Exploring strategies to improve healthcare infrastructure and services in underserved areas
- Investigating the impact of healthcare policy and funding on geographic health disparities
- Analyzing the role of community-based interventions in addressing geographic health disparities
6. Access to Healthcare Disparities
- Exploring barriers to healthcare access among vulnerable populations
- Analyzing the impact of health insurance coverage on access to care and health disparities
- Investigating the role of healthcare literacy in shaping access to care and health outcomes
- Exploring disparities in healthcare utilization and preventive services uptake
- Analyzing the impact of language barriers on healthcare access and disparities
- Investigating the role of cultural competence in reducing healthcare disparities
- Exploring strategies to improve access to mental healthcare services among underserved populations
- Investigating the impact of healthcare provider bias on access to care and health disparities
- Analyzing the role of patient navigation programs in reducing healthcare access disparities
- Exploring innovative approaches and interventions to improve access to healthcare among marginalized populations
7. Disparities in Mental Health
- Investigating disparities in mental health diagnosis and treatment among diverse populations
- Exploring the impact of socioeconomic factors on mental health disparities
- Analyzing the role of stigma and discrimination in shaping mental health disparities
- Investigating disparities in access to mental healthcare services and resources
- Exploring the relationship between cultural factors and mental health disparities
- Analyzing the impact of social support networks on mental health outcomes and disparities
- Investigating the role of trauma and adverse childhood experiences in contributing to mental health disparities
- Exploring disparities in mental health outcomes among LGBTQ+ populations
- Investigating the impact of socioeconomic policies on mental health disparities
- Analyzing strategies to promote mental health equity and reduce disparities
8. Disparities in Chronic Disease Management
- Exploring disparities in chronic disease prevalence and outcomes among diverse populations
- Investigating the impact of socioeconomic factors on chronic disease management disparities
- Analyzing the role of healthcare access and utilization in chronic disease disparities
- Exploring disparities in healthcare provider-patient communication and its influence on chronic disease management
- Investigating the impact of health literacy on chronic disease disparities
- Analyzing disparities in medication adherence and self-management practices
- Exploring the relationship between cultural factors and chronic disease management disparities
- Investigating the impact of lifestyle factors and health behaviors on chronic disease disparities
- Analyzing the role of social support networks in chronic disease management disparities
- Exploring strategies to improve chronic disease management and reduce disparities
9. Disparities in Maternal and Child Health
- Investigating racial and ethnic disparities in maternal and infant mortality rates
- Exploring disparities in prenatal care utilization and access among diverse populations
- Analyzing the impact of socioeconomic factors on maternal and child health disparities
- Investigating disparities in breastfeeding initiation and duration among different demographic groups
- Exploring the relationship between cultural factors and maternal and child health outcomes
- Analyzing disparities in access to quality prenatal and pediatric care services
- Investigating the impact of maternal mental health on birth outcomes and child health disparities
- Exploring disparities in childhood vaccination rates and its implications for health disparities
- Investigating the impact of social determinants of health on maternal and child health disparities
- Analyzing strategies to improve maternal and child health outcomes and reduce disparities
10. Disparities in Health Behaviors
- Exploring socioeconomic disparities in health behaviors and their impact on health outcomes
- Investigating disparities in physical activity levels and sedentary behaviors among diverse populations
- Analyzing the impact of socioeconomic factors on dietary disparities and their influence on health
- Investigating disparities in tobacco use and its relationship to health disparities
- Exploring cultural factors and their influence on health behavior disparities
- Analyzing disparities in alcohol and substance abuse rates and their implications for health disparities
- Investigating the impact of educational attainment on health behavior disparities
- Exploring disparities in sleep patterns and their effects on health outcomes
- Investigating the role of social determinants in shaping health behavior disparities
- Analyzing strategies to promote equitable health behaviors and reduce disparities
This comprehensive list provides an extensive range of health disparities research paper topics, allowing students to explore various aspects of health disparities and contribute to the understanding and resolution of health inequities.
Choosing Health Disparities Research Paper Topics
When it comes to choosing health disparities research paper topics, it is essential to select a subject that not only captivates your interest but also addresses significant gaps in knowledge and contributes to the understanding of health inequities. Here, we provide you with ten expert tips to guide you in selecting a compelling and impactful research topic in the field of health disparities.
- Identify your passion : Start by identifying the areas of health disparities that resonate with your interests and values. What populations or dimensions of health disparities do you feel most drawn to? Your passion will fuel your motivation and dedication throughout the research process.
- Conduct a comprehensive literature review : Before finalizing your research topic, conduct a thorough review of the existing literature. This will help you identify gaps, controversies, and emerging trends in the field of health disparities. It will also provide you with a foundation of knowledge to build upon and ensure the originality of your research.
- Engage with current debates : Explore ongoing debates and controversies within the field of health disparities. By immersing yourself in these discussions, you can identify research questions that address critical issues and contribute to the resolution of controversies.
- Consult with experts : Seek guidance from professors, advisors, or professionals who specialize in health disparities research. Their expertise can provide valuable insights, help refine your research questions, and direct you towards underexplored areas within the field.
- Consider social determinants of health : Health disparities are influenced by various social determinants such as socioeconomic status, education, environment, and cultural factors. Consider how these determinants intersect with specific populations or health outcomes to identify health disparities research paper topics that shed light on the complexities of health disparities.
- Examine policy implications : Evaluate the potential policy implications of your research topic. How can your findings inform interventions, programs, or policies that reduce health disparities? Consider the practical applications of your research and its potential impact on healthcare practices and policies.
- Address intersectionality : Recognize the intersecting identities and social positions that individuals hold, such as race, ethnicity, gender, socioeconomic status, and sexual orientation. Consider how multiple dimensions of inequality interact and compound health disparities. Choosing a research topic that explores intersectionality will provide a more comprehensive understanding of health inequities.
- Collaborate with affected communities : Engage with the communities most affected by health disparities. Collaborating with community organizations or advocacy groups can help ensure that your research is relevant, culturally sensitive, and informed by the lived experiences of those experiencing health inequities.
- Think beyond local contexts : Health disparities exist at local, regional, national, and global levels. Consider the broader implications of your research topic and how it connects to global health disparities. This will enable you to contribute to a more comprehensive understanding of health inequities.
- Seek ethical considerations : Reflect on the ethical implications of your research topic, particularly regarding potential harm to vulnerable populations. Ensure that your research design respects the principles of equity, justice, and autonomy. Seek institutional review board (IRB) approval and ethical clearance as necessary.
By following these expert tips, you can choose a health disparities research paper topic that is not only academically rigorous but also socially relevant and impactful. Remember, selecting a compelling topic is the first step towards making a meaningful contribution to the field of health disparities research.
How to Write a Health Disparities Research Paper
Writing a health disparities research paper requires careful planning, attention to detail, and a systematic approach. To guide you through this process, we have compiled ten essential tips to help you craft a well-structured and impactful research paper in the field of health disparities.
- Understand the research question : Begin by clearly defining your research question or objective. What specific aspect of health disparities are you investigating? Formulate a focused and concise research question that will guide your entire paper.
- Conduct a comprehensive literature review : Before diving into your research, conduct a thorough literature review to familiarize yourself with existing knowledge and research gaps related to your topic. This will help you identify key concepts, theories, methodologies, and research findings that will inform your own study.
- Develop a strong theoretical framework : Identify and utilize relevant theoretical frameworks that underpin the study of health disparities. Theoretical frameworks provide a lens through which you can analyze and interpret your research findings, helping to contextualize your study within existing literature and theories.
- Determine your research methodology : Select an appropriate research methodology that aligns with your research question and objectives. Consider quantitative, qualitative, or mixed-methods approaches, depending on the nature of your research topic and the data you intend to collect.
- Collect and analyze data : Collect data using reliable and appropriate methods. This may involve surveys, interviews, observations, or analysis of existing datasets. Ensure that your data collection methods capture the necessary information to answer your research question and address health disparities adequately.
- Interpret and analyze findings : Once you have collected your data, analyze and interpret the findings within the context of health disparities. Use statistical analysis, qualitative coding, or other relevant techniques to identify patterns, relationships, and disparities in your data. Consider the implications of your findings for addressing health inequities.
- Contextualize your findings : Situate your research findings within the broader context of health disparities. Analyze the social, economic, cultural, and political factors that contribute to health inequities. Consider the influence of structural determinants, social determinants, and individual-level factors on the observed disparities.
- Discuss limitations and potential biases : Acknowledge and discuss the limitations and potential biases of your research. Address any methodological constraints, sample limitations, or data collection challenges. Reflect on how these limitations may impact the generalizability and validity of your findings.
- Provide policy and practice recommendations : Based on your research findings, offer evidence-based recommendations for policy and practice interventions aimed at reducing health disparities. Consider the implications of your findings for healthcare systems, public health policies, community programs, and interventions targeted at improving health equity.
- Conclude with a strong summary and future directions : Summarize the key findings of your research paper, emphasizing the contributions to the field of health disparities. Reflect on the implications of your study and suggest avenues for future research, highlighting areas where further investigation is needed to address existing research gaps.
By following these ten tips, you can navigate the process of writing a health disparities research paper with confidence. Remember to maintain a clear focus on your research question, analyze your findings within the broader context of health disparities, and provide recommendations that can inform policy and practice to promote health equity. Through your research, you have the opportunity to contribute to the ongoing efforts to address health disparities and create a more equitable healthcare system for all.
iResearchNet’s Custom Writing Services
When it comes to writing a compelling and well-researched health disparities research paper, iResearchNet is your trusted partner. Our writing services are specifically tailored to meet the unique needs of students studying health sciences who are seeking assistance with their research papers. With a team of expert degree-holding writers, commitment to top quality, customized solutions, and a range of features, we ensure that your experience with iResearchNet is seamless and successful. Here are the 13 key features of our writing services:
- Expert degree-holding writers : Our team of writers consists of experts in the field of health sciences with advanced degrees. They possess a deep understanding of health disparities and are well-equipped to produce high-quality research papers.
- Custom written works : We provide custom-written research papers tailored to your specific requirements. Our writers will closely follow your instructions and incorporate the necessary elements to ensure a unique and original paper.
- In-depth research : Our writers are skilled in conducting in-depth research using reliable and up-to-date sources. They will ensure that your health disparities research paper is backed by robust evidence and explores the latest developments in the field.
- Custom formatting : We offer custom formatting options to match the style guidelines of your academic institution. Whether you require APA, MLA, Chicago/Turabian, or Harvard formatting, our writers will ensure that your paper adheres to the required standards.
- Top quality : Quality is our utmost priority. We have a rigorous quality control process in place to ensure that your health disparities research paper meets the highest standards of academic excellence. Our editors will review the paper for clarity, coherence, grammar, and adherence to formatting guidelines.
- Customized solutions : We understand that every research paper is unique. Our writers will work closely with you to understand your specific requirements, research objectives, and guidelines. They will tailor the research paper to your individual needs, ensuring that it aligns with your research question and objectives.
- Flexible pricing : We offer flexible pricing options to accommodate students’ budgets. Our pricing structure is transparent, and we provide detailed information about the cost of our services upfront. You can choose the pricing plan that best suits your needs.
- Short deadlines : We understand that deadlines can be tight. Our writers are skilled at working under pressure, and we offer short turnaround times, including deadlines as tight as 3 hours. You can rely on us to deliver your research paper promptly.
- Timely delivery : We are committed to delivering your health disparities research paper within the agreed-upon timeframe. We understand the importance of timely submission and will ensure that you have sufficient time to review and request revisions if necessary.
- 24/7 support : Our customer support team is available 24/7 to assist you with any inquiries or concerns. Whether you have questions about the progress of your paper or need clarification on our services, our dedicated support team is here to help.
- Absolute privacy : We prioritize the confidentiality of your personal information. Rest assured that all interactions and details related to your research paper will be handled with the utmost privacy and security. We adhere to strict data protection protocols to safeguard your information.
- Easy order tracking : Our user-friendly platform allows you to track the progress of your order conveniently. You can stay updated on the status of your research paper, communicate with your assigned writer, and access any necessary documents.
- Money-back guarantee : We stand behind the quality of our services. If you are not satisfied with the final research paper or if it does not meet your expectations, we offer a money-back guarantee. Your satisfaction is our top priority.
With iResearchNet’s comprehensive writing services, you can confidently embark on your health disparities research paper knowing that you have expert support and guidance every step of the way. We are dedicated to helping you achieve academic success and make a meaningful impact in the field of health disparities. Place your order today and experience the iResearchNet difference.
Empower Your Research with iResearchNet
When it comes to tackling the complex and critical field of health disparities research, iResearchNet is your trusted ally. We understand the importance of crafting a high-quality research paper that contributes to the understanding and resolution of health inequities. With our comprehensive writing services, we provide you with the support and resources you need to elevate your health disparities research to new heights.
Our team of expert writers specializes in health sciences and possesses in-depth knowledge of health disparities. They have the expertise to guide you through every step of the research process, ensuring that your paper is well-researched, well-structured, and academically rigorous.
By partnering with iResearchNet, you gain access to a range of benefits that will enhance your research experience. Our services are tailored to meet your unique needs and deliver exceptional results. At iResearchNet, we are committed to delivering top-quality research papers that make a meaningful impact in the field of health disparities. Our team will work diligently to ensure that your research paper meets the highest academic standards, while also being responsive to your specific needs and preferences.
Don’t let the challenges of health disparities research hold you back. Partner with iResearchNet today and unlock the full potential of your health disparities research. Together, we can contribute to the ongoing efforts to address health inequities and create a more equitable and inclusive healthcare system for all.
ORDER HIGH QUALITY CUSTOM PAPER


Health Disparities Research

The NINDS is committed to reducing the disproportionate burden of neurological disease borne by underserved groups of society, including racial and ethnic minority, rural, and socioeconomically disadvantaged populations, by funding a spectrum of research from basic science through clinical studies and training the next generation of health disparities investigators.
Health disparities populations are in need of effective tailored prevention and treatment approaches. Poorer health outcomes in these populations when compared to the general US population have a dramatic impact on public health and are a significant cost to society. Supporting research to diminish health disparities in neurological disorders is inherent in the NINDS mission to reduce the burden of neurological disease, a burden borne by every segment of society. (see NINDS Office of Global Health and Health Disparities )
NINDS Strategic Plan and Recommendations for Advancing Health Equity in Neurological Disorders NINDS Health Equity Strategic Plan will guide research investments and provide actionable recommendations to address health disparities and promote health equity in neurological disorders over the next 5 -10 years. View the Health Equity Strategic Plan High-Level Recommendations and Guide NINDS HERN Initiative Check out the NINDS Community-Engaged Health Equity Research in Neuroscience Initiative (HERN) website for additional info and related funding opportunities.
Health Disparities and Stroke
Stroke continues to be a major focus of NINDS health disparities research efforts, as it remains one of the largest and most burdensome disparities in neurological health with substantial opportunities for improving outcomes. NINDS supports research to better understand stroke disparities and to inform the development of effective interventions in specific population groups who suffer a disproportionately higher burden of stroke.
Current NINDS-supported stroke disparities research highlights:
- REGARDS (REasons for Geographic And Racial Differences in Stroke)
- The Northern Manhattan Study (NOMAS)
- Brain Attack Surveillance in Corpus Christi (BASIC)
- Stroke Health and Risk Education (SHARE)
- Hip Hop Stroke
- Columbia University's SWIFT (Stroke Warning Information and Faster Treatment)
Estimates of Funding for Various Research, Condition, and Disease Categories
Related federal programs, stroke disparities program.
The Georgetown University Stroke Disparities Program, is an integrated program of collaborative research designed to overcome current gaps in stroke care in underserved populations in Washington, DC. The research projects address 3 key areas of health disparities in stroke: 1) interventions to increase IV tPA utilization in underserved populations, 2) a health navigator intervention to improve secondary stroke prevention, and 3) further study the disparities in primary intracerebral hemorrhage and its pathophysiology. (Drs. Chelsea Kidwell, Bernadette Boden-Albala, and Alex Dromerick, Project PIs)
Alaska Native Stroke Registry (ANSR)
The Alaska Native Stroke Registry (ANSR) is the first study of Alaska Native populations to document the incidence of stroke among Native populations living in both rural and urban Alaska over a 4 year period. This work has also collected key information in rural communities focused on vascular risk behaviors which may be linked to the rapid increase in stroke risk factors in this culturally diverse Alaska Native population. (Drs. Bernadette Boden-Albala, James Allen, and Brian Trimble, Project PIs)
A Multi-Ethnic Comparative Effectiveness Study for Diagnosis of Cardiogenic Stroke
DeCODE Genetics' A Multi-Ethnic Comparative Effectiveness Study for the Diagnosis of Cardiogenic Stroke is an observational study that utilizes extended cardiac rhythm monitoring in stroke patients and studies the association of genetic variants to atrial fibrillation detection in blacks, whites, and Hispanics. (Dr. Jeffrey Gulcher, PI)
Greater Cincinnati Northern Kentucky Stroke Study (GCNKSS)
The Greater Cincinnati/Northern Kentucky Stroke Study (GCNKSS) is a large, population-based study of temporal trends in stroke incidence, risk factors, treatment and outcome within a biracial (African-American and white) population. Beginning in 1993, the GCNKSS identifies hospitalized and autopsied cases of stroke and transient ischemic attack in the 5-county region through screening of all hospitals and coroner's offices as well as sampling of nursing homes and physicians' offices. In addition, general population surveys have been conducted to assess stroke awareness in the community. (Drs. Brett Kissela and Dawn Kleindorfer, PIs)
Stroke Prevention/Intervention Research Program (SPIRP)
The Stroke Prevention/Intervention Research Program is comprised of several scientifically rigorous stroke culturally tailored interventions that address major contributors to stroke disparities including risk factor control, re-engineered treatment delivery, and state-wide barrier assessment and intervention. These multi-project cooperative agreements address major stroke disparities research gaps and have dissemination planning, training/education and community outreach as major components of their programs. The four funded SPIRP projects are described below.
Kaiser Permanente Northern California (KPNC) / University of California San Francisco (UCSF)
The vision of the Kaiser Permanente Northern California (KPNC) / University of California San Francisco (UCSF) collaboration for a Stroke Prevention/ Intervention Research Program in Health Disparities is the elimination in the United States of stroke disparities based on race, ethnicity, and socioeconomic status. Recognizing that there are multi-faceted reasons for the existence of stroke disparities and that these reasons vary across the populations, the initial focus will be the elimination of disparities in hypertension control between African Americans and Caucasians, with a secondary focus of developing knowledge that will help us understand the basis for the apparent increase of stroke incidence in recent years among young adults, most notably African Americans. The investigators will conduct pragmatic randomized controlled trial in the diverse adult population of KPNC that consists of both a clinical algorithm for rapid and effective blood pressure control, as well as a culturally-tailored dietary intervention aimed at more effective sustained blood pressure control. The results of this trial will be used in KPNC to model the impact of these interventions throughout the United States. The research team will also conduct an observational cohort study with KPNC to identify and quantify disparities in the temporal trends in known risk factors for stroke in young adulthood and identify novel factors that may contribute to stroke risk in young adults, and specifically to disparities in this risk. Finally, this project will include an education program for training in disparities issues related to stroke and for dissemination of the research methods and results.
New York University (NYU)/Columbia University
The New York University (NYU)/Columbia University’s Center for Stroke Disparities Solutions is a consortium between three academic institutions, a municipal healthcare system and home healthcare organization in New York City. The vision is to reduce stroke disparities with a particular focus on prevention of recurrent stroke among Blacks and Hispanics. Project 1 is a Practice-based Trial of Home BP Telemonitoring (HBPTM, )a comparative effectiveness trial of HBPTM alone versus HBPTM plus telephonic nurse case management on prevention of recurrent stroke. Project 2, Stroke Community Transitions Intervention, will evaluate the effectiveness of a culturally-tailored transition care program delivered by nurse practitioners and community health workers in improving BP control, functional outcomes and quality of life in homebound post-acute stroke patients. Project 3, Tailored Approaches to Stroke Health Education, will evaluate the effectiveness of a novel culturally tailored intervention using storytelling in increasing stroke literacy among adults in Black and Hispanic churches across NYC. These three projects address barriers that occur along the continuum of stroke care from the community to homecare, and primary care settings.
University of California, Los Angeles
The Los Angeles Stroke Prevention/ Intervention Research Program in Health Disparities is a multi-partnered, highly collaborative research and education center that spans the Los Angeles basin and aims to generate new knowledge about how to end disparities in stroke occurrence. It includes two randomized trials incorporating community health workers, mobile health technology, and the aging services network in Los Angeles, and embracing its most vulnerable and disadvantaged Hispanic, African-American, and Asian-American populations to generate evidence for sustainable, national models for preventing stroke. A third study will elucidate changes over two decades in novel biological and social risk factors for stroke among minorities using a national dataset. Community-academic research partnerships in stroke disparities will be continually sustained through bi-directional knowledge sharing.
University of Miami, Miller School of Medicine
The Hispanic Stroke Prevention/Intervention Research Program is a specialized collaborative center at the University of Miami, Miller School of Medicine, and involves collaborators in Puerto Rico at the University of Puerto Rico and Hospital HIMA. The mission of the center is to improve the treatment and prevention of stroke among Hispanics. This high-impact, multi-disciplinary research program will initiate the Florida Puerto Rico Stroke Registry and collate data from nearly 140 hospitals that are currently collecting American Heart Association’s Get With the Guidelines-Stroke data, as well as specific new data items. The aims are to help identify disparities in acute stroke care and secondary stroke prevention by race, ethnicity, and region and to educate stakeholders in approaches to improve stroke quality regarding stroke disparities. To effectively coordinate this bold initiative, create synergy among collaborating institutions, and support the public health and scientific aims of the registry, the center also contains an administrative core designed to effectively integrate the principal components of the registry and provide the requisite administrative infrastructure to enhance success; a training core focused on stroke disparities research and educational training for healthcare professionals including clinicians, nurses, and pharmacists in Florida and Puerto Rico; and a data management core to serve as the analytic hub of the center and to provide integration of data analysis and collection.
Proceedings & Outcomes
Inclusion research.
Findings from clinical trials are applied broadly in clinical practice and inform treatment guidelines that affect the clinical care of the general population. To ensure that new preventive, diagnostic, and treatment approaches are safe and effective for diverse subgroups represented in the population, the studies must enroll sufficient numbers of minority subjects. The NINDS helps its grantees adhere to the NIH policy for Inclusion of Women and Minorities in Clinical Research through several activities designed to facilitate investigators' efforts to meet enrollment targets. In addition to the activities described below, a clinical trials recruitment expert in the NINDS Office of Clinical Research works directly with the grantees and program directors on issues related to recruitment and retention.
Clinical Research United in Successful Enrollment (CRUiSE)
NINDS co-sponsored an NHLBI workshop to address successful recruitment in clinical trials. Three key areas were addressed: 1) public and professional awareness and acceptance of clinical trials; 2) human subject research policies, guidelines, and reimbursement; and 3) clinical trial enrollment experience and practice. A significant portion of the conference addressed the barriers and solutions to improve the inclusion of minorities in clinical trials. Seventy-five participants, including invited speakers representing clinical researchers, private advocacy groups, industry, and federal sponsors and regulatory agencies, attended.
Inclusion Research funded by NINDS
Resources and tools.
Richard T. Benson, M.D., Ph.D. | Director, Office of Global Health and Health Disparities [email protected]
Cheryse A. Sankar, Ph.D. | Program Director, Health Disparities [email protected]
Naomi E. Booker, M.P.H. | Health Program Specialist [email protected]
Funding Opportunities
OGHHD Funding Opportunities
NOFOs Highlight Community-Engaged Health Equity Research in Neuroscience Initiative (R34 CT Not Allowed) (RFA-NS-24-006) Community-Engaged Health Equity Research in Neuroscience Initiative (R34 CT Not Allowed) (RFA-NS-24-007)
News & Events
- NASEM Report Release: Advancing Anti-Racism, Diversity, Equity, and Inclusion in STEM Organizations: A Consensus Study | View Report
Subscribe to the NINDS-OGHHD Listserv
Related Topics Subscribe to the NINDS-OGHHD Listserv REGARDS (REasons for Geographic And Racial Differences in Stroke) REGARDS is a large cohort study evaluating the causes of racial and geographic differences in stroke mortality and cognitive decline in the United States. The Northern Manhattan Study (NOMAS) NOMAS is a prospective population-based study of stroke incidence, risk factors, and prognosis in a multiethnic, urban population. Stroke Warning Information and Faster Treatment (SWIFT) The Columbia University's SWIFT (Stroke Warning information and Faster Treatment) study identifies actions/barriers toward optimal "Stroke Preparedness" within a multiethnic community. Brain Attack Surveillance in Corpus Christi (BASIC) The BASIC project is a population-based study that examines the magnitude and etiologies of the stroke health disparity between Mexican Americans and non Hispanic whites. Stroke Health And Risk Education (SHARE) The SHARE study is a behavior change, educational intervention study aimed at primary stroke prevention for Mexican Americans and non Hispanic whites in Corpus Christi, Texas. SHARE is a partnership between University of Michigan researchers and the Diocese of Corpus Christi. Hip Hop Stroke Hip Hop Stroke is a musical multimedia stroke literacy intervention designed to raise stroke awareness and behavioral intent to call 911 for acute stroke.
Health Disparities

Health disparities are preventable differences in the burden of disease, injury, violence, or opportunities to achieve optimal health that are experienced by socially disadvantaged populations. 1
Despite significant progress in research, practice, and policy, disparities in youth health risk behaviors persist. Populations can be defined by factors such as race or ethnicity, gender, education or income, disability, geographic location (e.g., rural or urban), or sexual orientation.
Health disparities are inequitable and are directly related to the historical and current unequal distribution of social, political, economic, and environmental resources.
Health disparities result from multiple factors, including
- Environmental threats
- Inadequate access to health care
- Individual and behavioral factors
- Educational inequalities
We can improve health risks and reduce disparities and inequities by addressing social determinants of health .
The Education–Health Disparities Link
Health disparities are related to inequities in education. Dropping out of school is associated with multiple social and health problems. 2-3 Overall, individuals with less education are more likely to experience a number of health risks, such as obesity, substance abuse, and intentional and unintentional injury, compared with individuals with more education. 4 Higher levels of education are associated with a longer life and an increased likelihood of obtaining or understanding basic health information and services needed to make appropriate health decisions. 5-7
At the same time, good health is associated with academic success . Higher levels of protective health behaviors and lower levels of health risk behaviors are been associated with higher academic grades among high school students. 8

Health risks such as teenage pregnancy, poor dietary choices, inadequate physical activity, physical and emotional abuse, substance abuse, and gang involvement have a significant impact on how well students perform in school. 9-13
Addressing Adolescent Health Disparities
Lgbtq+ youth face mental health challenges.
The mental health of LGBTQ+ youth is worsening.
The Youth Risk Behavior Data Summary & Trends Report: 2011- 2021 brought into clear focus the level of distress many youth are experiencing. Of serious concern is that LGBQ+ youth are experiencing especially high rates of poor mental health.
Schools are a vital lifeline to help students struggling with their mental health . Research has shown that when youth feel connected , they do better not just in adolescence, but into adulthood. When schools focus on creating safe and supportive environments that support LGBQ+ youth, all youth have improved mental health outcomes.
When schools implement CDC’s What Works In Schools program, we see improvements in student mental health.
In 2021, CDC found that—
- 69% of LGBQ+ students experienced persistent feelings of sadness or hopelessness.
- 45% of LGBQ+ students seriously considered attempting suicide.
These percentages are higher than those of their heterosexual peers.
The What Works In Schools program supports schools in creating safer and more supportive environments that protect student mental health, while also supporting quality health education and connecting students to needed health services.
- Health Disparities and Populations at Risk
- HIV in the United States by Age
- Adolescents and Young Adults
- Youth Risk Behavior Surveillance System (YRBSS)
- School Health Profiles
- NCHHSTP Strategic Plan 2022-2026
- NCHHSTP Social Determinants of Health
- National HIV/AIDS Strategy (2022-2025)
- YRBS Data Summary & Trends Report 2011 - 2021
- CDC. Community Health and Program Services (CHAPS): Health Disparities Among Racial/Ethnic Populations. Atlanta: U.S. Department of Health and Human Services; 2008
- McCarty C, Mason W, Kosterman R, Hawkins J, Lengua L, McCauley E. Adolescent school failure predicts later depression among girls. Journal of Adolescent Health 2008;43:180–187.
- Ellickson P, Saner H, McGuigan K. Profiles of violent youth: substance use and concurrent problems. American Journal of Public Health 1997;87(6):985–991.4
- U.S. Department of Health and Human Services. Healthy People 2010 Objectives: Educational and Community Based Programs; 2000.
- Liao Y, McGee D, Kaufman J, Cao G, Cooper R. Socioeconomic status and morbidity in the last years of life. American Journal of Public Health 1999;89(4):569–572.
- Jemal A, Thun M, Ward E, Henley J, Cokkinides V, Murray T. Mortality from leading causes by education and race in the United States, 2001. American Journal of Preventive Medicine 2008;34(1):1–8.e7.
- Breese P, Burman W, Goldberg S, Weis S. Education level, primary language, and comprehension of the informed consent process. Journal of Empirical Research on Human Research Ethics 2007;2(4):69–79.
- Rasberry CN, Tiu GF, Kann L, McManus T, Michael SL, Merlo CL, Lee SM, Bohm MK, Annor F, Ethier K. Health-related behaviors and academic achievement among high school students—United States, 2015. MMWR Morb Mortal Wkly Rep 2917;66:922-927.
- Choi Y. Academic achievement and problem behaviors among Asian Pacific Islander American adolescents. Journal of Youth Adolescence 2007;(36)4:403–415.
- Stuart S, Sachs M, Lidicker J, Brett S, Wright A, Libonati J. Decreased scholastic achievement in overweight middle school students. Obesity 2008;16(7):1535–1538.
- Valois RF, MacDonald JM, Bretous L, Fischer MA, Drane JW. Risk factors and behaviors associated with adolescent violence and aggression. American Journal of Health Behavior 2002;26(6):454–464.
- Chomitz V, Slining M, McGowan R, Mitchell S, Dawson G, Hacker K. Is there a relationship between physical fitness and academic achievement? Positive results from public school children in the Northeastern United States. Journal of School Health 2009;79(1):30-37.
- Field T, Diego M, Sanders CE. Exercise is positively related to adolescents’ relationships and academics. Adolescence 2001;36(141):105-110.
To receive email updates about this page, enter your email address:
- Health Equity
- Disparities in HIV/AIDS, Viral Hepatitis, STDs, and TB
- Healthy Schools
- Minority Health
- Social Determinants of Health
Exit Notification / Disclaimer Policy
- The Centers for Disease Control and Prevention (CDC) cannot attest to the accuracy of a non-federal website.
- Linking to a non-federal website does not constitute an endorsement by CDC or any of its employees of the sponsors or the information and products presented on the website.
- You will be subject to the destination website's privacy policy when you follow the link.
- CDC is not responsible for Section 508 compliance (accessibility) on other federal or private website.
We're still accepting applications for fall 2024!
- Skip to content
- Skip to search
- Accessibility Policy
- Report an Accessibility Issue

Lending her voice to promote health equity: ‘You are always doing public health’

Jodi-Ann Burey, MPH ’14
- Health Behavior and Health Education
April 29, 2024
This spring marked six years since Jodi-Ann Burey, MPH ’14, had surgery to remove a tumor from her spinal cord. The effect on her health was harrowing enough, but it also took three years to properly diagnose the tumor.
It was a life-altering experience in more ways than one. Coming to terms with having cancer can be especially daunting, but for Burey, she knew from her lived experience as a Black woman and her classroom experience that health inequities don’t necessarily stop at the door to the doctor’s office.
Burey had learned all about health inequity while earning her Master of Public Health in Health Behavior and Health Education at the University of Michigan School of Public Health . She had become one of those data points.
“I was living out that experience—it was surreal,” Burey said. “One of the strategies I would use as a Black woman with institutional privileges to navigate the healthcare system is, I would go to appointments with a Michigan sweatshirt on, trying to find a way to mention that I have a degree in public health.
“I used my skill set of knowing how to read health research papers and understanding how a lot of that research was done to be able to position myself as a partner in my diagnosis journey.”
I was living out that experience—it was surreal. One of the strategies I would use as a Black woman with institutional privileges to navigate the healthcare system is, I would go to appointments with a Michigan sweatshirt on, trying to find a way to mention that I have a degree in public health.”
Her public health knowledge gave her the confidence to discuss complex medical topics with her physicians and empathize with her family’s concerns. Living through this ordeal not only transformed her personally but also shaped her career trajectory, deepening her understanding of her life’s fragility and urgency.
She transitioned from a global health practitioner to working for herself, leveraging her expertise in public health to help others with shared experiences.
“Going through that process made a lot of things just more pressing for me career wise, especially around social issues and trying not to be so abstract,” she said. “We’re talking about actual human beings and the things that they need to live a good life.”
Podcast inspires community dialogue
This transformation inspired her to start the podcast Black Cancer , about the lives of people of color and their cancer journeys. She also is investing her time and energy into learning more about disability rights and experiences.
“I didn't have anyone that I could talk to really about my own experience,” Burey said. “For a period after my surgery, I only really wanted to talk to other people who had cancer or were caregivers of people who had cancer. That became such a solace for me.”
The podcast demonstrated the impact such initiatives can have on communities seeking comfort and understanding. More importantly, it underscored how a public health perspective has informed her understanding and commentary on social issues.
The way I envision my work aligns with a lot of the public health frameworks that come from the discipline of Health Behavior and Health Education I learned at Michigan Public Health. I think that grounding in public health shapes a lot of my commentary.”
Burey has become a sought-after speaker and writer. Her forthcoming book, “AUTHENTIC” (Flatiron Books, 2025) extends the ideas first presented in her TED Talk, The Myth of Bringing Your Full Authentic Self to Work , disrupting traditional narratives about racism at work. She also is a regular contributor on KUOW-NPR in Seattle, where she has called home since leaving Ann Arbor in 2014.
“The way I envision my work aligns with a lot of the public health frameworks that come from the discipline of Health Behavior and Health Education I learned at Michigan Public Health,” Burey said. “ I think that grounding in public health shapes a lot of my commentary.”
Burey has conducted more than 100 keynotes, panels, conversations, and interviews, where she takes a stance on issues such as violence and policing, arguing that violence should be treated as a public health issue rather than solely a criminal one. She draws connections to factors such as income inequality, housing, healthcare access, suggesting that these elements contribute more to community health and violence prevention than an increased police presence.
Recently on KUOW-NPR, Burey discussed Seattle’s new dog parks through a public health lens.
“Seattle has something like 50,000 more dogs than children—this is a public health issue about green space, park management, urban infrastructure, social isolation and loneliness,” she said, echoing her HBHE mentors at Michigan Public Health Cleo Caldwell and Laurie Lachance. “My public health training allows me to be nimble and creative in the types of work that I do, the speaking that I do, the ideas that I create in my writing.
“So, whether I’m talking about dog parks, or violence, or weathering and chronic stress, or survivorship and the work of caregiving, public health is all of that. I don't know if I would be able to navigate these conversations without that training.”
Burey, who was born in Jamaica and grew up in Queens, New York City, has more than 15 years of entrepreneurial, corporate, non-profit and start-up professional experience. One of her recent ventures is co-creating Lit Lounge, a curated book collection and author interview series that she hosts.
‘You are always doing public health’
While at Michigan Public Health, part of Burey’s academic journey included a summer practicum through the William Davidson Institute, where she consulted for a global health organization focused on work in Malawi and Mozambique. This opportunity led to a three-month stint in Malawi performing an organizational assessment. Her insights into administrative and organizational design complemented their understanding of the programmatic aspects of the organization's work.
Before she graduated from Michigan, she accepted a full-time job at an NGO based in Seattle, where she contributed to health systems work, traveling to Malawi over a dozen times over five years. Despite never anticipating a career in global health, Burey found fulfillment in this field.
Since the pandemic, she has been working on her own, which has allowed her to have more freedom professionally.
Burey said she is humbled to be invited to speak at the school’s graduation and plans to convey a powerful message at the ceremony.
To realize that my relationship to this university matters enough that they would think about me and invite me to come back to speak for graduation, I was just very honored by that. I am very inspired to speak to public health students because I cannot imagine what the last four years have been like for them—living, working and going to school in a pandemic."
“To realize that my relationship to this university matters enough that they would think about me and invite me to come back to speak for graduation, I was just very honored by that,” she said. “I am very inspired to speak to public health students because I cannot imagine what the last four years have been like for them—living, working and going to school in a pandemic.
“What I want to share with the students, based on my own career path, is: You are always doing public health. The work students did at Michigan Public Health, what they learned, the relationship that they built, it’s never going to leave them. Even if they ‘leave the profession,’ they will always be doing public health, because I’m always doing public health. I want them to know, ‘No matter where you go, no matter how your life or career transitions, you are always a part of this team.’”
Jodi-Ann Burey will be the guest speaker for the University of Michigan School of Public Health graduating Class of 2024 on May 2 at the historic Hill Auditorium.
- Interested in public health? Learn more here.
- Learn more about the Health Behavior and Health Education program.
- Read more stories about students, alumni, faculty, and staff.
- Support research and engaged learning at the School of Public Health.
- We Are Michigan Public Health
- Health Communication
- Health Disparities
Recent Posts
- Lending her voice to promote health equity: 'You are always doing public health'
- 'Ready to do her part' in shaping a future with environmental health policy
- Fulbright Scholar takes aim at sustainable food systems in Indonesia
- Internship in Kenya enriches Global Health Epidemiology personal journey
What We’re Talking About
- Adolescent Health
- Air Quality
- Alternative Therapies
- Biostatistics
- Breastfeeding
- Child Health
- Chronic Disease
- Community Partnership
- Computational Epidemiology and Systems Modeling
- Disaster Relief
- Diversity Equity and Inclusion
- Engaged Learning
- Entrepreneurship
- Environmental Health
- Epidemiologic Science
- Epidemiology
- Epigenetics
- Field Notes
- First Generation Students
- Food Policy
- Food Safety
- General Epidemiology
- Global Health Epidemiology
- Global Public Health
- Graduation 2019
- HMP Executive Masters
- Health Care
- Health Care Access
- Health Care Management
- Health Care Policy
- Health Informatics
- Health for Men
- Health for Women
- Heart Disease
- Hospital Administration
- Hospital and Molecular Epidemiology
- Industrial Hygiene
- Infectious Disease
- Internships
- LGBT Health
- Maternal Health
- Mental Health
- Mobile Health
- Occupational and Environmental Epidemiology
- Pain Management
- Pharmaceuticals
- Precision Health
- Professional Development
- Reproductive Health
- Scholarships
- Sexual Health
- Social Epidemiology
- Social Media
- Student Organizations
- Urban Health
- Urban Planning
- Value-Based Care
- Water Quality
- What Is Public Health?
Information For
- Prospective Students
- Current Students
- Alumni and Donors
- Community Partners and Employers
- About Public Health
- How Do I Apply?
- Departments
- Findings magazine
Student Resources
- Career Development
- Certificates
- The Heights Intranet
- Update Contact Info
- Report Website Feedback
- Skip to main content
- Skip to FDA Search
- Skip to in this section menu
- Skip to footer links

The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
U.S. Food and Drug Administration
- Search
- Menu
- Medical Devices
- Medical Devices News and Events
FDA Launches Health Care at Home Initiative to Help Advance Health Equity
Initiative aims to better position agency to address health care needs by moving care into the home setting
FOR IMMEDIATE RELEASE April 23, 2024
The following is attributed to Jeff Shuren, M.D., J.D., director of the FDA's Center for Devices and Radiological Health (CDRH) and Michelle Tarver, M.D., Ph.D., deputy director for transformation at CDRH
Clinical care is undergoing an evolution that has been accelerated over the last few years by the COVID-19 public health emergency. Health care has primarily been centered on health care systems and their components—hospitals, clinics, providers, and payers. However, many challenges persist, such as primary care physician and specialist shortages, significant increases in health care costs, higher chronic disease prevalence rates, and often the inability to meet the health care needs of millions of people who have no or limited access to health care systems. People from various racial and ethnic minority populations and those who live in rural communities and lower-income neighborhoods are impacted the most by these system challenges, which furthers health disparities across the nation.
Today, the U.S. Food and Drug Administration is announcing the launch of a new initiative, Home as a Health Care Hub, to help reimagine the home environment as an integral part of the health care system, with the goal of advancing health equity for all people in the U.S. While many care options are currently attempting to use the home as a virtual clinical site, very few have considered the structural and critical elements of the home that will be required to absorb this transference of care. Moreover, devices intended for use in the home tend to be designed to operate in isolation rather than as part of an integrated, holistic environment. As a result, patients may have to use several disparate medical devices, some never intended for the home environment, rather than interact with medical-grade, consumer-designed, customizable technologies that seamlessly integrate into an individual person's lifestyle.
The FDA's Center for Devices and Radiological Health (CDRH) has contracted with an architectural firm that intentionally designs innovative buildings with health and equity in mind, to consider the needs of variable models of a home and tailor solutions with opportunities to adapt and evolve in complexity and scale. The hub will be designed as an Augmented Reality/Virtual Reality (AR/VR)-enabled home prototype and is expected to be completed later this year.
This partnership includes collaboration with patient groups, health care providers, and the medical device industry to build the Home as a Health Care Hub. This prototype will serve as an idea lab, not only to connect with populations most affected by health inequity, but also for medical device developers, policy makers, and providers to begin developing home-based solutions that advance health equity. Existing models that have examined care delivery at home have found great patient satisfaction, good adherence, and potential cost savings to health care systems. By beginning with dwellings in rural locations and lower-income communities, the planned prototype will be intentionally designed with the goal of advancing health equity.
The FDA is using diabetes as an example health condition for the hub prototype given the impacts over the lifecycle of someone living with this condition. According to the Centers for Disease Control and Prevention ( CDC ), over $300 billion per year was spent on medical costs for diabetes in the U.S. in 2022. This is a 35% increase over the past decade, which is disproportionately borne by underserved communities and communities of color. Diabetes is a condition that impacts most major organs and can result in significant morbidity and early mortality, including cardiovascular disease, kidney failure, blindness, and amputations.
To increase access to health care and maximize health outcomes, it is critical that the delivery of personalized care has people at the center. By shifting the care model from systems to people, the health care system can triage scarce resources to those with the most urgent and critical needs and tailor personalized care for those managing chronic conditions. The Home as a Health Care Hub prototype is the beginning of the conversation—helping device developers consider novel design approaches, aiding providers to consider opportunities to educate patients and extend care options, generating discussions on value-based care paradigms, and opening opportunities to bring clinical trials and other evidence generation processes to underrepresented communities through the home.
As a part of CDRH's strategic priority to advance health equity , CDRH continues to support innovation that addresses health equity by moving care, as well as prevention and wellness, into the home setting. CDRH is committed to fostering innovation that improves public health by launching the Home as a Health Care Hub effort to enable solutions that seamlessly integrate medical devices and health care, prevention and wellness into people's lives, leading to a longer, higher quality life for all.
Additional Resources:
- CDRH Strategic Priorities and Updates

COMMENTS
Eliminating racial health inequities requires a movement away from disparities as the focus of research and toward a research agenda centered on achieving equity by dismantling structural racism.
Research Framework for Health Disparities. The Research Framework in Exhibit 1 was developed by the National Institutes of Health (NIH) National Institute on Minority Health and Health Disparities (NIMHD). This framework is based on an evolving conceptualization of factors relevant to the understanding and promotion of minority health and to the understanding and reduction of health disparities.
A health disparity is a preventable difference between different groups of people in. health status. pain and suffering. rates of disease, disability, injury, and violence. lifespan, life expectancy, or mortality. access to health care. and other measures. Populations affected by health disparities contend with social, economic, and ...
Science Collaborative for Health disparities and Artificial intelligence bias Reduction. An innovative cloud computing platform where you can: Access and link population, behavioral, and social determinants of health datasets. Obtain cloud ready-to-use data analysis tools and training. Join multi-disciplinary, multi-career levels research ...
NIH is committed to: 1. Improving minority health and reducing health disparities. 2. Removing the barriers to advancing health disparities research. Health disparities are preventable differences in health status and outcomes that adversely affect certain populations. Research on health disparities examines the influence of environment, social ...
A more equitable future. The Science of Health Disparities Research is an in-depth volume for comprehensive information on conducting clinical and translational health disparities studies. NIMHD researchers—along with leading experts from around the country—have written this 26-chapter textbook to cover the spectrum of health disparities ...
10 January 2024. Health disparities or health inequalities are preventable differences in health outcomes in groups or populations as a result of social structure, access to services and ...
Discussed topics include stroke as an indicator of broad health inequity, challenges and opportunities in health disparities research, the need to diversify the research workforce, and the ongoing efforts and struggles to establish trust with disadvantaged communities during the COVID-19 pandemic.
Integrates the various disciplines of the science of health disparities in one comprehensive volume. The Science of Health Disparities Research is an indispensable source of up-to-date information on clinical and translational health disparities science.Building upon the advances in health disparities research over the past decade, this authoritative volume informs policies and practices ...
Minority health and health disparities are emphasized as 1 of 5 cross-disciplinary research areas fundamental in nutrition sciences (the complete list of topics is provided in the SPNR). The plan highlights the importance of understanding the factors that contribute to NHDs and developing interventions that can improve health.
The Top 100 Cited Papers in Health Care Disparities: a Bibliometric Analysis Karan Arul1 & Addisu Mesfin1 Received: 3 August 2016/Accepted: 8 September 2016 # W. Montague Cobb-NMA Health Institute 2016 Abstract Health care disparities research is an exponentially growing and multi-faceted field. Our objective was to identify
Highlighting Research on Health Disparities. A collection aimed at highlighting NPP articles and commentaries that address disparities related to gender, race, ethnicity, LGBTQ+ individuals, and ...
A health care disparity typically refers to differences between groups in health insurance coverage, affordability, access to and use of care, and quality of care. The terms "health inequality ...
Advancing health equity and eliminating health disparities have been and continue to be critical factors to PCD in addressing these topic areas. Healthy People 2020 defines health equity as the attainment of the highest level of health for all people (2). According to Healthy People 2020, "Achieving health equity requires valuing everyone ...
Black women in the United States experienced substantial improvements in health during the last century, yet health disparities persist. Black women continue to experience excess mortality relative to other U.S. women, including—despite overall improvements among Black women—shorter life expectancies 1 and higher rates of maternal mortality. 2 Moreover, Black women are disproportionately ...
The second and third most common topics were disparities related to sex and mental health condition. Very few studies focused on sexual or gender identity or homelessness. Understanding where data is lacking, according to the research team, can help VA further address health care disparities.
AHRQ has reports and data on disparities in health care related to race, ethnicity, and socioeconomic status. Healthcare disparities are differences in access to or availability of medical facilities and services and variation in rates of disease occurrence and disabilities between population groups defined by socioeconomic characteristics such ...
Among Black adults, 55% say they have ever had at least one of six negative experiences with doctors or other health care providers. Black Americans offer a mixed assessment of the progress that has been made improving health outcomes for Black people: 47% say health outcomes for Black people have gotten better over the past 20 years, while 31% ...
Advancing Racial Equity in U.S. Health Care. The Commonwealth Fund 2024 State Health Disparities Report. Dr. Reshma Chugani checks 7-year-old Zoe Oliver's ears during a medical visit at Atlanta Children's Clinical Center on September 29, 2023. Health care system performance varies widely by race and ethnicity, both within states and between ...
Lack of diversity of research participants limits generalizability of medical knowledge and subsequent health benefits for these communities, 2 which can, in turn, exacerbate health disparities. Investigators need to carefully monitor the changing reproductive health legal landscape in the context of state laws to ensure continued participation ...
In early 2020, shortly before the United States began to shut down due to the COVID-19 pandemic, leadership at the National Institute of Mental Health (NIMH) recognized the need to address the persistent mental health care disparities that continue to impact millions in this country, despite the significant advances made in mental health with respect to access and quality of care.
This page provides a comprehensive exploration of health disparities research paper topics, catering to students in health sciences who are tasked with writing impactful research papers. With a focus on addressing health inequities, the page offers a diverse and extensive list of research paper topics categorized into ten distinct areas.
KFF research has documented racial and ethnic disparities in health care that affect people of all ages, including access to care, use of services, outcomes, and experiences with unfair treatment ...
Health Disparities and Stroke. Stroke continues to be a major focus of NINDS health disparities research efforts, as it remains one of the largest and most burdensome disparities in neurological health with substantial opportunities for improving outcomes. NINDS supports research to better understand stroke disparities and to inform the development of effective interventions in specific ...
Health Disparities. Health disparities are preventable differences in the burden of disease, injury, violence, or opportunities to achieve optimal health that are experienced by socially disadvantaged populations. 1. Despite significant progress in research, practice, and policy, disparities in youth health risk behaviors persist.
Jodi-Ann Burey, MPH '14, turned her challenging cancer diagnosis and treatment journey into a passionate fight for health equity by starting a podcast on cancer experiences and advocating for minority health as a public speaker and writer.
Topics; Research Faculty; Consulting & Evaluation ... for an investigation into oral health care disparities of a preventive care program. Methods: Electronic health record data for eligible children in a dental accountable care organization of 30 offices, in Oregon, were extracted iteratively from January 1, 2014, through March 31, 2022 ...
Patients went out-of-network 3.5 times more often to see a behavioral health clinician than a medical/surgical clinician in 2021, and up to 20 times more often for certain behavioral health visits, according to a new study by RTI International. For example, patients went out-of-network 8.9 times more often to see a psychiatrist, 10.6 times more often to see a psychologist, 6.2 times more often ...
The ability to work on a thesis that ignites a conversation about cancer detection and health disparities helps Haas honor her grandmother and foster her passion for understanding societal implications on health. "I want to understand how racial, ethnic and socioeconomic inequalities change with increasing ability to prevent disease," Haas ...
Today, the U.S. Food and Drug Administration is announcing the launch of a new initiative, Home as a Health Care Hub, to help reimagine the home environment as an integral part of the health care ...