

Introduction to qualitative nursing research
This type of research can reveal important information that quantitative research can’t.
- Qualitative research is valuable because it approaches a phenomenon, such as a clinical problem, about which little is known by trying to understand its many facets.
- Most qualitative research is emergent, holistic, detailed, and uses many strategies to collect data.
- Qualitative research generates evidence and helps nurses determine patient preferences.
Research 101: Descriptive statistics
Differentiating research, evidence-based practice, and quality improvement
How to appraise quantitative research articles
All nurses are expected to understand and apply evidence to their professional practice. Some of the evidence should be in the form of research, which fills gaps in knowledge, developing and expanding on current understanding. Both quantitative and qualitative research methods inform nursing practice, but quantitative research tends to be more emphasized. In addition, many nurses don’t feel comfortable conducting or evaluating qualitative research. But once you understand qualitative research, you can more easily apply it to your nursing practice.
What is qualitative research?
Defining qualitative research can be challenging. In fact, some authors suggest that providing a simple definition is contrary to the method’s philosophy. Qualitative research approaches a phenomenon, such as a clinical problem, from a place of unknowing and attempts to understand its many facets. This makes qualitative research particularly useful when little is known about a phenomenon because the research helps identify key concepts and constructs. Qualitative research sets the foundation for future quantitative or qualitative research. Qualitative research also can stand alone without quantitative research.
Although qualitative research is diverse, certain characteristics—holism, subjectivity, intersubjectivity, and situated contexts—guide its methodology. This type of research stresses the importance of studying each individual as a holistic system (holism) influenced by surroundings (situated contexts); each person develops his or her own subjective world (subjectivity) that’s influenced by interactions with others (intersubjectivity) and surroundings (situated contexts). Think of it this way: Each person experiences and interprets the world differently based on many factors, including his or her history and interactions. The truth is a composite of realities.
Qualitative research designs
Because qualitative research explores diverse topics and examines phenomena where little is known, designs and methodologies vary. Despite this variation, most qualitative research designs are emergent and holistic. In addition, they require merging data collection strategies and an intensely involved researcher. (See Research design characteristics .)
Although qualitative research designs are emergent, advanced planning and careful consideration should include identifying a phenomenon of interest, selecting a research design, indicating broad data collection strategies and opportunities to enhance study quality, and considering and/or setting aside (bracketing) personal biases, views, and assumptions.
Many qualitative research designs are used in nursing. Most originated in other disciplines, while some claim no link to a particular disciplinary tradition. Designs that aren’t linked to a discipline, such as descriptive designs, may borrow techniques from other methodologies; some authors don’t consider them to be rigorous (high-quality and trustworthy). (See Common qualitative research designs .)
Sampling approaches
Sampling approaches depend on the qualitative research design selected. However, in general, qualitative samples are small, nonrandom, emergently selected, and intensely studied. Qualitative research sampling is concerned with accurately representing and discovering meaning in experience, rather than generalizability. For this reason, researchers tend to look for participants or informants who are considered “information rich” because they maximize understanding by representing varying demographics and/or ranges of experiences. As a study progresses, researchers look for participants who confirm, challenge, modify, or enrich understanding of the phenomenon of interest. Many authors argue that the concepts and constructs discovered in qualitative research transcend a particular study, however, and find applicability to others. For example, consider a qualitative study about the lived experience of minority nursing faculty and the incivility they endure. The concepts learned in this study may transcend nursing or minority faculty members and also apply to other populations, such as foreign-born students, nurses, or faculty.
Qualitative nursing research can take many forms. The design you choose will depend on the question you’re trying to answer.
A sample size is estimated before a qualitative study begins, but the final sample size depends on the study scope, data quality, sensitivity of the research topic or phenomenon of interest, and researchers’ skills. For example, a study with a narrow scope, skilled researchers, and a nonsensitive topic likely will require a smaller sample. Data saturation frequently is a key consideration in final sample size. When no new insights or information are obtained, data saturation is attained and sampling stops, although researchers may analyze one or two more cases to be certain. (See Sampling types .)
Some controversy exists around the concept of saturation in qualitative nursing research. Thorne argues that saturation is a concept appropriate for grounded theory studies and not other study types. She suggests that “information power” is perhaps more appropriate terminology for qualitative nursing research sampling and sample size.
Data collection and analysis
Researchers are guided by their study design when choosing data collection and analysis methods. Common types of data collection include interviews (unstructured, semistructured, focus groups); observations of people, environments, or contexts; documents; records; artifacts; photographs; or journals. When collecting data, researchers must be mindful of gaining participant trust while also guarding against too much emotional involvement, ensuring comprehensive data collection and analysis, conducting appropriate data management, and engaging in reflexivity.

Data usually are recorded in detailed notes, memos, and audio or visual recordings, which frequently are transcribed verbatim and analyzed manually or using software programs, such as ATLAS.ti, HyperRESEARCH, MAXQDA, or NVivo. Analyzing qualitative data is complex work. Researchers act as reductionists, distilling enormous amounts of data into concise yet rich and valuable knowledge. They code or identify themes, translating abstract ideas into meaningful information. The good news is that qualitative research typically is easy to understand because it’s reported in stories told in everyday language.
Evaluating a qualitative study
Evaluating qualitative research studies can be challenging. Many terms—rigor, validity, integrity, and trustworthiness—can describe study quality, but in the end you want to know whether the study’s findings accurately and comprehensively represent the phenomenon of interest. Many researchers identify a quality framework when discussing quality-enhancement strategies. Example frameworks include:
- Trustworthiness criteria framework, which enhances credibility, dependability, confirmability, transferability, and authenticity
- Validity in qualitative research framework, which enhances credibility, authenticity, criticality, integrity, explicitness, vividness, creativity, thoroughness, congruence, and sensitivity.
With all frameworks, many strategies can be used to help meet identified criteria and enhance quality. (See Research quality enhancement ). And considering the study as a whole is important to evaluating its quality and rigor. For example, when looking for evidence of rigor, look for a clear and concise report title that describes the research topic and design and an abstract that summarizes key points (background, purpose, methods, results, conclusions).
Application to nursing practice
Qualitative research not only generates evidence but also can help nurses determine patient preferences. Without qualitative research, we can’t truly understand others, including their interpretations, meanings, needs, and wants. Qualitative research isn’t generalizable in the traditional sense, but it helps nurses open their minds to others’ experiences. For example, nurses can protect patient autonomy by understanding them and not reducing them to universal protocols or plans. As Munhall states, “Each person we encounter help[s] us discover what is best for [him or her]. The other person, not us, is truly the expert knower of [him- or herself].” Qualitative nursing research helps us understand the complexity and many facets of a problem and gives us insights as we encourage others’ voices and searches for meaning.

When paired with clinical judgment and other evidence, qualitative research helps us implement evidence-based practice successfully. For example, a phenomenological inquiry into the lived experience of disaster workers might help expose strengths and weaknesses of individuals, populations, and systems, providing areas of focused intervention. Or a phenomenological study of the lived experience of critical-care patients might expose factors (such dark rooms or no visible clocks) that contribute to delirium.
Successful implementation
Qualitative nursing research guides understanding in practice and sets the foundation for future quantitative and qualitative research. Knowing how to conduct and evaluate qualitative research can help nurses implement evidence-based practice successfully.
When evaluating a qualitative study, you should consider it as a whole. The following questions to consider when examining study quality and evidence of rigor are adapted from the Standards for Reporting Qualitative Research.
Jennifer Chicca is a PhD candidate at the Indiana University of Pennsylvania in Indiana, Pennsylvania, and a part-time faculty member at the University of North Carolina Wilmington.
Amankwaa L. Creating protocols for trustworthiness in qualitative research. J Cult Divers. 2016;23(3):121-7.
Cuthbert CA, Moules N. The application of qualitative research findings to oncology nursing practice. Oncol Nurs Forum . 2014;41(6):683-5.
Guba E, Lincoln Y. Competing paradigms in qualitative research . In: Denzin NK, Lincoln YS, eds. Handbook of Qualitative Research. Thousand Oaks, CA: SAGE Publications, Inc.;1994: 105-17.
Lincoln YS, Guba EG. Naturalistic Inquiry . Thousand Oaks, CA: SAGE Publications, Inc.; 1985.
Munhall PL. Nursing Research: A Qualitative Perspective . 5th ed. Sudbury, MA: Jones & Bartlett Learning; 2012.
Nicholls D. Qualitative research. Part 1: Philosophies. Int J Ther Rehabil . 2017;24(1):26-33.
Nicholls D. Qualitative research. Part 2: Methodology. Int J Ther Rehabil . 2017;24(2):71-7.
Nicholls D. Qualitative research. Part 3: Methods. Int J Ther Rehabil . 2017;24(3):114-21.
O’Brien BC, Harris IB, Beckman TJ, Reed DA, Cook DA. Standards for reporting qualitative research: A synthesis of recommendations. Acad Med . 2014;89(9):1245-51.
Polit DF, Beck CT. Nursing Research: Generating and Assessing Evidence for Nursing Practice . 10th ed. Philadelphia, PA: Wolters Kluwer; 2017.
Thorne S. Saturation in qualitative nursing studies: Untangling the misleading message around saturation in qualitative nursing studies. Nurse Auth Ed. 2020;30(1):5. naepub.com/reporting-research/2020-30-1-5
Whittemore R, Chase SK, Mandle CL. Validity in qualitative research. Qual Health Res . 2001;11(4):522-37.
Williams B. Understanding qualitative research. Am Nurse Today . 2015;10(7):40-2.
Leave a Reply Cancel reply
Your email address will not be published. Required fields are marked *
Post Comment

NurseLine Newsletter
- First Name *
- Last Name *
- Hidden Referrer
*By submitting your e-mail, you are opting in to receiving information from Healthcom Media and Affiliates. The details, including your email address/mobile number, may be used to keep you informed about future products and services.
Test Your Knowledge
Recent posts.

Bird Flu Is Bad for Poultry and Dairy Cows. It’s Not a Dire Threat for Most of Us — Yet.

Virtual reality: Treating pain and anxiety

What is a healthy nurse?

Broken trust

Diabetes innovations and access to care

Breaking barriers: Nursing education in a wheelchair

Nearly 100 measles cases reported in the first quarter, CDC says

Infections after surgery are more likely due to bacteria already on your skin than from microbes in the hospital − new research

Honoring our veterans

Supporting the multi-generational nursing workforce

Vital practitioners

From data to action

Many travel nurses opt for temporary assignments because of the autonomy and opportunities − not just the big boost in pay

Effective clinical learning for nursing students

Nurse safety in the era of open notes
Log in using your username and password
- Search More Search for this keyword Advanced search
- Latest content
- Current issue
- Write for Us
- BMJ Journals More You are viewing from: Google Indexer
You are here
- Volume 21, Issue 3
- Data collection in qualitative research
- Article Text
- Article info
- Citation Tools
- Rapid Responses
- Article metrics
- David Barrett 1 ,
- http://orcid.org/0000-0003-1130-5603 Alison Twycross 2
- 1 Faculty of Health Sciences , University of Hull , Hull , UK
- 2 School of Health and Social Care , London South Bank University , London , UK
- Correspondence to Dr David Barrett, Faculty of Health Sciences, University of Hull, Hull HU6 7RX, UK; D.I.Barrett{at}hull.ac.uk
https://doi.org/10.1136/eb-2018-102939
Statistics from Altmetric.com
Request permissions.
If you wish to reuse any or all of this article please use the link below which will take you to the Copyright Clearance Center’s RightsLink service. You will be able to get a quick price and instant permission to reuse the content in many different ways.
Qualitative research methods allow us to better understand the experiences of patients and carers; they allow us to explore how decisions are made and provide us with a detailed insight into how interventions may alter care. To develop such insights, qualitative research requires data which are holistic, rich and nuanced, allowing themes and findings to emerge through careful analysis. This article provides an overview of the core approaches to data collection in qualitative research, exploring their strengths, weaknesses and challenges.
Collecting data through interviews with participants is a characteristic of many qualitative studies. Interviews give the most direct and straightforward approach to gathering detailed and rich data regarding a particular phenomenon. The type of interview used to collect data can be tailored to the research question, the characteristics of participants and the preferred approach of the researcher. Interviews are most often carried out face-to-face, though the use of telephone interviews to overcome geographical barriers to participant recruitment is becoming more prevalent. 1
A common approach in qualitative research is the semistructured interview, where core elements of the phenomenon being studied are explicitly asked about by the interviewer. A well-designed semistructured interview should ensure data are captured in key areas while still allowing flexibility for participants to bring their own personality and perspective to the discussion. Finally, interviews can be much more rigidly structured to provide greater control for the researcher, essentially becoming questionnaires where responses are verbal rather than written.
Deciding where to place an interview design on this ‘structural spectrum’ will depend on the question to be answered and the skills of the researcher. A very structured approach is easy to administer and analyse but may not allow the participant to express themselves fully. At the other end of the spectrum, an open approach allows for freedom and flexibility, but requires the researcher to walk an investigative tightrope that maintains the focus of an interview without forcing participants into particular areas of discussion.
Example of an interview schedule 3
What do you think is the most effective way of assessing a child’s pain?
Have you come across any issues that make it difficult to assess a child’s pain?
What pain-relieving interventions do you find most useful and why?
When managing pain in children what is your overall aim?
Whose responsibility is pain management?
What involvement do you think parents should have in their child’s pain management?
What involvement do children have in their pain management?
Is there anything that currently stops you managing pain as well as you would like?
What would help you manage pain better?
Interviews present several challenges to researchers. Most interviews are recorded and will need transcribing before analysing. This can be extremely time-consuming, with 1 hour of interview requiring 5–6 hours to transcribe. 4 The analysis itself is also time-consuming, requiring transcriptions to be pored over word-for-word and line-by-line. Interviews also present the problem of bias the researcher needs to take care to avoid leading questions or providing non-verbal signals that might influence the responses of participants.
Focus groups
The focus group is a method of data collection in which a moderator/facilitator (usually a coresearcher) speaks with a group of 6–12 participants about issues related to the research question. As an approach, the focus group offers qualitative researchers an efficient method of gathering the views of many participants at one time. Also, the fact that many people are discussing the same issue together can result in an enhanced level of debate, with the moderator often able to step back and let the focus group enter into a free-flowing discussion. 5 This provides an opportunity to gather rich data from a specific population about a particular area of interest, such as barriers perceived by student nurses when trying to communicate with patients with cancer. 6
From a participant perspective, the focus group may provide a more relaxing environment than a one-to-one interview; they will not need to be involved with every part of the discussion and may feel more comfortable expressing views when they are shared by others in the group. Focus groups also allow participants to ‘bounce’ ideas off each other which sometimes results in different perspectives emerging from the discussion. However, focus groups are not without their difficulties. As with interviews, focus groups provide a vast amount of data to be transcribed and analysed, with discussions often lasting 1–2 hours. Moderators also need to be highly skilled to ensure that the discussion can flow while remaining focused and that all participants are encouraged to speak, while ensuring that no individuals dominate the discussion. 7
Observation
Participant and non-participant observation are powerful tools for collecting qualitative data, as they give nurse researchers an opportunity to capture a wide array of information—such as verbal and non-verbal communication, actions (eg, techniques of providing care) and environmental factors—within a care setting. Another advantage of observation is that the researcher gains a first-hand picture of what actually happens in clinical practice. 8 If the researcher is adopting a qualitative approach to observation they will normally record field notes . Field notes can take many forms, such as a chronological log of what is happening in the setting, a description of what has been observed, a record of conversations with participants or an expanded account of impressions from the fieldwork. 9 10
As with other qualitative data collection techniques, observation provides an enormous amount of data to be captured and analysed—one approach to helping with collection and analysis is to digitally record observations to allow for repeated viewing. 11 Observation also provides the researcher with some unique methodological and ethical challenges. Methodologically, the act of being observed may change the behaviour of the participant (often referred to as the ‘Hawthorne effect’), impacting on the value of findings. However, most researchers report a process of habitation taking place where, after a relatively short period of time, those being observed revert to their normal behaviour. Ethically, the researcher will need to consider when and how they should intervene if they view poor practice that could put patients at risk.
The three core approaches to data collection in qualitative research—interviews, focus groups and observation—provide researchers with rich and deep insights. All methods require skill on the part of the researcher, and all produce a large amount of raw data. However, with careful and systematic analysis 12 the data yielded with these methods will allow researchers to develop a detailed understanding of patient experiences and the work of nurses.
- Twycross AM ,
- Williams AM ,
- Huang MC , et al
- Onwuegbuzie AJ ,
- Dickinson WB ,
- Leech NL , et al
- Twycross A ,
- Emerson RM ,
- Meriläinen M ,
- Ala-Kokko T
Competing interests None declared.
Patient consent Not required.
Provenance and peer review Commissioned; internally peer reviewed.
Read the full text or download the PDF:
- Open access
- Published: 27 May 2020
How to use and assess qualitative research methods
- Loraine Busetto ORCID: orcid.org/0000-0002-9228-7875 1 ,
- Wolfgang Wick 1 , 2 &
- Christoph Gumbinger 1
Neurological Research and Practice volume 2 , Article number: 14 ( 2020 ) Cite this article
728k Accesses
293 Citations
85 Altmetric
Metrics details
This paper aims to provide an overview of the use and assessment of qualitative research methods in the health sciences. Qualitative research can be defined as the study of the nature of phenomena and is especially appropriate for answering questions of why something is (not) observed, assessing complex multi-component interventions, and focussing on intervention improvement. The most common methods of data collection are document study, (non-) participant observations, semi-structured interviews and focus groups. For data analysis, field-notes and audio-recordings are transcribed into protocols and transcripts, and coded using qualitative data management software. Criteria such as checklists, reflexivity, sampling strategies, piloting, co-coding, member-checking and stakeholder involvement can be used to enhance and assess the quality of the research conducted. Using qualitative in addition to quantitative designs will equip us with better tools to address a greater range of research problems, and to fill in blind spots in current neurological research and practice.
The aim of this paper is to provide an overview of qualitative research methods, including hands-on information on how they can be used, reported and assessed. This article is intended for beginning qualitative researchers in the health sciences as well as experienced quantitative researchers who wish to broaden their understanding of qualitative research.
What is qualitative research?
Qualitative research is defined as “the study of the nature of phenomena”, including “their quality, different manifestations, the context in which they appear or the perspectives from which they can be perceived” , but excluding “their range, frequency and place in an objectively determined chain of cause and effect” [ 1 ]. This formal definition can be complemented with a more pragmatic rule of thumb: qualitative research generally includes data in form of words rather than numbers [ 2 ].
Why conduct qualitative research?
Because some research questions cannot be answered using (only) quantitative methods. For example, one Australian study addressed the issue of why patients from Aboriginal communities often present late or not at all to specialist services offered by tertiary care hospitals. Using qualitative interviews with patients and staff, it found one of the most significant access barriers to be transportation problems, including some towns and communities simply not having a bus service to the hospital [ 3 ]. A quantitative study could have measured the number of patients over time or even looked at possible explanatory factors – but only those previously known or suspected to be of relevance. To discover reasons for observed patterns, especially the invisible or surprising ones, qualitative designs are needed.
While qualitative research is common in other fields, it is still relatively underrepresented in health services research. The latter field is more traditionally rooted in the evidence-based-medicine paradigm, as seen in " research that involves testing the effectiveness of various strategies to achieve changes in clinical practice, preferably applying randomised controlled trial study designs (...) " [ 4 ]. This focus on quantitative research and specifically randomised controlled trials (RCT) is visible in the idea of a hierarchy of research evidence which assumes that some research designs are objectively better than others, and that choosing a "lesser" design is only acceptable when the better ones are not practically or ethically feasible [ 5 , 6 ]. Others, however, argue that an objective hierarchy does not exist, and that, instead, the research design and methods should be chosen to fit the specific research question at hand – "questions before methods" [ 2 , 7 , 8 , 9 ]. This means that even when an RCT is possible, some research problems require a different design that is better suited to addressing them. Arguing in JAMA, Berwick uses the example of rapid response teams in hospitals, which he describes as " a complex, multicomponent intervention – essentially a process of social change" susceptible to a range of different context factors including leadership or organisation history. According to him, "[in] such complex terrain, the RCT is an impoverished way to learn. Critics who use it as a truth standard in this context are incorrect" [ 8 ] . Instead of limiting oneself to RCTs, Berwick recommends embracing a wider range of methods , including qualitative ones, which for "these specific applications, (...) are not compromises in learning how to improve; they are superior" [ 8 ].
Research problems that can be approached particularly well using qualitative methods include assessing complex multi-component interventions or systems (of change), addressing questions beyond “what works”, towards “what works for whom when, how and why”, and focussing on intervention improvement rather than accreditation [ 7 , 9 , 10 , 11 , 12 ]. Using qualitative methods can also help shed light on the “softer” side of medical treatment. For example, while quantitative trials can measure the costs and benefits of neuro-oncological treatment in terms of survival rates or adverse effects, qualitative research can help provide a better understanding of patient or caregiver stress, visibility of illness or out-of-pocket expenses.
How to conduct qualitative research?
Given that qualitative research is characterised by flexibility, openness and responsivity to context, the steps of data collection and analysis are not as separate and consecutive as they tend to be in quantitative research [ 13 , 14 ]. As Fossey puts it : “sampling, data collection, analysis and interpretation are related to each other in a cyclical (iterative) manner, rather than following one after another in a stepwise approach” [ 15 ]. The researcher can make educated decisions with regard to the choice of method, how they are implemented, and to which and how many units they are applied [ 13 ]. As shown in Fig. 1 , this can involve several back-and-forth steps between data collection and analysis where new insights and experiences can lead to adaption and expansion of the original plan. Some insights may also necessitate a revision of the research question and/or the research design as a whole. The process ends when saturation is achieved, i.e. when no relevant new information can be found (see also below: sampling and saturation). For reasons of transparency, it is essential for all decisions as well as the underlying reasoning to be well-documented.
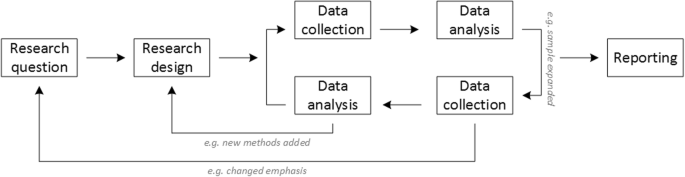
Iterative research process
While it is not always explicitly addressed, qualitative methods reflect a different underlying research paradigm than quantitative research (e.g. constructivism or interpretivism as opposed to positivism). The choice of methods can be based on the respective underlying substantive theory or theoretical framework used by the researcher [ 2 ].
Data collection
The methods of qualitative data collection most commonly used in health research are document study, observations, semi-structured interviews and focus groups [ 1 , 14 , 16 , 17 ].
Document study
Document study (also called document analysis) refers to the review by the researcher of written materials [ 14 ]. These can include personal and non-personal documents such as archives, annual reports, guidelines, policy documents, diaries or letters.
Observations
Observations are particularly useful to gain insights into a certain setting and actual behaviour – as opposed to reported behaviour or opinions [ 13 ]. Qualitative observations can be either participant or non-participant in nature. In participant observations, the observer is part of the observed setting, for example a nurse working in an intensive care unit [ 18 ]. In non-participant observations, the observer is “on the outside looking in”, i.e. present in but not part of the situation, trying not to influence the setting by their presence. Observations can be planned (e.g. for 3 h during the day or night shift) or ad hoc (e.g. as soon as a stroke patient arrives at the emergency room). During the observation, the observer takes notes on everything or certain pre-determined parts of what is happening around them, for example focusing on physician-patient interactions or communication between different professional groups. Written notes can be taken during or after the observations, depending on feasibility (which is usually lower during participant observations) and acceptability (e.g. when the observer is perceived to be judging the observed). Afterwards, these field notes are transcribed into observation protocols. If more than one observer was involved, field notes are taken independently, but notes can be consolidated into one protocol after discussions. Advantages of conducting observations include minimising the distance between the researcher and the researched, the potential discovery of topics that the researcher did not realise were relevant and gaining deeper insights into the real-world dimensions of the research problem at hand [ 18 ].
Semi-structured interviews
Hijmans & Kuyper describe qualitative interviews as “an exchange with an informal character, a conversation with a goal” [ 19 ]. Interviews are used to gain insights into a person’s subjective experiences, opinions and motivations – as opposed to facts or behaviours [ 13 ]. Interviews can be distinguished by the degree to which they are structured (i.e. a questionnaire), open (e.g. free conversation or autobiographical interviews) or semi-structured [ 2 , 13 ]. Semi-structured interviews are characterized by open-ended questions and the use of an interview guide (or topic guide/list) in which the broad areas of interest, sometimes including sub-questions, are defined [ 19 ]. The pre-defined topics in the interview guide can be derived from the literature, previous research or a preliminary method of data collection, e.g. document study or observations. The topic list is usually adapted and improved at the start of the data collection process as the interviewer learns more about the field [ 20 ]. Across interviews the focus on the different (blocks of) questions may differ and some questions may be skipped altogether (e.g. if the interviewee is not able or willing to answer the questions or for concerns about the total length of the interview) [ 20 ]. Qualitative interviews are usually not conducted in written format as it impedes on the interactive component of the method [ 20 ]. In comparison to written surveys, qualitative interviews have the advantage of being interactive and allowing for unexpected topics to emerge and to be taken up by the researcher. This can also help overcome a provider or researcher-centred bias often found in written surveys, which by nature, can only measure what is already known or expected to be of relevance to the researcher. Interviews can be audio- or video-taped; but sometimes it is only feasible or acceptable for the interviewer to take written notes [ 14 , 16 , 20 ].
Focus groups
Focus groups are group interviews to explore participants’ expertise and experiences, including explorations of how and why people behave in certain ways [ 1 ]. Focus groups usually consist of 6–8 people and are led by an experienced moderator following a topic guide or “script” [ 21 ]. They can involve an observer who takes note of the non-verbal aspects of the situation, possibly using an observation guide [ 21 ]. Depending on researchers’ and participants’ preferences, the discussions can be audio- or video-taped and transcribed afterwards [ 21 ]. Focus groups are useful for bringing together homogeneous (to a lesser extent heterogeneous) groups of participants with relevant expertise and experience on a given topic on which they can share detailed information [ 21 ]. Focus groups are a relatively easy, fast and inexpensive method to gain access to information on interactions in a given group, i.e. “the sharing and comparing” among participants [ 21 ]. Disadvantages include less control over the process and a lesser extent to which each individual may participate. Moreover, focus group moderators need experience, as do those tasked with the analysis of the resulting data. Focus groups can be less appropriate for discussing sensitive topics that participants might be reluctant to disclose in a group setting [ 13 ]. Moreover, attention must be paid to the emergence of “groupthink” as well as possible power dynamics within the group, e.g. when patients are awed or intimidated by health professionals.
Choosing the “right” method
As explained above, the school of thought underlying qualitative research assumes no objective hierarchy of evidence and methods. This means that each choice of single or combined methods has to be based on the research question that needs to be answered and a critical assessment with regard to whether or to what extent the chosen method can accomplish this – i.e. the “fit” between question and method [ 14 ]. It is necessary for these decisions to be documented when they are being made, and to be critically discussed when reporting methods and results.
Let us assume that our research aim is to examine the (clinical) processes around acute endovascular treatment (EVT), from the patient’s arrival at the emergency room to recanalization, with the aim to identify possible causes for delay and/or other causes for sub-optimal treatment outcome. As a first step, we could conduct a document study of the relevant standard operating procedures (SOPs) for this phase of care – are they up-to-date and in line with current guidelines? Do they contain any mistakes, irregularities or uncertainties that could cause delays or other problems? Regardless of the answers to these questions, the results have to be interpreted based on what they are: a written outline of what care processes in this hospital should look like. If we want to know what they actually look like in practice, we can conduct observations of the processes described in the SOPs. These results can (and should) be analysed in themselves, but also in comparison to the results of the document analysis, especially as regards relevant discrepancies. Do the SOPs outline specific tests for which no equipment can be observed or tasks to be performed by specialized nurses who are not present during the observation? It might also be possible that the written SOP is outdated, but the actual care provided is in line with current best practice. In order to find out why these discrepancies exist, it can be useful to conduct interviews. Are the physicians simply not aware of the SOPs (because their existence is limited to the hospital’s intranet) or do they actively disagree with them or does the infrastructure make it impossible to provide the care as described? Another rationale for adding interviews is that some situations (or all of their possible variations for different patient groups or the day, night or weekend shift) cannot practically or ethically be observed. In this case, it is possible to ask those involved to report on their actions – being aware that this is not the same as the actual observation. A senior physician’s or hospital manager’s description of certain situations might differ from a nurse’s or junior physician’s one, maybe because they intentionally misrepresent facts or maybe because different aspects of the process are visible or important to them. In some cases, it can also be relevant to consider to whom the interviewee is disclosing this information – someone they trust, someone they are otherwise not connected to, or someone they suspect or are aware of being in a potentially “dangerous” power relationship to them. Lastly, a focus group could be conducted with representatives of the relevant professional groups to explore how and why exactly they provide care around EVT. The discussion might reveal discrepancies (between SOPs and actual care or between different physicians) and motivations to the researchers as well as to the focus group members that they might not have been aware of themselves. For the focus group to deliver relevant information, attention has to be paid to its composition and conduct, for example, to make sure that all participants feel safe to disclose sensitive or potentially problematic information or that the discussion is not dominated by (senior) physicians only. The resulting combination of data collection methods is shown in Fig. 2 .
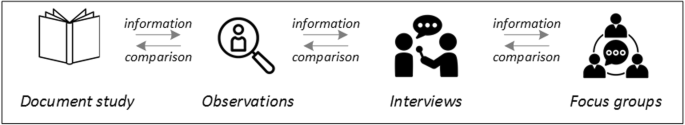
Possible combination of data collection methods
Attributions for icons: “Book” by Serhii Smirnov, “Interview” by Adrien Coquet, FR, “Magnifying Glass” by anggun, ID, “Business communication” by Vectors Market; all from the Noun Project
The combination of multiple data source as described for this example can be referred to as “triangulation”, in which multiple measurements are carried out from different angles to achieve a more comprehensive understanding of the phenomenon under study [ 22 , 23 ].
Data analysis
To analyse the data collected through observations, interviews and focus groups these need to be transcribed into protocols and transcripts (see Fig. 3 ). Interviews and focus groups can be transcribed verbatim , with or without annotations for behaviour (e.g. laughing, crying, pausing) and with or without phonetic transcription of dialects and filler words, depending on what is expected or known to be relevant for the analysis. In the next step, the protocols and transcripts are coded , that is, marked (or tagged, labelled) with one or more short descriptors of the content of a sentence or paragraph [ 2 , 15 , 23 ]. Jansen describes coding as “connecting the raw data with “theoretical” terms” [ 20 ]. In a more practical sense, coding makes raw data sortable. This makes it possible to extract and examine all segments describing, say, a tele-neurology consultation from multiple data sources (e.g. SOPs, emergency room observations, staff and patient interview). In a process of synthesis and abstraction, the codes are then grouped, summarised and/or categorised [ 15 , 20 ]. The end product of the coding or analysis process is a descriptive theory of the behavioural pattern under investigation [ 20 ]. The coding process is performed using qualitative data management software, the most common ones being InVivo, MaxQDA and Atlas.ti. It should be noted that these are data management tools which support the analysis performed by the researcher(s) [ 14 ].
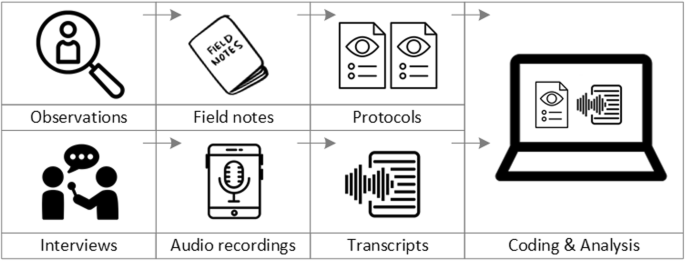
From data collection to data analysis
Attributions for icons: see Fig. 2 , also “Speech to text” by Trevor Dsouza, “Field Notes” by Mike O’Brien, US, “Voice Record” by ProSymbols, US, “Inspection” by Made, AU, and “Cloud” by Graphic Tigers; all from the Noun Project
How to report qualitative research?
Protocols of qualitative research can be published separately and in advance of the study results. However, the aim is not the same as in RCT protocols, i.e. to pre-define and set in stone the research questions and primary or secondary endpoints. Rather, it is a way to describe the research methods in detail, which might not be possible in the results paper given journals’ word limits. Qualitative research papers are usually longer than their quantitative counterparts to allow for deep understanding and so-called “thick description”. In the methods section, the focus is on transparency of the methods used, including why, how and by whom they were implemented in the specific study setting, so as to enable a discussion of whether and how this may have influenced data collection, analysis and interpretation. The results section usually starts with a paragraph outlining the main findings, followed by more detailed descriptions of, for example, the commonalities, discrepancies or exceptions per category [ 20 ]. Here it is important to support main findings by relevant quotations, which may add information, context, emphasis or real-life examples [ 20 , 23 ]. It is subject to debate in the field whether it is relevant to state the exact number or percentage of respondents supporting a certain statement (e.g. “Five interviewees expressed negative feelings towards XYZ”) [ 21 ].
How to combine qualitative with quantitative research?
Qualitative methods can be combined with other methods in multi- or mixed methods designs, which “[employ] two or more different methods [ …] within the same study or research program rather than confining the research to one single method” [ 24 ]. Reasons for combining methods can be diverse, including triangulation for corroboration of findings, complementarity for illustration and clarification of results, expansion to extend the breadth and range of the study, explanation of (unexpected) results generated with one method with the help of another, or offsetting the weakness of one method with the strength of another [ 1 , 17 , 24 , 25 , 26 ]. The resulting designs can be classified according to when, why and how the different quantitative and/or qualitative data strands are combined. The three most common types of mixed method designs are the convergent parallel design , the explanatory sequential design and the exploratory sequential design. The designs with examples are shown in Fig. 4 .
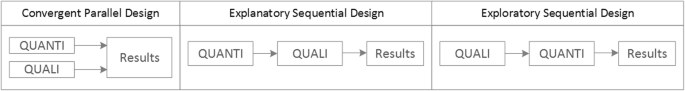
Three common mixed methods designs
In the convergent parallel design, a qualitative study is conducted in parallel to and independently of a quantitative study, and the results of both studies are compared and combined at the stage of interpretation of results. Using the above example of EVT provision, this could entail setting up a quantitative EVT registry to measure process times and patient outcomes in parallel to conducting the qualitative research outlined above, and then comparing results. Amongst other things, this would make it possible to assess whether interview respondents’ subjective impressions of patients receiving good care match modified Rankin Scores at follow-up, or whether observed delays in care provision are exceptions or the rule when compared to door-to-needle times as documented in the registry. In the explanatory sequential design, a quantitative study is carried out first, followed by a qualitative study to help explain the results from the quantitative study. This would be an appropriate design if the registry alone had revealed relevant delays in door-to-needle times and the qualitative study would be used to understand where and why these occurred, and how they could be improved. In the exploratory design, the qualitative study is carried out first and its results help informing and building the quantitative study in the next step [ 26 ]. If the qualitative study around EVT provision had shown a high level of dissatisfaction among the staff members involved, a quantitative questionnaire investigating staff satisfaction could be set up in the next step, informed by the qualitative study on which topics dissatisfaction had been expressed. Amongst other things, the questionnaire design would make it possible to widen the reach of the research to more respondents from different (types of) hospitals, regions, countries or settings, and to conduct sub-group analyses for different professional groups.
How to assess qualitative research?
A variety of assessment criteria and lists have been developed for qualitative research, ranging in their focus and comprehensiveness [ 14 , 17 , 27 ]. However, none of these has been elevated to the “gold standard” in the field. In the following, we therefore focus on a set of commonly used assessment criteria that, from a practical standpoint, a researcher can look for when assessing a qualitative research report or paper.
Assessors should check the authors’ use of and adherence to the relevant reporting checklists (e.g. Standards for Reporting Qualitative Research (SRQR)) to make sure all items that are relevant for this type of research are addressed [ 23 , 28 ]. Discussions of quantitative measures in addition to or instead of these qualitative measures can be a sign of lower quality of the research (paper). Providing and adhering to a checklist for qualitative research contributes to an important quality criterion for qualitative research, namely transparency [ 15 , 17 , 23 ].
Reflexivity
While methodological transparency and complete reporting is relevant for all types of research, some additional criteria must be taken into account for qualitative research. This includes what is called reflexivity, i.e. sensitivity to the relationship between the researcher and the researched, including how contact was established and maintained, or the background and experience of the researcher(s) involved in data collection and analysis. Depending on the research question and population to be researched this can be limited to professional experience, but it may also include gender, age or ethnicity [ 17 , 27 ]. These details are relevant because in qualitative research, as opposed to quantitative research, the researcher as a person cannot be isolated from the research process [ 23 ]. It may influence the conversation when an interviewed patient speaks to an interviewer who is a physician, or when an interviewee is asked to discuss a gynaecological procedure with a male interviewer, and therefore the reader must be made aware of these details [ 19 ].
Sampling and saturation
The aim of qualitative sampling is for all variants of the objects of observation that are deemed relevant for the study to be present in the sample “ to see the issue and its meanings from as many angles as possible” [ 1 , 16 , 19 , 20 , 27 ] , and to ensure “information-richness [ 15 ]. An iterative sampling approach is advised, in which data collection (e.g. five interviews) is followed by data analysis, followed by more data collection to find variants that are lacking in the current sample. This process continues until no new (relevant) information can be found and further sampling becomes redundant – which is called saturation [ 1 , 15 ] . In other words: qualitative data collection finds its end point not a priori , but when the research team determines that saturation has been reached [ 29 , 30 ].
This is also the reason why most qualitative studies use deliberate instead of random sampling strategies. This is generally referred to as “ purposive sampling” , in which researchers pre-define which types of participants or cases they need to include so as to cover all variations that are expected to be of relevance, based on the literature, previous experience or theory (i.e. theoretical sampling) [ 14 , 20 ]. Other types of purposive sampling include (but are not limited to) maximum variation sampling, critical case sampling or extreme or deviant case sampling [ 2 ]. In the above EVT example, a purposive sample could include all relevant professional groups and/or all relevant stakeholders (patients, relatives) and/or all relevant times of observation (day, night and weekend shift).
Assessors of qualitative research should check whether the considerations underlying the sampling strategy were sound and whether or how researchers tried to adapt and improve their strategies in stepwise or cyclical approaches between data collection and analysis to achieve saturation [ 14 ].
Good qualitative research is iterative in nature, i.e. it goes back and forth between data collection and analysis, revising and improving the approach where necessary. One example of this are pilot interviews, where different aspects of the interview (especially the interview guide, but also, for example, the site of the interview or whether the interview can be audio-recorded) are tested with a small number of respondents, evaluated and revised [ 19 ]. In doing so, the interviewer learns which wording or types of questions work best, or which is the best length of an interview with patients who have trouble concentrating for an extended time. Of course, the same reasoning applies to observations or focus groups which can also be piloted.
Ideally, coding should be performed by at least two researchers, especially at the beginning of the coding process when a common approach must be defined, including the establishment of a useful coding list (or tree), and when a common meaning of individual codes must be established [ 23 ]. An initial sub-set or all transcripts can be coded independently by the coders and then compared and consolidated after regular discussions in the research team. This is to make sure that codes are applied consistently to the research data.
Member checking
Member checking, also called respondent validation , refers to the practice of checking back with study respondents to see if the research is in line with their views [ 14 , 27 ]. This can happen after data collection or analysis or when first results are available [ 23 ]. For example, interviewees can be provided with (summaries of) their transcripts and asked whether they believe this to be a complete representation of their views or whether they would like to clarify or elaborate on their responses [ 17 ]. Respondents’ feedback on these issues then becomes part of the data collection and analysis [ 27 ].
Stakeholder involvement
In those niches where qualitative approaches have been able to evolve and grow, a new trend has seen the inclusion of patients and their representatives not only as study participants (i.e. “members”, see above) but as consultants to and active participants in the broader research process [ 31 , 32 , 33 ]. The underlying assumption is that patients and other stakeholders hold unique perspectives and experiences that add value beyond their own single story, making the research more relevant and beneficial to researchers, study participants and (future) patients alike [ 34 , 35 ]. Using the example of patients on or nearing dialysis, a recent scoping review found that 80% of clinical research did not address the top 10 research priorities identified by patients and caregivers [ 32 , 36 ]. In this sense, the involvement of the relevant stakeholders, especially patients and relatives, is increasingly being seen as a quality indicator in and of itself.
How not to assess qualitative research
The above overview does not include certain items that are routine in assessments of quantitative research. What follows is a non-exhaustive, non-representative, experience-based list of the quantitative criteria often applied to the assessment of qualitative research, as well as an explanation of the limited usefulness of these endeavours.
Protocol adherence
Given the openness and flexibility of qualitative research, it should not be assessed by how well it adheres to pre-determined and fixed strategies – in other words: its rigidity. Instead, the assessor should look for signs of adaptation and refinement based on lessons learned from earlier steps in the research process.

Sample size
For the reasons explained above, qualitative research does not require specific sample sizes, nor does it require that the sample size be determined a priori [ 1 , 14 , 27 , 37 , 38 , 39 ]. Sample size can only be a useful quality indicator when related to the research purpose, the chosen methodology and the composition of the sample, i.e. who was included and why.
Randomisation
While some authors argue that randomisation can be used in qualitative research, this is not commonly the case, as neither its feasibility nor its necessity or usefulness has been convincingly established for qualitative research [ 13 , 27 ]. Relevant disadvantages include the negative impact of a too large sample size as well as the possibility (or probability) of selecting “ quiet, uncooperative or inarticulate individuals ” [ 17 ]. Qualitative studies do not use control groups, either.
Interrater reliability, variability and other “objectivity checks”
The concept of “interrater reliability” is sometimes used in qualitative research to assess to which extent the coding approach overlaps between the two co-coders. However, it is not clear what this measure tells us about the quality of the analysis [ 23 ]. This means that these scores can be included in qualitative research reports, preferably with some additional information on what the score means for the analysis, but it is not a requirement. Relatedly, it is not relevant for the quality or “objectivity” of qualitative research to separate those who recruited the study participants and collected and analysed the data. Experiences even show that it might be better to have the same person or team perform all of these tasks [ 20 ]. First, when researchers introduce themselves during recruitment this can enhance trust when the interview takes place days or weeks later with the same researcher. Second, when the audio-recording is transcribed for analysis, the researcher conducting the interviews will usually remember the interviewee and the specific interview situation during data analysis. This might be helpful in providing additional context information for interpretation of data, e.g. on whether something might have been meant as a joke [ 18 ].
Not being quantitative research
Being qualitative research instead of quantitative research should not be used as an assessment criterion if it is used irrespectively of the research problem at hand. Similarly, qualitative research should not be required to be combined with quantitative research per se – unless mixed methods research is judged as inherently better than single-method research. In this case, the same criterion should be applied for quantitative studies without a qualitative component.
The main take-away points of this paper are summarised in Table 1 . We aimed to show that, if conducted well, qualitative research can answer specific research questions that cannot to be adequately answered using (only) quantitative designs. Seeing qualitative and quantitative methods as equal will help us become more aware and critical of the “fit” between the research problem and our chosen methods: I can conduct an RCT to determine the reasons for transportation delays of acute stroke patients – but should I? It also provides us with a greater range of tools to tackle a greater range of research problems more appropriately and successfully, filling in the blind spots on one half of the methodological spectrum to better address the whole complexity of neurological research and practice.
Availability of data and materials
Not applicable.
Abbreviations
Endovascular treatment
Randomised Controlled Trial
Standard Operating Procedure
Standards for Reporting Qualitative Research
Philipsen, H., & Vernooij-Dassen, M. (2007). Kwalitatief onderzoek: nuttig, onmisbaar en uitdagend. In L. PLBJ & H. TCo (Eds.), Kwalitatief onderzoek: Praktische methoden voor de medische praktijk . [Qualitative research: useful, indispensable and challenging. In: Qualitative research: Practical methods for medical practice (pp. 5–12). Houten: Bohn Stafleu van Loghum.
Chapter Google Scholar
Punch, K. F. (2013). Introduction to social research: Quantitative and qualitative approaches . London: Sage.
Kelly, J., Dwyer, J., Willis, E., & Pekarsky, B. (2014). Travelling to the city for hospital care: Access factors in country aboriginal patient journeys. Australian Journal of Rural Health, 22 (3), 109–113.
Article Google Scholar
Nilsen, P., Ståhl, C., Roback, K., & Cairney, P. (2013). Never the twain shall meet? - a comparison of implementation science and policy implementation research. Implementation Science, 8 (1), 1–12.
Howick J, Chalmers I, Glasziou, P., Greenhalgh, T., Heneghan, C., Liberati, A., Moschetti, I., Phillips, B., & Thornton, H. (2011). The 2011 Oxford CEBM evidence levels of evidence (introductory document) . Oxford Center for Evidence Based Medicine. https://www.cebm.net/2011/06/2011-oxford-cebm-levels-evidence-introductory-document/ .
Eakin, J. M. (2016). Educating critical qualitative health researchers in the land of the randomized controlled trial. Qualitative Inquiry, 22 (2), 107–118.
May, A., & Mathijssen, J. (2015). Alternatieven voor RCT bij de evaluatie van effectiviteit van interventies!? Eindrapportage. In Alternatives for RCTs in the evaluation of effectiveness of interventions!? Final report .
Google Scholar
Berwick, D. M. (2008). The science of improvement. Journal of the American Medical Association, 299 (10), 1182–1184.
Article CAS Google Scholar
Christ, T. W. (2014). Scientific-based research and randomized controlled trials, the “gold” standard? Alternative paradigms and mixed methodologies. Qualitative Inquiry, 20 (1), 72–80.
Lamont, T., Barber, N., Jd, P., Fulop, N., Garfield-Birkbeck, S., Lilford, R., Mear, L., Raine, R., & Fitzpatrick, R. (2016). New approaches to evaluating complex health and care systems. BMJ, 352:i154.
Drabble, S. J., & O’Cathain, A. (2015). Moving from Randomized Controlled Trials to Mixed Methods Intervention Evaluation. In S. Hesse-Biber & R. B. Johnson (Eds.), The Oxford Handbook of Multimethod and Mixed Methods Research Inquiry (pp. 406–425). London: Oxford University Press.
Chambers, D. A., Glasgow, R. E., & Stange, K. C. (2013). The dynamic sustainability framework: Addressing the paradox of sustainment amid ongoing change. Implementation Science : IS, 8 , 117.
Hak, T. (2007). Waarnemingsmethoden in kwalitatief onderzoek. In L. PLBJ & H. TCo (Eds.), Kwalitatief onderzoek: Praktische methoden voor de medische praktijk . [Observation methods in qualitative research] (pp. 13–25). Houten: Bohn Stafleu van Loghum.
Russell, C. K., & Gregory, D. M. (2003). Evaluation of qualitative research studies. Evidence Based Nursing, 6 (2), 36–40.
Fossey, E., Harvey, C., McDermott, F., & Davidson, L. (2002). Understanding and evaluating qualitative research. Australian and New Zealand Journal of Psychiatry, 36 , 717–732.
Yanow, D. (2000). Conducting interpretive policy analysis (Vol. 47). Thousand Oaks: Sage University Papers Series on Qualitative Research Methods.
Shenton, A. K. (2004). Strategies for ensuring trustworthiness in qualitative research projects. Education for Information, 22 , 63–75.
van der Geest, S. (2006). Participeren in ziekte en zorg: meer over kwalitatief onderzoek. Huisarts en Wetenschap, 49 (4), 283–287.
Hijmans, E., & Kuyper, M. (2007). Het halfopen interview als onderzoeksmethode. In L. PLBJ & H. TCo (Eds.), Kwalitatief onderzoek: Praktische methoden voor de medische praktijk . [The half-open interview as research method (pp. 43–51). Houten: Bohn Stafleu van Loghum.
Jansen, H. (2007). Systematiek en toepassing van de kwalitatieve survey. In L. PLBJ & H. TCo (Eds.), Kwalitatief onderzoek: Praktische methoden voor de medische praktijk . [Systematics and implementation of the qualitative survey (pp. 27–41). Houten: Bohn Stafleu van Loghum.
Pv, R., & Peremans, L. (2007). Exploreren met focusgroepgesprekken: de ‘stem’ van de groep onder de loep. In L. PLBJ & H. TCo (Eds.), Kwalitatief onderzoek: Praktische methoden voor de medische praktijk . [Exploring with focus group conversations: the “voice” of the group under the magnifying glass (pp. 53–64). Houten: Bohn Stafleu van Loghum.
Carter, N., Bryant-Lukosius, D., DiCenso, A., Blythe, J., & Neville, A. J. (2014). The use of triangulation in qualitative research. Oncology Nursing Forum, 41 (5), 545–547.
Boeije H: Analyseren in kwalitatief onderzoek: Denken en doen, [Analysis in qualitative research: Thinking and doing] vol. Den Haag Boom Lemma uitgevers; 2012.
Hunter, A., & Brewer, J. (2015). Designing Multimethod Research. In S. Hesse-Biber & R. B. Johnson (Eds.), The Oxford Handbook of Multimethod and Mixed Methods Research Inquiry (pp. 185–205). London: Oxford University Press.
Archibald, M. M., Radil, A. I., Zhang, X., & Hanson, W. E. (2015). Current mixed methods practices in qualitative research: A content analysis of leading journals. International Journal of Qualitative Methods, 14 (2), 5–33.
Creswell, J. W., & Plano Clark, V. L. (2011). Choosing a Mixed Methods Design. In Designing and Conducting Mixed Methods Research . Thousand Oaks: SAGE Publications.
Mays, N., & Pope, C. (2000). Assessing quality in qualitative research. BMJ, 320 (7226), 50–52.
O'Brien, B. C., Harris, I. B., Beckman, T. J., Reed, D. A., & Cook, D. A. (2014). Standards for reporting qualitative research: A synthesis of recommendations. Academic Medicine : Journal of the Association of American Medical Colleges, 89 (9), 1245–1251.
Saunders, B., Sim, J., Kingstone, T., Baker, S., Waterfield, J., Bartlam, B., Burroughs, H., & Jinks, C. (2018). Saturation in qualitative research: Exploring its conceptualization and operationalization. Quality and Quantity, 52 (4), 1893–1907.
Moser, A., & Korstjens, I. (2018). Series: Practical guidance to qualitative research. Part 3: Sampling, data collection and analysis. European Journal of General Practice, 24 (1), 9–18.
Marlett, N., Shklarov, S., Marshall, D., Santana, M. J., & Wasylak, T. (2015). Building new roles and relationships in research: A model of patient engagement research. Quality of Life Research : an international journal of quality of life aspects of treatment, care and rehabilitation, 24 (5), 1057–1067.
Demian, M. N., Lam, N. N., Mac-Way, F., Sapir-Pichhadze, R., & Fernandez, N. (2017). Opportunities for engaging patients in kidney research. Canadian Journal of Kidney Health and Disease, 4 , 2054358117703070–2054358117703070.
Noyes, J., McLaughlin, L., Morgan, K., Roberts, A., Stephens, M., Bourne, J., Houlston, M., Houlston, J., Thomas, S., Rhys, R. G., et al. (2019). Designing a co-productive study to overcome known methodological challenges in organ donation research with bereaved family members. Health Expectations . 22(4):824–35.
Piil, K., Jarden, M., & Pii, K. H. (2019). Research agenda for life-threatening cancer. European Journal Cancer Care (Engl), 28 (1), e12935.
Hofmann, D., Ibrahim, F., Rose, D., Scott, D. L., Cope, A., Wykes, T., & Lempp, H. (2015). Expectations of new treatment in rheumatoid arthritis: Developing a patient-generated questionnaire. Health Expectations : an international journal of public participation in health care and health policy, 18 (5), 995–1008.
Jun, M., Manns, B., Laupacis, A., Manns, L., Rehal, B., Crowe, S., & Hemmelgarn, B. R. (2015). Assessing the extent to which current clinical research is consistent with patient priorities: A scoping review using a case study in patients on or nearing dialysis. Canadian Journal of Kidney Health and Disease, 2 , 35.
Elsie Baker, S., & Edwards, R. (2012). How many qualitative interviews is enough? In National Centre for Research Methods Review Paper . National Centre for Research Methods. http://eprints.ncrm.ac.uk/2273/4/how_many_interviews.pdf .
Sandelowski, M. (1995). Sample size in qualitative research. Research in Nursing & Health, 18 (2), 179–183.
Sim, J., Saunders, B., Waterfield, J., & Kingstone, T. (2018). Can sample size in qualitative research be determined a priori? International Journal of Social Research Methodology, 21 (5), 619–634.
Download references
Acknowledgements
no external funding.
Author information
Authors and affiliations.
Department of Neurology, Heidelberg University Hospital, Im Neuenheimer Feld 400, 69120, Heidelberg, Germany
Loraine Busetto, Wolfgang Wick & Christoph Gumbinger
Clinical Cooperation Unit Neuro-Oncology, German Cancer Research Center, Heidelberg, Germany
Wolfgang Wick
You can also search for this author in PubMed Google Scholar
Contributions
LB drafted the manuscript; WW and CG revised the manuscript; all authors approved the final versions.
Corresponding author
Correspondence to Loraine Busetto .
Ethics declarations
Ethics approval and consent to participate, consent for publication, competing interests.
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Busetto, L., Wick, W. & Gumbinger, C. How to use and assess qualitative research methods. Neurol. Res. Pract. 2 , 14 (2020). https://doi.org/10.1186/s42466-020-00059-z
Download citation
Received : 30 January 2020
Accepted : 22 April 2020
Published : 27 May 2020
DOI : https://doi.org/10.1186/s42466-020-00059-z
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Qualitative research
- Mixed methods
- Quality assessment
Nurses’ and patients’ perceptions of physical health screening for patients with schizophrenia spectrum disorders: a qualitative study
- Långstedt Camilla 1 ,
- Bressington Daniel 2 , 3 &
- Välimäki Maritta 1 , 4
BMC Nursing volume 23 , Article number: 321 ( 2024 ) Cite this article
58 Accesses
Metrics details
Despite worldwide concern about the poor physical health of patients with schizophrenia spectrum disorders (SSD), physical health screening rates are low. This study reports nurses’ and patients’ experiences of physical health screening among people with SSD using the Finnish Health Improvement Profile (HIP-F) and their ideas for implementation improvements.
A qualitative exploratory study design with five group interviews with nurses ( n = 15) and individual interviews with patients with SSD ( n = 8) who had experience using the HIP-F in psychiatric outpatient clinics. Inductive content analysis was conducted.
Two main categories were identified. First, the characteristics of the HIP-F were divided into the subcategories of comprehensive nature, facilitating engagement, interpretation and rating of some items and duration of screening. Second, suggestions for the implementation of physical health screening consisted of two subcategories: improvements in screening and ideas for practice. Physical health screening was felt to increase the discussion and awareness of physical health and supported health promotion. The HIP-F was found to be a structured, comprehensive screening tool that included several items that were not otherwise assessed in clinical practice. The HIP-F was also considered to facilitate engagement by promoting collaboration in an interactive way. Despite this, most of the nurses found the HIP-F to be arduous and too time consuming, while patients found the HIP-F easy to use. Nurses found some items unclear and infeasible, while patients found all items feasible. Based on the nurses’ experiences, screening should be clear and easy to interpret, and condensation and revision of the HIP-F tool were suggested. The patients did not think that any improvements to the HIP-F were needed for implementation in clinical settings.
Conclusions
Patients with schizophrenia spectrum disorders are willing to participate in physical health screening. Physical health screening should be clear, easy to use and relatively quick. With this detailed knowledge of perceptions of screening, further research is needed to understand what factors affect the fidelity of implementing physical health screening in clinical mental health practice and to gain an overall understanding on how to improve such implementation.
Peer Review reports
The physical health state of people diagnosed with schizophrenia spectrum disorder (SSD) is a global problem [ 1 ]. Typically, poor physical health results from a range of issues, including the impact of psychiatric symptoms on health behavior, adverse effects of prescribed medication, difficulties observing physical health concerns, lifestyle, diagnostic overshadowing, and patient unwillingness to report health problems [ 2 , 3 ]. These factors may lead to obesity, metabolic syndrome, coronary vascular disease, diabetes, hypertension, or cancer [ 4 , 5 , 6 ]. High rates of infectious diseases such as hepatitis and HIV [ 7 ] and COVID-19 [ 8 ] have also been reported in patients with SSD. As an outcome of physical health issues, physical comorbidity is associated with psychiatric readmission [ 9 ] and high treatment costs. In Finland, the total healthcare costs caused by schizophrenia are approximately 700–900 million euros per year, mostly as a result of inpatient treatment costs [ 10 ]. Due to poor physical health, the life expectancy of persons with schizophrenia is approximately 20 years less than that of the general population [ 11 , 12 ]. Therefore, it is crucial that physical health screening is conducted regularly for patients with SSD. Improving regular screening helps to support earlier detection of risk factors that can, without detection and intervention, have deleterious effects on the physical health of patients with SSD [ 10 ].
Several international clinical guidelines have recommended how physical health screening for patients with SSD should be conducted [ 10 , 13 , 14 , 15 , 16 ]. According to guidelines persons with SSD who have been prescribed antipsychotic medication should have annual health checks focusing on full blood count, lipids, plasma glucose, prolactin, blood pressure, urea, electrolytes, liver function tests, weight, waist circumference measurement and electrocardiogram examination (ECG) [ 16 ]. Being aware of patients’ lifestyle habits, including smoking and use of other substances [ 10 , 13 , 15 ] is important for directing appropriate behavioral interventions to promote healthy lifestyles. In addition, a variety of screening instruments have been developed to assess physical health among people with SSD. Lamontagne-Godwin et al. [ 17 ] identified in their systematic review 44 intervention studies aiming to increase access to or uptake of physical health screening. Examples of monitoring tools in the included studies were Physical Health Check (PHC) [ 18 ]; physical health monitoring sheet [ 19 ]; systematic computerized cardiovascular health screening [ 20 ]; the Metabolic Syndrome Screening Tool (MSST) [ 21 ]; quality improvement (QI) [ 22 ] to increase rates of metabolic syndrome screening and the Health Improvement Profile (HIP), which is a comprehensive nurse-led profiling tool that assesses physical health risks, identifies unhealthy lifestyle behaviors, and provides associated recommended actions for health promotion [ 23 ]. Despite the abundance of available instruments, physical health screening is still poorly implemented in clinical mental health services [ 24 , 25 ].
To better understand this rationale for poor physical health screening, a quantitative study in Uganda [ 26 ] showed, that more than 75% of 28 nurses had a positive attitude towards metabolic screening and associated interventions. The same study reported that more than 50% of nurses were confident in providing physical activity and smoking cessation advice and nutritional counseling. However, 57% stated that their heavy workload prevented them from doing health screening. Voort et al. [ 27 ] reported in their qualitative study in Netherlands, that most nurses perceived physical health screening to be an important part of their professional role, but identified a discrepancy between their perceptions and actual clinical practice. Happell et al.’s qualitative study [ 28 ] reported in Australia that although nurses recognize their responsibility with respect to the physical health of patients with severe mental illness, they experienced factors such as staff shortages and lack of knowledge that prevented them from conducting screening properly. Further, Mwebe [ 29 ] reported in his UK study that nurses shared a clear commitment regarding their role in physical health screening in mental health care settings. Four themes emerged as follows: features of current practice and physical health monitoring; perceived barriers to physical health monitoring; education and training needs; and strategies to improve physical health monitoring. In the UK, Butler et al.’s qualitative study [ 30 ] revealed that patients varied in their awareness of the association between mental and physical health, but were engaged in physical health screening.
Moreover, Bressington et al. [ 31 ] revealed in their qualitative study, that nurses working in Hong Kong psychiatric care settings found the HIP (the Health Improvement Profile) to be comprehensive and perceived positive changes in their patients’ wellbeing, for example, by increasing motivation for patients to improve their health. HIP was developed to increase patient engagement in screening their physical health in collaboration with a nurse [ 32 ]. Earlier studies in the UK [ 33 ], Hong Kong [ 34 ], and Thailand [ 35 ] have reported patient acceptability and clinical utility of the HIP in identifying health risks where interventions are needed. These findings show that HIP may be feasible in engaging patients in discussions about physical health and in identifying areas of health risk [ 34 , 35 ]. Although Hardy et al. [ 33 ] found support for the usability of the HIP in clinical practice in a study in the UK, a subsequent RCT study conducted in the UK revealed that nurses found the use of the HIP unfeasible in a clinical setting due to its length [ 36 ]. In contrast, nurses in Hong Kong [ 31 ] found the HIP to be acceptable, feasible, and potentially useful in clinical practice. In Finland, our validation study of the Finnish Health Improvement Profile (HIP-F) supported this finding by detecting 399 areas of health and health behavior risk in a sample of 47 patients [ 37 ].
Previous international studies have only reported nurses’ and patients’ general attitudes toward health checks without detailed perceptions of the importance of comprehensively assessing different health parameters together with ideas for improvements. Implementation of physical health screening is influenced by services users’ perceptions and experiences. It is of paramount importance to involve potential users in the design and implementation of new procedures [ 38 ], and thus, when developing physical health screening for patients with SSD, the perceptions of both nurses and patients are vital [ 38 , 39 ]. Reconciling patients’ and nurses’ perceptions of physical health and its screening is an important step in promoting collaborative care and improving physical health screening rates [ 40 ]. Little detailed information is known about how nurses and patients perceive physical health screening; particularly, the assessment target areas and parameters, and how would nurses and patients improve screening so that it is more likely to regularly conducted in clinical practice. No previous studies have aimed to understand detailed perceptions and ideas for improvements of physical health screening by combining both nurses’ and patients’ perspectives using qualitative methods. The contrasting results regarding HIP instrument highlight that the acceptability and feasibility of HIP might be culturally and clinically context specific, and more research on patients’ and nurses’ perceptions of HIP in clinical practice is needed. To fulfill this knowledge gap, the current study sought to explore nurses’ and patients’ perceptions of physical health screening using the HIP-F profile as an example of physical health screening among patients with SSD in psychiatric settings in Finland and identify possible areas for improvement in the HIP-F tool and screening procedures.
The aim of this study was to explore (1) nurses’ and patients’ perceptions of physical health screening using the HIP-F profile as an example and (2) possible areas of improvement for implementation of physical health screening among patients with SSD in psychiatric settings in Finland. The information can be used to identify possible areas to be improved regarding implementation of systematic physical health screening activities as a part of treatment process among patients with SSD.
Study design
A qualitative exploratory study design, with focus group interviews for nurses and individual interviews for patients, was used to gain a better understanding of the real-life experiences of the study participants [ 41 , 42 ]. The qualitative exploratory design was appropriate for defining the terms of the research problem and to gain background information on a topic that little is known about [ 42 , 43 ]. For nurses, focus group interviews were used not only as a way of obtaining individual answers but also with the group interaction of participants to allow participants to explore and clarify individual and shared perspectives of specific phenomena in an open and flexible way [ 43 , 44 ]. For patients, individual interviews were chosen to receive deep insight into the respondent’s personal thoughts and feelings but also to ensure privacy, confidentiality, and a comfortable atmosphere, with concern for the vulnerability of patients with SSD [ 13 ] Moreover, individual interviews for patients were conducted to pursue personal disclosure and with consideration of the possible cognitive disabilities, such as attention and memory issues of patients with SSD [ 45 ]. Despite the potential for cognitive dysfunction, there is several benefits, such as receiving patients’ perspectives affecting engagement, involving consumers in developing interventions [ 46 ]. An exploratory approach was selected to obtain more detailed descriptions of the experiences of the participants. With this approach, we aimed to identify the phenomenon by using open-ended questions to allow nurses and patients to freely express their perceptions so that we could perform an inductive content analysis on the data without any theoretical framework or previously produced codes and categories [ 42 , 47 ].
We adhered to the consolidated criteria for reporting qualitative studies (COREQ) [ 48 ] when reporting the current study.
The study was conducted in five psychiatric outpatient clinics in Southern Finland. These clinics were selected because they offer a desirable representativeness of the study population, being part of the largest hospital area in Finland with a population of approximately 460,000 inhabitants [ 49 ]. The clinics provide mental health care for approximately 2,300 patients who have been diagnosed with a range of schizophrenia spectrum disorders (F20–29) [ 50 ]. The clinics provide both crisis and long-term mental health care and focuses on recovery and rehabilitation provided by multidisciplinary teams (psychiatrists, social workers, mental health nurses) as well as counseling and psychiatric examinations [ 51 ]. The patients’ frequency of attendance at the clinics depends on their individual treatment plan.
For nurses, a purposive sampling method was used to recruit enough participants and generate enough rich data to understand the studied phenomenon [ 52 ]. All 47 nurses who had previously been asked to use the HIP-F to assess the physical health of their patients, were invited to join the focus group interviews. These nurses had diverse backgrounds of various ages, education, and length of working experience and had the potential to provide relevant and diverse data pertinent to the research question [ 53 , 54 ]. The inclusion criteria for nurses were that they had professional education (registered nurse, mental health nurse), that they had permanent or long-term temporary employment and that they were currently working in mental health clinical practice as a patient’s primary nurse in coordinating and providing care. The exclusion criterion was being a nursing student. We aimed to sample a total of 5 focus groups, one from each study clinic, with 6–10 nurse participants in each focus group, which is close to an optimal size in focus groups to promote discussion. The sample size estimation was based on previous literature suggesting that at least four focus groups would be sufficient to identify new issues (code saturation), but more groups may be needed to completely understand these issues (meaning saturation)” [ 52 ].
For patients, a purposive sampling method was used to recruit eligible participants for the individual interviews. To be eligible to be invited to participate, the patients needed to have a diagnosis of a schizophrenia spectrum disorder, to have been treated as an outpatient in a clinic and to have been previously targeted for physical health screening with the HIP-F to elicit feedback on their experiences and perceptions [ 55 ]. We aimed to recruit 10 patients for the individual interviews since this number of interviews in qualitative content analysis was believed to allow us to reach a saturation of themes [ 56 ]. The inclusion criteria for patients were a minimum age of 18 years, being treated in outpatient clinics, having the ability to understand and speak Finnish, and a diagnosis of schizophrenia or another schizophrenia spectrum disorder F20-29 (ICD10) [ 50 ]. The exclusion criteria were having an acute psychosis or a very disturbed mental state, where participation would distress the patient or put nurses at risk.
Interview questions
Participants were asked to give their responses to open-ended questions, which focused on physical health screening with the HIP-F. The original HIP instrument, a physical health screening tool, was developed in the UK [ 32 ] and validated in Finland [ 37 ]. The HIP is a 27-item (28 for females) gender-specific profiling tool focusing on physical health and health behavior items (see Table 1 ). It enables nurses and patients to work together to assess physical health among patients with SSD. Health items (e.g., smoking status) are evaluated by categorizing them as green (e.g., nonsmoker) or red (e.g., passive smoker/smoker) depending on the result. If the health item is assessed as red, recommended actions (e.g., advice that all smoking is associated with health risks, refer to smoking cessation service) can be selected to produce a health care plan. The HIP is intended to be completed at least annually, which is the recommended frequency of screening for patients with SSD [ 12 , 50 ]. This assessment together with regular discussions with a nurse familiar with the patient might decrease barriers, for example, in talking about sensitive topics [ 17 ]. In this study, the perceptions of recommended actions have not been reported because we aimed to study only the nurses’ and patients’ experiences and perceptions of the screening procedure.
The interview questions were based on the process observation method used in a UK-based cluster-randomized controlled trial with HIP [ 36 ] and a qualitative descriptive HIP study in Hong Kong [ 31 ]. An overview of the open-ended questions is as follows:
How did you experience the physical health screening with the HIP-F?
What did you think about the physical health screening?
Which elements of assessing physical health with the HIP-F did you find most and least feasible?
How long did it take to complete the HIP-F?
What improvements could be made to physical health screening?
Recruitment
First, for potential nurse participants, one researcher (CL) provided information sessions about the study to each study clinic twice via Teams meetings. Information was given about the rights, voluntariness and confidentiality, and purpose of the study, as well as the process and the risks and benefits of participating. The main risk of participating would be the time spent participating in the research. The research would not produce immediate benefits for the nurse participants, but it would give an opportunity to influence the improvement of the usability of the HIP-F profile by giving feedback and suggestions for changes. Nurses were informed about what to expect from the focus group interviews to increase the likelihood of honesty. Participants also received written information by email before they gave their written informed consent. Nurses expressed verbally their possible desire to participate to the researcher during the information sessions and the researcher collected the consent form from the participating nurses from the study clinics at the agreed time. Of the 47 eligible nurses, 16 agreed to participate. However, one of the agreed nurses withdrew before the interview. The researcher regularly visited the study clinics (once a week), obtained informed consent from participants, and contacted the participating nurses to agree on dates for the focus groups.
Second, patients were recruited by nurses during their regular meetings in study clinics after they had been screened with the HIP-F. Nurses informed patients about the voluntariness and confidentiality as well as the purpose of the study, the process, and the risks and benefits of participating. There would be no direct benefit to the patients from participating, and no other disadvantages than the time spent on the interview. It was deemed unlikely that patient participants would experience any distress as a result of participating. Patients were given both oral and written information from nurses that participation or refusal to participate would affect their treatment in the clinic or their relationship with the clinical staff. Since cognitive problems may be associated with SSD [ 13 ], we aimed to ensure that each nurse would recruit familiar patients using an assessment of their cognitive ability and their capacity to give informed consent for participation [ 13 , 45 ]. Altogether, eight patients participated and gave their informed consent to a nurse who informed the researcher of the patient’s participation. The researcher contacted the patients to agree on dates for the individual interviews.
Data collection
Interviews were conducted using a semi-structured format to encourage participants to talk about issues that would answer the research question [ 57 , 58 ]. Before the interviews, participants gave their background information regarding gender and age. Nurses were also asked about their education and work experience in mental health care. The researcher guided the participants in the focus group interview and encouraged them to interact with each other [ 59 ]. The focus groups were preexisting work groups from clinics, and this facilitated open discussion and interaction with shared experiences in a comfortable and familiar setting [ 57 ].
All interviews were conducted between October and December 2022 by one female researcher (CL), a registered nurse (PhD student) with a long working experience with patients with SSD, who was working as a nurse manager in another unit. The researcher knew one nurse participant from an earlier HIP validation study. Participants knew that the research was a part of the researcher’s PhD study. Only the researcher and study participants were present during the interviews. Consent for recording was obtained from all participants. No pilot interviews were used. Altogether, four group interviews with nurses with two to six participants in each interview were conducted. One nurse was individually interviewed because the other consenting participant withdrew. Four of the nurses’ interviews occurred in clinic meeting rooms, and one was held via Microsoft Teams meeting. For the patients, eight individual interviews were conducted: seven by phone and one in Microsoft Teams meeting after the researcher called the patient with Microsoft Teams application. These approaches were chosen so that the subjects would experience as little harm as possible from participating in the study, for example an extra visit to the research outpatient clinic. When conducting the interviews, the current restrictions due to the COVID-19 pandemic also had to be taken into account. The duration of the interviews with nurses varied from 25 to 56 min, and the patients’ interviews lasted from 8 to 32 min. During the first two interviews, the researcher evaluated whether the questions were clear and relevant according to the information received. As no participant asked for clarification and the data were considered relevant, the questions were used in all interviews. No field notes were made during the focus group interviews and the patient interviews, but records were made about observations of nonverbal responses and reflections in the nurses’ interviews as soon as possible after each interview [ 60 ].
Data analysis
The data analysis was conducted concurrently with the interviews. The interviews, original transcriptions, and overall data analysis were in Finnish. An inductive content analysis method for audio-recorded interviews was chosen since there are no previous qualitative studies on the topic in Finland [ 61 ]. When conducting exploratory research in an area where little is known, content analysis might be suitable for the reporting of general issues in the data [ 62 ]. Furthermore, content analysis was well suited for analyzing our study topic, which is a sensitive, important, and multifaceted phenomenon of nursing [ 58 , 63 ]. Since we aimed to generate complementary perceptions and an enhanced understanding of the phenomenon, focus group and individual interview data were combined for analysis [ 64 ]. All interviews were transcribed in Word 2021 and analyzed using the five-step method by Graneheim and Lundman [ 65 ]. This approach enabled a systematic, reliable, and valid data analysis [ 58 ], which was led by research questions [ 66 ]. No software was used for coding in the analysis. First, all interviews were transcribed verbatim by one researcher (CL). Second, the researcher initially familiarized herself with the data through multiple careful readings of the transcripts to gain an understanding of the whole. Third, a sentence was selected as an analysis unit. Fourth, the text was distributed into meaning units, which were further condensed into sentences, and the condensed meaning units were abstracted and labeled with a code. Fifth, all 18 codes identified from the data were compared with each other for similarities and differences and sorted into six subcategories. The tentative categories were discussed between all authors and revised. A process of discussion and reflection resulted in an agreement on how to sort the codes.
Finally, the subcategories that were similar in terms of meaning and content were sorted into two main categories. Quotations from study participants were translated into English by one author (CL), checked by another bilingual researcher (MV) for equivalent meaning, and presented to illustrate the results (N as nurse, P as patient). From the first to the third nurses’ interview a total of 13 codes were added, and no further new codes were developed after the fourth interview. Based on code identification (88% of codes had been identified), code prevalence (90% of high-prevalence codes were identified) and codebook stability (94% of codebook changes were made), code saturation was reached after four interviews. Meaning saturation was reached at the last interview in which a new dimension of the code was identified. [52.] From patients’ interviews, code saturation was reached after the fourth individual interview and meaning saturation was achieved after the eighth interview as the repetition of content became obvious [ 52 , 67 ]. Examples of meaning units and codes are presented in Table 2 .
Demographic characteristics of study participants
A total of 15 nurses participated in the study (11 females and four males). The distribution of nurses was as follows: in the first interview there were three males and one female; in the second group there were two females; in group three there was one male and one female; the fourth interview contained one female and in the fifth interview there were six female nurses. The ages of the participants varied between 43 and 61 years, with a mean age of 49.47 years (SD 5.99). The majority were registered nurses. The length of their work experience in mental health nursing varied from one and a half years to 38 years, with a mean working experience of 21.73 years (SD 8.18). Among the patients, seven females and one male participated in the study. The ages of the participants varied between 21 and 65 years, with a mean age of 43.87 years (SD 17.27). The demographic characteristics of the study participants are presented in Table 3 .
Nurses’ and patients’ perceptions of physical health screening with the HIP-F and suggestions for improvement of screening in psychiatric settings
Both nurse and patient participants perceived physical health screening among patients with SSD to be important and the screening with HIP-F as an example screening tool to be comprehensive, but also highlighted some areas for improvement for conducting screening in psychiatric settings. Two main categories were identified from the analysis. First, the characteristics of the HIP-F were divided into subcategories: comprehensive nature , facilitating engagement , interpretation and rating of some items , and duration of screening . Second, suggestions for the implementation of physical health screening consisted of two subcategories: improvements in screening and ideas for practice . The summary of codes, subcategories and main categories is presented in Table 4 .
Characteristics of the HIP-F
Comprehensive nature.
The patients and nurses considered the HIP-F tool to be important, structured and able to comprehensively evaluate physical health. Patients found alcohol intake, activity and smoking status to be extremely important to assess among patients with SSD and expressed that it was the first time nurses had asked about several of the important items in HIP-F, including urine, caffeine intake and sexual satisfaction. Participants stated that the HIP-F includes several items, such as urine, caffeine intake, feet, and sexual satisfaction, which would not be assessed otherwise. Nurses expressed that in clinical practice a range of different nurses evaluate patients’ physical health parameters dependent on the clinical setting, however there is a current lack of appropriate structured, comprehensive screening tools. Based on the experiences of most nurses and all patient participants, all HIP-F items were considered feasible. Most of the nurses expressed that all items assessed with laboratory tests as well as body mass index (BMI), waist circumference, diet, activity, alcohol intake, teeth, smoking status, eyes, and caffeine intake were particularly feasible in physical health screening. However, despite the importance and feasibility, some HIP-F items were considered potentially challenging to talk about (e.g., sexual satisfaction) because of their sensitive nature.
The items are kind of structured here, because there is a lot, a lot of things we are asking, but they are being asked scattered in different situations, in different phases…yes, the comprehensiveness is good. (N5) Yes, there was the alcohol intake and smoking status and activity, they seemed essential. (P6) Yeah, well, it could be that for some people, the things related to their own sexual life are the same, which they don’t necessarily want to discuss. (P5) .
Facilitating engagement
All participants found the physical health screening with HIP-F to be an overall positive experience. Patients were fully aware of the significance of the relationship between physical health and mental health and were happy to have their physical health assessed. All study participants stated that physical health monitoring with the HIP-F on an annual basis is a relevant timespan for regular health checks. Based on the nurses’ and patients’ experiences, the participants felt that conducting the HIP-F together in an interactive way facilitates engagement with physical health screening and health promotion. The participants described this working model to be more desirable, making health checks easier and enabling patients to have feedback on their state of health immediately. Furthermore, nurses stressed the importance of engaging patients with SSD in their own care, something that is supported with HIP-F screening. The patients and most of the nurses expressed that the screening increased discussion in general, and discussion about physical health between nurses and patients in areas that would otherwise not be discussed. According to the study participants, screening improved information, raised some thoughts and increased awareness of physical health and health behavior in general and particularly about the items that affect patients with SSD. Nurses experienced that especially with patients with SSD it is more beneficial to conduct the screening together during a discussion because of patients’ potential cognitive challenges. The participants described that screening helped to identify physical health illnesses which helped them to start adequate treatment for the patient. Based on the participants’ experiences, screening might motivate patients to increase their activity, support physical health, and strengthen already healthy life behaviors.
Well, I wouldn’t mind if this assessment would be conducted once a year. (P5) Yes, it is very good, especially with our psychosis patients, that we are engaging them in treatment, especially in somatic health. (N5) Yes, it raised at least a little discussion about physical health. (P1) In fact, we caught quite a hypertension disease, so that was the end of it. (N2) .
Interpretation and rating of some items
Most of the nurse participants experienced HIP-F as arduous to conduct and challenging in screening, especially without routine. Nurses described the HIP-F to be too complicated and too precise and that some items were difficult to assess; for example, items pertaining to urine, fat intake (diet), five portions a day (diet), and activity were found to be difficult to assess. Nurses stated that the amount of urine passed is difficult to assess just by asking patients about it. Nurses also experienced that screening with HIP-F was too precise because nurses believed that their main work task is to evaluate mental health state, not physical health. Furthermore, some nurses were not familiar with the measurement units for some HIP-F items. However, patient participants expressed that HIP-F was easy to conduct. Moreover, nurses experienced that the HIP-F was ambiguous and partly difficult to interpret. Nurses described that some items, units of measure, and cutoff values were unclear; for example, the items for fluid, caffeine and alcohol intake, as well as the items concerning feet and urine, were overall experienced to be strange, and the significance of urine as an item remained unclear. Nurses stated that for some items, they could not find an adequate alternative to the cutoff values. This made most of the nurses consider the HIP-F to be ambiguous, which made conducting it frustrating. Some of the nurses experienced that the HIP-F also included items that were not feasible in physical health screening, such as safe sex, breast examination (men), body temperature, five portions a day (diet), caffeine intake, liver function, sexual satisfaction, BMI and feet check.
Some items felt weird, perhaps I didn’t quite understand why these were being asked so precisely in a mental health care context. (N10) I think one challenge was for example those…there are lipids or blood sugar, so, how was it, it’s quite a long time since you have done these…I had to check from the patient record how they are assessed in Finland, are they millimole or what, to find the congruent values and what are they then. (N1) The item alcohol intake is weird, there is no alternative to choose if you don’t use alcohol at all. (N9) It was a quite an easy questionnaire. Yes, it felt like that, and truly clear. (P6) .
Duration of screening
Nurses found the HIP-F too broad and time consuming to be used in clinical practice in a psychiatric setting and not feasible to be implemented in Finnish mental health services. Nurses described that although physical health screening among patients with SSD is crucial and the HIP-F includes important health items, it is too long to be used in clinical practice. Even those nurses who were first motivated to conduct screening, did not continue screening with several patients when they found out how long the screening took. Nurses reported the heavy workload of caring for many patients and their main tasks in the mental health treatment setting. Nurses experienced that the screening with HIP-F took all the time from the scheduled appointment and no time was left for discussion about the mental health of the patients, so they decided to choose to assess possible psychotic symptoms or patients’ functioning ability. Furthermore, nurses described that during screening, it was found that some health parameters, for example, annual laboratory tests, had not been conducted on patients, even if they should have been conducted according to the clinics’ regular procedures, and this challenged and delayed the screening. Nurses stated that conducting the HIP-F screening takes from 45 to 60 min, which they felt was too much for patient meetings, especially if patients only seldomly have appointments. Some nurses experienced the HIP-F to be easy to use but still too time consuming. Whereas, some of the patients had been prepared for a longer assessment and expressed that the HIP-F screening was suitable in length.
Well, I made one at the beginning, and when I noticed that it was arduous and how much time it takes, maybe that’s when the enthusiasm faded. (N9) I’m guessing 45–60 min, I haven’t recorded it, but usually we have 45-minute appointments and sometimes it takes slightly more, and it took me the whole time to do it. (N10) I was prepared for a longer questionnaire, but it wasn’t. (P5) .
Suggestions for the implementation of physical health screening
Improvements in screening.
Nurses suggested lightening and condensing the content of the HIP-F. They described that screening could be shorter and that some HIP-F items could be left out. For example, one nurse expressed that asking about temperature in physical health screening is pointless unless the patient has a cold. However, some of the nurses and all patients felt that no improvements were needed in screening for implementation. Some nurses suggested that the cutoff values could be removed, and the items could remain just as a checklist for discussion. However, other nurses thought that the cutoff values should be retained in screening and that there was nothing to develop or leave out. In addition, some nurses stated that items, such as blood pressure, could be assessed numerically but that there could be additional space for open narrative text. On the other hand, some nurse participants expressed that the assessment might be ineffective without cutoff values. Furthermore, participants expressed that some items could be assessed differently. Nurses suggested that, for example, instead of asking patients about their amount of urine output, patients could be asked about hematuria, and instead of asking about teeth checks, patients could be asked if they are brushing their teeth regularly. One patient suggested that instead of assessing activity levels, patients could be asked what kind of activity they prefer. Another patient suggested that sexual satisfaction could be assessed more broadly, taking sexual diversity into account. In addition, nurses suggested that the layout and order of the items could be different: the green and red areas could appear in green and red on the HIP-F form, and a yellow area could be added. This was considered to be more effective in demonstrating to patients their physical health state and highlighting possible areas which should be improved, rather than just discussing about the results of the HIP-F screening. Nurses stated, that adding yellow areas in HIP-F would show patients that although the result is still in a healthy area, if no improvements are made, subsequent physical health problems are likely.
I would remove temperature. It should be normal if you don’t have cold. (N12) I wouldn’t directly remove anything. (N5) Yes, I said that I could take all these cutoff values out of here and keep it just as a check list so these would be checked with a patient at least once a year. (N3) However, if there were no cutoff values for activity, sleep and smoking, then… I think these traffic light systems would be good if you could get it in color so that if it is shown to the patient who you now have this in red, that you should probably do something about it. (N1) Therefore, it could be three-part if there were the traffic light like you said just now, if it was the yellow light in between as well. (N4) .
Ideas for practice
Most of the nurses expressed that the HIP-F includes basic physical health items and that conducting health screening with the HIP-F in clinical practice does not require any additional training. However, one nurse expressed that education for talking about sensitive topics, such as safe sex and sexual satisfaction with patients, is needed. Some of the nurses suggested that the HIP-F could at least partly be completed beforehand by the patient before their clinic appointment so the screening would not take too much time from the appointment. One nurse suggested that this could happen by using an electronic version (i.e., a software application) instead of a paper questionnaire, especially for younger patients with technical skills. In addition, some of the nurses suggested a separate, longer appointment for patients in the clinics for physical health screening.
These are just basic things, there is no need for additional training. (N9) Yes, some could be doing it in advance, and some would be that who you would measure the blood pressure or something together…I think it would be reasonable, that it would already be…the patient would have already filled it in beforehand as best they could and perhaps thought about these things in peace at home, so that would speed it up in the appointment. (N10) .
As far we are aware, this study is the first study to explore perceptions among nurses and patients with SSD of physical health screening. We used the HIP-F profile as an example of a physical health screening tool. We aimed to identify possible areas for improvement in the tool and screening procedures. The study reveals several important aspects of how nurses and patients perceive physical health screening. At the same time, the HIP-F tool was also found to be arduous and time consuming, which led to recommendations on key improvements to the tool and physical health screening procedures.
Our study showed that nurses perceived physical health screening to be important [ 27 , 68 ] and that they appreciated the comprehensive physical health screening with HIP-F [ 28 , 31 ]. Nurses expressed that several HIP-F items were particularly feasible. Patients also found physical health screening beneficial in improving their awareness of physical health, which can potentially trigger health promotion conversations between nurses and patients [ 18 , 28 , 31 ]. Patients in our study were interested in and satisfied with having regular assessment of their health status [ 30 , 33 , 69 , 70 , 71 ]. Indeed, the theme ‘facilitating engagement’ was identified as a crucial factor for successful health screening in both nurses’ and patients’ data [ 26 , 27 , 30 ]. Our results are encouraging since previous studies have revealed that negative attitudes among nurses and a lack of support may restrict systematic health checks in mental health services [ 30 , 31 ]. In some countries, for example Turkey [ 72 ], nurses have stated that patients are not interested in participating in health checks. Positive perceptions among nurses towards any new intervention, including physical health screening, are important in facilitating the integration of new practices into patient care [ 73 , 74 ].
Some divergent perceptions were also found in nurses’ and patients’ perceptions in our study. Patients did not identify any infeasible or unclear items in their physical health assessment while nurses identified items regarding urine, caffeine intake, temperature, safe sex, or sexual satisfaction not meaningful or difficult to complete [ 37 ]. The finding regarding urine problems in patients with SSD is interesting as polydipsia may lead to water intoxication [ 75 ]. Patients with SSD are also 29 times more likely to get a urinary tract infection, which is a precipitating factor for acute psychosis [ 76 , 77 ]. Sometimes nurses perceive their subjective clinical view as more crucial in assessing patients’ health status than using the objective results of a standard screening tool [ 78 ]. In the future, the core reason for this discrepancy should be explored to fully understand nurses’ avoidant behavior in conducting systematic health screening with patients. This is important because our current results may be contradictory with the reality. For example, although health screening was seen as an important task in patient care, the nurses complained that using HIP-F took too much time, which made them avoid patient health screening. For example, in the current study out of 47 nurses who had been asked to conduct HIP-F screenings with their patients, only 16 were willing to use the HIP-F screening tool and monitor their patients’ physical health. This finding is interesting as it highlights the benefit of collaboration between nurses and patients when conducting screening together, as reported in previous studies [ 35 , 36 , 79 ]. At the same time, nurses expressed that the screening process was unclear and difficult to follow [ 17 , 29 , 80 ]. To adopt healthy lifestyles, e.g. physical activity and nutrition, nurses should integrate improvement initiatives for patient physical health into daily practice by making small changes [ 71 ]. In this study, however, nurses perceived assessment of patient physical health using HIP-F as a separate task, which caused double recording in patients’ health records. This finding concurs with earlier studies that health screening is poorly implemented into mental health practice [ 24 , 25 ].
In our study, nurses suggested condensation of the screening and revising the assessment with more culturally-understandable units of measurements. Item terminology should also be better suited into clinical practice [ 31 ]. To improve patients’ ability to understand the results of their health assessment, nurses suggested use of ‘a yellow traffic light’ as already used in the Chinese Health Improvement Profile (CHIP) [ 34 ]. Therefore, based on the data, some specific health components need a special effort, such as oral and general hygiene [ 72 ]. In addition, training in talking about such sensitive topics was suggested, such as topics around sexual health [ 81 , 82 ]. In addition, general training is needed to improve nurses’ understanding of the value of specific health screening items.
All these development ideas are feasible and realistic, but still leave us without a conclusion as to why these good ideas are not realized in daily practice. One reason for this may be nurses’ training needs [ 83 ]. For example, in our study, nurses had worked in mental health setting on average for over 20 years and still some health issues, e.g. adverse effects of medication, patients’ difficulties observing physical health concerns and lifestyle typical for patients with SSD, were unclear for nurses [ 2 , 3 ]. Furthermore, organizational culture can affect nurses’ self-confidence in conducting screenings [ 84 ] and our research results revealed that nurses have to prioritize the time used on an appointment between mental health and physical health assessment. Patients with SSD may not have the ability to fill the screening assessment by themself before the appointment [ 45 ] and may require the collaboration with a nurse. Moreover, possibilities of using digital technology [ 85 ] in physical health screening may be underrated.
Trustworthiness
We reflected on the trustworthiness of our study in terms of its credibility, dependability, conformability, and transferability [ 86 , 87 ] as follows. Credibility was confirmed by selecting the context and participants who had different experiences of the topic. By using focus groups and individual interviews in the data gathering, we gained knowledge of various experiences, which increased the possibility of shedding light on the research question from a variety of perspectives [ 40 ]. Credibility was further strengthened through presenting the coding process by illustrating how the meaning units from the interviews, extracted codes and categories were produced. The similarities and differences of the research findings are shown with representative quotations from the transcribed text. Dependability was improved through open dialogue among the authors and consistently during the data collection by asking all of the participants similar questions [ 63 ]. Conformability was achieved by reporting the research steps carefully. Transferability was increased by presenting a clear and distinct description of the context, recruitment and characteristics of the participants and of the data collection and data analysis.
Study strengths and limitations
The current study has some limitations that potentially impact the trustworthiness and transferability of the findings. Participants were recruited by a purposive sampling method, which likely caused bias by recruiting those more interested in discussing the topic [ 88 , 89 ]. Although nurses were trained to understand the meaning of specific inclusion and exclusion criteria for the patients, selection bias may still have occurred in the patient recruitment process and patient data may be biased toward those patients who are more motivated, capable and collaborative to join initiatives. All patient participants were diagnosed with a psychotic disorder (F20–29), but the sample size was relatively small and might limit the transferability of the findings to patients with SSD. Similarly, participants were recruited in one hospital only and due to their narrow ethnic background group, this may also may reduce the transferability of the findings outside Finland.
The qualitative study design itself might have imposed some limitations in several phases during the study. The researcher’s presence during the interviews may have affected the subjects’ responses, even if this is often unavoidable in qualitative research [ 88 , 90 ]. The researcher conducting the interviews had a deep understanding of the research topic based on her experience in working with persons with SSD. At the same time, having strong pre-assumptions may have caused bias due to a lack of openness to the topic, hence reducing the credibility. Furthermore, it is possible that the short duration of interviews limits the depth of understanding of the topic. Similarly, the small number of nurse participants in some of the focus groups is likely to have limited the potential for productive group discussion. Even though the interviews were conducted individually with patients, it is possible that the patients were hesitant to openly share their views to a person who represents a staff member. Moreover, the transcripts of the digitally recorded interviews were not returned to nurses or patient participants, so member checking of transcripts and categories was not carried out. Formal backtranslation was not conducted for the data, which might also decrease the credibility of the results. Regardless of these limitations, the study has some strengths and consists of rich and informative data regarding the perceptions of nurses and patients.
Our study results offer a novel diversity of perceptions from nurses and patients toward physical health screening in mental health settings. Patients with schizophrenia spectrum disorders are willing to participate in physical health screening. Although nurses found the HIP-F to be too long, they showed interest in assessing their patients’ physical health and suggested improvements to develop screening to improve its feasibility in clinical practice. Physical health screening should be clear, easy to use and relatively quick. Developing and improving health screening to better suit clinical practice, for example in their length, would further support professionals in conducting and encouraging patients to participate in physical health screening. With this detailed knowledge of perceptions of screening, further research is needed to understand what factors affect the implementation fidelity of physical health screening in clinical mental health practice and to gain an overall understanding on how to improve such implementation.
Implications
Several studies have emphasized the position of nurses in the assessment of physical health [ 28 , 68 , 73 ]. In order for patients to benefit from the results of physical health assessments in clinical practice, it is crucial that the treatment guidelines are followed, assessment results are available in patient record systems and actions are completed according to health promotion plans. Our findings can be used in supporting professionals to collaborate with patients to participate in physical health screening. Our results are also useful in planning curriculums in nursing education and clinical settings. Finally, our results should encourage nurses to implement regular physical health screenings for patients with SSD followed by appropriate effective health promotion interventions. For effective physical health screening and preventing physical comorbidity and premature deaths, the perceptions explored in our study can be taken into consideration by those who develop screening procedures and health screenings for clinical practice.
Data availability
Data generated during and/or analyzed during the study are not publicly available due to ethical restrictions and privacy.
Abbreviations
Body mass index
Chinese Health Improvement Profile
consolidated criteria for reporting qualitative studies
Coronavirus
electrocardiogram
Health improvement profile
Finnish health improvement profile
human immunodeficiency virus
Helsinki University Hospital
10th revision of the International Classification of Diseases and Related Health Problems
Metabolic Syndrome Screening Tool
metabolic syndrome
Nursing Research Center
The physical health check
Doctorate of Philosophy
quality improvement
randomized controlled trial
Standard deviation
schizophrenia spectrum disorder
World Health Organization. Available: https://www.who.int/news-room/fact-sheets/detail/schizophrenia Accessed 12th March 2023.
Filik R, Sipos A, Kehoe P, et al. Cardiovascular and respiratory health of people with schizophrenia. Acta Psychiatrica Scandinavica. 2006;113:298–305.
Article CAS PubMed Google Scholar
Grover S, Aggarwal M, Dutt A, Chakrabarti S, Avasthi A, Kulhara P, Chauhan N. Prevalence of metabolic syndrome in patients with schizophrenia in India. Psychiatry Res. 2012;200(2–3):1035–7.
Article PubMed Google Scholar
Larsen JR, Svensson CK, Vedtofte L, Jakobsen ML, Jespersen HS, Jakobsen MI, Holst JJ. High prevalence of prediabetes and metabolic abnormalities in overweight or obese schizophrenia patients treated with clozapine or olanzapine. CNS Spectr. 2018;31:1–12.
Google Scholar
Hägg S, Lindblom Y, Mjörndal T, Adolfsson R. High prevalence of the metabolic syndrome among a Swedish cohort of patients with schizophrenia. Int Clin Psychopharmacol. 2006;21(2):93–8.
Dickerson FB, Brown CH, Daumit GL, LiJuan F, Goldberg RW, Wohlheiter K, Dixon LB. Health status of individuals with serious mental illness. Schizophr Bull. 2006;32(3):584–9.
Article PubMed PubMed Central Google Scholar
Hughes E, Bassi S, Gilbody S, et al. Prevalence of HIV, hepatitisB, and hepatitis C in people with severe mental illness: asystematic review and meta-analysis. Lancet Psychiatry. 2016;3:40–488.
Taquet M, Luciano S, Geddes JR, et al. Bidirectional associa-tions between COVID-19 and psychiatric disorder: retrospec-tive cohort studies of 62354 COVID-19 cases in the USA. Lancet Psychiatry. 2020;8:130–1409.
Šprah L, Dernovšek MZ, Wahlbeck K, Haaramo P. Psychiatric readmissions and their association with physical comorbidity: a systematic literature review. BMC Psychiatry. 2017;17:1–17.
Article Google Scholar
Schizophrenia. Current Care Guidelines. Working group set up by the Finnish Medical Society Duodecim and the Finnish Psychiatric Association. Helsinki: the Finnish Medical Society Duodecim, 2023 (referred February 9, 2023). Available online at: www.kaypahoito.fi Accessed 8th December 2022.
Olfson M, Gerhard T, Huang C, et al. Premature mortalityamong adults with schizophrenia in the United States. JAMAPsychiatry. 2015;72:1172–11813.
Saha S, Chant D, McGrath J. A systematic review of mortalityin schizophrenia: is the differential mortality gap worseningover time? Arch Gen Psychiatry. 2007;64:1123–11314.
American Psychiatric Association. Practice guideline for the treatment of patients with schizophrenia. Am J Psychiatry. 2004;161(2):1–57.
Department of Health, & Great Britain. Dept. of Health. (2006). Our health, our care, our say: A new direction for community services (Vol. 6737). The Stationery Office.
National Institute for Health and Care Excellence. Psychosis and Schizophrenia in adults: Treatment and Management (NICE Clinical Guideline 178). NICE, 2014. https://www.nice.org.uk/guidance/cg178 Accessed 8th January 2023.
Taylor DM, Barnes TR, Young AH. The Maudsley prescribing guidelines in psychiatry. Wiley; 2021.
Lamontagne-Godwin F, Burgess C, Clement S, Gasston-Hales M, Greene C, Manyande A, Barley E. (2018). Interventions to increase access to or uptake of physical health screening in people with severe mental illness: a realist review. BMJ open, 8(2), e019412.
Phelan M, Stradins L, Amin D, Isadore R, Hitrov C, Doyle A, Inglis R. The physical health check: a tool for mental health workers. J Mental Health. 2004;13(3):277–85.
Vasudev K, Thakkar PB, Mitcheson N. (2012). Physical health of patients with severe mental illness: an intervention on medium secure forensic unit. Int J Health care Qual Assur.
Yeomans D, Dale K, Beedle K. Systematic computerized cardiovascular health screening for people with severe mental illness. Psychiatric Bull. 2014;38(6):280–4.
Brunero S, Lamont S. Systematic screening for metabolic syndrome in consumers with severe mental illness. Int J Ment Health Nurs. 2009;18(2):144–50.
Castillo EG, Rosati J, Williams C, Pessin N, Lindy DC. Metabolic syndrome screening and assertive community treatment: a quality improvement study. J Am Psychiatr Nurses Assoc. 2015;21(4):233–43.
Hardy S, White J, Gray R. The Health Improvement Profile: a manual to promote physical wellbeing in people with severe mental illness. M&K Update Ltd; 2015.
McGinty EE, Baller J, Azrin ST, et al. Quality of medical carefor persons with serious mental illness: a comprehensive review. Schizophr Res. 2015;165:227–23511.
Ilyas A, Chesney E, Patel R. Improving life expectancy in people with serious mental illness: should we place more emphasis on primary prevention? Br J Psychiatry. 2017;211(4):194–7.
Vancampfort D, Watkins A, Ward PB, Probst M, De Hert M, Van Damme T, Mugisha J. Barriers, attitudes, confidence, and knowledge of nurses regarding metabolic health screening and intervention in people with mental illness: a pilot study from Uganda. Afr Health Sci. 2019;19(3):2546–54.
Voort NTVD, Klaessen NC, Poslawsky IE, van Meijel B. (2022). Mental Health nurses’ perceptions of their role in physical screening and lifestyle coaching for patients with a severe Mental illness: a qualitative study. J Am Psychiatr Nurses Assoc, 10783903221085596.
Happell B, Scott D, Nankivell J, Platania-Phung C. Screening physical health? Yes! But… nurses’ views on physical health screening in mental health care. J Clin Nurs. 2013;22(15–16):2286–97.
Mwebe H. Physical health monitoring in mental health settings: a study exploring mental health nurses’ views of their role. J Clin Nurs. 2017;26(19–20):3067–78.
Butler J, de Cassan S, Turner P, Lennox B, Hayward G, Glogowska M. Attitudes to physical healthcare in severe mental illness; a patient and mental health clinician qualitative interview study. BMC Fam Pract. 2020;21:1–8.
Bressington D, Mui J, Wells H, Chien WT, Lam C, White J, Gray R. Refocusing on physical health: Community psychiatric nurses’ perceptions of using enhanced health checks for people with severe mental illness. Int J Ment Health Nurs. 2016;25(3):214–24.
White J, Gray R, Jones M. The development of the serious mental illness physical Health Improvement Profile. J Psychiatr Ment Health Nurs. 2009;16(5):493–8.
Hardy S, Deane K, Gray R. The Northampton Physical Health and Wellbeing Project: the views of patients with severe mental illness about their physical health check. Mental Health Family Med. 2012;9(4):233.
Bressington D, Chien WT, Mui J, Lam KKC, Mahfoud Z, White J, Gray R. The Chinese health improvement profile (CHIP) for people with severe mental illness: a cluster randomized controlled trial. Int J Ment Health Nurs. 2018;27:841–85.
Thongsai S, Gray R, Bressington D. The physical health of people with schizophrenia in Asia: baseline findings from a physical health check programme. J Psychiatr Ment Health Nurs. 2016;23(5):255–66.
White J, Lucas J, Swift L, Barton GR, Johnson H, Irvine L, Gray RJ. Nurse-facilitated health checks for persons with severe mental illness: a cluster-randomized controlled trial. Psychiatric Serv. 2018;69(5):601–4.
Werkkala C, Välimäki M, Anttila M, Pekurinen V, Bressington D. Validation of the Finnish Health Improvement Profile (HIP) with patients with severe mental illness. BMC Psychiatry. 2020;20(1):1–15.
Fleuren MAH, Wiefferink CH, Paulussen TGWM. Determinants of innovation within health care organizations: literature review and Delphi-study. Int J Qual Health Care. 2004;16:107–23.
Dickens GL, Ion R, Waters C, Atlantis E, Everett B. Mental health nurses’ attitudes, experience, and knowledge regarding routine physical healthcare: systematic, integrative review of studies involving 7,549 nurses working in mental health settings. BMC Nurs. 2019;18:1–21.
Renwick L, Drennan J, Sheridan A, Lyne J, Kinsella A, O’Callaghan E, Clarke M. Disagreement between service-users and clinicians assessment of physical health during early psychosis. Early Interv Psychiat. 2019;13(2):314–7.
Patton MQ. Qualitative Research & Evaluation Methods. 3rd edition. London: SAGE Publications; 2002.
Sandelowski M. Focus on research methods: whatever happened to qualitative description. Res Nurs Health. 2000;23(4):334–40.
Hunter D, McCallum J, Howes D. (2019). Defining exploratory-descriptive qualitative (EDQ) research and considering its application to healthcare. J Nurs Health Care, 4(1).
Morgan DL. Focus groups as qualitative research. Volume 16. Sage; 1996.
Gold JM, Harvey PD. Cognitive deficits in schizophrenia. Psychiatr Clin North Am. 1993;16(2):295–312.
Telford R, Faulkner A. (2004). Learning about service user involvement in mental health research. J Mental Health, 13(6).
Kleiman S. (2004). Phenomenology: to wonder and search for meanings. Nurse Res, 11(4).
Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care. 2007;19(6):349–57.
HUS Psychiatry. 2023. https://www.hus.fi/en/search?q=psychiatry&size=n_20_ Accessed 14th November 2022.
World Health Organization. ICD-10: international statistical classification of diseases and related health problems: tenth revision. 2004. https://apps.who.int/iris/bitstream/handle/10665/42980/9241546530_eng.pdf?sequence=1&isAllowed=y Accessed 16th November 2022.
HUS Psychiatry. 2023. https://www.hus.fi/en/patient/treatments-and-examinations/psychoses Accessed 14th November 2022.
Hennink MM, Kaiser BN, Weber MB. What influences saturation? Estimating sample sizes in focus group research. Qual Health Res. 2019;29(10):1483–96.
Giacomini MK, Cook DJ, Evidence-Based Medicine Working Group. Evidence-Based Medicine Working Group, &. (2000). Users’ guides to the medical literature: XXIII. Qualitative research in health care A. Are the results of the study valid? Jama , 284 (3), 357–362.
Côté L, Turgeon J. Appraising qualitative research articles in medicine and medical education. Med Teach. 2005;27(1):71–5.
Grove. SK, Burns N, Gray. J. 2013. The Practice of Nursing Research; Appraisal, Synthesis, and Generation of Evidence. 7th edition. W.B. Saunders Comp., Philadelphia.
Guest G, Bunce A, Johnson L. How many interviews are enough? An experiment with data saturation and variability. Field Methods. 2006;18(1):59–82.
Gill P, Stewart K, Treasure E, Chadwick B. Methods of data collection in qualitative research: interviews and focus groups. Br Dent J. 2008;204(6):291–5.
Elo S, Kyngäs H. The qualitative content analysis process. J Adv Nurs. 2008;62(1):107–15.
Krueger RA. Focus groups: a practical guide for applied research. Sage; 2014.
Maharaj N. Using field notes to facilitate critical reflection. Reflective Pract. 2016;17(2):114–24.
Malterud K, Siersma VD, Guassora AD. Sample size in qualitative interview studies: guided by information power. Qual Health Res. 2016;26(13):1753–60.
Green J, Thorogood N. (2004). Qualitative Research Methods.
Vaismoradi M, Turunen H, Bondas T. Content analysis and thematic analysis: implications for conducting a qualitative descriptive study. Nurs Health Sci. 2013;15(3):398–405.
Lambert SD, Loiselle CG. Combining individual interviews and focus groups to enhance data richness. J Adv Nurs. 2008;62(2):228–37.
Graneheim UH, Lundman B. Qualitative content analysis in nursing research: concepts, procedures and measures to achieve trustworthiness. Nurse Educ Today. 2004;24(2):105–12.
Polit DF, Beck CT. Nursing research: principles and methods. Lippincott Williams & Wilkins; 2004.
Lincoln Y. S., Guba E. G. However, is it rigorous? Trustworthiness and authenticity in naturalistic evaluation. New Dir Program Evaluation. 1986;1986(30):73–84.
Happell B, PLATANIA-PHUNG C, Gray R, Hardy S, Lambert T, McAllister M, Davies C. A role for mental health nursing in the physical health care of consumers with severe mental illness. J Psychiatr Ment Health Nurs. 2011;18(8):706–11.
Shuel F, White J, Jones M, Gray R. Using the serious mental illness health improvement profile [HIP] to identify physical problems in a cohort of community patients: a pragmatic case series evaluation. Int J Nurs Stud. 2010;47(2):136–45.
Brunero S, Lamont S. Health behavior beliefs and physical health risk factors for cardiovascular disease in an outpatient sample of consumers with a severe mental illness: a cross-sectional survey. Int J Nurs Stud. 2010;47(6):753–60.
Campion G, Francis V, Preston A, Wallis A, Lincoln N. Health behavior and motivation to change. Mental Health Nurs. 2005;25(6):12.
Çelik Ince S, Partlak Günüşen N, Serçe Ö. The opinions of Turkish mental health nurses on physical health care for individuals with mental illness: a qualitative study. J Psychiatr Ment Health Nurs. 2018;25(4):245–57.
Blanner Kristiansen C, Juel A, Vinther Hansen M, Hansen AM, Kilian R, Hjorth P. Promoting physical health in severe mental illness: patient and staff perspective. Acta Psychiatrica Scandinavica. 2015;132(6):470–8.
Kaltiala-Heino R, Välimäki M, Korkeila J, Tuohimäki C, Lehtinen V. Involuntary medication in psychiatric inpatient treatment. Eur Psychiatry. 2003;18(6):290–5.
de Leon J, Verghese C, Tracy JI, Josiassen RC, Simpson GM. Polydipsia and water intoxication in psychiatric patients: a review of the epidemiological literature. Biol Psychiatry. 1994;35(6):408–19.
Graham KL, Carson CM, Ezeoke A, Buckley PF, Miller BJ. Urinary tract infections in acute psychosis. J Clin Psychiatry. 2014;75(4):21977.
Miller BJ, Graham KL, Bodenheimer CM, Culpepper NH, Waller JL, Buckley PF. A prevalence study of urinary tract infections in acute relapse of schizophrenia. J Clin Psychiatry. 2013;74(3):15503.
Warnier RMJ, van Rossum E, Du Moulin MFMT, van Lottum M, Schols JMGA, Kempen GIJM. The opinions and experiences of nurses on frailty screening among older hospitalized patients. An exploratory study. BMC Geriatr. 2021;21(1):624. https://doi.org/10.1186/s12877-021-02586-z . PMID: 34732153; PMCID: PMC8565044.
Happell B, Platania-Phung C. Cardiovascular health promotion and consumers with mental illness in Australia. Issues Ment Health Nurs. 2015;36(4):286–93.
Robson D, Haddad M, Gray R, Gournay K. Mental health nursing and physical health care: a cross-sectional study of nurses’ attitudes, practice, and perceived training needs for the physical health care of people with severe mental illness. Int J Ment Health Nurs. 2013;22(5):409–17. https://doi.org/10.1111/j.1447-0349.2012.00883.x .
Quinn C, Platania-Phung C, Bale C, Happell B, Hughes E. Understanding the current sexual health service provision for mental health consumers by nurses in mental health settings: findings from a survey in Australia and England. Int J Ment Health Nurs. 2018;27(5):1522–34.
Quinn C, Happell B, Browne G. Opportunity lost? Psychiatric medications and problems with sexual function: a role for nurses in mental health. J Clin Nurs. 2012;21(3–4):415–23.
Blythe J, White J. Role of the mental health nurse toward physical health care in serious mental illness: an integrative review of 10 years of UK literature. Int J Ment Health Nurs. 2012;21(3):193–201.
Tzeng WC, Su PY, Yeh SH, Chang TW, Lin CH, Feng HP. Nurses’ views on the provision of physical healthcare for individuals with comorbid mental illness and chronic disease. Int J Ment Health Nurs. 2023;32(1):199–211. https://doi.org/10.1111/inm.13076 . Epub 2022 Oct 2. PMID: 36184847.
Chivilgina O, Elger BS, Jotterand F. Digital Technologies for Schizophrenia Management: a descriptive review. Sci Eng Ethics. 2021;27:1–22.
Polit DF, Beck CT, Polit F. Cheryl Tatano Beck-Details-Trove; Wolters Kluwer Health/Lippincott Williams & Wilkins: Philadelphia, PA, USA, 2010; 301–7.
Stalmeijer RE, McNaughton N, Van Mook WNKA. Using focus groups in medical education research: AMEE Guide 91. Med Teach. 2014;36:923–39. [CrossRef].
Firth J, Rosenbaum S, Stubbs B, Gorczynski P, Yung AR, Vancampfort D. Motivating factors and barriers toward exercise in severe mental illness: a systematic review and meta-analysis. Psychol Med. 2016;46(14):2869–81.
Mulder CL, Jochems E, Kortrijk HE. The motivation paradox: higher psychosocial problem levels in severely mentally ill patients are associated with less motivation for treatment. Soc Psychiatry Psychiatr Epidemiol. 2014;49(4):541–8.
Schonfeld IS, Mazzola JJ. Strengths and limitations of qualitative approaches to research in occupational health psychology1. In Research methods in occupational health psychology. Routledge. 2012. pp. 268–289.
PubMed Central Google Scholar
FINLEX 523/1999. Finnish Personal Data Act. Ministry of Social Affairs and Health, Finland. 2001. https://www.finlex.fi/fi/laki/kaannokset/1999/en19990523.pdf . Accessed 28 Jan 2023.
World Medical Associationon. World medical association declaration of Helsinki. Ethical principles for medical research involving human subjects. Bull World Health Organ. 2001;9(4):373.
Download references
Acknowledgements
We would like to thank all patients and nurses for their indispensable assistance in conducting this research.
Helsinki University Hospitals (HUH) Nursing Research Center (NRC) and HUH Funding, Psychiatry supported this study by granting a paid research period for the first author (CL).
Author information
Authors and affiliations.
University of Turku, Faculty of Medicine, Department of Nursing, Kiinamyllynkatu 10, Medisiina B, Turku, 20520, Finland
Långstedt Camilla & Välimäki Maritta
Professor in Mental Health, Faculty of Health, Charles Darwin University, Casuarina, Australia
Bressington Daniel
Faculty of Nursing, Chiang Mai University, 110/406 Inthawaroros Road, Sri Phum District, Chiang Mai, Thailand
University of Helsinki, School of Public Health, Helsinki, Finland
Välimäki Maritta
You can also search for this author in PubMed Google Scholar
Contributions
CL designed the study, collected the data, contributed to data input, analyzed the data, and contributed to the writing of the manuscript and all tables. MV led the study design, data analysis, and writing of the manuscript. DB contributed to the study design, the data analysis, and writing of the final manuscript. All the authors have read and approved the final manuscript.
Corresponding author
Correspondence to Långstedt Camilla .
Ethics declarations
Ethics approval and consent to participate.
The study was approved by the ethical committee (HUH/1556/2021) of the Helsinki University Hospital, and permission to conduct the study was obtained (HUH/153/2021) from the research organization. All participants received oral and written information about the study. All participants gave their written informed consent to participate. During the study, ethical principles regarding self-determination, harm avoidance, privacy and data protection and ethical considerations were considered and all methods were performed in accordance with the Declaration of Helsinki [ 89 , 90 , 91 , 92 ]. Confidentiality in reporting results was ensured by using codes instead of names in the quotations (e.g., nurse N1 and patient P1)
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Camilla, L., Daniel, B. & Maritta, V. Nurses’ and patients’ perceptions of physical health screening for patients with schizophrenia spectrum disorders: a qualitative study. BMC Nurs 23 , 321 (2024). https://doi.org/10.1186/s12912-024-01980-3
Download citation
Received : 11 September 2023
Accepted : 26 April 2024
Published : 11 May 2024
DOI : https://doi.org/10.1186/s12912-024-01980-3
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Schizophrenia spectrum disorder
- Severe mental illness
- Physical health
- Focus group
- Qualitative
BMC Nursing
ISSN: 1472-6955
- General enquiries: [email protected]
The role practice approach for exercise and enhancement of nursing research capacity: A qualitative study
Affiliations.
- 1 School of Nursing, Jinan University, Guangzhou, China.
- 2 Department of Nursing, Guangzhou Red Cross Hospital, Guangzhou, China.
- 3 School of Nursing, Jinan University, Guangzhou, China. Electronic address: [email protected].
- PMID: 37591112
- DOI: 10.1016/j.nedt.2023.105926
Background: Strategies to improve the teaching effectiveness of nursing research courses are a fundamental objective of contemporary nursing educators. The role practice method is the sum of ways, means, and procedures used to perform role-specific practical learning activities through the adaptation of concepts, models and subjective abilities in an authentic environment. This technique enhances teaching effectiveness by encouraging students to actively participate in practice.
Objective: The main aim of this study was to explore the effectiveness of the role practice approach within the framework of nursing research courses and provide guidance for subsequent teaching efforts.
Methods: The purposive sampling method was used to recruit 16 students who participated in teaching of the role practice approach and completed all tasks set within the nursing research course in the third year of the undergraduate nursing program of a comprehensive university in south China. Data obtained from semi-structured interviews were analyzed using Colaizzi's seven-step analysis method.
Results: Three themes were evaluated, specifically, self-improvement, self-inadequacy and course optimization.
Conclusion: The role practice method is effective in teaching nursing research courses and can enhance the ability of students to conduct research activities. However, deficiencies in the implementation plan exist that need further revision.
Keywords: Nursing education; Nursing research; Qualitative research; Role practice.
Copyright © 2023. Published by Elsevier Ltd.
- Education, Nursing, Baccalaureate*
- Nursing Research*
- Qualitative Research
- Students, Nursing*
An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.

StatPearls [Internet].
Qualitative study.
Steven Tenny ; Janelle M. Brannan ; Grace D. Brannan .
Affiliations
Last Update: September 18, 2022 .
- Introduction
Qualitative research is a type of research that explores and provides deeper insights into real-world problems. [1] Instead of collecting numerical data points or intervene or introduce treatments just like in quantitative research, qualitative research helps generate hypotheses as well as further investigate and understand quantitative data. Qualitative research gathers participants' experiences, perceptions, and behavior. It answers the hows and whys instead of how many or how much. It could be structured as a stand-alone study, purely relying on qualitative data or it could be part of mixed-methods research that combines qualitative and quantitative data. This review introduces the readers to some basic concepts, definitions, terminology, and application of qualitative research.
Qualitative research at its core, ask open-ended questions whose answers are not easily put into numbers such as ‘how’ and ‘why’. [2] Due to the open-ended nature of the research questions at hand, qualitative research design is often not linear in the same way quantitative design is. [2] One of the strengths of qualitative research is its ability to explain processes and patterns of human behavior that can be difficult to quantify. [3] Phenomena such as experiences, attitudes, and behaviors can be difficult to accurately capture quantitatively, whereas a qualitative approach allows participants themselves to explain how, why, or what they were thinking, feeling, and experiencing at a certain time or during an event of interest. Quantifying qualitative data certainly is possible, but at its core, qualitative data is looking for themes and patterns that can be difficult to quantify and it is important to ensure that the context and narrative of qualitative work are not lost by trying to quantify something that is not meant to be quantified.
However, while qualitative research is sometimes placed in opposition to quantitative research, where they are necessarily opposites and therefore ‘compete’ against each other and the philosophical paradigms associated with each, qualitative and quantitative work are not necessarily opposites nor are they incompatible. [4] While qualitative and quantitative approaches are different, they are not necessarily opposites, and they are certainly not mutually exclusive. For instance, qualitative research can help expand and deepen understanding of data or results obtained from quantitative analysis. For example, say a quantitative analysis has determined that there is a correlation between length of stay and level of patient satisfaction, but why does this correlation exist? This dual-focus scenario shows one way in which qualitative and quantitative research could be integrated together.
Examples of Qualitative Research Approaches
Ethnography
Ethnography as a research design has its origins in social and cultural anthropology, and involves the researcher being directly immersed in the participant’s environment. [2] Through this immersion, the ethnographer can use a variety of data collection techniques with the aim of being able to produce a comprehensive account of the social phenomena that occurred during the research period. [2] That is to say, the researcher’s aim with ethnography is to immerse themselves into the research population and come out of it with accounts of actions, behaviors, events, etc. through the eyes of someone involved in the population. Direct involvement of the researcher with the target population is one benefit of ethnographic research because it can then be possible to find data that is otherwise very difficult to extract and record.
Grounded Theory
Grounded Theory is the “generation of a theoretical model through the experience of observing a study population and developing a comparative analysis of their speech and behavior.” [5] As opposed to quantitative research which is deductive and tests or verifies an existing theory, grounded theory research is inductive and therefore lends itself to research that is aiming to study social interactions or experiences. [3] [2] In essence, Grounded Theory’s goal is to explain for example how and why an event occurs or how and why people might behave a certain way. Through observing the population, a researcher using the Grounded Theory approach can then develop a theory to explain the phenomena of interest.
Phenomenology
Phenomenology is defined as the “study of the meaning of phenomena or the study of the particular”. [5] At first glance, it might seem that Grounded Theory and Phenomenology are quite similar, but upon careful examination, the differences can be seen. At its core, phenomenology looks to investigate experiences from the perspective of the individual. [2] Phenomenology is essentially looking into the ‘lived experiences’ of the participants and aims to examine how and why participants behaved a certain way, from their perspective . Herein lies one of the main differences between Grounded Theory and Phenomenology. Grounded Theory aims to develop a theory for social phenomena through an examination of various data sources whereas Phenomenology focuses on describing and explaining an event or phenomena from the perspective of those who have experienced it.
Narrative Research
One of qualitative research’s strengths lies in its ability to tell a story, often from the perspective of those directly involved in it. Reporting on qualitative research involves including details and descriptions of the setting involved and quotes from participants. This detail is called ‘thick’ or ‘rich’ description and is a strength of qualitative research. Narrative research is rife with the possibilities of ‘thick’ description as this approach weaves together a sequence of events, usually from just one or two individuals, in the hopes of creating a cohesive story, or narrative. [2] While it might seem like a waste of time to focus on such a specific, individual level, understanding one or two people’s narratives for an event or phenomenon can help to inform researchers about the influences that helped shape that narrative. The tension or conflict of differing narratives can be “opportunities for innovation”. [2]
Research Paradigm
Research paradigms are the assumptions, norms, and standards that underpin different approaches to research. Essentially, research paradigms are the ‘worldview’ that inform research. [4] It is valuable for researchers, both qualitative and quantitative, to understand what paradigm they are working within because understanding the theoretical basis of research paradigms allows researchers to understand the strengths and weaknesses of the approach being used and adjust accordingly. Different paradigms have different ontology and epistemologies . Ontology is defined as the "assumptions about the nature of reality” whereas epistemology is defined as the “assumptions about the nature of knowledge” that inform the work researchers do. [2] It is important to understand the ontological and epistemological foundations of the research paradigm researchers are working within to allow for a full understanding of the approach being used and the assumptions that underpin the approach as a whole. Further, it is crucial that researchers understand their own ontological and epistemological assumptions about the world in general because their assumptions about the world will necessarily impact how they interact with research. A discussion of the research paradigm is not complete without describing positivist, postpositivist, and constructivist philosophies.
Positivist vs Postpositivist
To further understand qualitative research, we need to discuss positivist and postpositivist frameworks. Positivism is a philosophy that the scientific method can and should be applied to social as well as natural sciences. [4] Essentially, positivist thinking insists that the social sciences should use natural science methods in its research which stems from positivist ontology that there is an objective reality that exists that is fully independent of our perception of the world as individuals. Quantitative research is rooted in positivist philosophy, which can be seen in the value it places on concepts such as causality, generalizability, and replicability.
Conversely, postpositivists argue that social reality can never be one hundred percent explained but it could be approximated. [4] Indeed, qualitative researchers have been insisting that there are “fundamental limits to the extent to which the methods and procedures of the natural sciences could be applied to the social world” and therefore postpositivist philosophy is often associated with qualitative research. [4] An example of positivist versus postpositivist values in research might be that positivist philosophies value hypothesis-testing, whereas postpositivist philosophies value the ability to formulate a substantive theory.
Constructivist
Constructivism is a subcategory of postpositivism. Most researchers invested in postpositivist research are constructivist as well, meaning they think there is no objective external reality that exists but rather that reality is constructed. Constructivism is a theoretical lens that emphasizes the dynamic nature of our world. “Constructivism contends that individuals’ views are directly influenced by their experiences, and it is these individual experiences and views that shape their perspective of reality”. [6] Essentially, Constructivist thought focuses on how ‘reality’ is not a fixed certainty and experiences, interactions, and backgrounds give people a unique view of the world. Constructivism contends, unlike in positivist views, that there is not necessarily an ‘objective’ reality we all experience. This is the ‘relativist’ ontological view that reality and the world we live in are dynamic and socially constructed. Therefore, qualitative scientific knowledge can be inductive as well as deductive.” [4]
So why is it important to understand the differences in assumptions that different philosophies and approaches to research have? Fundamentally, the assumptions underpinning the research tools a researcher selects provide an overall base for the assumptions the rest of the research will have and can even change the role of the researcher themselves. [2] For example, is the researcher an ‘objective’ observer such as in positivist quantitative work? Or is the researcher an active participant in the research itself, as in postpositivist qualitative work? Understanding the philosophical base of the research undertaken allows researchers to fully understand the implications of their work and their role within the research, as well as reflect on their own positionality and bias as it pertains to the research they are conducting.
Data Sampling
The better the sample represents the intended study population, the more likely the researcher is to encompass the varying factors at play. The following are examples of participant sampling and selection: [7]
- Purposive sampling- selection based on the researcher’s rationale in terms of being the most informative.
- Criterion sampling-selection based on pre-identified factors.
- Convenience sampling- selection based on availability.
- Snowball sampling- the selection is by referral from other participants or people who know potential participants.
- Extreme case sampling- targeted selection of rare cases.
- Typical case sampling-selection based on regular or average participants.
Data Collection and Analysis
Qualitative research uses several techniques including interviews, focus groups, and observation. [1] [2] [3] Interviews may be unstructured, with open-ended questions on a topic and the interviewer adapts to the responses. Structured interviews have a predetermined number of questions that every participant is asked. It is usually one on one and is appropriate for sensitive topics or topics needing an in-depth exploration. Focus groups are often held with 8-12 target participants and are used when group dynamics and collective views on a topic are desired. Researchers can be a participant-observer to share the experiences of the subject or a non-participant or detached observer.
While quantitative research design prescribes a controlled environment for data collection, qualitative data collection may be in a central location or in the environment of the participants, depending on the study goals and design. Qualitative research could amount to a large amount of data. Data is transcribed which may then be coded manually or with the use of Computer Assisted Qualitative Data Analysis Software or CAQDAS such as ATLAS.ti or NVivo. [8] [9] [10]
After the coding process, qualitative research results could be in various formats. It could be a synthesis and interpretation presented with excerpts from the data. [11] Results also could be in the form of themes and theory or model development.
Dissemination
To standardize and facilitate the dissemination of qualitative research outcomes, the healthcare team can use two reporting standards. The Consolidated Criteria for Reporting Qualitative Research or COREQ is a 32-item checklist for interviews and focus groups. [12] The Standards for Reporting Qualitative Research (SRQR) is a checklist covering a wider range of qualitative research. [13]
Examples of Application
Many times a research question will start with qualitative research. The qualitative research will help generate the research hypothesis which can be tested with quantitative methods. After the data is collected and analyzed with quantitative methods, a set of qualitative methods can be used to dive deeper into the data for a better understanding of what the numbers truly mean and their implications. The qualitative methods can then help clarify the quantitative data and also help refine the hypothesis for future research. Furthermore, with qualitative research researchers can explore subjects that are poorly studied with quantitative methods. These include opinions, individual's actions, and social science research.
A good qualitative study design starts with a goal or objective. This should be clearly defined or stated. The target population needs to be specified. A method for obtaining information from the study population must be carefully detailed to ensure there are no omissions of part of the target population. A proper collection method should be selected which will help obtain the desired information without overly limiting the collected data because many times, the information sought is not well compartmentalized or obtained. Finally, the design should ensure adequate methods for analyzing the data. An example may help better clarify some of the various aspects of qualitative research.
A researcher wants to decrease the number of teenagers who smoke in their community. The researcher could begin by asking current teen smokers why they started smoking through structured or unstructured interviews (qualitative research). The researcher can also get together a group of current teenage smokers and conduct a focus group to help brainstorm factors that may have prevented them from starting to smoke (qualitative research).
In this example, the researcher has used qualitative research methods (interviews and focus groups) to generate a list of ideas of both why teens start to smoke as well as factors that may have prevented them from starting to smoke. Next, the researcher compiles this data. The research found that, hypothetically, peer pressure, health issues, cost, being considered “cool,” and rebellious behavior all might increase or decrease the likelihood of teens starting to smoke.
The researcher creates a survey asking teen participants to rank how important each of the above factors is in either starting smoking (for current smokers) or not smoking (for current non-smokers). This survey provides specific numbers (ranked importance of each factor) and is thus a quantitative research tool.
The researcher can use the results of the survey to focus efforts on the one or two highest-ranked factors. Let us say the researcher found that health was the major factor that keeps teens from starting to smoke, and peer pressure was the major factor that contributed to teens to start smoking. The researcher can go back to qualitative research methods to dive deeper into each of these for more information. The researcher wants to focus on how to keep teens from starting to smoke, so they focus on the peer pressure aspect.
The researcher can conduct interviews and/or focus groups (qualitative research) about what types and forms of peer pressure are commonly encountered, where the peer pressure comes from, and where smoking first starts. The researcher hypothetically finds that peer pressure often occurs after school at the local teen hangouts, mostly the local park. The researcher also hypothetically finds that peer pressure comes from older, current smokers who provide the cigarettes.
The researcher could further explore this observation made at the local teen hangouts (qualitative research) and take notes regarding who is smoking, who is not, and what observable factors are at play for peer pressure of smoking. The researcher finds a local park where many local teenagers hang out and see that a shady, overgrown area of the park is where the smokers tend to hang out. The researcher notes the smoking teenagers buy their cigarettes from a local convenience store adjacent to the park where the clerk does not check identification before selling cigarettes. These observations fall under qualitative research.
If the researcher returns to the park and counts how many individuals smoke in each region of the park, this numerical data would be quantitative research. Based on the researcher's efforts thus far, they conclude that local teen smoking and teenagers who start to smoke may decrease if there are fewer overgrown areas of the park and the local convenience store does not sell cigarettes to underage individuals.
The researcher could try to have the parks department reassess the shady areas to make them less conducive to the smokers or identify how to limit the sales of cigarettes to underage individuals by the convenience store. The researcher would then cycle back to qualitative methods of asking at-risk population their perceptions of the changes, what factors are still at play, as well as quantitative research that includes teen smoking rates in the community, the incidence of new teen smokers, among others. [14] [15]
Qualitative research functions as a standalone research design or in combination with quantitative research to enhance our understanding of the world. Qualitative research uses techniques including structured and unstructured interviews, focus groups, and participant observation to not only help generate hypotheses which can be more rigorously tested with quantitative research but also to help researchers delve deeper into the quantitative research numbers, understand what they mean, and understand what the implications are. Qualitative research provides researchers with a way to understand what is going on, especially when things are not easily categorized. [16]
- Issues of Concern
As discussed in the sections above, quantitative and qualitative work differ in many different ways, including the criteria for evaluating them. There are four well-established criteria for evaluating quantitative data: internal validity, external validity, reliability, and objectivity. The correlating concepts in qualitative research are credibility, transferability, dependability, and confirmability. [4] [11] The corresponding quantitative and qualitative concepts can be seen below, with the quantitative concept is on the left, and the qualitative concept is on the right:
- Internal validity--- Credibility
- External validity---Transferability
- Reliability---Dependability
- Objectivity---Confirmability
In conducting qualitative research, ensuring these concepts are satisfied and well thought out can mitigate potential issues from arising. For example, just as a researcher will ensure that their quantitative study is internally valid so should qualitative researchers ensure that their work has credibility.
Indicators such as triangulation and peer examination can help evaluate the credibility of qualitative work.
- Triangulation: Triangulation involves using multiple methods of data collection to increase the likelihood of getting a reliable and accurate result. In our above magic example, the result would be more reliable by also interviewing the magician, back-stage hand, and the person who "vanished." In qualitative research, triangulation can include using telephone surveys, in-person surveys, focus groups, and interviews as well as surveying an adequate cross-section of the target demographic.
- Peer examination: Results can be reviewed by a peer to ensure the data is consistent with the findings.
‘Thick’ or ‘rich’ description can be used to evaluate the transferability of qualitative research whereas using an indicator such as an audit trail might help with evaluating the dependability and confirmability.
- Thick or rich description is a detailed and thorough description of details, the setting, and quotes from participants in the research. [5] Thick descriptions will include a detailed explanation of how the study was carried out. Thick descriptions are detailed enough to allow readers to draw conclusions and interpret the data themselves, which can help with transferability and replicability.
- Audit trail: An audit trail provides a documented set of steps of how the participants were selected and the data was collected. The original records of information should also be kept (e.g., surveys, notes, recordings).
One issue of concern that qualitative researchers should take into consideration is observation bias. Here are a few examples:
- Hawthorne effect: The Hawthorne effect is the change in participant behavior when they know they are being observed. If a researcher was wanting to identify factors that contribute to employee theft and tells the employees they are going to watch them to see what factors affect employee theft, one would suspect employee behavior would change when they know they are being watched.
- Observer-expectancy effect: Some participants change their behavior or responses to satisfy the researcher's desired effect. This happens in an unconscious manner for the participant so it is important to eliminate or limit transmitting the researcher's views.
- Artificial scenario effect: Some qualitative research occurs in artificial scenarios and/or with preset goals. In such situations, the information may not be accurate because of the artificial nature of the scenario. The preset goals may limit the qualitative information obtained.
- Clinical Significance
Qualitative research by itself or combined with quantitative research helps healthcare providers understand patients and the impact and challenges of the care they deliver. Qualitative research provides an opportunity to generate and refine hypotheses and delve deeper into the data generated by quantitative research. Qualitative research does not exist as an island apart from quantitative research, but as an integral part of research methods to be used for the understanding of the world around us. [17]
- Enhancing Healthcare Team Outcomes
Qualitative research is important for all members of the health care team as all are affected by qualitative research. Qualitative research may help develop a theory or a model for health research that can be further explored by quantitative research. Much of the qualitative research data acquisition is completed by numerous team members including social works, scientists, nurses, etc. Within each area of the medical field, there is copious ongoing qualitative research including physician-patient interactions, nursing-patient interactions, patient-environment interactions, health care team function, patient information delivery, etc.
- Review Questions
- Access free multiple choice questions on this topic.
- Comment on this article.
Disclosure: Steven Tenny declares no relevant financial relationships with ineligible companies.
Disclosure: Janelle Brannan declares no relevant financial relationships with ineligible companies.
Disclosure: Grace Brannan declares no relevant financial relationships with ineligible companies.
This book is distributed under the terms of the Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International (CC BY-NC-ND 4.0) ( http://creativecommons.org/licenses/by-nc-nd/4.0/ ), which permits others to distribute the work, provided that the article is not altered or used commercially. You are not required to obtain permission to distribute this article, provided that you credit the author and journal.
- Cite this Page Tenny S, Brannan JM, Brannan GD. Qualitative Study. [Updated 2022 Sep 18]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.
In this Page
Bulk download.
- Bulk download StatPearls data from FTP
Related information
- PMC PubMed Central citations
- PubMed Links to PubMed
Similar articles in PubMed
- Suicidal Ideation. [StatPearls. 2024] Suicidal Ideation. Harmer B, Lee S, Duong TVH, Saadabadi A. StatPearls. 2024 Jan
- Folic acid supplementation and malaria susceptibility and severity among people taking antifolate antimalarial drugs in endemic areas. [Cochrane Database Syst Rev. 2022] Folic acid supplementation and malaria susceptibility and severity among people taking antifolate antimalarial drugs in endemic areas. Crider K, Williams J, Qi YP, Gutman J, Yeung L, Mai C, Finkelstain J, Mehta S, Pons-Duran C, Menéndez C, et al. Cochrane Database Syst Rev. 2022 Feb 1; 2(2022). Epub 2022 Feb 1.
- Macromolecular crowding: chemistry and physics meet biology (Ascona, Switzerland, 10-14 June 2012). [Phys Biol. 2013] Macromolecular crowding: chemistry and physics meet biology (Ascona, Switzerland, 10-14 June 2012). Foffi G, Pastore A, Piazza F, Temussi PA. Phys Biol. 2013 Aug; 10(4):040301. Epub 2013 Aug 2.
- Review Evidence Brief: The Effectiveness Of Mandatory Computer-Based Trainings On Government Ethics, Workplace Harassment, Or Privacy And Information Security-Related Topics [ 2014] Review Evidence Brief: The Effectiveness Of Mandatory Computer-Based Trainings On Government Ethics, Workplace Harassment, Or Privacy And Information Security-Related Topics Peterson K, McCleery E. 2014 May
- Review Public sector reforms and their impact on the level of corruption: A systematic review. [Campbell Syst Rev. 2021] Review Public sector reforms and their impact on the level of corruption: A systematic review. Mugellini G, Della Bella S, Colagrossi M, Isenring GL, Killias M. Campbell Syst Rev. 2021 Jun; 17(2):e1173. Epub 2021 May 24.
Recent Activity
- Qualitative Study - StatPearls Qualitative Study - StatPearls
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
Connect with NLM
National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894
Web Policies FOIA HHS Vulnerability Disclosure
Help Accessibility Careers

IMAGES
VIDEO
COMMENTS
Significance of Qualitative Research. The qualitative method of inquiry examines the 'how' and 'why' of decision making, rather than the 'when,' 'what,' and 'where.'[] Unlike quantitative methods, the objective of qualitative inquiry is to explore, narrate, and explain the phenomena and make sense of the complex reality.Health interventions, explanatory health models, and medical-social ...
Qualitative research is valuable because it approaches a phenomenon, such as a clinical problem, about which little is known by trying to understand its many facets. Most qualitative research is emergent, holistic, detailed, and uses many strategies to collect data. Qualitative research generates evidence and helps nurses determine patient ...
Introduction. Qualitative descriptive approaches to nursing and healthcare research provide a broad insight into particular phenomena and can be used in a variety of ways including as a standalone research design, as a precursor to larger qualitative studies and commonly as the qualitative component in mixed-methods studies.
Abstract. This paper aims to provide an overview of the use and assessment of qualitative research methods in the health sciences. Qualitative research can be defined as the study of the nature of phenomena and is especially appropriate for answering questions of why something is (not) observed, assessing complex multi-component interventions ...
Global Qualitative Nursing Research. Global Qualitative Nursing Research (GQNR) is an open access, peer-reviewed journal focusing on qualitative research in fields relevant to nursing and other health professionals world-wide. Please see the Aims and Scope tab for further information. View full journal description.
Useful terms. Some of the qualitative approaches used in nursing research include grounded theory, phenomenology, ethnography, case study (can lend itself to mixed methods) and narrative analysis. The data collection methods used in qualitative research include in depth interviews, focus groups, observations and stories in the form of diaries ...
Editor's note: This is the 11th article in a series on clinical research by nurses. The series is designed to give nurses the knowledge and skills they need to participate in research, step by step. Each column will present the concepts that underpin evidence-based practice—from research design to data interpretation.
Qualitative research methods began to appear in nursing in 1960s and 1970s amid cautious and reluctant acceptance. In the 1980s, qualitative health research emerged as a distinctive domain and mode of inquiry. 1 Qualitative research refers to any kind of research that produces findings not arrived at by means of statistical analysis or other means of quantification. 2,3 It uses a naturalistic ...
Good qualitative research uses a systematic and rigorous approach that aims to answer questions concerned with what something is like (such as a patient experience), what people think or feel about something that has happened, and it may address why something has happened as it has. Qualitative data often takes the form of words or text and can include images. Qualitative research covers a ...
Methods and rigor issues underpinning qualitative description research are also appraised to provide the researcher with a systematic approach to conduct research utilizing this approach. The key attributes and value of qualitative description research in the health care professions will be highlighted with the aim of extending its usage.
Longitudinal qualitative research (LQR) is an emerging methodology in health behavior and nursing research—fields focused on generating evidence to support nursing practices as well as programs, and policies promoting healthy behaviors (Glanz et al., 2008; Polit & Beck, 2017).Because human experiences are rarely comprised of concrete, time-limited events, but evolve and change across time ...
The three core approaches to data collection in qualitative research—interviews, focus groups and observation—provide researchers with rich and deep insights. All methods require skill on the part of the researcher, and all produce a large amount of raw data. However, with careful and systematic analysis 12 the data yielded with these ...
Qualitative research also explores personal experiences, often through phenomenological methods. Finally, qualitative research can aid in developing a new theory or expanding an existing theory. An example might be using a theory in a new setting or with a new group to expand the theory beyond the original conception.
Methods refer to the processes by which data are collected in the research study. A research publication should have a methods section that outlines these processes ( Singh, 2016 ). Methodology is the study of how research is done. It is the way we discover about procedures, and the way in which knowledge is gained.
This paper aims to provide an overview of the use and assessment of qualitative research methods in the health sciences. Qualitative research can be defined as the study of the nature of phenomena and is especially appropriate for answering questions of why something is (not) observed, assessing complex multi-component interventions, and focussing on intervention improvement. The most common ...
Qualitative research is critical for studies about regulatory issues in nursing and across all health professions. When in-depth stakeholder perspectives are needed, qualitative approaches are often the best methodological choice to ensure their viewpoints and experiences are captured when evaluating the consequences of policy implementation or when informing regulation design.
Nursing interventions can be evaluated qualitatively, as this method enhances the significance of clinical trials and emphasizes the distinctive work and outcomes of nursing care (Sandelowski, 1996 ). However, there are few examples of detailed methodological strategies for doing so (Schumacher et al., 2005 ).
"Written for nurses and nursing students, Nursing Research: A Qualitative Perspective, Fourth Edition defines qualitative research and presents information on the current state of this important field. Divided into three sections, Part One provides foundational content for understanding the qualitative research process; Part Two presents the more dominant methods, following each with an ...
This methodology, including terminology and concepts, is often invisible in qualitative study titles and abstracts. Case study is an exclusive methodology and an adjunct to exploring particular aspects of phenomena under investigation in larger or mixed-methods studies. A high quality of case study exists in nursing research.
The Journal of Clinical Nursing publishes research and developments relevant to all areas of nursing practice- community, geriatric, mental health, ... All the studies employed a qualitative method with semistructured focus group interviews, semistructured individual interviews (in person and by telephone) or in-depth interviews (Table 4).
As the use of qualitative research methods proliferates throughout health care, and specifically nursing research studies, there is a need for Clinical Nurse Specialists (CNSs) to become informed regarding the potential utility of qualitative research findings in practice. In this column, the questions of what qualitative findings mean, how the ...
S. Thorne et al. (2016) proposed that a "nursing disciplinary epistemology"—yet still evolving—be used in designing qualitative research about nursing (p. 455), and further than nursing itself contains the elements required to create a "credible frame" for applied qualitative research (S. Thorne et al., 2016, p. 458).
Patton MQ. Qualitative Research & Evaluation Methods. 3rd edition. London: SAGE Publications; 2002. Sandelowski M. Focus on research methods: whatever happened to qualitative description. Res Nurs Health. 2000;23(4):334-40. Article CAS PubMed Google Scholar Hunter D, McCallum J, Howes D. (2019).
Purpose: To shed light on and analyse the intersection between logical empiricism and qualitative nursing research, and to emphasize a post-structuralist critique to traditional methodological constraints. Methods: In this study, a critical examination is conducted through a post-structuralist lens, evaluating entrenched methodologies within nursing research. This approach facilitates a ...
Use of this methodology will help to determine how the use of a co-design approach may impact the development of culturally responsive perioperative nursing care for those from ethnically diverse communities. ABSTRACT This article outlines the use of a co-design methodological approach aimed at optimizing perioperative care experiences for ethnically diverse older adults and their family carers.
The definition of mixed methods, from the first issue of the Journal of Mixed Methods Research, is "research in which the investigator collects and analyzes data, integrates the findings, and draws inferences using both qualitative and quantitative approaches or methods in a single study or program of inquiry" ( Tashakkori & Creswell, 2007 ...
Background: Strategies to improve the teaching effectiveness of nursing research courses are a fundamental objective of contemporary nursing educators. The role practice method is the sum of ways, means, and procedures used to perform role-specific practical learning activities through the adaptation of concepts, models and subjective abilities in an authentic environment.
Intended for healthcare professionals. Search this journal; Search all journals; Enter search terms...
Qualitative research is a type of research that explores and provides deeper insights into real-world problems.[1] Instead of collecting numerical data points or intervene or introduce treatments just like in quantitative research, qualitative research helps generate hypotheses as well as further investigate and understand quantitative data. Qualitative research gathers participants ...