
- Advanced Life Support
- Endocrinology
- Gastroenterology
- Infectious disease
- Intensive care
- Palliative Care
- Respiratory
- Rheumatology
- Haematology
- Endocrine surgery
- General surgery
- Neurosurgery
- Ophthalmology
- Plastic surgery
- Vascular surgery
- Abdo examination
- Cardio examination
- Neurolo examination
- Resp examination
- Rheum examination
- Vasc exacmination
- Other examinations
- Clinical Cases
- Communication skills
- Prescribing


Dementia case study with questions and answers

Dementia case study with questions and answers
Common dementia exam questions for medical finals, OSCEs and MRCP PACES
The case below illustrates the key features in the assessment of a patient with dementia or undiagnosed memory decline. It works through history, examination and investigations – click on the plus symbols to see the answers to each question
Part 1: Mavis
- Mavis is an 84-year old lady, referred to you in the memory clinic for assessment of memory impairment. She attends in the company of her son and daughter-in-law.
- On the pre-clinic questionnaire her son has reported a severe deterioration in all aspects of her cognition over the past 12 months.
- The patient herself acknowledges that there have been memory problems, but feels it is just her short term memory that is an issue.
Question 1.
- To begin the history, start broadly. Build rapport and establish both the patient’s view on memory impairment (if any) and the family’s (or other collateral history).
- Patient’s (and collateral) view of memory decline
- Biographical history
- Objective view of memory decline (e.g. knowledge of current affairs)
- Impact of memory decline on day-to-day living and hobbies
- Social history, including safety and driving
- General medical history (especially medications)
- See below for details on these…
Question 2.
- Is it for everything or are specific details missed out/glossed over?
- Try to pin down specific details (e.g. names of people/places).
- At what time in chronological order do things start to get hazy?
Question 3.
- If under 12 years this will lead to additional point being awarded on some cognitive tests
- Ask about long term memories, e.g. wedding day or different jobs
- Then move on to more recent memories, e.g. last holiday
Question 4.
- If your patient watches the news/read newspapers on a regular basis, ask them to recount the headlines from the past few days.
- Be sure to look for specifics to prevent your patient masking memory deficiencies with broad statements. For example: “The government are incompetent, aren’t they?!” should be clarified by pinning down exactly why they are incompetent, for example: “Jeremy Hunt”.
- If they like to read, can they recall plotlines from current books or items from magazines?
- If they watch TV, can they recount recent plot lines from soaps, or formats of quiz shows?
Question 5.
- Ask about hobbies and other daily activities, and whether or not these have declined recently.
- If your patient no longer participates in a particular hobby, find out why: is it as a result of a physical impairment (e.g. arthritis making cooking difficult), or as the result of a loss of interest/ability to complete tasks (e.g. no longer able to complete crosswords/puzzles).
- Once you have a good idea of the memory decline itself, begin to ask about other features. Including a social and general medical history.
Question 6.
- Review their social history and current set-up, and also subjective assessments from both patient and family over whether or not the current arrangements are safe and sustainable as they are.
- Previous and ongoing alcohol intake
- Smoking history
- Still driving (and if so, how safe that is considered to be from collateral history)
- Who else is at home
- Any package of care
- Upstairs/downstairs living
- Meal arrangements (and whether weight is being sustained).
- Of all these issues, that of driving is perhaps one of the most important, as any ultimate diagnosis of dementia must be informed (by law) to both the DVLA and also the patient’s insurers. If you feel they are still safe to drive despite the diagnosis, you may be asked to provide a report to the DVLA to support this viewpoint.
Now perform a more generalised history, to include past medical history and – more importantly – a drug history.
Question 7.
- Oxybutynin, commonly used in primary care for overactive bladder (anticholinergic side effects)
- Also see how the medications are given (e.g. Dossett box)
- Are lots of full packets found around the house?
Part 2: The History
On taking a history you have found:
- Mavis was able to give a moderately detailed biographical history, but struggled with details extending as far back as the location of her wedding, and also her main jobs throughout her life.
- After prompting from her family, she was able to supply more information, but it was not always entirely accurate.
- Her main hobby was knitting, and it was noted that she had been able to successfully knit a bobble hat for her great-grand child as recently as last month, although it had taken her considerably longer to complete than it might have done a few years previously, and it was a comparatively basic design compared to what she has been able to create previously.
- She has a few children living in the area, who would frequently pop in with shopping, but there had been times when they arrived to find that she was packed and in her coat, stating that she was “just getting ready to go home again”.
- She had been helping occasionally with the school run, but then a couple of weekends ago she had called up one of her sons – just before she was due to drive over for Sunday lunch – and said that she could not remember how to drive to his house.
- Ever since then, they had confiscated her keys to make sure she couldn’t drive. Although she liked to read the paper every day, she could not recall any recent major news events. Before proceeding to examine her, you note that the GP referral letter has stated that her dementia screen investigations have been completed.
Question 8.
- Raised WCC suggests infection as a cause of acute confusion
- Uraemia and other electrolyte disturbances can cause a persistent confusion.
- Again, to help rule out acute infection/inflammatory conditions
- Liver failure can cause hyperammonaemia, which can cause a persistent confusion.
- Hyper- or hypothyroidism can cause confusion.
- B12 deficiency is an easily missed and reversible cause of dementia.
- This looks for space occupying lesions/hydrocephalus which may cause confusion.
- This can also help to determine the degree of any vascular component of an ultimately diagnosed dementia.
Part 3: Examination
- With the exception of age-related involutional changes on the CT head (noted to have minimal white matter changes/small vessel disease), all the dementia screen bloods are reassuring.
- You next decide to perform a physical examination of Mavis.
Question 9.
- Important physical findings that are of particular relevance to dementia, are looking for other diseases that may have an effect on cognition.
- To look for evidence of stroke – unlikely in this case given the CT head
- Gait (shuffling) and limb movements (tremor, rigidity, bradykinesia)
- Affect is also important here and may also point to underlying depression
- Pay attention to vertical gaze palsy, as in the context of Parkinsonism this may represent a Parkinson plus condition (e.g. progressive supranuclear palsy).
- It is also useful to look at observations including blood pressure (may be overmedicated and at risk of falls from syncope) and postural blood pressure (again, may indicate overmedication but is also associated with Parkinson plus syndromes e.g. MSA)
Part 4: Cognitive Testing
- On examination she is alert and well, mobilising independently around the clinic waiting room area. A neurological examination was normal throughout, and there were no other major pathologies found on a general examination.
- You now proceed to cognitive testing:
Question 10.
- Click here for details on the MOCA
- Click here for details on the MMSE
- Click here for details on the CLOX test
Part 5: Diagnosis
- Mavis scores 14/30 on a MOCA, losing marks throughout multiple domains of cognition.
Question 11.
- Given the progressive nature of symptoms described by the family, the impairment over multiple domains on cognitive testing, and the impact on daily living that this is starting to have (e.g. packing and getting ready to leave her own home, mistakenly believing she is somewhere else), coupled with the results from her dementia screen, this is most likely an Alzheimer’s type dementia .
Question 12.
- You should proceed by establishing whether or not Mavis would like to be given a formal diagnosis, and if so, explain the above.
- You should review her lying and standing BP and ECG, and – if these give no contraindications – suggest a trial of treatment with an acetylcholinesterase inhibitor, such as donepezil.
- It is important to note the potential side effects – the most distressing of which are related to issues of incontinence.
- If available, put her in touch with support groups
- Given the history of forgetting routes before even getting into the care, advise the patient that she should stop driving and that they need to inform the DVLA of this (for now, we will skip over the depravation of liberty issues that the premature confiscation of keys performed by the family has caused…)
- The GP should be informed of the new diagnosis, and if there are concerns over safety, review by social services for potential support should be arranged.
- Follow-up is advisable over the next few months to see whether the trial of treatment has been beneficial, and whether side effects have been well-tolerated.
Now click here to learn more about dementia
Perfect revision for medical students, finals, osces and mrcp paces, …or click here to learn about the diagnosis and management of delirium.
Change Password
Your password must have 6 characters or more:.
- a lower case character,
- an upper case character,
- a special character
Password Changed Successfully
Your password has been changed
Create your account
Forget yout password.
Enter your email address below and we will send you the reset instructions
If the address matches an existing account you will receive an email with instructions to reset your password
Forgot your Username?
Enter your email address below and we will send you your username
If the address matches an existing account you will receive an email with instructions to retrieve your username

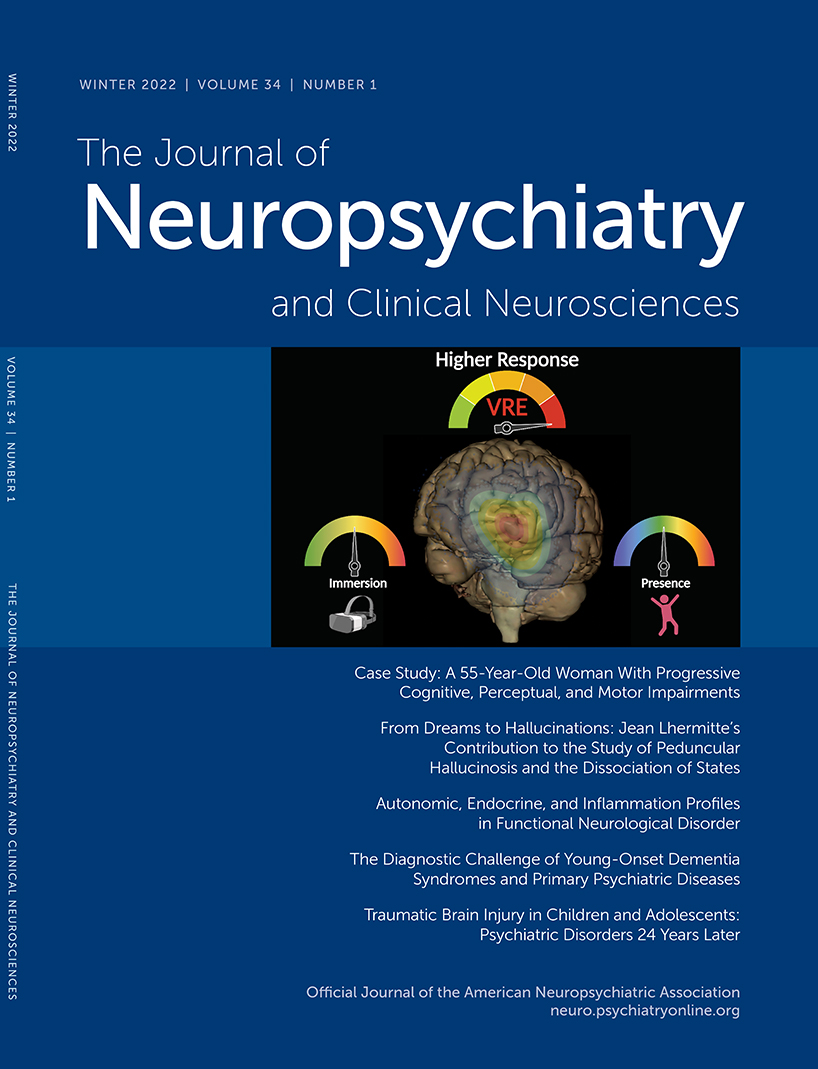
- Spring 2024 | VOL. 36, NO. 2 CURRENT ISSUE pp.A4-174
- Winter 2024 | VOL. 36, NO. 1 pp.A5-81
The American Psychiatric Association (APA) has updated its Privacy Policy and Terms of Use , including with new information specifically addressed to individuals in the European Economic Area. As described in the Privacy Policy and Terms of Use, this website utilizes cookies, including for the purpose of offering an optimal online experience and services tailored to your preferences.
Please read the entire Privacy Policy and Terms of Use. By closing this message, browsing this website, continuing the navigation, or otherwise continuing to use the APA's websites, you confirm that you understand and accept the terms of the Privacy Policy and Terms of Use, including the utilization of cookies.
Case Study 1: A 55-Year-Old Woman With Progressive Cognitive, Perceptual, and Motor Impairments
- Scott M. McGinnis , M.D. ,
- Andrew M. Stern , M.D., Ph.D. ,
- Jared K. Woods , M.D., Ph.D. ,
- Matthew Torre , M.D. ,
- Mel B. Feany , M.D., Ph.D. ,
- Michael B. Miller , M.D., Ph.D. ,
- David A. Silbersweig , M.D. ,
- Seth A. Gale , M.D. ,
- Kirk R. Daffner , M.D.
Search for more papers by this author
CASE PRESENTATION
A 55-year-old right-handed woman presented with a 3-year history of cognitive changes. Early symptoms included mild forgetfulness—for example, forgetting where she left her purse or failing to remember to retrieve a take-out order her family placed—and word-finding difficulties. Problems with depth perception affected her ability to back her car out of the driveway. When descending stairs, she had to locate her feet visually in order to place them correctly, such that when she carried her dog and her view was obscured, she had difficulty managing this activity. She struggled to execute relatively simple tasks, such as inserting a plug into an outlet. She lost the ability to type on a keyboard, despite being able to move her fingers quickly. Her symptoms worsened progressively for 3 years, over which time she developed a sad mood and anxiety. She was laid off from work as a nurse administrator. Her family members assumed responsibility for paying her bills, and she ceased driving.
Her past medical history included high blood pressure, Hashimoto’s thyroiditis with thyroid peroxidase antibodies, remote history of migraine, and anxiety. Medications included mirtazapine, levothyroxine, calcium, and vitamin D. She had no history of smoking, drinking alcohol, or recreational drug use. There was no known family history of neurologic diseases.
What Are Diagnostic Considerations Based on the History? How Might a Clinical Examination Help to Narrow the Differential Diagnosis?
Insidious onset and gradual progression of cognitive symptoms over the course of several years raise concern for a neurodegenerative disorder. It is helpful to consider whether or not the presentation fits with a recognized neurodegenerative clinical syndrome, a judgment based principally on familiarity with syndromes and pattern recognition. Onset of symptoms before age 65 should prompt consideration of syndromes in the spectrum of frontotemporal dementia (FTD) and atypical (nonamnesic) presentations of Alzheimer’s disease (AD) ( 1 , 2 ). This patient’s symptoms reflect relatively prominent early dysfunction in visual-spatial processing and body schema, as might be observed in posterior cortical atrophy (PCA), although the history also includes mention of forgetfulness and word-retrieval difficulties. A chief goal of the cognitive examination would be to survey major domains of cognition—attention, executive functioning, memory, language, visual-spatial functioning, and higher somatosensory and motor functioning—to determine whether any domains stand out as more prominently affected. In addition to screening for evidence of focal signs, a neurological examination in this context should assess for evidence of parkinsonism or motor neuron disease, which can coexist with cognitive changes in neurodegenerative presentations.
The patient’s young age and history of Hashimoto’s thyroiditis might also prompt consideration of Hashimoto’s encephalopathy (HE; also known as steroid-responsive encephalopathy), associated with autoimmune thyroiditis. This syndrome is most likely attributable to an autoimmune or inflammatory process affecting the central nervous system. The time course of HE is usually more subacute and rapidly progressive or relapsing-remitting, as opposed to the gradual progression over months to years observed in the present case ( 3 ).
The patient’s mental status examination included the Montreal Cognitive Assessment (MoCA), a brief global screen of cognition ( 4 ), on which she scored 12/30. There was evidence of dysfunction across multiple cognitive domains ( Figure 1 ). She was fully oriented to location, day, month, year, and exact date. When asked to describe a complex scene from a picture in a magazine, she had great difficulty doing so, focusing on different details but having trouble directing her saccades to pertinent visual information. She likewise had problems directing her gaze to specified objects in the room and problems reaching in front of her to touch target objects in either visual field. In terms of other symptoms of higher order motor and somatosensory functioning, she had difficulty demonstrating previously learned actions—for example, positioning her hand correctly to pantomime holding a brush and combing her hair. She was confused about which side of her body was the left and which was the right. She had difficulty with mental calculations, even relatively simple ones such as “18 minus 12.” In addition, she had problems writing a sentence in terms of both grammar and the appropriate spacing of words and letters on the page.
FIGURE 1. Selected elements of a 55-year-old patient’s cognitive examination at presentation a
a BNT-15=Boston Naming Test (15-Item); MoCA=Montreal Cognitive Assessment.
On elementary neurologic examination she had symmetrically brisk reflexes, with spread. She walked steadily with a narrow base, but when asked to pass through a doorway she had difficulty finding her way through it and bumped into the door jamb. Her elemental neurological examination was otherwise normal, including but not limited to brisk, full-amplitude vertical eye movements, normal visual fields, no evidence of peripheral neuropathy, and no parkinsonian signs such as slowness of movement, tremor, or rigidity.
How Does the Examination Contribute to Our Understanding of Diagnostic Considerations? What Additional Tests or Studies Are Indicated?
The most prominent early symptoms and signs localize predominantly to the parietal association cortex: The patient has impairments in visual construction, ability to judge spatial relationships, ability to synthesize component parts of a visual scene into a coherent whole (simultanagnosia or asimultagnosia), impaired visually guided reaching for objects (optic ataxia), and most likely impaired ability to shift her visual attention so as to direct saccades to targets in her field of view (oculomotor apraxia or ocular apraxia). The last three signs constitute Bálint syndrome, which localizes to disruption of dorsal visual networks (i.e., dorsal stream) with key nodes in the posterior parietal and prefrontal cortices bilaterally ( 5 ). She has additional salient symptoms and signs suggesting left inferior parietal dysfunction, including ideomotor limb apraxia and elements of Gerstmann syndrome, which comprises dysgraphia, acalculia, left-right confusion, and finger agnosia ( 6 ). Information was not included about whether she was explicitly examined for finger agnosia, but elements of her presentation suggested a more generalized disruption of body schema (i.e., her representation of the position and configuration of her body in space). Her less prominent impairment in lexical-semantic retrieval evidenced by impaired confrontation naming and category fluency likely localizes to the language network in the left hemisphere. Her impairments in attention and executive functions have less localizing value but would plausibly arise in the context of frontoparietal network dysfunction. At this point, it is unclear whether her impairment in episodic memory mostly reflects encoding and activation versus a rapid rate of forgetting (storage), as occurs in temporolimbic amnesia. Regardless, it does not appear to be the most salient feature of her presentation.
This localization, presenting with insidious onset and gradual progression, is characteristic of a PCA syndrome. If we apply consensus clinical diagnostic criteria proposed by a working group of experts, we find that our patient has many of the representative features of early disturbance of visual functions plus or minus other cognitive functions mediated by the posterior cerebral cortex ( Table 1 ) ( 7 ). Some functions such as limb apraxia also occur in corticobasal syndrome (CBS), a clinical syndrome defined initially in association with corticobasal degeneration (CBD) neuropathology, a 4-repeat tauopathy characterized by achromatic ballooned neurons, neuropil threads, and astrocytic plaques. However, our patient lacks other suggestive features of CBS, including extrapyramidal motor dysfunction (e.g., limb rigidity, bradykinesia, dystonia), myoclonus, and alien limb phenomenon ( Table 1 ) ( 8 ).
a Consensus diagnostic criteria for posterior cortical atrophy per Crutch et al. ( 7 ) require at least three cognitive features and relative sparing of anterograde memory, speech-nonvisual language functions, executive functions, behavior, and personality. Diagnostic criteria for probable corticobasal syndrome per Armstrong et al. ( 8 ) require asymmetric presentation of at least two motor features and at least two higher cortical features. AD=Alzheimer’s disease; CBD=corticobasal degeneration; FDG-PET=[ 18 ]F-fluorodexoxyglucose positron emission tomography; JCD=Jakob-Creutzfeldt disease; LBD=Lewy body disease; PSP=progressive supranuclear palsy; SPECT=single-photon emission computed tomography; TDP=TDP–43 proteinopathy.
TABLE 1. Clinical features and neuropathological associations of posterior cortical atrophy and corticobasal syndrome a
In addition to a standard laboratory work-up for cognitive impairment, it is important to determine whether imaging of the brain provides evidence of neurodegeneration in a topographical distribution consistent with the clinical presentation. A first step in most cases would be to obtain an MRI of the brain that includes a high-resolution T 1 -weighted MRI sequence to assess potential atrophy, a T 2 /fluid-attenuated inversion recovery (FLAIR) sequence to assess the burden of vascular disease and rule out less likely etiological considerations (e.g., infection, autoimmune-inflammatory, neoplasm), a diffusion-weighted sequence to rule out subacute infarcts and prion disease (more pertinent to subacute or rapidly progressive cases), and a T 2 *-gradient echo or susceptibility weighted sequence to examine for microhemorrhages and superficial siderosis.
A lumbar puncture would serve two purposes. First, it would allow for the assessment of inflammation that might occur in HE, as approximately 80% of cases have some abnormality of CSF (i.e., elevated protein, lymphocytic pleiocytosis, or oligoclonal bands) ( 9 ). Second, in selected circumstances—particularly in cases with atypical nonamnesic clinical presentations or early-onset dementia in which AD is in the neuropathological differential diagnosis—we frequently pursue AD biomarkers of molecular neuropathology ( 10 , 11 ). This is most frequently accomplished with CSF analysis of amyloid-β-42, total tau, and phosphorylated tau levels. Amyloid positron emission tomography (PET) imaging, and most recently tau PET imaging, represent additional options that are approved by the U.S. Food and Drug Administration for clinical use. However, insurance often does not cover amyloid PET and currently does not reimburse tau PET imaging. [ 18 ]-F-fluorodeoxyglucose (FDG) PET and perfusion single-photon emission computed tomography imaging may provide indirect evidence for AD neuropathology via a pattern of hypometabolism or hypoperfusion involving the temporoparietal and posterior cingulate regions, though without molecular specificity. Pertinent to this case, a syndromic diagnosis of PCA is most commonly associated with underlying AD neuropathology—that is, plaques containing amyloid-β and neurofibrillary tangles containing tau ( 12 – 15 ).
The patient underwent MRI, demonstrating a minimal burden of T 2 /FLAIR hyperintensities and some degree of bilateral parietal volume loss with a left greater than right predominance ( Figure 2A ). There was relatively minimal medial temporal volume loss. Her basic laboratory work-up, including thyroid function, vitamin B 12 level, and treponemal antibody, was normal. She underwent a lumbar puncture; CSF studies revealed normal cell counts, protein, and glucose levels and low amyloid-β-42 levels at 165.9 pg/ml [>500 pg/ml] and elevated total and phosphorylated tau levels at 1,553 pg/ml [<350 pg/ml] and 200.4 pg/ml [<61 pg/ml], respectively.
FIGURE 2. MRI brain scan of the patient at presentation and 4 years later a
a Arrows denote regions of significant atrophy.
Considering This Additional Data, What Would Be an Appropriate Diagnostic Formulation?
For optimal clarity, we aim to provide a three-tiered approach to diagnosis comprising neurodegenerative clinical syndrome (e.g., primary amnesic, mixed amnesic and dysexecutive, primary progressive aphasia), level of severity (i.e., mild cognitive impairment; mild, moderate or severe dementia), and predicted underlying neuropathology (e.g., AD, Lewy body disease [LBD], frontotemporal lobar degeneration) ( 16 ). This approach avoids problematic conflations that cause confusion, for example when people equate AD with memory loss or dementia, whereas AD most strictly describes the neuropathology of plaques and tangles, regardless of the patient’s clinical symptoms and severity. This framework is important because there is never an exclusive, one-to-one correspondence between syndromic and neuropathological diagnosis. Syndromes arise from neurodegeneration that starts focally and progresses along the anatomical lines of large-scale brain networks that can be defined on the basis of both structural and functional connectivity, a concept detailed in the network degeneration hypothesis ( 17 ). It is important to note that neuropathologies defined on the basis of specific misfolded protein inclusions can target more than one large-scale network, and any given large-scale network can degenerate in association with more than one neuropathology.
The MRI results in this case support a syndromic diagnosis of PCA, with a posteriorly predominant pattern of atrophy. Given the patient’s loss of independent functioning in instrumental activities of daily living (ADLs), including driving and managing her finances, the patient would be characterized as having a dementia (also known as major neurocognitive disorder). The preservation of basic ADLs would suggest that the dementia was of mild severity. The CSF results provide supportive evidence for AD amyloid plaque and tau neurofibrillary tangle (NFT) neuropathology over other pathologies potentially associated with PCA syndrome (i.e., CBD, LBD, TDP-43 proteinopathy, and Jakob-Creutzfeldt disease) ( 13 , 14 ). The patient’s formulation would thus be best summarized as PCA at a level of mild dementia, likely associated with underlying AD neuropathology.
The patient’s symptoms progressed. One year after initial presentation, she had difficulty locating the buttons on her clothing or the food on her plate. Her word-finding difficulties worsened. Others observed stiffness of her right arm, a new symptom that was not present initially. She also had decreased ability using her right hand to hold everyday objects such as a comb, a brush, or a pen. On exam, she was noted to have rigidity of her right arm, impaired dexterity with her right hand for fine motor tasks, and a symmetrical tremor of the arms, apparent when holding objects or reaching. Her right hand would also intermittently assume a flexed, dystonic posture and would sometime move in complex ways without her having a sense of volitional control.
Four to 5 years after initial presentation, her functional status declined to the point where she was unable to feed, bathe, or dress herself. She was unable to follow simple instructions. She developed neuropsychiatric symptoms, including compulsive behaviors, anxiety, and apathy. Her right-sided motor symptoms progressed; she spent much of the time with her right arm flexed in abnormal postures or moving abnormally. She developed myoclonus of both arms. Her speech became slurred and monosyllabic. Her gait became less steady. She underwent a second MRI of the brain, demonstrating progressive bilateral atrophy involving the frontal and occipital lobes in addition to the parietal lobes and with more left > right asymmetry than was previously apparent ( Figure 2B ). Over time, she exhibited increasing weight loss. She was enrolled in hospice and ultimately passed away 8 years from the onset of symptoms.
Does Information About the Longitudinal Course of Her Illness Alter the Formulation About the Most Likely Underlying Neuropathological Process?
This patient developed clinical features characteristic of corticobasal syndrome over the longitudinal course of her disease. With time, it became apparent that she had lost volitional control over her right arm (characteristic of an alien limb phenomenon), and she developed signs more suggestive of basal ganglionic involvement (i.e., limb rigidity and possible dystonia). This presentation highlights the frequent overlap between neurodegenerative clinical syndromes; any given person may have elements of more than one syndrome, especially later in the course of a disease. In many instances, symptomatic features that are less prominent at presentation but evolve and progress can provide clues regarding the underlying neuropathological diagnosis. For example, a patient with primary progressive apraxia of speech or nonfluent-agrammatic primary progressive aphasia could develop the motor features of a progressive supranuclear palsy (PSP) clinical syndrome (e.g., supranuclear gaze impairment, axial rigidity, postural instability), which would suggest underlying PSP neuropathology (4-repeat tauopathy characterized by globose neurofibrillary tangles, tufted astrocytes, and oligodendroglial coiled bodies).
If CSF biomarker data were not suggestive of AD, the secondary elements of CBS would substantially increase the likelihood of underlying CBD neuropathology presenting with a PCA syndrome and evolving to a mixed PCA-CBS. But the CSF amyloid and tau levels are unambiguously suggestive of AD (i.e., very low amyloid-β-42 and very high p-tau levels), the neuropathology of which accounts for not only a vast majority of PCA presentations but also roughly a quarter of cases presenting with CBS ( 18 , 19 ). Thus, underlying AD appears most likely.
NEUROPATHOLOGY
On gross examination, the brain weighed 1,150 g, slightly less than the lower end of normal at 1,200 g. External examination demonstrated mild cortical atrophy with widening of the sulci, relatively symmetrical and uniform throughout the brain ( Figure 3A ). There was no evidence of atrophy of the brainstem or cerebellum. On cut sections, the hippocampus was mildly atrophic. The substantia nigra in the midbrain was intact, showing appropriate dark pigmentation as would be seen in a relatively normal brain. The remainder of the gross examination was unremarkable.
FIGURE 3. Mild cortical atrophy with posterior predominance and neurofibrillary tangles, granulovacuolar degeneration, and a Hirano body a
a Panel A shows the gross view of the brain, demonstrating mild cortical atrophy with posterior predominance (arrow). Panel B shows the hematoxylin and eosin of the hippocampus at high power, demonstrating neurofibrillary tangles, granulovacuolar degeneration, and a Hirano body.
Histological examination confirmed that the neurons in the substantia nigra were appropriately pigmented, with occasional extraneuronal neuromelanin and moderate neuronal loss. In the nucleus basalis of Meynert, NFTs were apparent on hematoxylin and eosin staining as dense fibrillar eosinophilic structures in the neuronal cytoplasm, confirmed by tau immunohistochemistry (IHC; Figure 4 ). Low-power examination of the hippocampus revealed neuronal loss in the subiculum and in Ammon’s horn, most pronounced in the cornu ammonis 1 (CA1) subfield, with a relatively intact neuronal population in the dentate gyrus. Higher power examination with hematoxylin and eosin demonstrated numerous NFTs, neurons exhibiting granulovacuolar degeneration, and Hirano bodies ( Figure 3B ). Tau IHC confirmed numerous NFTs in the CA1 region and the subiculum. Amyloid-β IHC demonstrated occasional amyloid plaques in this region, less abundant than tau pathology. An α-synuclein stain revealed scattered Lewy bodies in the hippocampus and in the amygdala.
FIGURE 4. Tau immunohistochemistry demonstrating neurofibrillary tangles (staining brown) in the nucleus basalis of Meynert, in the hippocampus, and in the cerebral cortex of the frontal, temporal, parietal, and occipital lobes
In the neocortex, tau IHC highlighted the extent of the NFTs, which were very prominent in all of the lobes from which sections were taken: frontal, temporal, parietal and occipital. Numerous plaques on amyloid-β stain were likewise present in all cortical regions examined. The tau pathology was confined to the gray matter, sparing white matter. There were no ballooned neurons and no astrocytic plaques—two findings one would expect to see in CBD ( Table 2 ).
a AD=Alzheimer’s disease; CBD=corticobasal degeneration; CBS=corticobasal syndrome; PCA=posterior cortical atrophy.
TABLE 2. Neuropathological features of this case compared with a case of corticobasal degeneration a
The case was designated by the neuropathology division as Alzheimer’s-type pathology, Braak stage V–VI (of VI), due to the widespread neocortical tau pathology, with LBD primarily in the limbic areas.
Our patient had AD neuropathology presenting atypically with a young age at onset (52 years old) and a predominantly visual-spatial and corticobasal syndrome as opposed to prominent amnesia. Syndromic diversity is a well-recognized phenomenon in AD. Nonamnesic presentations include not only PCA and CBS but also the logopenic variant of primary progressive aphasia and a behavioral-dysexecutive syndrome ( 20 ). Converging lines of evidence link the topographical distribution of NFTs with syndromic presentations and the pattern of hypometabolism and cortical atrophy. Neuropathological case reports and case series suggest that atypical AD syndromes arise in the setting of higher than normal densities of NFTs in networks subserving the functions compromised, including visual association areas in PCA-AD ( 21 ), the language network in PPA-AD ( 22 ), and frontal regions in behavioral-dysexecutive AD ( 23 ). In a large sample of close to 900 cases of pathologically diagnosed AD employing quantitative assessment of NFT density and distribution in selected neocortical and hippocampal regions, 25% of cases did not conform to a typical distribution of NFTs characterized in the Braak staging scheme ( 24 ). A subset of cases classified as hippocampal sparing with higher density of NFTs in the neocortex and lower density of NFTs in the hippocampus had a younger mean age at onset, higher frequency of atypical (nonamnesic) presentations, and more rapid rate of longitudinal decline than subsets defined as typical or limbic-predominant.
Tau PET, which detects the spatial distribution of fibrillary tau present in NFTs, has corroborated postmortem work in demonstrating distinct patterns of tracer uptake in different subtypes of AD defined by clinical symptoms and topographical distributions of atrophy ( 25 – 28 ). Amyloid PET, which detects the spatial distribution of fibrillar amyloid- β found in amyloid plaques, does not distinguish between typical and atypical AD ( 29 , 30 ). In a longitudinal study of 32 patients at early symptomatic stages of AD, the baseline topography of tau PET signal predicted subsequent atrophy on MRI at the single patient level, independent of baseline cortical thickness ( 31 ). This correlation was strongest in early-onset AD patients, who also tended to have higher tau signal and more rapid progression of atrophy than late-onset AD patients.
Differential vulnerability of selected large-scale brain networks in AD and in neurodegenerative disease more broadly remains poorly understood. There is evidence to support multiple mechanisms that are not mutually exclusive, including metabolic stress to key network nodes, trophic failure, transneuronal spread of pathological proteins (i.e., prion-like mechanisms), and shared vulnerability within network regions based on genetic or developmental factors ( 32 ). In the case of AD, cortical hub regions with high intrinsic functional connectivity to other regions across the brain appear to have high metabolic rates across the lifespan and to be foci of convergence of amyloid-β and tau accumulation ( 33 , 34 ). Tau NFT pathology appears to spread temporally along connected networks within the brain ( 35 ). Patients with primary progressive aphasia are more likely to have a personal or family history of developmental language-based learning disability ( 36 ), and patients with PCA are more likely to have a personal history of mathematical or visuospatial learning disability ( 37 ).
This case highlights the symptomatic heterogeneity in AD and the value of a three-tiered approach to diagnostic formulation in neurodegenerative presentations. It is important to remember that not all AD presents with amnesia and that early-onset AD tends to be more atypical and to progress more rapidly than late-onset AD. Multiple lines of evidence support a relationship between the burden and topographical distribution of tau NFT neuropathology and clinical symptomatology in AD, instantiating network-based neurodegeneration via mechanisms under ongoing investigation.
The authors report no financial relationships with commercial interests.
Supported by NIH grants K08 AG065502 (to Dr. Miller) and T32 HL007627 (to Dr. Miller).
The authors have confirmed that details of the case have been disguised to protect patient privacy.
1 Balasa M, Gelpi E, Antonell A, et al. : Clinical features and APOE genotype of pathologically proven early-onset Alzheimer disease . Neurology 2011 ; 76:1720–1725 Crossref , Medline , Google Scholar
2 Mercy L, Hodges JR, Dawson K, et al. : Incidence of early-onset dementias in Cambridgeshire, United Kingdom . Neurology 2008 ; 71:1496–1499 Crossref , Medline , Google Scholar
3 Kothbauer-Margreiter I, Sturzenegger M, Komor J, et al. : Encephalopathy associated with Hashimoto thyroiditis: diagnosis and treatment . J Neurol 1996 ; 243:585–593 Crossref , Medline , Google Scholar
4 Nasreddine ZS, Phillips NA, Bédirian V, et al. : The Montreal Cognitive Assessment, MoCA: a brief screening tool for mild cognitive impairment . J Am Geriatr Soc 2005 ; 53:695–699 Crossref , Medline , Google Scholar
5 Rizzo M, Vecera SP : Psychoanatomical substrates of Bálint’s syndrome . J Neurol Neurosurg Psychiatry 2002 ; 72:162–178 Crossref , Medline , Google Scholar
6 Rusconi E : Gerstmann syndrome: historic and current perspectives . Handb Clin Neurol 2018 ; 151:395–411 Crossref , Medline , Google Scholar
7 Crutch SJ, Schott JM, Rabinovici GD, et al. : Consensus classification of posterior cortical atrophy . Alzheimers Dement 2017 ; 13:870–884 Crossref , Medline , Google Scholar
8 Armstrong MJ, Litvan I, Lang AE, et al. : Criteria for the diagnosis of corticobasal degeneration . Neurology 2013 ; 80:496–503 Crossref , Medline , Google Scholar
9 Marshall GA, Doyle JJ : Long-term treatment of Hashimoto’s encephalopathy . J Neuropsychiatry Clin Neurosci 2006 ; 18:14–20 Link , Google Scholar
10 Johnson KA, Minoshima S, Bohnen NI, et al. : Appropriate use criteria for amyloid PET: a report of the Amyloid Imaging Task Force, the Society of Nuclear Medicine and Molecular Imaging, and the Alzheimer’s Association . Alzheimers Dement 2013 ; 9:e-1–e-16 Crossref , Medline , Google Scholar
11 Shaw LM, Arias J, Blennow K, et al. : Appropriate use criteria for lumbar puncture and cerebrospinal fluid testing in the diagnosis of Alzheimer’s disease . Alzheimers Dement 2018 ; 14:1505–1521 Crossref , Medline , Google Scholar
12 Alladi S, Xuereb J, Bak T, et al. : Focal cortical presentations of Alzheimer’s disease . Brain 2007 ; 130:2636–2645 Crossref , Medline , Google Scholar
13 Renner JA, Burns JM, Hou CE, et al. : Progressive posterior cortical dysfunction: a clinicopathologic series . Neurology 2004 ; 63:1175–1180 Crossref , Medline , Google Scholar
14 Tang-Wai DF, Graff-Radford NR, Boeve BF, et al. : Clinical, genetic, and neuropathologic characteristics of posterior cortical atrophy . Neurology 2004 ; 63:1168–1174 Crossref , Medline , Google Scholar
15 Victoroff J, Ross GW, Benson DF, et al. : Posterior cortical atrophy: neuropathologic correlations . Arch Neurol 1994 ; 51:269–274 Crossref , Medline , Google Scholar
16 Dickerson BC, McGinnis SM, Xia C, et al. : Approach to atypical Alzheimer’s disease and case studies of the major subtypes . CNS Spectr 2017 ; 22:439–449 Crossref , Medline , Google Scholar
17 Seeley WW, Crawford RK, Zhou J, et al. : Neurodegenerative diseases target large-scale human brain networks . Neuron 2009 ; 62:42–52 Crossref , Medline , Google Scholar
18 Lee SE, Rabinovici GD, Mayo MC, et al. : Clinicopathological correlations in corticobasal degeneration . Ann Neurol 2011 ; 70:327–340 Crossref , Medline , Google Scholar
19 Whitwell JL, Jack CR Jr, Boeve BF, et al. : Imaging correlates of pathology in corticobasal syndrome . Neurology 2010 ; 75:1879–1887 Crossref , Medline , Google Scholar
20 Warren JD, Fletcher PD, Golden HL : The paradox of syndromic diversity in Alzheimer disease . Nat Rev Neurol 2012 ; 8:451–464 Crossref , Medline , Google Scholar
21 Hof PR, Archin N, Osmand AP, et al. : Posterior cortical atrophy in Alzheimer’s disease: analysis of a new case and re-evaluation of a historical report . Acta Neuropathol 1993 ; 86:215–223 Crossref , Medline , Google Scholar
22 Mesulam MM, Weintraub S, Rogalski EJ, et al. : Asymmetry and heterogeneity of Alzheimer’s and frontotemporal pathology in primary progressive aphasia . Brain 2014 ; 137:1176–1192 Crossref , Medline , Google Scholar
23 Blennerhassett R, Lillo P, Halliday GM, et al. : Distribution of pathology in frontal variant Alzheimer’s disease . J Alzheimers Dis 2014 ; 39:63–70 Crossref , Medline , Google Scholar
24 Murray ME, Graff-Radford NR, Ross OA, et al. : Neuropathologically defined subtypes of Alzheimer’s disease with distinct clinical characteristics: a retrospective study . Lancet Neurol 2011 ; 10:785–796 Crossref , Medline , Google Scholar
25 Ossenkoppele R, Lyoo CH, Sudre CH, et al. : Distinct tau PET patterns in atrophy-defined subtypes of Alzheimer’s disease . Alzheimers Dement 2020 ; 16:335–344 Crossref , Medline , Google Scholar
26 Phillips JS, Das SR, McMillan CT, et al. : Tau PET imaging predicts cognition in atypical variants of Alzheimer’s disease . Hum Brain Mapp 2018 ; 39:691–708 Crossref , Medline , Google Scholar
27 Tetzloff KA, Graff-Radford J, Martin PR, et al. : Regional distribution, asymmetry, and clinical correlates of tau uptake on [18F]AV-1451 PET in atypical Alzheimer’s disease . J Alzheimers Dis 2018 ; 62:1713–1724 Crossref , Medline , Google Scholar
28 Xia C, Makaretz SJ, Caso C, et al. : Association of in vivo [18F]AV-1451 tau PET imaging results with cortical atrophy and symptoms in typical and atypical Alzheimer disease . JAMA Neurol 2017 ; 74:427–436 Crossref , Medline , Google Scholar
29 Formaglio M, Costes N, Seguin J, et al. : In vivo demonstration of amyloid burden in posterior cortical atrophy: a case series with PET and CSF findings . J Neurol 2011 ; 258:1841–1851 Crossref , Medline , Google Scholar
30 Lehmann M, Ghosh PM, Madison C, et al. : Diverging patterns of amyloid deposition and hypometabolism in clinical variants of probable Alzheimer’s disease . Brain 2013 ; 136:844–858 Crossref , Medline , Google Scholar
31 La Joie R, Visani AV, Baker SL, et al. : Prospective longitudinal atrophy in Alzheimer’s disease correlates with the intensity and topography of baseline tau-PET . Sci Transl Med 2020 ; 12:12 Crossref , Google Scholar
32 Zhou J, Gennatas ED, Kramer JH, et al. : Predicting regional neurodegeneration from the healthy brain functional connectome . Neuron 2012 ; 73:1216–1227 Crossref , Medline , Google Scholar
33 Buckner RL, Sepulcre J, Talukdar T, et al. : Cortical hubs revealed by intrinsic functional connectivity: mapping, assessment of stability, and relation to Alzheimer’s disease . J Neurosci 2009 ; 29:1860–1873 Crossref , Medline , Google Scholar
34 Hoenig MC, Bischof GN, Seemiller J, et al. : Networks of tau distribution in Alzheimer’s disease . Brain 2018 ; 141:568–581 Crossref , Medline , Google Scholar
35 Liu L, Drouet V, Wu JW, et al. : Trans-synaptic spread of tau pathology in vivo . PLoS One 2012 ; 7:e31302 Crossref , Medline , Google Scholar
36 Rogalski E, Johnson N, Weintraub S, et al. : Increased frequency of learning disability in patients with primary progressive aphasia and their first-degree relatives . Arch Neurol 2008 ; 65:244–248 Crossref , Medline , Google Scholar
37 Miller ZA, Rosenberg L, Santos-Santos MA, et al. : Prevalence of mathematical and visuospatial learning disabilities in patients with posterior cortical atrophy . JAMA Neurol 2018 ; 75:728–737 Crossref , Medline , Google Scholar
- Jeffrey Maneval , M.D. ,
- Kirk R. Daffner , M.D. ,
- Scott M. McGinnis , M.D.
- Seth A. Gale , M.A., M.D. ,
- C. Alan Anderson , M.D. ,
- David B. Arciniegas , M.D.
- Posterior Cortical Atrophy
- Corticobasal Syndrome
- Atypical Alzheimer Disease
- Network Degeneration
- New Zealand
- [email protected]
- +974-55545283
- +353-858275584
Case Study of a Patient Dementia
Introduction
A nurse associate is responsible to provide adequate medical care to the dementia patients so that they get optimal well-being. This essay highlights the case of a dementia patient who is suffering from health issues due to sleep disorders, hallucinations and short-term memory loss. Dementia is the deterioration of the cortex region of the brain and cause abnormalities in the sensorimotor cortical regions. In order to maintain the patient's confidentialit y , the patient is named as Mrs. X as per NMC (2018). The responsibilities of a nurse associate are outlined sharply that helps a dementia patient to lead an independent and healthy life with the ability to overcome or face barriers and challenges. Hence, through the implementation of adequate medical care and effective social services, a dementia patient can be encouraged to feel motivated to live a healthy life.
Mrs. X is an eighty-four years old woman. She lives with husband and two daughters. Her professional career states that, she used to be a lawyer and enjoyed writing and reading books. Five years ago, she was diagnosed with vascular dementia. Due to this, she faces short-term memory loss, anxiety, depression, and loss of appetite. Mrs. X was suffering from reduced mobility as dementia has significant impact mobility at later stage of her life. The dementia report of 2014 stated, "more than 79.3% of people having dementia feel depressed and anxious” (T O'Brien and Thomas, 2015, pp. 1698). According to the dementia report of 2014, around 34% of all kinds of dementia are expected to occur due to vascular dysfunction. Mrs. X was diagnosed with delirium and that delirium is considered as a co-factor or early detection agent for dementia (Dewing and Dijk, 2016, pp. 107).
PHYSICAL AND PSYCHOSOCIAL HEALTH ISSUES "Any of several psychological illnesses, generally characterized by loss of a person's general brain, behavioural, or behavioural performance, and induced by biological or social reasons," is how The WHO describes mental illness. Although mental disorders can be a physical ailment, this is not always the case, unlike with conditions such as diabetes. Doctors can do tests to check for specific disease signs in the plasma, such as blood sugar and Glycosylated haemoglobin levels, in conditions like hypertension. Mental diseases can also be brought on by physical issues. Diagnoses for mental health conditions frequently rely more on the patient conveying their sensations and background than for illnesses like hypertension. If a patient has clinical depression, the primary care doctor may recommend medications. They can also perform tests to verify sure disease is not solely mental rather than biological in origin. A doctor could overlook a medical diagnosis that could be the root of a mental health issue if long-term health treatments are not provided together. All of the above basic information should be included in a mental health case study essay.
List Of Top Assignment Services Provided By BestAssignmentExperts.Com
When Mrs. X was admitted to a hospital having extreme urinary tract infection and severe agitation, delirium was diagnosed, as proven by the 4AT screening tool. Due to the disturbed sleep patterns, she used to feel agitated and anxious, which brought a feeling of apprehension and fear. This had a significant impact on the emotional, mental and psychological well-being of Mrs. X. As stated by Alzheimer’s society (2018), dementia is a progressive and long-term condition that destroys the brain cells of the patient. It leads to memory loss and the symptoms are seen to get worse with emerging time (Livingston et al . 2017, pp. 504). Through the development of an effective therapeutic approach, a healthy relationship was built with Mrs. X. Thus, the rationale behind the essay is to evaluate the usual causes of delirium that has affected the well-being of Mrs. X. As Mrs. X faced abnormal drowsiness due to delirium, she showed less eagerness in her interview.
The case study of Mrs. X revealed the adversities of Dementia like anxiety, short-term memory loss, and its potential impact on the well-being of the patient (Jönsson et al . 2019, pp. 3). Additionally, anxiety and depression have made her secluded from all other social activities. She used to remain confused between the time and place. Due to excessive disruption in the brain functioning, Mrs. X faced communication difficulties. Besides this, Mrs. X also faced reduced mobility. The medical reports of Mrs. X suggest that the progression of vascular dementia has a significant impact on the swallowing function of Mrs. X. Furthermore, this caused severe dehydration and additional weight loss. Thus, Mrs. X was provided with nursing aid so that she can take her regular nutritional intake by getting adequate nutrition support (Kontos et al. 2017, pp. 183).
The extreme impact of dementia caused Mrs. X to have communication difficulties. Therefore, use of simple words, low voice tone and utilization of verbal cues helped her to decode the information (Fazio et al. 2018, pp. S11). The nurses were given the responsibility to monitor the crucial signs of hourly-basis. This is because due to short-term memory loss or frequent drowsiness, the patients’ skip their medicines. Additionally, she was treated with antibiotics to prevent additional health issues besides dementia (Latham and Brooker 2017, pp. 504). In this regard, diagnostic tests and screening methodologies can help diagnose people with dementia for early detection (Alzheimer's society, 2018). A nurse must be responsible to support a dementia patient with adequate care. In the case of Mrs. X, the nurse was provided the task to aid Mrs. X with reassurance and empathy. This has also helped her to reduce fears and anxieties. Additionally, the role of the nurse was to promote her autonomy. The code of practice was maintained throughout the treatment phase of Mrs. X so that it can emphasize the best interest to generate effective decisions about the care of patients. A calm environment was given to Mrs. X so that she gets a peaceful sleep by avoiding noise (Corey 2017, pp. 575). Additionally, a pressure mattress was given to Mrs. X so that she can avoid pressure sores. Moreover, the integrity of the pressure skin was maintained in Mrs. X, as she was vulnerable to excessive illness due to poor nutritional intake. The role of the nurse was to carry out a urine dip stick to identify UTIs. Effective communication was done with Mrs. X so that the nurse can understand her problem effectively. Moreover, the nurse performed an effective role in maintaining the well-being of Mrs. X through continuous monitoring and hourly observations of her vital signs. This will help the physicians to monitor her health progress. Furthermore, the tasks of the nurse were to check her well-being to make sure that Mrs. X remained well-nourished, hydrated and sufficiently oxygenated, so that episodes of delirium were reduced. Additionally, the nurse associate was provided the responsibility to record fluid and food balance charts. Assessment of nutritional dietary intake acts to be an efficient intervention in dementia patients because lack of coordination between neurons affects their senses of hunger (Jones et al . 2016, pp. 280). Furthermore, the nurse associate assisted the dieticians with the regular monitoring reports so that an accurate nutritional balance is developed and the nurse associate can provide on-time nutritional content to Mrs. X. As Mrs. X was suffering from malnutrition (as evident from case study), it was necessary to monitor her diet charts to keep her healthy. Besides all these, the nurse associate was given the responsibility to monitor MUST (Malnutrition Universal Screening Tool) and Waterloo scale, and care plan was evaluated weekly. In comparison to this, intervention is a necessary element that will support the meal choices, drinking and eating habits of people suffering from dementia (Surr et al . 2016, pp. 145).
Several assisted activities were provided to Mrs. X so that she can lead her daily live independently. Numerous new symptoms restlessness, moaning, etc. came into effect due to the severe impact of delirium (Latham and Brooker 2017, pp. 506). This was difficult for Mrs. X and her family to cope with the situation. Personal centered care plan and discharge planning were designed based on the medical background and history. The alignment with effective medical care, provision of care package was formulated that supports Mrs. X’s daily activities at her home. Occupational therapists and physiotherapists encouraged Mrs. X’s behavior so that she becomes independent to carry out her daily exercises and other activities. This enhanced her confidence and she started to carry out her daily activities of living independently. Additionally, NHS England (2012) outlined the significance of supporting patients to re-gain their independence. A MTD (Multidisciplinary team) involved Mrs. X to plan her care and to highlight the importance of efficient delirium management. Additionally, health care promotional events have proven to be helpful for both Mrs. X and her husband to deal with a happy and healthy life. Thus, it helped to raise awareness regarding dehydration and UTIs. Mrs. X was able to eat and drink efficiently, which improved her nutrition intake. Mr. X was involved in numerous therapeutic activities and enjoyed listening to her favorite music. This enhanced her stimulation to live life happily, thereby reducing depression. Social services evaluated the potential needs for Mrs. X and numerous local authorities collaborated to meet the demands of her emotional, social and financial needs to promote independnce. The voluntary services that were provided to Mrs. X made her feel listened to and valued by other individuals. Hence, it had a positive impact on her mental health and well-being.
This essay has explored dementia and the impact of a UTI on dementia patients and the competency of the nurse associates to carry out their responsibilities efficiently. From the study, it is evident that Mrs. X is suffering from dementia for the past five years. Due to this, she has faced hallucination, memory loss, and other health issues. In this phase, a nurse associate must develop effective communication with a dementia patient so that she can express her needs through verbal cues, simple words and other means of communication. Thus, the importance of nurse associates to impose effective strategies will help a dementia patient to lead a happy, independent healthy life.
Alzheimer's society (2018) Dementia UK: The full report. London: Alzheimer’s Society
Corey, T, (2017). Genetic and environment factor associated with delirium severity in older adults with dementia: International journal of Geriatrics psychiatry. Vol. 32(5), pp,574-581.
Dewing, J. and Dijk, S., (2016). What is the current state of care for older people with dementia in general hospitals? A literature review. Dementia , 15 (1), pp.106-124.
Fazio, S., Pace, D., Flinner, J. and Kallmyer, B., (2018). The fundamentals of person-centered care for individuals with dementia. The Gerontologist , 58 (suppl_1), pp. S10-S19.
T O'Brien, J. and Thomas, A., 2015. Vascular dementia. The Lancet , 386 (10004), pp.1698-1706.
Jones, L., Candy, B., Davis, S., Elliott, M., Gola, A., Harrington, J., Kupeli, N., Lord, K., Moore, K., Scott, S. and Vickerstaff, V., (2016). Development of a model for integrated care at the end of life in advanced dementia: a whole systems UK-wide approach. Palliative medicine , 30 (3), pp.279-295.
Jönsson, K.E., Ornstein, K., Christensen, J. and Eriksson, J., (2019), June. A reminder system for independence in dementia care: a case study in an assisted living facility. In Proceedings of the 12th ACM International Conference on PErvasive Technologies Related to Assistive Environments (pp. 176-185). ACM.
Kontos, P., Miller, K.L. and Kontos, A.P., (2017). Relational citizenship: supporting embodied selfhood and relationality in dementia care. Sociology of Health & Illness , 39 (2), pp.182-198.
Latham, I. and Brooker, D., (2017). Reducing anti-psychotic prescribing for care home residents with dementia. Nurse Prescribing , 15 (10), pp.504-511.
Livingston, G., Sommerlad, A., Orgeta, V., Costafreda, S.G., Huntley, J., Ames, D., Ballard, C., Banerjee, S., Burns, A., Cohen-Mansfield, J. and Cooper, C., (2017). Dementia prevention, intervention, and care. The Lancet , 390 (10113), pp.2673-2734.
NHS England (2012). 6Cs of Nursing Standards. British Medical Journal. Accessed December 2011, Vol. 343.
Nursing and Midwifery Council (NMC, 2018). The Code. London: Nursing and Midwifery Council.
Surr, C.A., Smith, S.J., Crossland, J. and Robins, J., 2016. Impact of a person-centred dementia care training programme on hospital staff attitudes, role efficacy and perceptions of caring for people with dementia: A repeated measures study. International journal of nursing studies , 53 , pp.144-151.
List Of Biology Assignment Services Provided By BestAssignmentExperts.Com
No need to pay extra.
Turnitin Report
Proofreading and Editing
Consultation with Expert
Live Session 1-on-1
Quality Check
- Let's Proceed
New Special Offer
Get 25% Off
Our services.
- Academic Writing Help
- Marketing Assignment Help
- Computer Assignment Help
- Essay Types
- Case Study Help
- Management Assignment Help
- Academic Assignment Help
- Assignment Help
- Other Services
Enter Your Detail
Word count: 2000, share your reviews.

IN A HURRY?
GET A CALLBACK.
A sample case study: Mrs Brown
On this page, social work report, social work report: background, social work report: social history, social work report: current function, social work report: the current risks, social work report: attempts to trial least restrictive options, social work report: recommendation, medical report, medical report: background information, medical report: financial and legal affairs, medical report: general living circumstances.
This is a fictitious case that has been designed for educative purposes.
Mrs Beryl Brown URN102030 20 Hume Road, Melbourne, 3000 DOB: 01/11/33
Date of application: 20 August 2019
Mrs Beryl Brown (01/11/33) is an 85 year old woman who was admitted to the Hume Hospital by ambulance after being found by her youngest daughter lying in front of her toilet. Her daughter estimates that she may have been on the ground overnight. On admission, Mrs Brown was diagnosed with a right sided stroke, which has left her with moderate weakness in her left arm and leg. A diagnosis of vascular dementia was also made, which is overlaid on a pre-existing diagnosis of Alzheimer’s disease (2016). Please refer to the attached medical report for further details.
I understand that Mrs Brown has been residing in her own home, a two-story terrace house in Melbourne, for almost 60 years. She has lived alone since her husband died two years ago following a cardiac arrest. She has two daughters. The youngest daughter Jean has lived with her for the past year, after she lost her job. The eldest daughter Catherine lives on the Gold Coast with her family. Mrs Brown is a retired school teacher and she and both daughters describe her as a very private woman who has never enjoyed having visitors in her home. Mrs Brown took much encouragement to accept cleaning and shopping assistance once a week after her most recent admission; however, she does not agree to increase service provision. Jean has Enduring Power of Attorney (EPOA) paperwork that indicates that Mrs Brown appointed her under an EPOA two years ago. She does not appear to have appointed a medical treatment decision maker or any other decision-supporter.
I also understand from conversations with her daughters that Jean and Mrs Brown have always been very close and that there is a history of long-standing conflict between Catherine and Jean. This was exacerbated by the death of their father. Both daughters state they understand the impact of the stroke on their mother’s physical and cognitive functioning, but they do not agree on a discharge destination. Mrs Brown lacks insight into her care needs and says she will be fine once she gets back into her own home. Repeated attempts to discuss options with all parties in the same room have not resulted in a decision that is agreeable to all parties.
Mrs Brown has a history of Alzheimer’s disease; type II diabetes – insulin dependent; hypertension; high cholesterol and osteoarthritis. She has had two recent admissions to hospital for a urinary tract infection and a fall in the context of low blood sugars. She is currently requiring one to two people to assist her into and out of bed and one person with managing tasks associated with post-toilet hygiene. She can walk slowly for short distances with a four-wheel frame with one person to supervise. She benefits from prompting to use her frame; she needs someone to cut her food and to set her up to eat and drink regularly and to manage her medication routine. She requires one person to assist her to manage her insulin twice daily.
The team believe that Mrs Brown’s capacity for functional improvement has plateaued in the last ten days. They recommend that it is in her best interests to be discharged to a residential care setting due to her need for one to two people to provide assistance with the core tasks associated with daily living. Mrs Brown is adamant that she wants to return home to live with Jean who she states can look after her. Jean, who has a history of chronic back pain, has required several admissions to hospital over the past five years, and states she wants to be able to care for her mother at home. Jean states she is reluctant to agree to extra services as her mother would not want this. Her sister Catherine is concerned that Jean has not been coping and states that given this is the third admission to hospital in a period of few months, believes it is now time for her mother to enter residential care. Catherine states that she is very opposed to her mother being discharged home.
Mrs Brown is at high risk of experiencing falls. She has reduced awareness of the left side of her body and her ability to plan and process information has been affected by her stroke. She is now requiring one to two people to assist with all her tasks of daily living and she lacks insight into these deficits. Mrs Brown is also at risk of further significant functional decline which may exacerbate Jean’s back pain. Jean has stated she is very worried about where she will live if her mother is to enter residential care.
We have convened two family meetings with Mrs Brown, both her daughters and several members of the multi-disciplinary team. The outcome of the first meeting saw all parties agree for the ward to provide personalised carer training to Jean with the aim of trialling a discharge home. During this training Jean reported significant pain when transferring her mother from the bed and stated she would prefer to leave her mother in bed until she was well enough to get out with less support.
The team provided education to both Jean and Catherine about the progressive impact of their mother’s multiple conditions on her functioning. The occupational therapist completed a home visit and recommended that the downstairs shower be modified so that a commode can be placed in it safely and the existing dining room be converted into a bedroom for Mrs Brown. Mrs Brown stated she would not pay for these modifications and Jean stated she did not wish to go against her mother’s wishes. The team encouraged Mrs Brown to consider developing a back-up plan and explore residential care options close to her home so that Jean could visit often if the discharge home failed. Mrs Brown and Jean refused to consent to proceed with an Aged Care Assessment that would enable Catherine to waitlist her mother’s name at suitable aged care facilities. We proceeded with organising a trial overnight visit. Unfortunately, this visit was not successful as Jean and Catherine, who remained in Melbourne to provide assistance, found it very difficult to provide care without the use of an accessible bathroom. Mrs Brown remains adamant that she will remain at home. The team is continuing to work with the family to maximise Mrs Brown’s independence, but they believe that it is unlikely this will improve. I have spent time with Jean to explore her adjustment to the situation, and provided her with information on community support services and residential care services. I have provided her with information on the Transition Care Program which can assist families to work through all the logistics. I have provided her with more information on where she could access further counselling to explore her concerns. I have sought advice on the process and legislative requirements from the Office of the Public Advocate’s Advice Service. I discussed this process with the treating team and we decided that it was time to lodge an application for guardianship to VCAT.
The treating team believe they have exhausted all least restrictive alternatives and that a guardianship order is required to make a decision on Mrs Brown’s discharge destination and access to services. The team recommend that the Public Advocate be appointed as Mrs Brown’s guardian of last resort. We believe that this is the most suitable arrangement as her daughters are not in agreement about what is in their mother’s best interests. We also believe that there is a potential conflict of interest as Jean has expressed significant concern that her mother’s relocation to residential care will have an impact on her own living arrangements.
Mrs Brown’s medical history includes Alzheimer’s disease; type II diabetes; hypertension; high cholesterol and osteoarthritis. She was admitted to Hume Hospital on 3 March 2019 following a stroke that resulted in moderate left arm and leg weakness. This admission was the third hospital admission in the past year. Other admissions have been for a urinary tract infection, and a fall in the context hypoglycaemia (low blood sugars), both of which were complicated by episodes of delirium.
She was transferred to the subacute site under my care, a week post her admission, for slow-stream rehabilitation, cognitive assessment and discharge planning.
Mrs Brown was diagnosed with Alzheimer’s disease by Dr Joanne Winters, Geriatrician, in April 2016. At that time, Mrs Brown scored 21/30 on the Standardised Mini-Mental State Examination (SMMSE). During this admission, Mrs Brown scored 15/30. I have undertaken cognitive assessment and agree with the diagnosis; further cognitive decline has occurred in the context of the recent stroke. There are global cognitive deficits, but primarily affecting memory, attention and executive function (planning, problem solving, mental flexibility and abstract reasoning). The most recent CT-Brain scan shows generalised atrophy along with evidence of the new stroke affecting the right frontal lobe. My assessments suggest moderate to severe mixed Alzheimer’s and vascular dementia.
While able to recall some key aspects of her financial affairs, including the general monetary value of her pension and regular expenses, Mrs Brown was unable to account for recent expenditure (for repairs to her home) or provide an estimate of its value, and had difficulty describing her investments. In addition, I consider that she would be unable to make complex financial decisions due to her level of cognitive impairment. Accordingly, I am of the view that Mrs Brown now lacks capacity to make financial decisions.
Mrs Brown states that she previously made an Enduring Power of Attorney (EPOA) but could no longer recall aspects of the EPOA, such as when it would commence and the nature of the attorney’s powers. Moreover, she confused the EPOA with her will. Her understanding of these matters did not improve with education, and therefore I consider that she no longer has capacity to execute or revoke an EPOA.
Mrs Brown acknowledges that she needs some assistance but lacks insight into the type of assistance that she requires, apart from home help for cleaning and shopping. She does not appreciate her risk of falling. She is unable to get in and out of bed without at least one person assisting her. She frequently forgets to use her gait aid when mobilising and is not able to describe how she would seek help in the event of falling. She is not able to identify or describe how she would manage her blood sugar levels, and this has not improved with education. Accordingly, I consider that she lacks capacity to make decisions about accommodation arrangements and services.
Mrs Brown does not agree with the treating team’s recommendation to move into residential care and maintains her preference to return home. This is in spite of a failed overnight trial at home with both her daughters assisting her. Unfortunately, she was unable to get out of bed to get to the toilet and required two people to assist her to do so in the morning. In light of these matters, and in the context of family disagreement regarding the matter, the team recommends that the Office of the Public Advocate be appointed as a guardian of last resort.
Reviewed 22 July 2022
- Hospitals & health services
- Public hospitals in Victoria
- Patient care
- Ambulance and patient transport
- Non-emergency patient transport
- Non-emergency patient transport review
- NEPT legislation and clinical practice protocols
- Non-emergency patient transport licensing
- NEPT licensing fees
- NEPT services information and guidance
- First Aid Services
- First aid licences
- First aid services information and guidance
- First aid service fees
- Victorian State Trauma System
- Acute medicine
- Emergency care
- Surgical services
- Better at Home
- Critical care
- Hospital in the Home
- Virtual care (Telehealth)
- Perinatal and reproductive services
- Rehabilitation and complex care
- Renal health
- Renal services in Victoria
- Funding for renal services
- Different approaches to haemodialysis
- Specialist clinics
- Access to non-admitted services
- Minimum referral information
- Communication toolkit
- Integrated care
- HealthLinks: Chronic Care
- Community Health Integrated Program (CHIP) guidelines
- Service coordination in Victoria
- Victorian integrated care online resources
- Specialist clinics programs
- Specialist clinics reform
- Specialty diagnostics, therapeutics and programs
- Older people in hospital
- End of life and palliative care in Victoria
- Legislation and reform initiatives
- Quality, safety and service improvement
- Planned surgery recovery and reform program
- Digital Health
- Roadmap and Maturity Model
- Standards and guidelines
- Policies and frameworks
- Health Information Sharing Legislation Reform
- My Health Record
- Public hospital accreditation in Victoria
- Credentialing for senior medical staff in Victoria
- Clinical risk management
- Preventing infections in health services
- Healthy choices
- Victorian Perinatal Data Collection
- Rural health
- Improving Access to Primary Care in Rural and Remote Areas Initiative
- Rural x-ray services
- Rural health regions and locations
- Rural and regional medical director role
- Victorian Patient Transport Assistance Scheme
- Rural and isolated practice registered nurses
- Urgent care in regional and rural Victoria
- Private health service establishments
- Private hospitals
- Day procedure centres
- Mobile health services
- Fees for private health service establishments in Victoria
- Design resources for private health service establishments
- Professional standards in private health service establishments
- Legislation updates for private health service establishments
- Complaints about private health service establishments
- Cosmetic procedures
- Guideline for providers of liposuction
- Private hospital funding agreement
- Boards and governance
- About health service boards in Victoria
- Information and education
- Education resources for boards
- Sector leadership
- Data, reporting and analytics
- Health data standards and systems
- Funding, performance and accountability
- Statements of Priorities
- Performance monitoring framework
- Integrity governance framework and assessment tool
- Pricing and funding framework
- Patient fees and charges
- Fees and charges for admitted patients
- Non-admitted patients - fees and charges
- Other services
- Planning and infrastructure
- Sustainability in Healthcare
- Medical equipment asset management framework
- Health system design, service and infrastructure planning
- Complementary service and locality planning
- Primary & community health
- Primary care
- Community pharmacist pilot
- EOI - Victorian Community Pharmacist Statewide Pilot
- Victorian Community Pharmacist Statewide Pilot – Resources for pharmacists
- Emergency Response Planning Tool
- Working with general practice
- Victorian Supercare Pharmacies
- NURSE-ON-CALL
- Priority Primary Care Centres
- Local Public Health Units
- Community health
- Community health services
- Community health pride
- Registration and governance of community health centres
- Community Health Directory
- Community Health Program in Victoria
- Community health population groups
- Dental health
- Access to public dental care services
- Victoria's public dental care fees
- Victoria's public dental care waiting list
- Dental health for SRS residents
- Dental health program reporting
- Smile Squad school dental program
- Maternal and Child Health Service
- Nursery Equipment Program
- Maternal and Child Health Service Framework
- Maternal and Child Health Service resources
- Child Development Information System
- Early parenting centres
- Maternal Child and Health Reporting, Funding and Data
- Baby bundle
- Sleep and settling
- Maternal and Child Health Workforce professional development
- Aboriginal Maternal and Child Health
- Public Dental and Community Health Program funding model review
- Public health
- Women's Health and Wellbeing Program
- Inquiry into Women's Pain
- Inquiry into Women's Pain submissions
- Support groups and programs
- About the program
- Victorian Women's Health Advisory Council
- Cemeteries and crematoria
- Cemetery trust member appointments
- Cemetery search
- Cemeteries and crematoria complaints
- Exhumations
- Governance and finance
- Cemetery grants
- Interments and memorials
- Land and development
- Legislation governing Victorian cemeteries and crematoria
- Cemeteries and crematoria publications
- Repatriations
- Rights of interment
- Medicines and Poisons Regulation
- Patient Schedule 8 treatment permits
- Schedule 8 MDMA and Schedule 8 psilocybine
- Schedule 9 permits for clinical trials
- Documents and forms to print or download
- Legislation and Approvals
- Frequently Asked Questions - Medicines and Poisons Regulation
- Health practitioners
- Licences and permits to possess (& possibly supply) scheduled substances
- Medicinal cannabis
- Pharmacotherapy (opioid replacement therapy)
- Recent updates
- Environmental health
- Improving childhood asthma management in Melbourne's inner west
- Climate and weather, and public health
- Environmental health in the community
- Environmental health in the home
- Environmental health professionals
- Face masks for environmental hazards
- Human health risk assessments
- Lead and human health
- Per- and poly-fluoroalkyl substances (PFAS)
- Pesticide use and pest control
- Food safety
- Information for community groups selling food to raise funds
- Food businesses
- Food safety information for consumers
- Food regulation in Victoria
- Food safety library
- Food allergens
- Introducing Standard 3.2.2A: Food safety management tools
- Immunisation
- Respiratory syncytial virus (RSV) immunisation
- Seasonal influenza vaccine
- Immunisation schedule and vaccine eligibility criteria
- Ordering vaccine
- Immunisers in Victoria
- Immunisation provider information
- Cold chain management
- Adverse events following immunisation reporting
- Vaccine error management
- Vaccination for infants and children
- Vaccination for adolescents
- Vaccination program for adults
- Vaccination for special-risk groups
- Immunisation resources order form
- Victorian coverage rates for Victoria
- Infectious diseases guidelines & advice
- Infection control guidelines
- Disease information and advice
- Advice to the cruise industry: reporting infections
- Notifiable infectious diseases, conditions and micro-organisms
- Notification procedures for infectious diseases
- Infectious diseases surveillance in Victoria
- Germicidal ultraviolet light
- Protecting patient privacy in Victoria
- Population health systems
- Evidence and evaluation
- Health promotion
- Health status of Victorians
- Municipal public health and wellbeing planning
- Population screening
- Cancer screening
- Conditions not screened
- Improving outcomes in under-screened groups
- Infant hearing screening
- Newborn bloodspot screening
- Prenatal screening
- Screening registers
- Preventive health
- Type 2 diabetes and cardiovascular disease prevention
- Eye health promotion
- Injury prevention
- Healthy eating
- Oral health promotion
- Physical activity
- Sexual health
- Sex worker health
- Decriminalisation of sex work
- Automatic mutual recognition
- Domestic smoke detectors
- Lasers, IPL and LED devices for cosmetic treatments and beauty therapy
- Victoria's regulatory framework for radiation
- Radiation newsletter
- Tobacco reforms
- Tobacco reform legislation and regulations
- E-cigarettes and vaping
- Quitting smoking and vaping
- Smoke-free and vape-free areas
- Building entrances
- Children's indoor play centres
- Public hospitals and health centres
- Children's recreational areas
- Playground equipment
- Skate parks
- Swimming pools
- Under-age sporting events
- Enclosed workplaces
- Government buildings
- Learning environments
- Outdoor dining
- Outdoor drinking areas
- Patrolled beaches
- Train platforms and bus and tram shelters
- Under-age music or dance events
- Tobacco and e-cigarette retailers
- Making a report or complaint
- Resources and factsheets
- Alternative water supplies
- Aquatic facilities
- Blue-green algae (cyanobacteria)
- Drinking water in Victoria
- Legionella risk management
- Private drinking water
- Recreational water use and possible health risks
- Water fluoridation
- Chief Health Officer
- About the Chief Health Officer
- Chief Health Officer publications
- Health alerts and advisories
- Mental health
- Mental Health and Wellbeing Act 2022
- Mental Health and Wellbeing Act 2022 Handbook
- Community information
- Mental Health and Wellbeing Act 2022 in your language
- About Victoria's mental health services
- Area-based services
- Statewide and specialist mental health services
- Mental Health Community Support Services
- Support and intervention services
- Language services - when to use them
- Access to mental health services across areas
- Transport for people in mental health services
- Practice and service quality
- Medical Treatment Planning and Decisions Act
- Service quality
- Specialist responses
- Mental health and wellbeing reform
- Reform activity updates
- Priority areas
- Latest news
- Working with consumers and carers
- Consumer and carer engagement
- Consumer and Carer Experience Surveys
- Family support and crisis plans
- Consumer and carer financial support
- Supporting children whose parents have a mental illness
- Supporting parents with a mental illness
- Prevention and promotion
- Early intervention in mental illness
- Mental health promotion in Victoria
- Suicide prevention in Victoria
- Priorities and transformation
- Supporting the social and emotional wellbeing of Aboriginal and Torres Strait Islander Victorians
- National mental health strategy
- Rights and advocacy
- Making a complaint about a mental health service
- Chief Psychiatrist
- About the Chief Psychiatrist
- Principles in the Mental Health and Wellbeing Act and the Chief Psychiatrist's guidelines
- Obligations under the Mental Health and Wellbeing Act 2022
- Reporting a failure to comply with the Mental Health and Wellbeing Act 2022
- Governance and committees
- Reporting obligations for clinical mental health and wellbeing services
- Mental health and wellbeing support
- Making a complaint and seeking advocacy
- Second psychiatric opinion and process of review by Chief Psychiatrist
- Office of the Chief Psychiatrist's reform activities and news
- Oversight of forensic mental health and wellbeing services
- Resources and reports
- Chief psychiatrist guidelines
- Chief Mental Health Nurse
- About Victoria's Chief Mental Health Nurse
- Best practice
- Reducing restrictive interventions
- Research and reporting
- Mental health performance reports
- Reporting requirements and business rules for clinical mental health services
- Alcohol & drugs
- Alcohol and other drug treatment services
- Overview of Victoria's alcohol and drug treatment system
- Pathways into alcohol and other drugs treatment
- Prevention and harm reduction
- Medically supervised injecting room
- Victoria's Take-Home Naloxone Program
- Community-based AOD treatment services in Victoria
- Residential treatment services
- Mildura statewide alcohol and drug residential treatment service
- Drug rehabilitation plan
- Hospital-based services
- Forensic services
- Pharmacotherapy treatment
- Services for Aboriginal people
- Services for young people
- Statewide and specialist services
- Compulsory treatment
- Family and peer support
- Public intoxication reform
- New public intoxication response services
- Policy, research and legislation
- Alcohol and drug research and data
- Legislation governing alcohol and other drug treatment
- Alcohol and other drug service standards and guidelines
- Alcohol and other drug client charter and resources
- Alcohol and other drug treatment principles
- Service quality and accreditation
- Alcohol and other drug program guidelines
- Maintenance pharmacotherapy
- Drink and Drug Driving Behaviour Change Program
- Alcohol and Other Drug Residential Rehabilitation Facility Design Guidelines
- Specialist Family Violence Advisor capacity building program in mental health and alcohol and other drug services - Victoria
- Alcohol and other drug workforce
- Learning and development
- Alcohol and other drug workforce Minimum Qualification Strategy
- Workforce data and planning
- Funding and reporting for alcohol and other drug services
- Funding of alcohol and other drugs services in Victoria
- Reporting requirements and business rules for alcohol and other drug services
- Drug alerts
- 25C-NBOMe and 4-FA sold as '2C-B'
- Novel stimulants sold as MDMA, cocaine or speed
- Protonitazene sold as ketamine
- High potency benzodiazepine tablets
- MDMA adulterated with PMMA
- 25B-NBOH sold as powdered 'LSD'
- Green 'UPS' pills containing N-ethylpentylone (no MDMA)
- N-ethylpentylone in cocaine
- Ageing & aged care
- Supporting independent living
- Low cost accommodation support programs
- Personal Alert Victoria
- Dementia services
- Victorian Aids and Equipment Program
- Residential aged care services
- Public sector residential aged care services
- Safety and quality in public sector residential aged care
- Physical and social environments
- Emergency preparedness in residential aged care services
- My Aged Care assessment services
- Home and Community Care Program for Younger People
- HACC data reporting
- HACC PYP fees policy and schedule of fees
- Wellbeing and participation
- Age-friendly Victoria
- Healthy ageing
- Seniors participation
- Dementia-friendly environments
- Designing for people with dementia
- Maintaining personal identity
- Personal enjoyment
- Interior design
- Dining areas, kitchens and eating
- Bedrooms and privacy
- Gardens and outdoor spaces
- Assistive technology
- Staff education and support
- Strategies, checklists and tools
- Our Strategic Plan 2023-27
- Our organisation
- Our secretary
- Leadership charter
- Our services
- Our vision and values
- Specialist offices
- Senior officers in health
- Human Research Ethics Committee (HREC)
- Gifts, benefits and hospitality policy
- Information Asset Register
- Health legislation
- Health legislation overview
- Health Complaints legislation
- Health Records Act
- Human Tissue Act 1982
- Public Health and Wellbeing Act 2008
- Voluntary Assisted Dying Act
- Victoria's pandemic management framework
- Independent Pandemic Management Advisory Committee
- Pandemic Order Register
- Our ministers
- Our role in emergencies
- State Health Emergency Response Arrangements
- Emergency type
- Department's responsibilities in emergencies
- Health services’ responsibilities in emergencies
- Aboriginal employment
- Current vacancies
- Employment programs for students and graduates
- Rise program
- Inclusion and diversity at the Department of Health
- Health workforce
- Working in health
- Information sharing and MARAM
- Child Safe Standards
- Regulatory functions
- Reviews of decisions
- Victorian Public Healthcare Awards
- Aboriginal healthcare workers
- Mental health workforce
- Lived and living experience workforces
- Engaging with lived and living experience workforces
- Our workforce, our future
- Nursing and midwifery
- Free nursing and midwifery study
- Additional funding for nursing and midwifery positions
- Becoming a nurse or midwife
- Undergraduate nursing and midwifery scholarships
- Undergraduate student employment programs
- Nursing and midwifery graduates
- Nursing and midwifery graduate sign-on bonus
- Working as a nurse or midwife
- Enrolled nurse to registered nurse transition scholarships
- Support for new nurse practitioners
- Postgraduate scholarships for nurses and midwives
- Nurse practitioners
- Returning to nursing or midwifery
- Refresher pathway for nurses and midwives
- Re-entry pathway scholarships for nurses and midwives
- Nursing and midwifery - legislation and regulation
- Nursing and midwifery program - health sector
- Allied health workforce
- Education and training
- Enterprise agreements
- Worker health and wellbeing
- Working with us
- Grants and programs
- Freedom of Information
- Part II - Information Statements
- Procurement policies
- Protective markings
- Health and medical research
- Sponsorship application information
- Publications
- Annual reports
- Fact sheets
- Strategies, plans and charters
- Policies, standards and guidelines
- Research and reports
- Forms and templates
- Communities
- Designing for Diversity
- Vulnerable children
- Vulnerable children - responsibilities of health professionals
- Identifying and responding to children at risk
- Older people
- Aboriginal health
- Improving health for Victorians from culturally and linguistically diverse backgrounds
- Asylum seeker and refugee health in Victoria
- News and media hub
- Media releases
- Health alerts
- Feedback and complaints
- Make a payment
- Fees, charges and penalties subject to automatic indexation
- Our campaigns

Share this page
- Facebook , opens a new window
- X (formerly Twitter) , opens a new window
- LinkedIn , opens a new window

Case studies
These three case studies help you to consider different situations that people with dementia face. They are:
- Raj , a 52 year old with a job and family, who has early onset dementia
- Bob and Edith , an older married couple who both have dementia and are struggling to cope, along with their family
- Joan , an older woman, who lives alone and has just been diagnosed with dementia
Each case study contains:
- A vignette setting out the situation
- An ecogram showing who is involved
- An assessment which gives essential information about what is happening and the social worker’s conclusion
- A care and support plan which says what actions will be taken to achieve outcomes
You can use the practice guidance to think about how you would respond in these situations.

- Equal opportunities
- Complaints procedure
- Terms and conditions
- Privacy policy
- Cookie policy
- Accessibility

- Cancer Nursing Practice
- Emergency Nurse
- Evidence-Based Nursing
- Learning Disability Practice
- Mental Health Practice
- Nurse Researcher
- Nursing Children and Young People
- Nursing Management
- Nursing Older People
- Nursing Standard
- Primary Health Care
- RCN Nursing Awards
- Nursing Live
- Nursing Careers and Job Fairs
- CPD webinars on-demand
- --> Advanced -->

- Clinical articles
- CPD articles
- CPD Quizzes
- Practice question
- Expert advice
- Career advice
- Revalidation
Evidence & Practice Previous Next
Open access a relationship-centred approach to managing pain in dementia, sharron tolman admiral nurse, st cuthbert’s hospice, durham, england, karen harrison dening head of research and publications, dementia uk, london, england.
The presence of pain in a person with dementia can often be missed. The diagnosis of dementia can overshadow the pain-inducing symptoms of other co-morbid conditions with distress behaviours being attributed to the behavioural and psychological symptoms of dementia. Such distress behaviours of a person with dementia often have a profound and alarming effect on family carers. This Admiral Nurse case study explores the assessment and management of pain in a person with dementia in partnership with the family carer.
Nursing Older People . 30, 1, 27-32. doi: 10.7748/nop.2018.e985
This article has been subject to external double-blind peer review and checked for plagiarism using automated software
None declared
For information about writing for RCNi journals, contact [email protected]
For author guidelines, go to rcni.com/writeforus
Received: 07 August 2017
Accepted: 26 September 2017
Published: 29 January 2018
Admiral Nurses - carers - dementia - end of life care - mental health - older people - pain assessment
THE POPULATION of the UK, as in other developed nations, is ageing. In 2011, 9.2 million people in England and Wales were aged 65 and over, an increase of almost one million from 2001 ( Office for National Statistics 2013 , Alzheimer’s Society 2014 ). A UK study by Brayne et al ( 2006 ) found that people aged between 65 and 69 had a 6% chance of dying with dementia.
Deaths in early life from infectious disease have decreased and the management of other conditions, such as cardiovascular disease, is becoming more successful. The treatment of, and survival rates for, some cancers are also improving, therefore a higher proportion of the world’s population is living to older age. This has led to an increase in the number of people living long enough to develop the multiple co-morbidities associated with older age, in particular, neurodegenerative diseases such as dementia ( Sampson and Harrison Dening 2013 ). Such multiple co-morbidities will often have pain as one of their most significant symptoms ( Lichtner et al 2016 ).
Pain in dementia
People with dementia often experience several co-morbid conditions at the same time, but there is widespread evidence that untreated pain in this group is common ( Scherder et al 2009 ) and that they often have inequitable access to effective pain assessment and management.
Retrospective interviews with relatives and carers indicated that significantly more dementia patients were reported to experience pain in the last six months of life compared to those with cancer: 75% versus 60% ( McCarthy et al 1997 , Sampson et al 2015 ).
Untreated pain is a major contributor to reduced quality of life for people with dementia and can lead to increased discomfort and distress. Lack of proper pain assessment can cause a range of complications including delirium, sedation and increased confusion ( Pryor and Clarke 2017 ). It may also lead to the inappropriate prescribing of antipsychotic medication.
The assessment and treatment of pain are particularly challenging because some people with advanced dementia have a reduced ability to verbalise their pain and discomfort. Commonly used assessment tools may be unreliable and difficult to use, which leads to symptoms being missed and misunderstood ( Corbett et al 2014 ).
Most people living with dementia are supported by a family carer, who is well placed to assess their pain. This article presents a case study ( Case study one ) to illustrate how an Admiral Nurse ( Box 1 ) supported family carers in the assessment and recognition of pain in a person with dementia who was unable to communicate their pain in a conventional way. It also discusses how this led to more effective treatment and management of the person’s pain. The names and any identifiable factors have been changed to protect the anonymity of those involved.
Admiral Nurse service approach
Admiral Nurses focus on the needs of the whole family affected by dementia, including psychological support to help the person with dementia and carers to understand and deal with their thoughts, feelings and behaviour, and to adapt to the changing situation. The caregiver and recipient must adjust to the transformation of their relationship into a caregiving one; this includes a change in the balance of roles, as the caregiver takes more responsibility for the welfare of the recipient. Admiral Nurses can offer expert input here.
Admiral Nurses use a range of specialist interventions that help people live well with the condition and develop skills to improve communication and maintain relationships. The government-led dementia strategy emphasises early diagnosis, early interventions and support, intersectoral support and integrated working and support for carers.
Admiral Nurses’ work with families is an invaluable source of contact and support at points of difficulty in the dementia journey, including diagnosis, when the condition progresses or when tough decisions need to be made, such as moving a family member into residential care. Anticipated problems are misdiagnosis, delayed diagnosis and lack of information and services for people with dementia and their families, which give rise to the risk of inappropriate management, crises, poor psychological adjustment to the diagnosis, reduced coping capacity and ability to forward plan.
Admiral Nurses help families cope with feelings of loss and bereavement as the condition progresses. Family care does not end once ‘hands-on’ caregiving ceases. Dementia guidelines support the principle that family carers should be supported during the illness and into bereavement. For family carers, the more social support that is received during the years of caregiving, the easier it is to adjust and adapt post-bereavement.
Admiral Nurses provide advice on referrals to other appropriate services and liaise with other health professionals on behalf of the family. Such knowledge may help them provide general information, as opposed to just that which is medical such as further diagnosis and management of medical problems. For example, a nurse specialist could potentially make timely referrals, if needed, to sources of specialist legal advice and use legislation to reduce disputes.
( Rahman and Dening 2016 )
Case study one: Miriam
Miriam was 78 years old and had been referred to the Admiral Nurse by her district nurse. Miriam had received a diagnosis of dementia from her GP just over two years ago. Her GP wanted to refer Miriam for a full memory assessment at local mental health services but she declined. The stigma of being seen as having a ‘mental health’ problem was a concern for Miriam at that time. However, Miriam now had breast cancer with metastases in her bones. The district nurse was concerned as Miriam’s husband, George, was struggling to cope with his wife’s behaviour. The district nurse reported that Miriam’s cancer was ‘stable’ and that the behavioural symptoms appeared to be due to her dementia.
During the initial assessment visit to her home, Miriam appeared restless, unable to sit for any length of time, often getting up from the chair and wringing her hands constantly. She seemed tense, unhappy and irritable when her husband spoke about how she had been. She had an expressive aphasia where she experienced great difficulty expressing herself verbally, with conversation being stilted. George stated that her sleep was disturbed and appetite greatly reduced.
Miriam’s distress behaviour was perceived to be related to her diagnosis of dementia. However, evidence suggests that in people with a diagnosis of dementia, co-morbid conditions, especially pain, are often not identified until their signs and symptoms become severe ( Sampson et al 2009 ) or that distress behaviours due to pain are misinterpreted as the behavioural and psychological symptoms of dementia (BPSD). This is explored in the section headed Assessment of pain in dementia.
Assessment of pain in dementia
Self-report is the gold standard for pain assessment given the subjective and unique way that pain is experienced by individuals. Despite the problems in communication, and the widely held belief that people with dementia cannot articulate their pain, many with moderate to severe dementia can report pain reliably ( Zwakhalen et al 2006 ). However, Miriam had an expressive aphasia that resulted in marked communication difficulties and meant that she was unable to express or articulate symptoms or how she was feeling in a conventional way.
Pain and symptoms of other co-morbid illnesses may be missed in people with dementia due to the attribution of behaviours and signs to the behavioural and psychological symptoms of dementia (BPSD) (see Box 2 ), rather than an underlying physical pathology ( Kostopoulou et al 2008 ).
Behavioural and psychological symptoms of dementia
» Aggression
» Agitation or restlessness
» Screaming
» Depression
» Psychosis, delusions and hallucinations
» Repetitive vocalisation, cursing and swearing
» Sleep disturbance
» Shadowing, or following the carer closely
( Cerejeira et al 2012 )
On the face of it, Miriam’s signs and symptoms were seen as being due to her dementia and, given the known signs of BPSD ( Box 2 ), this response may not be unusual. George had coped as Miriam’s main carer for two years, but now struggled with Miriam’s behaviour. He too thought this was a progression of her dementia and expressed to the district nurse that he ‘could cope no longer’.
However, pain in a person with dementia who has difficulties with communication often manifests as behavioural change such as agitation, distress, social withdrawal, depression or resistive behaviour as included in BPSD ( Scherder et al 2009 , Sampson et al 2015 ). Important to note is the close similarity between the signs of BPSD and those that indicate that a person with dementia may be in pain ( Box 3 ), which may in part explain why the two may be difficult to differentiate.
The signs of possible pain in a person with dementia
» Agitation or fidgeting
» Repetitive movements
» Tense muscles
» Decreased function
» Body bracing
» Increased and repetitive calling out
» Changes in sleep patterns
» Tears or crying
» Withdrawal
( Pace et al 2011 )
Where a person with dementia has communication difficulties, as with Miriam, it may be necessary to use objective observation or a validated behavioural observational pain scale such as the Abbey pain scale ( Abbey et al 2004 ) or Pain Assessment in Advanced Dementia (PAINAD) scale ( Warden et al 2003 ). There is no consistent evidence to suggest that pain experience is more or less intense in people with dementia, but they may have difficulties in interpreting their pain signals as well as communicating this to others.
The assessment of pain in people with advanced dementia is, however, complex. It has been suggested that there is no evidence that pain produces any signs or behaviours that are unique to pain ( Regnard et al 2003 ). Regnard et al ( 2007 ) suggested that such symptoms, for example, agitation, restlessness and repeated vocalisation may be the result of other forms of distress and thus tools such as the Disability Distress Assessment Tool (DisDAT) may be more appropriate.
Sometimes, raising the issue of the possibility of pain is not straightforward. Family carers may feel confident the person they are caring for does not present with pain, as with George ( Case study two ), stating ‘I would know if she was in pain’. Not necessarily accepting the ‘no pain’ response can be a significant emotional challenge for family carers. They may also feel the care they provide is being questioned or judged. The guilt and grief of caring for a person they love with dementia can be overwhelming, painful and distressing for family carers ( Newbronner et al 2013 ).
Case study two: George (Miriam’s husband)
Through the initial discussions with George, he concurred that Miriam had experienced several health problems over many years and coped stoically, rarely ‘complaining’ or seeking help.
She had continued to work even during long and difficult chemotherapy treatments for primary breast cancer. I enabled George to see how historic elements of Miriam’s approach to managing illness and pain were still present even with dementia. This helped George to understand that Miriam may still be less likely to talk about any pain or discomfort she may be experiencing.
I explained that in people with dementia, it may also be that we need to use different words to help them express how they feel; words or descriptions they may be more familiar with now to express their pain.
Miriam’s recent behaviour had caused George much concern and he worried that her ‘dementia was becoming more advanced’ and that using an analgesic may make the situation even worse. He was also worried about possible side effects or the risk of Miriam becoming over-sedated. However, what made him most anxious was that Miriam clearly could not tell him whether she was in pain or not and that we may give her treatment she did not need and perhaps not act in her best interests.
People with dementia report higher levels of pain in the last six months of life than those with cancer, but pain control is often inadequate ( Davis and Srivastava 2003 , Kovach et al 2006 ). The assessment and treatment of pain are particularly challenging due to the reduced ability of some people with advanced dementia to verbalise their pain, discomfort and anguish ( Chatterjee 2008 ). This often manifests as behavioural change such as agitation, distress, social withdrawal or depression ( Sampson and Harrison Dening 2013 ). As with Miriam, in addition to the discomfort and distress caused by pain, her inability to verbalise pain was likely to be the underlying cause of behavioural symptoms. If such behaviours are misattributed to BPSD it can lead to inappropriate treatment with antipsychotic medications.
Managing pain in the person with advanced dementia requires careful assessment for possible underlying causes. This should include clinical examination, observation of behaviours at rest and during movement and discussion with family members or staff who know the person well. In some cases, response to a trial of analgesic may be a diagnostic tool ( Herr et al 2006 ). The aetiology of pain may be acute and may, for example, be associated with urinary retention, constipation ( Kovach et al 2006 ), myocardial infarction, deep vein thrombosis or acute infection. Common chronic causes of pain in people with advanced dementia include pressure ulcers, undetected fractures, poor dentition, awkward positioning in chair or bed and arthritis ( Davis and Srivastava 2003 ). With Miriam, it was more likely that the pain was related to conditions in her recent past medical history, namely cancer.
My (ST) initial assessment of Miriam was in-depth and holistic, largely to rule out any other treatable condition, such as depression. An assessment of pain in people with dementia often involves working closely with family carers to gain a collaborative history and support them to understand how pain can present in dementia (see Box 3 ). Presentation of pain can often come as a surprise to family carers and may be different to what they might have expected. Taking a short life history can help, specifically looking at how the person may have coped with pain or distress in the past and in helping them to understand what pain indicators they can look out for in the future. It can take time for the carer to feel confident and comfortable with your suggestions and ideas.
Monitoring Miriam’s distress behaviours
Miriam was receiving no analgesia. I (ST) asked George to keep an account of Miriam’s behaviour to enable us to observe for any patterns or triggers and to see if he had found any strategies helpful in reducing her distress. George was unable to identify anything that he felt was significant and increasingly struggled to cope.
As we have noted, pain tools are available for use with people with dementia. Sometimes family carers welcome their introduction to help them demonstrate the evidence of pain or otherwise in the person they care for, but in George’s case it added to his stress.
I asked George some questions, using the Abbey pain scale ( Abbey et al 2004 ), to determine if Miriam was experiencing pain and to support her GP in considering a trial of analgesia. For example, ‘Have you noticed Miriam whimpering or groaning?’ and ‘Have you noticed Miriam protecting parts of her body when care is given (guarding)?’ In this way, we started to get a picture of how Miriam’s distress behaviours were an expression of her unrecognised pain.
George became more confident with the scale and less stressed as he thought he was working towards making things better for his wife. Using this scale also helped George to recognise signs of contentment in Miriam as well as distress to build a picture of her overall well-being.
Most people living with dementia are supported, either in their own homes or other settings, by a spouse or other family member. This person usually has in-depth knowledge of the person and their methods of communication and nuances and may, therefore, be well placed to support the assessment of pain. They will often need guidance on those behaviours that can be characteristic of pain. We used the Abbey pain scale ( Abbey et al 2004 ) to observe Miriam’s behaviour.
The more commonly used pain assessment approaches, for example, self-report or pain thermometer (this assesses pain by asking patients to indicate the intensity or severity of their pain on a diagram of a thermometer), may be unreliable and difficult to use in people with a reduced ability to communicate, which often leads to symptoms being missed and misunderstood ( Bracegirdle 2012 ).
Untreated pain is a major contributor to reduced quality of life and disability, and can lead to increased behavioural and psychological symptoms, which can then become a vicious circle. However, the opposite to agitated and distressed behaviours can manifest itself, such as stillness, apathy and withdrawn behaviour which can all indicate pain in a person with dementia. However, as in Miriam’s case, it is more likely that agitated and aroused behaviour associated with pain is more commonly misinterpreted as being indicative of a decline in dementia.
Consistent use of an appropriate pain assessment tool is therefore vital to effective pain management ( Bray et al 2015 ).
Management of pain in dementia
Treating pain in people with dementia, as in the wider population ( World Health Organization (WHO) 2009 ), requires a stepped approach ( American Geriatrics Society Panel on Chronic Pain in Older Persons 1998 ). Depending on the cause, non-pharmacological interventions may be helpful, particularly where there is a musculoskeletal aetiology. Such interventions may include repositioning, provision of optimal seating or specialist beds, physiotherapy, massage, heat or cold.
Simple analgesia such as paracetamol or non-steroidal inflammatory drugs can be effective. There are anxieties about giving analgesia to older people. In a study involving patients with fractured neck of femur, participants with cognitive impairment were prescribed one third as much analgesia as cognitively intact controls ( Morrison and Siu 2000 ). There is no consistent evidence to suggest that pain experience is less intense, but people with advanced dementia will have difficulties in communicating that they are in pain and interpreting pain signals.
The key to achieving a good result is regular prescribing, as required medication is often not given because people with advanced dementia may not request it or report they are in pain.
If a regular analgesic regimen is ineffective, opioids should be considered. Side effects such as delirium, constipation or sedation may occur but in practice these can be managed.
An important study by Husebo et al ( 2011 ) demonstrated how this approach to the management of pain significantly reduced agitation in nursing home residents with moderate to severe dementia. Regular paracetamol was effective in 63% of participants and of the 25% who received opioids, only 2% had these discontinued because of side effects.
There are various risks of under-treating people with dementia at the end of life due to the lack of knowledge about the complexity and nuances of the condition ( Mahon and Sorrell 2008 ). Inadequate and ineffective pain management is high among these risks ( Torke et al 2010 , WHO 2011 ), and can lead to a range of complications including delirium, sedation and increased confusion ( Robinson et al 2008 , Bracegirdle 2012 ).
Treating Miriam’s pain
By using the Abbey pain scale ( Abbey et al 2004 ) George and I (ST) agreed that Miriam was experiencing pain. With Miriam’s GP, I discussed the results of the pain scale scores, taken over several days and at different times.
Miriam’s GP prescribed a buprenorphine patch. The pain-relieving medication helped to a certain extent, which highlighted that pain was a significant factor in Miriam’s distress. However, principles of good ‘total’ pain management ( Box 4 ) then needed to be considered, as well as having a robust, regular analgesic plan and treatment review in place.
Essential to my role was supporting George throughout as he too was distressed and finding the right treatment plan for Miriam took some time. Non-pharmacological options were considered to help George manage his distress. George needed time to reflect and talk about Miriam, their life together and what mattered to them most.
Sometimes, when the physical or emotional health needs of the person with dementia take priority, the family member can feel that their past and present relationship is being lost or overshadowed by the condition.
Once Miriam’s pain was becoming better controlled, I took the opportunity to undertake some life story work ( McKinney 2017 ) and to plan care for her in the future with George, by giving him the opportunity to talk about his past and present relationship and life with Miriam. Initially he chose to do this without her being present so that he could be honest and open about how he felt without fear of distressing her further. It became clear that it was important to George that I had the opportunity to ‘know’ Miriam before the diagnosis of dementia and to understand the changes in her over time.
Total pain is a clinical idea and approach developed by Cicely Saunders, the founder of the modern hospice movement. Total pain recognises pain as being physical, psychological, social and spiritual. Pain is not just a physical sensation, but can be a consequence of, for example, loneliness, spiritual distress or an inappropriate diet.
( Leleszi and Lewandowski 2005 )
Dementia is primarily a condition of older age and is, therefore, commonly associated with many other age-related conditions, including long-term health conditions. Multi-morbidity is common in people with dementia and, on average, they will experience an additional 4.6 chronic illnesses, many of which will induce pain ( Guthrie et al 2012 ). Nevertheless, family carers often feel ill equipped to manage the complex health needs of the person they care for and frequently do not know what to expect. ‘I’m not a nurse’ is commonly cited by family carers, yet they are relied on to make clinical assessments and judgements about the person they care for.
As with George, they have often supported the person with dementia through several episodes of ill health in the past, but the uncertain trajectory of decline ( Samsi and Manthorpe 2014 ) and recovery can be distressing and confusing for families. This can lead to heightened anxiety and apprehension in family carers, compounding the uncertainty about what to do for the best.
Pain can potentially be relatively simple to manage in dementia if attention is given to its possibility and assumptions about behavioural change being a natural consequence of dementia are avoided. A free resource to support family carers is published by the National Council for Palliative Care ( 2012 ) and is available to download.
Implications for practice
» Pain in dementia is often not complex but where there is little verbal communication and the emphasis is on nurses to determine the presence of pain, behavioural assessment tools can be useful.
» Be aware that a change in behaviour to stillness, quietness and withdrawal can also indicate the presence of pain in a person with dementia.
» Involve family members in your pain assessment to try to ascertain an individual’s past pain indicators and management strategies. Family carers play a vital role in monitoring the health and well-being of a person with dementia.
» Regularly assess for pain to ensure that it remains controlled, to avoid breakthrough pain and to assess whether the analgesia prescribed is having the desired effect.
» Initiate regular analgesic plan and ladder for treatment reviews.
- Abbey J, Piller N, De Bellis A et al (2004) The Abbey pain scale: a 1-minute numerical indicator for people with end-stage dementia. International Journal of Palliative Nursing. 10, 1, 6-13. [PUBMED] [CROSSREF] [Google Scholar]
- Alzheimer’s Society (2014) Dementia UK: Update. Second edition. www.alzheimers.org.uk/download/downloads/id/2323/dementia_uk_update.pdf (Last Accessed: 2 January 2018.) www.alzheimers.org.uk/download/downloads/id/2323/dementia_uk_update.pdf (Last Accessed: 2 January 2018.)'>[Google Scholar]
- American Geriatrics Society Panel on Chronic Pain in Older Persons (1998) The management of chronic pain in older persons. Journal of the American Geriatrics Society. 46, 5, 635-651. [CROSSREF] [Google Scholar]
- Bracegirdle L (2012) A tormented death: end-of-life care for people with dementia. British Journal of Nursing. 21, 12, 723-727. [PUBMED] [CROSSREF] [Google Scholar]
- Bray J, Evans S, Bruce M et al (2015) Enabling hospital staff to care for people with dementia. Nursing Older People. 27, 10, 28-31. [PUBMED] [CROSSREF] [Google Scholar]
- Brayne C, Gao L, Dewey M et al (2006) Dementia before death in ageing societies: the promise of prevention and the reality. PLoS Medicine. 3, 10, e397. [PUBMED] [Google Scholar]
- Cerejeira J, Lagarto L, Mukaetova-Ladinska E (2012) Behavioral and psychological symptoms of dementia. Frontiers in Neurology. 3:73. [PUBMED] [Google Scholar]
- Chatterjee J (2008) End-of-life care for patients with dementia. Nursing Older People. 20, 2, 29-34. [PUBMED] [Google Scholar]
- Corbett A, Achterberg W, Husebo B et al (2014) An international road map to improve pain assessment in people with impaired cognition: the development of the Pain Assessment in Impaired Cognition (PAIC) meta-tool. BMC Neurology. 14, 229. [PUBMED] [CROSSREF] [Google Scholar]
- Davis M, Srivastava M (2003) Demographics, assessment and management of pain in the elderly. Drugs & Aging. 20, 1, 23-57. [PUBMED] [CROSSREF] [Google Scholar]
- Guthrie B, Payne K, Alderson P et al (2012) Adapting clinical guidelines to take account of multimorbidity. BMJ. 345, e6341. [PUBMED] [CROSSREF] [Google Scholar]
- Herr K, Coyne P, Key T et al (2006) Pain assessment in the nonverbal patient: position statement with clinical practice recommendations. Pain Management Nursing. 7, 2, 44-52. [PUBMED] [CROSSREF] [Google Scholar]
- Husebo B, Ballard C, Sandvik R et al (2011) Efficacy of treating pain to reduce behavioural disturbances in residents of nursing homes with dementia: cluster randomised clinical trial. BMJ. 343, d4065. [PUBMED] [CROSSREF] [Google Scholar]
- Kostopoulou O, Oudhoff J, Nath R et al (2008) Predictors of diagnostic accuracy and safe management in difficult diagnostic problems in family medicine. Medical Decision Making. 28, 5, 668-680. [PUBMED] [CROSSREF] [Google Scholar]
- Kovach C, Noonan P, Schlidt A et al (2006) The Serial Trial Intervention: an innovative approach to meeting needs of individuals with dementia. Journal of Gerontological Nursing. 32, 4, 18-25. [PUBMED] [Google Scholar]
- Leleszi J, Lewandowski J (2005) Pain management in end-of-life care. Journal of the American Osteopathic Association. 105, 3 Suppl 1, S6-11. [PUBMED] [Google Scholar]
- Lichtner V, Dowding D, Allcock N et al (2016) The assessment and management of pain in patients with dementia in hospital settings: a multicase exploratory study from a decision making perspective. BMC Health Services Research. 16, 1, 427. [Google Scholar]
- Mahon M, Sorrell J (2008) Palliative care for people with Alzheimer’s disease. Nursing Philosophy. 9, 2, 110-120. [PUBMED] [CROSSREF] [Google Scholar]
- McCarthy M, Addington-Hall J, Altmann D (1997) The experience of dying with dementia: a retrospective study. International Journal of Geriatric Psychiatry. 12, 3, 404-409. [PUBMED] 3.0.CO;2-2">[CROSSREF] [Google Scholar]
- McKinney A (2017) The value of life story work for staff, people with dementia and family members. Nursing Older People. 29, 5, 25-29. [PUBMED] [CROSSREF] [Google Scholar]
- Morrison R, Siu A (2000) A comparison of pain and its treatment in advanced dementia and cognitively intact patients with hip fracture. Journal of Pain and Symptom Management. 19, 4, 240-248. [PUBMED] [CROSSREF] [Google Scholar]
- National Council for Palliative Care (2012) How Would I Know? What Can I Do? How to Help Someone with Dementia who is in Pain or Distress. www.ncpc.org.uk/sites/default/files/How_Would_I_know.pdf (Last Accessed: 2 January 2018.) www.ncpc.org.uk/sites/default/files/How_Would_I_know.pdf (Last Accessed: 2 January 2018.)'>[Google Scholar]
- Newbronner L, Chamberlain R, Borthwick R et al (2013) A Road Less Rocky – Supporting Carers of People with Dementia. Carers Trust, London. [Google Scholar]
- Office for National Statistics (2013) What Does the 2011 Census Tell Us About Older People. www.ons.gov.uk/peoplepopulationandcommunity/birthsdeathsandmarriages/ageing/articles/whatdoesthe2011censustellusaboutolderpeople/2013-09-06 (Last Accessed: 9 January 2018.) www.ons.gov.uk/peoplepopulationandcommunity/birthsdeathsandmarriages/ageing/articles/whatdoesthe2011censustellusaboutolderpeople/2013-09-06 (Last Accessed: 9 January 2018.)'>[Google Scholar]
- Pace V, Treloar A, Scott S (Eds) (2011) Dementia: From Advanced Disease to Bereavement. Oxford University Press, Oxford. [Google Scholar]
- Pryor C, Clarke A (2017) Nursing care for people with delirium superimposed on dementia. Nursing Older People. 29, 3, 18-21. [PUBMED] [Google Scholar]
- Rahman S, Dening KH (2016) The need for specialist nurses in dementia care. Nursing Times. 112, 16, 14-17. [PUBMED] [Google Scholar]
- Regnard C, Mathews D, Gibson L et al (2003) Difficulties in identifying distress and its causes in people with severe communication problems. International Journal of Palliative Nursing. 9, 4, 173-176. [PUBMED] [CROSSREF] [Google Scholar]
- Regnard C, Reynolds J, Watson B et al (2007) Understanding distress in people with severe communication difficulties: developing and assessing the Disability Distress Assessment Tool (DisDAT). Journal of Intellectual Disability Research. 51, Pt 4, 277-292. [PUBMED] [CROSSREF] [Google Scholar]
- Robinson S, Vollmer C, Jirka H et al (2008) Aging and delirium: too much or too little pain medication? Pain Management Nursing. 9, 2, 66-72. [PUBMED] [CROSSREF] [Google Scholar]
- Sampson E, Harrison Dening K (2013) Palliative care and end of life care. In Dening T, Thomas a (Eds) Oxford Textbook of Old Age Psychiatry. Second edition. Oxford University Press, Oxford, 359-370. [Google Scholar]
- Sampson E, Blanchard M, Jones L et al (2009) Dementia in the acute hospital: prospective cohort study of prevalence and mortality. British Journal of Psychiatry. 195, 1, 61-66. [PUBMED] [CROSSREF] [Google Scholar]
- Sampson E, White N, Lord K et al (2015) Pain, agitation, and behavioural problems in people with dementia admitted to general hospital wards: a longitudinal cohort study. Pain. 156, 4, 675-683. [PUBMED] [CROSSREF] [Google Scholar]
- Samsi K, Manthorpe J (2014) Care pathways for dementia: current perspectives. Clinical Interventions in Aging. 9, 2055-2063. [PUBMED] [Google Scholar]
- Scherder E, Herr K, Pickering G et al (2009) Pain in dementia. Pain. 145, 3, 276-278. [PUBMED] [CROSSREF] [Google Scholar]
- Torke A, Holtz L, Hui S et al (2010) Palliative care for patients with dementia: a national survey. Journal of the American Geriatrics Society. 58, 11, 2114-2121. [PUBMED] [CROSSREF] [Google Scholar]
- Warden V, Hurley A, Volicer L (2003) Development and psychometric evaluation of the Pain Assessment in Advanced Dementia (PAINAD) scale. Journal of the American Medical Directors Association. 4, 1, 9-15. [PUBMED] [CROSSREF] [Google Scholar]
- World Health Organization (2009) WHO’s Cancer Pain Ladder for Adults. www.who.int/cancer/palliative/painladder/en (Last Accessed: 2 January 2018.) www.who.int/cancer/palliative/painladder/en (Last Accessed: 2 January 2018.)'>[Google Scholar]
- World Health Organization (2011) WHO Definition of Palliative Care. www.who.int/cancer/palliative/definition/en (Last Accessed: 2 January 2018.) www.who.int/cancer/palliative/definition/en (Last Accessed: 2 January 2018.)'>[Google Scholar]
- Zwakhalen S, Hamers J, Abu-Saad H et al (2006) Pain in elderly people with severe dementia: a systematic review of behavioural pain assessment tools. BMC Geriatrics. 6, 3. [PUBMED] [CROSSREF] [Google Scholar]
User not found

29 January 2018 / Vol 30 issue 1
TABLE OF CONTENTS
DIGITAL EDITION
- LATEST ISSUE
- SIGN UP FOR E-ALERT
- WRITE FOR US
- PERMISSIONS
Related articles
Nurse-led home chemotherapy for patients with lung disease This article describes the development of a service for...
Criteria for initiating end of life treatment in cancer critical care As survival rates for patients with cancer improve, more...
Feasibility of a telephone support service for carers Aim The aim of the study was to assess the feasibility,...
Supporting patients with cancer and cognitive impairment A weekly drop-in memory service for patients and carers is...
Findings from the National Mesothelioma Experience Survey This article reports on the results of the National...
Copy Citation
Download citation, share article: a relationship-centred approach to managing pain in dementia.
We use cookies on this site to enhance your user experience.
By clicking any link on this page you are giving your consent for us to set cookies.
Nursing Assignment Sample on Case Study on Dementia
You can download the sample Nursing Case Study on Dementia with the following question for free at the end of this page. For further assistance with Nursing Assignment help , please check our offerings in Nursing assignment solutions. Our subject-matter experts provide online assignment help to Nursing students from across the world and deliver plagiarism free solution with a free Turnitin report with every solution.
(AssignmentEssayHelp does not recommend anyone to use this sample as their own work.)
Nursing Assignment Question
- What are the causes of Dementia? What are the signs & symptoms? What are the associated health problems
- Complete the risk assessment for your client, which may include: Falls risk Mini-mental examination
- Describe specific communication strategies to relieve distress, agitation, and challenging behaviours?
- Using a problem solving approach design activities which provide the client with opportunities for autonomy and promote independence
- Discuss the potential impact on family and others
Nursing Assignment Solution on Case Study on Dementia
Introduction.
Dementia is a mental disorder which affects an individual's intellectual and cognitive abilities which interfere with his/her daily activities (Birren, 2013) . In general, perception this disease was thought to be a normal part of ageing, but with the advent of medical genetics and molecular biology its underlying causes are slowly revealing. Although the exact underlying causes are yet to be fully understood from the mechanistic point of view, current progress in nursing care is able to assist dementia patients both qualitatively and quantitatively. This paper will take into consideration a client of dementia and provide a brief overview of the causes, sins and symptoms, risk assessment, services available, communication strategies and its impact. The main objective of this essay is to provide the reader a broader view on addressing dementia in a successful manner…
PATIENT/CLIENT INTRODUCTION
In the present case study an 85 year old man- named Mr. X has been admitted to the emergency department, post fall from the ladder in his living room. He was trying to get some old albums from the top shelf. After he regains his consciousness, he was unable to say how he got admitted and failed to provide any necessary medical history details of his family and his own. He was living with his wife named Alice. As per his wife's information he suffered from dementia for last 15 years. Based upon firsthand information facilitated a mini mental status examination was carried out. The score was just 18 out of 30 which is below than cut off score of 24. This implies he has cognitive impairment . His shoulder has been dislocated following the fall which has been reduced under anaesthesia . He hasn't taken any food or fluid after he was shifted to ward. After his wife leaves, post evening meal he became restless and experience difficulty in finding directions…
Dementia symptoms, don't follow a particular trend as symptoms vary greatly. But when two of the following symptoms are observed majorly a patient can be considered as a dementia patient. Memory, loss of ability to focus, communication impairment and language difficulty, visual perception, reasoning and judgments (Savva, 2009) . In the above case study, the client has memory loss and communication issues as well as loss of ability to focus and pay attention.
Dementia mostly occurs due to damage in the brain. Damage to any part of the brain leads to impairment of communication. In the present case study the client displays a significant loss of memory and cognitive abilities. It suggests his brain must be subjected to severe damage which could be due to any accident or any biophysical cause. The Hippocampus is the region in the brain, which is responsible for learning and memory. This region gets damaged first when any injury occurs in the brain. Thus, the dementia and Alzheimer disease earliest symptoms are memory loss. In most cased Alzheimer is the originating disease which leads to dementia (Salzman, 2008) . This is the most possible cause of dementia in the present case study…
PHYSICAL AND PSYCHOSOCIAL HEALTH ISSUES
Dementia can lead to a number of physical and psychosocial health issues . In the present case study the client is prone to malnutrition due to inadequate nutrition. Since they have a problem in remembering, eventually as the disease progresses they forget to take their meals or miss. In advance cases this might lead to loss of functional ability of chewing and swallowing. This can lead to serious issues such as choking or aspiration of food. With the progression of disease, the patient loose appetite (Sörensen, 2011) . As seen in the client in the present case study, he is unable to carry out his own work, such as bathing, brushing, using the toilet; he is more prone to fungal and bacterial infection. Unhygienic conditions such as dirty hands and food can cause food borne disorders and further affects physical health. Since, memory is affected the client fails to remember the timing of medications and tend to take wrong doses at the wrong time At times it can lead to serious medical side effects…
Due to memory loss and cognitive ability loss , in most cases, clients fail to assess their potential and ability. As a result, they tend to carry out activities which results into fall and challenge personal safety. The most prominent cause of the fall in the present case study is physical weakness and poor balance due to gait changes. Memory impairment, visual misperception are the associated causes of the fall (Härlein, 2009) . Mini mental examination – This test is usually done to assess the person's cognitive ability. This test must be carried out to assess the person's mental skills which are used on a daily basis. A Score of 20 to 24 out of 30 indicates mild dementia, score of 13 to 20 indicates moderate dementia and less than 13 indicates severe dementia (Mitchell, 2009) …
COMMUNICATION STRATEGY
The ability of perceiving information , processing it and respond accordingly becomes weaker, progressively in the dementia patients. The communication strategy with such patients include five main aspects, namely orientation , the environment , body language , words and use of simple language . The orientation consists of the right positioning of a person while conversing with dementia patients . Proper eye contact is important while conversing so that the individual is able to make dementia patients understand even through signs and make them concentrate on what is being said to them. Choosing the right environment helps in maximizing the ability of the patient to focus and communicate properly. Extra and loud noises should be avoided along with external stimuli (Vasse, 2010) …
PROBLEM SOLVING APPROACHES
For the above patient, the following approach will be carried out i.e. listing his strength and deficits, which will prevent the client’s aggressive nature . At many times clients are forced to perform beyond their ability. Short sentences which are easy to understand will be used for communication. To make him more independent care strategy must integrate with physiotherapy to increase his muscle strength and enhance motor skills . Training given during leisure hours will help him in gaining confidence and appraisal will motivate him (Gitlin, 2012) …
SERVICES AVAILABLE
A number of services are available for elderly dementia patients that can be facilitated at the client’s setting or else at residential aged care homes. Similarly the aged care assessment team can help Mr. X in assessing his mental and physical status, thereby providing him the best service available to him…
IMPACT ON FAMILY MEMBERS AND OTHERS
The family members of a dementia patient have extreme emotional, physical and economic pressure , which results in great stress upon them and other caregivers. Hence families of dementia patients require adequate support from health , social, legal and financial systems so that they are able to cope up with the situation. Apart from this maintaining the relationship with the member suffering from dementia is also a challenge for other family members. This affects the practical and emotional capacity of the family members for coping up with the changes that occurs on a daily basis or even at every moment otherwise it adversely affects the relationships within the family often leading to the cessation of relationships…
- Enter your Email Address (required) *
- This form collects your email so that we can correspond with you through our newsletters. Checkout our Privacy policy for more information.
- Yes, i consent to this conditions.
- Challenge question: 8+2=?
(Some parts of the solution has been blurred due to privacy protection policy)
- Free Samples
- Premium Essays
- Editing Services Editing Proofreading Rewriting
- Extra Tools Essay Topic Generator Thesis Generator Citation Generator GPA Calculator Study Guides Donate Paper
- Essay Writing Help
- About Us About Us Testimonials FAQ
- Studentshare
- Health Sciences & Medicine
- The Diagnosis of Dementia
The Diagnosis of Dementia - Case Study Example

- Subject: Health Sciences & Medicine
- Type: Case Study
- Level: Undergraduate
- Pages: 8 (2000 words)
- Downloads: 0
Extract of sample "The Diagnosis of Dementia"
- Cited: 0 times
- Copy Citation Citation is copied Copy Citation Citation is copied Copy Citation Citation is copied
CHECK THESE SAMPLES OF The Diagnosis of Dementia
Effects of acetylcholinesterase inhibitors on delay induced deficits in the novel object recognition, genetic and environmental contributions to dementia, dementia and caretaking, social problem: living with dementia// i prefer something in health care, ethics in qualitative research, dementia patient care plan, e-healthcare and dementia in poland, mental health and dementia.

- TERMS & CONDITIONS
- PRIVACY POLICY
- COOKIES POLICY

Mental Health - Dementia Case Study Assignment
Write a critical overview of a chosen mental health condition based on case scenarios.
Added on 2022-08-17
Added on 2022-08-17

End of preview
Want to access all the pages? Upload your documents or become a member.
Nursing Assignment for Alzheimer's Dementia Patient lg ...
Assignment on the mental health nursing lg ..., nursing assignment vascular dementia lg ..., clinical reasoning cycle case study for nursing professionals lg ..., cognitive psychology: understanding mental processes and brain functioning lg ..., gibbs reflective cycle for dementia case study lg ....
- Dementia care case studies

Who we're supporting with specialist dementia care at home
Seeing how dementia is affecting someone close to you can be distressing. We’ve been supporting people with dementia nationwide for almost 30 years. Read some of the stories below from the families we’ve helped.
Whether you’re looking for a visiting care service or more permanent live-in care support , our care is completely flexible to suit yours and your family’s needs.
To learn more about how we can provide dementia care in your own home, call our friendly care team today.
Dorothy’s story – dementia case study
How home care helps dorothy live the life she wants.

Dorothy says, “There really is no place like home, and with Magda’s support I am able to keep in touch with all of my friends and neighbours. We visit church every week for the Sunday morning service, I can visit the shops and I also take part in a local knitting group. This really is one of the greatest joys of staying in my own home around people I know.”
By helping her to do the activities that mean most, Magda has made such a difference in Dorothy’s life. An experienced carer with plenty of care knowledge, what matters most to Magda is that Dorothy is happy.
Dorothy says, “Live-in care means friendship, a sense of security and feeling comfortable in my own home. Having previously spent a brief but unhappy period of time in a care home, I am able to recognise how perfect my situation is now. I feel very lucky and comfortable; I have a true friend. Magda is going nowhere! I want this to continue forever.”
Joan’s story – dementia case study

Switching from a care home to live-in care
For the families that we support, deciding that their loved one needs additional support can be a difficult choice to make. For Joan, whose husband, Peter, had vascular dementia, having a live-in carer helped to keep her family together.
After feeling let down by a care home, Joan came across our 24-hour care support. After talking through our services and her family’s needs, we provided her with profiles of some of our carers. Lazlo’s profile stood out immediately.
Lazlo and Peter built a close friendship and other members of Joan’s family also loved having Lazlo around. As Peter neared the end of his life, Lazlo helped to make sure he was as comfortable as possible. He also worked closely with other healthcare professionals involved in Peter’s care, and helped his loved ones in any way he could.
Sue’s story – dementia case study
A daughter’s peace of mind.
What matters most to the families we support is that their loved one is safe and comfortable. When Sue needed some more support for her mother, Barbara, she decided that a live-in carer would be the best option.
Barbara’s carer, Rosemary, quickly became part of the family. She cooks Barbara’s favourite meals, tends to her personal care needs, and even listens to her stories about her adventures in the Pembrokeshire countryside, where they have also taken short breaks together.
Sue says, “Live-in care has made such a difference. [Mum] is so much more contented, she doesn’t have to worry – and neither do I – about somebody different coming in.”
Andy's story – dementia case study
Expert care for a declining condition.
Andy’s mother was living with dementia and her condition suddenly started to worsen. The daycare she was receiving couldn’t stretch to overnight support, and Andy and his siblings all lived an hour or more away.
On the recommendation of a visiting nurse, Andy contacted Helping Hands. “Very quickly things started falling into place,” he said. “I never felt that I was talking to anyone other than professionals, and yet it was done with an empathy which was greatly appreciated.”
Andy explained how we found the right carer for his mum. “Mum’s needs were expertly assessed without coming across as intrusive. We were also invited to provide our thoughts as to the sort of person who would get on best with Mum, the village environment and the friends with whom she would become acquainted.”
After three months of live-in care, during which time Andy said that his mother’s decline “seemed to have slowed”, the family made the decision to move her to a care home so she would be closer to them.
Andy described their Helping Hands carer saying, “I have absolutely no doubt that on this member of staff’s ‘watch’ Mum had a great time… We would often call to speak to Mum and simply had to bail out because Mum and them were giggling too much!
“I have to say I don’t know where we would have been over these three months without their dedication and support,” added Andy. “Thanks to all involved in my mother’s care.”
Other people are interested in...
We’re here seven days a week to talk through your home care needs and find the best option for you. Call 03300376958 or request a callback and we will call you.

Live in care
Quality live-in care at home, across England and Wales

What makes our carers and support workers so special

Testimonials
What our customers say about our home care
Page reviewed by Deanna Lane , Senior Clinical Lead on March 24, 2022
Find your perfect carer
Find the right affordable care for you
- After Hospital Care
- Comfort Care
- Community Care
- Comprehensive Home Care Packages for the Elderly
- Convalescent Care
- Critical Care
- Disability Care
- Domestic Care
- Hire a Carer
- Hospice care at home
- Intensive Care
- Intermediate Care
- Long term care
- Medication Management
- Personal care
- Postoperative Care
- Preventative Care
- Reablement Care
- Supported Living
- The Advantages of Home Care
- What is home care?
- Domiciliary care
- Loneliness is a guest nobody wants this Christmas
- Respite care
- Dementia Care Technology
- How Are Parkinson’s And Dementia Related?
- How Dementia Affects Day to Day Living
- How Is Dementia Diagnosed
- Types of dementia
- What Does Dementia Feel Like?
- What Is Dementia Care Mapping?
- What is dementia care?
- Dementia Life Story Book
- Dementia care questions
- Our dementia experts
- Live in care for dementia
- Dementia care guide
- Diet for dementia
- Overnight care
- Palliative care
- Elderly care
- Support for younger people
- Condition-led care
- End of life care
- Housekeeping services
- Emergency home care
- Mobility aids and home adaptations
- Carer supported holidays
- Home Care FAQs
- What Is Home Help?
- Alternative to care homes
- Preparing For Home Care
- What Is A Home Carer?
- Difficult conversations: How to start a conversation about care
- Emotional well-being
- Our independent life
- Home care for Christmas and New Year
Guide to dementia home care
Looking for local care?
Friendly, expert care is closer than you think

Show in maps

IMAGES
VIDEO
COMMENTS
Case Study Student-Dementia- Unfolding Reasoning. Keith RN case study. Course. Professional Nursing Concepts III (5-8-8) (HSNS 2118) 45 Documents. Students shared 45 documents in this course. University Rose State College. ... ##### Case Study Safe and Effective Care Environment
Common dementia exam questions for medical finals, OSCEs and MRCP PACES. The case below illustrates the key features in the assessment of a patient with dementia or undiagnosed memory decline. It works through history, examination and investigations - click on the plus symbols to see the answers to each question.
There was no first-degree family history of presenile dementia. Neurocognitive assessment at the first clinic visit revealed a Mini Mental State Examination (MMSE) score of 14/30; poor verbal fluency (patient was able to produce only 5 animal names and 1 F-word in 1 min) as well as poor visuospatial and executive skills ( Fig. 1 ).
CASE PRESENTATION. A 55-year-old right-handed woman presented with a 3-year history of cognitive changes. Early symptoms included mild forgetfulness—for example, forgetting where she left her purse or failing to remember to retrieve a take-out order her family placed—and word-finding difficulties.
Semantic Dementia (PPA) Final Case. Final Case. The patient is a male in his early 80s who has a two year history of gradually progressing short-term memory decline. His family reported that he used to be really sharp but over the past two years, he's had difficulty learning and remembering short-term information.
The case study of Mrs. X revealed the adversities of Dementia like anxiety, short-term memory loss, and its potential impact on the well-being of the patient (Jönsson et al. 2019, pp. 3). Additionally, anxiety and depression have made her secluded from all other social activities.
Summary. An 85-year-old woman with hypertension and hyperlipidemia presented with gradual and progressive cognitive impairment for more than 2 years, involving cognitive domains of memory, executive function, visuospatial and mood. She has short-term memory loss such as forgetting whether she has eaten or showered.
Dementia is a mental disorder which affects an individual's intellectual and cognitive abilities which interfere with his/her daily activities (Birren, 2013).The main objective of this essay is to provide the reader a broader view on addressing dementia in a successful manner. Read more. Education. 1 of 12. Download Now. Download to read offline.
This collection of case studies from around the world illustrates both common and unusual causes of dementia, emphasizing clinical reasoning, integrative thinking and problem-solving skills. Each case consists of a clinical history, examination findings and special investigations, followed by diagnosis and discussion.
Nursing Assignment Sample on Case Study on Dementia - Free download as PDF File (.pdf), Text File (.txt) or read online for free. Dementia is a mental disorder which affects an individual's intellectual and cognitive abilities which interfere with his/her daily activities (Birren, 2013).The main objective of this essay is to provide the ...
Check out Smart'n, the exclusive platform for nursing students, for more case study types. It offers over 2,500 NCLEX practice questionsand 60+ hours of NGN-NCLEX-style nursing case studies, helping you track progress and become a more confident registered nurse. Start your journey to NCLEX success with Smart'n. Understanding dementia.
A case study is given about an individual who has a dementia and explain what person centred care is and how dignity can be promoted whilst keeping their ... Unit 7 D1 assignment (what is malfunction in the body) anatomy and physiology ... A flexible approach is needed when planning care for one individual with dementia. In my case study with ...
Essay for assignment case study: my patient mrs. diagnosed with dementia has an advance directive of do not resuscitate (dnr). dnr is type of legal order from. ... Dementia case study - Essay for assignment. University: Northern Virginia Community College. Course: Bio ethics (227) 5 Documents. Students shared 5 documents in this course.
Disability: dementia with Lewy Bodies. First language: English. Family: estranged and in Ireland. Location: village in South West. Joan lives in a house in a small village. She has lived there for 28 years. She has two dogs and 11 chickens. Joan has always been quite private but is well known in her village. She goes to the nearby town on the ...
Social work report: Background. Mrs Beryl Brown (01/11/33) is an 85 year old woman who was admitted to the Hume Hospital by ambulance after being found by her youngest daughter lying in front of her toilet. Her daughter estimates that she may have been on the ground overnight. On admission, Mrs Brown was diagnosed with a right sided stroke ...
These three case studies help you to consider different situations that people with dementia face. They are: Raj, a 52 year old with a job and family, who has early onset dementia. Bob and Edith, an older married couple who both have dementia and are struggling to cope, along with their family. Joan, an older woman, who lives alone and has just ...
Such distress behaviours of a person with dementia often have a profound and alarming effect on family carers. This Admiral Nurse case study explores the assessment and management of pain in a person with dementia in partnership with the family carer. Nursing Older People. 30, 1, 27-32. doi: 10.7748/nop.2018.e985. Correspondence
3. Objectives In order to carry out the research in appropriate manner, there are aim that is set by the researcher. These are done so that proper steps can be taken with the help of which the research can be attained. In this context, below given are the aim and objectives of the research: Aim: To analyse the impact of dementia in older age people and identifying treatment provided: A study ...
Alzheimer's disease symptoms include memory loss, particularly difficulties learning new material or recalling recent events, speech issues such as repetition, loss of concentration, difficulty planning or organising, and hallucinations and delusions in the latter stages of dementia. Anjeela in the case study forgot that her husband had passed ...
Nursing Assignment Solution on Case Study on Dementia INTRODUCTION. Dementia is a mental disorder which affects an individual's intellectual and cognitive abilities which interfere with his/her daily activities (Birren, 2013).
Summary. The paper "The Diagnosis of Dementia" is a worthy example of a case study on health sciences and medicine. The essay is about Mrs. C who apparently checked into a hospital with clear symptoms of dementia…. Download full paper File format: .doc, available for editing.
MENTAL HEALTH CASE STUDY ASSIGNMENT Dementia is a syndrome that is used for discussing various symptoms that involve a decline in cognition. Specifically forgetfulness. It is caused due to a number of an underlying disorder and brain dysfunctioning. Livingston et al. (2017) opined that dementia is not a
Sue's story - dementia case study A daughter's peace of mind. What matters most to the families we support is that their loved one is safe and comfortable. When Sue needed some more support for her mother, Barbara, she decided that a live-in carer would be the best option. Barbara's carer, Rosemary, quickly became part of the family.