- - Google Chrome
Intended for healthcare professionals
- Access provided by Google Indexer
- My email alerts
- BMA member login
- Username * Password * Forgot your log in details? Need to activate BMA Member Log In Log in via OpenAthens Log in via your institution


Search form
- Advanced search
- Search responses
- Search blogs
- Quality improvement...
Quality improvement into practice
Read the full collection.
- Related content
- Peer review
- Adam Backhouse , quality improvement programme lead 1 ,
- Fatai Ogunlayi , public health specialty registrar 2
- 1 North London Partners in Health and Care, Islington CCG, London N1 1TH, UK
- 2 Institute of Applied Health Research, Public Health, University of Birmingham, B15 2TT, UK
- Correspondence to: A Backhouse adam.backhouse{at}nhs.net
What you need to know
Thinking of quality improvement (QI) as a principle-based approach to change provides greater clarity about ( a ) the contribution QI offers to staff and patients, ( b ) how to differentiate it from other approaches, ( c ) the benefits of using QI together with other change approaches
QI is not a silver bullet for all changes required in healthcare: it has great potential to be used together with other change approaches, either concurrently (using audit to inform iterative tests of change) or consecutively (using QI to adapt published research to local context)
As QI becomes established, opportunities for these collaborations will grow, to the benefit of patients.
The benefits to front line clinicians of participating in quality improvement (QI) activity are promoted in many health systems. QI can represent a valuable opportunity for individuals to be involved in leading and delivering change, from improving individual patient care to transforming services across complex health and care systems. 1
However, it is not clear that this promotion of QI has created greater understanding of QI or widespread adoption. QI largely remains an activity undertaken by experts and early adopters, often in isolation from their peers. 2 There is a danger of a widening gap between this group and the majority of healthcare professionals.
This article will make it easier for those new to QI to understand what it is, where it fits with other approaches to improving care (such as audit or research), when best to use a QI approach, making it easier to understand the relevance and usefulness of QI in delivering better outcomes for patients.
How this article was made
AB and FO are both specialist quality improvement practitioners and have developed their expertise working in QI roles for a variety of UK healthcare organisations. The analysis presented here arose from AB and FO’s observations of the challenges faced when introducing QI, with healthcare providers often unable to distinguish between QI and other change approaches, making it difficult to understand what QI can do for them.
How is quality improvement defined?
There are many definitions of QI ( box 1 ). The BMJ ’s Quality Improvement series uses the Academy of Medical Royal Colleges definition. 6 Rather than viewing QI as a single method or set of tools, it can be more helpful to think of QI as based on a set of principles common to many of these definitions: a systematic continuous approach that aims to solve problems in healthcare, improve service provision, and ultimately provide better outcomes for patients.
Definitions of quality improvement
Improvement in patient outcomes, system performance, and professional development that results from a combined, multidisciplinary approach in how change is delivered. 3
The delivery of healthcare with improved outcomes and lower cost through continuous redesigning of work processes and systems. 4
Using a systematic change method and strategies to improve patient experience and outcome. 5
To make a difference to patients by improving safety, effectiveness, and experience of care by using understanding of our complex healthcare environment, applying a systematic approach, and designing, testing, and implementing changes using real time measurement for improvement. 6
In this article we discuss QI as an approach to improving healthcare that follows the principles outlined in box 2 ; this may be a useful reference to consider how particular methods or tools could be used as part of a QI approach.
Principles of QI
Primary intent— To bring about measurable improvement to a specific aspect of healthcare delivery, often with evidence or theory of what might work but requiring local iterative testing to find the best solution. 7
Employing an iterative process of testing change ideas— Adopting a theory of change which emphasises a continuous process of planning and testing changes, studying and learning from comparing the results to a predicted outcome, and adapting hypotheses in response to results of previous tests. 8 9
Consistent use of an agreed methodology— Many different QI methodologies are available; commonly cited methodologies include the Model for Improvement, Lean, Six Sigma, and Experience-based Co-design. 4 Systematic review shows that the choice of tools or methodologies has little impact on the success of QI provided that the chosen methodology is followed consistently. 10 Though there is no formal agreement on what constitutes a QI tool, it would include activities such as process mapping that can be used within a range of QI methodological approaches. NHS Scotland’s Quality Improvement Hub has a glossary of commonly used tools in QI. 11
Empowerment of front line staff and service users— QI work should engage staff and patients by providing them with the opportunity and skills to contribute to improvement work. Recognition of this need often manifests in drives from senior leadership or management to build QI capability in healthcare organisations, but it also requires that frontline staff and service users feel able to make use of these skills and take ownership of improvement work. 12
Using data to drive improvement— To drive decision making by measuring the impact of tests of change over time and understanding variation in processes and outcomes. Measurement for improvement typically prioritises this narrative approach over concerns around exactness and completeness of data. 13 14
Scale-up and spread, with adaptation to context— As interventions tested using a QI approach are scaled up and the degree of belief in their efficacy increases, it is desirable that they spread outward and be adopted by others. Key to successful diffusion of improvement is the adaption of interventions to new environments, patient and staff groups, available resources, and even personal preferences of healthcare providers in surrounding areas, again using an iterative testing approach. 15 16
What other approaches to improving healthcare are there?
Taking considered action to change healthcare for the better is not new, but QI as a distinct approach to improving healthcare is a relatively recent development. There are many well established approaches to evaluating and making changes to healthcare services in use, and QI will only be adopted more widely if it offers a new perspective or an advantage over other approaches in certain situations.
A non-systematic literature scan identified the following other approaches for making change in healthcare: research, clinical audit, service evaluation, and clinical transformation. We also identified innovation as an important catalyst for change, but we did not consider it an approach to evaluating and changing healthcare services so much as a catch-all term for describing the development and introduction of new ideas into the system. A summary of the different approaches and their definition is shown in box 3 . Many have elements in common with QI, but there are important difference in both intent and application. To be useful to clinicians and managers, QI must find a role within healthcare that complements research, audit, service evaluation, and clinical transformation while retaining the core principles that differentiate it from these approaches.
Alternatives to QI
Research— The attempt to derive generalisable new knowledge by addressing clearly defined questions with systematic and rigorous methods. 17
Clinical audit— A way to find out if healthcare is being provided in line with standards and to let care providers and patients know where their service is doing well, and where there could be improvements. 18
Service evaluation— A process of investigating the effectiveness or efficiency of a service with the purpose of generating information for local decision making about the service. 19
Clinical transformation— An umbrella term for more radical approaches to change; a deliberate, planned process to make dramatic and irreversible changes to how care is delivered. 20
Innovation— To develop and deliver new or improved health policies, systems, products and technologies, and services and delivery methods that improve people’s health. Health innovation responds to unmet needs by employing new ways of thinking and working. 21
Why do we need to make this distinction for QI to succeed?
Improvement in healthcare is 20% technical and 80% human. 22 Essential to that 80% is clear communication, clarity of approach, and a common language. Without this shared understanding of QI as a distinct approach to change, QI work risks straying from the core principles outlined above, making it less likely to succeed. If practitioners cannot communicate clearly with their colleagues about the key principles and differences of a QI approach, there will be mismatched expectations about what QI is and how it is used, lowering the chance that QI work will be effective in improving outcomes for patients. 23
There is also a risk that the language of QI is adopted to describe change efforts regardless of their fidelity to a QI approach, either due to a lack of understanding of QI or a lack of intention to carry it out consistently. 9 Poor fidelity to the core principles of QI reduces its effectiveness and makes its desired outcome less likely, leading to wasted effort by participants and decreasing its credibility. 2 8 24 This in turn further widens the gap between advocates of QI and those inclined to scepticism, and may lead to missed opportunities to use QI more widely, consequently leading to variation in the quality of patient care.
Without articulating the differences between QI and other approaches, there is a risk of not being able to identify where a QI approach can best add value. Conversely, we might be tempted to see QI as a “silver bullet” for every healthcare challenge when a different approach may be more effective. In reality it is not clear that QI will be fit for purpose in tackling all of the wicked problems of healthcare delivery and we must be able to identify the right tool for the job in each situation. 25 Finally, while different approaches will be better suited to different types of challenge, not having a clear understanding of how approaches differ and complement each other may mean missed opportunities for multi-pronged approaches to improving care.
What is the relationship between QI and other approaches such as audit?
Academic journals, healthcare providers, and “arms-length bodies” have made various attempts to distinguish between the different approaches to improving healthcare. 19 26 27 28 However, most comparisons do not include QI or compare QI to only one or two of the other approaches. 7 29 30 31 To make it easier for people to use QI approaches effectively and appropriately, we summarise the similarities, differences, and crossover between QI and other approaches to tackling healthcare challenges ( fig 1 ).

How quality improvement interacts with other approaches to improving healthcare
- Download figure
- Open in new tab
- Download powerpoint
QI and research
Research aims to generate new generalisable knowledge, while QI typically involves a combination of generating new knowledge or implementing existing knowledge within a specific setting. 32 Unlike research, including pragmatic research designed to test effectiveness of interventions in real life, QI does not aim to provide generalisable knowledge. In common with QI, research requires a consistent methodology. This method is typically used, however, to prove or disprove a fixed hypothesis rather than the adaptive hypotheses developed through the iterative testing of ideas typical of QI. Both research and QI are interested in the environment where work is conducted, though with different intentions: research aims to eliminate or at least reduce the impact of many variables to create generalisable knowledge, whereas QI seeks to understand what works best in a given context. The rigour of data collection and analysis required for research is much higher; in QI a criterion of “good enough” is often applied.
Relationship with QI
Though the goal of clinical research is to develop new knowledge that will lead to changes in practice, much has been written on the lag time between publication of research evidence and system-wide adoption, leading to delays in patients benefitting from new treatments or interventions. 33 QI offers a way to iteratively test the conditions required to adapt published research findings to the local context of individual healthcare providers, generating new knowledge in the process. Areas with little existing knowledge requiring further research may be identified during improvement activities, which in turn can form research questions for further study. QI and research also intersect in the field of improvement science, the academic study of QI methods which seeks to ensure QI is carried out as effectively as possible. 34
Scenario: QI for translational research
Newly published research shows that a particular physiotherapy intervention is more clinically effective when delivered in short, twice-daily bursts rather than longer, less frequent sessions. A team of hospital physiotherapists wish to implement the change but are unclear how they will manage the shift in workload and how they should introduce this potentially disruptive change to staff and to patients.
Before continuing reading think about your own practice— How would you approach this situation, and how would you use the QI principles described in this article?
Adopting a QI approach, the team realise that, although the change they want to make is already determined, the way in which it is introduced and adapted to their wards is for them to decide. They take time to explain the benefits of the change to colleagues and their current patients, and ask patients how they would best like to receive their extra physiotherapy sessions.
The change is planned and tested for two weeks with one physiotherapist working with a small number of patients. Data are collected each day, including reasons why sessions were missed or refused. The team review the data each day and make iterative changes to the physiotherapist’s schedule, and to the times of day the sessions are offered to patients. Once an improvement is seen, this new way of working is scaled up to all of the patients on the ward.
The findings of the work are fed into a service evaluation of physiotherapy provision across the hospital, which uses the findings of the QI work to make recommendations about how physiotherapy provision should be structured in the future. People feel more positive about the change because they know colleagues who have already made it work in practice.
QI and clinical audit
Clinical audit is closely related to QI: it is often used with the intention of iteratively improving the standard of healthcare, albeit in relation to a pre-determined standard of best practice. 35 When used iteratively, interspersed with improvement action, the clinical audit cycle adheres to many of the principles of QI. However, in practice clinical audit is often used by healthcare organisations as an assurance function, making it less likely to be carried out with a focus on empowering staff and service users to make changes to practice. 36 Furthermore, academic reviews of audit programmes have shown audit to be an ineffective approach to improving quality due to a focus on data collection and analysis without a well developed approach to the action section of the audit cycle. 37 Clinical audits, such as the National Clinical Audit Programme in the UK (NCAPOP), often focus on the management of specific clinical conditions. QI can focus on any part of service delivery and can take a more cross-cutting view which may identify issues and solutions that benefit multiple patient groups and pathways. 30
Audit is often the first step in a QI process and is used to identify improvement opportunities, particularly where compliance with known standards for high quality patient care needs to be improved. Audit can be used to establish a baseline and to analyse the impact of tests of change against the baseline. Also, once an improvement project is under way, audit may form part of rapid cycle evaluation, during the iterative testing phase, to understand the impact of the idea being tested. Regular clinical audit may be a useful assurance tool to help track whether improvements have been sustained over time.
Scenario: Audit and QI
A foundation year 2 (FY2) doctor is asked to complete an audit of a pre-surgical pathway by looking retrospectively through patient documentation. She concludes that adherence to best practice is mixed and recommends: “Remind the team of the importance of being thorough in this respect and re-audit in 6 months.” The results are presented at an audit meeting, but a re-audit a year later by a new FY2 doctor shows similar results.
Before continuing reading think about your own practice— How would you approach this situation, and how would you use the QI principles described in this paper?
Contrast the above with a team-led, rapid cycle audit in which everyone contributes to collecting and reviewing data from the previous week, discussed at a regular team meeting. Though surgical patients are often transient, their experience of care and ideas for improvement are captured during discharge conversations. The team identify and test several iterative changes to care processes. They document and test these changes between audits, leading to sustainable change. Some of the surgeons involved work across multiple hospitals, and spread some of the improvements, with the audit tool, as they go.
QI and service evaluation
In practice, service evaluation is not subject to the same rigorous definition or governance as research or clinical audit, meaning that there are inconsistencies in the methodology for carrying it out. While the primary intent for QI is to make change that will drive improvement, the primary intent for evaluation is to assess the performance of current patient care. 38 Service evaluation may be carried out proactively to assess a service against its stated aims or to review the quality of patient care, or may be commissioned in response to serious patient harm or red flags about service performance. The purpose of service evaluation is to help local decision makers determine whether a service is fit for purpose and, if necessary, identify areas for improvement.
Service evaluation may be used to initiate QI activity by identifying opportunities for change that would benefit from a QI approach. It may also evaluate the impact of changes made using QI, either during the work or after completion to assess sustainability of improvements made. Though likely planned as separate activities, service evaluation and QI may overlap and inform each other as they both develop. Service evaluation may also make a judgment about a service’s readiness for change and identify any barriers to, or prerequisites for, carrying out QI.
QI and clinical transformation
Clinical transformation involves radical, dramatic, and irreversible change—the sort of change that cannot be achieved through continuous improvement alone. As with service evaluation, there is no consensus on what clinical transformation entails, and it may be best thought of as an umbrella term for the large scale reform or redesign of clinical services and the non-clinical services that support them. 20 39 While it is possible to carry out transformation activity that uses elements of QI approach, such as effective engagement of the staff and patients involved, QI which rests on iterative test of change cannot have a transformational approach—that is, one-off, irreversible change.
There is opportunity to use QI to identify and test ideas before full scale clinical transformation is implemented. This has the benefit of engaging staff and patients in the clinical transformation process and increasing the degree of belief that clinical transformation will be effective or beneficial. Transformation activity, once completed, could be followed up with QI activity to drive continuous improvement of the new process or allow adaption of new ways of working. As interventions made using QI are scaled up and spread, the line between QI and transformation may seem to blur. The shift from QI to transformation occurs when the intention of the work shifts away from continuous testing and adaptation into the wholesale implementation of an agreed solution.
Scenario: QI and clinical transformation
An NHS trust’s human resources (HR) team is struggling to manage its junior doctor placements, rotas, and on-call duties, which is causing tension and has led to concern about medical cover and patient safety out of hours. A neighbouring trust has launched a smartphone app that supports clinicians and HR colleagues to manage these processes with the great success.
This problem feels ripe for a transformation approach—to launch the app across the trust, confident that it will solve the trust’s problems.
Before continuing reading think about your own organisation— What do you think will happen, and how would you use the QI principles described in this article for this situation?
Outcome without QI
Unfortunately, the HR team haven’t taken the time to understand the underlying problems with their current system, which revolve around poor communication and clarity from the HR team, based on not knowing who to contact and being unable to answer questions. HR assume that because the app has been a success elsewhere, it will work here as well.
People get excited about the new app and the benefits it will bring, but no consideration is given to the processes and relationships that need to be in place to make it work. The app is launched with a high profile campaign and adoption is high, but the same issues continue. The HR team are confused as to why things didn’t work.
Outcome with QI
Although the app has worked elsewhere, rolling it out without adapting it to local context is a risk – one which application of QI principles can mitigate.
HR pilot the app in a volunteer specialty after spending time speaking to clinicians to better understand their needs. They carry out several tests of change, ironing out issues with the process as they go, using issues logged and clinician feedback as a source of data. When they are confident the app works for them, they expand out to a directorate, a division, and finally the transformational step of an organisation-wide rollout can be taken.
Education into practice
Next time when faced with what looks like a quality improvement (QI) opportunity, consider asking:
How do you know that QI is the best approach to this situation? What else might be appropriate?
Have you considered how to ensure you implement QI according to the principles described above?
Is there opportunity to use other approaches in tandem with QI for a more effective result?
How patients were involved in the creation of this article
This article was conceived and developed in response to conversations with clinicians and patients working together on co-produced quality improvement and research projects in a large UK hospital. The first iteration of the article was reviewed by an expert patient, and, in response to their feedback, we have sought to make clearer the link between understanding the issues raised and better patient care.
Contributors: This work was initially conceived by AB. AB and FO were responsible for the research and drafting of the article. AB is the guarantor of the article.
Competing interests: We have read and understood BMJ policy on declaration of interests and have no relevant interests to declare.
Provenance and peer review: This article is part of a series commissioned by The BMJ based on ideas generated by a joint editorial group with members from the Health Foundation and The BMJ , including a patient/carer. The BMJ retained full editorial control over external peer review, editing, and publication. Open access fees and The BMJ ’s quality improvement editor post are funded by the Health Foundation.
This is an Open Access article distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/ .
- Olsson-Brown A
- Dixon-Woods M ,
- Batalden PB ,
- Berwick D ,
- Øvretveit J
- Academy of Medical Royal Colleges
- Nelson WA ,
- McNicholas C ,
- Woodcock T ,
- Alderwick H ,
- ↵ NHS Scotland Quality Improvement Hub. Quality improvement glossary of terms. http://www.qihub.scot.nhs.uk/qi-basics/quality-improvement-glossary-of-terms.aspx .
- McNicol S ,
- Solberg LI ,
- Massoud MR ,
- Albrecht Y ,
- Illingworth J ,
- Department of Health
- ↵ NHS England. Clinical audit. https://www.england.nhs.uk/clinaudit/ .
- Healthcare Quality Improvement Partnership
- McKinsey Hospital Institute
- ↵ World Health Organization. WHO Health Innovation Group. 2019. https://www.who.int/life-course/about/who-health-innovation-group/en/ .
- Sheffield Microsystem Coaching Academy
- Davidoff F ,
- Leviton L ,
- Taylor MJ ,
- Nicolay C ,
- Tarrant C ,
- Twycross A ,
- ↵ University Hospitals Bristol NHS Foundation Trust. Is your study research, audit or service evaluation. http://www.uhbristol.nhs.uk/research-innovation/for-researchers/is-it-research,-audit-or-service-evaluation/ .
- ↵ University of Sheffield. Differentiating audit, service evaluation and research. 2006. https://www.sheffield.ac.uk/polopoly_fs/1.158539!/file/AuditorResearch.pdf .
- ↵ Royal College of Radiologists. Audit and quality improvement. https://www.rcr.ac.uk/clinical-radiology/audit-and-quality-improvement .
- Gundogan B ,
- Finkelstein JA ,
- Brickman AL ,
- Health Foundation
- Johnston G ,
- Crombie IK ,
- Davies HT ,
- Hillman T ,
- ↵ NHS Health Research Authority. Defining research. 2013. https://www.clahrc-eoe.nihr.ac.uk/wp-content/uploads/2014/04/defining-research.pdf .
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- My Account Login
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Perspective
- Open access
- Published: 09 April 2024
The potential for artificial intelligence to transform healthcare: perspectives from international health leaders
- Christina Silcox 1 ,
- Eyal Zimlichmann 2 , 3 ,
- Katie Huber ORCID: orcid.org/0000-0003-2519-8714 1 ,
- Neil Rowen 1 ,
- Robert Saunders 1 ,
- Mark McClellan 1 ,
- Charles N. Kahn III 3 , 4 ,
- Claudia A. Salzberg 3 &
- David W. Bates ORCID: orcid.org/0000-0001-6268-1540 5 , 6 , 7
npj Digital Medicine volume 7 , Article number: 88 ( 2024 ) Cite this article
2809 Accesses
39 Altmetric
Metrics details
- Health policy
- Health services
Artificial intelligence (AI) has the potential to transform care delivery by improving health outcomes, patient safety, and the affordability and accessibility of high-quality care. AI will be critical to building an infrastructure capable of caring for an increasingly aging population, utilizing an ever-increasing knowledge of disease and options for precision treatments, and combatting workforce shortages and burnout of medical professionals. However, we are not currently on track to create this future. This is in part because the health data needed to train, test, use, and surveil these tools are generally neither standardized nor accessible. There is also universal concern about the ability to monitor health AI tools for changes in performance as they are implemented in new places, used with diverse populations, and over time as health data may change. The Future of Health (FOH), an international community of senior health care leaders, collaborated with the Duke-Margolis Institute for Health Policy to conduct a literature review, expert convening, and consensus-building exercise around this topic. This commentary summarizes the four priority action areas and recommendations for health care organizations and policymakers across the globe that FOH members identified as important for fully realizing AI’s potential in health care: improving data quality to power AI, building infrastructure to encourage efficient and trustworthy development and evaluations, sharing data for better AI, and providing incentives to accelerate the progress and impact of AI.
Similar content being viewed by others

Guiding principles for the responsible development of artificial intelligence tools for healthcare
A short guide for medical professionals in the era of artificial intelligence
Reporting guidelines in medical artificial intelligence: a systematic review and meta-analysis
Introduction.
Artificial intelligence (AI), supported by timely and accurate data and evidence, has the potential to transform health care delivery by improving health outcomes, patient safety, and the affordability and accessibility of high-quality care 1 , 2 . AI integration is critical to building an infrastructure capable of caring for an increasingly aging population, utilizing an ever-increasing knowledge of disease and options for precision treatments, and combatting workforce shortages and burnout of medical professionals. However, we are not currently on track to create this future. This is in part because the health data needed to train, test, use, and surveil these tools are generally neither standardized nor accessible. This is true across the international community, although there is variable progress within individual countries. There is also universal concern about monitoring health AI tools for changes in performance as they are implemented in new places, used with diverse populations, and over time as health data may change.
The Future of Health (FOH) is an international community of senior health care leaders representing health systems, health policy, health care technology, venture funding, insurance, and risk management. FOH collaborated with the Duke-Margolis Institute for Health Policy to conduct a literature review, expert convening, and consensus-building exercise. In total, 46 senior health care leaders were engaged in this work, from eleven countries in Europe, North America, Africa, Asia, and Australia. This commentary summarizes the four priority action areas and recommendations for health care organizations and policymakers that FOH members identified as important for fully realizing AI’s potential in health care: improving data quality to power AI, building infrastructure to encourage efficient and trustworthy development and evaluations, sharing data for better AI, and providing incentives to accelerate the progress and impact of AI.
Powering AI through high-quality data
“Going forward, data are going to be the most valuable commodity in health care. Organizations need robust plans about how to mobilize and use their data.”
AI algorithms will only perform as well as the accuracy and completeness of key underlying data, and data quality is dependent on actions and workflows that encourage trust.
To begin to improve data quality, FOH members agreed that an initial priority is identifying and assuring reliable availability of high-priority data elements for promising AI applications: those with the most predictive value, those of the highest value to patients, and those most important for analyses of performance, including subgroup analyses to detect bias.
Leaders should also advocate for aligned policy incentives to improve the availability and reliability of these priority data elements. There are several examples of efforts across the world to identify and standardize high-priority data elements for AI applications and beyond, such as the multinational project STANDING Together, which is developing standards to improve the quality and representativeness of data used to build and test AI tools 3 .
Policy incentives that would further encourage high-quality data collection include (1) aligned payment incentives for measures of health care quality and safety, and ensuring the reliability of the underlying data, and (2) quality measures and performance standards focused on the reliability, completeness, and timeliness of collection and sharing of high-priority data itself.
Trust and verify
“Your AI algorithms are only going to be as good as the data and the real-world evidence used to validate them, and the data are only going to be as good as the trust and privacy and supporting policies.”
FOH members stressed the importance of showing that AI tools are both effective and safe within their specific patient populations.
This is a particular challenge with AI tools, whose performance can differ dramatically across sites and over time, as health data patterns and population characteristics vary. For example, several studies of the Epic Sepsis Model found both location-based differences in performance and degradation in performance over time due to data drift 4 , 5 . However, real-world evaluations are often much more difficult for algorithms that are used for longer-term predictions, or to avert long-term complications from occurring, particularly in the absence of connected, longitudinal data infrastructure. As such, health systems must prioritize implementing data standards and data infrastructure that can facilitate the retraining or tuning of algorithms, test for local performance and bias, and ensure scalability across the organization and longer-term applications 6 .
There are efforts to help leaders and health systems develop consensus-based evaluation techniques and infrastructure for AI tools, including HealthAI: The Global Agency for Responsible AI in Health, which aims to build and certify validation mechanisms for nations and regions to adopt; and the Coalition for Health AI (CHAI), which recently announced plans to build a US-wide health AI assurance labs network 7 , 8 . These efforts, if successful, will assist manufacturers and health systems in complying with new laws, rules, and regulations being proposed and released that seek to ensure AI tools are trustworthy, such as the EU AI Act and the 2023 US Executive Order on AI.
Sharing data for better AI
“Underlying these challenges is the investment required to standardize business processes so that you actually get data that’s usable between institutions and even within an institution.”
While high-quality internal data may enable some types of AI-tool development and testing, this is insufficient to power and evaluate all AI applications. To build truly effective AI-enabled predictive software for clinical care and predictive supports, data often need to be interoperable across health systems to build a diverse picture of patients’ health across geographies, and reliably shared.
FOH members recommended that health care leaders work with researchers and policymakers to connect detailed encounter data with longitudinal outcomes, and pilot opportunities across diverse populations and systems to help assure valid outcome evaluations as well as address potential confounding and population subgroup differences—the ability to aggregate data is a clear rate-limiting step. The South African National Digital Health Strategy outlined interventions to improve the adoption of digital technologies while complying with the 2013 Protection of Personal Information Act 9 . Although challenges remain, the country has made progress on multiple fronts, including building out a Health Patient Registration System as a first step towards a portable, longitudinal patient record system and releasing a Health Normative Standards Framework to improve data flow across institutional and geographic boundaries 10 .
Leaders should adopt policies in their organizations, and encourage adoption in their province and country, that simplify data governance and sharing while providing appropriate privacy protections – including building foundations of trust with patients and the public as previously discussed. Privacy-preserving innovations include ways to “share” data without movement from protected systems using approaches like federated analyses, data sandboxes, or synthetic data. In addition to exploring privacy-preserving approaches to data sharing, countries and health systems may need to consider broad and dynamic approaches to consent 11 , 12 . As we look to a future where a patient may have thousands of algorithms churning away at their data, efforts to improve data quality and sharing should include enabling patients’ access to and engagement with their own data to encourage them to actively partner in their health and provide transparency on how their data are being used to improve health care. For example, the Understanding Patient Data program in the United Kingdom produces research and resources to explain how the National Health Service uses patients’ data 13 . Community engagement efforts can further assist with these efforts by building trust and expanding understanding.
FOH members also stressed the importance of timely data access. Health systems should work together to establish re-usable governance and privacy frameworks that allow stakeholders to clearly understand what data will be shared and how it will be protected to reduce the time needed for data use agreements. Trusted third-party data coordinating centers could also be used to set up “precertification” systems around data quality, testing, and cybersecurity to support health organizations with appropriate data stewardship to form partnerships and access data rapidly.
Incentivizing progress for AI impact
“Unless it’s tied to some kind of compensation to the organization, the drive to help implement those tools and overcome that risk aversion is going to be very high… I do think that business driver needs to be there.”
AI tools and data quality initiatives have not moved as quickly in health care due to the lack of direct payment, and often, misalignment of financial incentives and supports for high-quality data collection and predictive analytics. This affects both the ability to purchase and safely implement commercial AI products as well as the development of “homegrown” AI tools.
FOH members recommended that leaders should advocate for paying for value in health – quality, safety, better health, and lower costs for patients. This better aligns the financial incentives for accelerating the development, evaluation, and adoption of AI as well as other tools designed to either keep patients healthy or quickly diagnose and treat them with the most effective therapies when they do become ill. Effective personalized health care requires high-quality, standardized, interoperable datasets from diverse sources 14 . Within value-based payments themselves, data are critical to measuring quality of care and patient outcomes, adjusted or contextualized for factors outside of clinical control. Value-based payments therefore align incentives for (1) high-quality data collection and trusted use, (2) building effective AI tools, and (3) ensuring that those tools are improving patient outcomes and/or health system operations.
Data have become the most valuable commodity in health care, but questions remain about whether there will be an AI “revolution” or “evolution” in health care delivery. Early AI applications in certain clinical areas have been promising, but more advanced AI tools will require higher quality, real-world data that is interoperable and secure. The steps health care organization leaders and policymakers take in the coming years, starting with short-term opportunities to develop meaningful AI applications that achieve measurable improvements in outcomes and costs, will be critical in enabling this future that can improve health outcomes, safety, affordability, and equity.
Data availability
Data sharing is not applicable to this article as no datasets were generated or analyzed during the current study.
Abernethy, A. et al. The promise of digital health: then, now, and the future. NAM Perspect. 6 (2022).
Akpakwu, E. Four ways AI can make healthcare more efficient and affordable. World Economic Forum https://www.weforum.org/agenda/2018/05/four-ways-ai-is-bringing-down-the-cost-of-healthcare/ (2018).
STANDING Together. https://www.datadiversity.org/home .
Wong, A. et al. External validation of a widely implemented proprietary sepsis prediction model in hospitalized patients. JAMA Intern Med 181 , 1065–1070 (2021).
Article PubMed Google Scholar
Ross, C. STAT and MIT rooted out the weaknesses in health care algorithms. Here’s how we did it. STAT https://www.statnews.com/2022/02/28/data-drift-machine-learning/ (2022).
Locke, T., Parker, V., Thoumi, A., Goldstein, B. & Silcox, C. Preventing bias and inequities in AI-enabled health tools . https://healthpolicy.duke.edu/publications/preventing-bias-and-inequities-ai-enabled-health-tools (2022).
Introducing HealthAI. The International Digital Health and AI Research Collaborative (I-DAIR) https://www.i-dair.org/news/introducing-healthai (2023).
Shah, N. H. et al. A nationwide network of health AI assurance laboratories. JAMA 331 , 245 (2024).
Singh, V. AI & Data in South Africa’s Health Sector . https://policyaction.org.za/sites/default/files/PAN_TopicalGuide_AIData6_Health_Elec.pdf (2020).
Zharima, C., Griffiths, F. & Goudge, J. Exploring the barriers and facilitators to implementing electronic health records in a middle-income country: a qualitative study from South Africa. Front. Digit. Health 5 , 1207602 (2023).
Article PubMed PubMed Central Google Scholar
Lee, A. R. et al. Identifying facilitators of and barriers to the adoption of dynamic consent in digital health ecosystems: a scoping review. BMC Med. Ethics 24 , 107 (2023).
Article CAS PubMed PubMed Central Google Scholar
Stoeklé, H. C., Hulier-Ammar, E. & Hervé, C. Data medicine: ‘broad’ or ‘dynamic’ consent? Public Health Ethics 15 , 181–185 (2022).
Article Google Scholar
Understanding Patient Data. Understanding Patient Data http://understandingpatientdata.org.uk/ .
Chén, O. Y. & Roberts, B. Personalized health care and public health in the digital age. Front. Digit. Health 3 , 595704 (2021).
Download references
Acknowledgements
The authors acknowledge Oranit Ido and Jonathan Gonzalez-Smith for their contributions to this work. This study was funded by The Future of Health, LLC. The Future of Health, LLC, was involved in all stages of this research, including study design, data collection, analysis and interpretation of data, and the preparation of this manuscript.
Author information
Authors and affiliations.
Duke-Margolis Institute for Health Policy, Duke University, Washington, DC, USA &, Durham, NC, USA
Christina Silcox, Katie Huber, Neil Rowen, Robert Saunders & Mark McClellan
Sheba Medical Center, Ramat Gan, Israel
Eyal Zimlichmann
Future of Health, Washington, DC, USA
Eyal Zimlichmann, Charles N. Kahn III & Claudia A. Salzberg
Federation of American Hospitals, Washington, DC, USA
Charles N. Kahn III
Division of General Internal Medicine, Brigham and Women’s Hospital, Boston, MA, USA
David W. Bates
Harvard Medical School, Boston, MA, USA
Department of Health Policy and Management, Harvard T. H. Chan School of Public Health, Boston, MA, USA
You can also search for this author in PubMed Google Scholar
Contributions
C.S., K.H., N.R., and R.S. conducted initial background research and analyzed qualitative data from stakeholders. All authors (C.S., E.Z., K.H., N.R., R.S., M.M., C.K., C.A.S., and D.B.) assisted with conceptualization of the project and strategic guidance. C.S., K.H., and N.R. wrote initial drafts of the manuscript. All authors contributed to critical revisions of the manuscript and read and approved the final manuscript.
Corresponding author
Correspondence to David W. Bates .
Ethics declarations
Competing interests.
C.S., K.H., N.R., and C.A.S. declare no competing interests. E.Z. reports personal fees from Arkin Holdings, personal fees from Statista and equity from Valera Health, Profility and Hello Heart. R.S. has been an external reviewer for The John A. Hartford Foundation, and is a co-chair for the Health Evolution Summit Roundtable on Value-Based Care for Specialized Populations. M.M. is an independent director on the boards of Johnson & Johnson, Cigna, Alignment Healthcare, and PrognomIQ; co-chairs the Guiding Committee for the Health Care Payment Learning and Action Network; and reports fees for serving as an adviser for Arsenal Capital Partners, Blackstone Life Sciences, and MITRE. C.K. is a Profility Board member and additionally reports equity from Valera Health and MDClone. D.W.B. reports grants and personal fees from EarlySense, personal fees from CDI Negev, equity from Valera Health, equity from Clew, equity from MDClone, personal fees and equity from AESOP, personal fees and equity from Feelbetter, equity from Guided Clinical Solutions, and grants from IBM Watson Health, outside the submitted work. D.W.B. has a patent pending (PHC-028564 US PCT), on intraoperative clinical decision support.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Silcox, C., Zimlichmann, E., Huber, K. et al. The potential for artificial intelligence to transform healthcare: perspectives from international health leaders. npj Digit. Med. 7 , 88 (2024). https://doi.org/10.1038/s41746-024-01097-6
Download citation
Received : 30 October 2023
Accepted : 29 March 2024
Published : 09 April 2024
DOI : https://doi.org/10.1038/s41746-024-01097-6
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
Service quality in the healthcare sector: a systematic review and meta-analysis
LBS Journal of Management & Research
ISSN : 0972-8031
Article publication date: 16 January 2023
Issue publication date: 4 September 2023
The purpose of this study is to summarize the available pool of literature on service quality to identify different dimensions of service quality in the healthcare industry and understand how it is measured. The study attempts to explore the research gaps in the literature about different service quality dimensions and patient satisfaction.
Design/methodology/approach
A systematic literature review process was followed to achieve the objectives of the study. Various inclusion and exclusion criteria were used to select relevant research articles from 2000–2020 for the study, and a total of 100 research articles were selected.
The study identified 41 different dimensions of healthcare service quality measurement and classified these dimensions into four categories, namely servicescape, personnel, hospital administration and patients. It can be concluded that SERVQUAL is the most widely used service quality measurement tool.
Originality/value
The study identified that a majority of the researchers deduced a positive relationship between SERVQUAL dimensions and the quality of healthcare services. The findings of study will assist hospital executives in formulating effective strategies to ensure that patients receive superior quality healthcare services.
- Healthcare sector
- Service quality
- Systematic review
Darzi, M.A. , Islam, S.B. , Khursheed, S.O. and Bhat, S.A. (2023), "Service quality in the healthcare sector: a systematic review and meta-analysis", LBS Journal of Management & Research , Vol. 21 No. 1, pp. 13-29. https://doi.org/10.1108/LBSJMR-06-2022-0025
Emerald Publishing Limited
Copyright © 2022, Mushtaq Ahmad Darzi, Sheikh Basharul Islam, Syed Owais Khursheed and Suhail Ahmad Bhat
Published in LBS Journal of Management & Research . Published by Emerald Publishing Limited. This article is published under the Creative Commons Attribution (CC BY 4.0) licence. Anyone may reproduce, distribute, translate and create derivative works of this article (for both commercial and no commercial purposes), subject to full attribution to the original publication and authors. The full terms of this licence may be seen at http://creativecommons.org/licences/by/4.0/legalcode
Introduction
The quality of healthcare services has long been a subject of concern for both private and public healthcare service providers across the globe. According to Senic and Marinkovic (2013) , integrity and competitiveness of a nation's healthcare structure are gauged by the quality of healthcare services rendered. Indian National Health Policy 2017 envisions that everyone should have access to high-quality healthcare without facing financial suffering ( MoHFW, 2017 ). Adherence to quality standards and improved quality design results in a better-perceived value, which leads to better prices, better income and greater profitability ( Zeithaml, 2000 ). Customers of the healthcare industry in developing countries are becoming more and more aware of their right to quality healthcare. Consequently, delivering high-quality service by healthcare service providers is gaining momentum ( Abuosi & Atinga, 2013 ). According to Yee, Yeung, and Cheng (2010) , healthcare service providers need to provide high-quality services to sustain the trustworthiness of patients. Demand for superior service quality is growing due to an increase in the per capita income of customers and increased aspirations of the customer ( Singh & Prasher, 2019 ). Also, as a result of competition from private healthcare service providers, public care providers are facing pressing demand for delivering high-quality services ( Zarei, Arab, Froushani, Rashidian, & Ghazi-Tabatabaei, 2012 ).
Mosadeghrad (2014, p. 78) defined healthcare quality as “ consistently delighting the patient by providing efficacious, effective and efficient healthcare services according to the latest clinical guidelines and standards, which meet the patient ' s needs and satisfies providers ”. Ovretveit (2009, p. 4) defines quality care as the “ p rovision of care that exceeds patient expectations and achieves the highest possible clinical outcomes with the resources available ”. Parasuraman, Zeithaml and Berry (1985) described service quality as the gap between a customer's expectations of service and the customer's perception of service after the service is rendered. When perception exceeds expectations, the customer will be satisfied ( Kalaja, Myshketa, & Scalera, 2016 ). Several studies have confirmed that customer expectations of service are much higher than the customer perception of services rendered by both public and private sector institutions ( Andaleeb, Siddiqui, & Khandakar, 2007 ; Zarei et al. , 2012 ; Manulik, Rosińczuk, & Karniej, 2016 ). A firm provides quality service when its services at least meet or exceed the expectations of the customer ( Owusu-Frimpong, Nwankwo, & Dason, 2010 ). Service quality evaluation varies from the service provider's and service receiver's point of view. Service delivery professionals evaluate service based on delivery and design aspects, while receivers of service evaluate it based on their overall perception after consuming the service ( Brown & Swartz, 1989 ). Traditionally healthcare quality was judged based on some objective criteria such as mortality rate, morbidity rate, infant mortality rate, etc. However, as time passes, the structure of the industry changed, and the role of patients in deciding quality has been given more and more consideration ( Dagger, Sweeney, & Johnson, 2007 ). To survive in the modern competitive markets, it has become of utmost importance for service providers to understand the needs and expectations of customers. They must deliver what the customer is expected instead of what they feel is important for a customer to maintain the business demand ( Singh & Prasher, 2019 ). Kotler and Keller (2006) suggest that in the consumer-oriented healthcare market where healthcare delivery is commodified and patient-led, the patient should be the judge of service quality. Hence, to provide better quality services, healthcare service providers need to identify the main dimensions of service quality in healthcare and focus on those dimensions rated more important by the patients ( Singh & Prasher, 2019 ).
Studies on healthcare service quality have been conducted in a variety of settings worldwide, namely Albania ( Kalaja et al. , 2016 ), Australia ( Copnell et al. , 2009 ; Dagger et al. , 2007 ; Levesque & Sutherland, 2020 ), Bangladesh ( Andaleeb et al. , 2007 ), China ( Li et al. , 2015 ; Wu, Li, & Li, 2016 ), Denmark ( Engelbrecht, 2005 ; Groene, Skau, & Frølich, 2008 ), Ghana ( Abuosi & Atinga, 2013 ; Agyapong, Afi, & Kwateng, 2018 ), India ( Chahal, 2008 ; Aagja & Garg, 2010 ; Chahal & Kumari, 2010 ; Gupta & Rokade, 2016 ; Singh & Prasher, 2019 ; Upadhyai, Jain, Roy, & Pant, 2019 ; Jog et al. , 2020 ), Iran ( Goshtasebi et al. , 2009 ; Mohammadkarim, Jamil, Pejman, Seyyed, & Mostafa, 2011 ; Mosadeghrad, 2014 ), Malaysia ( Ahmad & Sungip, 2008 ; Hasan, Ilias, Rahman, & Razak, 2009 ), Pakistan ( Irfan & Ijaz, 2011 ; Shabbir, Malik, & Malik, 2016 ; Fatima, Malik, & Shabbir, 2018 ; Dhahri, Iqbal, & Khan, 2020 ), Turkey ( Beyan & Baykal, 2012 ) and USA ( Lee, 2003 ; Hegji & Self, 2009 ; Mustafa, Yang, Mortezavi, Vadamalai, & Ramsey, 2020 ; Thompson, Shen, & Lee, 2020 ). The purpose of this paper is to investigate and summarize the available literature on healthcare service quality to understand what constitutes healthcare service quality and its principal dimensions and also to highlight the prominent research gaps that will provide direction for future research.
Methodology
The study followed a systematic review process to obtain research articles relevant to the research problem understudy. The systematic review process is a structured way of identifying, evaluating and interpreting the available literature related to any particular area ( Kamboj & Rahman, 2015 ). A systematic literature review is a two-step process. First, defining the criteria for inclusion of articles and second, identifying databases and research studies ( McLean & Antony, 2014 ).
Inclusion criteria
Papers published during 2000–2020 were considered for the study. This was done by applying a custom range filter. The reason for selecting the above mention time frame is the most recent two decades were selected for article search.
Research articles related to healthcare service quality were included in the review process. The criterion was adopted in line with the primary objective of the review process.
Empirical and review articles published in peer-reviewed journals were considered.
Only papers in the English language were included.
Database and article selection
The literature search was conducted in the autumn of 2021. The databases selected for the literature search included Emerald, Elsevier, Sage, Taylor and Francis and Google Scholar. Filters such as custom range and sort by relevance were applied to restrict the search results to keywords. The systematic review process is presented in Figure 1 . In stage 1 of the review process, the literature was searched using the keywords such as healthcare, healthcare services, service quality and SERVQUAL. The search obtained 209 research articles. The research papers were selected based on relevance to the topic understudy and the popularity of the articles. Researchers such as Beaulieu (2015) argued that the popularity of journal articles with above 10 citations are considered in top 24% of the highest cited articles, and articles that receive 100 citations are considered among 1.8% of the most popular articles across the globe, which makes the current study a worth addition to the existing body of literature. In stage 2, the screening of articles was then conducted first based on title and abstract and then based on inclusion criteria. Screening of articles based on the title and abstract resulted in the exclusion of 63 research articles, and 146 articles were moved to the next level of screening.
Then articles were screened by applying inclusion criteria to exclude articles that do not fulfill the above-stated criteria ( Kamboj & Rahman, 2015 ). This screening obtained 100 research articles that were finally considered for review, and the rest of the articles (46) were excluded from the study. Finally, in stage 3 of the review process, the study provides a summary (publication trend, journal-wise distribution, methodology that includes sampling method and data analysis tools used and key findings) of the 100 articles included in the review.
Common characteristics of reviewed articles
Classification of articles by research type and hospital setting
Table 1 displays the classification of research articles based on research type and hospital setting. The research type describes the nature of the research and yields that a maximum number of articles were quantitative studies (62 articles) followed by qualitative studies (15 articles) and only 07 studies that were both qualitative and quantitative. A few review articles (14 articles) were also considered during the process. The results of the review substantiate that there is a need of conducting qualitative research that can provide an in-depth understanding of how various service quality dimensions affect the perceived quality of care among patients and the treatment satisfaction level. Qualitative studies can also provide insights into the priorities of patients while receiving medical services.
The classification based on hospital setting yields more than 77 articles that have purposively chosen a specific hospital setting and the rest have collected data from respondents in general. Out of 77 articles, 49% of research studies were conducted in a public hospital setting, and 25% were conducted in a private hospital setting. Around 26% of research were conducted in both public and private hospital settings. The direct comparison of healthcare services and perceived service quality among patients was observed as the main motivator in choosing both hospital settings ( Ovretveit, 2000 ; Mostafa, 2005 ; Taner & Antony, 2006 ; Andaleeb et al. , 2007 ; Owusu-Frimpong et al. , 2010 ; Manulik et al. , 2016 ; Dhahri et al. , 2020 ).
Data analysis tool
Figure 2 presents the frequency of various data analysis tools used by researchers to obtain meaningful results. The examination of articles selected for review revealed that 15 different data analysis techniques have been utilized in the past two decades. Descriptive statistics (29 articles) including mean and standard deviation has been the most frequently applied technique in healthcare service quality research followed by t -test (18 articles). It was also found that both techniques have been applied in combination because service quality can be obtained by ascertaining the difference between service perception and service expectation of patients using the SERVQUAL model ( Ahmad & Sungip, 2008 ; Irfan & Ijaz, 2011 ; Zarei, Daneshkohan, Khabiri, & Arab, 2015 ; Torabipour, Sayaf, Salehi, & Ghasemzadeh, 2016 ). Other major techniques preferred by researchers include correlation (17 articles), regression (17 articles), systematic literature review (12 articles) and ANOVA (11 articles). However, only 20 articles in total have applied structural equation modeling (SEM), MANOVA, content analysis, chi-square test, Shapiro–Wilk test, Mann–Whitney U-test, Kruskal–Wallis tests and Wilcoxon test, making them among the least preferred techniques in healthcare service quality research.
Sampling method
Articles selected for review depict that both nonprobability and probability sampling have been applied to study healthcare service quality and patient satisfaction. The articles have adopted 08 different sampling methods in addition to the complete enumeration (Census), which was employed for 03 articles. From nonprobability sampling techniques, convenience sampling (18 articles) is the most widely used sampling technique, and simple random sampling (19 articles) is the most frequently applied sampling method from the probability sampling group. Cluster sampling was found to be the least applied sampling technique among probability sampling methods because most of the studies were focused on specific regions with a limited geographical area. Targeting a smaller geographical area or specific site increases the feasibility of reaching out to sampling units because of the limited population spread. Therefore, when further segregation based on the geographical area seems impossible, the applicability of cluster sampling becomes impractical ( Cameron & Miller, 2015 ).
Findings and discussion
The systematic review of 100 articles has fetched several important findings in terms of measures of healthcare service quality and the theories applied in examining healthcare service quality.
Measures of healthcare service quality
Healthcare service quality, because of its intangible character and subjective nature, is difficult to define and measure. The comprehensive study of research articles about healthcare service quality illustrated that service quality in healthcare is examined by using different measures primarily related to servicescape, personnel, hospital administration and patients. The study has identified 41 distinctive measures of healthcare service quality ( Table 2 ). The factors commonly used to measure the quality of servicescape are identified as physical environmental quality, diagnostic aspect of care, resources and capacity, tangibility, financial and physical access to care and access ( Herstein & Gamliel, 2006 ; Ahmad & Sungip, 2008 ; Sharma & Narang, 2011 ; Simou, Pliatsika, Koutsogeorgou, & Roumeliotou, 2014 ; Marzban, Najafi, Etedal, Moradi, & Rajaee, 2015 ). Among the mentioned dimensions of servicescape, utilization has been less studied in the past. Future researchers can explore these areas because often in healthcare centers, the infrastructure capacity is overutilized or underutilized, which hinders the delivery of healthcare services. The determinants mostly employed to determine the quality of human resources (personnel) include healthcare personnel conduct, efficacy, efficiency, empathy, interaction quality, physician and staff performance, provider competency/performance, reliability, responsiveness, timeliness and trustworthiness ( Chahal & Kumari, 2012 ; Manulik et al. , 2016 ; Singh & Prasher, 2019 ). Some of the fewer studied factors under personnel characteristics include quality of patient-staff communication, outcome quality, professional quality, provider motivation and satisfaction encounters. These factors can influence the service quality of healthcare centers but are less researched in the past. The factors concerning quality aspects of hospital management/administration include admission, assurance, healthcare delivery system, infection rate, standard operating procedures, leadership and management and medical service ( Ovretveit, 2000 ; Herstein & Gamliel, 2006 ; Taner & Antony, 2006 ; Aagja & Garg, 2010 ; Irfan & Ijaz, 2011 ; Gupta & Rokade, 2016 ; Torabipour et al. , 2016 ). Among the determinants of hospital administration availability of doctors and paramedical staff, discharge mechanism of patients, documentation procedure in the hospital, social responsibility consciousness among the staff, management quality and drug availability in the hospital are some of the key factors that influence the service encounters between staff and patients. These determinants are less studied in the literature. Future researchers can build their research on these less studied variables. Lastly, the factors affecting service quality in terms of patient characteristics include patient satisfaction, the average length of stay, patient cooperation, patient quality/illness and patient socio-demographic variables ( Ovretveit, 2000 ; Mosadeghrad, 2014 ; Gupta & Rokade, 2016 ). It was observed that most of the service quality determinants identified can be summarized under the major 05 SERVQUAL determinants.
Theories applied to healthcare service quality
The list of popular theories that have been applied to examine healthcare service quality across the globe is presented in Figure 3 . A total of 11 different theories were identified during the review process. Less than 50% of papers identified for review have adopted one or the other service quality measurement framework and around 70% (32 research articles) among them have applied the SERVQUAL framework by Parasuraman, Zeithaml, and Berry (1988) . This makes SERVQUAL the mostly widely applied service quality framework. The other theories that have been utilized in the recent decade to examine the service quality of healthcare system include total quality management, fuzzy analytical hierarchy process, service performance model and health monitoring indicators system: health map ( Chahal & Kumari, 2012 ; Ramez, 2012 ; Zarei et al. , 2015 ; Amole, Oyatoye, & Adebiyi, 2015 ; Singh & Prasher, 2019 ; Zaid, Arqawi, Mwais, Al Shobaki, & Abu-Naser, 2020 ). The elements used to measure the perceived service quality of hospitals under different theories other than the SERVQUAL model can largely be classified under five SERVQUAL dimensions. However, outcome quality, process quality, administrative/management quality, utilization, technical quality and trustworthiness are identified as additional new dimensions being used to examine the service quality of hospitals ( Ovretveit, 2000 ; Chahal & Kumari, 2010 ; Simou et al. , 2014 ; Singh & Prasher, 2019 ; Zaid et al. , 2020 ).
Limitations and future research directions
The current study has some shortcomings which open up opportunities for future research. The present study followed a systematic review process to obtain research articles from different databases, like Emerald, Elsevier, Sage, Taylor and Francis and Google Scholar. Several inclusion criteria were applied, and only those full-text articles that are available in the English language were selected for the review. Therefore, there is the possibility of excluding some articles that are not available in these databases or are available in some other languages. Further, most of the studies selected for review were from developed nations. There is a lot of difference between the healthcare system of developed and developing nations. Thus, the findings of the present study cannot be generalized to developing nations without additional validation ( Kamboj & Rahman, 2015 ). Therefore, there is a need of carrying out empirical research in developing nations in this area.
The review of available literature has revealed that there are a large number of measurement tools available for the assessment of service quality in healthcare. However, the majority of these measurement instruments developed by the researchers assess quality from patients' perspectives and do not take into consideration service providers' perspectives. The technical aspect of service quality cannot be assessed by patients alone ( Upadhyai et al. , 2019 ). For a better understanding of service quality evaluation and satisfaction of service encounters, both service providers' and receivers' perspectives should be taken into consideration ( Brown & Swartz, 1989 ). Therefore, future researchers need to explore the knowledge gap (gap 1) of the SERVQUAL gap given proposed by Parasuraman et al. (1985) .
Practical implications
The study has attempted to identify and describe all dimensions and measurement tools relevant to healthcare service quality in light of the available literature. The study provides a thorough description of a vast number of investigations and reflects their outcomes. This research could help understand the diverse conceptualizations of service quality in healthcare compared to other types of services. The study also identified various gaps in the available literature that could be answered by future research.
The results of this study will help hospital executives in understanding the various constituents of quality and their impact on patient satisfaction. This will help hospital managers in formulating strategies that will improve patient satisfaction and ultimately improving the overall performance of hospitals. The study also highlighted the factors in which patients weigh more, thereby helping hospital managers to set priorities and help in proper resource utilization.
The current study presents an in-depth review of the literature concerning service quality and patient satisfaction in the healthcare industry. Service quality is a subjective measure and hence tends to vary from place to place and from patient to patient based on preference. The study has identified different measures that have been utilized to date to examine service quality or quality gaps in various hospital settings. Most of the studies selected for review have employed SERVQUAL dimensions of quality as service quality parameters. Service quality in the majority of the studies was established based on a difference between perceived and expected scores of service quality determinants, and the t -test was identified as the widely used statistical measure for testing its significance. In addition to this, various measures to determine patient satisfaction were identified and classified based on extra 3Ps of services marketing, namely physical evidence, people and process. The maximum number and most weighted factors affecting patient satisfaction are related to human resources actively engaged in providing medical services. It was observed that SERVQUAL determinants are popularly being used as a tool to determine the level of satisfaction among patients. All SERVQUAL determinants were found to have a significant positive relationship with patient satisfaction. Finally, 11 popular theories were identified among which SERVQUAL is widely applied.
Systematic literature review process
Theories applied in healthcare service quality
Aagja , J. P. , & Garg , R. ( 2010 ). Measuring perceived service quality for public hospitals (PubHosQual) in the Indian context . International Journal of Pharmaceutical and Healthcare Marketing , 4 ( 1 ), 60 – 83 .
Abu-Kharmeh , S. S. ( 2012 ). Evaluating the quality of health care services in the Hashemite Kingdom of Jordan . International Journal of Business and Management , 7 ( 4 ), 195 – 205 .
Abuosi , A. A. , & Atinga , R. A. ( 2013 ). Service quality in healthcare institutions: Establishing the gaps for policy action . International Journal of Health Care Quality Assurance , 26 ( 5 ), 481 – 492 .
Adebayo , E. T. , Adesina , B. A. , Ahaji , L. E. , & Hussein , N. A. ( 2014 ). Patient assessment of the quality of dental care services in a Nigerian hospital . Journal of Hospital Administration , 3 ( 6 ), 20 – 28 .
Aghamolaei , T. , Eftekhaari , T. E. , Rafati , S. , Kahnouji , K. , Ahangari , S. , Shahrzad , M. E. , & Hoseini , S. H. ( 2014 ). Service quality assessment of a referral hospital in southern Iran with SERVQUAL technique: Patients' perspective . BMC Health Services Research , 14 ( 1 ), 1 – 5 .
Agyapong , A. , Afi , J. D. , & Kwateng , K. O. ( 2018 ). Examining the effect of perceived service quality of health care delivery in Ghana on behavioural intentions of patients: The mediating role of customer satisfaction . International Journal of Healthcare Management , 11 ( 4 ), 276 – 288 .
Ahmad , A. , & Sungip , Z. ( 2008 ). An assessment on service quality in Malaysia insurance industry . Communications of the IBIMA , 1 , 13 – 26 . Available from: https://www.airitilibrary.com/Publication/alDetailedMesh?docid=19437765-200802-201406040030-201406040030-13-26
Ahmed , R. , & Samreen , H. ( 2011 ). Assessing the Service quality of some selected hospitals in Karachi based on the SERVQUAL model . Pakistan Business Review , 32 ( 5 ), 266 – 314 .
Al Fraihi , K. J. , Famco , D. , & Latif , S. A. ( 2016 ). Evaluation of outpatient service quality in Eastern Saudi Arabia: Patient's expectations and perceptions . Saudi Medical Journal , 37 ( 4 ), 420 – 428 .
Amole , B. B. , Oyatoye , E. O. , & Adebiyi , S. O. ( 2015 ). Prioritization of service quality influences on patients satisfaction using analytic hierarchy process: The Nigeria experience . Economics and Applied Informatics , 3 , 25 – 35 . Available from: https://www.ceeol.com/search/article-detail?id=530660
Andaleeb , S. S. , Siddiqui , N. , & Khandakar , S. ( 2007 ). Patient satisfaction with health services in Bangladesh . Health Policy and Planning , 22 ( 4 ), 263 – 273 .
Andrews , M. A. , Areekal , B. , Rajesh , K. R. , Krishnan , J. , Suryakala , R. , Krishnan , B. , & Santhosh , P. V. ( 2020 ). First confirmed case of COVID-19 infection in India: A case report . The Indian Journal of Medical Research , 151 ( 5 ), 490 – 492 .
Bahadori , M. , Raadabadi , M. , Jamebozorgi , M. H. , Salesi , M. , & Ravangard , R. ( 2014 ). Measuring the quality of provided services for patients with chronic kidney disease . Nephro-urology Monthly , 6 ( 5 ), e21810 .
Beaulieu , L. ( 2015 ). How many citations are actually a lot of citations? . Available from: https://lucbeaulieu.com/2015/11/19/how-many-citations-are-actually-a-lot-of-citations/ (accessed on: 11 December 2021) .
Beyan , O. D. , & Baykal , N. ( 2012 ). A knowledge-based search tool for performance measures in health care systems . Journal of Medical Systems , 36 ( 1 ), 201 – 221 .
Boshoff , C. , & Gray , B. ( 2004 ). The relationship between service quality, customer satisfaction and buying intentions in the private hospital industry . South African Journal of Business Management , 35 ( 4 ), 27 – 37 .
Brady , M. K. , & Cronin , J. J. ( 2001 ). Some new thoughts on conceptualizing perceived service quality: A hierarchical approach . Journal of Marketing , 65 , 34 – 49 .
Brown , S. W. , & Swartz , T. A. ( 1989 ). A gap analysis of professional service quality . The Journal of Marketing , 53 ( 2 ), 92 – 98 .
Cameron , A. C. , & Miller , D. L. ( 2015 ). A practitioner’s guide to cluster-robust inference . Journal of Human Resources , 50 ( 2 ), 317 – 372 .
Carini , E. , Gabutti , I. , Frisicale , E. M. , Di Pilla , A. , Pezzullo , A. M. , de Waure , C. , & Specchia , M. L. ( 2020 ). Assessing hospital performance indicators. What dimensions? Evidence from an umbrella review . BMC Health Services Research , 20 ( 1 ), 1 – 13 .
Chahal , H. ( 2008 ). Predicting patient loyalty and service quality relationship: A case study of civil hospital, Ahmedabad, India . Vision , 12 ( 4 ), 45 – 55 .
Chahal , H. , & Kumari , N. ( 2010 ). Development of multidimensional scale for healthcare service quality (HCSQ) in Indian context . Journal of Indian Business Research , 2 ( 4 ), 230 – 255 .
Chahal , H. , & Kumari , N. ( 2012 ). Service quality and performance in the public health-care sector . Health Marketing Quarterly , 29 ( 3 ), 181 – 205 .
Chahal , H. , & Mehta , S. ( 2013 ). Modeling patient satisfaction construct in the Indian health care context . International Journal of Pharmaceutical and Healthcare Marketing , 7 ( 1 ), 75 – 92 .
Chakravarty , A. ( 2011 ). Evaluation of service quality of hospital outpatient department services . Medical Journal Armed Forces India , 67 ( 3 ), 221 – 224 .
Chaudhury , N. , Hammer , J. , Knemer , M. , Muralidharan , K. , & Rogers , F. H. ( 2006 ). Missing in action: Teacher and health worker absence in developing countries . Journal of Economic Perspectives , 20 ( 1 ), 91 – 116 .
Choi , K.-S. , Lee , H. , Kim , C. , & Lee , S. ( 2005 ). The service quality dimensions and patient satisfaction relationships in South Korea: Across gender, age and type of service . Journal of Service Marketing , 19 ( 3 ), 140 – 149 .
Conly , J. , Seto , W. H. , Pittet , D. , Holmes , A. , Chu , M. , & Hunter , P. R. ( 2020 ). Use of medical face masks versus particulate respirators as a component of personal protective equipment for health care workers in the context of the COVID-19 pandemic . Antimicrobial Resistance and Infection Control , 9 ( 1 ), 1 – 7 .
Copnell , B. , Hagger , V. , Wilson , S. G. , Evans , S. M. , Sprivulis , P. C. , & Cameron , P. A. ( 2009 ). Measuring the quality of hospital care: An inventory of indicators . Internal Medicine Journal , 39 ( 6 ), 352 – 360 .
Dagger , T. S. , Sweeney , J. C. , & Johnson , L. W. ( 2007 ). A hierarchical model of health service quality: Scale development and investigation of an integrated model . Journal of Service Research , 10 ( 2 ), 123 – 142 .
De los Santos , J. A. A. , & Labrague , L. J. ( 2021 ). The impact of fear of COVID-19 on job stress, and turnover intentions of frontline nurses in the community: A cross-sectional study in the Philippines . Traumatology , 27 ( 1 ), 52 – 59 .
Dhahri , A. A. , Iqbal , M. R. , & Khan , A. F. A. ( 2020 ). A cross-sectional survey on availability of facilities to healthcare workers in Pakistan during the COVID-19 pandemic . Annals of Medicine and Surgery , 59 , 127 – 130 .
D'Souza , S. C. , & Sequeira , A. H. ( 2011 ). Application of MBNQA for service quality management and performance in healthcare organizations . International Journal of Engineering, Science and Technology , 3 ( 7 ), 73 – 88 .
Engelbrecht , S. ( 2005 ). Motivation and burnout in human service work: The case of midwifery in Denmark: Roskilde university, faculty of psychology . Philosophy and Science Studies .
Fatima , T. , Malik , S. A. , & Shabbir , A. ( 2018 ). Hospital healthcare service quality, patient satisfaction and loyalty: An investigation in context of private healthcare systems . International Journal of Quality and Reliability Management , 35 ( 6 ), 1195 – 1214 .
Gandjour , A. , Kleinschmit , F. , Littmann , V. , & Lauterbach , K. W. ( 2002 ). An evidence-based evaluation of quality and efficiency indicators . Quality Management in Healthcare , 10 ( 4 ), 41 – 52 .
Goshtasebi , A. , Vahdaninia , M. , Gorgipour , R. , Samanpour , A. , Maftoon , F. , Farzadi , F. , & Ahmadi , F. ( 2009 ). Assessing hospital performance by the pabon Lasso model . Iranian Journal of Public Health , 38 ( 2 ), 119 – 124 .
Groene , O. , Skau , J. K. , & Frølich , A. ( 2008 ). An international review of projects on hospital performance assessment . International Journal for Quality in Health Care , 20 ( 3 ), 162 – 171 .
Gupta , K. S. , & Rokade , V. ( 2016 ). Importance of quality in health care sector: A review . Journal of Health Management , 18 ( 1 ), 84 – 94 .
Gustafsson , A. , Johnson , M. D. , & Roos , I. ( 2005 ). The effects of customer satisfaction, relationship commitment dimensions, and triggers on customer retention . Journal of Marketing , 69 ( 4 ), 210 – 218 .
Haque , A. , Sarwar , A. A. I.-M. , Yasmin , F. , & Nuruzzaman , A. A. ( 2012 ). The impact of customer perceived service quality on customer satisfaction for private health centre in Malaysia: A structural equation modeling approach . Information Management and Business Review , 4 ( 5 ), 257 – 267 .
Hasan , H. F. A. , Ilias , A. , Rahman , R. A. , & Razak , M. Z. A. ( 2009 ). Service quality and student satisfaction: A case study at private higher education institutions . International Business Research , 1 ( 3 ), 163 – 175 .
Hegji , C. E. , & Self , D. R. ( 2009 ). The impact of hospital quality on profits, volume, and length of stay . Health Marketing Quarterly , 26 , 209 – 223 .
Herstein , R. , & Gamliel , E. ( 2006 ). The role of private branding in improving service quality . Managing Service Quality , 16 ( 4 ), 306 – 319 .
Herzlinger , R. E. ( 2003 ). Consumer-driven health care: Implications for providers, payers, and policy-makers . Healthplan , 44 ( 6 ), 26 – 29 .
Irfan , S. M. , & Ijaz , A. ( 2011 ). Comparison of service quality between private and public hospitals: Empirical evidences from Pakistan . Journal of Quality and Technology Management , 7 ( 1 ), 1 – 22 .
Israr , M. , Awan , N. , Jan , D. , Ahmad , N. , & Ahmad , S. ( 2016 ). Patients' perception, views and satisfaction with community health center services at mardan district of Khyber Pakhtunkhwa . American Journal of Public Health Research , 4 ( 3 ), 79 – 87 .
Iyengar , S. , & Dholakia , R. H. ( 2012 ). Access of the rural poor to primary healthcare in India . Review of Market Integration , 4 ( 1 ), 71 – 109 .
Jog , S. , Kelkar , D. , Bhat , M. , Patwardhan , S. , Godavarthy , P. , Dhundi , U. , & Bhavsar , R. ( 2020 ). Preparedness of acute care facility and a hospital for COVID-19 pandemic: What we did! . Indian Journal of Critical Care Medicine: Peer-Reviewed, Official Publication of Indian Society of Critical Care Medicine , 24 ( 6 ), 385 .
Kalaja , R. , Myshketa , R. , & Scalera , F. ( 2016 ). Service quality assessment in health care sector: The case of Durres public hospital . Procedia-Social and Behavioral Sciences , 235 , 557 – 565 .
Kamboj , S. , & Rahman , Z. ( 2015 ). Marketing capabilities and firm performance: Literature review and future research agenda . International Journal of Productivity and Performance Management , 64 ( 8 ), 1041 – 1067 .
Karydis , A. , Komboli‐Kodovazeniti , M. , Hatzigeorgiou , D. , & Panis , V. ( 2001 ). Expectations and perceptions of Greek patients regarding the quality of dental health care . International Journal for Quality in Health Care , 13 ( 5 ), 409 – 416 .
Kazemi , N. , Ehsani , P. , Abdi , F. , & Bighami , M. ( 2013 ). Measuring hospital service quality and its influence on patient satisfaction: An empirical study using structural equation modelling . Management Science Letters , 3 ( 7 ), 2125 – 2136 .
Kotler , P. , & Keller , K. ( 2006 ). Marketing management ( 12th ed. ). London : Pearson Education .
Lee , F. ( 2003 ). To build loyalty, hospitals need to exceed customer's expectation . Marketing Health Service , ( Summer ), 33 – 37 .
Levesque , J. F. , & Sutherland , K. ( 2017 ). What role does performance information play in securing improvement in healthcare? A conceptual framework for levers of change . BMJ Open , 7 ( 8 ), 1 – 9 , e014825 .
Levesque , J. F. , & Sutherland , K. ( 2020 ). Combining patient, clinical and system perspectives in assessing performance in healthcare: An integrated measurement framework . BMC Health Services Research , 20 ( 1 ), 1 – 14 .
Li , M. , Lowrie , D. B. , Huang , C. Y. , Lu , X. C. , Zhu , Y. C. , Wu , X. H. … Lu , H. Z. ( 2015 ). Evaluating patients' perception of service quality at hospitals in nine Chinese cities by use of the ServQual scale . Asian Pacific Journal of Tropical Biomedicine , 5 ( 6 ), 497 – 504 .
Lim , J. , Lim , K. , Heinrichs , J. , Al-Aali , K. , Aamir , A. , & Qureshi , M. ( 2018 ). The role of hospital service quality in developing the satisfaction of the patients and hospital performance . Management Science Letters , 8 ( 12 ), 1353 – 1362 .
Liu , J. W. , Lu , S. N. , Chen , S. S. , Yang , K. D. , Lin , M. C. , Wu , C. C. … Chen , C. L. ( 2006 ). Epidemiologic study and containment of a nosocomial outbreak of severe acute respiratory syndrome in a medical center in Kaohsiung, Taiwan . Infection Control and Hospital Epidemiology , 27 ( 5 ), 466 – 472 .
Loiacono , E. T. , Watson , R. T. , & Goodhue , D. L. ( 2007 ). WebQual: An instrument for consumer evaluation of web sites . International Journal of Electronic Commerce , 11 ( 3 ), 51 – 87 .
Mahajan , N. N. , Pednekar , R. , Patil , S. R. , Subramanyam , A. A. , Rathi , S. , Malik , S. … Srivastava , S.A. ( 2020 ). Preparedness, administrative challenges for establishing obstetric services, and experience of delivering over 400 women at a tertiary care COVID‐19 hospital in India . International Journal of Gynecology and Obstetrics , 151 ( 2 ), 188 – 196 .
Manulik , S. , Rosińczuk , J. , & Karniej , P. ( 2016 ). Evaluation of health care service quality in Poland with the use of SERVQUAL method at the specialist ambulatory health care center . Patient Preference and Adherence , 10 , 1435 – 1442 .
Marzban , S. , Najafi , M. , Etedal , M. G. , Moradi , S. , & Rajaee , R. ( 2015 ). The evaluation of outpatient quality services in physiotherapy in the teaching health centers of Shahid Beheshti University based on SERVQUAL tools . European Journal of Biology and Medical Science Research , 3 ( 3 ), 46 – 53 .
McLean , R. , & Antony , J. ( 2014 ). Why continuous improvement initiatives fail in manufacturing environments? A systematic review of the evidence . International Journal of Productivity and Performance Management , 63 ( 3 ), 370 – 376 .
Ministry of Health and Family Welfare (MoHFW) ( 2017 ). National health policy 2017 . Available from: https://main.mohfw.gov.in/documents/policy ( accessed 15 January 2022 ).
Mohammadkarim , B. , Jamil , S. , Pejman , H. , Seyyed , M. H. , & Mostafa , N. ( 2011 ). Combining multiple indicators to assess hospital performance in Iran using the Pabon Lasso Model . The Australasian Medical Journal , 4 ( 4 ), 175 – 179 .
Mosadeghrad , A. M. ( 2014 ). Factors influencing healthcare service quality . International Journal of Health Policy and Management , 3 ( 2 ), 77 – 89 .
Mostafa , M. M. ( 2005 ). An empirical study of patient's expectations and satisfactions in Egyptian hospitals . International Journal of Health Care Quality Assurance , 18 ( 7 ), 516 – 532 .
Murti , A. , Deshpande , A. , & Srivastava , N. ( 2013 ). Service quality, customer (patient) satisfaction and behavioural intention in health care services: Exploring the Indian perspective . Journal of Health Management , 15 ( 1 ), 29 – 44 .
Mustafa , S. S. , Yang , L. , Mortezavi , M. , Vadamalai , K. , & Ramsey , A. ( 2020 ). Patient satisfaction with telemedicine encounters in an allergy and immunology practice during the coronavirus disease 2019 pandemic . Annals of Allergy, Asthma and Immunology , 125 ( 4 ), 478 – 479 .
Nasiripour , A. A. , Kazemi , M. A. A. , & Izadi , A. ( 2012 ). Designing a hospital performance assessment model based on balanced scorecard . HealthMED , 6 ( 9 ), 2983 – 2989 .
Ovretveit , J. ( 2000 ). Total quality management in European healthcare . International Journal of Health Care Quality Assurance , 13 ( 2 ), 74 – 80 .
Ovretveit , J. ( 2009 ). Does improving quality save money? . In A Review of Evidence of Which Improvements to Quality Reduce Costs to Health Service Providers , London : The Health Foundation .
Owusu-Frimpong , N. , Nwankwo , S. , & Dason , B. ( 2010 ). Measuring service quality and patient satisfaction with access to public and private healthcare delivery . International Journal of Public Sector Management , 23 ( 3 ), 203 – 220 .
Pandey , N. , Kaushal , V. , Puri , G. D. , Taneja , S. , Biswal , M. , Mahajan , P. , … Agarwal , R. ( 2020 ). Transforming a general hospital to an infectious disease hospital for COVID-19 over 2 weeks . Frontiers in Public Health , 8 , 1 – 8 .
Parasuraman , A. , Zeithaml , V. A. , & Berry , L. L. ( 1985 ). A conceptual model of service quality and its implications for future study . Journal of Marketing , 49 ( 10 ), 41 – 50 .
Parasuraman , A. , Zeithaml , V. A. , & Berry , L. ( 1988 ). Servqual: A multiple-item scale for measuring consumer perceptions of service quality . Journal of Retailing , 64 ( 1 ), 12 – 40 .
Prajoko , Y. W. , & Supit , T. ( 2020 ). Cancer patient satisfaction and perception of chemotherapy services during COVID-19 pandemic in central Java, Indonesia . Asian Pacific Journal of Cancer Care , 5 ( 1 ), 43 – 50 .
Rameshan , P. , & Singh , S. ( 2004 ). Quality of service of primary health centres: Insights from a field study . Vikalpa , 29 ( 3 ), 71 – 82 .
Ramez , W. S. ( 2012 ). Patients' perception of health care quality, satisfaction and behavioral intention: An empirical study in Bahrain . International Journal of Business and Social Science , 3 ( 18 ), 131 – 141 .
Robb , C. E. , de Jager , C. A. , Ahmadi-Abhari , S. , Giannakopoulou , P. , Udeh-Momoh , C. , McKeand , J. , & Middleton , L. ( 2020 ). Associations of social isolation with anxiety and depression during the early COVID-19 pandemic: A survey of older adults in London, UK . Frontiers in Psychiatry , 11 , 1 – 12 .
Saleh , S. , Alameddine , M. , Mourad , Y. , & Natafgi , N. ( 2015 ). Quality of care in primary health care setting in the eastern mediterranean region: A systematic review of the literature . International Journal for Quality in Health Care , 27 ( 2 ), 79 – 88 .
Senic , V. , & Marinkovic , V. ( 2013 ). Patient care, satisfaction and service quality in health care . International Journal of Consumer Studies , 37 ( 3 ), 312 – 319 .
Shabbir , A. , Malik , S. A. , & Malik , S. A. ( 2016 ). Measuring patients' healthcare service quality perceptions, satisfaction, and loyalty in public and private sector hospitals in Pakistan . International Journal of Quality and Reliability Management , 33 ( 5 ), 538 – 557 .
Sharma , J. K. , & Narang , R. ( 2011 ). Quality of healthcare services in rural India: The user perspective . Vikalpa , 36 ( 1 ), 51 – 60 .
Sharma , A. , Prinja , S. , & Aggarwal , A. K. ( 2019 ). Comprehensive measurement of health system performance at district level in India: Generation of a composite index . The International Journal of Health Planning and Management , 34 ( 4 ), e1783 – e1799 .
Simou , E. , Pliatsika , P. , Koutsogeorgou , E. , & Roumeliotou , A. ( 2014 ). Developing a national framework of quality indicators for public hospitals . The International Journal of Health Planning and Management , 29 ( 3 ), e187 – e206 .
Singh , A. , & Prasher , A. ( 2019 ). Measuring healthcare service quality from patients' perspective: Using fuzzy AHP application . Total Quality Management and Business Excellence , 30 ( 3-4 ), 284 – 300 .
Sohail , M. S. ( 2003 ). Service quality in hospitals: More favourable than you might think . Managing Service Quality , 13 ( 3 ), 197 – 206 .
Taner , T. , & Antony , J. ( 2006 ). Comparing public and private hospital care service quality in Turkey . Leadership in Health Services , 19 ( 2 ), 1 – 10 .
Taqi , M. , Bidhuri , S. , Sarkar , S. , Ahmad , W. S. , & Wangchok , P. ( 2017 ). Rural healthcare infrastructural disparities in India: A critical analysis of availability and accessibility . Journal of Multidisciplinary Research in Healthcare , 3 ( 2 ), 125 – 149 .
Tashobya , C. K. , da Silveira , V. C. , Ssengooba , F. , Nabyonga-Orem , J. , Macq , J. , & Criel , B. ( 2014 ). Health systems performance assessment in low-income countries: Learning from international experiences . Globalization and Health , 10 ( 1 ), 1 – 19 .
Taylor , G. ( 2012 ). Readability of OHS documents–A comparison of surface characteristics of OHS text between some languages . Safety Science , 50 ( 7 ), 1627 – 1635 .
Thompson , C. C. , Shen , L. , & Lee , L. S. ( 2020 ). COVID-19 in endoscopy: Time to do more? Gastrointestinal Endoscopy , 92 ( 2 ), 435 – 439 .
Torabipour , A. , Sayaf , R. , Salehi , R. , & Ghasemzadeh , R. ( 2016 ). Analyzing the quality Gapsin the services of rehabilitation centers using the SERVQUAL technique in Ahvaz, Iran . Jundishapur Journal of Health Sciences , 8 ( 1 ), 25 – 30 .
Tucker , J. L. III. , & Adams , S. R. ( 2001 ). Incorporating patient's assessment of satisfaction and quality: An integrative model of patient's evaluations of their care . Managing Service Quality , 11 ( 4 ), 272 – 286 .
Upadhyai , R. , Jain , A. K. , Roy , H. , & Pant , V. ( 2019 ). A review of healthcare service quality dimensions and their measurement . Journal of Health Management , 21 ( 1 ), 102 – 127 .
Wiesniewski , M. , & Wiesniewski , H. ( 2005 ). Measuring service in a hospital colposcopy clinic . International Journal of Health Care Quality Assurance , 18 ( 3 ), 217 – 228 .
Wu , H. Y. , Lin , Y. K. , & Chang , C. H. ( 2011 ). Performance evaluation of extension education centres in universities based on the balanced scorecard . Evaluation and Program Planning , 34 ( 1 ), 37 – 50 .
Wu , H. C. , Li , T. , & Li , M. Y. ( 2016 ). A study of behavioral intentions, patient satisfaction, perceived value, patient trust and experiential quality for medical tourists . Journal of Quality Assurance in Hospitality and Tourism , 17 ( 2 ), 114 – 150 .
Wu , B. , Xiao , H. , Dong , X. , Wang , M. , & Xue , L. ( 2012 ). Tourism knowledge domains: A keyword analysis . Asia Pacific Journal of Tourism Research , 17 ( 4 ), 355 – 380 .
Yee , R. W. , Yeung , A. C. , & Cheng , T. E. ( 2010 ). An empirical study of employee loyalty, service quality and firm performance in the service industry . International Journal of Production Economics , 124 ( 1 ), 109 – 120 .
Yeşilada , F. , & Direktör , E. ( 2010 ). Health care service quality: A comparison of public and private hospitals . African Journal of Business Management , 4 ( 6 ), 962 – 971 .
Zaid , A. A. , Arqawi , S. M. , Mwais , R. M. A. , Al Shobaki , M. J. , & Abu-Naser , S. S. ( 2020 ). The impact of total quality management and perceived service quality on patient satisfaction and behavior intention in Palestinian healthcare organizations . Technology Reports of Kansai University , 62 ( 03 ), 221 – 232 .
Zarei , A. , Arab , M. , Froushani , A. R. , Rashidian , A. , & Ghazi-Tabatabaei , S. M. ( 2012 ). Service quality of private hospitals: The Iranian Patients' perspective . BMC Health Services Research , 12 ( 31 ), 66 – 76 .
Zarei , E. , Daneshkohan , A. , Khabiri , R. , & Arab , M. ( 2015 ). The effect of hospital service quality on patient's trust . Iranian Red Crescent Medical Journal , 17 ( 1 ), 1 – 5 .
Zeithaml , V. A. ( 2000 ). Service quality, profitability, and the economic worth of customers: what we know and what we need to learn . Journal of the Academy of Marketing Science , 28 ( 1 ), 67 – 85 .
Zineldin , M. ( 2006 ). The quality of health care and patient satisfaction: An exploratory investigation of the 5Qs model at some Egyptian and Jordanian medical clinics . International Journal of Health Care Quality Assurance , 19 , 60 – 92 .
Corresponding author
About the authors.
Related articles
We’re listening — tell us what you think, something didn’t work….
Report bugs here
All feedback is valuable
Please share your general feedback
Join us on our journey
Platform update page.
Visit emeraldpublishing.com/platformupdate to discover the latest news and updates
Questions & More Information
Answers to the most commonly asked questions here
Log in using your username and password
- Search More Search for this keyword Advanced search
- Latest content
- Current issue
- BMJ Journals More You are viewing from: Google Indexer
You are here
- Volume 33, Issue 5
- Equitable and accessible informed healthcare consent process for people with intellectual disability: a systematic literature review
- Article Text
- Article info
- Citation Tools
- Rapid Responses
- Article metrics
- http://orcid.org/0000-0002-8498-7329 Manjekah Dunn 1 , 2 ,
- Iva Strnadová 3 , 4 , 5 ,
- Jackie Leach Scully 4 ,
- Jennifer Hansen 3 ,
- Julie Loblinzk 3 , 5 ,
- Skie Sarfaraz 5 ,
- Chloe Molnar 1 ,
- Elizabeth Emma Palmer 1 , 2
- 1 Faculty of Medicine & Health , University of New South Wales , Sydney , New South Wales , Australia
- 2 The Sydney Children's Hospitals Network , Sydney , New South Wales , Australia
- 3 School of Education , University of New South Wales , Sydney , New South Wales , Australia
- 4 Disability Innovation Institute , University of New South Wales , Sydney , New South Wales , Australia
- 5 Self Advocacy Sydney , Sydney , New South Wales , Australia
- Correspondence to Dr Manjekah Dunn, Paediatrics & Child Health, University of New South Wales Medicine & Health, Sydney, New South Wales, Australia; manjekah.dunn{at}unsw.edu.au
Objective To identify factors acting as barriers or enablers to the process of healthcare consent for people with intellectual disability and to understand how to make this process equitable and accessible.
Data sources Databases: Embase, MEDLINE, PsychINFO, PubMed, SCOPUS, Web of Science and CINAHL. Additional articles were obtained from an ancestral search and hand-searching three journals.
Eligibility criteria Peer-reviewed original research about the consent process for healthcare interventions, published after 1990, involving adult participants with intellectual disability.
Synthesis of results Inductive thematic analysis was used to identify factors affecting informed consent. The findings were reviewed by co-researchers with intellectual disability to ensure they reflected lived experiences, and an easy read summary was created.
Results Twenty-three studies were included (1999 to 2020), with a mix of qualitative (n=14), quantitative (n=6) and mixed-methods (n=3) studies. Participant numbers ranged from 9 to 604 people (median 21) and included people with intellectual disability, health professionals, carers and support people, and others working with people with intellectual disability. Six themes were identified: (1) health professionals’ attitudes and lack of education, (2) inadequate accessible health information, (3) involvement of support people, (4) systemic constraints, (5) person-centred informed consent and (6) effective communication between health professionals and patients. Themes were barriers (themes 1, 2 and 4), enablers (themes 5 and 6) or both (theme 3).
Conclusions Multiple reasons contribute to poor consent practices for people with intellectual disability in current health systems. Recommendations include addressing health professionals’ attitudes and lack of education in informed consent with clinician training, the co-production of accessible information resources and further inclusive research into informed consent for people with intellectual disability.
PROSPERO registration CRD42021290548.
- Decision making
- Healthcare quality improvement
- Patient-centred care
- Quality improvement
- Standards of care
Data availability statement
Data are available upon reasonable request. Additional data and materials such as data collection forms, data extraction and analysis templates and QualSyst assessment data can be obtained by contacting the corresponding author.
This is an open access article distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited, appropriate credit is given, any changes made indicated, and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/ .
https://doi.org/10.1136/bmjqs-2023-016113
Statistics from Altmetric.com
Request permissions.
If you wish to reuse any or all of this article please use the link below which will take you to the Copyright Clearance Center’s RightsLink service. You will be able to get a quick price and instant permission to reuse the content in many different ways.
What is already known on this topic
People with intellectual disability are frequently excluded from decision-making processes and not provided equal opportunity for informed consent, despite protections outlined in the United Nations Convention on the Rights of Persons with Disabilities.
People with intellectual disability have the capacity and desire to make informed medical decisions, which can improve their well-being, health satisfaction and health outcomes.
What this review study adds
Health professionals lack adequate training in valid informed consent and making reasonable adjustments for people with intellectual disability, and continue to perpetuate assumptions of incapacity.
Health information provided to people with intellectual disability is often inaccessible and insufficient for them to make informed decisions about healthcare.
The role of support people, systemic constraints, a person-centred approach and ineffective healthcare communication also affect informed consent.
How this review might affect research, practice or policy
Health professionals need additional training on how to provide a valid informed consent process for people with intellectual disability, specifically in using accessible health information, making reasonable adjustments (e.g., longer/multiple appointments, options of a support person attending or not, using plain English), involving the individual in discussions, and communicating effectively with them.
Inclusive research is needed to hear the voices and opinions of people with intellectual disability about healthcare decision-making and about informed consent practices in specific healthcare settings.
Introduction
Approximately 1% of the world’s population have intellectual disability. 1 Intellectual disability is medically defined as a group of neurodevelopmental conditions beginning in childhood, with below average cognitive functioning and adaptive behaviour, including limitations in conceptual, social and practical skills. 2 People with intellectual disability prefer an alternative strength-based definition, reflected in the comment by Robert Strike OAM (Order of Australia Medal): ‘We can learn if the way of teaching matches how the person learns’, 3 reinforcing the importance of providing information tailored to the needs of a person with intellectual disability. A diagnosis of intellectual disability is associated with significant disparities in health outcomes. 4–7 Person-centred decision-making and better communication have been shown to improve patient satisfaction, 8 9 the physician–patient relationship 10 and overall health outcomes 11 for the wider population. Ensuring people with intellectual disability experience informed decision-making and accessible healthcare can help address the ongoing health disparities and facilitate equal access to healthcare.
Bodily autonomy is an individual’s power and agency to make decisions about their own body. 12 Informed consent for healthcare enables a person to practice bodily autonomy and is protected, for example, by the National Safety and Quality Health Service Standards (Australia), 13 Mental Capacity Act (UK) 14 and the Joint Commission Standards (USA). 15 In this article, we define informed consent according to three requirements: (1) the person is provided with information they understand, (2) the decision is free of coercion and (3) the person must have capacity. 16 For informed consent to be valid, this process must be suited to the individual’s needs so that they can understand and communicate effectively. Capacity is the ability to give informed consent for a medical intervention, 17 18 and the Mental Capacity Act outlines that ‘a person must be assumed to have capacity unless it is established that he lacks capacity’ and that incapacity can only be established if ‘all practicable steps’ to support capacity have been attempted without success. 14 These assumptions of capacity are also decision-specific, meaning an individual’s ability to consent can change depending on the situation, the choice itself and other factors. 17
Systemic issues with healthcare delivery systems have resulted in access barriers for people with intellectual disability, 19 despite the disability discrimination legislation in many countries who are signatories to the United Nations (UN) Convention on the Rights of Persons with Disabilities. 20 Patients with intellectual disability are not provided the reasonable adjustments that would enable them to give informed consent for medical procedures or interventions, 21 22 despite evidence that many people with intellectual disability have both the capacity and the desire to make their own healthcare decisions. 21 23
To support people with intellectual disability to make independent health decisions, an equitable and accessible informed consent process is needed. 24 However, current health systems have consistently failed to provide this. 21 25 To address this gap, we must first understand the factors that contribute to inequitable and inaccessible consent. To the best of our knowledge, the only current review of informed consent for people with intellectual disability is an integrative review by Goldsmith et al . 26 Many of the included articles focused on assessment of capacity 27–29 and research consent. 30–32 The review’s conclusion supported the functional approach to assess capacity, with minimal focus on how the informed consent processes can be improved. More recently, there has been a move towards ensuring that the consent process is accessible for all individuals, including elderly patients 33 and people with aphasia. 34 However, there remains a paucity of literature about the informed consent process for people with intellectual disability, with no systematic reviews summarising the factors influencing the healthcare consent process for people with intellectual disability.
To identify barriers to and enablers of the informed healthcare consent process for people with intellectual disability, and to understand how this can be made equitable and accessible.
A systematic literature review was conducted following the Preferred Reporting Items for Systematic Reviews and Meta-Analysis Protocols (PRISMA-P) systematic literature review protocol. 35 The PRISMA 2020 checklist 36 and ENhancing Transparency in REporting the synthesis of Qualitative research (ENTREQ) reporting guidelines were also followed. 37 The full study protocol is included in online supplemental appendix 1 .
Supplemental material
No patients or members of the public were involved in this research for this manuscript.
Search strategy
A search strategy was developed to identify articles about intellectual disability, consent and healthcare interventions, described in online supplemental appendix 2 . Multiple databases were searched for articles published between January 1990 to January 2022 (Embase, MEDLINE, PsychINFO, PubMed, SCOPUS, Web of Science and CINAHL). These databases include healthcare and psychology databases that best capture relevant literature on this topic, including medical, nursing, social sciences and bioethical literature. The search was limited to studies published from 1990 as understandings of consent have changed since then. 38 39 This yielded 4853 unique papers which were imported into Covidence, a specialised programme for conducting systematic reviews. 40
Study selection
Citation screening by abstract and titles was completed by two independent researchers (MD and EEP). Included articles had to:
Examine the informed consent process for a healthcare intervention for people with intellectual disability.
Have collected more than 50% of its data from relevant stakeholders, including adults with intellectual disability, families or carers of a person with intellectual disability, and professionals who engage with people with intellectual disability.
Report empirical data from primary research methodology.
Be published in a peer-reviewed journal after January 1990.
Be available in English.
Full text screening was completed by two independent researchers (MD and EEP). Articles were excluded if consent was only briefly discussed or if it focused on consent for research, capacity assessment, or participant knowledge or comprehension. Any conflicts were resolved through discussion with an independent third researcher (IS).
Additional studies were identified through an ancestral search and by hand-searching three major journals relevant to intellectual disability research. Journals were selected if they had published more than one included article for this review or in previous literature reviews conducted by the research team.
Quality assessment
Two independent researchers (MD and IS) assessed study quality with the QualSyst tool, 41 which can assess both qualitative and quantitative research papers. After evaluating the distribution of scores, a threshold value of 55% was used, as suggested by QualSyst 41 to exclude poor-quality studies but capture enough studies overall. Any conflicts between the quality assessment scores were resolved by a third researcher (EEP). For mixed-method studies, both qualitative and quantitative quality scores were calculated, and the higher value used.
Data collection
Two independent researchers (MD and JH) reviewed each study and extracted relevant details, including study size, participant demographics, year, country of publication, study design, data analysis and major outcomes reported. Researchers used standardised data collection forms designed, with input from senior researchers with expertise in qualitative research (IS and EEP), to extract data relevant to the review’s research aims. The form was piloted on one study, and a second iteration made based on feedback. These forms captured data on study design, methods, participants, any factors affecting the process of informed consent and study limitations. Data included descriptions and paragraphs outlining key findings, the healthcare context, verbatim participant quotes and any quantitative analyses or statistics. Missing or unclear data were noted.
Data analysis
A pilot literature search showed significant heterogeneity in methodology of studies, limiting the applicability of traditional quantitative analysis (ie, meta-analysis). Instead, inductive thematic analysis was chosen as an alternative methodology 42 43 that has been used in recent systematic reviews examining barriers and enablers of other health processes. 44 45 The six-phase approach described by Braun and Clarke was used. 46 47 A researcher (MD) independently coded the extracted data of each study line-by-line, with subsequent data grouped into pre-existing codes or new concepts when necessary. Codes were reviewed iteratively and grouped into categories, subthemes and themes framed around the research question. Another independent researcher (JH) collated and analysed the data on study demographics, methods and limitations. The themes were reviewed by two senior researchers (EEP and IS).
Qualitative methods of effect size calculations have been described in the literature, 48 49 which was captured in this review by the number of studies that identified each subtheme, with an assigned frequency rating to compare their relative significance. Subthemes were given a frequency rating of A, B, C or D if they were identified by >10, 7–9, 4–6 or <3 articles, respectively. The overall significance of each theme was estimated by the number of studies that mentioned it and the GRADE framework, a stepwise approach to quality assessment using a four-tier rating system. Each study was evaluated for risk of bias, inconsistency, indirectness, imprecision and publication bias. 50 51 Study sensitivity was assessed by counting the number of distinct subthemes included. 52 The quality of findings was designated high, moderate or low depending on the frequency ratings, the QualSyst score and the GRADE scores of studies supporting the finding. Finally, the relative contributions of each study were evaluated by the number of subthemes described, guided by previously reported methods for qualitative reviews. 52
Co-research
The findings were reviewed by two co-researchers with intellectual disability (JL and SS), with over 30 years combined experience as members and employees of a self-advocacy organisation. Guidance on the findings and an easy read summary was produced in line with best-practice inclusive research 53 54 over multiple discussions. Input from two health professional researchers (MD and EEP) provided data triangulation and sense-checking of findings.
Twenty-three articles were identified ( figure 1 ): 14 qualitative, 6 quantitative and 3 mixed-methods. Two papers included the same population of study participants: McCarthy 55 and McCarthy, 56 but had different research questions. Fovargue et al 57 was excluded due to a quality score of 35%. Common quality limitations were a lack of verification procedures to establish credibility and limited researcher reflexivity. No studies were excluded due to language requirements (as all were in English) or age restrictions (all studies had majority adult participants).
- Download figure
- Open in new tab
- Download powerpoint
PRISMA 2020 flowchart for the systematic review. 36
Studies were published from 1999 to 2020 and involved participant populations from the UK (n=18), USA (n=3), Sweden (n=1) and Ireland (n=1). Participant numbers ranged from 9 to 604 (median 21), and participants included people with intellectual disability (n=817), health professionals (n=272), carers and support people (n=48), and other professionals that work with people with intellectual disability (n=137, community service agency directors, social workers, administrative staff and care home staff). Ages of participants ranged from 8 to 84 years, though only Aman et al 58 included participants <18 years of age. This study was included as the article states very few children were included. Studies examined consent in different contexts, including contraception and sexual health (6/23 articles), 58–60 medications (5/23 articles), 58–62 emergency healthcare, 63 cervical screening, 64 community referrals, 58–61 65 mental health, 66 hydrotherapy, 64 blood collection 67 and broad decision-making consent without a specific context. 65 68–71 A detailed breakdown of each study is included in online supplemental appendix 3 .
Six major themes were identified from the studies, summarised in figure 2 . An overview of included studies showing study sensitivity, effect size, QualSyst and GRADE scores is given in online supplemental appendix 4 . Studies with higher QualSyst and GRADE scores contributed more to this review’s findings and tended to include more subthemes; specifically, Rogers et al , 66 Sowney and Barr, 63 Höglund and Larsson, 72 and McCarthy 55 and McCarthy. 56 Figure 3 gives the easy read version of theme 1, with the full easy read summary in online supplemental appendix 5 .
Summary of the identified six themes and subthemes.
Theme 1 of the easy read summary.
Theme 1—Health professionals’ attitudes and lack of education about informed consent
Health professionals’ attitudes and practices were frequently (18/21) identified as factors affecting the informed consent process, with substantial evidence supporting this theme. Studies noted the lack of training for health professionals in supporting informed consent for people with intellectual disability, their desire for further education, and stereotypes and discrimination perpetuated by health professionals.
Lack of health professional education on informed consent and disability discrimination legislation
Multiple studies reported inconsistent informed consent practices, for various reasons: some reported that health professionals ‘forgot’ to or ‘did not realise consent was necessary’, 63 73 but inconsistent consent practices were also attributed to healthcare providers’ unfamiliarity with consent guidelines and poor education on this topic. Carlson et al 73 reported that only 44% of general practitioners (GPs) were aware of consent guidelines, and there was the misconception that consent was unnecessary for people with intellectual disability. Similarly, studies of psychologists 66 and nurses 63 found that many were unfamiliar with their obligations to obtain consent, despite the existence of anti-discrimination legislation. People with intellectual disability describe feeling discriminated against by health professionals, reflected in comments such as ‘I can tell, my doctor just thinks I’m stupid – I'm nothing to him’. 74 Poor consent practices by health professionals were observed in Goldsmith et al , 67 while health professionals surveyed by McCarthy 56 were unaware of their responsibility to provide accessible health information to women with intellectual disability. Improving health professional education and training was suggested by multiple studies as a way to remove this barrier. 63 65–67 69 73

Lack of training on best practices for health professions caring for people with intellectual disability
A lack of training in caring for and communicating with people with intellectual disability was also described by midwives, 72 psychologists, 66 nurses, 63 pharmacists 61 and GPs. 56 72 75 Health professionals lacked knowledge about best practice approaches to providing equitable healthcare consent processes through reasonable adjustments such as accessible health information, 56 60 66 longer appointments times, 60 72 simple English 62 67 and flexible approaches to patient needs. 63 72
Health professionals’ stereotyping and assumptions of incapacity
Underlying stereotypes contributed to some health professionals’ (including nurses, 63 GPs 56 and physiotherapists 64 ) belief that people with intellectual disability lack capacity and therefore, do not require opportunities for informed consent. 56 64 In a survey of professionals referring people with intellectual disability to a disability service, the second most common reason for not obtaining consent was ‘patient unable to understand’. 73
Proxy consent as an inappropriate alternative
People with intellectual disability are rarely the final decision-maker in their medical choices, with many health providers seeking proxy consent from carers, support workers and family members, despite its legal invalidity. In McCarthy’s study (2010), 18/23 women with intellectual disability said the decision to start contraception was made by someone else. Many GPs appeared unaware that proxy consent is invalid in the UK. 56 Similar reports came from people with intellectual disability, 55 56 60 64 69 76 health professionals (nurses, doctors, allied health, psychologists), 56 63 64 66 77 support people 64 77 and non-medical professionals, 65 73 and capacity was rarely documented. 56 62 77
Exclusion of people with intellectual disability from decision-making discussions
Studies described instances where health professionals made decisions for their patients with intellectual disability or coerced patients into a choice. 55 72 74 76 77 In Ledger et al 77 , only 62% of women with intellectual disability were involved in the discussion about contraception, and only 38% made the final decision, and others stated in Wiseman and Ferrie 74 : ‘I was not given the opportunity to explore the different options. I was told what one I should take’. Three papers outlined instances where the choices of people with intellectual disability were ignored despite possessing capacity 65 66 69 and when a procedure continued despite them withdrawing consent. 69
Theme 2—Inadequate accessible health information
Lack of accessible health information.
The lack of accessible health information was the most frequently identified subtheme (16/23 studies). Some studies reported that health professionals provided information to carers instead, 60 avoided providing easy read information due to concerns about ‘offending’ patients 75 or only provided verbal information. 56 67 Informed consent was supported when health professionals recognised the importance of providing medical information 64 and when it was provided in an accessible format. 60 Alternative approaches to health information were explored, including virtual reality 68 and in-person education sessions, 59 with varying results. Overall, the need to provide information in different formats tailored to an individual’s communication needs, rather than a ‘one size fits all’ approach, was emphasised by both people with intellectual disability 60 and health professionals. 66
Insufficient information provided
Studies described situations where insufficient information was provided to people with intellectual disability to make informed decisions. For example, some people felt the information from their GP was often too basic to be helpful (Fish et al 60 ) and wanted additional information on consent forms (Rose et al 78 ).
Theme 3—The involvement of support people
Support people (including carers, family members and group home staff) were identified in 11 articles as both enablers of and barriers to informed consent. The antagonistic nature of these findings and lower frequency of subthemes are reflected in the lower quality assessments of evidence.
Support people facilitated communication with health professionals
Some studies reported carers bridging communication barriers with health to support informed consent. 63 64 McCarthy 56 found 21/23 of women with intellectual disability preferred to see doctors with a support person due to perceived benefits: ‘Sometimes I don’t understand it, so they have to explain it to my carer, so they can explain it to me easier’. Most GPs in this study (93%) also agreed that support people aided communication.
Support people helped people with intellectual disability make decisions
By advocating for people with intellectual disability, carers encouraged decision-making, 64 74 provided health information, 74 77 emotional support 76 and assisted with reading or remembering health information. 55 58 76 Some people with intellectual disability explicitly appreciated their support person’s involvement, 60 such as in McCarthy’s 55 study where 18/23 participants felt supported and safer when a support person was involved.
Support people impeded individual autonomy
The study by Wiseman and Ferrie 74 found that while younger participants with intellectual disability felt family members empowered their decision-making, older women felt family members impaired their ability to give informed consent. This was reflected in interviews with carers who questioned the capacity of the person with intellectual disability they supported and stated they would guide them to pick the ‘best choice’ or even over-ride their choices. 64 Studies of psychologists and community service directors described instances where the decision of family or carers was prioritised over the wishes of the person with intellectual disability. 65 66 Some women with intellectual disability in McCarthy’s studies (2010, 2009) 55 56 appeared to have been coerced into using contraception by parental pressures or fear of losing group home support.
Theme 4—Systemic constraints within healthcare systems
Time restraints affect informed consent and accessible healthcare.
Resource limitations create time constraints that impair the consent process and have been identified as a barrier by psychologists, 66 GPs, 56 hospital nurses 63 and community disability workers. 73 Rogers et al 66 highlighted that a personalised approach that could improve informed decision-making is restricted by inflexible medical models. Only two studies described flexible patient-centred approaches to consent. 60 72 A survey of primary care practices in 2007 reported that most did not modify their cervical screening information for patients with intellectual disability because it was not practical. 75
Inflexible models of consent
Both people with intellectual disability 76 and health professionals 66 recognised that consent is traditionally obtained through one-off interactions prior to an intervention. Yet, for people with intellectual disability, consent should ideally be an ongoing process that begins before an appointment and continues between subsequent ones. Other studies have tended to describe one-off interactions where decision-making was not revisited at subsequent appointments. 56 60 72 76
Lack of systemic supports
In one survey, self-advocates highlighted a lack of information on medication for people with intellectual disability and suggested a telephone helpline and a centralised source of information to support consent. 60 Health professionals also want greater systemic support, such as a health professional specialised in intellectual disability care to support other staff, 72 or a pharmacist specifically to help patients with intellectual disability. 61 Studies highlighted a lack of guidelines about healthcare needs of people with intellectual disabilities such as contraceptive counselling 72 or primary care. 75
Theme 5—Person-centred informed consent
Ten studies identified factors related to a person-centred approach to informed consent, grouped below into three subthemes. Health professionals should tailor their practice when obtaining informed consent from people with intellectual disability by considering how these subthemes relate to the individual. Each subtheme was described five times in the literature with a relative frequency rating of ‘C’, contributing to overall lower quality scores.
Previous experience with decision-making
Arscott et al 71 found that the ability of people with intellectual disability to consent changed with their verbal and memory skills and in different clinical vignettes, supporting the view of ‘functional’ capacity specific to the context of the medical decision. Although previous experiences with decision-making did not influence informed consent in this paper, other studies suggest that people with intellectual disability accustomed to independent decision-making were more able to make informed medical decisions, 66 70 and those who live independently were more likely to make independent healthcare decisions. 56 Health professionals should be aware that their patients with intellectual disability will have variable experience with decision-making and provide individualised support to meet their needs.
Variable awareness about healthcare rights
Consent processes should be tailored to the health literacy of patients, including emphasising available choices and the option to refuse treatment. In some studies, medical decisions were not presented to people with intellectual disability as a choice, 64 and people with intellectual disability were not informed of their legal right to accessible health information. 56
Power differences and acquiescence
Acquiescence by people with intellectual disability due to common and repeated experiences of trauma—that is, their tendency to agree with suggestions made by carers and health professionals, often to avoid upsetting others—was identified as an ongoing barrier. In McCarthy’s (2009) interviews with women with intellectual disability, some participants implicitly rejected the idea that they might make their own healthcare decisions: ‘They’re the carers, they have responsibility for me’. Others appeared to have made decisions to appease their carers: ‘I have the jab (contraceptive injection) so I can’t be blamed for getting pregnant’. 55 Two studies highlighted that health professionals need to be mindful of power imbalances when discussing consent with people with intellectual disability to ensure the choices are truly autonomous. 61 66
Theme 6—Effective communication between health professionals and patients
Implementation of reasonable adjustments for verbal and written information.
Simple language was always preferred by people with intellectual disability. 60 67 Other communication aids used in decision-making included repetition, short sentences, models, pictures and easy read brochures. 72 Another reasonable adjustment is providing the opportunity to ask questions, which women with intellectual disability in McCarthy’s (2009) study reported did not occur. 55
Tailored communication methods including non-verbal communication
Midwives noted that continuity of care allows them to develop rapport and understand the communication preferences of people with intellectual disability. 72 This is not always possible; for emergency nurses, the lack of background information about patients with intellectual disability made it challenging to understand their communication preferences. 63 The use of non-verbal communication, such as body language, was noted as underutilised 62 66 and people with intellectual disability supported the use of hearing loops, braille and sign language. 60
To the best of our knowledge, this is the first systematic review investigating the barriers and enablers of the informed consent process for healthcare procedures for people with intellectual disability. The integrative review by Goldsmith et al 26 examined capacity assessment and shares only three articles with this systematic review. 69 71 73 Since the 2000s, there has been a paradigm shift in which capacity is no longer considered a fixed ability that only some individuals possess 38 39 but instead as ‘functional’: a flexible ability that changes over time and in different contexts, 79 reflected in Goldsmith’s review. An individual’s capacity can be supported through various measures, including how information is communicated and how the decision-making process is approached. 18 80 By recognising the barriers and enablers identified in this review, physicians can help ensure the consent process for their patients with intellectual disability is both valid and truly informed. This review has highlighted the problems of inaccessible health information, insufficient clinical education on how to make reasonable adjustments and lack of person-centred trauma-informed care.
Recommendations
Health professionals require training in the informed consent process for people with intellectual disability, particularly in effective and respectful communication, reasonable adjustments and trauma-informed care. Reasonable adjustments include offering longer or multiple appointments, using accessible resources (such as easy read information or shared decision-making tools) and allowing patient choices (such as to record a consultation or involve a support person). Co-researchers reported that many people with intellectual disability prefer to go without a support person because they find it difficult to challenge their decisions and feel ignored if the health professional only talks to the support person. People with intellectual disability also feel they cannot seek second opinions before making medical decisions or feel pressured to provide consent, raising the possibility of coercion. These experiences contribute to healthcare trauma. Co-researchers raised the importance of building rapport with the person with intellectual disability and of making reasonable adjustments, such as actively advocating for the person’s autonomy, clearly stating all options including the choice to refuse treatment, providing opportunities to contribute to discussions and multiple appointments to ask questions and understand information. They felt that without these efforts to support consent, health professionals can reinforce traumatic healthcare experiences for people with intellectual disability. Co-researchers noted instances where choices were made by doctors without discussion and where they were only given a choice after requesting one and expressed concern that these barriers are greater for those with higher support needs.
Co-researchers showed how these experiences contributed to mistrust of health professionals and poorer health outcomes. In one situation, a co-researcher was not informed of a medication’s withdrawal effects, resulting in significant side-effects when it was ceased. Many people with intellectual disability describe a poor relationship with their health professionals, finding it difficult to trust health information provided due to previous traumatic experiences of disrespect, coercion, lack of choice and inadequate support. Many feel they cannot speak up due to the power imbalance and fear of retaliation. Poor consent practices and lack of reasonable adjustments directly harm therapeutic alliances by reducing trust, contribute to healthcare trauma and lead to poorer health outcomes for people with intellectual disability.
Additional education and training for health professionals is urgently needed in the areas of informed consent, reasonable adjustments and effective communication with people with intellectual disability. The experiences of health professionals within the research team confirmed that there is limited training in providing high-quality healthcare for people with intellectual disability, including reasonable adjustments and accessible health information. Co-researchers also suggested that education should be provided to carers and support people to help them better advocate for people with intellectual disability.
Health information should be provided in a multimodal format, including written easy read information. Many countries have regulation protecting the right to accessible health information and communication support to make an informed choice, such as UK’s Accessible Information Standard, 81 and Australia’s Charter of Health Care Rights, 24 yet these are rarely observed. Steps to facilitate this include routinely asking patients about information requirements, system alerts for an individual’s needs or routinely providing reasonable adjustments. 82 Co-researchers agreed that there is a lack of accessible health information, particularly about medications, and that diagrams and illustrations are underutilised. There is a critical need for more inclusive and accessible resources to help health professionals support informed consent in a safe and high-quality health system. These resources should be created through methods of inclusive research, such as co-production, actively involving people with intellectual disability in the planning, creation, and feedback process. 53
Strengths and limitations
This systematic review involved two co-researchers with intellectual disability in sense-checking findings and co-creating the easy read summary. Two co-authors who are health professionals provided additional sense-checking of findings from a different stakeholder perspective. In future research, this could be extended by involving people with intellectual disability in the design and planning of the study as per recommendations for best-practice inclusive research. 53 83
The current literature is limited by low use of inclusive research practices in research involving people with intellectual disability, increasing vulnerability to external biases (eg, inaccessible questionnaires, involvement of carers in data collection, overcompliance or acquiescence and absence of researcher reflexivity). Advisory groups or co-research with people with intellectual disability were only used in five studies. 58 60 68 74 76 Other limitations include unclear selection criteria, low sample sizes, missing data, using gatekeepers in patient selection and predominance of UK-based studies—increasing the risk of bias and reducing transferability. Nine studies (out of 15 involving people with intellectual disability) explicitly excluded those with severe or profound intellectual disability, reflecting a selection bias; only one study specifically focused on people with intellectual disability with higher support needs. Studies were limited to a few healthcare contexts, with a focus on consent about sexual health, contraception and medications.
The heterogeneity and qualitative nature of studies made it challenging to apply traditional meta-analysis. However, to promote consistency in qualitative research, the PRISMA and ENTREQ guidelines were followed. 36 37 Although no meta-analyses occurred, the duplication of study populations in McCarthy 2009 and 2010 likely contributed to increased significance of findings reported in both studies. Most included studies (13/23) were published over 10 years ago, reducing the current relevance of this review’s findings. Nonetheless, the major findings reflect underlying systemic issues within the health system, which are unlikely to have been resolved since the articles were published, as the just-released final report of the Australian Royal Commission into Violence, Abuse, Neglect and Exploitation of People with Disability highlights. 84 There is an urgent need for more inclusive studies to explore the recommendations and preferences of people with intellectual disability about healthcare choices.
Informed consent processes for people with intellectual disability should include accessible information and reasonable adjustments, be tailored to individuals’ needs and comply with consent and disability legislation. Resources, guidelines and healthcare education are needed and should cover how to involve carers and support people, address systemic healthcare problems, promote a person-centred approach and ensure effective communication. These resources and future research must use principles of inclusive co-production—involving people with intellectual disability at all stages. Additionally, research is needed on people with higher support needs and in specific contexts where informed consent is vital but under-researched, such as cancer screening, palliative care, prenatal and newborn screening, surgical procedures, genetic medicine and advanced therapeutics such as gene-based therapies.
Ethics statements
Patient consent for publication.
Not applicable.
Ethics approval
- Maulik PK ,
- Mascarenhas MN ,
- Mathers CD , et al
- World Health Organisation
- Council for Intellectual Disability
- Emerson E ,
- Shogren KA ,
- Wehmeyer ML ,
- Reese RM , et al
- Cordasco KM
- Hallock JL ,
- Jordens CFC ,
- McGrath C , et al
- Brenner LH ,
- Brenner AT ,
- United Nations Population Fund
- Australian Commission on Safety and Quality in Health Care
- The Joint Commission
- Beauchamp TL ,
- Childress JF
- New South Wales Attorney General
- United Nations General Assembly
- Strnadová I ,
- Loblinzk J ,
- Scully JL , et al
- MacPhail C ,
- McKay K , et al
- Keywood K ,
- Fovargue S ,
- Goldsmith L ,
- Skirton H ,
- Cash J , et al
- Morris CD ,
- Niederbuhl JM ,
- Arscott K ,
- Fisher CB ,
- Davidson PW , et al
- Giampieri M
- Shamseer L ,
- Clarke M , et al
- McKenzie JE ,
- Bossuyt PM , et al
- Flemming K ,
- McInnes E , et al
- Appelbaum PS
- ↵ Covidence systematic review software . Melbourne, Australia ,
- Proudfoot K
- Papadopoulos I ,
- Koulouglioti C ,
- Lazzarino R , et al
- Onwuegbuzie AJ
- BMJ Best Practice
- Guyatt GH ,
- Vist GE , et al
- Garcia-Lee B
- Brimblecombe J , et al
- Benson BA ,
- Farmer CA , et al
- Ferguson L ,
- Graham YNH ,
- Gerrard D ,
- Laight S , et al
- Huneke NTM ,
- Halder N , et al
- Ferguson M ,
- Jarrett D ,
- McGuire BE , et al
- Woodward V ,
- Jackson L , et al
- Conboy-Hill S ,
- Leafman J ,
- Nehrenz GM , et al
- Höglund B ,
- Carlson T ,
- English S , et al
- Wiseman P ,
- Walmsley J ,
- Tilley E , et al
- Khatkar HS , et al
- Holland AJ , et al
- Beauchamp TL
- England National Health Service
- National Health Service England
- Royal Commission into Violence, Abuse, Neglect and Exploitation of People with Disability
Supplementary materials
Supplementary data.
This web only file has been produced by the BMJ Publishing Group from an electronic file supplied by the author(s) and has not been edited for content.
- Data supplement 1
- Data supplement 2
- Data supplement 3
- Data supplement 4
- Data supplement 5
Contributors MD, EEP and IS conceived the idea for the systematic review. MD drafted the search strategy which was refined by EEP and IS. MD and EEP completed article screening. MD and IS completed quality assessments of included articles. MD and JH completed data extraction. MD drafted the original manuscript. JL and SS were co-researchers who sense-checked findings and were consulted to formulate dissemination plans. JL and SS co-produced the easy read summary with MD, CM, JH, EEP and IS. MD, JLS, EEP and IS reviewed manuscript wording. All authors critically reviewed the manuscript and approved it for publication. The corresponding author attests that all listed authors meet authorship criteria and that no others meeting the criteria have been omitted. MD is the guarantor responsible for the overall content of this manuscript.
Funding This systematic literature review was funded by the National Health & Medical Research Council (NHMRC), Targeted Call for Research (TCR) into Improving health of people with intellectual disability. Research grant title "GeneEQUAL: equitable and accessible genomic healthcare for people with intellectual disability". NHMRC application ID: 2022/GNT2015753.
Competing interests None declared.
Provenance and peer review Not commissioned; externally peer reviewed.
Supplemental material This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Linked Articles
- Editorial It is up to healthcare professionals to talk to us in a way that we can understand: informed consent processes in people with an intellectual disability Jonathon Ding Richard Keagan-Bull Irene Tuffrey-Wijne BMJ Quality & Safety 2024; 33 277-279 Published Online First: 30 Jan 2024. doi: 10.1136/bmjqs-2023-016830
Read the full text or download the PDF:
- Open access
- Published: 22 April 2024
Let the records speak: an exploration of rehabilitation services offered in primary healthcare, Johannesburg metropolitan district
- Lebogang Maseko ORCID: orcid.org/0000-0002-6126-5104 1 ,
- Fasloen Adams ORCID: orcid.org/0000-0001-6742-3727 2 &
- Hellen Myezwa ORCID: orcid.org/0000-0003-4562-6413 3
BMC Health Services Research volume 24 , Article number: 501 ( 2024 ) Cite this article
87 Accesses
Metrics details
Primary healthcare in South Africa aims to transform the national health system by emphasising community-based care and preventive strategies. However, rehabilitation services, particularly for individuals with disabilities and chronic non-communicable diseases, are often overlooked in primary healthcare. This study aimed to investigate the provision of primary healthcare rehabilitation services in the Johannesburg Metropolitan District by exploring client sociodemographics and variations in services provided by rehabilitation professionals.
A retrospective review of clinic rehabilitation records from 2011 to 2020 was conducted at nine provincially funded community health centres (CHCs) offering rehabilitation services. Stratified sampling facilitated record selection based on rehabilitation service type and year. A specifically designed data extraction tool captured demographics, disabilities, rehabilitation received, and referral sources. Descriptive analysis used means, standard deviations, and frequencies.
The findings show a diverse client population with a wide age range, with a significant proportion falling into the < 5 years and 30–49 years age groups. Neuromusculoskeletal and movement-related disabilities were most prevalent, affecting approximately two-thirds of clients. Referral sources were often undocumented, and inconsistent discharge information with no record of patient follow up, highlighted the need for improved documentation practices. Clinic visits were the primary service delivery mode, followed by limited home visits and outreach services. Occupational therapy and physiotherapy were the most used services. Speech and language therapy services were underused, and some CHCs lacked audiology services. There were variations in the number of individual and group sessions provided by the different rehabilitation services, and there were age- and disability-specific differences in service use.
This study offers insights into rehabilitation service provision in the Johannesburg Metropolitan District and enhances our understanding of rehabilitation services in primary healthcare settings. It underscores the importance of a multidisciplinary rehabilitation team to address diverse rehabilitation needs, improving documentation and discharge practices, expanding service delivery models, and reducing disparities in service use. The findings inform strategies for optimising service delivery, workforce, resource allocation, and intersectoral collaboration to ultimately enhance the quality and accessibility of integrated rehabilitation services.
Peer Review reports
International studies consistently show that increased investment in a broad range of rehabilitation services yields substantial health, social, and economic benefits [ 1 ]. Ensuring the provision of rehabilitation services to the entire population is considered a crucial aspect of achieving universal health coverage (UHC) [ 2 ]. The rehabilitation services contribute to community participation and wellbeing by improving capacity, functioning, and modifying the environment of people suffering from a wide range of health conditions [ 3 ]. Moreover, the provision of services using a primary healthcare (PHC) approach for optimal health, is achieved through meeting people’s health needs and preferences as close as possible to their everyday environment. This encompasses a range of healthcare activities, along the continuum of health care including promotion, prevention, treatment, rehabilitation, and palliative care. The PHC approach has been shown to reduce hospital admissions, healthcare costs, and promote community development [ 4 ].
There is international recognition of the importance of rehabilitation in health systems supporting first-contact and providing accessible, continued, comprehensive and coordinated patient-focused primary health care. However, the integration of rehabilitation services into health systems has progressed slowly in low- and middle-income countries [ 5 ]. A mere 25% of countries in the West Pacific region of the World Health Organisation (WHO) have sustainable PC rehabilitation services [ 6 ]. Fragmented healthcare and inadequate integration of rehabilitation into comprehensive health services are also reported in Iran and Nigeria in the African region [ 7 , 8 ]. Consequently, individuals with disabilities, the ageing population, and those burdened with chronic communicable and non-communicable diseases face inadequate access to rehabilitation services at PC level [ 5 ]. Recognising the need for solutions and practical guidance on integrating rehabilitation in PHC is highlighted by the WHO in their Rehabilitation 2030 initiative [ 9 ], and the Astana declaration on PHC and rehabilitation [ 10 ].
The Joint Learning Network for Universal Health Coverage emphasises the significance of raising awareness, capacity-building, and providing adequate data about services [ 11 ]. This action is supported, in the context of the WHO vision for primary care which also recognises the importance of functioning as a third health indicator [ 2 ]. Therefore, the data collected for our study incorporated the concept of function defined by the body functioning domains of the International Classification of Functioning, Disability and Health (ICF) [ 12 ].
In South Africa, PHC plays a pivotal role in the healthcare system as proposed by government policies, including the White Paper for the Transformation of the Health System [ 13 ] and the National Health Act of 2003 [ 14 ], which underscore the significance of the PHC approach as the cornerstone of the country’s healthcare transformation. Although the commitment to the PHC approach is reinforced by the National Health Insurance (NHI) Bill of July 2019, adopted in November 2023 [ 15 ], the current recognition of PC in South Africa is predominantly rooted in a medical model philosophy. The medical model emphasises nurse-driven services with support from doctors, pharmacists, and dentists, while rehabilitation services and person-centred care are not adequately encompassed or prioritised [ 16 , 17 ]. Efforts to address deficiencies in PHC facilities in South Africa are outlined in the ‘Ideal Clinic’ programme. However, the programme does not explicitly address the staffing or resource allocation for rehabilitation services, apart from a general acknowledgment of the significance of providing access to rehabilitation services for patients [ 18 , 19 ]..
The provision of multidisciplinary rehabilitation depends on the availability of skilled personnel, and these professions include occupational therapy, physiotherapy, physical and rehabilitation medicine, prosthetics and orthotics, psychology, social work and speech and language therapy [ 20 ]. In South Africa, PC rehabilitation services are only offered by rehabilitation professionals such as occupational therapists, physiotherapist, speech and language therapist and audiologists as professionally designated by the Health Professionals Council of South Africa (HPCSA). The rehabilitation services are far from optimal in that they are mainly hospital based with little consideration of broad multi-, inter-and trans- disciplinary teams [ 21 ] that can contribute to health care in conjunction with those registered as allied health services [ 22 ]. Other health professionals in shortage at the primary care level include nurses, psychologists, prosthetists and orthotists, social workers, and doctors. Therefore, the implementation of intersectoral rehabilitation services in PHC facilities remains limited in South Africa with less than a quarter of facilities currently providing such services [ 23 , 24 ].
In contrast, PHC rehabilitation research in high-income countries indicates that occupational therapy, physiotherapy and speech and language therapy services are well established. Studies show that these services primarily focus on chronic disease, self-management and improving physical functioning, which is often supplemented with online support for clients [ 25 ]. In Sweden, PC physiotherapists predominantly provide physical activity programmes to middle-aged and older adults with conditions such as musculoskeletal disorders, obesity, hypertension, and diabetes [ 26 ]. Occupational therapists practicing in PC settings in Norway report that over 80% of their clients are adults and 44% are old age pensioners. The study reported that the conditions treated by occupational therapists included neurological diseases, particularly stroke, as well as musculoskeletal and mental illnesses, which accounted for 13–20% of referrals. Notably, 96% of clients presented with movement impairments, and 94% of them experience challenges in activities and participation related to education, work, and leisure [ 27 ]. In the UK, the duration of physiotherapy intervention and referral patterns in PC indicate that services may be offered for less than a month. However, most clients receive supportive treatment over a two-year period, with many referrals originating from triage at the clinic reception or through self-referral [ 28 ]. A Norwegian study indicates physiotherapy services for smaller numbers of children in PHC clinics where most clients present with motor development impairments and lower limb orthopaedic diagnoses [ 27 ]. Additionally, clients with prematurity and heart or lung disease also receive PC rehabilitation services [ 29 ].
In low to middle income countries such as Brazil, referrals for speech and language therapy PC services are mainly for children. They treat learning disorders, poor language development, Attention Deficit Hyperactivity Disorder, stuttering, mutism, and hearing issues [ 30 ]. A study from Indonesia noted a higher percentage of patients with neurological conditions receiving treatment [ 31 ]. A study conducted in South Africa highlights that clients who receive physiotherapy services at PHC clinics most commonly present with back pain, stroke, and upper and lower limb injuries [ 32 ]. However, despite this information, there is a critical lack of supporting evidence in South Africa regarding the use of rehabilitation services at a PC level and the extent to which they are integrated into PHC [ 24 ].
In South Africa sociodemographic data concerning the individuals who use PC rehabilitation services, the specific rehabilitation professionals who provide these services, and the services provided are scarce. The WHO Rehabilitation Programme [ 33 ] acknowledges the importance of gathering information on existing services and the sociodemographic information of the people accessing these services to inform the development of comprehensive rehabilitation interventions at both national and sub-national levels to effectively meet the individual needs of diverse populations and boost rehabilitation planning efforts [ 24 , 33 ].
Therefore, the objective of the current study was to investigate the extent and nature of rehabilitation services provided in the Johannesburg Metropolitan District. The study specifically focussed on examining the structure, accessibility, delivery, and use of these services to address this knowledge gap.
A retrospective review of clinic rehabilitation records was conducted in an urban setting to investigate the rehabilitation services provided between 2011 and 2020. The research setting was the Johannesburg Metropolitan District, which encompasses 125 PC clinics and CHCs across seven regions, serving a population of 5.5 million [ 34 ]. Of the 5.5 million, 2.35 million have a monthly income that falls below the upper limit poverty line of ZAR 1227 (estimated $61) per person [ 35 ]. Only nine of the 125 PC clinics and CHCs in the Johannesburg Metropolitan District are managed by the provincial rather than municipal health services. These nine facilities provide rehabilitation services and were selected for our study. The rehabilitation services encompass individual and group outpatient therapy, community reintegration as a focus, outreach and home visits, as well as education and awareness campaigns facilitated by multidisciplinary teams [ 36 ].
Stratified sampling was used to select rehabilitation service paper-based records according to the only rehabilitation service providers employed at the clinics: occupational therapists, physiotherapists, speech and language therapists and audiologists. Within each discipline, further stratification was performed based on the year of the records available. The sample size was determined using Cochran’s formula [ 37 ], setting a 95% confidence level and a 5% margin of error. There were 238 740 records spanning a 9-year period, and therefore, a review of at least 540 records was deemed necessary. Although the period 2011–2020 was initially identified for the record review, not all facilities had rehabilitation service user records for those years because of varying record storage practices. Therefore, the sampling included client rehabilitation paper-based records for the years available at each facility ranging from 2011 to 2020, inclusively. A random sample was extracted from the records stratified for each rehabilitation service and year from the available records at each facility to fulfil the required sample size.
Data extraction was done using a data extraction tool designed and piloted by the first author in Microsoft Excel. The tool facilitated the collection of various data points, including sociodemographic information such as age and disability related to impairment, which was classified using the classification of the ICF based on body functioning domains [ 12 ]. Additionally, data regarding the referral source and nature and duration of received rehabilitation and of services provided by rehabilitation discipline, were extracted. Permission to conduct the study was obtained from the Gauteng Department of Health and the Human Research Ethics Committee (Medical) of the Faculty of Health Sciences at the University of the Witwatersrand (M190466). Descriptive analysis was used to analyse the collected data using means, standard deviations, and frequencies to describe the profile of the service users and the characteristics of the rehabilitation services they received.
A total of 630 paper-based records were reviewed. The number of records extracted varied across the clinics due to the differences in the availability of records; Lenasia Clinic had the highest availability (13.5%) of records, and the Hillbrow CHC had the lowest (7.0%) (Table 1 ).
Sociodemographic profile of clients
The analysis of client sociodemographics revealed that the mean age at the time of assessment was 32 years (SD = 35.2) and ranged from 0 to 102 years. Most clients fell into the age groups < 5 years (22.9%) and 30–49 years (24.1%). Older participants constituted only 11% of the sample (Table 2 ).
Disability related to impairments (ICF body function)
Regarding affected functioning categorized by the WHO ICF domains of body function, neuromusculoskeletal and movement-related functions (b7) were the most common and occurred in approximately two-thirds of clients (66.2%), followed by mental function impairments (b1) (15.6%).
However, only 4.4% of clients were recorded as having multiple impairments although most clients had multiple functioning domains affected (Table 3 ).
Rehabilitation services received
Source of referral.
Clients were referred to the PC facility from various sources. However, the referral source for most clients (61.4%) was not recorded. Among the recorded source of referrals, most were down referrals from secondary and tertiary hospitals. Referrals from other sources include NGOs, private doctors, and other services at the PC level (Table 4 ).
Reasons for discontinued therapy
Discharge information was inadequately reported in the records, but most clients were lost to follow-up (64.1%), and 15.1% were referred elsewhere. (Table 5 ).
Number and types of visits for all rehabilitation services
Clinic visits, where clients attend outpatient rehabilitation services, accounted for the largest number of visits, ranging from one to six or more, with most clients only seen once (48.7%). Six home visits to clients, and eight outreach visits were recorded where clients were at school or a community group. (Table 6 ).
Rehabilitation services received and frequency of sessions
Occupational therapy and physiotherapy were the most frequently provided rehabilitation services across the nine facilities at more than 40%, while audiology had the lowest use (7.1%). It is important to note that many clients attended multiple therapies (Table 7 ).
Individual and group sessions received
The records indicated that most clients received at least one individual or group session from specific rehabilitation services (ranging from 87 to 100%). The mean number of individual sessions varied across services, with occupational therapy and speech and language therapy averaging 2.5 sessions and audiology averaging 1.7 sessions. The number of individual sessions ranged from 1 to 13 for occupational therapy, 1 to 12 for physiotherapy and speech and language therapy, and 1 to 6 for audiology (Table 8 ).
Rehabilitation provided per clinic
No significant difference was found between occupational therapy and physiotherapy services across the nine clinics. However, speech and language therapy was provided to less than 20% of total clients at only four of the nine CHCs. Four CHCs did not offer audiology services (Table 9 ).
Rehabilitation received per discipline by disability related to body function
The analysis of client demographics and disabilities in relation to rehabilitation services revealed that clients with mental function disabilities were predominantly seen by occupational therapists. Physiotherapists primarily worked with clients with movement-related dysfunction while speech and language therapists treated those with voice and speech impairments associated with neuromusculoskeletal disabilities.
As expected, audiologists saw a higher proportion of clients with sensory function and pain-related disabilities (Table 10 ).
Rehabilitation received per discipline by age at assessment
A significant difference was observed in the percentage of clients seen in different age groups across all four rehabilitation services. A significantly greater percentage of younger age groups, including children and adolescents, received occupational therapy and speech and language therapy, while young, middle, and older adults received services from physiotherapy and audiology services (Table 11 ).
The review of client records across the nine PC facilities providing rehabilitation services in the Johannesburg Metropolitan District revealed the sociodemographic profile of clients accessing rehabilitation services, and indicated a wide age range, with a mean age of 32 years. The high proportion of clients in the < 5 years and 30–49 years age groups suggests that rehabilitation services are used by both children and adults within the district, while the older adults constituted a smaller portion of the sample. The wide age range of rehabilitation service users is encouraging, thus rehabilitation PC services should be available across the life course of service users, along the continuum of care, and reflective of all types of care required in the healthcare system in trying to achieve UHC [ 4 ]. The age distribution is different to trends in Europe and the UK where most clients are older adults [ 27 , 28 , 29 ]. The age distribution aligns with the diverse population demographics of the Johannesburg Metropolitan District [ 38 ] where, services for children under the age of 5 years and the older adults are free of charge in South African clinics, which may contribute to the observed age distribution.
Both the Department of Education and the Department of Health share responsibilities for children over the age of six, with the Department of Education specifically accountable for learning and developmental interventions [ 39 ]. Furthermore, the high proportion of children under 5 years is aligned with population-based data that shows that the proportion of children with disabilities in low- and middle-income countries is high [ 40 , 41 ]. It would further explain the high proportion of paediatric neuromusculoskeletal, and movement-related functions (b7) seen in the CHCs in this study. The records reviewed in our study indicate that over 33% of clients receiving services were children and adolescents, compared to 20% reported in a high income country such as Norway [ 27 ]. The findings are congruent with the South African statistics indicating nearly 30% of the population is under the age of 15 years [ 42 ].
Thus, services must be configured to optimise outcomes for clients across different life stages according to the specific national context to ensure that age-specific rehabilitation needs are adequately addressed in the planning and delivery of services.
Among the clients accessing rehabilitation services, neuromusculoskeletal and movement-related functions were the most prevalent disabilities, followed by mental function (b1) disabilities. These findings are consistent with global trends, emphasising the high prevalence of musculoskeletal and neurological conditions and the importance of addressing mental health within rehabilitation services [ 26 , 43 , 44 ]. This aligns with international studies where physiotherapists and occupational therapists treating adults confirmed they most frequently provide interventions for clients with these conditions using a PHC approach [ 45 ]. Mental health, which is rarely mentioned in relation to PC rehabilitation, can be considered in two categories, namely individuals with mental health conditions as a diagnosis, and those with physical impairments who experience associated mental health concerns [ 2 ]. The presence of multiple impairments in a subset of clients further highlights the complexities present in rehabilitation service users and underscores the need for comprehensive and interdisciplinary approaches to rehabilitation [ 46 , 47 , 48 ] that excel in a wide range of generalist competencies rather than specialised or narrow competencies.
Our study indicated poor recording of the referral sources for most clients which represents a substantial data gap. It hinders the understanding and formalising of the referral pathways through which clients access rehabilitation services and impedes efforts to improve coordination and continuity of care required to provide integrated rehabilitation services in PHC [ 49 ]. Enhancing data collection practices to capture this information uniformly and accurately would provide valuable insights into care coordination and identify potential areas for intervention. The prevalence of hospital down referrals suggests that collaboration between PC facilities and higher-level healthcare institutions is essential in facilitating access to rehabilitation services [ 49 ]. It could be, however, that overstretched hospital based services may account for an influx of patients referred to PC rehabilitation services who still require acute in-hospital care, but are down-referred due to high patient numbers in hospitals and increased demand for in-patient beds [ 50 ].
Discharge information was inadequately reported in the records, with most clients being lost to follow-up. While hospitals are identified as the primary source of down referrals, the absence of documented discharge information at the PC level raises concerns regarding the extent of collaborative referrals and feedback on referrals, particularly for clients with complex diseases. This finding highlights a gap in record-keeping practices and long-term follow-up of clients. It emphasises the need for strategies to improve accessible record keeping, post-rehabilitation support, and long-term management in PC. Understanding the reasons for discharge and lack of treatment continuity is essential. Ways to enhance patient engagement and adherence to rehabilitation programmes are essential for achieving optimal outcomes and should be explored[ 51 ]. Addressing accessible and comprehensive record keeping and long-term follow-up is important for evaluating the effectiveness of interventions and providing appropriate support to clients throughout their rehabilitation journey.
Clinic visits were found to be the most common mode of service delivery, with limited home visits and outreach visits to NGOs. This suggests that the current focus of rehabilitation services primarily revolves around clinic-based care, with limited attention given to delivering services in clients’ homes, care institutions or reaching out to underserved communities [ 52 ]. The literature highlights alternative models of care, such as community-based rehabilitation and the use of community health workers in areas with limited access to PC rehabilitation services [ 53 ]. Expanding service delivery beyond PHC clinic settings through outreach services and home-based rehabilitation programmes could enhance accessibility for vulnerable populations and ensure a more comprehensive approach to rehabilitation. Although tele-rehabilitation may be an option this is impacted by high data costs and lack of constant electricity supply in South Africa [ 54 ].
Increasing investment in rehabilitation is important for expanding the workforce and capacity in South Africa. The investment includes funding human resources for primary care rehabilitation services. Such services should be integrated into multidisciplinary ward-based outreach teams located in primary care facilities. These teams would provide a range of services—outreach, preventive, promotive, curative, rehabilitative, and palliative—to individuals, groups, and communities. Additionally, fostering partnerships between government and NGOs is essential to enhance these efforts. [ 55 , 56 ]. Moreover, alternative service delivery models have the potential to improve the reach and effectiveness of rehabilitation services and enhance their integration into PHC. Community-based rehabilitation with an emphasis on community participation and empowerment has been shown to improve health outcomes [ 53 ]. Trained community health workers can serve as liaisons between the healthcare system and the community by building trust and establishing open communication channels between rehabilitation providers and users [ 57 ].
The frequency of clinic visits and the number of group sessions also varied slightly between the different rehabilitation services, with a small percentage of clients receiving six to 13 individual sessions or more than five group sessions. This is a concern considering the chronic nature of some conditions receiving intervention at clinics. Research in the UK indicates that most PC physiotherapy clients are seen for at least two years for initial rehabilitative and later supportive care [ 28 ]. The poor records, loss to follow-up with limited resources in the clinics, and clients experiencing barriers in terms of transport and finances to access clinics may play a role in the shorter intervention periods and fewer sessions of rehabilitation [ 58 ].
The Gauteng Health Strategic Plan 2019/2021–2024/25 highlights the insufficient number of audiologists available to assess patients with chronic illnesses and provide universal hearing diagnostic services for babies as a gap in planning of adequate rehabilitation services, technologies and required hearing devices [ 39 ]. It is concerning, yet unsurprising, that audiologists primarily provide services to older adults. A study by Swanepoel et al., which used mobile phone diagnosis for children in the community in South Africa, found a low referral rate of 24.9% for further assessment in preschool children [ 59 ]. Additionally, a low follow-up return rate of 39.4% was discovered, primarily due to extended waiting periods before follow-up appointments at PHC clinics. The effective implementation of ear and hearing services at the PHC level requires careful planning, clear programme goals, and defined care pathways [ 60 ]. It is important to explore strategies, such as including audiology services into the School Health Programme of the reengineered PHC approach, to enhance the provision of audiology services and increase awareness of their importance. Given the shortage of available services at a limited number of clinics and a national shortage of rehabilitation personnel, especially at PC level a task-sharing approach for a limited set of basic interventions should also be considered to improve access [ 61 ].
The number of individual sessions varied across the rehabilitation services, with occupational therapy and speech and language therapy having higher average session numbers compared to physiotherapy and audiology. These variations may reflect differences in treatment protocols, severity of conditions, complexity of the functional outcome or resource allocation. Further research is needed to determine the optimal frequency and duration of rehabilitation sessions to maximise outcomes and patient satisfaction. This research would also inform the packages of care to be funded under the NHI in South Africa.
The findings highlight significant differences in the distribution of rehabilitation services across impairments and age groups [ 62 ]. Our study provides an indication of differences in PC rehabilitation services in an urban South African context, considering five rehabilitation services rather than focusing on a single service. This information is valuable for planning rehabilitation services based on disability needs and age-specific patterns. Tailoring rehabilitation services to the unique requirements of people with different disabilities and age groups has the potential to enhance their effectiveness and relevance within UHC provision [ 2 ].
An important limitation impacting PC in South Africa is the lack of planning and monitoring, which is essential to inform further development of rehabilitation. The inability to monitor rehabilitation services is due in part to the absence of national agreed minimum data sets for rehabilitation services as well as rehabilitation records and health records in South Africa not being in electronic format. Indeed, the WHO emphasises the functionality of shared electronic health records linked to other health facilities and services to support two-way referrals, multidisciplinary teamwork, and continuity of treatment along clinical pathways [ 2 ]. In the current study, the record review was compounded by the variations in record availability and storage among the CHCs and rehabilitation services. Some of the CHCs store their records at a central storage facility while others keep them on-site. The cause of these differences is unknown, but it could be due to a lack of clear record-management policy and storage guidelines, as well as insufficient implementation or resources by rehabilitation professionals to implement existing guidelines. According to the HPCSA, records should be specific, include important information, and should be stored for a minimum of six years from the date of the patient’s last treatment by a healthcare practitioner [ 63 ], but the life cycle [ 64 ]for other medical records varies for hospitals, health funders and different categories of patients. These discrepancies in record-keeping practicesunderscore the need for a consistent and standardised single record-keeping system across PHC facilities [ 56 ]. Additionally, the fact that each rehabilitation service is required to maintain separate records, even during combined sessions for financial and legal/litigation purposes, suggests a lack of integration and siloed service delivery, which affects integration and multidisciplinary teamwork.
Given that the CHCs included in the study serve densely populated and overcrowded townships, where 95% of the population resides, it is crucial to implement integrated and coordinated approaches to rehabilitation service record keeping to ensure continuity of care and integrated service delivery [ 38 ].
Strengthening the Routine Health Information System for rehabilitation in the country is needed to allow for regular, easy accessibility and analysis of -real time data compared with population needs, -user profile data, -referral practices and -completion of rehabilitation episodes. This monitoring is essential to plan and evaluate rehabilitation to appreciate the impact of improvement and outcomes [ 65 ].
While our study provides valuable insights into the provision of rehabilitation services in the Johannesburg Metropolitan District, it is important to acknowledge some limitations. The retrospective nature of the study and its reliance on the accessibility and accuracy of CHC records may have introduced bias. Moreover, the study’s focus on provided services overlooks those that are not provided and the reasons behind it. Additionally, the study focussed on the nine CHCs offering rehabilitation services, and the findings may not be generalisable to other regions or healthcare settings. Future research should address these limitations and further explore the identified gaps in rehabilitation services to inform policy and practice in a broader context.
The results from our study outline data available on the rehabilitation services in PHC clinics in the Johannesburg Metropolitan District. The analysis of clinical rehabilitation records from nine provincially funded CHCs between 2011 and 2020 revealed valuable insights into the demographics of clients, types of disabilities, referral sources, service use, and variations in rehabilitation services across the nine CHCs. The findings underscore the diverse rehabilitation needs across different age groups and disabilities and the differences in services offered by different rehabilitation disciplines. Rehabilitation services should be tailored to meet the needs of individuals with a diverse age range, from children to older adults. This includes ensuring services are reflective of all types of care required at different life stages. Missing data revealed the need to improve documentation practices, enhance coordination between healthcare facilities, and expand service delivery models. Future research should explore the alignment of the South African PHC approach with the WHO Package of interventions for rehabilitation [ 66 ], the effectiveness of rehabilitation interventions, the impact on patient outcomes, and the factors influencing service provision and access, including the lacking healthcare professions. Strategies to improve the provision and awareness of audiology services should be implemented, especially in the context of the School Health Programme and other community-based initiatives. By addressing these issues, we can strive towards delivering inclusive, person-centred, and integrated rehabilitation services that maximise independence, functioning, and quality of life for individuals in need. Further research using qualitative and mixed method studies are recommended as well as research to develop an agreed minimum rehabilitation dataset for rehabilitation services at the PC level.
Data availability
The data that support the findings of this study are available from the corresponding author, LM, upon reasonable request.
Abbreviations
- Community health centres
non-governmental organisations
national health insurance
primary care
primary healthcare
Universal Health Coverage
United Kingdom
World Health Organization
Stucki G, Bickenbach J, Gutenbrunner C, Melvin J. Rehabilitation: The health strategy of the 21st century. J Rehabil Med [Internet]. 2017 Jan 31 [cited 2018 Mar 18];50(4):1–8. Accessed 2020. https://pubmed.ncbi.nlm.nih.gov/28140419/
World Health Organization, United Nations Children’s Fund. A vision for Primary health care in the 21st Century [Internet]. World Health Organizarion. Geneva, Switzerland. 2018. Accessed June 2022. https://www.who.int/docs/default-source/primary-health/vision.pdf
Gutenbrunner C, Nugraha B. Rehabilitation as a Health Strategy. J Int Soc Phys Rehabil Med. 2019;2(June):15.
Article Google Scholar
World Health Organization. Rehabilitation in Health Systems: Guide for Action [Internet]. Geneva, Switzerland. 2019. Accessed March 2021. https://www.who.int/publications-detail-redirect/9789241515986
Bickenbach J, Cieza A, Kleinitz P, Marks E, Mills J-A. Access to rehabilitation in primary health care: an ongoing challenge. Tech Ser Prim Heal Care [Internet]. 2018;1–27. Accessed May 2021. https://www.who.int/publications-detail-redirect/WHO-HIS-SDS-2018.40
WHO. Rehabilitation and disability in the Western Pacific. World Health Organization. Manila, Philippines: World Health Organization Western Pacific Region; 2017.
Google Scholar
Shahabi S, Kiekens C, Etemadi M, Mojgani P, Teymourlouei AA. Integrating rehabilitation services into primary health care: policy options for Iran. 2022;1–12.
Atulomah NO, Health A, Remo I. Integrating Medical Rehabilitation Services in Community and Primary Health Care in Nigeria and Sub- Sahara Africa. In: Maiden International Conference of Medical Rehabilitation Professionals. 2017. pp. 1–8.
World Health Organization. Rehabilitation 2030: A Call for Action Meeting Report. 2017. pp. 1–3.
World Health Organization; UNICEF. Declaration of Astanap.8–9. Declaration of Astana. Glob Conf Prim Heal Care [Internet]. 2018;2893–4. Accessed September 2020. https://www.who.int/publications-detail-redirect/WHO-HIS-SDS-2018.61
Joint Learning Network. Can rehabilitation be integrated into primary health care? [Internet]. 2023. Accessed October 2023. https://jointlearningnetwork.org/can-rehabilitation-be-integrated-into-primary-health-care/
World Health Organization. International Classification of Functioning, Disability and Health [Internet]. 2001. Accessed November 2018. https://www.who.int/standards/classifications/international-classification-of-functioning-disability-and-health
National Department of Health. White Paper for the transformation of the health system in South Africa: Towards a National Health System. 1997 p. 1–140.
National Department of Health SA. National Health Act 61 of 2003: Emergency Medical Services Regulations [Internet]. Government Gazette. 2017. Accessed April 2021. https://www.gov.za/sites/default/files/gcis_document/202102/44161gon94.pdf
Republic of South Africa. National Health Insurance Bill. 2019. p. 1–60. https://www.gov.za/sites/default/files/gcis_document/201908/national-health-insurance-bill-b-11-2019.pdf
Kautzky K, Tollman SM. A Perspective on Primary Health Care in South Africa [Internet]. South African Health Review. 2008. Accessed August 2018. https://www.hst.org.za/publications/South%20African%20Health%20Reviews/2%20A%20Perspective%20on%20Primary%20Health%20Care%20in%20South%20Africa%20SAHR%202008.pdf
Africa L, Frantz J, Mlenzana N. Analysis of a primary healthcare facility for the development of an interprofessional intervention: a logical framework approach. South Afr J Public Heal. 2022;5(3):77–85.
National Department of Health. Ideal ClinicManual. Version. 2017;17:1–348.
National Department of Health. Framework and strategy for disability and rehabilitation services in South Africa 2015–2020. Republic of South Africa. 2015. pp. 3–25.
World Health Organisation. Rehabilitation in Health Systems [Internet]. 2017. 92 p. Accessed January 2019. https://www.who.int/publications-detail-redirect/9789241515986
Van Bewer V. Transdisciplinarity in Health Care: a Concept Analysis. Nurs Forum. 2017;52(4).
Health Professions Council of South Africa. Professional boards [Internet]. 2024. Accessed January 2023. https://www.hpcsa.co.za/?contentId=0&menuSubId=47&actionName=Professional%20Boards
Louw Q, Grimme K, Berner K, Conradie T, Bedada D, Jesus T. Towards a needs-based design of the physical rehabilitation workforce in South Africa: trend analysis [1990–2017] and a 5-year forecasting for the most impactful health conditions based on global burden of disease estimates. BMC Public Health. 2021;13(21):913.
Morris LD, Grimmer KA, Twizeyemariya A, Coetzee M, Leibbrandt DC, Louw QA. Health system challenges affecting rehabilitation services in South Africa. Disabil Rehabil. 2021;43(6):877–83.
Article PubMed Google Scholar
Richardson J, Letts L, Chan D, Officer A, Wojkowski S, Oliver D, et al. Monitoring physical functioning as the sixth vital sign: evaluating patient and practice engagement in chronic illness care in a primary care setting - A quasi-experimental design. BMC Fam Pract. 2012;13:1–13.
Leijon M, Bendtsen P, Nilsen P, Ekberg K. Physical activity referrals in Swedish primary health care– prescriber and patient characteristics, reasons for prescriptions. BMC Health Serv Res. 2008;8(1):1–9.
Aas RW, Grotle M. Clients using community occupational therapy services: Sociodemographic factors and the occurrence of diseases and disabilities. Scand J Occup Ther. 2007;14(3):150–9.
Halls S, Thomas R, Stott H, Cupples ME, Kersten P, Cramp F, et al. Provision of first contact physiotherapy in primary care across the UK: a survey of the service. Physiotherapy. 2020;108:2–9.
Evensen KAI, Robinson HS, Meisingset I, Woodhouse A, Thielemann M, Bjorbækmo WS et al. Characteristics, course and outcome of patients receiving physiotherapy in primary health care in Norway: design of a longitudinal observational project. 2018;1–10.
Guckert SB, de Souza CR, Arakawa-Belaunde AM. The role of speech-language therapists in primary healthcare from the perspective of professionals in family health support centers. Codas. 2020;32(5):1–8.
Manik JW, Wardhani K, Putri A, Bernardito J, Wiranata A, YatiWulang A, et al. Direct Access Physiotherapy Service Model in Primary Health Care Facility: an observational study. Int J Med Exerc Sci. 2022;8(1):1210–8.
Kloppers M, Pretorius B, Vlok ED. Clients’ subjective experience of their participation in rehabilitation at an out-patient community rehabilitation center. South Afr J Occup Ther. 2016;46(1):59–63.
Rauch A, Negrini S, Cieza A. Toward Strengthening Rehabilitation in Health Systems: Methods Used to Develop a WHO Package of Rehabilitation Interventions. Arch Phys Med Rehabil [Internet]. 2019;100(11):2205–11. Accessed October 2020. https://pubmed.ncbi.nlm.nih.gov/31207218/
City of Johannesburg. Health [Internet]. 2018. Accessed January 2022. https://www.joburg.org.za/services_/JoburgCares/Pages/Health.aspx
Department of Coopertaive Governance and Tradition Affairs. Profile and Analysis: City of Johannesburg Metro [Internet]. 2020. https://www.cogta.gov.za/ddm/wp-content/uploads/2020/08/Take2_DistrictProfile_JHB1606-2-2.pdf . Accessed January 2023.
Jhb Metro Rehab. Audiology,occupational therapy, physiotherapy, podiatry, speech-language therapy [Internet]. 2023. Accessed June 2023. https://jhbmetrorehab.co.za/
Bartlett JE, Kotrlik JW, Higgins CC. Organizational research: Determining the appropriate sample size in survey research. Inf Technol Learn Perform J [Internet]. 2001;19(1):43. Accessed March 2019. https://www.opalco.com/wp-content/uploads/2014/10/Reading-Sample-Size1.pdf
Gauteng Province Co-operative Governance and Traditional Affairs. Metro One Plan: City of Johannesburg [Internet]. 2021. City Of Johannesburg District Development Model One Plan. Accessed January 2024. https://cmbinary.gauteng.gov.za
Gauteng Department of Health. Allied Health and Rehabilitation Services Strategic Plan 2019/2021–2024/25. Vol. 53. 2013.
Jahan I, Muhit M, Hardianto D, Laryea F, Chhetri AB, Smithers-Sheedy H, et al. Epidemiology of cerebral palsy in low and middle income countries: preliminary findings from an international multi-centre cerebral palsy register. Dev Med Child Neurol. 2021;63:1327–36.
Kamiya Y. Current situation of children with disabilities in low- and middle-income countries. Pediatr Int. 2021;63(11):1277–81.
Stats SA. South Africa Mid-year population estimates 2022 [Internet]. Statistics South Africa. 2022. https://www.statssa.gov.za/publications/P0302/P03022022.pdf . Accessed January 2023.
Petersen I, Fairall L, Bhana A, Kathree T, Selohilwe O, Brooke-Sumner C, et al. Integrating mental health into chronic care in South Africa: the development of a district mental healthcare plan. Br J Psychiatry. 2015;208(October):s29–39.
PubMed Google Scholar
Abdul Aziz AF, Mohd Nordin NA, Mohd FA, Aziz NAA, Sulong S, Aljunid SM. The integrated care pathway for post-stroke patients (iCaPPS): a shared care approach between stakeholders in areas with limited access to specialist stroke care services. BMC Health Serv Res [Internet]. 2017;17(35):1–11. Accessed June 2021. https://pubmed.ncbi.nlm.nih.gov/28086871/
Donnelly C, Leclair L, Hand C, Wener P, Letts L. Occupational therapy services in primary care: a scoping review. Prim Heal Care Res Dev. 2023;24.
Gregg CD, Hoffman CW, Hall H, McIntosh G, Robertson PA. Outcomes of an interdisciplinary rehabilitation programme for the management of chronic low back pain. J Prim Health Care. 2011.
Gutenbrunner C, Bickenbach J, Kiekens C, Meyer T, Skempes D, Nugraha B et al. Isprm discussion paper: Proposing dimensions for an international classification system for service organization in health-related rehabilitation. J Rehabil Med. 2015;47(9):809–15.
National Department of Health. Strengthening the South African health system: Towards an integrated and unified health system. Presidential Health Summit 2018. 2018. pp. 1–35.
Magaqa Q, Ariana P, Polack S. Examining the availability and accessibility of rehabilitation services in a rural district of South Africa: a mixed-methods study. Int J Environ Res Public Health. 2021;18(9).
Hussey M, Maclachlan M, Mji G. Barriers to the Implementation of the Health and Rehabilitation Articles of the United Nations Convention on the Rights of Persons with Disabilities in South Africa. Int J Heal Policy Manag [Internet]. 2017;6(4):207–218. Accessed January 2019. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5384983/
Kagee A, Van der Merwe M. Predicting treatment adherence among patients attending primary health care clinics: the utility of the theory of planned behaviour. South Afr J Psychol. 2006;36(4):699–714.
Sherry K. Essential considerations for equitable, accessible and poverty-reducing health care in South Africa. South African Heal Rev 2014/2015 [Internet]. 2015;1(2014):89–99. Accessed January 2018. https://journals.co.za/doi/10.10520/EJC189294
CBR Africa Network. Transition from CBR to CBID: A Situation analysis of community based rehabilitation (CBR) and community based inclusive development (CBID) in Africa. 2020;1–34.
Mars M. Telerehabilitation in South Africa– is there a Way Forward? Int J Telerehabilitation. 2011;3(1):11–8.
National Department of Health. Policy Framework and Strategy for Ward-Based Primary Healthcare Outreach Teams 2018/19-2023/24. 2018. p. 22.
Louw QA, Conradie T, Xuma-Soyizwapi N, Davis-Ferguson M, White J, Stols M et al. Rehabilitation Capacity in South Africa—A situational analysis. Int J Environ Res Public Health. 2023;20(4).
Mash R, Goliath C, Mahomed H, Reid S, Hellenberg D, Perez G. A framework for implementation of community-orientated primary care in the Metro Health Services, Cape Town, South Africa. Afr J Prim Heal Care Fam Med. 2020;12(1):1–5.
Nteta T, Mokgatle-Nthabu M, Oguntibeju O. Utilization of the primary health care services in the Tshwane Region of Gauteng Province, South Africa. PLoS ONE. 2010;5(11):e13909.
Article PubMed PubMed Central Google Scholar
Swanepoel DW. We Used Smartphones to Screen Young Children for Vision and Hearing Loss [Internet]. All Africa Global Media. 2019. Accessed January 2020. https://theconversation.com/we-used-smartphones-to-screen-young-children-for-vision-and-hearing-loss-125080
Louw C, Swanepoel DW, Eikelboom RH, Hugo J. Prevalence of hearing loss at primary health care clinics in South Africa. Afr Health Sci. 2018;18(2):313–20.
McColl MA. What do we need to know to Practice Occupational Therapy in the community? Am J Occup Ther. 1998;52(1):11–8.
Article CAS PubMed Google Scholar
Cieza A, Causey K, Kamenov K, Hanson SW, Chatterji S, Vos T. Global estimates of the need for rehabilitation based on the Global Burden of Disease study 2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet [Internet]. 2020;396(10267):2006–17. Accessed November 2020. https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(20)32340-0/fulltext
Health Professions Council of South Africa. Guidelines on the keeping of patient health records- Booklet 9. Pretoria; 2022. p. 2011.
Marutha N. Medical records preservation strategies in improving healthcare service providers’ access to patients’ medical histories in the Limpopo hospitals, South Africa. Inf Dev. 2021;37(1):174–88.
WHO. Routine health information systems-rehabilitation toolkit Information sheet [Internet]. Geneva, Switzerland: World Health Organization. 2023. https://www.who.int/publications/m/item/routine-health-information-systems--rehabilitation-toolkit--information-sheet . Accessed Fenruary 2024.
World Health Organization. Package of Interventions for Rehabilitation - Information Sheet [Internet], Geneva. Switzerland: WHO; 2023. https://www.who.int/publications/m/item/package-of-interventions-for-rehabilitation-information-sheet . Accessed February 2024.
Download references
Acknowledgements
The authors would like to acknowledge Prof de Witt and Dr Franzsen for their input in the review of the manuscript.
This research was supported by the Consortium for Advanced Research Training in Africa (CARTA), which is jointly led by the African Population and Health Research Center and the University of the Witwatersrand. It is funded by the Carnegie Corporation of New York (Grant No. G-19-57145), Sida (Grant No: 54100113), Uppsala Monitoring Center, Norwegian Agency for Development Cooperation (Norad), the Wellcome Trust (reference no. 107768/Z/15/Z) and the UK Foreign, Commonwealth & Development Office, with support from the Developing Excellence in Leadership, Training and Science in Africa (DELTAS Africa) programme. The statements and views expressed are solely the responsibility of the Fellow. For the purpose of open access, the author has applied a CC BY public copyright licence to any author accepted manuscript version arising from this submission.
Author information
Authors and affiliations.
Occupational Therapy Department, School of Therapeutic Sciences, Faculty of Health Sciences, University of the Witwatersrand, Johannesburg, Gauteng, South Africa
Lebogang Maseko
Department of Health and Rehabilitation Sciences, Division of Occupational Therapy, Faculty of Medicine and Health Sciences, Stellenbosch University, Stellenbosch, Western Cape, South Africa
Fasloen Adams
Physiotherapy Department, School of Therapeutic Sciences, Faculty of Health Sciences, University of the Witwatersrand, Johannesburg, Gauteng, South Africa
Hellen Myezwa
You can also search for this author in PubMed Google Scholar
Contributions
LM conceptualised and designed the study, collected data, carried out the initial and secondary analysis, and drafted, reviewed, and revised the manuscript. HM and FA supervised the study, including conceptualisation and critically reviewing the manuscript for important intellectual content. All authors approved the final manuscript submitted and agreed to be accountable for all aspects of the work.
Corresponding author
Correspondence to Lebogang Maseko .
Ethics declarations
Ethics approval and consent to participate.
Ethics approval was obtained from the Human Research Ethics Committee (Medical) of the Faculty of Health Sciences at the University of the Witwatersrand (M190466). The study was in accordance with the Helsinki Declaration of 1975 as revised in 2008. The need for Informed Consent was waived by the Human Research Ethics Committee (Medical) of the Faculty of Health Sciences at the University of the Witwatersrand due to the retrospective nature of the study.
Consent for publication
Not applicable.
Statement of human and animal rights
All procedures in this study were conducted in accordance with the Helsinki Declaration of 1975 as revised in 2008.
Competing interests
The authors declare that they have no financial or personal relationships that may have inappropriately influenced them in writing this article.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Maseko, L., Adams, F. & Myezwa, H. Let the records speak: an exploration of rehabilitation services offered in primary healthcare, Johannesburg metropolitan district. BMC Health Serv Res 24 , 501 (2024). https://doi.org/10.1186/s12913-024-10965-6
Download citation
Received : 22 June 2023
Accepted : 08 April 2024
Published : 22 April 2024
DOI : https://doi.org/10.1186/s12913-024-10965-6
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Rehabilitation
- Delivery of health care
- Integrated services
- Speech therapy
- Occupational therapy, physiotherapy, audiology
- Patient-centred care
- Health services for persons with disabilities
BMC Health Services Research
ISSN: 1472-6963
- General enquiries: [email protected]
Women are less likely to die when treated by female doctors, study suggests
Hospitalized women are less likely to die or be readmitted to the hospital if they are treated by female doctors, a study published Monday in the Annals of Internal Medicine found.
In the study of people ages 65 and older, 8.15% of women treated by female physicians died within 30 days, compared with 8.38% of women treated by male physicians.
Although the difference between the two groups seems small, the researchers say erasing the gap could save 5,000 women’s lives each year.
The study included nearly 800,000 male and female patients hospitalized from 2016 through 2019. All patients were covered by Medicare. For male hospitalized patients, the gender of the doctor didn’t appear to have an effect on risk of death or hospital readmission.
The data alone doesn’t explain why women fare better when treated by other women. But other studies suggest that women are less likely to experience “miscommunication, misunderstanding and bias” when treated by female doctors, said lead study author Dr. Atsushi Miyawaki, a senior assistant professor of health services research at the University of Tokyo Graduate School of Medicine.
The new research is part of a growing field of study examining why women and minorities tend to receive worse medical care than men and white patients. For example, women and minority patients are up to 30% more likely to be misdiagnosed than white men.
“Our pain and our symptoms are often dismissed,” said Dr. Megan Ranney, dean of the Yale School of Public Health. “It may be that women physicians are more aware of that and are more empathetic.”
Research shows that women are less likely than men to receive intensive care but more likely to report having negative experiences with health care, having their concerns dismissed, and having their heart or pain symptoms ignored, the authors wrote in the new study. Male physicians are also more likely than female doctors to underestimate women’s risk of stroke .
Part of the problem, Miyawaki said, is that medical students get “limited training in women’s health issues.”
Dr. Ronald Wyatt, who is Black, said his 27-year-old daughter recently had trouble getting an accurate diagnosis for her shortness of breath. An emergency room physician told her the problem was caused by asthma. It took two more trips to the emergency room for his daughter to learn that she actually had a blood clot in her lungs, a potentially life-threatening situation.
“There is a tendency for doctors to harbor sexist stereotypes about women, regardless of age, such as the notion that women’s symptoms are more emotional or their pain is less severe or more psychological in origin,” said Wyatt, former chief science and chief medical officer at the Society to Improve Diagnosis in Medicine, a nonprofit research and advocacy group.
Women seem to experience fewer of these problems when treated by other women.
For example, a study published JAMA Surgery in 2021 found that women patients developed fewer complications if their surgeon was female. Another JAMA Surgery study published in 2023 found all patients had fewer complications and shorter hospital stays if they were operated on by female surgeons, who worked more slowly than their male counterparts.
Women primary care doctors also tend to spend more time with their patients , Ranney said. Although that extra attention is great for patients, it also means that women see fewer patients per day and earn less, on average, than male doctors.
Dr. Ashish Jha, dean of the Brown University School of Public Health, said several studies suggest that female doctors follow medical evidence and guidelines , and that their patients have better outcomes.
“There’s lots of variation between women and men physicians,” said Jha, who was not involved in the new study. Women “tend to be better at communication, listening to patients, speaking openly. Patients report that communication is better. You put these things together, and you can understand why there are small but important differences.”
The authors of the study said it’s also possible that women are more forthcoming about sensitive issues with female physicians, allowing them to make more informed diagnoses.
That doesn’t mean that women should switch doctors, said Dr. Preeti Malani, a professor of medicine at the University of Michigan. For an individual patient, the differences in mortality and readmission rates seen in the new study are tiny.
“It would be a mistake to suggest that people need to find physicians of the same gender or race as themselves,” Jha said. “The bigger issue is that we need to understand why these differences exist.”
Malani said she’s curious about what women doctors are doing to prevent patients from needing to be readmitted soon after discharge. “How much care and thought is going into that discharge plan?” Malani asked. “Is that where women are succeeding? What can we learn about cultural humility and asking the right questions?”
Others aren’t convinced that the new study proves a physician’s gender makes a big difference.
Few hospitalized patients are treated by a single doctor, said Dr. Hardeep Singh, a professor at Baylor College of Medicine in Houston and a patient safety researcher at the Michael E. DeBakey VA Medical Center.
Hospital patients are treated by teams of physicians, especially if they need specialist care, in addition to nurses and other professionals, Singh said.
“How often do you see the same doc every day in the hospital?” Singh asked. “The point is that it’s not a one-man or one-woman show. Outcomes are unlikely to depend on one individual, but rather on a clinical team and the local context of care. … One name may appear on your bill, but the care is team-based.”
However, Singh said his research on misdiagnoses shows that doctors in general need to do a better job listening to patients.
Jha said he’d like the health system to learn what women doctors are doing right when they treat other women, then teach all physicians to practice that way.
“We should train everyone to be better at generating trust and being worthy of trust,” Jha said.
Wyatt said the country needs to take several steps to better care for women patients, including “de-biasing training” to teach doctors to overcome stereotypes. The health care system also needs to increase the number of women physicians in leadership, recruit more female doctors and do a better job at retaining them. All physicians also need more understanding of how adverse childhood experiences affect patient health, particularly for women, he said.
“More than once I’ve had white female patients tell me they came to be because I listened and they trusted me,” Wyatt said.
Liz Szabo is an independent health and science journalist. Her work has won multiple national awards. One of her investigations led to a new state law in Virginia.
The independent source for health policy research, polling, and news.
- Ten Things to Know About Consolidation in Health Care Provider Markets
Zachary Levinson , Jamie Godwin , Scott Hulver , and Tricia Neuman Published: Apr 19, 2024
National health spending totaled $4.5 trillion in 2022 —17% of gross domestic product (GDP)—and is projected to grow faster than GDP through 2031, contributing to higher costs for families, employers, states, and the federal government. As policymakers consider a variety of strategies to make health care more affordable, they have been increasingly attentive to consolidation in health care markets—including mergers and acquisitions of health care providers—and the potential effects of consolidation on the cost and quality of care and other outcomes. Consolidation may allow providers to operate more efficiently, and could help struggling providers keep their doors open in underserved areas, but also often reduces competition. A substantial body of evidence has found that consolidation has led to higher prices, but the evidence on quality is unclear.
In response to concerns about the effects of consolidation and reduced competition on prices and quality, the Federal Trade Commission (FTC) recently authorized a lawsuit to block a hospital acquisition in North Carolina. And, just last month, the FTC, Department of Justice, and Department of Health and Human Services issued a request for information (RFI) seeking input on the effects of consolidation involving health care providers and related products and services as part of a broader effort to clamp down on anticompetitive practices.
This issue brief identifies ten things to know about consolidation in health care provider markets, touching on topics such as the different types of consolidation, trends, ways in which consolidation can be beneficial or harmful for patients and other consumers, some key findings from existing research, and policy options for increasing competition. This brief focuses on consolidation among health care providers, rather than health insurers, and builds on a 2020 KFF issue brief on provider consolidation. More recent research has not altered the key takeaways pulled from that brief.
Efforts to promote more competitive provider markets could help address health spending and affordability issues, but also entail a number of challenges, given that many markets are already highly concentrated and that some regions cannot support competitive markets. Some have considered more direct regulation of prices and spending, and the two approaches could play complimentary roles when address rising health care costs, such as by encouraging providers to compete on quality when prices are regulated.
1. Consolidation in health care markets can take many forms and involve various types of providers
Health care consolidation often refers to scenarios where hospitals and other health care entities join together under common ownership through either a merger or acquisition (referred to as “mergers” in this brief). There are three main types of mergers:
- Horizontal mergers occur when there is consolidation between entities that offer the same or similar services, such as when a health system acquires a hospital or when two physician practices that provide overlapping services merge. For instance, in August 2023 , Oregon Health & Science University and Legacy Health—two of the largest health systems in the Portland area—announced plans to merge.
- Vertical mergers occur when there is consolidation between entities that offer different services along the same supply chain, such as when a hospital or health plan acquires a physician practice. For instance, in May 2023 , the health system HCA Healthcare announced a deal to acquire 41 urgent care centers in Texas, where HCA already had a large presence. Some mergers may entail both vertical and horizontal consolidation (e.g., if a health system acquires a physician practice that provides services offered by the system’s existing physician group).
- Cross-market mergers occur when there is consolidation between two providers that operate in different geographic markets for patient care. For example, in March 2024 , Kaiser Permanente closed its merger with Geisinger Health through a new organization called Risant. These systems operate in different regions of the United States, with Kaiser Permanente operating in five states in the West (including California) and Georgia, Maryland, Virginia, and DC and Geisinger operating in Pennsylvania.
Aside from merging, health care entities can form other types of affiliations without necessarily changing ownership, which may also have implications for patient care. Examples include the creation of accountable care organizations (i.e., groups of doctors, hospitals, and other providers who form partnerships to collaborate and share accountability for the cost and quality of care delivered to their patients) and joint ventures (i.e., agreements to collaborate on a particular goal, such as a health system and group practice that work together to create a new ambulatory surgery center). These affiliations can raise similar issues as mergers and are sometimes referred to as “soft” forms of consolidation.
2. There has been a large amount of consolidation in provider markets over the past 30 years
Provider markets have become increasingly consolidated over the past 30 years. Following a wave of consolidation in the early- and mid-1990s, there were 1,573 hospital mergers from 1998 to 2017 and another 428 hospital and health system mergers announced from 2018 to 2023. The share of community hospitals that are part of a larger health system also increased from 53% in 2005 to 68% in 2022 (see Figure 1). Relatedly, the share of physicians working for a hospital or in a practice owned at least partially by a hospital or health system increased from 29% in 2012 to 41% in 2022.
Consolidation has also contributed to the emergence of large health systems . For example, the ten largest health systems (see Table 1) accounted for about one in five (22%) of nonfederal general acute care hospital beds in 2022. These systems are the size of large corporations. For example, HCA Healthcare, which operates the largest number of nonfederal general acute care hospital beds in the country, had greater operating revenues than each of Netflix, Uber, and Starbucks in 2023. AdventHealth, the smallest of the ten largest health systems in terms of beds, had greater operating revenues than Zoom and Lyft combined in 2023 (as did Community Health Systems, the smallest of the ten largest systems in terms of operating revenues). Consolidation, which often occurs between providers based in the same region, has also contributed to highly concentrated markets where patients have limited options among large provider organizations.
Today, many provider markets are highly concentrated, particularly markets for hospital care. One study estimated that the vast majority (90%) of metropolitan statistical areas (MSAs) had highly concentrated hospital markets in 2016, while another estimated that the share of metro areas with highly concentrated hospital markets increased from 71% to 77% over the period from 2017 to 2021 (differences in magnitudes across these studies likely reflect their distinct methods, including market definitions). The former also found that most MSAs (65%) had highly concentrated specialist physician markets in 2016, and nearly two in five (39%) had highly concentrated markets for primary care physicians. Physician markets may have become more concentrated in recent years due to the ongoing trends in consolidation described above.
3. Corporations such as CVS, Amazon, and UnitedHealth and private equity firms have recently acquired many physician practices
In addition to hospitals and health systems, other types of entities have also been involved in a large number of acquisitions in recent years:
- Corporate buyers. Corporations that have not traditionally specialized in the provision of health care services—including large national companies such as CVS, Amazon, and UnitedHealth—have acquired many physician practices in recent years. The share of physicians employed by corporate entities increased over a three-year period from 15% in January 2019 to 22% in January 2022. Optum, a division of the insurer UnitedHealth, now employs or is affiliated with about 10% of all practicing physicians . Some policymakers have expressed concern about the role that large corporate buyers could have in increasing consolidation and reducing competition, which could lead to higher costs and reduced quality, although evidence is not yet available on this trend.
- Private equity firms. Private equity is a form of corporate ownership that often entails relying on loans to acquire a business, taking it private (if not so already), and attempting to increase its value with the goal of selling it at a profit in three to seven years. One common strategy is to consolidate providers through a series of mergers and acquisitions. Private equity provider acquisitions have increased by a large amount since 2010 —e.g., with physician practice deals increasing more than six-fold from 2012 to 2021—though deals have slowed somewhat since a peak in 2021. Some policymakers have expressed concern about the role of private equity in consolidation and the effect of the short-term profit motive of private equity firms on the prices, quality, and financial standing of acquired providers.
4. A substantial body of evidence shows that consolidation has led to higher prices, but the evidence on quality is unclear
Consolidation could in principle benefit consumers in some instances and be harmful in others. On the one hand, consolidation could allow providers to operate more efficiently, such as by obtaining supplies at steeper discounts (by purchasing them in greater volume); sharing resources (such as medical imaging equipment); and achieving the scale necessary to participate in value-based payment programs. These potential efficiencies could in turn benefit patients, for example, if they lead to higher quality care or reduced costs (e.g., if providers share savings through lower prices), and the latter could benefit health plan enrollees more generally to the extent that it leads to lower plan spending and premiums. On the other hand, consolidation often reduces market competition and therefore the pressure on providers to lower prices or invest in quality improvement. Critics have also questioned the extent to which mergers allow providers to operate more efficiently. Efficiencies may depend , in part, on the degree to which providers integrate their operations, which can be complex and may or may not be a priority.
The following discussion describes key findings from the research.
A substantial body of research shows that consolidation has led to higher health care prices , as noted in a 2020 KFF issue brief on provider consolidation. The evidence that consolidation leads to higher prices is strongest for hospitals, though studies that have evaluated physician and hospital-physician consolidation have also tended to find that they are associated with higher prices. Studies that have looked specifically at consolidation among nonprofit hospitals—which account for 58% of all community hospitals—have found price increases as well. A RAND Corporation review from 2022 (which also informs other sections of this brief) found that estimated price increases associated with hospital mergers have ranged from 3 to 65 percent. The large variation in estimated price increases may reflect differences in the types of mergers that were evaluated (e.g., the extent to which they reduced competition), the context of these mergers (e.g., the competitiveness of local insurance markets), and methodology. In addition to increases in the prices that commercial insurers pay providers, consolidation can also lead to higher Medicare reimbursement rates, as the program often provides greater reimbursement for a given service when provided in a hospital outpatient department versus a freestanding physician office (see discussion of site-neutral payment reforms below).
Relatedly, studies have typically found that consolidation leads to higher health care spending, which could increase costs for families, employers, states, and public programs, like Medicare and Medicaid . Several studies have found that consolidation leads to higher spending, which reflects both the price and volume of care. This includes studies evaluating hospital consolidation and hospital-physician consolidation. Only a small number of studies have evaluated physician consolidation, with mixed results. Increases in health care spending can be passed onto health plan enrollees through higher premiums and workers with employer-sponsored insurance through lower wages. Notably, a couple of studies have found an association between consolidation and premium increases, and one study found that hospital mergers led to decreases in wages among non-health care workers with employer health plans.
The evidence on the effect of provider consolidation on the quality of patient care is unclear . The evidence on the impact of horizontal and vertical consolidation on quality has been mixed, as described in a 2020 KFF issue brief and 2022 RAND Corporation review . For example, most of the research on horizontal hospital consolidation has found no difference 1 in or a negative impact on quality. Among other analyses, one study found that increased market concentration was associated with higher risk-adjusted one-year mortality rates for heart attacks and another found that hospital mergers were associated with a small decrease in patient experience measures and no changes in 30-day readmission and mortality rates (with inconclusive findings regarding clinical process measures). However, some studies have included mixed or positive findings relating to hospital consolidation. For example, a study funded by the American Hospital Association found that mergers were associated with decreases in 30-day readmission rates but no change in 30-day mortality rates (though an earlier version of the study found decreases in mortality rates as well).
The evidence is also mixed on the effects of vertical hospital-physician consolidation on quality. For example, one fairly recent study found that clinical process and patient experience measures were “marginally” higher for patients when their primary care physician was part of a system, another study found no difference in patients’ 30-day readmission rates when their primary care physician was part of a large system, and a third study found that complications following colonoscopies were higher for patients when their gastroenterologist was part of a system (though the evidence was less clear for clinical process measures).
Interpreting the evidence on quality is further complicated by the fact that there are many dimensions and measures of quality that have been or could be used to assess the effects of consolidation and that it could take time for changes in quality to materialize. Additionally, it is likely that the effects of consolidation vary based on the extent to which providers have integrated their operations and across different patient populations.
5. Mergers between hospitals and health systems can lead to higher prices even when entities operate in different markets
While policymakers and regulators have historically focused on consolidation within the same region, many mergers have occurred between hospitals and health systems that operate in different regions, as discussed in a KFF issue brief , including several multi-billion dollar deals over just the past couple of years. The small number of studies that have focused on cross-market mergers have estimated price increases ranging from 6% to 17%, even though these deals entail hospitals and health systems that are not competing against each other in the same area. There are a few reasons why cross-market mergers might lead to price increases. For instance, a combined health system with providers in, say, different areas of a state may be able to use its dominant position in one market to negotiate higher prices in another when contracting with a given health plan (e.g., a state employee plan with enrollees that reside in several markets). As another example, a large system that, say, acquires a small hospital may have more expertise in bargaining with insurers, which it could use to negotiate for higher prices.
6. The impact of consolidation on the availability of health care services for rural and other underserved patients is unclear
Consolidation could in principle have mixed implications for access to care. For example, it is conceivable that the acquisition of a small, financially struggling, rural hospital by a large health system based in another region could increase the availability of services in the community in some instances and reduce it in others. On the one hand, being acquired could benefit the hospital financially—such as by providing access to a wide range of resources, managerial expertise, and capital—which could help the hospital keep its doors open and maintain or expand the services it offers. On the other hand, the system that acquires the rural hospital may be less responsive to the needs of the local community, such as when deciding whether to close the hospital or to stop offering certain services, such as maternity care (an outcome supported by some research, as described below).
A small number of studies have evaluated the association between consolidation with rural hospital closures and service eliminations, with mixed results . Two studies found that rural hospitals that merged with other hospitals or health systems were more likely to eliminate certain service lines, such as obstetrics care, and another study found that independent hospitals (urban and rural) that joined a health system were more likely to stop offering inpatient pediatric services. One study found that system affiliation was associated with a lower likelihood of closing among rural hospitals with weaker finances but a higher likelihood among those with stronger finances.
A small number of studies have evaluated the association between consolidation and access to care among Medicaid patients, also with mixed results . On the one hand, two studies found that physician practices were more likely to accept Medicaid patients after becoming affiliated with a health system. This may be because the broader system has a commitment or obligation to treat patients regardless of their ability to pay (e.g., for emergency care) or because efficiencies allow providers to treat more patients. On the other hand, one study found that increases in hospital market concentration were associated with fewer Medicaid admissions and a shift in care from nonprofit to public hospitals. This could be because increases in commercial prices resulting from greater market concentration may lead private hospitals to focus more on commercial versus Medicaid patients. Another study found that system affiliation was associated with a decrease in Medicaid as a percentage of all hospital discharges, although that study also found that the number of beds in a hospital or health system was associated with an increase in Medicaid discharges as a share of the total.
A small number of studies have evaluated the effect of consolidation on hospital charity care and total community benefits, with mixed results . For example, one study found no association between the acquisition of independent hospitals and charity care or total community benefit spending overall but a decrease in the latter when focusing on hospitals acquired by an out-of-state system. Another study found that the association of higher market concentration with hospital charity care varied depending on the method used, with an increase under one approach and no difference under another. One study found that higher market concentration was associated with higher income thresholds for charity care eligibility, which effectively increases the number of patients who could qualify for charity care in a hospital.
7. Hospital consolidation can lead to lower wages for some skilled workers, such as nurses, but the broader evidence on employment and compensation effects is limited
Consolidation could in principle have both benefits and drawbacks for health care workers. On the one hand, consolidation could increase the negotiating leverage of hospitals and their ability to extract concessions from workers. For example, in 2023, a coalition of labor unions filed a complaint with the DOJ that UPMC, a large health system in Pennsylvania, had used its market power to suppress the wages of nurses and other health care workers, increase workloads, and restrict the ability of health care workers to seek better employment elsewhere. Mergers could also lead to layoffs, for example, to the extent that providers consolidate their staff and operations. On the other hand, health care workers could benefit from hospital mergers in some scenarios where consolidation allows hospitals to remain open and operate more efficiently. For example, the acquisition of a struggling rural hospital by a health system could help the facility sustain its operations in certain circumstances, which could protect jobs and possibly bolster wages.
A couple of studies have found that hospital consolidation has led to lower wages for some skilled workers, such as nurses, though the implications of other studies on health care worker wages are less clear . For example, one study found that hospital mergers were associated with lower wages for nurses and pharmacy workers and for skilled nonmedical mergers following mergers that caused large increases in market concentration (but not for unskilled workers). Research from the Center for Economic and Policy Research also found that increases in hospital market concentration were associated with lower wages for nurses in small metropolitan statistical areas. An earlier study did not find consistent evidence when evaluating nurses’ wages but did find that hospital mergers in California were associated with greater work effort (as measured by patient caseload). A small number of studies that looked more broadly at the financial impact of consolidation, including average compensation across all hospital workers, have produced mixed results .
Some studies find that hospital consolidation has led to reductions in staffing, though others have not, and the evidence is unclear on whether mergers avert closures, which could preserve jobs . A small number of studies have analyzed the effects of hospital consolidation on employment, with some finding an association with reduced staffing levels. For example, one study evaluating independent hospitals in New York found an association between joining a system and a reduction in employment, especially among employees with overhead and support functions. However, other studies have found no differences or inconsistent or unclear results. Additionally, as noted above, there is no clear evidence regarding the effect of mergers on hospital closures. If mergers lead to efficiencies that prevent closures, they may help preserve jobs.
8. The FTC, the DOJ, and state antitrust agencies each play a role in challenging consolidation and other potentially anticompetitive practices
Federal and state antitrust agencies each play a role in challenging consolidation and other potentially anticompetitive practices of health care providers and other businesses, as described in a KFF issue brief . At the federal level, the Federal Trade Commission (FTC) and the Department of Justice (DOJ) share responsibility for enforcing federal antitrust laws, including the Sherman Act, the Clayton Act, and the FTC Act. State attorneys general (AG) offices also have the authority to bring action under federal antitrust law, as well as under state statutes, which sometimes expand upon federal law. Antitrust agencies challenge mergers, acquisitions, and other practices that may hinder competition (such as the use of anticompetitive contract clauses). They do so to promote competitive markets, often for the benefit of consumers (such as patients and health plan enrollees).
There are at least a few challenges that may limit the ability of the federal government and states to foster competitive provider markets through antitrust enforcement:
- It is difficult to break up mergers after they have already occurred, and many provider markets are already highly concentrated . Breaking up a merger after providers have already consolidated can be difficult. At the same time, regulating the behavior of merged providers—such as through restrictions on the prices they charge—may be difficult to monitor and enforce on an ongoing basis.
- Some regions cannot support competitive provider markets . For instance, rural communities may not have enough residents to support several providers that offer the same service.
- Antitrust litigation can be complex and expensive . Without adequate funding, it may be impractical to challenge a large number of provider business practices that raise anticompetitive concerns.
- Antitrust agencies may have difficulty staying ahead of market trends . For example, it could take time for the government to develop strong guidelines for challenging vertical or cross-market mergers and to accumulate enough evidence to convince courts that these practices harm competition. In the meantime, these mergers will likely continue.
- The benefits of competitive provider markets for individuals with health insurance will depend in part on the competitiveness of health insurance markets . One study estimated that most MSAs (57%) had highly concentrated insurance markets in 2016. When insurance markets are not competitive, cost savings from competitive provider markets might not be fully passed along to consumers.
The FTC and DOJ have recently signaled an interest in expanding their scrutiny of different types of mergers. For example, in December 2023, the agencies released updated merger guidelines that indicate that they may challenge a broader range of deals. Among other changes, the guidelines expand the definition of highly concentrated markets, rely on a lower threshold for identifying large changes in market concentration, consider the combined effect of a series of acquisitions (e.g., of a health system acquiring several small physician practices over time), add an explicit discussion of the agencies’ views on how workers may be negatively impacted when their employers merge, and touch on cross-market mergers.
The FTC and DOJ have also indicated an interest in challenging provider acquisitions by private equity firms and private payers. For instance, the agencies, along with HHS, specifically mentioned these types of entities in a March 2024 request for information on the effects of transactions involving health care providers and related products and services. Further, in September 2023 , for the first time, the FTC challenged a common strategy of private equity firms that entails amassing market power through a series of physician practice acquisitions.
9. Site-neutral payment reforms, if enacted, could reduce incentives for vertical consolidation by lowering the rates at which acquired providers bill Medicare
Policymakers have expressed interest in aligning Medicare reimbursement rates for outpatient services across care settings through “site-neutral payment reforms,” which could directly lower program costs and reduce the incentive for hospitals to buy up physician practices. Under current payment rules, Medicare reimbursement is often higher for a given outpatient service when provided in a hospital outpatient department versus a freestanding physician office or ambulatory surgical center. Two studies have found that these payment differences are associated with an increase in hospital-physician consolidation, which can allow providers to bill Medicare at higher rates.
Through legislation and rulemaking, Medicare has aligned payments for office visits across freestanding physician offices and off-campus hospital outpatient departments—which often resemble physician offices—as well as for other services for relatively new off-campus facilities. Policymakers have considered other site-neutral reforms with varying scope that would extend to additional sites of care and services. Proponents of these reforms assert there are no grounds to pay different amounts for the same service based on site of care (physician office or outpatient hospital department) while hospitals and other opponents counter that patients treated in hospital outpatient settings have greater needs than patients in physician settings and that their cost structure justifies higher payment rates.
10. Policymakers have considered a number of options to increase the competitiveness of provider markets
Several policies have been proposed to rein in provider consolidation or increase the competitiveness of provider markets in other ways:
- Strengthen antitrust enforcement . This approach would make it easier for the FTC and DOJ to enforce antitrust law. Specific policies include: requiring more providers to report planned mergers, lowering the legal standards by which mergers are deemed anticompetitive, and mandating that providers receive approval from the government before merging. Other proposals to strengthen antitrust enforcement include: eliminating state Certificate of Public Advantage (COPA) laws (which some states use to shield mergers from federal antitrust challenges in exchange for state regulation), increasing the scope of antitrust law (such as by giving the FTC full authority to regulate nonprofit providers and outlawing anticompetitive contracting clauses), and providing greater resources to agencies that enforce antitrust law.
- Reduce incentives for health care providers to consolidate . This could include site-neutral payment reforms (as described above), changes to the 340B program (which currently allows certain providers acquired by a 340B entity to purchase drugs at a substantial discount), and efforts to reduce the administrative burden of government regulations on providers (which may incentivize small practices that have difficulty shouldering these requirements to merge with other providers).
- Increase price transparency . Greater price transparency could help patients, plans, and employers shop for health care providers (e.g., to receive care from or include in provider networks) and may in turn encourage greater competition among providers. As discussed in a KFF issue brief , information about hospital and other health care prices remains elusive, despite recent federal transparency rules.
- Allow more providers to enter the market . This could include reforming state Certificate of Need (CON) statues (which can be used to limit, for example, the construction of new health care facilities) and scope of practice laws (which regulate what work various health care professionals, such as nurse practitioners, are allowed to perform).
Each of these proposals would involve tradeoffs that would be important to consider.
This work was supported in part by Arnold Ventures. KFF maintains full editorial control over all of its policy analysis, polling, and journalism activities.
References to no differences, no changes, or no associations in this issue brief indicate that there were no statistically significant differences.
← Return to text
- Health Costs
- Quality Measures
- Access to Care
- Affordability
- Health System Performance
news release
Also of interest.
- Understanding the Role of the FTC, DOJ, and States in Challenging Anticompetitive Practices Of Hospitals and Other Health Care Providers
- Understanding Mergers Between Hospitals and Health Systems in Different Markets
- Gaps in Data About Hospital and Health System Finances Limit Transparency for Policymakers and Patients
An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
Busse R, Klazinga N, Panteli D, et al., editors. Improving healthcare quality in Europe: Characteristics, effectiveness and implementation of different strategies [Internet]. Copenhagen (Denmark): European Observatory on Health Systems and Policies; 2019. (Health Policy Series, No. 53.)

Improving healthcare quality in Europe: Characteristics, effectiveness and implementation of different strategies [Internet].
1 an introduction to healthcare quality: defining and explaining its role in health systems.
Reinhard Busse , Dimitra Panteli , and Wilm Quentin .
1.1. The relevance of quality in health policy
Quality of care is one of the most frequently quoted principles of health policy, and it is currently high up on the agenda of policy-makers at national, European and international levels (EC, 2016 ; OECD, 2017 ; WHO, 2018 ; WHO/OECD/World Bank, 2018 ). At the national level, addressing the issue of healthcare quality may be motivated by various reasons – ranging from a general commitment to high-quality healthcare provision as a public good or the renewed focus on patient outcomes in the context of popular value-based healthcare ideas to the identification of specific healthcare quality problems ( see Box 1.1 ).
Reasons for (re)focusing on quality of care.
At the European level, the European Council’s Conclusions on the Common Values and Principles in European Union Health Systems highlight that “the overarching values of universality, access to good quality care, equity, and solidarity have been widely accepted in the work of the different EU institutions” (European Council, 2006 ). The European Commission (EC, 2014 ; EC, 2016 ) also recognizes quality as an important component of health system performance (i.e. the extent to which health systems meet their goals; we return to the link between quality and performance later in the chapter).
At the international level, quality is receiving increasing attention in the context of the Sustainable Development Goals (SDGs), as the SDGs include the imperative to “achieve universal health coverage, including financial risk protection, access to quality essential health-care services and access to safe, effective, quality and affordable essential medicines and vaccines for all”. This is reflected in two World Health Organization (WHO) reports published in 2018, a handbook for national quality policies and strategies (WHO, 2018 ) and a guide aiming to facilitate the global understanding of quality as part of universal health coverage aspirations (WHO/OECD/World Bank, 2018 ).
A previous study on quality of care by the European Observatory on Health Systems and Policies (Legido-Quigley et al., 2008 ) noted that the literature on quality of care in health systems was already very extensive and difficult to systematize ten years ago – and this is even truer today. Research is available on a vast range of approaches or strategies for assuring or improving quality of care, often focusing on certain organizations (hospitals, health centres, practices) or particular areas of care (emergency care, maternal care, etc.) (Flodgren, Gonçalves & Pomey, 2016 ; Ivers et al., 2014 ; Houle et al., 2012 ; Gharaveis et al., 2018 ). This body of evidence has contributed to a better understanding of the effectiveness of particular interventions in particular settings for particular groups of patients. However, the available literature rarely addresses the question of the superiority of individual strategies and usually does not provide guidance to policy-makers on which strategy to implement in a particular setting.
In addition, despite the vast literature base and the universal acknowledgement of its importance in health systems, there is no common understanding of the term “quality of care”, and there is disagreement about what it encompasses. The definition of quality often differs across contexts, disciplinary paradigms and levels of analysis. Yet, as prescribed by the seminal work of Avedis Donabedian ( 1980 ), assessing and improving quality predicates an understanding of what it entails. Therefore, the aim of this chapter is to provide clarity about the definition of quality and its relation to health system performance as well as introduce the level of analysis adopted in this book. The chapter concludes with a brief introduction to the aims and the structure of the book.
1.2. Definitions of healthcare quality
Early definitions of healthcare quality were shaped almost exclusively by health professionals and health service researchers. However, there has been increasing recognition that the preferences and views of patients, the public and other key players are highly relevant as well (Legido-Quigley et al., 2008 ). Table 1.1 summarizes some of the most influential definitions of healthcare quality from different contexts, starting with the definition of Donabedian ( 1980 ) and ending with the definition provided by WHO’s handbook for national quality policy and strategy (WHO, 2018 ).
Selected definitions of quality, 1980–2018.
Donabedian defined quality in general terms as “the ability to achieve desirable objectives using legitimate means”. This definition reflects the fact that the term “quality” is not specific to healthcare and is used by many different people in various sectors of society. People use the term quality when they describe a range of positive aspects of hospitals and doctors – but also when they speak about food or cars. In fact, the widespread use of the term quality explains part of the confusion around the concept of healthcare quality when policy-makers or researchers use the term for all kinds of positive or desirable attributes of health systems. However, Donabedian also provides a more specific definition of quality of care, stating that it is “care which is expected to maximize an inclusive measure of patient welfare, after one has taken account of the balance of expected gains and losses that attend the process of care in all its parts” (Donabedian, 1980 ).
Donabedian’s definition is interesting because it specifies that quality of care is related to the process of care in all its parts and that the goal of high-quality care is to maximize patient welfare. Patient welfare certainly includes the health status of the patient (later specified as encompassing physical, physiological and psychological dimensions; see also Donabedian, Wheeler & Wyszewianski, 1982 ). However, the concept of patient welfare is also in line with an approach that considers what patients find important. Furthermore, Donabedian’s definition recognizes the natural limits of quality and its improvement, by highlighting that gains and losses are expected in the process of care.
A decade later the Institute of Medicine (IOM) in the US defined quality of care as “the degree to which health services for individuals and populations increase the likelihood of desired health outcomes and are consistent with current professional knowledge” ( see Table 1.1 ). At first glance, the IOM’s definition’s focus on “health outcomes” seems to be more restrictive than Donabedian’s notion of “patient welfare”. However, in their elaboration of the definition, the IOM specified that these “desired” health outcomes were expected to reflect patient satisfaction and well-being next to broad health status or quality-of-life measures. The IOM’s definition has inspired the understanding of quality by many other organizations in the USA and internationally.
In contrast to other popular definitions of quality in healthcare around that time (including Donabedian’s), which mainly referred to medical or patient care, the IOM’s definition set the focus on health services in general (as “health care implies a broad set of services, including acute, chronic, preventive, restorative, and rehabilitative care, which are delivered in many different settings by many different health care providers”) and on individuals and populations (rather than patients), thus strengthening the link of quality with prevention and health promotion. Finally, the concept of “current professional knowledge” both reinforced the movement for evidence-based care and highlighted that the concept of quality is dynamic and continuously evolving. In that sense, providers can only be assessed against the current state of knowledge as a service that is considered “good quality” at any given time may be regarded as “poor quality” twenty years later in light of newer insights and alternatives.
The definition of quality by the Council of Europe included in Table 1.1 , published seven years after the IOM’s definition as part of the Council’s recommendations on quality improvement systems for EU Member States, is the first to explicitly include considerations about the aspect of patient safety. It argues that quality of care is not only “the degree to which the treatment dispensed increases the patient’s chances of achieving the desired results”, which basically repeats the IOM definition, but it goes on to specify that high-quality care also “diminishes the chances of undesirable results” (The Council of Europe, 1997 ). In the same document the Council of Europe also explicitly defines a range of dimensions of quality of care – but, surprisingly, does not include safety among them.
The final two definitions included in Table 1.1 are from the European Commission ( 2010 ) and from WHO ( 2018 ). In contrast to those discussed so far, both of these definitions describe quality by specifying three main dimensions or attributes: effectiveness, safety and responsiveness or patient-centredness. It is not by chance that both definitions are similar as they were both strongly influenced by the work of the OECD’s Health Care Quality Indicators (HCQI) project (Arah et al., 2006 ; see below). These final two definitions are interesting also because they list a number of further attributes of healthcare and healthcare systems that are related to quality of care, including access, timeliness, equity and efficiency. However, they note that these other elements are either “part of a wider debate” (EC, 2010 ) or “necessary to realize the benefits of quality health care” (WHO, 2018 ), explicitly distinguishing core dimensions of quality from other attributes of good healthcare.
In fact, the dimensions of quality of care have been the focus of considerable debate over the past forty years. The next section focuses on this international discussion around the dimensions of quality of care.
1.3. Dimensions of healthcare quality
As mentioned earlier, Donabedian posited that assessing and improving quality of care presupposes an understanding of what it does and does not entail. Different definitions of quality often specify relatively long lists of various attributes that they recognize as part of quality. Table 1.2 provides an overview of the dimensions of quality mentioned by ten selected definitions (including those in Table 1.1 ).
Quality dimensions in ten selected definitions of quality, 1980–2018.
The table shows that effectiveness, patient safety and responsiveness/patient-centredness seem to have become universally accepted as core dimensions of quality of care. However, many definitions – also beyond those shown in Table 1.2 – include attributes such as appropriateness, timeliness, efficiency, access and equity. This is confusing and often blurs the line between quality of care and overall health system performance. In an attempt to order these concepts, the table classifies its entries into core dimensions of quality, subdimensions that contribute to core dimensions of quality, and other dimensions of health system performance.
This distinction is based on the framework of the OECD HCQI project, which was first published in 2006 (Arah et al., 2006 ). The purpose of the framework was to guide the development of indicators for international comparisons of healthcare quality. The HCQI project selected the three dimensions of effectiveness, safety and patient-centredness as the core dimensions of healthcare quality, arguing that other attributes, such as appropriateness, continuity, timeliness and acceptability, could easily be accommodated within these three dimensions. For example, appropriateness could be mapped into effectiveness, whereas continuity and acceptability could be absorbed into patient-centredness. Accessibility, efficiency and equity were also considered to be important goals of health systems. However, the HCQI team argued – referring to the IOM ( 1990 ) definition – that only effectiveness, safety and responsiveness are attributes of healthcare that directly contribute to “increasing the likelihood of desired outcomes”.
Some definitions included in Table 1.2 were developed for specific purposes and this is reflected in their content. As mentioned above, the Council of Europe ( 1997 ) definition was developed to guide the development of quality improvement systems. Therefore, it is not surprising that it includes the assessment of the process of care as an element of quality on top of accessibility, efficacy, effectiveness, efficiency and patient satisfaction.
In 2001 the IOM published “Crossing the Quality Chasm”, an influential report which specified that healthcare should pursue six major aims: it should be safe, effective, patient-centred, timely, efficient and equitable. These six principles have been adopted by many organizations inside and outside the United States as the six dimensions of quality, despite the fact that the IOM itself clearly set them out as “performance expectations” (“a list of performance characteristics that, if addressed and improved, would lead to better achievement of that overarching purpose. To this end, the committee proposes six specific aims for improvement. Health care should be …”; IOM, 2001 ). For example, WHO ( 2006b ) adapted these principles as quality dimensions in its guidance for making strategic choices in health systems, transforming the concept of timeliness into “accessibility” to include geographic availability and progressivity of health service provision. However, this contributed to the confusion and debate about quality versus other dimensions of performance.
The European Commission’s Expert Panel on Effective Ways for Investing in Health Care also opted for a broad consideration of quality, including the dimensions of appropriateness, equity and efficiency in its recommendations for the future EU agenda on quality of care in 2014 (EC, 2014 ). Similarly, WHO ( 2016 ) used timeliness (as originally described by the IOM) instead of accessibility (as used by WHO in 2006b ), and added integration in healthcare provision as a dimension of high-quality care, in line with the approach taken by the Health Care Council of Canada (Health Care Council of Canada, 2013 ). The understanding of integrated care as part of patient-centredness can also be found in the updated version of the HCQI framework published by the OECD in 2015 (Carinci et al., 2015 ).
This long and inconsistent list of different dimensions inevitably contributes to the confusion about the concept of quality of care. However, conceptual clarity about quality is crucial, as it will influence the types of healthcare policies and strategies that are adopted to improve it. Part of the confusion around the demarcation between quality of care and health system performance originates from insufficiently distinguishing between intermediate and final goals of health systems and between different levels at which quality can be addressed.
The next section aims to provide more clarity about the role of quality in health systems and health systems performance assessment by highlighting the difference between healthcare service quality and healthcare system quality. In so doing, the section sets the background for the way quality is understood in the remainder of the book.
1.4. The role of quality in health systems and health system performance assessment
Numerous frameworks have been developed over the past 20 years with the aim of facilitating a better understanding of health systems and enabling health system performance assessments (Papanicolas, 2013 ; Fekri, Macarayan & Klazinga, 2018 ). Most of these frameworks implicitly or explicitly include quality as an important health system goal but they differ in how they define quality and how they describe its contribution to overall health system goals. A particularly influential framework is the WHO ( 2006a ) “building blocks” framework for health systems strengthening ( see Fig. 1.1 ). The framework conceptualizes health systems in terms of building blocks, including service delivery, health workforce, information, medical products, financing and leadership/governance. In addition, the framework defines quality and safety as intermediate goals of health systems, together with access and coverage. Achievement of these intermediate goals will ultimately contribute to achieving overall health system goals of improved health, responsiveness, financial protection and improved efficiency.
Quality is an intermediate goal of health systems. Source: WHO, 2006
It is worth noting that quality and safety are mentioned separately in the framework, while most of the definitions of quality discussed above include safety as a core dimension of quality. For more information about the relationship between quality and safety, see also Chapter 11 .
As mentioned above, Donabedian defined quality in general terms as “the ability to achieve desirable objectives using legitimate means” (Donabedian, 1980 ). Combining Donabedian’s general definition of quality with the WHO building blocks framework ( Fig. 1.1 ), one could argue that a health system is “of high quality” when it achieves these (overall and intermediate) goals using legitimate means. In addition, Donabedian highlighted that it is important to distinguish between different levels when assessing healthcare quality (Donabedian, 1988 ). He distinguished between four levels at which quality can be assessed – individual practitioners, the care setting, the care received (and implemented) by the patient, and the care received by the community. Others have conceptualized different levels at which policy developments with regard to quality may take place: the health system (or “macro”) level, the organizational (“meso”) level and the clinical (“micro”) level (Øvretveit, 2001 ).
While the exact definition of levels is not important, it is essential to recognize that the definition of quality changes depending on the level at which it is assessed. For simplicity purposes, we condense Donabedian’s four tiers into two conceptually distinct levels ( see Fig. 1.2 ). The first, narrower level is the level of health services, which may include preventive, acute, chronic and palliative care (Arah et al., 2006 ). At this level, there seems to be an emerging consensus that “quality of care is the degree to which health services for individuals and populations are effective, safe and people-centred” (WHO, 2018 ).
Two levels of healthcare quality.
The second level is the level of the healthcare system as a whole. Healthcare systems are “of high quality” when they achieve the overall goals of improved health, responsiveness, financial protection and efficiency. Many of the definitions of healthcare quality included in Table 1.2 seem to be concerned with healthcare system quality as they include these attributes among stated quality dimensions. However, such a broad definition of healthcare quality can be problematic in the context of quality improvement: while it is undoubtedly important to address access and efficiency in health systems, confusion about the focus of quality improvement initiatives may distract attention away from those strategies that truly contribute to increasing effectiveness, safety and patient-centredness of care.
To avoid confusion and achieve conceptual clarity, we therefore propose reserving the use of the term “healthcare quality” for the first level, i.e. the healthcare services level. Concerning the second level, i.e. the health(care) system level, there seems to be an international trend towards using the term “health system performance” to describe the degree to which health systems achieve their overall and intermediate goals.
Frameworks to assess health system performance by the OECD (Carinci, 2015 ) and the European Commission ( 2014 ) include healthcare quality at the service level as a core dimension – besides other elements of performance such as accessibility, efficiency and population health. In other words, health system performance is a better term for health system “quality” (according to Donabedian’s broad definition of the term), and healthcare service quality is one of its core components.
The relationship between quality and the achievement of final health system goals is aptly illustrated in another, relatively recent framework for health system performance comparisons ( Fig. 1.3 ). The framework has condensed the four intermediate goals of the WHO building blocks model into only two: access (including coverage) and quality (including safety). It posits that population health outcomes and system responsiveness depend on the extent to which the entire population has access to care and the extent to which health services are of good quality (i.e. they are effective, safe and patient-centred). The resources, financial or otherwise, required to produce final health system goals determine efficiency in the system.
The link between health system performance and quality of healthcare services. Source: Busse, 2017. Note: *Financial protection is both an enabling condition for access as well as a final outcome.
The framework highlights that health systems have to ensure both access to care and quality in order to achieve the final health system goals. However, it is important to distinguish conceptually between access and quality because very different strategies are needed to improve access (for example, improving financial protection, ensuring geographic availability of providers) than are needed to improve quality of care. This book focuses on quality and explores the potential of different strategies to improve it.
1.5. What are quality improvement strategies? Aims and structure of this book
As mentioned in the Preface, the purpose of the book is to provide a framework for understanding, measuring and ultimately improving the quality of healthcare through a variety of strategies. In general, a strategy can be viewed as an approach or plan that is designed or selected to achieve a desired outcome (for example, attain a goal or reach a solution to a problem). The 2018 WHO Handbook for National Quality Policy and Strategy differentiates between the two titular concepts by underlining that policy refers to an agreed ambition for the health system with an explicit statement of intention, i.e. a “course of action”. Accordingly, it would usually mainly outline broad priorities to be addressed rather than the concrete steps to address them. The corresponding strategy, on the other hand, provides a clear roadmap for achieving these priorities (WHO, 2018 ). In this conceptualization, a number of tools, or interventions, can be used to implement the strategy and aid in the attainment of its milestones.
For the purpose of this book, we use the term “strategy” more narrowly and in a sectoral way to denote a mechanism of action geared towards achieving specific quality assurance or improvement goals by addressing specific targets within healthcare provision (for example, health professionals, provider organizations or health technologies). For example, we consider accreditation of healthcare providers and clinical practice guidelines as quality strategies, whereas the same concepts would be described as “quality interventions”, “quality initiatives”, “quality improvement tools” or “quality improvement activities” elsewhere.
Table 1.3 summarizes a range of selected quality strategies (or interventions) and clusters them into system level strategies, institutional/organizational strategies and patient/community level strategies. This categorization follows the one used by the OECD in its Country Quality Reviews and the recent report on the economics of patient safety (OECD, 2017 ; Slawomirksi, Auraaen & Klazinga, 2017 ). Table 1.3 also includes strategies listed in the 2018 WHO Handbook (WHO, 2018 ), as well as a few others. The strategies discussed in more detail in the second part of this book are marked in grey in the table.
A selection of prominent quality strategies (marked in grey are the strategies discussed in Chapters 5 to 14 of this book).
As becomes evident in Table 1.3 , the focus of this book is on system level and organizational/institutional level strategies. Its aim is to provide guidance to policy-makers who have to make choices about investing political and economic resources into the implementation or scale-up of different options from this vast number of different strategies. The book does not attempt to rank the best quality strategies to be implemented across countries, because different strategies will need to be prioritized depending on the motivation, the identified quality improvement needs and the existing structures or initiatives already in place. Instead, it hopes (1) to provide an overview of the experience with the selected strategies to date in Europe and beyond, (2) to summarize the available evidence on their effectiveness and – where available – cost-effectiveness and the prerequisites for their implementation, and (3) to provide recommendations to policy-makers about how to select and actually implement different strategies.
The book is structured in three parts. Part I includes four chapters and deals with cross-cutting issues that are relevant for all quality strategies. Part II includes ten chapters each dealing with specific strategies. Part III focuses on overall conclusions for policy-makers.
The aim of Part I is to clarify concepts and frameworks that can help policy-makers to make sense of the different quality strategies explored in Part II . Chapter 2 introduces a comprehensive framework that enables a systematic analysis of the key characteristics of different quality strategies. Chapter 3 summarizes different approaches and data sources for measuring quality. Chapter 4 explores the role of international governance and guidance, in particular at EU level, to foster and support quality in European countries.
Part II , comprising Chapters 5 to 14 , provides clearly structured and detailed information about ten of the quality strategies presented in Table 1.3 (those marked in grey). Each chapter in Part II follows roughly the same structure, explaining the rationale of the strategy, exploring its use in Europe and summarizing the available evidence about its effectiveness and cost-effectiveness. This is followed by a discussion of practical aspects related to the implementation of the strategy and conclusions for policy-makers. In addition, each chapter is accompanied by an abstract that follows the same structure as the chapter and summarizes the main points on one or two pages.
Finally, Part III concludes with the main findings from the previous parts of the book, summarizing the available evidence about quality strategies in Europe and providing recommendations for policy-makers.
- Arah OA, et al. A conceptual framework for the OECD Health Care Quality Indicators Project. International Journal for Quality in Health Care . 2006; 18 S1:5–13. [ PubMed : 16954510 ]
- Busse R. High Performing Health Systems: Conceptualizing, Defining, Measuring and Managing. Presentation at the “Value in Health Forum: Standards, Quality and Economics”; Edmonton. 19 January 2017. 2017.
- Carinci F, et al. Towards actionable international comparisons of health system performance: expert revision of the OECD framework and quality indicators. International Journal for Quality in Health Care . 2015; 27 (2):137–46. [ PubMed : 25758443 ]
- Donabedian A. The Definition of Quality and Approaches to Its Assessment. Vol 1. Explorations in Quality Assessment and Monitoring. Ann Arbor, Michigan, USA: Health Administration Press; 1980.
- Donabedian A. The quality of care. How can it be assessed. Journal of the American Medical Association . 1988; 260 (12):1743–8. [ PubMed : 3045356 ]
- Donabedian A, Wheeler JR, Wyszewianski L. Quality, cost, and health: an integrative model. Medical Care . 1982; 20 (10):975–92. [ PubMed : 6813605 ]
- EC. EU Actions on Patient Safety and Quality of Healthcare. European Commission, Healthcare Systems Unit. Madrid: European Commission; 2010.
- EC. Communication from the Commission – On effective, accessible and resilient health systems. European Commission. Brussels: European Commission; 2014.
- EC. Report by the Expert Group on Health Systems Performance Assessment. European Commission (EC). Brussels: European Commission; 2016. So What? Strategies across Europe to assess quality of care.
- European Council. Council Conclusions on Common values and principles in European Union Health Systems. Official Journal of the European Union . 2006; C146 :1–2.
- Fekri O, Macarayan ER, Klazinga N. Health system performance assessment in the WHO European Region: which domains and indicators have been used by Member States for its measurement? Copenhagen: WHO Regional Office for Europe; 2018. (Health Evidence Network (HEN) synthesis report 55) [ PubMed : 30091869 ]
- Flodgren G, Gonçalves-Bradley DC, Pomey MP. External inspection of compliance with standards for improved healthcare outcomes. Cochrane Database Syst Rev. 2016; 12 :CD008992. [ PMC free article : PMC6464009 ] [ PubMed : 27911487 ] [ CrossRef ]
- Gharaveis A, et al. The Impact of Visibility on Teamwork, Collaborative Communication, and Security in Emergency Departments: An Exploratory Study. HERD: Health Environments Research & Design Journal . 2018; 11 (4):37–49. [ PubMed : 29069916 ]
- Health Council of Canada. Better health, better care, better value for all: refocussing health care reform in Canada. Toronto: Health Care Council of Canada; 2013. 2013.
- Houle SK, et al. Does performance-based remuneration for individual health care practitioners affect patient care? A systematic review. Annals of Internal Medicine . 2012; 157 (12):889–99. [ PubMed : 23247940 ]
- IOM. Medicare: A Strategy for Quality Assurance: Volume 1. Washington (DC), US: National Academies Press; 1990. [ PubMed : 25144047 ]
- IOM. Crossing the Quality Chasm: A New Health System for the 21st Century. Washington (DC), US: National Academies Press; 2001. [ PubMed : 25057539 ]
- Ivers N, et al. Growing literature, stagnant science? Systematic review, meta-regression and cumulative analysis of audit and feedback interventions in health care. Journal of General Internal Medicine . 2014; 29 (11):1534–41. [ PMC free article : PMC4238192 ] [ PubMed : 24965281 ]
- Legido-Quigley H, et al. Observatory Studies Series, 12. Copenhagen: WHO on behalf of the European Observatory on Health Systems and Policies; 2008. Assuring the Quality of Health Care in the European Union: A case for action.
- OECD. OECD Reviews of Health Care Quality. Paris: OECD Publishing; 2017. Caring for Quality in Health: Lessons learnt from 15 reviews of health care quality. Available at: http://dx .doi.org/10 .1787/9789264267787-en , accessed 9 April 2019.
- Øvretveit J. Quality evaluation and indicator comparison in health care. International Journal of Health Planning Management . 2001; 16 :229–41. [ PubMed : 11596559 ]
- Papanicolas I. International frameworks for health system comparison. In: Papanicolas I, & Smith P (eds.), editors. Health system performance comparison: An agenda for policy, information and research. European Observatory on Health Systems and Policies, Open University Press; New York: 2013.
- Slawomirski L, Auraaen A, Klazinga N. The economics of patient safety. Paris: Organisation for Economic Co-operation and Development; 2017.
- The Council of Europe. The development and implementation of quality improvement systems (QIS) in health care. Recommendation No. R (97) 17 and explanatory memorandum. Strasbourg: The Council of Europe; 1997.
- WHO. Everybody’s business: Strengthening health systems to improve health outcomes: WHO’s framework for action. Geneva: World Health Organization; 2006a.
- WHO. Quality of care: a process for making strategic choices in health systems. Geneva: World Health Organization; 2006b.
- WHO. WHO global strategy on people centred and integrated health services. Interim Report. Geneva: World Health Organization; 2016.
- WHO. Handbook for national quality policy and strategy – A practical approach for developing policy and strategy to improve quality of care. Geneva: World Health Organization; 2018.
- WHO/OECD/World Bank. Delivering quality health services: a global imperative for universal health coverage. Geneva: World Health Organization, Organisation for Economic Co-operation and Development, and The World Bank; 2018. Licence: CC BY-NC-SA 3.0 IGO.
- Cite this Page Busse R, Panteli D, Quentin W. An introduction to healthcare quality: defining and explaining its role in health systems. In: Busse R, Klazinga N, Panteli D, et al., editors. Improving healthcare quality in Europe: Characteristics, effectiveness and implementation of different strategies [Internet]. Copenhagen (Denmark): European Observatory on Health Systems and Policies; 2019. (Health Policy Series, No. 53.) 1.
- PDF version of this title (4.8M)
In this Page
- The relevance of quality in health policy
- Definitions of healthcare quality
- Dimensions of healthcare quality
- The role of quality in health systems and health system performance assessment
- What are quality improvement strategies? Aims and structure of this book
Other titles in this collection
- European Observatory Health Policy Series
Related information
- PMC PubMed Central citations
- PubMed Links to PubMed
Recent Activity
- An introduction to healthcare quality: defining and explaining its role in healt... An introduction to healthcare quality: defining and explaining its role in health systems - Improving healthcare quality in Europe
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
Connect with NLM
National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894
Web Policies FOIA HHS Vulnerability Disclosure
Help Accessibility Careers
- MUSC Health MyChart
- Schedule an Appointment
- Adult Patient Care
- Children's Health
- Education at MUSC
- Research at MUSC
- Latest News
- E-cigarettes
Tobacco researchers suggest health care providers talk with adult patients who smoke about relative risks of tobacco products, including e-cigarettes

Health care providers who are working with adult patients struggling to stop smoking should consider discussing e-cigarettes as a potential tool if they’ve already tried FDA-approved medications, say tobacco researchers with MUSC Hollings Cancer Center .
Benjamin Toll, Ph.D. , director of the MUSC Health Tobacco Treatment Program , and Tracy Smith, Ph.D. , associate professor in the Addiction Sciences Division of the Department of Psychiatry and Behavioral Sciences, partnered with Brian King, Ph.D. , director of the Center for Tobacco Products at the U.S. Food and Drug Administration, to write a commentary in Nature Medicine that lays out the relative risk of e-cigarettes compared with traditional combustible cigarettes. Existing scientific evidence indicates that both products have health risks, but that e-cigarettes generally have lower risks than cigarettes.
To be clear – neither option is good for your health, Toll and Smith said. And they certainly don’t want any youth, or adults who don’t smoke, to take up e-cigarette use. But among adults who have already tried FDA-approved cessation medicines, if the choice is between continuing to smoke traditional cigarettes or switching completely to e-cigarettes, then a complete switch should be encouraged, they said. They were motivated to work with King to write this commentary because they saw confusion among the general public and doctors about the relative harms of each product.
“It really bothered me that there are well-intentioned, smart health care providers who think that e-cigarettes are worse than smoking cigarettes,” Toll said. “It’s simply not true.”
Toll, who is currently serving as president of the Society for Research on Nicotine and Tobacco, wanted to expand the conversation that health care providers can have with patients about ways to stop smoking.
There are seven FDA-approved smoking cessation aids, including medication and nicotine replacement options like the patch. These smoking cessation products, especially when combined with behavioral counseling, improve a person’s chances of quitting smoking. But because nicotine is so addictive, many people still struggle. That’s where Smith and Toll see a place for e-cigarettes.
“Doctors and other health care professionals don't know what to say or how to talk about it,” Smith said. “I always say, ‘If you have somebody who smokes cigarettes, they are standing in a convenience store every single day, buying the most harmful tobacco product they could possibly be buying.’ And it’s a real injustice not to say to them, ‘Hey, there are nicotine products you could buy every day that would be a whole lot less likely to kill you.’”
However, Toll and Smith are very specific about which types of e-cigarettes they’re referring to. When they say that e-cigarettes have fewer toxicants and cause less harm than cigarettes, they’re referring specifically to the 23 products that have received FDA authorization for marketing. It’s worth noting that all 23 of these products are tobacco-flavored, not fruity, chocolatey or candy-flavored.
Smith explained that the FDA created two paths for e-cigarette manufacturers to gain authorization. The first path would allow manufacturers to market their e-cigarettes as smoking cessation devices.
“Thus far, no company has done that – as far as we know, they have not even applied,” Smith said.
The second path allows companies to market their products as tobacco products, but makes no claims about smoking cessation. Companies have to show that their products are appropriate for the protection of public health – specifically, that the benefits of the product for helping adults who smoke to transition completely outweighs the known risk of these products to youth and nonusers.
Besides the likelihood that the product will entice young people, the FDA looks at everything from environmental impact to whether users completely switch to the e-cigarette product from cigarettes. Complete switching, rather than going back and forth between e-cigarettes and cigarettes, is an important factor. If people use both products – something that researchers call “dual use” – then they’re still exposing themselves to the carcinogens and toxicants in cigarettes.
“So far, the FDA has issued more than a million denials and 23 authorizations,” Smith said.
Due to the rigorous nature of the reviews, Smith and Toll believe that doctors can reasonably share that list of 23 authorized e-cigarettes with people who are struggling to stop smoking.
In addition, there’s increasing evidence suggesting that e-cigarettes can help adults who smoke to completely transition away from cigarettes, they said. Recent large-scale studies published in JAMA Internal Medicine and the New England Journal of Medicine showed that e-cigarettes helped people to stop smoking. Further, Smith said, a Cochrane Review conducted earlier this year concluded that there is evidence from enough high-quality studies to say that e-cigarettes are more likely to help people to quit than nicotine replacement therapy, which includes nicotine gum, nicotine lozenges and the patch.
E-cigarettes remain controversial though.
“Some believe that we shouldn’t be allowing new tobacco products on the market that could potentially be appealing to youth, no matter what the benefit is to adults who smoke. And I’m just not in that camp because cigarettes are the primary way that tobacco kills people,” Smith said. “For me, because cigarettes are responsible for the vast majority of the deaths and illnesses from tobacco, I think that having less harmful alternatives out there for adults, especially if we can reduce the appeal to youth, is really important.”

Vaping on the Rise
New research shows that, for the first time, there are more young people who begin to use nicotine through vaping rather than through cigarettes.
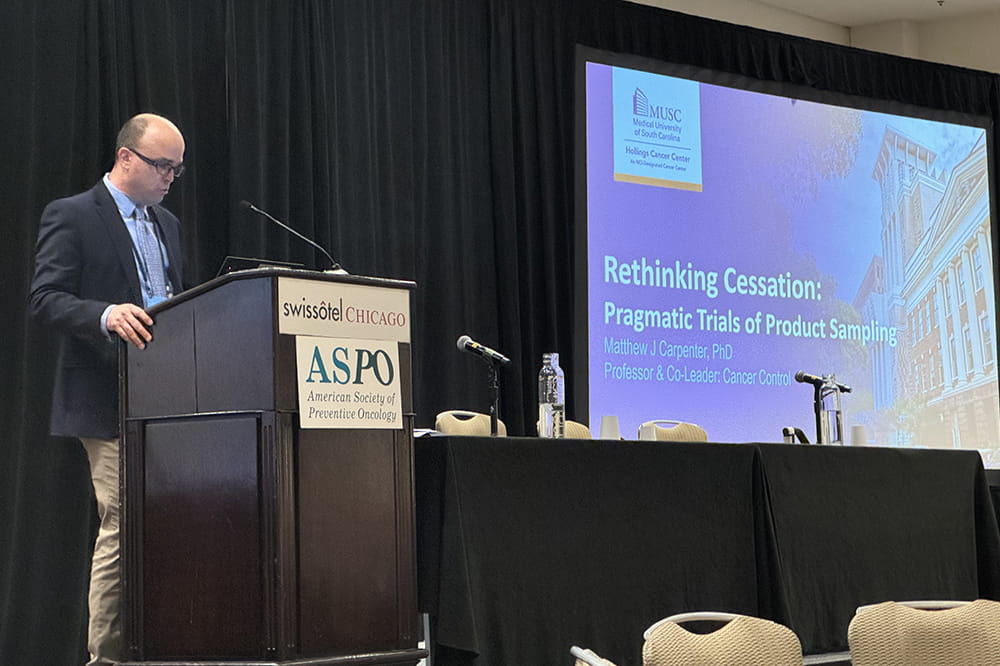
A tobacco researcher at MUSC Hollings Cancer Center was honored by the American Society of Preventive Oncology for his work.

Doll-Wynder Award
Dr. Michael Cummings was honored for the groundbreaking advances he's made over a 40-year career in tobacco control research.
Related Links
More MUSC Hollings Cancer Center news
Subscribe to our newsletter
Hollings Horizons magazine
About the Author
Leslie Cantu MUSC Hollings Cancer Center
Categories: Cancer , Influence , Research

IMAGES
VIDEO
COMMENTS
The growing adoption of continuous quality improvement (CQI) initiatives in healthcare has generated a surge in research interest to gain a deeper understanding of CQI. However, comprehensive evidence regarding the diverse facets of CQI in healthcare has been limited. Our review sought to comprehensively grasp the conceptualization and principles of CQI, explore existing models and tools ...
Abstract. Improving the quality of health care across a nation is complex and hard. Countries often rely on multiple single national level programmes to make progress. But the key is to use a framework to develop a balanced overall strategy, and evaluate the main elements continuously and over time. Achieving that requires having a critical ...
The foundation of quality healthcare is doing the right thing at the right time in the right way for the right person and having the best results possible. Quality healthcare often means striking the right balance when providing healthcare services by avoiding overuse (e.g., unnecessary tests), underuse (e.g., missed blood pressure screening), or misuse (e.g., prescribing of drugs with harmful ...
Health system quality has received much attention since The Lancet Global Health Commission on high quality health systems in 2018, which proposed new ways to define, measure, and improve the performance of health systems.1 Factors influencing quality of health systems are well known, both as inputs and processes, including WHO's six building blocks (service delivery, health workforce, health ...
The Journal for Healthcare Quality (JHQ), a peer-reviewed journal, is an official publication of the National Association for Healthcare Quality. JHQ is a professional forum that continuously advances healthcare quality practice in diverse and changing environments, and is the first choice for creative and scientific solutions in the pursuit of healthcare quality.
Within healthcare there is no universally accepted definition of 'quality', but those commonly used pick up on this multi-dimensionality. The following popular definition, from the US Institute of Medicine and also used by the World Health Organization, describes quality as 'the degree to which health services for individuals and populations increase the likelihood of desired health ...
Despite nearly two decades of experimentation with standardized measurement, public reporting, and reward-and-penalty programs, average quality performance in U.S. health care remains about the sam...
The Journal for Healthcare Quality (JHQ), a peer-reviewed journal, is an official publication of the National Association for Healthcare Quality. ... The Journal publishes scholarly articles that are targeted to leaders of all healthcare settings, leveraging applied research and producing practical, timely and impactful evidence in healthcare ...
Improving quality involves assessing process and outcome measures of safety, effectiveness, patient-centredness, timeliness, efficiency and equity, as well as strengthening the capacity of health systems and clinical practices to create and sustain an organisational culture of quality and safety (Institute of Medicine, 2001).This Perspectives piece highlights several promising topic areas in ...
Results. A total of 17 articles were identified. All studies reported a positive association between the use of benchmarking and quality improvement in terms of processes (N = 10), outcomes (N = 13) or both (N = 7).In the majority of studies (N = 12), at least one intervention, complementary to benchmarking, was undertaken to stimulate quality improvement.
Definitions of quality improvement. Improvement in patient outcomes, system performance, and professional development that results from a combined, multidisciplinary approach in how change is delivered. 3. The delivery of healthcare with improved outcomes and lower cost through continuous redesigning of work processes and systems. 4.
Artificial intelligence (AI) has the potential to transform care delivery by improving health outcomes, patient safety, and the affordability and accessibility of high-quality care. AI will be ...
Background. Quality improvement is the focus of senior managers and leaders in healthcare worldwide. While it rose to the forefront of the public's attention with the Institute of Medicine's (IOM) report (Institute of Medicine & Committee on Quality of Health Care in America Citation 2000), the emphasis on patient safety and quality of care is now central to all standards of care and ...
The quality of the healthcare system can be measured, for example, through: (a) the perceptions and satisfaction of patients, (b) the views of healthcare delivery professionals, or (c) a combination of the two ().The demand for greater patient-centric and volume-to-value delivery models makes the measurement of patient perceptions and experiences imperative despite underpinning complexities ...
Findings from health services research highlight continuing health care disparities in the United States, especially in the areas of access to health care and quality of care. Although attention to health care disparities has increased, considerable knowledge gaps still exist. A better understanding of how cultural, behavioral, and health system factors converge and contribute to unequal ...
The Agency for Healthcare Research and Quality's (AHRQ) mission is to produce evidence to make health care safer, higher quality, more accessible, equitable, and affordable, and to work within the U.S. Department of Health and Human Services and with other partners to make sure that the evidence is understood and used.
Previously published as. () is the official Journal of the Spanish Society of Quality Healthcare (Sociedad Española de Calidad Asistencial, SECA) and is a tool for the dissemination of knowledge and considerations about the quality management of health services. publishes articles in Spanish and English associated with any aspect of research ...
Various inclusion and exclusion criteria were used to select relevant research articles from 2000-2020 for the study, and a total of 100 research articles were selected.,The study identified 41 different dimensions of healthcare service quality measurement and classified these dimensions into four categories, namely servicescape, personnel ...
Quality in healthcare is a subject in need of continuous attention. Quality improvement (QI) programmes with the purpose of increasing service quality are therefore of priority for healthcare leaders and governments. This study explores the implementation process of two different QI programmes, one externally driven implementation and one internally driven, in Norwegian nursing homes and home ...
The Agency for Healthcare Research and Quality recently released a guide to help health systems and other stakeholders assess and advance equity in health care solutions that involve digital technologies. "Considerations ranging from a lack of patient digital literacy to a lack of broadband access, collectively referred to as the 'digital divide,' may impact the viability of healthcare ...
The COVID-19 pandemic shone a light on the work and needs of the healthcare workforce like never before, resulting in an increased focus of workforce well-being research, policy and within mainstream media. Despite this recent attention, the relevance of workforce well-being for healthcare delivery and efficiency is not a new phenomenon. The National Health Service (NHS) in England employs ...
What is Quality Improvement (QI)? Paul Batalden and Frank Davidoff, in 2008, described QI as "the combined and unceasing efforts of everyone—healthcare professionals, patients and their families, researchers, payers, planners and educators—to make the changes that will lead to better patient outcomes (health), better system performance (care) and better professional development" .
It's an idea as old as modern medicine and as new as the latest medical research. No matter how you look at health equity, the conversation involves contradictions. ... experts who have watched the conversation move from the fringes of scholarly debate to the mainstream of 21st century health care. The term can be abstract, but the facts are ...
The Agency for Healthcare Research and Quality (AHRQ), on behalf of the Department of Health and Human Services (HHS), has established the National Action Alliance for Patient and Workforce Safety as a public-private collaboration to improve both patient and workforce safety. The National Action Alliance is a partnership between HHS and its ...
Objective To identify factors acting as barriers or enablers to the process of healthcare consent for people with intellectual disability and to understand how to make this process equitable and accessible. Data sources Databases: Embase, MEDLINE, PsychINFO, PubMed, SCOPUS, Web of Science and CINAHL. Additional articles were obtained from an ancestral search and hand-searching three journals ...
Primary healthcare in South Africa aims to transform the national health system by emphasising community-based care and preventive strategies. However, rehabilitation services, particularly for individuals with disabilities and chronic non-communicable diseases, are often overlooked in primary healthcare. This study aimed to investigate the provision of primary healthcare rehabilitation ...
Although the difference between the two groups seems small, the researchers say erasing the gap could save 5,000 women's lives each year. The study included nearly 800,000 male and female ...
KFF Headquarters: 185 Berry St., Suite 2000, San Francisco, CA 94107 | Phone 650-854-9400 Washington Offices and Barbara Jordan Conference Center: 1330 G Street, NW, Washington, DC 20005 | Phone ...
Quality of care is one of the most frequently quoted principles of health policy, and it is currently high up on the agenda of policy-makers at national, European and international levels (EC, 2016; OECD, 2017; WHO, 2018; WHO/OECD/World Bank, 2018). At the national level, addressing the issue of healthcare quality may be motivated by various reasons - ranging from a general commitment to ...
Health care providers who are working with adult patients struggling to stop smoking should consider discussing e-cigarettes as a potential tool if they've already tried FDA-approved medications, say tobacco researchers with MUSC Hollings Cancer Center.. Benjamin Toll, Ph.D., director of the MUSC Health Tobacco Treatment Program, and Tracy Smith, Ph.D., associate professor in the Addiction ...