- Open access
- Published: 10 September 2022

Living with tuberculosis: a qualitative study of patients’ experiences with disease and treatment
- Juliet Addo 1 ,
- Dave Pearce 2 ,
- Marilyn Metcalf 3 ,
- Courtney Lundquist 1 ,
- Gillian Thomas 4 ,
- David Barros-Aguirre 5 ,
- Gavin C. K. W. Koh 6 &
- Mike Strange 1
BMC Public Health volume 22 , Article number: 1717 ( 2022 ) Cite this article
10k Accesses
5 Citations
2 Altmetric
Metrics details
Although tuberculosis (TB) is a curable disease, treatment is complex and prolonged, requiring considerable commitment from patients. This study aimed to understand the common perspectives of TB patients across Brazil, Russia, India, China, and South Africa throughout their disease journey, including the emotional, psychological, and practical challenges that patients and their families face.
This qualitative market research study was conducted between July 2020 and February 2021. Eight TB patients from each country ( n = 40) completed health questionnaires, video/telephone interviews, and diaries regarding their experiences of TB. Additionally, 52 household members were interviewed. Patients at different stages of their TB treatment journey, from a range of socioeconomic groups, with or without TB risk factors were sought. Anonymized data underwent triangulation and thematic analysis by iterative coding of statements.
The sample included 23 men and 17 women aged 13–60 years old, with risk factors for TB reported by 23/40 patients. Although patients were from different countries and cultural backgrounds, experiencing diverse health system contexts, five themes emerged as common across the sample. 1) Economic hardship from loss of income and medical/travel expenses. 2) Widespread stigma, delaying presentation and deeply affecting patients’ emotional wellbeing. 3) TB and HIV co-infection was particularly challenging, but increased TB awareness and accelerated diagnosis. 4) Disruption to family life strained relationships and increased patients’ feelings of isolation and loneliness. 5) The COVID-19 pandemic made it easier for TB patients to keep their condition private, but disrupted access to services.
Conclusions
Despite disparate cultural, socio-economic, and systemic contexts across countries, TB patients experience common challenges. A robust examination of the needs of individual patients and their families is required to improve the patient experience, encourage adherence, and promote cure, given the limitations of current treatment.
Peer Review reports
Tuberculosis (TB) is a communicable infectious disease affecting around one quarter of the world’s population [ 1 ]. The ‘BRICS’ countries of Brazil, Russia, India, China, and South Africa account for 47% of the total number of TB cases annually [ 1 , 2 , 3 ].
Caused by the bacillus Mycobacterium tuberculosis , around 5–10% of those infected will develop active disease. In 2019, 10 million new active cases and 1.4 million deaths were reported [ 1 ]. In 2020, the coronavirus disease 2019 (COVID-19) pandemic severely impacted the reporting of new cases and impeded diagnosis and treatment [ 3 ]. Treatment for multidrug-resistant TB (MDR-TB) also declined by 15% (from 177,100 in 2019 to 150,359 in 2020), with only about a third of patients who needed this treatment obtaining access [ 3 ].
Ambitious targets to end the TB epidemic by 2035 were established in 2015 by the WHO’s End TB Strategy [ 4 ], aligned with the United Nations Sustainable Development Goals [ 5 ]. In 2018, a United Nations General Assembly High-Level Meeting on Tuberculosis resulted in a Political Declaration on Tuberculosis, committing to end TB globally by 2030 [ 6 ]. Achieving these goals requires more equitable deployment of existing measures, and the development of new tools for TB prevention, diagnosis and treatment [ 7 ]. Progress towards ending TB also demands that interventions are aligned to patients’ experiences and address the challenges that they face [ 8 , 9 ].
TB typically involves the lungs (pulmonary TB) and is acquired via inhalation of droplet nuclei in the air following exposure usually over several hours. Close contact and the infectiousness of the source patient are key risk factors for the infection of tuberculin-negative persons [ 10 ]. Current treatment of drug-susceptible TB requires combination therapy consisting of an intensive phase of 2 months of isoniazid, rifampin, pyrazinamide, and ethambutol, followed by a continuation phase of 4 months of isoniazid and rifampin [ 11 ]. Directly observed therapy (DOT) is recommended to ensure adherence to the complex regimen and to deter the emergence and spread of MDR-TB. Treatment is successful in around 85% of patients following 6 months’ therapy [ 1 ]. Also, individuals can become non-infectious within two weeks of treatment initiation, restraining disease transmission [ 1 ]. Thus, prompt initiation of therapy is important for both the patient and their close contacts. However, the management of TB is complicated by the increasing prevalence of MDR-TB, which requires prolonged and complex therapy, and is more likely to be associated with poor outcomes [ 12 ]. Even after successful treatment, patients may have ongoing lung disease and a decreased life expectancy [ 13 , 14 , 15 ].
The drugs used to treat tuberculosis are well understood clinically, and susceptibility testing will indicate which treatment regimen is appropriate [ 11 , 12 ]. However, treatment effectiveness depends on patient adherence to a demanding and lengthy treatment regimen with associated side effects. In this context, a patient-focused approach which considers the individual’s specific circumstances is needed to ensure sufficient adherence and good outcomes from therapy. Interest in this field has been building steadily and is most suited to a qualitative investigational approach which allows deep exploration of motivations, reactions, goals, aspirations, and circumstances. However, studies more often consider the challenges faced by healthcare workers caring for TB patients [ 16 ], or the implementation of new management tools [ 17 , 18 ].
Previous studies have examined how patients manage their illness and the impact that TB has on their daily lives, their families, and the wider community [ 19 , 20 ], as well as the stigma associated with poverty and HIV and the effects of discrimination [ 21 ]. However, defining studies on the experiences of TB patients and their families are not available for all the BRICS countries, and comparison between studies with different methodologies and objectives is problematic. It is, therefore, unclear to what extent the experiences of TB patients are shared across countries.
We report the findings of a qualitative evaluation of TB patients’ experiences across the five BRICS countries. The study aimed to identify commonalities across the different country contexts, by examining the perspectives of TB patients throughout their full disease journey, including the emotional, psychosocial and practical challenges that patients and their families face. A greater understanding of these factors could inform care more focused on patients’ needs, with the aim of improving outcomes and directing the development of new tools to end TB.
Study design
This qualitative market research study was designed collaboratively by GSK and Adelphi Research and conducted between July 2020 and February 2021 across the five BRICS countries (Brazil, Russia, India, China, and South Africa). The study was non-interventional and without clinical endpoints. The aim was to achieve a better understanding of the TB market across the BRICS countries by identifying common challenges faced by TB patients and their families in their daily lives throughout their treatment journey.
The study conformed to ethical principles laid down in the Declaration of Helsinki, all national data protection laws and industry guidelines. Participants’ data was protected by compliance with General Data Protection Regulation [ 22 ]. All participating patients and household members provided written voluntary informed consent, and parents provided written consent for children under the age of consent. Consent was also provided for anonymized publication of the findings. For consent forms see supplementary materials, Additional file 1.
To investigate the experiences, meanings, and perspectives of TB patients, qualitative methodology was employed to identify themes within and across countries from in-depth interviews and self-recorded videos, supported by a self-completed health questionnaire.
Participants with experiences relevant to the study objectives were actively recruited from BRICS countries because they account for more TB cases than any other country in their respective WHO regions, and because of the different additional challenges confronting these countries such as the burden of TB-HIV co-infection in South Africa, the diversity of private sector care in India, and the burden of MDR-TB in India, China and Russia [ 1 , 2 , 23 ]. Remote data collection both preserved the privacy of participants and ensured the safety of moderators given the infectious nature of TB and the timing of the study during the COVID-19 pandemic.
Recruitment
Participants were recruited through independent healthcare fieldwork agencies in the different countries via referral from healthcare professionals and social or community workers, as well as using market research databases, posters and adverts in TB clinics, patient groups, and word of mouth referrals. Participants had the opportunity to discuss the study with recruiters before completing a screening guide to confirm patient eligibility (Additional file 2). Recruited participants received an honorarium at fair market value for their participation.
Recruitment continued until TB patients from 40 households, that is 8 per country, plus 1–5 members of their households had been sampled. The minimum target sample size was 80 participants. Previous studies have indicated that for this type of qualitative research as few as 6 interviews per setting are required to identify major themes [ 24 , 25 ], with saturation occurring within 12 interviews [ 26 ].
Participants
Eligible participants had a confirmed diagnosis of TB and were receiving treatment or had completed treatment within the previous 12 months. Close family and other household members were included where appropriate for support and additional information, except for China where the social stigma prevented discussion with individuals other than the patient. Participants were recruited from a range of socio-economic backgrounds, assessed based on income, education levels, and living standard. At least three participants from each country were to be female. The study sought to include a range of specific patient types, for example, persons living with HIV (PLWH), those with diabetes, smokers, those with a history of excessive alcohol consumption, and those with MDR-TB/relapsed TB. At least two patients per country were to be living in households which included a child diagnosed with TB or receiving preventive treatment. No participant was excluded because of lack of access to technology as the necessary equipment was loaned to participants where needed.
Data collection
The interview moderators, fluent in the local languages, were taken through a training process in each setting, detailing study objectives, inclusion criteria, and study methodology, followed by subsequent monitoring of the process and active feedback to ensure quality control. Data quality was assured by consistent and thorough briefing of the field workers, including regular follow up to ensure study procedures were followed. The discussion guide and videoing instructions were carefully designed to contain clear respondent instructions at each question.
Patients first completed a 5-min health questionnaire based on their physical health over the previous four weeks. Interviews with TB patients and household members were conducted remotely by a trained moderator in the form of either a 60-min video-streamed interview or a 60-min telephone interview. The questionnaire and interview guides are provided in the supplementary materials (Additional file 3). Participants also completed a 45-min follow up video task to create four short videos on a mobile phone in their own time to capture their personal experience, such as their living environment, changes in their living arrangements as a result of TB, the biggest challenges since the diagnosis, perception of the changes in their life from others around them, and their hopes and expectations for the future.
The interviews were transcribed verbatim from the original languages, that is: Brazil, Portuguese; Russia, Russian; India, Hindi and English; China, Mandarin; South Africa, English, Sesotho, isiZulu, Tswana, or Afrikaans with switching between languages as necessary. Following translation into English, the information was analysed manually using a thematic and comparative analysis approach to identify key themes both within countries and across all participants’ responses [ 27 , 28 ]. Analysts had no access to patient medical records and all patient identifying information was anonymized.
Interviews were coded thematically by three analysts, aiming to reach consensus through regular team meetings where the emerging findings were discussed. Additionally, non-verbal communication (including visual evidence of living conditions) present in the videos from the streamed interviews and the video tasks were shared with the full team at regular intervals and discussed/analysed using the thematic framework developed from the transcripts. Triangulation across the different data sources was done using cross-checking to assess convergence, complementarity and divergence at the individual participant level, between patients and their families, and at the country level between informants from the same country. The analysis was therefore grouped initially by country and then analysed for cross-cutting themes across all respondents. Quality control was achieved by continuous review by two senior analysts, one of whom was not involved in the initial analysis, plus a final check through all the analyses.
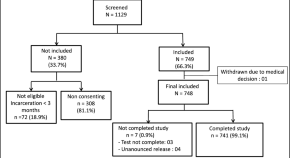
The sample consisted of 40 TB patients (8 from each country) plus 52 household members. Each patient was assigned an identifier to illustrate their country and number. Of the TB patients, 23 were men and 17 women, ranging between 13 and 60 years old. Fourteen were receiving first-line treatment, 10 second-line treatment, 2 patients had received multiple treatment lines, 11 had completed treatment, and 3 patients (all from Russia) were on a treatment break (Table 1 , Fig. 1 ). Risk factors for TB were reported in 23/40 patients, with some patients having multiple risk factors (Table 1 , Fig. 1 ). Most patients were of medium socio-economic status for their country (26/40), and no patients with high socio-economic status were recruited (Table 1 ). Except for India and South Africa, it was not possible to recruit at least two households with a child diagnosed with TB or receiving preventive treatment (Table 1 ).
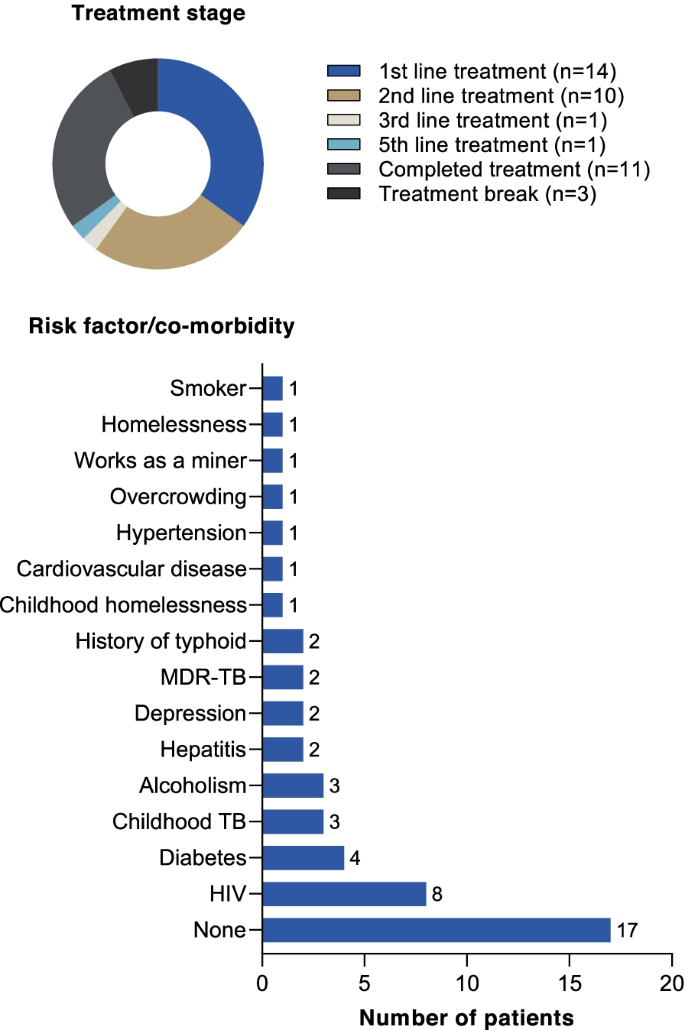
Summary of patient characteristics. Note that patients may have had more than one risk factor/co-morbidity
Patient health status
The self-reported health questionnaire indicated that most respondents (25/40) found that the physical impact of TB limited their activity. A higher proportion of patients who were currently receiving treatment (69.6% [16/23]) reported a physical impact of TB compared with those that had completed treatment (57.1% [8/14]) or who were on a treatment break (33.3% [1/3]). Most patients whose physical activity was impacted by TB reported that this affected them all or most of the time (88.0% [22/25]) (Fig. 2 A). Most patients (38/40) reported that their daily living was impacted in at least two ways (Fig. 2 B). Seven patients, five of whom were receiving treatment and two who had completed first-line treatment, stated that they were impacted by all six areas assessed (Fig. 2 B). Looking at specific impacts, the most reported were that TB stopped patients doing things that they liked to do (35/40), and economic hardship (28/40) (Fig. 2 C). Overall, it was clear that TB had significantly impaired the health status of patients and had a negative impact on daily living.
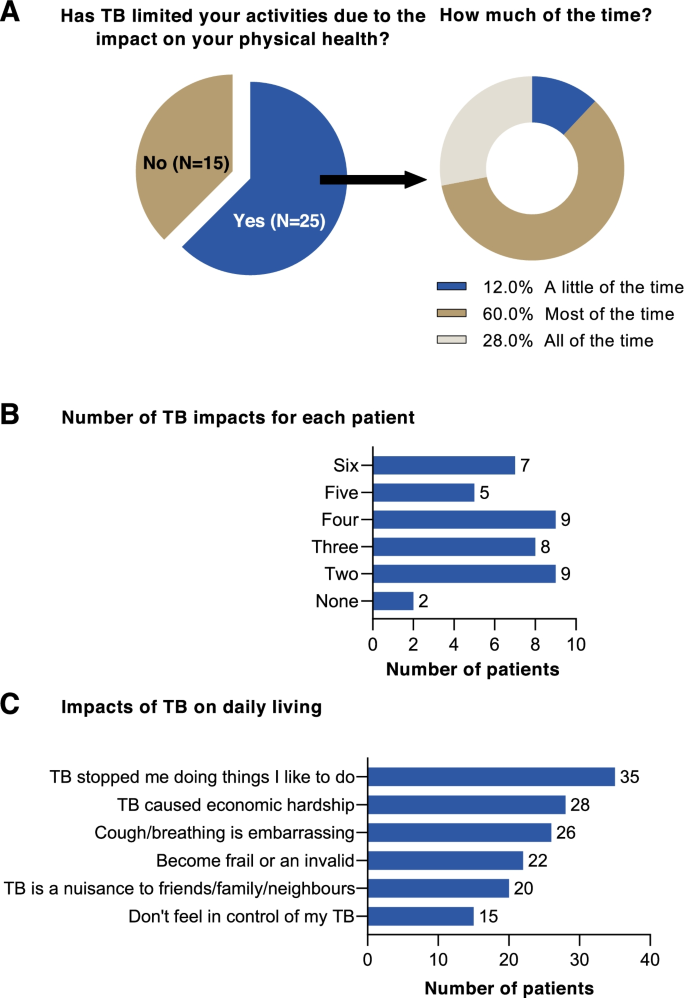
Results of a self-reported health questionnaire. A The effect of TB on limiting daily activity due to patients’ physical health; B ) the impact of TB on daily living; and C ) the number of impacts on daily living experienced by patients
Patient journey
Pre-diagnosis.
The most common initial symptoms reported by patients were a long-lasting cough increasing in severity over time, fever, weight loss, and tiredness. Some patients experienced more severe symptoms such as haemoptysis, and pleural effusion. However, symptoms were often non-specific, and unless they were aware of a source of infection or had known risk factors (e.g. HIV), most patients did not consider TB as a potential cause. Notably, patients in South Africa were more likely to suspect TB because of a higher awareness in the community and the link with HIV. In India, recent typhoid infection was suspected as the cause of symptoms in some cases.
Patients tended to hope that the symptoms would resolve on their own using over-the-counter products and traditional medicine. Patients with addiction to alcohol did not always perceive the severity of their symptoms and were less willing to engage with healthcare providers. However, avoidance of healthcare providers was common across all settings, because of concerns for the associated costs.
“The symptoms were there for the last 2 ½ months but I did not know. He was coughing a lot, so I asked him to go to the doctor. He did not listen to me. He feared talking to the doctor.” Relative of TB patient, India (IN19). “One day, I started to have fever in the afternoon. After work, I went to receive infusion in a small local clinic. I remember my body temperature was 39.5 to 39.6 degrees Celsius. The doctor said my condition was very serious, so he prescribed 5 bottles of infusion to me, and I received all of them. But my fever persisted after such a lengthy infusion.” China (CN09).
The pathway for TB cases depended on symptom severity at presentation but navigating the healthcare system was tortuous for some patients. Patients first sought help using a familiar and accessible route (Fig. 3 ).
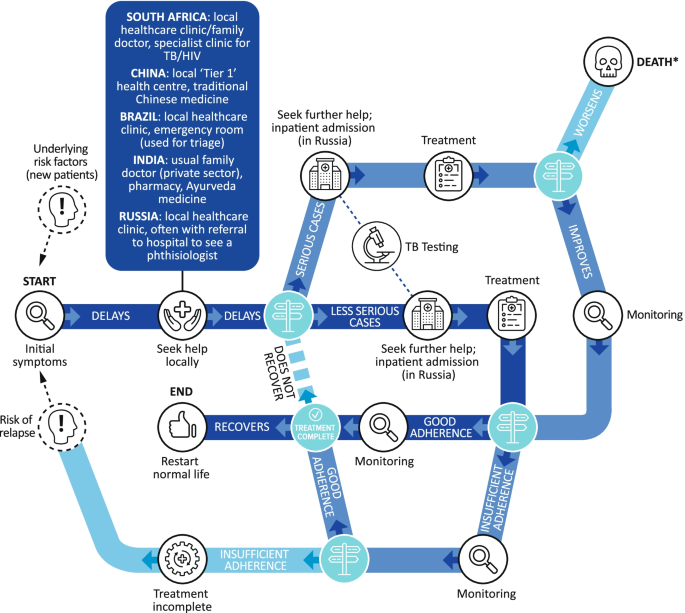
The TB patient pathway. *There were no deaths during the study
Across all countries, the TB diagnosis came as a shock to most patients – their initial thought was ‘Will I die?’. PLWH were less surprised as they were aware of the association with TB. Some patients in South Africa believed they had been vaccinated against TB as children and were therefore protected. Many patients questioned how they had caught TB and worried about the negative misconceptions associated with the disease, particularly in Russia and Brazil. Patients feared that they would be ostracized and shunned by their families and communities. Young people with TB feared for their future, for example their careers, education, and prospects of marriage. Further concerns expressed by patients included the potential disruption to their life, job security and providing for their dependents, especially in India. Overall, there was uncertainty among patients as to whether they could cope; some expressed the fear of unintentional disclosure of their TB diagnosis to others. Notably, across all countries, families were often fearful of the potential costs, with a lack of clarity regarding which elements of treatment would be covered by insurance (where available) or were refundable from the public health system.
“[I thought] it is some kind of prison disease, which occurs more and more often in people who have served a sentence somewhere. That is, more disadvantaged groups of the population. I always thought about it in this way until I met it myself.” Russia (RU10).
Following diagnosis, healthcare providers were quick to reassure patients that TB is treatable but that it will take time and that they must try not to infect others. In South Africa some patients reported being warned of drug resistance. However, beyond this, TB-focused education was limited, and patients often conducted their own research via the Internet and word of mouth, though patient-friendly resources were described as inadequate in some settings.
“[The nurse] said if you don’t take your meds, they send you to [a TB hospital] and then you will receive extreme treatment. They inject you with needles and stuff. That is if you don’t use this meds at home, they will send you there and stay for six months.” South Africa (SA05).
Treatment side effects, pill burden, lifestyle restrictions and the long-term commitment required were very challenging for patients (Fig. 4 ). Patients generally did not know the names of their medications, but described having to take many pills of different types several times a day. Patients reported intolerable side effects, including nausea and vomiting, and patients with MDR-TB faced painful daily injections. In Russia, and to a lesser extent in China, patients were admitted to hospital to increase adherence. In Russia, patients recounted being admitted to sanatoriums for the treatment of TB.
“I take many anti-TB pills every day, covering 4–5 classes, about 20 tablets in total. Sometimes, it’s difficult for me to take medication, as I was quite reluctant to take it initially, but I had no choice, but to take it as a treatment.” China (CN11).

Factors identified by patients as affecting adherence to TB therapy
Monitoring and adherence
Across countries and socioeconomic bands, patients perceived minimal therapy monitoring by healthcare providers, with little evidence of DOT. It is possible that this was because of interruption to normal healthcare services because of the COVID-19 pandemic (see below). Most patients visited healthcare settings frequently to pick up their medications. Less frequently, their weight was measured during clinic visits, sputum tests were conducted, and some patients were informed when they were no longer infectious and could return to work/education. Family played a key role in monitoring during treatment, encouraging patients to continue with their treatment, sharing regular reminders, and helping to pick up medication from health centres. Motivation to comply was prompted by the desire to get back to normal family life and work, the fear of death, potential drug resistance, and hospitalization. Although patients would briefly lapse without serious consequences, they were usually encouraged to continue treatment by family and healthcare providers.
“Sometimes [redacted] forgets to take the medication, and I argue with him because if one of us forgets the treatment and the other one doesn’t then it won’t work, if we don’t take it together, it won’t work.” Brazil (BR04).
Once treatment was initiated, health improvements were quickly apparent to most patients, with resolution of fever and abatement in cough. Although this increased patients’ optimism and secured a return to some of their previous activities, it could also lead patients to believe that they had recovered, undermining adherence to therapy. Adherence was also jeopardized where there were high barriers to accessing treatment, a poor understanding of drug resistance, and when patients were alcohol dependent (Fig. 4 ). Patients who did adhere to treatment were often well supported by family and well informed of the consequences of non-adherence. Conversely, those who did not adhere to treatment were often unaware of the consequences.
“By December I was already feeling like I’m already cured, I nearly decided not to continue with the treatment.” South Africa (SA01). “Actually, they didn’t tell me about the details then. It was very important to emphasize it to me, but the physician didn’t do it. If he did, it would draw my attention and it won’t lead to drug resistance, as I often missed the dose I was supposed to take.” China (CN06). “I live in a little town which is quite far from the city. I can either go by bus which takes at least an hour and a half, or I can get to the nearest bullet train, but there aren’t many trains available and they are expensive.” China (CN08).
Completion of treatment
Eleven patients had completed treatment, 4 from South Africa, 4 from India, 2 from Brazil, and 1 from China. All had recovered, 10 following first-line treatment and 1 following second-line treatment (India). Some respondents said that their time in isolation was a time of reflection where their lives had been ‘put on pause’ making them ‘appreciate the little things in life’ they had really missed. A few patients said that their experience with TB has driven them to want to increase awareness, and remove stigma around the disease e.g., patients in Brazil and China set up informal support networks with fellow patients, particularly where patients met during hospital stays. Most patients expressed relief that they were cured, and that treatment was over, and were generally hopeful for their future.
"My TB is cured, and I want to start again with my studies. I was preparing for a railway job but I had to give that up because of TB. Now I will start my studies again and apply for a government job." India (IN04). "Thanks to this [TB] I got rid of bad habits, I do not drink alcohol now and smoke less… And I found a job, and I earn some money at the moment, during the first period my brother supported me fully, thanks to him, and my mother helped what she could.” Russia (RU05). "After these three months since I have recovered, this is what it has brought me, the willingness to fight, to battle, also to take even more care of my health, not just mine but also of people around me, and take this story, my testament, my lived experience with TB… So it’s a goal in my life, to spread information among all those who are close to me." Relative of TB patient (BR01).
Access to services
Before TB was diagnosed, in some cases patients consulted healthcare providers in the private sector, for example, the local family doctor, traditional medicine providers, or pharmacies. Following diagnosis, more affluent patients claimed on insurance or paid for private sector treatment due to poor perceptions of the public sector, and some sought support in the private sector for a ‘second opinion’ or for problems which they felt were not being addressed in the public sector. However, the majority of patients (36/40) obtained their TB care through the public sector; three patients used the private sector with one accessing both public and private sector healthcare. Treatment was provided for free through the national programs, with relatively good access in most settings, though travel distance and wait times were a barrier to access. There were reports of drug stock outs and out of pocket expenses for additional diagnostic tests or prescriptions, including having to pay for MDR-TB treatment in some settings (China). A minority of patients reported being turned away from the public sector for not having the correct paperwork or not being able to book an appointment. The public sector had a poor reputation for long queues and poor service and most patients aspired to be able to afford private treatment where services were described as being better.
“In public [sector healthcare] those nurses don’t care, I remember when I accompanied him, I was told I was not allowed to get inside, so he went in on his own. You go in pick up whatever you need and get out because those people don’t have time for anything.” Relative of TB patient, South Africa (SA01). “In the Government hospital, the doctors do not listen to us. They come when they wish and give medicines. As it is, the doctors do not listen to poor people. I had to buy some medicines from outside.” Relative of TB patient, India (IN17). “Obtaining the medication – because the drugs can only be obtained in the hospital, you can’t buy them in retail pharmacies. If I run out of my medication, I wouldn’t be able to buy it from the retail pharmacy, I would have to go the hospital, which is inconvenient.” China (CN08).
The use of sanatoriums in Russia was unique. Following diagnosis, patients were sent to a dedicated facility or a TB unit within a hospital where they remained for at least 3–4 months, though confinement could last for up to a year. They were only allowed to leave with permission, for example, at weekends or holidays. Although patients generally accepted that it was for the ‘greater good’ it was frightening at first because some other patients on the ward had very severe disease. However, some patients expressed surprise that other patients were ‘normal’, because they believed the disease to be often associated with homelessness and prisons.
“They told me I had a resistant form of TB and that the treatment is very, very long lasting. At first, they said I would have to be hospitalized three to four months and that then I would be able to go home but when I got to the hospital, the ‘girls’ told me that three to four months is optimistic… In short, eight months. Eight in the hospital and a year after the hospital. That was a shock.” Russia (RU12). “In my room there were all young women and all were so great. All of them were socially adapted: an accountant, a paediatrician student. So, let’s say it was good company.” Russia (RU01).
Thematic analysis
Five major themes were identified as common across all the countries studied (Fig. 5 ).
Thematic areas identified as common across five countries describing the challenges faced by TB patients
Economic hardship
Loss of earnings has the greatest economic impact for TB patients. Most patients stopped work because they felt too unwell to continue or were embarrassed by the symptoms, such as the persistent cough and severe weight loss. Some patients also felt the need to stay away from work to limit transmission to others or were ‘asked to leave’ by their employers as they were not covered by contracts. Many had no entitlement to sick pay. In some cases, patients were concerned that their financial situation could get worse as their diagnosis may mean prospective employers may be reluctant to take them on.
“The main problem is money. There is no problem greater than financial problems.” India (IN01). “I had to keep away from work because there was a lot of dust involved.” Brazil (BR15). “I cannot officially get a job, and I cannot unofficially either. But, what? Am I going to work as a loader? I cannot. This has seriously affected my finances… And who would hire if information comes out that there was TB? You will not get a job. I received a disability [payment].” Russia (RU05).
Even in regions where TB treatment was publicly funded, associated costs such as tests, hospitalization, prescriptions, travel, special food/supplements to manage weight loss, and medications to manage adverse effects were often borne by patients. The financial impact of TB meant that most patients had to rely on family or sometimes charities for support or take out loans. Time off for appointments still impacted earnings even after patients had returned to work.
“I also buy medications at my own expense [for gastric side effects] i.e. for TB, everything is free of charge due to the medical insurance policy, everything is fine, but if there is something secondary or something else not related to the diagnosis, then that is at your own expense.” Russia (RU07). “We are not educated people. I just wanted my child to recover. We are poor people; we could not work during lockdown. We had to borrow money from many people and requested help from doctors too. I thought my child would recover, but he did not. We were very stressed out.” Relative of TB patient, India (IN21). “To avoid delaying treatment, the doctor told me to take these four drugs upon diagnosis, and urged me to buy them elsewhere, as they were unavailable in the hospital. My wife found they were unavailable in many pharmacies either. Finally, she found them in several pharmacies, from where we bought them in early stage.” China (CN09).
Stigma associated with TB
Across all countries stigma was associated with TB, though it manifested in different ways. In China, TB was often kept a secret, even from family, whereas in South Africa, there was greater openness. In Brazil, though patients were open with family, there was reluctance to acknowledge their diagnosis with their community as TB is associated with wider social issues such as poverty, incarceration and ‘immoral lifestyles’. In India, TB patients felt discriminated against for other reasons, such as poverty, as well as TB. Stigma in Russia was related to the personal circumstances of the patient.
Young patients faced bullying at school/college and being dropped by friendship groups. Adults were ostracized by friends and relatives afraid of contracting TB, and relationships with friends and family suffered, leading to loneliness and depression. Respondents described instances when they were not invited to family events even after they had completed treatment and were cured. In some cases, TB appeared to ‘run in families’ meaning the stigma was intergenerational. Importantly, a family with TB was often considered a ‘low status’ family and this was compounded by the financial difficulties that accompany TB.
“A lot of my friends kept away from me because of this, because that’s what people know, that it’s contagious, but they don’t understand that the person on the other side is suffering as well, and we don’t only suffer a little bit, at least myself, it’s a very painful process, very painful, very complicated.” Relative of TB patient, Brazil (BR01). “The community was no longer as close to us because we are staying with a person that has TB – people at the queue at shops would turn around and come back when we have left.” Relative of TB patient, South Africa (SA14). “When a person has TB he becomes very annoyed as he has to go through a lot of things, plus there also comes a phase were people start avoiding you, they feel that if we come in contact with this person even we might acquire it.” India (IN01). “A person who has TB is not somebody who is well-regarded.” Brazil (BR04).
HIV co-infection played a major role in the TB experience, particularly in South Africa. Awareness of TB was higher among PLWH given their greater risk and regular contact with healthcare services. Also, the path to diagnosis was shorter given their engagement with HIV services with rapid referral reflecting the associated co-infection risks. In many cases, the HIV and TB clinics were co-located improving patient access. However, PLWH were highly aware of the stigma that TB carries with fear around the community reaction during the early stages of their journey.
"Now I’m scared I’m HIV positive, I have TB and now there’s Corona [COVID-19], what’s going to happen when I have all three of them?" South Africa (SA18). “So people were really scared, I think they are now more afraid of TB than HIV. I told my neighbour that I was diagnosed with TB and luckily she doesn’t talk much but still I was aware of their behaviour when they came by to do my laundry they would wait outside to hand it over to them and when they are done they would leave it by the door." South Africa (SA10).
Disruption to family life
A diagnosis of TB affects everyone in the household and the wider family. Cleaning and disinfecting routines have to be established and maintained, and there was a general awareness that separate cutlery must be used, living spaces needed good ventilation, and clothes and bedding should be washed more frequently. Sleeping arrangements to isolate TB patients were particularly problematic in India and South Africa where large families live together, and parental co-sleeping with children was no longer possible where this was practiced. In some cases, children were looked after in the homes of extended family members, away from parents with TB. Married patients feared abandonment or divorce and respondents felt ‘lucky’ that their partners had stayed with them despite their TB status. The reduced family contact, demands of treatment and financial hardship often strained family relationships.
“Life at home isn’t the same because I had to begin separating my cutlery and a glass – my clothes had to be washed separately, we have to clean down the house and open the windows to let the air circulate.” Brazil (BR15). “I’m worried I may infect my parents. So I’ve had to reduce my interactions with them, the time spent with them, the number of occasions I’m with them. And as they get older, they become confused and they don’t understand why I stay away.” China (CN08). “Our house always used to be full at weekends, friends would come around to watch films, sometimes we would make lunch, get pizza and sit and watch films, and then suddenly the house was empty.” Relative of TB patient, Brazil (BR01).
Mixed effects of COVID-19
Some TB patients observed that the COVID-19 pandemic normalized the idea of infection prevention, with mask wearing becoming common. Also, TB patients were able to hide their diagnosis more easily with social distancing measures. There was also less fear that they could infect the wider community. However, access to healthcare and medication was compromised with restrictions to movement and hospitals not accepting admissions for other conditions. Patients were fearful of ‘catching’ COVID-19 given their impaired respiratory health and existing co-morbidities, such as HIV and diabetes. Some respondents who were coming to the end of their isolation and anticipating greater freedoms and a return to a more normal life then faced COVID-19 restrictions.
“During the pandemic I was unable to go to the hospital for my regular follow-ups and prescription renewal, and so because of that my condition worsened, and I eventually ended up infecting my family.” CN08.
Assuming that efficacious treatment is provided, TB is curable. However, outcomes are often sub-optimal. This study aimed to explore common themes in the experiences of TB patients and their families in the five BRICS countries from diagnosis to completion of treatment. Using consistent methodology, economic hardship, stigma, TB-HIV co-infection, disruption to family life, and the mixed effects of COVID-19 were identified as themes encompassing the challenges facing TB patients across the five BRICS countries (Fig. 5 ). These factors, therefore, appear to be independent of the country setting. Further research should investigate the degree to which these factors and are potentially mutable by targeting systemic changes in healthcare and social provision and providing attention to patients’ individual needs.
Economic hardship was reported across all countries. TB is associated with economic vulnerability but can also drive families into poverty through loss of income, the costs of transportation and food supplements, and associated medical expenses [ 29 , 30 , 31 , 32 , 33 , 34 , 35 , 36 ]. Programs providing social protection to TB patients have been linked to improved outcomes and the increased uptake of preventive therapy but must be easily accessible [ 29 , 37 , 38 ]. Improvement of TB services can also reduce the number of families facing financial hardship [ 39 ]. Even though most healthcare systems in our study provided TB drugs free of charge, to be effective, treatment should encompass the wider economic impacts that patients experience. Despite various approaches, patients from all of the countries surveyed found themselves struggling financially and a more holistic approach to patient support is needed.
Stigma attached to TB is culturally distinct, but stems from a lack of awareness of TB and the persistence of stereotypes [ 40 , 41 ]. For example, in Russia, an association with prisons and poverty has persisted, despite TB affecting all sectors of society [ 42 ]. Stigma was most acutely felt in China, and a recent study described psychological distress in nearly two-thirds of TB patients, associated with a high experienced stigma [ 43 ]. In our study, some patients did not even disclose their diagnosis to close family. In newly diagnosed Chinese TB patients, non-disclosure of their TB status magnified patient-perceived stigma and was associated with depression – a risk factor for non-adherence [ 44 , 45 ]. Social support and doctor–patient communication appeared key factors for reducing TB-related stigma in China [ 46 ]. Also, educational approaches to raise awareness of TB diagnosis and treatment among the public are needed, particularly focused on those with low educational levels and more rural communities [ 40 , 47 , 48 ].
The association between TB and HIV is well documented. However, the impact on patients is less well understood. In this study, PLWH were more aware of TB and were more likely to seek care early and be diagnosed quickly. This is in contrast to a study in Thailand where PLWH had low TB awareness and attributed their early symptoms to AIDS, resulting in delayed TB diagnosis [ 49 ]. This emphasizes the importance of raising TB awareness in PLWH. In South Africa, TB and HIV services are often co-located and integrated [ 50 ]. However, a detailed analysis in South Africa of the challenges faced by PLWH who had MDR-TB highlighted similar issues to those described here for all TB patients, such as fear, stigma, dissociation from family and social networks, poor provider support, drug adverse events, and financial insecurity [ 51 ]. Also, patients tended to prioritize adherence to anti-retroviral therapy versus TB therapy because it was less challenging in terms of pill burden and adverse effects [ 52 ]. Until less demanding treatment regimens are available, targeted support to address the challenges of adherence in patients co-infected with TB-HIV is necessary.
The respondents in this study described a severely disrupted home life following a TB diagnosis. Patients were isolated and often infirm, and the economic and care responsibilities for family members were considerable. Families also suffered socially, being isolated or shunned by friends and the wider family. In many cases, it was family members who ensured adherence to medication, and social and family support for patients has been previously shown as a key factor in therapy adherence [ 41 , 53 , 54 ]. Despite this, the impact of the TB diagnosis on the family and how family members can best be supported has been rarely investigated [ 47 ], and we identify this as an important area for further research.
The COVID-19 epidemic has disrupted healthcare access globally [ 55 ]. In our study, TB patients reported drug shortages and restrictions to services during the period. TB patients also expressed concern regarding the consequences of contracting COVID-19. Similarly, a recent study in Brazil reported that TB patients were fearful of attending medical appointments [ 56 ]. TB patients do appear to be at greater risk of death or poor outcome with COVID-19 [ 57 ], and should therefore socially isolate or ‘shield’ [ 58 ]. TB patients did feel less stigmatized as social distancing and infection control measures were deployed for COVID-19. However, the interruption of treatment, with the risk of therapy failure, selection of MDR-TB, and increased transmissibility is a major threat to TB patients and their close contacts [ 59 ].
This study has several limitations. Although participants were identified through a variety of channels and a range of socioeconomic groups were sampled, this was not a randomized sample and we acknowledge that both marginalized and privileged groups may not engage in this kind of research. Also, there were no data on whether susceptibility testing was conducted following the TB diagnosis, so the appropriateness of therapy could not be assessed. Neither did we examine the differences between patients’ experiences of drug-susceptible versus MDR-TB; patients were not consistently aware of the difference and most patients were receiving or had recently completed first-line therapy. The patient pathway was not integrated into the thematic analysis but analysed separately in terms of the systemic challenges that patients face. This was because the complexity of the pathway did not map onto the themes in a meaningful way. For example, patients experienced economic hardship, stigma, and disruption to family life at most stages in the patient pathway, whereas TB-HIV co-infection had an important effect on the speed of diagnosis. Thus, patient pathway was examined systematically and separately to the thematic analysis which focused on the emotional, socio-economic and practical impacts of TB on patients’ daily lives. The analysis methods sought to remain impartial with repeated reviews by multiple analysts to reach consensus. However, the analysts were all based in the UK and we recognize that the cultural subtleties of some of the patients’ experiences may not have been fully appreciated.
In our study, TB patients’ perceptions and needs were expressed in their own words, from within their home environment, in confidence, to interviewers who were not involved in their healthcare. Most had struggled to adjust to their diagnosis, had poor access to information, lacked support from healthcare workers, were under significant financial pressure, and were highly conscious of stigma and the burden TB placed on their families.
Our findings highlight that much work still needs to be done before the goal of ending TB can be achieved. Structural changes require simplification of the TB patient pathway, reliable access to services, and the alleviation of financial pressures. Health education for patients, their families, healthcare providers and the public to increase awareness of TB symptoms and diagnosis, to encourage adherence, and to reduce stigma around the disease is needed. Importantly, TB patients do better with strong family and social networks to sustain them, and a greater understanding of how these can be better supported at the level of the individual patient throughout the TB treatment journey requires further investigation.
Despite the different cultural, political, and healthcare settings across the BRICS countries, TB patients faced very similar challenges. This commonality would not necessarily have been expected. It suggests that these factors are not only a product of the healthcare provision in the countries or the social, economic, and cultural pressures that patients face, but reflect an overarching insufficiency in the treatment of TB. The efficient delivery of comprehensive individualized care and support would certainly mitigate the negative impacts of TB on patients. However, these issues will likely not be fully resolved until treatment options are available that rapidly cure TB and prevent onward transmission.
Availability of data and materials
All relevant data are included in this publication. Recorded interviews will not be made available in order to maintain patient confidentiality. However, anonymised transcripts are available on reasonable request to the authors for ten years following study completion. For data requests please contact the corresponding author at [email protected].
Abbreviations
Coronavirus disease of 2019 (severe acute respiratory syndrome coronavirus 2)
Human immunodeficiency virus
Multidrug-resistant tuberculosis
People living with HIV
- Tuberculosis
World Health Organization. Global tuberculosis report 2021. 2021. https://www.who.int/publications/i/item/9789240037021 . Accessed 1 Nov 2021.
Creswell J, Sahu S, Sachdeva KS, Ditiu L, Barreira D, Mariandyshev A, Mingting C, Pillay Y. Tuberculosis in BRICS: challenges and opportunities for leadership within the post-2015 agenda. Bull World Health Organ. 2014;92(6):459–60.
Article PubMed PubMed Central Google Scholar
World Health Organization. Global tuberculosis report 2020. 2020. https://www.who.int/publications/i/item/9789240013131 . Accessed 1 Nov 2021.
World Health Organization. The End TB Strategy: Global strategy and targets for tuberculosis prevention, care and control after 2015. 2014. https://www.who.int/tb/strategy/End_TB_Strategy.pdf . Accessed 4 July 2021.
Floyd K, Glaziou P, Houben R, Sumner T, White RG, Raviglione M. Global tuberculosis targets and milestones set for 2016–2035: definition and rationale. Int J Tuberc Lung Dis. 2018;22(7):723–30.
Article CAS PubMed PubMed Central Google Scholar
United Nations General Assembly. A/RES/73/3. Political declaration of the high-level meeting of the General Assembly on the fight against tuberculosis. 2018. https://www.un.org/en/ga/search/view_doc.asp?symbol=A/RES/73/3 . Accessed 4 July 2021.
World Health Organization. WHO consolidated guidelines on tuberculosis. Module 1: prevention – tuberculosis preventive treatment. 2020. https://www.who.int/publications/i/item/who-consolidated-guidelines-on-tuberculosis-module-1-prevention-tuberculosis-preventive-treatment . Accessed 4 July 2020.
Shete PB, Reid M, Goosby E. Message to world leaders: we cannot end tuberculosis without addressing the social and economic burden of the disease. Lancet Glob Health. 2018;6(12):e1272–3.
Article PubMed Google Scholar
Hoos A, Anderson J, Boutin M, Dewulf L, Geissler J, Johnston G, Joos A, Metcalf M, Regnante J, Sargeant I, et al. Partnering with patients in the development and lifecycle of medicines: A call for action. Ther Innov Regul Sci. 2015;49(6):929–39.
Reichler MR, Khan A, Yuan Y, Chen B, McAuley J, Mangura B, Sterling TR. Tuberculosis epidemiologic studies consortium task order team: Duration of exposure among close contacts of patients with infectious tuberculosis and risk of latent tuberculosis infection. Clin Infect Dis. 2020;71(7):1627–34.
World Health Organization. Guidelines for treatment of drug-susceptible tuberculosis and patient care. 2017. https://apps.who.int/iris/bitstream/handle/10665/255052/9789241550000-eng.pdf . Accessed 4 July 2021.
World Health Organization. WHO consolidated guidelines on tuberculosis. Module 4: treatment - drug-resistant tuberculosis treatment. 2020. https://www.who.int/publications/i/item/9789240007048 . Accessed 4 July 2021.
Hoger S, Lykens K, Beavers SF, Katz D, Miller TL. Longevity loss among cured tuberculosis patients and the potential value of prevention. Int J Tuberc Lung Dis. 2014;18(11):1347–52.
Article CAS PubMed Google Scholar
Allwood BW, Byrne A, Meghji J, Rachow A, van der Zalm MM, Schoch OD. Post-tuberculosis lung disease: Clinical review of an under-recognised global challenge. Respiration. 2021;100(8):751–63.
Mkoko P, Naidoo S, Mbanga LC, Nomvete F, Muloiwa R, Dlamini S. Chronic lung disease and a history of tuberculosis (post-tuberculosis lung disease): Clinical features and in-hospital outcomes in a resource-limited setting with a high HIV burden. S Afr Med J. 2019;109(3):169–73.
Matakanye H, Ramathuba DU, Tugli AK. Caring for tuberculosis patients: Understanding the plight of nurses at a regional hospital in Limpopo Province, South Africa. Int J Environ Res Public Health. 2019;16(24):4977.
Article PubMed Central Google Scholar
Thomas BE, Kumar JV, Periyasamy M, Khandewale AS, Hephzibah Mercy J, Raj EM, Kokila S, Walgude AS, Gaurkhede GR, Kumbhar JD, et al. Acceptability of the medication event reminder monitor for promoting adherence to multidrug-resistant tuberculosis therapy in two Indian cities: Qualitative study of patients and health care providers. J Med Internet Res. 2021;23(6): e23294.
Milligan H, Iribarren SJ, Chirico C, Telles H, Schnall R. Insights from participant engagement with the tuberculosis treatment support tools intervention: Thematic analysis of interactive messages to guide refinement to better meet end user needs. Int J Med Inform. 2021;149: 104421.
Dias AA, de Oliveira DM, Turato ER, de Figueiredo RM. Life experiences of patients who have completed tuberculosis treatment: a qualitative investigation in southeast Brazil. BMC Public Health. 2013;13:595.
Bhattacharya Chakravarty A, Rangan S, Dholakia Y, Rai S, Kamble S, Raste T, Shah S, Shah S, Mistry N. Such a long journey: What health seeking pathways of patients with drug resistant tuberculosis in Mumbai tell us. PLoS ONE. 2019;14(1): e0209924.
Courtwright A, Turner AN. Tuberculosis and stigmatization: pathways and interventions. Public Health Rep. 2010;125(Suppl 4):34–42.
The European Parliament and the Council of the European Union: Regulation (EU) 2016/679 of the European Parliament and of the Council of 27 April 2016 on the protection of natural persons with regard to the processing of personal data and on the free movement of such data, and repealing Directive 95/46/EC (General Data Protection Regulation). Official Journal of the European Union. 2016;L119:1-88.
An Q, Song W, Liu J, Tao N, Liu Y, Zhang Q, Xu T, Li S, Liu S, Li Y, et al. Primary drug-resistance pattern and trend in elderly tuberculosis patients in Shandong, China, from 2004 to 2019. Infect Drug Resist. 2020;13:4133–45.
Isman E, Ekeus C, Berggren V. Perceptions and experiences of female genital mutilation after immigration to Sweden: an explorative study. Sex Reprod Healthc. 2013;4(3):93–8.
Isman E, Mahmoud Warsame A, Johansson A, Fried S, Berggren V. Midwives’ experiences in providing care and counselling to women with female genital mutilation (FGM) related problems. Obstet Gynecol Int. 2013;2013:785148.
Guest G, Bunce A, Johnson L. How many interviews are enough?: An experiment with data saturation and variability. Field Methods. 2006;18:59–82.
Article Google Scholar
Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3:77–101.
Green J, Thorogood N. Qualitative methods for health research. 2nd ed. London: Sage; 2009.
Google Scholar
Aragao FBA, Arcencio RA, Fuentealba-Torres M, Carneiro TSG, Souza LLL, Alves YM, Fiorati RC. Impact of social protection programs on adults diagnosed with tuberculosis: systematic review. Rev Bras Enferm. 2021;74(3): e20190906.
Sinha P, Carwile M, Bhargava A, Cintron C, Acuna-Villaorduna C, Lakshminarayan S, Liu AF, Kulatilaka N, Locks L, Hochberg NS. How much do Indians pay for tuberculosis treatment? A cost analysis. Public Health Action. 2020;10(3):110–7.
Xu CH, Jeyashree K, Shewade HD, Xia YY, Wang LX, Liu Y, Zhang H, Wang L. Inequity in catastrophic costs among tuberculosis-affected households in China. Infect Dis Poverty. 2019;8(1):46.
Stracker N, Hanrahan C, Mmolawa L, Nonyane B, Tampi R, Tucker A, West N, Lebina L, Martinson N, Dowdy D. Risk factors for catastrophic costs associated with tuberculosis in rural South Africa. Int J Tuberc Lung Dis. 2019;23(6):756–63.
Yang T, Chen T, Che Y, Chen Q, Bo D. Factors associated with catastrophic total costs due to tuberculosis under a designated hospital service model: a cross-sectional study in China. BMC Public Health. 2020;20(1):1009.
Lu L, Jiang Q, Hong J, Jin X, Gao Q, Bang H, DeRiemer K, Yang C. Catastrophic costs of tuberculosis care in a population with internal migrants in China. BMC Health Serv Res. 2020;20(1):832.
Moreira A, Kritski AL, Carvalho ACC. Social determinants of health and catastrophic costs associated with the diagnosis and treatment of tuberculosis. J Bras Pneumol. 2020;46(5):e20200015.
Hutchison C, Khan MS, Yoong J, Lin X, Coker RJ. Financial barriers and coping strategies: a qualitative study of accessing multidrug-resistant tuberculosis and tuberculosis care in Yunnan, China. BMC Public Health. 2017;17(1):221.
Patel BH, Jeyashree K, Chinnakali P, Vijayageetha M, Mehta KG, Modi B, Chavda PD, Dave PV, Zala CC, Shewade HD, et al. Cash transfer scheme for people with tuberculosis treated by the National TB Programme in Western India: a mixed methods study. BMJ Open. 2019;9(12):e033158.
Rudgard WE, Evans CA, Sweeney S, Wingfield T, Lonnroth K, Barreira D, Boccia D. Comparison of two cash transfer strategies to prevent catastrophic costs for poor tuberculosis-affected households in low- and middle-income countries: An economic modelling study. PLoS Med. 2017;14(11):e1002418.
Verguet S, Riumallo-Herl C, Gomez GB, Menzies NA, Houben R, Sumner T, Lalli M, White RG, Salomon JA, Cohen T, et al. Catastrophic costs potentially averted by tuberculosis control in India and South Africa: a modelling study. Lancet Glob Health. 2017;5(11):e1123–32.
Lu SH, Tian BC, Kang XP, Zhang W, Meng XP, Zhang JB, Lo SK. Public awareness of tuberculosis in China: a national survey of 69 253 subjects. Int J Tuberc Lung Dis. 2009;13(12):1493–9.
PubMed Google Scholar
Deshmukh RD, Dhande DJ, Sachdeva KS, Sreenivas AN, Kumar AMV, Parmar M. Social support a key factor for adherence to multidrug-resistant tuberculosis treatment. Indian J Tuberc. 2018;65(1):41–7.
Zvonareva O, van Bergen W, Kabanets N, Alliluyev A, Filinyuk O. Experiencing syndemic: Disentangling the biosocial complexity of tuberculosis through qualitative research. J Biosoc Sci. 2019;51(3):403–17.
Chen X, Wu R, Xu J, Wang J, Gao M, Chen Y, Pan Y, Ji H, Duan Y, Sun M, et al. Prevalence and associated factors of psychological distress in tuberculosis patients in Northeast China: a cross-sectional study. BMC Infect Dis. 2021;21(1):563.
Lee LY, Tung HH, Chen SC, Fu CH. Perceived stigma and depression in initially diagnosed pulmonary tuberculosis patients. J Clin Nurs. 2017;26(23–24):4813–21.
Qiu L, Tong Y, Lu Z, Gong Y, Yin X. Depressive symptoms mediate the associations of stigma with medication adherence and quality of life in tuberculosis patients in China. Am J Trop Med Hyg. 2019;100(1):31–6.
Chen X, Du L, Wu R, Xu J, Ji H, Zhang Y, Zhu X, Zhou L. Tuberculosis-related stigma and its determinants in Dalian, Northeast China: a cross-sectional study. BMC Public Health. 2021;21(1):6.
Sathar F, Velen K, Peterson M, Charalambous S, Chetty-Makkan CM. “Knock”: a qualitative study exploring the experience of household contacts on home visits and their attitude towards people living with TB in South Africa. BMC Public Health. 2020;20(1):1047.
Rajalakshmi M, Kalaiselvan G, Sudhakar R, Dhikale PT. An exploratory mixed method study on the follow up status and quality of life among recurrent tuberculosis patients in South India. Indian J Tuberc. 2020;67(4):515–22.
Ngamvithayapong J, Winkvist A, Diwan V. High AIDS awareness may cause tuberculosis patient delay: results from an HIV epidemic area. Thailand AIDS. 2000;14(10):1413–9.
Lince-Deroche N, Leuner R, Kgowedi S, Moolla A, Madlala S, Manganye P, Xhosa B, Govathson C, White Ndwanya T, Long L. Voices from the front lines: A qualitative study of integration of HIV, tuberculosis, and primary healthcare services in Johannesburg, South Africa. PLoS ONE. 2020;15(10):e0230849.
Daftary A, Mondal S, Zelnick J, Friedland G, Seepamore B, Boodhram R, Amico KR, Padayatchi N, O’Donnell MR. Dynamic needs and challenges of people with drug-resistant tuberculosis and HIV in South Africa: a qualitative study. Lancet Glob Health. 2021;9(4):e479–88.
Daftary A, Padayatchi N, O’Donnell M. Preferential adherence to antiretroviral therapy over tuberculosis treatment: a qualitative study of drug-resistant TB/HIV co-infected patients in South Africa. Glob Public Health. 2014;9(9):1107–16.
Daniels J, Medina-Marino A, Glockner K, Grew E, Ngcelwane N, Kipp A. Masculinity, resources, and retention in care: South African men’s behaviors and experiences while engaged in TB care and treatment. Soc Sci Med. 2021;270: 113639.
da Silva RD, de Luna FDT, de Araujo AJ, Camelo ELS, Bertolozzi MR, Hino P, Lacerda SNB, Fook SML, de Figueiredo T. Patients’ perception regarding the influence of individual and social vulnerabilities on the adherence to tuberculosis treatment: a qualitative study. BMC Public Health. 2017;17(1):725.
Migliori GB, Thong PM, Akkerman O, Alffenaar JW, Alvarez-Navascues F, Assao-Neino MM, Bernard PV, Biala JS, Blanc FX, Bogorodskaya EM, et al. Worldwide effects of coronavirus disease pandemic on tuberculosis services, January-April 2020. Emerg Infect Dis. 2020;26(11):2709–12.
Santos FLD, Souza LLL, Bruce ATI, Crispim JA, Arroyo LH, Ramos ACV, Berra TZ, Alves YM, Scholze AR, Costa F, et al. Patients’ perceptions regarding multidrug-resistant tuberculosis and barriers to seeking care in a priority city in Brazil during COVID-19 pandemic: A qualitative study. PLoS ONE. 2021;16(4):e0249822.
Sy KTL, Haw NJL, Uy J. Previous and active tuberculosis increases risk of death and prolongs recovery in patients with COVID-19. Infect Dis (Lond). 2020;52(12):902–7.
Maciel ELN, Goncalves Junior E, Dalcolmo MMP. Tuberculosis and coronavirus: what do we know? Epidemiol Serv Saude. 2020;29(2):e2020128.
Singh A, Prasad R, Gupta A, Das K, Gupta N. Severe acute respiratory syndrome coronavirus-2 and pulmonary tuberculosis: convergence can be fatal. Monaldi Arch Chest Dis. 2020;90(3):441–50.
European Pharmaceutical Market Research Association. Code of Conduct 2020. 2020. https://www.ephmra.org/media/4857/ephmra-2020-code-of-conduct-final.pdf . Accessed 8 Feb 2022.
International Chamber of Commerce, European Society for Opinion and Marketing Research. ICC/ESOMAR International Code on Market, Opinion and Social Research and Data Analytics. 2016. https://esomar.org/code-and-guidelines/icc-esomar-code . Accessed 8 February 2022.
British Healthcare Business Intelligence Association. Legal and Ethical Guidelines for Healthcare Market Research: Your essential guide. 2021. https://www.bhbia.org.uk/guidelines-and-legislation/legal-and-ethical-guidelines . Accessed 8 Feb 2022.
Download references
Acknowledgements
Naomi Richardson of Magenta Communications Ltd. in collaboration with Juliet Addo developed the first draft of this article from a research report, provided editorial and graphic services and was funded by GSK. Elizabeth Kehler, Francesca Trewartha and Thea Westwater Smith of Adelphi were co-authors of the original report and co-analysts. Carly Davies, Vera Gielen and Myriam Drysdale from GSK reviewed and provided comments on the screening and interview guides.
This study was funded by GSK Plc.
Author information
Authors and affiliations.
Global Health Catalyst, Global Health R&D, GSK, 980 Great West Road, Brentford, Middlesex, TW8 9GS, United Kingdom
Juliet Addo, Courtney Lundquist & Mike Strange
Product Development and Supply, GSK, Stevenage, United Kingdom
Dave Pearce
Global Medical, GSK, Research Triangle Park, USA
Marilyn Metcalf
Adelphi Research, Bollington, United Kingdom
Gillian Thomas
Global Health Pharma Research Unit, Tres Cantos, Spain
David Barros-Aguirre
Global Health Clinical, Stockley Park West, United Kingdom
Gavin C. K. W. Koh
You can also search for this author in PubMed Google Scholar
Contributions
J.A. made substantial contributions to the conception and design of the work, interpretation of the data and drafting of the manuscript. C.L., M.M., M.S., D.B-A., G.C.K.W.K. and D.P. made substantial contributions to the conception and design of the work and interpretation of the data and critically revised the manuscript for intellectual content. G.T. made significant contributions to the design of the work, the acquisition of data, analysis and interpretation of data for the work and critically revised the manuscript for intellectual content. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Juliet Addo .
Ethics declarations
Ethics approval and consent to participate.
The research was conducted in accordance with the Helsinki Declaration, and all national data protection laws. In compliance with European Union and UK legislation, General Data Protection Regulation guidelines were followed to ensure full patient data confidentiality [ 22 ]. Informed consent was obtained electronically from all individual participants included in the study or their parents/guardians if under the age of consent. Consent was also provided for anonymized consolidated publication of the findings. Participants’ rights and privacy were protected at all times throughout the study. Participants were granted the right to withdraw from the study at any time during the study conduct and to withhold information as they saw fit. All information/data that could identify respondents to third parties was kept strictly confidential; all respondents remained anonymous by using nicknames for the study.
The study complied with international guidance on the conduct of market research, including the European Pharmaceutical Market Research Association (EphMRA) [ 60 ], the European Society for Opinion and Marketing Research (ESOMAR) [ 61 ], and the British Healthcare Business Intelligence Association (BHBIA) [ 62 ], and all other relevant national codes of conduct. Formal ethics approval was waived on the basis that only anonymised data were collected for market research purposes, without treatment intervention, the assessment of clinical endpoints, or the testing of any clinical hypothesis. Specifically, EphMRA defines market research as:
the systematic gathering and interpretation of information about individuals, organisations and marketplaces;
using the information gathering and analytical methods and techniques of the applied social, behavioural and data sciences;
its purpose is to gain insight or support decision making;
the identity of Market Research subjects will not be revealed to the user of the information without explicit consent, Market Research has no interest in the individual identity of Market Research subjects;
no direct action e.g. a sales approach will be taken in relation to individuals or organisations as a result of the Market Research (except following up adverse events when permitted), Market Research is not a commercial communication or a selling opportunity.
Market Research is defined by the objective(s) and the approach, not by the title of the work or those involved in it. Consequently, the EphMRA Code of Conduct includes areas such as digital listening (the use of social media content for Market Research), the use of observational/ethnographic approaches and work carried out online via mobile devices. Section 1.3 of the EphMRA code states that ‘Market Research (as defined above) relating to market or consumer behaviour of the sort that pharmaceutical companies routinely commission, whether involving healthcare professionals, patients, carers or members of the public does not require Clinical Research Ethics Committee or Independent Review Board approval (Institutional Review Board in the USA).’ [ 60 ]. Investigational tools and procedures were reviewed and approved by the GSK Medical Governance Boards in each participating country prior to recruitment to ensure that these were fully compliant with the above conditions and any additional national codes and legislation.
Consent for publication
Consent for publication is not applicable.
Competing interests
The authors declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article. The following authors are employees of GSK (J.A., D.P., M.M., C.L., M.S., and D.B-A.) and hold stocks in GSK. G.C.K.W.K. is a former employee of GSK and holds stocks in the company. The opinions expressed in this article are those of the authors and do not necessarily reflect the views of their employers or organizations. G.T. is an employee of Adelphi Research which received funding from GSK Plc for the conduct of this study.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1..
Consent forms.
Additional file 2.
Screening questions.
Additional file 3.
Health questionnaire and interview guide.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Addo, J., Pearce, D., Metcalf, M. et al. Living with tuberculosis: a qualitative study of patients’ experiences with disease and treatment. BMC Public Health 22 , 1717 (2022). https://doi.org/10.1186/s12889-022-14115-7
Download citation
Received : 19 December 2021
Accepted : 30 August 2022
Published : 10 September 2022
DOI : https://doi.org/10.1186/s12889-022-14115-7
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Treatment failure
BMC Public Health
ISSN: 1471-2458
- Submission enquiries: [email protected]
- General enquiries: [email protected]

A systemic review on tuberculosis
Affiliations.
- 1 Department of Microbiology, Sri Devaraj Urs Medical College, Sri Devaraj Urs Academy of Higher Education and Research, Kolar, India.
- 2 Department of Microbiology, S Nijalingappa Medical College, Bagalkot, India.
- 3 SDM Narayanaya Heart Centre, Sri Dharmasthala Manjunatheshwara Medical College, Sri Dharmasthala Manjunatheshwara University, Dharwad, India. Electronic address: [email protected].
- PMID: 32825856
- DOI: 10.1016/j.ijtb.2020.02.005
Tuberculosis (TB), which is caused by bacteria of the Mycobacterium tuberculosis complex, is one of the oldest diseases known to affect humans and a major cause of death worldwide. Tuberculosis continues to be a huge peril disease against the human population and according to WHO, tuberculosis is a major killer of the human population after HIV/AIDS. Tuberculosis is highly prevalent among the low socioeconomic section of the population and marginalized sections of the community. In India, National strategic plan (2017-2025) has a national goal of elimination of tuberculosis by 2025. It requires increased awareness and understanding of Tuberculosis. In this review article history, taxonomy, epidemiology, histology, immunology, pathogenesis and clinical features of both pulmonary tuberculosis (PTB) and extra-pulmonary tuberculosis (EPTB) has been discussed. A great length of detailed information regarding diagnostic modalities has been explained along with diagnostic algorithm for PTB and EPTB. Treatment regimen for sensitive, drug resistant and extensive drug resistant tuberculosis has been summarized along with newer drugs recommended for multi drug resistant tuberculosis. This review article has been written after extensive literature study in view of better understanding and to increase awareness regarding tuberculosis, as a sincere effort that will help eliminate tuberculosis off the face of the earth in near future.
Keywords: Immunology; Tuberculosis diagnosis; Tuberculosis pathogenesis; Tuberculosis treatment.
Copyright © 2020 Tuberculosis Association of India. Published by Elsevier B.V. All rights reserved.
Publication types
- Historical Article
- Systematic Review
- Culture Techniques
- Extensively Drug-Resistant Tuberculosis
- History, 15th Century
- History, 16th Century
- History, 17th Century
- History, 18th Century
- History, 19th Century
- History, 20th Century
- History, Ancient
- Interferon-gamma Release Tests
- Mycobacterium tuberculosis
- Nucleic Acid Amplification Techniques
- Polymerase Chain Reaction
- Tuberculin Test
- Tuberculosis* / diagnosis
- Tuberculosis* / epidemiology
- Tuberculosis* / history
- Tuberculosis* / immunology
- Tuberculosis, Multidrug-Resistant
- Tuberculosis, Pulmonary* / diagnosis
- Tuberculosis, Pulmonary* / epidemiology
- Tuberculosis, Pulmonary* / history
- Tuberculosis, Pulmonary* / immunology
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
Tuberculosis articles from across Nature Portfolio
Tuberculosis (TB) is an infectious disease caused by strains of bacteria known as mycobacteria. The disease most commonly affects the lungs and can be fatal if not treated. However, most infected individuals show no disease symptoms. One third of the worlds population is thought to have been infected with TB.
Latest Research and Reviews

Age and sex influence antibody profiles associated with tuberculosis progression
Analysis of Mycobacterium tuberculosis -specific antibody responses in previously exposed South African cohorts reveals that profile features associated with progression to active tuberculosis are affected by age and sex.
- Leela R. L. Davies
- Chuangqi Wang
- Sarah M. Fortune
Bacterial diversity dominates variable macrophage responses of tuberculosis patients in Tanzania
- Hellen Hiza
- Michaela Zwyer
- Damien Portevin
Prevalence of pulmonary tuberculosis and HIV infections and risk factors associated to tuberculosis in detained persons in Antananarivo, Madagascar
- Fanjasoa Rakotomanana
- Anou Dreyfus
- Rindra V. Randremanana
The recent rapid expansion of multidrug resistant Ural lineage Mycobacterium tuberculosis in Moldova
Chitwood et al. report on the rapid expansion of a Ural-lineage multidrug resistant strain of Mycobacterium tuberculosis in Moldova. This strain has an estimated reproduction number more than two times greater than otherwise similar drug susceptible strains.
- Melanie H. Chitwood
- Caroline Colijn
- Benjamin Sobkowiak
Genomic insights into anthropozoonotic tuberculosis in captive sun bears ( Helarctos malayanus ) and an Asiatic black bear ( Ursus thibetanus ) in Cambodia
- Kirsty Officer
- Timothy M. Walker
- Bethany Jackson

TOLLIP inhibits lipid accumulation and the integrated stress response in alveolar macrophages to control Mycobacterium tuberculosis infection
Toll-interacting protein (TOLLIP) prevents inflammation and lipid accumulation in alveolar macrophages to limit integrated stress response activation, macrophage necrosis and promote control of Mycobacterium tuberculosis .
- Sambasivan Venkatasubramanian
- Courtney R. Plumlee
- Javeed A. Shah
News and Comment
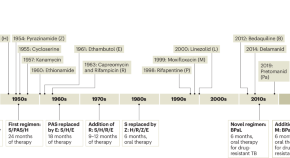
Restocking the tuberculosis drug arsenal
After many lean years, important progress has been made in updating the anti-tuberculosis drug armamentarium; a new drug that targets bacterial protein synthesis is one of several that could help transform the treatment of this neglected and deadly disease.
- Eric L. Nuermberger
- Richard E. Chaisson

Digital intervention improves tuberculosis treatment outcomes
An intervention that incorporates electronic pill boxes and remote adherence monitoring improved treatment success in patients with tuberculosis in Tibet — making this a promising strategy for low-resource settings.
- Karen O’Leary

A spotlight on the tuberculosis epidemic in South Africa
Tuberculosis is the leading cause of death from a single infectious agent, with over 25% of these occurring in the African region. Multi-drug resistant strains which do not respond to first-line antibiotics continue to emerge, putting at risk numerous public health strategies which aim to reduce incidence and mortality. Here, we speak with Professor Valerie Mizrahi, world-leading researcher and former director of the Institute of Infectious Disease and Molecular Medicine at the University of Cape Town, regarding the tuberculosis burden in South Africa. We discuss the challenges faced by researchers, the lessons that need to be learnt and current innovations to better understand the overall response required to accelerate progress.
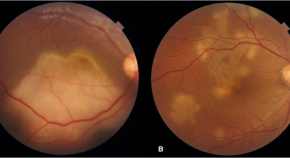
Presumed ocular tuberculosis – need for caution before considering anti-tubercular therapy
- Rohan Chawla
- Urvashi B. Singh
- Pradeep Venkatesh
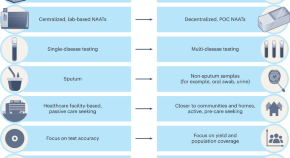
Transforming tuberculosis diagnosis
Diagnosis is the weakest aspect of tuberculosis (TB) care and control. We describe seven critical transitions that can close the massive TB diagnostic gap and enable TB programmes worldwide to recover from the pandemic setbacks.
- Madhukar Pai
- Puneet K. Dewan
- Soumya Swaminathan

B cells and T follicular helper-like cells within lung granulomas are required for TB control
We show a crucial protective function for T follicular helper (T FH )-like cells localized within granuloma-associated lymphoid tissue for Mycobacterium tuberculosis control in mouse models of tuberculosis. Antigen-specific B cells contribute to this strategic localization and the maturation of cytokine-producing T FH -like cells.
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Tuberculosis Epidemiologic Studies Consortium (TBESC)
Study 1: evaluating tests for tb infection, study 2: the latent tb infection care cascade, study 3: closing the gaps in the tb care cascade.
Study Sites
- California Department of Public Health
- Denver Health and Hospital Authority, Colorado
- Duke University, North Carolina and Tennessee
- Emory University, Georgia
- Hawaii Department of Health
- Public Health-Seattle and King County, Washington
- Maricopa County Department of Public Health, Arizona
- Maryland Department of Health and Mental Hygiene
- University of Florida
- University of North Texas Health Science Center
This first TBESC-II study was a head-to-head comparison of the three tests for TB infection in populations at high risk of latent TB infection and/or progression to TB disease.
Sub studies
- Repeatability and reproducibility of two interferon-gamma release assay (IGRA) blood tests– the QuantiFERON ® -TB Gold In-Tube (QFT-GIT), and T-SPOT ® . TB test (T-SPOT)
- Feasibility and cost of testing for prediabetes and diabetes in high-risk persons tested for TB infection
- Cost-effectiveness of TB infection testing in high-risk populations
The second study focused on describing and quantifying the steps in the TB prevention cascade of care within health department clinics. This included better understanding the proportions of patients with latent TB infection who are identified, offered treatment, accept treatment, and complete treatment.
- Developed algorithms to estimate latent TB infection prevalence at any county or state level.
- Developed tools for local TB programs to identify local clinicians who treat underserved populations at high risk, so they can partner with these groups to increase latent TB infection treatment.
- Used insurance billing codes to estimate the extent and magnitude of latent TB infection testing and treatment in commercial and community health sectors.
The third study focused on identifying barriers and facilitators to latent TB infection diagnosis and treatment at community health clinics (CHCs). Researchers collected and analyzed quantitative and qualitative data that can be used to inform development of interventions to improve targeted TB testing and latent TB infection treatment at CHCs.
To receive email updates about this page, enter your email address:
Exit Notification / Disclaimer Policy
- The Centers for Disease Control and Prevention (CDC) cannot attest to the accuracy of a non-federal website.
- Linking to a non-federal website does not constitute an endorsement by CDC or any of its employees of the sponsors or the information and products presented on the website.
- You will be subject to the destination website's privacy policy when you follow the link.
- CDC is not responsible for Section 508 compliance (accessibility) on other federal or private website.
Tuberculosis Research Paper

View sample tuberculosis research paper. Browse research paper examples for more inspiration. If you need a health research paper written according to all the academic standards, you can always turn to our experienced writers for help. This is how your paper can get an A! Feel free to contact our writing service for professional assistance. We offer high-quality assignments for reasonable rates.
Mycobacteria are Gram-positive, nonmotile rods whose species show great microbiological diversity. Many have natural habitats in water and soil. However, some have become intracellular pathogens of higher vertebrates causing disease in animals and humans. Mycobacterium tuberculosis belongs to this group and has been in our midst since antiquity, but our ability to fight the organism is less than 150 years old.
Academic Writing, Editing, Proofreading, And Problem Solving Services
Get 10% off with 24start discount code, charting the disease through history.
A study that determined the frequency of genetic polymorphisms in clinical strains led to the hypothesis that M. tuberculosis originated around 15 000 years ago and that M. bovis was the likely pathogen in humans until 1000 BC (Sreevatsan et al., 1997). After this, widespread M. tuberculosis infection emerged. Early evidence of infection in mankind dates from examinations of the spines of Egyptian mummies and of tomb paintings from 3500 BC, which confirm tuberculosis as a common disease in Egypt at this time (Zink et al., 2003). Around 2000 BC, tuberculosis was established in Europe, but the earliest evidence of the disease in Britain comes from graves dating from approximately 200 BC (Taylor et al., 2005).
There are references in the book of Deuteronomy, thought to have been written in the seventh century BC, to tuberculosis: ‘‘The lord shall smite thee with a consumption, and with a fever, and with an inflammation, and with an extreme burning’’. In the Dark Ages (400–1000 AD), references to tuberculosis are infrequent. As the Roman Empire declined, King Clovis of 5th century France founded the Merovingian dynasty of kings and claimed to heal tuberculosis by the touch of his hand. The King’s evil became the term used for tuberculosis of the lymph glands as English and French monarchs laid hands on scrofulous patients in regular healing services. Queen Elizabeth I, for one, was faithful to this custom. However, the powers of the monarchy were not enough to protect themselves. King Edward VI succeeded to the throne in 1547 as the last in the male line of the house of Tudor. The king’s reign was cut brutally short when he died from tuberculosis at Greenwich in 1553, aged 15 (Holmes and McMorrough, 2001).
Although it has been suggested that colonial Europe brought tuberculosis to the Americas, there is evidence from Peruvian and Chilean mummified tissue a millennium old, that humans inhabiting the Americas had been exposed to mycobacterial disease before the advent of the European ships. Unlike bubonic plague, which in the Middle Ages swept through Europe in short, swift frenzies, tuberculosis burned with a steady, consuming flame. The disease was known as the white plague because of the anemia of chronic disease that rendered sufferers pale. Urbanization across Europe in the sixteenth and seventeenth centuries provided the perfect breeding ground for tuberculosis, as poor populations with bad sanitation gathered in close contact. Tuberculosis was responsible for 20% of deaths in London in the 1600s, as recorded in the Bills of Mortality. Characters in Shakespeare’s Much Ado About Nothing (1600) and Macbeth (1606) were afflicted with consumption. The British heavily colonized Australia in the eighteenth and nineteenth centuries, leading to bitter conflict with the native Aboriginal populations. More devastating than the conflict, however, was the impact of European diseases to which Aboriginal people had no immunity, including tuberculosis. Aboriginal numbers decreased from an estimated 1 000 000 in 1788 to approximately 93 000 in 1901.
The epidemic of tuberculosis in the nineteenth and early twentieth centuries in Europe and the Americas is illustrated in Figure 1 and underscored by the many people who succumbed to the disease, both real and in the arts. The heroine, Mimi, of Puccini’s La Bohe`me suffers from tuberculosis (a theme carried over in the modern film adaptation ‘Moulin Rouge’). Violetta, heroine of Verdi’s La Traviata also dies of the disease. Dickens described tuberculosis in Nicholas Nickleby as a ‘‘disease in which death and life are so strangely blended, that death takes the glow and hue of life.’’ Tuberculosis patients were frequent characters in nineteenth-century Russian literature, and even inspired a character type; the consumptive nihilist, examples of which include Bazarov from Turgenev’s Fathers and Sons, Katerina Ivanovna from Dostoevsky’s Crime and Punishment, Kirillov from Dostoevsky’s Demons, and Ippolit and Marie from Dostoevsky’s The Idiot.
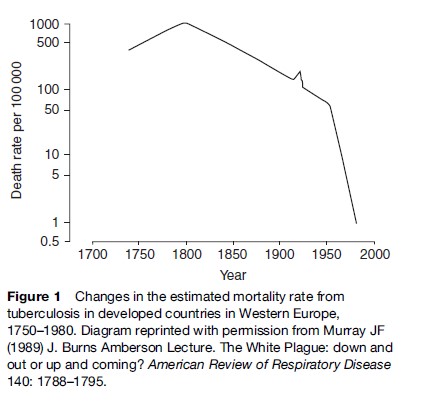
The real death toll was much more profound. Consumption was probably the most common killer of American colonial adults and accounted for more than 25% of deaths in New York City between 1810 and 1815 (Holmberg, 1990). James McGill, the founder of McGill University, reported in his journal the culmination of months of hopeless vigilance ‘‘At 2:00 am on July 4, 1812, my adopted daughter died of decay.’’ John Keats died from tuberculosis at the age of 25 in 1821, as did Frederic Chopin at 39 years in 1849. Tuberculosis killed Emily Bronte in 1848 (Wuthering Heights), Anne Bronte in 1849 (Agnes Grey) and Charlotte Bronte in 1855 (Jane Eyre). Doc Holliday, the American gunfighter and gambler, worked as a dentist until 1872 when tuberculosis forced him to move to the West for its dry climate, where he eventually succumbed to the disease in 1887. Robert Louis Stevenson died at 44 years in 1894 from tuberculosis despite a partial recovery while in Saranac in 1887–88. Franz Kafka, the Austrian Jewish novelist, contracted tuberculosis in 1917 and died in a sanatorium in Kierling, Austria in 1924. Jimmie Rodgers was American country music’s first important recording star but died from tuberculosis in 1933 shortly after writing one of his last songs, ‘TB Blues.’ Mohammed Ali Jinnah, the founding father of Pakistan and its first governor-general, died of tuberculosis in Karachi in 1948. George Orwell died of tuberculosis in January 1950, 1 year after the publication of Nineteen Eighty-Four. Of course, these were the famous; the death toll on the huddled masses was much more far-reaching.
During World War II, increases in tuberculosis were evident in all great cities. In Poland, the rate of tuberculosis tripled and the death rate in Warsaw from tuberculosis in 1944 was 500 per 100 000 people, a sharp increase compared with the background mortality in Western Europe at the time (Figure 1). By April 1945, British Army forces had advanced across Lower Saxony toward Bergen-Belsen. That day, the Germans opened negotiations for the surrender of the concentration camp, stating that the camp had 9000 sick inmates. When the British took the camp on 15 April, the first sights that they encountered were distressing. The appalling conditions of the camp had been a perfect breeding ground for tuberculosis.
Describing The Disease
An early written description of pulmonary tuberculosis was from the last great king of ancient Assyria, Assurbanipal (668–627 BC): ‘‘The patient coughs frequently; his sputum is thick and sometimes contains blood. His breathing is like a flute.’’ Two centuries later, Hippocrates (460–370 BC), in his writings, described phthisis (a Greek word meaning chronic wasting or consumption) as the most prevalent disease of the times, and believed that it killed almost everyone affected. During the reign of the Roman Empire, Claudius Galen (129–216 AD) served as personal physician to Marcus Aurelius and recognized that tuberculosis was contagious.
Advances in the understanding of the disease were few and far between for several centuries thereafter. However, from the origins of the Renaissance came a revolution in the knowledge of disease. In 1546, Girolamo Tracastoro wrote the book De Morbis Contagiosis. Tracastoro wrote that the seeds of contagion remain in such bodies as articles of clothing and bedsheets used by the infected. In the seventeenth century, the anatomical revolution produced knowledge about the body from the study of the dead. In his Opera Medica of 1679, the Dutch physician Dr. Sylvius was the first to identify tubercles in the lungs of consumptive patients. An edict issued by the Italian Republic of Lucca in 1699 states that, ‘‘henceforth, human health should no longer be endangered by objects remaining after the death of a consumptive.’’ In 1720, the English physician Benjamin Marten speculated, in his publication, A New Theory of Consumption, that tuberculosis could be caused by ‘‘wonderfully minute living creatures’’ (Doetsch, 1978). In 1761, Leopold Auenbrugger of Austria, the father of percussion, published a book about the relation of pathological changes and clinical signs of tuberculosis. In 1782, the physicist Graumann presented a treatise where he proved tuberculosis and syphilis were not identical.
Significant research into the causes and cure of tuberculosis began in earnest in the nineteenth century. In 1810, Carmichael, a London physician, declared that the tuberculosis of cattle is transmissible to man through the use of tuberculoid meat or milk. The French physician Gaspard Bayle described the damage caused by tuberculosis in 900 autopsies. Rene´-The´ophile-Hyacinthe Lae¨nnec, most famous for designing the stethoscope, described the evolution of the disease from the initial tubercle through its final stages. Lae¨nnec died of pulmonary tuberculosis in 1826 at the age of 45. Known until then as scrofula or consumption, the name tuberculosis seems first to have been used in 1839 by Johann Schoenlein. The Lancet in 1847 blamed London’s milk supply for the rise in scrofula. In 1865, the French military doctor Jean-Antoine Villemin demonstrated that consumption could be passed from humans to cattle. On the basis of this evidence, he postulated a specific microorganism as the cause.
In 1880, Robert Koch was appointed director of the bacteriological laboratories at the Imperial Health Office in Berlin. In 1882, Koch discovered a staining technique that enabled him to see Mycobacterium tuberculosis under a microscope and showed that bacilli could be isolated in pure cultures and produce tuberculosis in animals that were inoculated. He published his work under the title ‘The Etiology of Tuberculosis,’ in the Berliner Klinische Wochenschrift in which he proved the infectious nature of the disease which ultimately earned him the Nobel Prize in physiology or medicine in 1905 (Kaufmann, 2005). Although meticulously documented, his research met with some opposition; because of its chronic nature, tuberculosis until then was widely believed to be inherited rather than inhaled. However, the description of humanity’s deadliest enemy had now truly begun and a century later, in June 1998, the genome sequence of M. tuberculosis was published (Cole et al., 1998).
Beginning The Fight Against The Disease
Early measures.
While the real fight against the disease began in the nineteenth century, the foresight of Pliny the Elder (28–79 AD), the Roman Senator, cannot be understated. He sent one of his freedmen, who suffered from tuberculosis, on a cruise to Egypt and when the dry air of the desert did not cure the patient, he sent him to a chalet in the Alps. However, his dietary prescription was less conventional: ‘‘For phthisis one had the liver of a wolf in wine, the lard of a thin sow fed on herbs, the flesh of an ass with a bouillon made from it.’’
Eighteen centuries later, Hermann Brehmer, a Silesian botany student suffering from tuberculosis, traveled to the Himalayan Mountains to pursue his botanical studies. He returned home cured and began to study medicine. In 1854, he presented his doctoral dissertation, Tuberculosis is a Curable Disease. In the same year, he built the first sanitorium in Gorbersdorf. In 1883, Dr. Edward Livingston Trudeau, dying from pulmonary tuberculosis, traveled to Saranac Lake in the Adirondack Mountains of New York to spend his final days. He attributed his subsequent recovery to the fresh air of the mountains and in 1885, built the first American sanatorium. By 1930, the United States had 600 sanatoriums with a total of 84 000 beds. For the wealthy, the sanatorium was a combination luxury hotel and hospital, as immortalized in Thomas Mann’s novel The Magic Mountain. The sanatoria provided the first effective step to control tuberculosis by separating those infected from those who were not and providing a healthy diet and climate for those who had the disease.
The Italian Forlanini in 1890 observed that lung collapse tended to have a favorable impact on the outcome of the disease. This is because M. tuberculosis is an obligate aerobe and the absence of oxygen in the collapsed lungs led to its demise. With the introduction of artificial pneumothorax (Figure 2) and other surgical methods to reduce lung volume, the depressing era of helplessness in the face of tuberculosis was over, and active therapy had begun.
In 1886, de Cerenville introduced rib resection to collapse the underlying lung. In 1900, Dr. Edward Archibald, the father of thoracic surgery in North America, had tuberculosis and was treated in the Trudeau Sanatorium at Saranac Lake. In 1912, Archibald was the first surgeon to perform thoracoplasty in North America at Montreal. Thoracoplasty emerged from the array of collapse techniques to become the predominant form of collapse therapy. Furthermore, the discovery of radiation by Von Ro¨ ntgen in 1895 meant the progress and severity of a patient’s disease could now be accurately followed.
By 1890, Koch had published a series of four papers describing a remedy for tuberculosis – a glycerol extract of pure culture of tubercle bacilli – as well as the reaction of animals infected with M. tuberculosis and the differential responses to tuberculin in healthy and diseased persons. Koch noted that the extract ‘‘will enable us to diagnose questionable cases of early consumption even when we fail to detect bacilli’’ (Kaufmann, 2005). Arthur Conan Doyle correctly challenged the therapeutic value of Koch’s lymph, arguing that it might remove traces of the enemy, but it left deadly germs ‘‘deep in the invaded country.’’ Its real value, Conan Doyle asserted, was as ‘‘an admirable aid to diagnosis’’ to determine if a patient was ‘‘in any way tubercular’’. In Paris, French bacteriologists Albert Calmette and Camille Guerin serially passaged M. bovis 230 times from 1908 to 1919 at the Pasteur Institute (Hagwood, 1999). The resulting strain, bacille Calmette-Gue´rin, known commonly as BCG, was found to be avirulent. It was first administered to humans in 1921 and is still applied today with varying efficacy.
Wade Hampton Frost’s epidemiologic studies in the 1930s showed that, even without chemotherapy, the incidence of tuberculosis in the United States was declining steadily (Frost, 1995). In Western countries, deaths from tuberculosis fell from 200 per 100 000 in 1900 to 50 per 100 000 by 1950 (Figure 3).
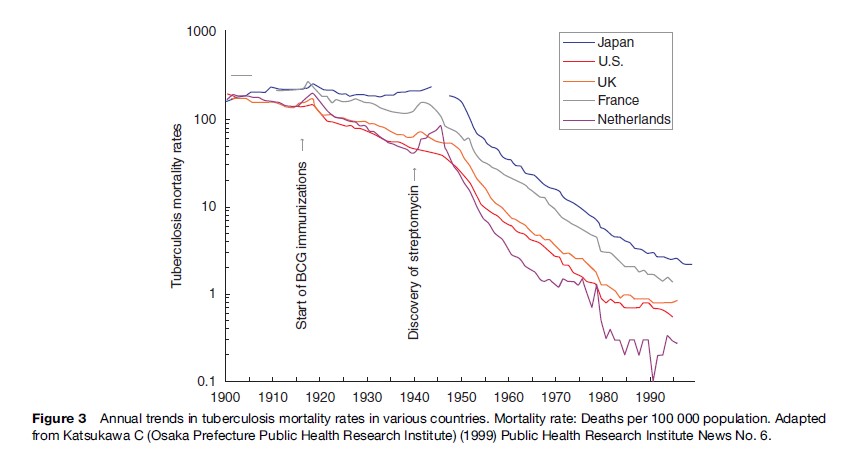
The Antibiotic Era
In 1885, the Italian bacteriologist Cantani had tuberculosis patients inhale cultures of nonpathogenic bacteria, which led to a fall in the quantity of tubercle bacilli in patients’ sputum. In 1939, Selman A. Waksman had discovered the inhibitory effect of certain fungi, especially actinomycetes, on bacterial growth. In 1940, his team at the University of California were able to isolate an effective antituberculous antibiotic, actinomycin; however, this proved to be too toxic for clinical use (Waksman, 1969). In the years that followed, research with actinomycetes, aspergillus, and other microorganisms demonstrated the antituberculous activities of their products. In January 1944, Waksman announced the discovery of a drug called streptomycin isolated from a fungus, Streptomyces lavendula and Patricia, a 21-year-old woman was the first patient to be successfully treated with the drug (Schatz, 1944).
In 1946, Lehmann announced the discovery of paraamino-salicylic (PAS). By 1947, strains of M. tuberculosis had developed resistance to streptomycin. In 1948, the combination of streptomycin and PAS was found to be very effective against M. tuberculosis. In 1952 at Seaview Hospital, New York, a new drug called isoniazid was used to treat tuberculosis patients by Robitzek and Selikoff. Other antituberculous drugs followed with the discovery of pyrazinamide in 1954, cycloserine in 1955, ethambutol in 1962, and rifampicin in 1963. The combination of the early bactericidal activity of isoniazid and the sterilizing activity of rifampicin shortened treatment to less than a year, resulting in short-course chemotherapy. Several studies from Madras and elsewhere demonstrated that treatment was effective when given at home rather than in the sanitorium and that antituberculous drugs were effective when given intermittently rather than daily. The clinical effectiveness of antituberculous drugs led to the closure of the sanatoria in the 1950s and 1960s.
Deaths from tuberculosis in the United States dropped from 188 per 100 000 in 1904 to approximately 1 per 100 000 in 1980. M. tuberculosis was no longer a bacteriological exception. It could be assailed and beaten into retreat.
Tuberculosis Resurgent
From the 1950s to 1985, the Western world saw a rapid decline in the incidence of tuberculosis. For example, 84 304 contracted the disease in 1953 in the United States, falling to 22 201 in 1985. In 1960, Dr. John Crofton at the University of Edinburgh proposed that a combination of streptomycin, PAS, and isoniazid made tuberculosis completely curable and he declared all-out war to conquer the disease. In 1970, William Stewart, the U.S. Surgeon General, is reported to have told the U.S. Congress that the United States was ‘‘ready to close the book on infectious disease.’’ In 1984, the Public Health Service reported that the number of tuberculosis cases reported annually in 1953 had declined by 74% (Huebner and Castro, 1995). In 1987, the Advisory Council for the Elimination of Tuberculosis put forth a plan to eliminate tuberculosis (1 case per 1 million population) by the year 2010 (Anonymous, 1993). These advances contributed to the sense that mankind had prevailed over M. tuberculosis and funding for the fight against tuberculosis was dramatically reduced in Western countries. Humanity had won the war … or had it?
M. tuberculosis was not ready to leave without a fight. Patients recovering rapidly after starting treatment and then defaulting from further treatment as well as inadequate therapy of tuberculosis in counties with poor access to antituberculous drugs led to the development of multidrug resistance. A survey (1961–1968) in the United States that examined drug susceptibility results found 3.5% drug monoresistance and the United States reported the first outbreak of drug-resistant tuberculosis in 1970. In 1985, for the first time in that century, the decline in tuberculosis stagnated and then began a slow, steady increase. Tuberculosis had outsmarted its smartest opponent.
From 1990 to 1992, the Centers for Disease Control in Atlanta investigated outbreaks of multidrug-resistant tuberculosis in eight hospitals in Florida, New York, and New Jersey (Young and Wormser, 1994). Tuberculosis was found to be transmitted not only from patient to patient, but also from patient to health-care worker. The WHO reported that the death rate of patients with multidrug-resistant tuberculosis in the United States was approximately 70%. The typical interval from diagnosis to death was 4–16 weeks and 80% of cases were HIV-positive. HIV and tuberculosis had forged a secret alliance.
The International Union against Tuberculosis and Lung Disease (IUATLD) tested a countrywide system for tuberculosis control by treating tuberculous patients in several poor developing countries. It was proven effective even in difficult settings. As part of this system, it was noted that the emergence of multidrug resistance could be avoided by supervision of drug taking. The World Health Organization (WHO) adopted the strategy and named it DOTS (Directly Observed Therapy, shortcourse) as a framework for global prevention and control of tuberculosis that can be modified according to local needs in its implementation. DOTS was crucial to the restoration of tuberculosis control during the multidrugresistant outbreaks of tuberculosis in North America.
The possibility of an untreatable form of tuberculosis attracted extensive media attention and the funding that had been pulled from tuberculosis management was reinstated in many Western countries. From 1993 to 2003, the incidence of tuberculosis in the United States decreased 44% and is now occurring at a historic low level (14 093 cases in 2005) (Taylor et al., 2005). However, the WHO estimated that in 1995, there were more global deaths from tuberculosis than in any previous year in history. Once again, tuberculosis had adapted to its environment and found new potential for survival in developing countries, where poor health infrastructure and poverty have contributed to a sustained increase in the incidence of tuberculosis.
Currently, the WHO estimates that 2 billion people (one-third of the world’s population) are infected with tuberculosis. There are 2 million deaths annually from tuberculosis and 98% of these are in the developing world. If left unchecked, within 20 years tuberculosis will kill a further 35 million people. In 2003, 8.8 million new cases of tuberculosis arose, with 80% occurring in 22 countries. There are approximately 425 000 new multidrug-resistant cases every year, with the highest rates in the former USSR and China. Tuberculosis has reestablished its position as the leading infectious killer in the world, simply by changing its predominant hunting ground.
Bibliography:
- Anonymous (1993) Tuberculosis control laws – United States, 1993. Recommendations of the Advisory Council for the Elimination of Tuberculosis (ACET). MMWR Recommendations Report 42(RR-15): 1–28.
- Cole ST, Brosch R, Parkhill J, et al. (1998) Deciphering the biology of Mycobacterium tuberculosis from the complete genome sequence. Nature 393(6685): 537–544.
- Doetsch RN (1978) Benjamin Marten and his ‘‘New Theory of Consumptions’’ Microbiology Review 42(3): 521–528.
- Frost WH (1995) The age selection of mortality from tuberculosis in successive decades. 1939. American Journal of Epidemiology 141(1): 4–9.
- Hawgood BJ (1999) Doctor Albert Calmette 1863–1933: Founder of antivenomous serotherapy and of antituberculous BCG vaccination. Toxicon 37(9): 1241–1258.
- Holmberg SD (1990) The rise of tuberculosis in America before 1820. American Review of Respiratory Diseases 142(5): 1228–1232.
- Holmes G, Holmes F, and McMorrough J (2001) The death of young King Edward VI. New England Journal of Medicine 345(1): 60–62.
- Huebner RE and Castro KG (1995) The changing face of tuberculosis. Annual Review of Medicine 46: 47–55.
- Kaufmann SH (2005) Robert Koch, the Nobel Prize, and the ongoing threat of tuberculosis. New England Journal of Medicine 353(23): 2423–2426.
- Murray JF (1989) J. Burns Amberson Lecture. The White Plaque: down and out or up and coming? American Review of Respiratory Disease 140: 1788–1795.
- Schatz A, Bugie E, and Waksman SA (1944) Streptomycin, a substance exhibiting antibiotic activity against gram-positive and gram-negative bacteria. 1944. Clinical Orthopaedics and Related Research 437: 3–6.
- Sreevatsan S, Pan X, Stockbauer KE, et al. (1997) Restricted structural gene polymorphism in the Mycobacterium tuberculosis complex indicates evolutionarily recent global dissemination. Proceedings of the National Academy of Sciences USA 94(18): 9869–9874.
- Taylor GM, Young DB, and Mays SA (2005) Genotypic analysis of the earliest known prehistoric case of tuberculosis in Britain. Journal of Clinical Microbiology 43(5): 2236–2240.
- Taylor Z, Nolan CM, and Blumberg HM (2005) Controlling tuberculosis in the United States. Recommendations from the American Thoracic Society, CDC, and the Infectious Diseases Society of America. MMWR Recommended Report 54(RR-12): 1–81.
- Waksman SA (1969) Successes and failures in the search for antibiotics. Advanced Applied Microbiology 11: 1–16.
- Young LS and Wormser GP (1994) The resurgence of tuberculosis. Scandinavian Journal of Infectious Disease Supplement 193: 9–19.
- Zink AR, Grabner W, Reischl U, Wolf H, and Nerlich AG (2003) Molecular study on human tuberculosis in three geographically distinct and time delineated populations from ancient Egypt. Epidemiology and Infection 130(2): 239–249.
- Barnes D (1995) The Making of a Social Disease. Tuberculosis in Nineteenth-Century France. Berkeley, CA: University of California Press.
- Crofton J, Horne N, and Miller F (1999) Clinical Tuberculosis. 2nd ed. London: Macmillan.
- Davies PDO (2003) Clinical Tuberculosis. 3rd edn. London: Arnold.
- Dormandy T (2000) The White Death: A History of Tuberculosis. New York: New York University Press.
- Enarson DA (1991) Principles of IUATLD collaborative TB programmes. Bulletin of the International Union of Tuberculous and Lung Diseases 66: 195–200.
- Frieden T (ed.) (2004) Toman’s Tuberculosis. Case detections, Treatment and Monitoring – Questions and Answers, 2nd edn. Geneva, Switzerland: World Health Organization.
- Hecker JFC (2003) The Black Death and the Dancing Mania. https://biotech.law.lsu.edu/Books/hecker/Death_c.htm
- Mitchison DA (2005) The diagnosis and therapy of tuberculosis during the past 100 years. American Journal of Respiratory and Critical Care Medicine 171: 699–706.
- Murray JF (2001) A thousand years of pulmonary medicine: good news and bad. The Millennial Lecture. European Respiratory Journal 17: 558–565.
- Murray JF (2004) A century of tuberculosis. American Journal of Respiratory and Critical Care Medicine 169: 1181–1186.
- http://www.stoptb.org/ – Stop TB Partnership.
- https://www.who.int/ – World Health Organization.
ORDER HIGH QUALITY CUSTOM PAPER

An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.

StatPearls [Internet].
Tuberculosis.
Rotimi Adigun ; Rahulkumar Singh .
Affiliations
Last Update: July 11, 2023 .
- Continuing Education Activity
Tuberculosis (TB) is a human disease caused by Mycobacterium tuberculosis. It mainly affects the lungs, making pulmonary disease the most common presentation. Other commonly affected organ systems include the respiratory system, the gastrointestinal (GI) system, the lymphoreticular system, the skin, the central nervous system, the musculoskeletal system, the reproductive system, and the liver. In the past few decades, there has been a concerted global effort to eradicate tuberculosis. Despite the gains in tuberculosis control and the decline in both new cases and mortality, it still accounts for a huge burden of morbidity and mortality worldwide. This activity reviews the evaluation and management of tuberculosis and highlights the role of interprofessional team members in collaborating to provide well-coordinated care and enhance outcomes for affected patients.
- Identify the epidemiology of tuberculosis.
- Review the presentation of a patient with tuberculosis.
- Outline the treatment and management options available for tuberculosis.
- Employ interprofessional team strategies for improving care and outcomes in patients with tuberculosis.
- Introduction
Tuberculosis (TB) is an ancient human disease caused by Mycobacterium tuberculosis which mainly affects the lungs, making pulmonary disease the most common presentation (K Zaman, 2010) [1] . However, TB is a multi-systemic disease with a protean presentation. The organ system most commonly affected includes the respiratory system, the gastrointestinal (GI) system, the lymphoreticular system, the skin, the central nervous system, the musculoskeletal system, the reproductive system, and the liver [2] [3] .
Evidence of TB has been reported in human remains dated thousands of years (Hershkovitz et al., 2017, K Zaman, 2010). For a human pathogen with no known environmental reservoir, Mycobacterium tuberculosis has honed the art of survival and has persisted in human communities from antiquity through modern times.
In the past few decades, there has been a concerted global effort to eradicate TB. These efforts had yielded some positive dividends, especially since 2000 when the World Health Organization (WHO, 2017) estimated that the global incidence rate for tuberculosis has fallen by 1.5% every year. Furthermore, mortality arising from tuberculosis has significantly and steadily declined. The World Health Organization (WHO, 2016) reports a 22% drop in global TB mortality from 2000 through 2015.
Despite the gains in tuberculosis control and the decline in both new cases and mortality, TB still accounts for a huge burden of morbidity and mortality worldwide. The bulk of the global burden of new infection and tuberculosis death is borne by developing countries, with 6 countries, India, Indonesia, China, Nigeria, Pakistan, and South Africa, accounting for 60% of TB death in 2015 (WHO, 2017). [4]
Tuberculosis remains a significant cause of both illness and death in developed countries, especially among individuals with a suppressed immune system [5] [6] . People with HIV are particularly vulnerable to death due to tuberculosis. Tuberculosis accounted for 35% of global mortality in individuals with HIV/AIDS in 2015. (W.H.O, 2017). Children are also vulnerable, and tuberculosis was responsible for one million illnesses in children in 2015, according to the WHO.
M. tuberculosis causes tuberculosis. M. tuberculosis is an alcohol and acid-fast bacillus. It is part of a group of organisms classified as the M. tuberculosis complex. Other members of this group are Mycobacterium africanum, Mycobacterium bovis, and Mycobacterium microti [1] . Most other mycobacteria organisms are classified as non-tuberculous or atypical mycobacterial organisms.
M. tuberculosis is a non-spore-forming, non-motile, obligate-aerobic, facultative, catalase-negative, intracellular bacteria. The organism is neither gram-positive nor gram-negative because of a very poor reaction with the Gram stain. Weakly positive cells can sometimes be demonstrated on Gram stain, a phenomenon known as "ghost cells."
The organism has several unique features compared to other bacteria, such as the presence of several lipids in the cell wall, including mycolic acid, cord factor, and Wax-D. The high lipid content of the cell wall is thought to contribute to the following properties of M. tuberculosis infection:
- Resistance to several antibiotics
- Difficulty staining with Gram stain and several other stains
- Ability to survive under extreme conditions such as extreme acidity or alkalinity, low oxygen situation, and intracellular survival(within the macrophage)
The Ziehl-Neelsen stain is one of the most commonly used stains to diagnose T.B. The sample is initially stained with carbol fuchsin (pink color stain), decolorized with acid-alcohol, and then counter-stained with another stain (usually, blue-colored methylene blue). A positive sample would retain the pink color of the original carbol fuchsin, hence the designation, alcohol, and acid-fast bacillus (AAFB).
- Epidemiology
Geographic Distribution
Tuberculosis is present globally [1] . However, developing countries account for a disproportionate share of tuberculosis disease burden. In addition to the six countries listed above, several countries in Asia, Africa, Eastern Europe, and Latin and Central America continue to have an unacceptably high burden of tuberculosis.
In more advanced countries, high-burden tuberculosis is seen among recent arrivals from tuberculosis-endemic zones, healthcare workers, and HIV-positive individuals. The use of immunosuppressive agents such as long-term corticosteroid therapy has also been associated with an increased risk.
More recently, the use of a monoclonal antibody targeting the inflammatory cytokine, tumor necrotic factor alpha (TNF-alpha), has been associated with an increased risk. Antagonists of this cytokine include several monoclonal antibodies (biologics) used for the treatment of inflammatory disorders. Drugs in this category include infliximab, adalimumab, etanercept, and golimumab. Patients using any of these medications should be monitored for tuberculosis before and during the period of drug treatment.
Other Major Risk Factors
- Socioeconomic factors: Poverty, malnutrition, wars
- Immunosuppression: HIV/AIDS, chronic immunosuppressive therapy (steroids, monoclonal antibodies against tumor necrotic factor), a poorly developed immune system (children, primary immunodeficiency disorders)
- Occupational: Mining, construction workers, pneumoconiosis (silicosis)
Multi-Drug Resistant Tuberculosis (MDR-TB) and Extremely Multi-Drug Resistant Tuberculosis (XDR-TB)
- This refers to tuberculosis with strains of Mycobacterium which have developed resistance to the classic anti-tuberculosis medications. TB is especially a problem among patients with HIV/AIDS. Resistance to multiple anti-tuberculosis medications, including at least the two standard anti-tuberculous medications, Rifampicin or Isoniazid, is required to make a diagnosis of MDR-TB.
- Seventy-five percent of MDR-TB is considered primary MDR-TB, caused by infection with MDR-TB pathogens. The remaining 25% are acquired and occur when a patient develops resistance to treatment for tuberculosis. Inappropriate treatment for tuberculosis because of several factors such as antibiotic abuse; inadequate dosage; incomplete treatment, is the number one cause of acquired MDR-TB.
- This is a more severe type of MDR-TB. Diagnosis requires resistance to at least four anti-tuberculous medications, including resistance to Rifampicin, Isoniazid, and resistance to any two of the newer anti-tuberculous medications. The newer medications implicated in XDR-TB are the fluoroquinolones (Levofloxacin and moxifloxacin) and the injectable second-line aminoglycosides, Kanamycin, Capreomycin, and amikacin.
- The mechanism of developing XDR-TB is similar to the mechanism for developing MDR-TB.
- XDR -TB is an uncommon occurrence.
- Pathophysiology
Although usually a lung infection, tuberculosis is a multi-system disease with protean manifestation. The principal mode of spread is through the inhalation of infected aerosolized droplets.
The body's ability to effectively limit or eliminate the infective inoculum is determined by the immune status of the individual, genetic factors, and whether it is a primary or secondary exposure to the organism. Additionally, M. tuberculosis possesses several virulence factors that make it difficult for alveolar macrophages to eliminate the organism from an infected individual. The virulence factors include the high mycolic acid content of the bacteria's outer capsule, which makes phagocytosis to be more difficult for alveolar macrophages. Furthermore, some of the other constituents of the cell wall, such as the cord factor, may directly damage alveolar macrophages. Several studies have shown that mycobacteria tuberculosis prevents the formation of an effective phagolysosome, hence, preventing or limiting the elimination of the organisms.
The first contact of the Mycobacterium organism with a host leads to manifestations known as primary tuberculosis. This primary TB is usually localized to the middle portion of the lungs, and this is known as the Ghon focus of primary TB. In most infected individuals, the Ghon focus enters a state of latency. This state is known as latent tuberculosis.
Latent tuberculosis is capable of being reactivated after immunosuppression in the host. A small proportion of people would develop an active disease following first exposure. Such cases are referred to as primary progressive tuberculosis. Primary progressive tuberculosis is seen in children, malnourished people, people with immunosuppression, and individuals on long-term steroid use.
Most people who develop tuberculosis do so after a long period of latency (usually several years after the initial primary infection). This is known as secondary tuberculosis. Secondary tuberculosis usually occurs because of the reactivation of latent tuberculosis infection. The lesions of secondary tuberculosis are in the lung apices. A smaller proportion of people who develop secondary tuberculosis do so after getting infected a second time (re-infection).
The lesions of secondary tuberculosis are similar for both reactivation and reinfection in terms of location (at the lung apices), and the presence of cavitation enables a distinction from primary progressive tuberculosis which tends to be in the middle lung zones and lacks marked tissue damage or cavitation.
Type-IV Hypersensitivity and Caseating Granuloma
Tuberculosis is a classic example of a cell-mediated delayed type IV hypersensitivity reaction.
Delayed Hypersensitivity Reaction: By stimulating the immune cells (the helper T-Lymphocyte, CD4+ cells), Mycobacterium tuberculosis induces the recruitment and activation of tissue macrophages. This process is enhanced and sustained by the production of cytokines, especially interferon-gamma.
Two main changes involving macrophages occur during this process, namely, the formation of multinucleated giant cells and the formation of epithelioid cells. Giant cells are aggregates of macrophages that are fused together and function to optimize phagocytosis. The aggregation of giant cells surrounding the Mycobacterium particle and the surrounding lymphocytes and other cells is known as a granuloma.
Epithelioid cells are macrophages that have undergone a change in shape and have developed the ability for cytokine synthesis. Epithelioid cells are modified macrophages and have a flattened (spindle-like shape) as opposed to the globular shape characteristic of normal macrophages. Epithelioid cells often coalesce together to form giant cells in a tuberculoid granuloma.
In addition to interferon-gamma (IFN-gamma), the following cytokines play important roles in the formation of a tuberculosis granuloma, Interleukin-4 (IL-4), Interleukin-6 (IL-6), and tumor necrotic factor-alpha (TNF-alpha).
The appearance of the granuloma in tuberculosis has been described as caseous or cheese-like on gross examination. This is principally explained by the rich mycolic acid content of the mycobacterium cell wall. Because of this unique quality, the term caseous or caseating necrosis has been used to describe granulomatous necrosis caused by mycobacteria tuberculosis.
Histologically, caseous necrosis would present as a central area of uniform eosinophilia on routine hematoxylin and eosin stain.
- Histopathology
The granuloma is the diagnostic histopathological hallmark of tuberculosis.
The defining features of the granuloma of tuberculosis are:
- Caseation or caseous necrosis is demonstrable as a region of central eosinophilia.
- Multinucleated giant cells
- History and Physical
A chronic cough, hemoptysis, weight loss, low-grade fever, and night sweats are some of the most common physical findings in pulmonary tuberculosis.
Secondary tuberculosis differs in clinical presentation from primary progressive disease. In secondary disease, the tissue reaction and hypersensitivity are more severe, and patients usually form cavities in the upper portion of the lungs.
Pulmonary or systemic dissemination of the tubercles may be seen in active disease, and this may manifest as miliary tuberculosis characterized by millet-shaped lesions on chest x-ray. Disseminated tuberculosis may also be seen in the spine, the central nervous system, or the bowel.
Screening Tests
Tuberculin skin testing: Mantoux test (skin testing with PP D)
The Mantoux reaction following the injection of a dose of PPD (purified protein derivative) is the traditional screening test for exposure to Tuberculosis. The result is interpreted taking into consideration the patient's overall risk of exposure. Patients are classified into 3 groups based on the risk of exposure with three corresponding cut-off points. The 3 major groups used are discussed below.
Low Risk
- Individuals with minimal probability of exposure are considered to have a positive Mantoux test only if there is very significant induration following intradermal injection of PPD. The cut-off point for this group of people (with minimal risk of exposure) is taken to be 15 mm.
Intermediate Risk
- Individuals with intermediate probability are considered positive if the induration is greater than 10 mm.
- Individuals with a high risk of a probability of exposure are considered positive if the induration is greater than 5 mm.
Examples of Patients in the Different Risk Categories
- Low Risk/Low Probability: Patients with no known risk of exposure to TB. Example: No history of travel, military service, HIV-negative, no contact with a chronic cough patient, no occupational exposure, no history of steroids. Not a resident of a TB-endemic region.
- Intermediate Risk/Probability: Residents of TB-endemic countries (Latin America, Sub -Sahara Africa, Asia), workers or residents of shelters, Medical or microbiology department personnel.
- High Risk/Probability: HIV-positive patient, a patient with evidence of the previous TB such as the healed scar on an x-ray), contact with chronic cough patients.
Note that a Mantoux test indicates exposure or latent tuberculosis. However, this test lacks specificity, and patients would require subsequent visits for interpreting the results as well as chest x-ray for confirmation. Although relatively sensitive, the Mantoux reaction is not very specific and may give false-positive reactions in individuals who have been exposed to the BCG vaccine.
Interferon release assays (IGRA, Quantiferon Assays)
This is a tuberculosis screening test that is more specific and equally as sensitive as the Mantoux test. This test assays for the level of the inflammatory cytokine, especially interferon-gamma.
The advantages of antigen-specific stimulation of IFN-γ release, especially in those with prior vaccination with BCG vaccine, include the test requires a single blood draw, obviating the need for repeat visits to interpret results. Furthermore, additional investigations, such as HIV screening, could be performed (after patient consent) on the same blood draw.
Quantiferon's disadvantages include cost and the technical expertise required to perform the test.
Screening in Immunocompromised Patients
Immunocompromised patients may show lower levels of reaction to PPD or false-negative Mantoux because of cutaneous anergy.
A high level of suspicion should be entertained when reviewing negative screening tests for tuberculosis in HIV-positive individuals.
The Significance of Screening
A positive screening test indicates exposure to tuberculosis and a high chance of developing active tuberculosis in the future. Tuberculosis incidence in patients with positive Mantoux test averages between 2% to 10% without treatment.
Patients with a positive test should have a chest x-ray as a minimum diagnostic test. In some cases, these patients should have additional tests. Patients meeting the criteria for latent tuberculosis should receive prophylaxis with isoniazid.
Screening Questionnaires for Resource-Poo r Settings
Several screening questionnaires have been validated to enable healthcare workers working in remote and resource-poor environments to screen for tuberculosis.
These questionnaires make use of an algorithm that combines several clinical signs and symptoms of tuberculosis. Some of the commonly used symptoms are:
- Chronic cough
- Weight loss
- Fever and night sweats
- History of contact
- Blood in sputum
Several studies have confirmed the utility of using several criteria rather than a focus on only chronic cough or weight loss.
Confirmatory and Diagnostic Tests
- A chest x-ray is indicated to rule out or rule in the presence of active disease in all screening test-positive cases.
- Acid Fast Staining-Ziehl-Neelsen
- Nuclear Amplification and Gene-Based Tests: These represent a new generation of diagnostic tools for tuberculosis. These tests enable the identification of bacteria or bacteria particles by making use of DNA-based molecular techniques.
The new molecular-based techniques are faster and enable rapid diagnosis with high precision. Confirmation of TB could be made in hours rather than the days or weeks it takes to wait for a standard culture. This is very important, especially among immunocompromised hosts where there is a high rate of false-negative results. Some molecular-based tests also allow for the identification of multidrug-resistant tuberculosis.
- Treatment / Management
Latent Tuberculosis
2020 LTBI treatment guidelines include the NTCA- and CDC-recommended treatment regimens that comprise three preferred rifamycin-based regimens and two alternative monotherapy regimens with daily isoniazid. These are only recommended for persons infected with Mycobacterium tuberculosis that is presumed to be susceptible to isoniazid or rifampin. A regimen of 3 months of once-weekly isoniazid plus rifapentine is a preferred regimen that is strongly recommended for children aged more than 2 years and adults. Another option is 4 months of daily rifampin for HIV-negative adults and children of all ages. Three months of daily isoniazid plus rifampin is a preferred treatment that is conditionally recommended for adults and children of all ages and for patients with HIV. Regimens of 6 or 9 months of daily isoniazid are alternative recommended regimens.
Treatment of Active Infection
Treatment of confirmed TB requires a combination of drugs. Combination therapy is always indicated, and monotherapy should never be used for tuberculosis. The most common regimen for TB includes the following anti-TB medications:
First-Line Medications, Group 1
- Isoniazid - Adults (maximum): 5 mg/kg (300 mg) daily; 15 mg/kg (900 mg) once, twice, or three times weekly.Children (maximum): 10-15 mg/kg (300 mg) daily; 20--30 mg/kg (900 mg) twice weekly (3).Preparations. Tablets (50 mg, 100 mg, 300 mg); syrup (50 mg/5 ml); aqueous solution (100 mg/ml) for IV or IM injection.
- Rifampicin - Adults (maximum): 10 mg/kg (600 mg) once daily, twice weekly, or three times weekly.Children (maximum): 10-20 mg/kg (600 mg) once daily or twice weekly.Preparations. Capsules (150 mg, 300 mg)
- Rifabutin- Adults (maximum): 5 mg/kg (300 mg) daily, twice, or three times weekly. When rifabutin is used with efavirenz the dose of rifabutin should be increased to 450--600 mg either daily or intermittently.Children (maximum): Appropriate dosing for children is unknown. Preparations: Capsules (150 mg) for oral administration.
- RIfapentine - Adults (maximum): 10 mg/kg (600 mg), once weekly (continuation phase of treatment)Children: The drug is not approved for use in children.Preparation. Tablet (150 mg, film-coated).
- Pyrazinamide - Adults: 20-25 mg/kg per day. Children (maximum): 15-30 mg/kg (2.0 g) daily; 50 mg/kg twice weekly (2.0 g).Preparations. Tablets (500 mg).
- Ethambutol - Adults: 15-20 mg/kg per day: Children (maximum): 15-20 mg/kg per day (2.5 g); 50 mg/kg twice weekly (2.5 g). The drug can be used safely in older children but should be used with caution in children in whom visual acuity cannot be monitored (generally less than 5 years of age) (66). In younger children, EMB can be used if there is a concern with resistance to INH or RIF.Preparations. Tablets (100 mg, 400 mg) for oral administration.
Isoniazid and Rifampicin follow a 4-drug regimen (usually including Isoniazid, Rifampicin, Ethambutol, and Pyrazinamide) for 2 months or six months. Vitamin B6 is always given with Isoniazid to prevent neural damage (neuropathies).
Several other antimicrobials are effective against tuberculosis, including the following categories:
Second-Line Anti-tuberculosis Drugs, Group 2
Injectable aminoglycosides and injectable polypeptides
Injectable aminoglycosides
- Streptomycin
Injectable polypeptides
- Capreomycin
- Viomycin
Second - Line Anti-Tuberculosis Drugs, Group 3, Oral and Injectable Fluoroquinolones
Fluoroquinolones
- Levofloxacin
- Moxifloxacin
- Gatifloxacin
Second-Line Anti-tuberculosis Drugs, Group 4
- Para-aminosalicylic acid
- Cycloserine
- Ethionamide
- Prothionamide
- Thioacetazone
Third- Line Anti-Tuberculosis Drugs, Group 5
These are medications with variable but unproven efficacy against TB. They are used for total drug-resistant TB as drugs of last resort.
- Clofazimine
- Amoxicillin/clavulanic acid
- Imipenem/cilastatin
- Clarithromycin
MDR-TB, XDR-TB
Multi-drug-resistant TB is becoming increasingly common.
The combination of first-line and second-line medications is used at high doses to treat this condition.
Bedaquiline
On December 28, 2012, the United States Food and Drug Administration Agency (FDA) approved Bedaquiline as a drug for treating MDR-TB. This is the first FDA approval for an anti-TB medication in 40 years. While showing remarkable promise in drug-resistant tuberculosis, cost remains a big obstacle to delivering this drug to the people most affected by MDR-TB.
Clinical and Laboratory Monitoring
Liver function tests are required for all patients taking isoniazid. Other monitoring in TB includes monitoring for retinopathies for patients on ethambutol.
Treatment of Patients with HIV
In patients with active TB and HIV with severe immunosuppression (CD4+ 60/microliter), the recommendations are to immediately start antituberculous therapy, followed by the initiation of anti-retroviral after 2 to 4 weeks. Delaying treatment with antiretroviral drugs prevents the development of immune reconstitution inflammatory syndrome (IRIS). This is a syndrome characterized by paradoxical worsening of symptoms of primary disease when treatment with antiretroviral agents is initiated. The presenting infection should be treated immediately, and retroviral should start no earlier than 2 weeks. The earlier the antiretroviral agents are initiated, the greater the likelihood of IRIS. Unnecessary delay of antiretroviral therapy leads to an increased risk of death from AIDS.
- Differential Diagnosis
Tuberculosis is a great mimic and should be considered in the differential diagnosis of several systemic disorders. The following is a non-exhaustive list of conditions to be strongly considered when evaluating the possibility of pulmonary tuberculosis.
- Non-tuberculous mycobacterium
- Fungal infection
- Histoplasmosis
- Sarcoidosis
- Toxicity and Adverse Effect Management
Side Effect associated with most commonly used anti-TB drugs [7]
1) Isoniazid- Asymptomatic elevation of aminotransferases (10-20%), clinical hepatitis (0.6%), peripheral neurotoxicity, hypersensitivity. [8]
2) Rifampin- Pruritis, nausea & vomiting, flulike symptoms, hepatotoxicity, orange discoloration of bodily fluid.
3) Rifabutin- Neutropenia, uveitis (0.01%), polyarthralgias, hepatotoxicity (1%))
4) Rifapentine- Similar to rifampin
5) Pyrazinamide- Hepatotoxicity (1%), nausea & vomiting, polyarthralgias (40%), acute gouty arthritis, rash, and photosensitive dermatitis
6) Ethambutol- Retrobulbar neuritis (18%)
One of the most important aspects of tuberculosis treatment is close follow-up and monitoring for these side effects. Most of these side effects can be managed by either close monitoring or adjusting the dose. In some cases, the medication needs to be discontinued, and second-line therapy should be considered if other alternatives are not available.
The majority of patients with a diagnosis of TB have a good outcome. This is mainly because of effective treatment. Without treatment mortality rate for tuberculosis is more than 50%.
The following group of patients is more susceptible to worse outcomes or death following TB infection:
- Extremes of age, elderly, infants, and young children
- Delay in receiving treatment
- Radiologic evidence of extensive spread.
- Severe respiratory compromise requiring mechanical ventilation
- Immunosuppression
- Multidrug resistance (MDR) tuberculosis
- Complications
Most patients have a relatively benign course. Complications are more frequently seen in patients with the risk factors mentioned above. Some of the complications associated with tuberculosis are:
- Extensive lung destruction
- Damage to cervical sympathetic ganglia leading to Horner's syndrome.
- Acute respiratory distress syndrome
- Milliary spread (disseminated tuberculosis), including TB meningitis.
- Pneumothorax
- Systemic amyloidosis
- Pearls and Other Issues
Tuberculosis is a preventable and treatable infectious disease. Having said that, it is still one of the major contributors to morbidity and mortality in developing countries where we are still struggling to provide adequate access to care. Other challenges include lack of awareness, delayed diagnosis, poor accessibility to medication and vaccination as well as medication adherence. DOTS (Direct Observed Therapy), proposed by WHO, has been very effective in recent years to improve adherence to treatment in tuberculosis patients. [9] [10] Also, vaccination drive in developing countries has played a bigger role in decreasing the prevalence of this infection. The preventive effect of BCG vaccination is controversial, but many studies have identified vaccination as a very important tool in the fight against tuberculosis, and we need to keep our focus on childhood vaccination, especially in developing countries. [11] WHO and other health organizations have to continue their investment in developing strategies and research until we eradicate this disease from the world map. New antituberculosis drugs need to be developed to shorten or otherwise simplify the treatment of tuberculosis caused by drug-susceptible organisms, to improve the treatment of drug-resistant tuberculosis, and to provide more efficient and effective treatment of latent tuberculosis infection.
- Enhancing Healthcare Team Outcomes
A team approach involving nurses, clinicians, and technicians will lead to the best outcomes in treating patients with tuberculosis. [Level 5]
- Review Questions
- Access free multiple choice questions on this topic.
- Comment on this article.
Granuloma of Tuberculosis. Arrows pointed at multi-nucleated giant cells. Contributed By Dr. Rotimi Adigun (with permission from Kingston General Hospital)
Disclosure: Rotimi Adigun declares no relevant financial relationships with ineligible companies.
Disclosure: Rahulkumar Singh declares no relevant financial relationships with ineligible companies.
This book is distributed under the terms of the Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International (CC BY-NC-ND 4.0) ( http://creativecommons.org/licenses/by-nc-nd/4.0/ ), which permits others to distribute the work, provided that the article is not altered or used commercially. You are not required to obtain permission to distribute this article, provided that you credit the author and journal.
- Cite this Page Adigun R, Singh R. Tuberculosis. [Updated 2023 Jul 11]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.
In this Page
Bulk download.
- Bulk download StatPearls data from FTP
Related information
- PMC PubMed Central citations
- PubMed Links to PubMed
Similar articles in PubMed
- Review Tuberculosis. [Major Infectious Diseases. 2017] Review Tuberculosis. Bloom BR, Atun R, Cohen T, Dye C, Fraser H, Gomez GB, Knight G, Murray M, Nardell E, Rubin E, et al. Major Infectious Diseases. 2017 Nov 3
- Active Tuberculosis. [StatPearls. 2024] Active Tuberculosis. Jilani TN, Avula A, Zafar Gondal A, Siddiqui AH. StatPearls. 2024 Jan
- Review The global tuberculosis epidemic and progress in care, prevention, and research: an overview in year 3 of the End TB era. [Lancet Respir Med. 2018] Review The global tuberculosis epidemic and progress in care, prevention, and research: an overview in year 3 of the End TB era. Floyd K, Glaziou P, Zumla A, Raviglione M. Lancet Respir Med. 2018 Apr; 6(4):299-314.
- Fighting the tuberculosis epidemic in the Western Pacific region: current situation and challenges ahead. [Kekkaku. 2010] Fighting the tuberculosis epidemic in the Western Pacific region: current situation and challenges ahead. van Maaren PJ. Kekkaku. 2010 Jan; 85(1):9-16.
- Consensus statement. Global burden of tuberculosis: estimated incidence, prevalence, and mortality by country. WHO Global Surveillance and Monitoring Project. [JAMA. 1999] Consensus statement. Global burden of tuberculosis: estimated incidence, prevalence, and mortality by country. WHO Global Surveillance and Monitoring Project. Dye C, Scheele S, Dolin P, Pathania V, Raviglione MC. JAMA. 1999 Aug 18; 282(7):677-86.
Recent Activity
- Tuberculosis - StatPearls Tuberculosis - StatPearls
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
Connect with NLM
National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894
Web Policies FOIA HHS Vulnerability Disclosure
Help Accessibility Careers

IMAGES
VIDEO
COMMENTS
Abstract. Tuberculosis (TB) remains one of the deadliest infectious diseases responsible for millions of deaths annually across the world. In this paper we present a general overview of TB ...
Introduction. Tuberculosis (TB) continues to pose a major threat to global health , and research is a key component of the Global Plan to Stop TB2011-2015 .Research is particularly critical for developing new tools and approaches needed for eliminating TB by 2050 .Recognizing this, the Stop TB Partnership and the World Health Organization's (WHO) Stop TB Department have launched the TB ...
Abstract. Tuberculosis (TB) is one of the most ancient diseases of mankind, with molecular evidence going back to over 17,000 years. In spite of newer modalities for diagnosis and treatment of TB, unfortunately, people are still suffering, and worldwide it is among the top 10 killer infectious diseases, second only to HIV.
Introduction. Tuberculosis (TB) represents a major global health threat that, despite being preventable and treatable, is the 13th leading cause of death worldwide and the second leading infectious killer after coronavirus disease 2019 (COVID-19) [1, 2].In the past decades, the TB burden has been slowly decreasing; however, with the emergence of COVID-19 and the current political conflicts ...
Science 313, 1632-1636 (2006). Munoz-Elias, E.J. & McKinney, J.D. Mycobacterium tuberculosis isocitrate lyases 1 and 2 are jointly required for in vivo growth and virulence. Nat. Med. 11, 638 ...
Abstract. Tuberculosis (TB), an old disease caused by the bacteria Mycobacterium tuberculosis is still responsible for more deaths worldwide each year than any other infectious disease, including ...
Abstract and Figures. Tuberculosis Is a major bluster to humanity resist to progress in health-care systems and the widespread weapon of TB control programs. The World Health Organization (WHO ...
Background Although tuberculosis (TB) is a curable disease, treatment is complex and prolonged, requiring considerable commitment from patients. This study aimed to understand the common perspectives of TB patients across Brazil, Russia, India, China, and South Africa throughout their disease journey, including the emotional, psychological, and practical challenges that patients and their ...
Tuberculosis (TB) research and innovation is essential to achieve the global TB targets of the United Nations (UN) Sustainable Development Goals (SDGs) and the World Health Organization (WHO) End TB Strategy. The SDG target is to "end the epidemic" by 2030; more specific targets for 2030 set in the End TB Strategy are a 90% reduction in TB ...
29 Mar 2023. 19 Nov 2022. 08 Nov 2022. Tuberculosis Research and Treatment publishes original research articles and review articles related to all aspects of tuberculosis, from the immunological basis of disease to translational and clinical research.
Tuberculosis is highly prevalent among the low socioeconomic section of the population and marginalized sections of the community. In India, National strategic plan (2017-2025) has a national goal of elimination of tuberculosis by 2025. It requires increased awareness and understanding of Tuberculosis. In this review article history, taxonomy ...
Tuberculosis (TB) is an airborne disease caused by Mycobacterium tuberculosis (MTB) that usually affects the lungs leading to severe coughing, fever, and chest pains. Although current research in the past four years has provided valuable insight into TB transmission, diagnosis, and treatment, much remains to be discovered to effectively decrease the incidence of and eventually eradicate TB.
Cegielski JP, Chan PC, Lan Z, Udwadia ZF, Viiklepp P, Yim JJ, Menzies D. Aminoglycosides and Capreomycin in the Treatment of Multidrug-resistant Tuberculosis: Individual Patient Data Meta-analysis of 12 030 Patients From 25 Countries, 2009-2016. Clin Infect Dis. 2020 Oct 30:ciaa621. doi: 10.1093/cid/ciaa621.
1. Introduction. Tuberculosis (TB) is a leading global public health problem, with high morbidity and mortality in humans. Until the COVID-19 pandemic, TB was still the leading cause of death from a single infectious agent, ranking above HIV/acquired immune deficiency syndrome [].The number of people newly diagnosed with TB fell from 7.1 million in 2019 to 5.8 million in 2020, and reduced ...
Tuberculosis is the leading cause of death from a single infectious agent, with over 25% of these occurring in the African region. Multi-drug resistant strains which do not respond to first-line ...
High-quality research evidence is critical for improving global health and health equity, and for achieving the World Health Organization (WHO)'s objective of the attainment of the highest possible level of health by all peoples [1]. This need is most apparent when responding to complex epidemics such as tuberculosis (TB). TB is the leading killer among diseases caused by an infectious agent ...
This first TBESC-II study was a head-to-head comparison of the three tests for TB infection in populations at high risk of latent TB infection and/or progression to TB disease. Sub studies. Repeatability and reproducibility of two interferon-gamma release assay (IGRA) blood tests- the QuantiFERON ® -TB Gold In-Tube (QFT-GIT), and T-SPOT ®.
Tuberculosis research. Tuberculosis is the leading cause of death from a single infectious agent and remains a global health emergency. In 2018 alone, there were 1.5 million deaths and 10 million new cases globally, among whom half a million had rifampicin resistant TB.
1. Introduction. Tuberculosis (TB) is still a major global health problem as the global incidence in 2018 was estimated to be 10.0 millions, and the mortality 1.2 millions .The World Health Organization (WHO) and the United Nations' Millennium Development Goals (MDG) together with the Stop TB Strategy have developed strategies for eliminating TB, which have led to a decline in absolute ...
Tuberculosis was reported to be curable by 74.6% of the subjects and 67.9% knew that there are medications for treatment of tuberculosis, while 11.5% knew the duration of treatment. Conclusion.
View sample tuberculosis research paper. Browse research paper examples for more inspiration. If you need a health research paper written according to all the academic standards, you can always turn to our experienced writers for help. This is how your paper can get an A! Feel free to contact our writing service for professional assistance.
This paper aims to illustrate the use and effectiveness of real-time operational research. Specific objectives are to: (i) focus on tuberculosis (TB) and show how four real-time operational research studies were conducted in Africa and Asia, with the findings leading to important changes in policy and practice; and (ii) consider and discuss how ...
Tuberculosis (TB) is an ancient human disease caused by Mycobacterium tuberculosis which mainly affects the lungs, making pulmonary disease the most common presentation (K Zaman, 2010) [1]. However, TB is a multi-systemic disease with a protean presentation. The organ system most commonly affected includes the respiratory system, the gastrointestinal (GI) system, the lymphoreticular system ...